HUMAN REPRODUCTION Anjali Chamail REPRODUCTIVE EVENTS Humans sexual


- Slides: 71
HUMAN REPRODUCTION Anjali Chamail
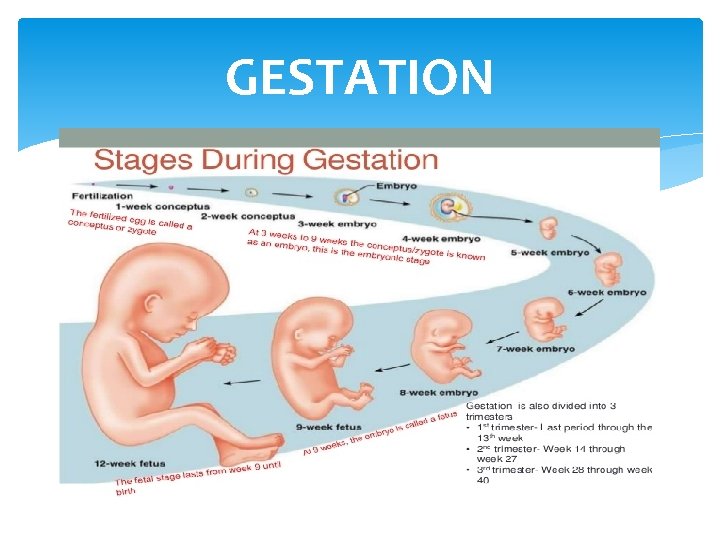
REPRODUCTIVE EVENTS Humans- sexual reproduction, viviparous, unisexual. Each sex has pair of gonads, reproductive duct and accessory structures. Sex organs- Testis (paired) male, ovaries (paired), gamete formation, hormones. Puberty 1. Gametogenesis- formation of gametes (sperms/ova) 2. Insemination- transfer of sperms into the female genital tract. 3. Fertilisation- fusion of male and female gametes leading to formation of zygote. 4. Implantation- development of blastocyst and its attachment to the uterine wall. 5. Gestation- embryonic development (from conception to birth). 6. Parturition- delivery of the baby (child birth).
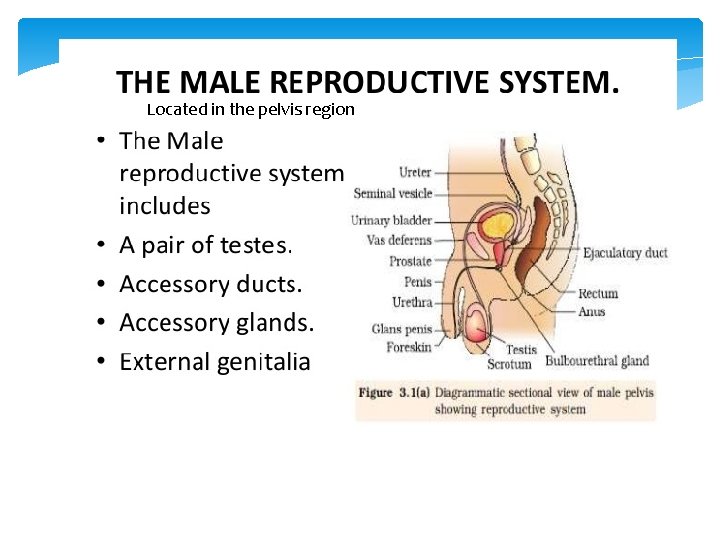
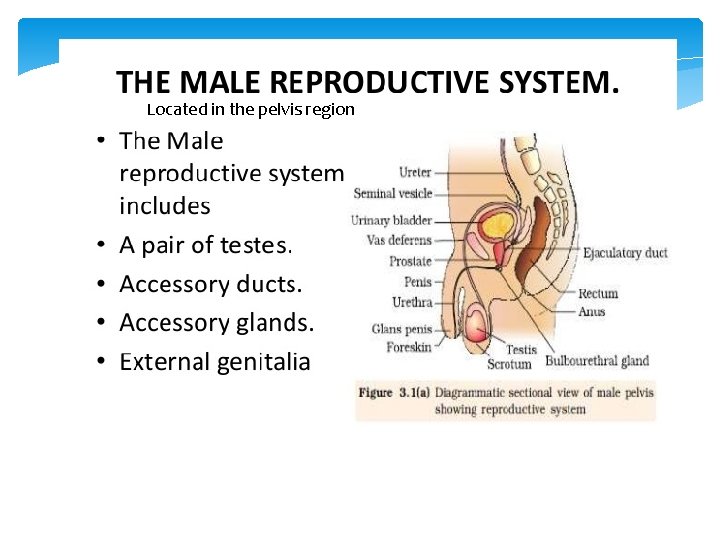
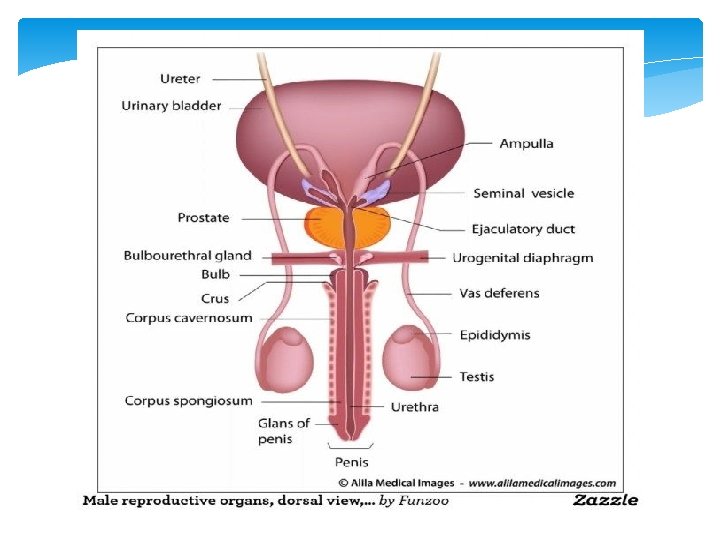
Located in the pelvis region
TESTES Paired male gonads- sperm, hormones. Oval in shape, length 4 -5 cm, a width 2 -3 cm. Situated outside the abdominal cavity within a pouch called scrotum. Scrotum- low temperature of the testes (2 -2. 5°C lower than the normal internal body temperature) necessary for spermatogenesis. Testes is covered by a dense fibrous membrane- tunica albuginea. Each testes is divided into 250 compartments called testicular lobules. Each lobule- 1 to 3 highly coiled seminiferous tubule.
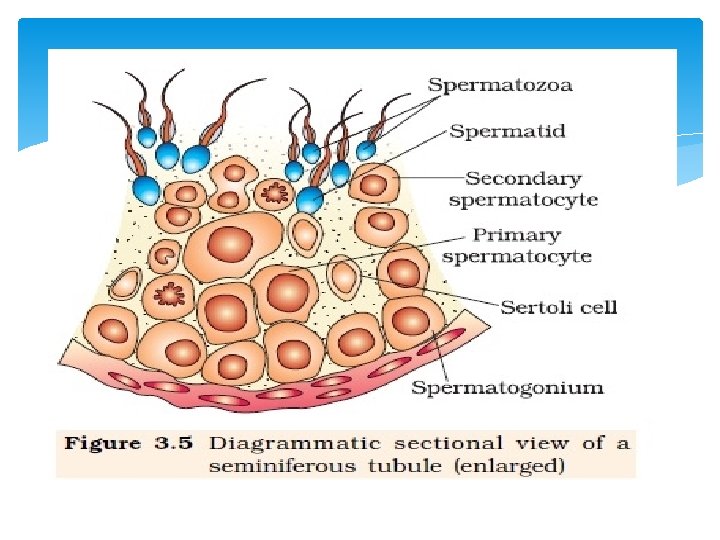
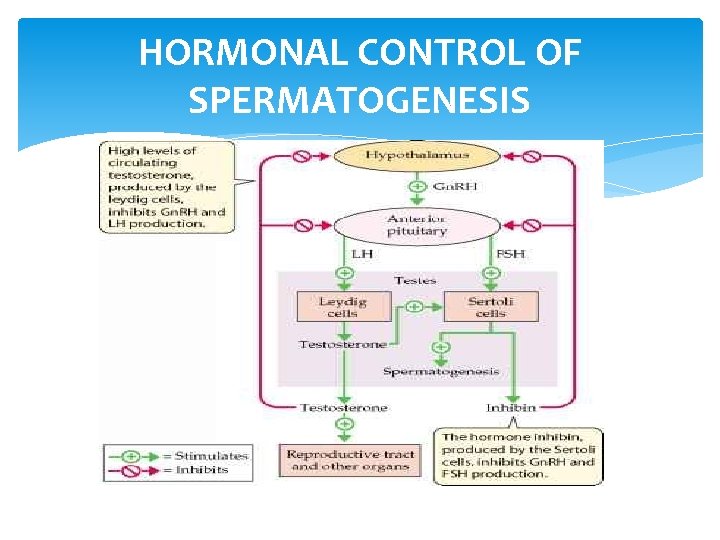
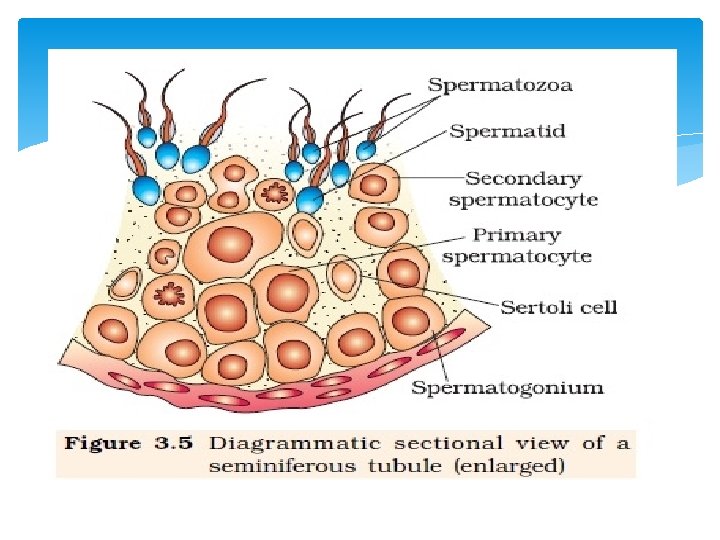
SEMINIFEROUS TUBULE- SPERM PRODUCTION It is lined on its inside by two types of cells a) Male germ cells- (spermatogonia)- meiotic divisions - sperm formation. b) Sertoli cells- provide nutrition to the germ cells, secrete androgen binding protein (concentrates testosterone) and inhibin (suppresses FSH synthesis). Regions outside the seminiferous tubules called interstitial spaces, contain small blood vessels and interstitial cells/ Leydigs cells. Leydig cells- synthesise and secrete male hormone Androgen (testosterone).
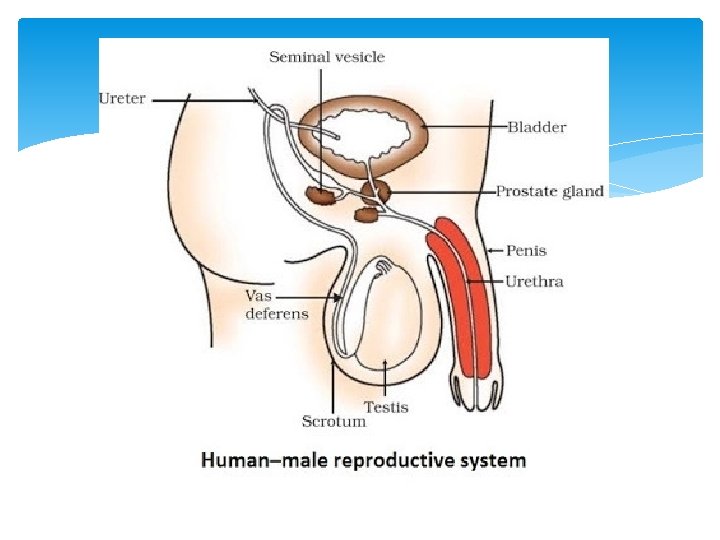
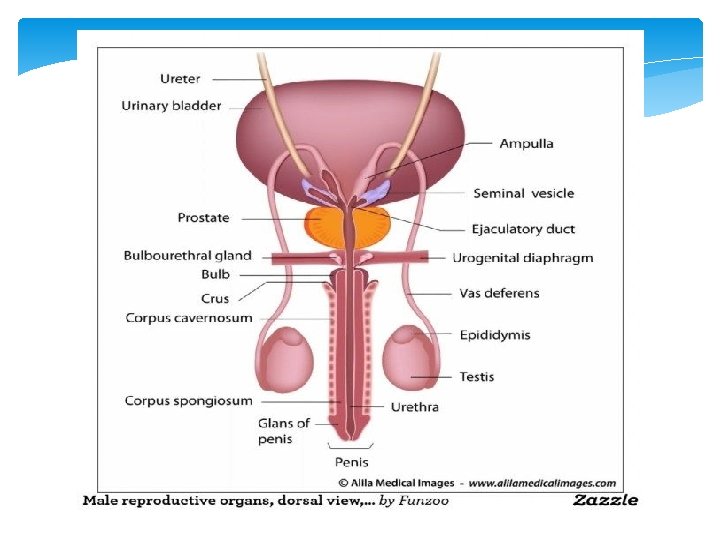
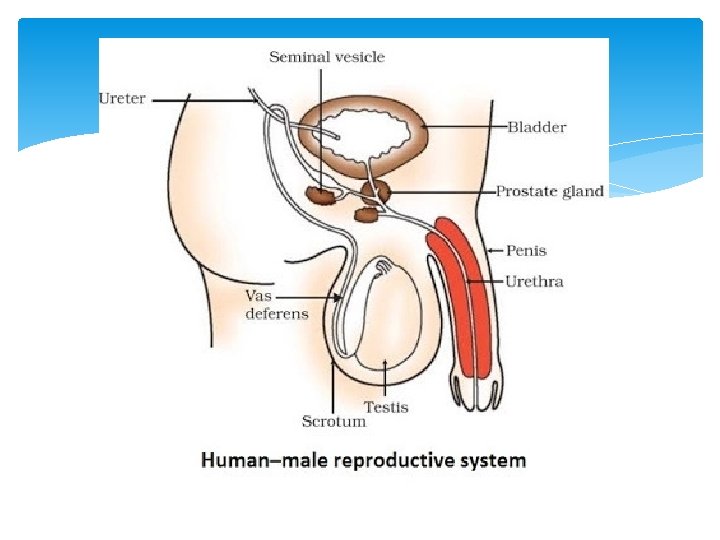
ACCESSORY DUCTS Rete testis, vasa efferentia, epididymis and Vas deferens. i) Seminiferous tubule opens into ii) Vasa efferentia through rete testis iii) Epididymis (posterior surface of testis) iv) Vas deferens- ascend to abdomen and loop over urinary bladder v) Vas deferens receives duct- seminal vesicle vi) Opens into urethra as Ejaculatory duct. Function- Stores and transports sperm from testis to urethra. Urethra- originates from urinary bladder extends through penis to external opening- urethral meatus.
EXTERNAL GENITALIA- PENIS External copulatory organ- external genitalia Made of special tissue- erection to facilitate insemination. Enlarged distal end glans penis covered by loose skin called fore skin ACCESSORY GLANDS 1. Seminal vesicles (paired) 2. A Prostate gland 3. Bulbourethral glands (paired) Seminal plasma- secretion of all the accessory glands. Rich in fructose, calcium and certain enzymes. Helps in lubrication
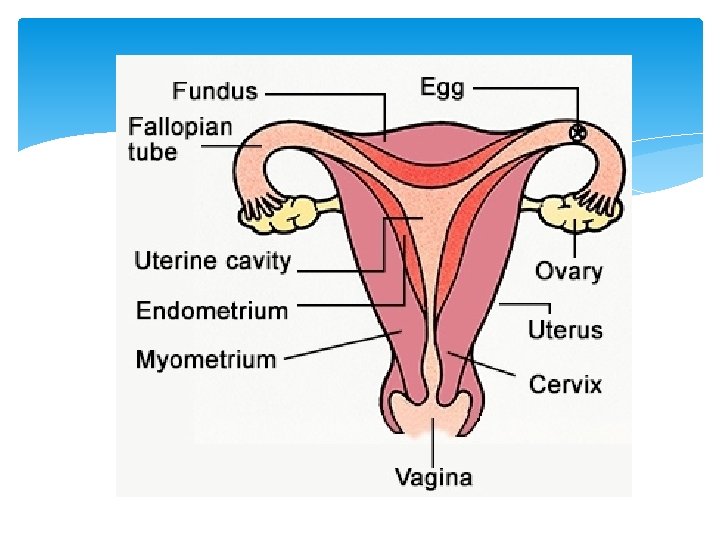
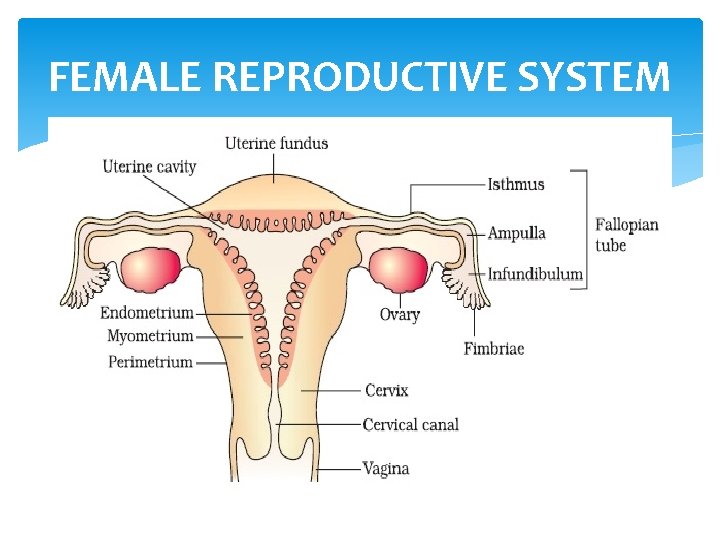
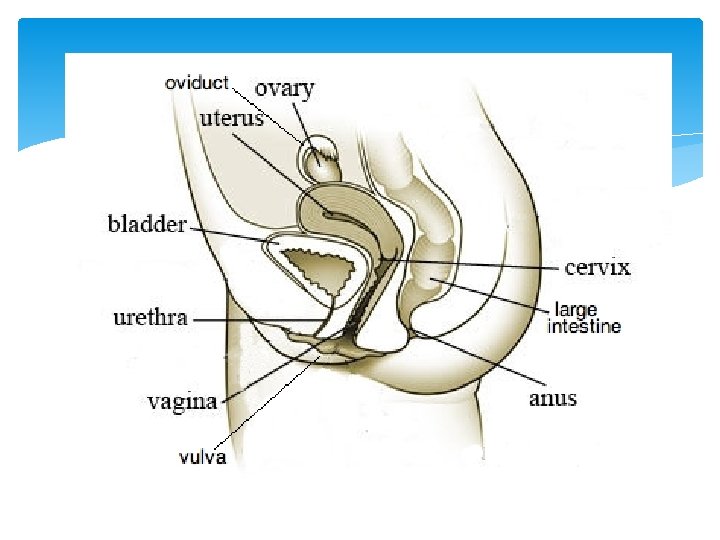
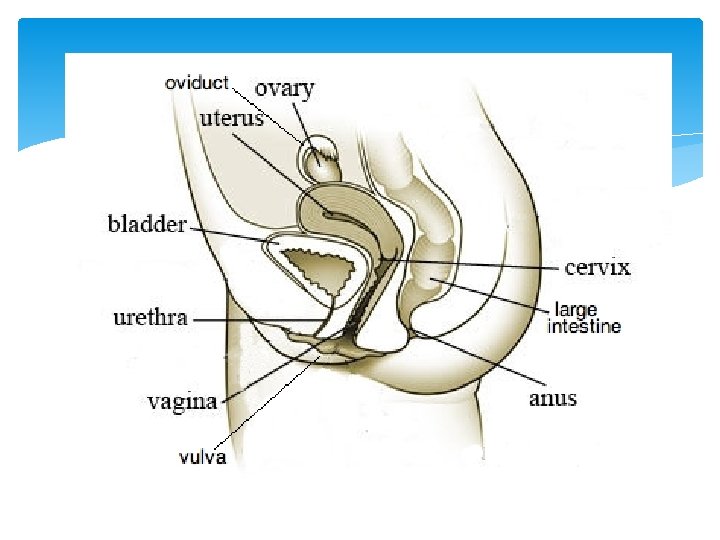
FEMALE REPRODUCTIVE SYSTEM It is made up of: i) A pair of ovaries ii) Oviducts iii) Uterus iv) Cervix v) Vagina vi) External genitalia
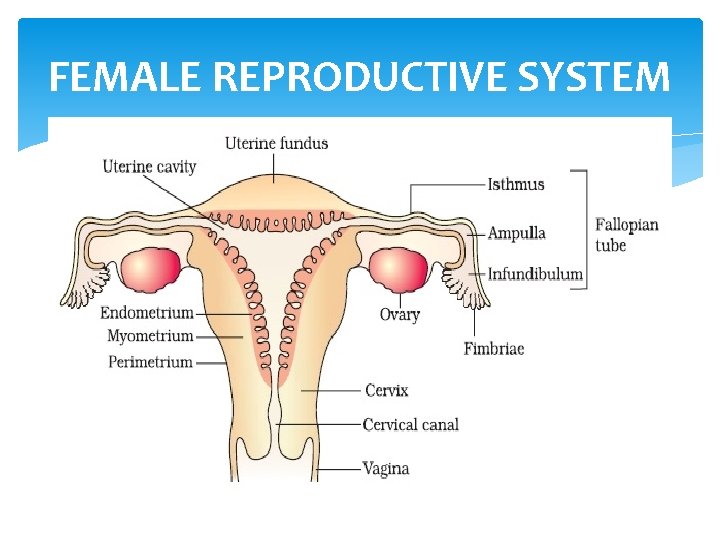
FEMALE REPRODUCTIVE SYSTEM
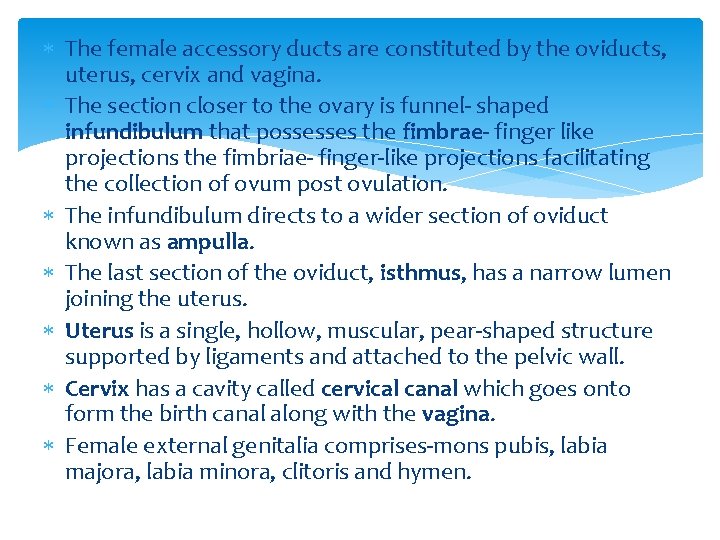
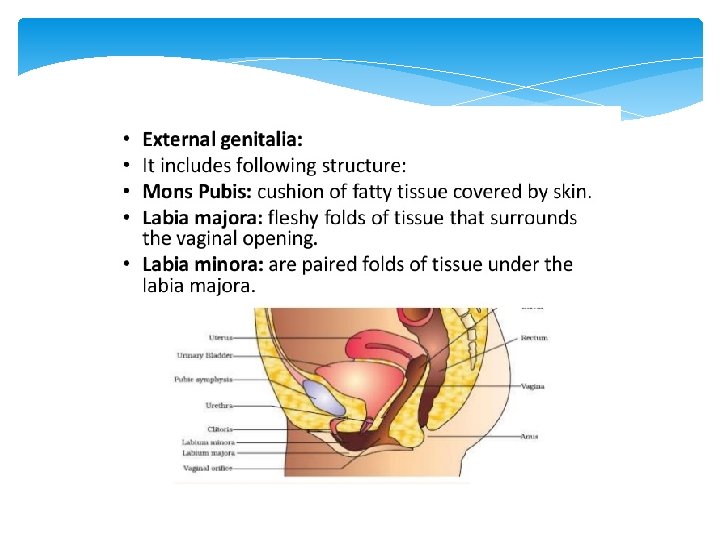
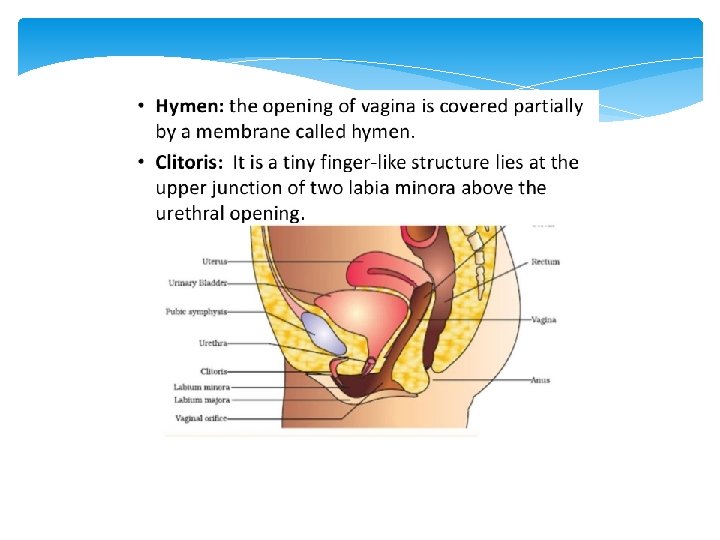
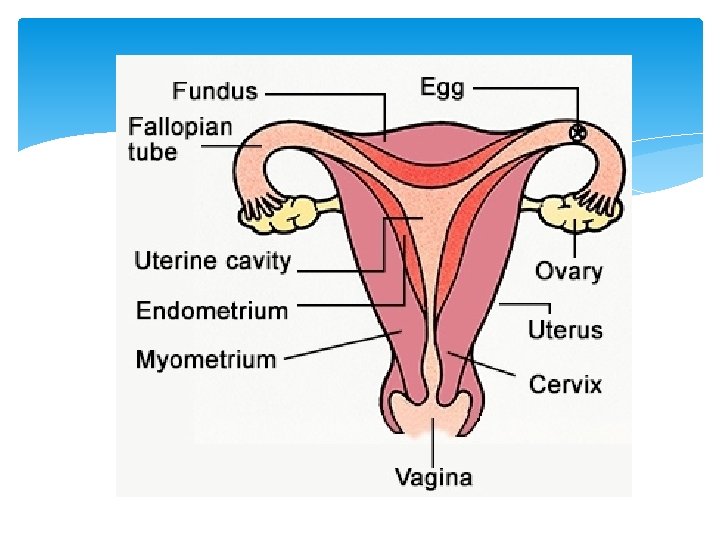
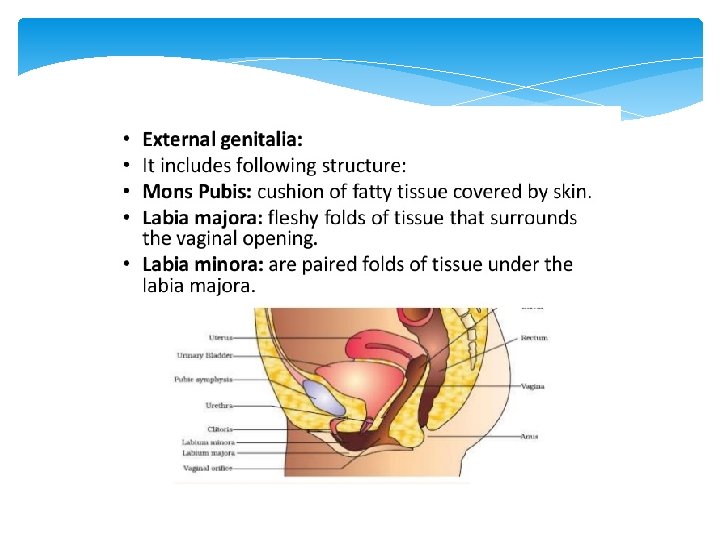
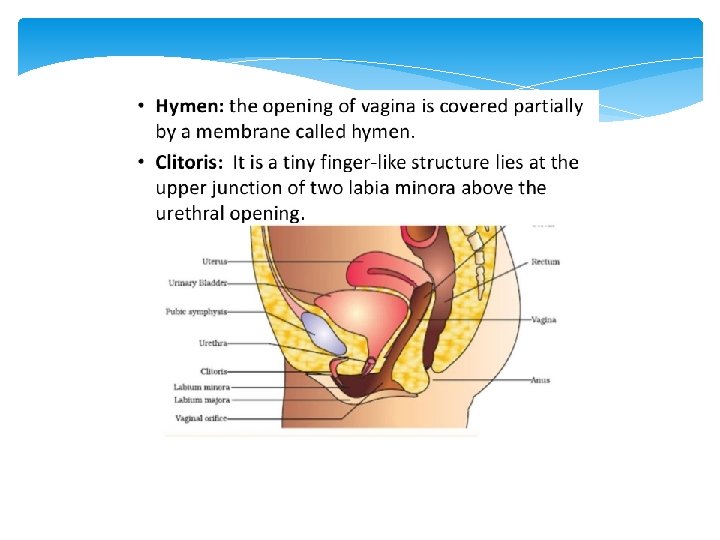
The female accessory ducts are constituted by the oviducts, uterus, cervix and vagina. The section closer to the ovary is funnel- shaped infundibulum that possesses the fimbrae- finger like projections the fimbriae- finger-like projections facilitating the collection of ovum post ovulation. The infundibulum directs to a wider section of oviduct known as ampulla. The last section of the oviduct, isthmus, has a narrow lumen joining the uterus. Uterus is a single, hollow, muscular, pear-shaped structure supported by ligaments and attached to the pelvic wall. Cervix has a cavity called cervical canal which goes onto form the birth canal along with the vagina. Female external genitalia comprises-mons pubis, labia majora, labia minora, clitoris and hymen.
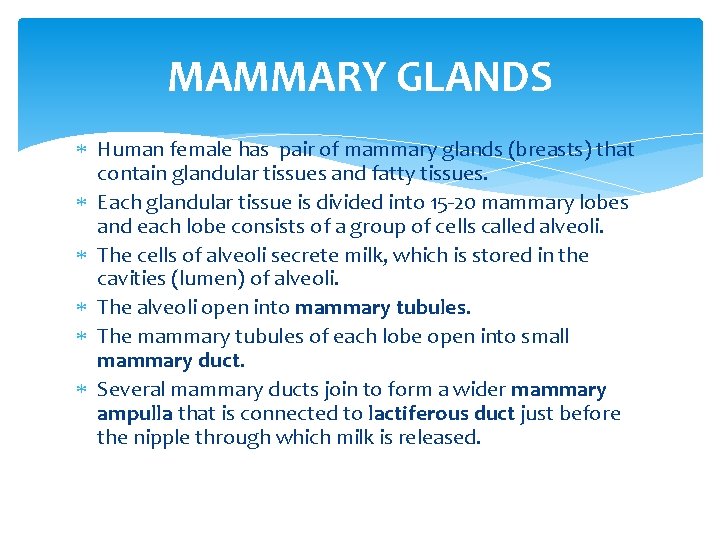
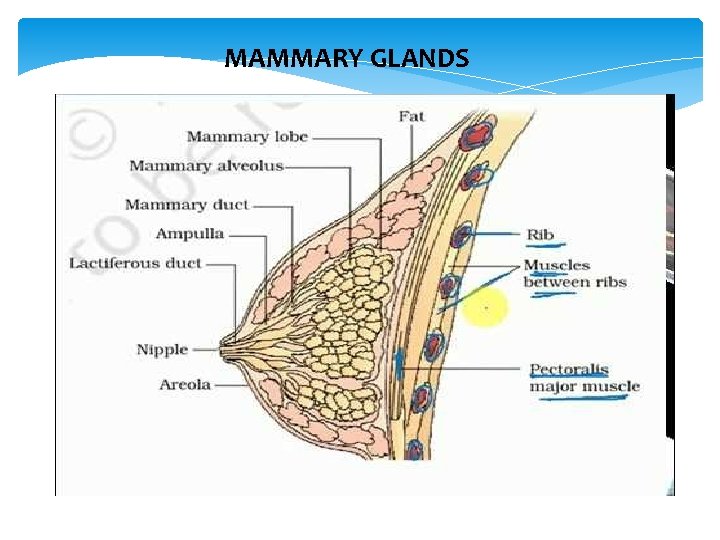
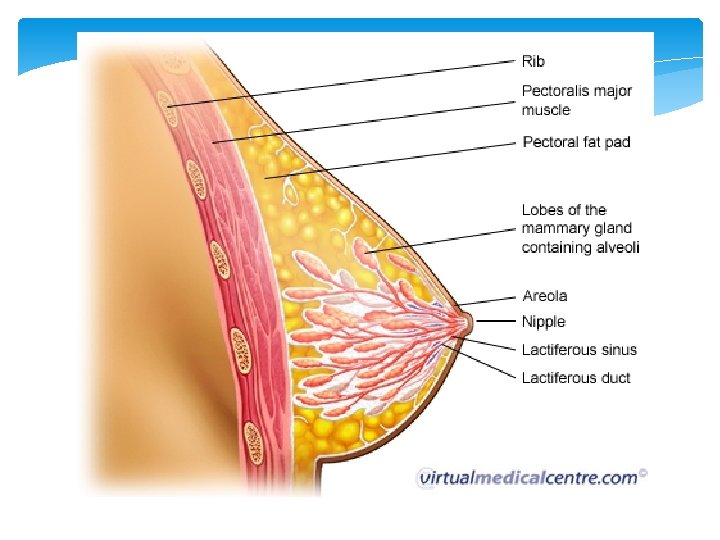
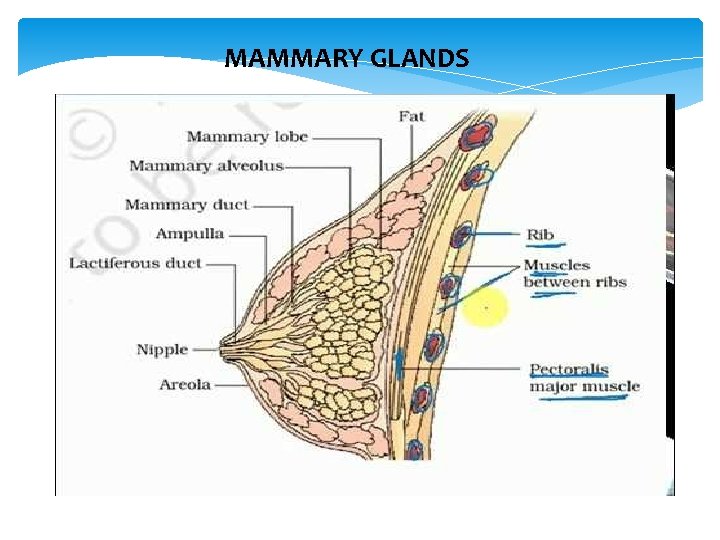
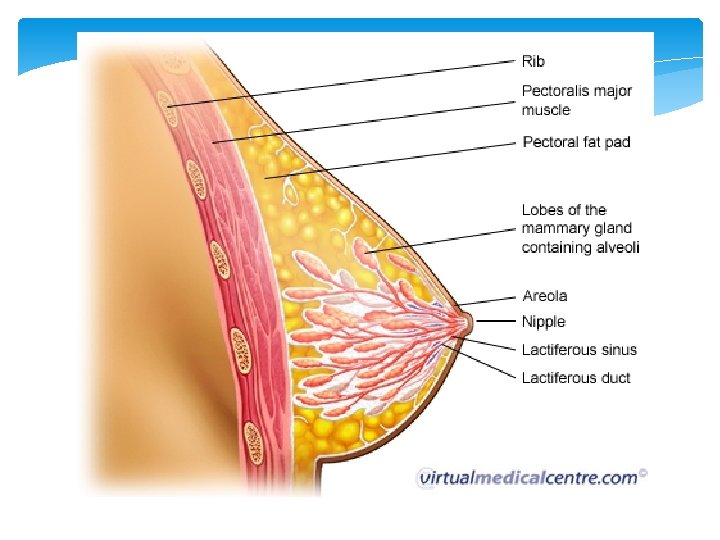
MAMMARY GLANDS Human female has pair of mammary glands (breasts) that contain glandular tissues and fatty tissues. Each glandular tissue is divided into 15 -20 mammary lobes and each lobe consists of a group of cells called alveoli. The cells of alveoli secrete milk, which is stored in the cavities (lumen) of alveoli. The alveoli open into mammary tubules. The mammary tubules of each lobe open into small mammary duct. Several mammary ducts join to form a wider mammary ampulla that is connected to lactiferous duct just before the nipple through which milk is released.
MAMMARY GLANDS
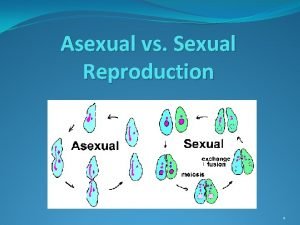
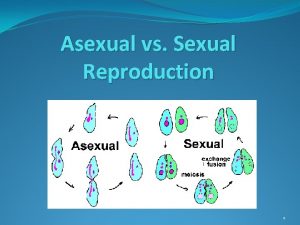
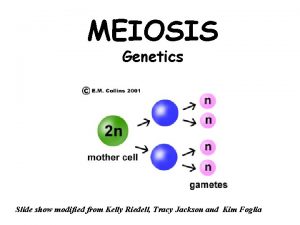
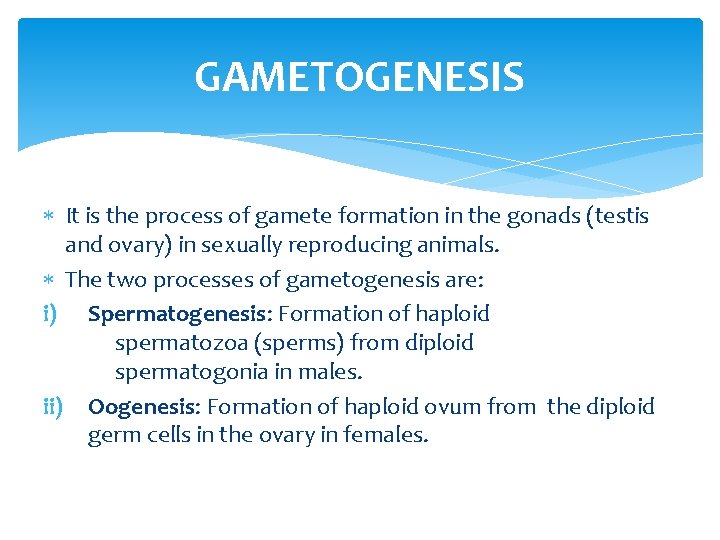
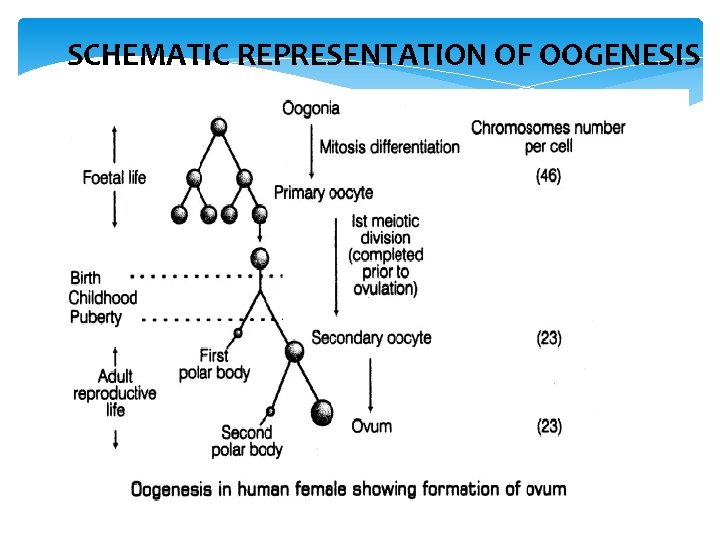
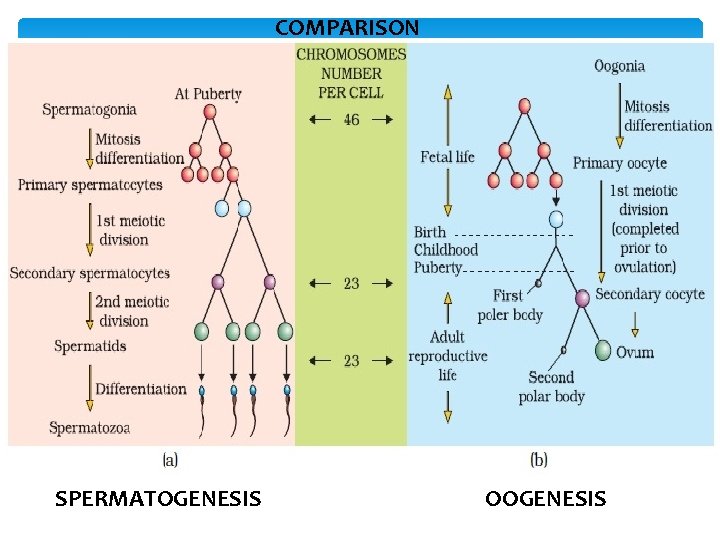
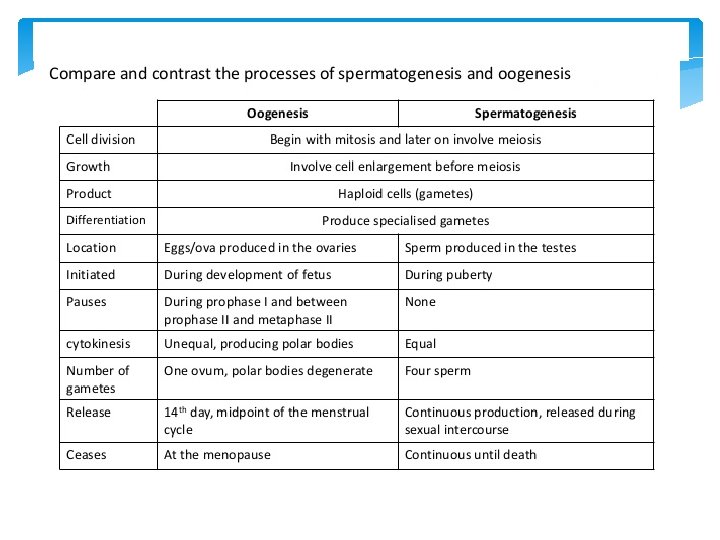
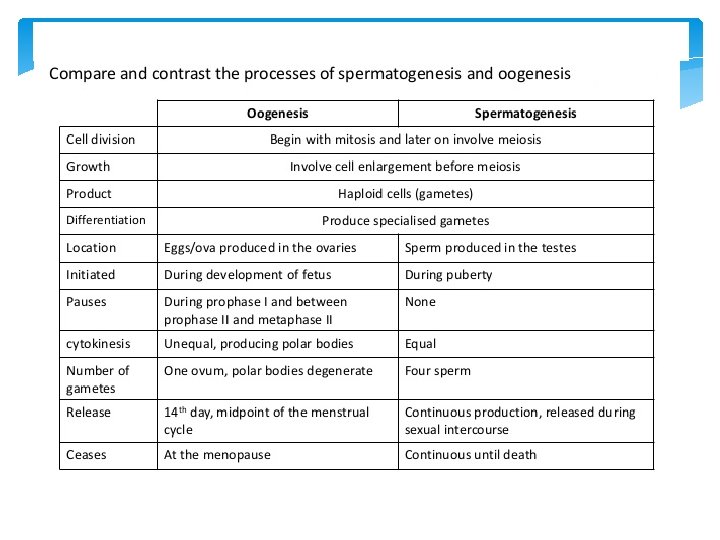
GAMETOGENESIS It is the process of gamete formation in the gonads (testis and ovary) in sexually reproducing animals. The two processes of gametogenesis are: i) Spermatogenesis: Formation of haploid spermatozoa (sperms) from diploid spermatogonia in males. ii) Oogenesis: Formation of haploid ovum from the diploid germ cells in the ovary in females.
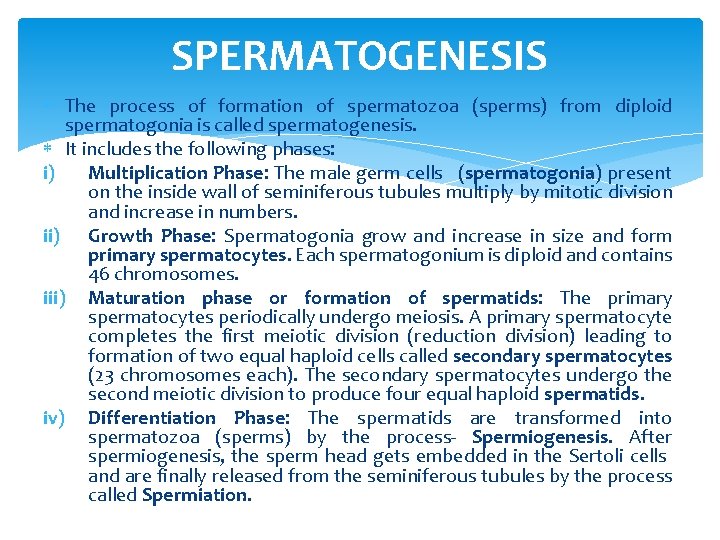
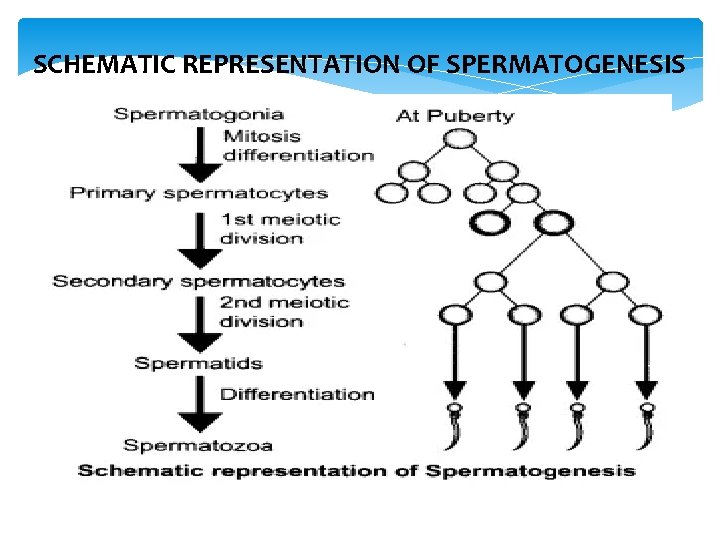
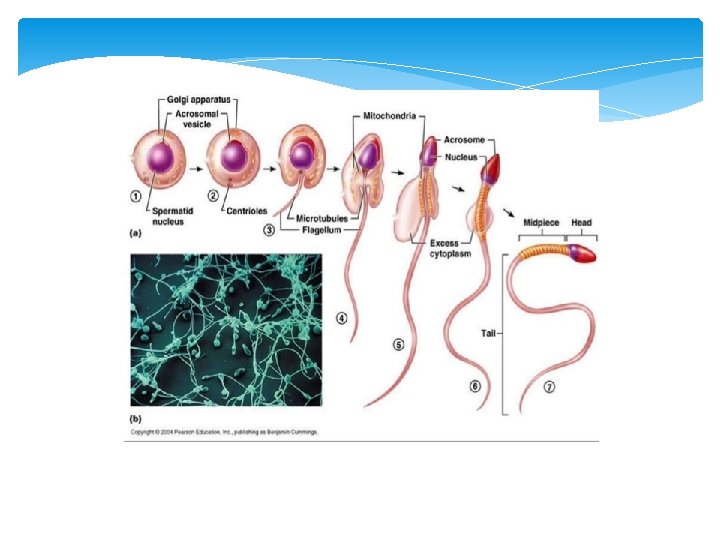
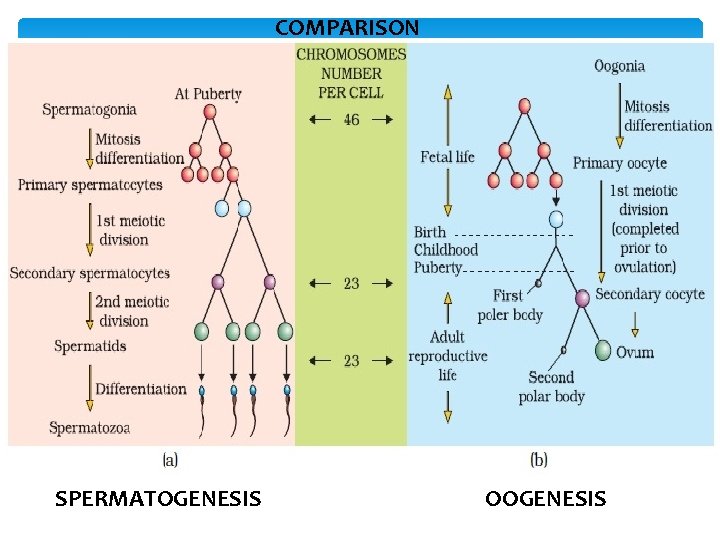
SPERMATOGENESIS The process of formation of spermatozoa (sperms) from diploid spermatogonia is called spermatogenesis. It includes the following phases: i) Multiplication Phase: The male germ cells (spermatogonia) present on the inside wall of seminiferous tubules multiply by mitotic division and increase in numbers. ii) Growth Phase: Spermatogonia grow and increase in size and form primary spermatocytes. Each spermatogonium is diploid and contains 46 chromosomes. iii) Maturation phase or formation of spermatids: The primary spermatocytes periodically undergo meiosis. A primary spermatocyte completes the first meiotic division (reduction division) leading to formation of two equal haploid cells called secondary spermatocytes (23 chromosomes each). The secondary spermatocytes undergo the second meiotic division to produce four equal haploid spermatids. iv) Differentiation Phase: The spermatids are transformed into spermatozoa (sperms) by the process- Spermiogenesis. After spermiogenesis, the sperm head gets embedded in the Sertoli cells and are finally released from the seminiferous tubules by the process called Spermiation.
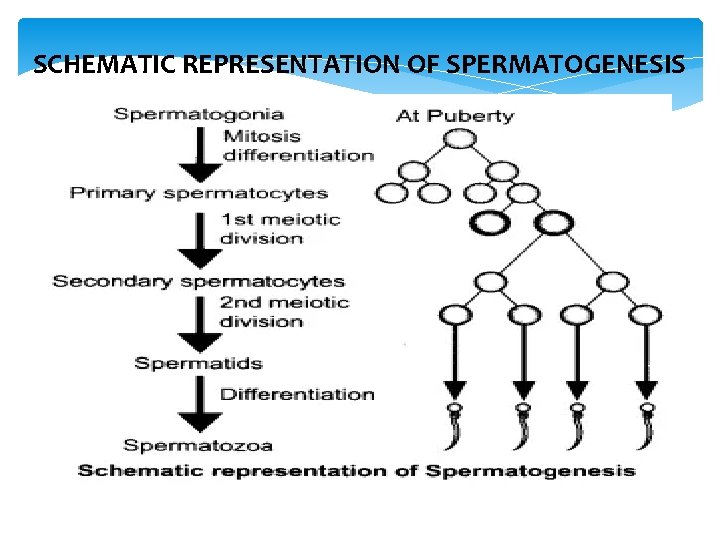
SCHEMATIC REPRESENTATION OF SPERMATOGENESIS
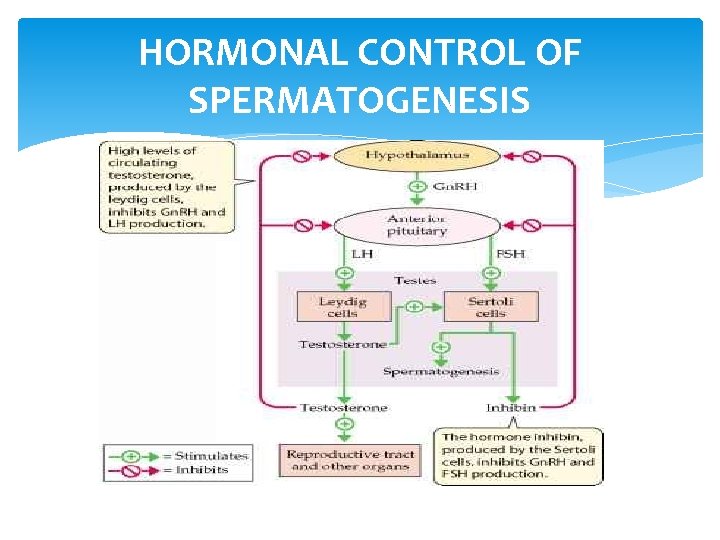
HORMONAL CONTROL OF SPERMATOGENESIS
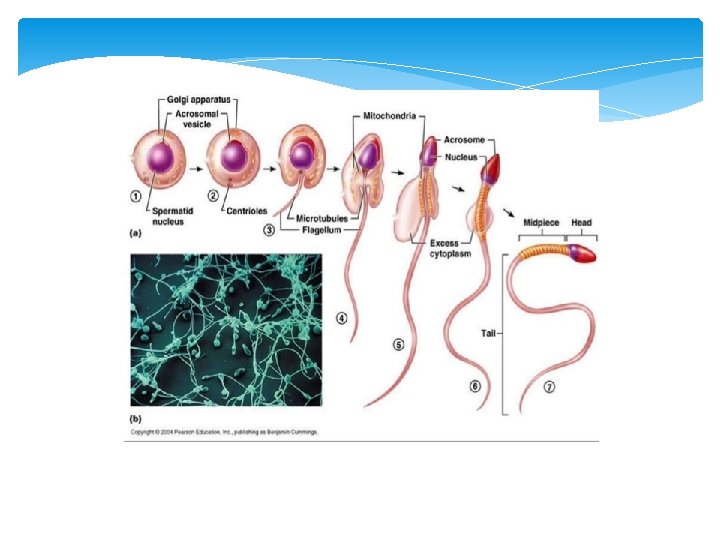
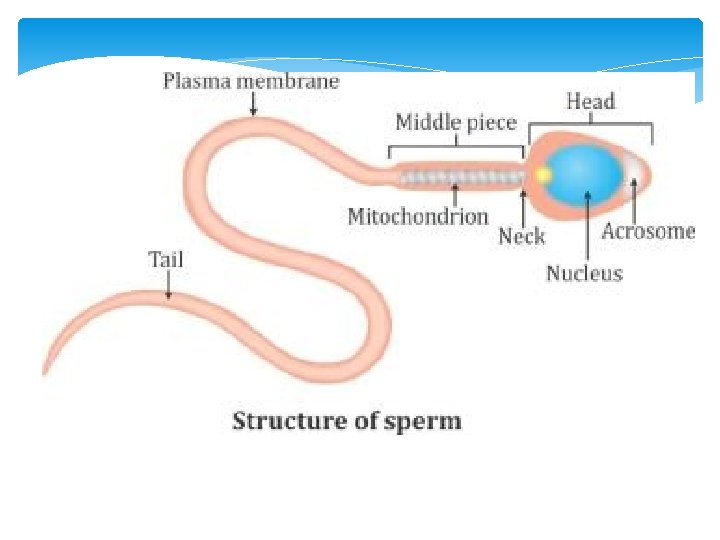
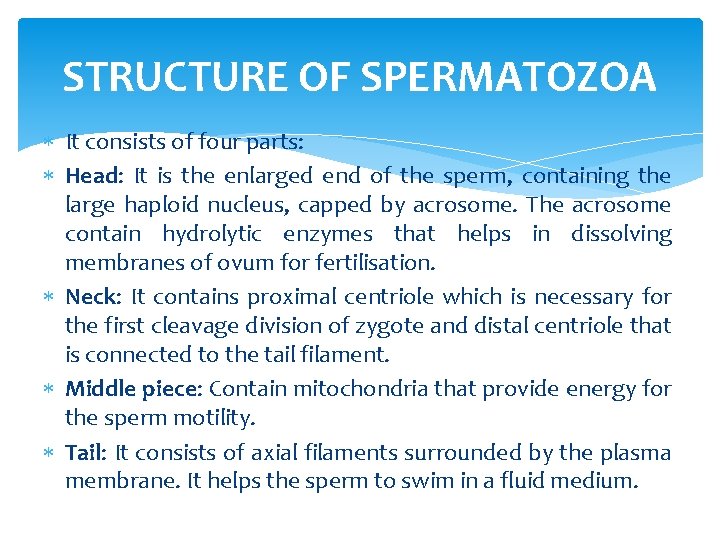
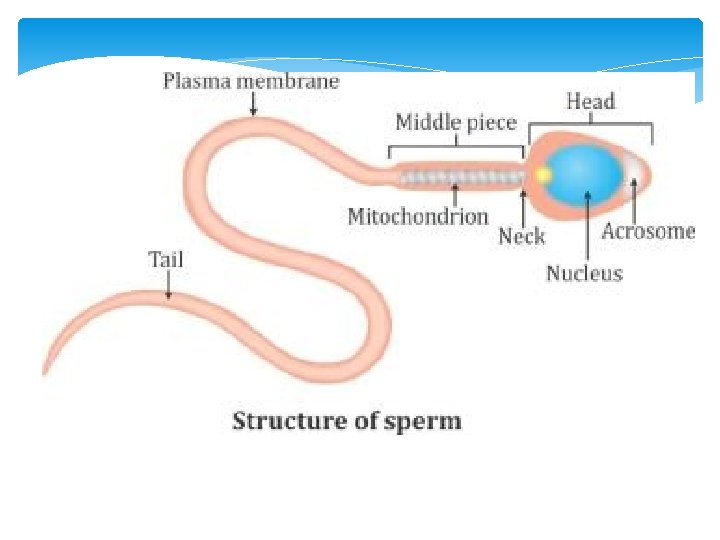
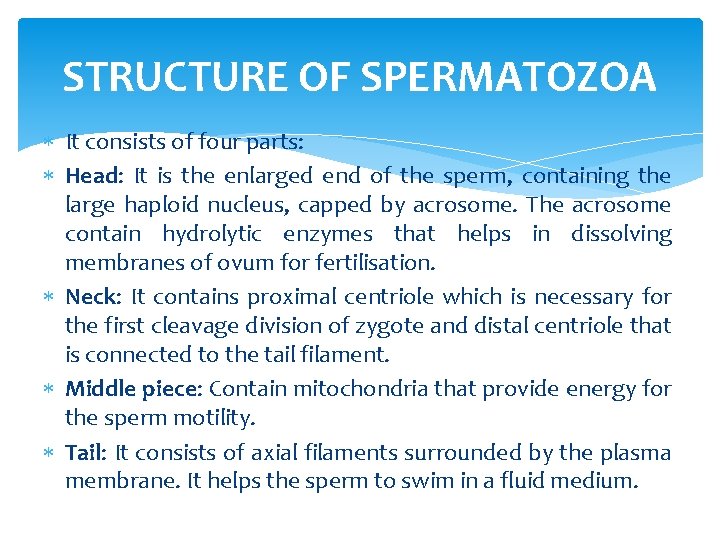
STRUCTURE OF SPERMATOZOA It consists of four parts: Head: It is the enlarged end of the sperm, containing the large haploid nucleus, capped by acrosome. The acrosome contain hydrolytic enzymes that helps in dissolving membranes of ovum for fertilisation. Neck: It contains proximal centriole which is necessary for the first cleavage division of zygote and distal centriole that is connected to the tail filament. Middle piece: Contain mitochondria that provide energy for the sperm motility. Tail: It consists of axial filaments surrounded by the plasma membrane. It helps the sperm to swim in a fluid medium.
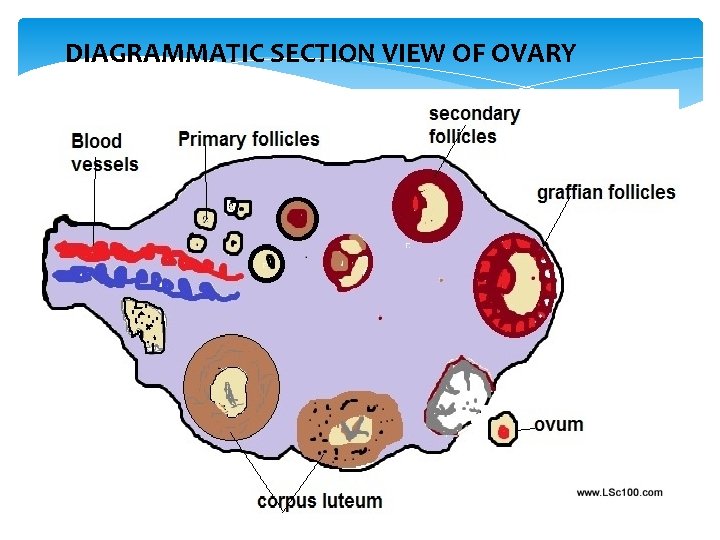
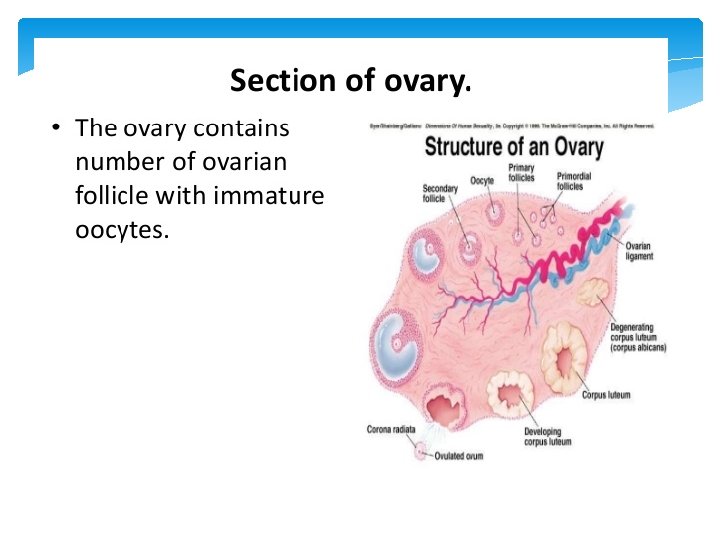
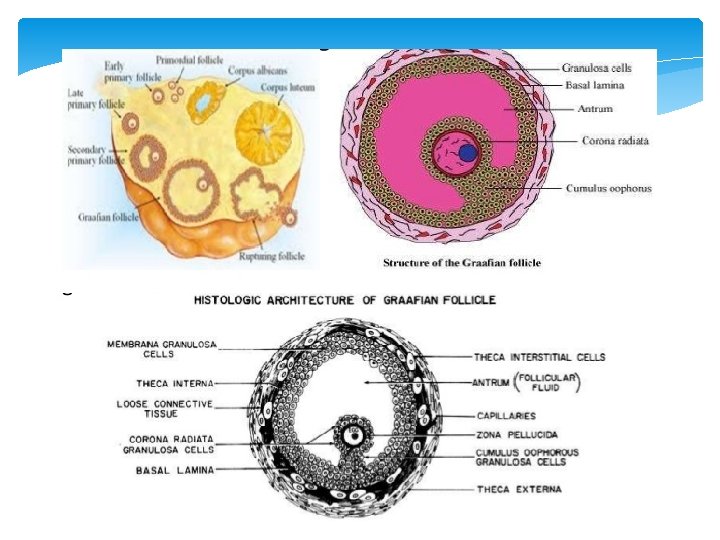
DIAGRAMMATIC SECTION VIEW OF OVARY
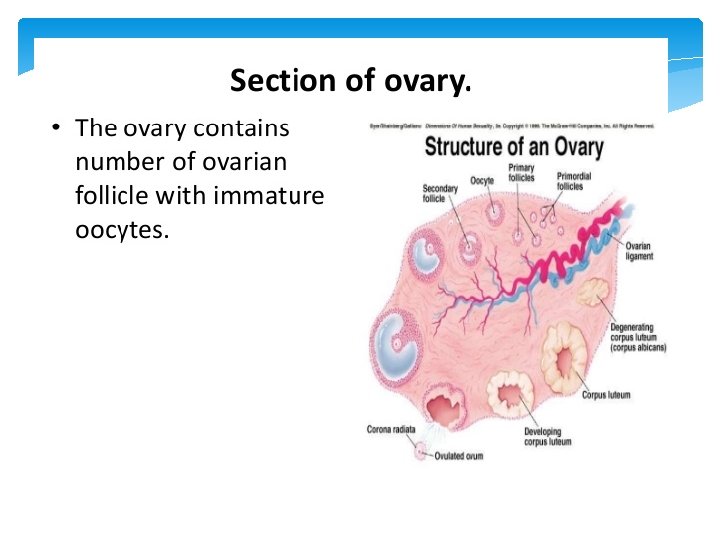
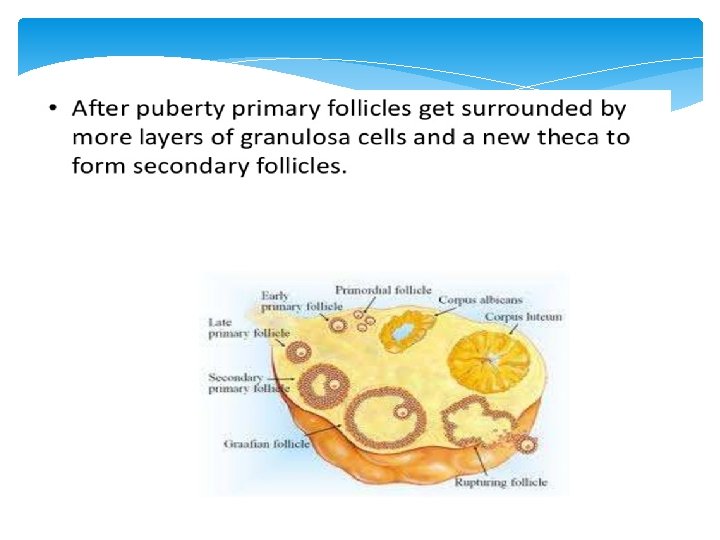
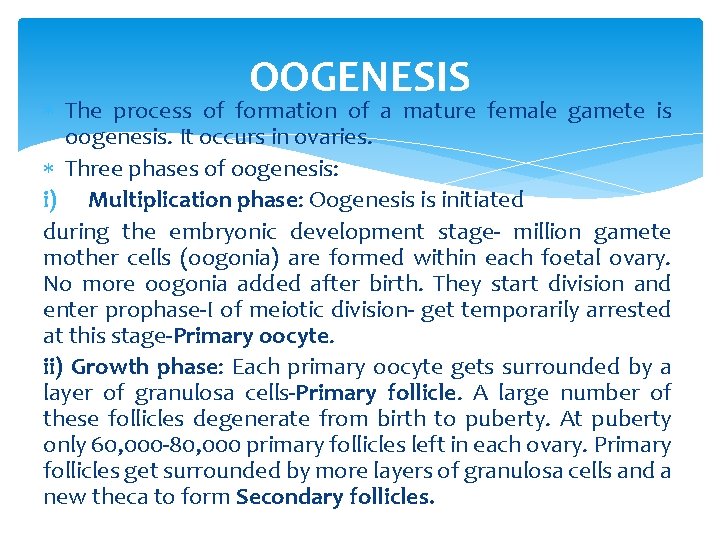
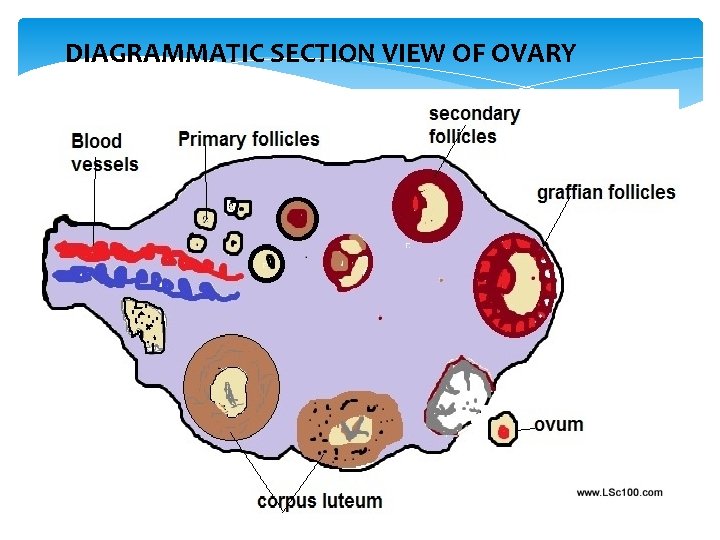
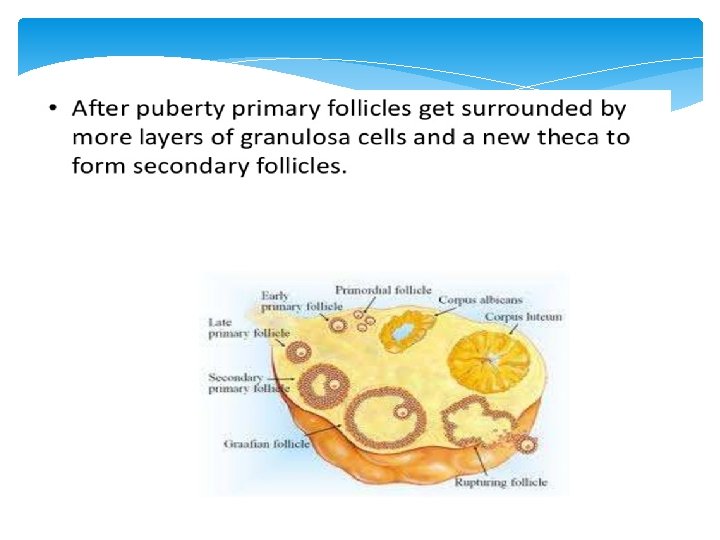
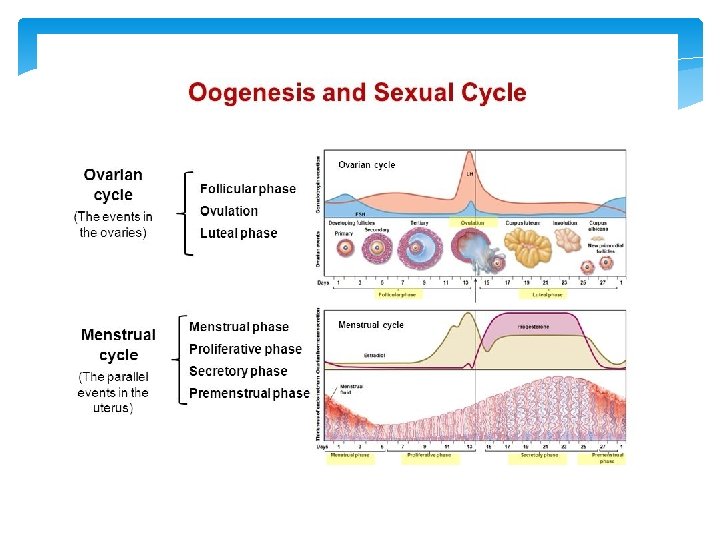
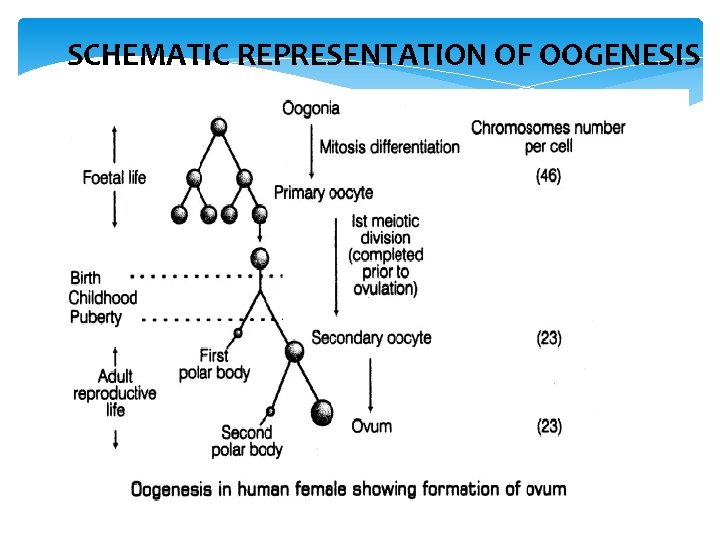
OOGENESIS The process of formation of a mature female gamete is oogenesis. It occurs in ovaries. Three phases of oogenesis: i) Multiplication phase: Oogenesis is initiated during the embryonic development stage- million gamete mother cells (oogonia) are formed within each foetal ovary. No more oogonia added after birth. They start division and enter prophase-I of meiotic division- get temporarily arrested at this stage-Primary oocyte. ii) Growth phase: Each primary oocyte gets surrounded by a layer of granulosa cells-Primary follicle. A large number of these follicles degenerate from birth to puberty. At puberty only 60, 000 -80, 000 primary follicles left in each ovary. Primary follicles get surrounded by more layers of granulosa cells and a new theca to form Secondary follicles.
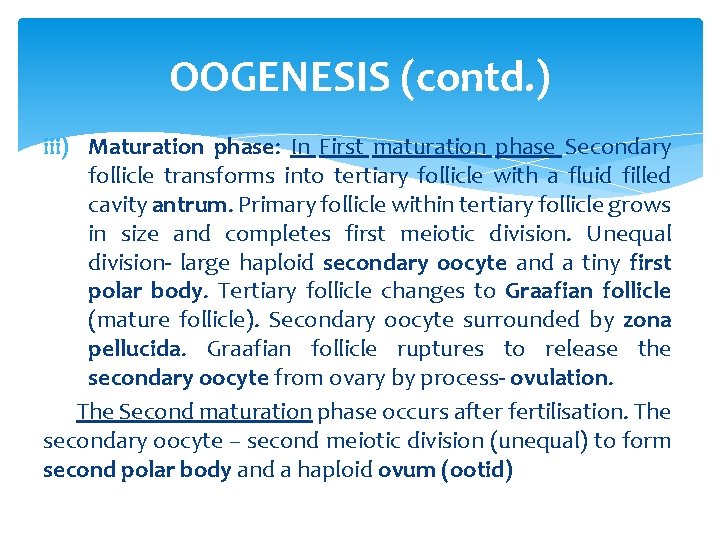
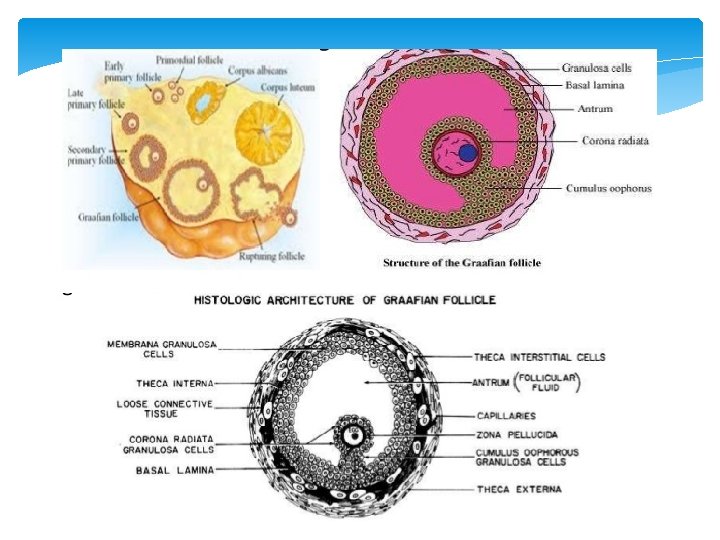
OOGENESIS (contd. ) iii) Maturation phase: In First maturation phase Secondary follicle transforms into tertiary follicle with a fluid filled cavity antrum. Primary follicle within tertiary follicle grows in size and completes first meiotic division. Unequal division- large haploid secondary oocyte and a tiny first polar body. Tertiary follicle changes to Graafian follicle (mature follicle). Secondary oocyte surrounded by zona pellucida. Graafian follicle ruptures to release the secondary oocyte from ovary by process- ovulation. The Second maturation phase occurs after fertilisation. The secondary oocyte – second meiotic division (unequal) to form second polar body and a haploid ovum (ootid)
SCHEMATIC REPRESENTATION OF OOGENESIS
COMPARISON SPERMATOGENESIS OOGENESIS
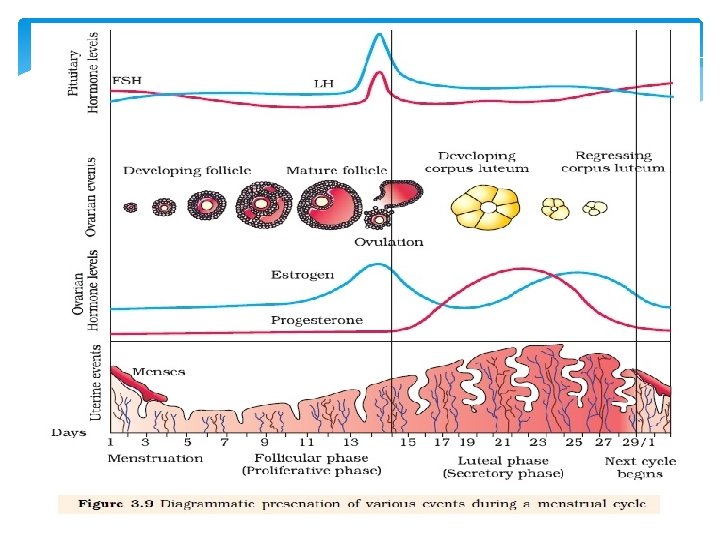
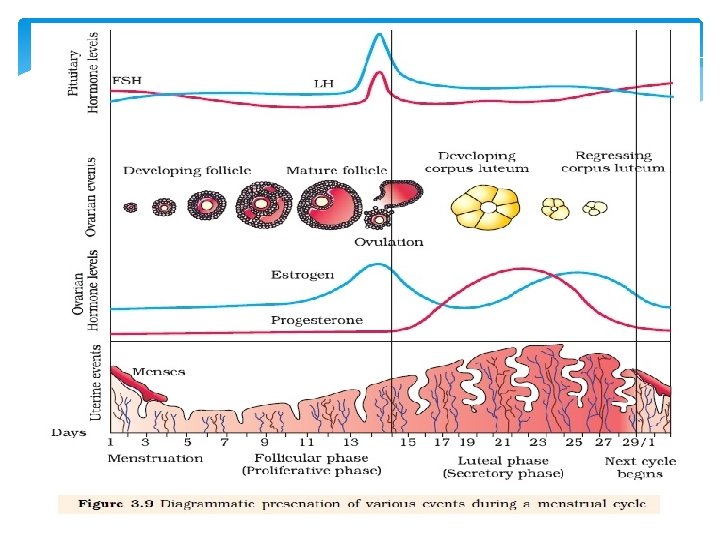
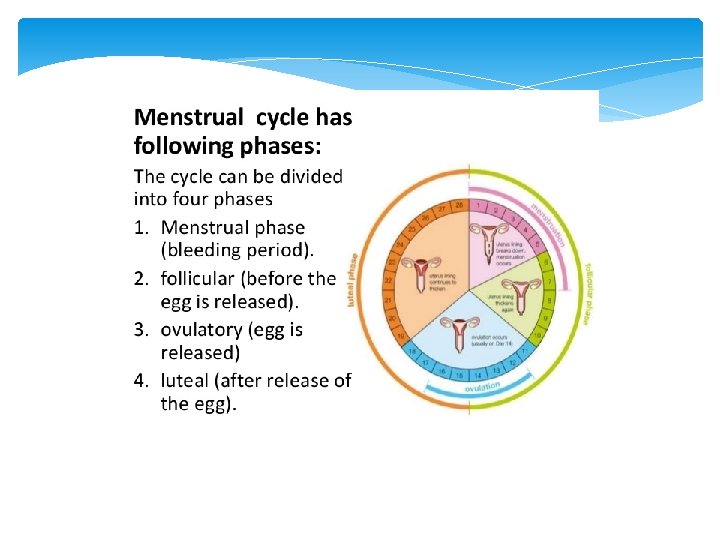
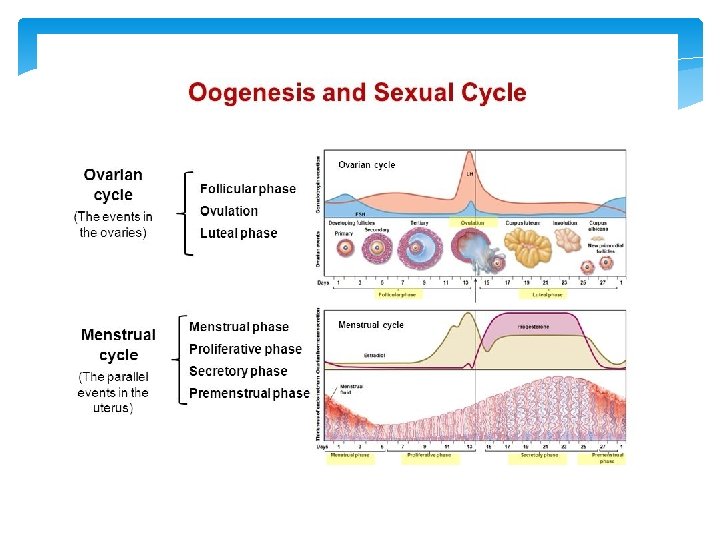
MENSTRUAL CYCLE The rhythmic series of changes that occur in the reproductive organs of female primates (monkeys, apes and human beings) is called menstrual cycle. It is repeated at an average interval of about 28/29 days. The first appearance of menstruation at puberty is called menarche. In human beings, menstrual cycle ceases after 50 years of age; that is termed as menopause.
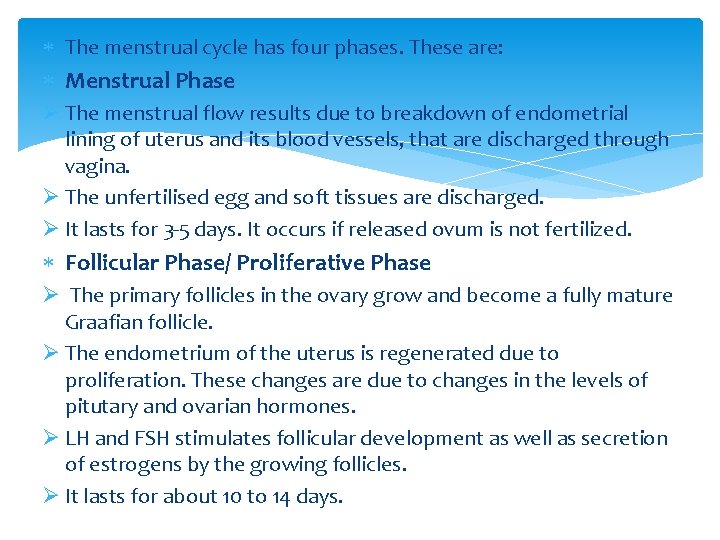
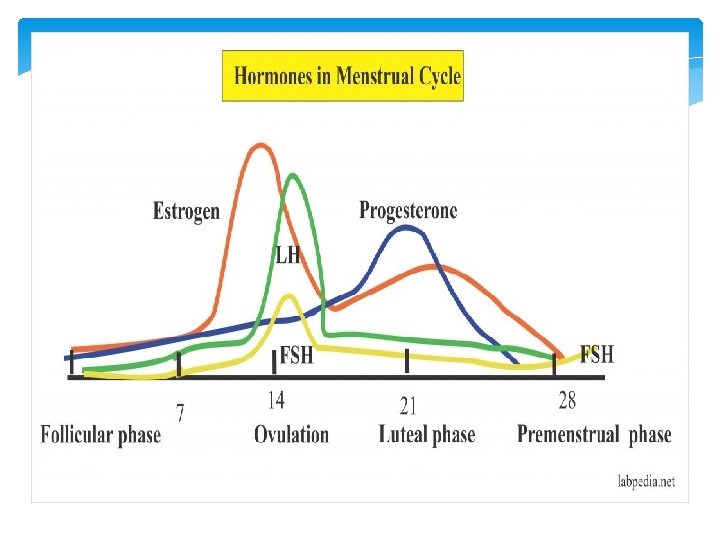
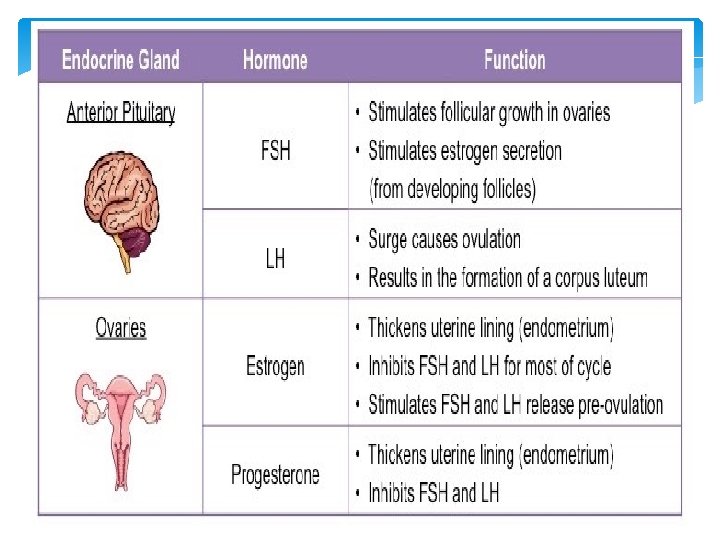
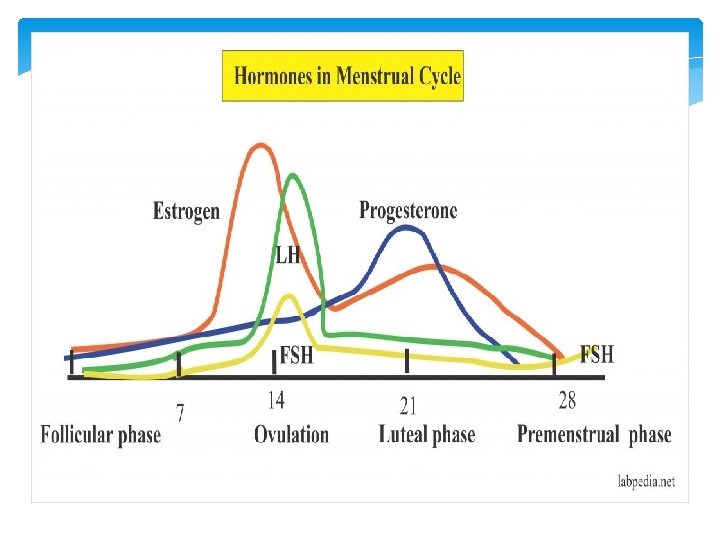
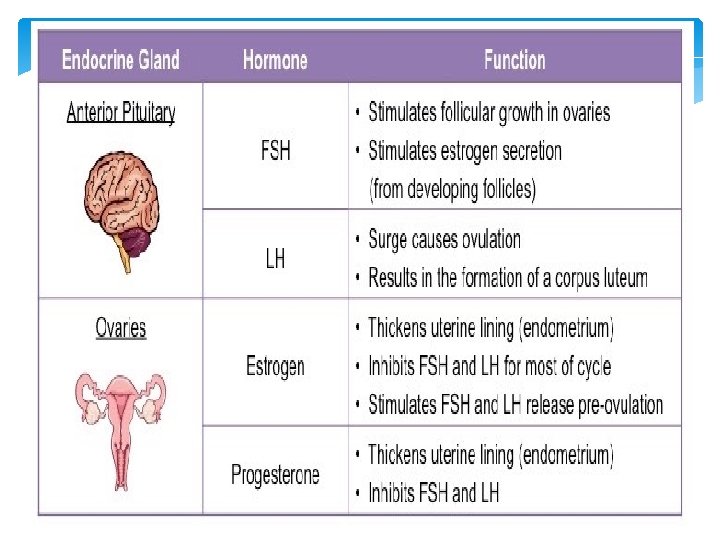
The menstrual cycle has four phases. These are: Menstrual Phase Ø The menstrual flow results due to breakdown of endometrial lining of uterus and its blood vessels, that are discharged through vagina. Ø The unfertilised egg and soft tissues are discharged. Ø It lasts for 3 -5 days. It occurs if released ovum is not fertilized. Follicular Phase/ Proliferative Phase Ø The primary follicles in the ovary grow and become a fully mature Graafian follicle. Ø The endometrium of the uterus is regenerated due to proliferation. These changes are due to changes in the levels of pitutary and ovarian hormones. Ø LH and FSH stimulates follicular development as well as secretion of estrogens by the growing follicles. Ø It lasts for about 10 to 14 days.
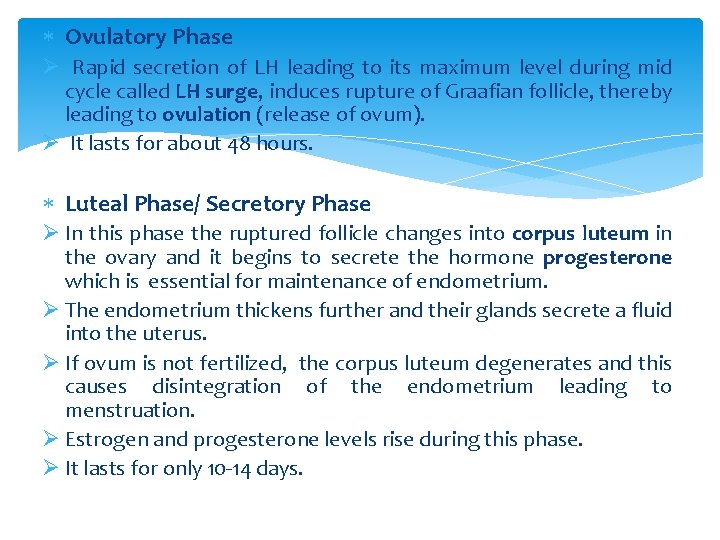
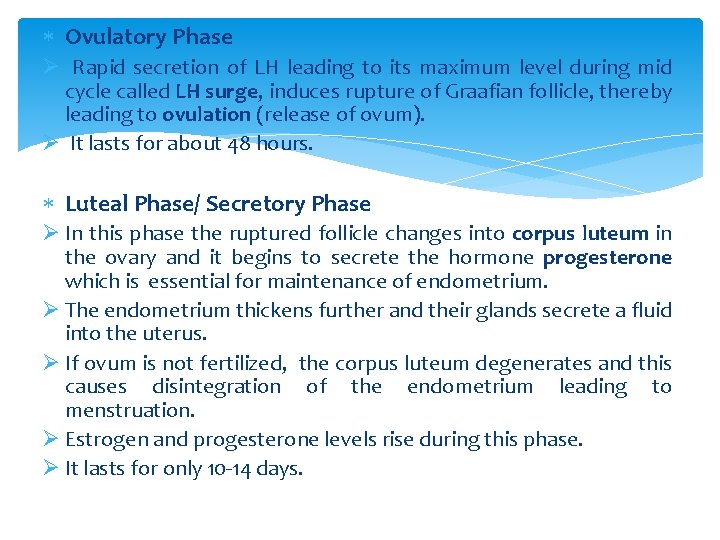
Ovulatory Phase Ø Rapid secretion of LH leading to its maximum level during mid cycle called LH surge, induces rupture of Graafian follicle, thereby leading to ovulation (release of ovum). Ø It lasts for about 48 hours. Luteal Phase/ Secretory Phase Ø In this phase the ruptured follicle changes into corpus luteum in the ovary and it begins to secrete the hormone progesterone which is essential for maintenance of endometrium. Ø The endometrium thickens further and their glands secrete a fluid into the uterus. Ø If ovum is not fertilized, the corpus luteum degenerates and this causes disintegration of the endometrium leading to menstruation. Ø Estrogen and progesterone levels rise during this phase. Ø It lasts for only 10 -14 days.
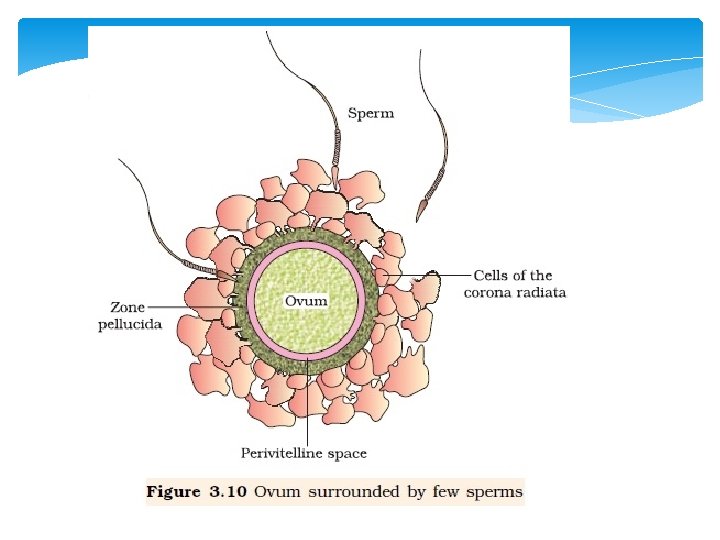
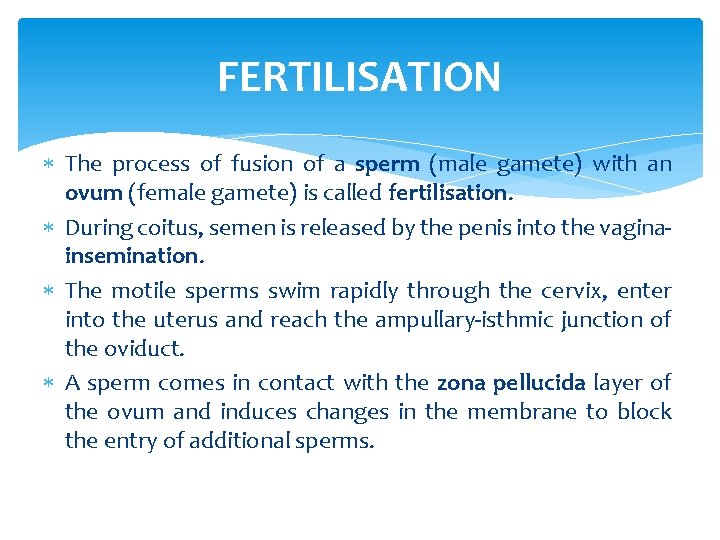
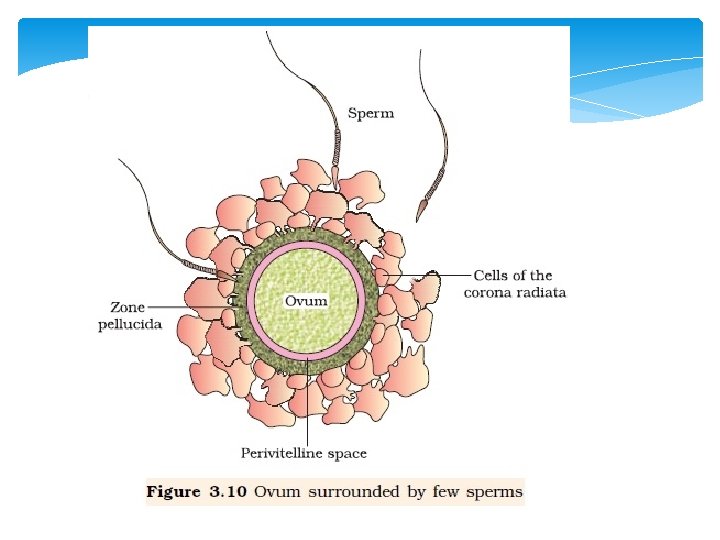
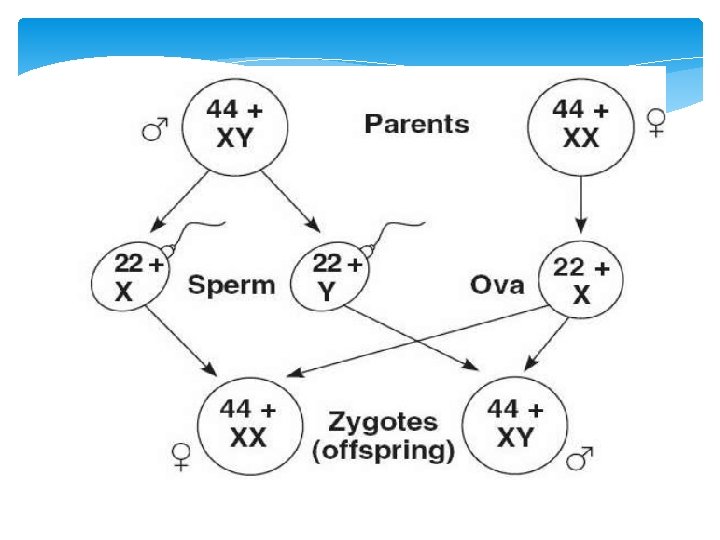
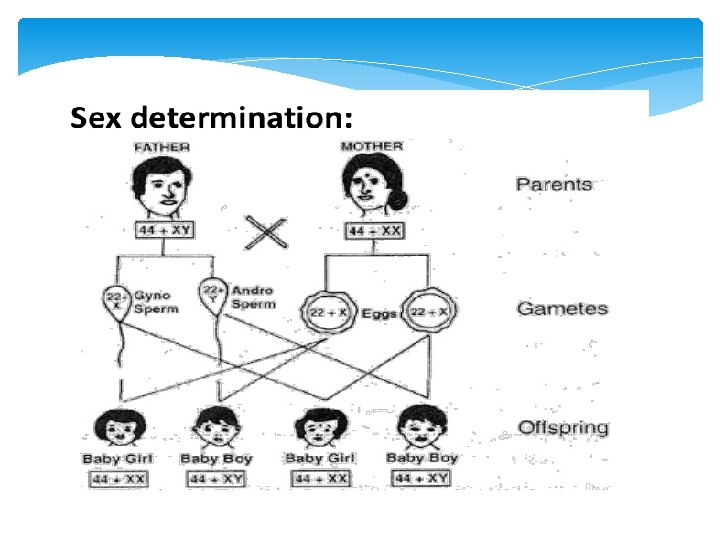
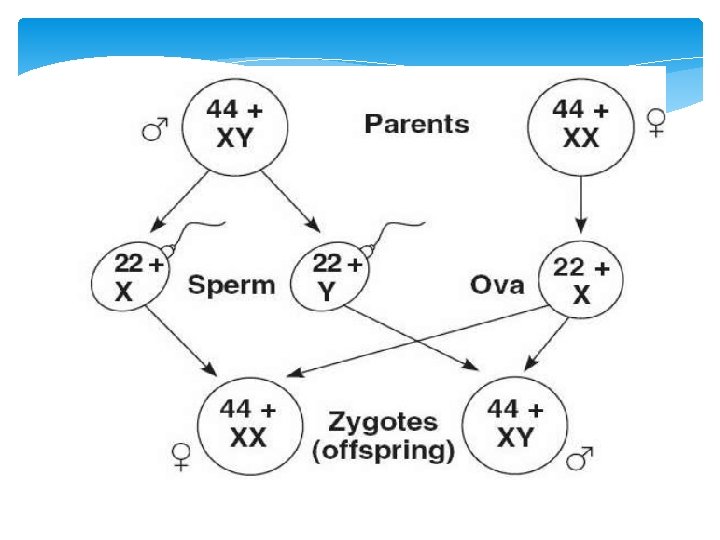
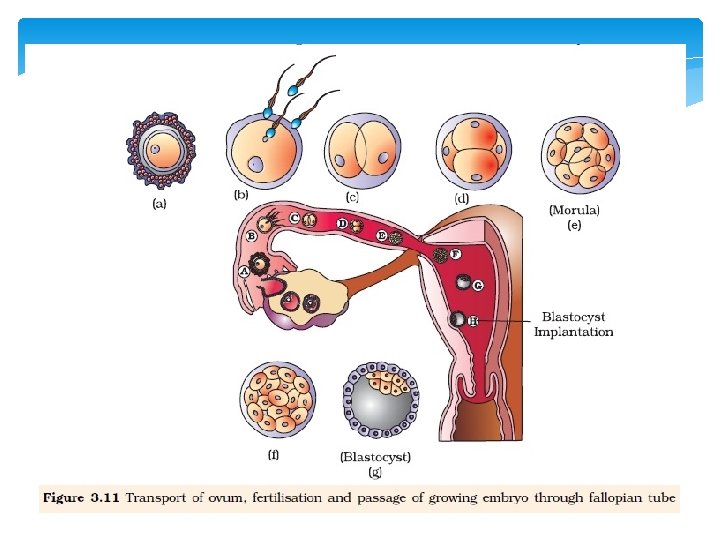
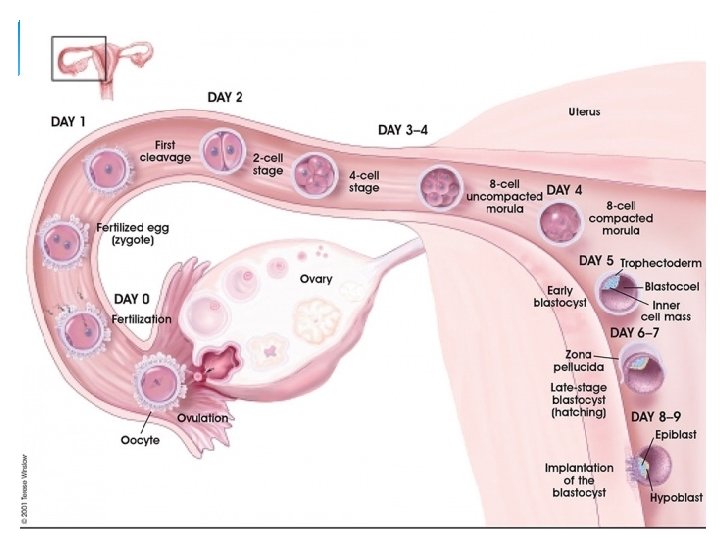
FERTILISATION The process of fusion of a sperm (male gamete) with an ovum (female gamete) is called fertilisation. During coitus, semen is released by the penis into the vaginainsemination. The motile sperms swim rapidly through the cervix, enter into the uterus and reach the ampullary-isthmic junction of the oviduct. A sperm comes in contact with the zona pellucida layer of the ovum and induces changes in the membrane to block the entry of additional sperms.
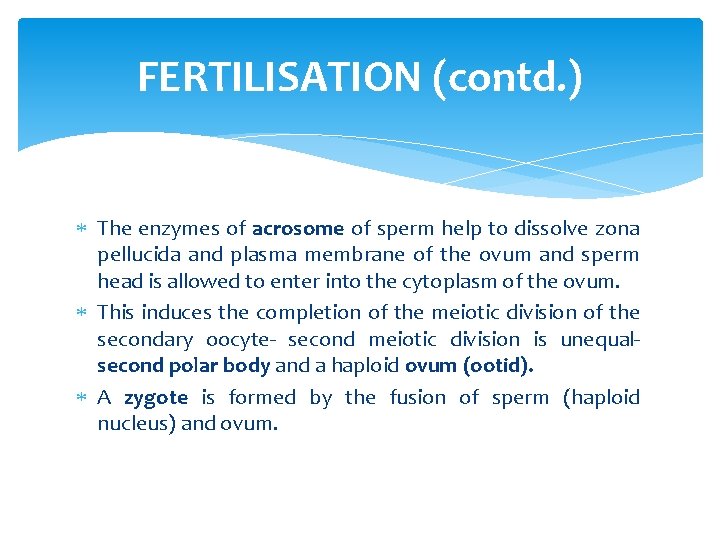
FERTILISATION (contd. ) The enzymes of acrosome of sperm help to dissolve zona pellucida and plasma membrane of the ovum and sperm head is allowed to enter into the cytoplasm of the ovum. This induces the completion of the meiotic division of the secondary oocyte- second meiotic division is unequalsecond polar body and a haploid ovum (ootid). A zygote is formed by the fusion of sperm (haploid nucleus) and ovum.
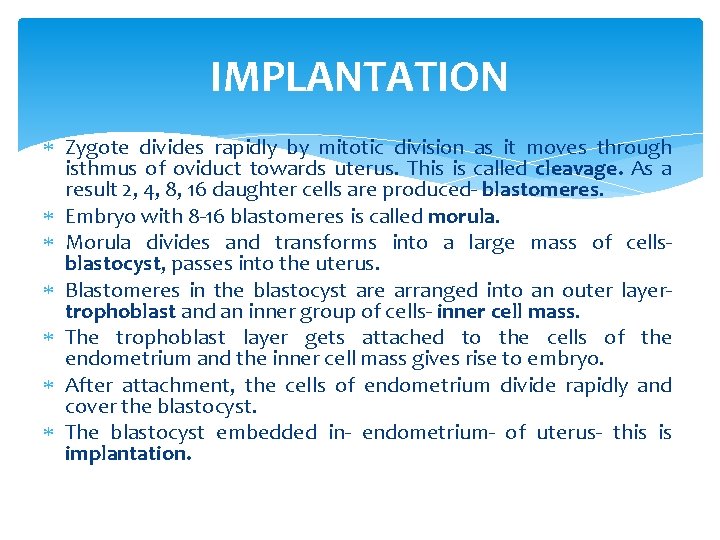
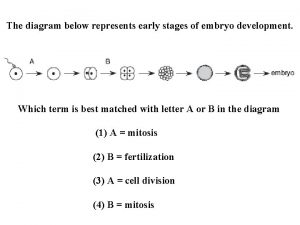
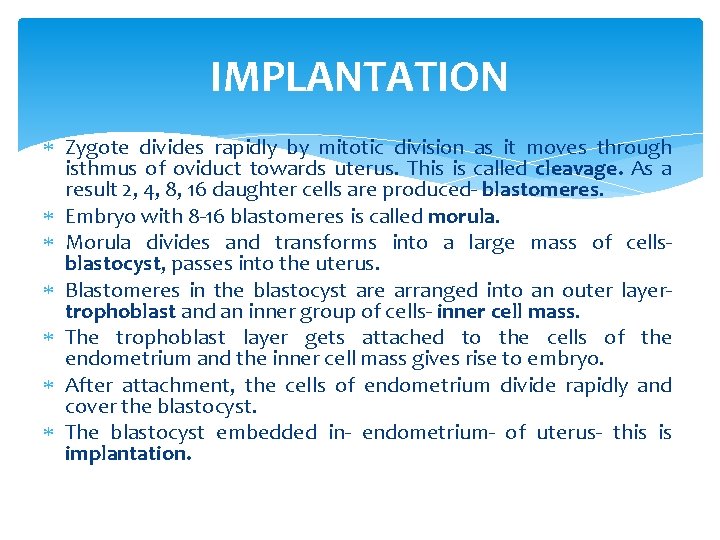
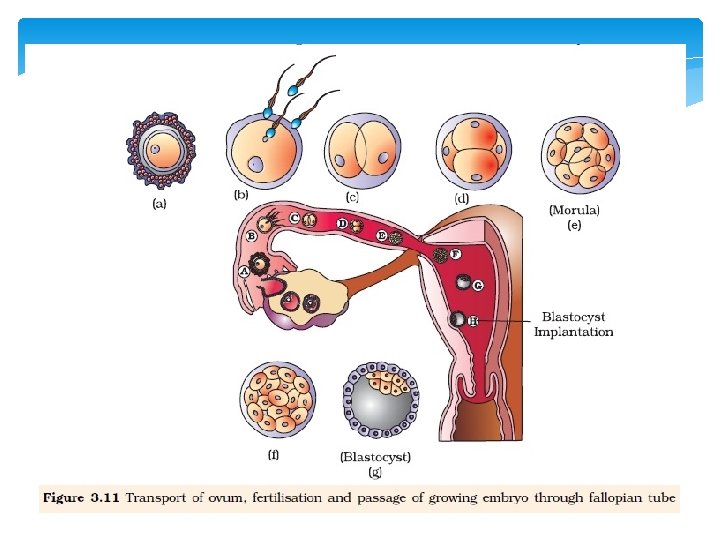
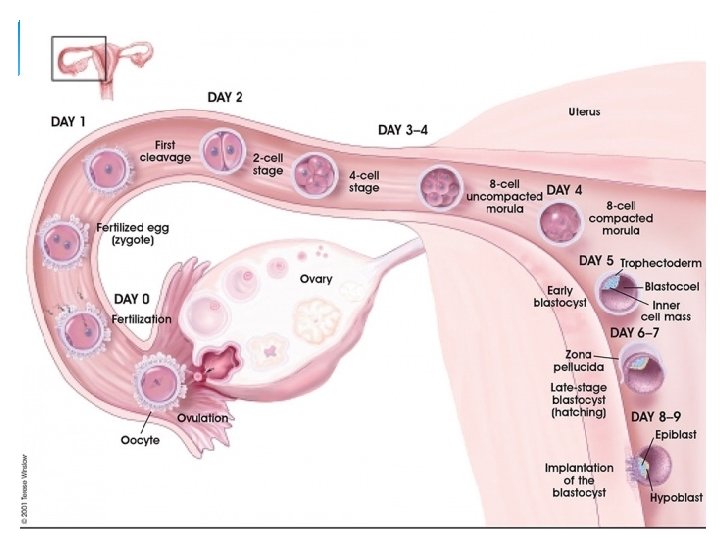
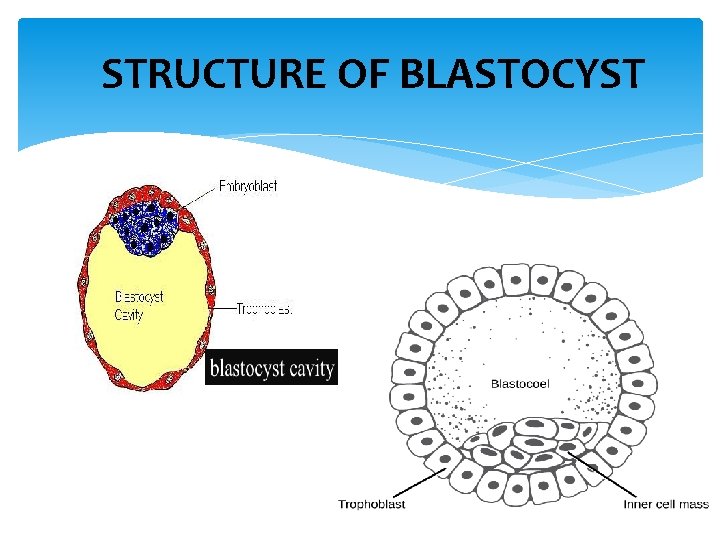
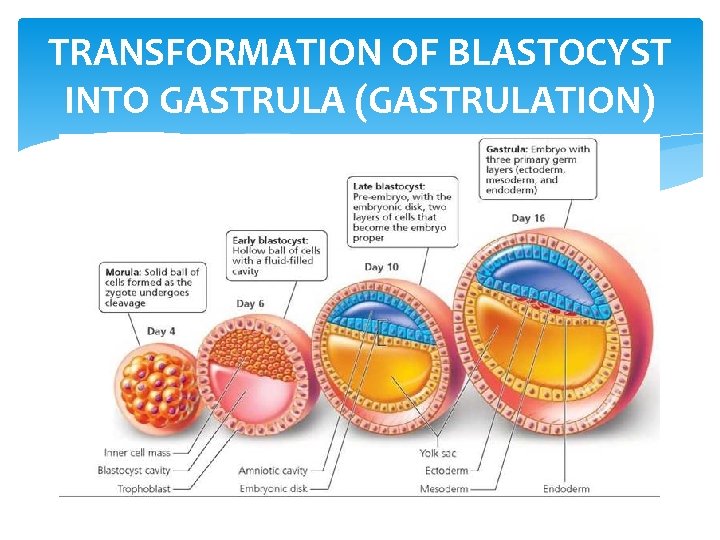
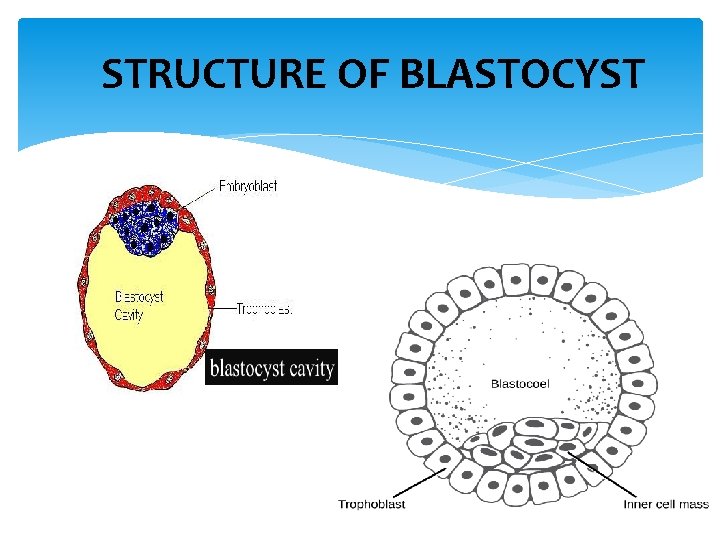
IMPLANTATION Zygote divides rapidly by mitotic division as it moves through isthmus of oviduct towards uterus. This is called cleavage. As a result 2, 4, 8, 16 daughter cells are produced- blastomeres. Embryo with 8 -16 blastomeres is called morula. Morula divides and transforms into a large mass of cellsblastocyst, passes into the uterus. Blastomeres in the blastocyst are arranged into an outer layertrophoblast and an inner group of cells- inner cell mass. The trophoblast layer gets attached to the cells of the endometrium and the inner cell mass gives rise to embryo. After attachment, the cells of endometrium divide rapidly and cover the blastocyst. The blastocyst embedded in- endometrium- of uterus- this is implantation.

STRUCTURE OF BLASTOCYST
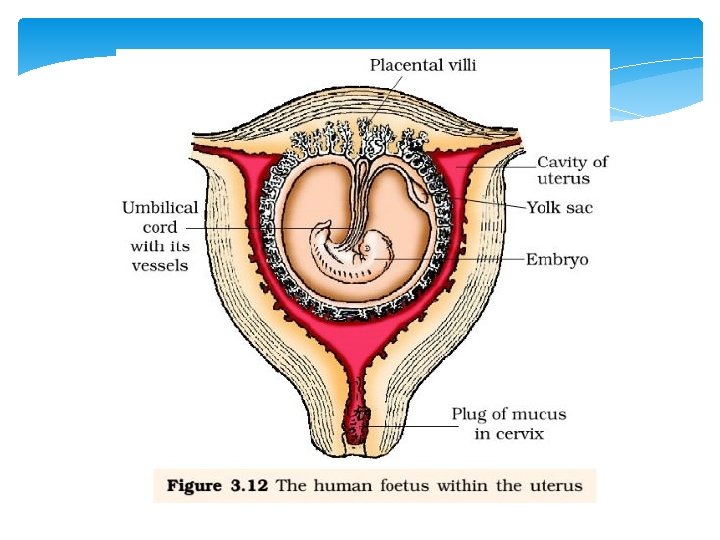
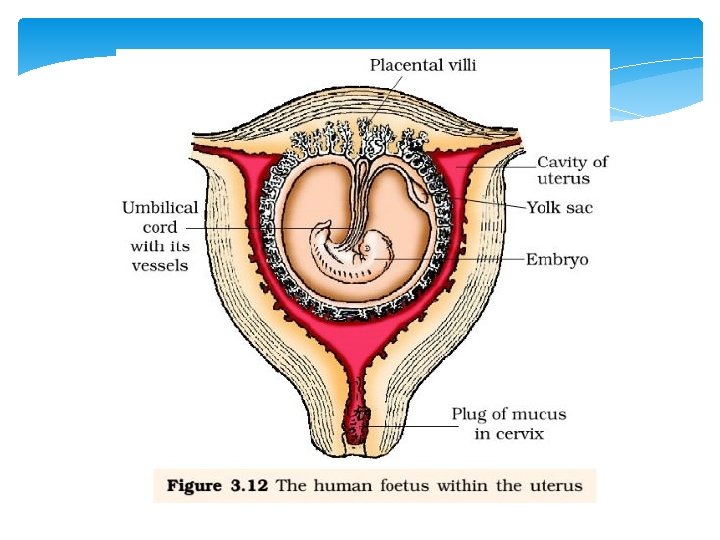
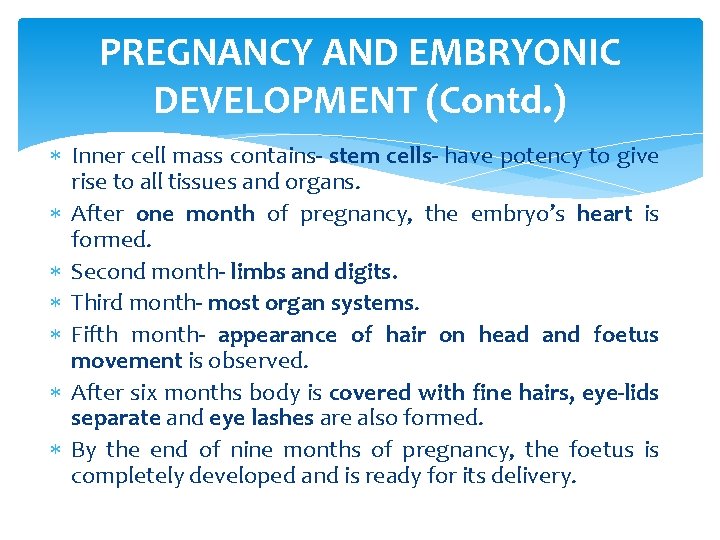
PREGNANCY AND EMBRYONIC DEVELOPMENT Cells of trophoblast differentiate into inner layer and outer layer. The outer layer is chorion and forms chorionic villi (finger-like projections) that grow into endometrium. The chorionic villi and uterine tissue become interdigiated with each other. It forms a structural and functional unit between the developing embryo and the maternal body called placenta.
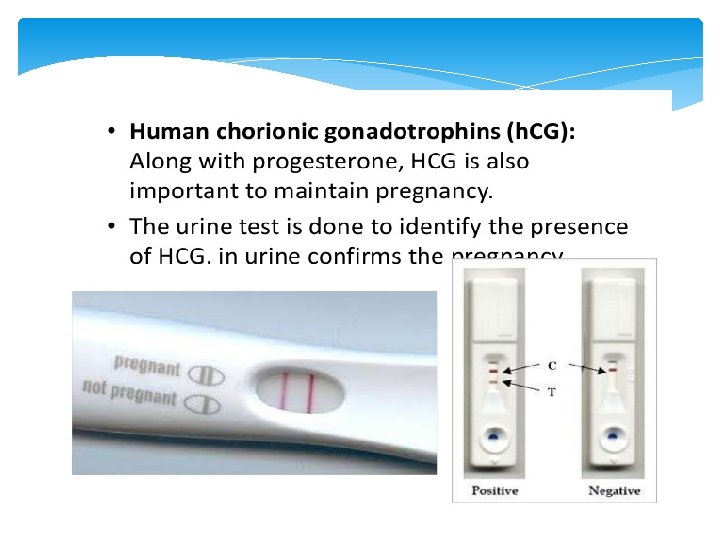
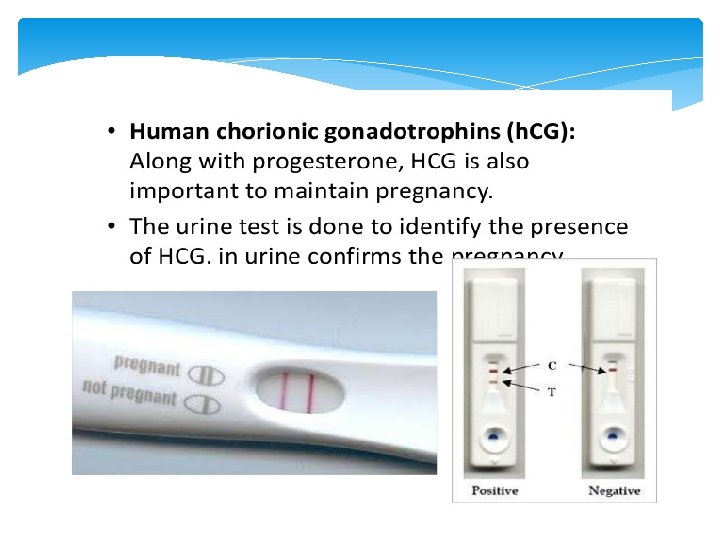
FUNCTIONS OF PLACENTA i) Provides nutrients and oxygen to the developing embryo. ii) Removes carbon-dioxide and waste materials from the embryo. iii) Acts as an endocrine tissue and produces several hormones like human chorionic gonadotrophin (h. CG), human placental lactogen (h. PL), estrogens, progesterones and are essential to maintain pregnancy.
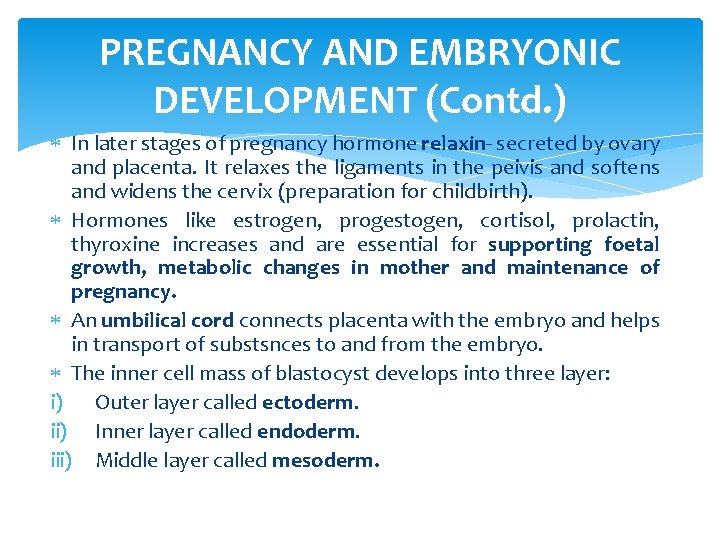
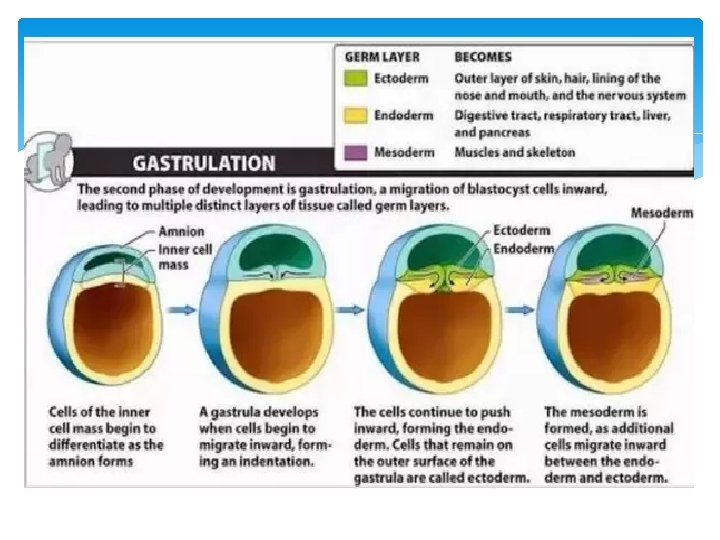
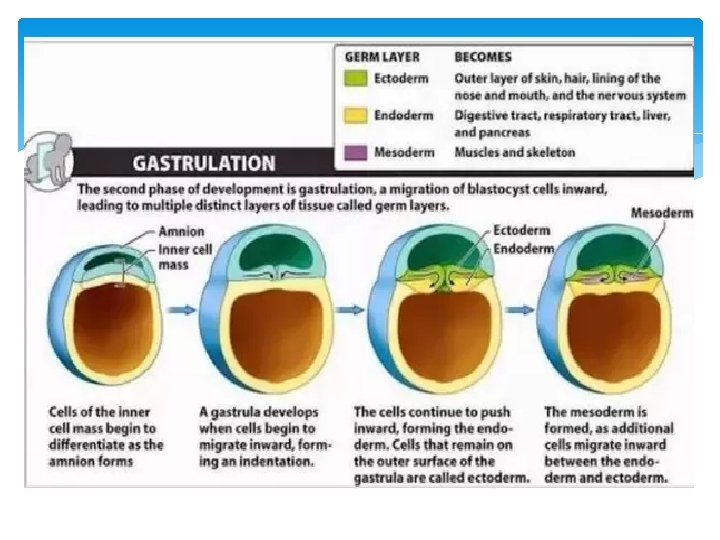
PREGNANCY AND EMBRYONIC DEVELOPMENT (Contd. ) In later stages of pregnancy hormone relaxin- secreted by ovary and placenta. It relaxes the ligaments in the peivis and softens and widens the cervix (preparation for childbirth). Hormones like estrogen, progestogen, cortisol, prolactin, thyroxine increases and are essential for supporting foetal growth, metabolic changes in mother and maintenance of pregnancy. An umbilical cord connects placenta with the embryo and helps in transport of substsnces to and from the embryo. The inner cell mass of blastocyst develops into three layer: i) Outer layer called ectoderm. ii) Inner layer called endoderm. iii) Middle layer called mesoderm.
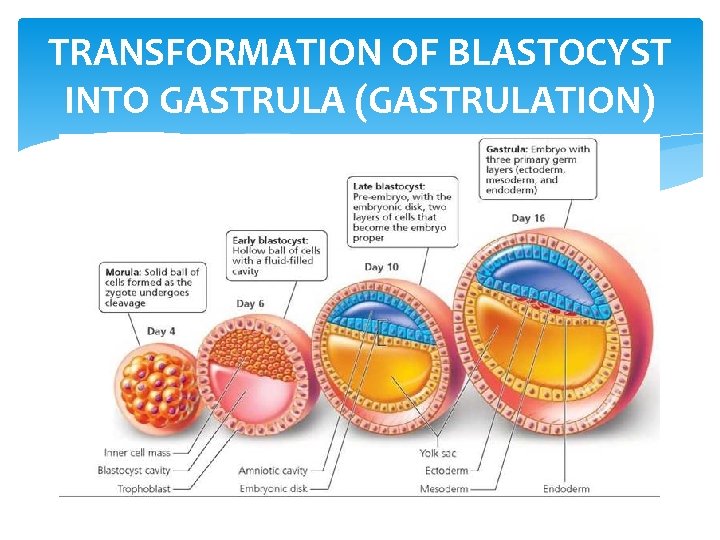
TRANSFORMATION OF BLASTOCYST INTO GASTRULA (GASTRULATION)
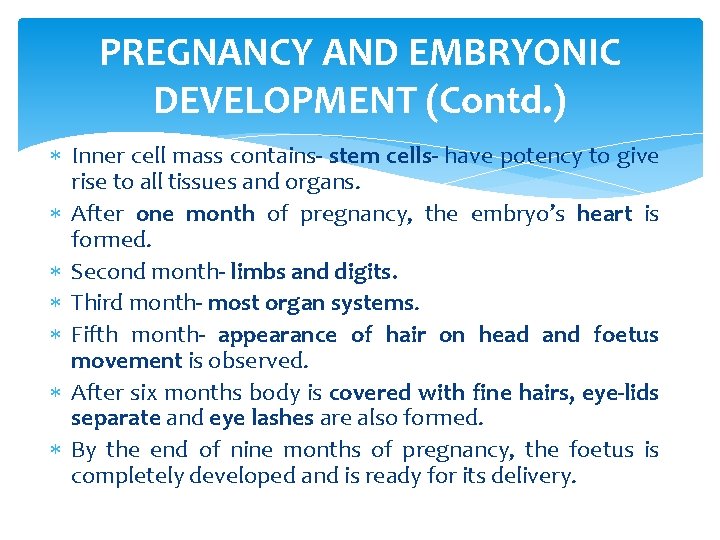
PREGNANCY AND EMBRYONIC DEVELOPMENT (Contd. ) Inner cell mass contains- stem cells- have potency to give rise to all tissues and organs. After one month of pregnancy, the embryo’s heart is formed. Second month- limbs and digits. Third month- most organ systems. Fifth month- appearance of hair on head and foetus movement is observed. After six months body is covered with fine hairs, eye-lids separate and eye lashes are also formed. By the end of nine months of pregnancy, the foetus is completely developed and is ready for its delivery.
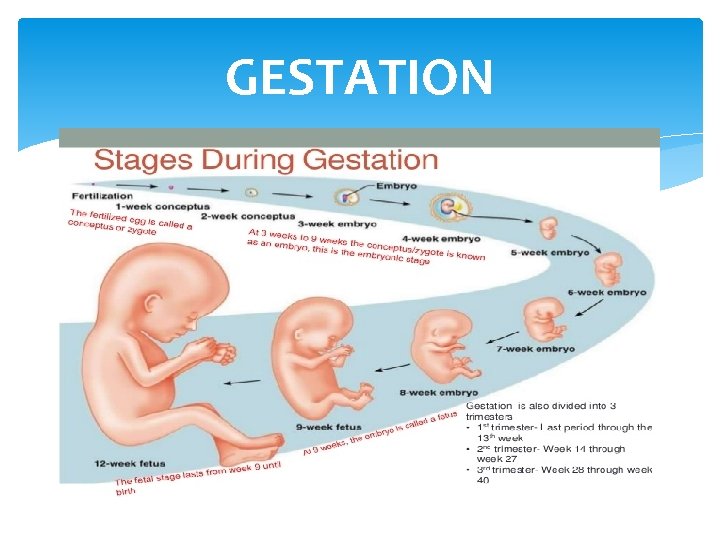
GESTATION
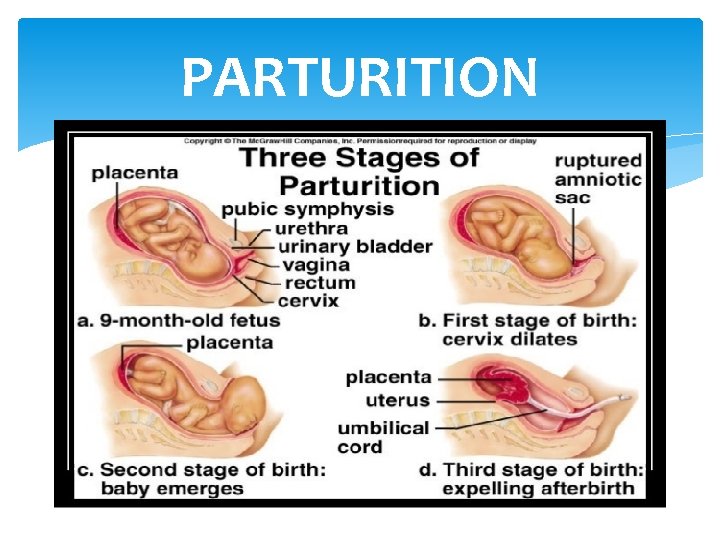
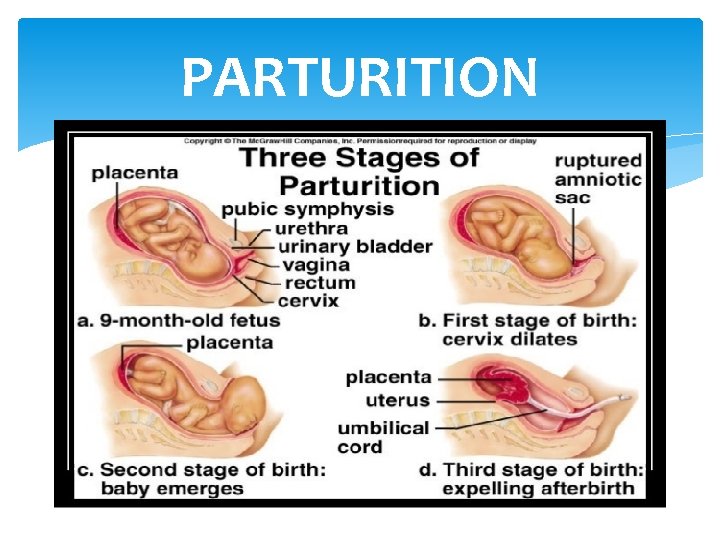
PARTURITION
PARTURITION The average duration of human pregnancy is about 9 months which is called the gestation period. The act of expelling the full term foetus from the mother’s uterus at the end of gestation period by vigorous contraction of uterus is called parturition. It is induced by a complex neuroendocrine mechanism. Parturition signals originate from the fully developed foetus and the placenta which induce mild uterine contractions called foetal ejection reflex. This triggers the release of oxytocin from the maternal pituitary. Oxytocin induces stronger uterine muscle contractions which in turn stimulate further secretions of oxytocin. Stimulatory reflex between contraction and oxytocin secretion results in stronger and stronger contradiction which leads to expulsion of baby out of the uterus through birth canal.
LACTATION Mammary glands of female undergo differentiation and start producing milk at the end of pregnancy. This is called lactation. This helps the mother in feeding the newborn. The milk that comes out of the mammary glands during initial days of lactation is called colostrum. It contains several antibodies (Ig. A) and nutrients (like calcium, fats, lactose) for the baby. It provides passive immunity to the baby. Thus, breastfeeding is recommended by doctors for bringing up a healthy baby. The milk production is controlled by prolactin hormone secreted by anterior pitutary.
ASSIGNMENT HUMAN REPRODUCTION Q 1. Q 2. Q 3. Q 4. Q 5. Q 6. Q 7. Q 8. Q 9. How is a primary spermatocyte different from a secondary spermatocyte? Not all copulations lead to pregnancy. Give reasons. State where the signals for parturition arise from, in humans. Name the hormones produced only during pregnancy in a human female. Mention their source organs. Why is parturition called a neuro-endocrine mechanism? Explain Spermatogenesis in human males is a hormone-regulated process. Justify Draw a diagram of Human sperm. Label its parts and write their functions. Draw a diagrammatic labelled sketch of a sectional view of human ovary. How is placenta formed in human female? Name two hormones, which are secreted by it and are also present in a non-pregnant woman.
Q 10. Q 11. Q 12. Q 13. Q 14. Q 15. Name the stages of human embryo and the stage at which it gets implanted. Explain the process of implantation. a. ) Where does spermatogenesis occur in human testes? Describe the process of spermatogenesis upto the formation of spermatozoa. b. Trace the path of spermatozoa from the testes upto the ejaculatory duct only. Give a schematic representation of oogenesis in humans. Mentionthe number of chromosomes at each stage. Correlate the life phases of the individual with the stages of the process. Explain the ovarian and uterine events that occur during a menstrual cycle, in a human female, under the influence of pituitary and ovarian hormones, respectively. Differentiate between spermatogenesis and oogenesis on the basis of: i) Time of initiation of the process ii) Site of completion of the process iii) Nature of meiotic division undergone by gamete mother cells. Describe the events that occur after fertilisation of an ovum till implantation in human female.

Thank You
 A sexual reproduction in humans
A sexual reproduction in humans Sexual reproduction in humans
Sexual reproduction in humans Blastula
Blastula Sexual reproduction vs asexual reproduction venn diagram
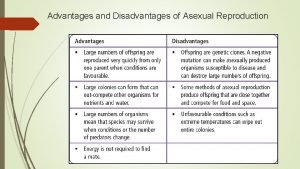
Sexual reproduction vs asexual reproduction venn diagram Asexualk
Asexualk Venn diagram asexual vs sexual reproduction
Venn diagram asexual vs sexual reproduction Reproduction human
Reproduction human Reproduction in humans
Reproduction in humans Human reproductive system
Human reproductive system Zygomycota class
Zygomycota class Fungi
Fungi Chapter 20 sexual reproduction in animals packet answers
Chapter 20 sexual reproduction in animals packet answers Sexual reproduction?
Sexual reproduction? Define sexual reproduction
Define sexual reproduction Section 1 meiosis
Section 1 meiosis Whats sexual reproduction
Whats sexual reproduction Mendelian genetics
Mendelian genetics Disadvantage of sexual reproduction
Disadvantage of sexual reproduction Connecting the concepts sexual reproduction
Connecting the concepts sexual reproduction Sexual reproduction and genetics section 1 meiosis
Sexual reproduction and genetics section 1 meiosis Mitosis sexual reproduction
Mitosis sexual reproduction Connecting the concepts sexual reproduction
Connecting the concepts sexual reproduction Whats sexual reproduction
Whats sexual reproduction Asexual amphibians
Asexual amphibians Disadvantages of sexual reproduction
Disadvantages of sexual reproduction Mitosis and meiosis
Mitosis and meiosis Significance of sexual reproduction
Significance of sexual reproduction Sexual reproduction
Sexual reproduction Chromosome number of animals
Chromosome number of animals Sexual and asexual reproduction in animals venn diagram
Sexual and asexual reproduction in animals venn diagram Chapter 19 protists study guide answers
Chapter 19 protists study guide answers Sexual or asexual reproduction
Sexual or asexual reproduction Plural form of fungus
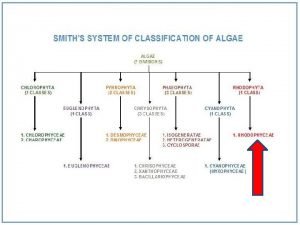
Plural form of fungus Red algae classification
Red algae classification Chapter 10 sexual reproduction and genetics
Chapter 10 sexual reproduction and genetics Sexual or asexual reproduction
Sexual or asexual reproduction Asexual or sexual reproduction
Asexual or sexual reproduction Asexual or sexual reproduction
Asexual or sexual reproduction External fertilization
External fertilization Requires two parents
Requires two parents Asexual and sexual reproduction difference
Asexual and sexual reproduction difference Sexual reproduction
Sexual reproduction Sexual reproduction
Sexual reproduction Mitotic meaning
Mitotic meaning Algea
Algea Difference between sexual and asexual reproduction
Difference between sexual and asexual reproduction Meiosis ii stages
Meiosis ii stages Sexual reproduction
Sexual reproduction Benefits of sexual propagation
Benefits of sexual propagation Example of asexual propagation
Example of asexual propagation 11/15
11/15 A sexual reproduction
A sexual reproduction A sexual reproduction in plants
A sexual reproduction in plants Dr payal arora
Dr payal arora Coen 311
Coen 311 Anjali vadlamudi
Anjali vadlamudi Dr anjali singh
Dr anjali singh Mutually exclusive vs non mutually exclusive
Mutually exclusive vs non mutually exclusive Chapter 2 human reproductive anatomy and physiology
Chapter 2 human reproductive anatomy and physiology Male reproductive system in plant
Male reproductive system in plant Human reproductive system
Human reproductive system The diagram below shows stages of human reproduction
The diagram below shows stages of human reproduction Human reproduction webquest
Human reproduction webquest Human reproduction introduction
Human reproduction introduction Reproduction in human
Reproduction in human Human reproduction
Human reproduction Introduction of transport
Introduction of transport Teixits humans
Teixits humans Inbreeding depression
Inbreeding depression First humans location
First humans location Karyotype
Karyotype Family order genus species
Family order genus species