Oral Surgery GIL Contents Preop Medical assessment Case





- Slides: 32

Oral Surgery GIL
Contents ● Pre-op ○ ○ ○ Medical assessment Case selection ■ Clinical + Radiographic assessment Consent ● Simple Extractions ● Complex Extractions ● Post-op
Pre-op assessments ● Aim of pre-op assessments: ○ ○ Ensure the exo is safe for the patient Ensure exo is achievable for your level of skill and experience ● Medical assessment ○ ○ Contraindications for extractions Medications/Med treatments that are significant to oral surgery ■ Blood thinning medications ■ Bisphonates ■ Radiotherapy
Contraindications ● Absolute vs Relative ○ definition ● Systemic contraindications ○ ○ Uncontrolled Metabolic diseases Myocardial infarction Lymphoma and leukemia Severe coagulopathy eg. bleeding diathesis ● Local contraindications ○ ○ Radiation zone tumour/cancer Severe infections Severe abscess
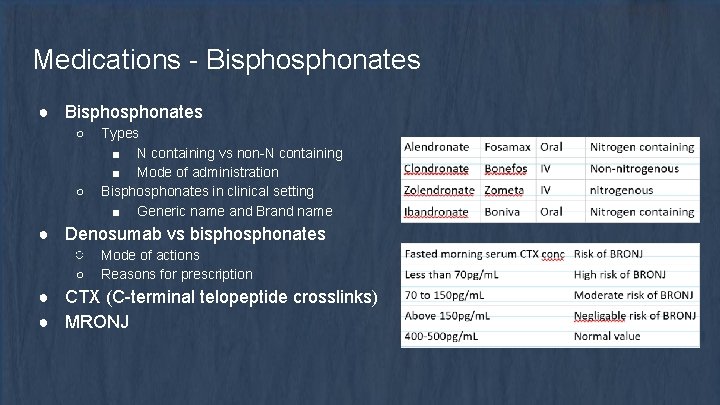
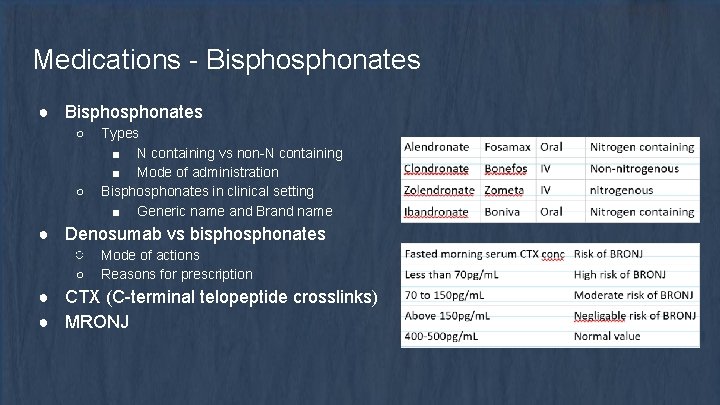
Medications - Bisphonates ● Bisphonates ○ ○ Types ■ N containing vs non-N containing ■ Mode of administration Bisphonates in clinical setting ■ Generic name and Brand name ● Denosumab vs bisphonates ○ Mode of actions ○ Reasons for prescription ● CTX (C-terminal telopeptide crosslinks) ● MRONJ

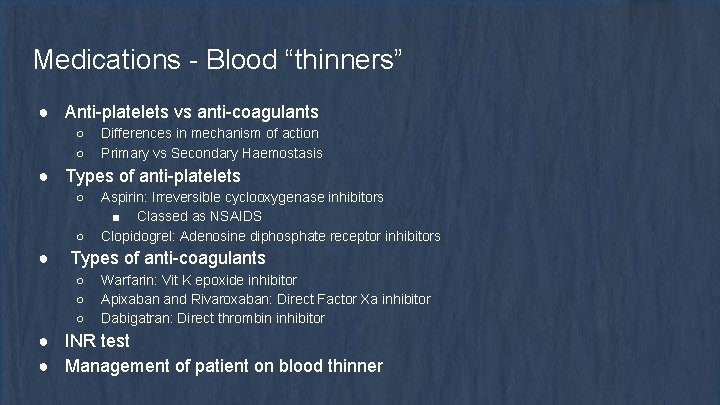
Medications - Blood “thinners” ● Anti-platelets vs anti-coagulants ○ ○ Differences in mechanism of action Primary vs Secondary Haemostasis ● Types of anti-platelets ○ ○ ● Aspirin: Irreversible cyclooxygenase inhibitors ■ Classed as NSAIDS Clopidogrel: Adenosine diphosphate receptor inhibitors Types of anti-coagulants ○ ○ ○ Warfarin: Vit K epoxide inhibitor Apixaban and Rivaroxaban: Direct Factor Xa inhibitor Dabigatran: Direct thrombin inhibitor ● INR test ● Management of patient on blood thinner
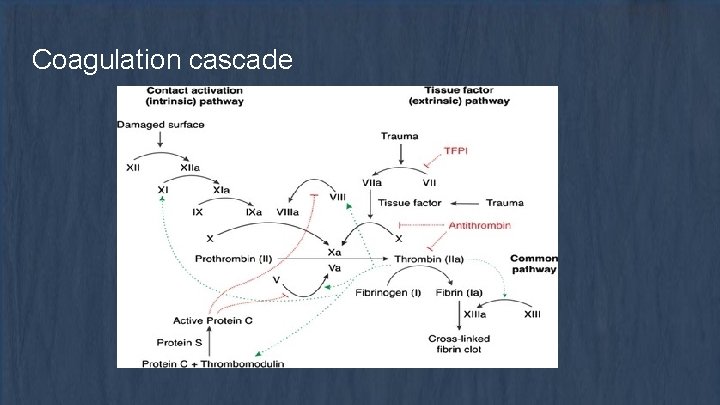
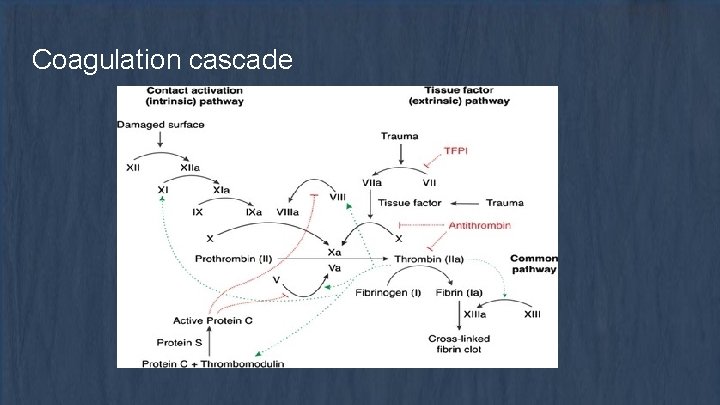
Coagulation cascade
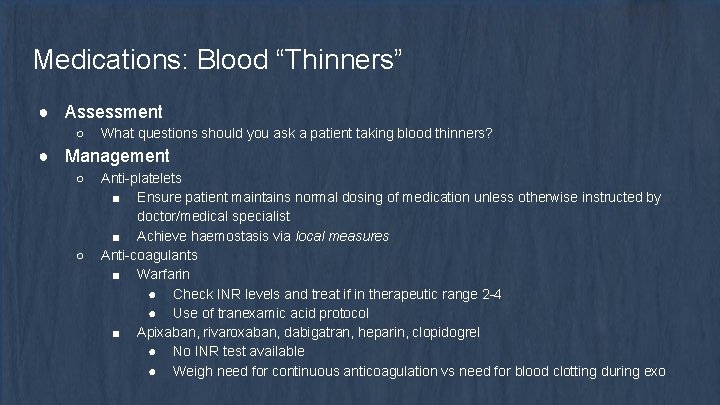
Medications: Blood “Thinners” ● Assessment ○ What questions should you ask a patient taking blood thinners? ● Management ○ ○ Anti-platelets ■ Ensure patient maintains normal dosing of medication unless otherwise instructed by doctor/medical specialist ■ Achieve haemostasis via local measures Anti-coagulants ■ Warfarin ● Check INR levels and treat if in therapeutic range 2 -4 ● Use of tranexamic acid protocol ■ Apixaban, rivaroxaban, dabigatran, heparin, clopidogrel ● No INR test available ● Weigh need for continuous anticoagulation vs need for blood clotting during exo
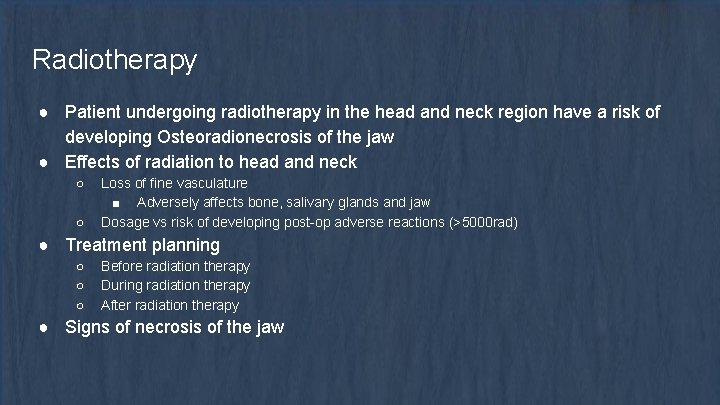
Radiotherapy ● Patient undergoing radiotherapy in the head and neck region have a risk of developing Osteoradionecrosis of the jaw ● Effects of radiation to head and neck ○ ○ Loss of fine vasculature ■ Adversely affects bone, salivary glands and jaw Dosage vs risk of developing post-op adverse reactions (>5000 rad) ● Treatment planning ○ ○ ○ Before radiation therapy During radiation therapy After radiation therapy ● Signs of necrosis of the jaw
Clinical evaluation ● Access to tooth ○ ○ ○ Mouth opening Inclination of tooth crowding ● Mobility of tooth ○ ○ Hypermobility usually noted in pts with periodontal disease - usually uneventful exos Hypomobility cases should be more carefully evaluated for… ■ Hypercementosis ■ Ankylosis ● Condition of crown ○ ○ Strength of crown ■ Caries or loss of tooth structure ■ Restorations Adjacent teeth ● Age of patient
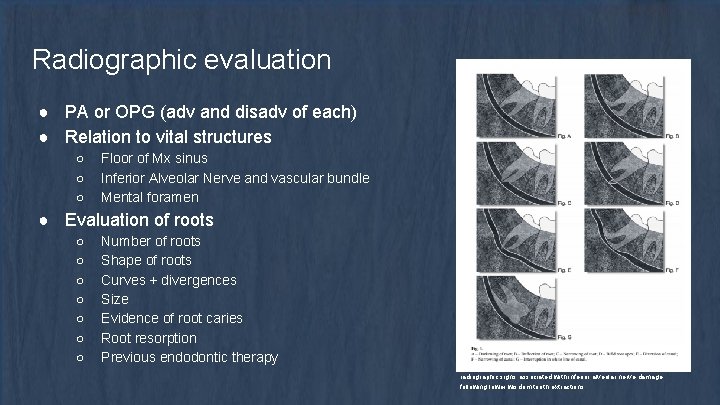
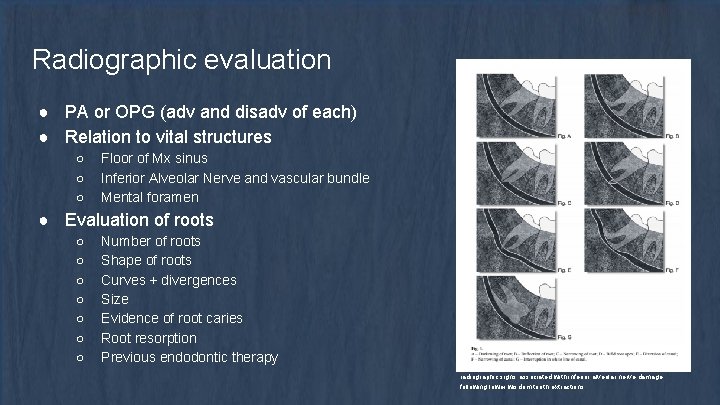
Radiographic evaluation ● PA or OPG (adv and disadv of each) ● Relation to vital structures ○ ○ ○ Floor of Mx sinus Inferior Alveolar Nerve and vascular bundle Mental foramen ● Evaluation of roots ○ ○ ○ ○ Number of roots Shape of roots Curves + divergences Size Evidence of root caries Root resorption Previous endodontic therapy radiographic signs associated with inferior alveolar nerve damage following lower wisdom tooth extractions

Radiographic evaluation ● Evaluation of surrounding tissues ○ ○ ○ Bone ■ Density of bone Acute periapical pathology Any pathology of surrounding tissues ■ What kinds of pathology noted on a radiograph might affect your treatment?
Consent ● How to gain informed consent? ○ ○ ○ What is the problem? What are the treatment options What they will expect during each treatment option What will they expect after tx What Risks are there for the treatments ● No treatment can proceed without patients consent. Consent can also be revoked at any time of treatment. ● What risks and adverse events can happen with exo?
Risks and Adverse reactions re: Extractions ● Iatrogenic damage ○ ○ ○ Slipping of instruments Overzealous use of instruments Incorrect use of instruments ● Swallowing of tooth and instruments ○ Inhalation - asphyxiation or infections ● Damage to vital structures ○ ○ OAC Nerve damage ● Displacement of tooth/root ○ ○ ○ Mx sinus Infratemporal space Submandibular space ● Inability to remove all or part of tooth
Local Anaesthesia ● Mandibular ○ ○ IANB, Lingual, Long Buccal Blocks Infiltrations ● Maxilla ○ Buccal and Palatal Infiltrations ● Failed anaesthesia ○ ○ Intraligamental Intrapulpal
Procedures of Simple Extractions 1. Loosening of soft tissue attachment from cervical portion of tooth 2. Break PDL 3. Break interdigitation of bone via expansion of socket a. Luxating the tooth b. Wedging c. Use of dental forceps 4. Delivery of tooth via extrusive force a. Specific technique for different teeth

Instruments ● Elevators ○ ○ ○ Straight: Luxator, Couplands Curved: Cryer, Warwick James Picks: Root picks ● Forceps ○ ○ Various Not all types of forceps available at ADH ● Handpieces ○ ○ Impact Air Surg. XT

Elevators ● D/d ∝ F ○ D = diameter of blade, d = diameter of handle ● Used to expand socket through various movements
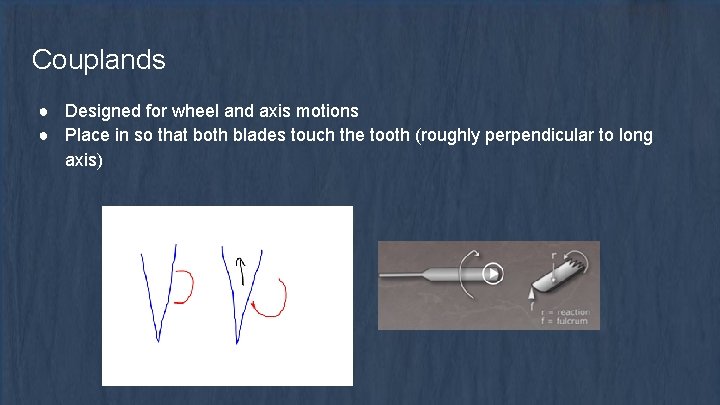
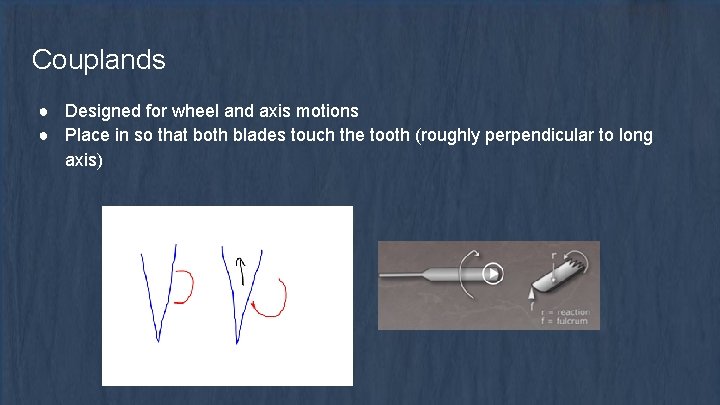
Couplands ● Designed for wheel and axis motions ● Place in so that both blades touch the tooth (roughly perpendicular to long axis)
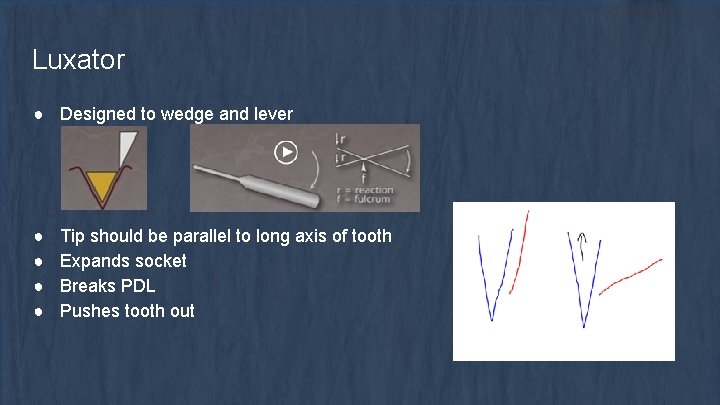
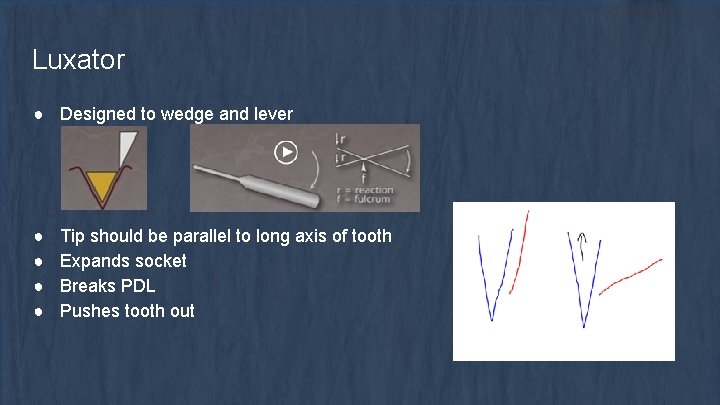
Luxator ● Designed to wedge and lever ● ● Tip should be parallel to long axis of tooth Expands socket Breaks PDL Pushes tooth out
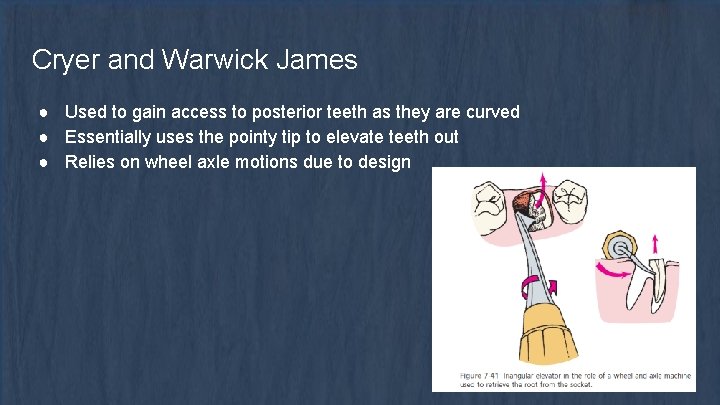
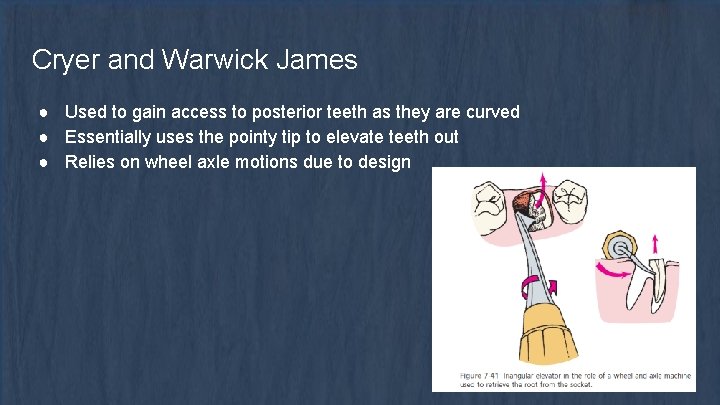
Cryer and Warwick James ● Used to gain access to posterior teeth as they are curved ● Essentially uses the pointy tip to elevate teeth out ● Relies on wheel axle motions due to design
Forceps ● Mx ○ ○ ○ Upper uni Stubbies Right, Left Upper molar Root forceps ● Md ○ ○ ○ Lower anterior Lower molar Hawksbill Cowhorn Root forceps
Forceps ● Choose angle depending on location of tooth ● Shape of blade important ○ Want them to encircle crown as much as possible ● Movements ○ ○ Apical Torsional ■ Safe movement, unlikely to break tooth (single rooted teeth) Lateral ■ Bucco-palatal ■ Risk of tooth breaking but should be mobile at this point ■ Figure 8 on lowers Tractional
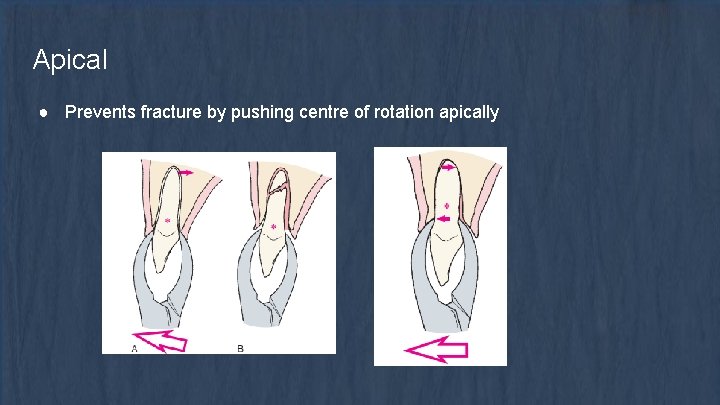
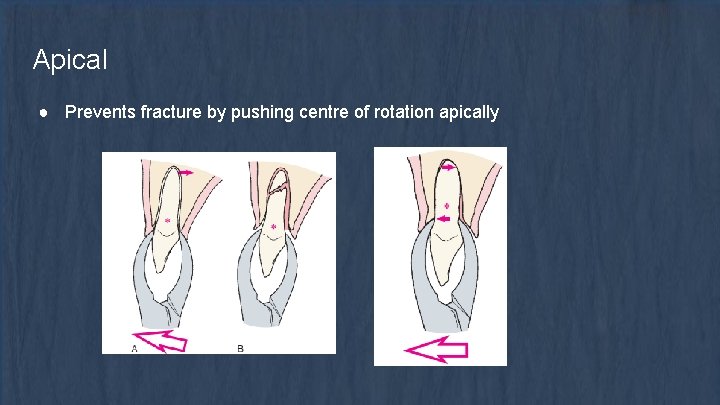
Apical ● Prevents fracture by pushing centre of rotation apically
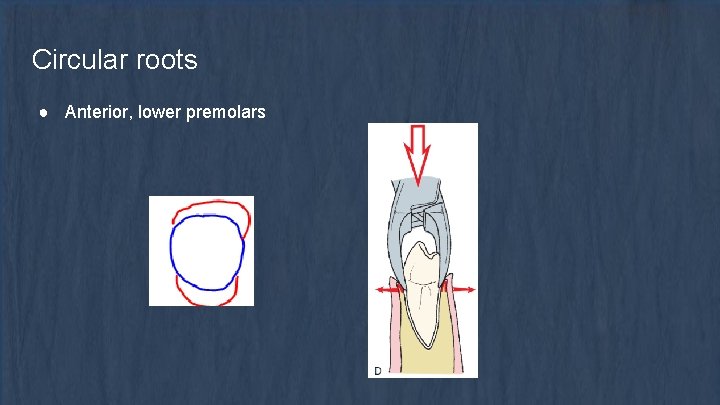
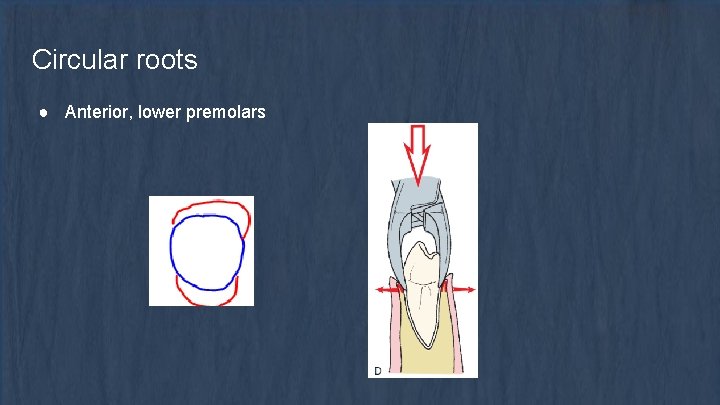
Circular roots ● Anterior, lower premolars
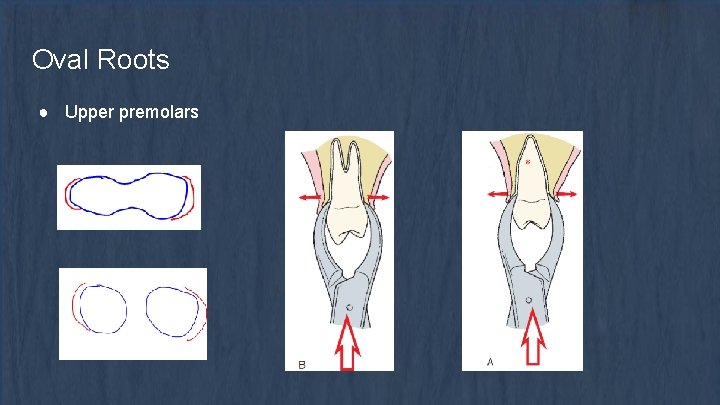
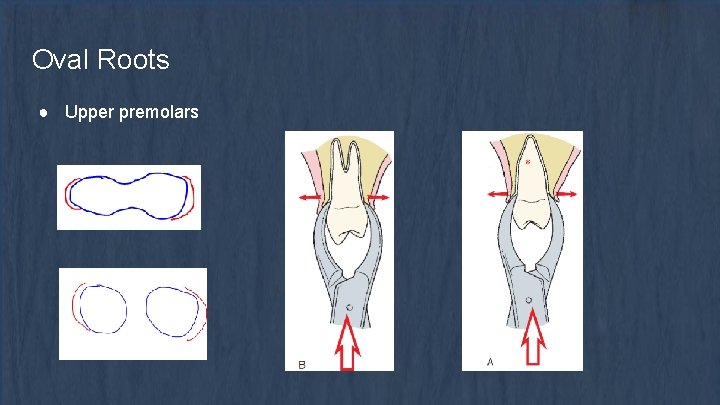
Oval Roots ● Upper premolars
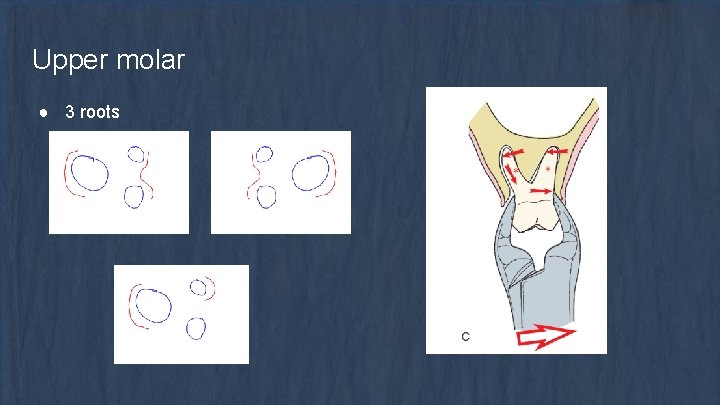
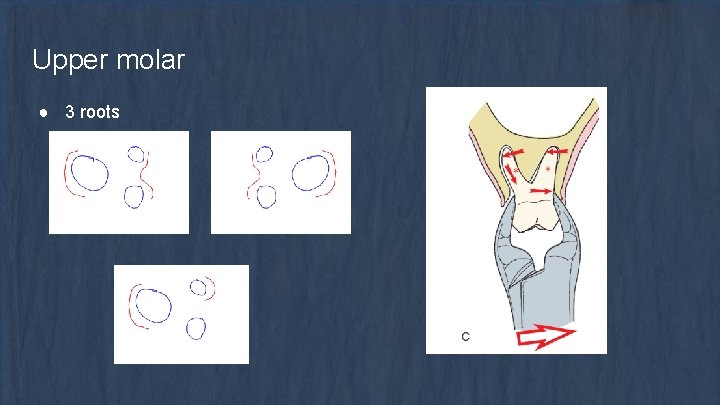
Upper molar ● 3 roots
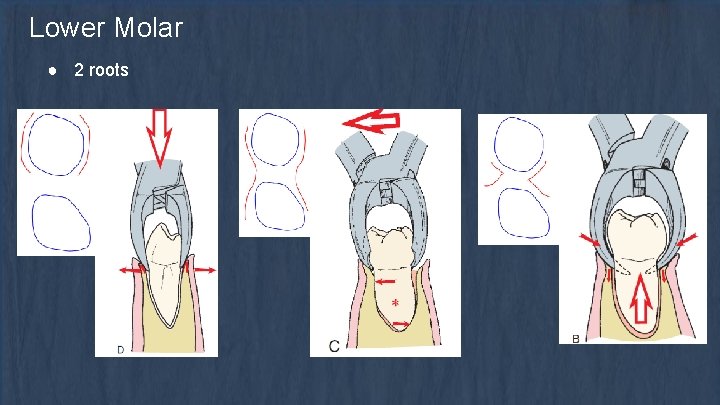
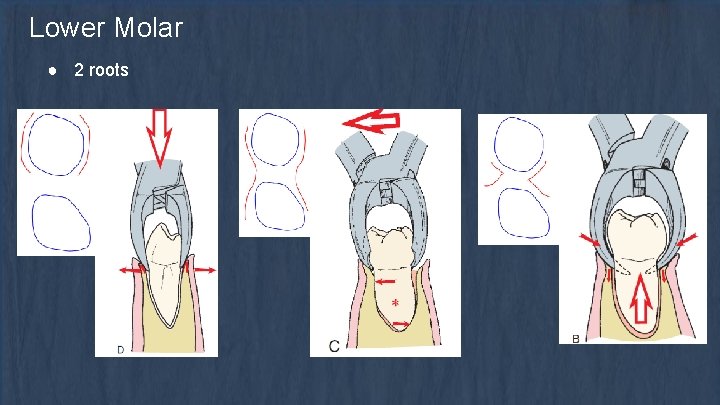
Lower Molar ● 2 roots
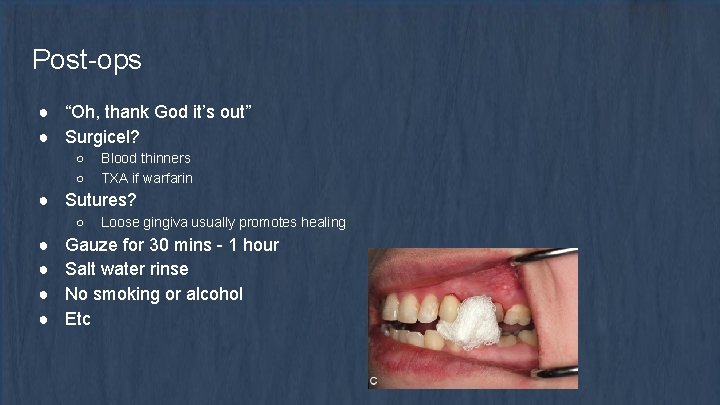
Post-ops ● “Oh, thank God it’s out” ● Surgicel? ○ ○ Blood thinners TXA if warfarin ● Sutures? ○ ● ● Loose gingiva usually promotes healing Gauze for 30 mins - 1 hour Salt water rinse No smoking or alcohol Etc
Surgicals 1. Assess the tooth a. Planning essential, should know exactly what you are doing before touching the patient b. Determine whether bone needs to be removed c. Section tooth 2. Visualisation and Access a. May require flap to be raised b. 2 anterior 1 posterior or 1 anterior and 1 posterior if relieving incision placed 3. Bone Removal a. May not be required 4. Deliver Tooth 5. Smoothen sharp edges on bone 6. Suture
Happy Exo!
 Chapter 56 oral and maxillofacial surgery
Chapter 56 oral and maxillofacial surgery Chapter 26 oral and maxillofacial surgery
Chapter 26 oral and maxillofacial surgery Chapter 56 oral and maxillofacial surgery
Chapter 56 oral and maxillofacial surgery Best worst and average case
Best worst and average case Case description
Case description Table of contents case study
Table of contents case study Surgery case presentation
Surgery case presentation Fire risk assessment surgery
Fire risk assessment surgery Rubrik penilaian tes lisan
Rubrik penilaian tes lisan Roag
Roag Gil kalai quantum computing
Gil kalai quantum computing Gil kalai quantum computing
Gil kalai quantum computing Gil kirkpatrick
Gil kirkpatrick Robledo lima gil
Robledo lima gil Caroline prenat hugo
Caroline prenat hugo Richard ramirez ac dc hat for sale
Richard ramirez ac dc hat for sale Redondilha maior e menor
Redondilha maior e menor Imagenes de gil gonzalez davila
Imagenes de gil gonzalez davila Ayaa elgoharry
Ayaa elgoharry Robledo lima gil
Robledo lima gil Gil kirkpatrick
Gil kirkpatrick Don manuel camus
Don manuel camus Fiona gil
Fiona gil Vida e obra de gil vicente
Vida e obra de gil vicente Nelson javier duenas gil
Nelson javier duenas gil Farsa ines pereira personagens
Farsa ines pereira personagens Velho da horta
Velho da horta Nerea gil
Nerea gil Jaime gil aluja
Jaime gil aluja Lorenzo gil macia
Lorenzo gil macia Abhorrèd
Abhorrèd Jody apostolu
Jody apostolu Gil naor
Gil naor