Nausea Lifestyle Oral Health 2008 Nausea and vomiting





- Slides: 83
Nausea, Lifestyle & Oral Health 2008
• Nausea and vomiting • Lifestyle concerns with nutritional implications: – alcohol – caffeine – smoking – drugs – Non-nutritive sweeteners – physical activity • oral health
Nausea & Vomiting: Cochrane Library, 2003 Quinlan et al, Am Fam Phys, 2003
Background • 70 -85% of women experience nausea with pregnancy • ~ ½ experience vomiting • 35% of women with employment lose time from work due to nausea – an average of 62 hours • Almost 50% of women report that their work efficiency is reduced by n&v
Etiology • Unknown • Nausea less common in those who subsequently experience miscarriage • More common in twin pregnancies • Emerging findings: recent studies implicate helicobacter pylori – H pylori infections more common in women with n&v – Case reports that eradication of infection with antibiotics ameliorates symptoms
Hyperemesis Gravidarum • Severe nausea and vomiting • Affects one in 200 pregnancies • Most common reason for hospitalization in early pregnancy • Clinical features: Persistent vomiting, dehydration, ketonuria, electrolyte disturbances, weight loss • 159 per million pregnant women died in England between 1931 -1940 (before IV fluid replacement therapy was available) • (Charlotte Bronte died of hyperemesis in her fourth month of pregnancy)
Cochrane Conclusions: 2003 • B 6 “appears to be effective in reducing the severity of nausea. ” • Results of P 6 acupressure trends are “equivocal. ” • “No trials of treatment for hyperemesis gravidarum show evidence of benefit. ”
Effectiveness and safety of ginger in the treatment of pregnancy-induced nausea and vomiting (Borelli. Obstet Gynecol. 2005) • Six double-blind RCTs with a total of 675 participants and a prospective observational cohort study (n = 187) met all inclusion criteria • Four of the 6 RCTs (n = 246) showed superiority of ginger over placebo; the other 2 RCTs (n = 429) indicated that ginger was as effective as the reference drug (vitamin B 6) in relieving the severity of nausea and vomiting episodes.
Borelli, cont. • absence of significant side effects or adverse effects on pregnancy outcomes • CONCLUSION: Ginger may be an effective treatment for nausea and vomiting in pregnancy. However, more observational studies, with a larger sample size, are needed to confirm the encouraging preliminary data on ginger safety.
Nausea and vomiting of pregnancy: an evidence-based review (Davis, J Perinat Neonatal Nurs. 2004) • n&v rates less in women taking perinatal multivitamin • Mild to moderate n&v reduced by P 6 acupuncture site pressure wristband (new battery operated electrical nerve stimulator) • First step is dietary & lifestyle changes


Davis, cont…. • If diet/lifestyle fail to bring relief drug therapy may be indicated. • Most drugs will not be tested in pregnant women • Pharmacologic treatments include: – B 6 (pyradoxine) – B 6 plus doxylamine (an antihistamine)= Bendectin
American Gastroenterological Association Institute Medial Position Statement on the Use of Gastrointestinal Medication in Pregnancy (2006) • Metoclopramide, prochlorperazine, promethazine, trimethobenzamide and ondansetron* are considered low-risk drugs based on studies in pregnant women and can be used for nausea and vomiting and for hyperemesis gravidarum. Granisetron and dolasetron have not been studied in human pregnancies. ” *Reglan, Compazine , Phenergan , Tebamide, Zofran
Letter from Staroselsky et al. , Gastroenterology, 2007: Re Bendectin • AGA guideline missing doxylamine (with or without B 6) • Doxyamine-pyridozine (Bendectin) was approved by FDA for Tx of N&V in pregnancy, but “unfounded” lawsuits claiming risk of congenital malformations forced company to stop production in 1983.
Starokelsky letter, cont. • Meta-analysis of studies found no differences in birth defects with Bendectin. • Doxalamin-pyridoxine available in Canada and use associated with lower hospitalization for HG. • >30 million infants have been exposed without increased malformations. • “Failure to acknowledge the safety and effectiveness of this drug is against the principals of evidence-based medicine. ”
Mahadevan reply, 2007 • “We limited our scope to agents used by physicians practicing in the United States who treat women during pregnancy. ”
Stress Associated with N&V • Lack of understanding and support from others • Inability to take vitamins or eat healthy • Taking medications perceived as risky • Missing out on the “fun” of being pregnant • Loss of a “normal” pregnancy • Lost work days or quitting work • Putting life “on hold” • Longing to eat and drink normally • Money expended on care and support • Lack of energy, fatigue • Irritability and lack of enjoyment of life • Memory loss or inability to think clearly • Burden of care and time on others • Lack of socialization, isolation cont…
• Inability to prepare for birth and arrival of baby • Inability to care for family and home • Wanting pregnancy over or to end the misery • Others’ perception that hyperemesis is only in her mind • Reluctance of doctors to treat because of cost or liability • Weight loss or inadequate weight gain for gestational age of baby • Sense of inadequacy and failure at being unable to cope or function • Difficulty bonding with infant • Lack of energy and socialization with other children • Lack of excitement about infant’s arrival
Adverse effects of substance use determined by: • • • Timing Dosage Duration Number of substances Environment (nutrition, health status) Individual susceptibility
Effects of substance abuse include: • Increased health problems, including risk of AIDS • Compromised nutritional status/weight gain • Higher rates of OB complications • Psychosocial/economic/legal problems • Parenting difficulties • Higher rates of child abuse/neglect
Alcohol: Background · Per capita alcohol consumption has risen through the second half of this century in the US · 70% of individuals between the ages of 20 and 34 consume alcohol · Alcohol consumption peaks in the 20 -40 year old group
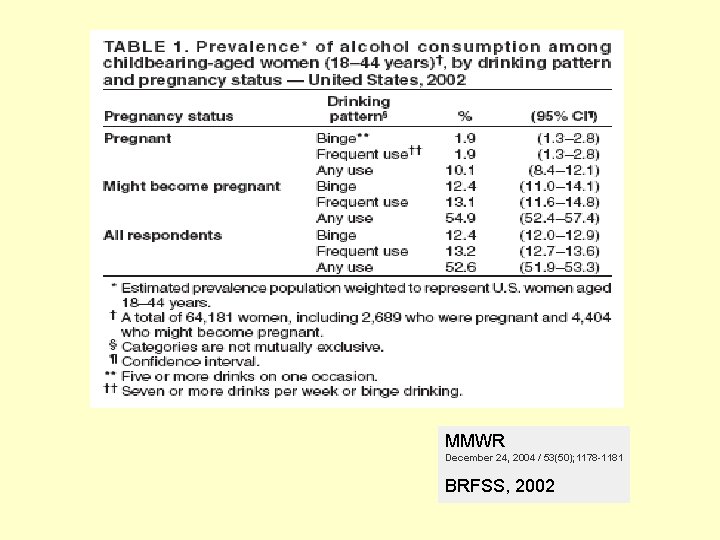
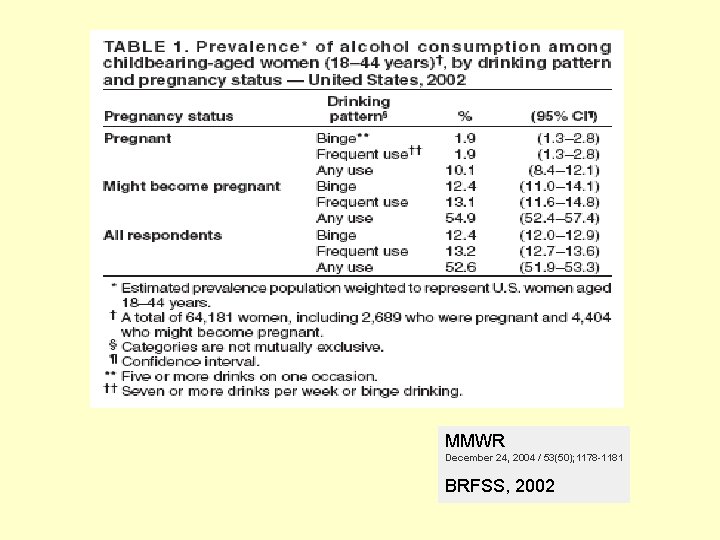
MMWR December 24, 2004 / 53(50); 1178 -1181 BRFSS, 2002
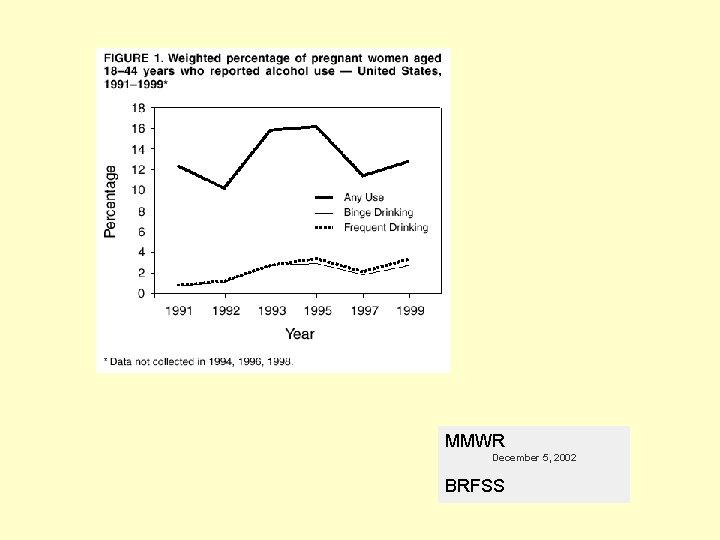
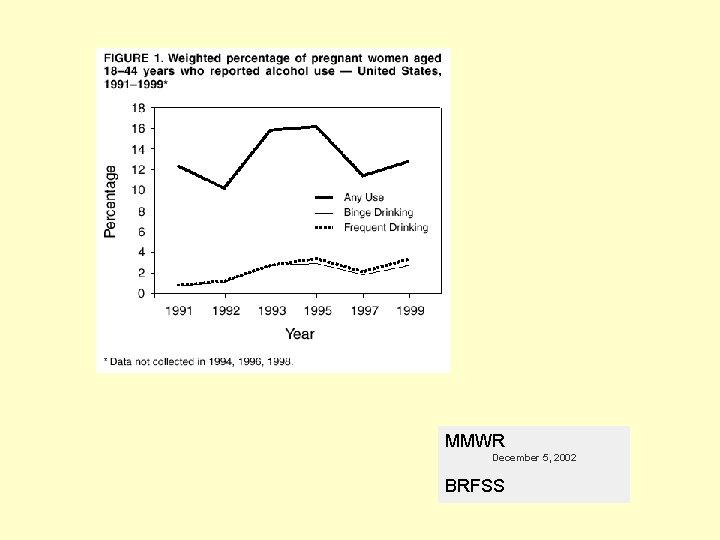
MMWR December 5, 2002 BRFSS
Alcohol: Background, cont. · Women are at disadvantage because less gastric first pass metabolism due to lower levels of alcohol dehydrogenate in intestinal mucosa · Fetus has no alcohol dehydrogenase activity · Alcohol crosses placenta easily by passive diffusion – fetal levels mimic maternal levels · The amniotic fluid acts as a reservoir for alcohol.
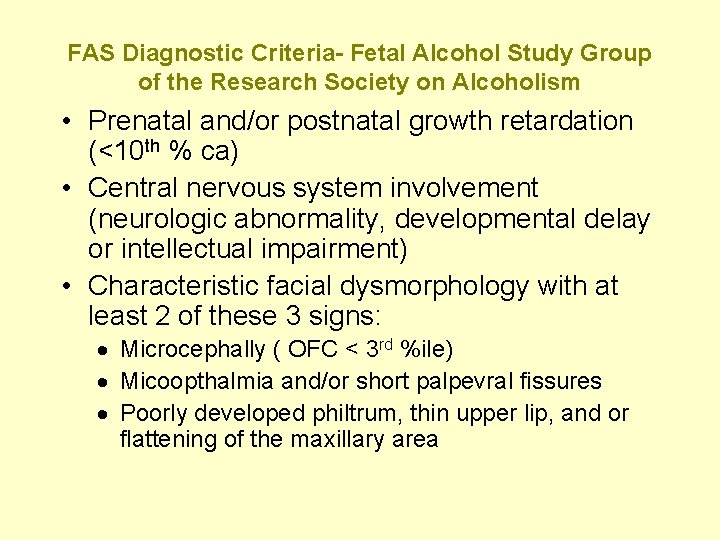
FAS Diagnostic Criteria- Fetal Alcohol Study Group of the Research Society on Alcoholism • Prenatal and/or postnatal growth retardation (<10 th % ca) • Central nervous system involvement (neurologic abnormality, developmental delay or intellectual impairment) • Characteristic facial dysmorphology with at least 2 of these 3 signs: · Microcephally ( OFC < 3 rd %ile) · Micoopthalmia and/or short palpevral fissures · Poorly developed philtrum, thin upper lip, and or flattening of the maxillary area
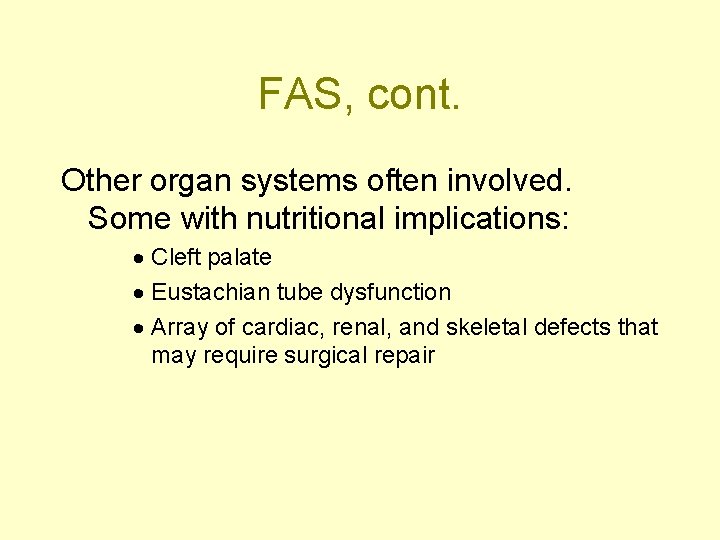
FAS, cont. Other organ systems often involved. Some with nutritional implications: · Cleft palate · Eustachian tube dysfunction · Array of cardiac, renal, and skeletal defects that may require surgical repair
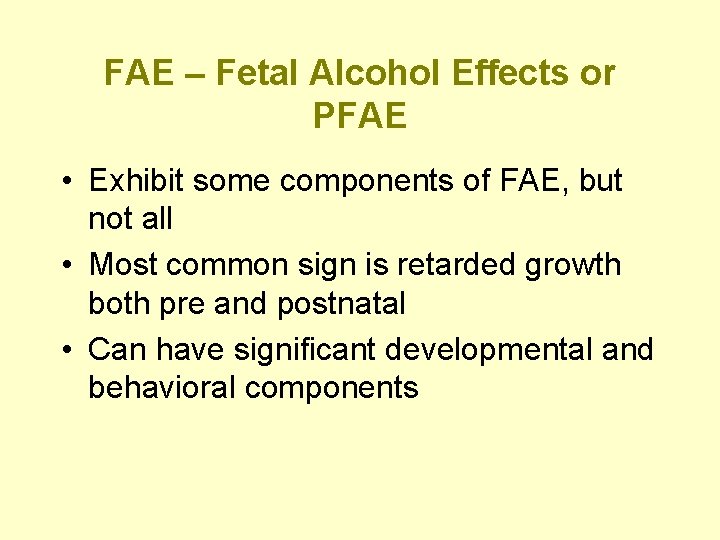
FAE – Fetal Alcohol Effects or PFAE • Exhibit some components of FAE, but not all • Most common sign is retarded growth both pre and postnatal • Can have significant developmental and behavioral components
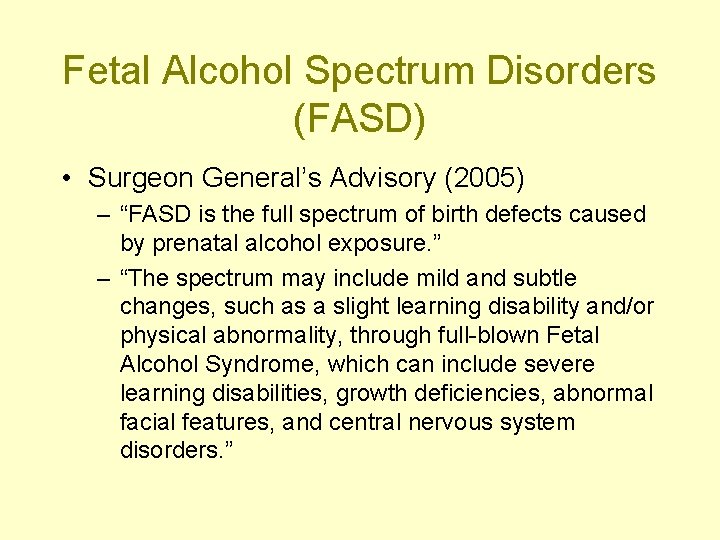
Fetal Alcohol Spectrum Disorders (FASD) • Surgeon General’s Advisory (2005) – “FASD is the full spectrum of birth defects caused by prenatal alcohol exposure. ” – “The spectrum may include mild and subtle changes, such as a slight learning disability and/or physical abnormality, through full-blown Fetal Alcohol Syndrome, which can include severe learning disabilities, growth deficiencies, abnormal facial features, and central nervous system disorders. ”
FAS/FAE Incidence · FAS – 1. 9 per 1000 births, 25 per 1000 among women who drink heavily · FAE – 3 to 5 per 1000 births, 90 per 1000 among women who drink heavily · FASD is leading cause of mental retardation in the western world
Pathophysiology • Combination of – Toxic effects of ethanol and it’s derivatives – Nutritional factors – Genetic predisposition
Toxic effects • Both alcohol and derivative acetaldehyde directly damage developing and mature nervous systems • Impair nucleic acid synthesis • Disrupts protein synthesis • Cell membrane narcosis • High maternal alcohol levels associated with dehydration, fetal hypoxia and acidosis, placental pathology and dysfunction, and endocrine disturbances.
Nutrition Related Effects of Alcohol • Poor nutritional status of mother • Reduced placental transfer of zinc and folic acid associated in animal models • Alcohol impairs absorption, utilization, and metabolism of nutrients • Poor zinc status has been associated with adverse effects of alcohol many studies
Surgeon General’s Advisory (2005) • Science: – Alcohol consumed during pregnancy increases the risk of alcohol related birth defects, including growth deficiencies, facial abnormalities, central nervous system impairment, behavioral disorders, and impaired intellectual development. – No amount of alcohol consumption can be considered safe during pregnancy. – Alcohol can damage a fetus at any stage of pregnancy. Damage can occur in the earliest weeks of pregnancy, even before a woman knows that she is pregnant. – The cognitive deficits and behavioral problems resulting from prenatal alcohol exposure are lifelong. – Alcohol-related birth defects are completely preventable
Surgeon General’s Advisory (2005) Recommendations: 1. 2. 3. 4. 5. A pregnant woman should not drink alcohol during pregnancy. A pregnant woman who has already consumed alcohol during her pregnancy should stop in order to minimize further risk. A woman who is considering becoming pregnant should abstain from alcohol. Recognizing that nearly half of all births in the United States are unplanned, women of child-bearing age should consult their physician and take steps to reduce the possibility of prenatal alcohol exposure. Health professionals should inquire routinely about alcohol consumption by women of childbearing age, inform them of the risks of alcohol consumption during pregnancy, and advise them not to drink alcoholic beverages during pregnancy.
Caffeine • History: – Rat based studies with high levels of caffeine found adverse pregnancy outcomes – Early 1980 s US FDA issued advisory about adverse effects of caffeine in pregnancy – Further research found little association, FDA concludes that no strong evidence, urges moderation – 1996 IOM review for WIC advised removing excessive caffeine intake from WIC risk criteria – 1998 - USDA removed as WIC risk criteria
The Effects of Caffeine on Pregnancy Outcome Variables (Hinds et al. Nutrition Review, 1996) • Consumption: – In US 70 -95% of pregnant women consume caffeine - average intake is 99185 mg/day – 5 -30% of pregnant women consume >300 mg/day – Heavy caffeine intake more likely in women who smoke and those with lower education levels
The Effects of Caffeine on Pregnancy Outcome Variables (Hinds et al. Nutrition Review, 1996) • Metabolism – methylxantines cross the placenta to the fetus where an equilibrium is achieved between maternal and fetal plasma – half-life of caffeine in pregnancy changes from 5. 2 to 18. 1 hours in T 2 and T 3 and returns to non-pg levels a few weeks pp
Caffeine Metabolism, Genetics and Perinatal Outcomes (Ann Epidemiol 2005) • Wide individual variation in caffeine metabolism – Due to variation in CYP 1 A 2 enzyme activity • “Measuring maternal, fetal and neonatal caffeine metabolites may allow for a more precise measure of fetal caffeine exposure. ”
Maternal exposure to caffeine and risk of congenital anomalies (Brown, Epidemiology, 2006) • Review of 7 (of 25 published) studies that met inclusion criteria • Conclusion: “There is no evidence to support a teratogenic effect of caffeine in humans. Current epidemiologic evidence is not adequate to assess the possibility of a small change in risk of congenital anomalies resulting from maternal caffeine consumption. ”
Maternal Caffeine Consumption and Spontaneous Abortion: Review of Epidemiologic Evidence (Epidemiology, 2004) • Most studies find positive association between maternal caffeine intake and sp ab, but causality has not been established • All studies have limitations: – selection and recall bias – poor exposure measurements – issues related to timing of exposure and fetal demise • (Lively discussion in other venues: Are women who have strong coffee aversion due to nausea early in pregnancy more likely to sustain pregnancy? Ann Epi, 2006)
Coffee and Health: A Review of Recent Human Research (Higdon and Frei; Crit Rev Food Sci and Nutrition, 2006)
Conception • Many studies find > 300 mg/d associated with delay in time to conception (some do not find this effect) • Author’s conclusions: “it may be prudent for women who are having difficulty conceiving to limit caffeine consumption to less than 300 mg/d in addition to eliminating tobacco use and decreasing alcohol consumption. ”
Spontaneous Abortion • Conflicting studies • Women who decrease Caffeine due to N&V, more likely to have viable pregnancies. • “Most studies that observed significant associations between self-reported coffee or caffeine consumption and the risk of spontaneous abortion did so at intake levels of at least 300 mg/d of caffeine. ”
Fetal Growth • “Several studies found that maternal caffeine intakes ranging from 200 -400 mg/d were associated with decreases in mean birth weight of about 100 g. ” • “A meta-analysis that combined the results of eight epidemiological studies found that maternal caffeine consumption greater than 150 mg/d increased the risk of low birth weight by approximately 50%. ”
Preterm Delivery • “Most epidemiological studies have not found coffee or caffeine consumption to be associated with the risk of preterm delivery. ”
Birth Defects • “At present, there is no convincing evidence from epidemiological studies that maternal caffeine consumption ranging from 300 -1000 mg/d increases the risk of congenital malformations in humans. ”
Coffee and Health: A Review of Recent Human Research (Higdon and Frei; crit rev food sci and nutrition, 2006) • “Currently available evidence suggests that it may be prudent for pregnant women to limit coffee consumption to 3 cups/d providing no more than 300 mg/d of caffeine to exclude any increased probability of spontaneous abortion of impaired fetal growth. ”
Smoking • 25 -30% of US women smoke during pregnancy; down from 40% in 1967 • Cochran review found that 30 trials of intensive intervention programs in pregnant women lead to smoking cessation in 6. 6 -9. 2% of women.
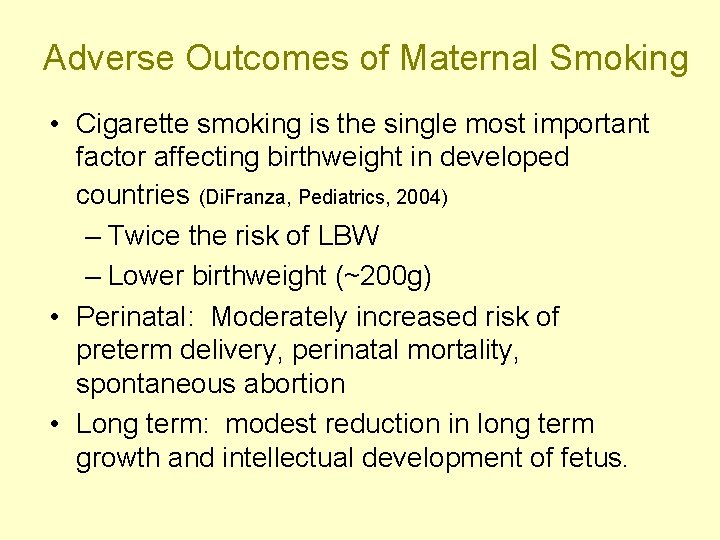
Adverse Outcomes of Maternal Smoking • Cigarette smoking is the single most important factor affecting birthweight in developed countries (Di. Franza, Pediatrics, 2004) – Twice the risk of LBW – Lower birthweight (~200 g) • Perinatal: Moderately increased risk of preterm delivery, perinatal mortality, spontaneous abortion • Long term: modest reduction in long term growth and intellectual development of fetus.
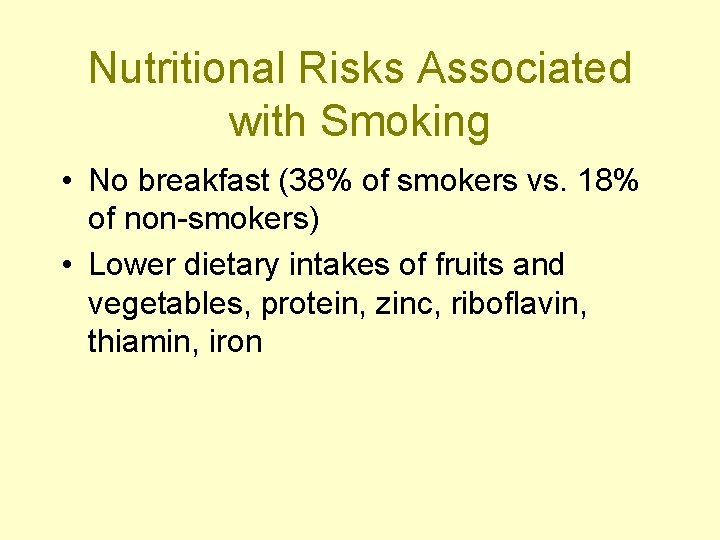
Nutritional Risks Associated with Smoking • No breakfast (38% of smokers vs. 18% of non-smokers) • Lower dietary intakes of fruits and vegetables, protein, zinc, riboflavin, thiamin, iron
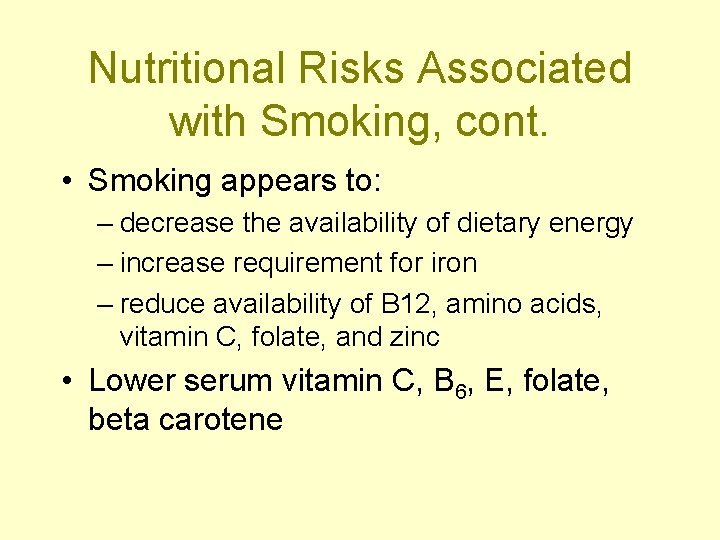
Nutritional Risks Associated with Smoking, cont. • Smoking appears to: – decrease the availability of dietary energy – increase requirement for iron – reduce availability of B 12, amino acids, vitamin C, folate, and zinc • Lower serum vitamin C, B 6, E, folate, beta carotene
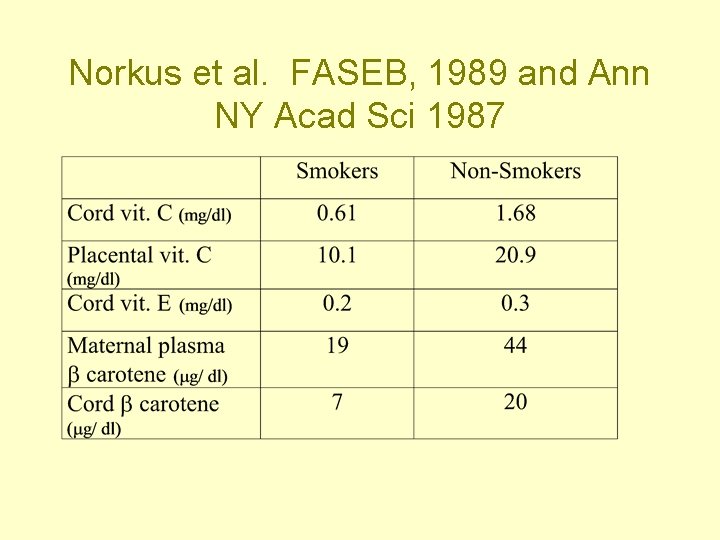
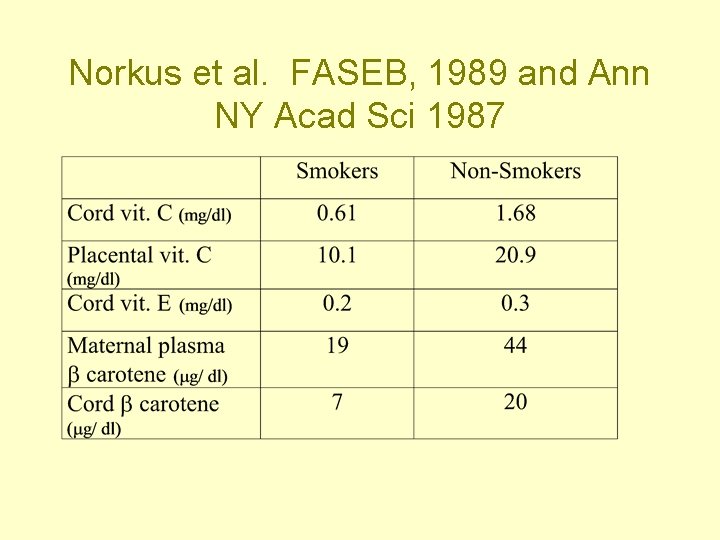
Norkus et al. FASEB, 1989 and Ann NY Acad Sci 1987
Vitamin C and PROM • PROM occurs in 8 -10 % of all pregnancies • Vitamin C is required for collagen synthesis • Maternal plasma and placental vitamin C is lower in women with PROM
Nutritional Risks Associated with Smoking, cont. • Increased carboxyhemoglobin in smokers blood leads to requires increased cutoff point for anemia in smokers. • Women who smoke may have lower prepregnancy weights and may have lower pregnancy weight gains.
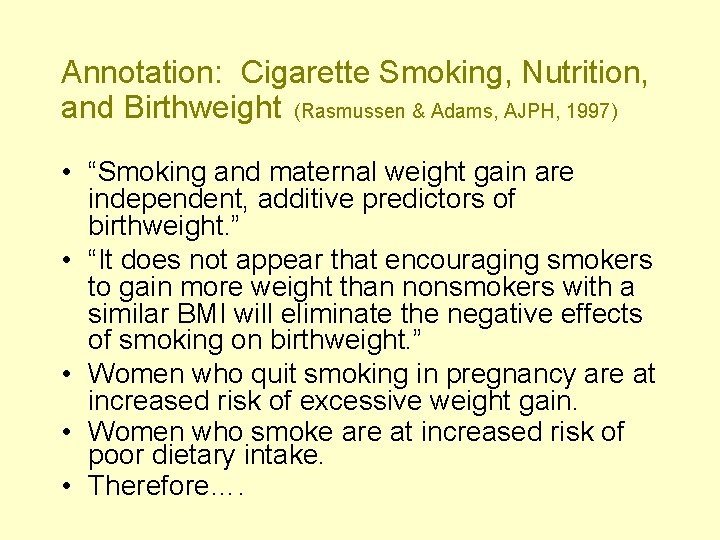
Annotation: Cigarette Smoking, Nutrition, and Birthweight (Rasmussen & Adams, AJPH, 1997) • “Smoking and maternal weight gain are independent, additive predictors of birthweight. ” • “It does not appear that encouraging smokers to gain more weight than nonsmokers with a similar BMI will eliminate the negative effects of smoking on birthweight. ” • Women who quit smoking in pregnancy are at increased risk of excessive weight gain. • Women who smoke are at increased risk of poor dietary intake. • Therefore….
Annotation: Cigarette Smoking, Nutrition, and Birthweight (Rasmussen & Adams, AJPH, 1997) “…individualized nutrition counseling is recommended in addition to smoking cessation. ”
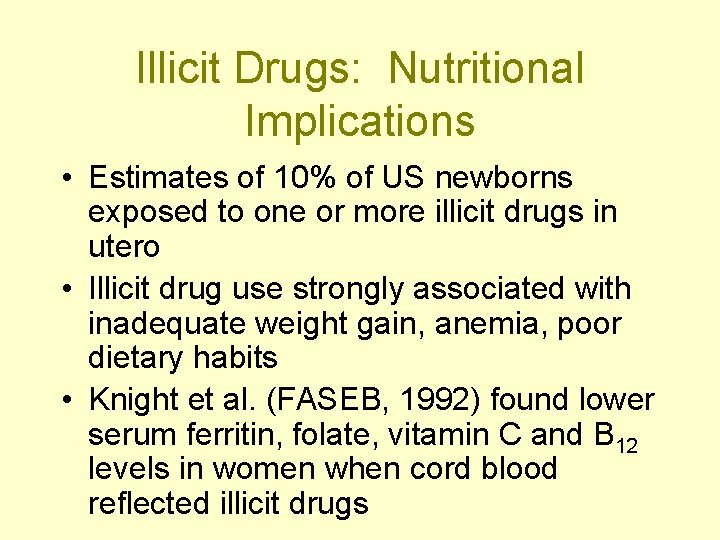
Illicit Drugs: Nutritional Implications • Estimates of 10% of US newborns exposed to one or more illicit drugs in utero • Illicit drug use strongly associated with inadequate weight gain, anemia, poor dietary habits • Knight et al. (FASEB, 1992) found lower serum ferritin, folate, vitamin C and B 12 levels in women when cord blood reflected illicit drugs
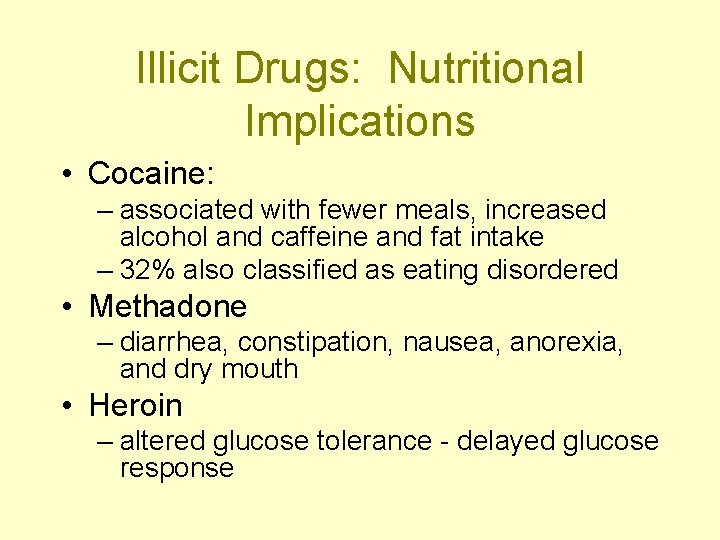
Illicit Drugs: Nutritional Implications • Cocaine: – associated with fewer meals, increased alcohol and caffeine and fat intake – 32% also classified as eating disordered • Methadone – diarrhea, constipation, nausea, anorexia, and dry mouth • Heroin – altered glucose tolerance - delayed glucose response
Position of the American Dietetic Association: Use of nutritive and nonnutritive sweeteners (Affirmed 2000, in effect until 2009) • Toxicity testing during reproduction is required for FDA approval. • “The safety of acesulfame-K, aspartame, sucralose, and neotame in pregnancy has been determined with rat studies. ” • Saccharin can cross the placenta and may remain in fetal tissues because of slow fetal clearance - It has been suggested that women consider careful use of saccharin during pregnancy.
Position of the American Dietetic Association: Use of nutritive and nonnutritive sweeteners • Aspartame: issue relates to fetal exposure to aspartic acid, phe, or methanol. – Animal models show no changed fetal exposure to aspartic acid with aspartame – Maternal bolus of aspartame at the 99 th %ile of intake results in peak plasma phe level in both normal (1. 85 mg/dl) and PKU heterozygote subjects (2. 67 mg/dl) below levels associated with neurological problems (18 mg/dl) – Plasma response of methanol and formate are not significant after aspartame load • “Use of aspartame within FDA guidelines appears safe for pregnant women. ”
Exercise • Benefits: – improved or maintained fitness – reduces anxiety and depression – eases pregnancy discomforts such as constipation, backache, fatigue and varicose veins
Exercise • Contraindications – previous experience of preterm labor – ob complications including vaginal bleeding, incompetent cervix, ruptured membranes, compromised fetal growth – Hx of medical problems (hypertension, heart disease, etc. ) requires health care provider approval
Exercise • Changes with pregnancy – tolerance for strenuous exercise decreases as pregnancy progresses • work of breathing increases as enlarging uterus crowds the diaphragm • oxygen needs increase – if lying flat on back after the 4 th month, risk of compression of vena cava with dizziness and interference with blood flow to the uterus
Exercise Changes with pregnancy, cont. – may have increased efficiency of heat dissipation – altered sense of balance with shift in center of gravity – high hormonal levels associated with lax connective tissue and increased joint susceptibility
Cochrane: Aerobic Exercise for Women During Pregnancy (2006) • 11 trials involving 472 women • “The trials were not of high methodologic quality. ” • Results: – Regular aerobic exercise during pregnancy appears to improve (or maintain) maternal physical fitness – Non significant, but concerning increased risk of preterm birth in exercise groups. From 7 trials: Pooled RR 1. 82 (95% CI 0. 35 -9. 57). – Data insufficient to infer important risk or benefits for mother or infant
Continuous, Strenuous, Vigorous Activity Throughout Pregnancy (Gunderson, Clin Obstet gynecology, 2003) • Can reduce birth weight & length of gestation • Additional carbohydrate recommended before activity • Increased need for B vitamins • Careful screening for nutritional & herbal supplements • Athletes at higher risk for Fe depletion.
Exercise during pregnancy and the postpartum period. ACOG Committee on Obstetric Practice. January 2002 “The current Centers for Disease Control and Prevention and American College of Sports Medicine recommendation for exercise, aimed at improving the health and well-being of nonpregnant individuals, suggests that an accumulation of 30 minutes or more of moderate exercise a day should occur on most, if not all, days of the week. In the absence of either medical or obstetric complications, pregnant women also can adopt this recommendation. ”
Exercise during pregnancy and the postpartum period. ACOG Committee on Obstetric Practice. January 2002 • Exercise may be beneficial in primary prevention of GDM • Avoid – supine position (may result in obstruction of venous return) – motionless standing – exertion above 6, 000 feet altitude
Avoid • Sports with high potential for trauma: ice hockey, soccer, basketball • Increased risk of falling: gymnastics, downhill skiing, vigorous racket sports, horseback riding • Scuba diving (increased risk of decompression sickness)
Postpartum • Physiological changes persist 4 to 6 weeks postpartum • Return to vigorous exercise should be gradual • Return to physical activity may be protective against postpartum depression if exercise is stress relieving - not inducing



Oral Health: Major Concepts (Academy of General Dentistry) • Increased risk for gingivitis (red, swollen, tender gums that are more likely to bleed) associated with increased estrogen and progesterone • Frequent consumption of high cho foods may be used to combat nausea • Cariogenic bacteria may be passed from mother to infant • Periodontal disease is associated with preterm birth
Pregnancy Gingivitis • 30 -75% of women experience gingival changes such as edema, hyperplasia, redness, and bleeding • Hormonal changes cause greater reaction to dental plaque • Women who are plaque and inflammation-free at beginning of pregnancy have only 0. 03 chance of gingivitis
Periodontitis • Definition: an infection caused by specific bacterial plaque that involves loss of bone, fiber, and gum tissue attachment for the tooth. • Smoking associated with increased prevalence and severity of periodontitis • Periodontal infections caused by gramnegative pathogens are associated with increase in preterm delivery and/or PROM one mediating factor is prostaglandin production triggered by bacterial products. • Women with diabetes are at higher risk
Periodontitis (cont. ) • Pathogens and bacterial products may translocate and inhibit normal clearance of enteric organisms from genitourinary tract. • Overgrowth of gram negative bacteria and infection can be associated with preterm birth.
Can preterm birth be prevented by periodontal treatment? • NIDCR funded two large RCT – women assigned to treatment or no treatment – Oral Therapy to Reduce Obstetric Risk (OPT) – results published in 2006 – Maternal Oral Therapy to Reduce Obstetric Risk (MOTOR) – results due in 2008
OPT: Treatment of Periodontal Disease and the Risk of Preterm Birth (Michalowicz et al. NEJM, Nov. 2006) • 823 women with periodontal disease, enrolled between 13 -17 weeks gestation, randomized to: – Scaling and root planing before 21 weeks; monthly polishings – Scaling and root planing after delivery • Major Outcomes: – no difference in rates of preterm birth or low birthweight – no adverse outcomes associated with treatment
Periodontal Health and Birth Outcomes (Xu et al. Ob Gyn Survey, 2007) • Evidence of an association between periodontal disease and increased risk of preterm birth and low birthweight, especially in economically disadvantaged populations, but potential biases and limited number of RCTs. • “Currently, there is insufficient evidence to support the provision of treatment during pregnancy for the purpose of reducing adverse birth outcomes. ”
American Academy of Periodontology Statement Regarding Periodontal Management of the Pregnant Patient (2004) • Achieve a high level of oral hygiene prior to becoming pregnant and throughout pregnancy • Periodonal treatment (eg; scaling and root planing) is usually scheduled in second trimester • Emergencies such as acute infection and abcess may require immediate treatment regardless of stage of pregnancy) • Consultation with prenatal care provider
Oral Health: Recommendations • Frequent dental cleanings (3 to 6 months) • Daily oral care routines including brushing and flossing at least twice daily and after eating • Use of toothpastes and rinses with fluoride • Consider cariogensis in food choices and patterns. • Offer smoking cessation programs
 Nausea elderly woman
Nausea elderly woman Antiemetic pediatric dose
Antiemetic pediatric dose Anorexia, nausea and vomiting
Anorexia, nausea and vomiting 2008 2008
2008 2008 Jamaica health and lifestyle survey
Jamaica health and lifestyle survey Exercise health and lifestyle
Exercise health and lifestyle Exercise health and lifestyle
Exercise health and lifestyle Exercise health and lifestyle
Exercise health and lifestyle Nice guidelines diarrhoea and vomiting in adults
Nice guidelines diarrhoea and vomiting in adults Concussion and contusion
Concussion and contusion Perimenopausa
Perimenopausa Atrofia vaginale
Atrofia vaginale Hiatal hernia nausea
Hiatal hernia nausea Existetialism
Existetialism Hyperkalemia symptoms and signs
Hyperkalemia symptoms and signs Nursing intervention of vomiting
Nursing intervention of vomiting Vomiting centre in brain
Vomiting centre in brain Vomiting reflex
Vomiting reflex Substance p vomiting
Substance p vomiting Gastric outlet obstruction differential diagnosis
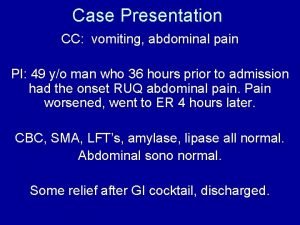
Gastric outlet obstruction differential diagnosis Vomiting case presentation
Vomiting case presentation Vomiting
Vomiting Vomiting types
Vomiting types Vomiting blood
Vomiting blood Xyphoidynia
Xyphoidynia Causes of abdominal pain in children
Causes of abdominal pain in children Ascites mnemonic
Ascites mnemonic Pregnant or period
Pregnant or period Health and social care act 2008
Health and social care act 2008 Health and social care act regulated activities
Health and social care act regulated activities Lifestyle modern
Lifestyle modern Lifestyle hobbies
Lifestyle hobbies Oxid wms
Oxid wms Introduction to wellness fitness and lifestyle management
Introduction to wellness fitness and lifestyle management Wellness and lifestyle management
Wellness and lifestyle management Self concept and lifestyle
Self concept and lifestyle Sparta lifestyle
Sparta lifestyle Hobbies and leisure time
Hobbies and leisure time Hhs
Hhs Infant oral health care
Infant oral health care Health and social care component 3 health and wellbeing
Health and social care component 3 health and wellbeing Healthy lifestyle wrap up lecture
Healthy lifestyle wrap up lecture Packet countable or uncountable
Packet countable or uncountable Healthy living sentences
Healthy living sentences Anunsyo klasipikado meaning
Anunsyo klasipikado meaning Domestic discipline contracts
Domestic discipline contracts Chapter 1 making wellness a lifestyle
Chapter 1 making wellness a lifestyle What was the nomadic lifestyle
What was the nomadic lifestyle Lesson 3-4 lifestyle answer key
Lesson 3-4 lifestyle answer key Lifestyle dimensions
Lifestyle dimensions Gaa life style
Gaa life style Seventh day adventist lifestyle
Seventh day adventist lifestyle Jelaskan peranan keluarga dalam gaya hidup modern
Jelaskan peranan keluarga dalam gaya hidup modern Healthy lifestyle moodboard
Healthy lifestyle moodboard Unit 2 lifestyle
Unit 2 lifestyle Teenager unhealthy lifestyle essay
Teenager unhealthy lifestyle essay Planning gaa
Planning gaa Gaa lifestyle
Gaa lifestyle Lifestyle reporting
Lifestyle reporting Acrostic poem life
Acrostic poem life Active lifestyle definition
Active lifestyle definition Lifestyle performance profile
Lifestyle performance profile Marita leachon
Marita leachon Ayurvedic lifestyle consultant
Ayurvedic lifestyle consultant Factors affecting oxygenation pdf
Factors affecting oxygenation pdf Athens and sparta classroom activities
Athens and sparta classroom activities Industrial lifestyle
Industrial lifestyle Masters in lifestyle medicine
Masters in lifestyle medicine Now lifestyle autoresponder
Now lifestyle autoresponder Lifestyle
Lifestyle Lifestyle medicine
Lifestyle medicine Lifestyle entrepreneur characteristics
Lifestyle entrepreneur characteristics 101 lolitas
101 lolitas Thedacare lifestyle intervention program
Thedacare lifestyle intervention program Www.youtube
Www.youtube Lifestyle entrepreneurship
Lifestyle entrepreneurship Endocrinologist lifestyle
Endocrinologist lifestyle Food related lifestyle model
Food related lifestyle model Firstbeat lifestyle assessment
Firstbeat lifestyle assessment Atkins lifestyle
Atkins lifestyle Performance lifestyle advisor
Performance lifestyle advisor Compare sparta and athens
Compare sparta and athens How are giraffes long necks adapted to their lifestyle
How are giraffes long necks adapted to their lifestyle Lifestyle countable or uncountable
Lifestyle countable or uncountable