HRT and Menopause Urinary incontinence Polycystic ovarian syndrome


![NICE GUIDANCE • Altered sexual function • 1. 4. 8 Consider testosterone[1] supplementation for NICE GUIDANCE • Altered sexual function • 1. 4. 8 Consider testosterone[1] supplementation for](https://slidetodoc.com/presentation_image_h/c0bafdbf8fbd1e2305cefff6ad400bcf/image-6.jpg)




- Slides: 26

HRT and Menopause Urinary incontinence Polycystic ovarian syndrome Miss Sujata Gupta (Risk lead and Endometriosis specialist) Consultant Gynaecologist Stepping Hill Hospital, Stockport

Life expectancy • Life expectancy at older ages is the highest it’s ever been • From: Public Health England First published: 12 February 2016 • men can now expect to live for a further 19 years at age 65, 12 years at 75, 6 years at 85 and 3 years at 95 • women can expect to live for a further 21 years at age 65, 13 years at 75, 7 years at 85, and 3 years at 95
Menopause • Definition • Perimenopause • Diagnosis‐ Women less than 45 vs women over 45‐ Serum FSH test only in under 45 s but useful in women on hormonal treatments.
Effects of menopause • vasomotor symptoms (for example, hot flushes and sweats) • musculoskeletal symptoms (for example, joint and muscle pain) • effects on mood (for example, low mood) • urogenital symptoms (for example, vaginal dryness) • sexual difficulties (for example, low sexual desire
Cure • • • Acceptance Life‐style Herbal remedies Non hormonal remedies HRT Contraception
![NICE GUIDANCE Altered sexual function 1 4 8 Consider testosterone1 supplementation for NICE GUIDANCE • Altered sexual function • 1. 4. 8 Consider testosterone[1] supplementation for](https://slidetodoc.com/presentation_image_h/c0bafdbf8fbd1e2305cefff6ad400bcf/image-6.jpg)
NICE GUIDANCE • Altered sexual function • 1. 4. 8 Consider testosterone[1] supplementation for menopausal women with low sexual desire if HRT alone is not effective • Urogenital atrophy • 1. 4. 9 Offer vaginal oestrogen to women with urogenital atrophy (including those on systemic HRT) and continue treatment for as long as needed to relieve symptoms
NICE GUIDANCE the BNF states ". . continuous combined preparations or tibolone are not suitable for use in the perimenopause or within 12 months of the last menstrual period, women who use such preparations may bleed irregularly in the early stages of treatment ‐ if bleeding continues endometrial abnormality should be ruled out and consideration given to changing to cyclical HRT. . “ • vaginal bleeding whilst on cc. HRT • Less than 6/12‐ reduce estrogen, increase/ change progesterone‐abnormal bleeding starts when using continuous combined HRT, in women >54 or > 1 year after their last period, within 6 months of starting treatment then initially a trial of oestrogen reduction should be attempted. If bleeding recurs then refer for routine hysteroscopy as benign pathology would be anticipated • More than 6/12‐ Hysteroscopy
NICE GUIDANCE • 1. 5. 2 Consider transdermal rather than oral HRT for menopausal women who are at increased risk of VTE, including those with a BMI over 30 kg/m 2. • 1. 5. 3 Consider referring menopausal women at high risk of VTE (for example, those with a strong family history of VTE or a hereditary thrombophilia) to a haematologist for assessment before considering HRT.
Review • 3 months then annual • Check for side‐effects ‐ eg, breast tenderness or enlargement, nausea, headaches or bleeding ‐ and manage appropriately (see 'Management of side‐effects', below). • Check blood pressure and weight. • Encourage breast awareness and participation in screening mammography and also cervical screening if appropriate for age. • A review and discussion of an individual's risk: benefit ratio concerning HRT should occur at least annually. • If appropriate, consider switching from cyclical HRT to continuous combined HRT (see below).
Urinary incontinence
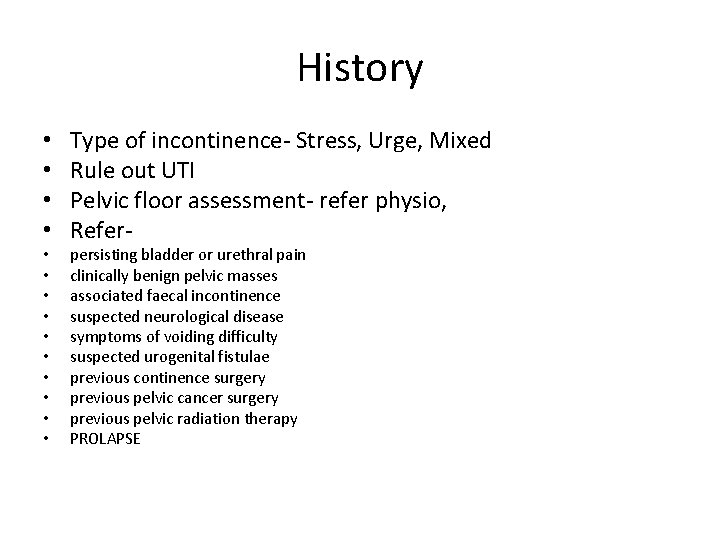
History • • • • Type of incontinence‐ Stress, Urge, Mixed Rule out UTI Pelvic floor assessment‐ refer physio, Refer‐ persisting bladder or urethral pain clinically benign pelvic masses associated faecal incontinence suspected neurological disease symptoms of voiding difficulty suspected urogenital fistulae previous continence surgery previous pelvic cancer surgery previous pelvic radiation therapy PROLAPSE

Management Bladder diary Physio Urodynamic testing Not needed for conservative management or pure SUI symptoms of OAB leading to a clinical suspicion of detrusor overactivity, • symptoms suggestive of voiding dysfunction or anterior compartment prolapse • had previous surgery for stress incontinence • • •
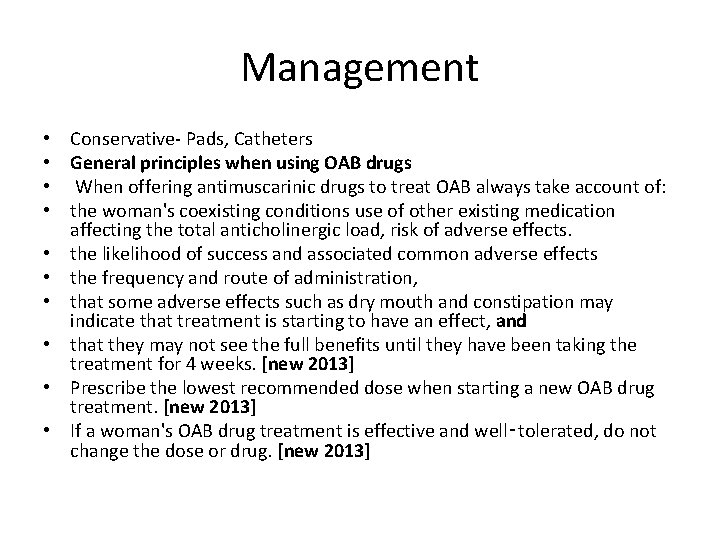
Management • • • Conservative‐ Pads, Catheters General principles when using OAB drugs When offering antimuscarinic drugs to treat OAB always take account of: the woman's coexisting conditions use of other existing medication affecting the total anticholinergic load, risk of adverse effects. the likelihood of success and associated common adverse effects the frequency and route of administration, that some adverse effects such as dry mouth and constipation may indicate that treatment is starting to have an effect, and that they may not see the full benefits until they have been taking the treatment for 4 weeks. [new 2013] Prescribe the lowest recommended dose when starting a new OAB drug treatment. [new 2013] If a woman's OAB drug treatment is effective and well‑tolerated, do not change the dose or drug. [new 2013]
Choosing OAB drugs • • • Do not use flavoxate, propantheline and imipramine for the treatment of UI or OAB in women. [2006] Do not offer oxybutynin (immediate release) to frail older women[7]. [new 2013] Offer one of the following choices first to women with OAB or mixed UI: oxybutynin (immediate release), or tolterodine (immediate release), or darifenacin (once daily preparation). [new 2013] If the first treatment for OAB or mixed UI is not effective or well‑tolerated, offer another drug with the lowest acquisition cost[8]. Offer a transdermal OAB drug to women unable to tolerate oral medication. [new 2013] For guidance on mirabegron for treating symptoms of overactive bladder, refer to mirabegron for treating symptoms of overactive bladder (NICE technology appraisal guidance 290). [new 2013] 1. 1 Mirabegron is recommended as an option for treating the symptoms of overactive bladder only for people in whom antimuscarinic drugs are contraindicated or clinically ineffective, or have unacceptable side effects. 1. 2 People currently receiving mirabegron that is not recommended for them in 1. 1 should be able to continue treatment until they and their clinician consider it appropriate to stop.

Review • 4 wks – face to face or telephone • 6 monthly in over 75 s • Annual in under 75 s
Referral to MDT • Invasive treatment for SUI or OAB ( Botox, sacral nerve stimulation, augmented cystoplasty, urinary diversion) • SUI‐ Synthetic tapes, autologous tapes, colposuspension), intramural bulking agents • Surgeons undertaking continence surgery should maintain careful audit data and submit their outcomes to national registries such as those held by the British Society of Urogynaecology (BSUG) and British Association of Urological Surgeons Section of Female and Reconstructive Urology (BAUS‑SFRU). [2006]
PCOS
PCOS • Incidence‐ 26% • The symptoms of polycystic ovary syndrome (PCOS) include menstrual cycle disturbance and features of hyperandrogenism (hirsutism, acne and alopecia), with associated fertility problems, obesity and psychological issues. • Obesity has a major impact on the expression of PCOS • The management of anovulatory infertility involves lifestyle modification and therapies to induce ovulation, namely clomifene citrate, gonadotrophin therapy and laparoscopic ovarian diathermy. • management of menstrual problems requires prevention of endometrial hyperplasia and adenocarcinoma.
Symptoms • • • Hyperandrogenism (hirsutism, acne, alopecia) Menstrual disturbance Infertility Obesity Possible late sequelae Type II diabetes mellitus Dyslipidaemia Hypertension Cardiovascular disease Endometrial carcinoma
Diagnosis( ESHRE 2003) Rotterdam criteria‐ two out of three criteria • • clinical or biochemical features of hyperandrogenism, ( A total testosterone level of greater than 5 nmol/l (depending upon the assay) or rapid onset of signs of hyperandrogenism requires further investigation. Non‐classic (late onset) congenital adrenal hyperplasia (CAH) is not common in the UK but is more prevalent in certain ethnic groups (e. g. Mediterranean, South American and some Jewish populations). oligo‐ovulation or anovulation (i. e. menstrual cycle disturbance) and/or polycystic ovaries on ultrasound, once appropriate investigations have been performed to exclude other causes of menstrual disturbance androgen excess Exclude‐ hyperprolactinemia, acromegaly, congenital adrenal hyperplasia, Cushing's syndrome androgen‐secreting tumours of the ovary or adrenal gland), which could predispose to similar ultrasound and biochemical features and also the exclusion of other causes of menstrual cycle irregularity secondary to hypothalamic, pituitary or ovarian dysfunction.
Treatment • Symptomatic‐ life style • Hirsutism‐ • • Dianette® (Bayer PLC, Newbury, Berkshire, UK), which contains ethinyloestradiol (35 μg) in combination with cyproterone acetate (2 mg). The addition of higher doses of cyproterone acetate (50– 100 mg) does not appear to confer additional benefit. The effect on acne and seborrhoea is usually evident within a couple of months. Sometimes additional topical antibiotic and anti‐inflammatory preparations may be helpful. Spironolactone is a weak diuretic with antiandrogenic properties that may be used in women in whom the combined oral contraceptive pill is contraindicated at a daily dose of 25– 100 mg. Drosperinone is a derivative of spironolactone and is contained in the combined oral contraceptive pill Yasmin® (Bayer PLC, Newbury, Berkshire, UK), which may also be beneficial for women with PCOS The management of alopecia is difficult but may be stabilised by the anti‐androgen preparations mentioned above. Iron deficiency may have an impact on hair loss and so ferritin levels should be assessed.
Menstrual irregularity • women with PCOS shed their endometrium at least every 3 months. • For those women with oligo/amenorrhea who do not wish to use cyclical hormone therapy, we recommend an ultrasound scan to measure endometrial thickness and morphology every 6– 12 months (depending on menstrual history). • An endometrial thickness greater than 10 mm in an amenorrheic woman warrants an artificially induced bleed, which should be followed by a repeat ultrasound scan and endometrial biopsy if the endometrium has not been shed. • Another option is to consider a progestogen‐secreting intrauterine system, such as the Mirena® (Bayer PLC, Newbury, Berkshire, UK).


 Hrt to hrt merrylands
Hrt to hrt merrylands Infantile polycystic kidney
Infantile polycystic kidney Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Coital incontinence
Coital incontinence Acfi behaviour
Acfi behaviour Acupuncture for incontinence
Acupuncture for incontinence Bulbocavernosus reflex
Bulbocavernosus reflex Dr wilson adrenal rebuilder side effects
Dr wilson adrenal rebuilder side effects Symplex f for menopause
Symplex f for menopause Menopause definition
Menopause definition Vaginal atrophy
Vaginal atrophy Premature menopause quiz
Premature menopause quiz Menopause wann
Menopause wann Menopause defination
Menopause defination Hrt gp notebook
Hrt gp notebook Hrt
Hrt Trans
Trans Edh cern
Edh cern Hrt wetter
Hrt wetter Hrt
Hrt Hrt
Hrt Vaginal seeding
Vaginal seeding Dr sharan pobbathi
Dr sharan pobbathi Ftm hrt
Ftm hrt Functions ovary
Functions ovary Accessory structures of female reproductive system
Accessory structures of female reproductive system Ovarian cancer marker
Ovarian cancer marker