CLINICAL PATHOLOGICAL CONFERENCE PEDIATRICS UMAR SOOMRO 4 th














- Slides: 43
CLINICAL PATHOLOGICAL CONFERENCE - PEDIATRICS UMAR SOOMRO 4 th Year MBBS JINNAH MEDICAL & DENTAL COLLEGE KARACHI, PAKISTAN 1
CASE A 9 month old male infant, came to the ward through OPD on 18 th November 2019, weighing 7. 7 kg, with presenting complaints of fever, loose stools and vomiting for one week. 2

BIO DATA � Age: 9 months � Male infant � Weighing 7. 7 kg � OPD - admitted 18 th November 2019 3
PRESENTING COMPLAINTS � Fever for 1 week � Vomiting and passage of loose stools for 1 week 4
HISTORY OF PRESENTING COMPLAINTS � Patient was in his usual state of health a week before the date of admission until he developed sudden onset of fever which was documented by the mother to be 101*F � Fever was intermittent and aggravated during evening hours and used to subside during the day time and was also temporarily relieved after taking anti-pyretic medication � Fever was not associated with rigors and chills however it was associated with cold extremities 5
HOPC (continued) � Patient also had complaints of vomiting � Vomiting was non-projectile, about a table spoon in volume, after feed, 2 -3 times a day, usually emitted contents fed � He also had complaints of loose stools which were soft, odorless, 4 -5 times a day, had no relation with feed � Took medication at home including Flagyl, and Zinc supplements which temporarily relieved the symptoms 6

HOPC (continued) � Mother also complained of developing generalized rash all over the body after 2 days of onset of fever which resembled allergic reaction as appreciated by mother � However, the rash started vanishing with in 2 days, from the body in a head to toe pattern. � The child was brought to the ward via OPD, where he was given IV fluids. Blood samples were sent on daily bases. The child was also given oral Zinc supplements � Intensity of fever, frequency of vomiting and passage of loose stools was improved. 7
SYSTEMIC REVIEW � CNS—Child was irritable and sleepy � Cardiovascular— N/S � Respiratory–N/S � Urinary—N/S � Abdominal—Passage of loose stools 8
Past History Past Medical � � No history of previous admissions Blood Transfusions—N/S Drug Hx– N/S Allergy—N/S Past Surgical Unremarkable 9

BIRTH HISTORY � Ante-Natal: The case was registered in JMCH Regular Ante-natal check-ups were done Mother had the desired nutritional intake during gestation She took Folic acid supplements and Iron supplements No history of developing gestational diabetes Routine tests were performed along with Ultra sounds Had no history of smoking, alcohol consumption or substance abuse � Natal: Delivery held at Hospital Full termed, vaginal delivery No complications at the time of birth reported, No history of cord prolapse Baby was not cyanosed and did not require resuscitation � Post-Natal: Child cried after birth Child was not cyanosed Physiological Jaundice appeared 2 days after the birth and subsided 3 days later 10
Feeding History � � � First feed was given 1 hour after birth Exclusively breastfed Breast feeding continued till date Weaning started at 6 months of age (custard) Fruit and vegetable diet—Poor Staple diet (wheat, barley, rice etc)—Poor 11

Developmental History � � � � Eye contact and social smile at 6 weeks Neck support started at 4 months of age Babbling started (6 months) Sits without support (8 months) Started Crawling (9 months) Can stand by support Visually alert to stimulus Responds on calling name 12

Family History FATHER Patient was the second product of a non-consanguineous marriage. First child was healthy with no antenatal, natal or post-natal � complications. First Child MOTHER Second Child (The Patient) 13
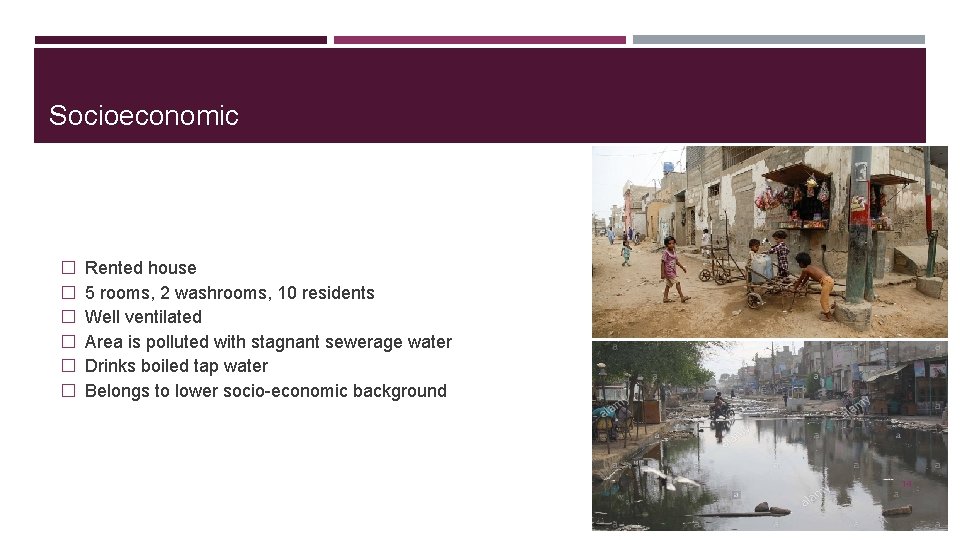
Socioeconomic � � � Rented house 5 rooms, 2 washrooms, 10 residents Well ventilated Area is polluted with stagnant sewerage water Drinks boiled tap water Belongs to lower socio-economic background 14
EXAMINATION � � � � The patient looked weak and lethargic and was irritable CNS Examination: GCS 15/15, motor and sensory examination were unremarkable CVS Examination: Pulses were weak, cold peripheries, tacchycardic 150 bpm, audible S 1, S 2, CRT 2 -3 seconds Respiratory: Resp. rate was 55 bpm, vesicular breathing, no added sounds Urinary: Unremarkable Abdominal/GI: Abdomen tender, no palpable swelling, increased gut sounds FOC— 46 cm Mid-arm Circumference— 15 cm Length— 68 cm Temperature— 99*F Pallor—Unremarkable Jaundice—Unremarkable Cyanosis—Unremarkable CVS and Respiratory review and examination gave a clue of the patient to be in compensated shock 15
Differential Diagnosis � � Malaria Enteric Fever Dengue Fever Acute Gastroenteritis 16

Inclusion/Exclusion Criteria Malaria INCLUSION Intermittent fever Vomiting EXCLUSION No history of rigors and chills No splenomegaly Presence of diarrhea 17
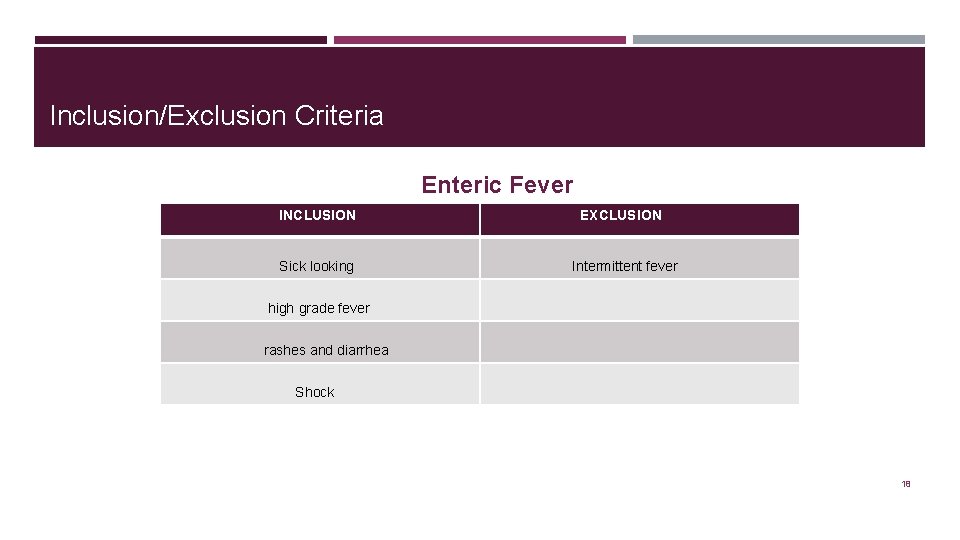
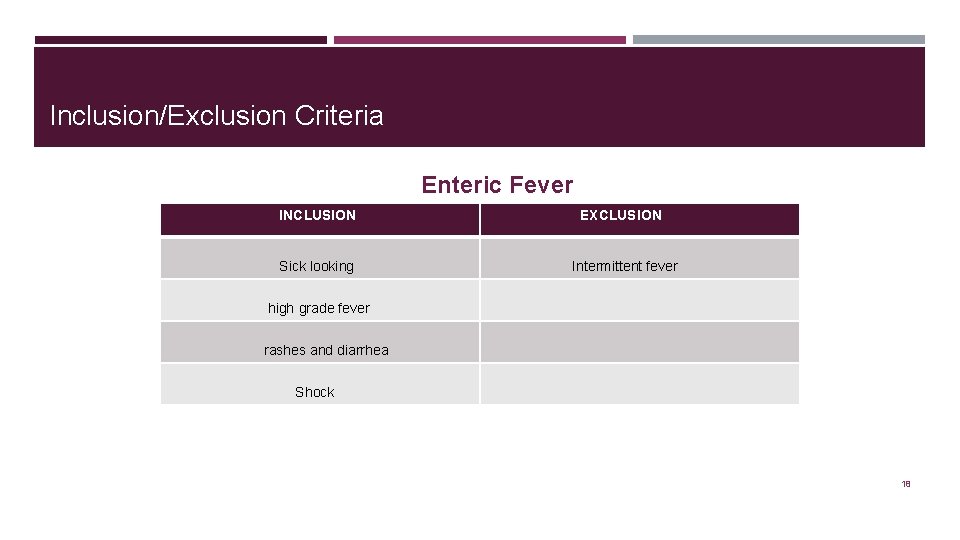
Inclusion/Exclusion Criteria Enteric Fever INCLUSION Sick looking EXCLUSION Intermittent fever high grade fever rashes and diarrhea Shock 18

Inclusion/Exclusion Criteria Dengue Fever INCLUSION Shock EXCLUSION Loose stools High grade fever 19
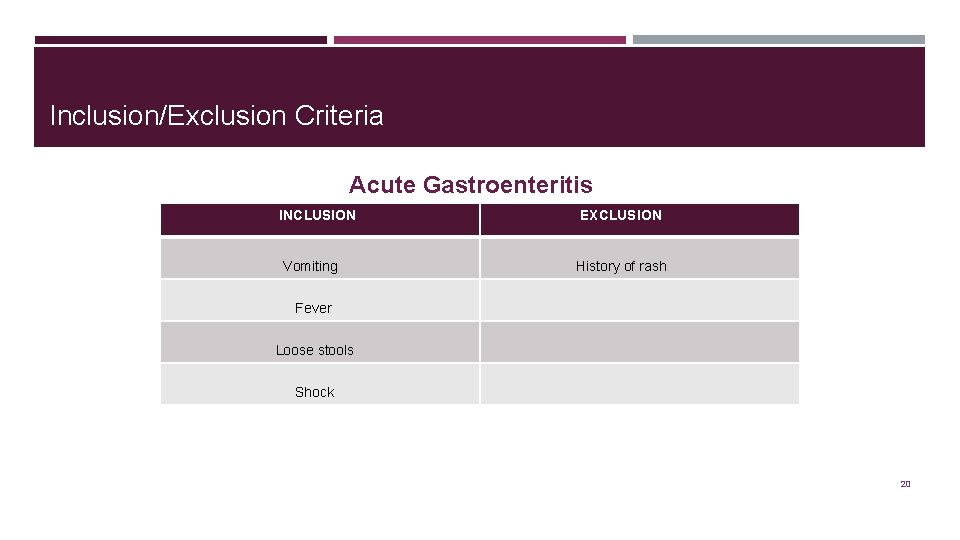
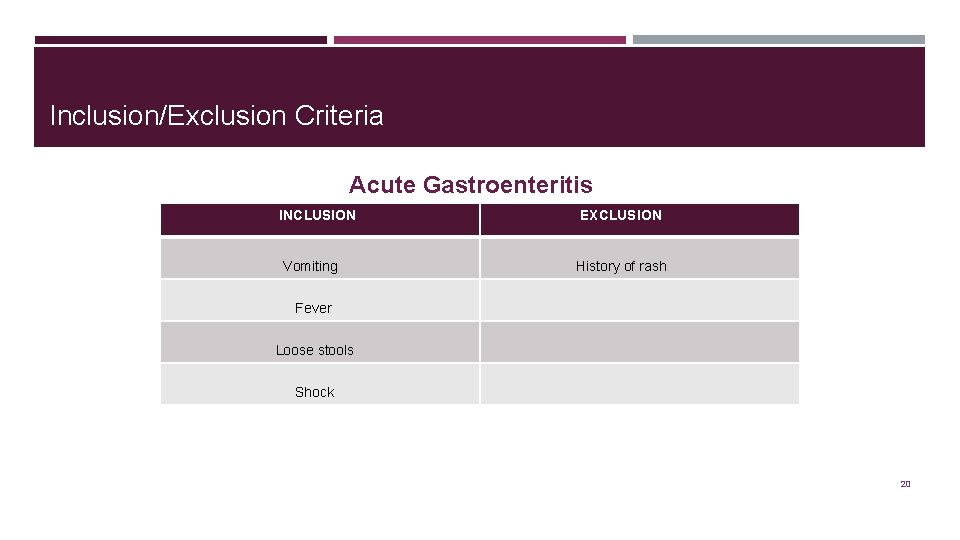
Inclusion/Exclusion Criteria Acute Gastroenteritis INCLUSION Vomiting EXCLUSION History of rash Fever Loose stools Shock 20
Final Diagnosis DENGUE FEVER 21
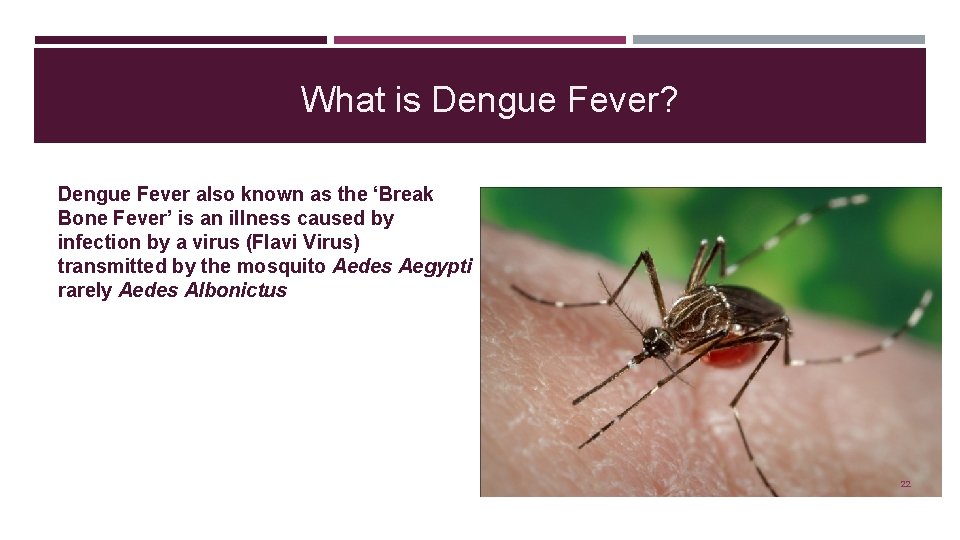
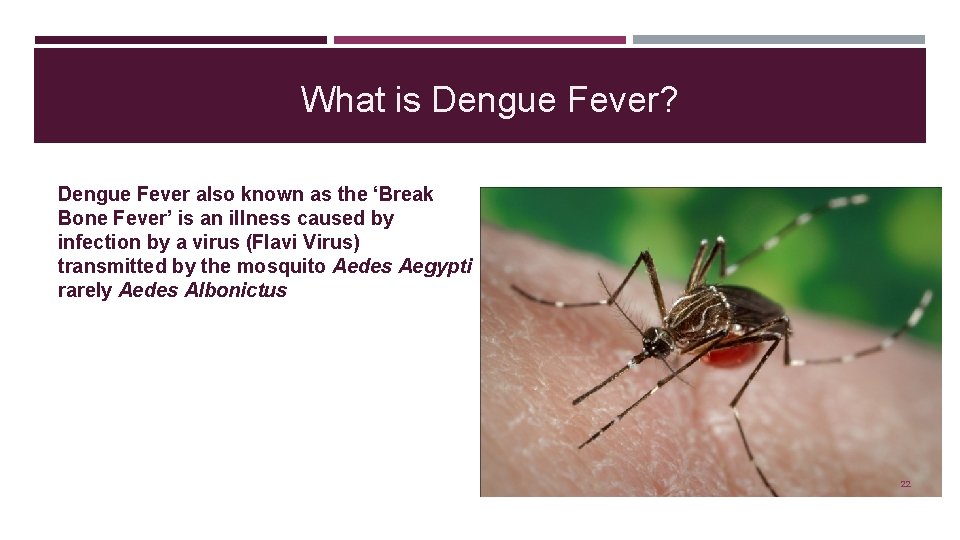
What is Dengue Fever? Dengue Fever also known as the ‘Break Bone Fever’ is an illness caused by infection by a virus (Flavi Virus) transmitted by the mosquito Aedes Aegypti rarely Aedes Albonictus 22
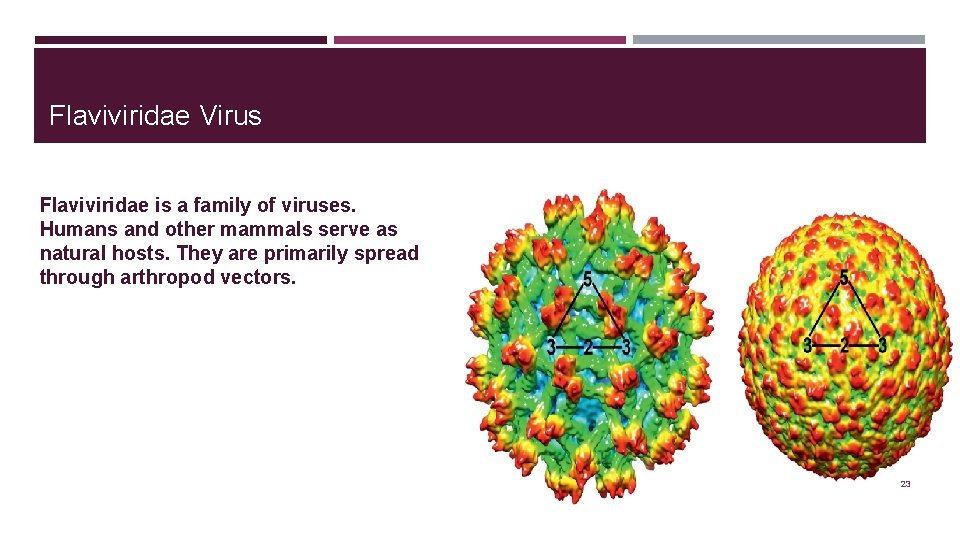
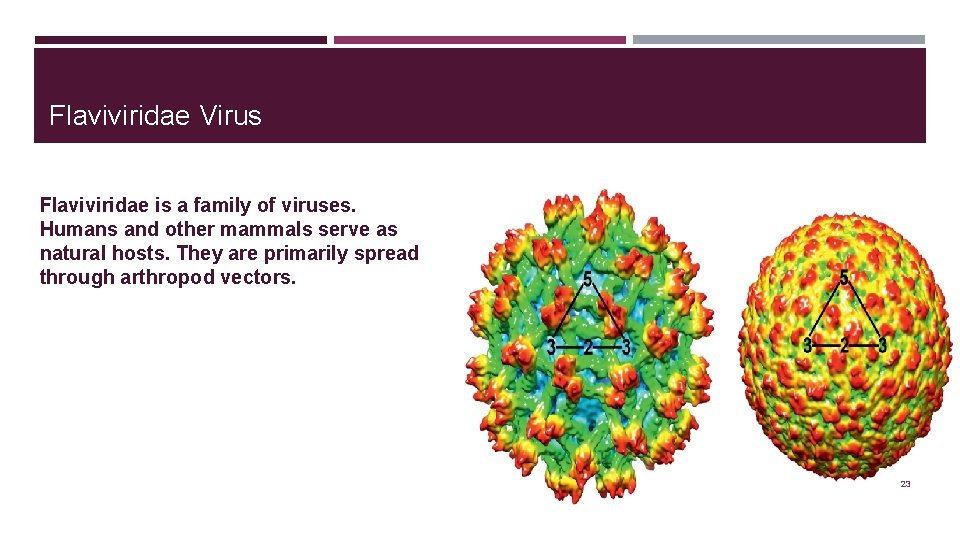
Flaviviridae Virus Flaviviridae is a family of viruses. Humans and other mammals serve as natural hosts. They are primarily spread through arthropod vectors. 23
Characteristics of Aedes Aegypti � One distinct physical feature – black and white stripes on its body and legs � Bites during the day � Lays its eggs in clean, stagnant water 24
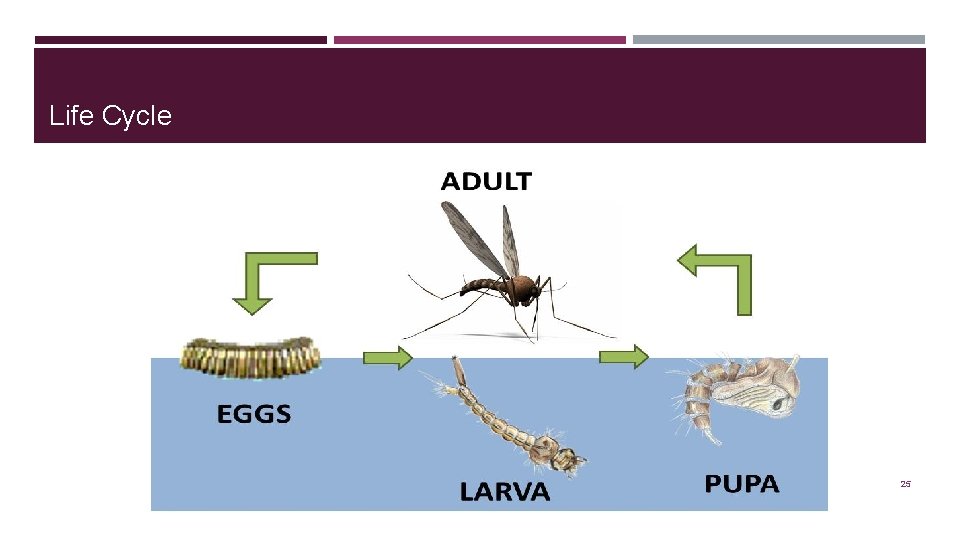
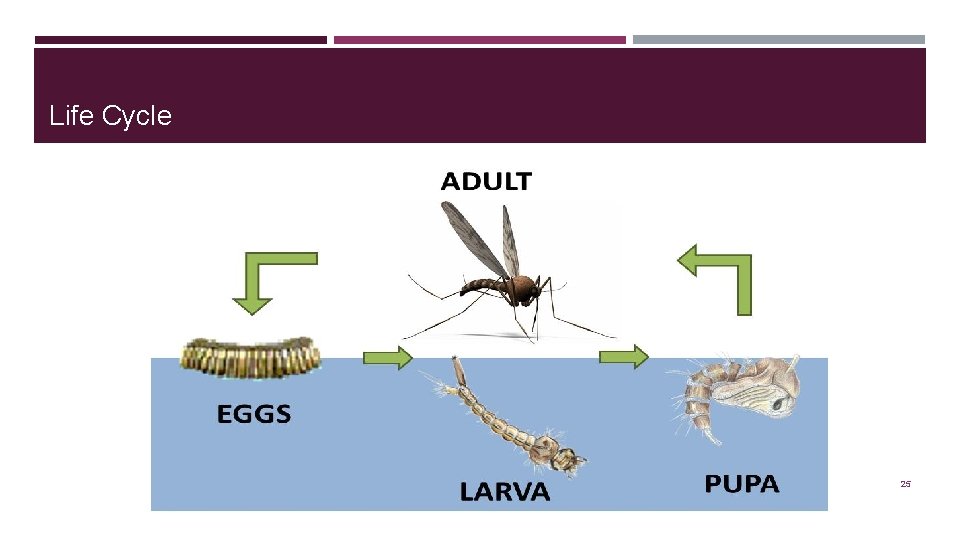
Life Cycle 25
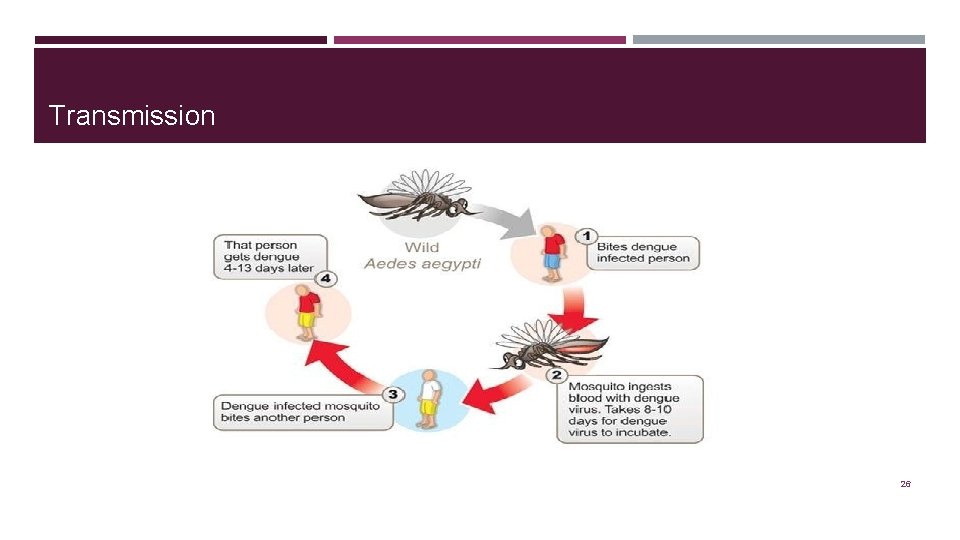
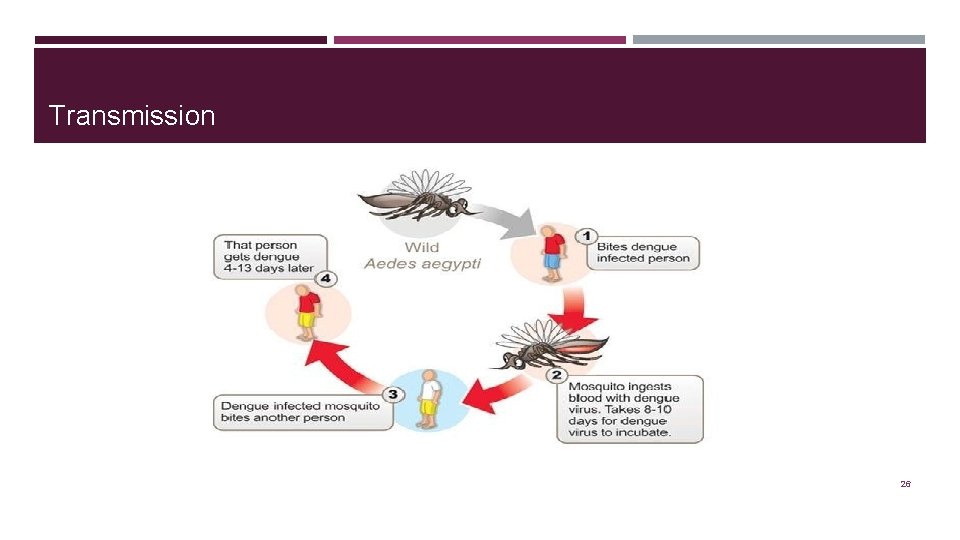
Transmission 26

Global Status of Dengue � New infections annually -- 50 million � Death -- 24, 000 annually � People at risk -- 2. 5 to 3 bn � Hospitalized cases -- 50, 000 /yr (90% affected are children) � Disease burden -- 4, 65, 000 27
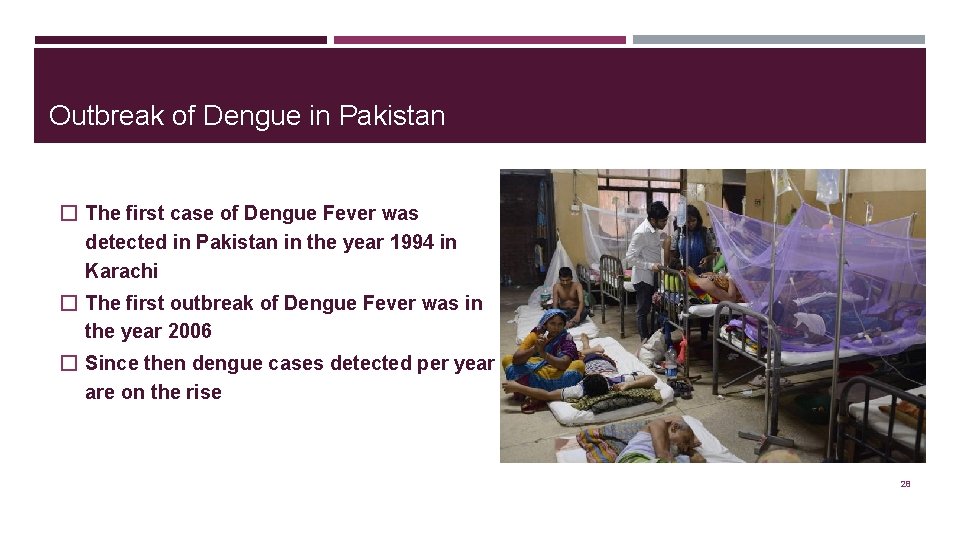
Outbreak of Dengue in Pakistan � The first case of Dengue Fever was detected in Pakistan in the year 1994 in Karachi � The first outbreak of Dengue Fever was in the year 2006 � Since then dengue cases detected per year are on the rise 28

Causes � Unplanned urban overpopulation of areas � Inadequate housing and public health systems (water, sewerage and waste management) � Poor vector control, e. g. , stagnant pools of water for mosquito breeding � Climate change and viral evolution � Increased international travel (recreational, business or military) to endemic areas 29

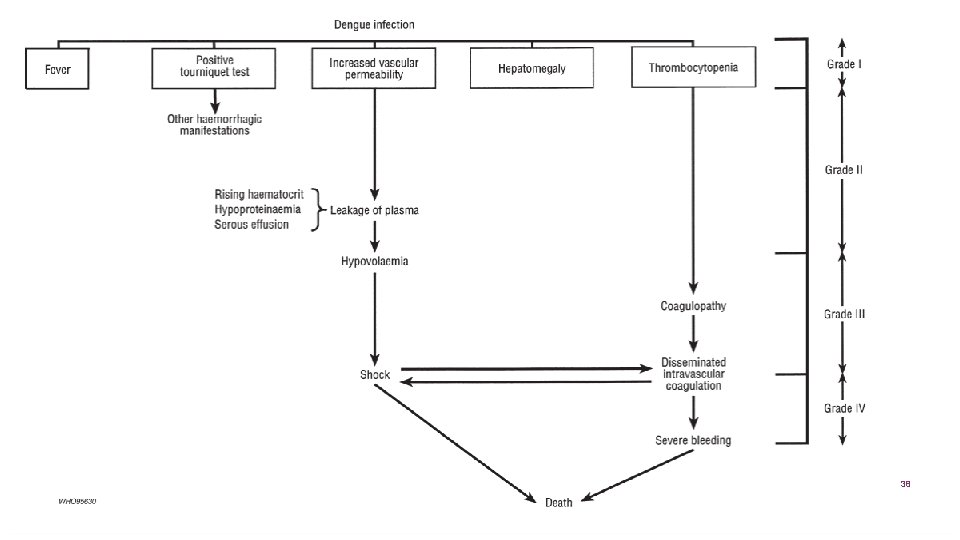
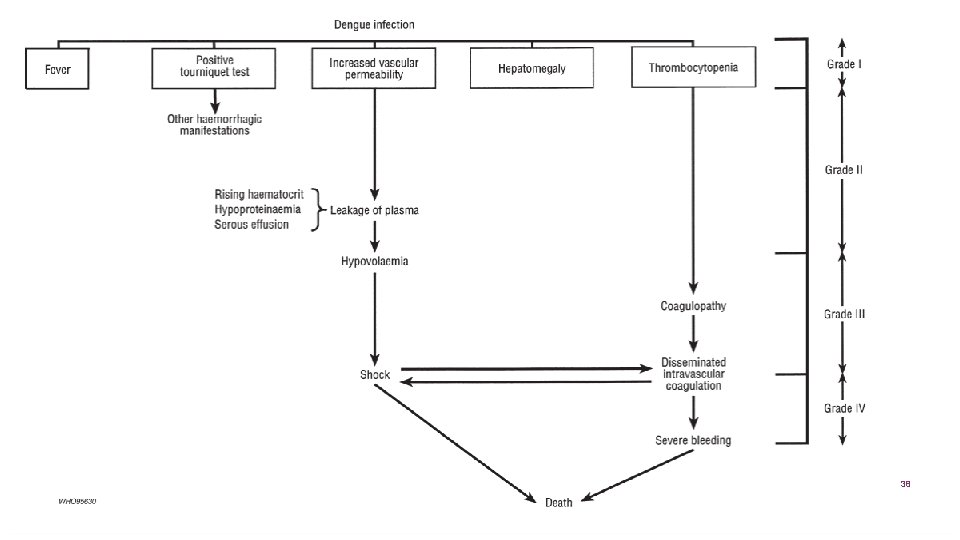
Manifestation of Dengue Fever ➢ Dengue Fever (DF) ➢ Dengue Hemorrhagic Fever (DHF) ➢ Dengue Shock Syndrome (DSS) 30
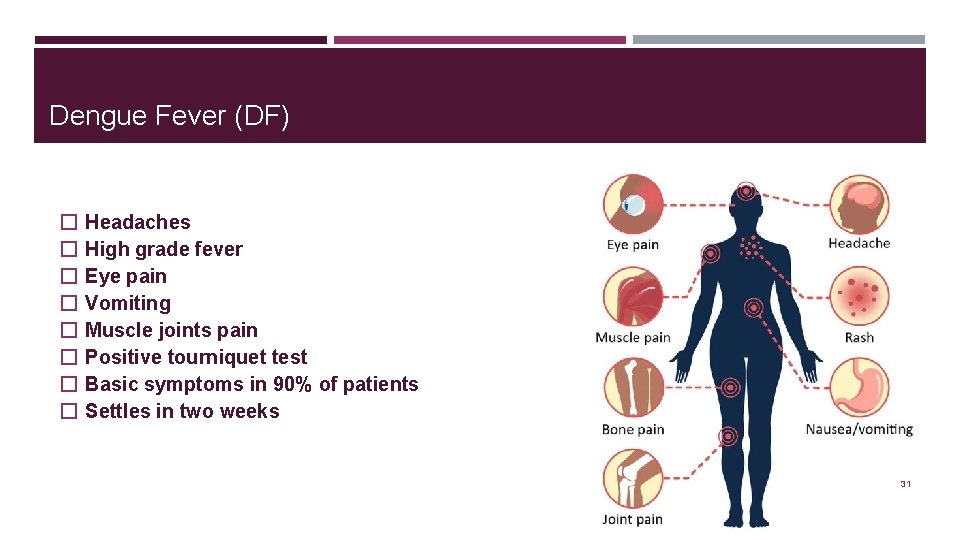
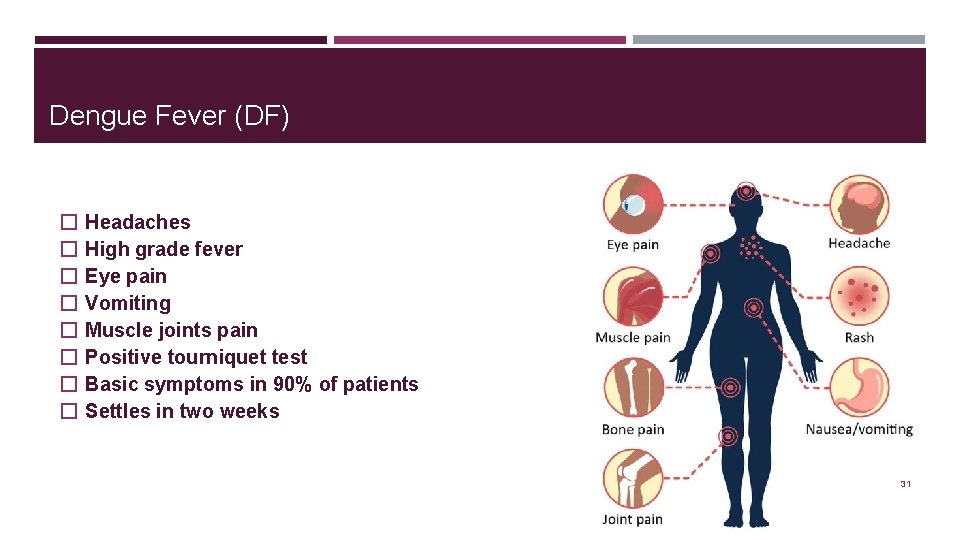
Dengue Fever (DF) � � � � Headaches High grade fever Eye pain Vomiting Muscle joints pain Positive tourniquet test Basic symptoms in 90% of patients Settles in two weeks 31

Dengue Hemorrhagic Fever (DHF) � All previous symptoms of Dengue Fever � Spontaneous bleeding � 9% of patient � Recover with hospital care 32
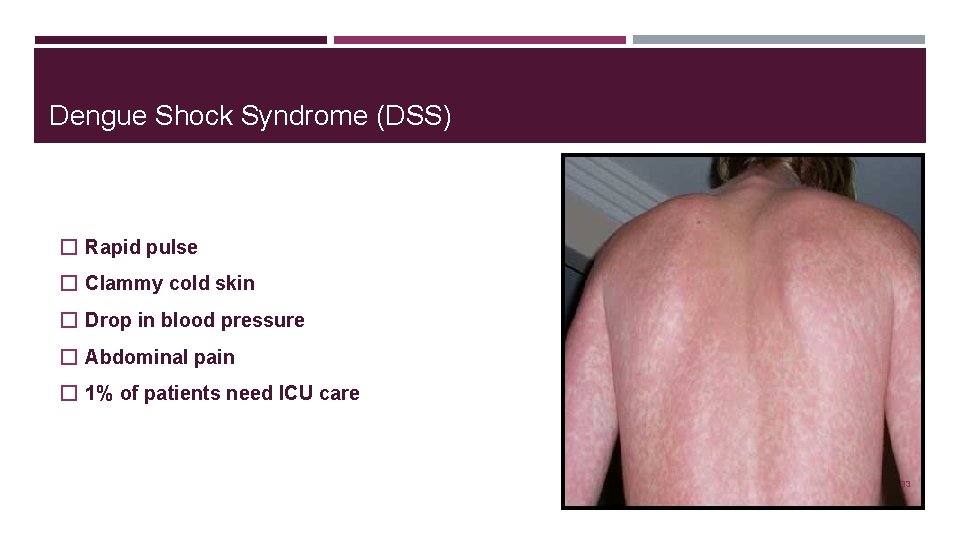
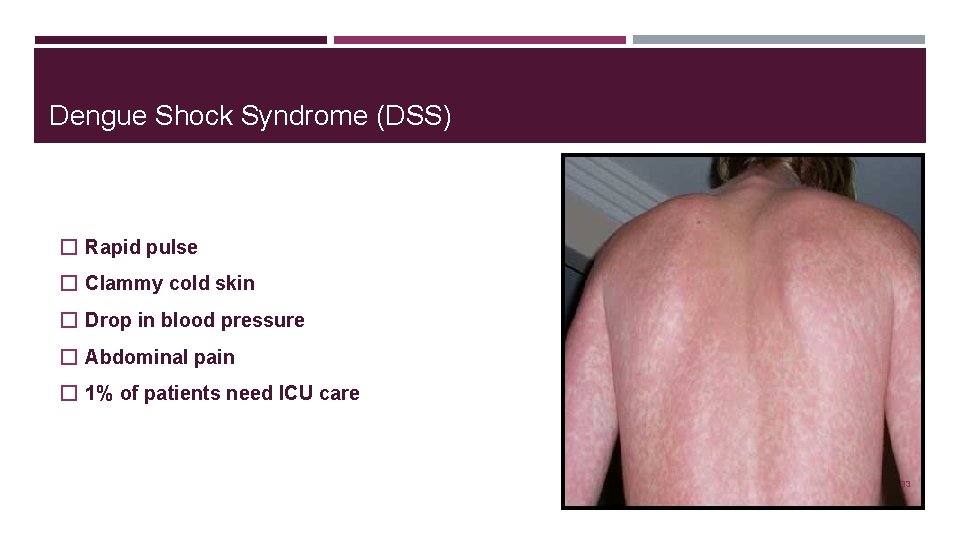
Dengue Shock Syndrome (DSS) � Rapid pulse � Clammy cold skin � Drop in blood pressure � Abdominal pain � 1% of patients need ICU care 33
Compensated Shock � Low blood volume � Body still maintains blood pressure and organ perfusion by increasing the heart rate � Blood vessels are constricted � Cold extremities, increased CRT, agitation, restlessness.
Decompensated Shock � � Compensated shock progresses to Decompensated shock Low blood volume Body unable to maintain blood pressure and organ perfusion Organ damage and failure
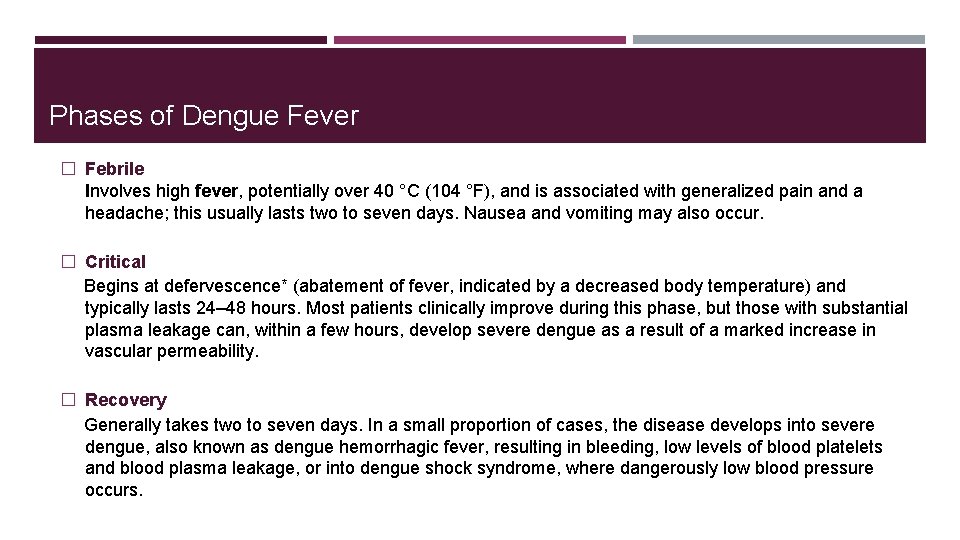
Phases of Dengue Fever � Febrile Involves high fever, potentially over 40 °C (104 °F), and is associated with generalized pain and a headache; this usually lasts two to seven days. Nausea and vomiting may also occur. � Critical Begins at defervescence* (abatement of fever, indicated by a decreased body temperature) and typically lasts 24– 48 hours. Most patients clinically improve during this phase, but those with substantial plasma leakage can, within a few hours, develop severe dengue as a result of a marked increase in vascular permeability. � Recovery Generally takes two to seven days. In a small proportion of cases, the disease develops into severe dengue, also known as dengue hemorrhagic fever, resulting in bleeding, low levels of blood platelets and blood plasma leakage, or into dengue shock syndrome, where dangerously low blood pressure occurs.

WHO Diagnostic Criteria 37
38
Lab Investigations � � � CBC PT/INR Viral anti-gene detection (NS-1) Ultrasounds for organomegaly PCR 39
Management � � � Rest Fluid intake for adequate hydration Aspirin NSAID Acetaminophen Codeine 40
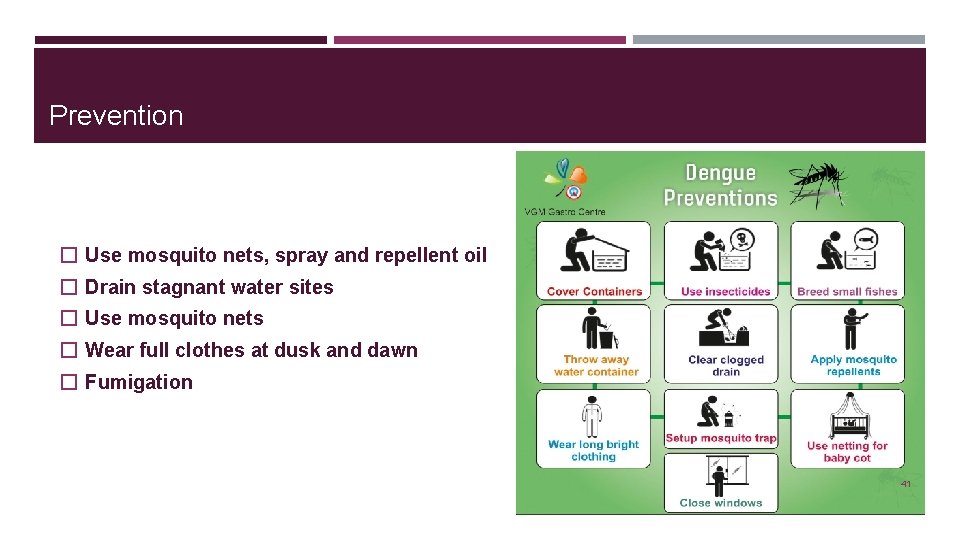
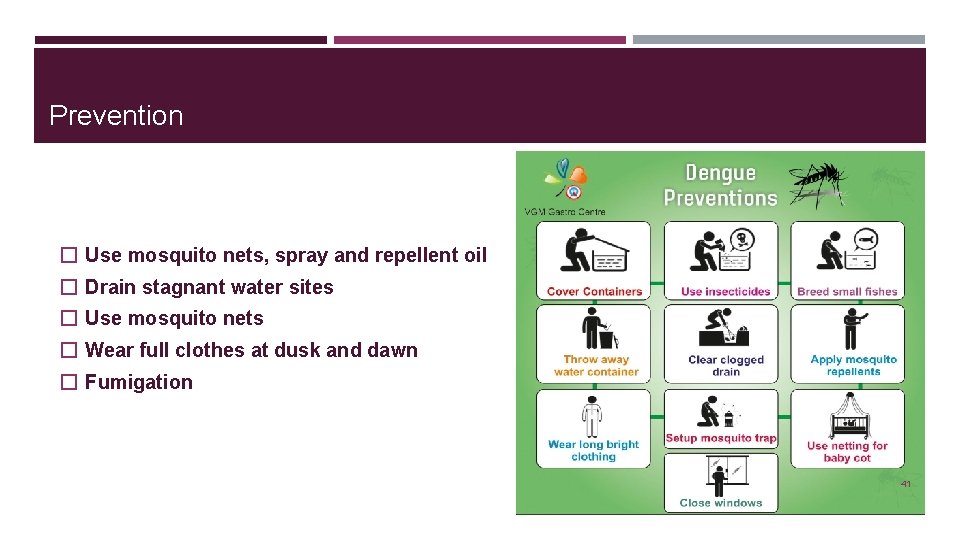
Prevention � Use mosquito nets, spray and repellent oil � Drain stagnant water sites � Use mosquito nets � Wear full clothes at dusk and dawn � Fumigation 41

42

43