Nutrition Therapy for Paralytic Ileus Lara Snead Sodexo









- Slides: 40
Nutrition Therapy for Paralytic Ileus Lara Snead Sodexo Dietetic Intern February 4, 2013
Objectives Differentiate an ileus from a small bowel obstruction Identify indications for nutrition support Discuss medical and nutrition care throughout case study’s hospital course
General Information GG is a 64 YO Male Admitted on 11/12/2012 w/COPD Initially seen as a Nursing Screen Referral on 11/13 by RD Seen by dietetic intern 9 times Remains an inpatient @ WAH
Past Medical History COPD HTN Anemia Cellulitis of LEs Rashes PVD

Social History Lives with parents Smokes about 1 pack/day Drinks alcohol almost qday
Anthropometric Data Ht: 5’ 7” (67”) Admit Wt: 139# (63 kg) IBW: 148# (67 kg) BMI: 21. 8 kg/m 2 (Normal wt category)
Hospital Course 11/12: Right femoral endarterectomy & embolectomy; fasciotomies 11/13: Seen by RD – intubated, sedated, on 2 pressors, nonresponsive to voice/questions NPO; banana bag Drsg to R shin & thigh Kcal: 1134 -1449 (18 -23), Prot: 63 -76 (1. 0 -1. 2) Lactate-4. 5 H ↓, MAP-80’s Rec. initiate EN w/Glucerna 1. 2 @ 30 m. L/hr, ↑ as tol. to 45 m. L/hr (1296 kcal, 65 g prot)
Hospital Course, Cont. 11/15: Tolerating Nepro @ 20 m. L/hr RLE w/inner & outer incisions w/staples OTA, leg is warm, ecchymotic Rec. to Δ TF to Glucerna 1. 2 @ 45 m. L/hr (1296 kcal, 64 g prot) ↑ BG (167, 235, 193 mg/d. L) 11/19: Extubated, alert & responsive but delirious Likely need amputation of R toes vs. foot Kcal: 1575 -1890 (25 -30), Prot: 75 -88 (1. 2 -1. 4) Tolerating feeds – rec. advance to Glucerna 1. 2 @ 60 m. L/hr (1728 kcal, 86 g prot)
Hospital Course, Cont. � 11/27: �Reintubated – full vent �NPO – OGT on LCS (500 m. L out in 4 hrs) �KUB: SBO, perforated viscus - no plan for surgery (allow to heal) �Rec. TPN – 2 L (NS): 11% Dex, 4. 2% AA, 175 m. L Lipids (1434 kcal, 84 g prot) � 11/30: �KUB: C/w ileus vs. SBO �Gastrografin via NGT �Cont. TPN �If no extravasation, begin Osmolite 1. 5 @ 20 and ↑ as tol. to 35 m. L/hr + PS (1332 kcal, 68 g prot)
SBO vs. Ileus SBO – partial/complete blockage of small/large intestine Tumor, adhesions, hernias, twisting/narrowing of intestines Ileus – absence of intestinal peristalsis without mechanical obstruction Normal times after surgery: Small bowel – several hrs Stomach – 24 -48 hrs Colon – 48 -72 days When postop ileus persists longer, considered pathologic and called a paralytic ileus
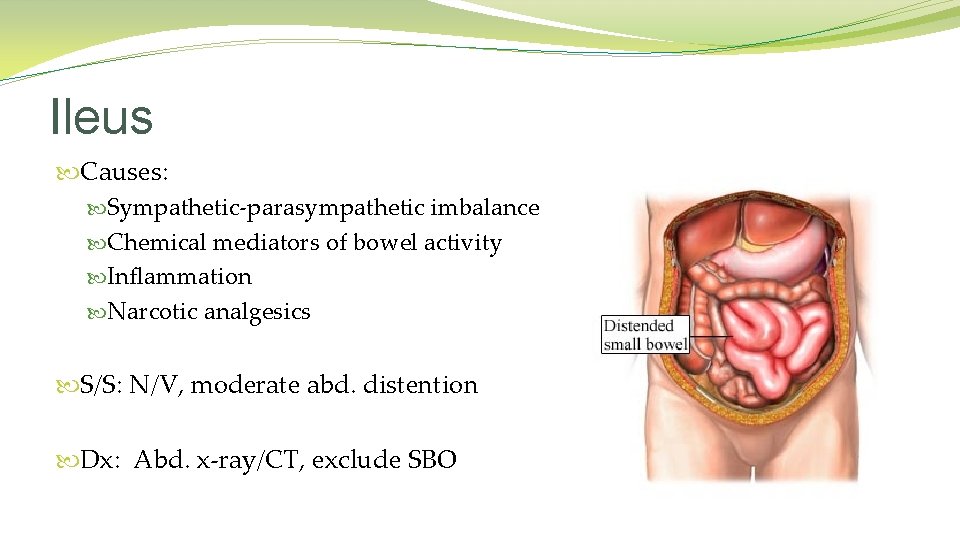
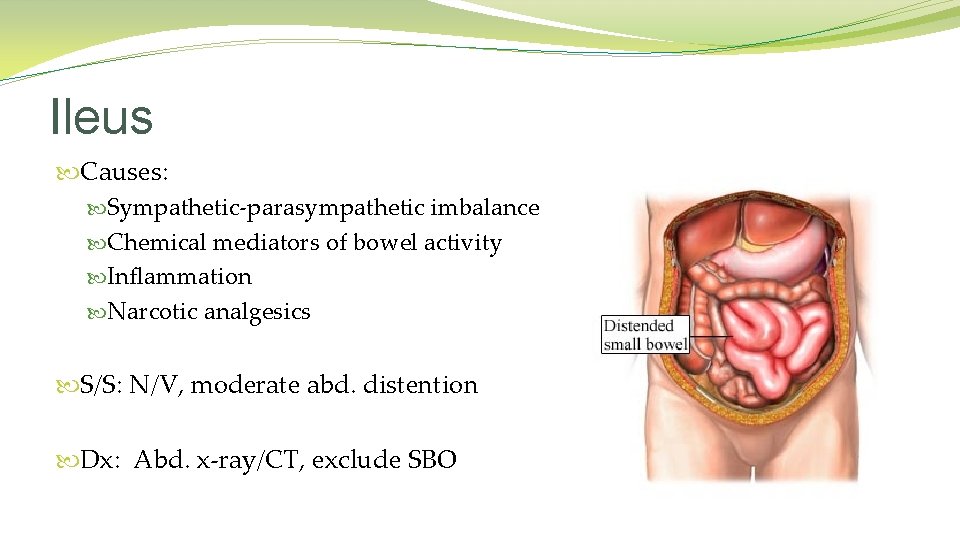
Ileus Causes: Sympathetic-parasympathetic imbalance Chemical mediators of bowel activity Inflammation Narcotic analgesics S/S: N/V, moderate abd. distention Dx: Abd. x-ray/CT, exclude SBO
Ileus Management Nasogastric tube for decompression Early postop enteral feeding Gum-chewing Meds: Limit narcotics Erythromycin – antibiotics, motilin receptor antagonist Metoclopramide (Reglan) – antiemetic, prokinetic
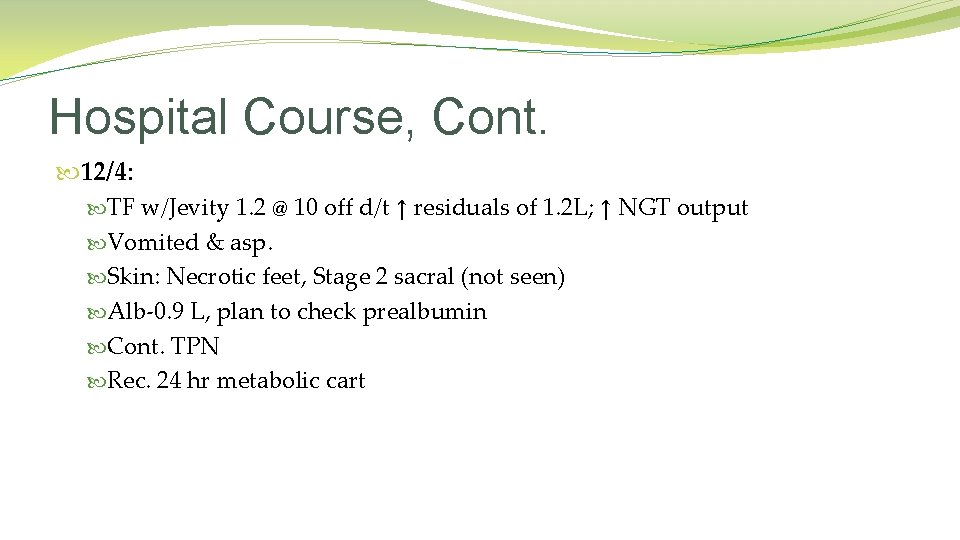
Hospital Course, Cont. 12/4: TF w/Jevity 1. 2 @ 10 off d/t ↑ residuals of 1. 2 L; ↑ NGT output Vomited & asp. Skin: Necrotic feet, Stage 2 sacral (not seen) Alb-0. 9 L, plan to check prealbumin Cont. TPN Rec. 24 hr metabolic cart

Hospital Course, Cont. 12/7: CT on 12/5 showed↑ dilated SB c/w high-grade SBO Tracheostomy on 12/6 Indirect Calorimetry – avg. 2200 kcal, RQ <0. 8 NGT on LCS w/100 m. L out overnight Δ TPN to 2 L (NS): 19% Dex, 4. 5% AA, 275 m. L Lipids (2206 kcal, 90 g prot) Trial Jevity 1. 2 @ 10 m. L/hr if NGT output remains <400 m. L/next 24 hrs
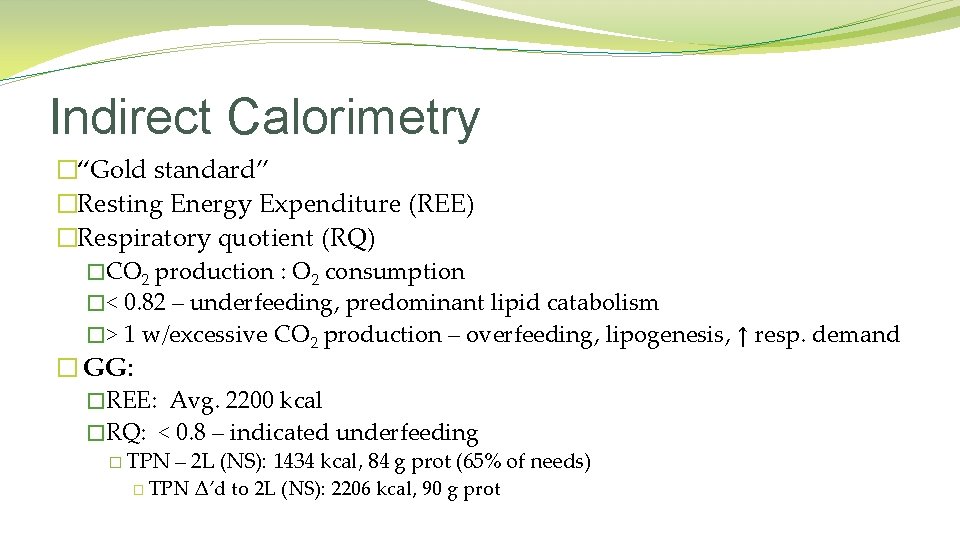
Indirect Calorimetry �“Gold standard” �Resting Energy Expenditure (REE) �Respiratory quotient (RQ) �CO 2 production : O 2 consumption �< 0. 82 – underfeeding, predominant lipid catabolism �> 1 w/excessive CO 2 production – overfeeding, lipogenesis, ↑ resp. demand � GG: �REE: Avg. 2200 kcal �RQ: < 0. 8 – indicated underfeeding � TPN – 2 L (NS): 1434 kcal, 84 g prot (65% of needs) � TPN Δ’d to 2 L (NS): 2206 kcal, 90 g prot
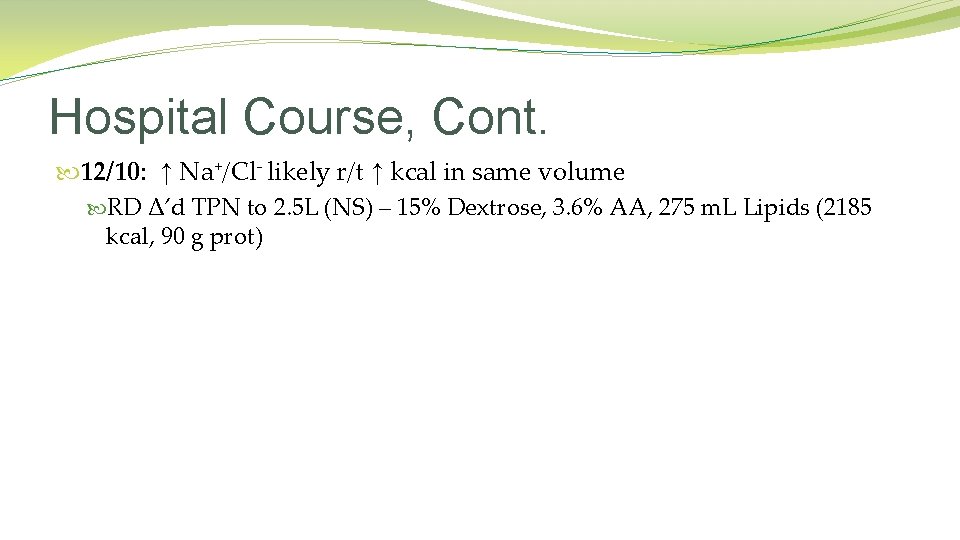
Hospital Course, Cont. 12/10: ↑ Na+/Cl- likely r/t ↑ kcal in same volume RD Δ’d TPN to 2. 5 L (NS) – 15% Dextrose, 3. 6% AA, 275 m. L Lipids (2185 kcal, 90 g prot)

Hospital Course, Cont. � 12/11: �Alert, more responsive, tolerating T-piece �Did not tolerate EN on 12/9 �SBFT: Not SBO, normal transit times; SB & LB dilation c/w ileus �↓ abd. distention, NGT clamped but had 800 m. L out overnight �Flexiseal w/600 m. L out overnight �Skin: Unchanged �Na+-148 H, Cl--111 H, BUN-21 H, Prealbumin-4. 4 L �Cont. TPN, add ½NS IVF’s until stooling improves, trial Reglan, check prealbumin �If NG output <500 m. L in next 24 hrs, trial Jevity 1. 2 @ 10 m. L/hr
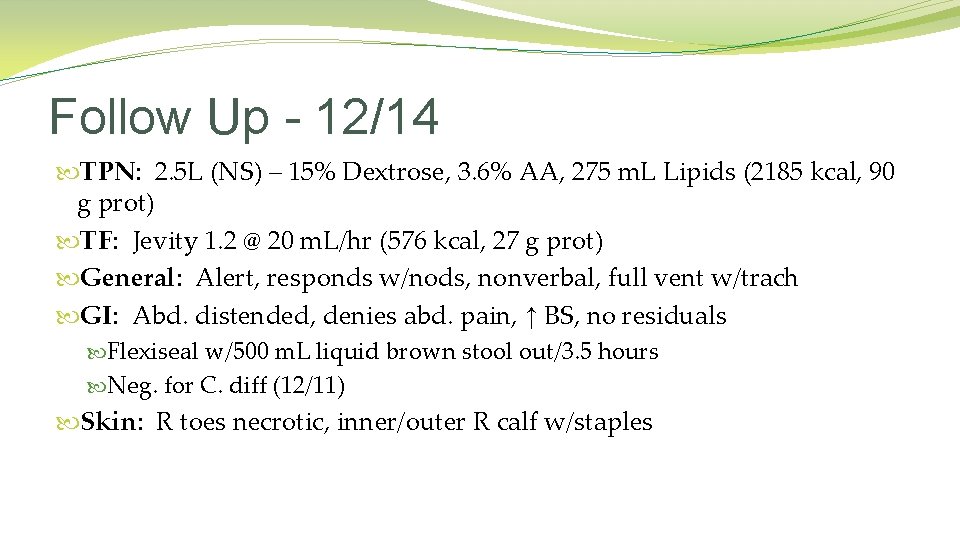
Follow Up - 12/14 TPN: 2. 5 L (NS) – 15% Dextrose, 3. 6% AA, 275 m. L Lipids (2185 kcal, 90 g prot) TF: Jevity 1. 2 @ 20 m. L/hr (576 kcal, 27 g prot) General: Alert, responds w/nods, nonverbal, full vent w/trach GI: Abd. distended, denies abd. pain, ↑ BS, no residuals Flexiseal w/500 m. L liquid brown stool out/3. 5 hours Neg. for C. diff (12/11) Skin: R toes necrotic, inner/outer R calf w/staples
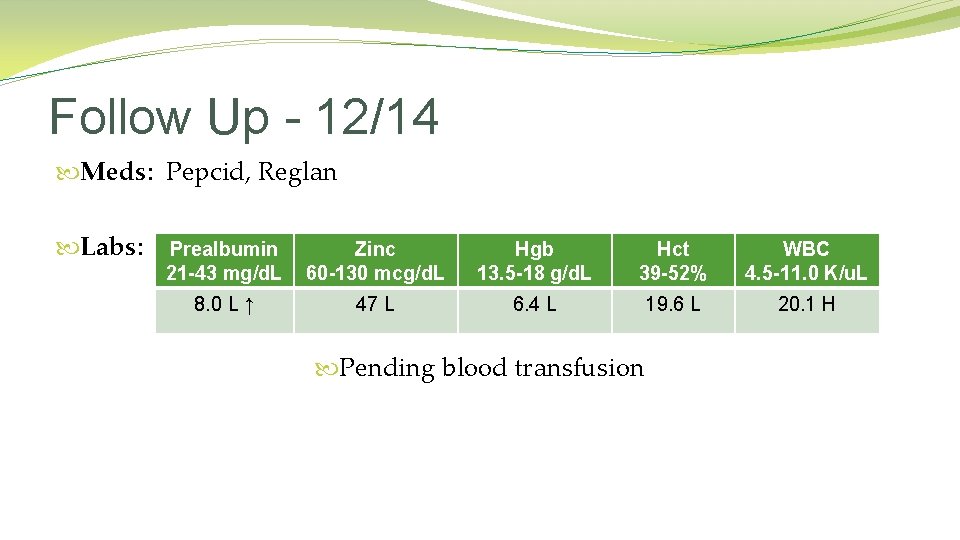
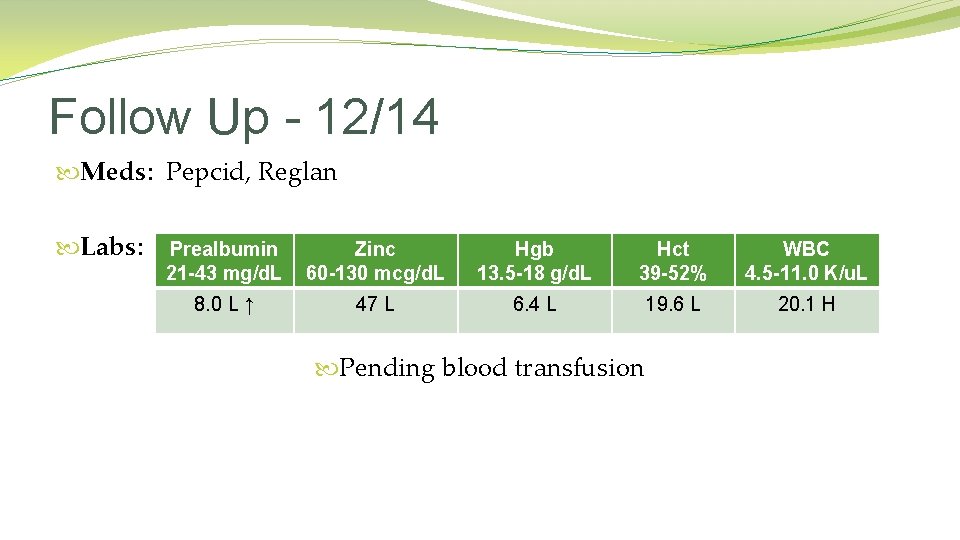
Follow Up - 12/14 Meds: Pepcid, Reglan Labs: Prealbumin 21 -43 mg/d. L Zinc 60 -130 mcg/d. L Hgb 13. 5 -18 g/d. L Hct 39 -52% WBC 4. 5 -11. 0 K/u. L 8. 0 L ↑ 47 L 6. 4 L 19. 6 L 20. 1 H Pending blood transfusion
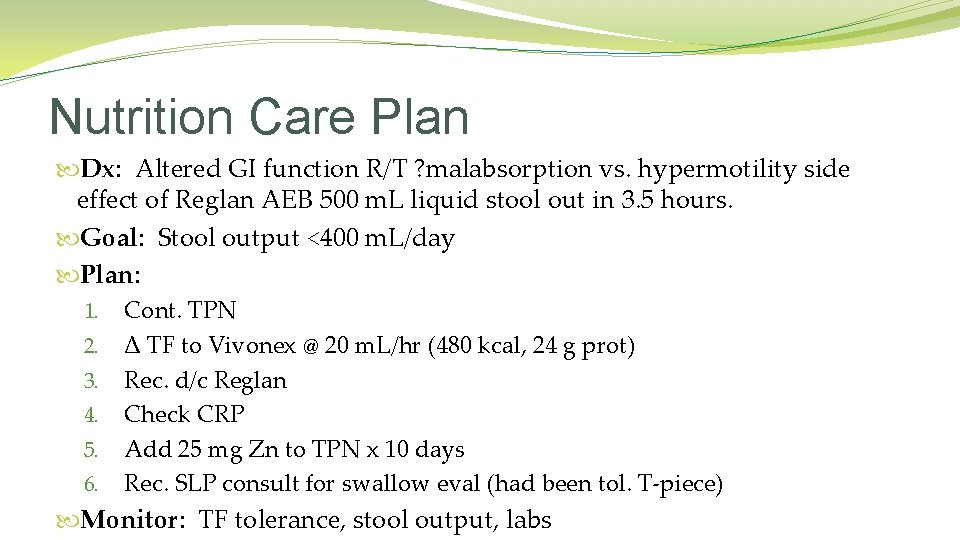
Nutrition Care Plan Dx: Altered GI function R/T ? malabsorption vs. hypermotility side effect of Reglan AEB 500 m. L liquid stool out in 3. 5 hours. Goal: Stool output <400 m. L/day Plan: 1. Cont. TPN 2. Δ TF to Vivonex @ 20 m. L/hr (480 kcal, 24 g prot) 3. Rec. d/c Reglan 4. Check CRP 5. Add 25 mg Zn to TPN x 10 days 6. Rec. SLP consult for swallow eval (had been tol. T-piece) Monitor: TF tolerance, stool output, labs
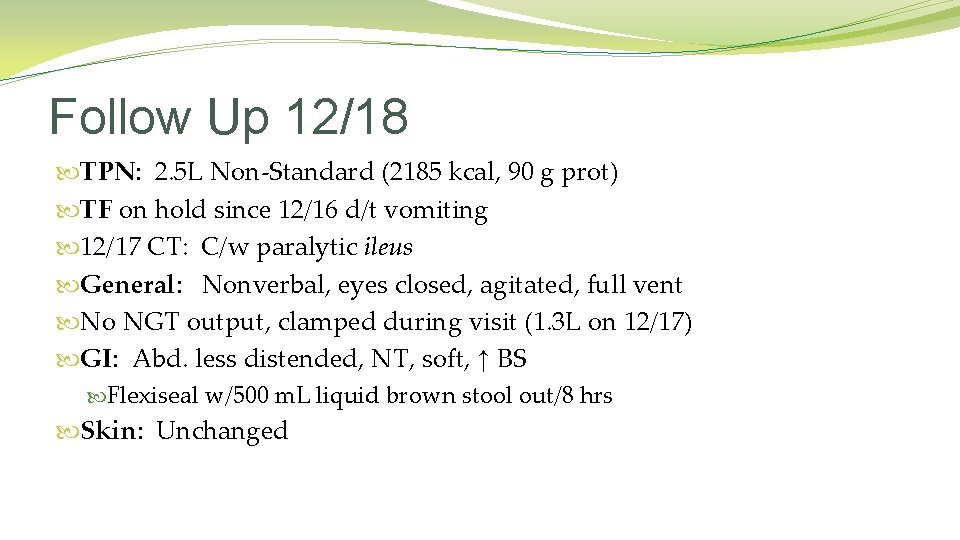
Follow Up 12/18 TPN: 2. 5 L Non-Standard (2185 kcal, 90 g prot) TF on hold since 12/16 d/t vomiting 12/17 CT: C/w paralytic ileus General: Nonverbal, eyes closed, agitated, full vent No NGT output, clamped during visit (1. 3 L on 12/17) GI: Abd. less distended, NT, soft, ↑ BS Flexiseal w/500 m. L liquid brown stool out/8 hrs Skin: Unchanged

Follow Up 12/18 Meds: Pepcid, Ativan, KCl *Reglan d/c’d – no Δ’s in stool output; ↑ vomiting Labs: K+ 3. 5 -5. 1 m. Eq/L Cl 98 -107 mmol/L CO 2 21 -32 mmol/L Hgb 13. 5 -18 g/d. L Hct 39 -51% WBC 4. 5 -11 K/u. L 3. 1 L 115 H 18 L 6. 7 L ↑ 20. 5 L ↑ 14. 0 H ↓ Pending blood transfusion Low K+ r/t ↑ vomiting & NGT output High Cl- and low CO 2 r/t diarrhea
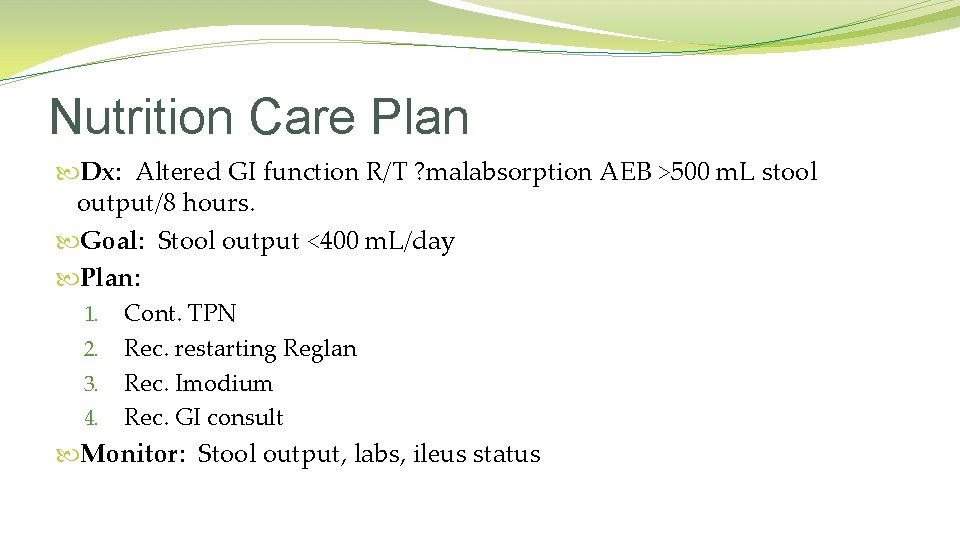
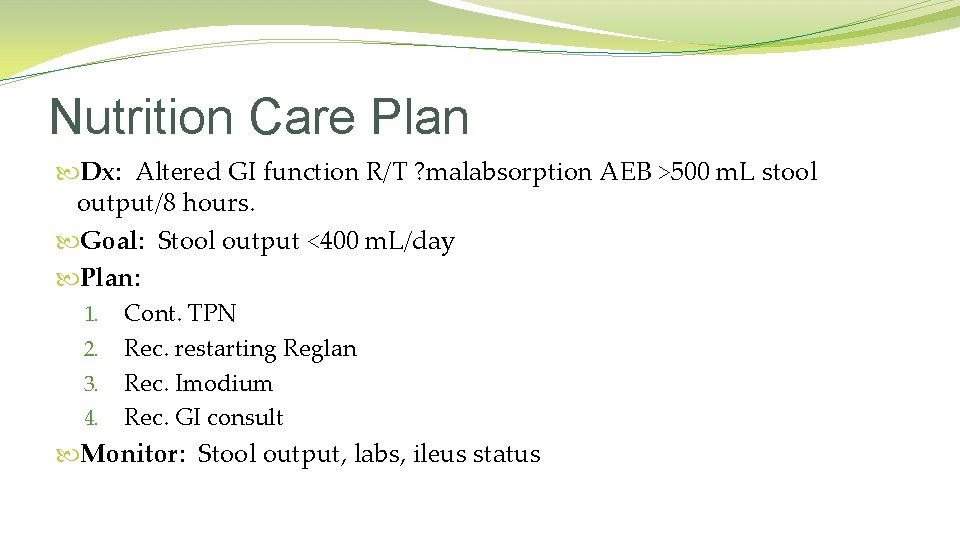
Nutrition Care Plan Dx: Altered GI function R/T ? malabsorption AEB >500 m. L stool output/8 hours. Goal: Stool output <400 m. L/day Plan: 1. Cont. TPN 2. Rec. restarting Reglan 3. Rec. Imodium 4. Rec. GI consult Monitor: Stool output, labs, ileus status
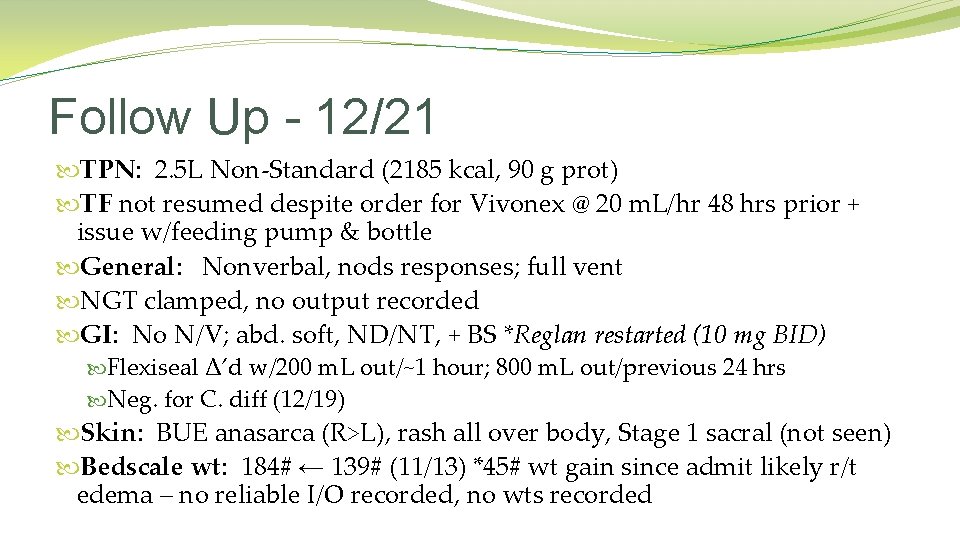
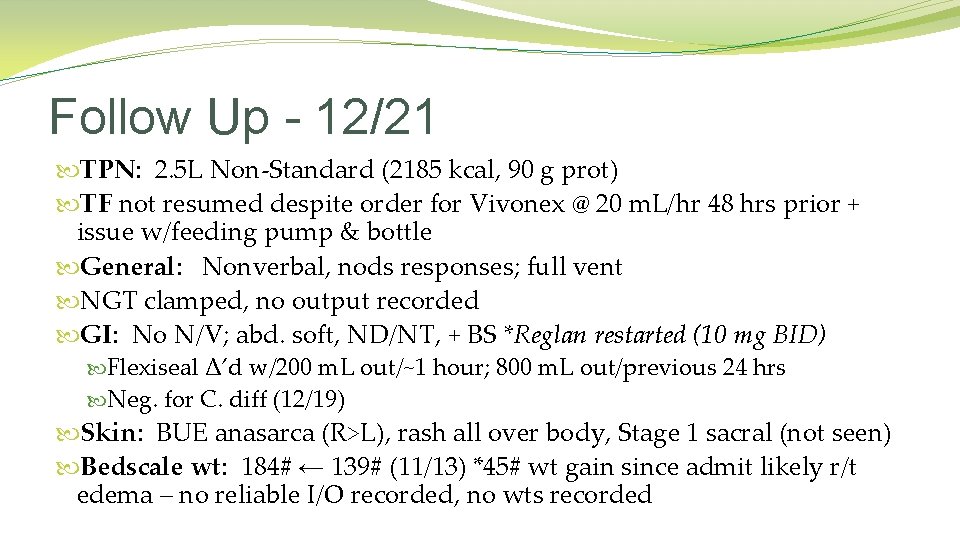
Follow Up - 12/21 TPN: 2. 5 L Non-Standard (2185 kcal, 90 g prot) TF not resumed despite order for Vivonex @ 20 m. L/hr 48 hrs prior + issue w/feeding pump & bottle General: Nonverbal, nods responses; full vent NGT clamped, no output recorded GI: No N/V; abd. soft, ND/NT, + BS *Reglan restarted (10 mg BID) Flexiseal Δ’d w/200 m. L out/~1 hour; 800 m. L out/previous 24 hrs Neg. for C. diff (12/19) Skin: BUE anasarca (R>L), rash all over body, Stage 1 sacral (not seen) Bedscale wt: 184# ← 139# (11/13) *45# wt gain since admit likely r/t edema – no reliable I/O recorded, no wts recorded
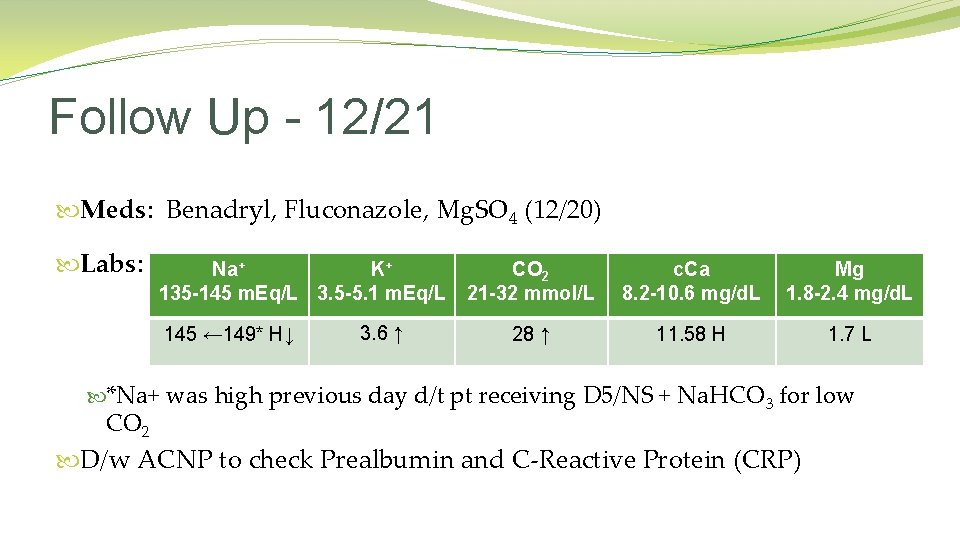
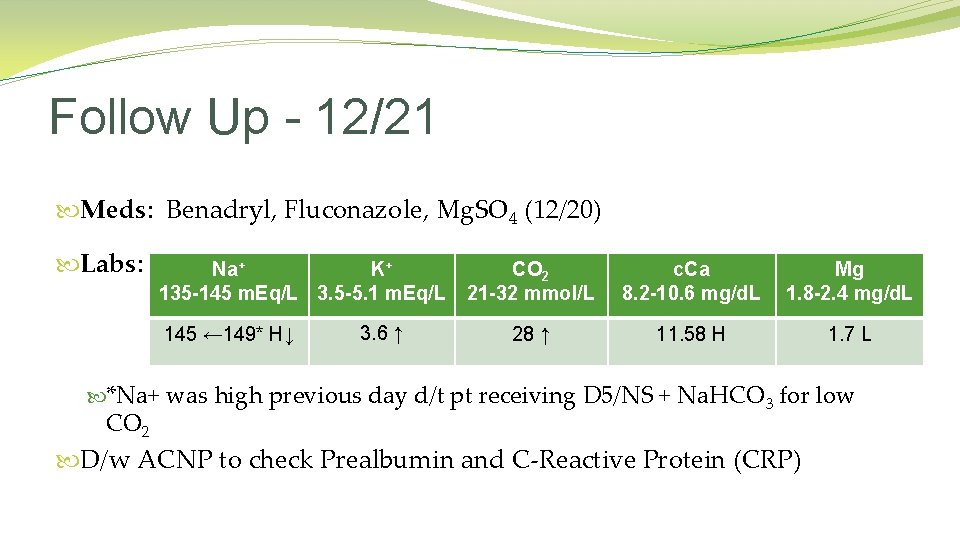
Follow Up - 12/21 Meds: Benadryl, Fluconazole, Mg. SO 4 (12/20) Labs: Na+ K+ 135 -145 m. Eq/L 3. 5 -5. 1 m. Eq/L 145 ← 149* H↓ 3. 6 ↑ CO 2 21 -32 mmol/L c. Ca 8. 2 -10. 6 mg/d. L Mg 1. 8 -2. 4 mg/d. L 28 ↑ 11. 58 H 1. 7 L *Na+ was high previous day d/t pt receiving D 5/NS + Na. HCO 3 for low CO 2 D/w ACNP to check Prealbumin and C-Reactive Protein (CRP)
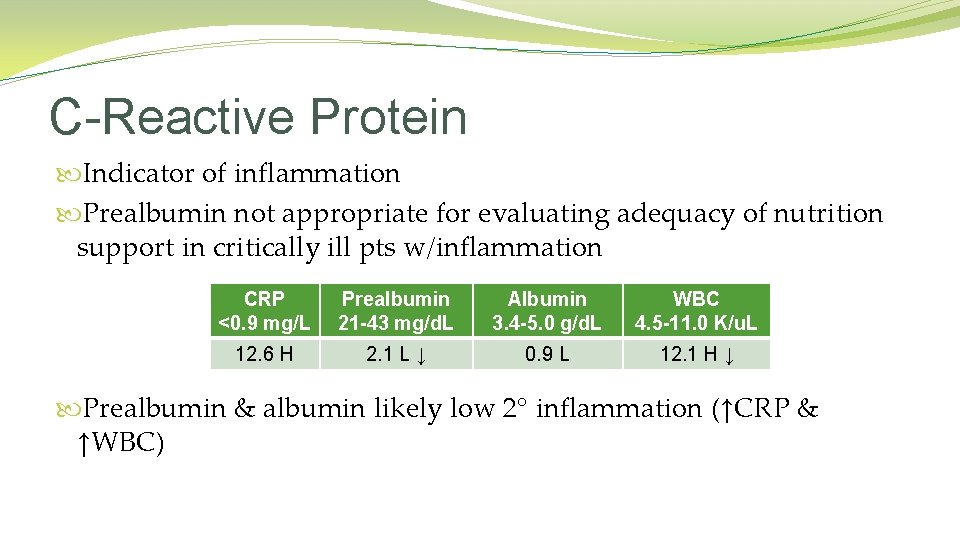
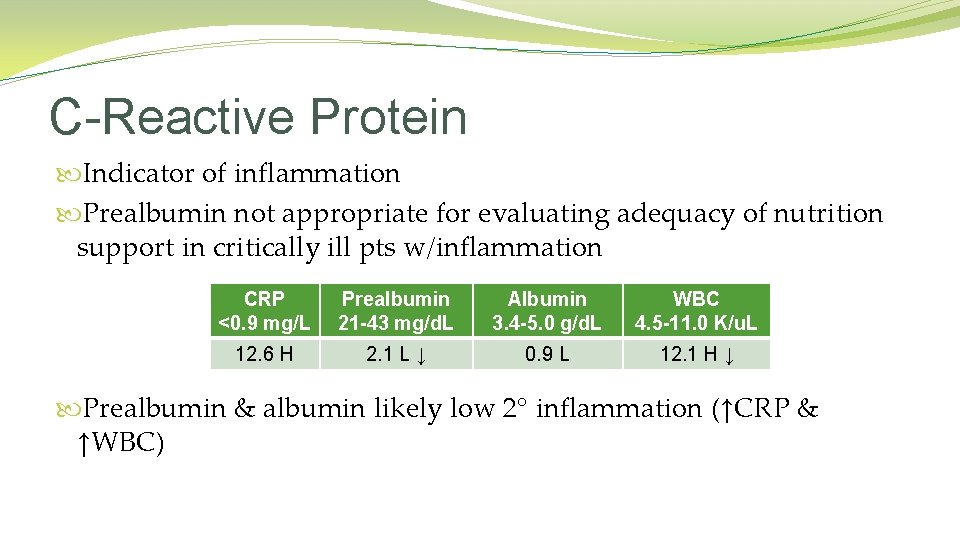
C-Reactive Protein Indicator of inflammation Prealbumin not appropriate for evaluating adequacy of nutrition support in critically ill pts w/inflammation CRP <0. 9 mg/L Prealbumin 21 -43 mg/d. L Albumin 3. 4 -5. 0 g/d. L WBC 4. 5 -11. 0 K/u. L 12. 6 H 2. 1 L ↓ 0. 9 L 12. 1 H ↓ Prealbumin & albumin likely low 2° inflammation (↑CRP & ↑WBC)

Nutrition Care Plan �Dx: Altered GI function R/T ? zinc deficiency vs. unknown etiology AEB stool output of 800 m. L/24 hrs. �Goal: Decrease stool output to <600 m. L/24 hrs �Plan: 1. 2. 3. 4. 5. 6. 7. 8. Rec. Octreotide & Cholestyramine Rec. Lactinex Add 25 mg Zn to TPN x 10 days Remove Ca from TPN Decrease Reglan to 5 mg BID Rec. GI consult Trial trophic feeds of Vivonex @ 20 m. L/hr – do not advance Strict I/O’s �Monitor: Stool output, labs, wt, GI input, TF tolerance, I/O’s

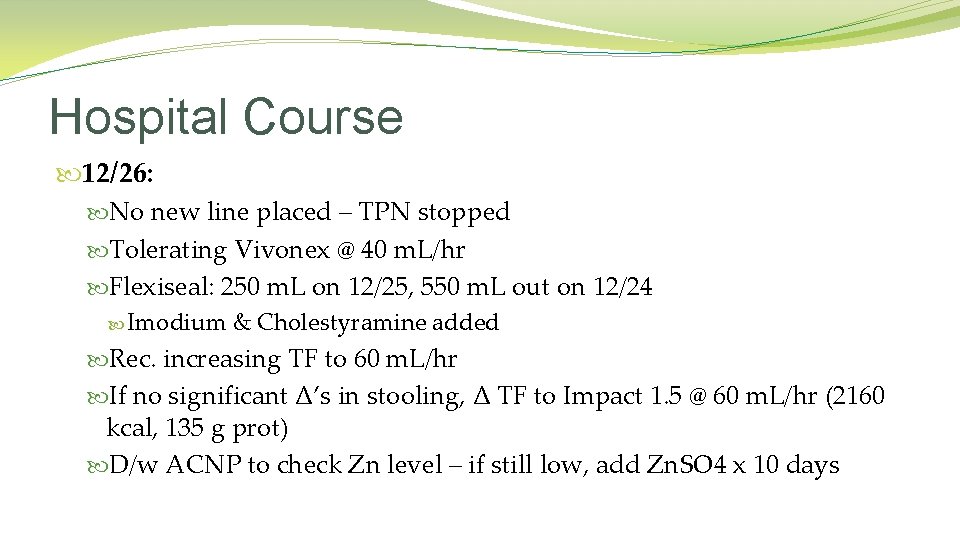
Hospital Course 12/24: TPN: 2. 5 L Non-Standard (2185 kcal, 90 g prot) TF: Vivonex @ 20 m. L/hr (480 kcal, 24 g prot) R subclavian central line infection – plan for new line on L GI consulted – did not see pt, rec. d/c Reglan W/Reglan, no significant residuals, no vomiting Flexiseal: 1. 2 L out on 12/23, 770 m. L out on 12/22 (Neg. for C. diff) Cont. TPN Rec. Imodium & Cholestyramine Trial increase Vivonex to 40 m. L/hr if stool decreases
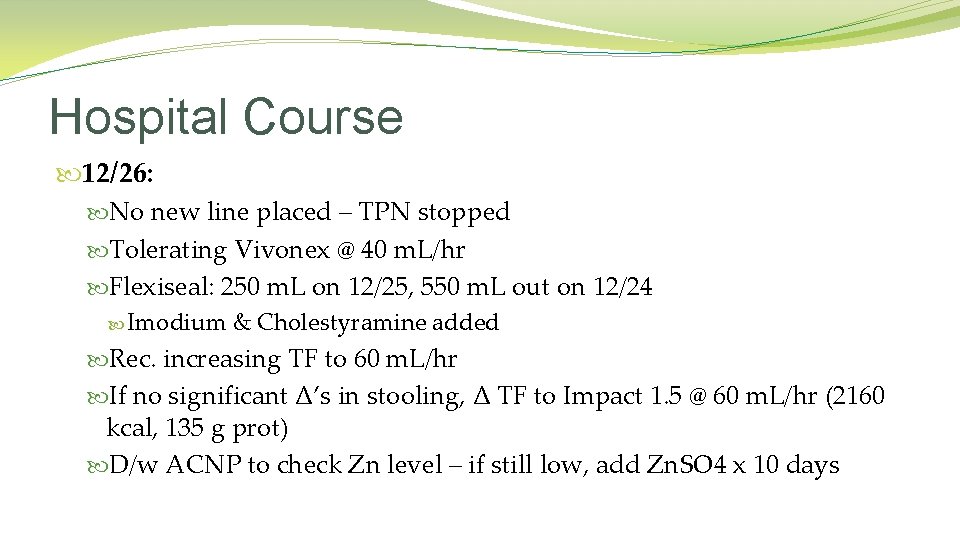
Hospital Course 12/26: No new line placed – TPN stopped Tolerating Vivonex @ 40 m. L/hr Flexiseal: 250 m. L on 12/25, 550 m. L out on 12/24 Imodium & Cholestyramine added Rec. increasing TF to 60 m. L/hr If no significant Δ’s in stooling, Δ TF to Impact 1. 5 @ 60 m. L/hr (2160 kcal, 135 g prot) D/w ACNP to check Zn level – if still low, add Zn. SO 4 x 10 days
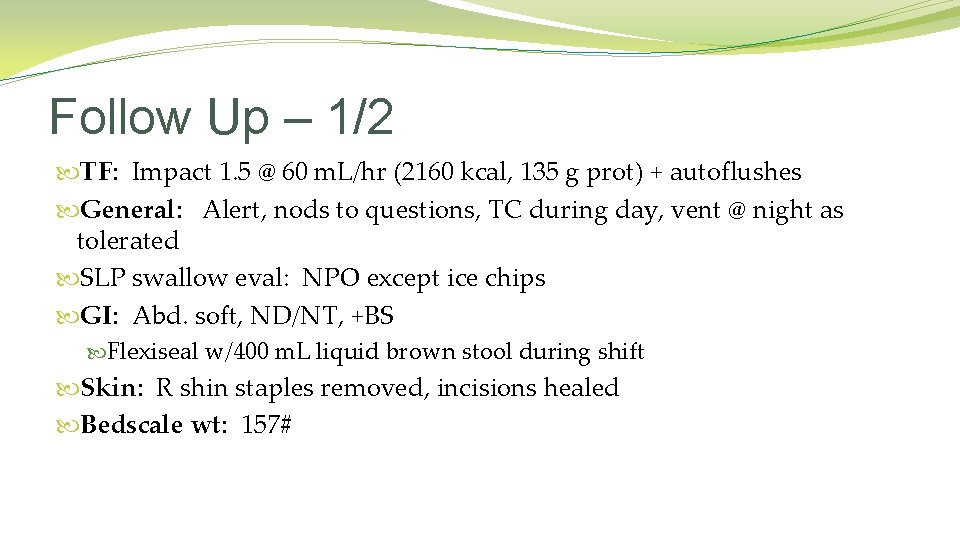
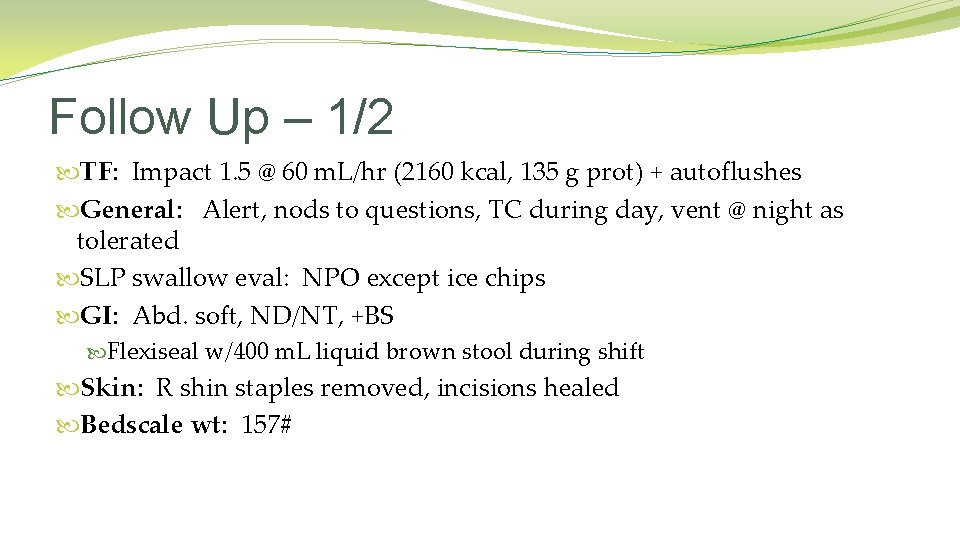
Follow Up – 1/2 TF: Impact 1. 5 @ 60 m. L/hr (2160 kcal, 135 g prot) + autoflushes General: Alert, nods to questions, TC during day, vent @ night as tolerated SLP swallow eval: NPO except ice chips GI: Abd. soft, ND/NT, +BS Flexiseal w/400 m. L liquid brown stool during shift Skin: R shin staples removed, incisions healed Bedscale wt: 157#
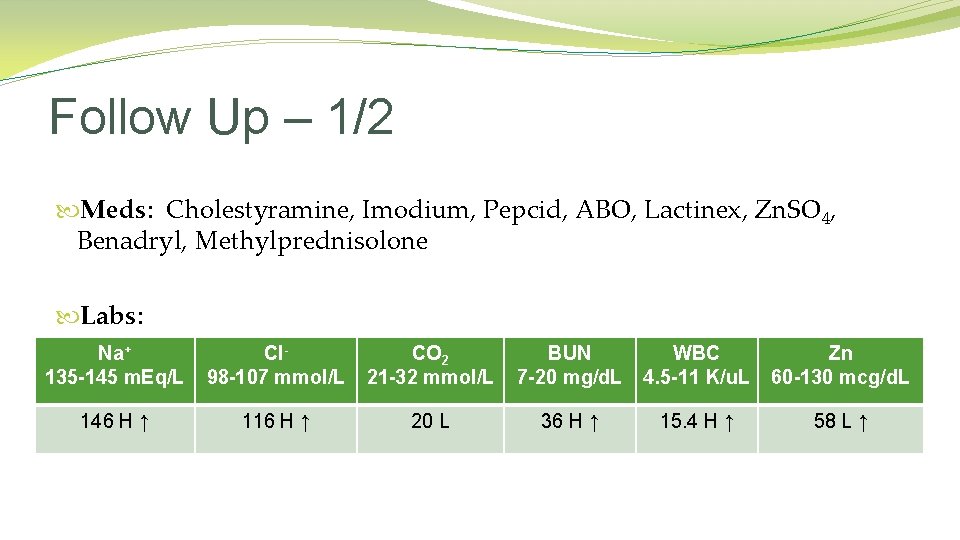
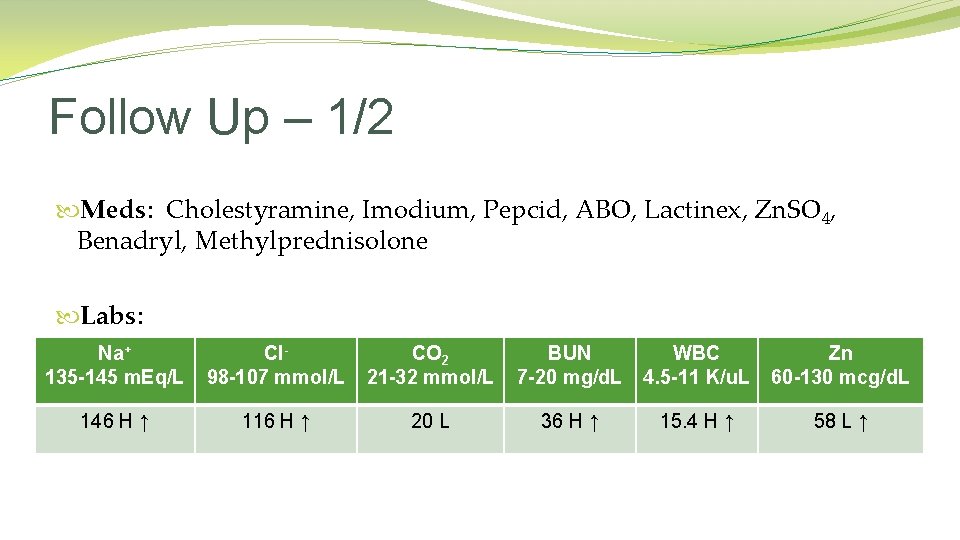
Follow Up – 1/2 Meds: Cholestyramine, Imodium, Pepcid, ABO, Lactinex, Zn. SO 4, Benadryl, Methylprednisolone Labs: Na+ 135 -145 m. Eq/L Cl 98 -107 mmol/L CO 2 21 -32 mmol/L BUN 7 -20 mg/d. L WBC 4. 5 -11 K/u. L Zn 60 -130 mcg/d. L 146 H ↑ 116 H ↑ 20 L 36 H ↑ 15. 4 H ↑ 58 L ↑
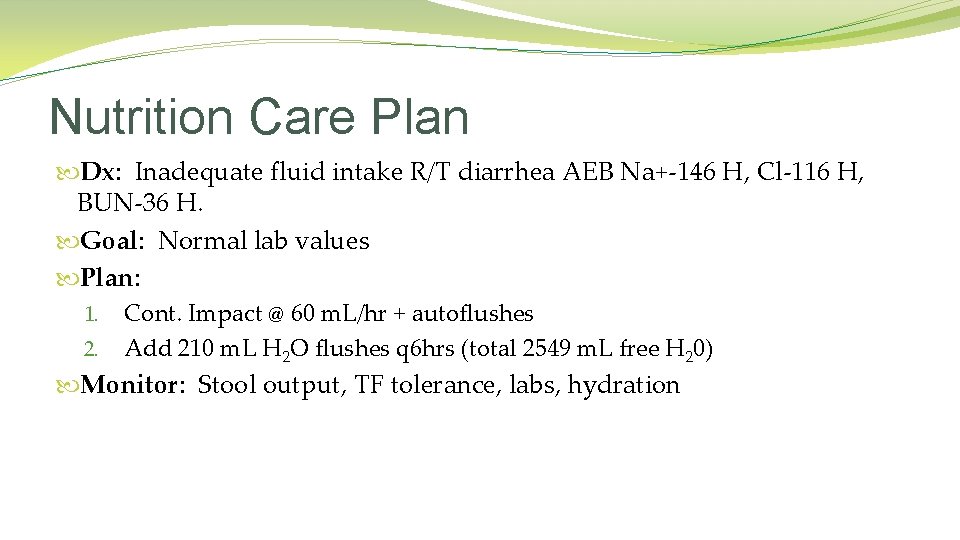
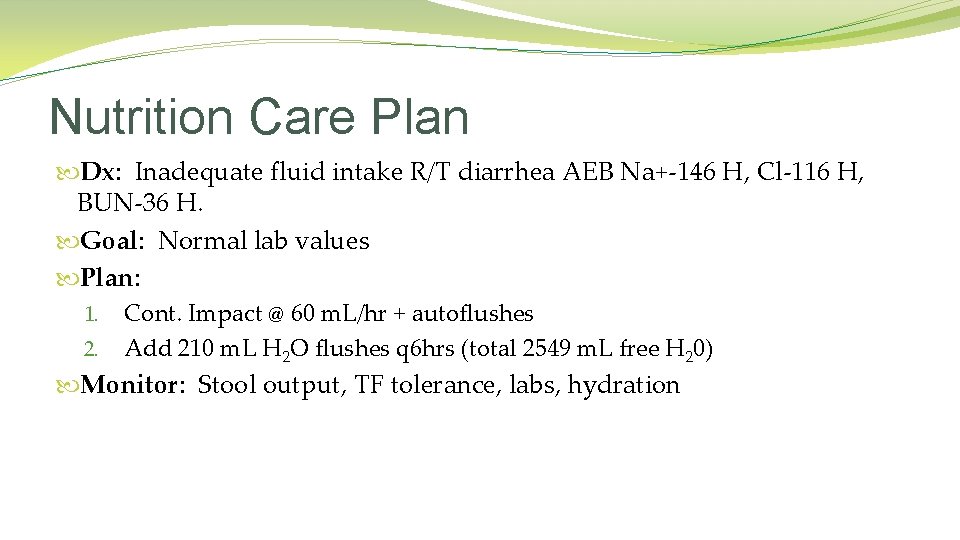
Nutrition Care Plan Dx: Inadequate fluid intake R/T diarrhea AEB Na+-146 H, Cl-116 H, BUN-36 H. Goal: Normal lab values Plan: 1. Cont. Impact @ 60 m. L/hr + autoflushes 2. Add 210 m. L H 2 O flushes q 6 hrs (total 2549 m. L free H 20) Monitor: Stool output, TF tolerance, labs, hydration

Follow Up – 1/8 � 1/4: �Off vent – pt “coughed” out trach �NGT removed �MBS : Mild-mod pharyngeal dysphagia w/delayed swallow & silent asp. �Diet: Mechanical Soft, Nectar Thick Liquids �General: Alert & oriented, able to converse �Drinking liquids, not eating a lot of solid foods; willing to try Resource Shake Thickened �GI: Flexiseal w/350 m. L liquid green stool during shift; abd. ND/NT +BS �Skin: Less anasarcic in BUE, bandage over throat stoma �Bedscale wt: 138# ← 157# (1/2) *Wt loss likely r/t less edema
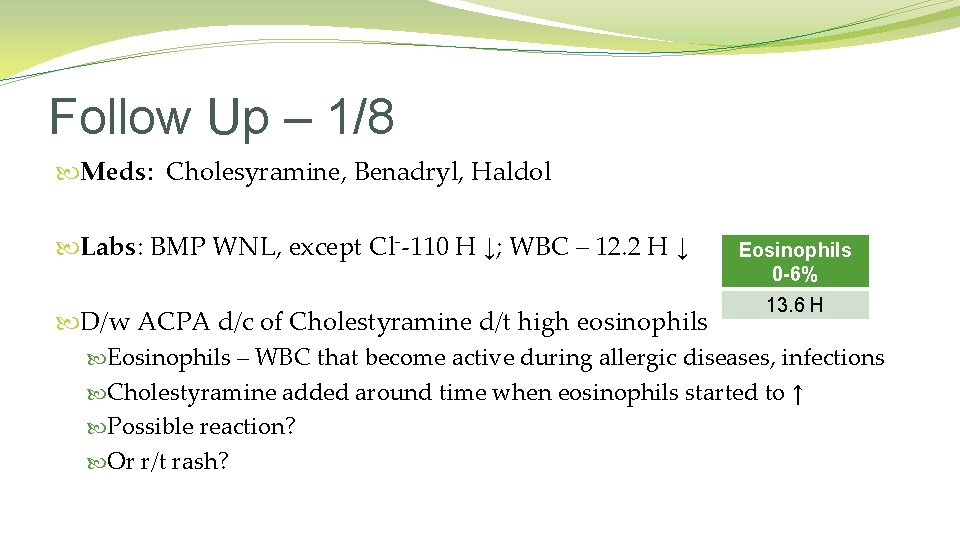
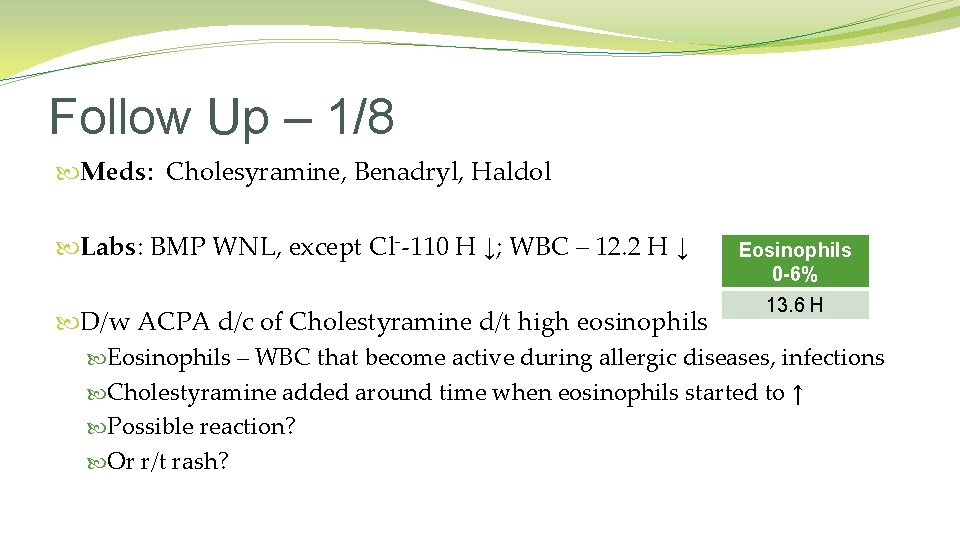
Follow Up – 1/8 Meds: Cholesyramine, Benadryl, Haldol Labs: BMP WNL, except Cl--110 H ↓; WBC – 12. 2 H ↓ Eosinophils 0 -6% 13. 6 H D/w ACPA d/c of Cholestyramine d/t high eosinophils Eosinophils – WBC that become active during allergic diseases, infections Cholestyramine added around time when eosinophils started to ↑ Possible reaction? Or r/t rash?
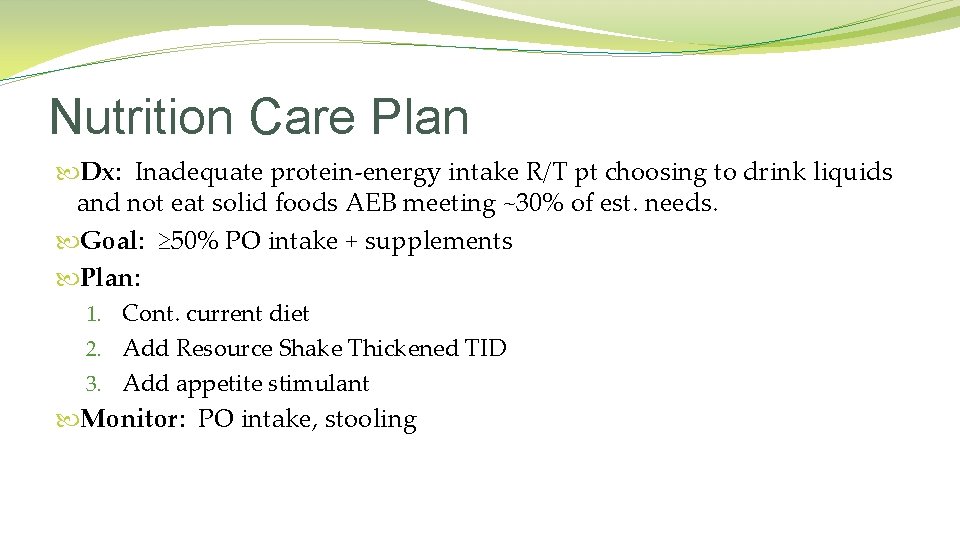
Nutrition Care Plan Dx: Inadequate protein-energy intake R/T pt choosing to drink liquids and not eat solid foods AEB meeting ~30% of est. needs. Goal: ≥ 50% PO intake + supplements Plan: 1. Cont. current diet 2. Add Resource Shake Thickened TID 3. Add appetite stimulant Monitor: PO intake, stooling
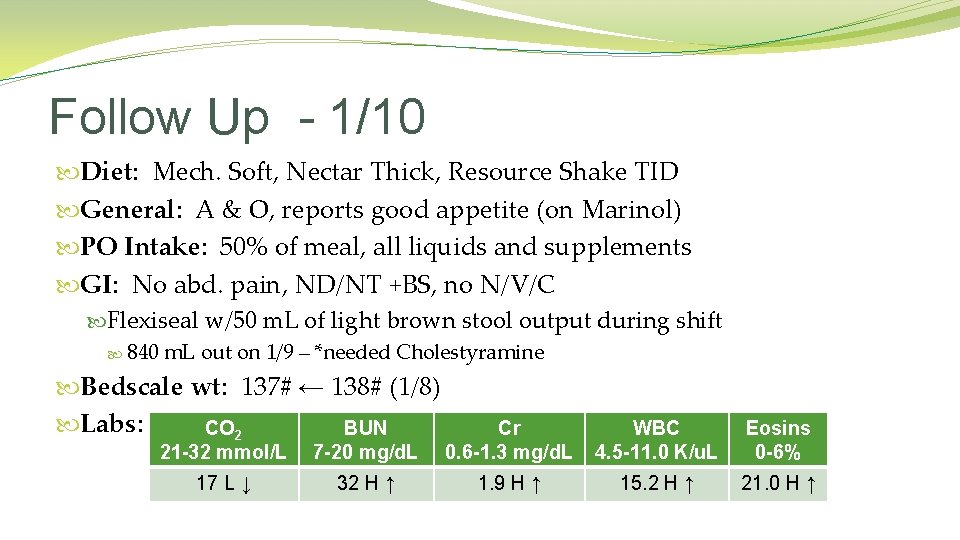
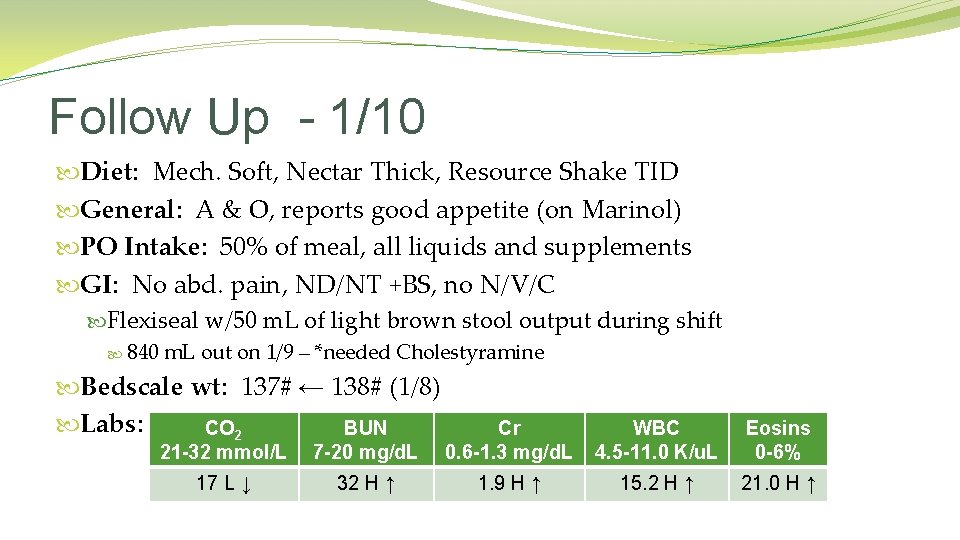
Follow Up - 1/10 Diet: Mech. Soft, Nectar Thick, Resource Shake TID General: A & O, reports good appetite (on Marinol) PO Intake: 50% of meal, all liquids and supplements GI: No abd. pain, ND/NT +BS, no N/V/C Flexiseal w/50 m. L of light brown stool output during shift 840 m. L out on 1/9 – *needed Cholestyramine Bedscale wt: 137# ← 138# (1/8) Labs: CO 2 BUN 21 -32 mmol/L 7 -20 mg/d. L Cr 0. 6 -1. 3 mg/d. L 17 L ↓ 32 H ↑ 1. 9 H ↑ WBC 4. 5 -11. 0 K/u. L Eosins 0 -6% 15. 2 H ↑ 21. 0 H ↑

Nutrition Care Plan Dx: No acute nutrition problems @ this time. Goal: ≥ 75% PO intake Plan: 1. Cont. current diet & supplements 2. Add Imodium – d/w ACPA Monitor: PO intake, stooling GG LIVED HAPPILY EVER AFTER…
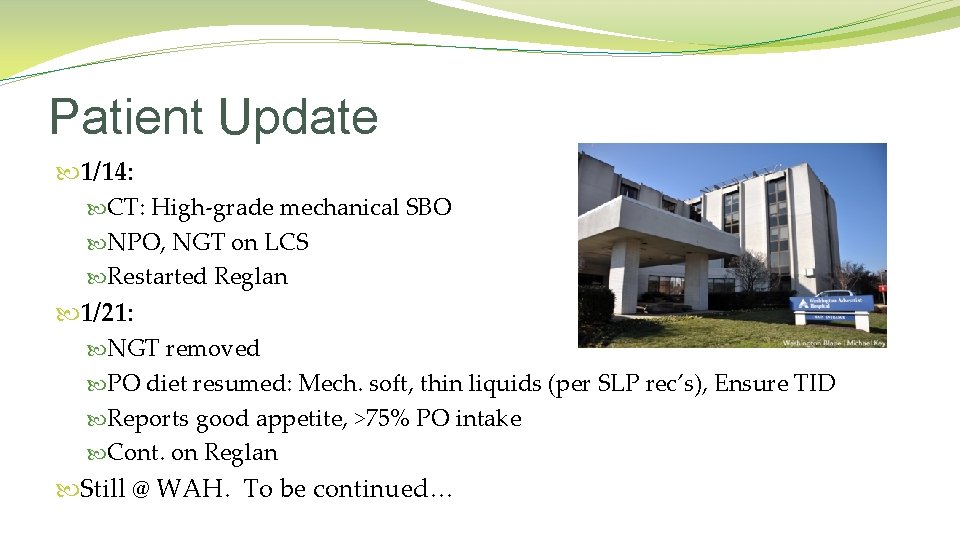
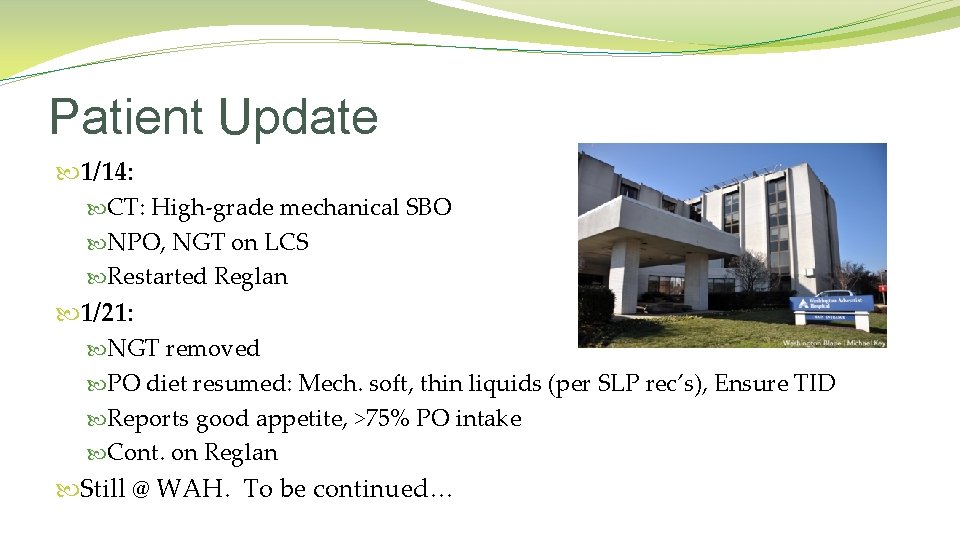
Patient Update 1/14: CT: High-grade mechanical SBO NPO, NGT on LCS Restarted Reglan 1/21: NGT removed PO diet resumed: Mech. soft, thin liquids (per SLP rec’s), Ensure TID Reports good appetite, >75% PO intake Cont. on Reglan Still @ WAH. To be continued…
Questions?

 Charles snead
Charles snead Por eso estamos aqui conmigo puedes contar
Por eso estamos aqui conmigo puedes contar False projection in paralytic squint
False projection in paralytic squint Jesus heals a paralytic
Jesus heals a paralytic The paralytic man by the pool
The paralytic man by the pool Lumbagon
Lumbagon Neostigmin paralytisk ileus
Neostigmin paralytisk ileus Gas-filled bowel loops in abdomen meaning
Gas-filled bowel loops in abdomen meaning Visible peristalsis indicates
Visible peristalsis indicates Epidemiologi ileus obstruktif
Epidemiologi ileus obstruktif Proelastaza
Proelastaza Mekanisk ileus
Mekanisk ileus Feaculent
Feaculent Gootsteengeruisen buik
Gootsteengeruisen buik Sodexo accounts payable
Sodexo accounts payable Cartes sodexo perdues
Cartes sodexo perdues Sodexo energie et maintenance
Sodexo energie et maintenance Sodexo dietetic internship interview questions
Sodexo dietetic internship interview questions Sodexo dietetic internship
Sodexo dietetic internship Vital pass
Vital pass Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Nutrition and diet therapy nursing
Nutrition and diet therapy nursing Small bowel obstruction nutrition management
Small bowel obstruction nutrition management Medical nutrition therapy for stroke
Medical nutrition therapy for stroke Bioness bits cost
Bioness bits cost Psychoanalytic therapy is to as humanistic therapy is to
Psychoanalytic therapy is to as humanistic therapy is to Psychoanalytic vs humanistic
Psychoanalytic vs humanistic Bamse för de yngsta
Bamse för de yngsta Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Kanaans land
Kanaans land Vad är hsil
Vad är hsil Boverket ka
Boverket ka Romarriket tidslinje
Romarriket tidslinje Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? Informationskartläggning
Informationskartläggning Typiska novell drag
Typiska novell drag Tack för att ni har lyssnat
Tack för att ni har lyssnat Matematisk modellering eksempel
Matematisk modellering eksempel Centrum för kunskap och säkerhet
Centrum för kunskap och säkerhet Shivaismen
Shivaismen Kyssande vind analys
Kyssande vind analys