Squint 5 By Prof Dr Ahmad Mostafa Professor

Squint 5 By Prof. Dr. Ahmad Mostafa Professor of Ophthalmology
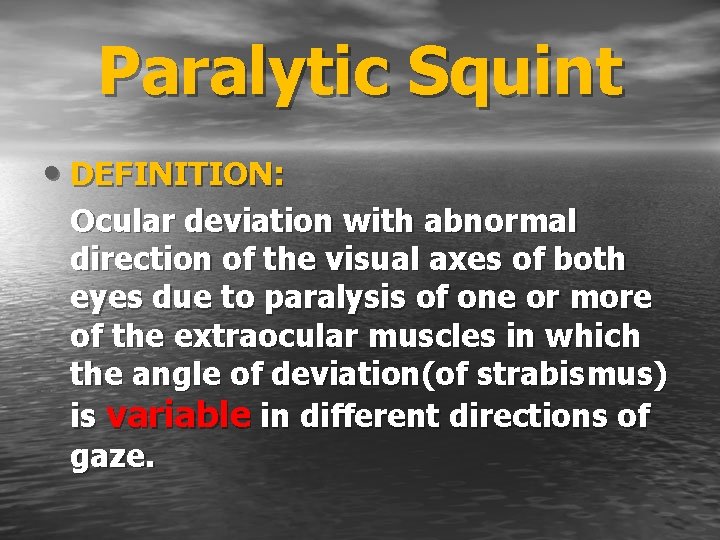
Paralytic Squint • DEFINITION: Ocular deviation with abnormal direction of the visual axes of both eyes due to paralysis of one or more of the extraocular muscles in which the angle of deviation(of strabismus) is variable in different directions of gaze.
AETIOLOGY • (I) Central Causes (= Nuclear Lesions) • (II) Peripheral Causes • (= Nerve lesions, Muscle lesions)
(I) Central Causes (Nuclear lesions) (A) Congenital Ophthalmoplegia Defective development of the nuclei (B) Acquired Ophthalmoplegia
(B) Acquired Ophthalmoplegia • 1. Trauma • 2. Inflammatory • 3. Vascular • 4. Neoplastic • 5. Toxic a. Endogenous intoxication b. Exogenous intoxication • 6. Metabolic
(II) Peripheral Causes: A. Nerve lesions • (1) Congenital • (2) Acquired causes: • 1. Traumatic • 2. Inflammatory • 3. Vascular • 4. Neoplastic
B. Muscle Lesions: • (1) Congenital • (2) Acquired • 1. Traumatic • 2. Myopathic : Myasthenia gravis.
CLINICAL PICTURE (1)Symptoms: • 1. Ocular deviation • 2. Diplopia • 3. Nausea, vomiting, vertigo, dizziness, uncertain gait nausea and vomiting
(2) Signs: • occur in the direction of action of paralysed muscle. 1. Ocular deviation with limitation of the movements of the affected eye 2. Binocular Diplopia 3. False projection 4. Compensatory head posture
1. Squint & Limitation of Ocular Motility 1. Primary ocular deviation : • Occurs in a direction opposite to that of action of the paralysed muscle (as inwards in right L R paralysis). 2. Secondary ocular deviation: • Is deviation of normal eye when it is covered by a screen to force the patient to fix with paralysed eye.
• 3. The angle of secondary deviation: • is much larger than the angle of primary deviation: Due to overaction of the contralateral synergist of the paralysed muscle (a) Normally: Brain sends nerve impulses to the eyes for fixation in any direction which are equally distributed between both eyes Hering’s law).
• (b) When the paralysed eye is fixing: • a) The brain sends more nerve impulses to the • • paralysed muscle to force it to contract. b) At the same time equal amount of these nerve impulses are sent to the synergistic muscle of the other normal eye and so produce overaction of that muscle. c) This leads to increased movement of the normal eye under the cover with increased angle of secondary deviation.
2. Binocular Diplopia • Double vision by the use of both eyes because two retinal images fall on non-corresponding points of retina: 1 - It disappears when one eye is covered: • Unlike uniocular diplopia. 2 - Two different images are seen: • (a) True image (clear → by the fovea of the normal eye). • (b) A false image (blurred → by a point outside the fovea of the paralysed eye).
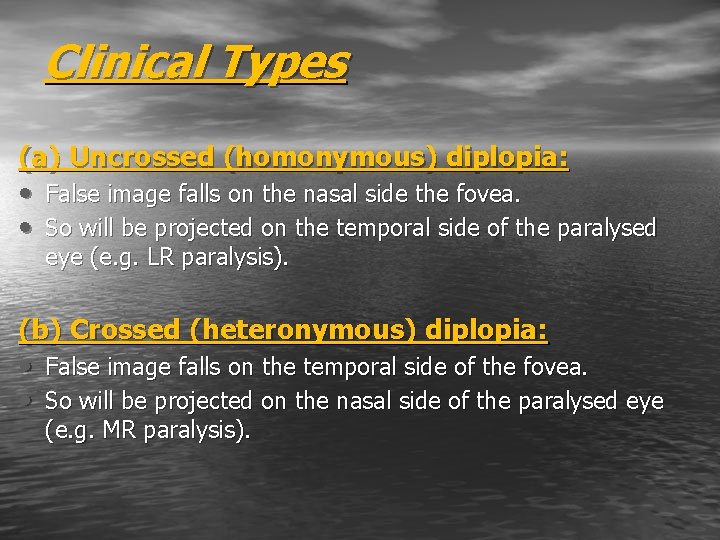
Clinical Types (a) Uncrossed (homonymous) diplopia: • False image falls on the nasal side the fovea. • So will be projected on the temporal side of the paralysed eye (e. g. LR paralysis). (b) Crossed (heteronymous) diplopia: • False image falls on the temporal side of the fovea. • So will be projected on the nasal side of the paralysed eye (e. g. MR paralysis).
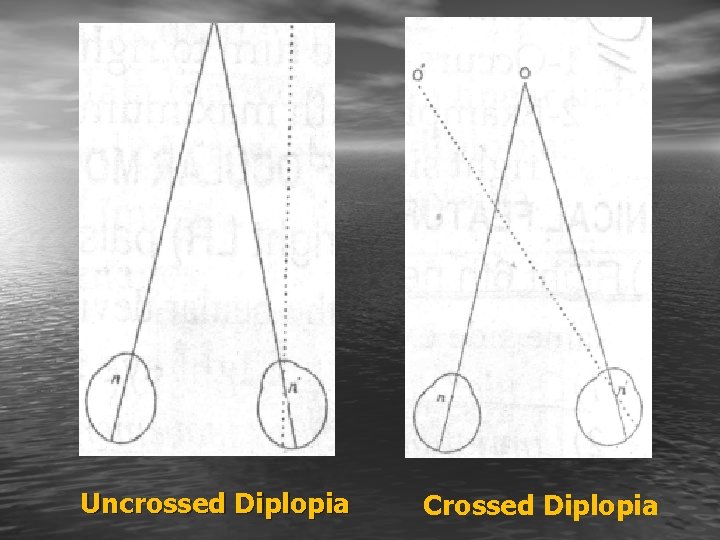
Uncrossed Diplopia Crossed Diplopia
3. False Projection • The affected eye does not see objects in their exact location. • Cause: is due to increased innervation to the paralysed muscle in an effort to force it to act
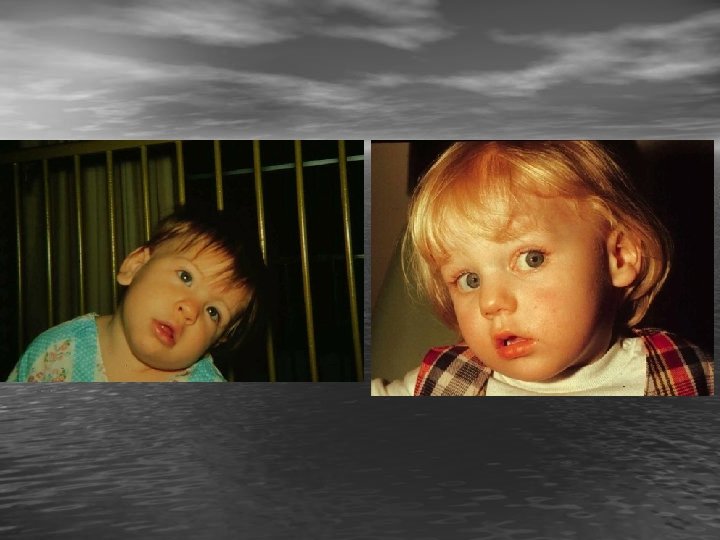
4. Compensatory Head Posture • Aim: To avoid diplopia • Direction: movement of the head is always in the direction of action of the paralysed muscle i. e. in which the diplopia is greater
Compensatory Head Postures • 1. Face turn (to R. or L. ) in Horizontal muscle palsy. • 2. Head tilt (torticollis) towards the shoulder of the side of the higher image i. e. that of the hypotropic eye in Vertical muscle palsy Value: to neutralize the vertical & torsional displacement, so that the 2 images are brought to the same level
• 3. Chin elevation or depression: in an elevator or depressor palsy respectively
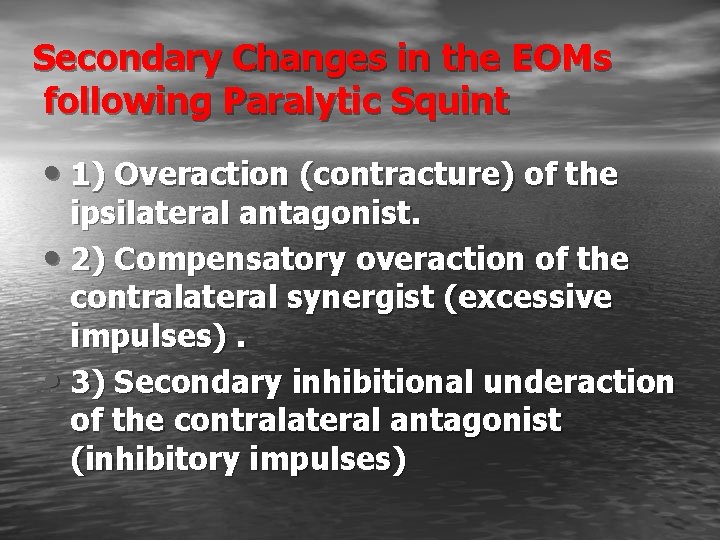
Secondary Changes in the EOMs following Paralytic Squint • 1) Overaction (contracture) of the ipsilateral antagonist. • 2) Compensatory overaction of the contralateral synergist (excessive impulses). • 3) Secondary inhibitional underaction of the contralateral antagonist (inhibitory impulses)
Diagnosis of Paralytic squint • (1) Signs and symptoms: Diplopia , limitation • • of movements, . . . etc. (2) Examination of ocular motility (3) Diplopia chart (4) Hess screen
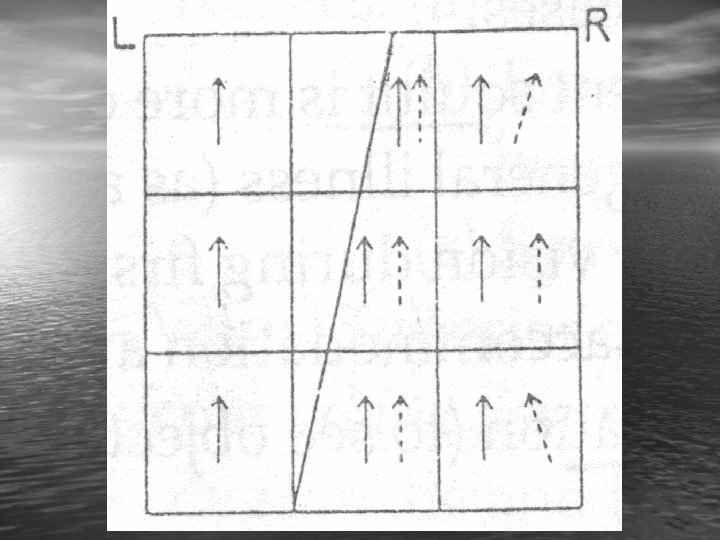
Diplopia chart • 1) A red glass in front of the right eye and • • a green glass in front of the left eye of the patient (to differentiate between the 2 images) in a dark room. 2) A torch with a stenopaeic slit is used to project a linear light. 3) The patient is asked about data to investigate diplopia: – – – 1 - Areas and type (uncrossed or crossed) of diplopia. 2 - Relative position of the 2 images. 3 - Distance between the 2 images.
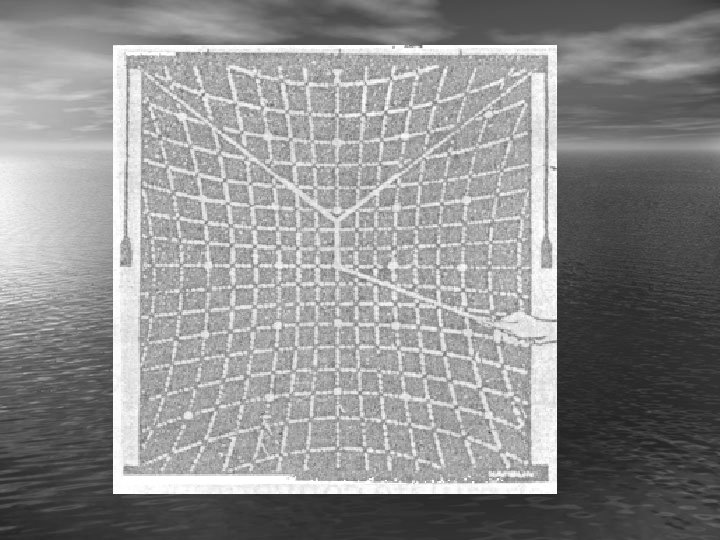
Hess Screen • Aim: • l)To determine the degree of the paralysed muscle. • 2) To determine the secondary changes affecting the other muscles. • Principle: Special screen records the degree of false projection in different directions of gaze by dissociating the images of the 2 eyes with coloured goggles (red and green glasses).
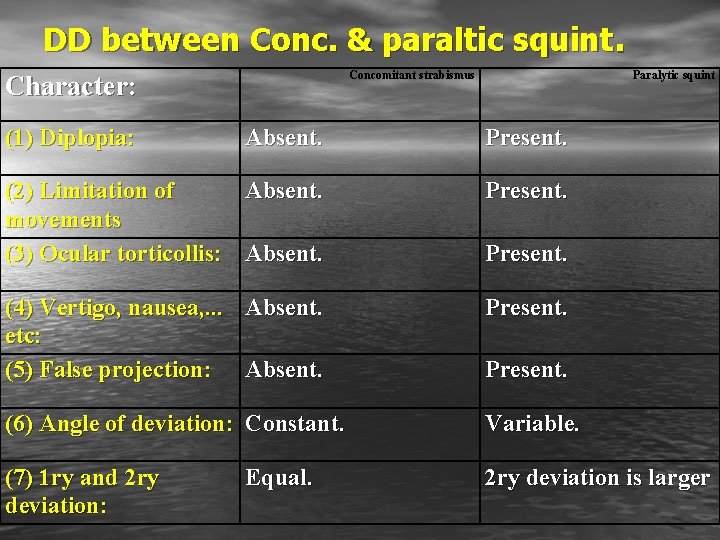
DD between Conc. & paraltic squint. Concomitant strabismus Character: (1) Diplopia: Paralytic squint Absent. Present. (2) Limitation of Absent. movements (3) Ocular torticollis: Absent. Present. (4) Vertigo, nausea, . . . Absent. etc: (5) False projection: Absent. Present. (6) Angle of deviation: Constant. Variable. (7) 1 ry and 2 ry deviation: 2 ry deviation is larger Equal. Present.
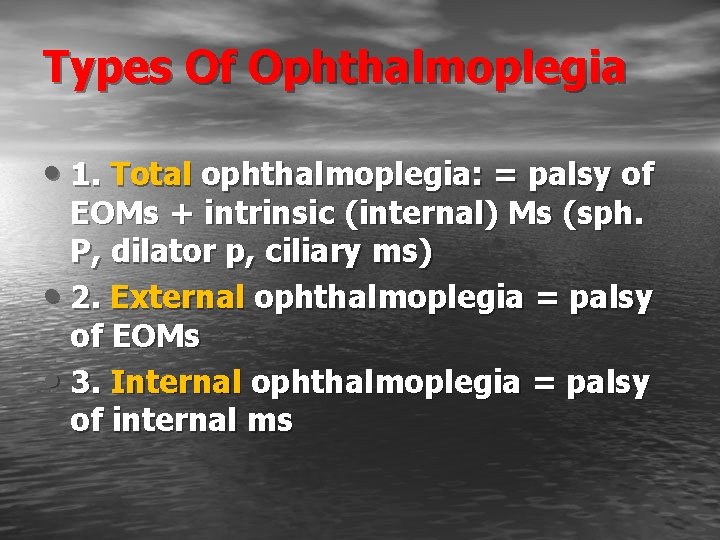
Types Of Ophthalmoplegia • 1. Total ophthalmoplegia: = palsy of EOMs + intrinsic (internal) Ms (sph. P, dilator p, ciliary ms) • 2. External ophthalmoplegia = palsy of EOMs • 3. Internal ophthalmoplegia = palsy of internal ms
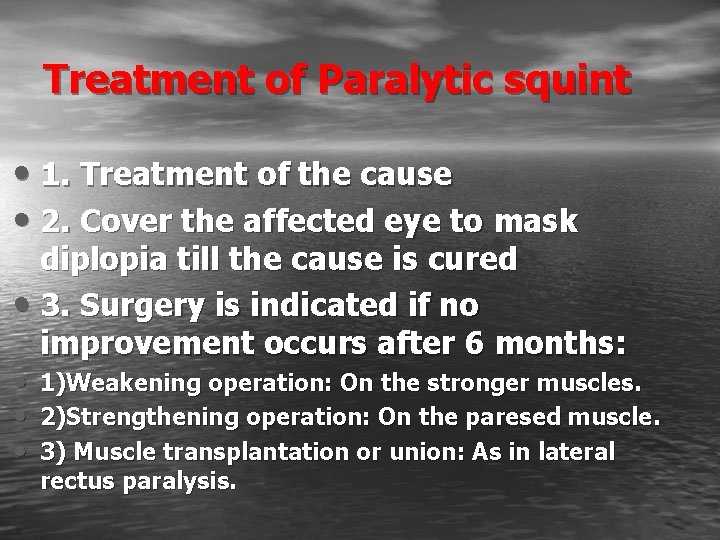
Treatment of Paralytic squint • 1. Treatment of the cause • 2. Cover the affected eye to mask diplopia till the cause is cured • 3. Surgery is indicated if no improvement occurs after 6 months: • • • 1)Weakening operation: On the stronger muscles. 2)Strengthening operation: On the paresed muscle. 3) Muscle transplantation or union: As in lateral rectus paralysis.
- Slides: 29