Polycystic Ovarian Syndrome Polycystic Ovarian Syndrome Overview Presented








![Srotas: Srotodushti Prakara: • Rasavaha, Raktavaha, Medovaha, Artavavaha [Asthi & Shukra] • Sanga- Growth Srotas: Srotodushti Prakara: • Rasavaha, Raktavaha, Medovaha, Artavavaha [Asthi & Shukra] • Sanga- Growth](https://slidetodoc.com/presentation_image_h2/faff4d09a01c3bcba7b99b48dbe77a69/image-40.jpg)
![Oligomenorrhoea /Amenorrhea Aat. Rv]y n: qat. Rv rj> ]y Anat. Rv dae; Erav «tmag. Oligomenorrhoea /Amenorrhea Aat. Rv]y n: qat. Rv rj> ]y Anat. Rv dae; Erav «tmag.](https://slidetodoc.com/presentation_image_h2/faff4d09a01c3bcba7b99b48dbe77a69/image-44.jpg)





- Slides: 77

Polycystic Ovarian Syndrome
Polycystic Ovarian Syndrome: Overview Presented by Dr. Poonam Choudhary LECTURER P. G. DEPARTMENT OF PRASUTI & STRI ROGA NATIONAL INSTITUTE OF AYURVEDA JAIPUR-302002, RAJASTHAN, INDIA

? Why this topic …? ? ?
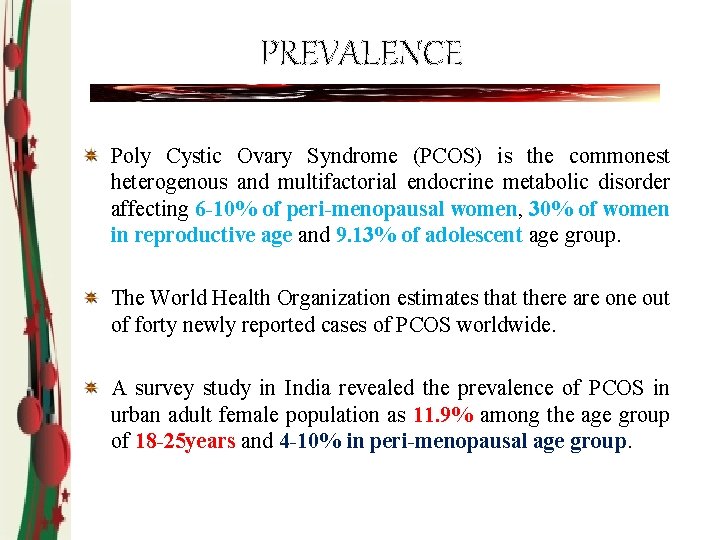
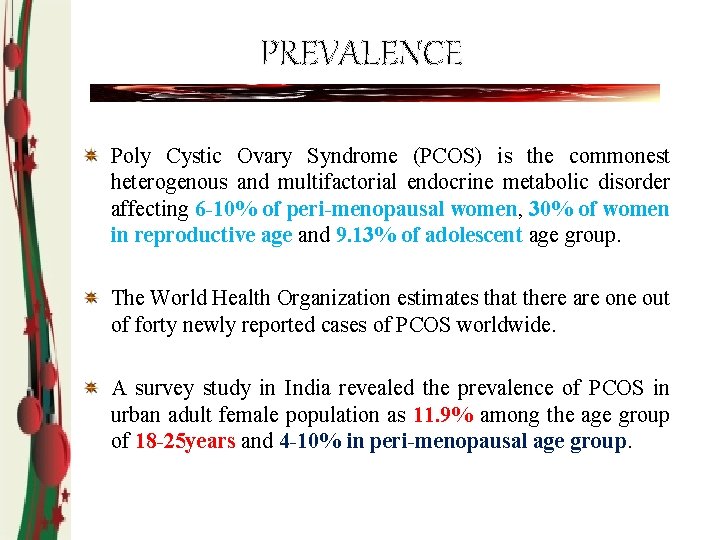
PREVALENCE Poly Cystic Ovary Syndrome (PCOS) is the commonest heterogenous and multifactorial endocrine metabolic disorder affecting 6 -10% of peri-menopausal women, 30% of women in reproductive age and 9. 13% of adolescent age group. The World Health Organization estimates that there are one out of forty newly reported cases of PCOS worldwide. A survey study in India revealed the prevalence of PCOS in urban adult female population as 11. 9% among the age group of 18 -25 years and 4 -10% in peri-menopausal age group.
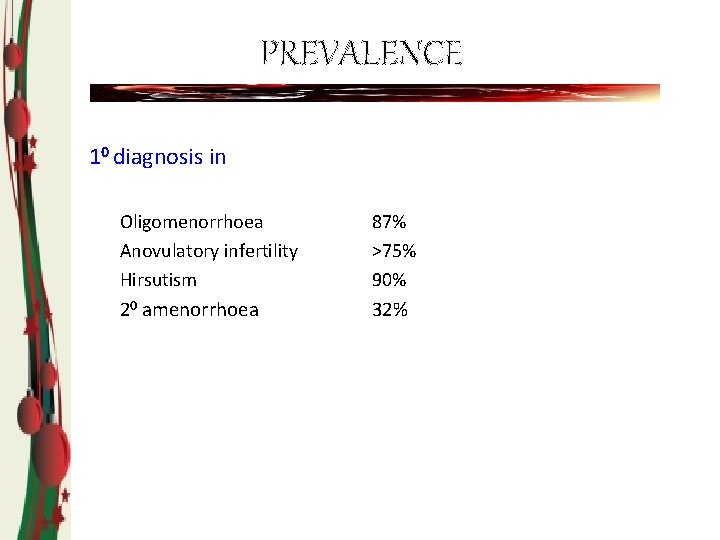
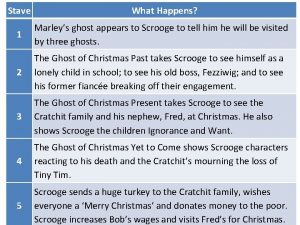
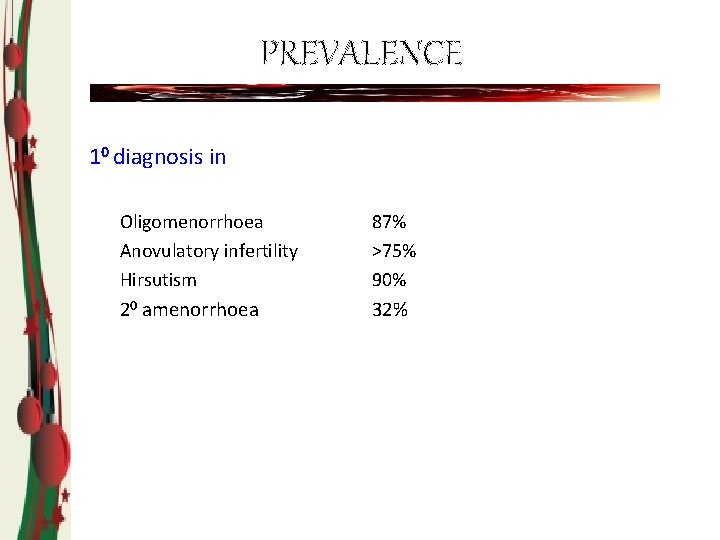
PREVALENCE 10 diagnosis in Oligomenorrhoea Anovulatory infertility Hirsutism 87% >75% 90% 20 amenorrhoea 32%
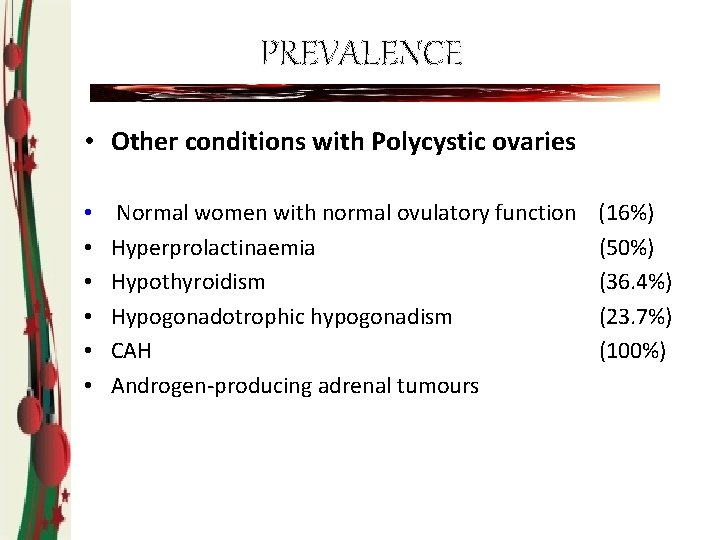
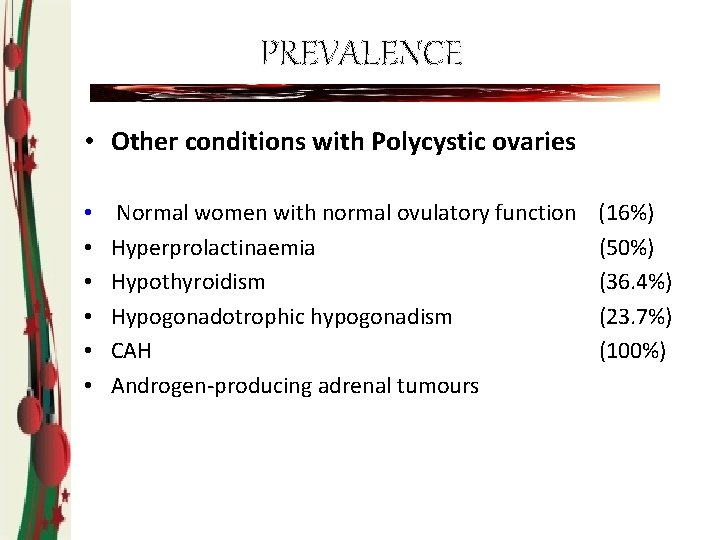
PREVALENCE • Other conditions with Polycystic ovaries • • • Normal women with normal ovulatory function Hyperprolactinaemia Hypothyroidism Hypogonadotrophic hypogonadism CAH Androgen-producing adrenal tumours (16%) (50%) (36. 4%) (23. 7%) (100%)
Peak incidence rate in high level due to. Faulty dietary habits & lifestyle, rapid urbanization, excessive work load etc. and individual error like self negligence, shame, hesitation to submit to doctor etc.

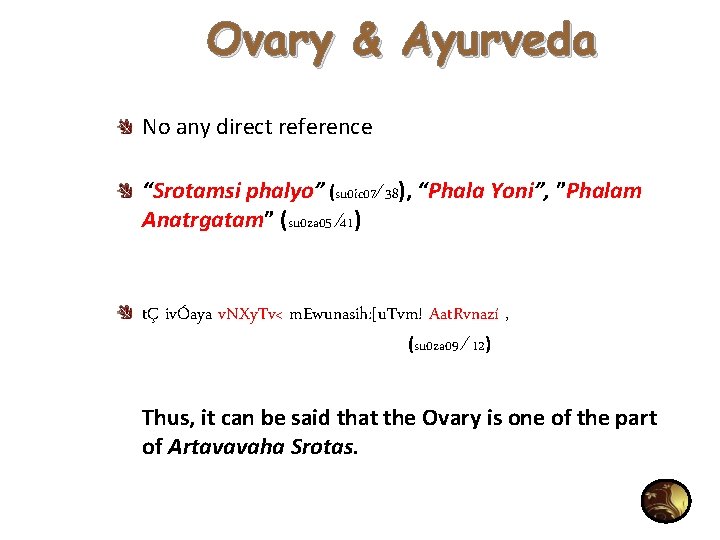
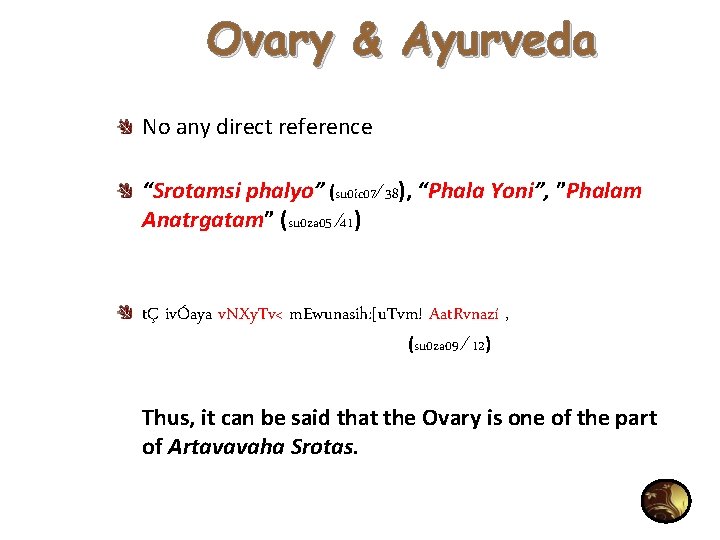
Ovary & Ayurveda No any direct reference “Srotamsi phalyo” (su 0 ic 07∕ 38), “Phala Yoni”, ”Phalam Anatrgatam” (su 0 za 05 ∕ 41) tÇ ivÓaya v. NXy. Tv< m. Ewunasih: [u. Tvm! Aat. Rvnazí , (su 0 za 09 ∕ 12) Thus, it can be said that the Ovary is one of the part of Artavavaha Srotas.
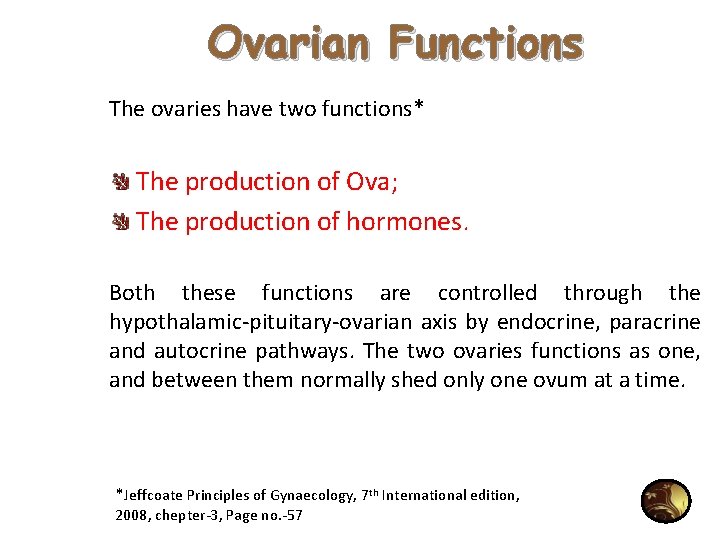
Ovarian Functions The ovaries have two functions* The production of Ova; The production of hormones. Both these functions are controlled through the hypothalamic-pituitary-ovarian axis by endocrine, paracrine and autocrine pathways. The two ovaries functions as one, and between them normally shed only one ovum at a time. *Jeffcoate Principles of Gynaecology, 7 th International edition, 2008, chepter-3, Page no. -57
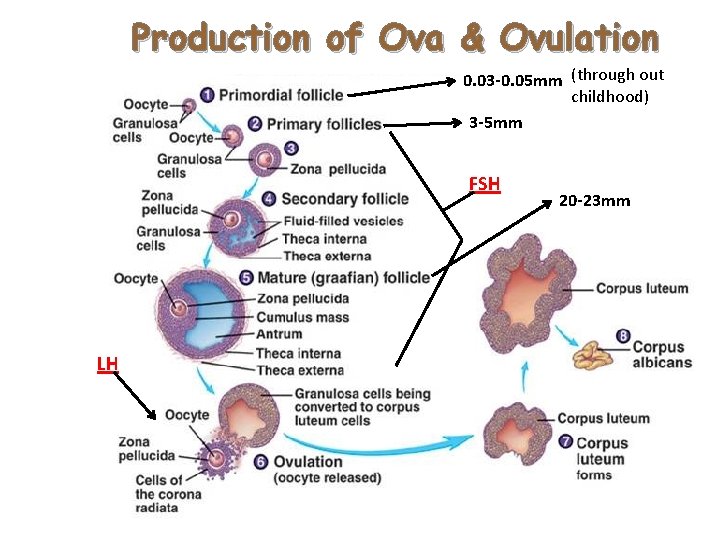
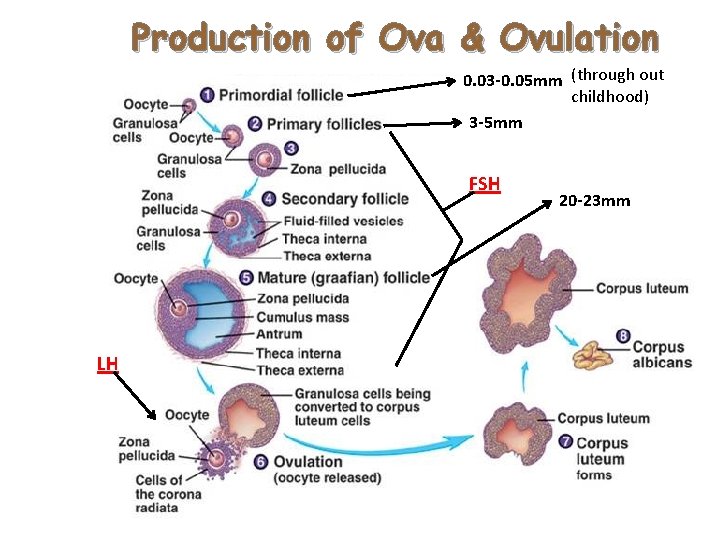
Production of Ova & Ovulation 0. 03 -0. 05 mm (through out childhood) 3 -5 mm FSH LH 20 -23 mm
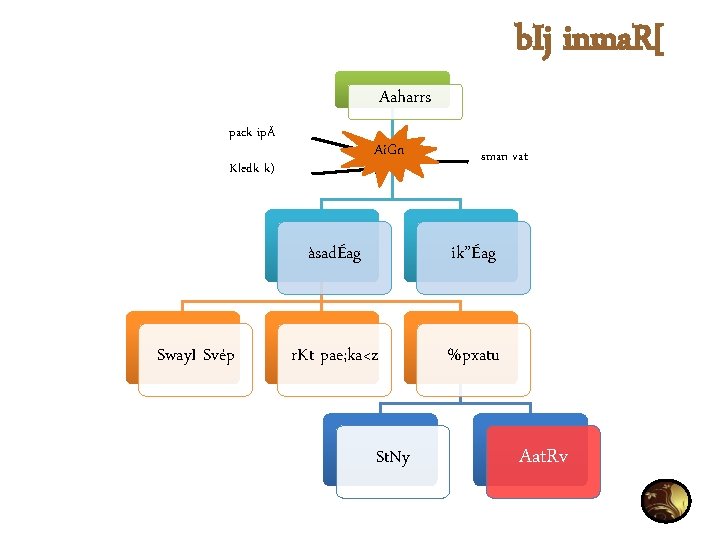
b. Ij inma. R[ Aaharrs pack ipÄ Ai. Gn Kledk k) Sway. I Svép sman vat àsadÉag ik”Éag r. Kt pae; ka<z %pxatu St. Ny Aat. Rv
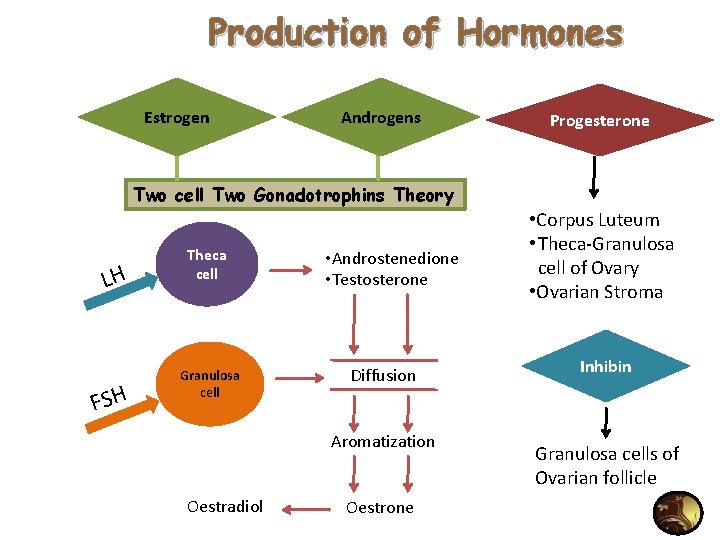
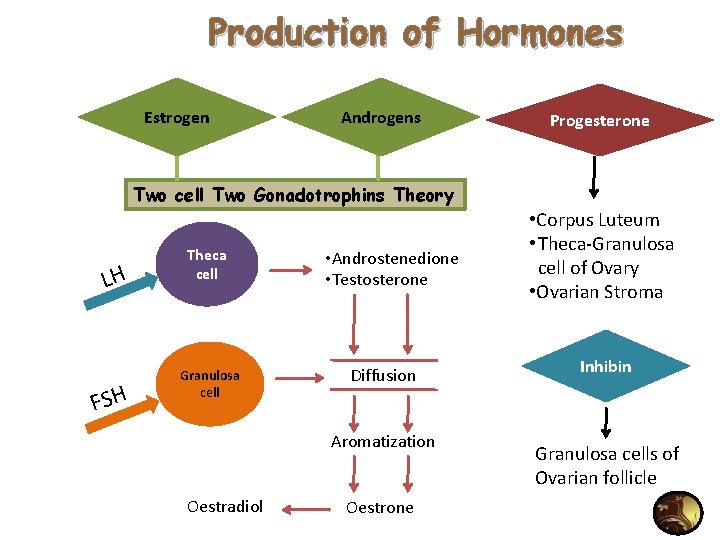
Production of Hormones Estrogen Androgens Progesterone Two cell Two Gonadotrophins Theory LH FSH Theca cell Granulosa cell • Androstenedione • Testosterone Diffusion Aromatization Oestradiol Oestrone • Corpus Luteum • Theca-Granulosa cell of Ovary • Ovarian Stroma Inhibin Granulosa cells of Ovarian follicle
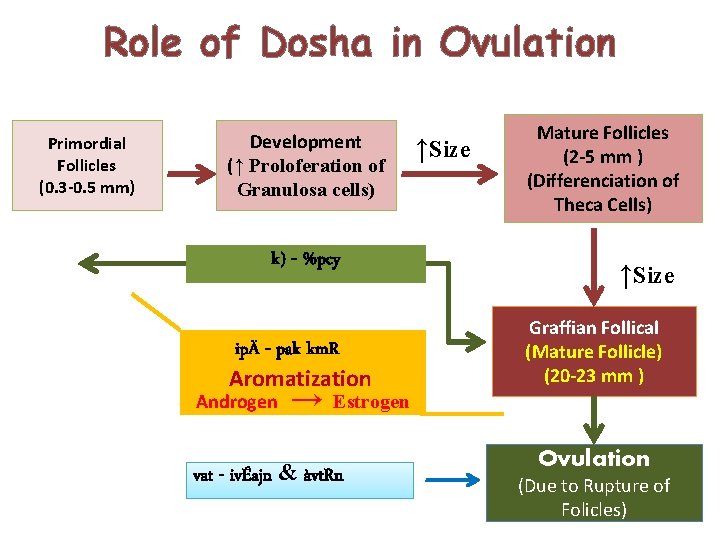
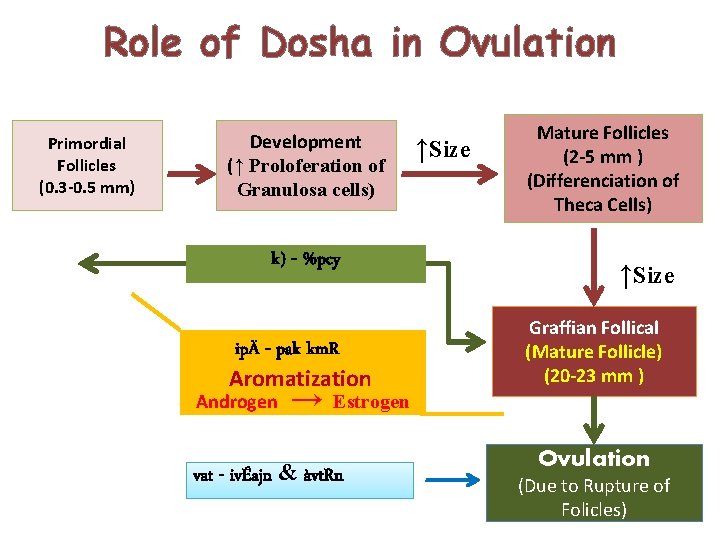
Role of Dosha in Ovulation Primordial Follicles (0. 3 -0. 5 mm) Development (↑ Proloferation of Granulosa cells) k) - %pcy ipÄ - pak km. R Aromatization Androgen → ↑Size Mature Follicles (2 -5 mm ) (Differenciation of Theca Cells) ↑Size Graffian Follical (Mature Follicle) (20 -23 mm ) Estrogen vat - ivÉajn & àvt. Rn Ovulation (Due to Rupture of Folicles)
Etiology • A large number of genomic variants has been associated with PCOS and many of these associations have not been replicated in different populations. • It is believed that the picture is of a multigenic etiology in which non-genetic factors such as diet and exercise have strong influence on the development of the disorder
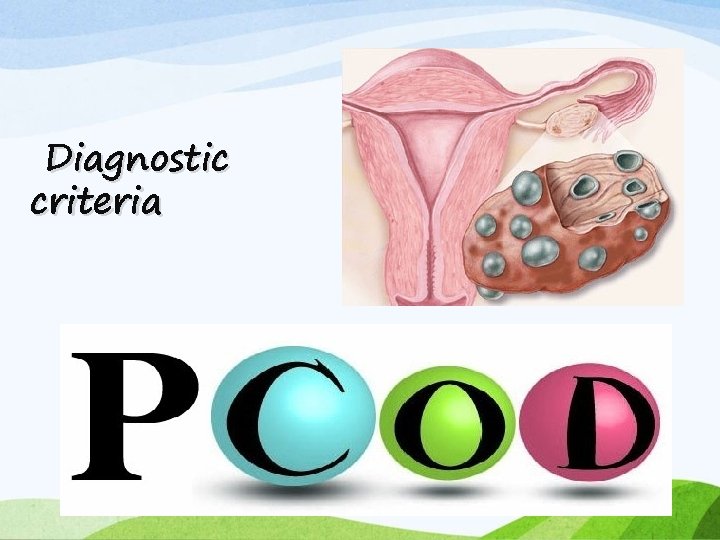
Diagnostic criteria
• Classic syndrome originally described by Stein and Levanthal (1935) • • Hyperandrogenism Menstrual irregularity Polycystic ovaries Central adiposity • Few of these original features are now considered consistent findings in PCOS
• Sonographic picture of PCO was also found with other metabolic findings and sometimes with less other symptoms. So, it was then known as PCOD- Poly Cystic Ovarian Disease.
NATIONAL INSTITUTES OF HEALTH AND CHILD HEALTH AND HUMAN DEVELOPMENT(1990) • Chronic anovulation • Hyperandrogenemia • Clinical signs of hyperandrogenism • Exclusion of other androgenic disorders

ROTTERDAM CRITERIA (2003) ESHRE (European Society for Human Reproduction) & ASRM (American Society of Reproductive Medicine) 2 out of 3 • Polycystic ovaries (>12 peripheral follicles or increased ovarian volume >10 cm 3) • Oligo- or anovulation • Clinical and/or biochemical signs of hyperandrogenism • And exclusion of other etiologies such as hypothyroidism, hyperprolactinemia, congenital adrenal hyperplasia, cushing syndrome, androgen secreting tumors
AE-PCOS SOCIETY 2006 • Hyperandrogenism-hirsutism and/ or hyperandrogenemia • And • Ovarian dysfunction-oligo-anovulation and/ or polycystic ovaries • Exclusion of other androgen excess or related disorders
pathogenesis
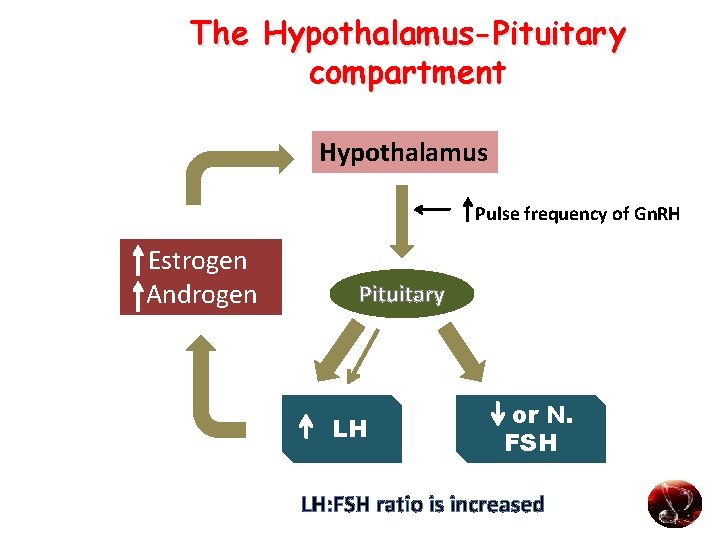
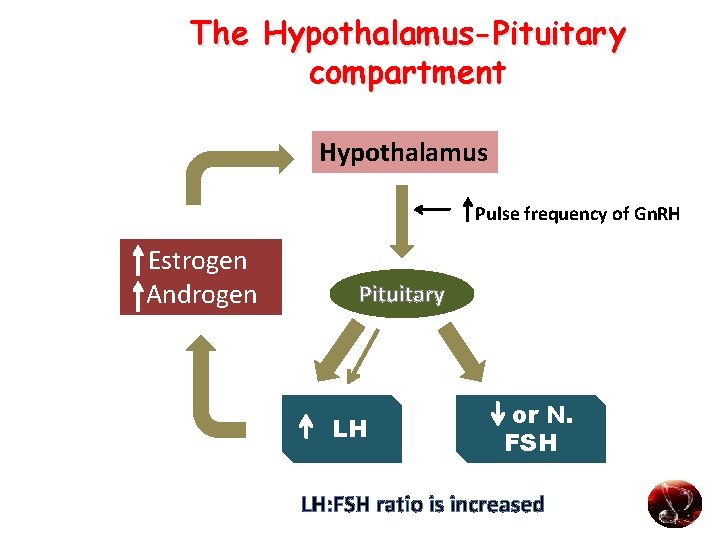
The Hypothalamus-Pituitary compartment Hypothalamus Pulse frequency of Gn. RH Estrogen Androgen Pituitary LH or N. FSH LH: FSH ratio is increased
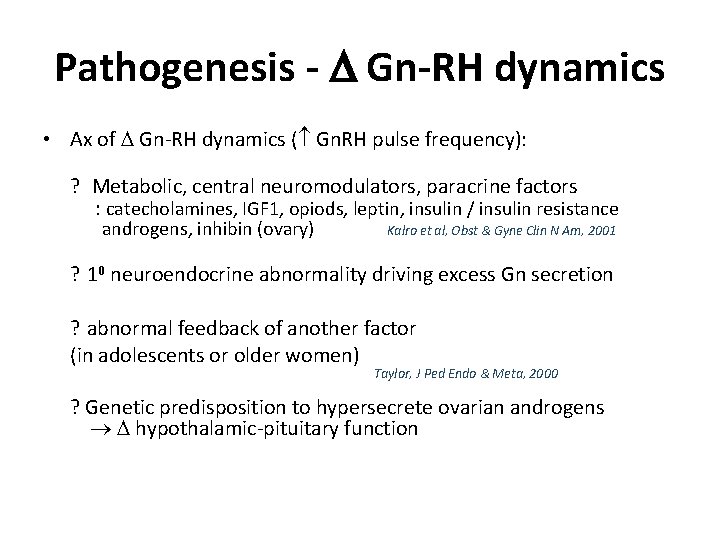
Pathogenesis - Gn-RH dynamics • Ax of Gn-RH dynamics ( Gn. RH pulse frequency): ? Metabolic, central neuromodulators, paracrine factors : catecholamines, IGF 1, opiods, leptin, insulin / insulin resistance androgens, inhibin (ovary) Kalro et al, Obst & Gyne Clin N Am, 2001 ? 10 neuroendocrine abnormality driving excess Gn secretion ? abnormal feedback of another factor (in adolescents or older women) Taylor, J Ped Endo & Meta, 2000 ? Genetic predisposition to hypersecrete ovarian androgens hypothalamic-pituitary function
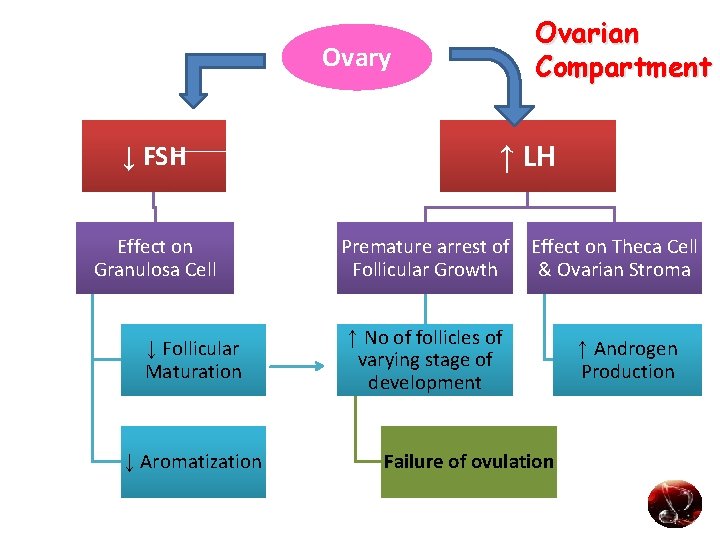
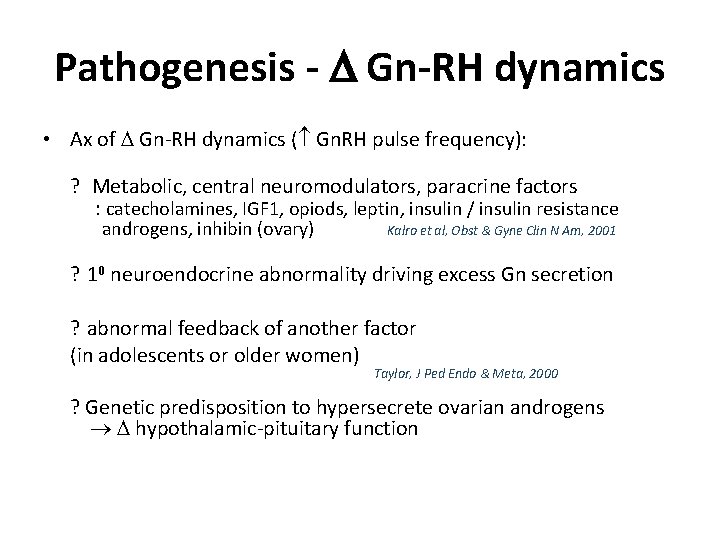
Ovarian Compartment Ovary ↓ FSH Effect on Granulosa Cell ↓ Follicular Maturation ↓ Aromatization ↑ LH Premature arrest of Follicular Growth Effect on Theca Cell & Ovarian Stroma ↑ No of follicles of varying stage of development Failure of ovulation ↑ Androgen Production
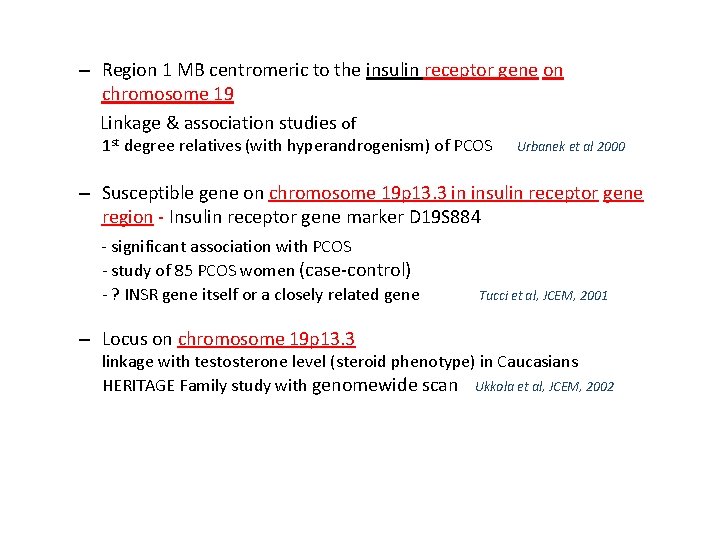
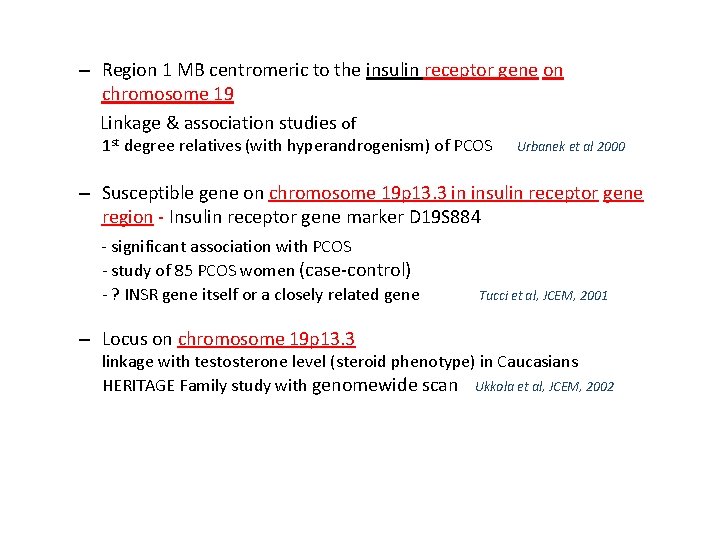
– Region 1 MB centromeric to the insulin receptor gene on chromosome 19 Linkage & association studies of 1 st degree relatives (with hyperandrogenism) of PCOS Urbanek et al 2000 – Susceptible gene on chromosome 19 p 13. 3 in insulin receptor gene region - Insulin receptor gene marker D 19 S 884 - significant association with PCOS - study of 85 PCOS women (case-control) - ? INSR gene itself or a closely related gene – Locus on chromosome 19 p 13. 3 Tucci et al, JCEM, 2001 linkage with testosterone level (steroid phenotype) in Caucasians HERITAGE Family study with genomewide scan Ukkola et al, JCEM, 2002
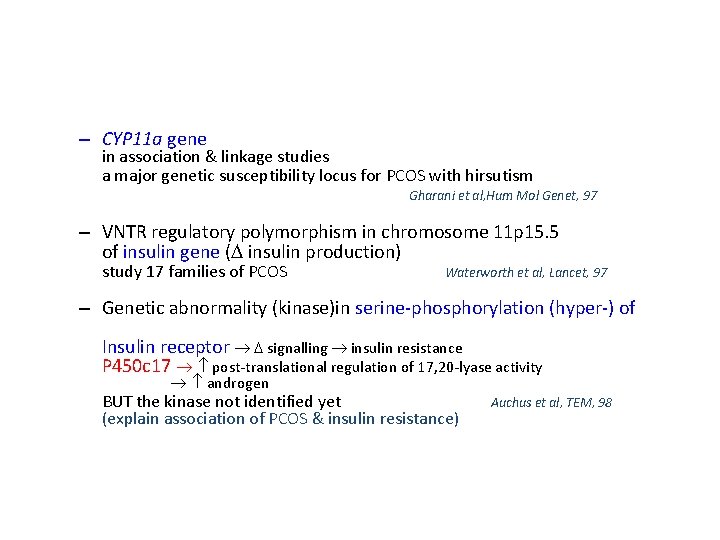
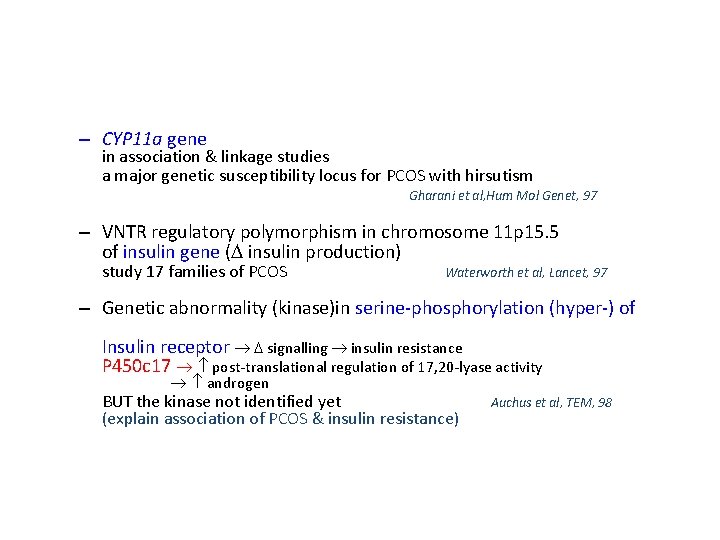
– CYP 11 a gene in association & linkage studies a major genetic susceptibility locus for PCOS with hirsutism Gharani et al, Hum Mol Genet, 97 – VNTR regulatory polymorphism in chromosome 11 p 15. 5 of insulin gene ( insulin production) study 17 families of PCOS Waterworth et al, Lancet, 97 – Genetic abnormality (kinase)in serine-phosphorylation (hyper-) of Insulin receptor signalling insulin resistance P 450 c 17 post-translational regulation of 17, 20 -lyase activity androgen BUT the kinase not identified yet (explain association of PCOS & insulin resistance) Auchus et al, TEM, 98
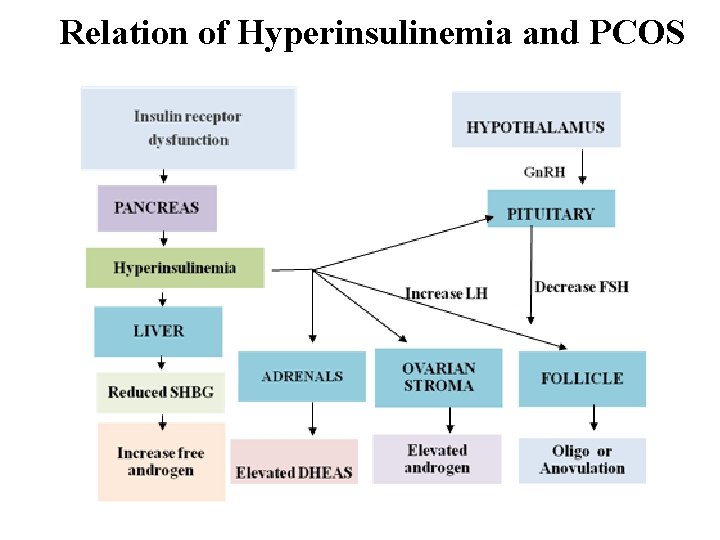
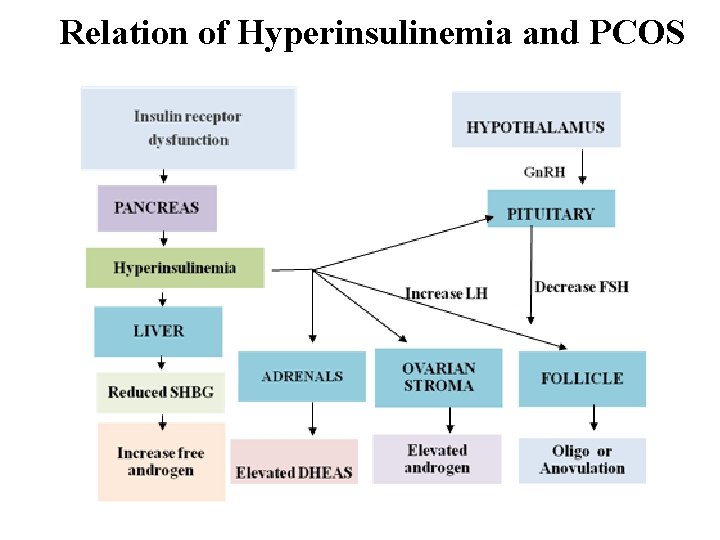
Relation of Hyperinsulinemia and PCOS
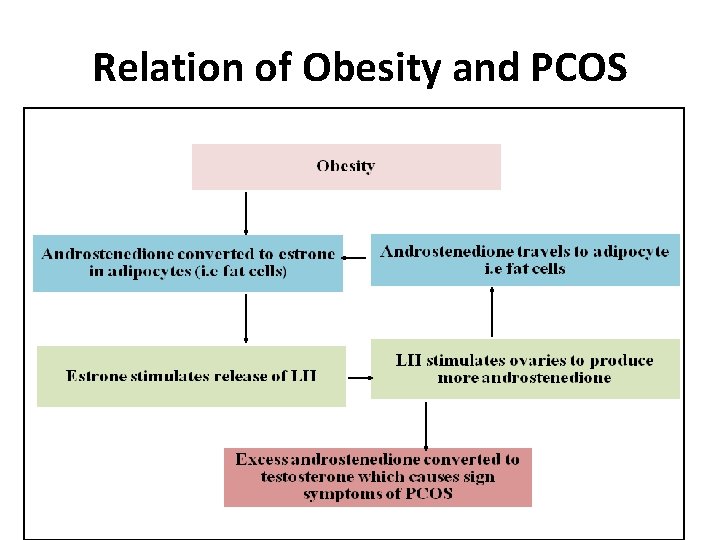
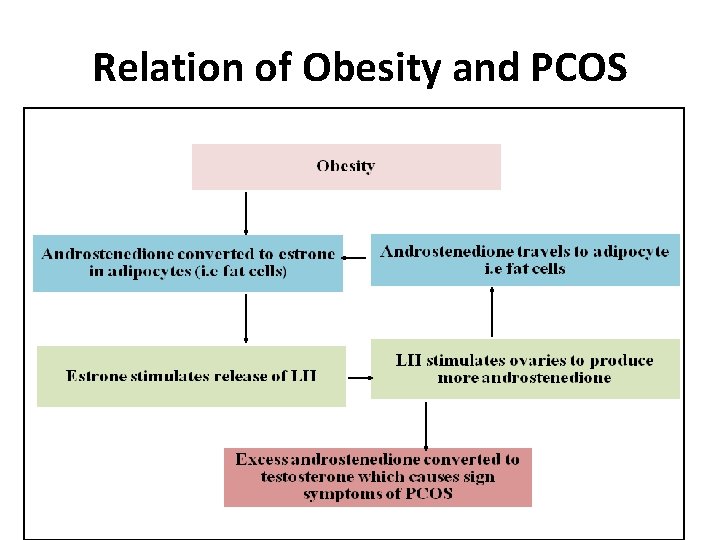
Relation of Obesity and PCOS
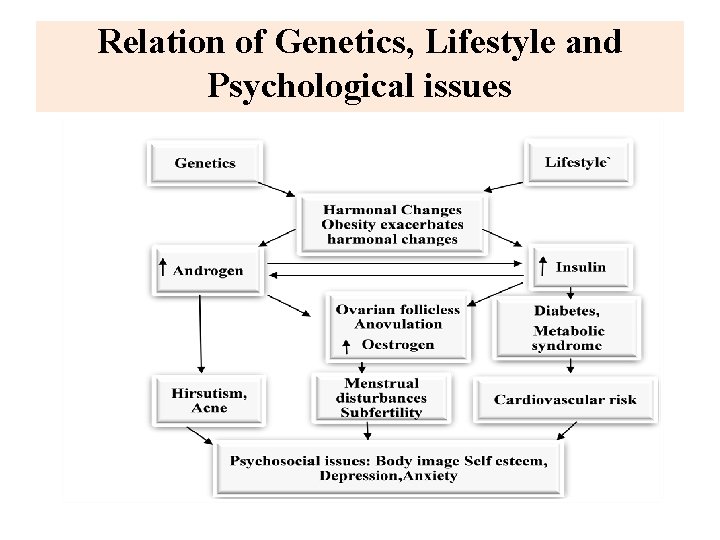
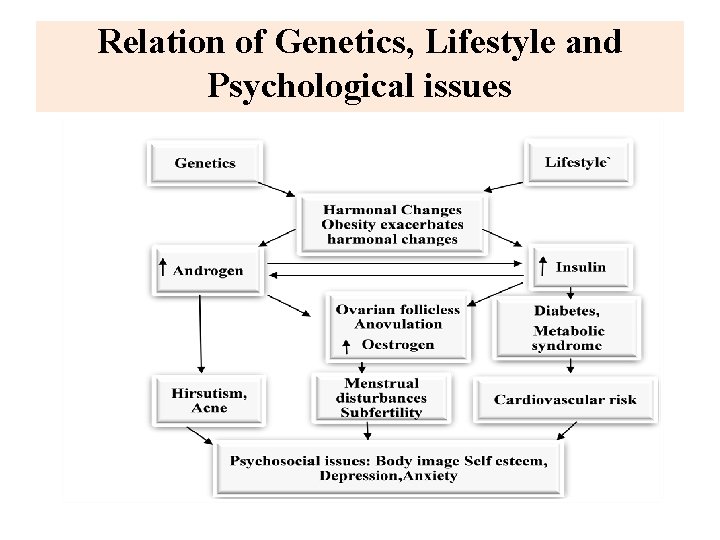
Relation of Genetics, Lifestyle and Psychological issues
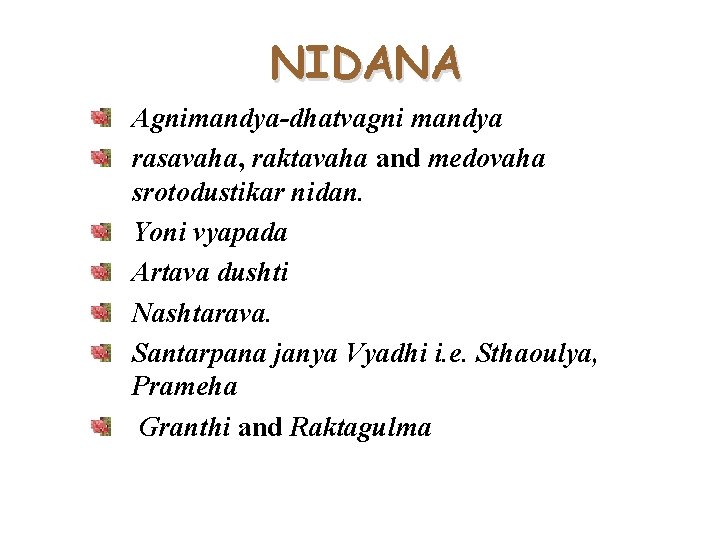
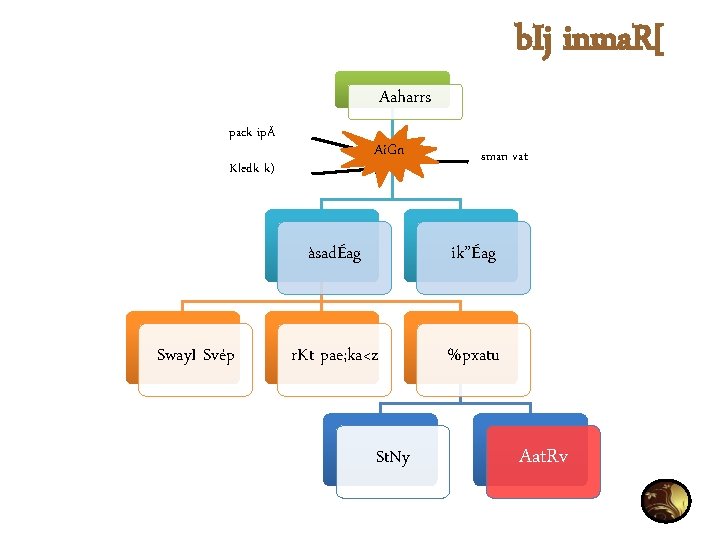
NIDANA Agnimandya-dhatvagni mandya rasavaha, raktavaha and medovaha srotodustikar nidan. Yoni vyapada Artava dushti Nashtarava. Santarpana janya Vyadhi i. e. Sthaoulya, Prameha Granthi and Raktagulma



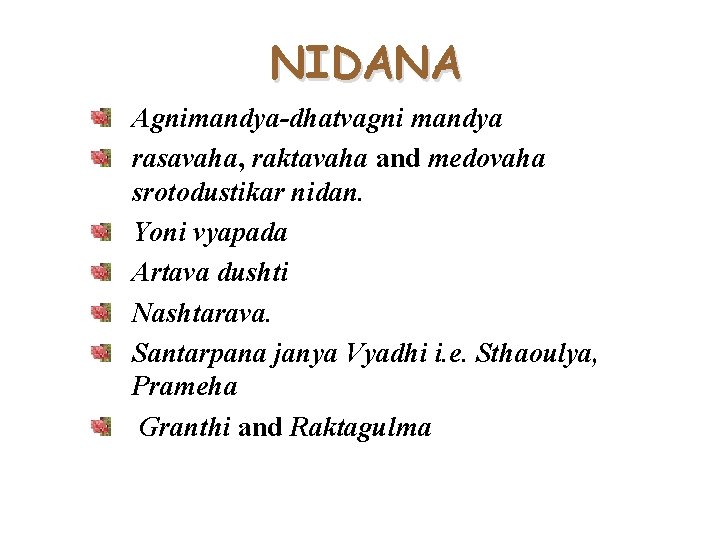
Nidana
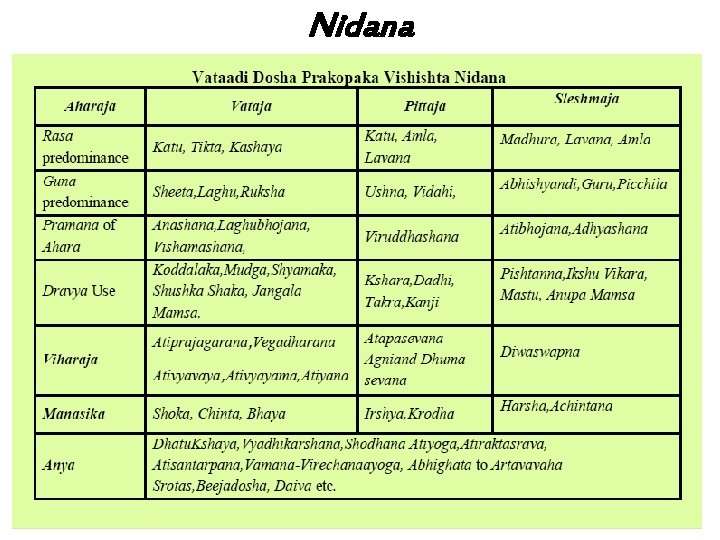
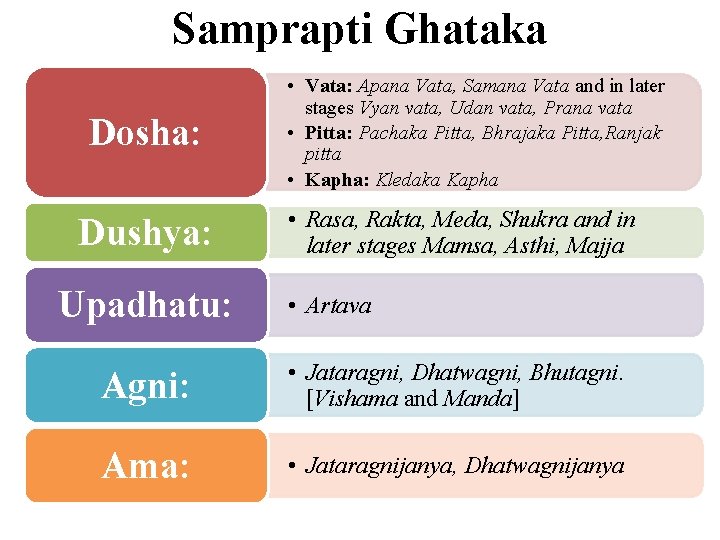
Pathophysiology of PCOS

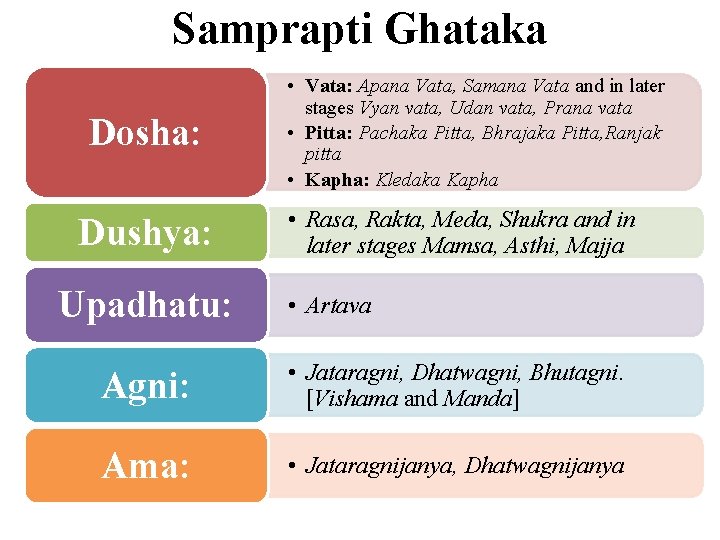
Samprapti Ghataka Dosha: Dushya: Upadhatu: • Vata: Apana Vata, Samana Vata and in later stages Vyan vata, Udan vata, Prana vata • Pitta: Pachaka Pitta, Bhrajaka Pitta, Ranjak pitta • Kapha: Kledaka Kapha • Rasa, Rakta, Meda, Shukra and in later stages Mamsa, Asthi, Majja • Artava Agni: • Jataragni, Dhatwagni, Bhutagni. [Vishama and Manda] Ama: • Jataragnijanya, Dhatwagnijanya
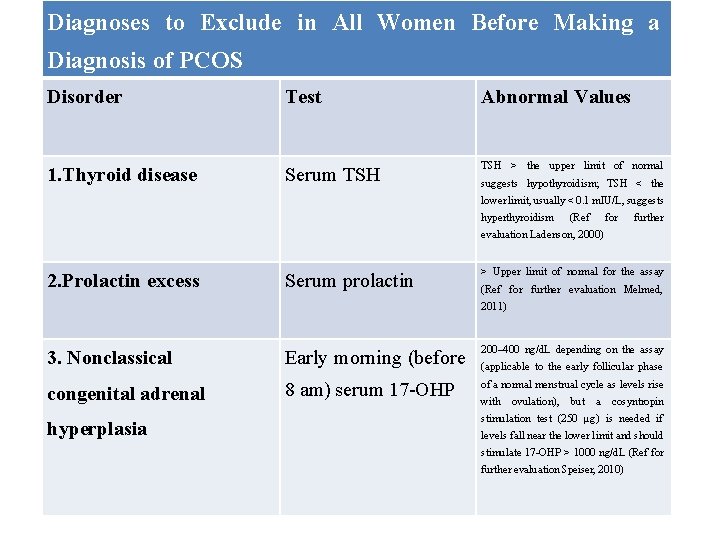
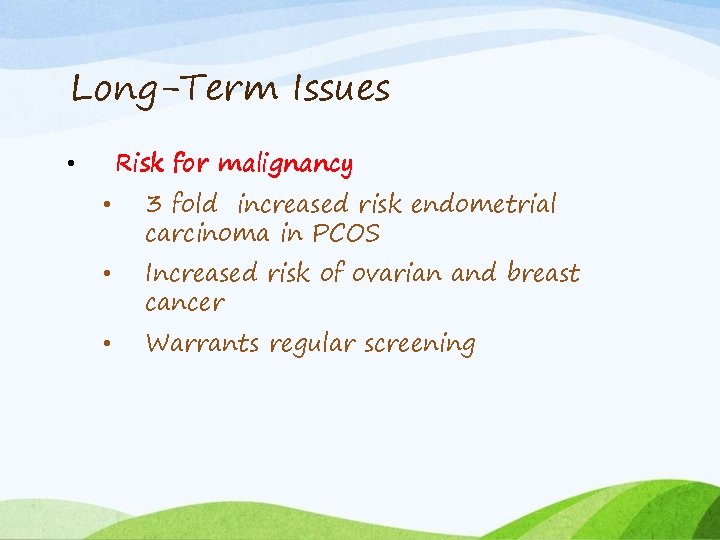
![Srotas Srotodushti Prakara Rasavaha Raktavaha Medovaha Artavavaha Asthi Shukra Sanga Growth Srotas: Srotodushti Prakara: • Rasavaha, Raktavaha, Medovaha, Artavavaha [Asthi & Shukra] • Sanga- Growth](https://slidetodoc.com/presentation_image_h2/faff4d09a01c3bcba7b99b48dbe77a69/image-40.jpg)
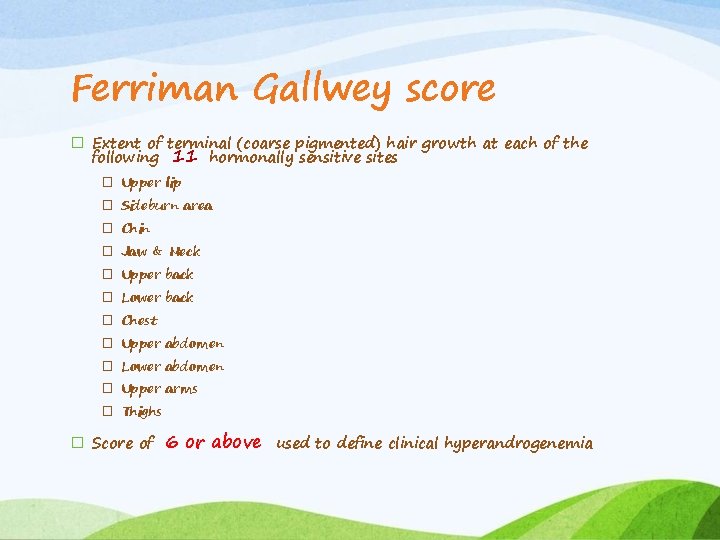
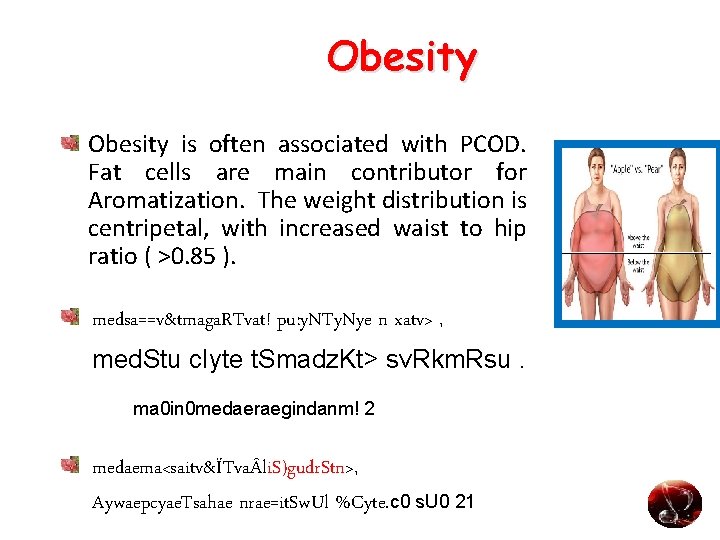
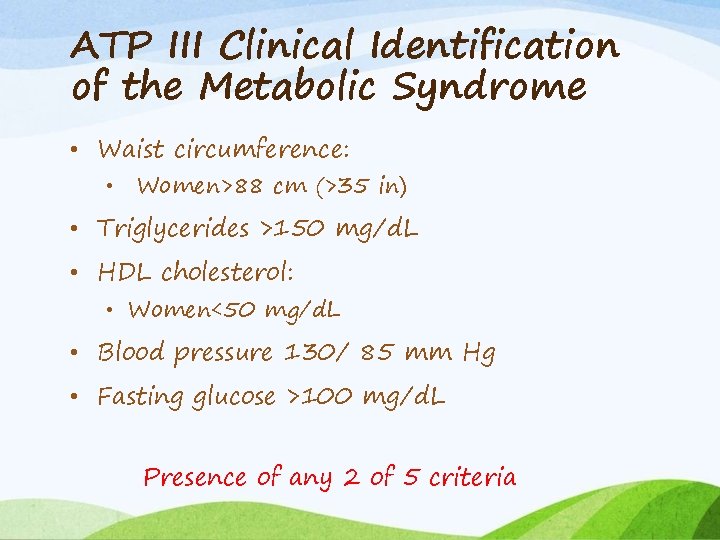
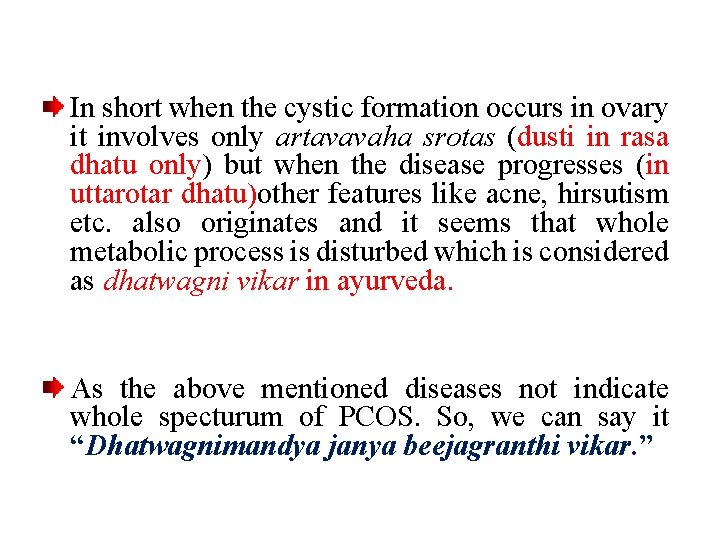
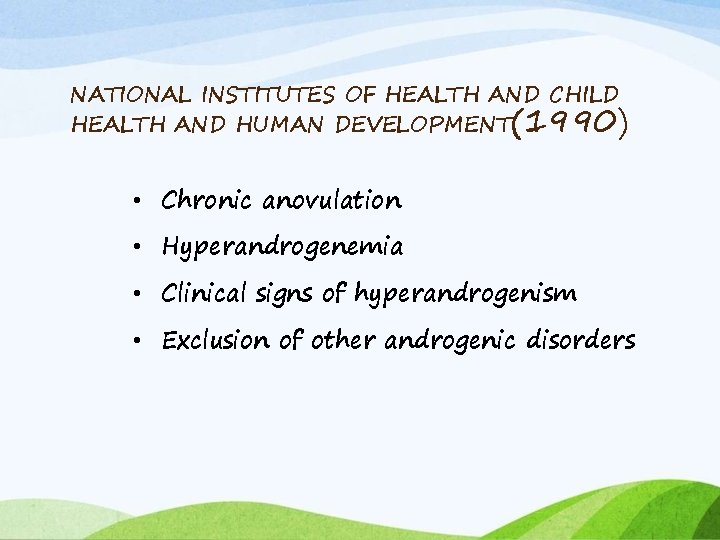
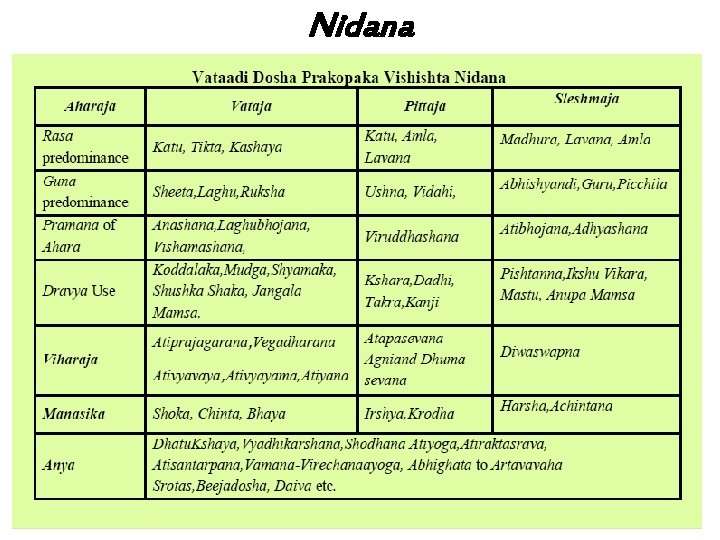
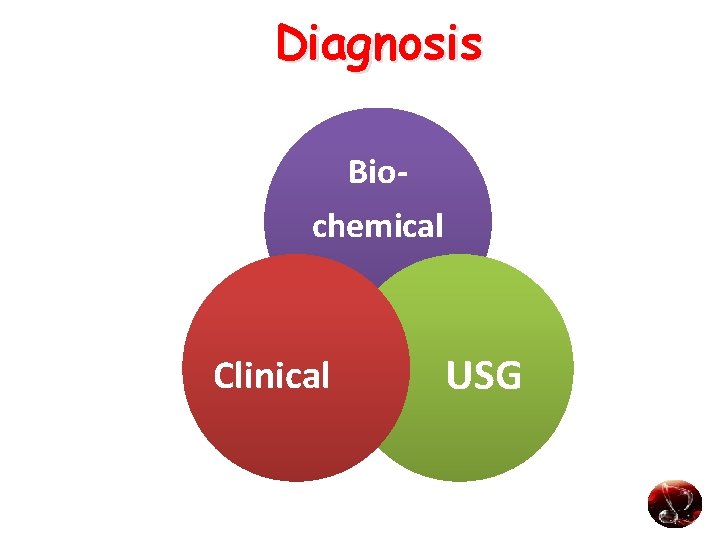
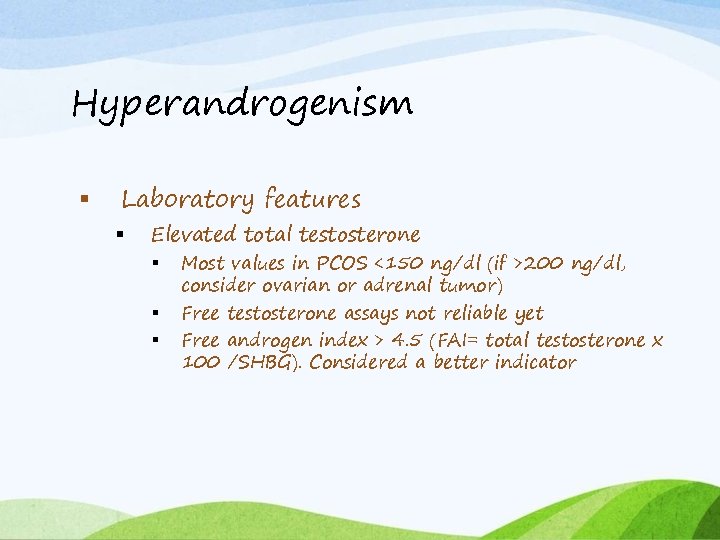
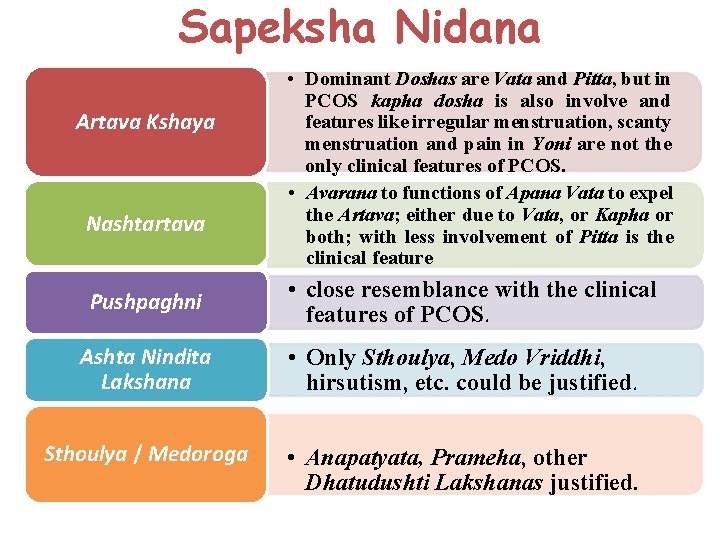
Srotas: Srotodushti Prakara: • Rasavaha, Raktavaha, Medovaha, Artavavaha [Asthi & Shukra] • Sanga- Growth & development of follicle and release of ovum, and menstrual blood. • Siragranthi- Cysts in Ovaries. • Atipravritti- Asrigdara.
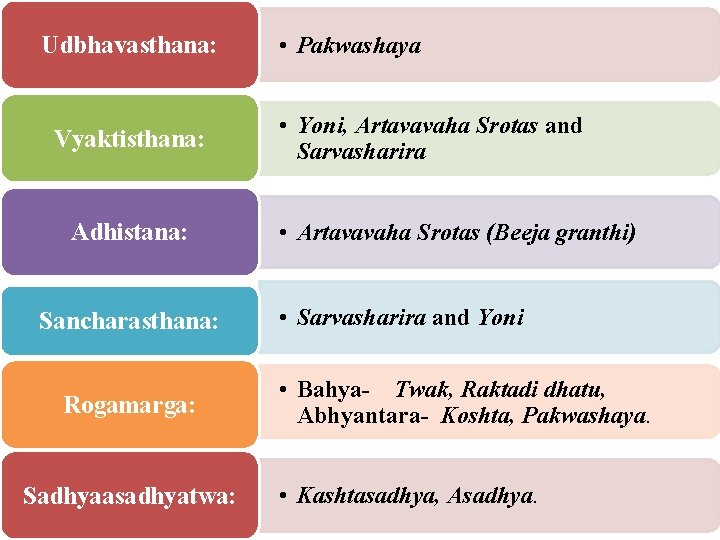
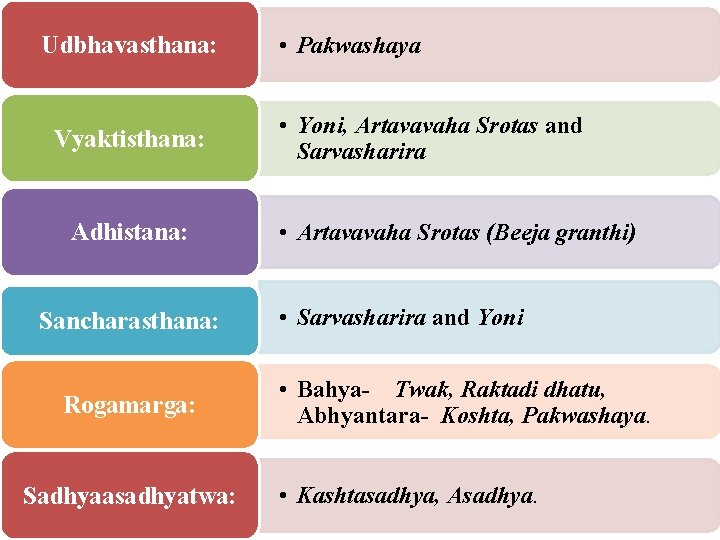
Udbhavasthana: Vyaktisthana: Adhistana: Sancharasthana: Rogamarga: Sadhyaasadhyatwa: • Pakwashaya • Yoni, Artavavaha Srotas and Sarvasharira • Artavavaha Srotas (Beeja granthi) • Sarvasharira and Yoni • Bahya- Twak, Raktadi dhatu, Abhyantara- Koshta, Pakwashaya. • Kashtasadhya, Asadhya.
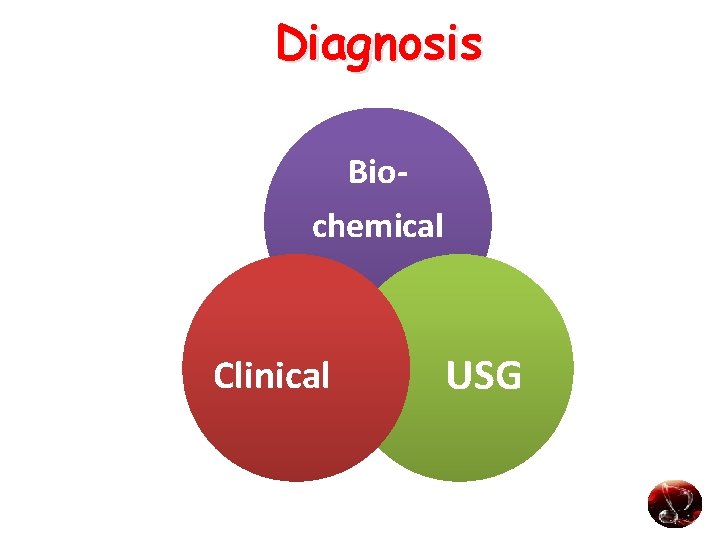
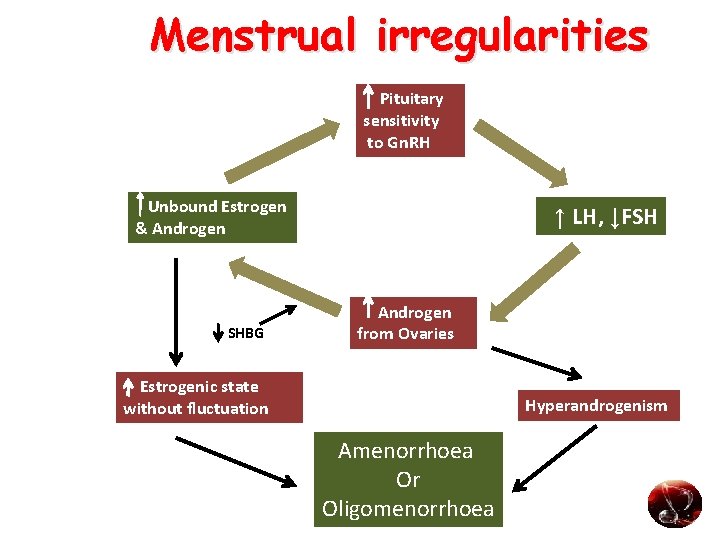
Diagnosis Biochemical Clinical USG
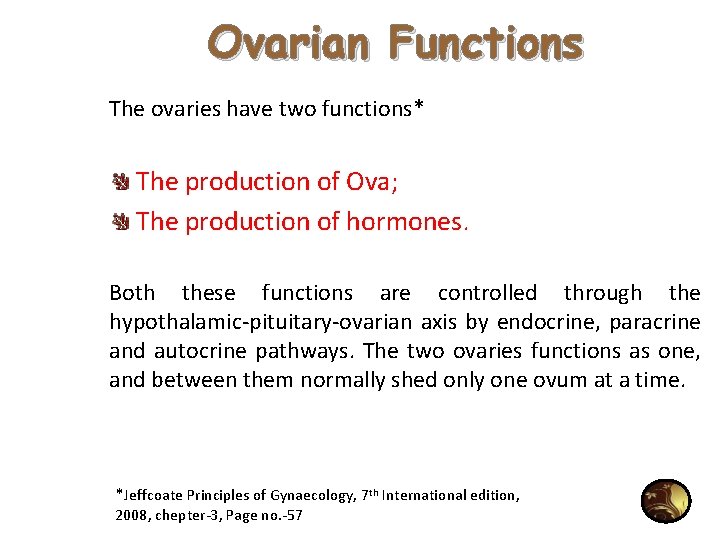
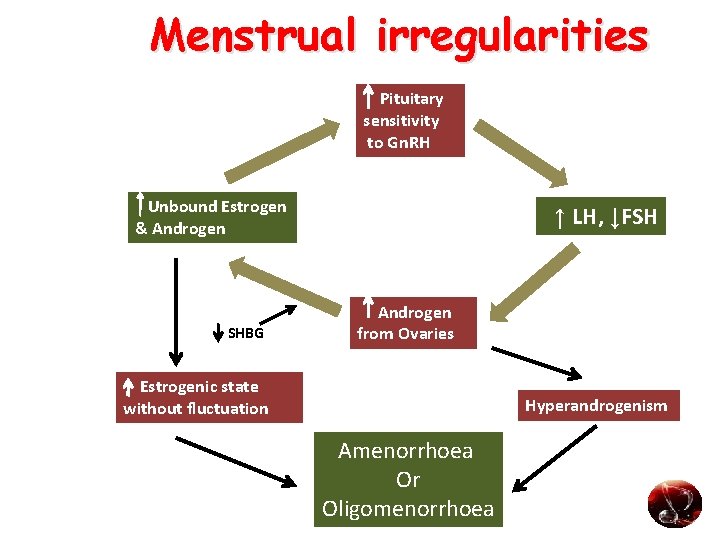
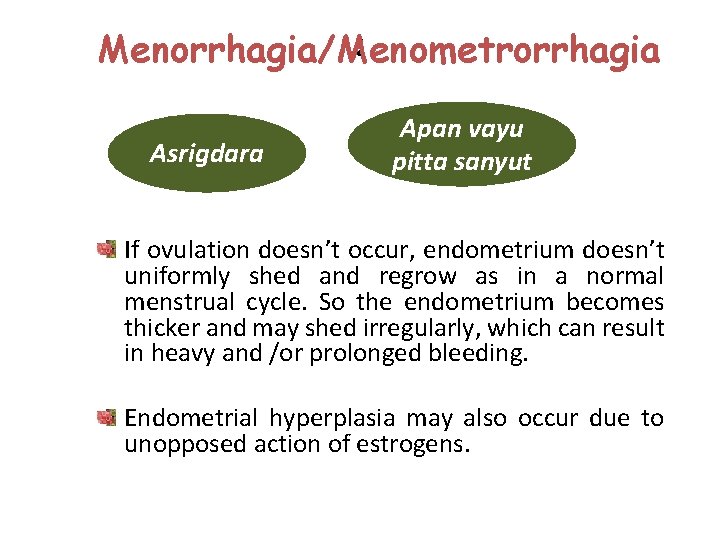
Menstrual irregularities Pituitary sensitivity to Gn. RH Unbound Estrogen & Androgen SHBG ↑ LH, ↓FSH Androgen from Ovaries Estrogenic state without fluctuation Hyperandrogenism Amenorrhoea Or Oligomenorrhoea
![Oligomenorrhoea Amenorrhea Aat Rvy n qat Rv rj y Anat Rv dae Erav tmag Oligomenorrhoea /Amenorrhea Aat. Rv]y n: qat. Rv rj> ]y Anat. Rv dae; Erav «tmag.](https://slidetodoc.com/presentation_image_h2/faff4d09a01c3bcba7b99b48dbe77a69/image-44.jpg)
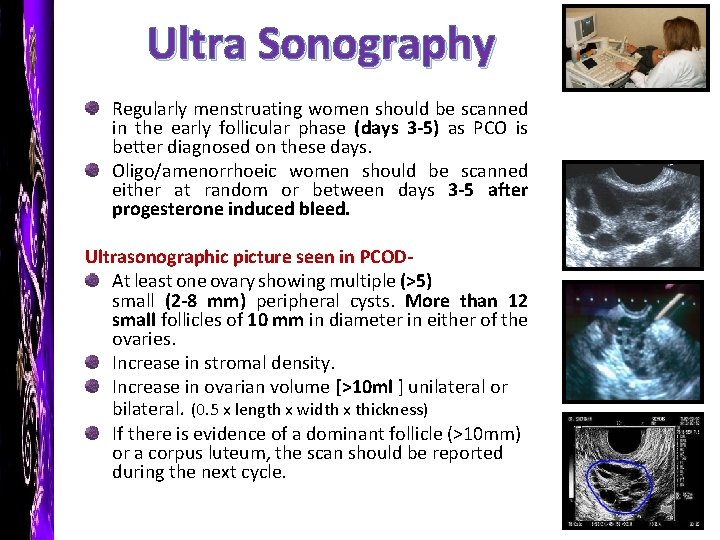
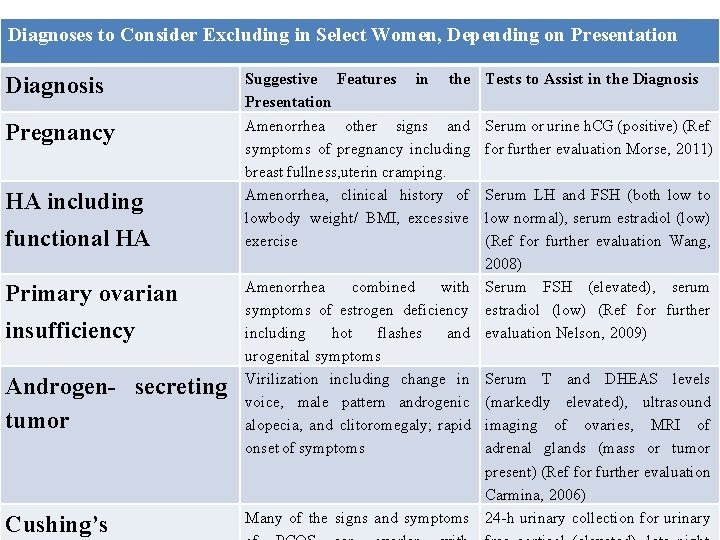
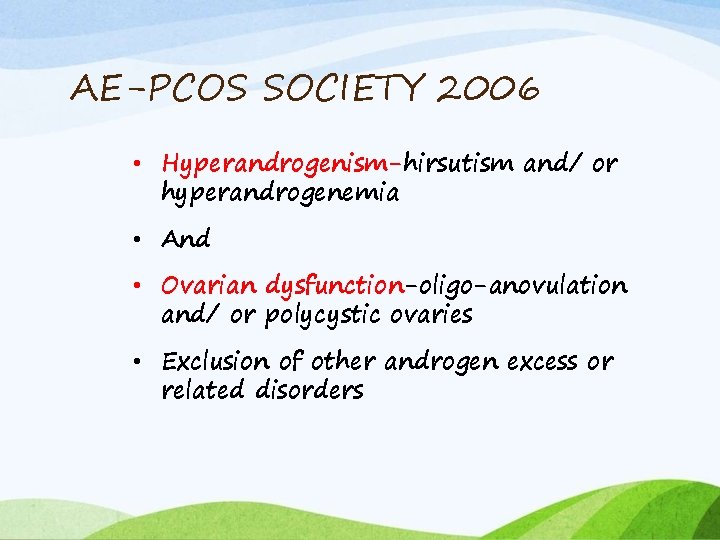
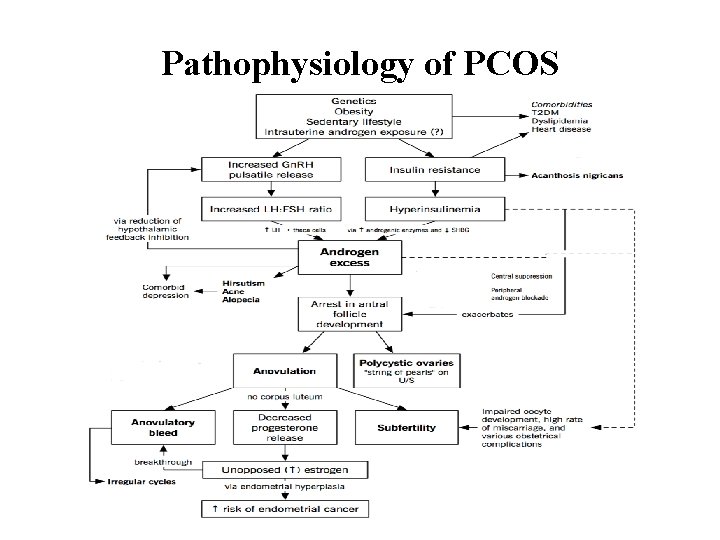
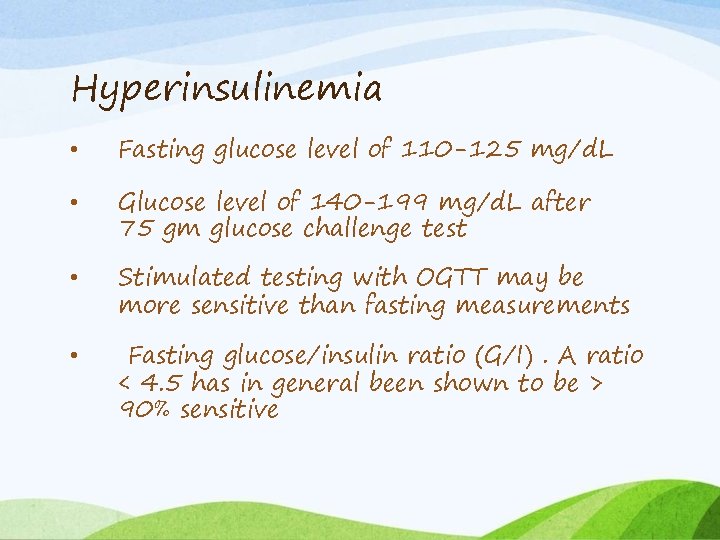
Oligomenorrhoea /Amenorrhea Aat. Rv]y n: qat. Rv rj> ]y Anat. Rv dae; Erav «tmag. RTvadat. Rv< n. Zyit iöya> , suˆ zaˆ 2/ ∕ 21 AÇ dae; a> k)ae vayu> vatk)a. E c , f. Lh[ n. Zyt. Iit< àvt. Rman< n ÔZyte, n tu sv. Rwa ]y< yait , f. Lh[ vkr. Zo{k; s ; Fkksfprdkykn'k. Zue. Yirk ok ; ksfuosnuk p--(lq-'kkr= fo)k; k o. U? ; Roa e. SFkquklfg". kq. Roe~ vkr. Zouk'kÜp. A
: Menorrhagia/Menometrorrhagia Asrigdara Apan vayu pitta sanyut If ovulation doesn’t occur, endometrium doesn’t uniformly shed and regrow as in a normal menstrual cycle. So the endometrium becomes thicker and may shed irregularly, which can result in heavy and /or prolonged bleeding. Endometrial hyperplasia may also occur due to unopposed action of estrogens.
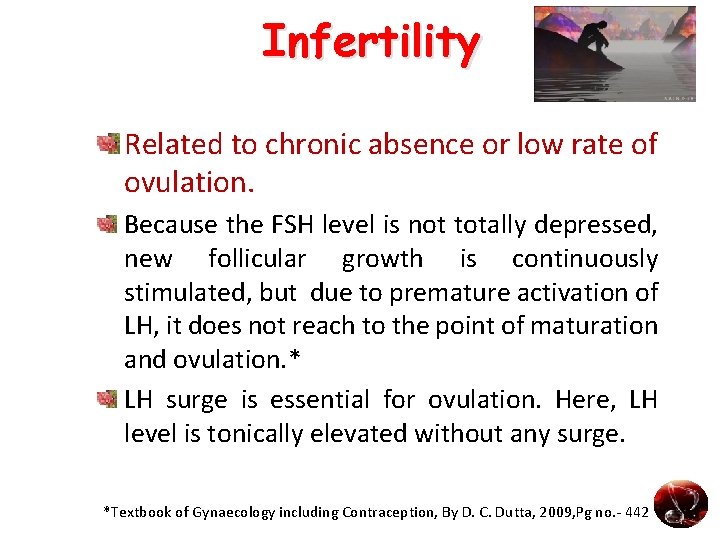
Infertility Related to chronic absence or low rate of ovulation. Because the FSH level is not totally depressed, new follicular growth is continuously stimulated, but due to premature activation of LH, it does not reach to the point of maturation and ovulation. * LH surge is essential for ovulation. Here, LH level is tonically elevated without any surge. *Textbook of Gynaecology including Contraception, By D. C. Dutta, 2009, Pg no. - 442
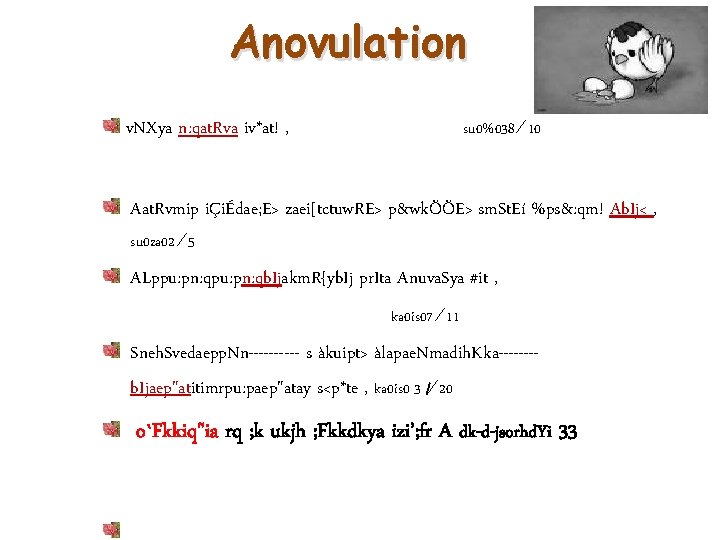
Anovulation su 0%038 ∕ 10 v. NXya n: qat. Rva iv*at! , Aat. Rvmip iÇiÉdae; E> zaei[tctuw. RE> p&wkÖÖE> sm. St. Eí %ps&: qm! Ab. Ij< , su 0 za 02 ∕ 5 ALppu: pn: qb. Ijakm. R{yb. Ij pr. Ita Anuva. Sya #it , ka 0 is 07 ∕ 11 Sneh. Svedaepp. Nn----- s àkuipt> àlapae. Nmadih. Kka-------b. Ijaep"atitimrpu: paep"atay s<p*te , ka 0 is 0 3 /∕ 20 o`Fkkiq"ia rq ; k ukjh ; Fkkdkya izi’; fr A dk-d-jsorhd. Yi 33
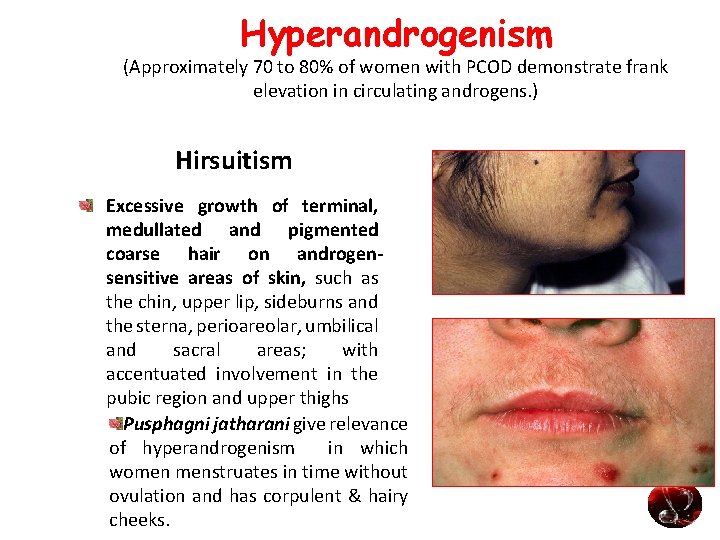
Hyperandrogenism (Approximately 70 to 80% of women with PCOD demonstrate frank elevation in circulating androgens. ) Hirsuitism Excessive growth of terminal, medullated and pigmented coarse hair on androgensensitive areas of skin, such as the chin, upper lip, sideburns and the sterna, perioareolar, umbilical and sacral areas; with accentuated involvement in the pubic region and upper thighs Pusphagni jatharani give relevance of hyperandrogenism in which women menstruates in time without ovulation and has corpulent & hairy cheeks.
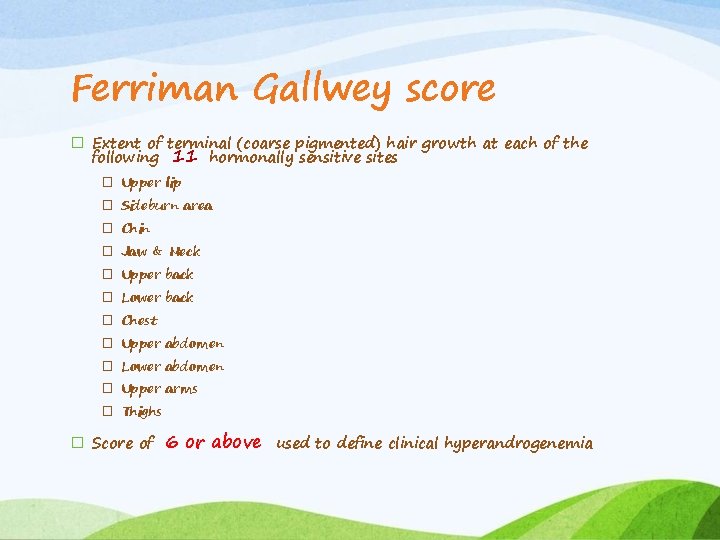
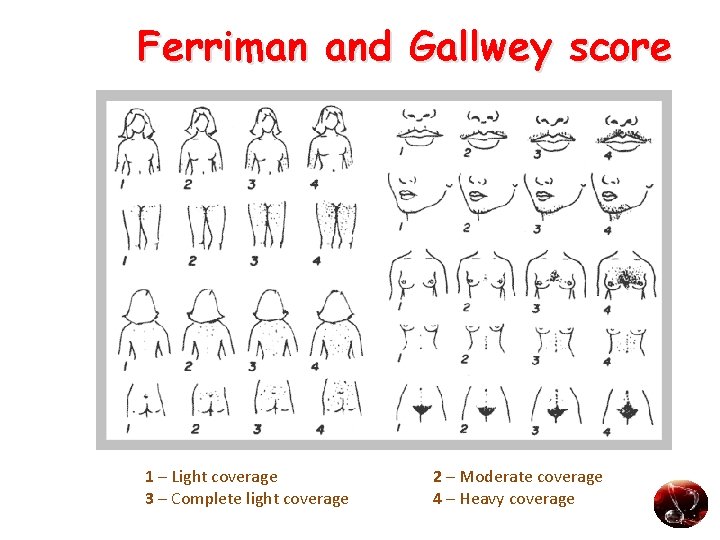
Ferriman Gallwey score � Extent of terminal (coarse pigmented) hair growth at each of the following 11 hormonally sensitive sites � Upper lip � Sideburn area � Chin � Jaw & Neck � Upper back � Lower back � Chest � Upper abdomen � Lower abdomen � Upper arms � Thighs � Score of 6 or above used to define clinical hyperandrogenemia
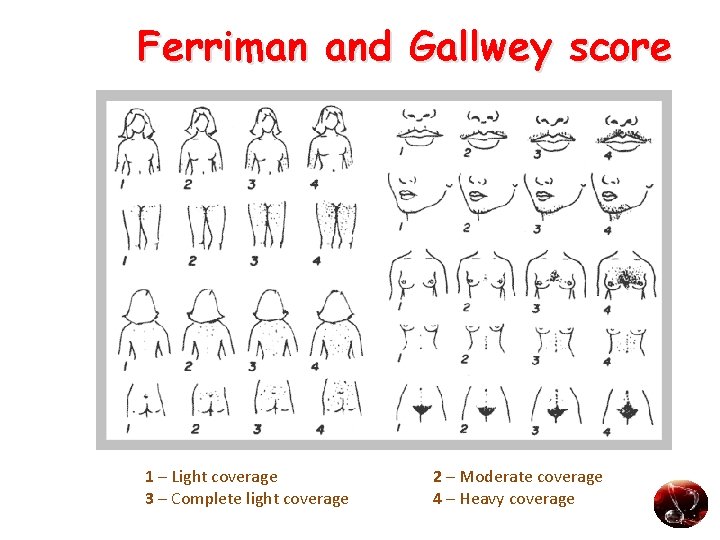
Ferriman and Gallwey score 1 – Light coverage 3 – Complete light coverage 2 – Moderate coverage 4 – Heavy coverage

Modified Ferriman Gallwey score 9 areas • Score 1 -4 • 0 -absence of terminal hair • 4 -extensive terminal hair growth >8 - hirsutism
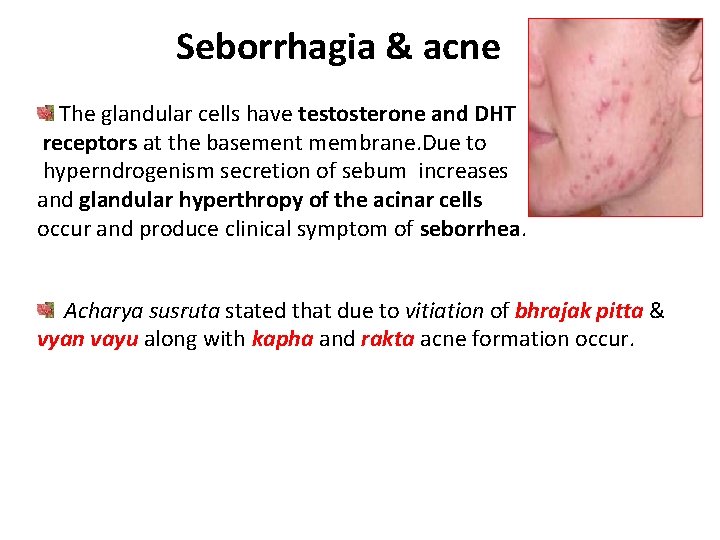
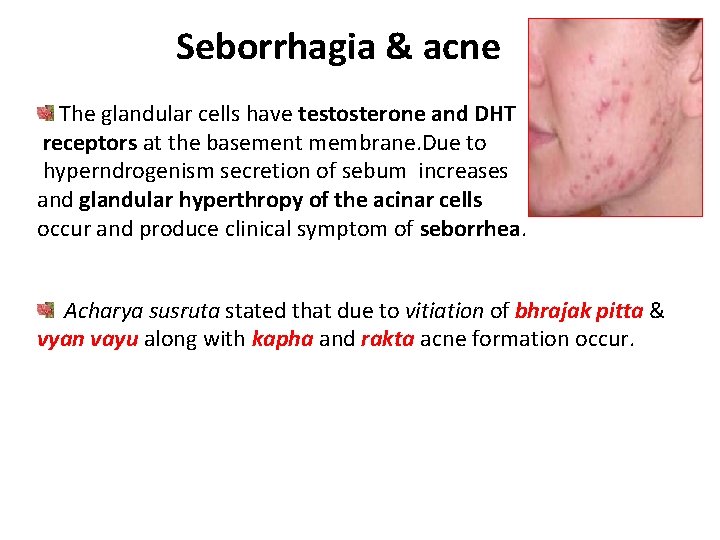
Seborrhagia & acne The glandular cells have testosterone and DHT receptors at the basement membrane. Due to hyperndrogenism secretion of sebum increases and glandular hyperthropy of the acinar cells occur and produce clinical symptom of seborrhea. Acharya susruta stated that due to vitiation of bhrajak pitta & vyan vayu along with kapha and rakta acne formation occur.
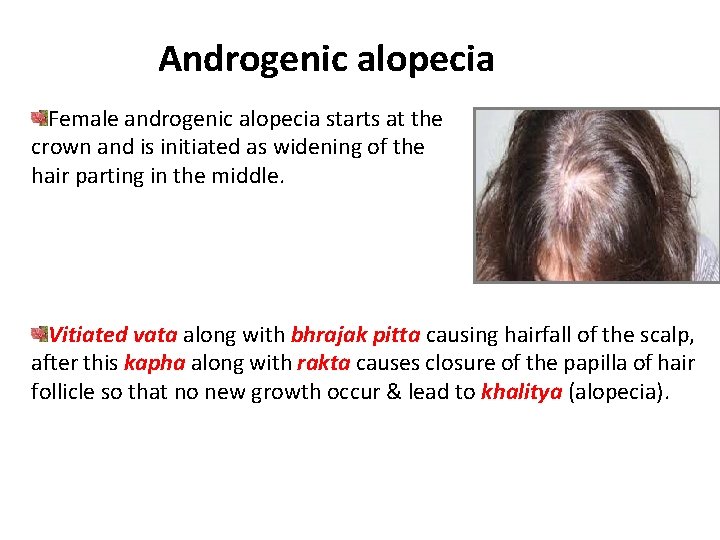
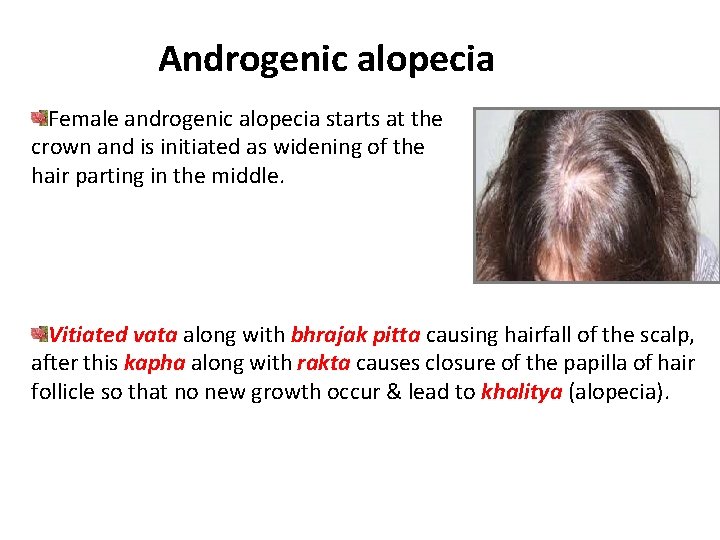
Androgenic alopecia Female androgenic alopecia starts at the crown and is initiated as widening of the hair parting in the middle. Vitiated vata along with bhrajak pitta causing hairfall of the scalp, after this kapha along with rakta causes closure of the papilla of hair follicle so that no new growth occur & lead to khalitya (alopecia).
Obesity is often associated with PCOD. Fat cells are main contributor for Aromatization. The weight distribution is centripetal, with increased waist to hip ratio ( >0. 85 ). medsa==v&tmaga. RTvat! pu: y. NTy. Nye n xatv> , med. Stu c. Iyte t. Smadz. Kt> sv. Rkm. Rsu. ma 0 in 0 medaeraegindanm! 2 medaema<saitv&ÏTva li. S)gudr. Stn>, Aywaepcyae. Tsahae nrae=it. Sw. Ul %Cyte. c 0 s. U 0 21
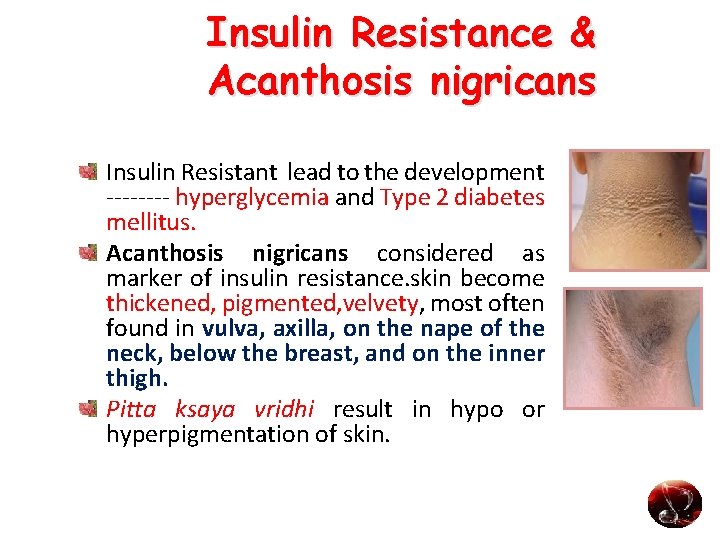
Insulin Resistance & Acanthosis nigricans Insulin Resistant lead to the development ---- hyperglycemia and Type 2 diabetes mellitus. Acanthosis nigricans considered as marker of insulin resistance. skin become thickened, pigmented, velvety, most often found in vulva, axilla, on the nape of the neck, below the breast, and on the inner thigh. Pitta ksaya vridhi result in hypo or hyperpigmentation of skin.

Laboratory investigations
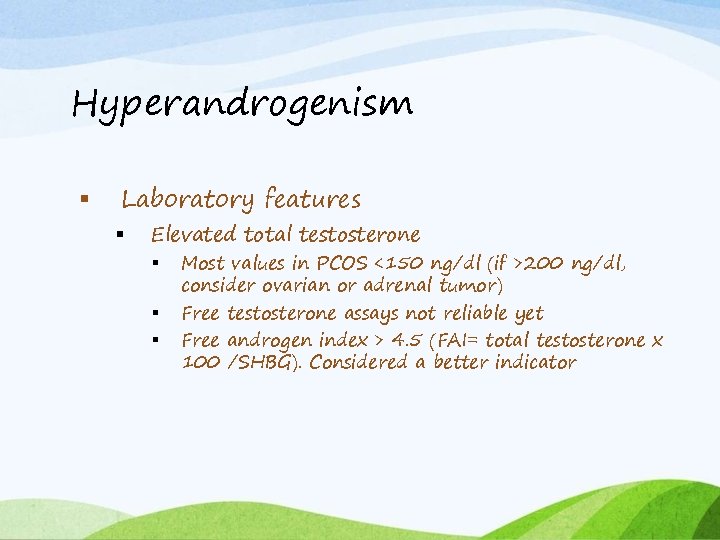
Hyperandrogenism Laboratory features Elevated total testosterone Most values in PCOS <150 ng/dl (if >200 ng/dl, consider ovarian or adrenal tumor) Free testosterone assays not reliable yet Free androgen index > 4. 5 (FAI= total testosterone x 100 /SHBG). Considered a better indicator

DHEA-S Most normal or slightly high in PCOS If >800 mcg/dl, consider adrenal tumor LH/FSH ratio Levels vary over menstrual cycle, released in pulsatile fashion, affected by OCPs LH/FSH ratio >2 has little diagnostic sensitivity and need not be documented
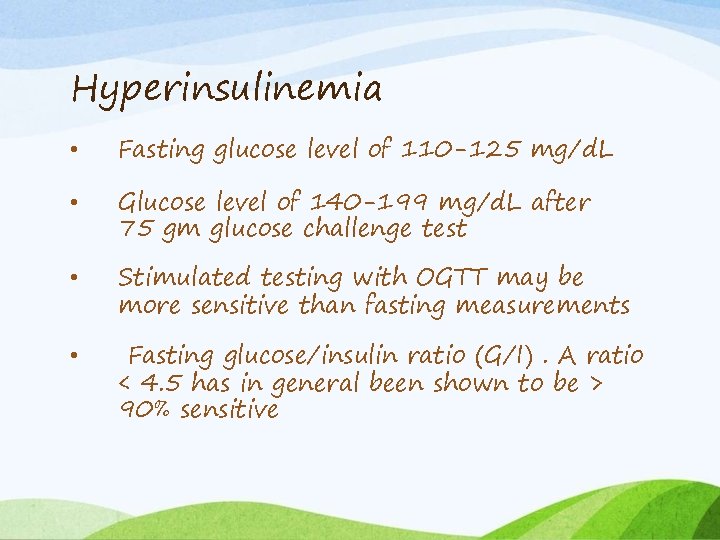
Hyperinsulinemia • Fasting glucose level of 110 -125 mg/d. L • Glucose level of 140 -199 mg/d. L after 75 gm glucose challenge test • Stimulated testing with OGTT may be more sensitive than fasting measurements • Fasting glucose/insulin ratio (G/I). A ratio < 4. 5 has in general been shown to be > 90% sensitive
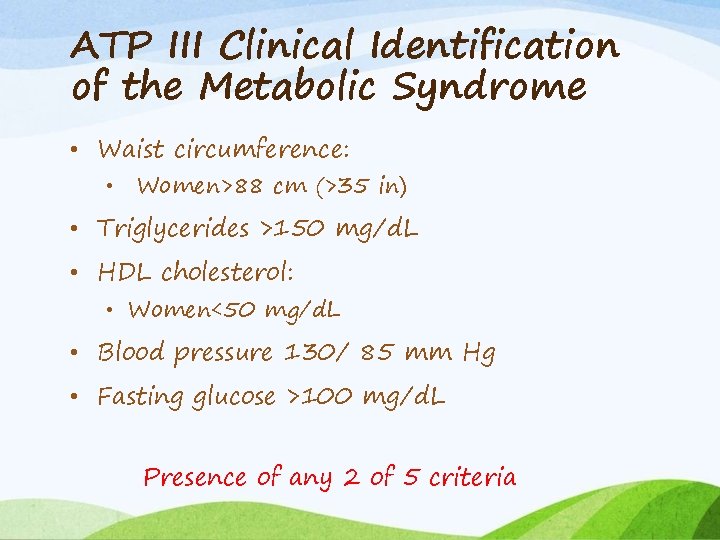
ATP III Clinical Identification of the Metabolic Syndrome • Waist circumference: • Women>88 cm (>35 in) • Triglycerides >150 mg/d. L • HDL cholesterol: • Women<50 mg/d. L • Blood pressure 130/ 85 mm Hg • Fasting glucose >100 mg/d. L Presence of any 2 of 5 criteria
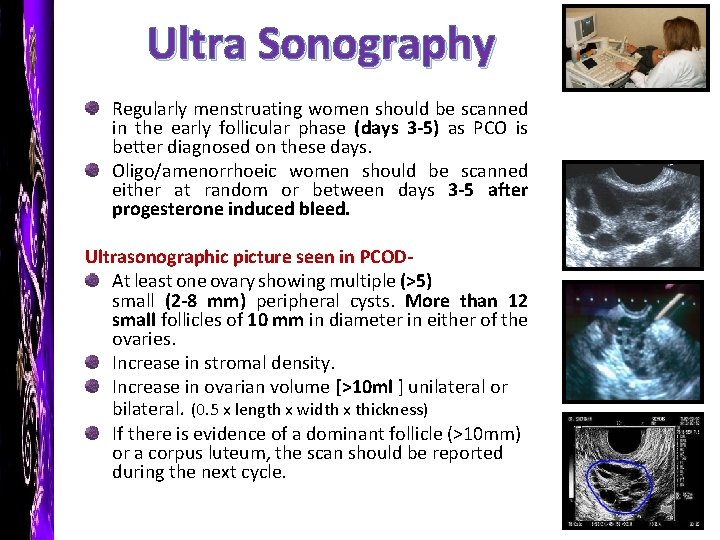
Ultra Sonography Regularly menstruating women should be scanned in the early follicular phase (days 3 -5) as PCO is better diagnosed on these days. Oligo/amenorrhoeic women should be scanned either at random or between days 3 -5 after progesterone induced bleed. Ultrasonographic picture seen in PCODAt least one ovary showing multiple (>5) small (2 -8 mm) peripheral cysts. More than 12 small follicles of 10 mm in diameter in either of the ovaries. Increase in stromal density. Increase in ovarian volume [>10 ml ] unilateral or bilateral. (0. 5 x length x width x thickness) If there is evidence of a dominant follicle (>10 mm) or a corpus luteum, the scan should be reported during the next cycle.
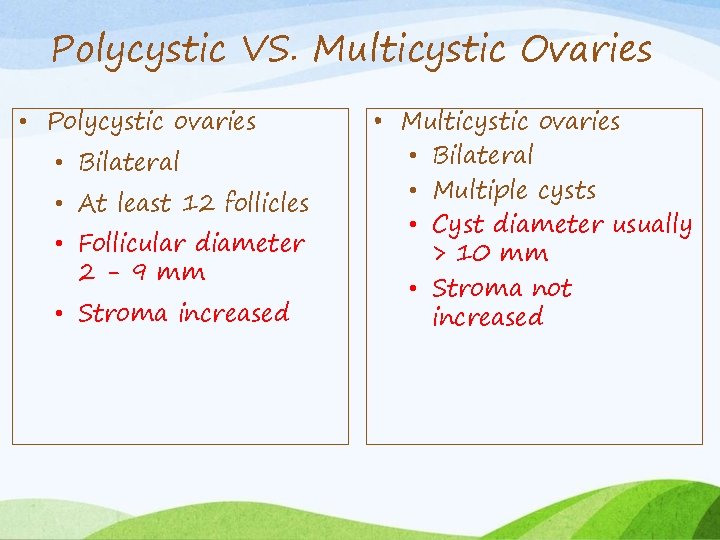
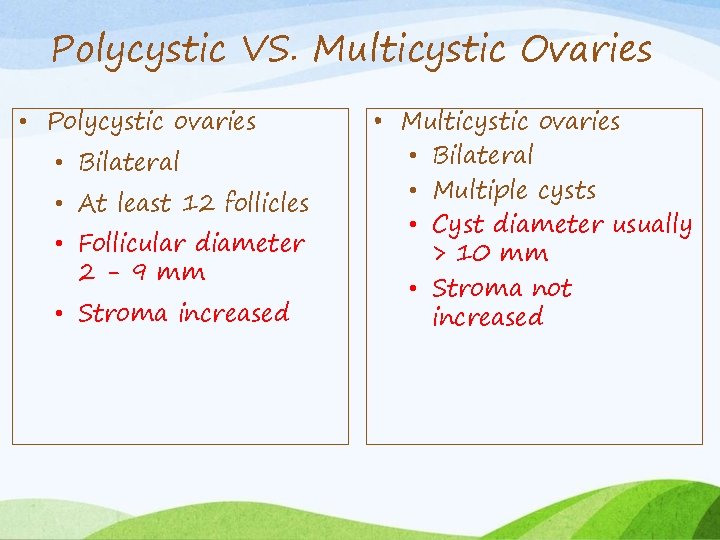
Polycystic VS. Multicystic Ovaries • Polycystic ovaries • Bilateral • At least 12 follicles • Follicular diameter 2 - 9 mm • Stroma increased • Multicystic ovaries • Bilateral • Multiple cysts • Cyst diameter usually > 10 mm • Stroma not increased
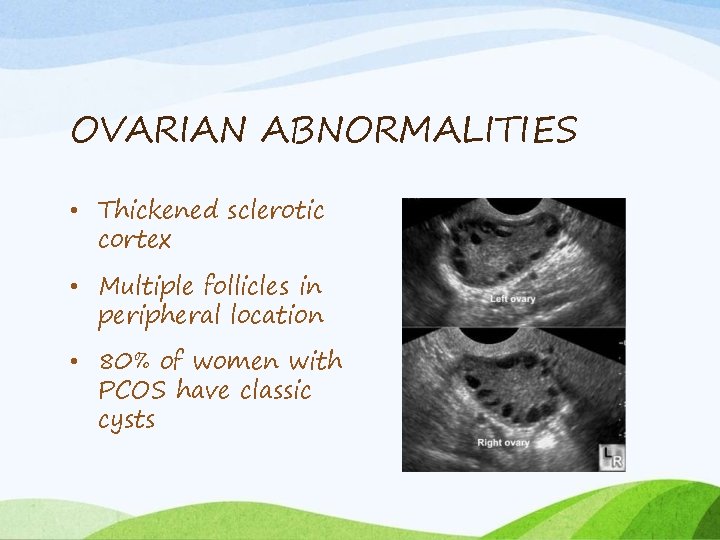
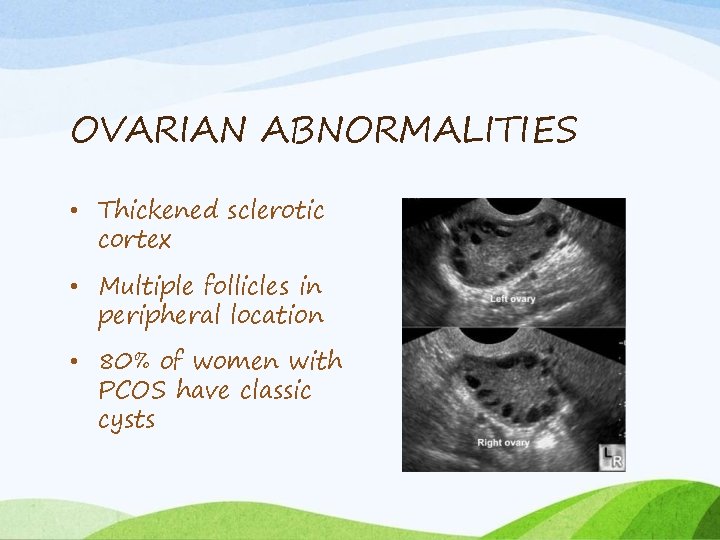
OVARIAN ABNORMALITIES • Thickened sclerotic cortex • Multiple follicles in peripheral location • 80% of women with PCOS have classic cysts
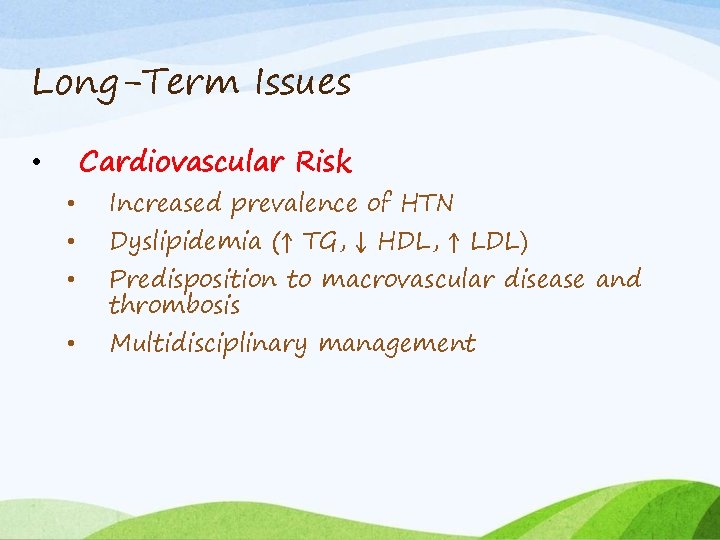
Long-Term Issues Cardiovascular Risk • • • Increased prevalence of HTN Dyslipidemia (↑ TG, ↓ HDL, ↑ LDL) Predisposition to macrovascular disease and thrombosis Multidisciplinary management
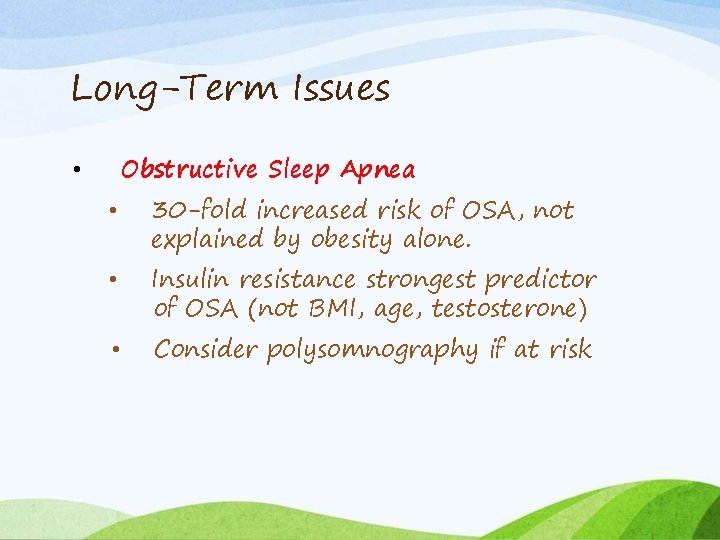
Long-Term Issues Obstructive Sleep Apnea • • 30 -fold increased risk of OSA, not explained by obesity alone. Insulin resistance strongest predictor of OSA (not BMI, age, testosterone) Consider polysomnography if at risk
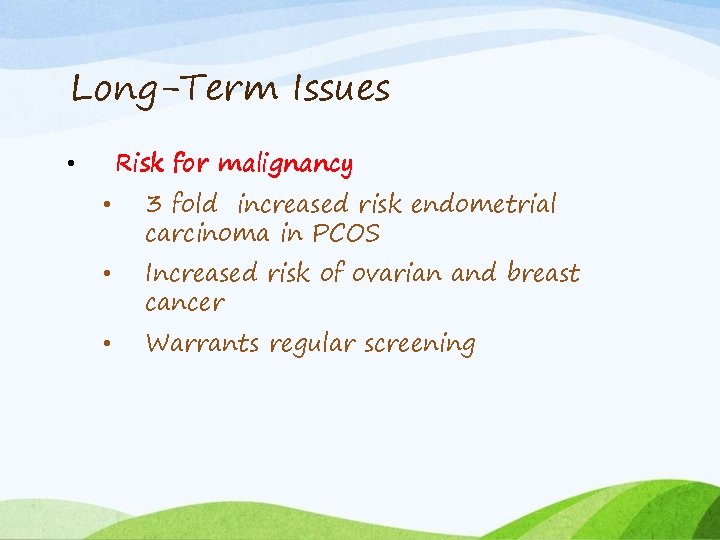
Long-Term Issues Risk for malignancy • • 3 fold increased risk endometrial carcinoma in PCOS Increased risk of ovarian and breast cancer Warrants regular screening
Differential Diagnosis
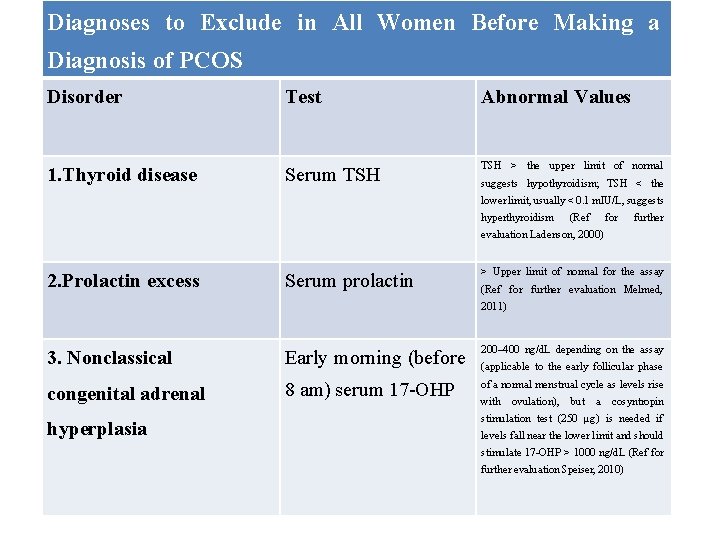
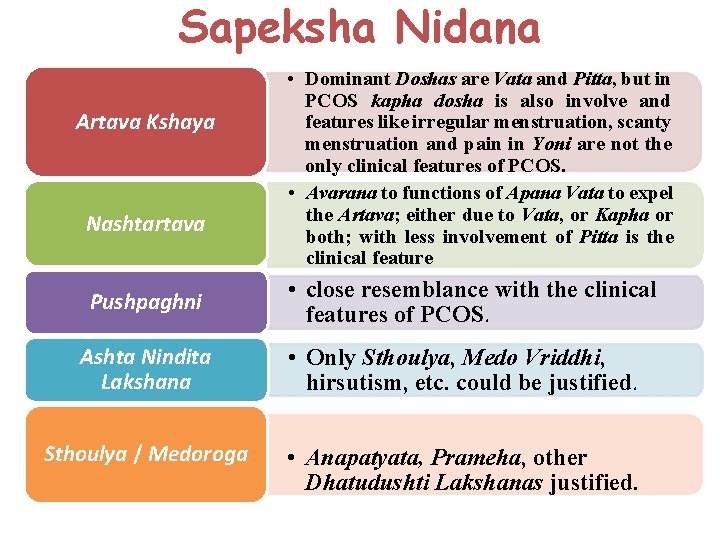
Diagnoses to Exclude in All Women Before Making a Diagnosis of PCOS Disorder Test Abnormal Values 1. Thyroid disease Serum TSH > the upper limit of normal suggests hypothyroidism; TSH < the lower limit, usually < 0. 1 m. IU/L, suggests hyperthyroidism (Ref for further evaluation Ladenson, 2000) 2. Prolactin excess Serum prolactin > Upper limit of normal for the assay (Ref for further evaluation Melmed, 2011) 3. Nonclassical Early morning (before 200– 400 ng/d. L depending on the assay congenital adrenal 8 am) serum 17 -OHP of a normal menstrual cycle as levels rise hyperplasia (applicable to the early follicular phase with ovulation), but a cosyntropin stimulation test (250 µg) is needed if levels fall near the lower limit and should stimulate 17 -OHP > 1000 ng/d. L (Ref for further evaluation Speiser, 2010)
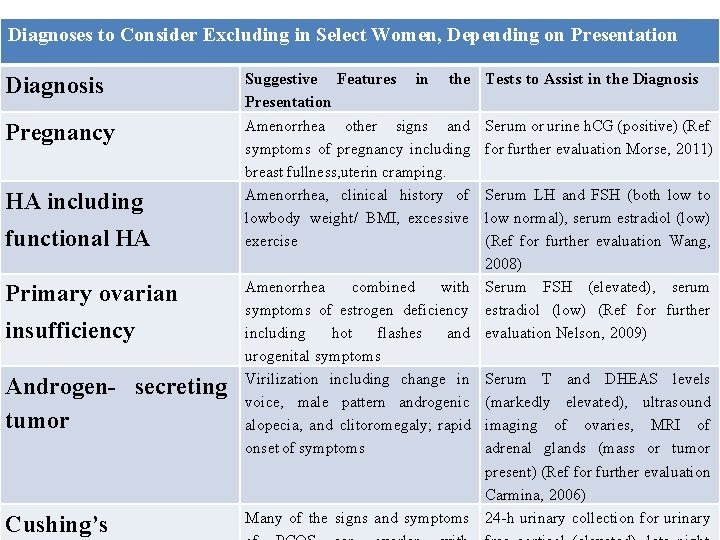
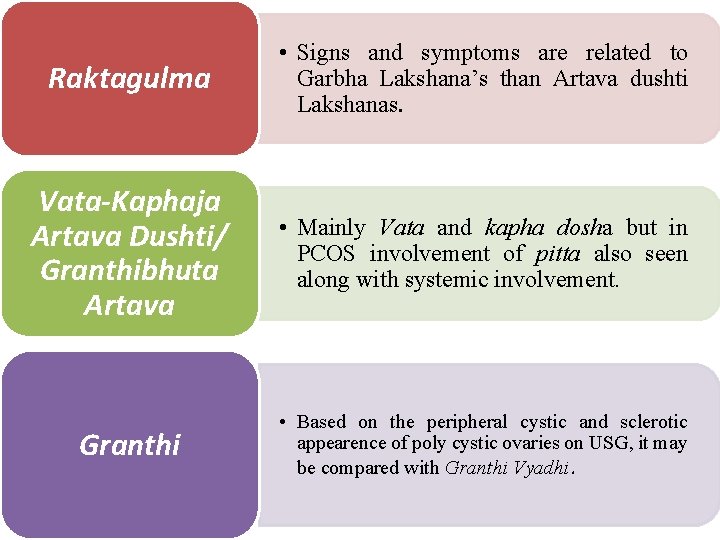
Diagnoses to Consider Excluding in Select Women, Depending on Presentation Diagnosis Suggestive Features Presentation Pregnancy Amenorrhea other signs and symptoms of pregnancy including breast fullness, uterin cramping. Amenorrhea, clinical history of lowbody weight/ BMI, excessive exercise HA including functional HA Primary ovarian insufficiency Androgen- secreting tumor Cushing’s in the Tests to Assist in the Diagnosis Serum or urine h. CG (positive) (Ref for further evaluation Morse, 2011) Serum LH and FSH (both low to low normal), serum estradiol (low) (Ref for further evaluation Wang, 2008) Amenorrhea combined with Serum FSH (elevated), serum symptoms of estrogen deficiency estradiol (low) (Ref for further including hot flashes and evaluation Nelson, 2009) urogenital symptoms Virilization including change in Serum T and DHEAS levels voice, male pattern androgenic (markedly elevated), ultrasound alopecia, and clitoromegaly; rapid imaging of ovaries, MRI of onset of symptoms adrenal glands (mass or tumor present) (Ref for further evaluation Carmina, 2006) Many of the signs and symptoms 24 -h urinary collection for urinary
Sapeksha Nidana Artava Kshaya Nashtartava Pushpaghni • Dominant Doshas are Vata and Pitta, but in PCOS kapha dosha is also involve and features like irregular menstruation, scanty menstruation and pain in Yoni are not the only clinical features of PCOS. • Avarana to functions of Apana Vata to expel the Artava; either due to Vata, or Kapha or both; with less involvement of Pitta is the clinical feature • close resemblance with the clinical features of PCOS. Ashta Nindita Lakshana • Only Sthoulya, Medo Vriddhi, hirsutism, etc. could be justified. Sthoulya / Medoroga • Anapatyata, Prameha, other Dhatudushti Lakshanas justified.
Raktagulma • Signs and symptoms are related to Garbha Lakshana’s than Artava dushti Lakshanas. Vata-Kaphaja Artava Dushti/ Granthibhuta Artava • Mainly Vata and kapha dosha but in PCOS involvement of pitta also seen along with systemic involvement. Granthi • Based on the peripheral cystic and sclerotic appearence of poly cystic ovaries on USG, it may be compared with Granthi Vyadhi.

conclusion
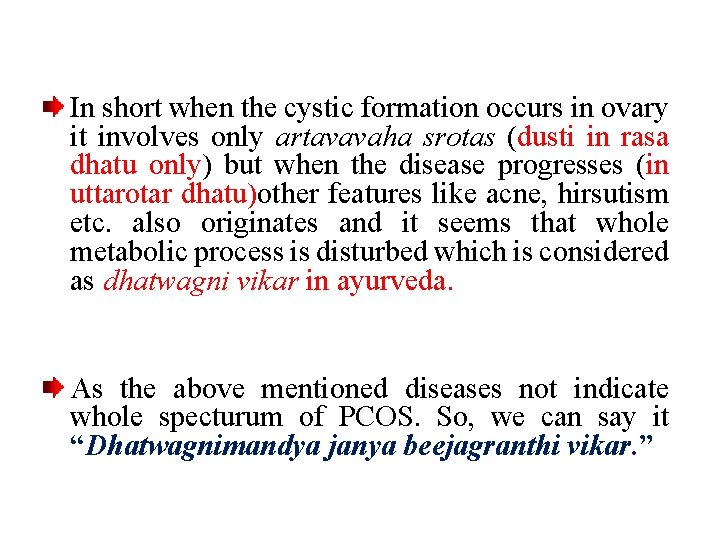
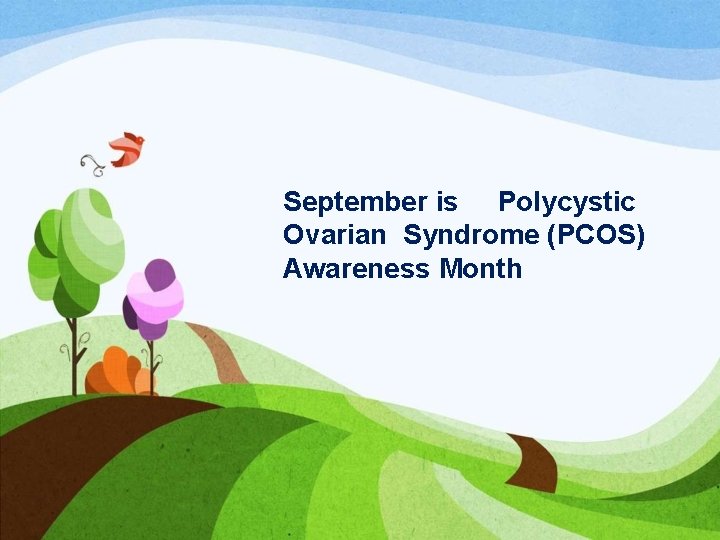
In short when the cystic formation occurs in ovary it involves only artavavaha srotas (dusti in rasa dhatu only) but when the disease progresses (in uttarotar dhatu)other features like acne, hirsutism etc. also originates and it seems that whole metabolic process is disturbed which is considered as dhatwagni vikar in ayurveda. As the above mentioned diseases not indicate whole specturum of PCOS. So, we can say it “Dhatwagnimandya janya beejagranthi vikar. ”

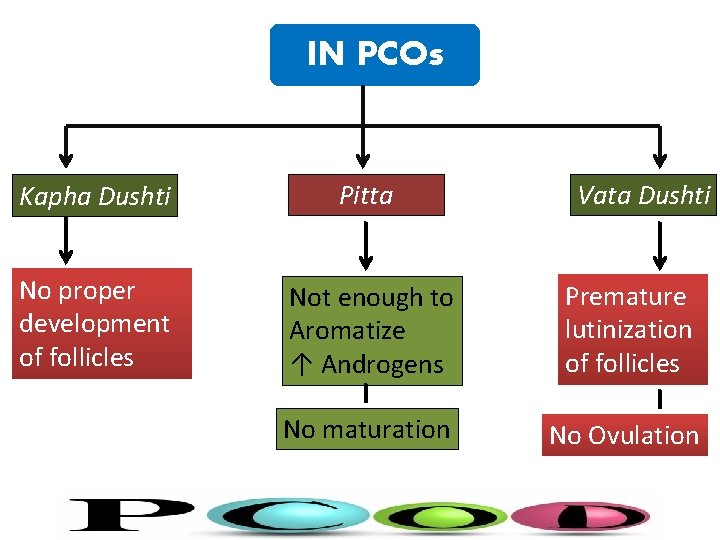
IN PCOs Kapha Dushti Pitta Vata Dushti No proper development of follicles Not enough to Aromatize ↑ Androgens Premature lutinization of follicles No maturation No Ovulation
September is Polycystic Ovarian Syndrome (PCOS) Awareness Month
Thank You
 Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Infantile polycystic kidney
Infantile polycystic kidney Ovarian cancer causes
Ovarian cancer causes Benjamin cummings
Benjamin cummings Ovarian teratoma
Ovarian teratoma Ovarian ligament
Ovarian ligament Ovarian cyst about to rupture
Ovarian cyst about to rupture Ovarian ligament
Ovarian ligament Ovarian follicle
Ovarian follicle Functions of overies
Functions of overies The ovarian cycle
The ovarian cycle Ovarian cycke
Ovarian cycke 3 layers of fallopian tube
3 layers of fallopian tube Ovarian duct
Ovarian duct Ovarian benign tumor
Ovarian benign tumor Immature teratoma
Immature teratoma Ovarian ligament.
Ovarian ligament. Infundibulum female reproductive system
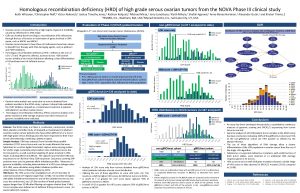
Infundibulum female reproductive system Hrd score ovarian cancer
Hrd score ovarian cancer Ovarian cancer brca
Ovarian cancer brca Pathoma slides
Pathoma slides Stratum parabasale
Stratum parabasale Sru consensus ovarian cysts
Sru consensus ovarian cysts Ovarian cycle
Ovarian cycle Follicular development diagram
Follicular development diagram Ovarian cancer marker
Ovarian cancer marker Ovarian cycle
Ovarian cycle Prism is presented with
Prism is presented with Generic structure of spoof text
Generic structure of spoof text Topic, main idea supporting details
Topic, main idea supporting details Theme of love romeo and juliet
Theme of love romeo and juliet Headline news examples
Headline news examples Professionally presented
Professionally presented How it's made presented by
How it's made presented by Reducing balance method
Reducing balance method How is the text presented
How is the text presented Jerome bruner cognitive theory
Jerome bruner cognitive theory Young and dyslexic benjamin zephaniah
Young and dyslexic benjamin zephaniah Proudly presented to
Proudly presented to Kamikaze power of nature
Kamikaze power of nature Both passages
Both passages Name of presenter
Name of presenter Caltech bursar
Caltech bursar Plant assets are
Plant assets are As presented below
As presented below Text structure cause and effect examples
Text structure cause and effect examples Conic sections
Conic sections Martha stoddard holmes
Martha stoddard holmes Presented sy
Presented sy The tragedy of macbeth act 5
The tragedy of macbeth act 5 The technological design model is presented as a
The technological design model is presented as a Setting in jekyll and hyde
Setting in jekyll and hyde Presenters name
Presenters name Polygon presented
Polygon presented How is power presented in ozymandias and my last duchess
How is power presented in ozymandias and my last duchess Technical drawing means
Technical drawing means Talisman presented
Talisman presented A combination of tones that sounds discordant
A combination of tones that sounds discordant The kitchen presented by
The kitchen presented by Macbeth act 1 scene 5 translation
Macbeth act 1 scene 5 translation How is marley's ghost presented in stave 1
How is marley's ghost presented in stave 1 How is power presented in ozymandias and london
How is power presented in ozymandias and london Co presented by
Co presented by Xfinity home security battery backup
Xfinity home security battery backup App service overview
App service overview Foundations in personal finance answers chapter 1
Foundations in personal finance answers chapter 1 Informal e-mail
Informal e-mail Overview of the major systemic arteries
Overview of the major systemic arteries Introduction product overview
Introduction product overview System architecture of gsm
System architecture of gsm Example of project overview
Example of project overview Chapter 1 an overview of financial management
Chapter 1 an overview of financial management Data quality and data cleaning an overview
Data quality and data cleaning an overview Sap sd overview
Sap sd overview Streamer overview
Streamer overview British school system overview
British school system overview Chapter 2 an overview of the financial system
Chapter 2 an overview of the financial system Lync vs skype for business
Lync vs skype for business