Medical Nutrition Therapy in Neurological Disorders Part 1
- Slides: 50
Medical Nutrition Therapy in Neurological Disorders Part 1
Nutrition and Neurologic Disease • • May have nutritional etiologies resulting from deficiency or excess May be nonnutritional in origin but have significant nutritional implications
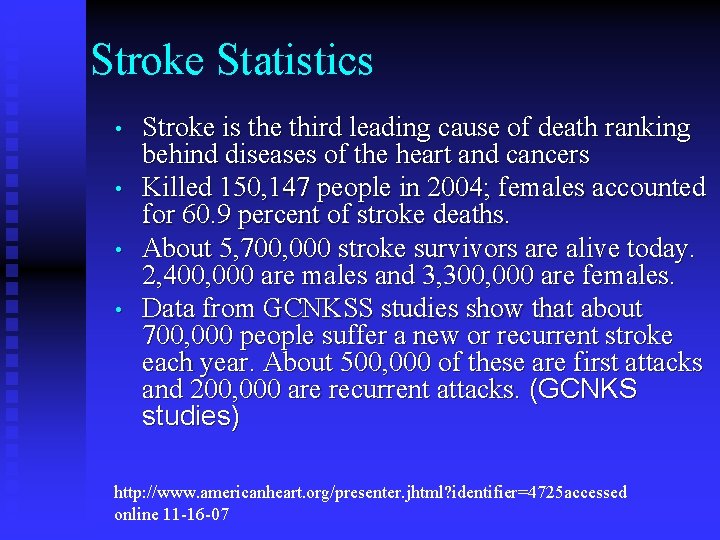
Stroke Statistics • • Stroke is the third leading cause of death ranking behind diseases of the heart and cancers Killed 150, 147 people in 2004; females accounted for 60. 9 percent of stroke deaths. About 5, 700, 000 stroke survivors are alive today. 2, 400, 000 are males and 3, 300, 000 are females. Data from GCNKSS studies show that about 700, 000 people suffer a new or recurrent stroke each year. About 500, 000 of these are first attacks and 200, 000 are recurrent attacks. (GCNKS studies) http: //www. americanheart. org/presenter. jhtml? identifier=4725 accessed online 11 -16 -07
Stroke Statistics • • From 1992 to 2002 the death rate from stroke declined 13. 8 percent, but the actual number of stroke deaths rose 6. 9 percent. A leading cause of functional disability – 15 -30% permanently disabled Primary Prevention of Ischemic Stroke, AHA/ASA Guideline, Stroke 2006; 37: 1583 -1633, accessed online 11 -16 -06
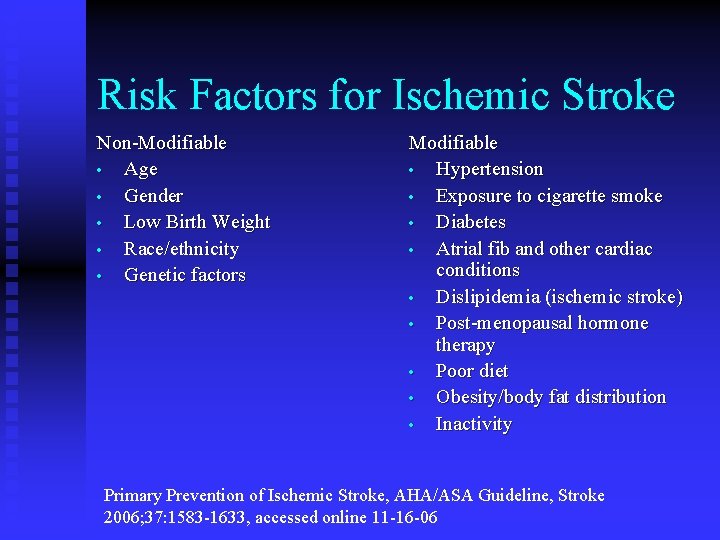
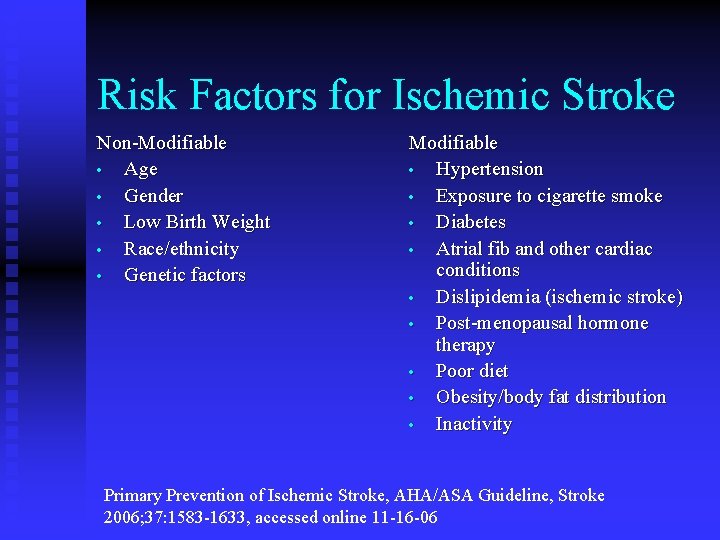
Risk Factors for Ischemic Stroke Non-Modifiable • Age • Gender • Low Birth Weight • Race/ethnicity • Genetic factors Modifiable • Hypertension • Exposure to cigarette smoke • Diabetes • Atrial fib and other cardiac conditions • Dislipidemia (ischemic stroke) • Post-menopausal hormone therapy • Poor diet • Obesity/body fat distribution • Inactivity Primary Prevention of Ischemic Stroke, AHA/ASA Guideline, Stroke 2006; 37: 1583 -1633, accessed online 11 -16 -06
Pathophysiology of Stroke • 85% of strokes caused by a thromboembolic event (related to atherosclerosis, hypertension, diabetes, gout) • Embolic stroke: cholesterol plaque is dislodged from vessel, travels to the brain, blocks an artery • Thrombotic stroke: cholesterol plaque within an artery ruptures, platelets aggregate and clog a narrow artery
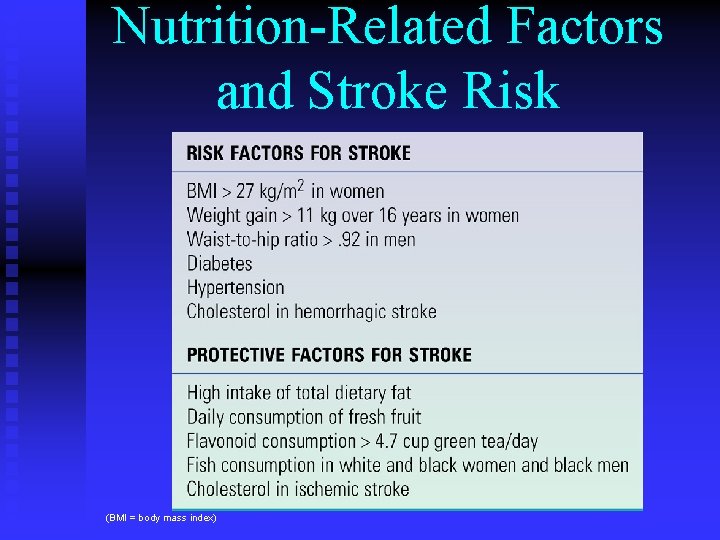
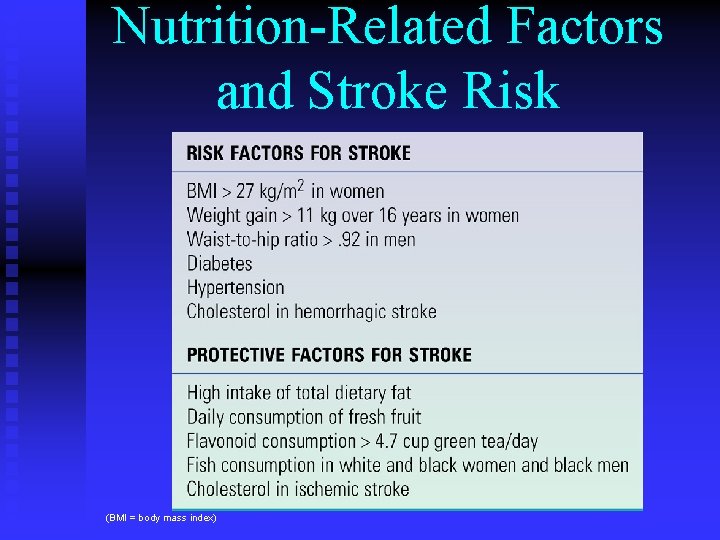
Nutrition-Related Factors and Stroke Risk (BMI = body mass index)
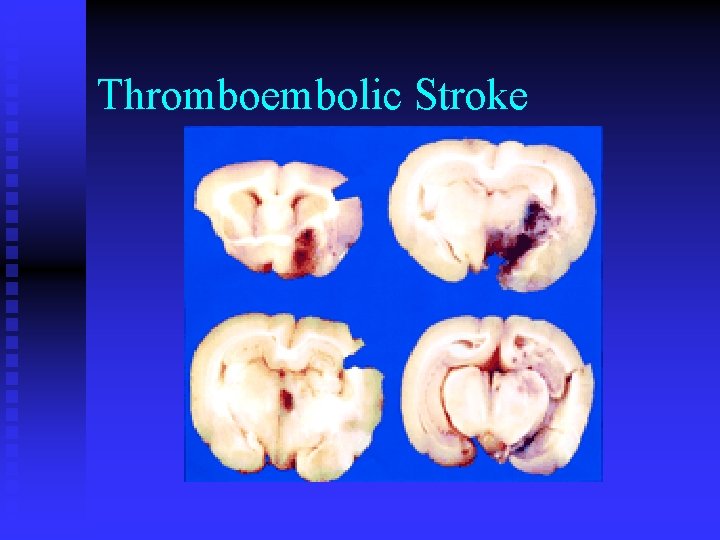
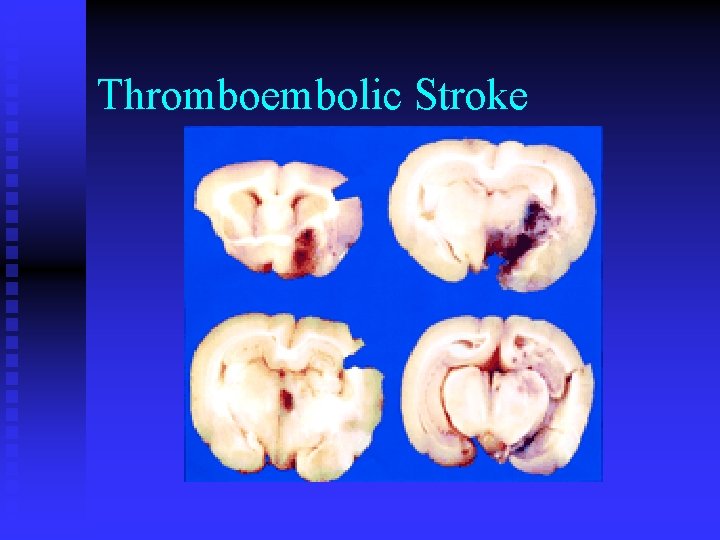
Thromboembolic Stroke
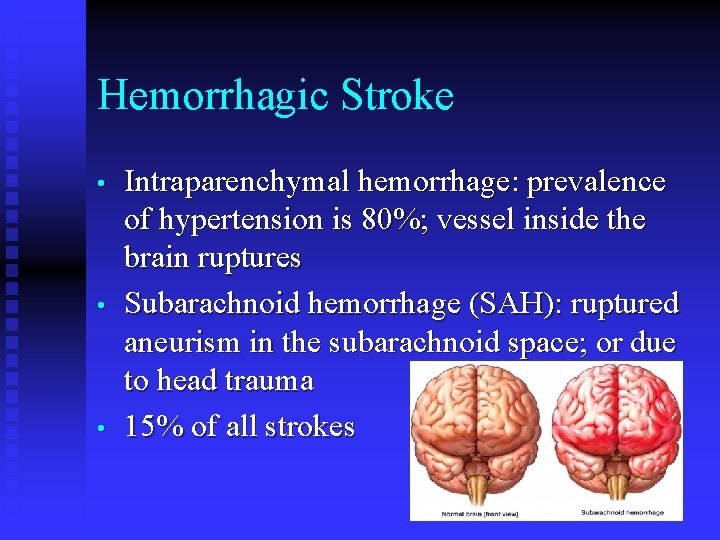
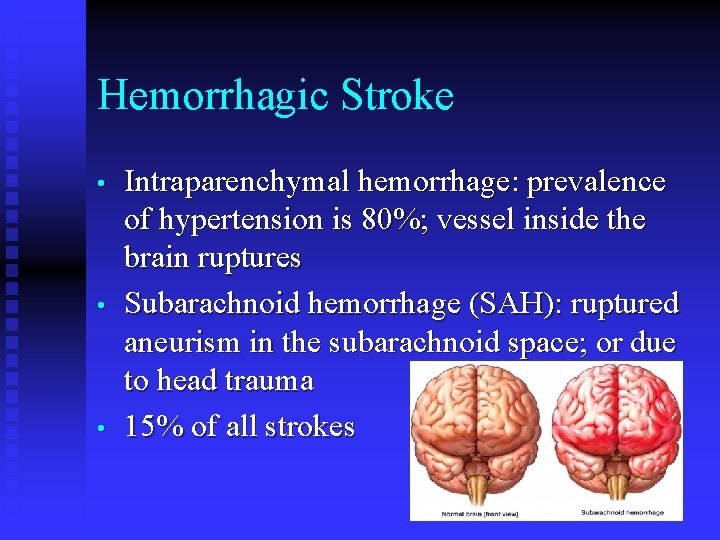
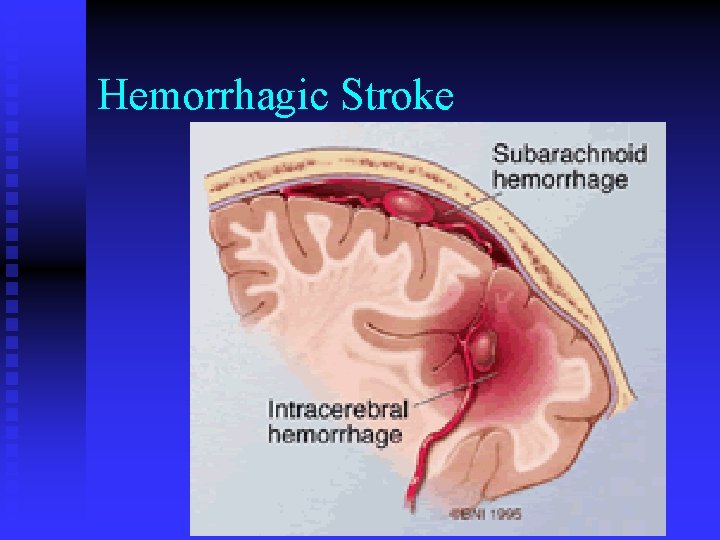
Hemorrhagic Stroke • • • Intraparenchymal hemorrhage: prevalence of hypertension is 80%; vessel inside the brain ruptures Subarachnoid hemorrhage (SAH): ruptured aneurism in the subarachnoid space; or due to head trauma 15% of all strokes
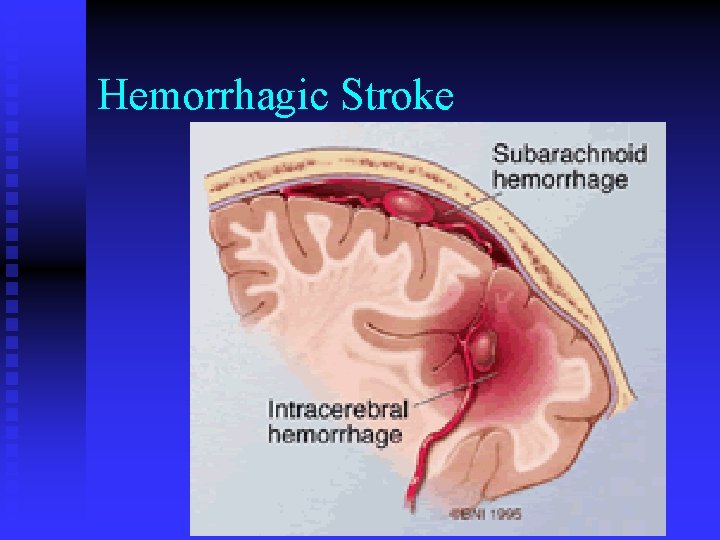
Hemorrhagic Stroke
Medical Treatment for Stroke • • Thrombolytic or “clot-busting” drugs to restore perfusion to affected areas within 6 hours of onset of stroke Controlling intracranial pressure (ICP) while maintaining sufficient perfusion of the brain
Nutritional Management in Stroke • • • Primary prevention Acute management (screening for dysphagia and nutritional risk) Intervention for swallowing disorders via consistency changes
AHA Guidelines for Primary Prevention of CVD and Stroke: 2006 Update • • • Smoking: complete cessation (Class I, evidence level B Avoid exposure to environmental tobacco smoke (Class IIA, evidence C) BP control: goal <140/90 mm. Hg with lower targets in some subgroups (<130/80 in diabetes) Goldstein et al, Primary Prevention of Ischemic Stroke, Stroke 2006; 37: 15831633)
AHA Guidelines for Primary Prevention of CVD and Stroke: 2006 Update • Blood lipid mgt: • NCP III guidelines for pts who have not had a stroke and have high TC or non-HDL-C w/ high TG • Pts with known CAD and high risk HTN even w/ normal LDL treat with lifestyle/statin (Class I, evidence A) • Rec wt loss, ↑ physical activity, smoking cessation, niacin or gemfibrozil (Class IIA, evidence B) Goldstein et al, Primary Prevention of Ischemic Stroke, Stroke 2006; 37: 1583 -1633)
AHA Diet/Lifestyle Guidelines for Primary Prevention of CVD/Stroke: 2006 Update • • • Reduced intake of sodium and increased intake of potassium to lower blood pressure (Class I, evidence A) Recommended sodium intake <2. 3 g/day; potassium >4. 7 g/day DASH diet emphasizing fruits, vegetables, lowfat dairy products is recommended to lower BP (Class I, evidence A) High fruit and vegetable intake may lower risk of stroke (Evidence C) Wt reduction is recommended because it lowers BP Increased physical activity (>30 minutes of moderateintensity activity daily) Pearson et al. (Circulation. 2002; 106: 388 -391. )
Lipids and Stroke • • • Cholesterol is a very weak risk factor for ischemic stroke, in contrast to CAD Cholesterol reduction with diet and nonstatin drugs is not effective in stroke prevention, although reductions in levels of cholesterol are modest Statins produce a statistically significant 25% reduction in the risk of stroke Briel M, et al Am J Med 2004; 117: 596 -606
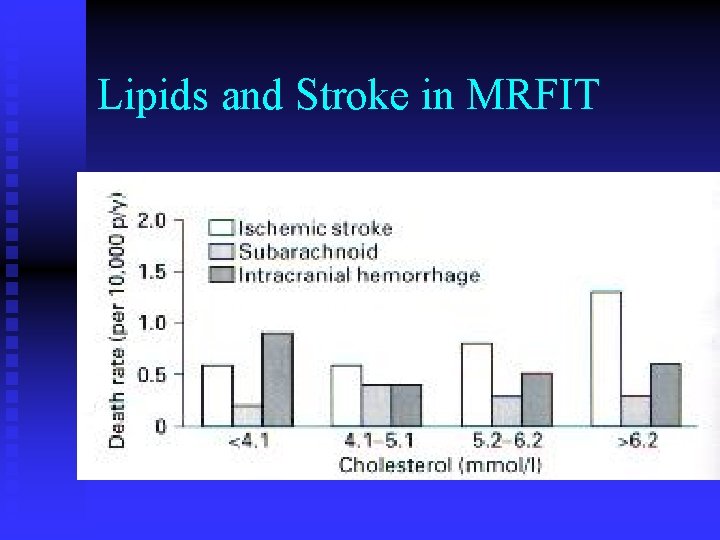
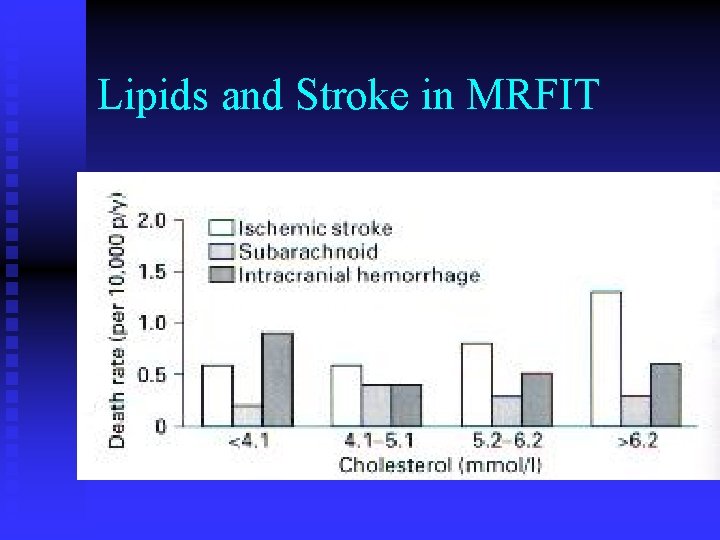
Lipids and Stroke in MRFIT
Lipids and Stroke: ARIC Study • • • Cohort study of 14, 175 men and women After 10 -year followup, there weak and inconsistent associations between ischemic stroke and LDL-C, HDL-C, apo-B, apo-A-1, triglycerides Most consistent relationship was lower risk in women with higher HDL and higher risk with lower TG Shahar E, et al. Stroke, 2003; 34: 623 -631
Lipids and Stroke • • Problem may be the heterogenicity of stroke, although even when looking at homogeneous ischemic stroke, relationship is weak The protective effect of statins may be due to their non-cholesterol-lowering effects.
Relationship Between Fat/Cholesterol and Stroke Risk • • • Dietary cholesterol, MFA, PUFA not related to risk of stroke Low intake of SFA and animal protein associated with risk of intraparenchymal hemorrhage In DCCT trial, intensive treatment lowered LDL, TC and TG and cerebrovascular events
Guidelines for Management of Acute Stroke Rehab (AHA/ASA) • • Dysphagia occurs in 45% of all hospitalized stroke patients; can lead to aspiration pneumonia and death. Malnutrition is present in 15% of patients admitted to the hospital, and this percentage doubles during the first week after stroke. A bedside swallow screening should be completed before oral intake (Evidence Level=B). If the patient’s swallow screening is abnormal, a complete bedside swallow examination is recommended (Evidence Level=I). AHA/ASA Endorsed Veterans Affairs/Department of Defense Clinical Practice Guideline for the Management of Adult Stroke Rehabilitation Care (Stroke. 2005; 36: 2049. )
Dysphagia Treatment- AHA/ASA • • • Dysphagia treatment may involve posture changes, heightening sensory input, swallow maneuvers, active exercise programs, or diet modifications. Dysphagia management may include nonoral feeding and psychological support. At this time, it is unclear how dysphagic patients should be fed after acute stroke. AHA/ASA Endorsed Veterans Affairs/Department of Defense Clinical Practice Guideline for the Management of Adult Stroke Rehabilitation Care (Stroke. 2005; 36: 2049. )
Dysphagia Treatment- AHA/ASA • • The literature supports the use of tube feeding for patients who cannot sustain sufficient oral caloric and/or fluid intake to meet nutritional needs. Limited evidence suggests that percutaneous endoscopic gastrostomy feeding compares favorably with nasogastric tube feeding (Evidence Level=B). AHA/ASA Endorsed Veterans Affairs/Department of Defense Clinical Practice Guideline for the Management of Adult Stroke Rehabilitation Care (Stroke. 2005; 36: 2049. )
FOOD (Feed or Ordinary Diet) Trial • • • Tested feeding strategies after acute stroke including oral supplementation, early vs delayed NG feeding, and NG vs PEG feeding Poor baseline nutritional status is associated with worse outcomes at 6 months. This relationship persists after adjustment for pt’s age, prestroke functional level, living conditions, and severity of stroke. AHA/ASA Guidelines for the Early Management of Patients with Ischemic Stroke. (Stroke. 2005; 36: 916. )
FOOD (Feed or Ordinary Diet) Trial • • • Found no benefit to routine oral supplementation of post-stroke patients who had not been identified as malnourished (1) Early tube feeding was associated with an absolute reduction in risk of death of 5. 8% (p=0. 09) and a reduction in death or poor outcome of 1. 2% (p=0. 7) (2) PEG feeding (vs NG) was associated with an absolute increase in risk of death of 1. 0%, p=0. 9) and an increased risk of death or poor outcome of 7. 8% (p=0. 05). 1: Lancet. 2005 Feb 26 -Mar 4; 365(9461): 755 -63. 2: Lancet. 2005 Feb 26 Mar 4; 365(9461): 764 -72
AHA Guidelines for Early Management of Pts with Ischemic Stroke • • A poor nutritional status was associated with an increased risk of infections including pneumonia, gastrointestinal bleeding, and pressure sores. These data provide a strong rationale for assessment of the patient’s nutritional status at the time of admission. AHA/ASA Guidelines for the Early Management of Patients with Ischemic Stroke. (Stroke. 2005; 36: 916. )
Alzheimer’s Disease • • Most common form of dementia Increases exponentially after age 40 Prevalence in white males at age 100 is 41. 5% Higher prevalence in women (3 X) due to lower mortality
Symptoms of Alzheimer’s Disease • • • Forgetfulness: may forget recent events, activities, names of familiar people or things (anomia). Forget how to do simple tasks, such as brushing teeth, brushing hair Get lost in familiar surroundings Repeat words spoken by others (echolalia) Loss of comprehension (agnosia)
Symptoms of Alzheimer’s Disease (cont) • • • Motor skills deteriorate: loss of reflexes and shuffling gait Bowel and bladder control lost Limb weakness and contractures Intellectual activity ceases Vegetative state
Alzheimer’s Disease Risk Factors • • • Age: risk doubles every five years after age 65 Family history: early onset strongly hereditary; late onset has a genetic component Those with a parent or sibling with AD are 2 -3 times more likely to develop AD
Alzheimer’s Disease Risk Factors • • Head injury Down syndrome Low level of education Female gender
Alzheimer’s Disease Prevention: Research Areas • • AD risk is associated with CVD, hypertension, diabetes AD risk associated with exercise, staying mentally active, social engagement Research ongoing into use of antioxidants (vitamins E and C), ginkgo biloba Research into estrogen and AD suggests that estrogen treatment in postmenopausal women may risk of dementia
Treatment of Alzheimer’s Disease • • • No drug can stop or reverse AD Some drugs may slow progress (tacrine (Cognex®), donepezil (Aricept®), rivastigmine (Exelon®), or galantamine (Razadyne®) Other medications may treat symptoms such as sleeplessness, agitation, wandering, anxiety, and depression National Institutes on Aging, Alzheimer’s Disease Education and Referral Center http: //www. alzheimers. org/treatment. htm
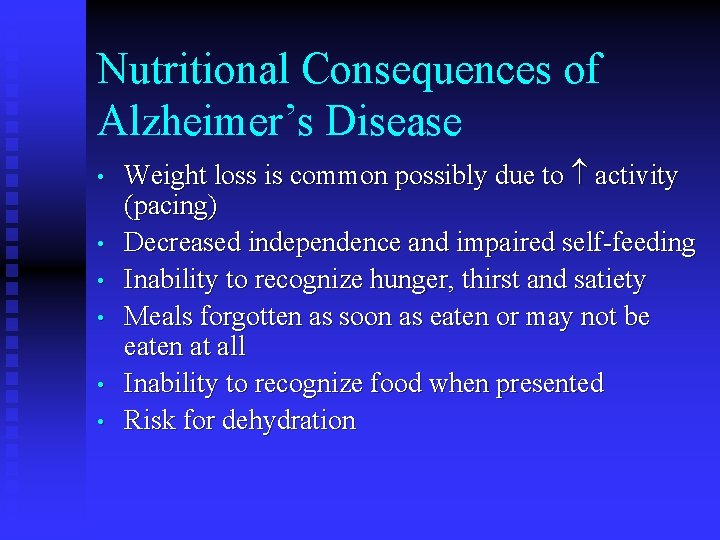
Nutritional Consequences of Alzheimer’s Disease • • • Weight loss is common possibly due to activity (pacing) Decreased independence and impaired self-feeding Inability to recognize hunger, thirst and satiety Meals forgotten as soon as eaten or may not be eaten at all Inability to recognize food when presented Risk for dehydration
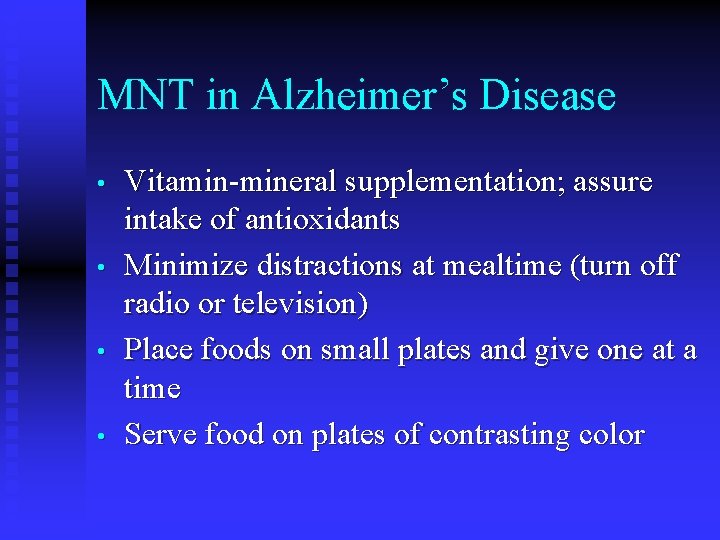
MNT in Alzheimer’s Disease • • Vitamin-mineral supplementation; assure intake of antioxidants Minimize distractions at mealtime (turn off radio or television) Place foods on small plates and give one at a time Serve food on plates of contrasting color
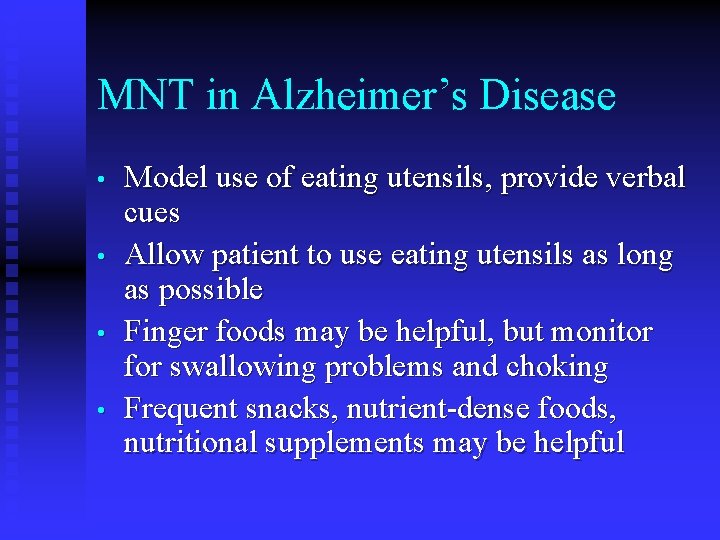
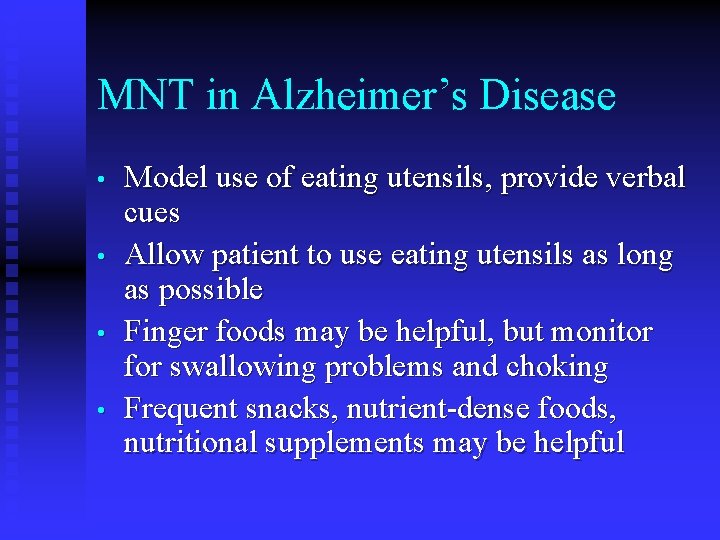
MNT in Alzheimer’s Disease • • Model use of eating utensils, provide verbal cues Allow patient to use eating utensils as long as possible Finger foods may be helpful, but monitor for swallowing problems and choking Frequent snacks, nutrient-dense foods, nutritional supplements may be helpful
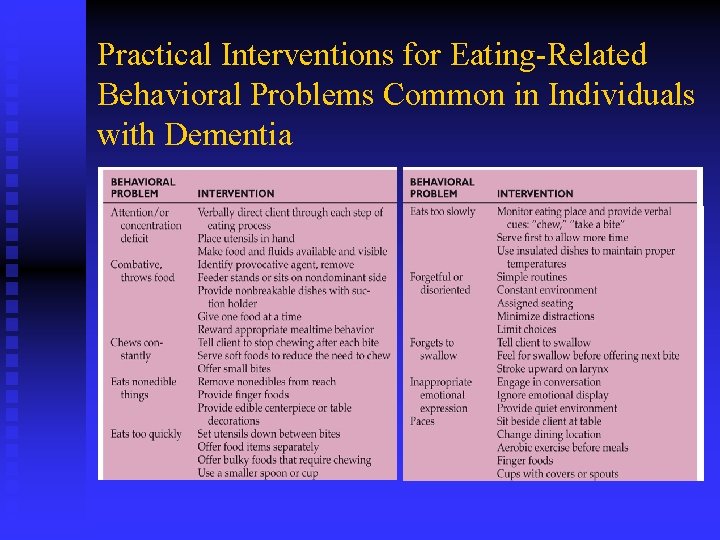
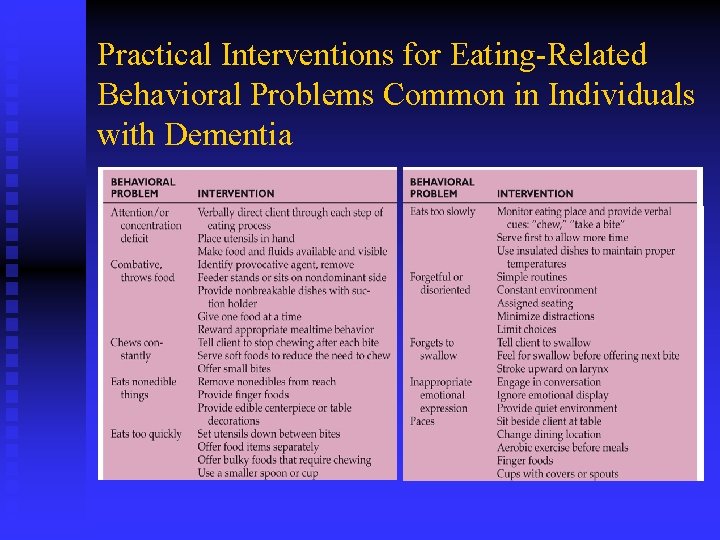
Practical Interventions for Eating-Related Behavioral Problems Common in Individuals with Dementia
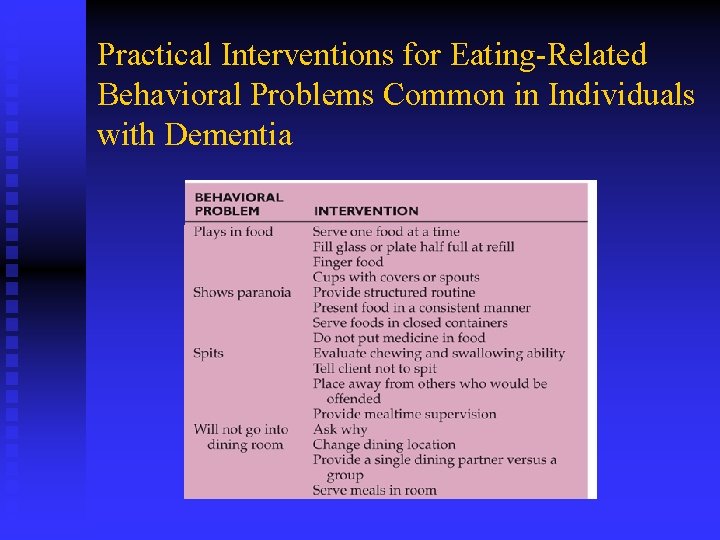
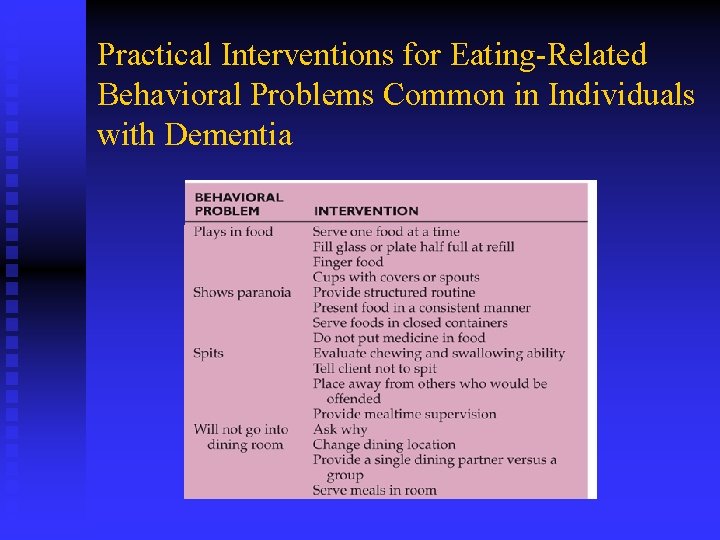
Practical Interventions for Eating-Related Behavioral Problems Common in Individuals with Dementia
Migraine Headache • • Thought to be vascular in origin Throbbing, episodic, and intense History of intercurrent nausea, vomiting, photophobia, visual or olfactory auras Treated with NSAIDs, sympathomimetics, seritonin agonists; prophylaxis with calcium channel blockers, beta-adrenergic blockers, serotonin antagonists
Migraine Headache • • • Headaches may be triggered by food Varies by individual and tolerance thresholds vary over time No general recommendations about food avoidance Foods often cited are citrus fruits, tea, coffee, pork, chocolate, milk, nuts, vegetables, cola drinks Evaluate through food and symptom diary
Myasthenia Gravis (MG) • • Autoimmune disorder of the neuromuscular junction Body makes antibodies to acetylcholine receptors; make them unresponsive to Ach Nervous system signal to the muscle is garbled Relapsing and remitting weakness and fatigability; diplopia, facial muscle weakness, dysphagia (33%)
Myasthenia Gravis (MG) Medical Treatment • • • Anticholinesterases inhibit acetylcholesterase and increase the amount of Ach Removal of the thymus gland Corticosteroids
Myasthenia Gravis (MG) MNT • • • Nutritionally dense foods at the beginning of meals before the patient tires Small frequent meals Time medication with feeding to facilitate optimal swallowing Limit physical activity before meals Don’t encourage food consumption when patient is tired; may aspirate
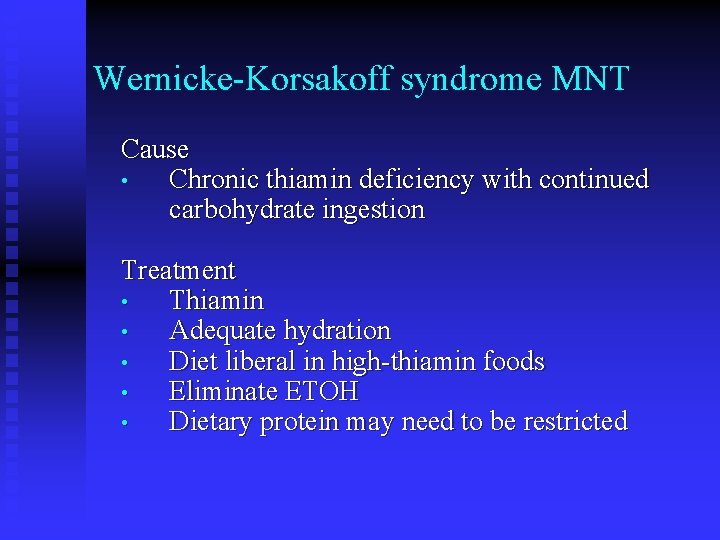
Wernicke-Korsakoff syndrome MNT Cause • Chronic thiamin deficiency with continued carbohydrate ingestion Treatment • Thiamin • Adequate hydration • Diet liberal in high-thiamin foods • Eliminate ETOH • Dietary protein may need to be restricted
Amyotrophic Lateral Sclerosis • • • Also called Lou Gehrig’s Disease Most common motor system disease Progressive denervation atrophy and weakness of muscles Both upper and lower motor neurons are lost in the spinal cord, brain stem, and motor cortex Progresses to death in 2 to 6 years
Amyotrophic Lateral Sclerosis • • • Prevalence constant throughout the world Men affected more than women Age of onset mid-50 s (40 -70) Cause unknown 5% familial, rest sporadic
Amyotrophic Lateral Sclerosis Presentation • • • Muscle weakness commences in the legs and hands and progresses to the proximal arms and oropharynx Voluntary skeletal muscles are at risk for atrophy and complete loss of function Spasticity of jaw muscles resulting in slurred speech Dysphagia, difficulty chewing weight loss Death from respiratory failure
Amyotrophic Lateral Sclerosis Nutritional Implications • • • Dysphagia, chewing, swallowing problems Decreased body fat, lean body mass, nitrogen balance and increased REE as death approaches Late stage patients may not tolerate PEG placement d/t respiratory compromise Initiate discussions about whether to place a feeding tube early in disease process Enteral feedings do not prolong life
Amyotrophic Lateral Sclerosis MNT • • Correlates with ALS Severity Scale (pp 11021103) Emphasize fluids as patients may limit fluids d/t toileting difficulties Get baseline weight; 10% loss increased risk Modify consistency as eating problems develop using easy-chew foods, thickened liquids, using small frequent meals, cool food temperatures
Amyotrophic Lateral Sclerosis MNT • • If nutrition support is planned, use EN Initiate early rather than later; dehydration occurs before malnutrition Purpose of nutrition support should be to enhance quality of life Eventually patients will not be able to manage oral secretions
 Medical nutrition therapy for stroke
Medical nutrition therapy for stroke Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Small bowel obstruction medical nutrition therapy
Small bowel obstruction medical nutrition therapy Fundamentals of nursing nutrition
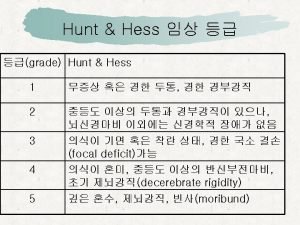
Fundamentals of nursing nutrition World federation of neurological surgeons scale
World federation of neurological surgeons scale Neuro checks pupil size
Neuro checks pupil size Motor function neurological assessment
Motor function neurological assessment What is focal neurological signs
What is focal neurological signs Level of consciousness assessment
Level of consciousness assessment Is adhd a neurological disorder
Is adhd a neurological disorder Mrc grade
Mrc grade Haapsalu neurological rehabilitation centre
Haapsalu neurological rehabilitation centre Neurological based behavior
Neurological based behavior Neurological examination
Neurological examination Muscle power neurological examination
Muscle power neurological examination Neurological exam
Neurological exam Neurological considerations in language acquisition
Neurological considerations in language acquisition What is trait theory in criminology
What is trait theory in criminology Solent physiotherapy
Solent physiotherapy Papilloedema
Papilloedema Neurological disease
Neurological disease Amy lee plastic surgery
Amy lee plastic surgery Ryan waters neurosurgeon
Ryan waters neurosurgeon Neurological observations glasgow coma scale
Neurological observations glasgow coma scale Both psychoanalysis and humanistic therapy stress
Both psychoanalysis and humanistic therapy stress Bioness integrated therapy system occupational therapy
Bioness integrated therapy system occupational therapy Humanistic therapy aims to
Humanistic therapy aims to Medical family therapy
Medical family therapy Jay haley strategic family therapy
Jay haley strategic family therapy Schools of family therapy
Schools of family therapy California medical license for foreign medical graduates
California medical license for foreign medical graduates Gbmc infoweb
Gbmc infoweb Difference between medical report and medical certificate
Difference between medical report and medical certificate Torrance memorial map
Torrance memorial map Cartersville medical center medical records
Cartersville medical center medical records Part part whole addition
Part part whole addition Unit ratio definition
Unit ratio definition Brainpop ratios
Brainpop ratios Technical description
Technical description Parts of a pub
Parts of a pub The phase of the moon you see depends on ______.
The phase of the moon you see depends on ______. Minitab adalah
Minitab adalah Unit 14 physiological disorders examples
Unit 14 physiological disorders examples Unit 14 health and social care level 3
Unit 14 health and social care level 3 Neurocognitive disorders
Neurocognitive disorders Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders Flinders model
Flinders model Assistive technology for emotional disturbance
Assistive technology for emotional disturbance Somatization disorder
Somatization disorder Egodystone
Egodystone