Current Concepts in Polycystic Ovarian Syndrome Mark N


- Slides: 74
Current Concepts in Polycystic Ovarian Syndrome Mark N. Simon, MD Exempla Uptown Women’s Healthcare Specialists October 17, 2003
Disclosure Dr. Simon has no significant financial interests or other relationships with industry relative to the subject of this lecture.
Objectives l l l Cite the physical manifestations of PCOS. Describe the pathophysiology of PCOS. Formulate a treatment plan for patients with PCOS.
Scope of the Problem l l l PCOS is the MOST common endocrine disorder of reproductive age women Effects 5 -10% of these women Commonly presents to primary care providers
Diagnosis l North America (NIH Consensus): – – Menstrual Irregularity (oligo- or anovulation) Hyperandrogenism l l – Clinical evidence OR Laboratory evidence Absence of other endocrine disorders l l l Congenital Adrenal Hyperplasia Hyperprolactinemia Thyroid dysfunction
Diagnosis l Europe: – – – Morphological features of polycystic ovaries Menstrual disturbance AND/OR Hyperandrogenism l l Hirsuitism Acne Alopecia Laboratory data are not needed
Ultrasound l Polycystic Ovaries – – – l Found in around 20% of general population May be a predictor of future development of PCOS Found in 80% of women with PCOS Appearance – – Many, peripheral, small follicles Increased ovarian stroma
European Diagnosis l l Increases prevalence to about 15% Proposed unifying protocol: – – Determine if symptoms are present If present, proceed with ultrasound If ultrasound positive – diagnosis confirmed If ultrasound negative – check lab tests Homberg, Human Reproduction, 2002
Diagnosis l North America (NIH Consensus): – – Menstrual Irregularity (oligo- or anovulation) Hyperandrogenism l l – Clinical evidence OR Laboratory evidence Absence of other endocrine disorders l l l Congenital Adrenal Hyperplasia Hyperprolactinemia Thyroid dysfunction
Patient Presentation l l l Symptoms of hyperandrogenism Irregular menstrual cycles Infertility – Most Common Presentation
Symptoms of Hyperandrogenism l l l Hirsutism Acne Rarely see Virilization – – Male pattern balding Clitoromegaly Deepening of voice Increased muscle mass
Hirsutism l l Occurs in 80% of PCOS patients Excess terminal body hair – Male Pattern l l Back, Sternum, Upper Abdomen, Shoulder More common areas – – Upper Lip, Around breast nipples, Linea alba ¼ of women have hair in these areas l Excluding Scandinavian, Asian
Hirsutism - DDx l l l l Idiopathic PCOS Drugs (Danazol) Hyperthecosis Ovarian Tumors Adrenal Tumors CAH
Ovarian Hyperthecosis l l Ovary has nests of luteinized theca cells Signs and Symptoms – – Hirsutism, Alopecia, Obesity HTN Clitoromegaly Markedly elevated testosterone
Red Flags with Hirsutism l l l Rapid onset of hirsutism Rapid progression of hirsutism Late onset – l Outside of early reproductive years Virilization
Tumors l l l RED FLAGS Testosterone > 150 ng/d. L (> 200 ng/d. L) LH low DHES > 800 mcg/d. L Further investigation warranted – MRI abdomen/pelvis
Nonclassic Congenital Adrenal Hyperplasia l l Partial deficiency of 21 -hydroxylase Elevation of 17 -hydroxyprogesterone – l l l Precursor of androgens Rare Do NOT have adrenal insufficiency Treat with anti-androgen therapy
Nonclassic Congenital Adrenal Hyperplasia l l Consider in patients not responding to typical PCOS treatment Measure 17 -hydroxyprogesterone – – – Follicular phase Morning Levels > 2 ng/m. L need to be tested further l Adrenal stimulation
Acne l l l Common in adolescent girls (30 -50%) Severe acne is uncommon (<1%) Severe acne is a predictor of PCOS
Irregular Menses l Most common to have erratic menses – l Due to Anovulation Patients present with oligomenorrhea or amenorrhea
PCOS with Regular Menses? l Androgens converted to estrogens – – l l Peripheral conversion Aromatase Estrogens stimulate uterine lining Can have regular shedding of endometrial lining despite anovulation
PCOS with Regular Menses? l l l Hyperandrogenism does NOT automatically cause anovulation Women with hyperandrogenism and polycystic ovaries may still ovulate regularly Affect on fertility is unclear
Infertility l l l Usually long-standing infertility PCOS typically develops in early reproductive years Infertility usually due to anovulation
Clinical Presentations l Hyperandrogenism – – l l Hirsutism Acne Menstrual Irregularity Infertility
Initial Evaulation l l History to determine onset PCOS usually has long course – l l l Rapid onset of hirsutism – Red Flag Usually develops early in reproductive years PCOS is diagnosis of exclusion Lab tests help to exclude other problems
What tests to order l Prolactin – – l l Rule out hyperprolactinemia Cause of menstrual dysfunction Little signs of hyperandrogenism Lactotroph stimulation from estrogen Testosterone DHEAS
Laboratory Tests l 17 -Hydroxyprogesterone – l TSH – l l In patients suspected of NCAH When symptoms warrant Glucose Tolerance Test Fasting Lipid Profile
Laboratory Tests l LH, FSH – l Little benefit Insulin
Pathophysiology l l Exact problems have not been identified Hypothalamic-pituitary abnormalities – Elevated LH l – – – Increased frequency and amplitude of pulses Low-normal FSH LH: FSH ratio increased Gn. RH pulse generator may be disrupted causing the elevated LH
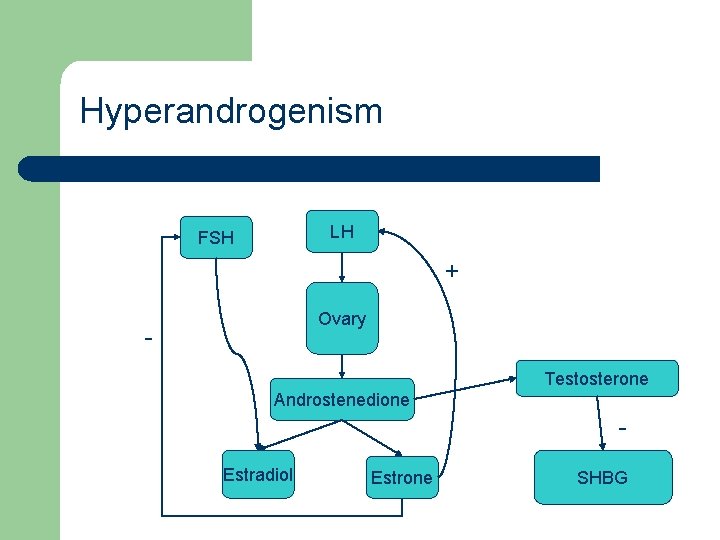
Hyperandrogenism l Androstenedione – – Produced in ovarian thecal cells Production is stimulated by LH Converted to estradiol by FSH-stimulated aromatase Excess is converted to estrone which suppresses FSH and is tonic to LH
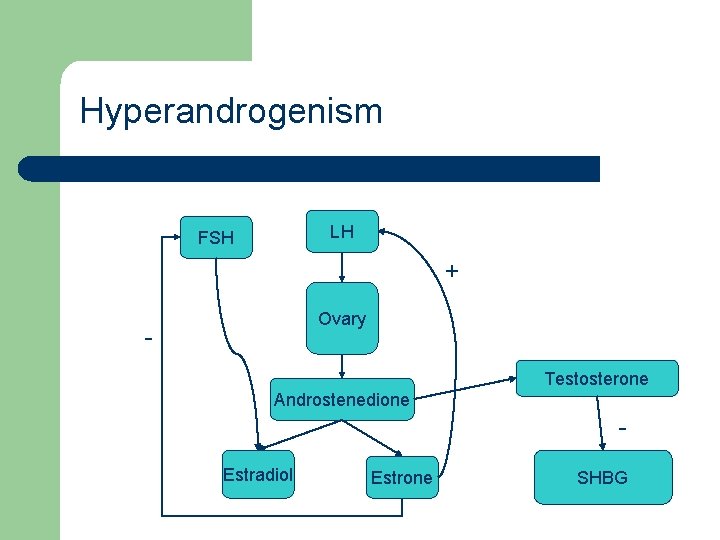
Hyperandrogenism LH FSH + Ovary - Testosterone Androstenedione Estradiol Estrone SHBG
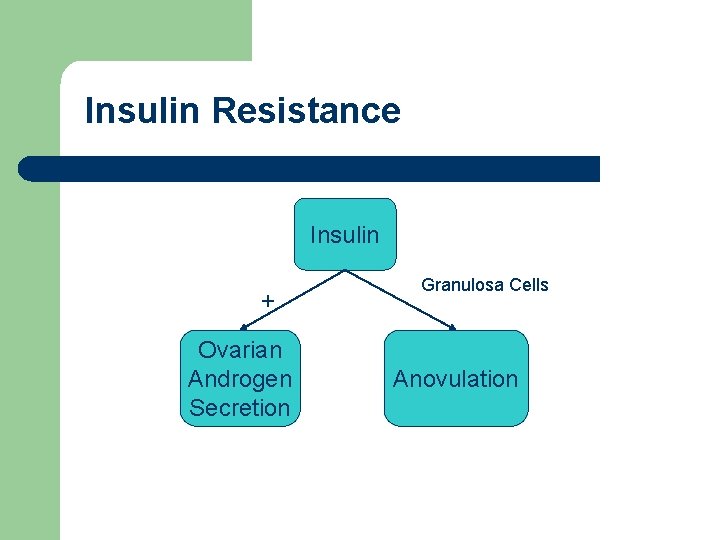
Insulin Resistance l l Feature of PCOS Both obese and lean women are affected Affects a number of systems Reduction in tissue response to insulin
Insulin Resistance l Insulin causes androgen production – l In women with PCOS Insulin – – Amplifies LH response in granulosa cells Arrest of follicular development
Insulin Resistance l Insulin-like growth factor 1 (IGF-1) – – l Insulin-like growth factor binding protein 3 (IGFBP-3) – – l Amplifies LH androgen synthesis Helps to regulate follicular maturation Decreased in patients with ovarian hirsuitism When decreased, more bioavailability of IGF-1 Shobokshi, et al, J Soc Gynecol Investig, 2003
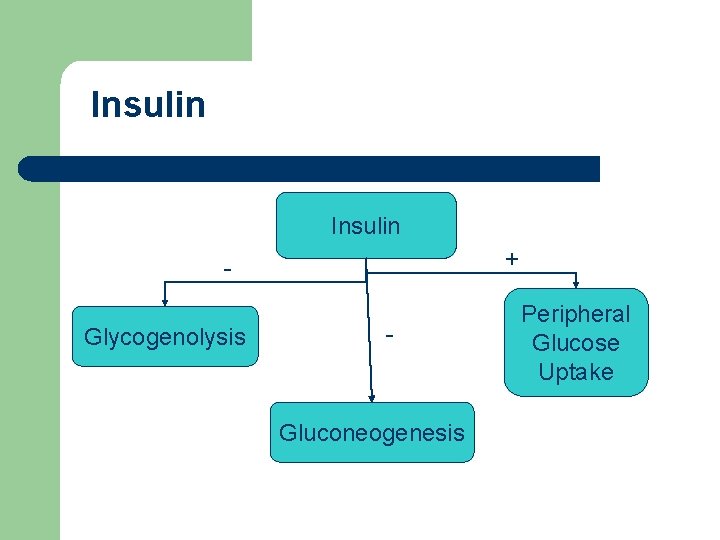
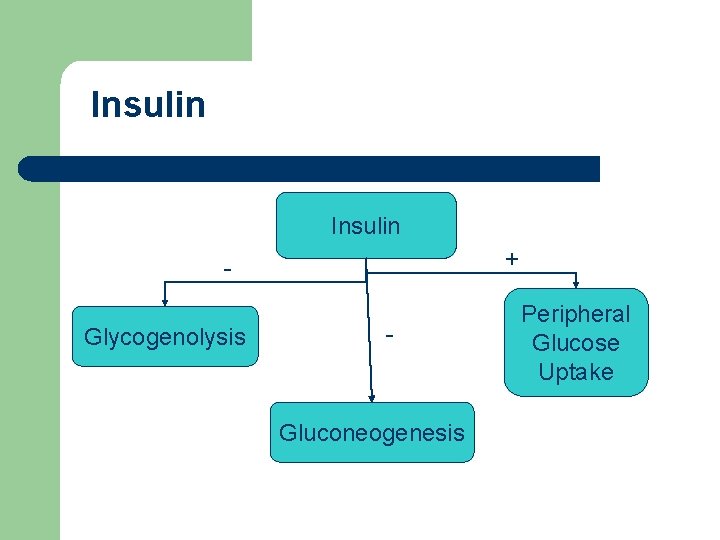
Insulin + Glycogenolysis - Gluconeogenesis Peripheral Glucose Uptake
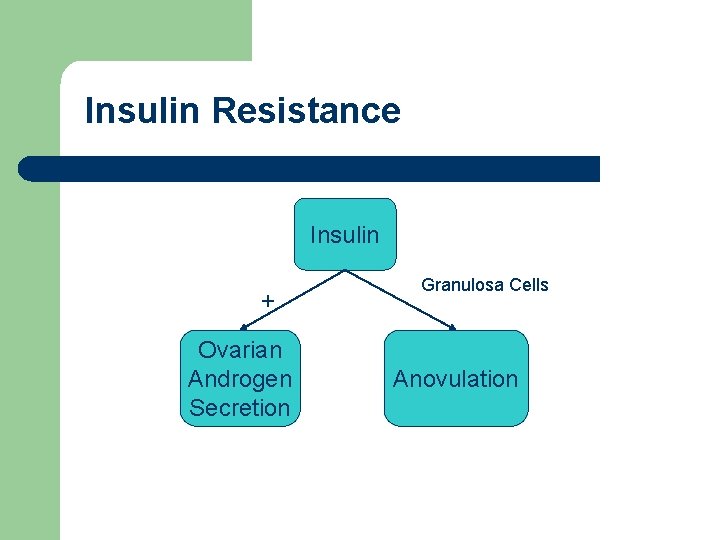
Insulin Resistance Insulin + Ovarian Androgen Secretion Granulosa Cells Anovulation
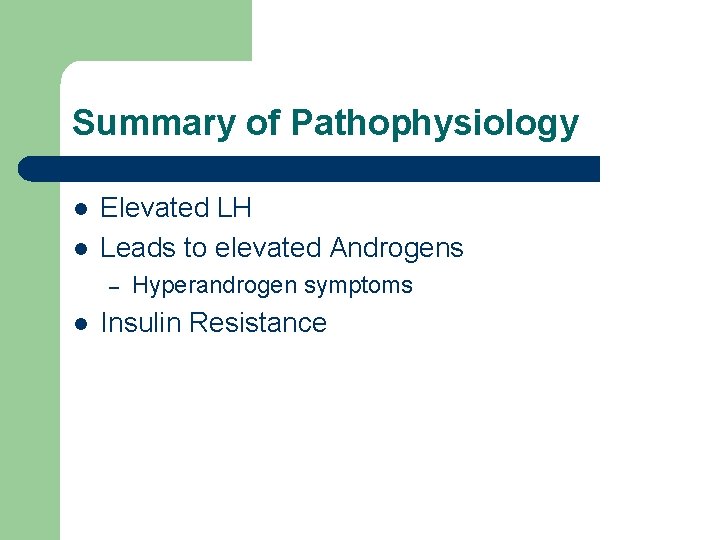
Summary of Pathophysiology l l Elevated LH Leads to elevated Androgens – l Hyperandrogen symptoms Insulin Resistance

Treatment l l Depends on symptoms Depends on patient’s goals
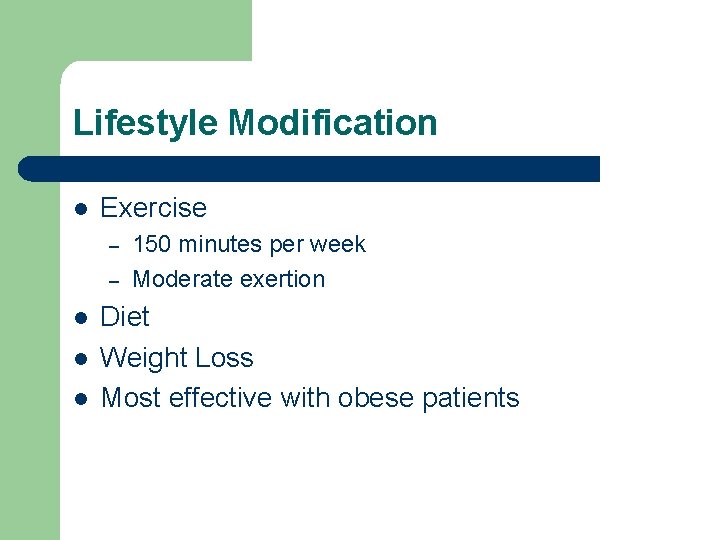
Lifestyle Modification l Exercise – – l l l 150 minutes per week Moderate exertion Diet Weight Loss Most effective with obese patients
Weight Loss l Improves ovulatory and fertility rates – – l 5 -7% loss Restored ovulation in 75% Decreases LH pulse amplitude – Decreases androgen production l Reduces insulin levels l Kiddy et al. , Clin Endocrinol, 1992.
Insulin Sensitizers l Metformin – – – Most extensively studied Increases peripheral uptake of glucose Decreases gluconeogenesis Does not cause hypoglycemia Relatively inexpensive l Generic 500 mg, 60 tabs $33. 99 (drugstore. com 10/15/03)
Metformin l Side Effects – – l Gastrointestinal distress Most common in first few weeks of use Improves over time Lactic acidosis Dosage is 500 mg TID or 875 mg BID
Metformin l Lactic Acidosis – – l Contraindicated in – – l Severe, potentially fatal Concern with elevated creatinine (>1. 4 mg/d. L) CHF, Sepsis, Liver disease, history of lactic acidosis Surgery
Rosiglitazone l l l Insulin-sensitizing agent Stimulate production of glucose transporter proteins Few studies in PCOS Dosage is 4 mg BID More expensive – 4 mg, 30 tabs cost $77. 99 (drugstore. com, 10/15/03)
Rosiglitazone l l Improved clinical symptoms Corrects insulin resistance Improves ovulation rates Fewer side effects – l l l Especially GI Fertility rates not studied Shobokshi, et al, J Soc Gynecol Investig, 2003 Ghazeeri, et al, Fertil Steril, 2003

Treatment Algorithms l l Path depends primarily on fertility desires Also depends on primary symptoms of patient
Desires Fertility l l l The Problem: Anovulation The Solution: Reestablish Ovulation Question for patient: Willingness to wait? – – – l Weight Loss Insulin-sensitizers may take 3 -5 months Ovulation induction much quicker Harborne et al, The Lancet, April 8, 2003.
Weight Loss l Modest weight loss (5%) can help – – l Lower androgen levels Induce regular cycles Other health benefits for pregnancy – – Diabetes Hypertension
Metformin l l l 5 weeks of treatment Ovulation rate of 34 % vs. 4% in placebo No ovulation – Given Clomiphene citrate – l Increased ovulation rate to 90% Nestler et al, NEJM, 1998
Metformin and Pregnancy l l Pregnancy Class B PCOS increases risk of miscarriage – l Plaminogen activator inhibitor (PAI) – – l 30 -50% higher Causes placental insufficiency Increases with increased insulin levels Kosasa, Contemporary OB/Gyn, March 2003
Metformin and Pregnancy l l Patients receiving 1. 5 g to 2. 55 g per day Decreased rate of miscarriage – From 73% to 10% l Thought to be related to decrease PAI activity l Glueck et al, Fertil Steril, 2001.
Metformin and Gestational Diabetes l l PCOS increases risk of GDM Metformin treatment decreases development of GDM – From 31% to 3% l Further studies are warranted l Glueck et al, Fertil Steril, 2002.
Ovulation Induction l Clomiphene citrate – – Can start at 50 mg/day on days 5 -9 Up to 150 mg/day l – – Effective in about 85% of women with PCOS Metformin-CC combination even more effective l l l Some sources up to 200 mg/day in morbidly obese 90% in small study Further studies ongoing Stovall, OBG Management, June 2003
Other Induction Agents l l l Human menopausal gonadotropin Follicle-stimulating hormone Referral to specialist
Fertility NOT Desired l Regulate Cycles – Hormonal Contraception l l l – Oral Pills Patch Ring Progesterone withdrawal l l Every 3 months Monthly
Hormonal Contraception l l l Reduces gonadotropin stimulation on ovary Reduces androgen production Can help with hirsutism, acne Increase SHBG Use newer progestins – Desogestrel, Norgestimate
Caution l Hormonal Contraception – – Not as effective in morbidly obese Increased risk of thrombotic event
Hirsutism - Treatment l Reduce Androgens – – – l Weight Loss Hormonal Contraception Anti-Androgens Mechanical Treatment – – – Shaving Electrolysis Laser
Hirsutism l l Treatment takes a long time Spironolactone – – Binds to androgen receptor Blocks 5α-Reductase 25 mg, 50 mg, 100 mg, 200 mg divided daily Side effects l Light-headedness, lethargy, menstrual irregularity, mastodynia
Spironolactone l l l Use with contraception Theoretical risk of teratogenicity Minimize menstrual irregularity
Spironolactone l Effectiveness – – l 40 -88% reduction in diameter of hair growth 6 -12 months of use Futterweit, Obs and Gyn Survey, 1999.
Other Antiandrogens l Flutamide – – l Blocks androgen binding to tissue Rare fatal hepatotoxicity Finasteride – – 5α-reductase inhibitor 5 mg/day Don’t use in pregnancy As effective as Spironolactone
Other treatments of hirsutism l Eflornithine – – – Topical agent Slows hair growth Apply twice a day Mechanical hair removal is required Hair will reappear 2 months after stopping tx
Mechanical Treatment l l Can be used after medical treatment Laser – l Most success in light skin, dark hair Electrolysis – Long-term treatments
Long-Term Consequences of PCOS l l Endometrial Cancer Coronary Risk
Endometrial Cancer l l Most common invasive gyn cancer Risks include – – Unopposed estrogen Obesity High androstenedione levels Risks that are common in PCOS patients
Decreasing Endometrial Risk l l l Regulate menses Combination hormones Progesterone withdrawal
Coronary Risk l l l Prediliction to Diabetes Dyslipidemia Obesity
Diabetes Risk l l Study of 122 obese women with PCOS Impaired Glucose Tolerance – l Type 2 Diabetes – l 30 -40% 10% Ehrmann, et al. , Diabetes Care, 1999.
Diabetes Risk l What screening test? – – l Risk of Diabetes with PCOS – – – l Fasting Glucose 75 gram GTT 254 women with PCOS 3. 2% by fasting glucose alone 7. 5% with GTT Legro, et al, J Clin Endocrinol Metab, 2002.
Dyslipidemia l l l Elevated Triglycerides Decreased HDL Increased LDL/HDL ratio
Overall Coronary Risk l l Hard to determine Studies have been poorly defined – – l Ovarian morphology Oligomenorrhea Can be confounded by other known risk factors – Diabetes, Obesity
Long-Term Therapy l Cyclic Estrogen/Progesterone – l Insulin-sensitizers – – l Reduces risk of endometrial hyperplasia and cancer Uncertain of long-term benefit May reduce risk of diabetes Need further studies
Take Home l l l Treatment needs to be guided by patient desires and concerns Lifestyle modification Protect the endometrium
 Infantile polycystic kidney
Infantile polycystic kidney Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Fuctions of ovary
Fuctions of ovary Female reproductive system
Female reproductive system Ca 125
Ca 125 Ovarian cyst rupture discharge look like
Ovarian cyst rupture discharge look like Figure of reproductive system
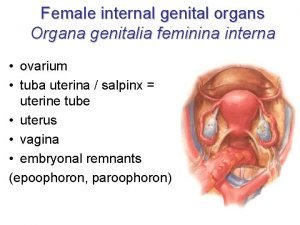
Figure of reproductive system Organa genitalia feminina nedir
Organa genitalia feminina nedir Ovarian cancer causes
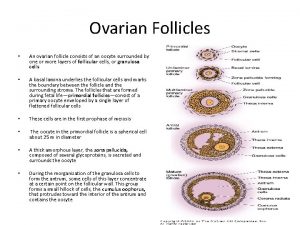
Ovarian cancer causes Ovarian follicle
Ovarian follicle Ovarian cyst
Ovarian cyst Ovarian cycle
Ovarian cycle Ovarian teratoma
Ovarian teratoma Uterus
Uterus Ovarian cancer brca
Ovarian cancer brca Hrd score ovarian cancer
Hrd score ovarian cancer Spermiogenesis
Spermiogenesis Ovarian ligament
Ovarian ligament Ovarian benign tumor
Ovarian benign tumor Sru consensus ovarian cysts
Sru consensus ovarian cysts Benjamin cummings
Benjamin cummings The ovarian cycle
The ovarian cycle The reproductive system chapter 16
The reproductive system chapter 16 Ovarian follicle
Ovarian follicle Ovarian ligament
Ovarian ligament Follicle stage
Follicle stage Liver cyst size chart
Liver cyst size chart A balanced delta connected load having an impedance 20-j15
A balanced delta connected load having an impedance 20-j15 Line vs phase voltage
Line vs phase voltage Energy band diagram of pn junction diode
Energy band diagram of pn junction diode Line current and phase current
Line current and phase current Drift current and diffusion current
Drift current and diffusion current What is diffusion current and drift current
What is diffusion current and drift current The constant current region of a fet lies between
The constant current region of a fet lies between In a triangle connected source feeding a y connected load
In a triangle connected source feeding a y connected load Holding current and latching current
Holding current and latching current Drift current and diffusion current in semiconductor
Drift current and diffusion current in semiconductor Dcep welding
Dcep welding Hazard based safety engineering
Hazard based safety engineering Non planar circuit
Non planar circuit Data management concepts
Data management concepts Concepts of communication
Concepts of communication Virtualization concepts
Virtualization concepts Basic concepts of microprocessor
Basic concepts of microprocessor Compile and go loader scheme
Compile and go loader scheme Ra 10121 salient features
Ra 10121 salient features Six basic concepts of tqm
Six basic concepts of tqm Clock and compass time management
Clock and compass time management Threshold human geography
Threshold human geography Innateness hypothesis
Innateness hypothesis Basic concepts of family
Basic concepts of family Evolution and interpretation of computer architecture
Evolution and interpretation of computer architecture Concepts and terminology
Concepts and terminology Symbolic interactionism concepts
Symbolic interactionism concepts Oops concepts in system verilog
Oops concepts in system verilog A company's resources and capabilities represent
A company's resources and capabilities represent Spreadsheet concepts
Spreadsheet concepts Software testing concepts
Software testing concepts Cognitive psychology concepts
Cognitive psychology concepts What is simple recall test
What is simple recall test Literariness in russian formalism
Literariness in russian formalism Key concepts examples
Key concepts examples Old and new matrix algebra useful for statistics
Old and new matrix algebra useful for statistics Mark tinka
Mark tinka Renewable energy source definition
Renewable energy source definition Chapter 17 promotional concepts and strategies answer key
Chapter 17 promotional concepts and strategies answer key Professional nursing practice concepts and perspectives
Professional nursing practice concepts and perspectives Provision of essential drugs
Provision of essential drugs Period 6 key concepts apush
Period 6 key concepts apush Apush period 5 key concepts
Apush period 5 key concepts Apush review.com
Apush review.com Apush key concepts period 2
Apush key concepts period 2 Pearson physical science concepts in action answers
Pearson physical science concepts in action answers Mqseries primer
Mqseries primer Polymorphism in oops concept
Polymorphism in oops concept