REPRODUCTION Asexual Reproduction Sexual Reproduction in Animal Sexual

- Slides: 72
REPRODUCTION Asexual Reproduction Sexual Reproduction in Animal Sexual Reproduction in Plant
Asexual Reproduction q. Binary fission q. Fragmentation q. Budding q. Spore formation q. Vegetative propagation q. Biotechnology
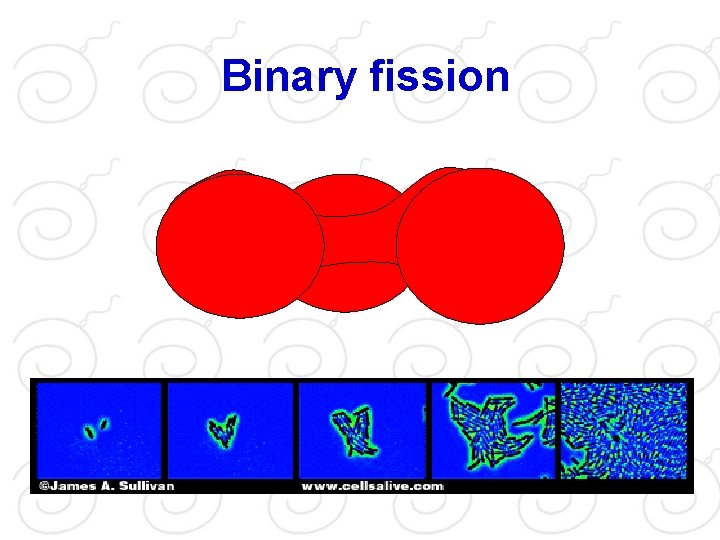
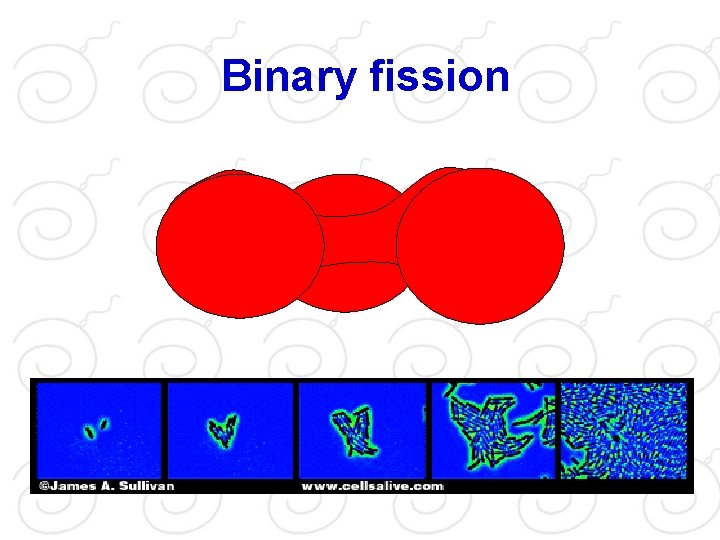
Binary fission
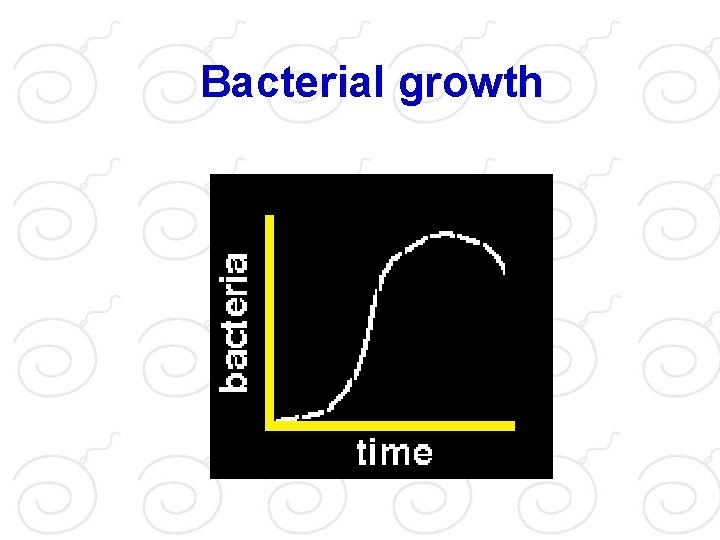
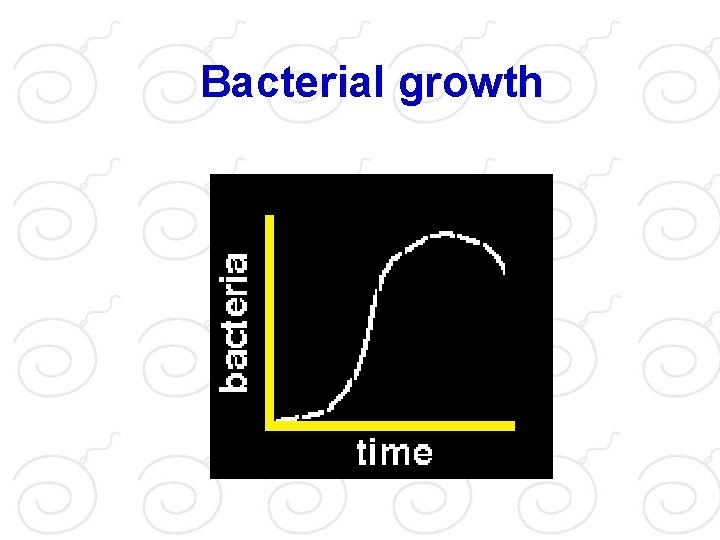
Bacterial growth
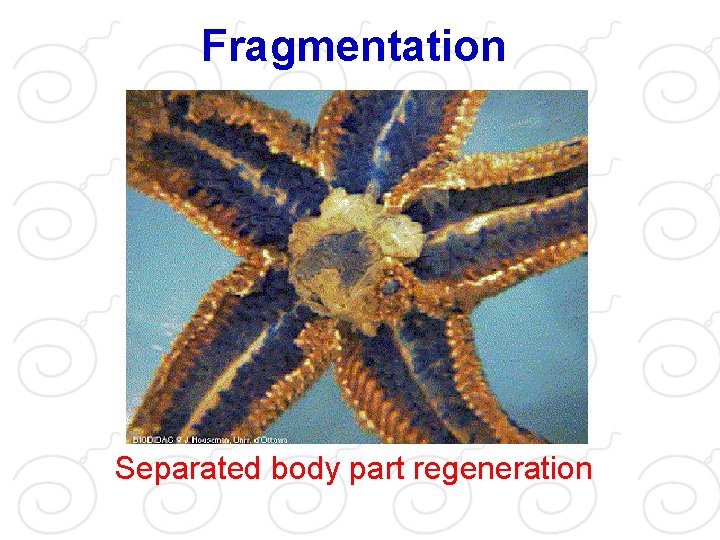
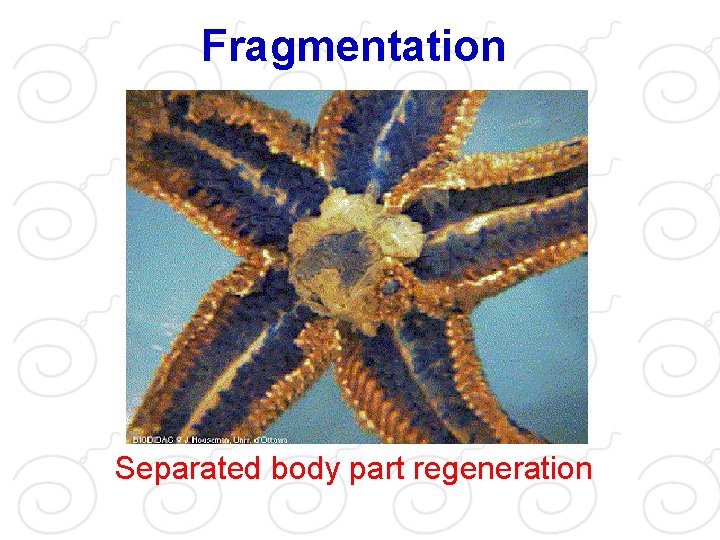
Fragmentation Separated body part regeneration
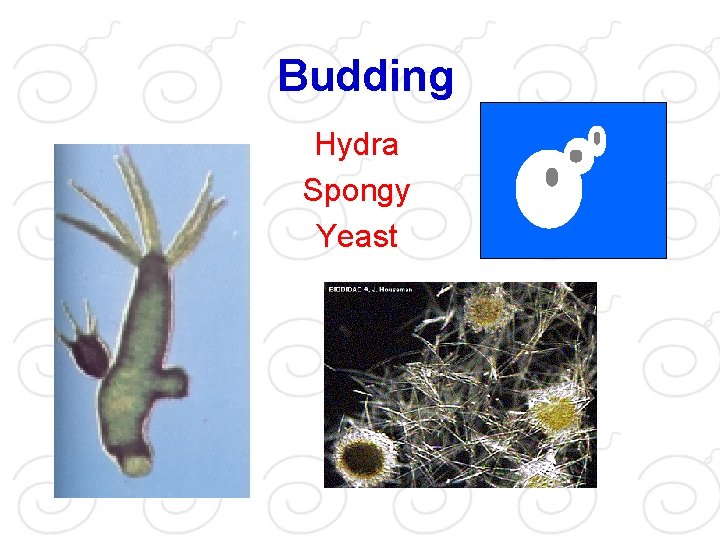
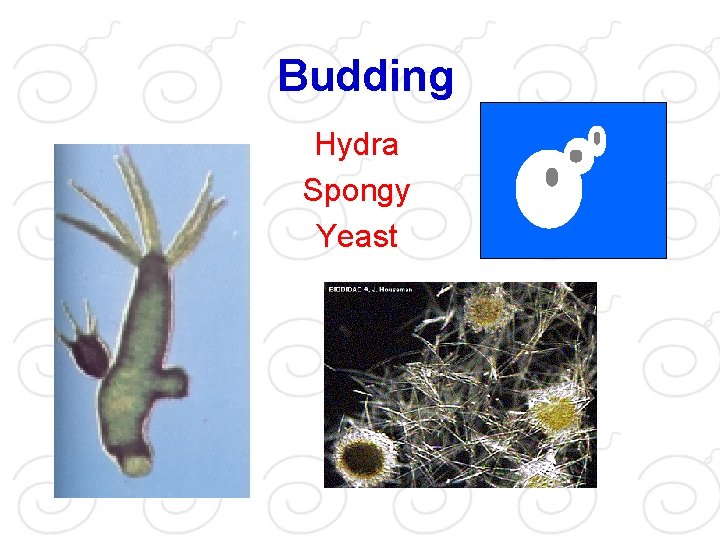
Budding Hydra Spongy Yeast

Spore formation Fungi Spore formed at sporangium
Vegetative propagation Stem tuber Corm Bulb Artificial propagation
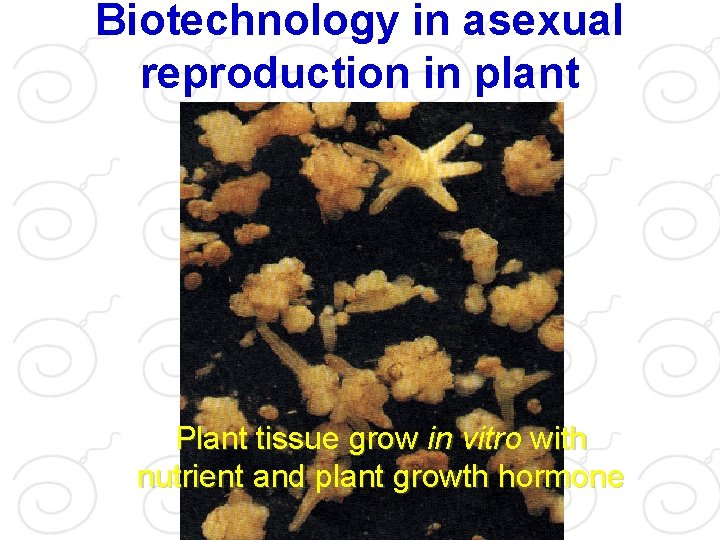
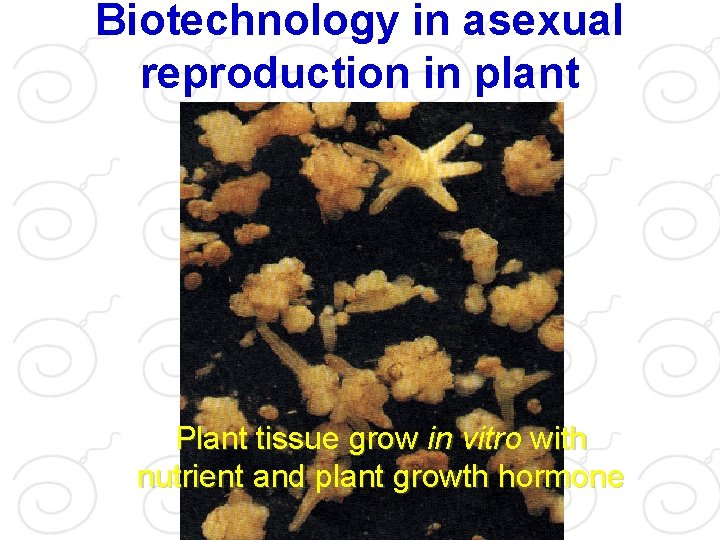
Biotechnology in asexual reproduction in plant Plant tissue grow in vitro with nutrient and plant growth hormone
Animal Reproduction
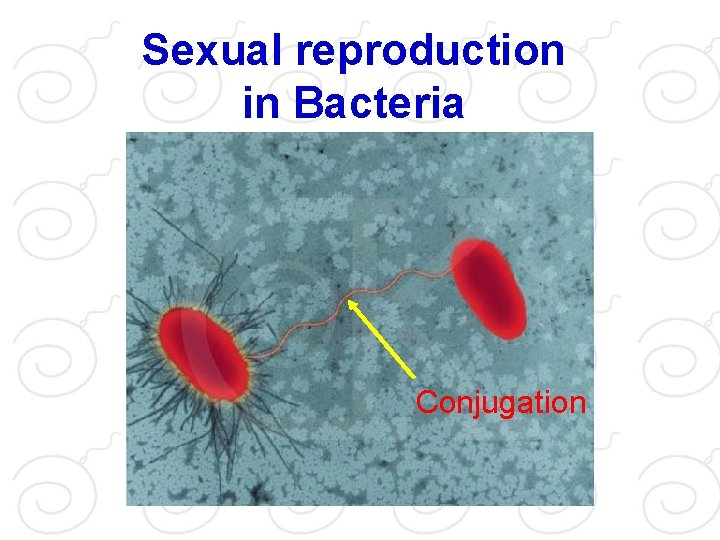
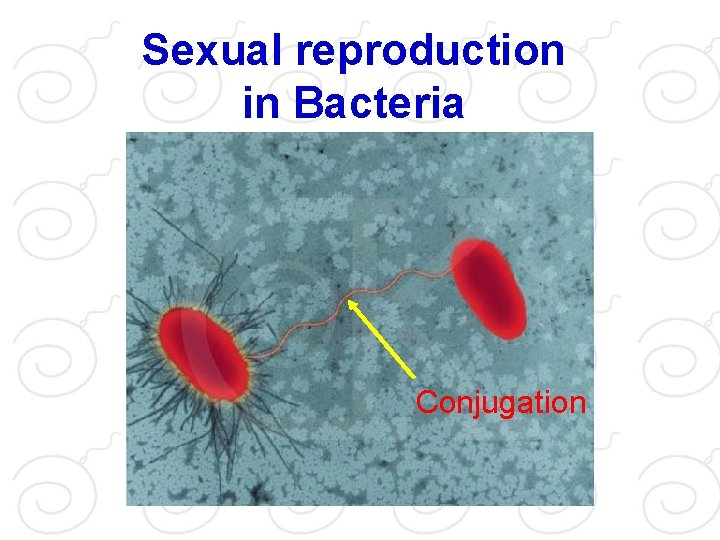
Sexual reproduction in Bacteria Conjugation
Human reproduction Male sex organ Embryo develop Female sex organ Hormonal control Fertilization Birth control
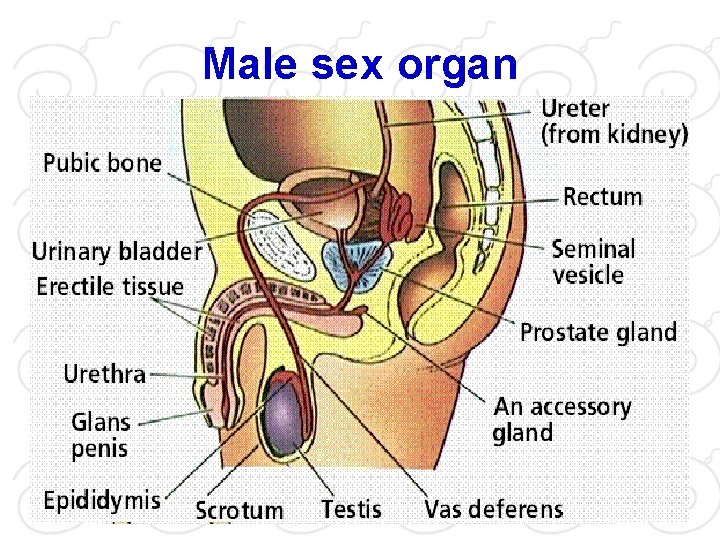
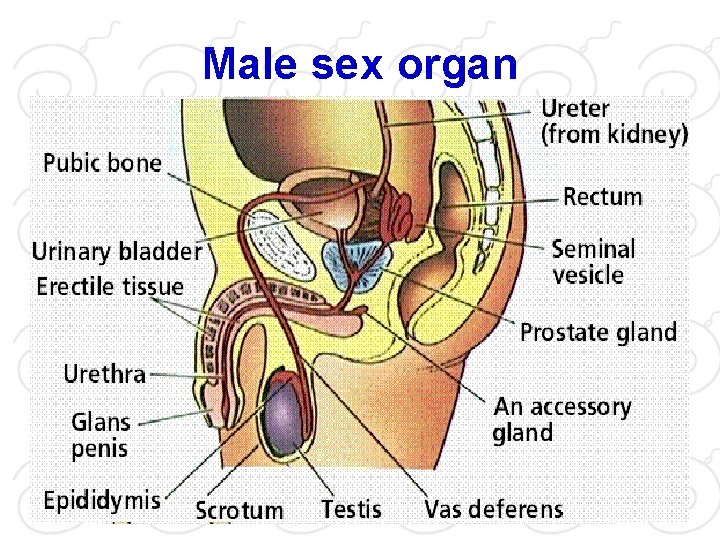
Male sex organ
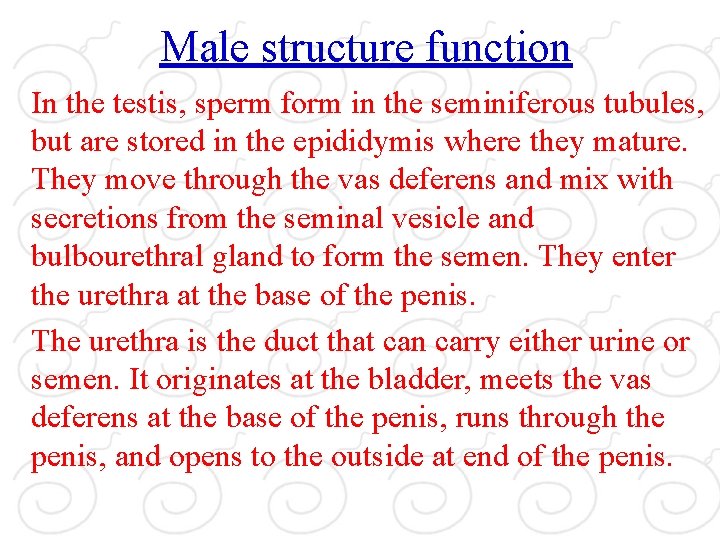
Male structure function In the testis, sperm form in the seminiferous tubules, but are stored in the epididymis where they mature. They move through the vas deferens and mix with secretions from the seminal vesicle and bulbourethral gland to form the semen. They enter the urethra at the base of the penis. The urethra is the duct that can carry either urine or semen. It originates at the bladder, meets the vas deferens at the base of the penis, runs through the penis, and opens to the outside at end of the penis.
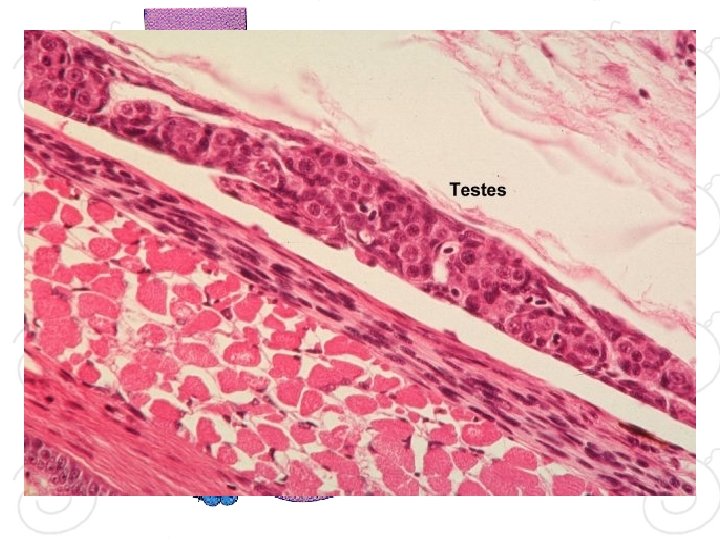
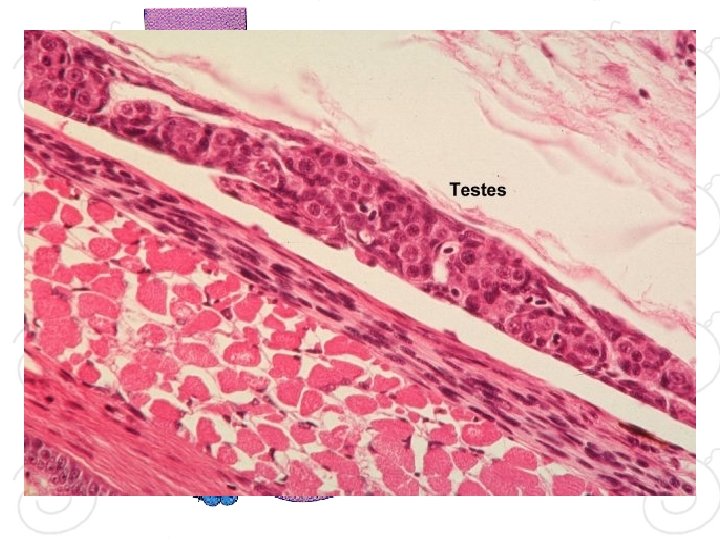
Testis
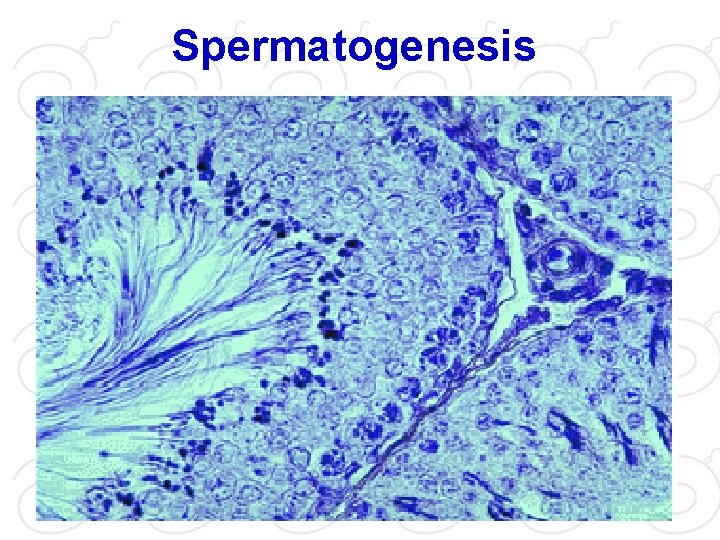
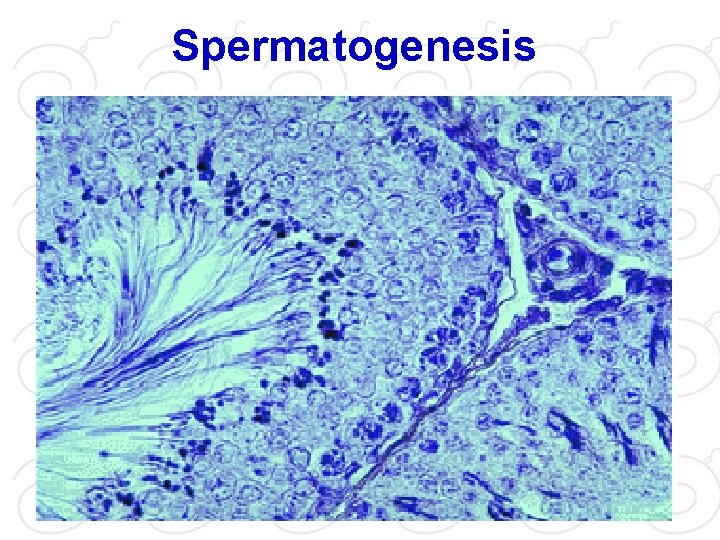
Spermatogenesis
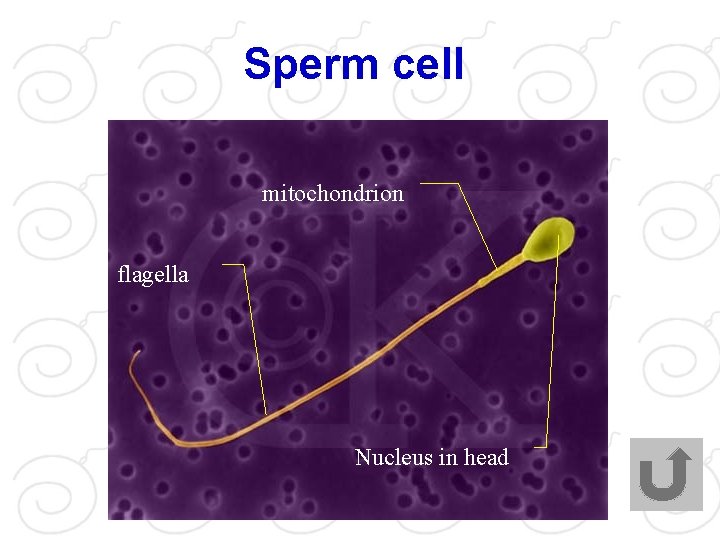
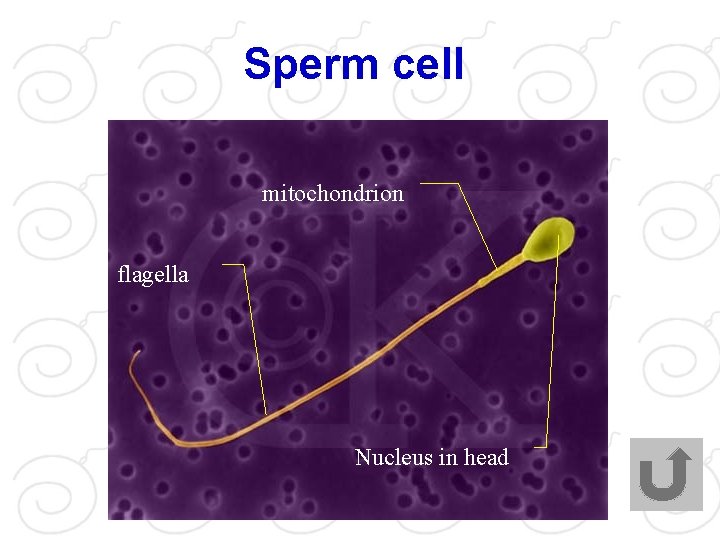
Sperm cell mitochondrion flagella Nucleus in head
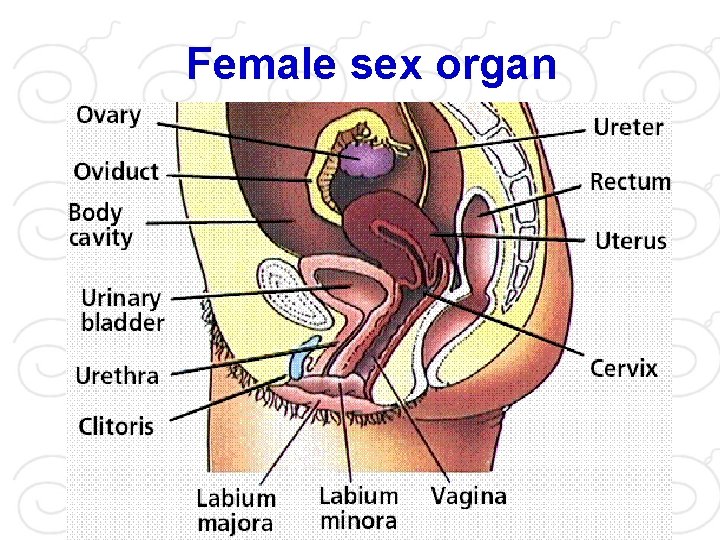
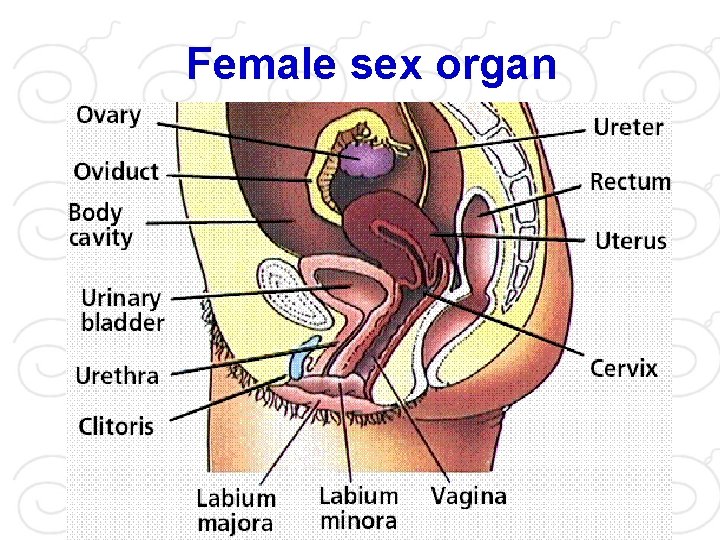
Female sex organ
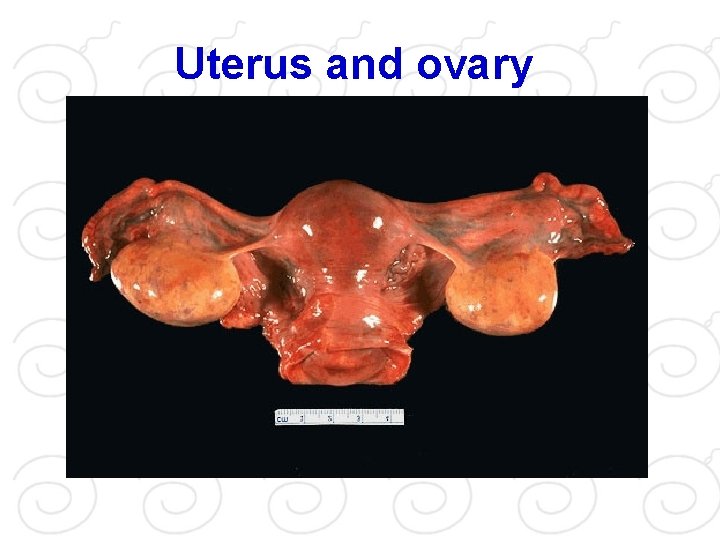
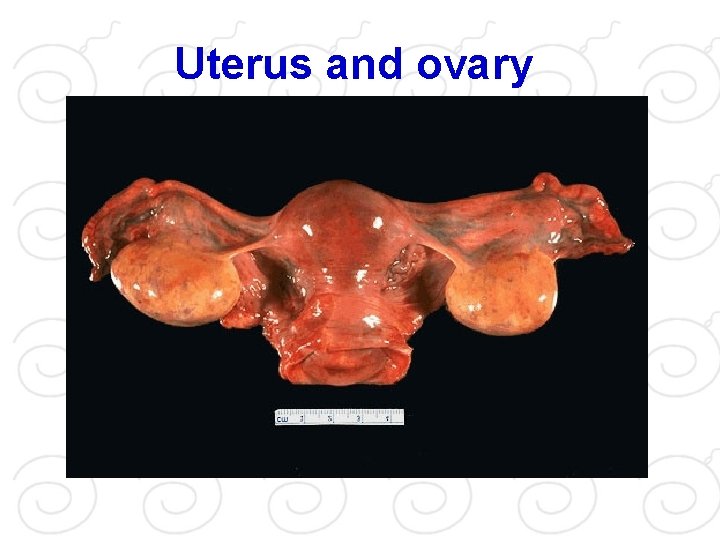
Uterus and ovary
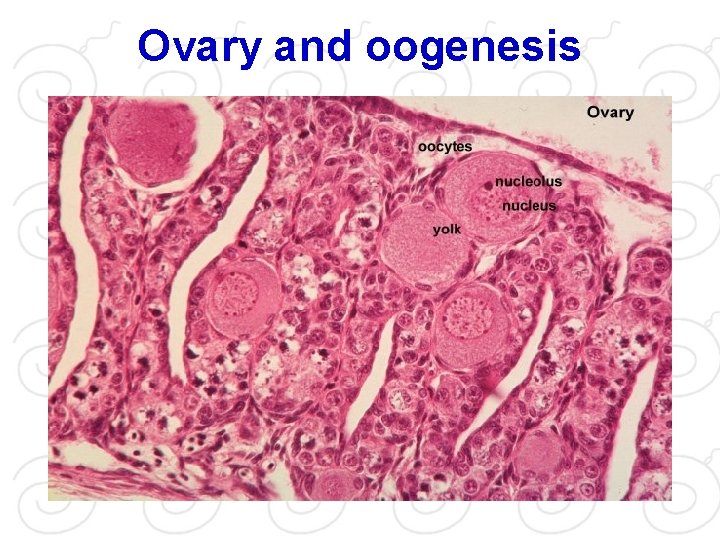
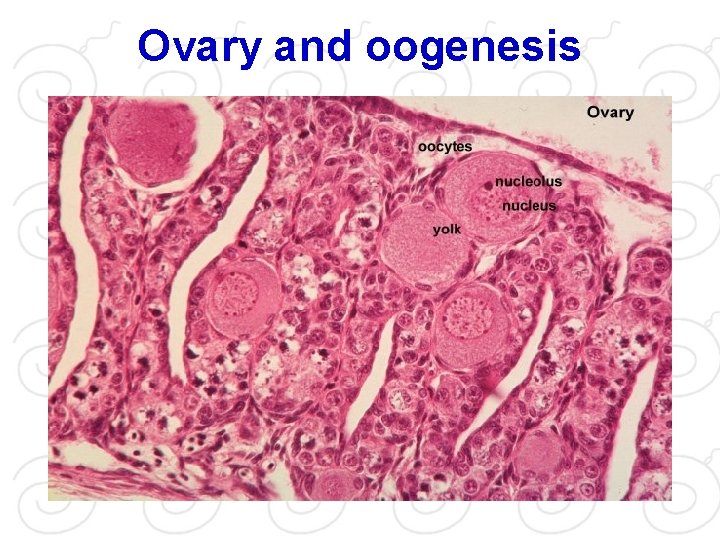
Ovary and oogenesis
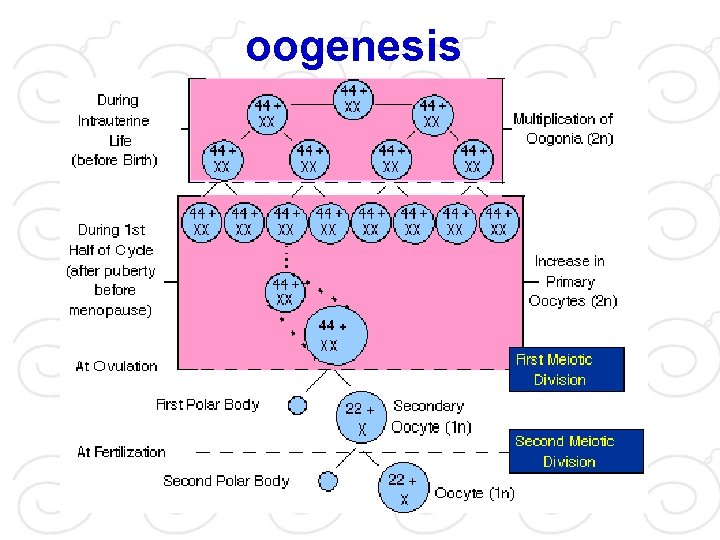
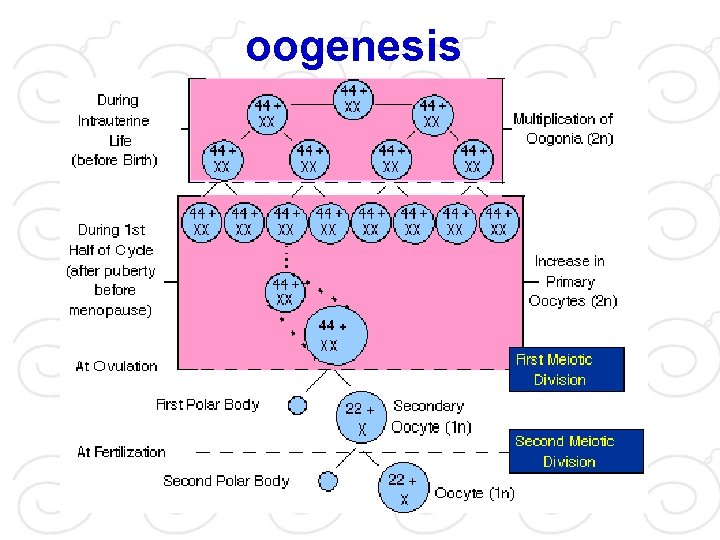
oogenesis
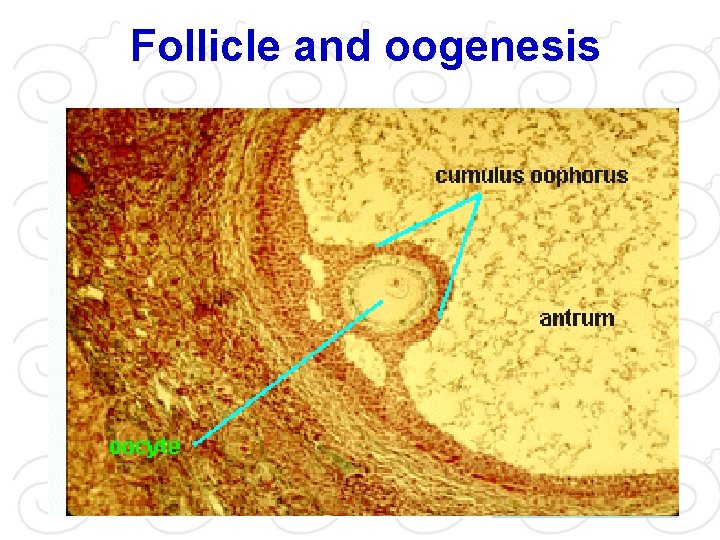
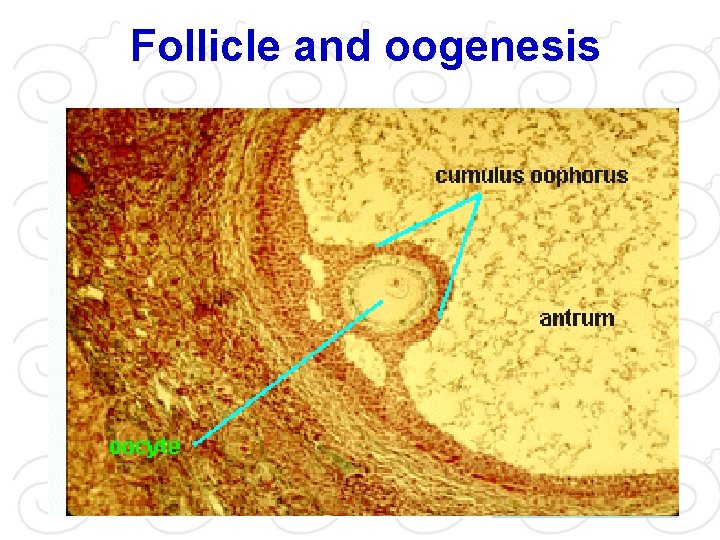
Follicle and oogenesis
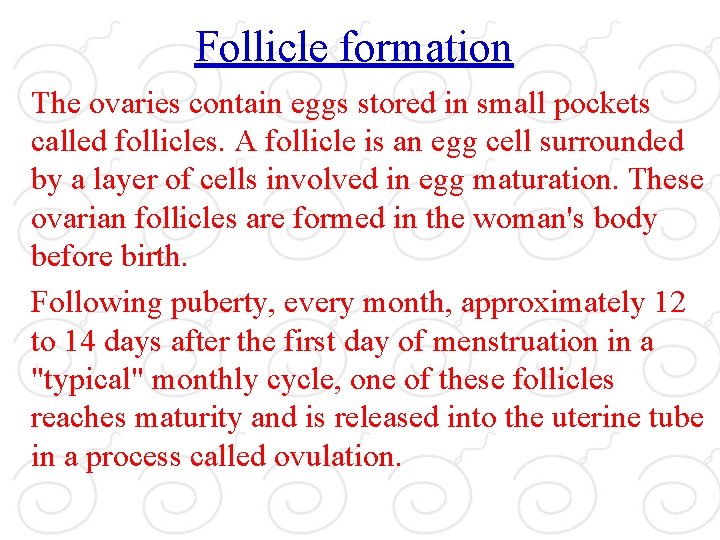
Follicle formation The ovaries contain eggs stored in small pockets called follicles. A follicle is an egg cell surrounded by a layer of cells involved in egg maturation. These ovarian follicles are formed in the woman's body before birth. Following puberty, every month, approximately 12 to 14 days after the first day of menstruation in a "typical" monthly cycle, one of these follicles reaches maturity and is released into the uterine tube in a process called ovulation.
Oocyte
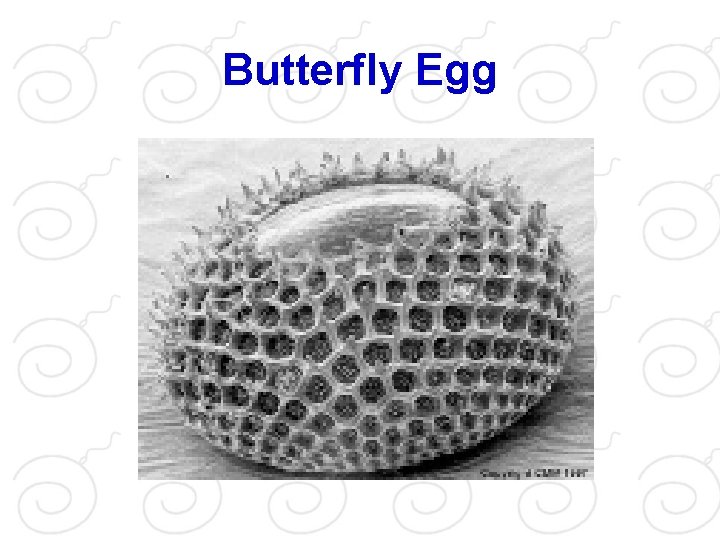
Butterfly Egg
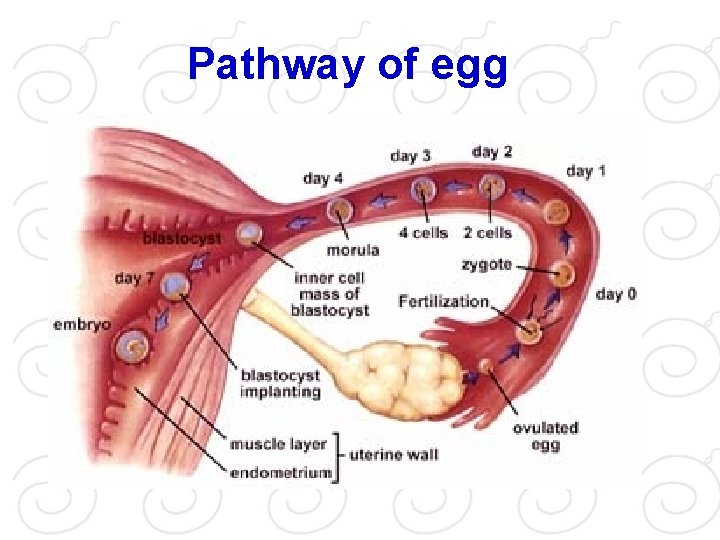
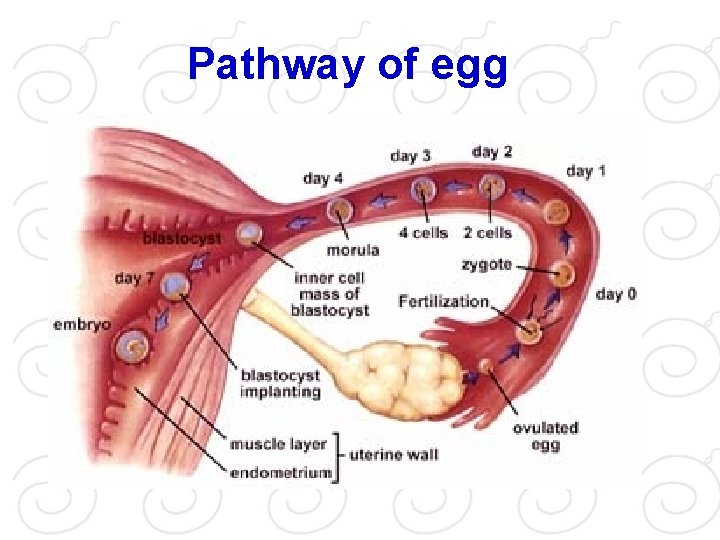
Pathway of egg
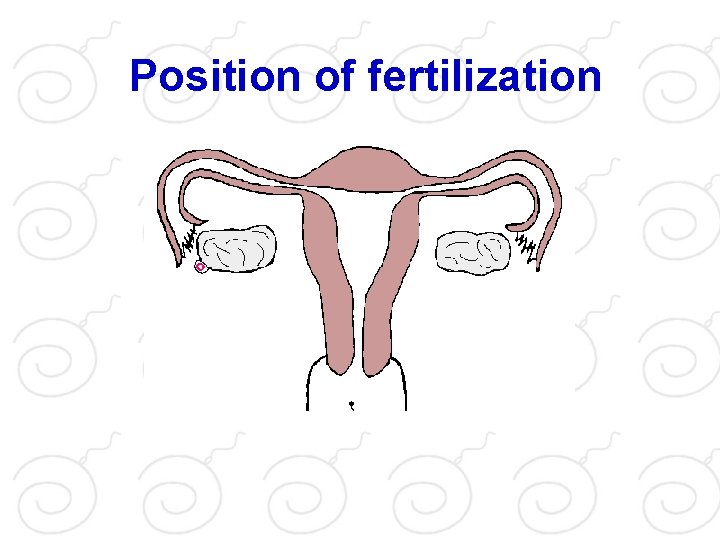
Egg travel At ovulation, a mature egg is released from one of the ovaries into the body cavity. Before it has a chance of getting lost it is captured by one of the paired tubes called Fallopian tubes or oviducts. In the Fallopiian tube, the egg is slowly propelled toward the uterus. If sperm are present in the female reproductive system, one of the sperm will penetrate the egg, normally while it is still in the upper third of the Fallopian tube.
Fertilization
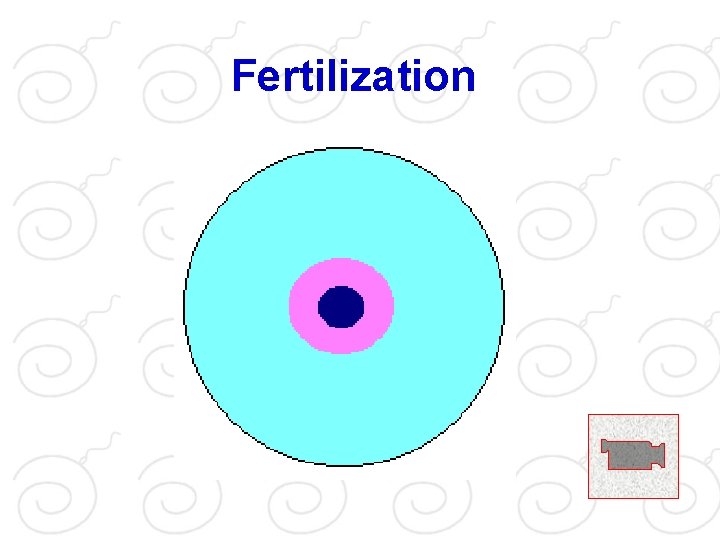
Sperm journey through female reproductive system It is possible to fertilize an egg with a sperm ejaculated into the vagina up to 3 days prior to ovulation. Sperm will have reached the uterus through the cervix. From there a few hundred of the original hundreds of millions sperm will have traveled up into the Fallopian tubes in search of an egg to fertilize. It is in the upper third of the Fallopian tubes that fertilization most commonly occurs.
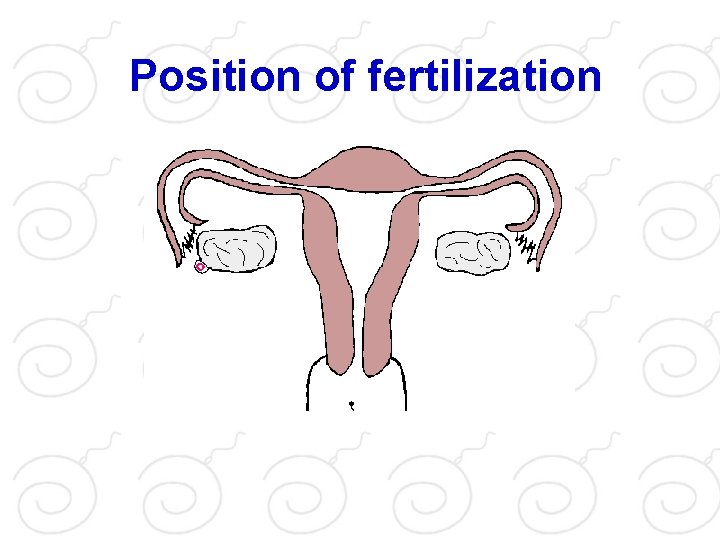
Position of fertilization
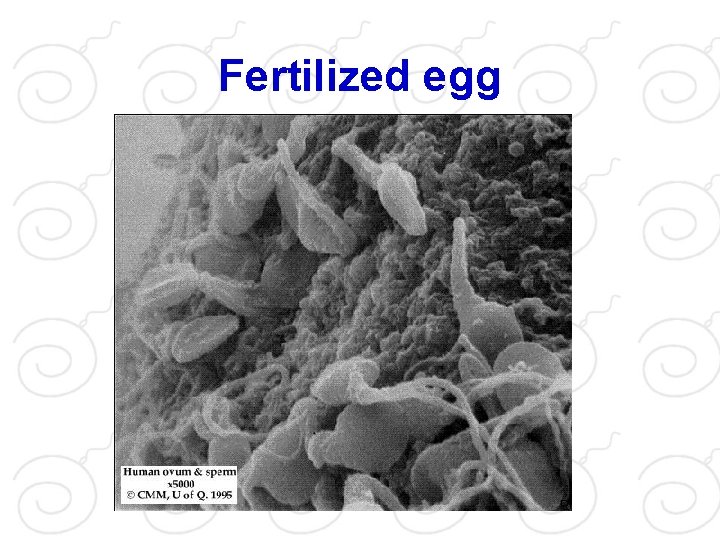
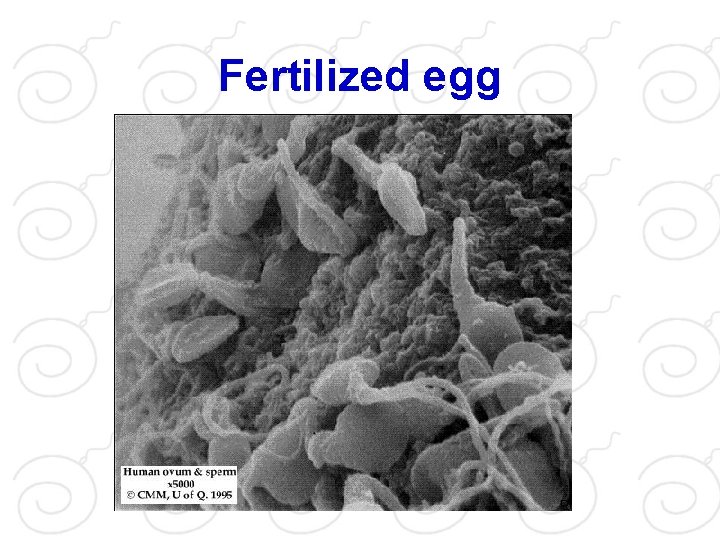
Fertilized egg
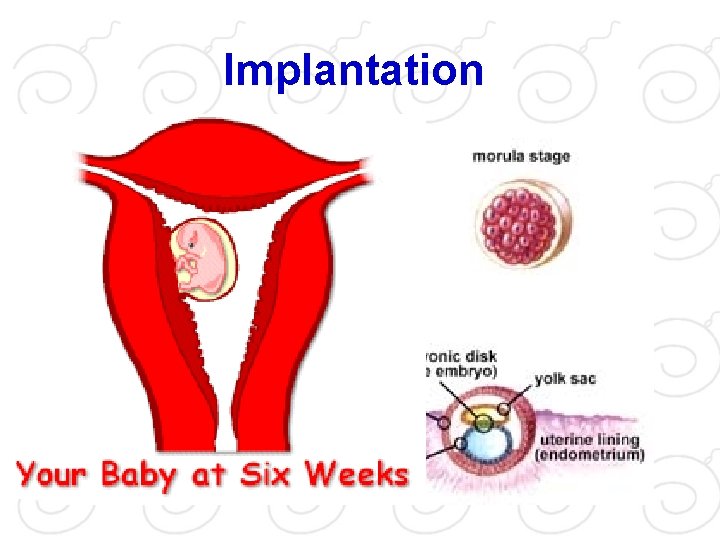
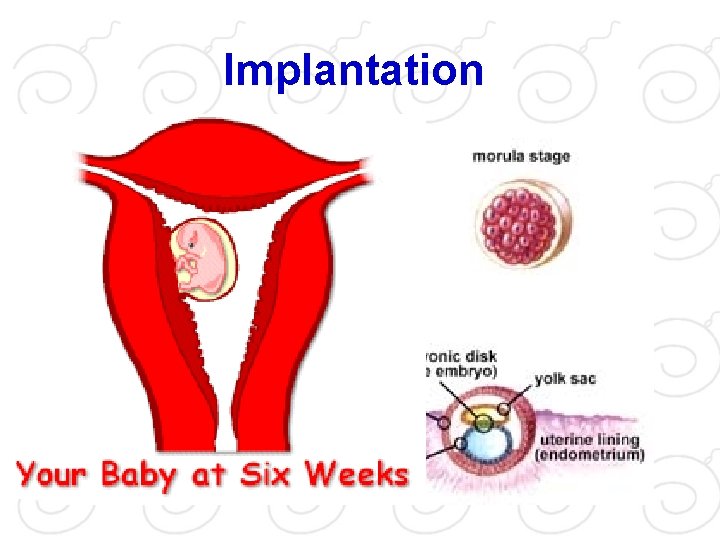
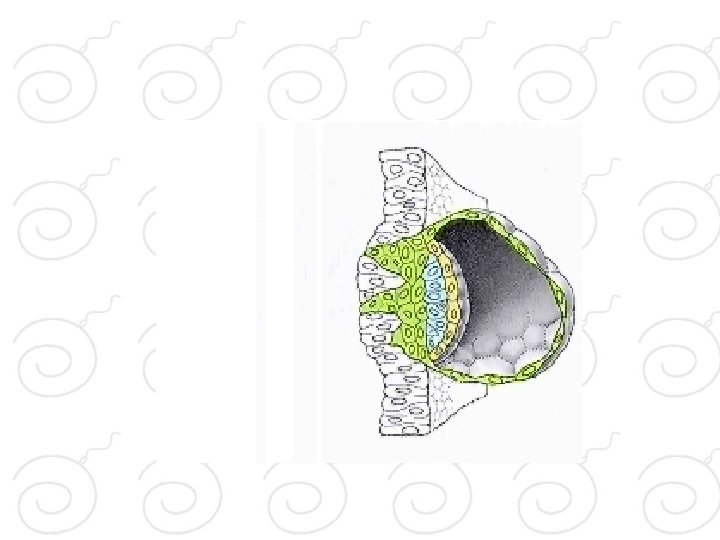
Implantation
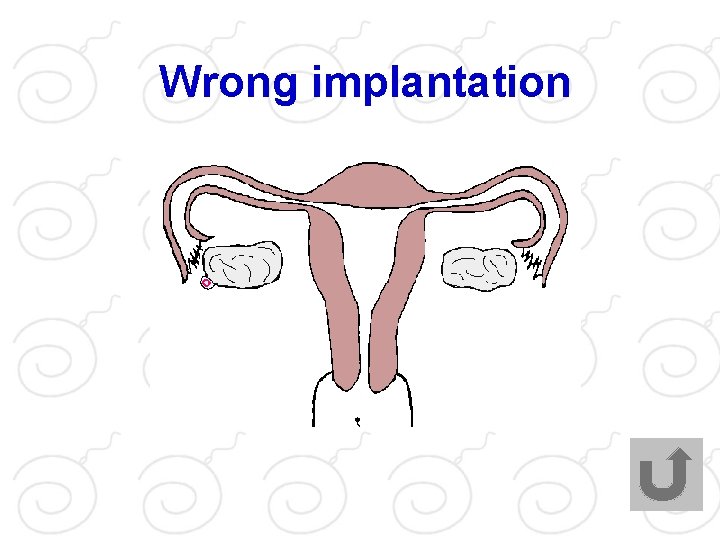
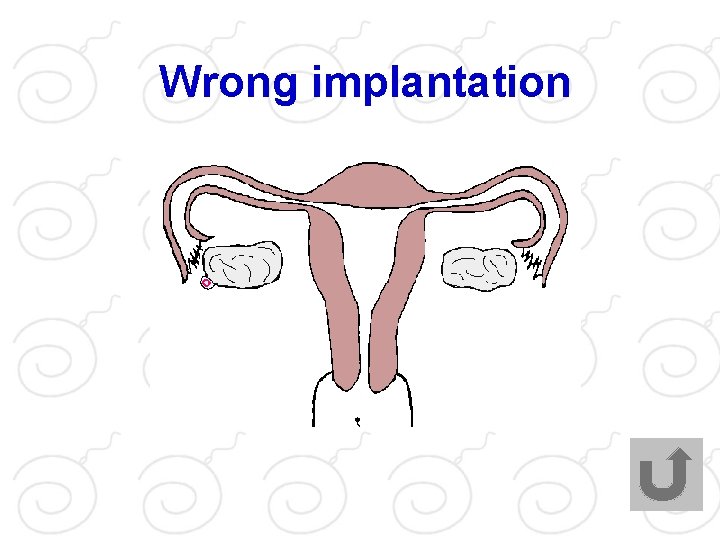
Wrong implantation
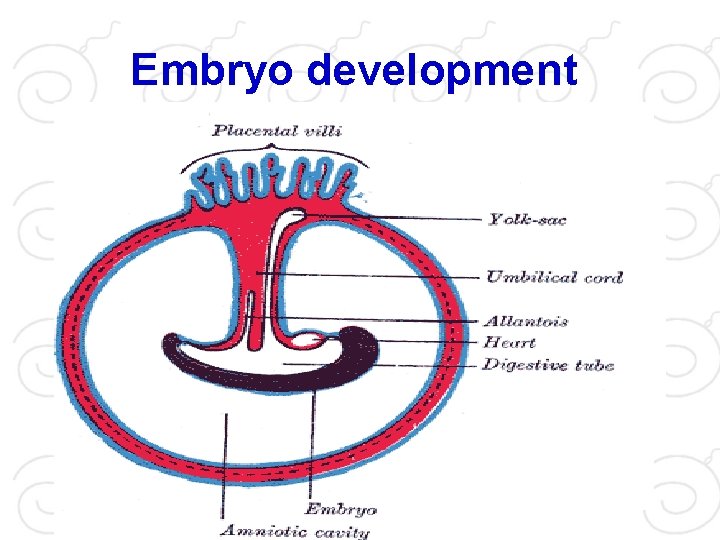
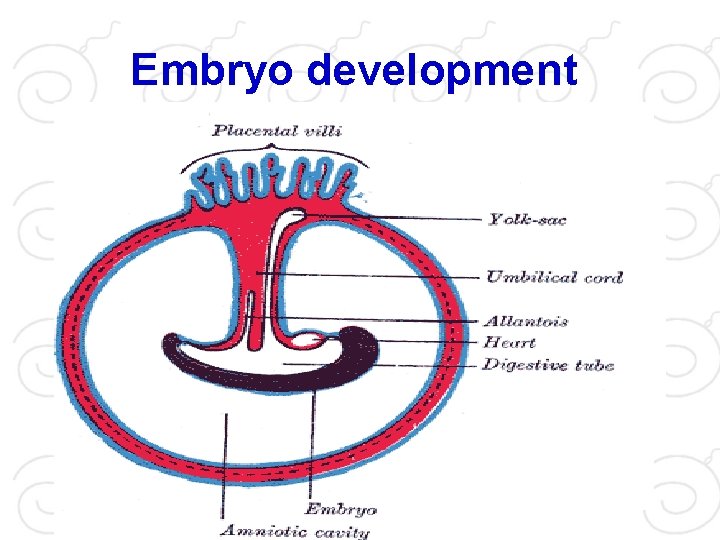
Embryo development
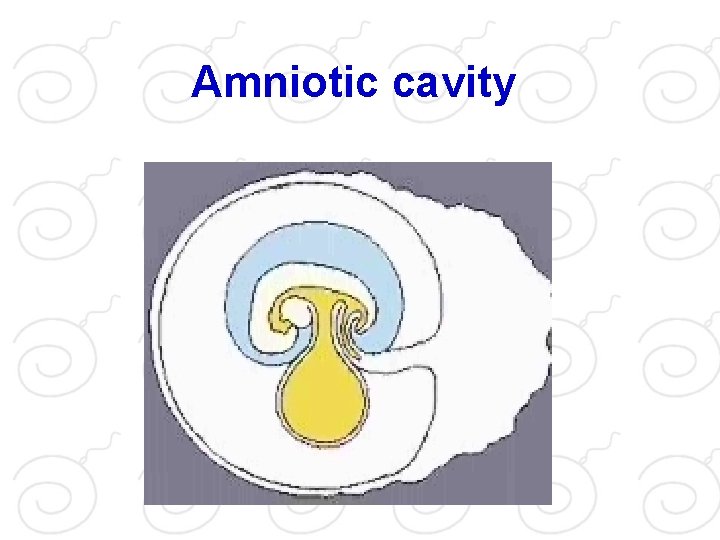
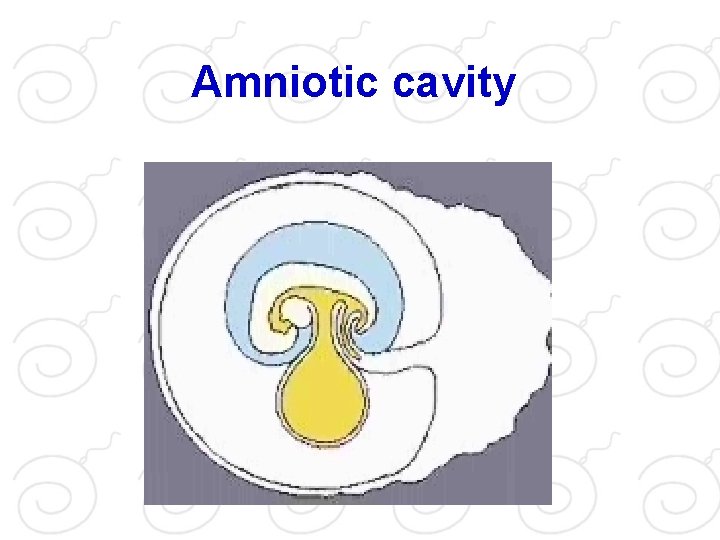
Amniotic cavity
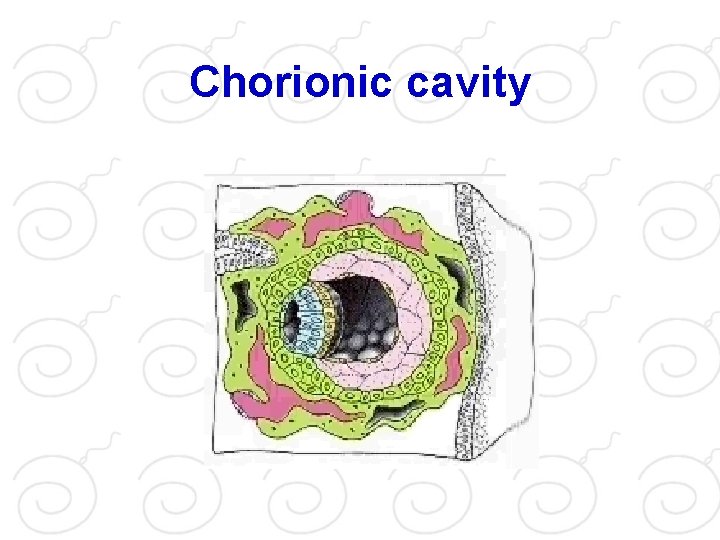
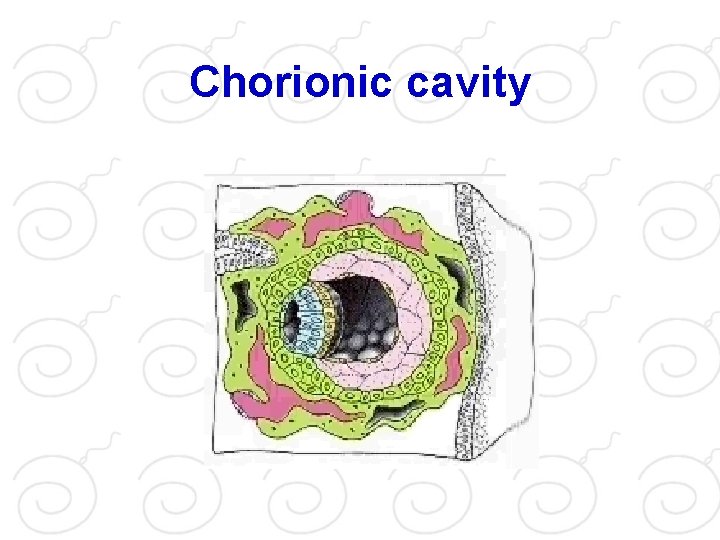
Chorionic cavity
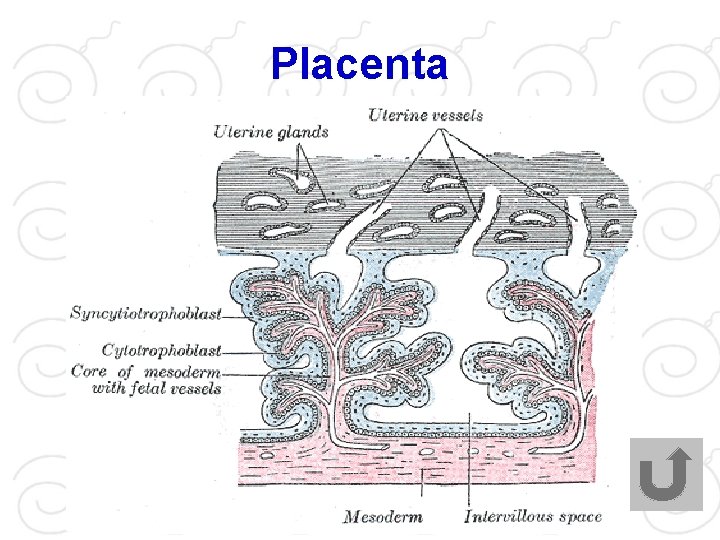
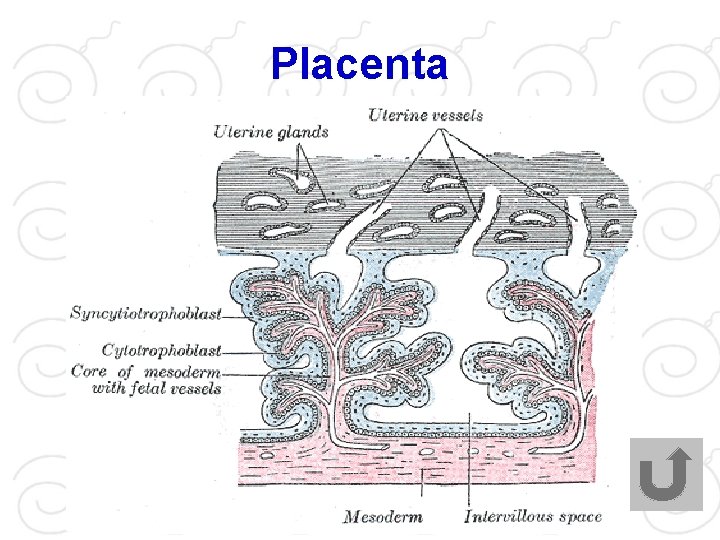
Placenta
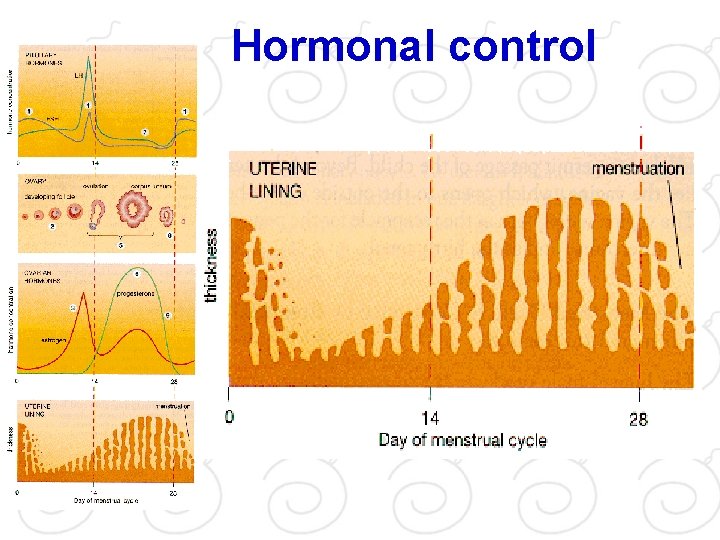
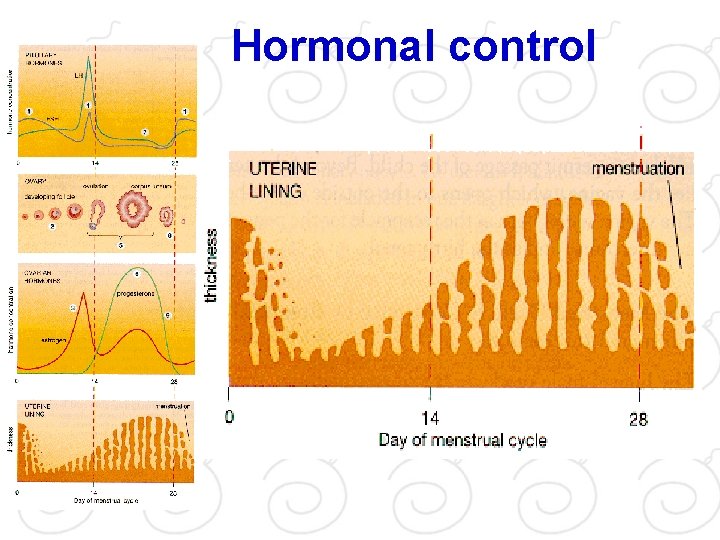
Hormonal control
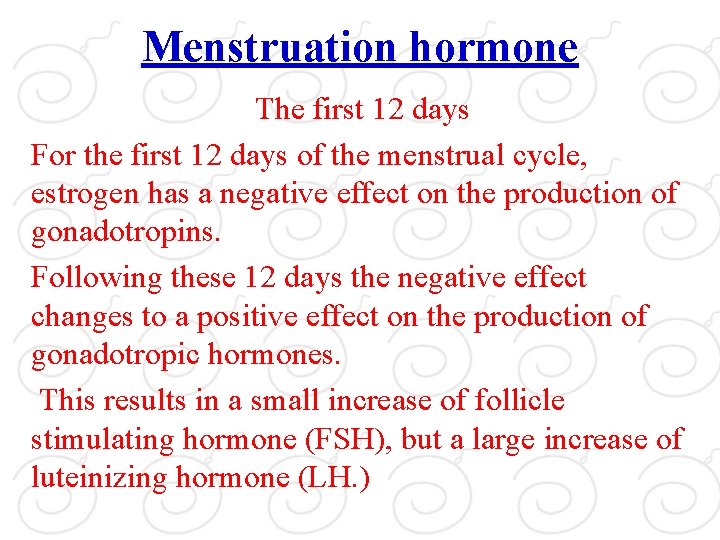
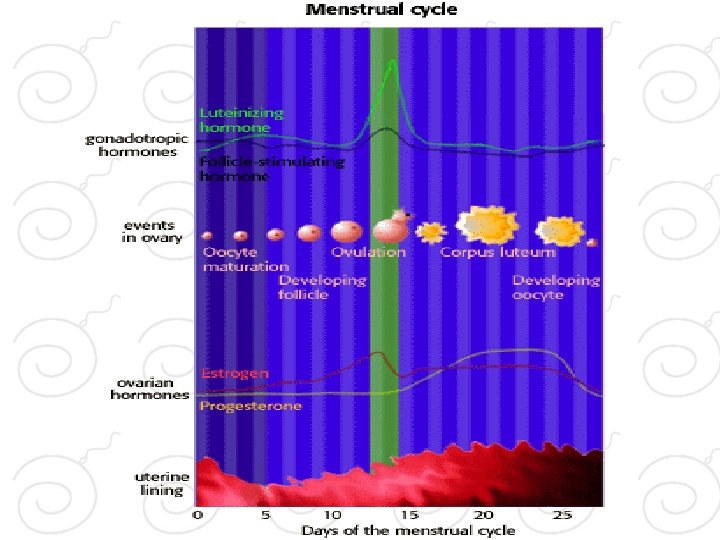
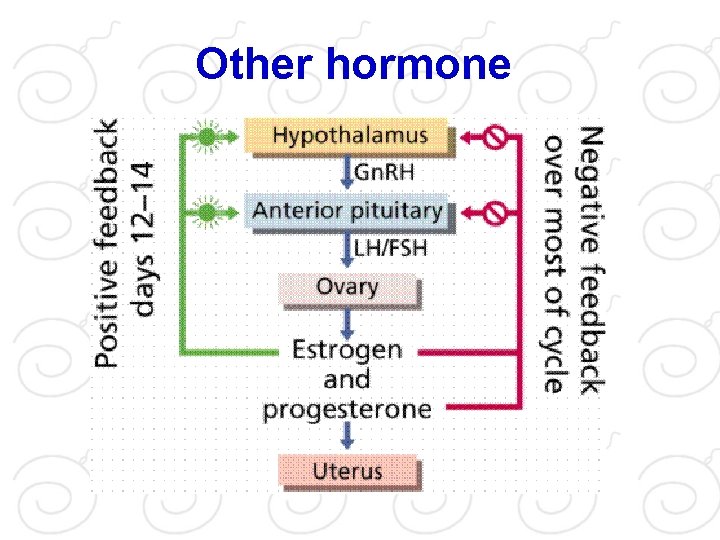
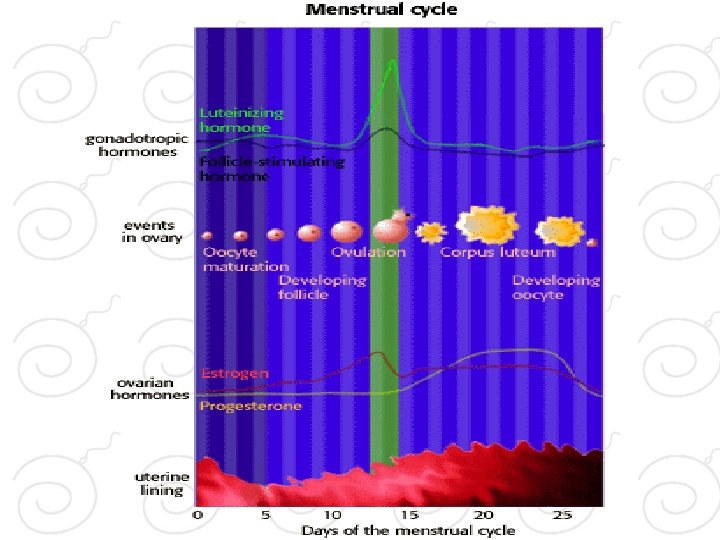
Menstruation hormone The first 12 days For the first 12 days of the menstrual cycle, estrogen has a negative effect on the production of gonadotropins. Following these 12 days the negative effect changes to a positive effect on the production of gonadotropic hormones. This results in a small increase of follicle stimulating hormone (FSH), but a large increase of luteinizing hormone (LH. )
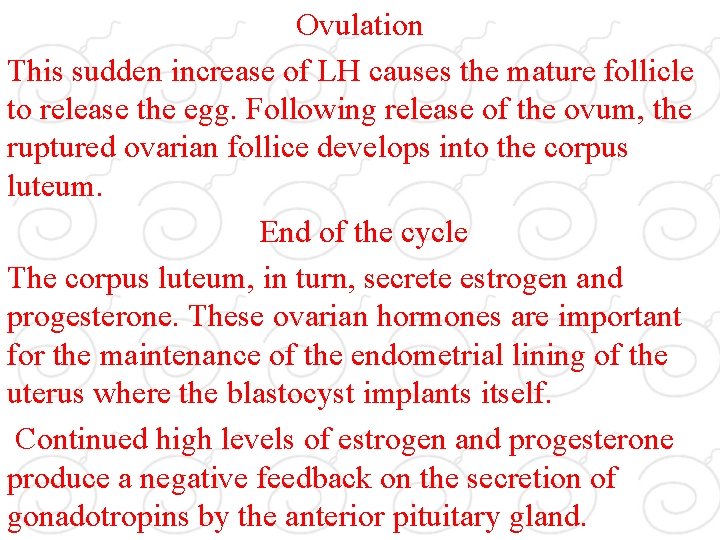
Ovulation This sudden increase of LH causes the mature follicle to release the egg. Following release of the ovum, the ruptured ovarian follice develops into the corpus luteum. End of the cycle The corpus luteum, in turn, secrete estrogen and progesterone. These ovarian hormones are important for the maintenance of the endometrial lining of the uterus where the blastocyst implants itself. Continued high levels of estrogen and progesterone produce a negative feedback on the secretion of gonadotropins by the anterior pituitary gland.
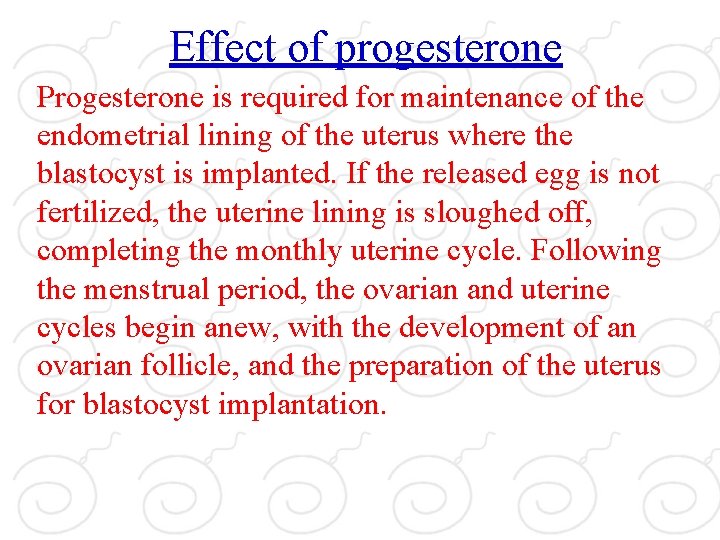
Effect of progesterone Progesterone is required for maintenance of the endometrial lining of the uterus where the blastocyst is implanted. If the released egg is not fertilized, the uterine lining is sloughed off, completing the monthly uterine cycle. Following the menstrual period, the ovarian and uterine cycles begin anew, with the development of an ovarian follicle, and the preparation of the uterus for blastocyst implantation.
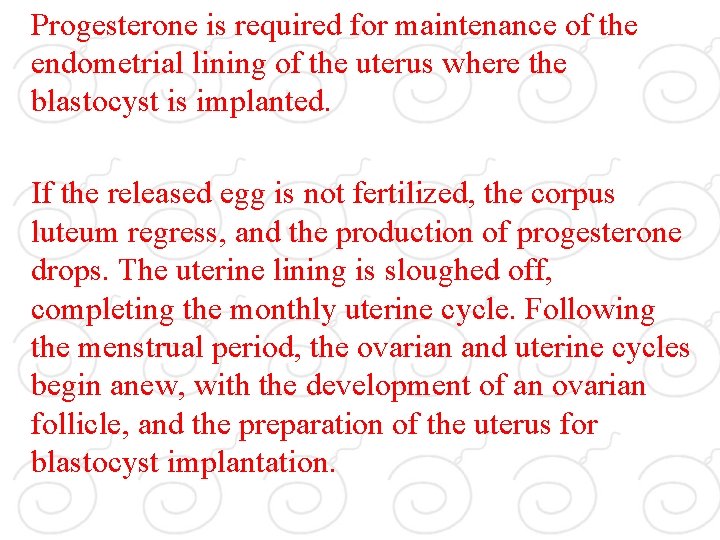
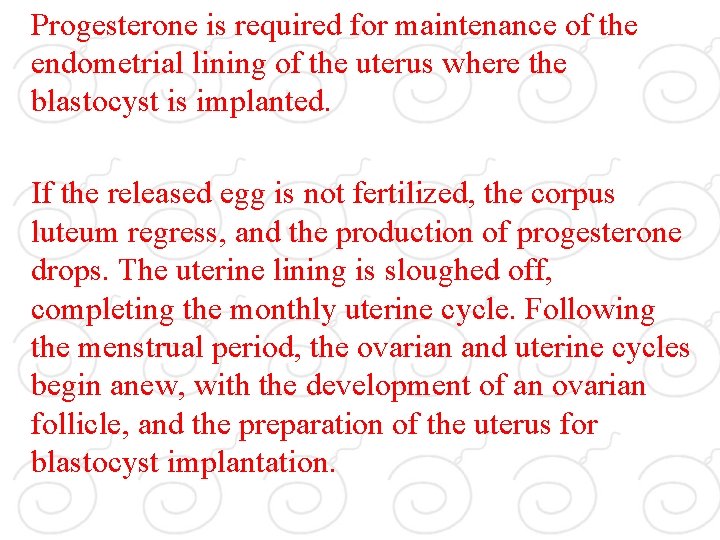
Progesterone is required for maintenance of the endometrial lining of the uterus where the blastocyst is implanted. If the released egg is not fertilized, the corpus luteum regress, and the production of progesterone drops. The uterine lining is sloughed off, completing the monthly uterine cycle. Following the menstrual period, the ovarian and uterine cycles begin anew, with the development of an ovarian follicle, and the preparation of the uterus for blastocyst implantation.
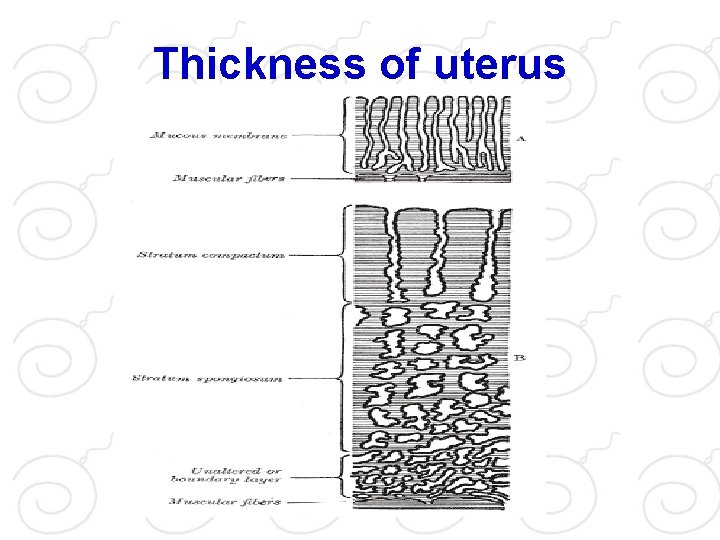
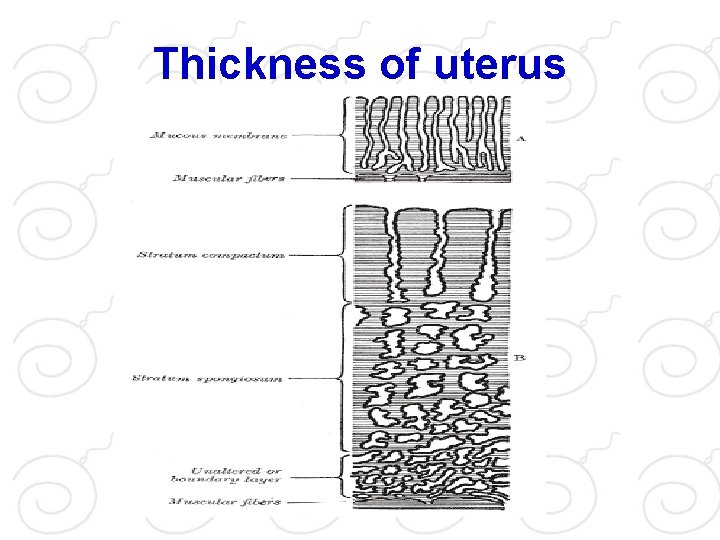
Thickness of uterus
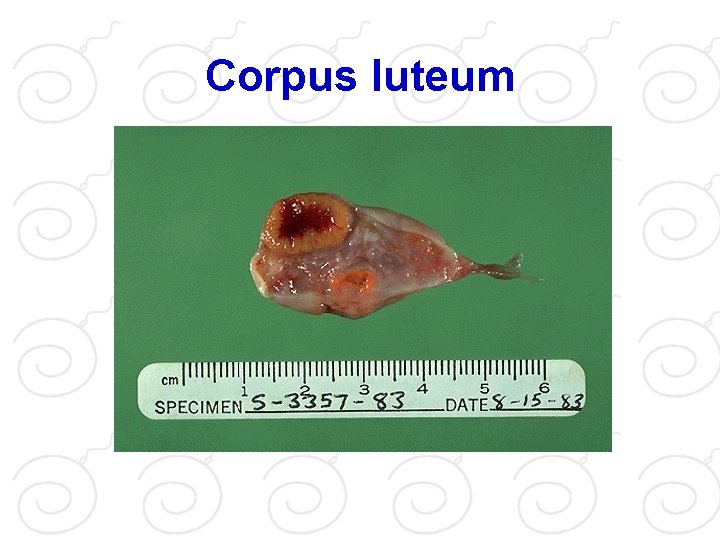
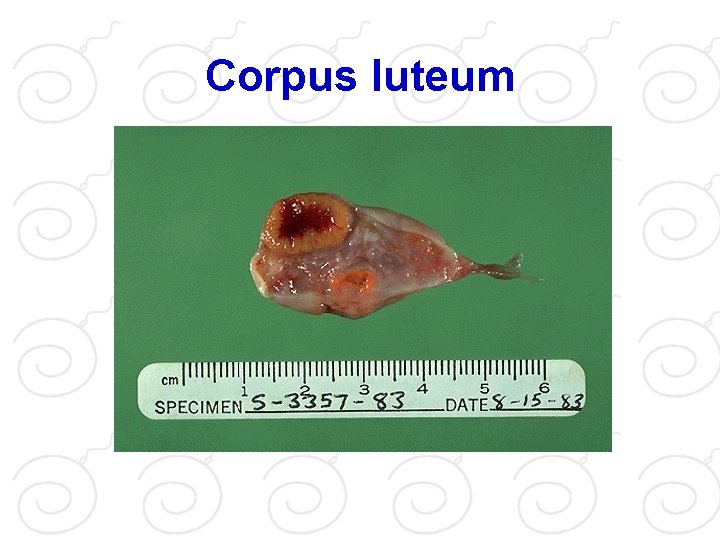
Corpus luteum
Ovarian follicles following ovulation After ovulation, changes continue to take place in the ovaries. The remaining follicular cells undergo structural and biochemical changes. They develop into the corpus luteum. While the ovarian follicles produced estrogen, the corpus luteum produce both estrogen and progesterone. After ovulation, the ruptured ovarial follicle becomes the corpus luteum. While the ovarian follicles produced estrogen, the corpus luteum produce both estrogen and progesterone.
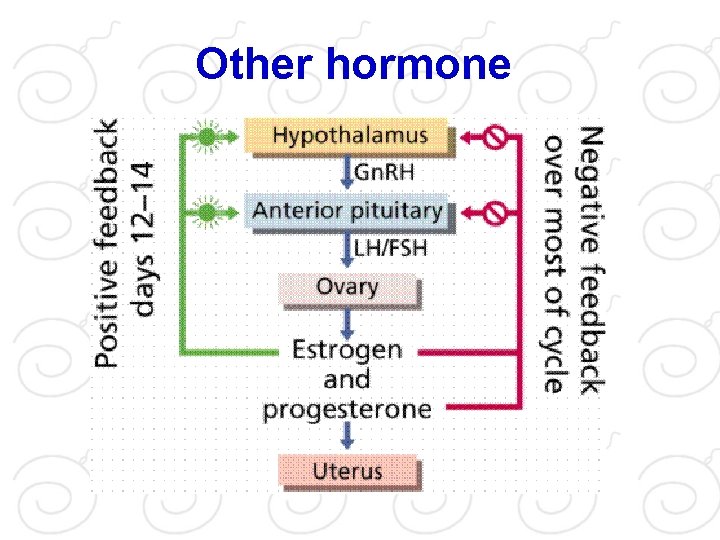
Other hormone
Hormone With the onset of puberty, the hypothalamus increases the release of gonadotropin releasing hormone (Gn. RH). This hormone is needed for sexual maturity and normal reproduction. Gn. RH stimulates the anterior pituitary gland to release several hormones. Among them are the gonadotropings "follicle stimulating hormone" (FSH) and "lutenizing hormone" (LH. ) These gonadotropins act by stimulating the production of sex hormones in the gonads (testes and ovary. )
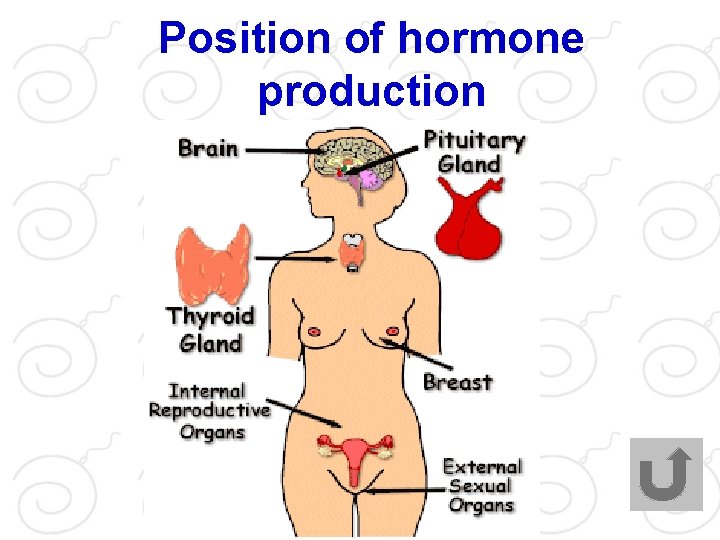
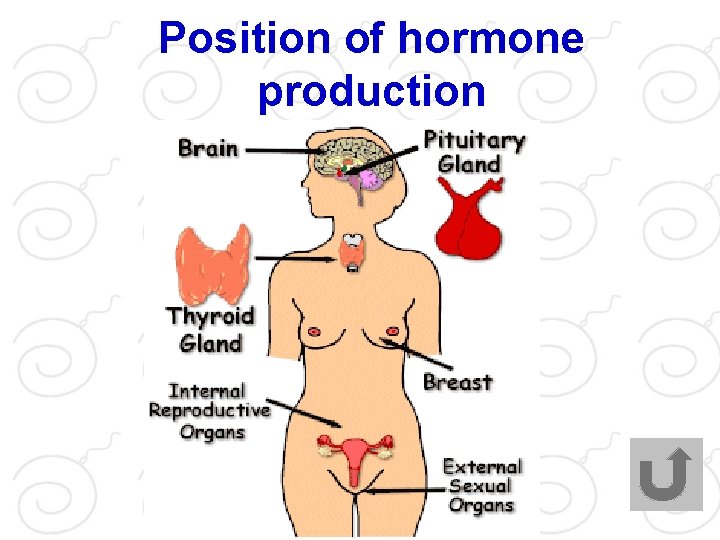
Position of hormone production
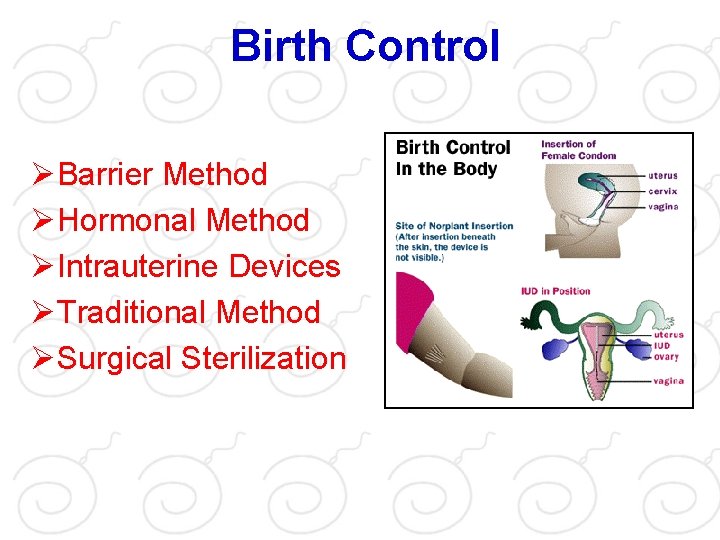
Birth Control ØBarrier Method ØHormonal Method ØIntrauterine Devices ØTraditional Method ØSurgical Sterilization
Barrier Method • Male Condom • Female Condom • Diaphragm • Cervical cap • Sponge • Vaginal Spermicide
Male Condom. The male condom is a sheath placed over the erect penis before penetration, preventing pregnancy by blocking the passage of sperm
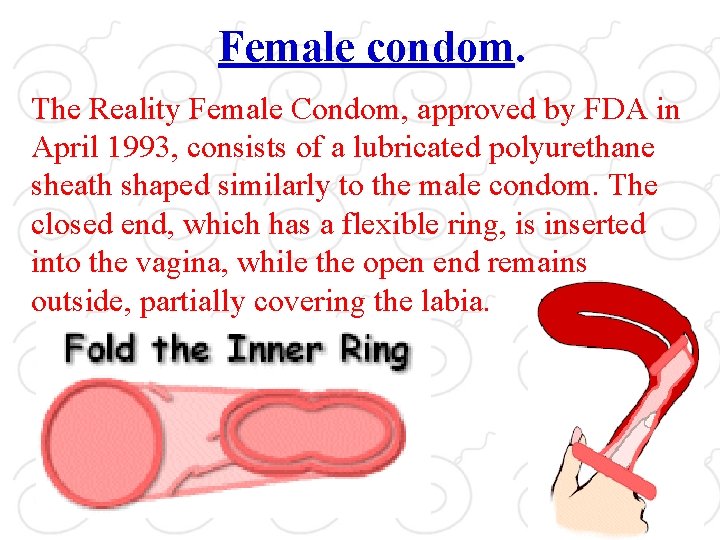
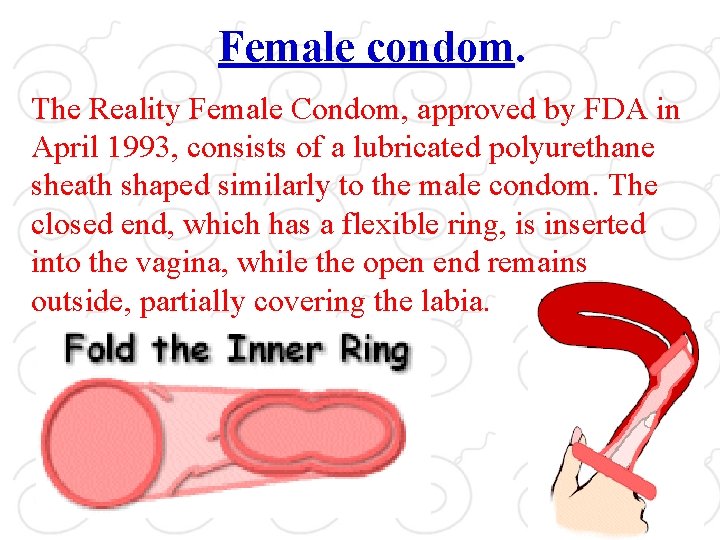
Female condom. The Reality Female Condom, approved by FDA in April 1993, consists of a lubricated polyurethane sheath shaped similarly to the male condom. The closed end, which has a flexible ring, is inserted into the vagina, while the open end remains outside, partially covering the labia.
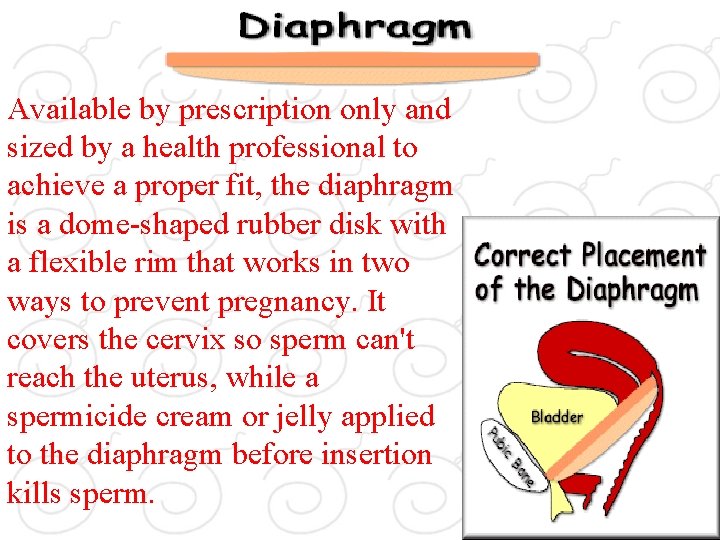
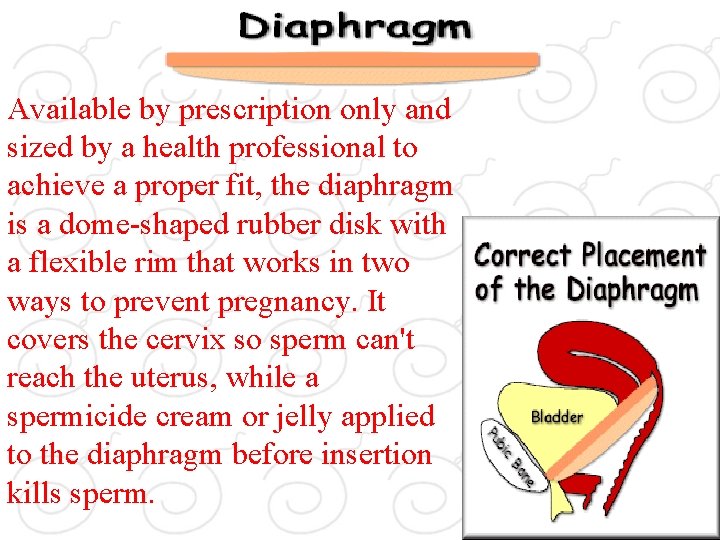
Available by prescription only and sized by a health professional to achieve a proper fit, the diaphragm is a dome-shaped rubber disk with a flexible rim that works in two ways to prevent pregnancy. It covers the cervix so sperm can't reach the uterus, while a spermicide cream or jelly applied to the diaphragm before insertion kills sperm.
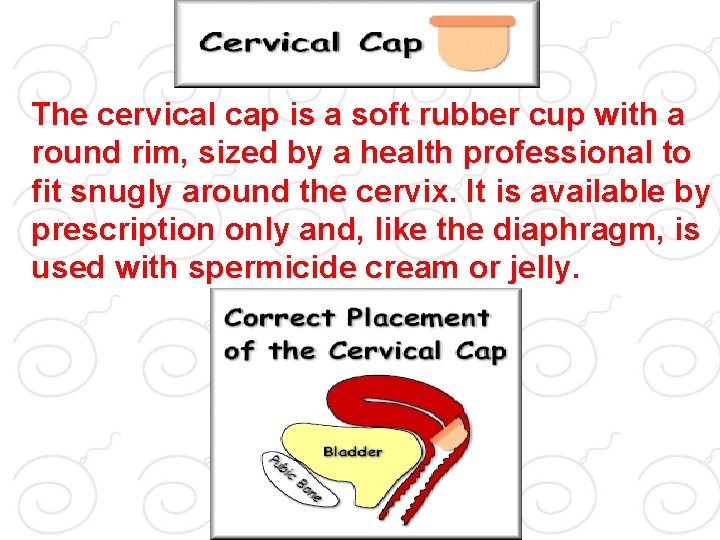
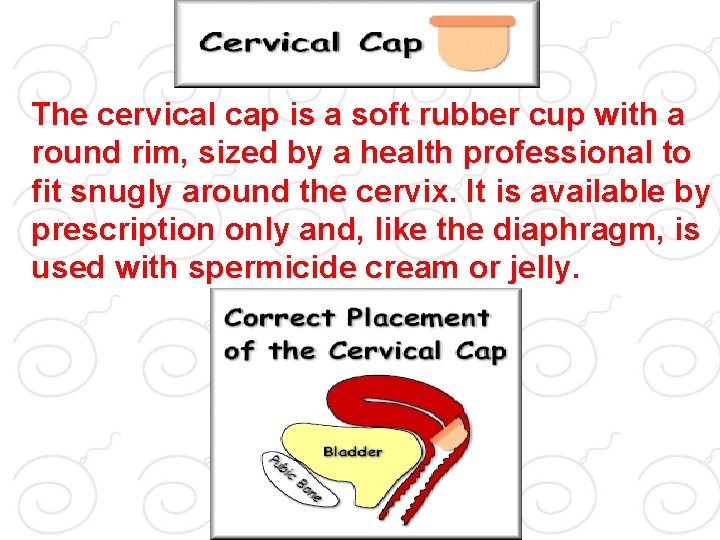
The cervical cap is a soft rubber cup with a round rim, sized by a health professional to fit snugly around the cervix. It is available by prescription only and, like the diaphragm, is used with spermicide cream or jelly.
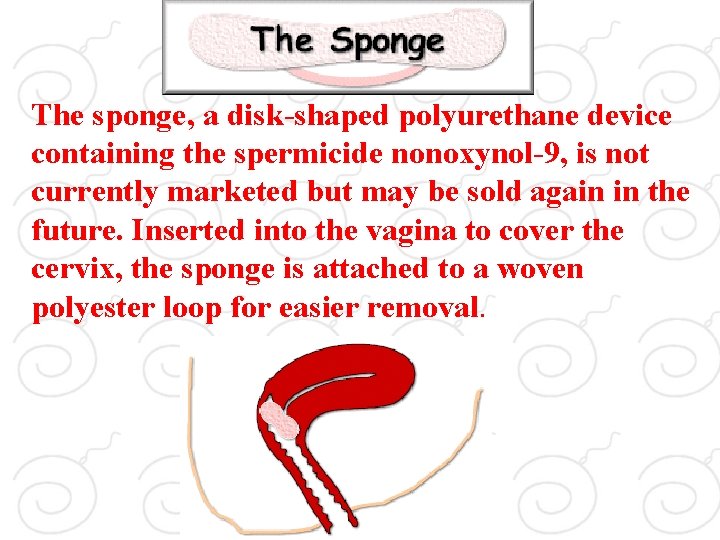
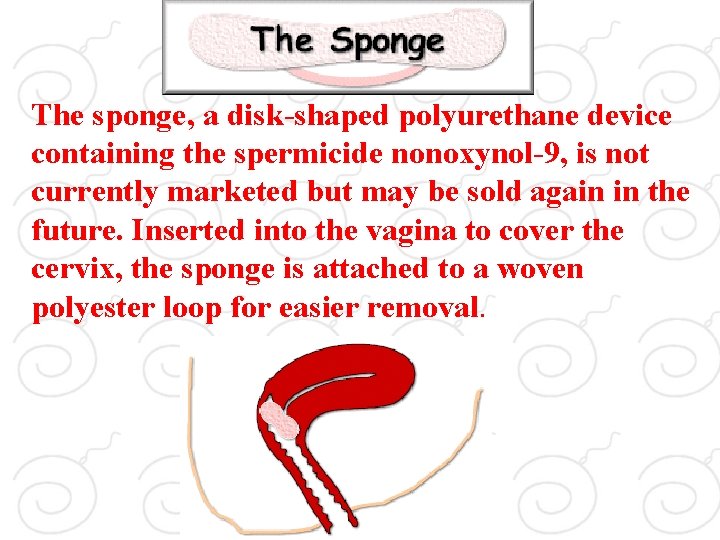
Sponge. The sponge, a disk-shaped polyurethane device containing the spermicide nonoxynol-9, is not currently marketed but may be sold again in the future. Inserted into the vagina to cover the cervix, the sponge is attached to a woven polyester loop for easier removal.
Vaginal Spermicides Alone Vaginal spermicides are available in foam, cream, jelly, film, suppository, or tablet forms. All types contain a sperm-killing chemical. Studies have not produced definitive data on how well spermicides alone prevent pregnancy, but according to the authors of Contraceptive Technology, a leading resource for contraceptive information, the failure rate for typical users may be 26 percent per year.
Hormonal Method • • • Oral contraceptive Minipills Emergency Contraceptive(Morning after) Injectable progestins Implantable progestins
Combined oral contraceptives. Typically called "the pill, " combined oral contraceptives have been on the market for 40 years and are the most popular form of reversible birth control in the United States. This form of birth control suppresses ovulation (the monthly release of an egg from the ovaries) by the combined actions of the hormones estrogen and progestin. Side effects of the pill, which often subside after a few months' use, include nausea, headache, breast tenderness, weight gain, irregular bleeding, and depression.
Minipills. Although taken daily like combined oral contraceptives, minipills contain only the hormone progestin and no estrogen. They work by reducing and thickening cervical mucus to prevent sperm from reaching the egg. They also keep the uterine lining from thickening, which prevents a fertilized egg from implanting in the uterus. These pills are slightly less effective than combined oral contraceptives. Side effects of minipills include menstrual cycle changes, weight gain, and breast tenderness.
Emergency Contraceptive ("Morning After Pill") Two emergency contraceptive pill products have been approved by FDA for use in preventing pregnancy after intercourse when standard contraceptives have failed or when no contraceptives were used at all. One product contains the hormones progestin and estrogen; the other contains just progestin. Side effects include nausea and vomiting, both of which were reported less frequently in women taking the progestin-only pills.
Injectable progestins is injected by a health professional into the buttocks or arm muscle every three months. Depo-Provera prevents pregnancy in three ways: It inhibits ovulation, changes the cervical mucus to help prevent sperm from reaching the egg, and changes the uterine lining to prevent the fertilized egg from implanting in the uterus.
Implantable progestins Made up of matchstick-sized rubber rods, this contraceptive is surgically implanted under the skin of the upper arm, where it steadily releases the contraceptive steroid levonorgestrel. The six-rod Norplant provides protection for up to five years
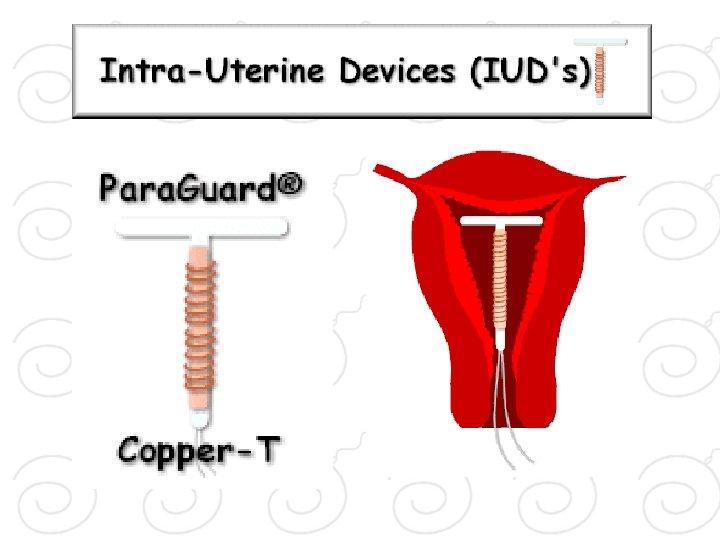
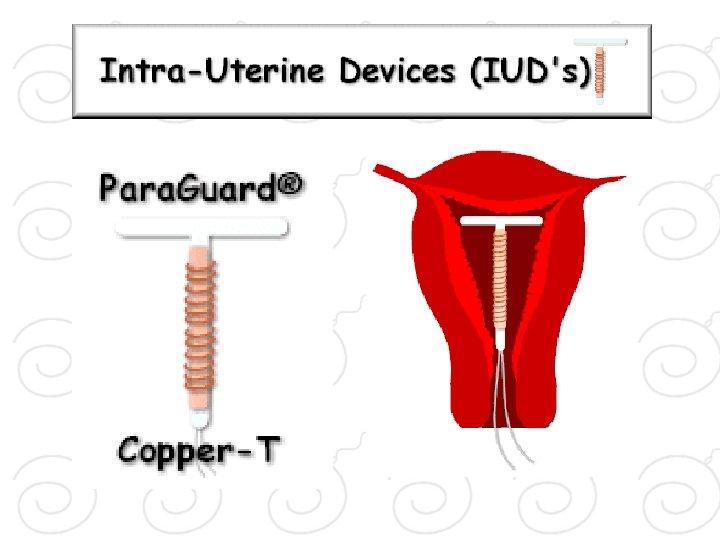
Intrauterine Devices An IUD is a mechanical device inserted into the uterus by a health-care professional. The Paragard IUD can remain in place for 10 years, while the Progestasert IUD must be replaced every year. It's not entirely clear how IUDs prevent pregnancy. They seem to prevent sperm and eggs from meeting by either immobilizing the sperm on their way to the fallopian tubes or changing the uterine lining so the fertilized egg cannot implant in it. Side effects can include pelvic inflammatory disease (an infection of a woman's reproductive organs), ectopic pregnancy (in which a fertilized egg implants in the fallopian tube instead of the uterus), perforation of the uterus, heavierthan-normal bleeding, and cramps. Complications occur most often during and immediately after insertion.
Traditional Method • Fertility awareness • Withdrawal
Fertility awareness. Also known as natural family planning or periodic abstinence, fertility awareness entails not having sexual intercourse or using a barrier method of birth control on the days of a woman's menstrual cycle when she is more likely to become pregnant.
Withdrawal. In this method, also called coitus interruptus, the man withdraws his penis from the vagina before ejaculation. Fertilization is prevented if the sperm don't enter the vagina.
Surgical Sterilization • Vasectomy • Tubal ligation
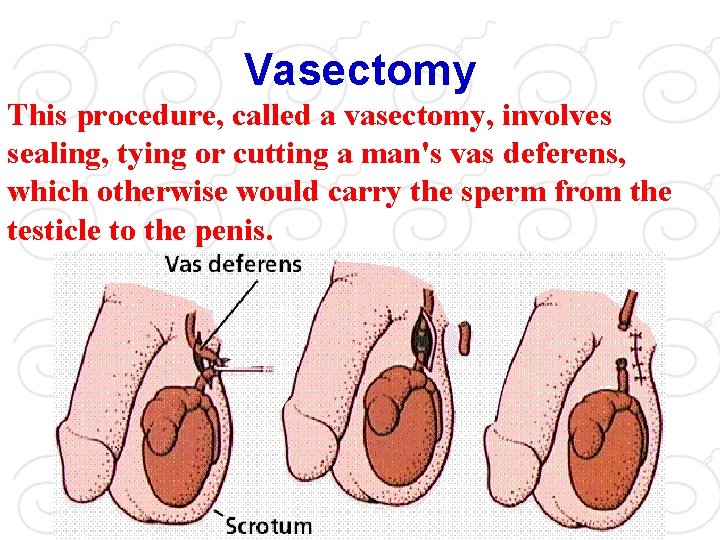
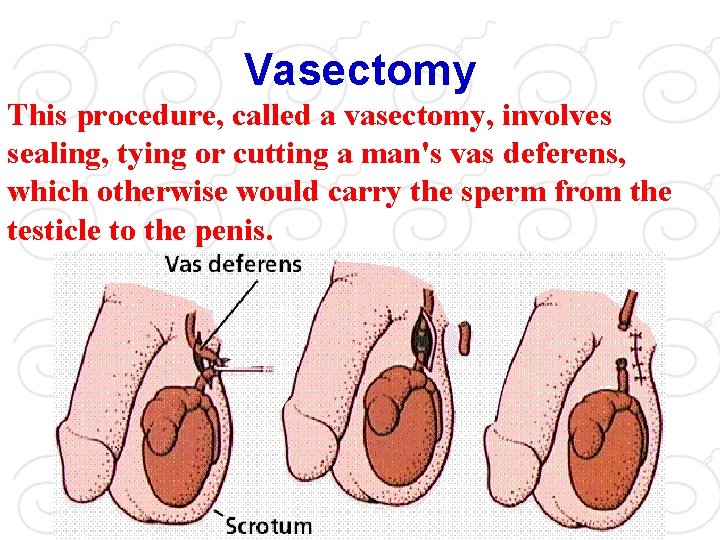
Vasectomy This procedure, called a vasectomy, involves sealing, tying or cutting a man's vas deferens, which otherwise would carry the sperm from the testicle to the penis.
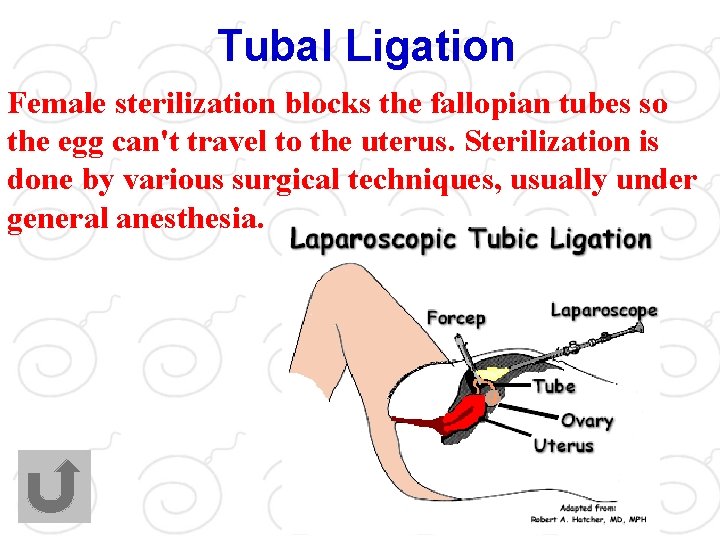
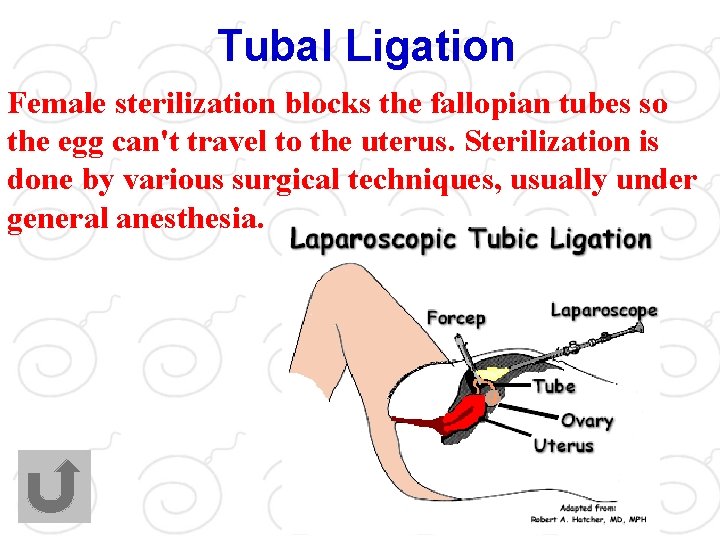
Tubal Ligation Female sterilization blocks the fallopian tubes so the egg can't travel to the uterus. Sterilization is done by various surgical techniques, usually under general anesthesia.