Myocardial Diseases Saad S Ahmad MD FACC Assistant














- Slides: 60

Myocardial Diseases Saad S. Ahmad, MD, FACC Assistant Professor of Clinical Medicine Advanced Heart Failure and Interventional Cardiology
Outline • • • Hypertrophic Cardiomyopathy Myocarditis Heart Failure with Preserved Ejection Fraction Restrictive Cardiomyopathy Dilated Cardiomyopathy Cor Pulmonale
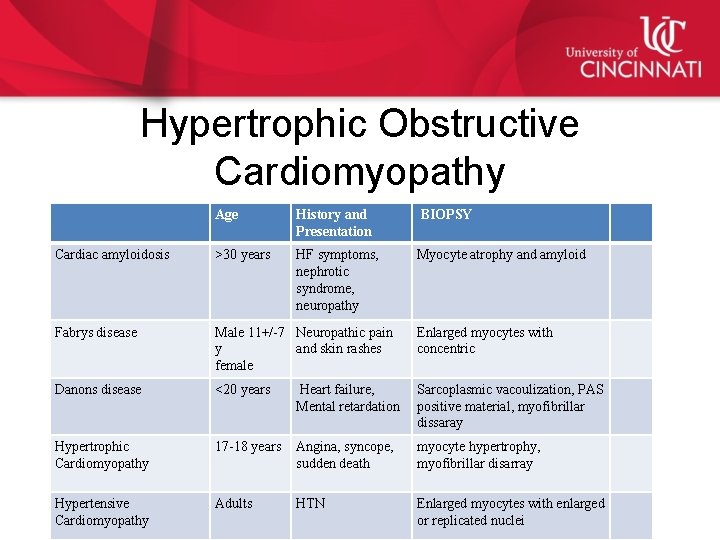
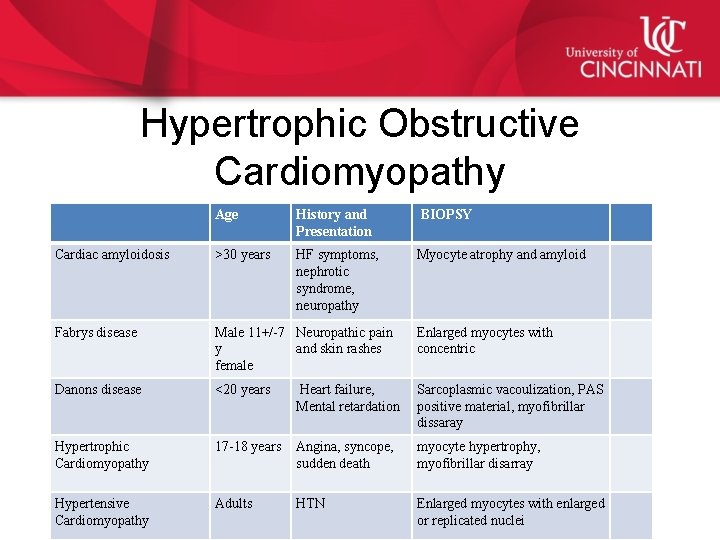
Hypertrophic Obstructive Cardiomyopathy Age History and Presentation BIOPSY Cardiac amyloidosis >30 years HF symptoms, nephrotic syndrome, neuropathy Myocyte atrophy and amyloid Fabrys disease Male 11+/-7 Neuropathic pain y and skin rashes female Enlarged myocytes with concentric Danons disease <20 years Heart failure, Mental retardation Sarcoplasmic vacoulization, PAS positive material, myofibrillar dissaray Hypertrophic Cardiomyopathy 17 -18 years Angina, syncope, sudden death myocyte hypertrophy, myofibrillar disarray Hypertensive Cardiomyopathy Adults HTN Enlarged myocytes with enlarged or replicated nuclei
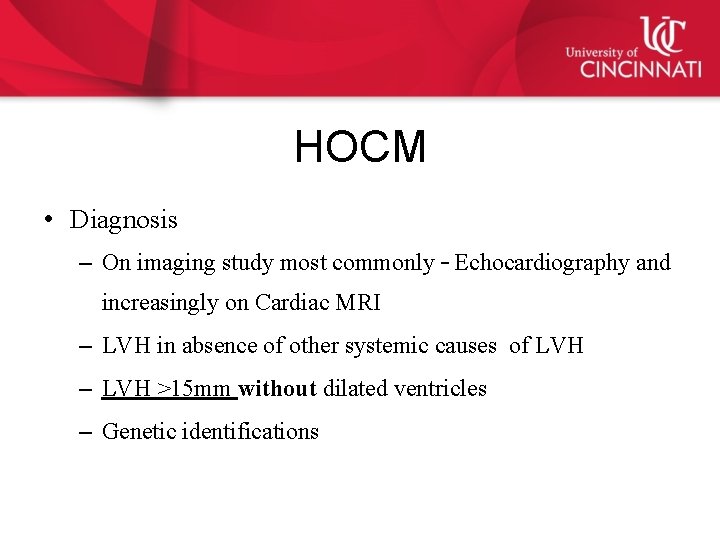
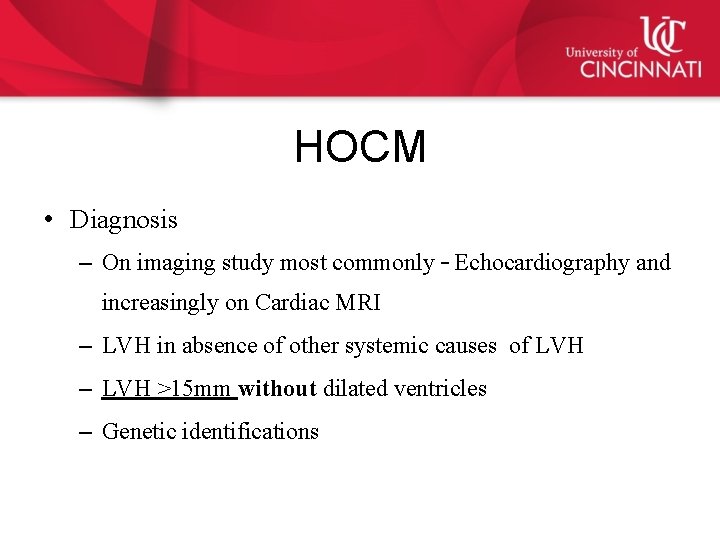
HOCM • Diagnosis – On imaging study most commonly – Echocardiography and increasingly on Cardiac MRI – LVH in absence of other systemic causes of LVH – LVH >15 mm without dilated ventricles – Genetic identifications
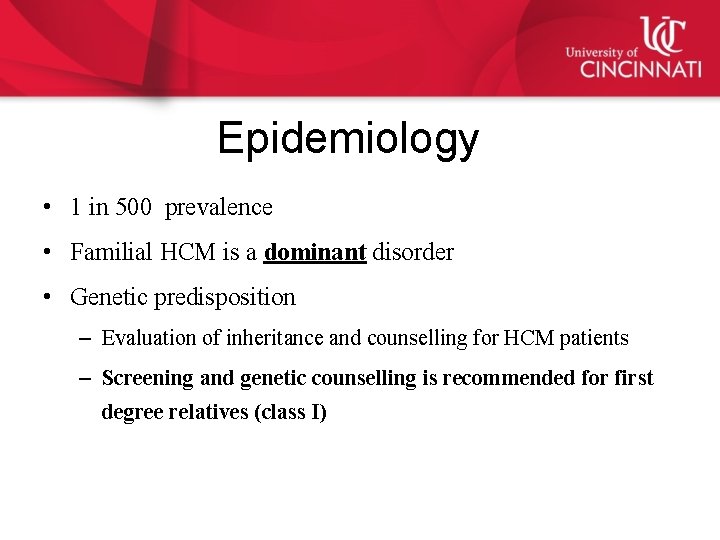
Epidemiology • 1 in 500 prevalence • Familial HCM is a dominant disorder • Genetic predisposition – Evaluation of inheritance and counselling for HCM patients – Screening and genetic counselling is recommended for first degree relatives (class I)
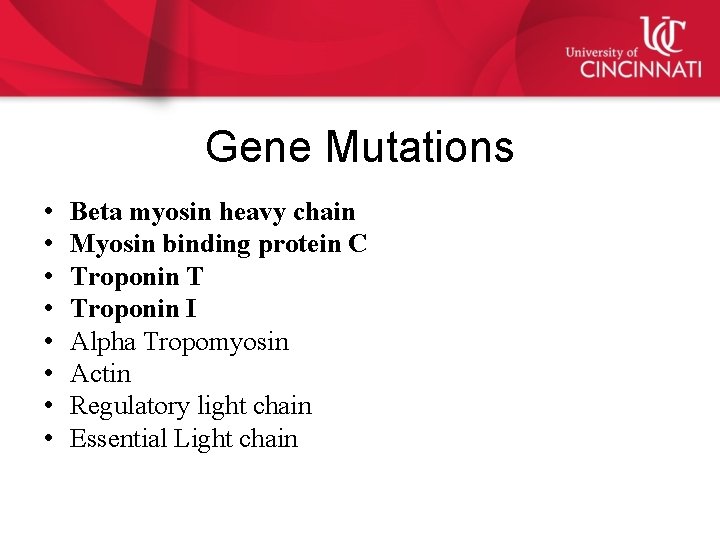
Gene Mutations • • Beta myosin heavy chain Myosin binding protein C Troponin T Troponin I Alpha Tropomyosin Actin Regulatory light chain Essential Light chain
• Age <12 y – Optional unless – Malignant family history of premature death from HCM or other adverse complications – Patient is a competitive athlete in an intense training program Onset of symptoms Other clinical suspicion of early LV hypertrophy • Age 12 to 18 – 21 y† – Every 12– 18 mo • Age 18– 21 y At onset of symptoms or at least every 5 y. More frequent intervals are – appropriate in families with a malignant clinical course or late-onset HCM.

Natural History of HOCM Sudden Cardiac Death 0. 2 -0. 8%/year Heart Failure AF and Stroke 25% of the patients Benign Clinical course
Pathophysiology • Diastolic dysfunction • Myocardial ischemia : demand perfusion mismatch • Mitral regurgitation • Poor augmentation of blood pressure during exercise or drop in BP • Left ventricular outflow obstruction

Physical Examination • • Bifid pulse SEM at apex Presence of S 4 LLSB murmur : some times absent at rest and provoked by – Valsalva – Squat to stand – Amyl nitrite
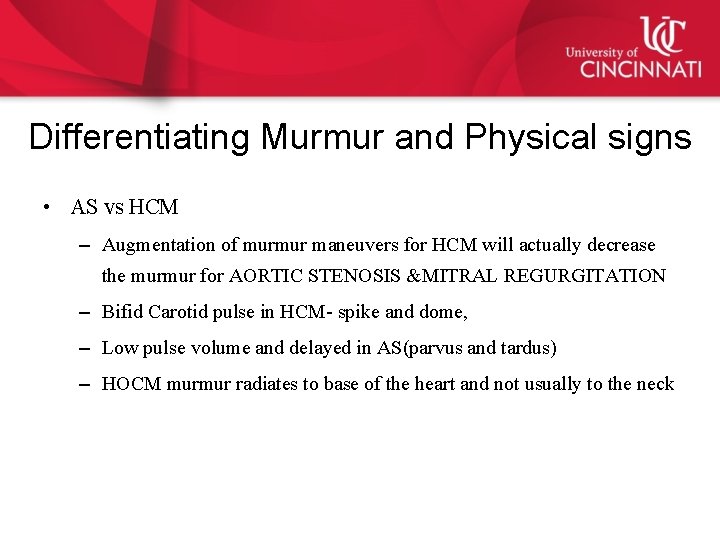
Differentiating Murmur and Physical signs • AS vs HCM – Augmentation of murmur maneuvers for HCM will actually decrease the murmur for AORTIC STENOSIS &MITRAL REGURGITATION – Bifid Carotid pulse in HCM- spike and dome, – Low pulse volume and delayed in AS(parvus and tardus) – HOCM murmur radiates to base of the heart and not usually to the neck
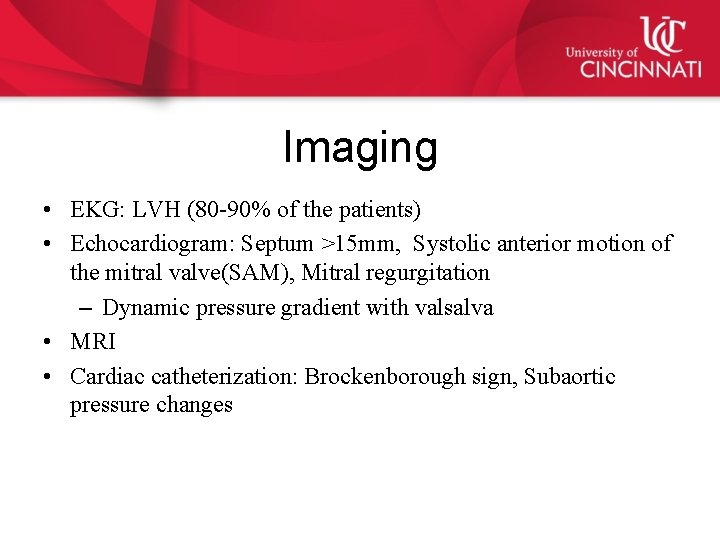
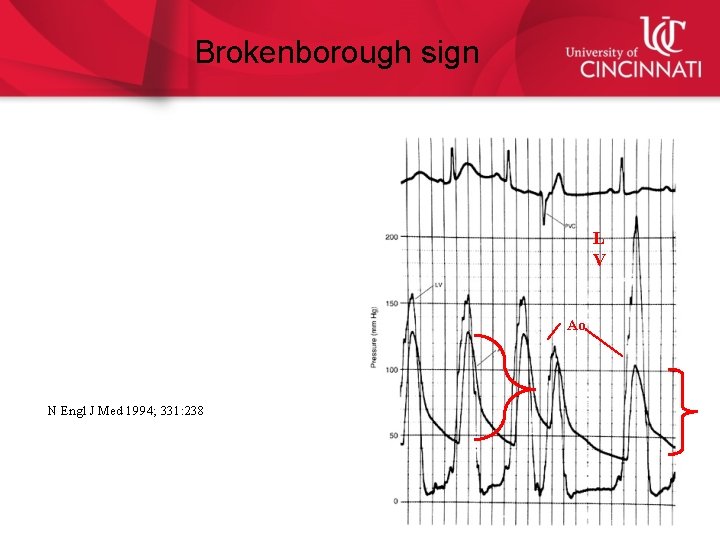
Imaging • EKG: LVH (80 -90% of the patients) • Echocardiogram: Septum >15 mm, Systolic anterior motion of the mitral valve(SAM), Mitral regurgitation – Dynamic pressure gradient with valsalva • MRI • Cardiac catheterization: Brockenborough sign, Subaortic pressure changes
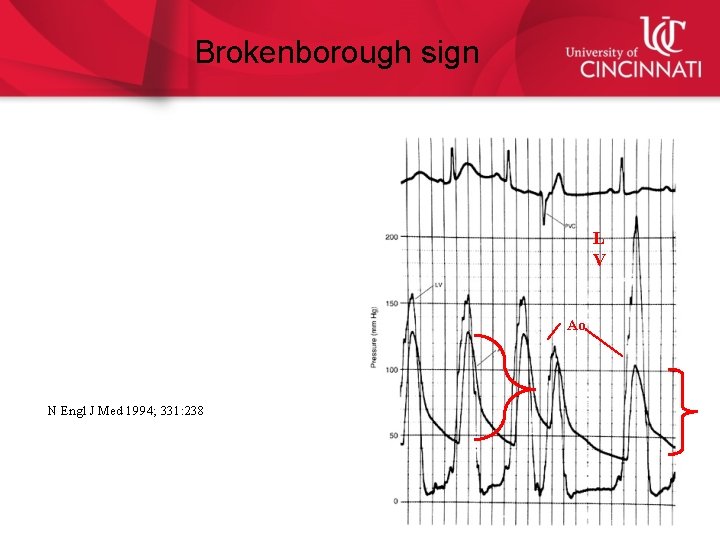
Brokenborough sign L V Ao N Engl J Med 1994; 331: 238
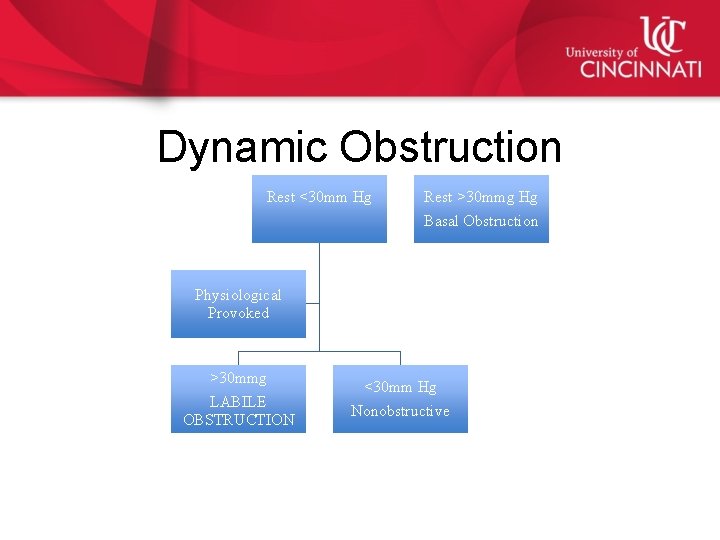
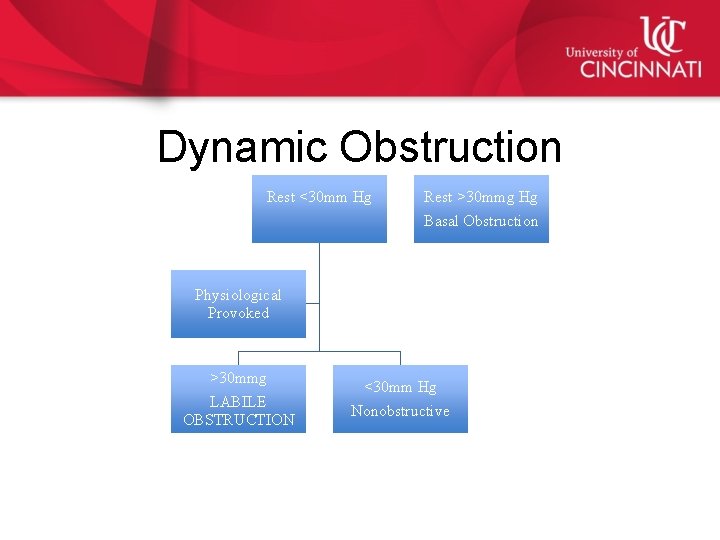
Dynamic Obstruction Rest <30 mm Hg Rest >30 mmg Hg Basal Obstruction Physiological Provoked >30 mmg LABILE OBSTRUCTION <30 mm Hg Nonobstructive
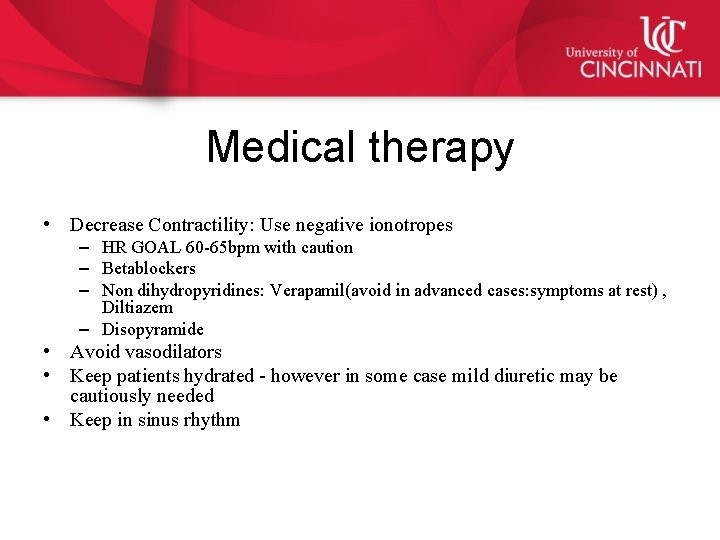
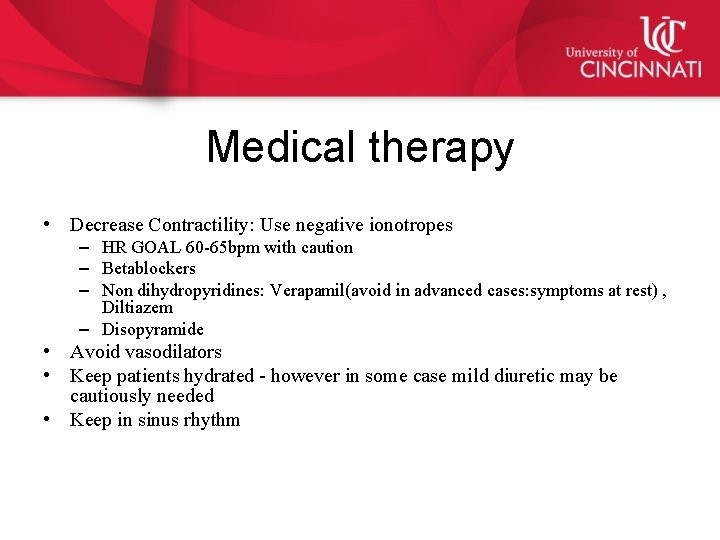
Medical therapy • Decrease Contractility: Use negative ionotropes – HR GOAL 60 -65 bpm with caution – Betablockers – Non dihydropyridines: Verapamil(avoid in advanced cases: symptoms at rest) , Diltiazem – Disopyramide • Avoid vasodilators • Keep patients hydrated - however in some case mild diuretic may be cautiously needed • Keep in sinus rhythm
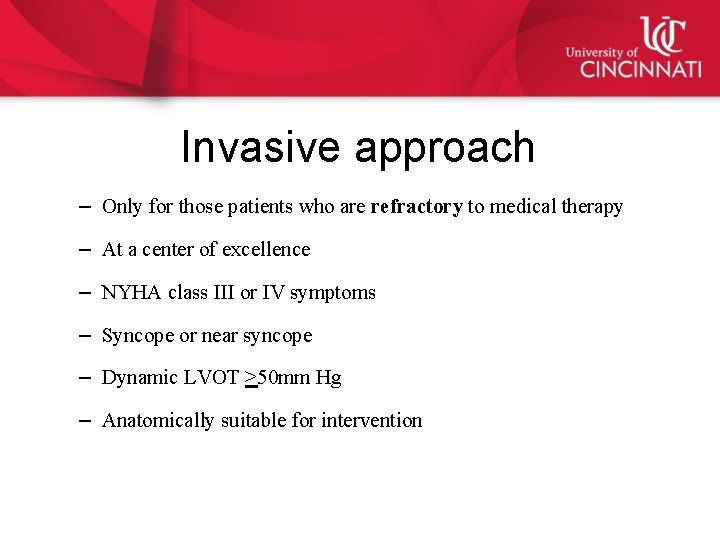
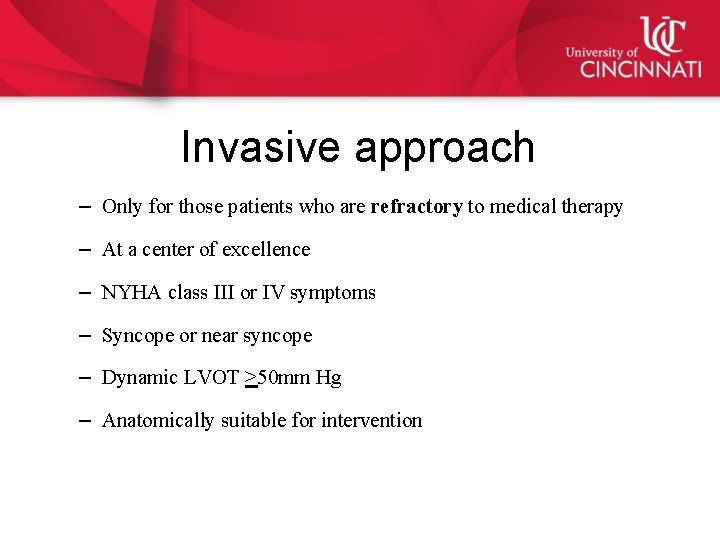
Invasive approach – Only for those patients who are refractory to medical therapy – At a center of excellence – NYHA class III or IV symptoms – Syncope or near syncope – Dynamic LVOT >50 mm Hg – Anatomically suitable for intervention
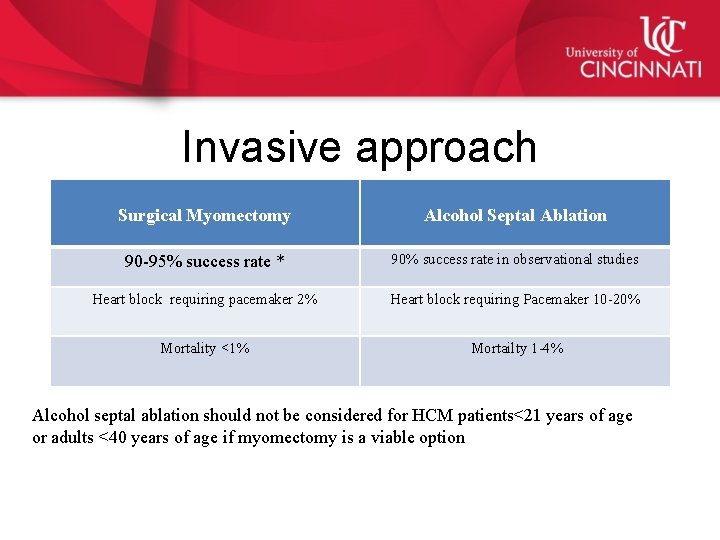
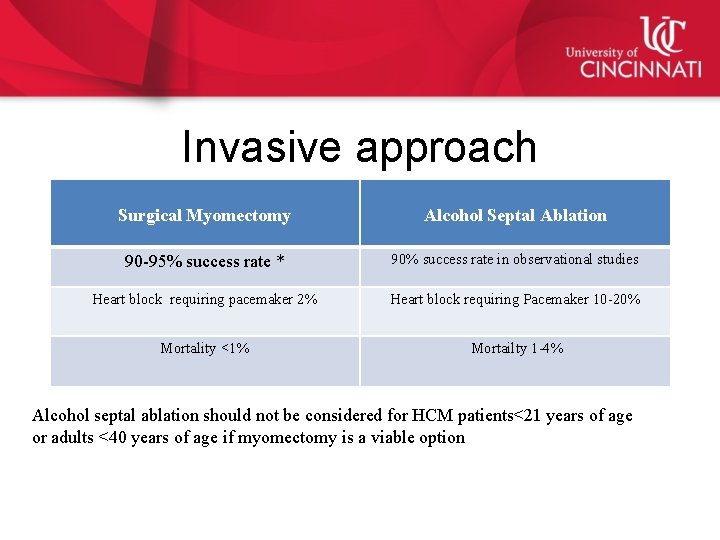
Invasive approach Surgical Myomectomy Alcohol Septal Ablation 90 -95% success rate * 90% success rate in observational studies Heart block requiring pacemaker 2% Heart block requiring Pacemaker 10 -20% Mortality <1% Mortailty 1 -4% Alcohol septal ablation should not be considered for HCM patients<21 years of age or adults <40 years of age if myomectomy is a viable option

Refractory to Drug therapy Amenable to invasive approach MYOMECTOMY IIa Ablation IIb Not a candidate for invasive therapy DDD pacing IIB
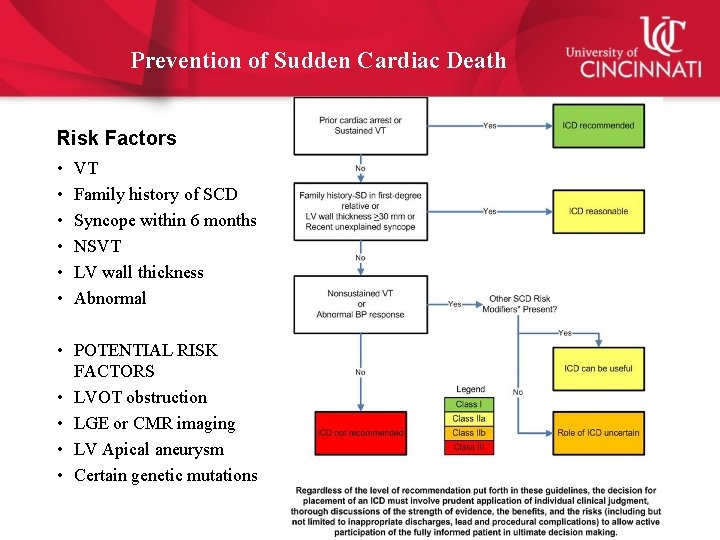
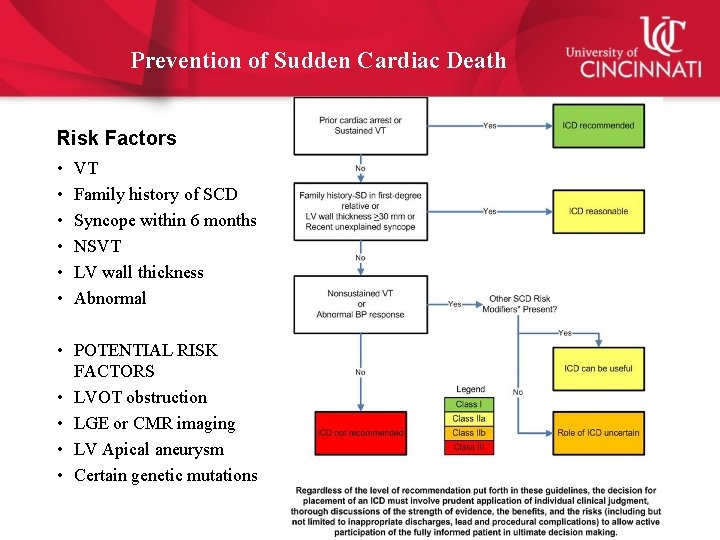
Prevention of Sudden Cardiac Death Risk Factors • • • VT Family history of SCD Syncope within 6 months NSVT LV wall thickness Abnormal • POTENTIAL RISK FACTORS • LVOT obstruction • LGE or CMR imaging • LV Apical aneurysm • Certain genetic mutations
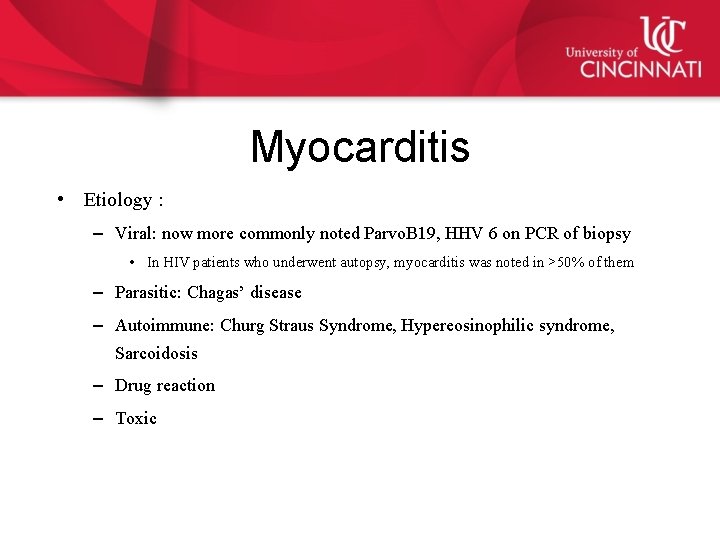
Myocarditis • Etiology : – Viral: now more commonly noted Parvo. B 19, HHV 6 on PCR of biopsy • In HIV patients who underwent autopsy, myocarditis was noted in >50% of them – Parasitic: Chagas’ disease – Autoimmune: Churg Straus Syndrome, Hypereosinophilic syndrome, Sarcoidosis – Drug reaction – Toxic
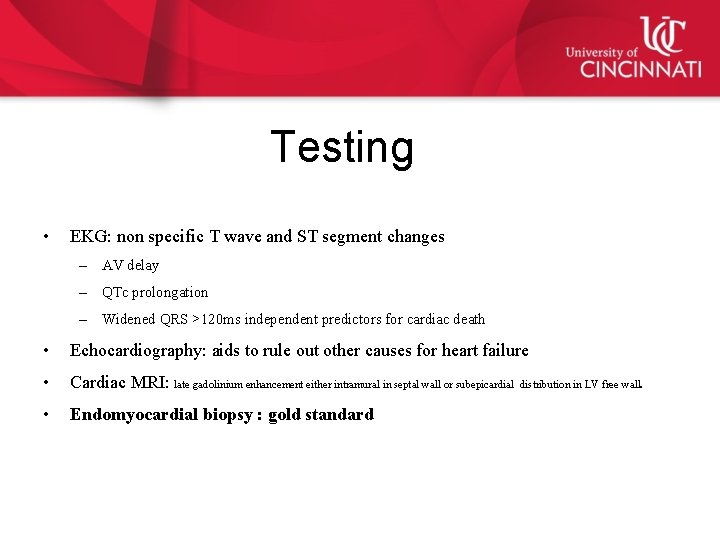
Testing • EKG: non specific T wave and ST segment changes – AV delay – QTc prolongation – Widened QRS >120 ms independent predictors for cardiac death • Echocardiography: aids to rule out other causes for heart failure • Cardiac MRI: late gadolinium enhancement either intramural in septal wall or subepicardial • Endomyocardial biopsy : gold standard . distribution in LV free wall
Management • LV dysfunction: Heart failure therapy per guideline • Cardiogenic shock: may need mechanical circulatory support • Immunosuppression : for those with giant cell myocarditis and sarcoidosis • NSAIDS: used in PERICARDITIS, no role in myocarditis – Use lowest possible dose in PERIMYOCARDITIS when LV function is preserved and there is prominent chest pain from pericarditis J Am Coll Cardiol 2012; 59: 779– 92 : Update on Myocarditis

Pacemaker or ICD therapy • Lyme carditis • Sarcoidosis • Chagas disease
J Am Coll Cardiol 2012; 59: 779– 92)
Heart Failure with Preserved Ejection Fraction HFp. EF • • Approximately 50% of all HF patients HFp. EF defined as EF >50% in current ACC/AHA 2013 guidelines Often refers to a heterogenous group of diseases and not single entity Risk factors: – – – HTN Women Old age DM Obesity

Pathophysiology Diastolic stiffness and abnormal relaxation Other factors involved: • Chronotropic incompetence • Elevated diastolic filling pressure during exercise • Atrial fibrillation Elevated LA pressures Pulmonary HTN RV dysfunction

Diagnosis • Clinical diagnosis – Complains of Dyspnea, orthopnea – Signs of hypervolemia, raised JVD , ascites and edema – CXR may show similar size heart as HFr. EF – ECG: may show LVH – Invasive catheterization has been the gold standard and exercise PA systolic pressure >45 mm Hg identified HFp. EF with sensitivity and specificity 96% and 95% respectively
Therapeutics • Control BP as per guidelines • Diuretic to relieve volume • CAD revascularization : when angina or demonstrated angina is having an adverse effect.
Cor Pulmonale
Cor Pulmonale • Currently defined as dilation and hypertrophy of the right ventricle in response to diseases of the pulmonary vasculature and /or lung parenchyma. • Excludes diseases of the right heart secondary to the left side of the heart or congenital diseases.
Etiology of Chronic Cor Pulmonale • COPD • Cystic fibrosis • Chronic hypoventilation – High altitude – Chest wall dysfunction • Sarcoidosis • Interstitial lung diseases • Thromboembolic diseases • Pulmonary arterial HTN • Pulmonary veno occlusive disease
Physical examination • • • Elevated JVP- with prominent V wave Hepatomegaly Ascites Lower extremity edema RV heave • Harrison’s Princinples of Internal Medicine 18 th ed
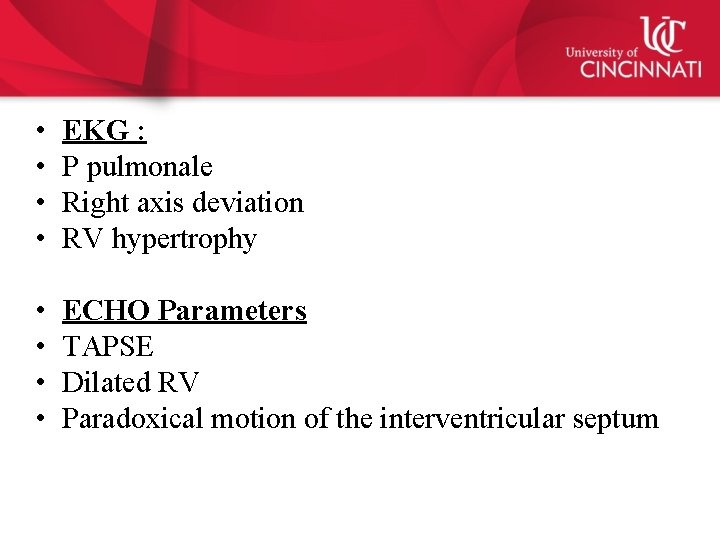
• • EKG : P pulmonale Right axis deviation RV hypertrophy • • ECHO Parameters TAPSE Dilated RV Paradoxical motion of the interventricular septum
Treatment • Underlying pulmonary cause needs to be treated • Diuretics for fluid over load • Consideration for pulmonary vasodilators when isolated pulmonary arterial hypertension is present
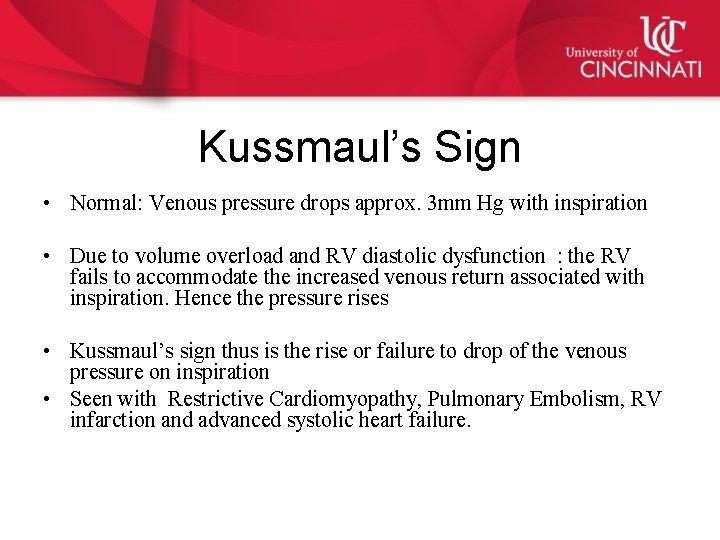
Kussmaul’s Sign • Normal: Venous pressure drops approx. 3 mm Hg with inspiration • Due to volume overload and RV diastolic dysfunction : the RV fails to accommodate the increased venous return associated with inspiration. Hence the pressure rises • Kussmaul’s sign thus is the rise or failure to drop of the venous pressure on inspiration • Seen with Restrictive Cardiomyopathy, Pulmonary Embolism, RV infarction and advanced systolic heart failure.
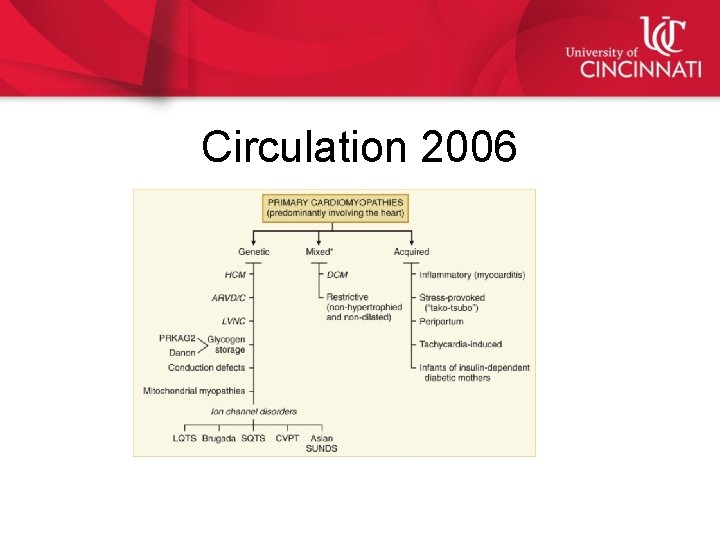
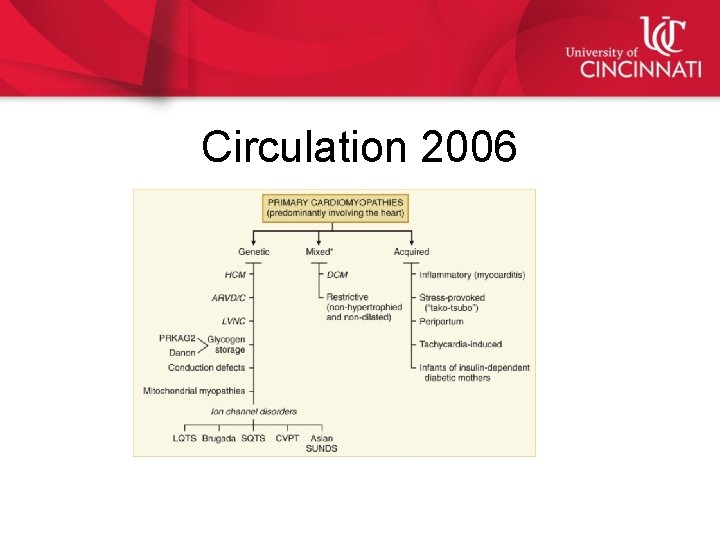
Circulation 2006
Cardiac Sarcoidosis • Cardiac sarcoidosis clinically manifests in 5% of patients with sarcoidosis • Up to 35% of patients age<60 years with AV block or VT without underlying cause, may have undiagnosed VT • Cardiac manifestations: – – VT SCD Conduction abnormalities Heart Failure

Cardiac Sarcoidosis • EKG: various degrees of conduction blocks – RBBB is more common – Pseudo infarct pattern – Epsilon waves • • • Echo: non specific Biomarkers: ACE levels 60% of patients (low sensitivity and specificity) CMR: non specific pattern diagnostic : LGE patchy FDG PET imaging Biopsy: Extracardiac Lymph node or lung biopsy – Heart biopsy: has low sensitivity due to patchy distribution
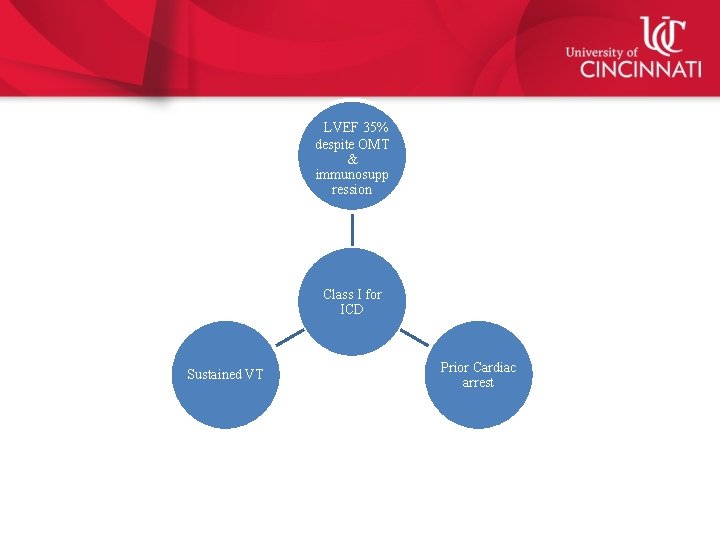
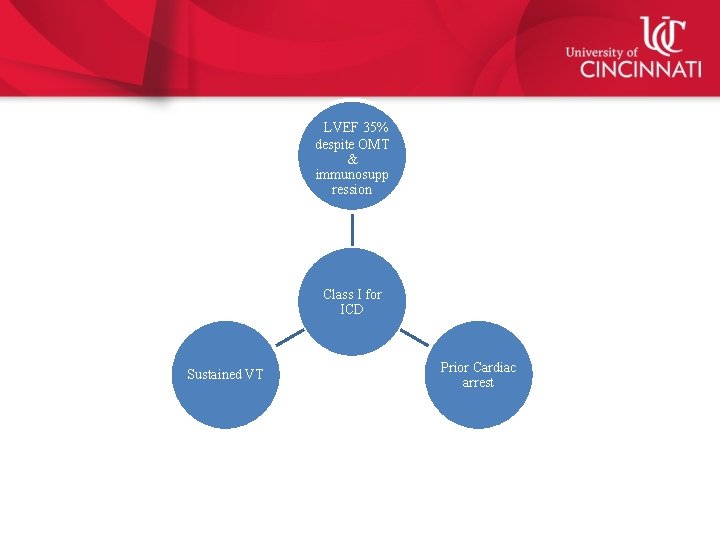
LVEF 35% despite OMT & immunosupp ression Class I for ICD Sustained VT Prior Cardiac arrest
Constrictive vs Restrictive • Both initially present with preserved systolic function • History is important for predisposition to Constriction – Radiation, scleroderma, TB, malignancy, CTD • Physical examination is challenging to differentiate the two • BNP may be more elevated in the cases of restrictive disease compared to constrictive cardiomyopathy • Most common cause for restriction is infiltrative disorder caused by genetic disorder in Amyloidosis
Constrictive vs Restrictive • Hemodynamics: equalization of diastolic pressures in all 4 chambers • Dip and plateau in ventricular pressure during early diastole • Rapid X and Y descent of atrial pressure curves • Other hemodynamic criteria involving PA pressures LV RV pressure difference, not specific
RC DC
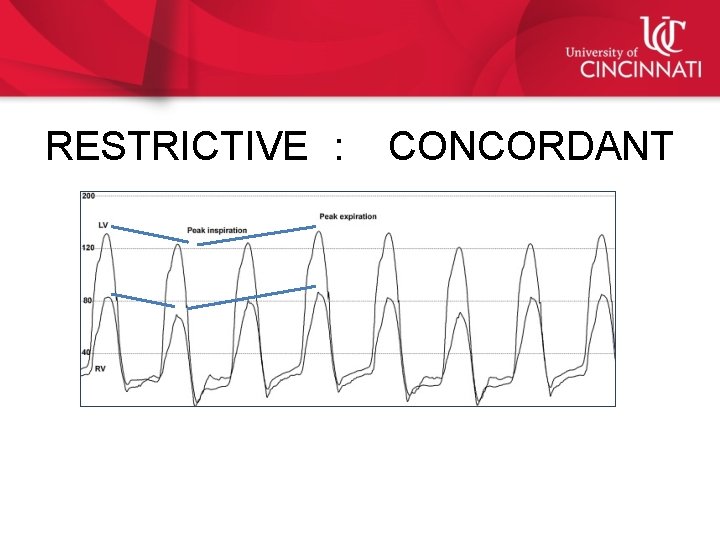
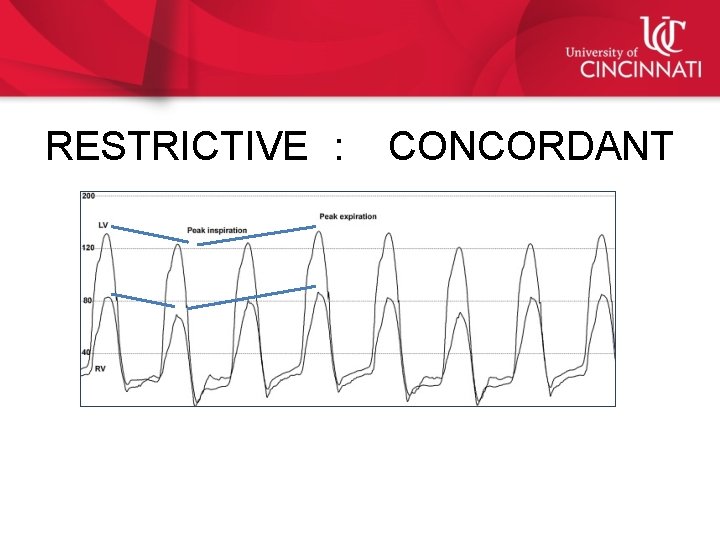
RESTRICTIVE : CONCORDANT

DICORDANT : CONSTRICTIVE
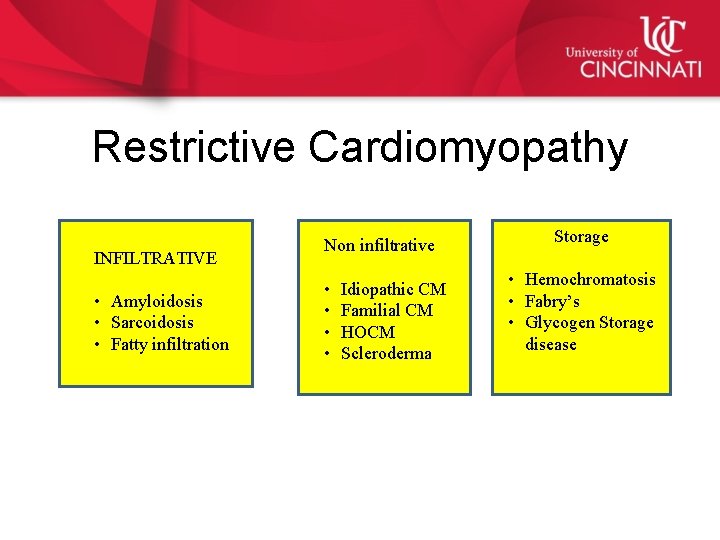
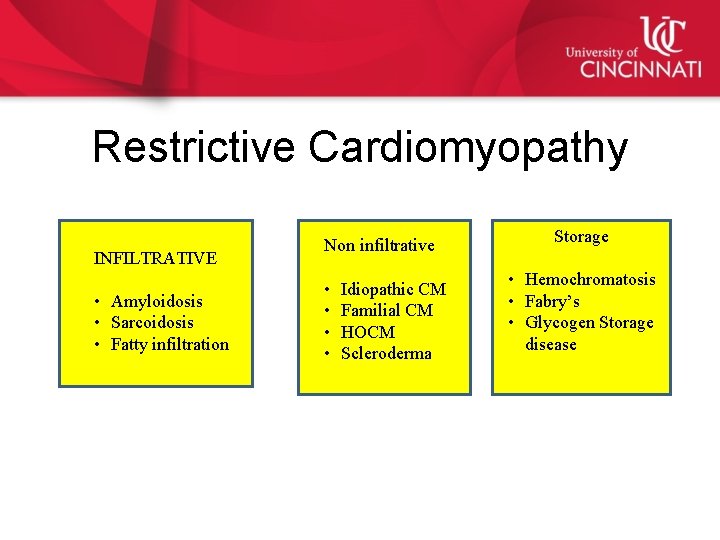
Restrictive Cardiomyopathy INFILTRATIVE • Amyloidosis • Sarcoidosis • Fatty infiltration Non infiltrative • • Idiopathic CM Familial CM HOCM Scleroderma Storage • Hemochromatosis • Fabry’s • Glycogen Storage disease

Signs and Symptoms • Dyspnea , edema • Exercise intolerance • Ascites, hepatomegaly and anasarca • Raised JVD • Kussmauls sign • S 3, S 4 • Abnormal diastolic dysfunction on echocardiography
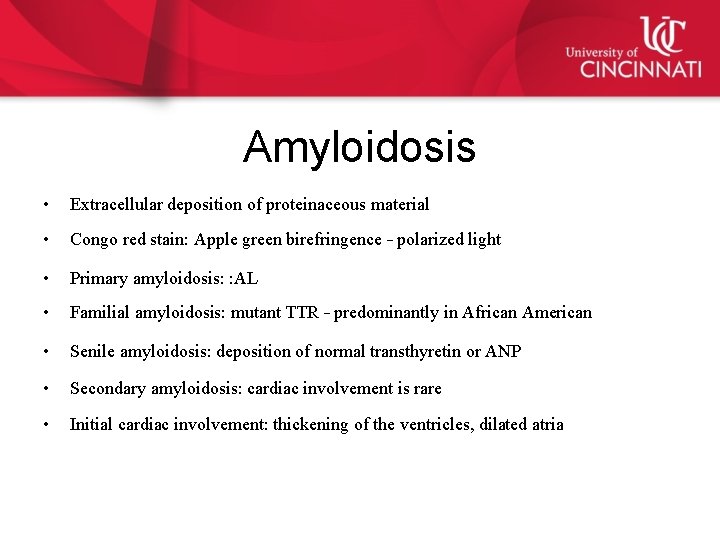
Amyloidosis • Extracellular deposition of proteinaceous material • Congo red stain: Apple green birefringence – polarized light • Primary amyloidosis: : AL • Familial amyloidosis: mutant TTR – predominantly in African American • Senile amyloidosis: deposition of normal transthyretin or ANP • Secondary amyloidosis: cardiac involvement is rare • Initial cardiac involvement: thickening of the ventricles, dilated atria
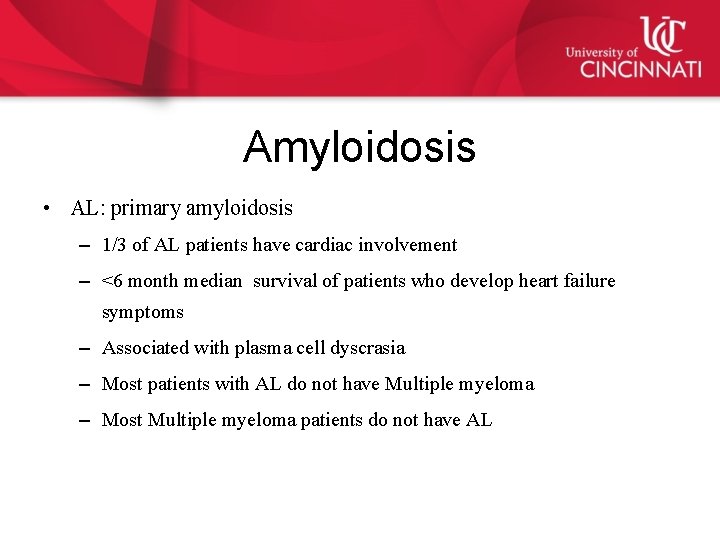
Amyloidosis • AL: primary amyloidosis – 1/3 of AL patients have cardiac involvement – <6 month median survival of patients who develop heart failure symptoms – Associated with plasma cell dyscrasia – Most patients with AL do not have Multiple myeloma – Most Multiple myeloma patients do not have AL
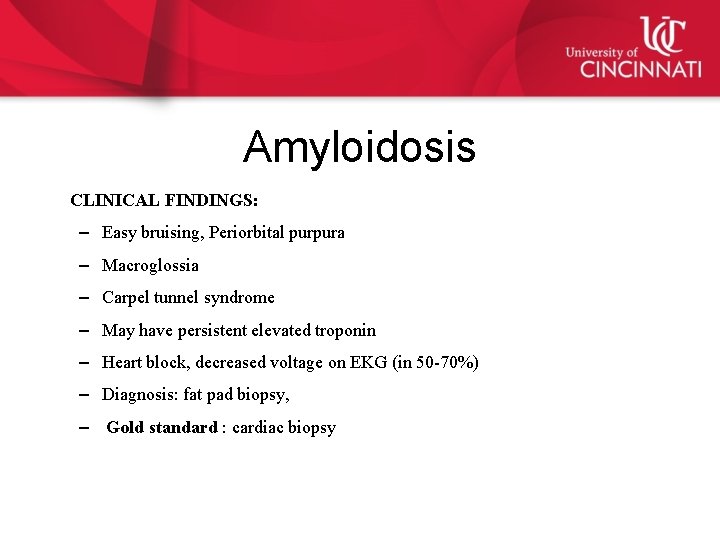
Amyloidosis CLINICAL FINDINGS: – Easy bruising, Periorbital purpura – Macroglossia – Carpel tunnel syndrome – May have persistent elevated troponin – Heart block, decreased voltage on EKG (in 50 -70%) – Diagnosis: fat pad biopsy, – Gold standard : cardiac biopsy
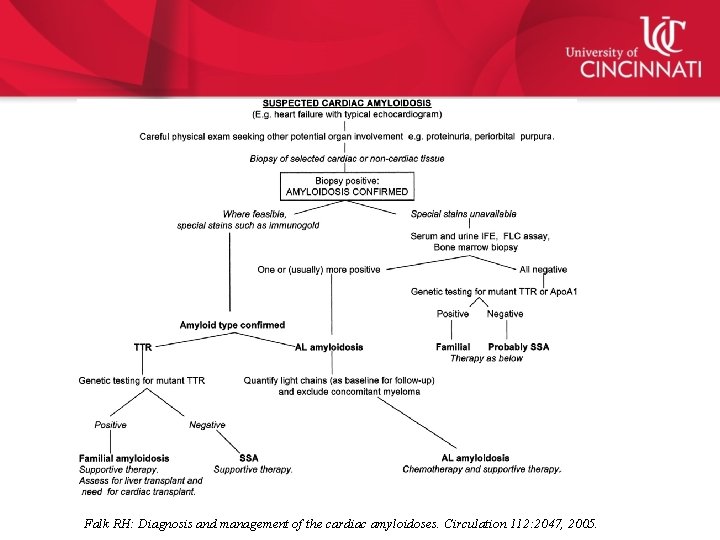
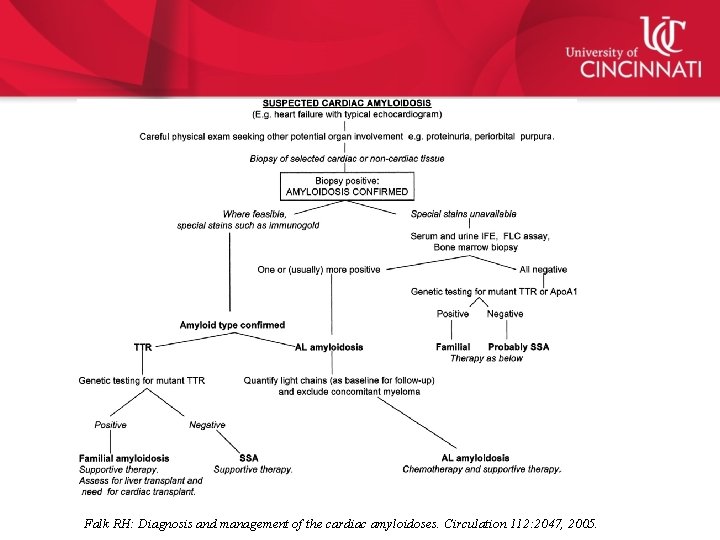
Falk RH: Diagnosis and management of the cardiac amyloidoses. Circulation 112: 2047, 2005.
Fabry’s Disease • X linked autosomal recessive: hence affects men more commonly • Lysosomal enzyme: Alpha galactosidase A deficiency • 3 rd to 4 th Decade for cardiac manifestation • Morphologically mimics HOCM • EKG: LVH • CMR: late gadolinium enhancement sparing subendocardium

Danon Disease • X linked • Afflicts men in teens and women in 20 s • Clinical signs: myopathy, mental retardation and heart failure (MEN) Women: predominant cardiac involvement • Symmetrical thickness of LV > HOCM • Normal QRS • Short PR interval
Hemochromatosis • Restrictive disease which leads to dilated Cardiomyopathy • Hereditary or secondary • Clinical presentation: cirrhosis, diabetes and hypogonadism, heart failure and arthritis (pentad) • CMR helps detect and quantify Cardiac involvement • QRS preserved unless very advanced • Definitive diagnosis: Liver biopsy • Treatment: cessation of blood transfusion, phlebotomy and chelation therapy
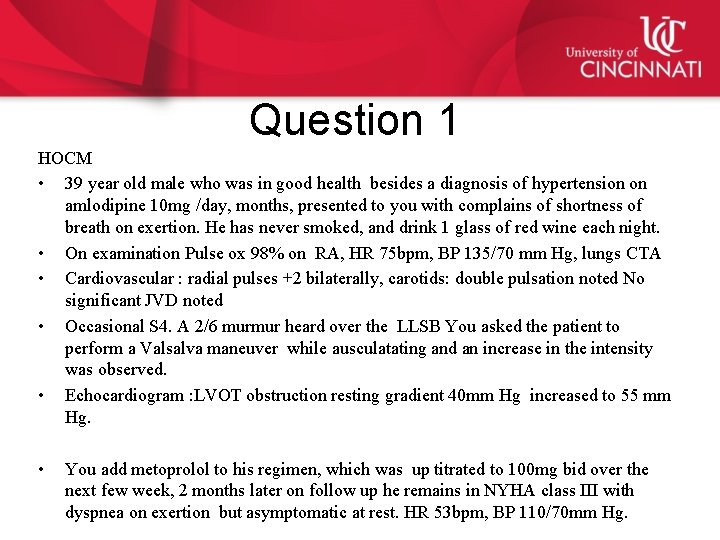
Question 1 HOCM • 39 year old male who was in good health besides a diagnosis of hypertension on amlodipine 10 mg /day, months, presented to you with complains of shortness of breath on exertion. He has never smoked, and drink 1 glass of red wine each night. • On examination Pulse ox 98% on RA, HR 75 bpm, BP 135/70 mm Hg, lungs CTA • Cardiovascular : radial pulses +2 bilaterally, carotids: double pulsation noted No significant JVD noted • Occasional S 4. A 2/6 murmur heard over the LLSB You asked the patient to perform a Valsalva maneuver while ausculatating and an increase in the intensity was observed. • Echocardiogram : LVOT obstruction resting gradient 40 mm Hg increased to 55 mm Hg. • You add metoprolol to his regimen, which was up titrated to 100 mg bid over the next few week, 2 months later on follow up he remains in NYHA class III with dyspnea on exertion but asymptomatic at rest. HR 53 bpm, BP 110/70 mm Hg.
What will be the next best step ? A. B. C. D. Refer him for a pacemaker Refer him for a septal ablation further up titrate betablocker and reassess in 2 weeks Discontinue Amlodipine

Question 2 77 y old lady with a history of GERD , HTN, CKD and Scleroderma presents to the hospital with shortness of breath from nursing home. You examine her on the inpatient service and she is in moderate distress. JVD 14 cm, Kussmauls sign present, Lower extremity edema 4+, moderate to severe tense ascites. Lungs are clear to auscultation. Heart sounds were generally distant, although a loud p 2 is noted. EKG: Sinus rhythm HR 95 , left anterior hemi block, Echocardiogram: No pericardial effusion, mild LVH, LVEF 55%, no wall motion abnormality Mild to moderate TR, and trivial MR, dilated IVC.

What test would you want to order next to confirm your diagnosis A. B. C. D. Stress test Fat pad biopsy Simultaneous rhc and lhc FDG PET
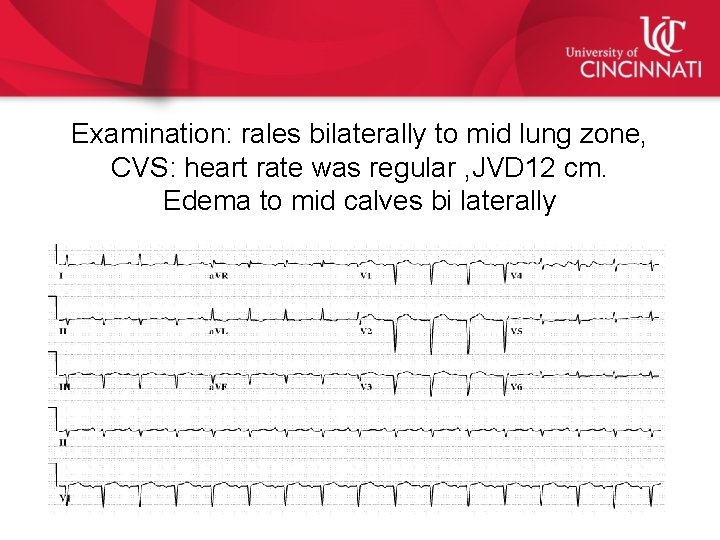
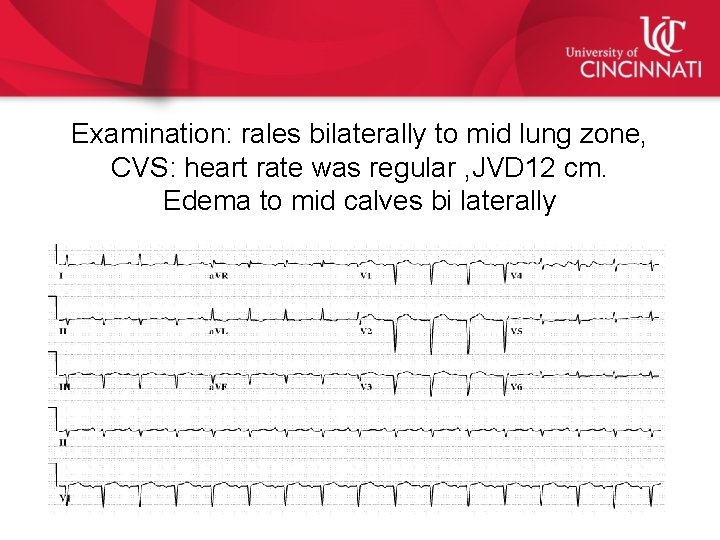
Examination: rales bilaterally to mid lung zone, CVS: heart rate was regular , JVD 12 cm. Edema to mid calves bi laterally
What is the most likely diagnosis: A. B. C. D. HCM Hemochromatosis Constrictive cardiomyopathy Amyloid

THANK YOU AND GOOD LUCK
 Kussmaul sign
Kussmaul sign Myocardial infarction
Myocardial infarction Myocardial ischemia meaning
Myocardial ischemia meaning Stemi location
Stemi location Myocardial infarction pain location
Myocardial infarction pain location Authentic synonm
Authentic synonm Pico question myocardial infarction
Pico question myocardial infarction Pancreas wiki
Pancreas wiki Dr hussein saad
Dr hussein saad Saad ahmed economics
Saad ahmed economics Saad bashir
Saad bashir Joanne saad
Joanne saad Saad alshahrani
Saad alshahrani Is an extended erp module
Is an extended erp module Télégestion saad
Télégestion saad Mohsen hassan
Mohsen hassan Saad ahmed javed
Saad ahmed javed Dr sadia saad
Dr sadia saad Salman azhar
Salman azhar Klodia saad
Klodia saad Ryan saad
Ryan saad Saad ahmed javed
Saad ahmed javed Sejarah penubuhan pengakap
Sejarah penubuhan pengakap Kausar ahmad
Kausar ahmad Fridoon
Fridoon Zamri ahmad
Zamri ahmad Nephrotic syndrome causes
Nephrotic syndrome causes Autocratic leadership
Autocratic leadership Dr shahzad ahmad
Dr shahzad ahmad Waseem ahmad khan
Waseem ahmad khan Nur ahmad husin
Nur ahmad husin Precapillary sphincter contraction
Precapillary sphincter contraction Sipnosis
Sipnosis Political services of sir syed ahmad khan
Political services of sir syed ahmad khan Ahmad aulia jusuf
Ahmad aulia jusuf Rabiah ahmad
Rabiah ahmad Ahmad rafay alam
Ahmad rafay alam Yamin ahmad
Yamin ahmad Nur ahmad husin
Nur ahmad husin Advantages of filtration
Advantages of filtration Ahmad kamal
Ahmad kamal Ahmad aulia jusuf
Ahmad aulia jusuf Fouzia khursheed ahmad
Fouzia khursheed ahmad National allegory examples
National allegory examples Asidiosis
Asidiosis Ahmad ibrahim primary school review
Ahmad ibrahim primary school review Nephrtic syndrome
Nephrtic syndrome Dr adnan ahmad
Dr adnan ahmad Ahmad makki hasan
Ahmad makki hasan What do you mean by duty cycle
What do you mean by duty cycle Dr mirza ahmad
Dr mirza ahmad Ahmad zahir kite runner
Ahmad zahir kite runner Hadi ahmad md
Hadi ahmad md Dr. ahmad muchlis
Dr. ahmad muchlis Ain syafinaz mohd razip
Ain syafinaz mohd razip Dr nur ahmad tabri
Dr nur ahmad tabri 7 stars doctor fkui
7 stars doctor fkui Ahmad gozali perencana keuangan
Ahmad gozali perencana keuangan Dr ani binti ahmad
Dr ani binti ahmad Ahmad rafiki
Ahmad rafiki Dr ahmad faisal
Dr ahmad faisal