Pancreatic and Islet Cell Transplantation l yekehfallahphd student



- Slides: 59
Pancreatic and Islet Cell Transplantation l. yekehfallah-phd student of nursing education-2012 1
Critical Care of Pancreas Transplant Recipients l. yekehfallah-phd student of nursing education-2012 2
Pancreatic transplantation Indications • Diabetic renal failure - Simultaneous pancreas and kidney transplantation • Prerenal failure, unstable diabetic control, severe neuropathy – Pancreas transplant alone • Extensive abdominal tumour – Multivisceral (pancreas, liver, small bowel) l. yekehfallah-phd student of nursing education-2012 3

GENERAL PRINCIPLES • A/ pancreas transplantation is the only: -diabetes treatment with normalizes glycosylated hemoglobin (Hb. A 1 c) levels positively influences the progression of : 1/secondary diabetic complications 2/ameliorates quality of life 3/prolong life. Most pancreas transplants are done for selected, medically suitable patients with type I diabetes. Type II diabetes is a relatively infrequent indication (<10% of all pancreas transplants). l. yekehfallah-phd student of nursing education-2012 4
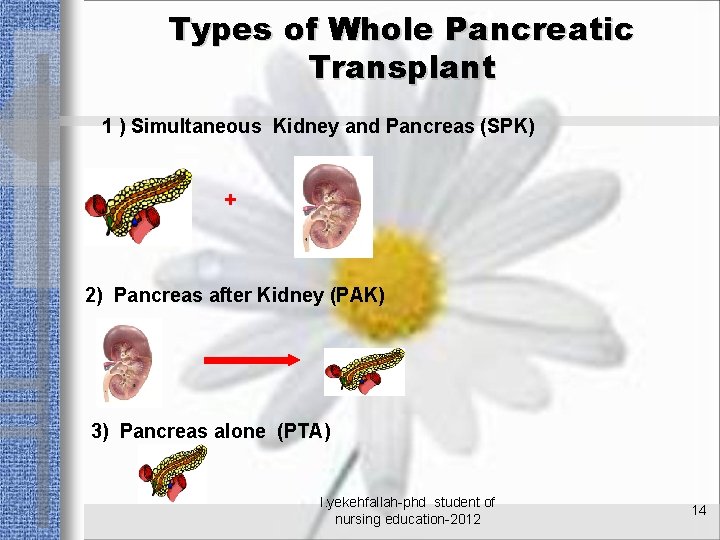
GENERAL PRINCIPLES • B/Depending on the kidney status, pancreas transplants are performed in three recipient categories: • 1 -Simultaneous pancreas-kidney transplants (SPK) in preuremic and uremic patients • 2 -Pancreas after kidney transplants (PAK) in posturemic recipients of a previous kidney transplant (from a deceased or a live donor) • 3 -Pancreas transplants alone (PTA) in nonuremic recipients with extremely labile diabetes but adequate native renal function l. yekehfallah-phd student of nursing education-2012 5
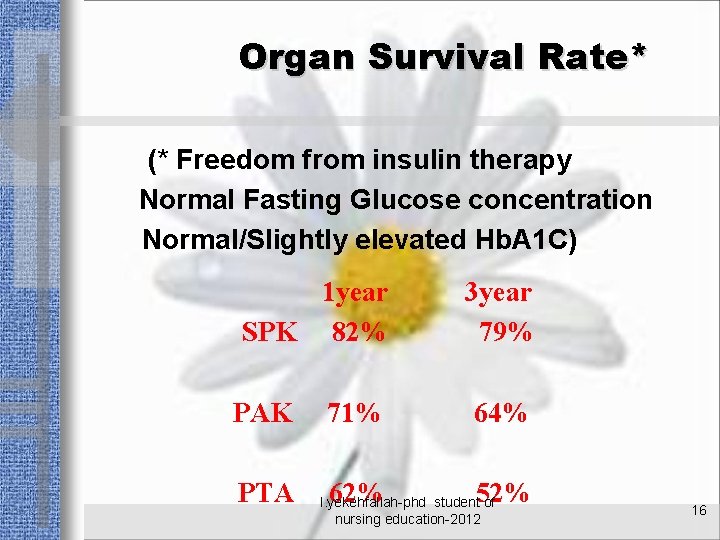
GENERAL PRINCIPLES • Pancreas graft survival rates have significantly improved over the past decade, and now exceed 95% at 1 year and 70% at 5 years (SPK). l. yekehfallah-phd student of nursing education-2012 6
PRETRANSPLANT EVALUATION 1/Coronary artery disease High incidence of coronary artery disease in diabetics (with and without end-stage renal disease [ESRD]). a/ noninvasive tests or coronary angiography b/ attention to new symptoms of : - angina - congestive heart failure - recent changes in exercise tolerance - changes on the ECG. l. yekehfallah-phd student of nursing education-2012 7
PRETRANSPLANT EVALUATION 2/Peripheral vascular disease - Decreased peripheral pulses - new bruits on peripheral vascular - Infected diabetic foot ulcers (contraindication to transplantation) - Check for new signs and symptoms of stroke and ischemic cerebrovascular disease l. yekehfallah-phd student of nursing education-2012 8
PRETRANSPLANT EVALUATION 3/Infectious disease Diabetes in combination with uremia is a significant risk factor for infection Preoperatively assessment: -chest radiograph - urinalysis - assessment of indwelling catheters and catheter exit sites : * hemodialysis catheters * peritoneal dialysis catheters [including a peritoneal fluid culture] * vascular access grafts Active infection is a contraindication to transplantation l. yekehfallah-phd student of nursing education-2012 9
PRETRANSPLANT EVALUATION 4/Metabolic and fluid status a/ Hyperkalemic uremic Management: -oral sodium polystyrene sulfonate [Kayexalate] - intravenous [IV] insulin and glucose - dialysis b/Hypervolemic - dialysis c/ Hyperglycemia with metabolic acidosis requires preoperative correction l. yekehfallah-phd student of nursing education-2012 10
PRETRANSPLANT EVALUATION Absolute contraindications to transplantation 1/Active sepsis 2/Active viral infection 3/Acquired immunodeficiency syndrome (AIDS) 4/Malignancy (except if treated, nonmetastatic, without recurrence, and with sufficient posttreatment follow-up) l. yekehfallah-phd student of nursing education-2012 11
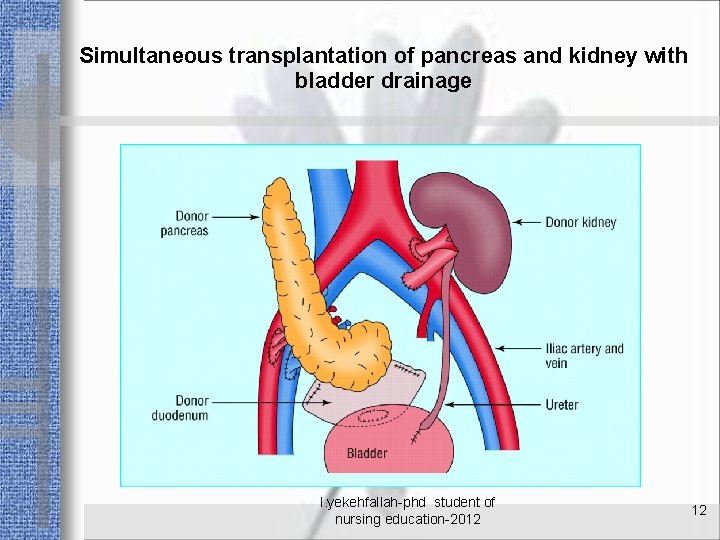
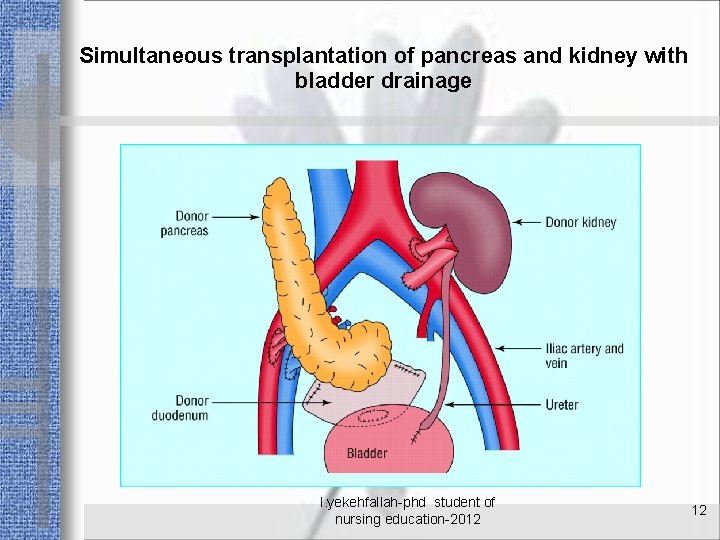
Simultaneous transplantation of pancreas and kidney with bladder drainage l. yekehfallah-phd student of nursing education-2012 12
Types of Transplantation WHOLE PANCREATIC ISLET CELL l. yekehfallah-phd student of nursing education-2012 13
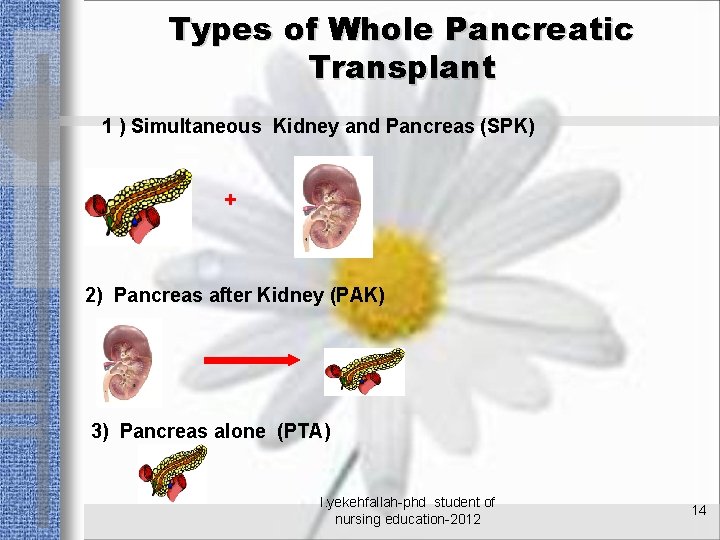
Types of Whole Pancreatic Transplant 1 ) Simultaneous Kidney and Pancreas (SPK) + 2) Pancreas after Kidney (PAK) 3) Pancreas alone (PTA) l. yekehfallah-phd student of nursing education-2012 14
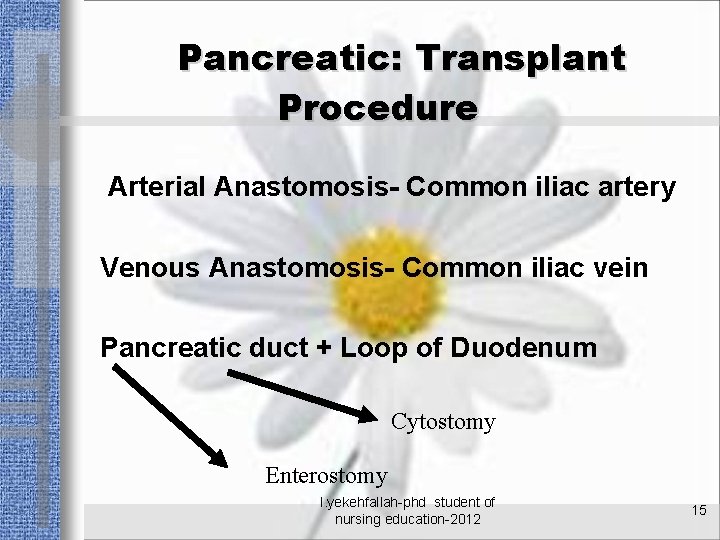
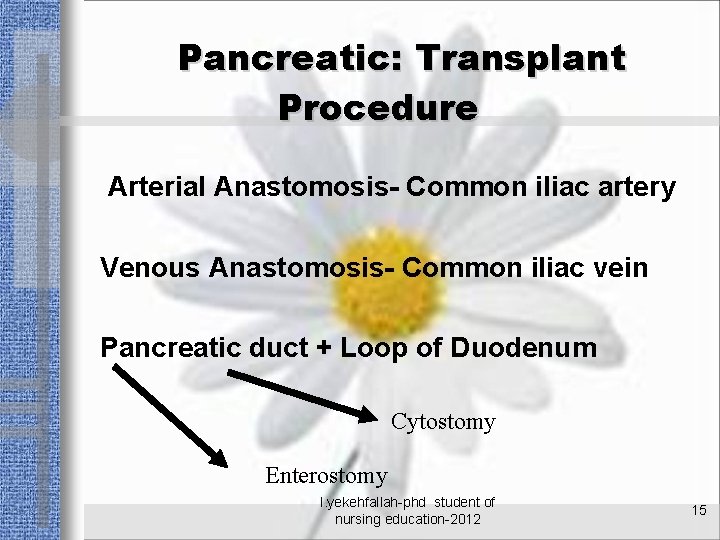
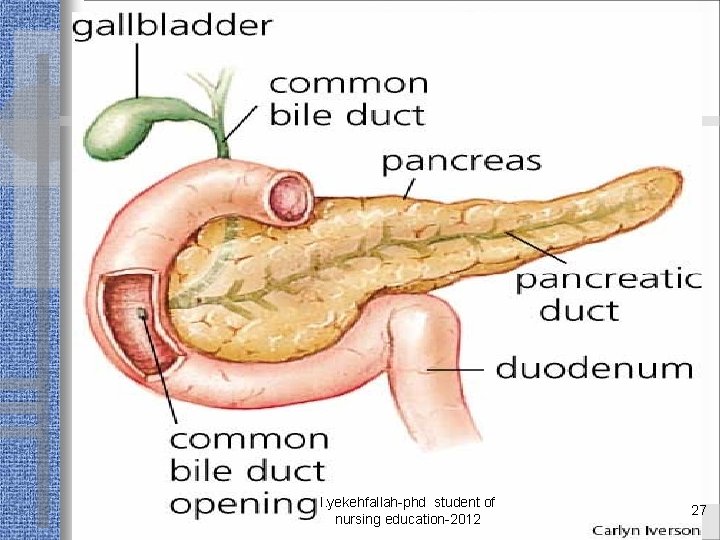
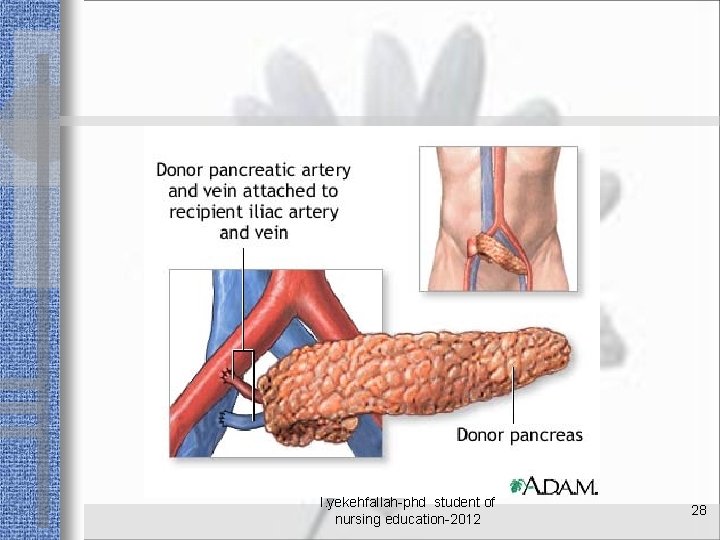
Pancreatic: Transplant Procedure Arterial Anastomosis- Common iliac artery Venous Anastomosis- Common iliac vein Pancreatic duct + Loop of Duodenum Cytostomy Enterostomy l. yekehfallah-phd student of nursing education-2012 15
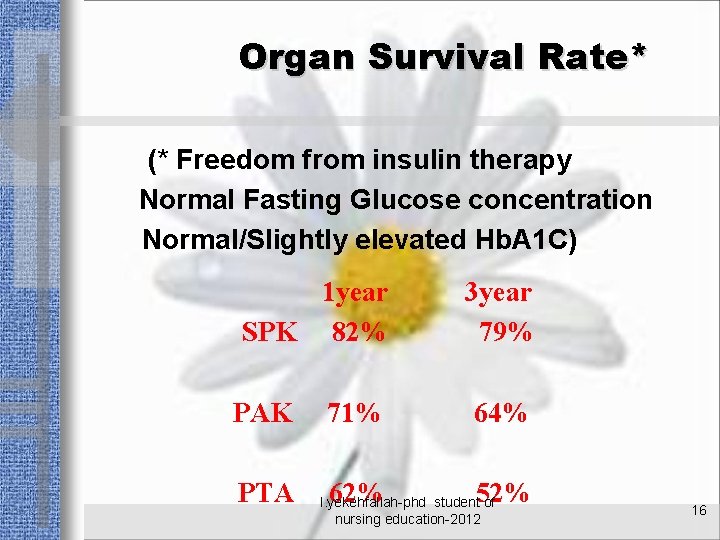
Organ Survival Rate* (* Freedom from insulin therapy Normal Fasting Glucose concentration Normal/Slightly elevated Hb. A 1 C) 1 year SPK 82% PAK PTA 3 year 79% 71% 64% 62% 52% l. yekehfallah-phd student of nursing education-2012 16
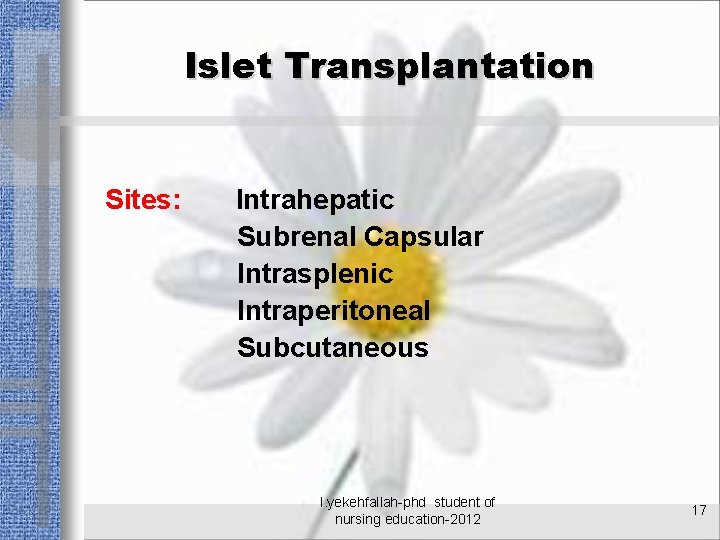
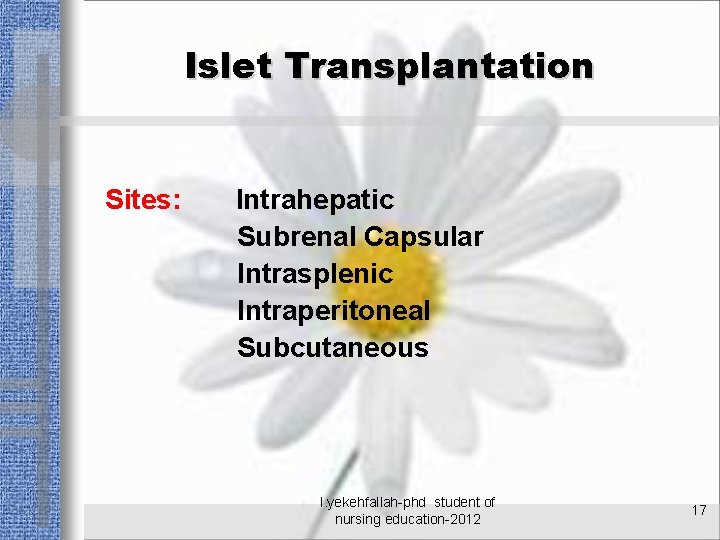
Islet Transplantation Sites: Intrahepatic Subrenal Capsular Intrasplenic Intraperitoneal Subcutaneous l. yekehfallah-phd student of nursing education-2012 17
Islet Transplantation Sites: Intrahepatic Subrenal Capsular Intrasplenic Intraperitoneal Subcutaneous Time: At laparotomy Renal Transplant Surgery Percutaneous Route Advantages: Less invasive Disadvantage: More Technical Expertise l. yekehfallah-phd student of nursing education-2012 18
ISLET ISOLATION Pancreas dissected from the duodenum. Main and accessory ducts are identified, clamped, and divided. Pancreatic duct Cannulated Collagenase(LIBERASE) to distend Pancreas (Low endotoxin) l. yekehfallah-phd student of nursinginto education-2012 Pancreas placed Ricordi chamber, 19
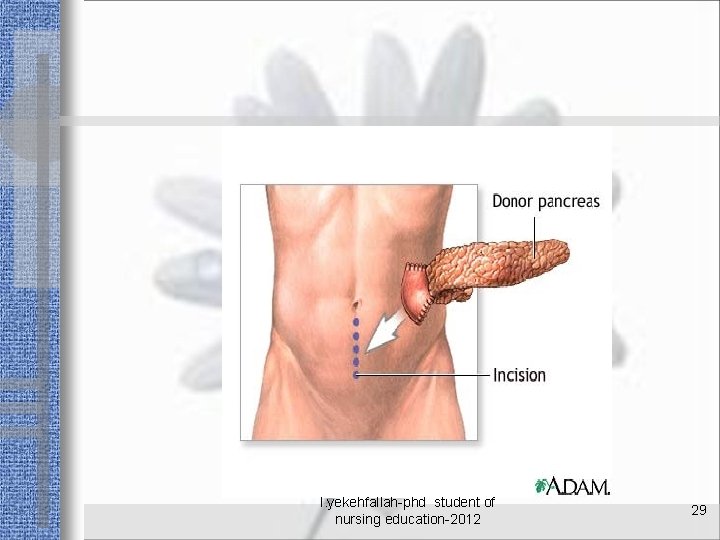
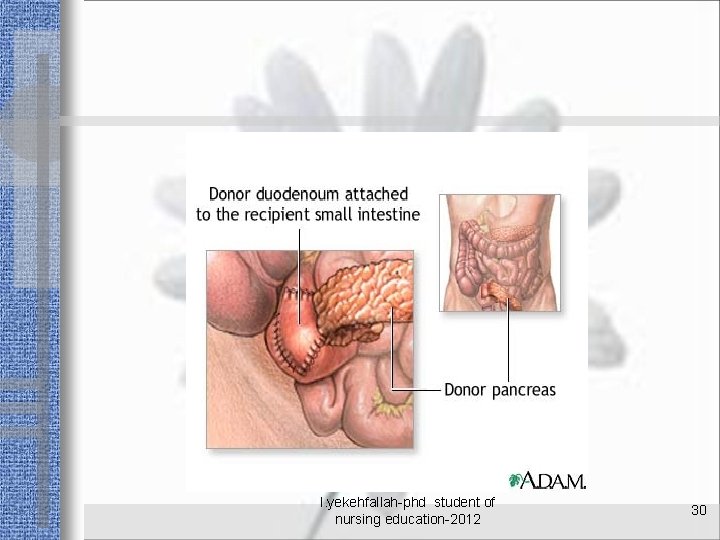
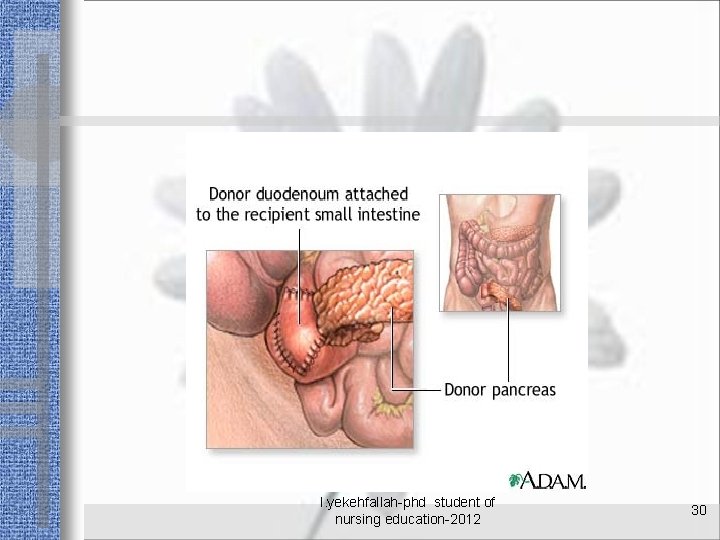
INTRAOPERATIVE CONSIDERATIONS Operative technique Nearly all pancreas transplants currently performed are from deceased donors and entail transplantation of the entire organ with an attached segment of duodenum that serves as conduit for the exocrine secretions. l. yekehfallah-phd student of nursing education-2012 20
INTRAOPERATIVE CONSIDERATIONS Operative technique Management of pancreatic exocrine secretions. The exocrine secretions of most pancreas transplants are drained enterically via an anastomosis of the graft's duodenal segment to the recipient's small intestine. For PAK and PTA recipients, bladder drainage (creation of a duodenocystostomy) can provide a useful additional means to monitor for rejection (by measuring urinary amylase). l. yekehfallah-phd student of nursing education-2012 21
INTRAOPERATIVE CONSIDERATIONS Operative technique Venous pancreas graft drainage. The venous effluent of the pancreas graft can be drained systemically, into an iliac vein, or portally, into the superior mesenteric vein. Portal drainage has theoretical, but clinically to date unproved advantages (host tolerance facilitation by portally delivered graft antigen; avoidance of potential systemic hyperinsulinemia sequelae). l. yekehfallah-phd student of nursing education-2012 22
INTRAOPERATIVE CONSIDERATIONS Cardiovascular care monitoring Recipients benefit from perioperative cardioprotection with: B²-blockers (e. g. , atenolol, 5 to 10 mg IV started preoperatively, repeat every 12 hours, and then 50 to 100 mg by mouth every day for at least the first postoperative week) l. yekehfallah-phd student of nursing education-2012 23
INTRAOPERATIVE CONSIDERATIONS Cardiovascular care and monitoring Hemodynamic monitoring: - central venous pressure (CVP) catheter - arterial line pulmonary artery catheter (presence of left ventricular dysfunction) l. yekehfallah-phd student of nursing education-2012 24
INTRAOPERATIVE CONSIDERATIONS Cardiovascular care and monitoring Maintain adequate intravascular volume status: 1/ avoiding high CVPs that can predispose pancreas grafts with systemic venous drainage to edema 2/ providing adequate preload for optimal perfusion of the kidney graft (SPK recipients) 3/fluid management to avoid fluid overload and acute myocardial strain is paramount. l. yekehfallah-phd student of nursing education-2012 25
INTRAOPERATIVE CONSIDERATIONS Metabolic care Frequent (at least hourly) intraoperative monitoring of blood glucose levels is important, because the pancreas graft often begins to function immediately postreperfusion, resulting in decreasing blood glucose levels and no further need for exogenous insulin l. yekehfallah-phd student of nursing education-2012 26
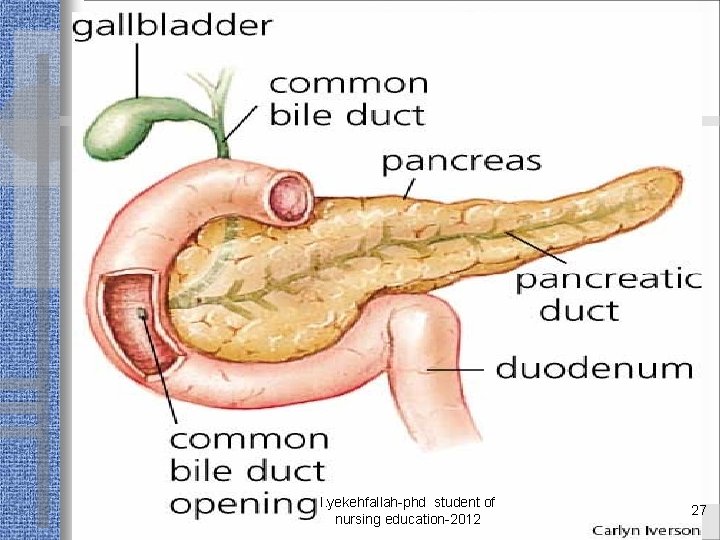
l. yekehfallah-phd student of nursing education-2012 27
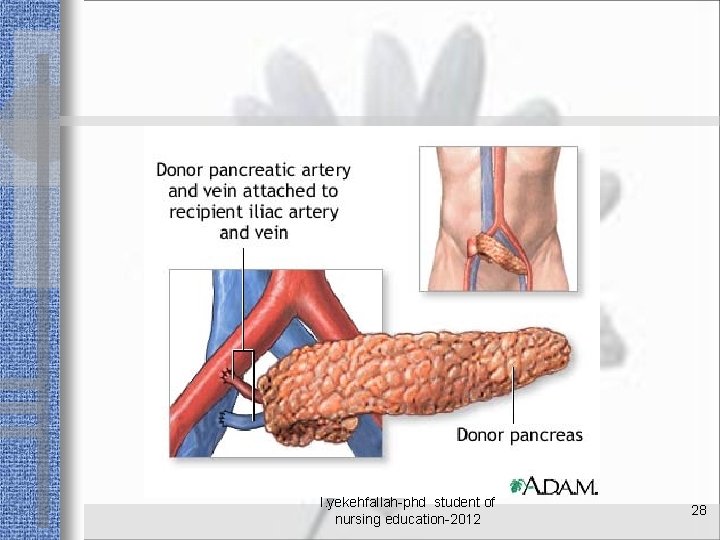
l. yekehfallah-phd student of nursing education-2012 28
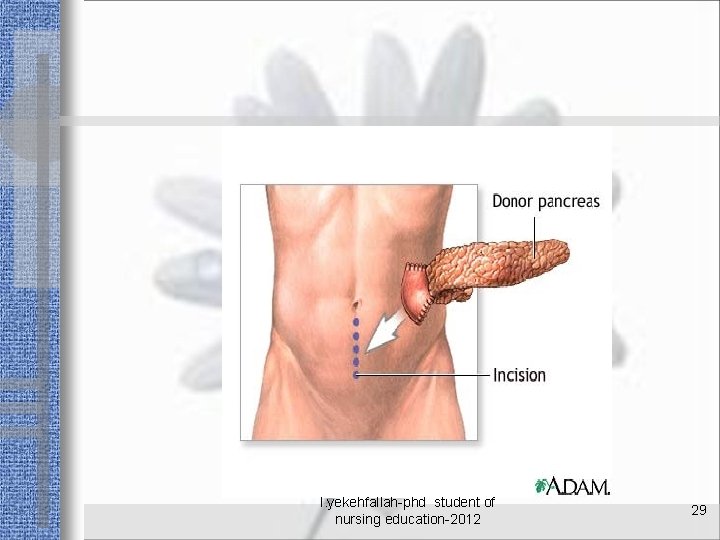
l. yekehfallah-phd student of nursing education-2012 29
l. yekehfallah-phd student of nursing education-2012 30
POSTOPERATIVE CARE General: Immediate postoperative: -chest radiograph -frequent electrolyte monitoring -daily serum amylase -lipase levels l. yekehfallah-phd student of nursing education-2012 31
POSTOPERATIVE CARE Metabolic In the few grafts that have delayed function, temporary administration of exogenous insulin may be necessary - IV insulin infusion - hourly blood glucose monitoring Bladder-drained monitoring : - dehydration and metabolic acidosis - fluid and electrolyte losses from the exocrine pancreas - Urine is collected over an 8 -hour period on each postoperative day - hourly urinary amylase production (expressed as amylase U/hr) - urinary amylase excretion should increase daily l. yekehfallah-phd student of nursing education-2012 32
POSTOPERATIVE CARE Kidney graft monitoring and management l. yekehfallah-phd student of nursing education-2012 33
POSTOPERATIVE CARE immunosuppression Immunosuppression combination : -polyclonal or monoclonal anti-T-cell antibodies for induction therapy during the first week (e. g. , antithymocyte globulin, alemtuzumab [Campath]) - steroids - calcineurin inhibitors (tacrolimus, cyclosporine) - mycophenolate mofetil -m. TOR inhibitors (sirolimus, everolimus). Solitary pancreas transplants (PAK and PTA) are more immunogenic and do not have a kidney from the same donor (as SPK recipients do) that would easily allow for rejection monitoring (i. e. , by checking serum creatine levels). They therefore require closer surveillance for rejection and often more immunosuppression. l. yekehfallah-phd student of nursing education-2012 34
POSTOPERATIVE CARE Graft thrombosis prophylaxis • No prospective data are available to support current empiric practices. • Some centers partially anticoagulate recipients perioperatively for the first 3 to 7 days (e. g. , heparin infusion at 300 to 700 U/h IV). • Many transplant programs start recipients perioperatively on oral acetylsalicylic acid, which is continued indefinitely. l. yekehfallah-phd student of nursing education-2012 35
POSTOPERATIVE CONSIDERATIONS Surgical complications 1/Postoperative bleeding Diagnosis: • 1/serial hemoglobin/hematocrit levels • 2/ hemodynamic changes (hypotension, tachycardia, decreased CVP, decreased left ventricular filling pressures). Most common bleeding sources: • 1/free intraabdominal bleeding from the graft or the vascular anastomoses; intravesical bleeding with massive hematuria (from the duodenovesical anastomosis in bladder-drained grafts) • 2/gastrointestinal bleeding from the duodenoenteric anastomosis in entericdrained grafts Treatment: • 1/Check platelets, prothrombin time (PT), and partial thromboplastin time (PTT). Replace coagulation factors and platelets as indicated. • 2/For ongoing intraabdominal bleeding, relaparotomy for hemostasis and evacuation of hematoma may be necessary l. yekehfallah-phd student of nursing education-2012 36
POSTOPERATIVE CONSIDERATIONS Surgical complications 2/Pancreas graft thrombosis Most frequent serious surgical complication (incidence: 5% to 10%); results nearly always in graft loss. 1/Symptoms: - Sudden onset of otherwise unexplained hyperglycemia (arterial and/or venous thrombosis) - graft tenderness and enlargement (venous thrombosis) - dark, massive hematuria (venous thrombosis of bladder-drained pancreas grafts) - markedly decreased or absent urinary amylase on spot urinary amylase check (bladder-drained grafts). l. yekehfallah-phd student of nursing education-2012 37
POSTOPERATIVE CONSIDERATIONS 2/Diagnosis (a) Imaging studies: -Doppler duplex ultrasonography -magnetic resonance angiography -computed tomographic angiography -conventional angiography (b) Diagnosis made during exploratory relaparotomy. 3/Treatment: Transplant pancreatectomy. l. yekehfallah-phd student of nursing education-2012 38
POSTOPERATIVE CONSIDERATIONS Surgical complications 3/Surgical wound infection a/Superficial wound infection (1) Symptoms: - fever - wound drainage - cellulitis - leukocytosis. (2) Treatment: - IV antibiotics - local incision and drainage - open wound care with daily dressing changes l. yekehfallah-phd student of nursing education-2012 39
POSTOPERATIVE CONSIDERATIONS Surgical complications Surgical wound infection b/Deep wound infection (intraabdominal abscess) (1) Occurs usually within the first 30 days posttransplant; bacterial abscesses are diagnosed earlier than fungal abscesses. Of all intraabdominal infections, 50% are diffuse and 50% are localized; 30% are associated with a leak. (2) Clinical presentation: - diffuse peritonitis - fever - ileus - nausea, vomiting - leukocytosis - hyperglycemia - sepsis. (3) Risk factors: - age greater than 45 years - retransplant - pretransplant peritoneal dialysis - graft pancreatitis l. yekehfallah-phd student of nursing education-2012 40
POSTOPERATIVE CONSIDERATIONS (4) Diagnosis: - abdominal CT with oral and IV contrast (for bladder-drained grafts also with retrograde bladder contrast to rule out leak) (5) Treatment: • (a) Percutaneous catheter drainage is appropriate as first line treatment in stable recipients with localized intraabdominal abscess. • (b) For unstable recipients and those with diffuse peritonitis, relaparotomy and open abscess drainage. If leak is present, relaparotomy in enteric drained recipients is mandatory, but in stable bladder-drained recipients, conservative treatment (prolonged Foley catheterization and percutaneous drainage of localized abscesses) may be attempted. • (c) IV antibiotics; bowel rest and nasogastric tube if ileus is present l. yekehfallah-phd student of nursing education-2012 41
POSTOPERATIVE CONSIDERATIONS Surgical complications 4/Leaks a/Enteric drained grafts (1) Incidence: 5 to 10% (2) Symptoms: - abdominal pain - peritonitis - ileus - fever - leukocytosis - hyperamylasemia (3) Diagnosis: (a) Abdominal computed tomography (CT) with oral contrast (b) Diagnosis made at exploratory relaparotomy (4) Treatment: - relaparotomy is mandatory (anastomotic revision or transplant pancreatectomy) l. yekehfallah-phd student of nursing education-2012 42
POSTOPERATIVE CONSIDERATIONS Surgical complications 4/Leaks b/Bladder-drained grafts (1) Incidence: 10% to 15% (2) Early leaks (<4 weeks posttransplant) usually at the duodenocystostomy anastomosis late leaks (>4 weeks posttransplant) typically from the graft duodenum (e. g. , duodenal ulceration or perforation, CMV infection). (3) Symptoms: - abdominal pain - distention - fever - vomiting - decreased urine output, peritonitis - improvement after Foley catheter placement. Differential diagnosis must include early ureteral anastomotic leak of a simultaneously transplanted kidney (SPK). (4) Diagnosis: (a) Low-pressure cystography (b) CT with retrograde bladder contrast (most accurate) (5) Treatment: (a) Early leaks: prolonged bladder decompression using Foley catheterization, percutaneous drainage of all intraabdominal fluid collections. (b) Infected leaks with peritonitis: relaparotomy and direct leak repair or transplant pancreatectomy. (c) Late leaks: usually require conversion from bladder to enteric drainage, irrespective of etiology l. yekehfallah-phd student of nursing education-2012 43
POSTOPERATIVE CONSIDERATIONS Surgical complications 5/Graft pancreatitis a/Prolonged posttransplant hyperamylasemia observed in up to 35% of all pancreas transplant recipients. b/Risk factors: - donor quality (e. g. , obesity, age, excessive inotropic requirements) - prolonged preservation time (ischemia-reperfusion pancreatitis) - pancreatic duct outflow impairment, bladder drainage c/Complications: - (peri-)pancreatic abscess - pancreatic necrosis (sterile and infected) - pancreatic fistula - pseudocyst. l. yekehfallah-phd student of nursing education-2012 44
POSTOPERATIVE CONSIDERATIONS d/Symptoms: - abdominal pain - graft tenderness - nausea, vomiting - ileus - Serum amylase and lipase levels may be elevated but correlate poorly with severity of pancreatitis - Endocrine secretory capacity often is only mildly impaired, even with severe pancreatitis. e/Diagnostic studies: - CT with appropriately timed IV contrast l. yekehfallah-phd student of nursing education-2012 45
POSTOPERATIVE CONSIDERATIONS f/Treatment: (1) Moderate and severe pancreatitis: nasogastric tube, bowel rest, total parenteral nutrition. (2) Reflux pancreatitis in bladder-drained recipients: insertion of a Foley catheter not only is diagnostic but also constitutes effective treatment. Repetitive episodes of reflux pancreatitis usually require conversion from bladder to enteric drainage. (3) Mechanical pancreatic duct obstruction: relaparotomy to address underlying surgical-technical problem. (4) No definitive data available on the utility of the somatostatin analogue octreotide for prevention and treatment of established pancreatitis l. yekehfallah-phd student of nursing education-2012 46
POSTOPERATIVE CONSIDERATIONS Surgical complications 6/Hematuria (bladder-drained recipients) Early postoperative hematuria: usually anastomotic and self-limited. Severe cases must be treated by continuous bladder irrigation and normalization of coagulation parameters. Late hematuria: frequently associated with duodenal pathology (e. g. , CMV infection). Cystoscopy and graft duodenal segment biopsy may be required. Depending on pathology, conversion to enteric drainage and antiviral treatment may be necessary l. yekehfallah-phd student of nursing education-2012 47
POSTOPERATIVE CONSIDERATIONS Medical complications 1/Rejection a/Acute rejection (1) Symptoms : - hyperamylasemia - fever - graft tenderness - decreasing urinary amylase - serum creatinine elevation in recipients of a simultaneously transplanted kidney (SPK) - Hyperglycemia is a late symptom (2) Diagnosis confirmation: - percutaneous graft biopsy (gold standard). (3) Treatment: (a) High-dose IV steroids (b) Anti-T-cell therapy l. yekehfallah-phd student of nursing education-2012 48

POSTOPERATIVE CONSIDERATIONS Medical complications 1/Rejection b/Chronic rejection (1) Associated with graft fibrosis and graft vasculopathy; irreversible. (2) Symptoms: - decreasing glucose tolerance - hyperglycemia - increasing Hb. A 1 c levels - decreasing or absent urinary amylase (bladder-drained grafts). (3) Treatment: (a) Symptomatic: oral antidiabetic agents, return to exogenous insulin therapy (b) Pancreas retransplantation (c) Graft pancreatectomy usually not necessary • l. yekehfallah-phd student of nursing education-2012 49
POSTOPERATIVE CONSIDERATIONS Medical complications 2/Acute perioperative myocardial ischemia: a/diagnose: -ECG -troponin and CK-MB levels b/Treatment: - as in any nontransplant patient l. yekehfallah-phd student of nursing education-2012 50
POSTOPERATIVE CONSIDERATIONS Medical complications 3/Metabolic complications a/Hypokalemia, hypocalcemia, hypophosphatemia, and hypomagnesemia: all can occur as the consequence of large-volume diuresis of a simultaneous kidney graft (SPK). Monitor at least every 12 hours; substitute electrolytes as indicated. l. yekehfallah-phd student of nursing education-2012 51
POSTOPERATIVE CONSIDERATIONS Medical complications 3/Metabolic complications b/Hyperkalemia (in SPK recipients) can be encountered with delayed kidney graft function and may, depending on severity, require IV calcium chloride, insulin and dextrose, and bicarbonate. Potassium excretion can be augmented by IV loop diuretics; if diuresis cannot be induced, oral Kayexalate and dialysis may become necessary l. yekehfallah-phd student of nursing education-2012 52
POSTOPERATIVE CONSIDERATIONS Medical complications 3/Metabolic complications c/Hyperglycemia may reflect transient delayed graft function (rare) and may require temporary exogenous insulin l. yekehfallah-phd student of nursing education-2012 53
POSTOPERATIVE CONSIDERATIONS Medical complications 4/Infectious complications Most early posttransplant infections are bacterial or fungal. Viral and parasitic infections begin to emerge after 6 weeks posttransplant l. yekehfallah-phd student of nursing education-2012 54
POSTOPERATIVE CONSIDERATIONS Medical complications 5/Neurologic complications a/Seizures Overall rare; rule out electrolyte abnormalities, drug side effects (e. g. , muromonab-CD 3 [Orthoclone OKT 3], tacrolimus), central nervous system infection (may require lumbar puncture). b/Acute cerebrovascular events must be considered in all patients with new onset of seizures or otherwise unexplained postoperatively altered level of consciousness or new onset of other neurologic symptoms l. yekehfallah-phd student of nursing education-2012 55
POSTOPERATIVE CONSIDERATIONS Medical complications 6/Immunosuppressive drug side effects a/Hematologic: leukopenia or thrombocytopenia (e. g. , secondary to anti-T-cell therapy with antithymocyte globulin, alemtuzumab; mycophenolate mofetil, sirolimus). Adjust or hold drug doses as necessary. b/Acute nephrotoxicity: (calcineurin inhibitors [cyclosporine, tacrolimus]). c/Neurologic: seizures, tremor, peripheral neuropathic symptoms (calcineurin inhibitors), aseptic meningitis and seizures (Orthoclone OKT 3). d/Pulmonary: pulmonary edema (cytokine release syndrome associated with polyclonal or monoclonal anti-T-cell therapy), interstitial pulmonary fibrosis (sirolimus). e/Hyperlipidemia: associated with steroids, cyclosporine, tacrolimus, and sirolimus l. yekehfallah-phd student of nursing education-2012 56
POSTOPERATIVE CONSIDERATIONS Medical complications Posttransplant malignancies: posttransplant lymphoproliferative disease; increased incidence of skin cancers. l. yekehfallah-phd student of nursing education-2012 57
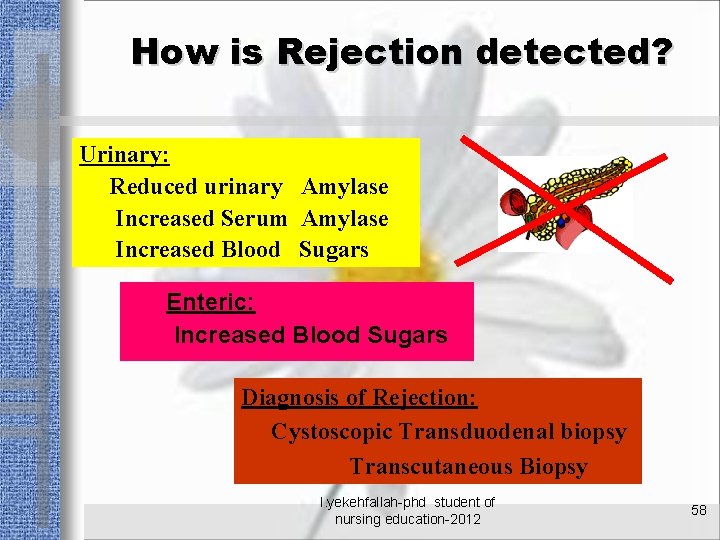
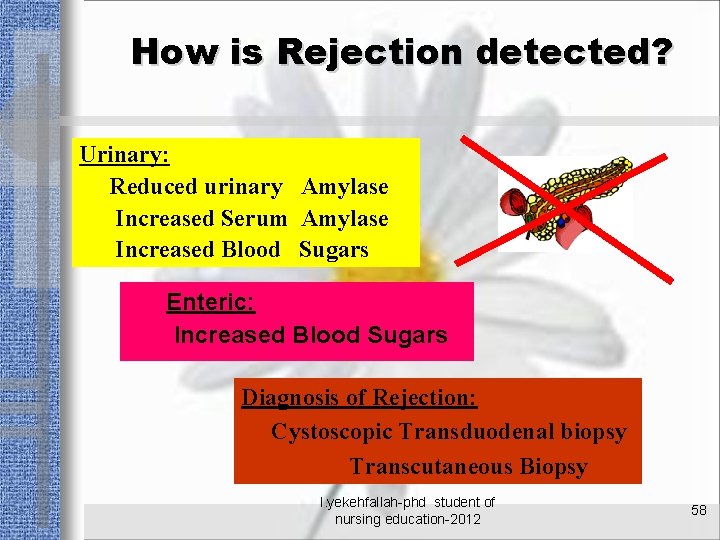
How is Rejection detected? Urinary: Reduced urinary Amylase Increased Serum Amylase Increased Blood Sugars Enteric: Increased Blood Sugars Diagnosis of Rejection: Cystoscopic Transduodenal biopsy Transcutaneous Biopsy l. yekehfallah-phd student of nursing education-2012 58

? l. yekehfallah-phd student of nursing education-2012 59
 Stem cell phuket
Stem cell phuket Bone marrow transplantation sri lanka
Bone marrow transplantation sri lanka Law of transplantation
Law of transplantation Patrick evrard mont godinne
Patrick evrard mont godinne Evaluation of crude drug
Evaluation of crude drug Ash value definition in pharmacognosy
Ash value definition in pharmacognosy Evaluation of crude drugs
Evaluation of crude drugs Cultural transplantation examples
Cultural transplantation examples Uchsc
Uchsc Transplant
Transplant The main jobs of the large intestine are _____.
The main jobs of the large intestine are _____. Where is bile juice produced
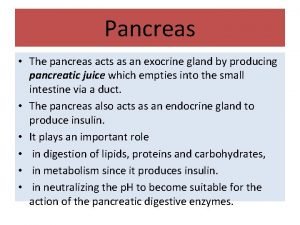
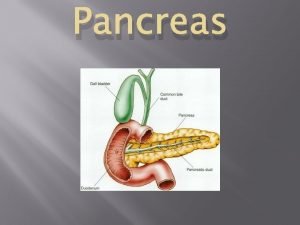
Where is bile juice produced Pancreas funzione
Pancreas funzione Pancreatic digestive secretions
Pancreatic digestive secretions Function of vitamin a
Function of vitamin a Radiologix verdun
Radiologix verdun Daughter mother grandmother pancreatic lesions
Daughter mother grandmother pancreatic lesions Cck function in digestion
Cck function in digestion How are carbs digested
How are carbs digested Absorption
Absorption Ranson score
Ranson score Stage 2b pancreatic cancer
Stage 2b pancreatic cancer Acute pancreatitis pes statement
Acute pancreatitis pes statement Pancreas
Pancreas Pancreatic histology
Pancreatic histology Pancreatic tissue
Pancreatic tissue Pancreatic juice
Pancreatic juice Pancreatic calcification
Pancreatic calcification Ralph steinman pancreatic cancer
Ralph steinman pancreatic cancer Pancreatic calcification
Pancreatic calcification Mrcp pancreatic cyst
Mrcp pancreatic cyst Glucagon function
Glucagon function Pancreatic enzymes
Pancreatic enzymes Pancreatic juice
Pancreatic juice Hydrohepatosis
Hydrohepatosis Pancreatitis stool pictures
Pancreatitis stool pictures Difference between mercury cell and diaphragm cell
Difference between mercury cell and diaphragm cell Prokaryotic reproduction
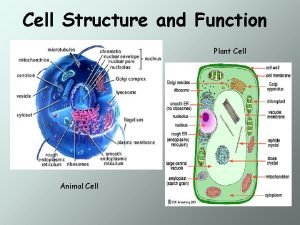
Prokaryotic reproduction Venn diagram of plant and animal cell
Venn diagram of plant and animal cell Plant cell structure
Plant cell structure Structure of plant cell
Structure of plant cell Types of secondary cells
Types of secondary cells Difference between plant and animal cell
Difference between plant and animal cell Events of the cell cycle
Events of the cell cycle Prokaryotic cell and eukaryotic cell
Prokaryotic cell and eukaryotic cell Chapter 4 cell theory and cell study
Chapter 4 cell theory and cell study Idealized animal cell
Idealized animal cell Walker cell and hadley cell
Walker cell and hadley cell Cell cycle and cell division
Cell cycle and cell division Animal cell plant cell venn diagram
Animal cell plant cell venn diagram Cell cycle and cell division
Cell cycle and cell division Electrolytic cell
Electrolytic cell Animal cell and plant cell
Animal cell and plant cell What i did last weekend essay
What i did last weekend essay What did you do in london last weekend
What did you do in london last weekend Clearinghouse student tracker
Clearinghouse student tracker Class maths student student1 class student string name
Class maths student student1 class student string name National student clearinghouse student tracker
National student clearinghouse student tracker Https://student.freckle.com/
Https://student.freckle.com/ Hello teacher good morning
Hello teacher good morning