POLYCYSTIC OVARY SYNDROME PCOS Dr Mouna Dakar INTRODUCTION





![The major features of PCOS include menstrual dysfunction, anovulation, and signs of hyperandrogenism. [2] The major features of PCOS include menstrual dysfunction, anovulation, and signs of hyperandrogenism. [2]](https://slidetodoc.com/presentation_image_h2/5f9ce77b0329413d2fb73ce4f39eca14/image-16.jpg)





- Slides: 68
POLYCYSTIC OVARY SYNDROME PCOS Dr. Mouna Dakar
INTRODUCTION TO THE PCOS � The association of amenorrhea with bilateral polycystic ovaries was first described in 1935 by Stein and Levental and was known for decades as Stein-Levental syndrome. � In the past the clinical diagnosis rested on the triad of hirsutism , amenorrhea and obesity.


Defect in Insulin receptor gene -Hyperglycemia

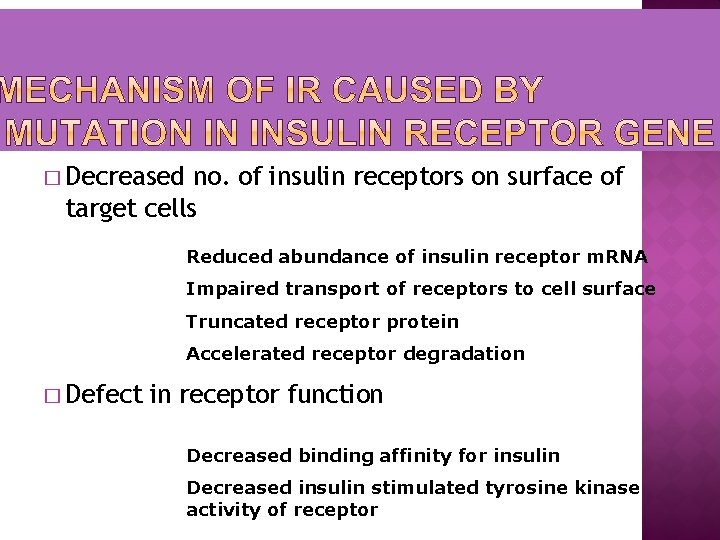
� Decreased no. of insulin receptors on surface of target cells Reduced abundance of insulin receptor m. RNA Impaired transport of receptors to cell surface Truncated receptor protein Accelerated receptor degradation � Defect in receptor function Decreased binding affinity for insulin Decreased insulin stimulated tyrosine kinase activity of receptor
� Insulin is a growth factor for the ovary � Women who are obese sometimes have insulin resistance (it takes higher and higher insulin levels to keep glucose in the normal range) � Fat cells are insulin resistant, but the ovaries are not
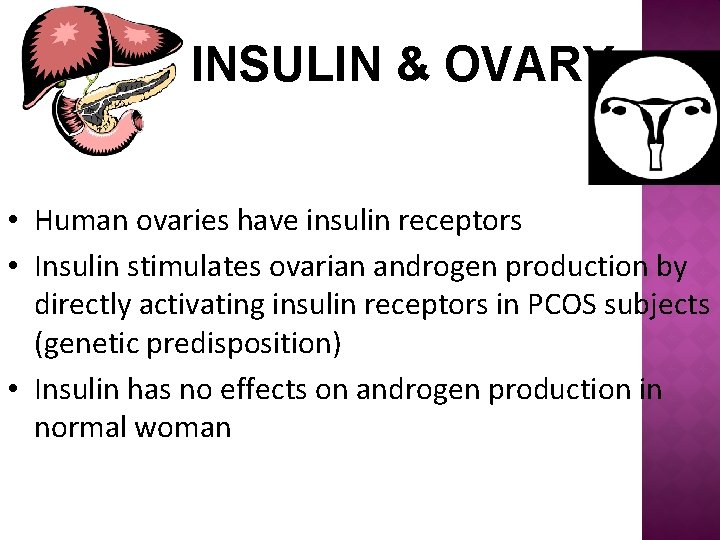
INSULIN & OVARY • Human ovaries have insulin receptors • Insulin stimulates ovarian androgen production by directly activating insulin receptors in PCOS subjects (genetic predisposition) • Insulin has no effects on androgen production in normal woman
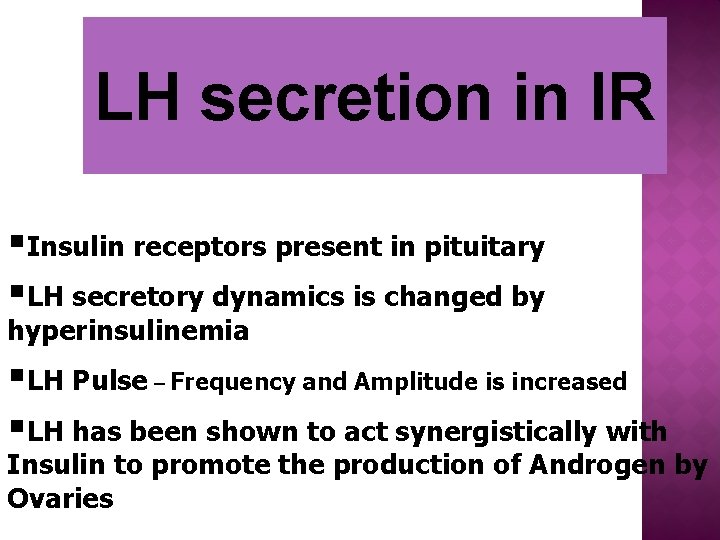
LH secretion in IR §Insulin receptors present in pituitary §LH secretory dynamics is changed by hyperinsulinemia §LH Pulse – Frequency and Amplitude is increased §LH has been shown to act synergistically with Insulin to promote the production of Androgen by Ovaries

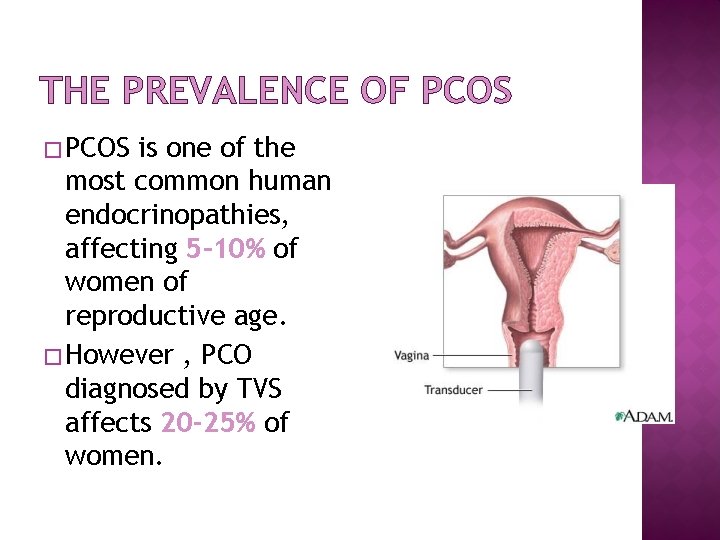
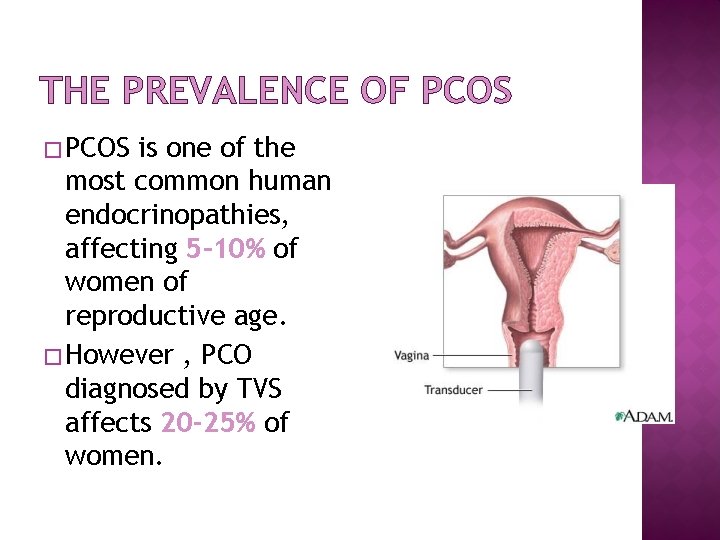
THE PREVALENCE OF PCOS � PCOS is one of the most common human endocrinopathies, affecting 5– 10% of women of reproductive age. � However , PCO diagnosed by TVS affects 20 -25% of women.

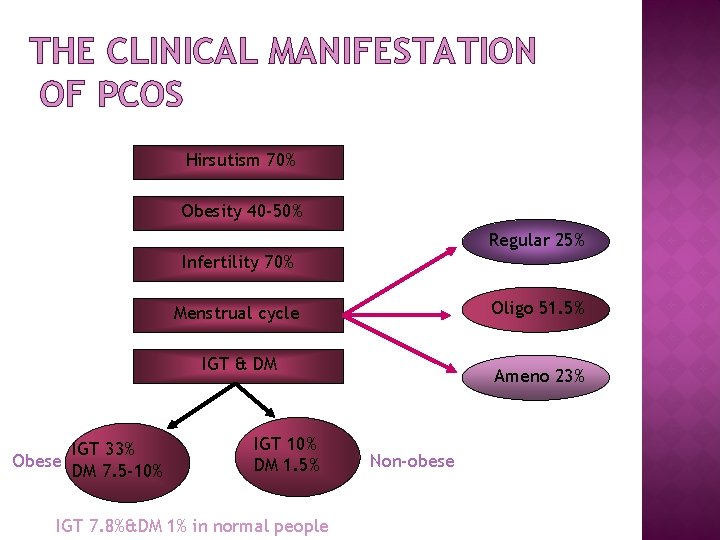
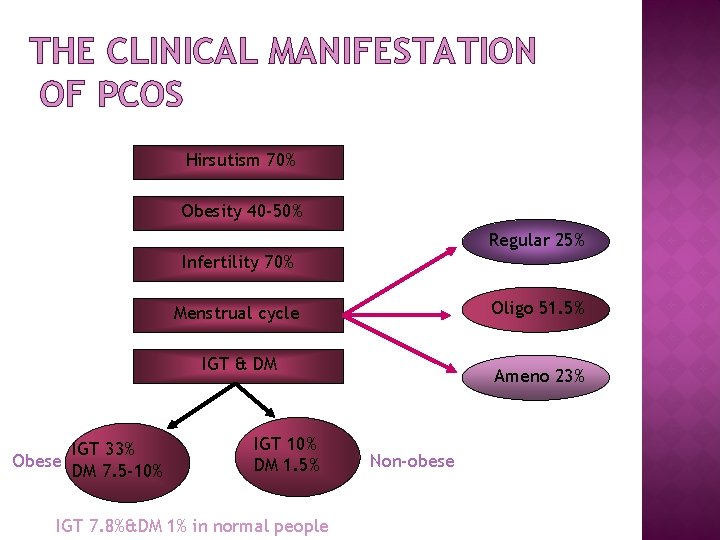
THE CLINICAL MANIFESTATION OF PCOS Hirsutism 70% Obesity 40 -50% Regular 25% Infertility 70% Oligo 51. 5% Menstrual cycle IGT & DM IGT 33% Obese DM 7. 5 -10% IGT 10% DM 1. 5% IGT 7. 8%&DM 1% in normal people Ameno 23% Non-obese
Essential update: AACE/ACE and AESSociety release new guidelines. In November 2015, the American Association of Clinical Endocrinologists (AACE), American College of Endocrinology (ACE), and Androgen Excess and PCOS Society (AES) released new guidelines in the evaluation and treatment of PCOS. [1] Among their opinions and recommendations are the following[1] :
![The major features of PCOS include menstrual dysfunction anovulation and signs of hyperandrogenism 2 The major features of PCOS include menstrual dysfunction, anovulation, and signs of hyperandrogenism. [2]](https://slidetodoc.com/presentation_image_h2/5f9ce77b0329413d2fb73ce4f39eca14/image-16.jpg)
The major features of PCOS include menstrual dysfunction, anovulation, and signs of hyperandrogenism. [2] Other signs and symptoms of PCOS may include the following: Hirsutism. Infertility. Obesity and metabolic syndrome. Diabetes. Obstructive sleep apnea
Menstrual abnormalities
Menstrual abnormalities. Patients with PCOS have abnormal menstruation patterns attributed to chronic anovulation. Some women have oligomenorrhea (ie, menstrual bleeding that occurs at intervals of 35 days to 6 months, with < 9 menstrual periods per year) or secondary amenorrhea (an absence of menstruation for 6 months).
MENSTRUAL DISTURBANCES � Around 25% of women with confirmed PCOS still have regular menses. � 21% of hyperandrogenic anovulatory women have regular menses. � The presence of regular menses does not rule out the diagnosis of PCOS. � Just over the half of patients with PCOS have oligomenorrhea. About 25 % of PCOS patients have amonorrhea. � The reason for menstrual disturbance are the effect of androgens on the endometrium as well as the increased levels of esteron that comes from the peripheral aromatization of increased androgens to esteron which stimulates the endometrium to proliferates.
Hyperandrogenism
70% HIRSUTISM PCOS is the most common cause of hyperandrogenism and hirsutism.
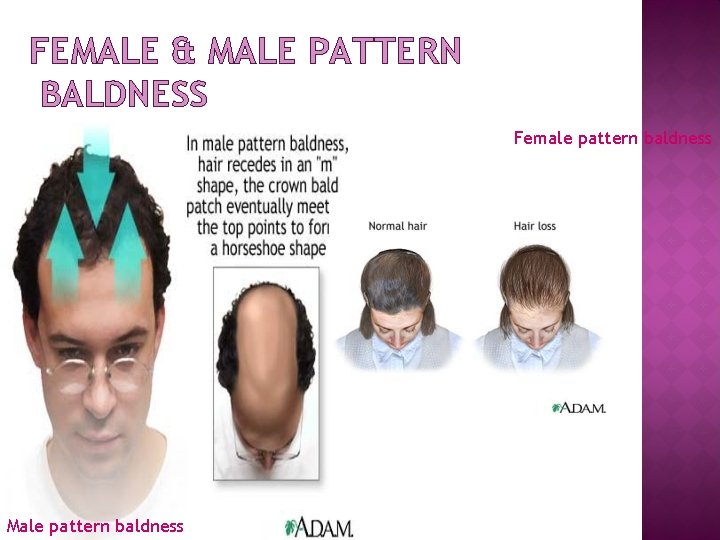
Hyperandrogenism clinically manifests as excess terminal body hair in a male distribution pattern. Hair is commonly seen on the upper lip, on the chin, around the nipples, and along the linea alba of the lower abdomen. Some patients have acne and/or male-pattern hair loss (androgenic alopecia).
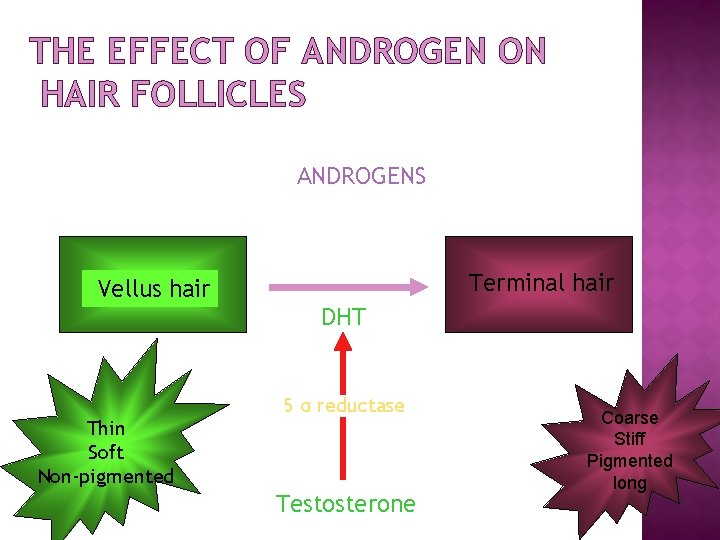
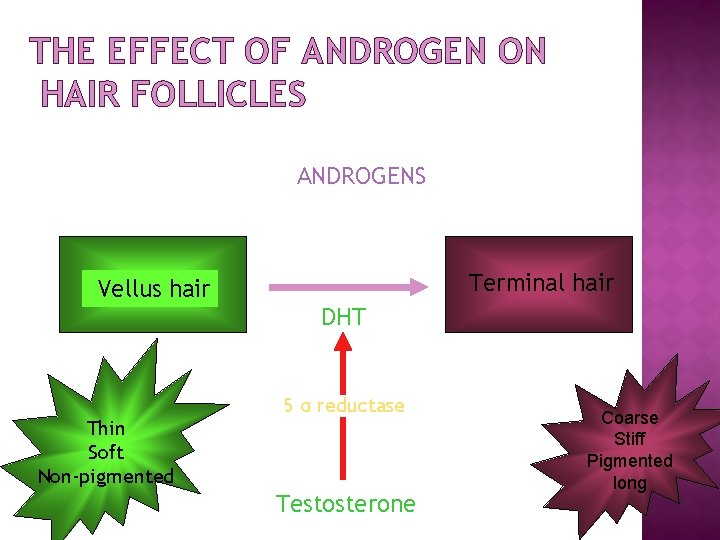
THE EFFECT OF ANDROGEN ON HAIR FOLLICLES ANDROGENS Terminal hair Vellus hair DHT Thin Soft Non-pigmented 5 α reductase Testosterone Coarse Stiff Pigmented long

HIRSUTISM Hirsutism is a sign of increased androgen action on hair follicles, from increased circulating levels of androgens or increased sensitivity of hair follicles to normal levels of. circulating androgens
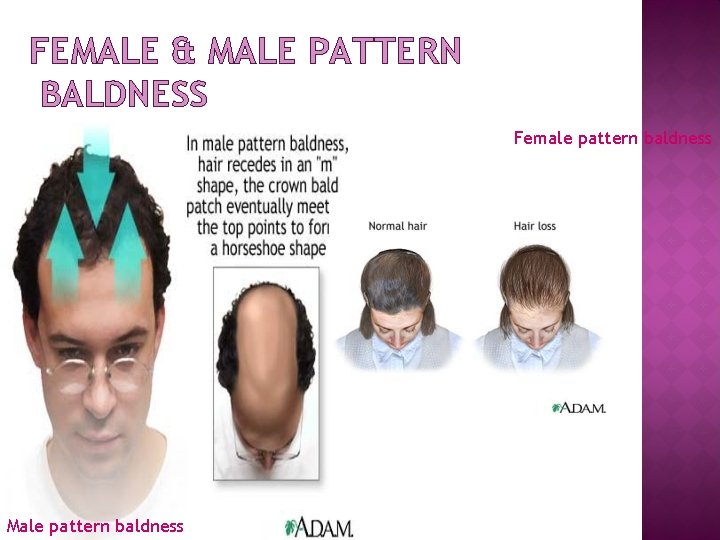
FEMALE & MALE PATTERN BALDNESS Female pattern baldness Male pattern baldness
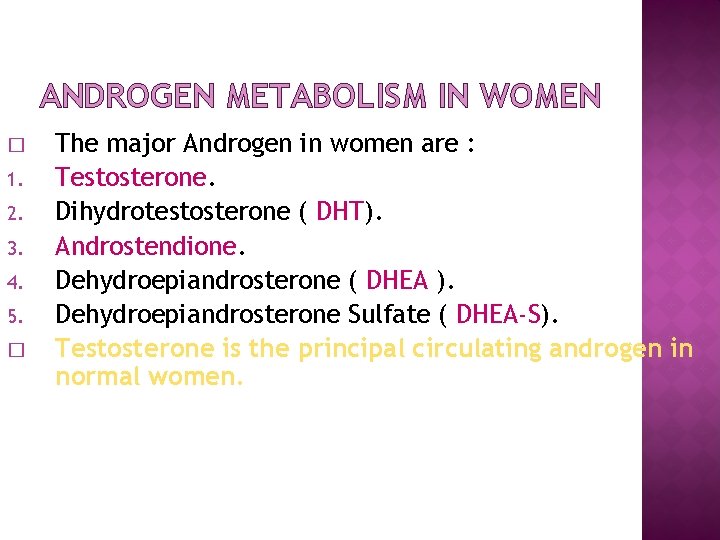
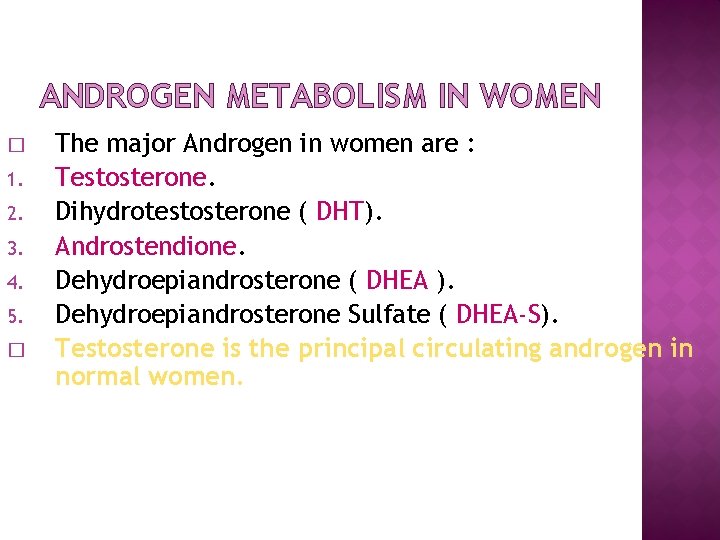
ANDROGEN METABOLISM IN WOMEN � 1. 2. 3. 4. 5. � The major Androgen in women are : Testosterone. Dihydrotestosterone ( DHT). Androstendione. Dehydroepiandrosterone ( DHEA ). Dehydroepiandrosterone Sulfate ( DHEA-S). Testosterone is the principal circulating androgen in normal women.
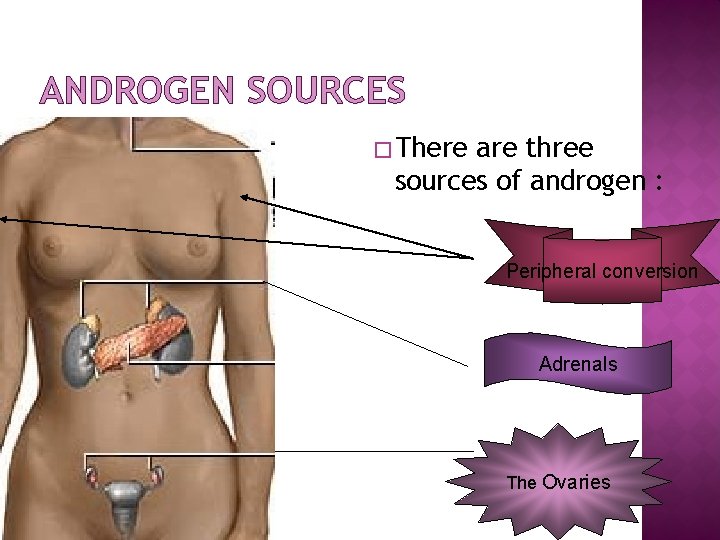
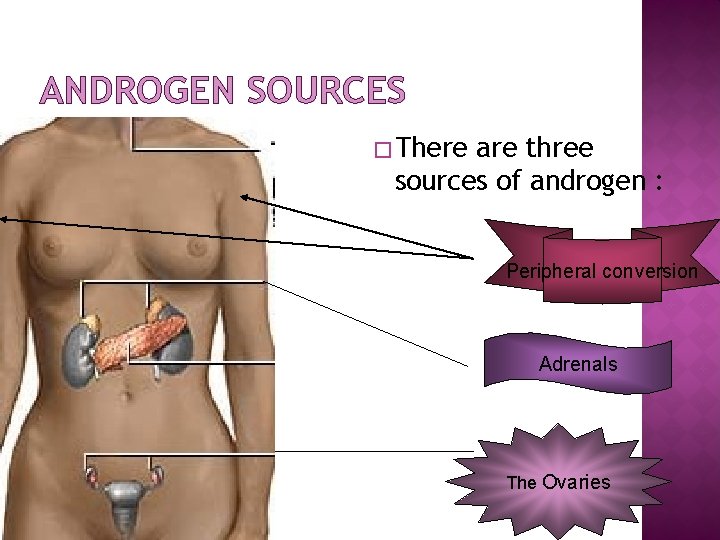
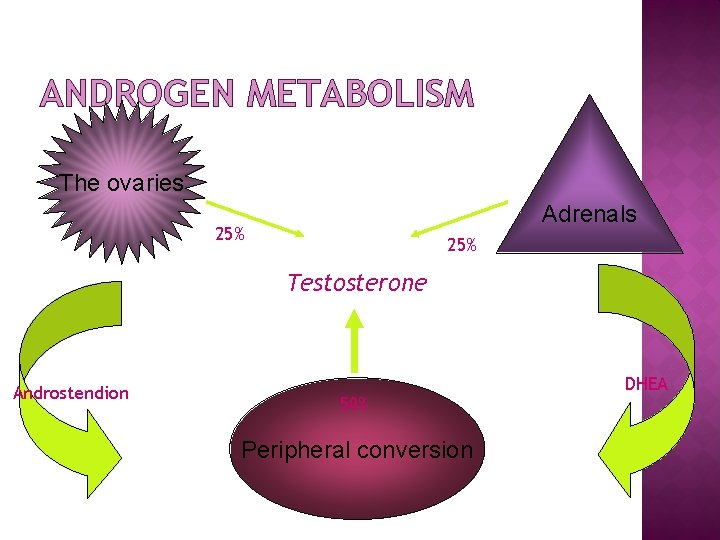
ANDROGEN SOURCES � There are three sources of androgen : Peripheral conversion Adrenals The Ovaries
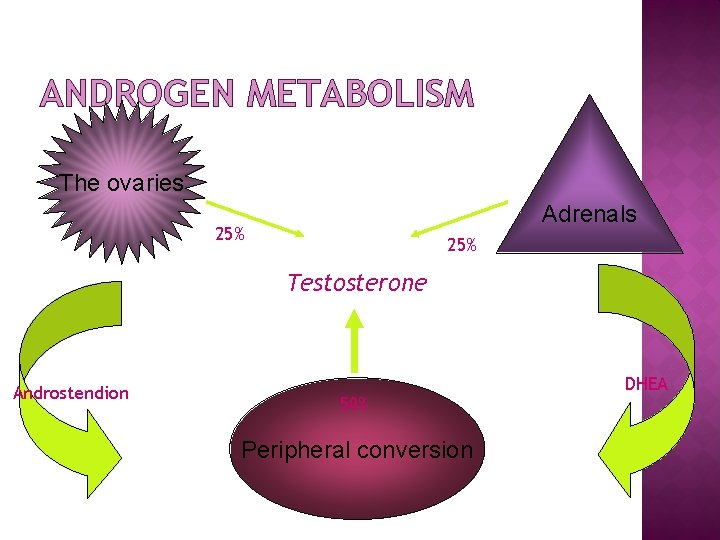
ANDROGEN METABOLISM The ovaries Adrenals 25% Testosterone Androstendion 50% Peripheral conversion DHEA
INFERTILITY About 70% of PCOS patients may have different degrees of subfertility due to anovulation. Group 2 WHO classification.
Conception may take longer than in other women, or women with PCOS may have fewer children than they had planned. In addition, the rate of miscarriage is also higher in affected women.
40 -50% OBESITY& INSULIN RESISTANCE Not all PCOS patients are obese
Obesity and metabolic syndrome
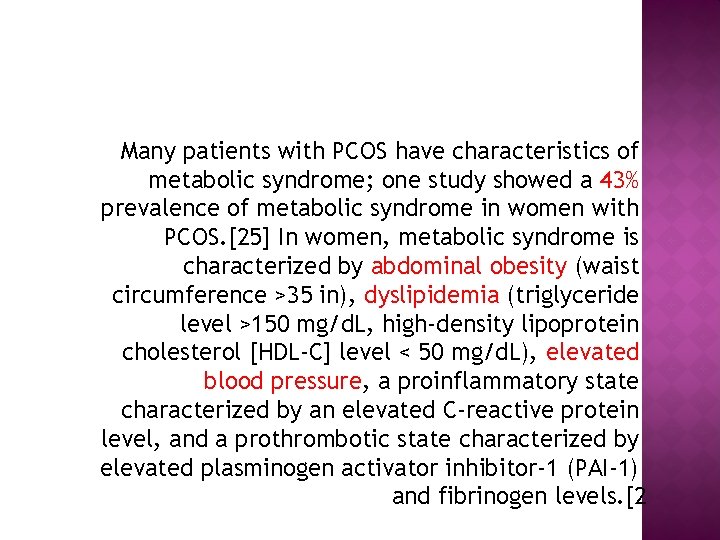
Many patients with PCOS have characteristics of metabolic syndrome; one study showed a 43% prevalence of metabolic syndrome in women with PCOS. [25] In women, metabolic syndrome is characterized by abdominal obesity (waist circumference >35 in), dyslipidemia (triglyceride level >150 mg/d. L, high-density lipoprotein cholesterol [HDL-C] level < 50 mg/d. L), elevated blood pressure, a proinflammatory state characterized by an elevated C-reactive protein level, and a prothrombotic state characterized by elevated plasminogen activator inhibitor-1 (PAI-1) and fibrinogen levels. [2
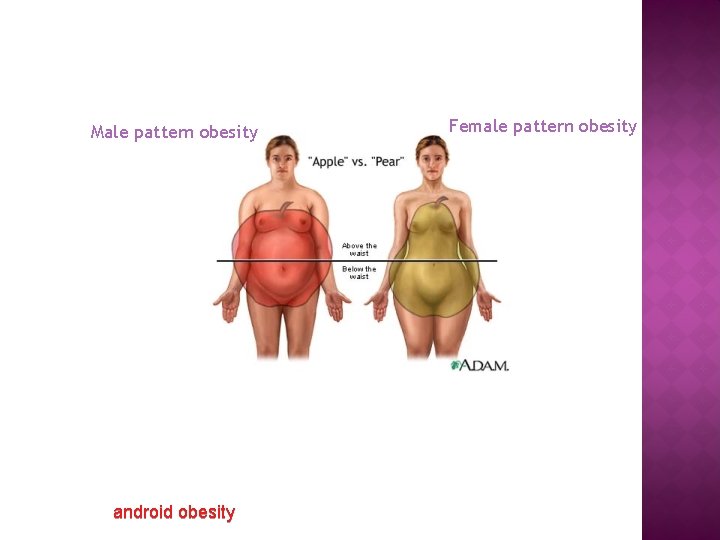
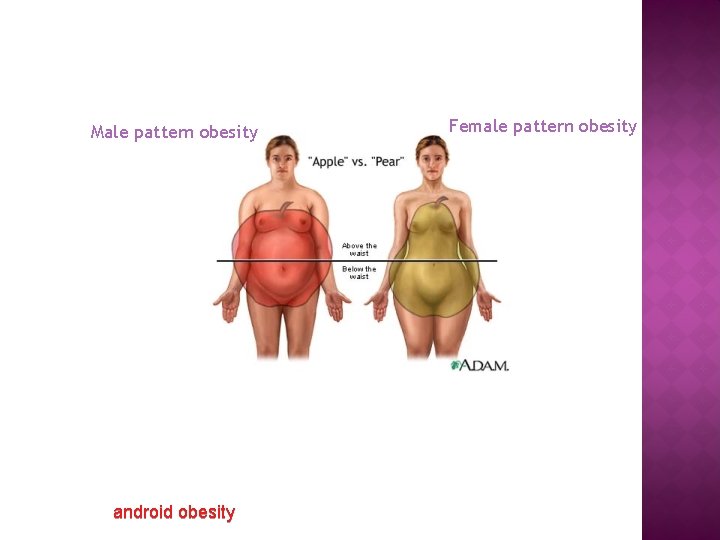
Male pattern obesity android obesity Female pattern obesity
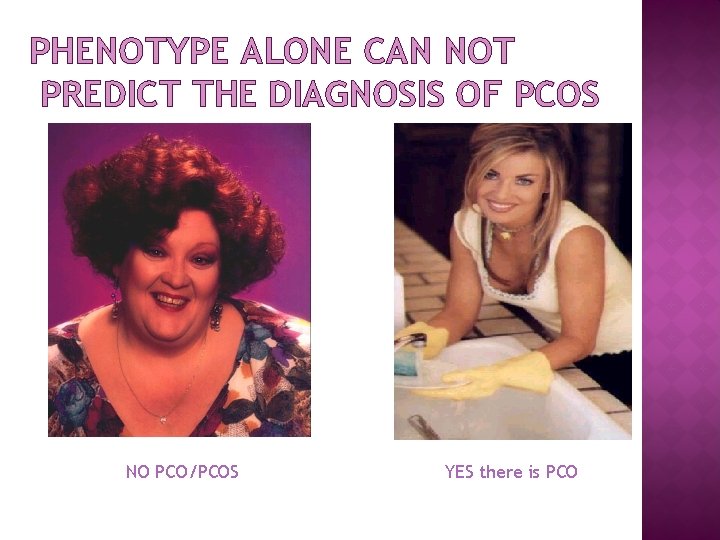
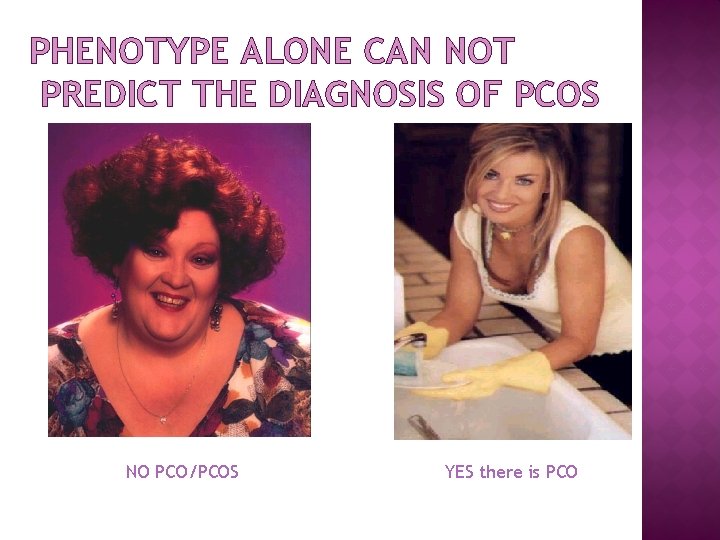
PHENOTYPE ALONE CAN NOT PREDICT THE DIAGNOSIS OF PCOS NO PCO/PCOS YES there is PCO
Diabetes mellitus
ACOG recommends screening for type 2 diabetes and impaired glucose tolerance in women with PCOS by obtaining a fasting glucose level and then a 2 -hour glucose level after a 75 -g glucose load. [4] Approximately 10% of women with PCOS have type 2 diabetes mellitus, and 30 -40% of women with PCOS have impaired glucose tolerance by 40 years of age.
Sleep apnea
Many women with PCOS have obstructive sleep apnea syndrome (OSAS), which is an independent risk factor for cardiovascular disease. [5] Ask these patients and/or their partners about excessive daytime somnolence; individuals with obstructive sleep apnea experience apnea/hypopnea episodes during sleep. [40, 41] For women with PCOS with suspected OSAS, there should be a low threshold for referral for sleep assessment.
ENDOMETRIAL HYPERPLASIA AND CARCINOMA � Unopposed estrogen secretion promots endometrial hyperplasia � Several studies have shown that this results in a 2 -4 fold excess risk of endometrial carcinoma in females with PCOS
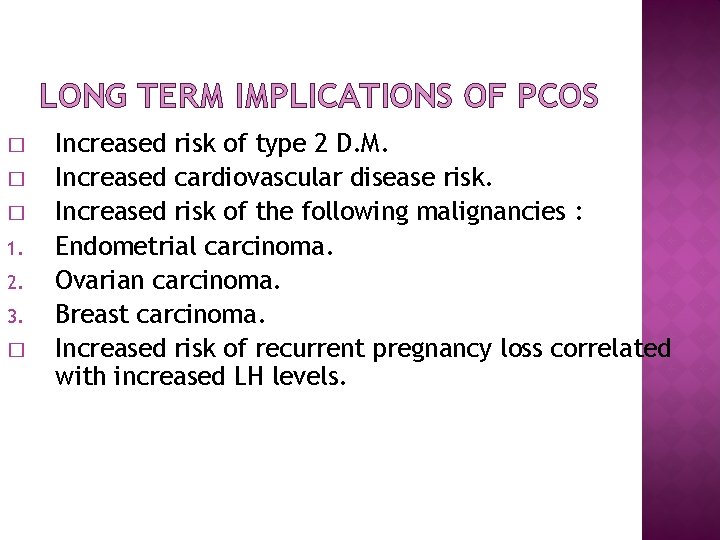
LONG TERM IMPLICATIONS OF PCOS � � � 1. 2. 3. � Increased risk of type 2 D. M. Increased cardiovascular disease risk. Increased risk of the following malignancies : Endometrial carcinoma. Ovarian carcinoma. Breast carcinoma. Increased risk of recurrent pregnancy loss correlated with increased LH levels.
DIAGNOSIS
The diagnostic criteria for PCOS should include one of the following three criteria: chronic anovulation, hyperandrogenism (clinical/biologic), and polycystic ovaries
Use the Rotterdam criteria for diagnosing PCOS (presence of 2 of the following: androgen excess, ovulatory dysfunction, or polycystic ovaries).
� The absence of PCO on ultrasound does not rule out the diagnosis of PCOS.

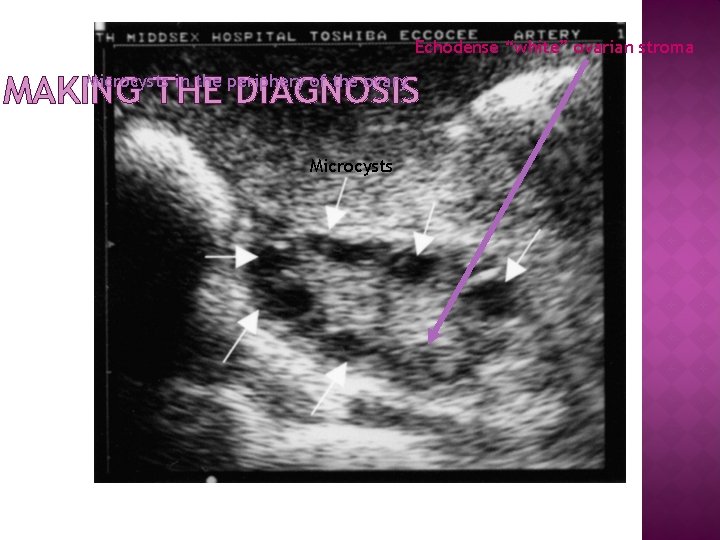
MAKING THE DIAGNOSIS � � 1. 2. 3. � � � Ovarian morphology remains the most sensitive marker for the PCOS. There are ultrasound criteria to diagnose the PCO : Increased ovary area/volume. 10 -15 microcysts less than 10 mm organized in a peripheral rosary pattern. (generally > 5 cysts) Increased echogenicity of ovarian stroma. Transvaginal sonography (TVS) is the gold standard and the most sensitive method to detect PCO. The presence of PCO does not mean that the patient has PCOS. Around 20 -25% of women have PCO detected by TVS , only about 5 -10% have PCOS.
A woman is diagnosed with polycystic ovaries (as opposed to PCOS) if she has 12 or more follicles in at least 1 ovary
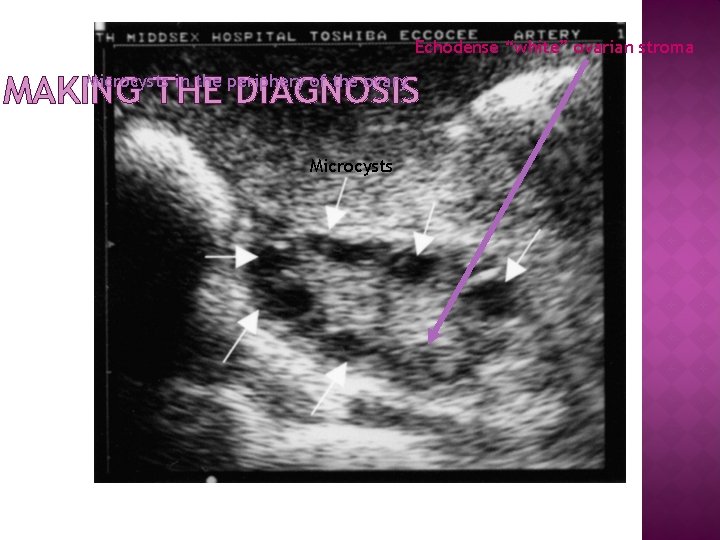
Echodense “white” ovarian stroma MAKING THE DIAGNOSIS Microcysts in the periphery of the ovary Microcysts
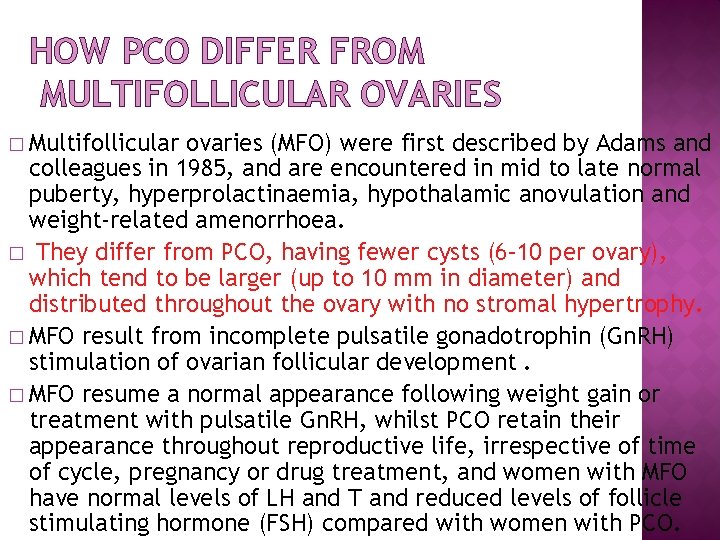
HOW PCO DIFFER FROM MULTIFOLLICULAR OVARIES � Multifollicular ovaries (MFO) were first described by Adams and colleagues in 1985, and are encountered in mid to late normal puberty, hyperprolactinaemia, hypothalamic anovulation and weight-related amenorrhoea. � They differ from PCO, having fewer cysts (6– 10 per ovary), which tend to be larger (up to 10 mm in diameter) and distributed throughout the ovary with no stromal hypertrophy. � MFO result from incomplete pulsatile gonadotrophin (Gn. RH) stimulation of ovarian follicular development. � MFO resume a normal appearance following weight gain or treatment with pulsatile Gn. RH, whilst PCO retain their appearance throughout reproductive life, irrespective of time of cycle, pregnancy or drug treatment, and women with MFO have normal levels of LH and T and reduced levels of follicle stimulating hormone (FSH) compared with women with PCO.
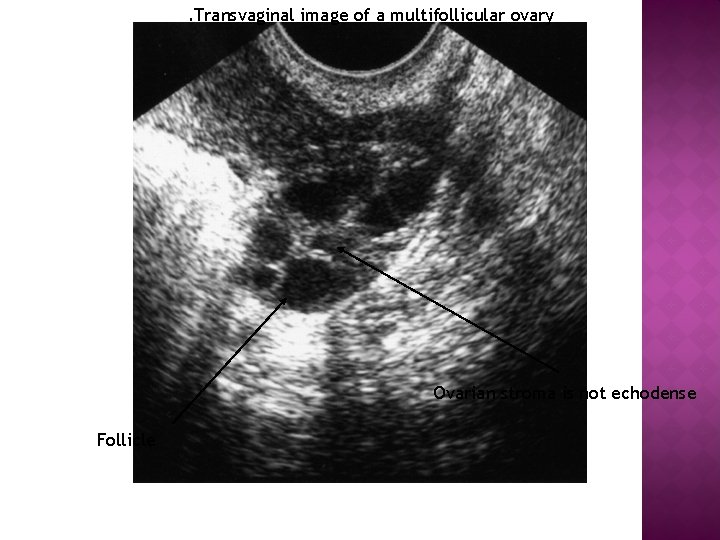
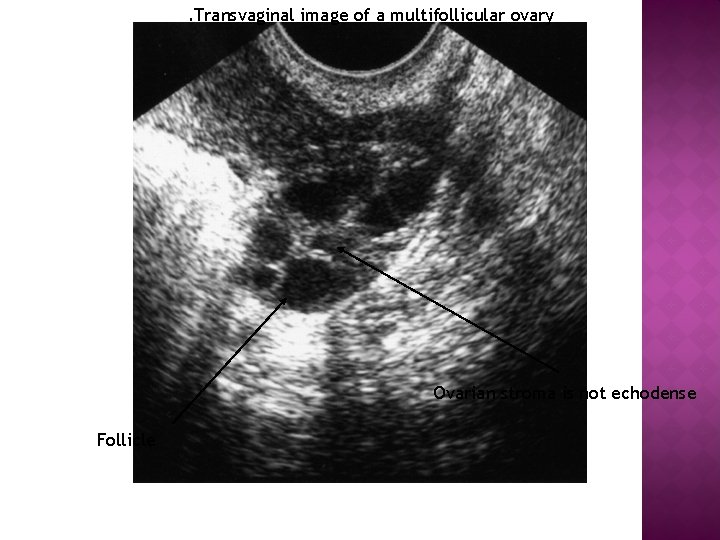
. Transvaginal image of a multifollicular ovary Ovarian stroma is not echodense Follicle

INVESTIGATIONS Confirmation of diagnosis � Testosterone � LH concentrations concentrate � Pelvic US of ovaries and endometrium.
Free testosterone levels are more sensitive for determining androgen excess than total T levels and should be obtained with equilibrium dialysis techniques
In addition to clinical findings, obtain levels of serum 17 hydroxyprogesterone and anti. Müllerian hormone to aid the diagnosis of PCOS.
PATHOPHYSIOLOGY & LAB FINDING � 1. 2. 3. 4. The hypothalamic pituitary compartment also participates in aspects critical to the development of PCOS. An increase in the LH pulse frequency is the result of increased pulse frequency of Gn. RH. This increase in LH pulse frequency results typically in elevated LH to FSH ratio. FSH is not increased with LH, probably because of the synergistic negative feedback of chronically elevated estrogen level and normal follicular Inhibin. About 25% of patients with PCOS exhibit elevated PRL levels. This may result in abnormal estrogen feedback to the pituitary gland. In some patients with PCOS , bromocriptine has reduced LH levels and restored ovulation.

MANAGEMENT OF PCOS
Lifestyle modifications are considered first-line treatment for women with PCOS. Such changes include the following[3, 4] : Diet Exercise Weight loss
treatments are reserved for so-called metabolic derangements, such as anovulation, hirsutism, and menstrual irregularities. First-line medical therap. Pharmacotherapy. Pharmacologic y usually consists of an oral contraceptive to induce regular menses. If symptoms such as hirsutism are not sufficiently alleviated, an androgen-blocking agent may be added. First-line treatment for ovulation induction when fertility is desired is clomiphene citrate. [3
Medications used in the management of PCOS include the following: Oral contraceptive agents (eg, ethinyl estradiol, medroxyprogesterone). Antiandrogens (eg, spironolactone, leuprolide, finasteride). Hypoglycemic agents (eg, metformin, insulin). Selective estrogen receptor modulators (eg, clomiphene citrate)
In October 2013, the Endocrine Society released practice guidelines for the diagnosis and treatment of PCOS. The following were among their conclusions
In adolescents with PCOS, hyperandrogenism is central to the presentation; hormonal contraceptives and metformin are treatment options in this population.
Postmenopausal women do not have a consistent PCOS phenotype.
For menstrual abnormalities and hirsutism/acne, hormonal contraceptives are first-line treatment.
For infertility, clomiphene is firstline treatment
. For metabolic/glycemic abnormalities and for improving menstrual irregularities, metformin is beneficial. Metformin is of limited or no benefit for managing hirsutism, acne, or infertility.

Good Luck
 Pcos ovary size in cm
Pcos ovary size in cm Infantile polycystic kidney
Infantile polycystic kidney Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Mouna akacha
Mouna akacha Mouna diet
Mouna diet Savage syndrome
Savage syndrome Pcos ultrasound report
Pcos ultrasound report Pcos macros
Pcos macros Normoz tablet side effects
Normoz tablet side effects Is byetta used to treat pcos
Is byetta used to treat pcos Ferriman-gallwey scale
Ferriman-gallwey scale Esp informatique
Esp informatique Programme de formation cesag dakar
Programme de formation cesag dakar Groupe afi
Groupe afi Atci group dakar
Atci group dakar Spets dakar
Spets dakar Esmp dakar
Esmp dakar Functions of the ovary
Functions of the ovary Figure of female reproductive system
Figure of female reproductive system Difference between ovary and ovule
Difference between ovary and ovule Female anatomy
Female anatomy Squid gonads
Squid gonads Structure that will become the fruit
Structure that will become the fruit Penyebab benign neoplasm of breast d24
Penyebab benign neoplasm of breast d24 Parts and functions of a flower
Parts and functions of a flower Chicken ovary function
Chicken ovary function Stroma
Stroma Lemon diagram
Lemon diagram Caesalpinaceous flower
Caesalpinaceous flower Floral formula key
Floral formula key Difference between ovule and ovary
Difference between ovule and ovary 38
38 Anatomy of the human ovary
Anatomy of the human ovary Figure 16-5 is a sagittal view of the female
Figure 16-5 is a sagittal view of the female Ovary superior
Ovary superior Ovary
Ovary Corpus luteum
Corpus luteum Ovary parts
Ovary parts Ovary labelled
Ovary labelled What is a mature ripened ovary
What is a mature ripened ovary Wandering ovary
Wandering ovary Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Ovary in hibiscus
Ovary in hibiscus Lymphatic drainage of vulva diagram
Lymphatic drainage of vulva diagram Uterus diagram
Uterus diagram Ovary anatomy
Ovary anatomy Ovarian follicle
Ovarian follicle Pollen picks
Pollen picks Flower parts
Flower parts Ovary hormones
Ovary hormones Prostatic urethra
Prostatic urethra Diagrammatic sectional view of ovary
Diagrammatic sectional view of ovary Ovary support formula dr berg
Ovary support formula dr berg Ovary hormones
Ovary hormones Alstroemeria flower labeled
Alstroemeria flower labeled Primary follicle
Primary follicle Flowersexual
Flowersexual Introduction paragraph structure
Introduction paragraph structure L
L Cherry blossom appearance radiology
Cherry blossom appearance radiology What is fetal hydantoin syndrome
What is fetal hydantoin syndrome Wartenburg syndrome
Wartenburg syndrome Kanners syndrome
Kanners syndrome Marfan syndrome face
Marfan syndrome face Karyotyping
Karyotyping Serum osmolarity formula
Serum osmolarity formula Waist circumference
Waist circumference Wernicke-korsakoff syndrome
Wernicke-korsakoff syndrome Ecmo harlequin syndrome
Ecmo harlequin syndrome