Polycystic ovarian syndrome 2018 Dr Jane Wilcock GP
- Slides: 10
Polycystic ovarian syndrome 2018 Dr Jane Wilcock GP assessment year 4 lead uni of Liverpool BSc FRCGP PGCert. Med. Ed. MAHEd. SFHEA RCOG Long term consequences of PCOS 3 rd Ed Green Top guide Metformin Therapy for the management of infertility in women with PCOS scientific impact paper No 13 BJOG 2017
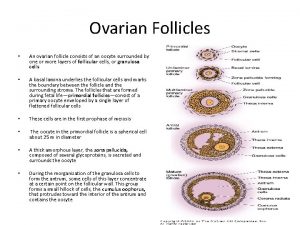
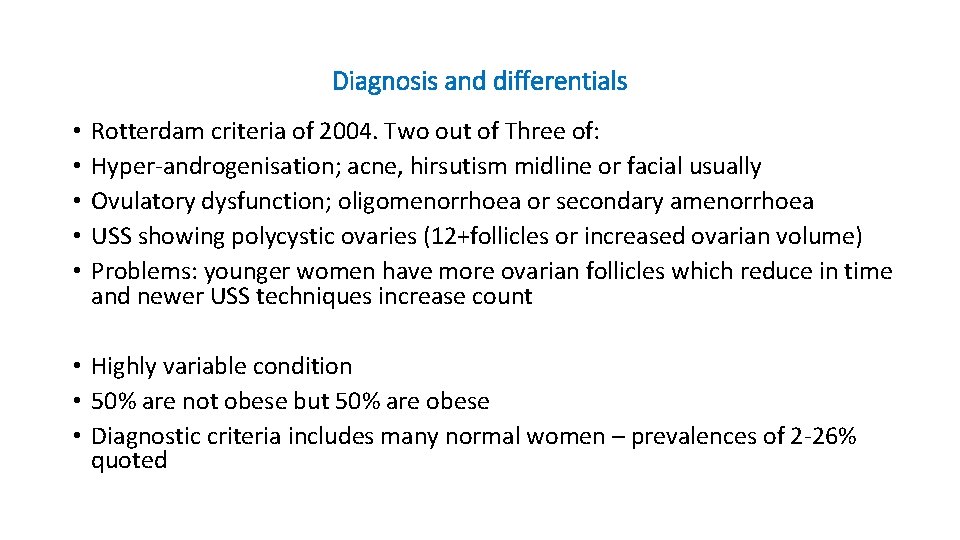
Diagnosis and differentials • • • Rotterdam criteria of 2004. Two out of Three of: Hyper-androgenisation; acne, hirsutism midline or facial usually Ovulatory dysfunction; oligomenorrhoea or secondary amenorrhoea USS showing polycystic ovaries (12+follicles or increased ovarian volume) Problems: younger women have more ovarian follicles which reduce in time and newer USS techniques increase count • Highly variable condition • 50% are not obese but 50% are obese • Diagnostic criteria includes many normal women – prevalences of 2 -26% quoted
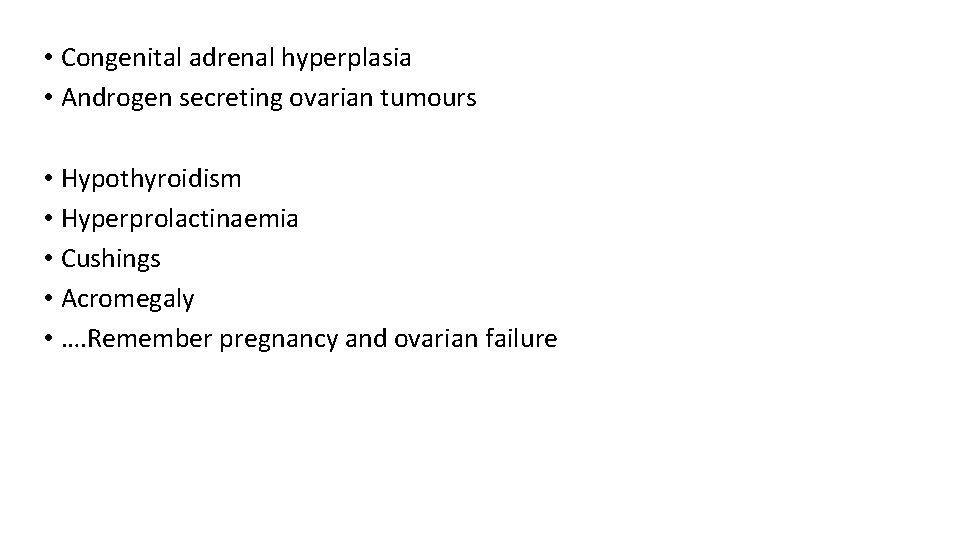
• Congenital adrenal hyperplasia • Androgen secreting ovarian tumours • Hypothyroidism • Hyperprolactinaemia • Cushings • Acromegaly • …. Remember pregnancy and ovarian failure
Risks and associations • T 2 DM; insulin resistance; IGT • Obesity and its sequelae • Dyslipidaemia: Qrisk not validated in PCOS but seems reasonable to use ( statins CI in pregnancy) • Hypertension • Depression • Endometrial hyperplasia… atypical…cancer • Hirsutism, alopecia • Acne • Subfertility • Fatigue, somnolence, sleep apnoea
investigations • USS plus • Blood for free androgen index (total testosterone/SHBG x 100) • Total testosterone>5 nmol/L or x 2 upper limit of normal consider tumour or Congenital adrenal hyperplasia • OPC do a 17 hydroxyprogesterone level in follicular phase • Consider referral if rapid/recent androgenisation
Insulin resistance (IR) • Up to 15% slim PCOS and 40% obese PCOS • High insulin levels stimulate ovarian androgen secretion • Insulin reduced sex hormone binding globulin production in liver so increases free androgens in plasma • Higher BMI increases IR • Rate of T 2 DM in women with IR with PCOS is estimated at 10% • FBG and Hb. A 1 c. May need GTT to assess in subfertility or as well person assessment and in pregnancy
Metformin in PCOS • Does not improve weight loss compared to exercise and calorie restriction • In anovulation less effective than clomiphene in helping conception • (metformin may be added in before moving to ovarian drilling) • Safe in pregnancy for fetus • May reduce miscarriage in obese women • 16% women report side-effects (GIT) • Long-term use not evidence based for improving metabolic parameters
Endometrial hyperplasia • Abnormal uterine bleeding or amenorrhoea >3 months consider pelvic USS. This may require specialist FU if a repeating pattern • Endometrial thickness <7 mm ( non PCOS< 4 -5 mm) associated with low probability of endometrial hyperplasia (specialist) • Thick endometrium or polyps prompt endometrial biopsy/ hysteroscopy • X 2 -3 risk of endometrial cancer, esp. premenopause • OPC may insert LNG-IUS or 12 days progesterone tablets in a cycle to induce a bleed if >3 months amenorrhoea • No association with breast or ovarian cancer
Treatment PCOS • • Diet, exercise, weight loss first line Loss of 5% body weight reduces testosterone, IR and CVD risk factors Possibly orlistat (not if trying to conceive) Lap bypass if BMI>40 or BMI>35+ other factor like T 2 DM. May reduce excess weight by 60%; can reverse the diagnosis Antidiabetic drugs are either not licensed or not shown to have outcome benefits at present unless patients also have T 2 DM Metformin may reduce testosterone levels by 11% Preconception in pregnancy is folic acid 5 mg a day Support group: www. verity-pcos. org. uk
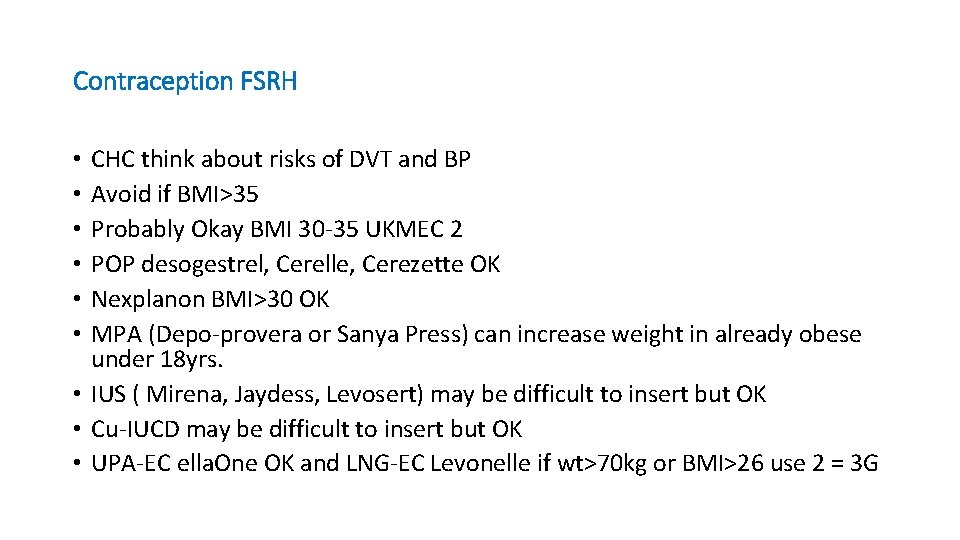
Contraception FSRH CHC think about risks of DVT and BP Avoid if BMI>35 Probably Okay BMI 30 -35 UKMEC 2 POP desogestrel, Cerelle, Cerezette OK Nexplanon BMI>30 OK MPA (Depo-provera or Sanya Press) can increase weight in already obese under 18 yrs. • IUS ( Mirena, Jaydess, Levosert) may be difficult to insert but OK • Cu-IUCD may be difficult to insert but OK • UPA-EC ella. One OK and LNG-EC Levonelle if wt>70 kg or BMI>26 use 2 = 3 G • • •