23 Year Old Female with polycystic ovarian syndrome

- Slides: 36
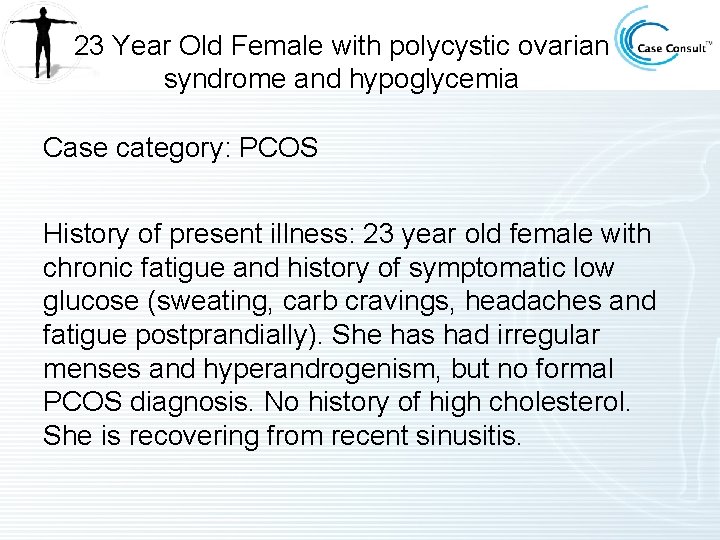
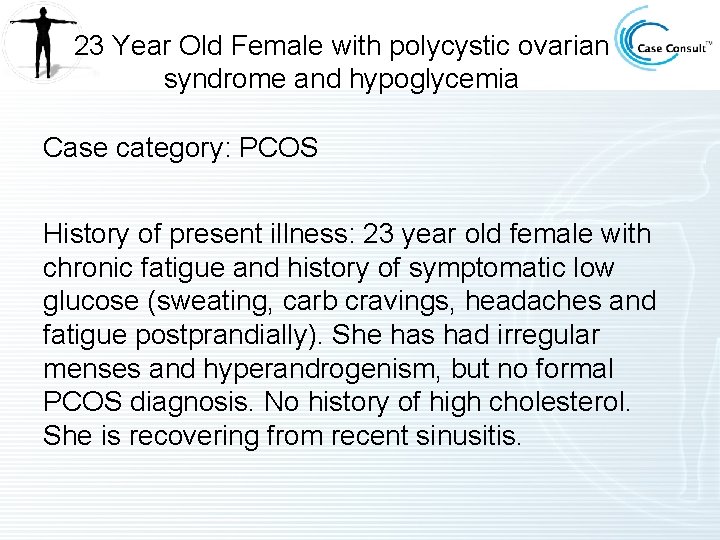
23 Year Old Female with polycystic ovarian syndrome and hypoglycemia Case category: PCOS History of present illness: 23 year old female with chronic fatigue and history of symptomatic low glucose (sweating, carb cravings, headaches and fatigue postprandially). She has had irregular menses and hyperandrogenism, but no formal PCOS diagnosis. No history of high cholesterol. She is recovering from recent sinusitis.
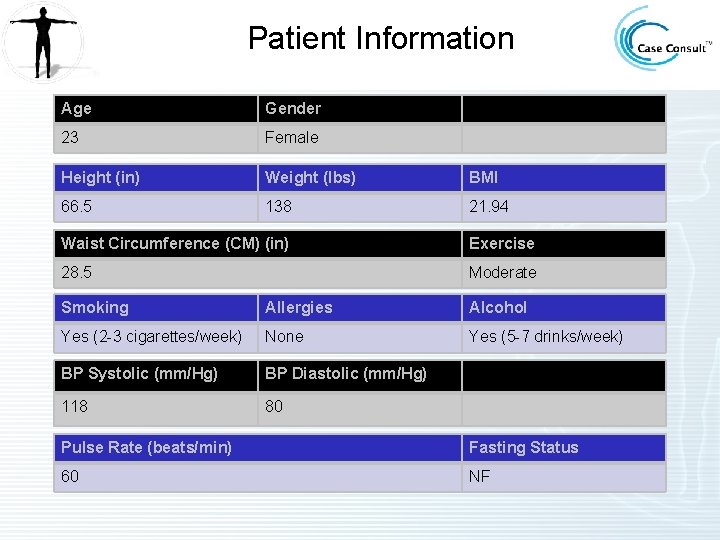
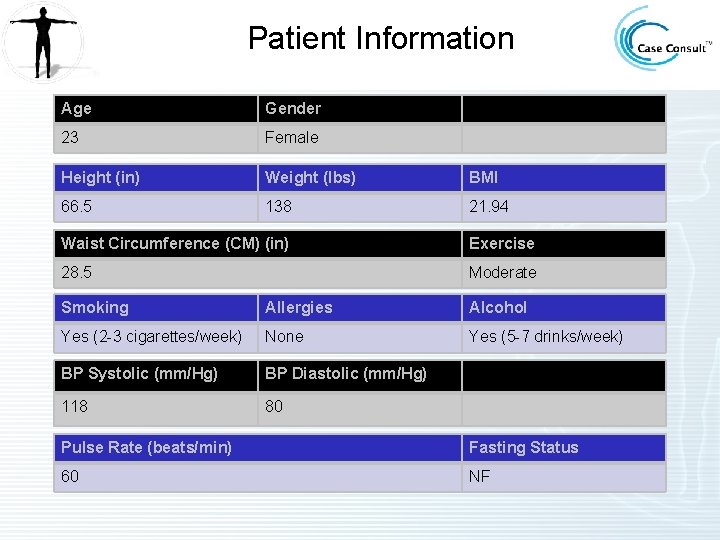
Patient Information Age Gender 23 Female Height (in) Weight (lbs) BMI 66. 5 138 21. 94 Waist Circumference (CM) (in) Exercise 28. 5 Moderate Smoking Allergies Alcohol Yes (2 -3 cigarettes/week) None Yes (5 -7 drinks/week) BP Systolic (mm/Hg) BP Diastolic (mm/Hg) 118 80 Pulse Rate (beats/min) Fasting Status 60 NF
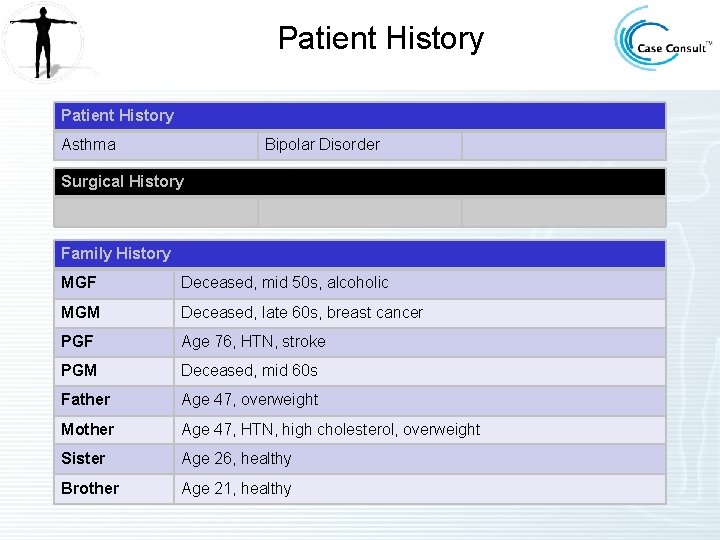
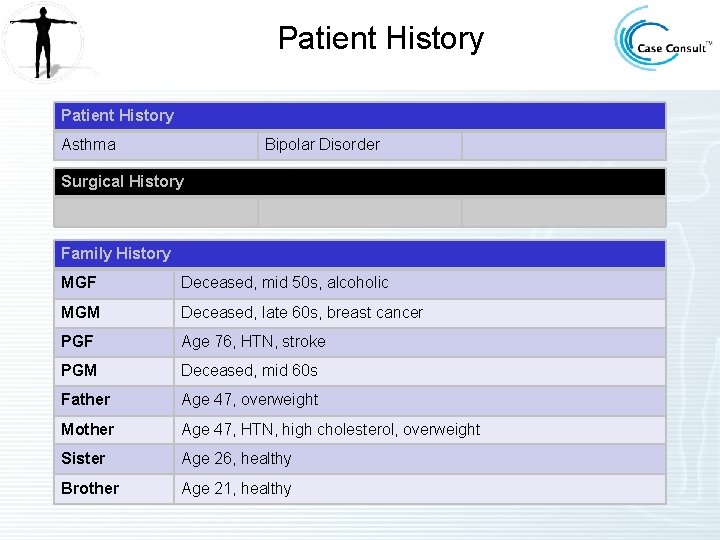
Patient History Asthma Bipolar Disorder Surgical History Family History MGF Deceased, mid 50 s, alcoholic MGM Deceased, late 60 s, breast cancer PGF Age 76, HTN, stroke PGM Deceased, mid 60 s Father Age 47, overweight Mother Age 47, HTN, high cholesterol, overweight Sister Age 26, healthy Brother Age 21, healthy
Current Medications Current Medication Prior to this Visit None
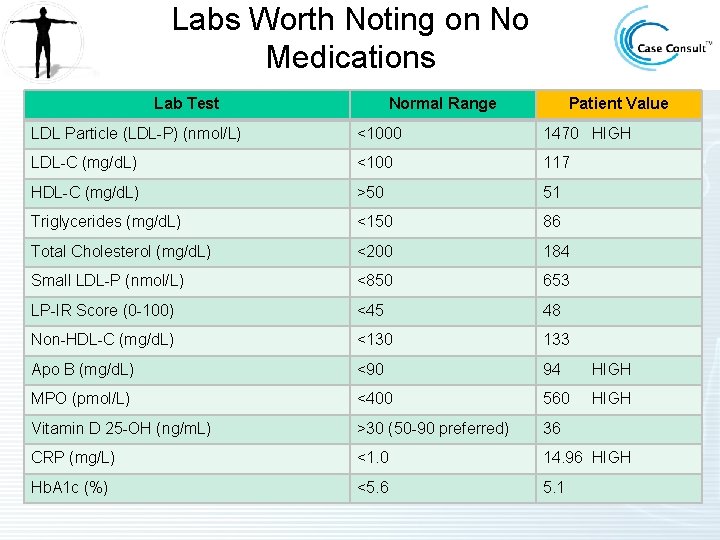
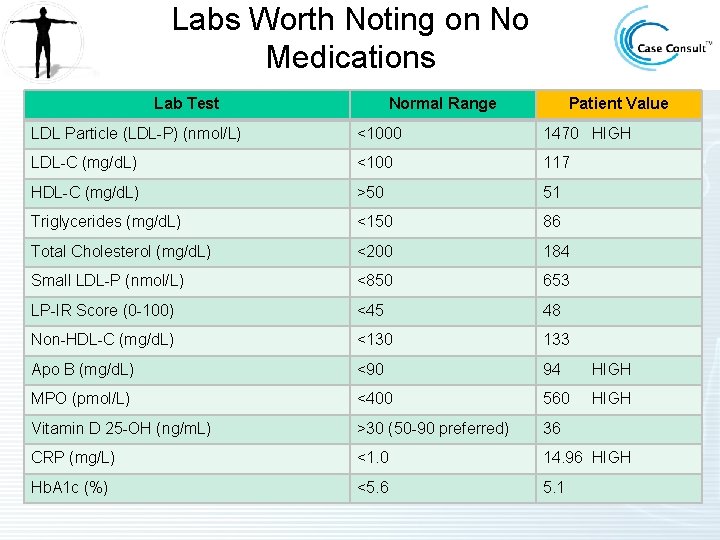
Labs Worth Noting on No Medications Lab Test Normal Range Patient Value LDL Particle (LDL-P) (nmol/L) <1000 1470 HIGH LDL-C (mg/d. L) <100 117 HDL-C (mg/d. L) >50 51 Triglycerides (mg/d. L) <150 86 Total Cholesterol (mg/d. L) <200 184 Small LDL-P (nmol/L) <850 653 LP-IR Score (0 -100) <45 48 Non-HDL-C (mg/d. L) <130 133 Apo B (mg/d. L) <90 94 HIGH MPO (pmol/L) <400 560 HIGH Vitamin D 25 -OH (ng/m. L) >30 (50 -90 preferred) 36 CRP (mg/L) <1. 0 14. 96 HIGH Hb. A 1 c (%) <5. 6 5. 1
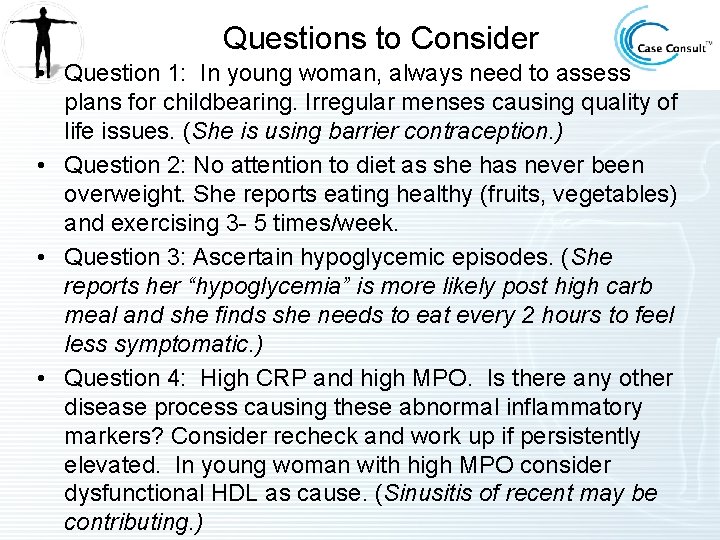
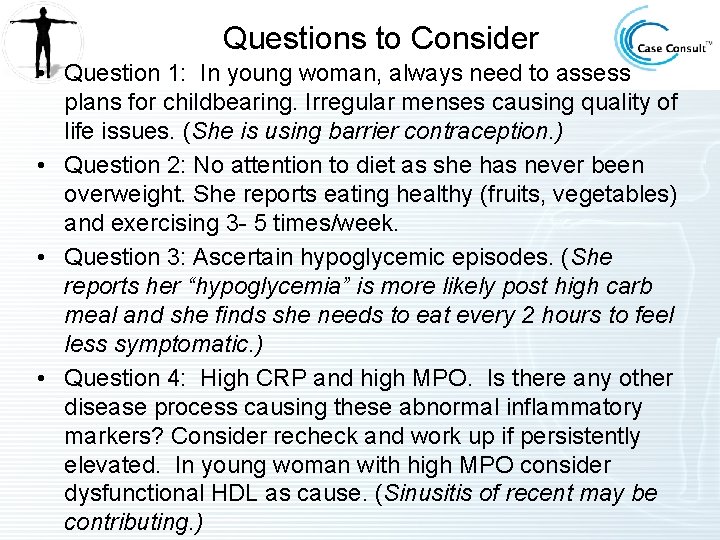
Questions to Consider • Question 1: In young woman, always need to assess plans for childbearing. Irregular menses causing quality of life issues. (She is using barrier contraception. ) • Question 2: No attention to diet as she has never been overweight. She reports eating healthy (fruits, vegetables) and exercising 3 - 5 times/week. • Question 3: Ascertain hypoglycemic episodes. (She reports her “hypoglycemia” is more likely post high carb meal and she finds she needs to eat every 2 hours to feel less symptomatic. ) • Question 4: High CRP and high MPO. Is there any other disease process causing these abnormal inflammatory markers? Consider recheck and work up if persistently elevated. In young woman with high MPO consider dysfunctional HDL as cause. (Sinusitis of recent may be contributing. )
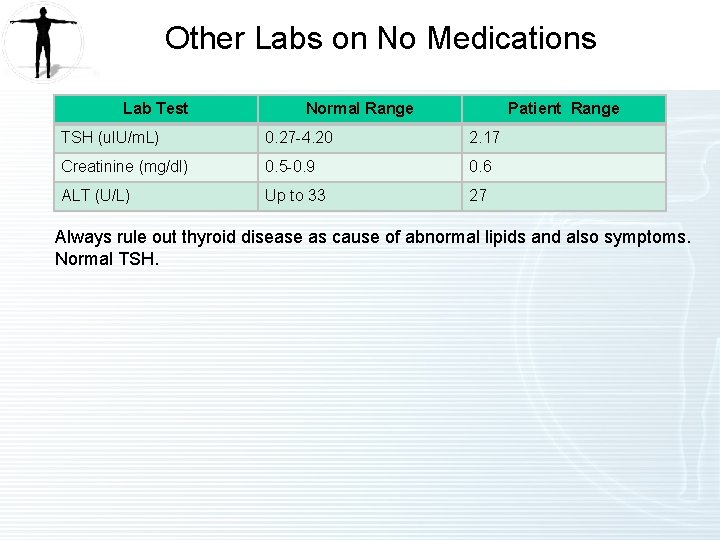
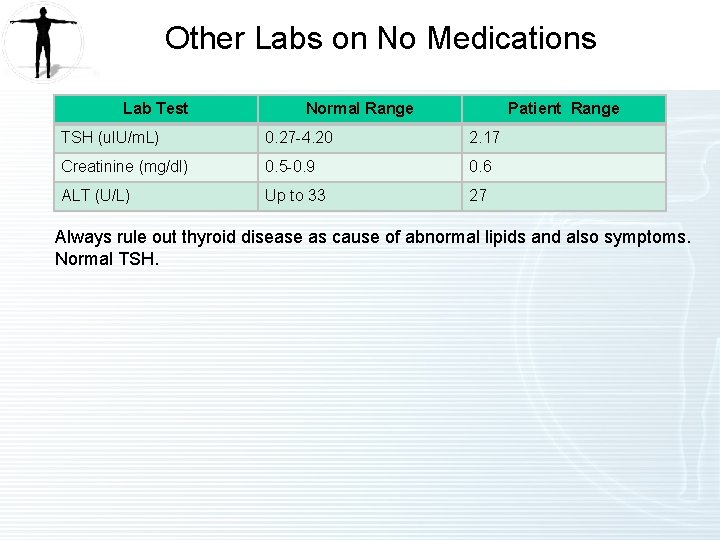
Other Labs on No Medications Lab Test Normal Range Patient Range TSH (u. IU/m. L) 0. 27 -4. 20 2. 17 Creatinine (mg/dl) 0. 5 -0. 9 0. 6 ALT (U/L) Up to 33 27 Always rule out thyroid disease as cause of abnormal lipids and also symptoms. Normal TSH.
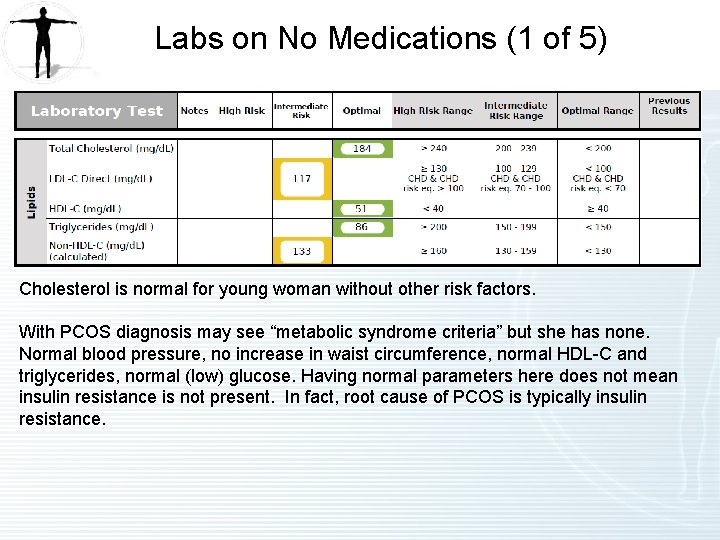
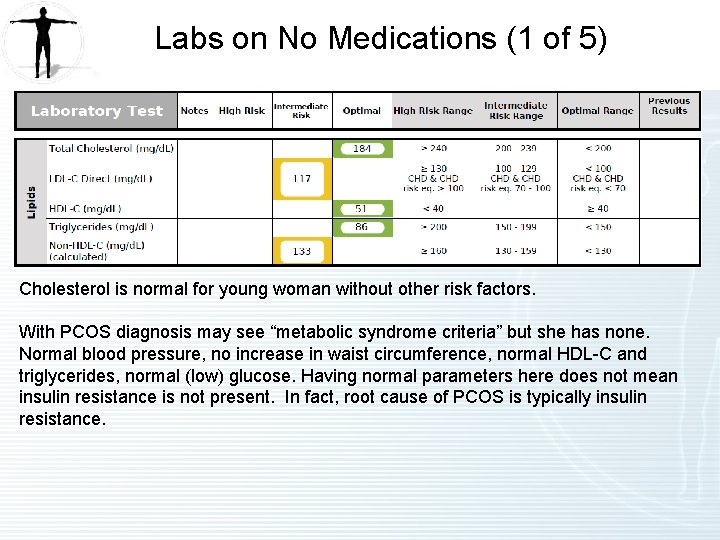
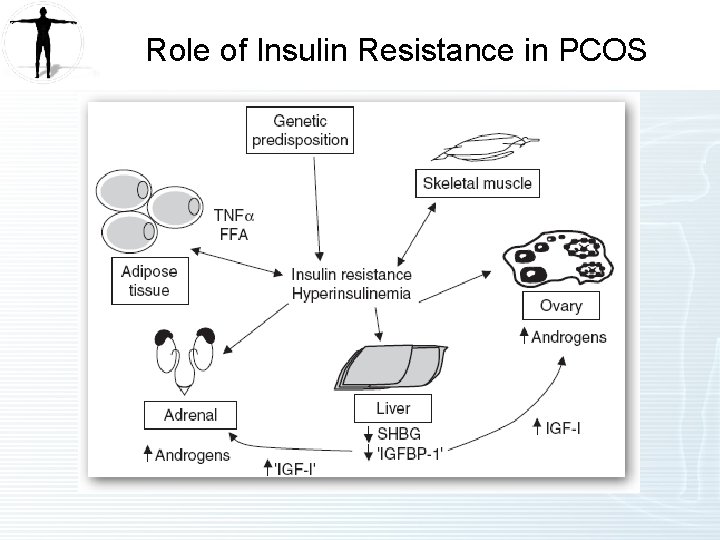
Labs on No Medications (1 of 5) Cholesterol is normal for young woman without other risk factors. With PCOS diagnosis may see “metabolic syndrome criteria” but she has none. Normal blood pressure, no increase in waist circumference, normal HDL-C and triglycerides, normal (low) glucose. Having normal parameters here does not mean insulin resistance is not present. In fact, root cause of PCOS is typically insulin resistance.
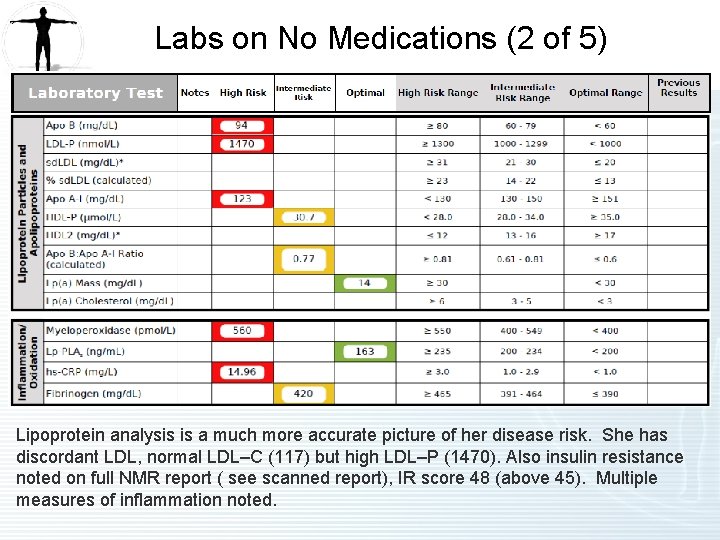
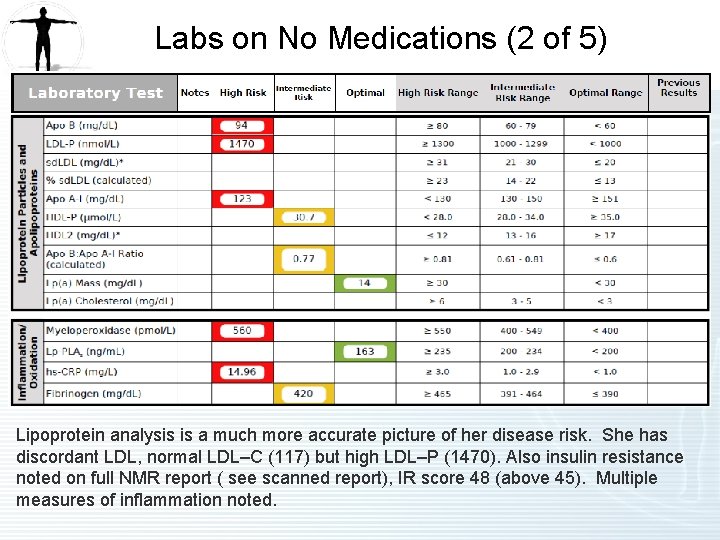
Labs on No Medications (2 of 5) Lipoprotein analysis is a much more accurate picture of her disease risk. She has discordant LDL, normal LDL–C (117) but high LDL–P (1470). Also insulin resistance noted on full NMR report ( see scanned report), IR score 48 (above 45). Multiple measures of inflammation noted.
NMR Lipo. Profile • Insert NMR Lipoprofile 07122011 DW 88 Insert
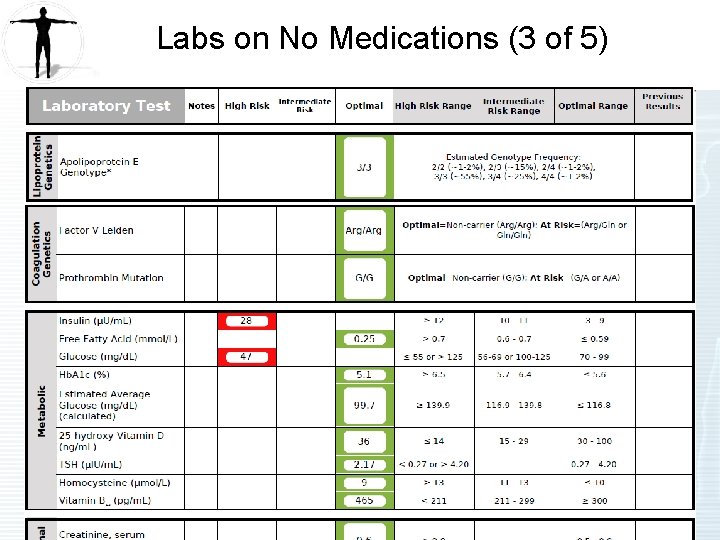
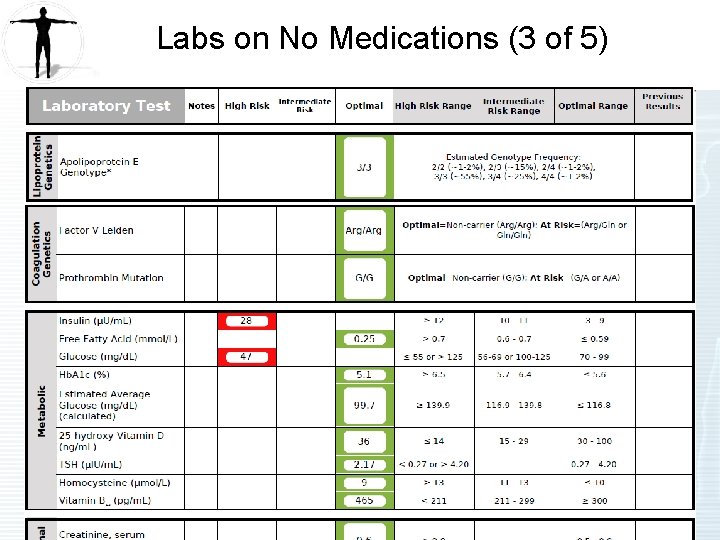
Labs on No Medications (3 of 5)
Comments regarding genetic testing • She had additional genetic testing done to better define her cardiovascular risk as there were some unknown early deaths in her family history. She reassuringly has normal apo E genotype E 3 E 3 but also normal Factor V and prothrombin. This is important to know in a young woman that may be prescribed oral contraceptive hormone therapy. I would not prescribe oral estrogen if high risk mutations in either of these present. This would increase her DVT risk. PCOS often is treated with OCPs when irregular menses present.
Hypoglycemia • She has self-reported “hypoglycemia”, which is confirmed with high insulin and low glucose on this report. She also has low normal Hb. A 1 C at 5. 1. This is very common in the setting of insulin resistance. She has insulin resistance which causes the pancreas to work harder when glucose load postmeal, this leads to hyperinsulinemia which in turn drops her glucose low.
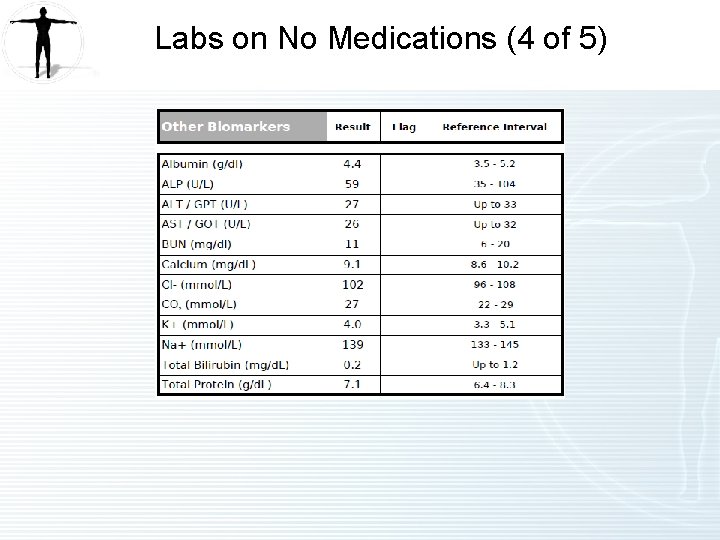
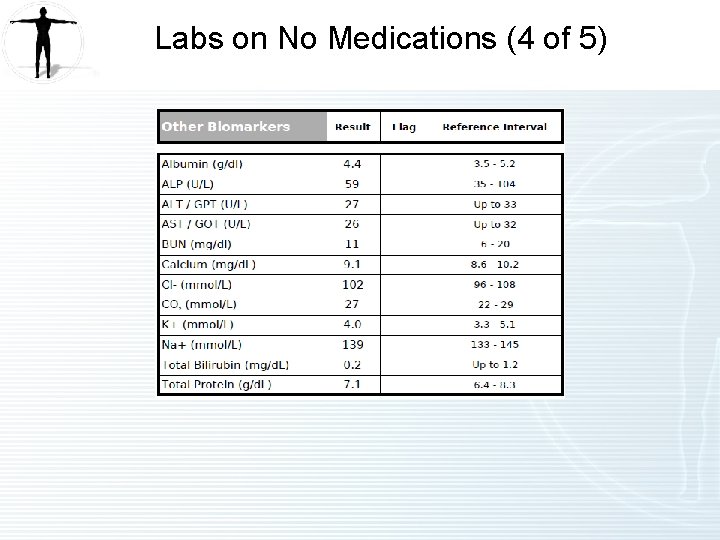
Labs on No Medications (4 of 5)
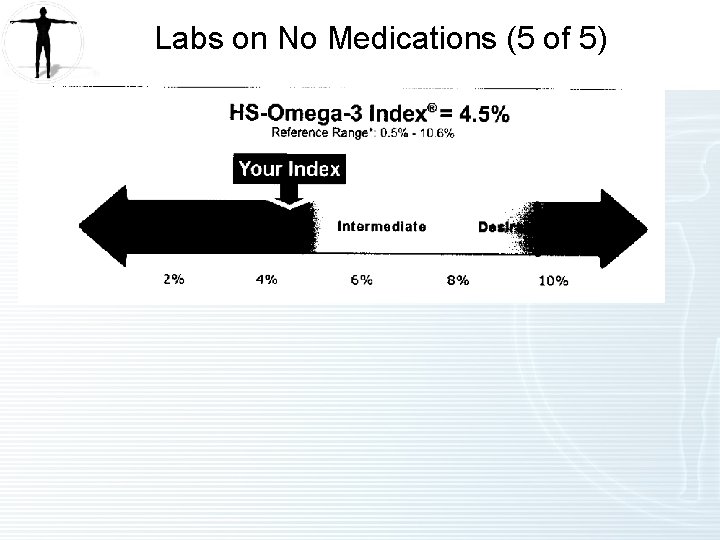
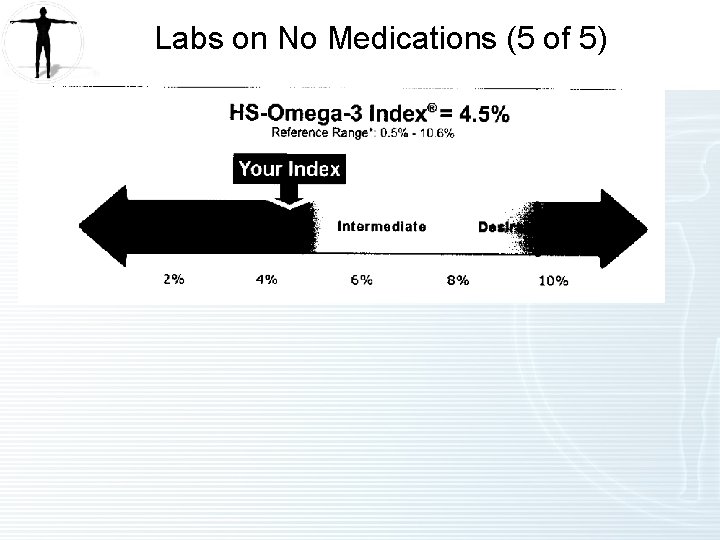
Labs on No Medications (5 of 5)
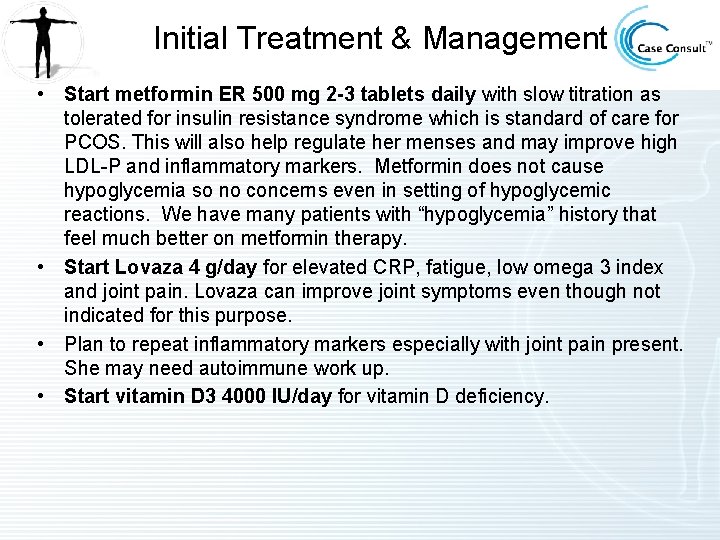
Initial Treatment & Management • Start metformin ER 500 mg 2 -3 tablets daily with slow titration as tolerated for insulin resistance syndrome which is standard of care for PCOS. This will also help regulate her menses and may improve high LDL-P and inflammatory markers. Metformin does not cause hypoglycemia so no concerns even in setting of hypoglycemic reactions. We have many patients with “hypoglycemia” history that feel much better on metformin therapy. • Start Lovaza 4 g/day for elevated CRP, fatigue, low omega 3 index and joint pain. Lovaza can improve joint symptoms even though not indicated for this purpose. • Plan to repeat inflammatory markers especially with joint pain present. She may need autoimmune work up. • Start vitamin D 3 4000 IU/day for vitamin D deficiency.
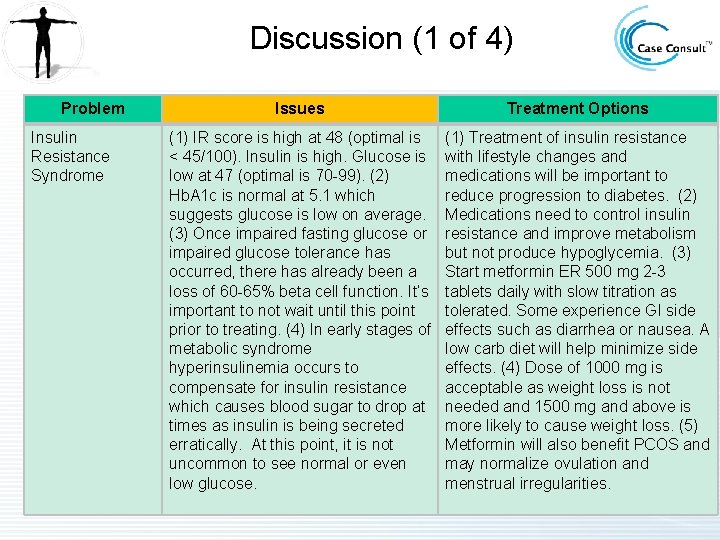
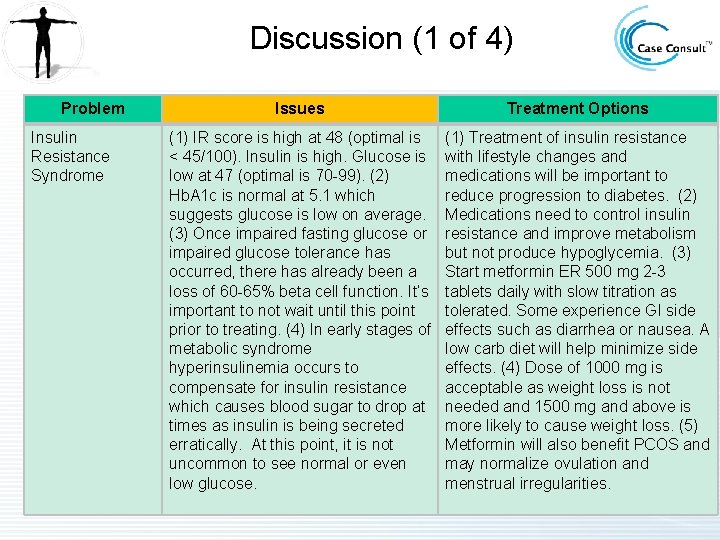
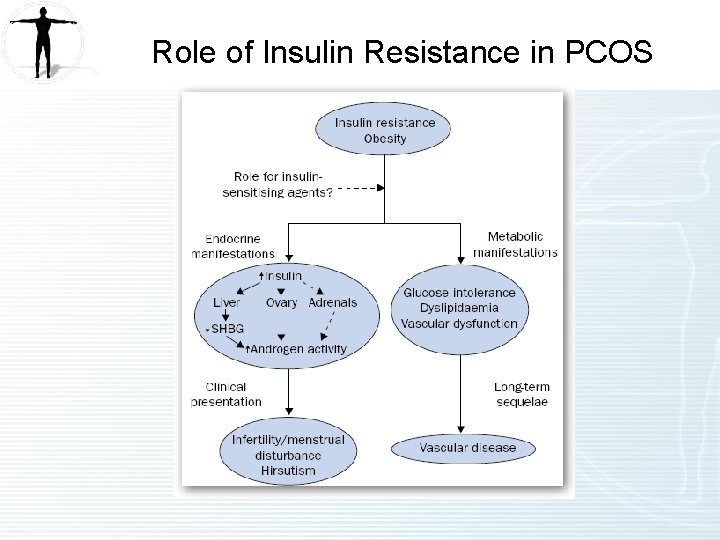
Discussion (1 of 4) Problem Insulin Resistance Syndrome Issues Treatment Options (1) IR score is high at 48 (optimal is < 45/100). Insulin is high. Glucose is low at 47 (optimal is 70 -99). (2) Hb. A 1 c is normal at 5. 1 which suggests glucose is low on average. (3) Once impaired fasting glucose or impaired glucose tolerance has occurred, there has already been a loss of 60 -65% beta cell function. It’s important to not wait until this point prior to treating. (4) In early stages of metabolic syndrome hyperinsulinemia occurs to compensate for insulin resistance which causes blood sugar to drop at times as insulin is being secreted erratically. At this point, it is not uncommon to see normal or even low glucose. (1) Treatment of insulin resistance with lifestyle changes and medications will be important to reduce progression to diabetes. (2) Medications need to control insulin resistance and improve metabolism but not produce hypoglycemia. (3) Start metformin ER 500 mg 2 -3 tablets daily with slow titration as tolerated. Some experience GI side effects such as diarrhea or nausea. A low carb diet will help minimize side effects. (4) Dose of 1000 mg is acceptable as weight loss is not needed and 1500 mg and above is more likely to cause weight loss. (5) Metformin will also benefit PCOS and may normalize ovulation and menstrual irregularities.
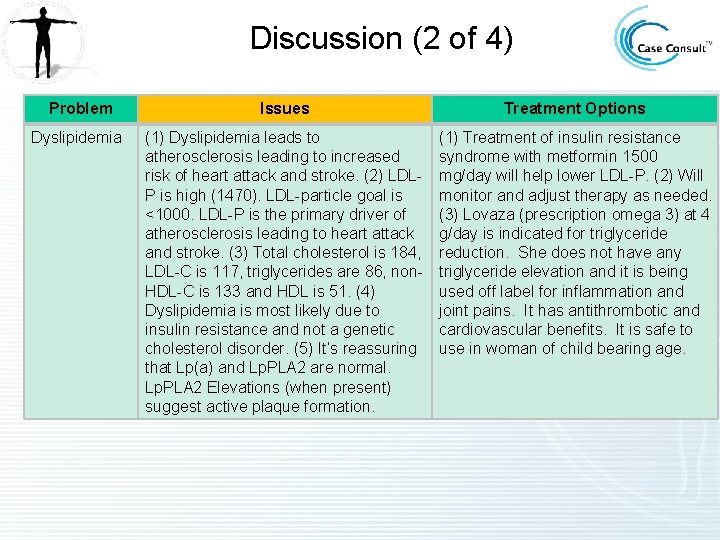
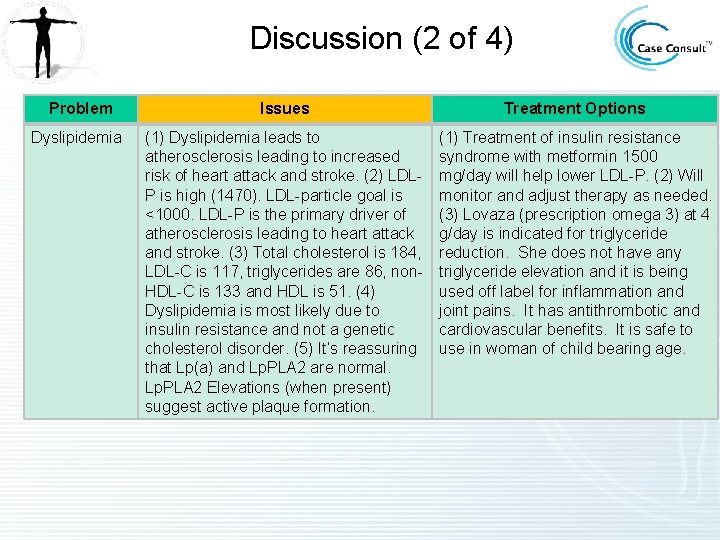
Discussion (2 of 4) Problem Issues Treatment Options Dyslipidemia (1) Dyslipidemia leads to atherosclerosis leading to increased risk of heart attack and stroke. (2) LDLP is high (1470). LDL-particle goal is <1000. LDL-P is the primary driver of atherosclerosis leading to heart attack and stroke. (3) Total cholesterol is 184, LDL-C is 117, triglycerides are 86, non. HDL-C is 133 and HDL is 51. (4) Dyslipidemia is most likely due to insulin resistance and not a genetic cholesterol disorder. (5) It’s reassuring that Lp(a) and Lp. PLA 2 are normal. Lp. PLA 2 Elevations (when present) suggest active plaque formation. (1) Treatment of insulin resistance syndrome with metformin 1500 mg/day will help lower LDL-P. (2) Will monitor and adjust therapy as needed. (3) Lovaza (prescription omega 3) at 4 g/day is indicated for triglyceride reduction. She does not have any triglyceride elevation and it is being used off label for inflammation and joint pains. It has antithrombotic and cardiovascular benefits. It is safe to use in woman of child bearing age.
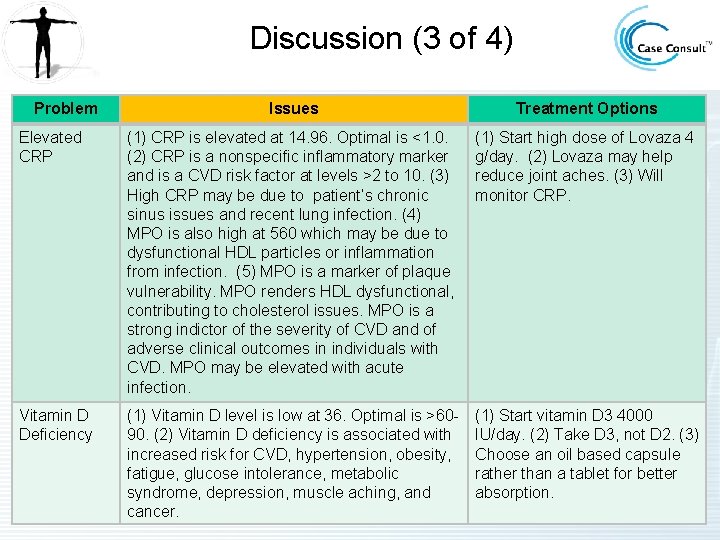
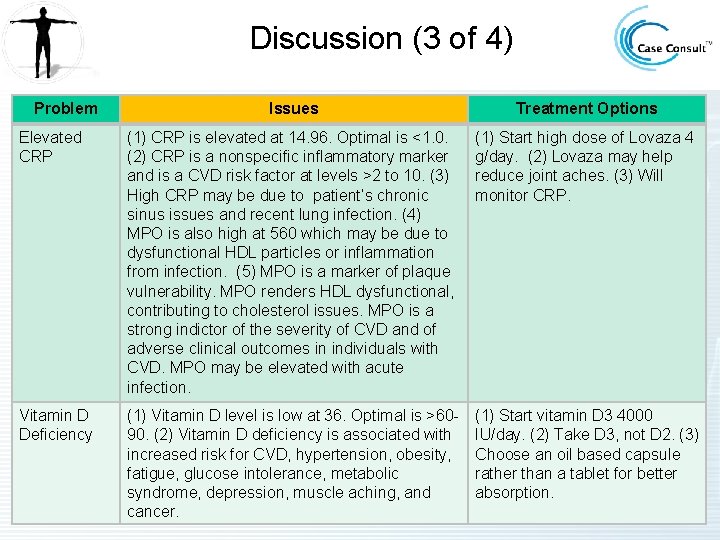
Discussion (3 of 4) Problem Issues Treatment Options Elevated CRP (1) CRP is elevated at 14. 96. Optimal is <1. 0. (2) CRP is a nonspecific inflammatory marker and is a CVD risk factor at levels >2 to 10. (3) High CRP may be due to patient’s chronic sinus issues and recent lung infection. (4) MPO is also high at 560 which may be due to dysfunctional HDL particles or inflammation from infection. (5) MPO is a marker of plaque vulnerability. MPO renders HDL dysfunctional, contributing to cholesterol issues. MPO is a strong indictor of the severity of CVD and of adverse clinical outcomes in individuals with CVD. MPO may be elevated with acute infection. (1) Start high dose of Lovaza 4 g/day. (2) Lovaza may help reduce joint aches. (3) Will monitor CRP. Vitamin D Deficiency (1) Vitamin D level is low at 36. Optimal is >6090. (2) Vitamin D deficiency is associated with increased risk for CVD, hypertension, obesity, fatigue, glucose intolerance, metabolic syndrome, depression, muscle aching, and cancer. (1) Start vitamin D 3 4000 IU/day. (2) Take D 3, not D 2. (3) Choose an oil based capsule rather than a tablet for better absorption.
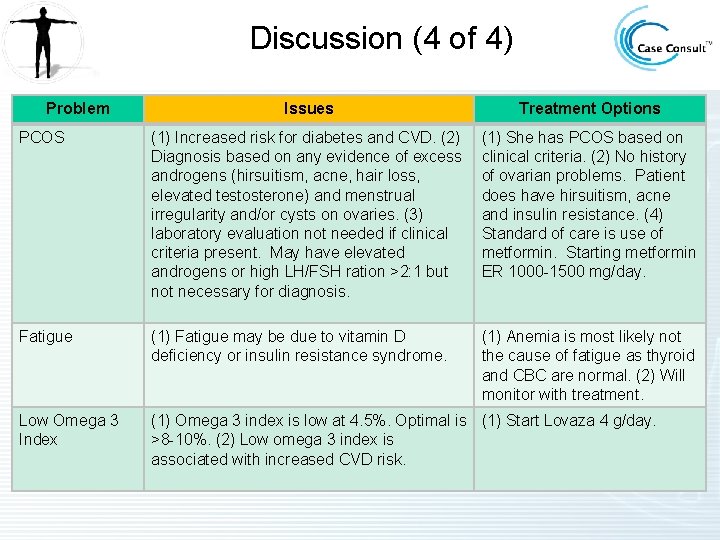
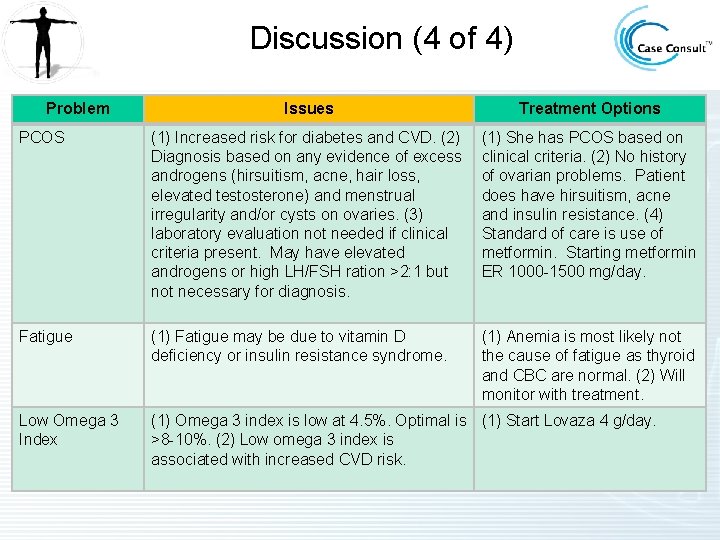
Discussion (4 of 4) Problem Issues Treatment Options PCOS (1) Increased risk for diabetes and CVD. (2) Diagnosis based on any evidence of excess androgens (hirsuitism, acne, hair loss, elevated testosterone) and menstrual irregularity and/or cysts on ovaries. (3) laboratory evaluation not needed if clinical criteria present. May have elevated androgens or high LH/FSH ration >2: 1 but not necessary for diagnosis. (1) She has PCOS based on clinical criteria. (2) No history of ovarian problems. Patient does have hirsuitism, acne and insulin resistance. (4) Standard of care is use of metformin. Starting metformin ER 1000 -1500 mg/day. Fatigue (1) Fatigue may be due to vitamin D deficiency or insulin resistance syndrome. (1) Anemia is most likely not the cause of fatigue as thyroid and CBC are normal. (2) Will monitor with treatment. Low Omega 3 Index (1) Omega 3 index is low at 4. 5%. Optimal is (1) Start Lovaza 4 g/day. >8 -10%. (2) Low omega 3 index is associated with increased CVD risk.
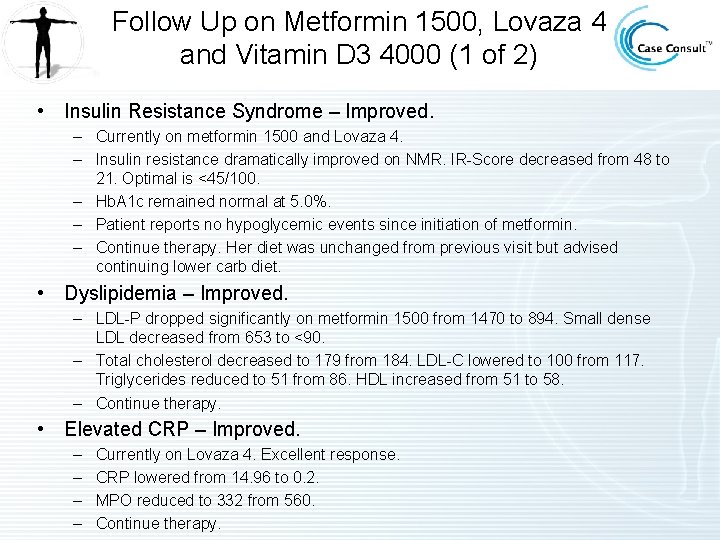
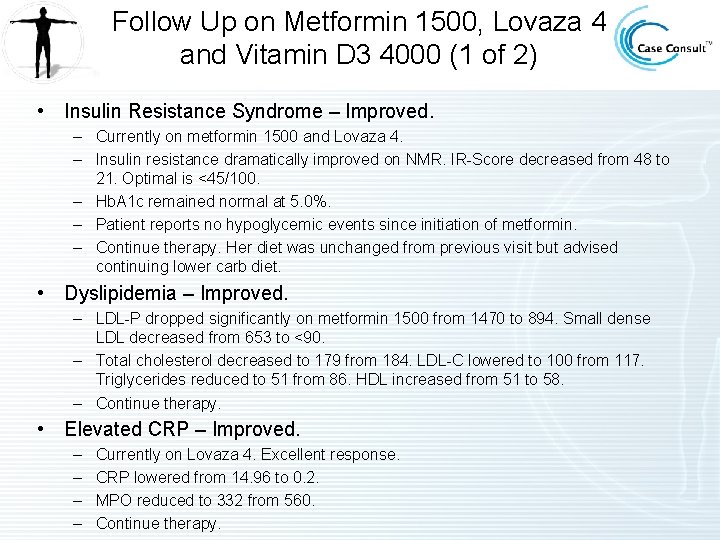
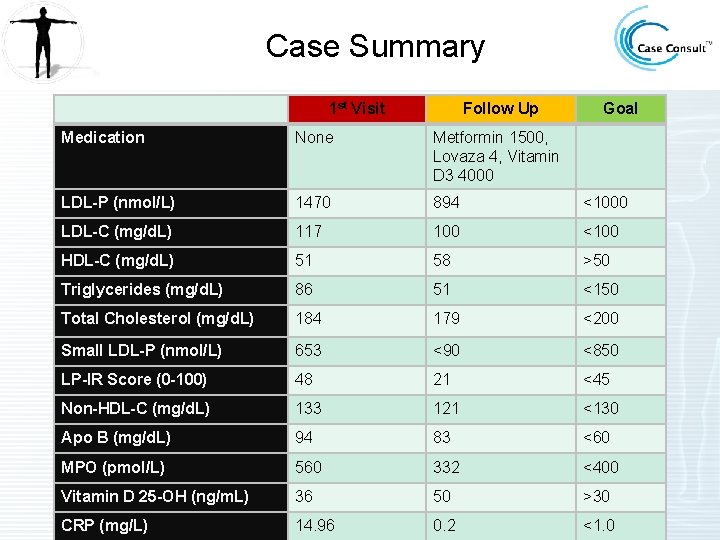
Follow Up on Metformin 1500, Lovaza 4 and Vitamin D 3 4000 (1 of 2) • Insulin Resistance Syndrome – Improved. – Currently on metformin 1500 and Lovaza 4. – Insulin resistance dramatically improved on NMR. IR-Score decreased from 48 to 21. Optimal is <45/100. – Hb. A 1 c remained normal at 5. 0%. – Patient reports no hypoglycemic events since initiation of metformin. – Continue therapy. Her diet was unchanged from previous visit but advised continuing lower carb diet. • Dyslipidemia – Improved. – LDL-P dropped significantly on metformin 1500 from 1470 to 894. Small dense LDL decreased from 653 to <90. – Total cholesterol decreased to 179 from 184. LDL-C lowered to 100 from 117. Triglycerides reduced to 51 from 86. HDL increased from 51 to 58. – Continue therapy. • Elevated CRP – Improved. – – Currently on Lovaza 4. Excellent response. CRP lowered from 14. 96 to 0. 2. MPO reduced to 332 from 560. Continue therapy.
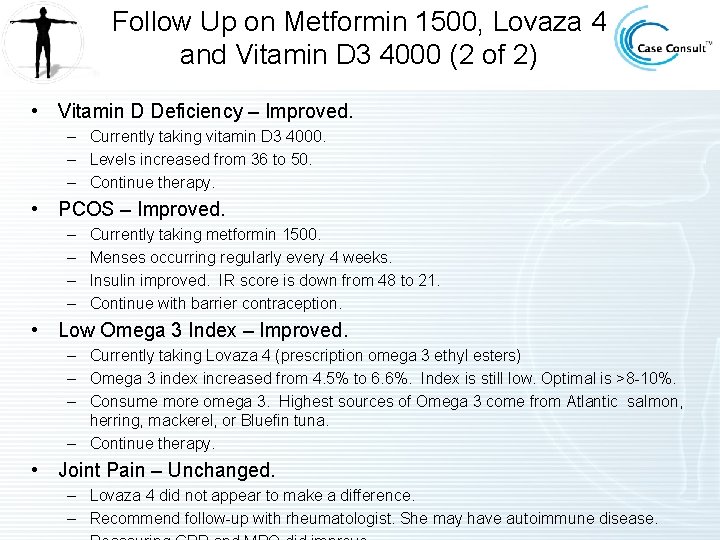
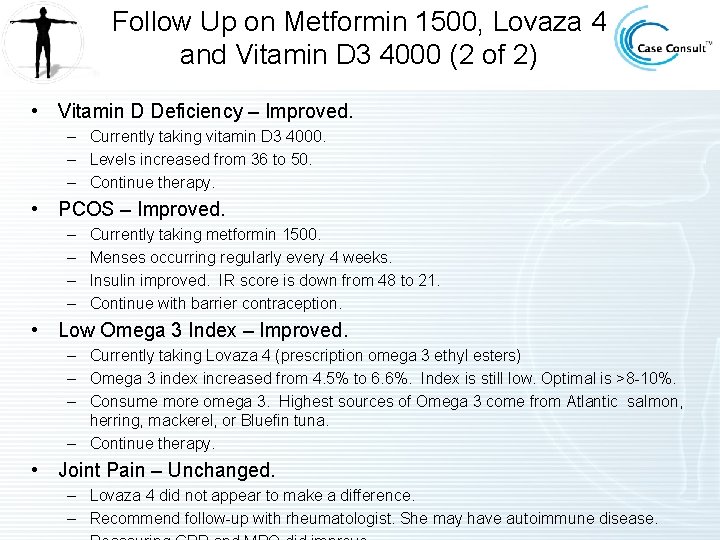
Follow Up on Metformin 1500, Lovaza 4 and Vitamin D 3 4000 (2 of 2) • Vitamin D Deficiency – Improved. – Currently taking vitamin D 3 4000. – Levels increased from 36 to 50. – Continue therapy. • PCOS – Improved. – – Currently taking metformin 1500. Menses occurring regularly every 4 weeks. Insulin improved. IR score is down from 48 to 21. Continue with barrier contraception. • Low Omega 3 Index – Improved. – Currently taking Lovaza 4 (prescription omega 3 ethyl esters) – Omega 3 index increased from 4. 5% to 6. 6%. Index is still low. Optimal is >8 -10%. – Consume more omega 3. Highest sources of Omega 3 come from Atlantic salmon, herring, mackerel, or Bluefin tuna. – Continue therapy. • Joint Pain – Unchanged. – Lovaza 4 did not appear to make a difference. – Recommend follow-up with rheumatologist. She may have autoimmune disease.
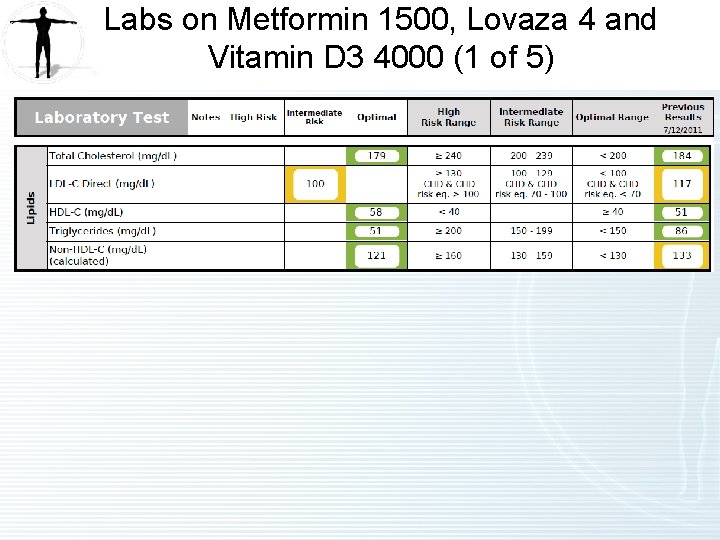
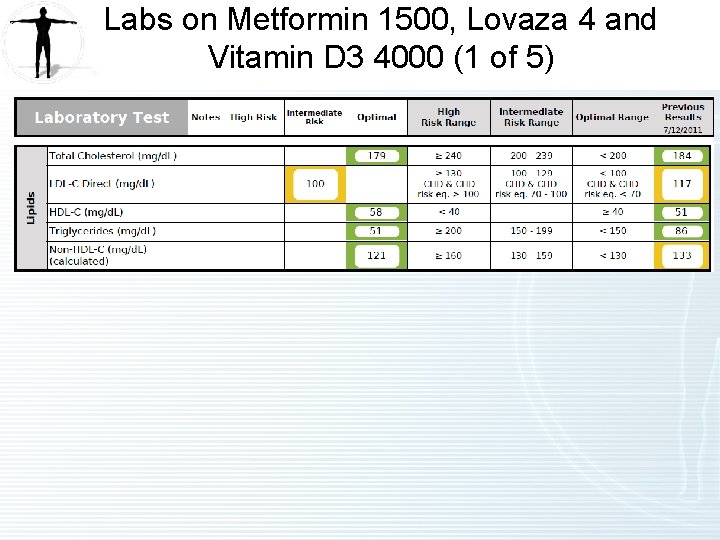
Labs on Metformin 1500, Lovaza 4 and Vitamin D 3 4000 (1 of 5)

Labs on Metformin 1500, Lovaza 4 and Vitamin D 3 4000 (2 of 5)
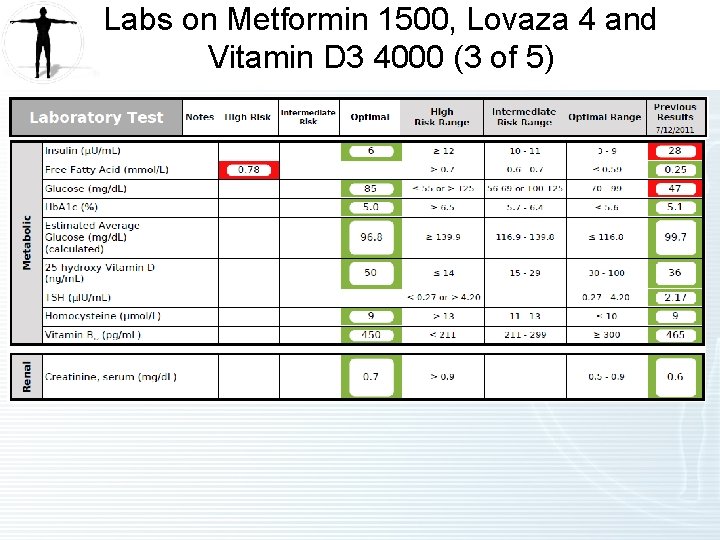
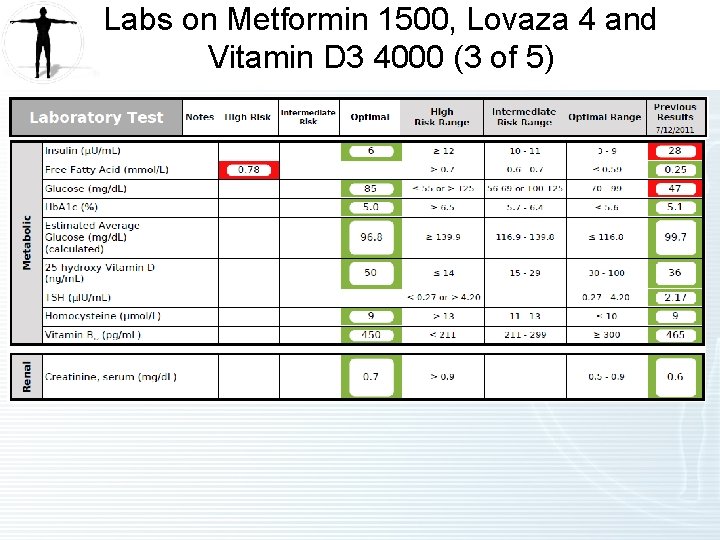
Labs on Metformin 1500, Lovaza 4 and Vitamin D 3 4000 (3 of 5)
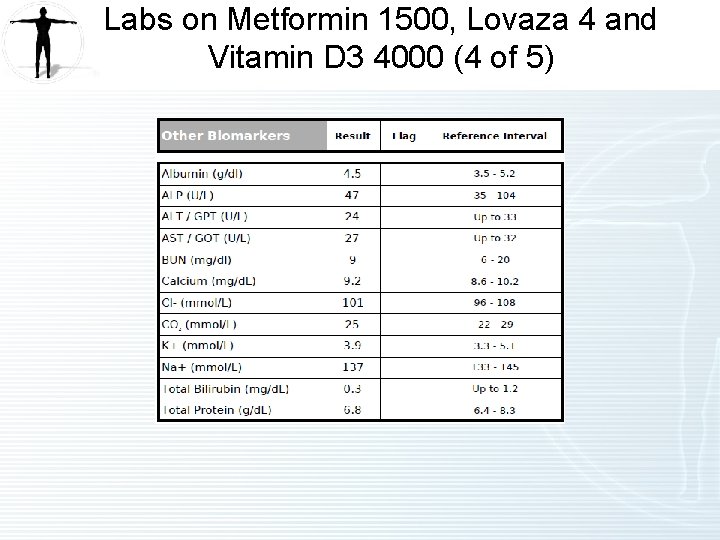
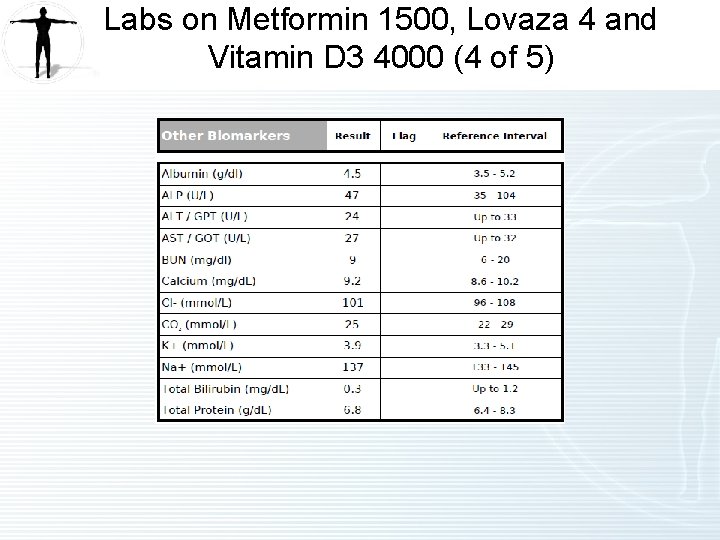
Labs on Metformin 1500, Lovaza 4 and Vitamin D 3 4000 (4 of 5)
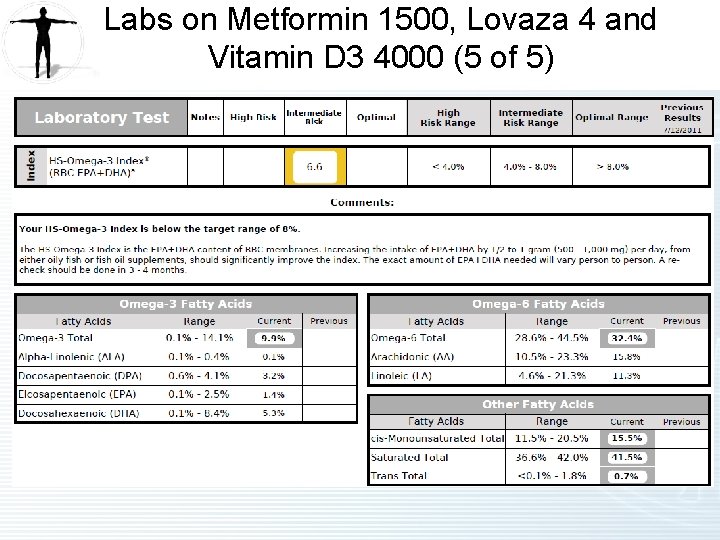
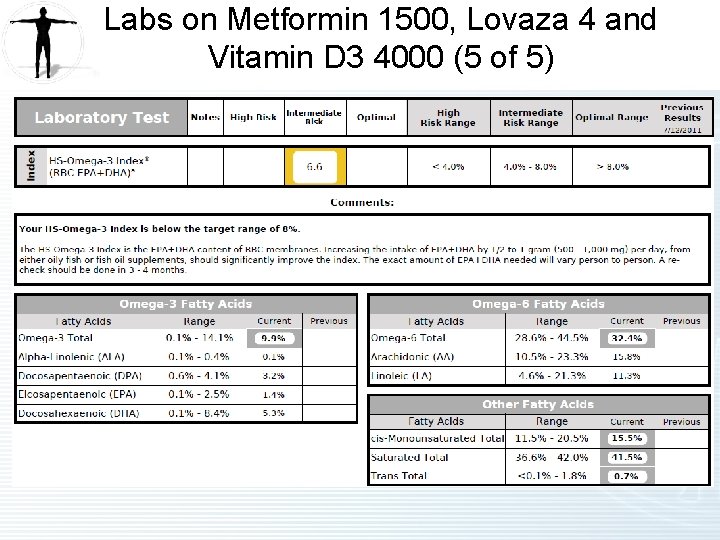
Labs on Metformin 1500, Lovaza 4 and Vitamin D 3 4000 (5 of 5)
NMR Lipo. Profile • Insert NMR Lipoprofile 10192011 DW 88 Insert
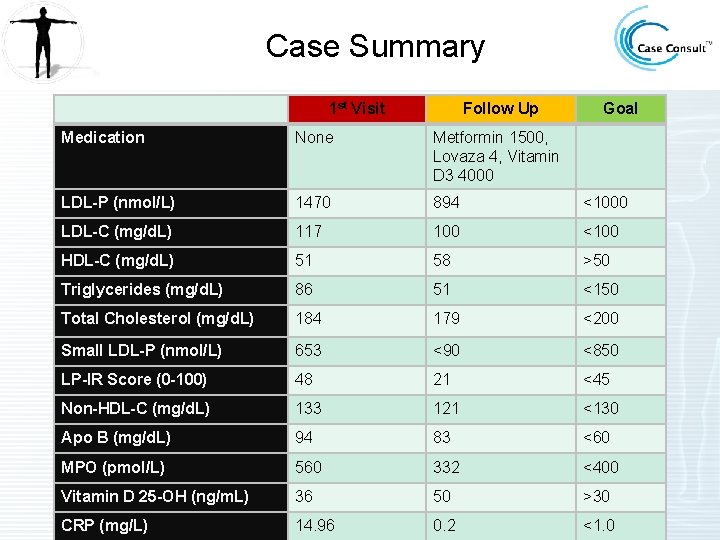
Case Summary 1 st Visit Follow Up Goal Medication None Metformin 1500, Lovaza 4, Vitamin D 3 4000 LDL-P (nmol/L) 1470 894 <1000 LDL-C (mg/d. L) 117 100 <100 HDL-C (mg/d. L) 51 58 >50 Triglycerides (mg/d. L) 86 51 <150 Total Cholesterol (mg/d. L) 184 179 <200 Small LDL-P (nmol/L) 653 <90 <850 LP-IR Score (0 -100) 48 21 <45 Non-HDL-C (mg/d. L) 133 121 <130 Apo B (mg/d. L) 94 83 <60 MPO (pmol/L) 560 332 <400 Vitamin D 25 -OH (ng/m. L) 36 50 >30 CRP (mg/L) 14. 96 0. 2 <1. 0
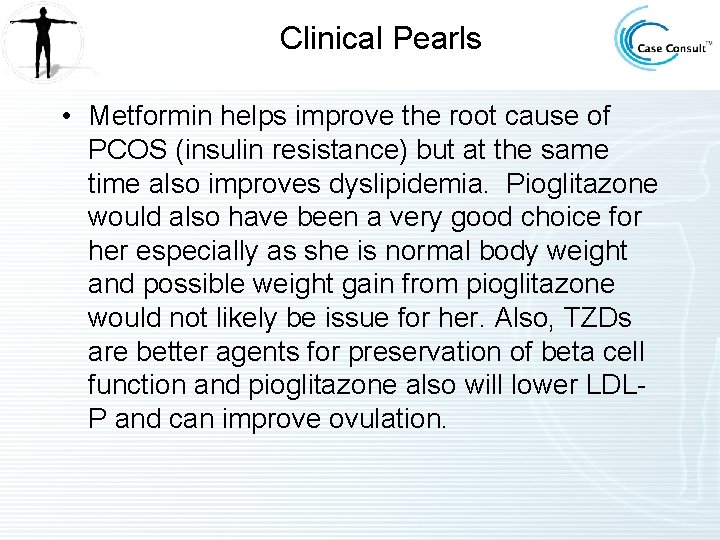
Clinical Pearls • Metformin helps improve the root cause of PCOS (insulin resistance) but at the same time also improves dyslipidemia. Pioglitazone would also have been a very good choice for her especially as she is normal body weight and possible weight gain from pioglitazone would not likely be issue for her. Also, TZDs are better agents for preservation of beta cell function and pioglitazone also will lower LDLP and can improve ovulation.
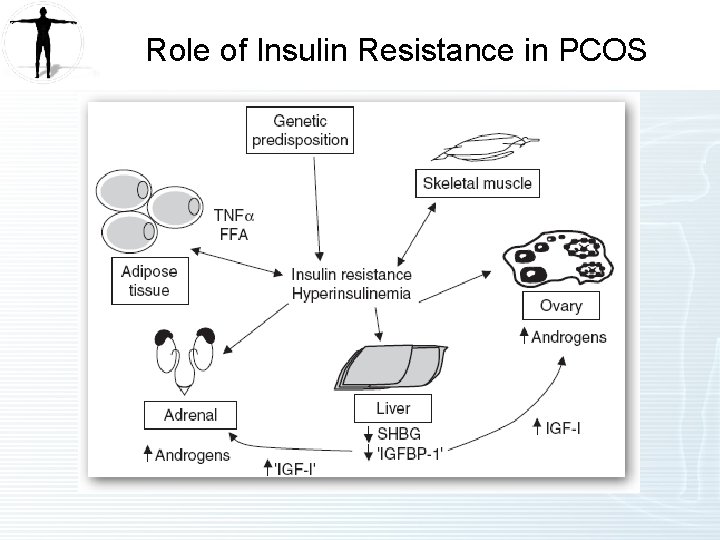
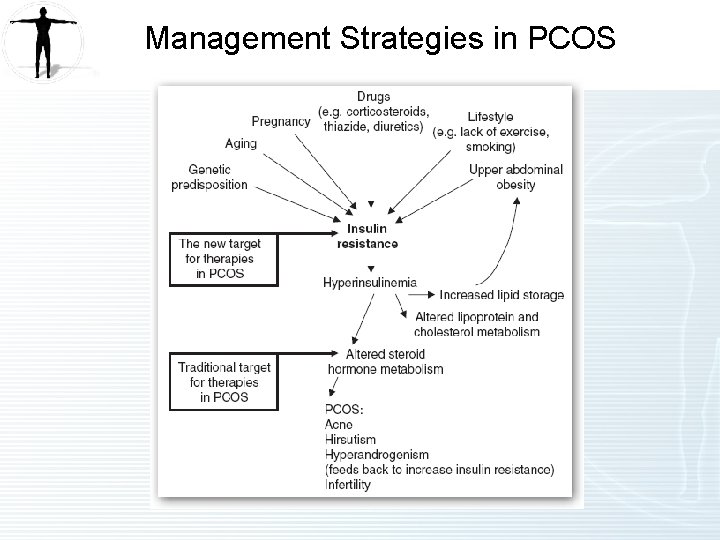
Role of Insulin Resistance in PCOS
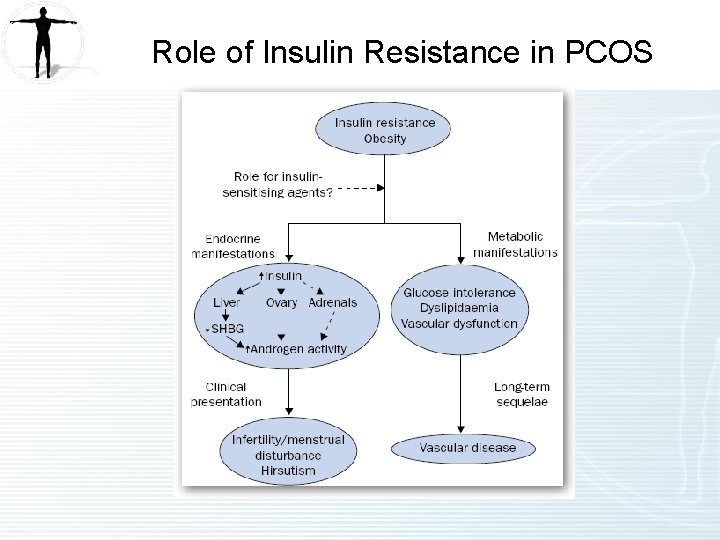
Role of Insulin Resistance in PCOS
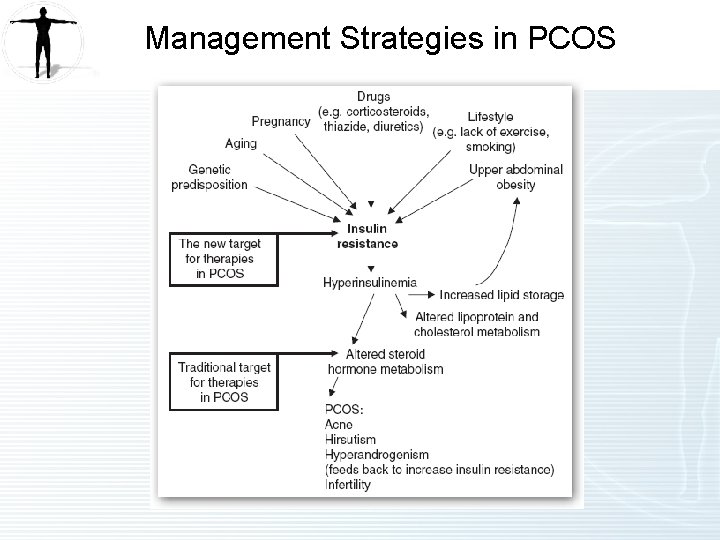
Management Strategies in PCOS
References (1 of 3) Insulin Resistance Syndrome • • ADA Standards of Medical Care in Diabetes - 2012. Diabetes Care. Jan 2012 35(1)11 -63. Orchard TJ, Temprosa M, Goldberg R, et al. The effect of metformin and intensive lifestyle intervention on the metabolic syndrome: the Diabetes Prevention Program randomized trial. Ann Intern Med. 2005 Apr 19; 142(8): 611 -9. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002 Feb 7; 346(6): 393 -403. Nathan DM, Davidson M, De. Fronzo RA, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. A consensus statement from the American Diabetes Association. Diabetes Care. 2007; 30: 753 -759. Dyslipidemia • • El Harchaoui K, van der Steeg WA, Stroes ES, et al. Value of low-density lipoprotein particle number and size as predictors of coronary artery disease in apparently healthy men and women: the EPIC-Norfolk Prospective Population Study. J Am Coll Cardiol. 2007 Feb 6; 49(5): 547 -53. Mora S, Szklo M, Otvos JD, et al. LDL particle subclasses, LDL particle size, and carotid atherosclerosis in the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis. 2007 May; 192(1): 211 -7. Festa A, Williams K, Hanley AJ, et al. Nuclear magnetic resonance lipoprotein abnormalities in prediabetic subjects in the Insulin Resistance Atherosclerosis Study. Circulation. 2005 Jun 28; 111(25): 3465 -72. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Lancet. 1999 Aug 7; 354(9177): 447 -55.
References (2 of 3) Elevated CRP • • National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002 Dec 17; 106(25): 3143 -421. Ridker PM, Hennekens CH, Buring JE, et al. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000 Mar 23; 342(12): 836 -43. Vitamin D Deficiency • • Dobnig H, Pilz S, Scharnagl H, et al. Independent association of low serum 25 hydroxyvitamin d and 1, 25 -dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med. 2008; 168(12): 1340 -1349. Giovannucci E, Liu Y, Hollis B, Rimm E. 25 -hydroxyvitamin d and risk of myocardial infarction in men. Arch Intern Med. 2008; 168(11): 1174 -1180. Michos E and Blumenthal R. Vitamin D Supplementation and Cardiovascular Disease Risk. Circulation. 2007; 115(7): 827 -828. Hathcock J, Shao A, Vieth R, et al. Risk assessment for vitamin D. Am J Clin Nutr. 2007; 85: 6 -18. Holick M. Vitamin D Deficiency. N Engl J Med. 2007; 357: 266 -81.
References (3 of 3) PCOS • • Harborne L, Fleming R, Lyall H, et al. Descriptive review of the evidence for the use of metformin in polycystic ovary syndrome. Lancet. 2003 May 31; 361(9372): 1849 -901. Brettenthaler N, De Geyter C, Huber PR, et al. Effect of the insulin sensitizer pioglitazone on insulin resistance, hyperandrogenism, and ovulatory dysfunction in women with polycystic ovary syndrome. J Clin Endrocrinol Metab. 2004 Aug; 89(8): 3835 -40.
 Infantile polycystic kidney
Infantile polycystic kidney Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease A 26 year old female presents
A 26 year old female presents Karyotype gizmo
Karyotype gizmo Fragile x syndrome female
Fragile x syndrome female Fuctions of ovary
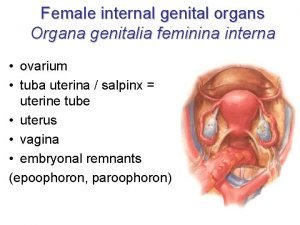
Fuctions of ovary Female reproductive system
Female reproductive system Ca 125
Ca 125 Ovarian cyst about to rupture
Ovarian cyst about to rupture Structure of female
Structure of female Lymph drainage of uterus
Lymph drainage of uterus Ovarian cancer causes
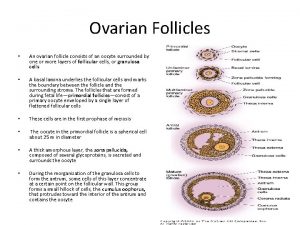
Ovarian cancer causes Ovarian follicle
Ovarian follicle Ovarian cyst
Ovarian cyst Ovarian cycle
Ovarian cycle Ovarian teratoma
Ovarian teratoma Lutalphase
Lutalphase Ovarian cancer brca
Ovarian cancer brca Hrd score ovarian cancer
Hrd score ovarian cancer Ovarian cycle
Ovarian cycle Ovarian ligament
Ovarian ligament Ovarian benign tumor
Ovarian benign tumor Sru consensus ovarian cysts
Sru consensus ovarian cysts Ovarian cycle
Ovarian cycle The ovarian cycle
The ovarian cycle Ovarian ligament.
Ovarian ligament. Ovarian follicle
Ovarian follicle Ovarian ligament
Ovarian ligament Primary oocyte
Primary oocyte Complex ovarian cyst size chart
Complex ovarian cyst size chart Leaving school poems from teachers
Leaving school poems from teachers Healthy heart rate for women
Healthy heart rate for women What were daisy's assets as an eighteen year old
What were daisy's assets as an eighteen year old 42 year old woman
42 year old woman Plep b examples
Plep b examples Average height of a 3 year old in centimeters
Average height of a 3 year old in centimeters 9-year-old physical development
9-year-old physical development