Internal Medicine Clinical Pathological Conference July 18 2008
- Slides: 19
Internal Medicine Clinical Pathological Conference July 18, 2008
Diagnostic Procedure n Right thigh skeletal muscle biopsy
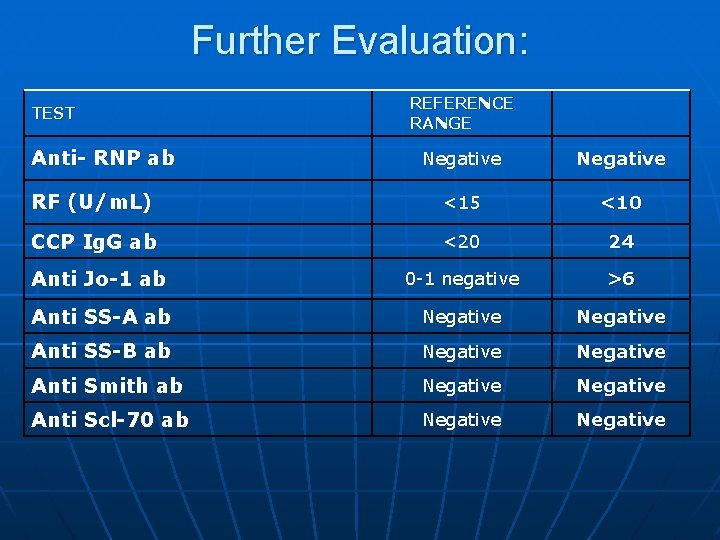
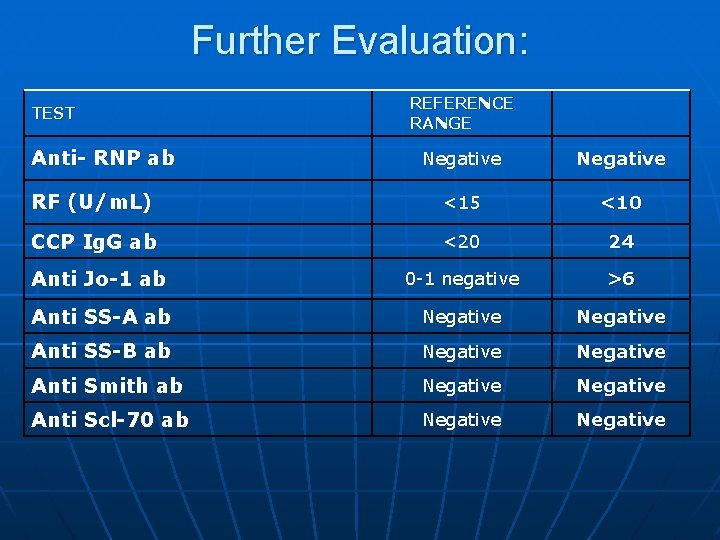
Further Evaluation: TEST Anti- RNP ab REFERENCE RANGE Negative RF (U/m. L) <15 <10 CCP Ig. G ab <20 24 Anti Jo-1 ab 0 -1 negative >6 Anti SS-A ab Negative Anti SS-B ab Negative Anti Smith ab Negative Anti Scl-70 ab Negative
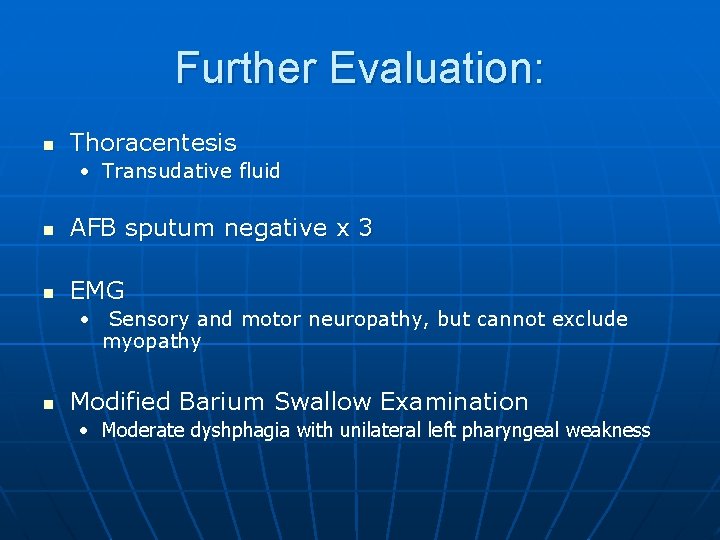
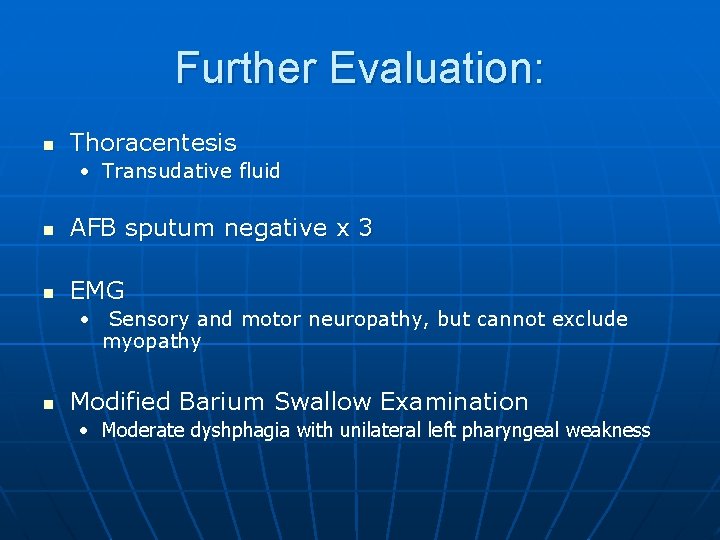
Further Evaluation: n Thoracentesis • Transudative fluid n AFB sputum negative x 3 n EMG • Sensory and motor neuropathy, but cannot exclude myopathy n Modified Barium Swallow Examination • Moderate dyshphagia with unilateral left pharyngeal weakness
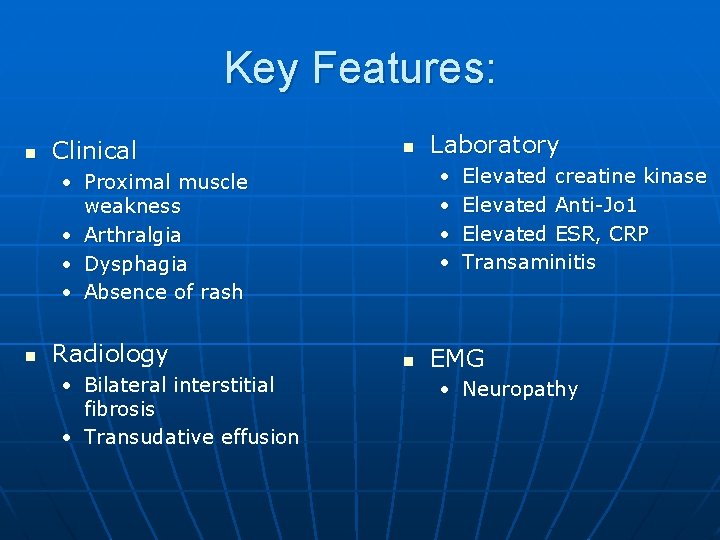
Key Features: n Clinical n • • • Proximal muscle weakness • Arthralgia • Dysphagia • Absence of rash n Radiology • Bilateral interstitial fibrosis • Transudative effusion Laboratory n Elevated creatine kinase Elevated Anti-Jo 1 Elevated ESR, CRP Transaminitis EMG • Neuropathy
Idiopathic Inflammatory Myopathy n Subclassified • Polymyositis • Dermatomyositis • Inclusion body myositis n Histological: endomysial inflammation and activation of the immune response
Idiopathic Inflammatory Myopathy n Epidemiology • Annual incidence: 2 -10 per million • Polymyositis: n Disease of adult; rare in people younger than 20 years old • Dermatomyositis: n n Two peaks: 5 -10 years old and 50 years old Female to male – 2: 1 • Inclusion body myositis n Older than 50 years of age
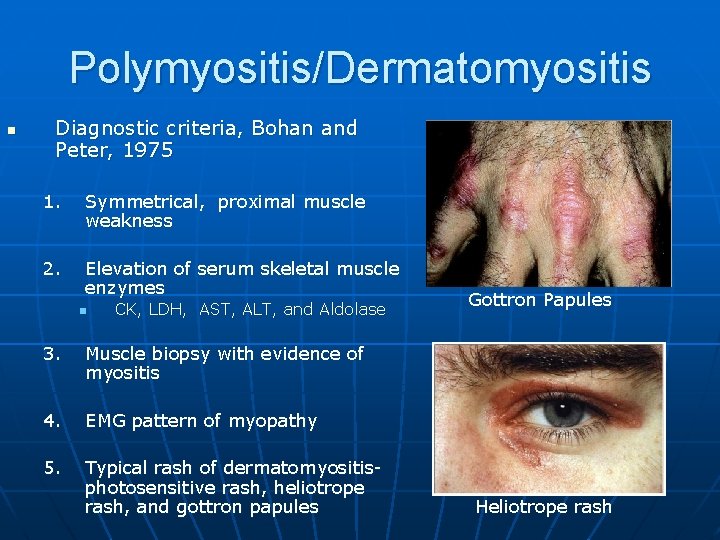
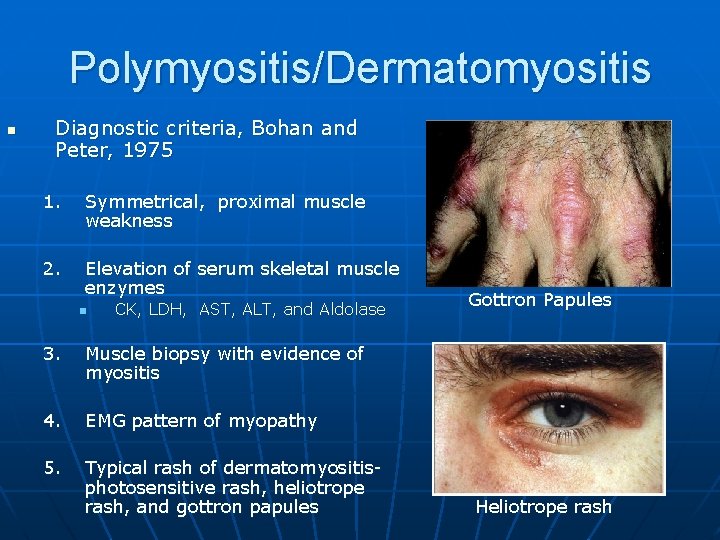
Polymyositis/Dermatomyositis n Diagnostic criteria, Bohan and Peter, 1975 1. Symmetrical, proximal muscle weakness 2. Elevation of serum skeletal muscle enzymes n CK, LDH, AST, ALT, and Aldolase 3. Muscle biopsy with evidence of myositis 4. EMG pattern of myopathy 5. Typical rash of dermatomyositisphotosensitive rash, heliotrope rash, and gottron papules Gottron Papules Heliotrope rash
Polymyositis/ Dermatomyositis n Esophageal involvement (8 -30%), inflammation of cardiac muscle n Interstitial Lung disease (50%) • Nonspecific interstitial pneumonia (NSIP) • Usual interstitial pneumonia (UIP) n Anti-Jo 1 and Anti-Mi 2 • Anti- Jo-1 commonly have Interstitial lung disease • Anti-M 1 have skin findings n Increase cancer risk • 7 -10% of polymyositis • 15 -20% of dermatomyositis
Polymyositis/ Dermatomyositis n Cellular immunity • Polymyositis- Class II HLA antigen DR 3, predominant CD 8 T cells • Dermatomyositis- Predominant B cells and CD 4 T cells in inflammatory infiltrates
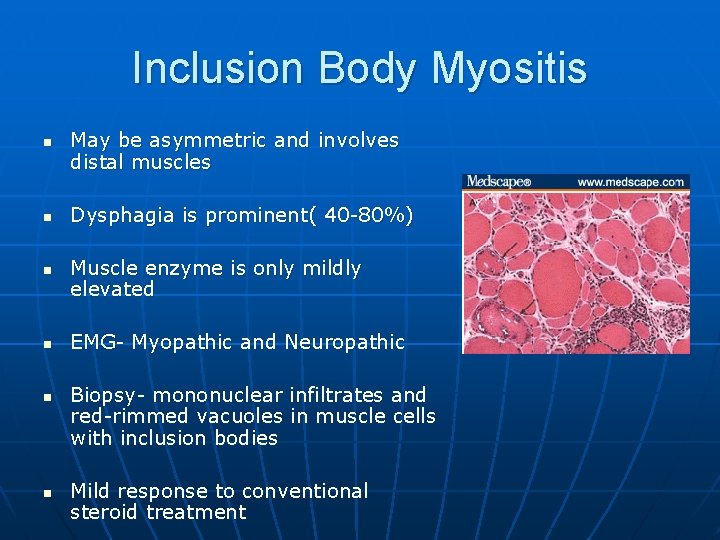
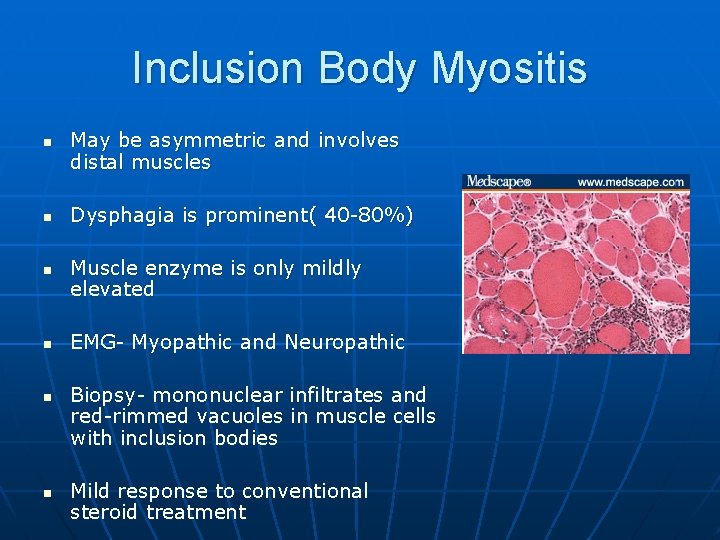
Inclusion Body Myositis n n n May be asymmetric and involves distal muscles Dysphagia is prominent( 40 -80%) Muscle enzyme is only mildly elevated EMG- Myopathic and Neuropathic Biopsy- mononuclear infiltrates and red-rimmed vacuoles in muscle cells with inclusion bodies Mild response to conventional steroid treatment
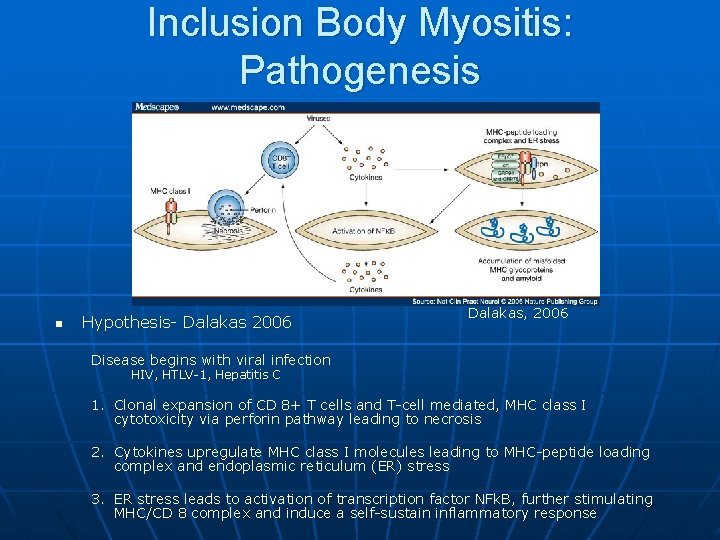
Inclusion Body Myositis: Pathogenesis n Engel and Arahata 1984 • Endomysial infiltrates are composed of primarily CD 8+ T Cells n Engela and Engel 1988; Orimo 1994; Schmidt 2004 • CD 8+ T Cells surrounds MHC class I myofibers and express perforin n Cupler 1996; Saperstien 1999; Tsuruta 2001; Dalakas 2006 • Association with chronic viral infection
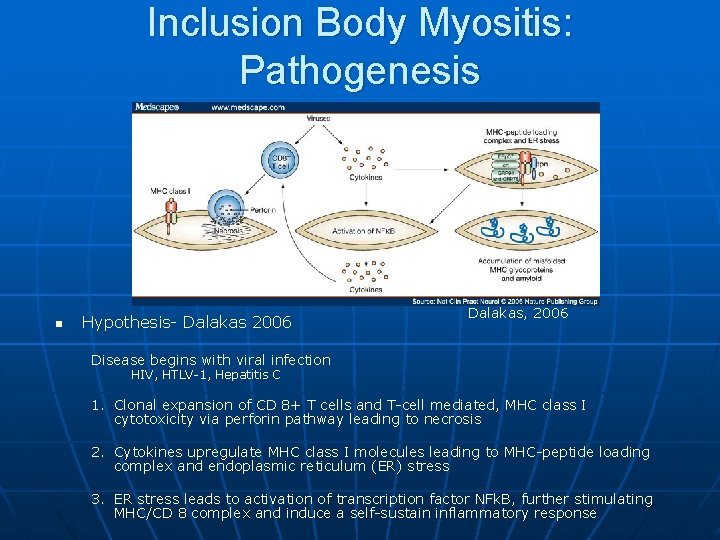
Inclusion Body Myositis: Pathogenesis n Hypothesis- Dalakas 2006 Dalakas, 2006 Disease begins with viral infection HIV, HTLV-1, Hepatitis C 1. Clonal expansion of CD 8+ T cells and T-cell mediated, MHC class I cytotoxicity via perforin pathway leading to necrosis 2. Cytokines upregulate MHC class I molecules leading to MHC-peptide loading complex and endoplasmic reticulum (ER) stress 3. ER stress leads to activation of transcription factor NFk. B, further stimulating MHC/CD 8 complex and induce a self-sustain inflammatory response
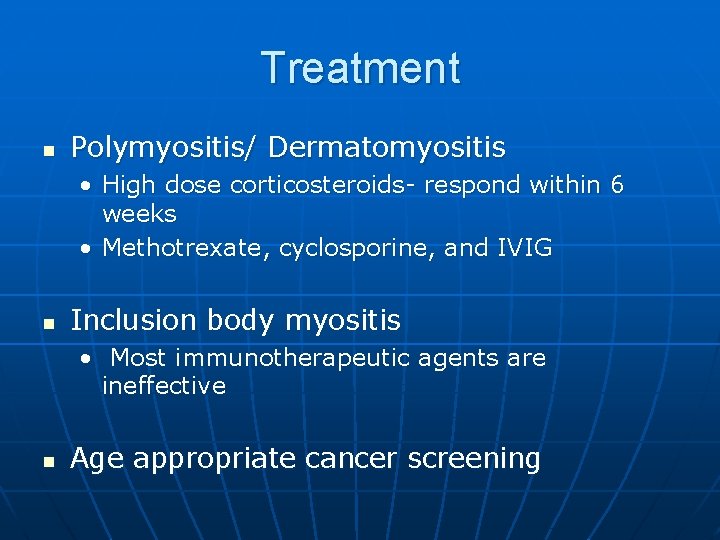
Treatment n Polymyositis/ Dermatomyositis • High dose corticosteroids- respond within 6 weeks • Methotrexate, cyclosporine, and IVIG n Inclusion body myositis • Most immunotherapeutic agents are ineffective n Age appropriate cancer screening
FINAL DIAGNOSIS: Inclusion Body Myositis Dermatomyositis sine dermatitis
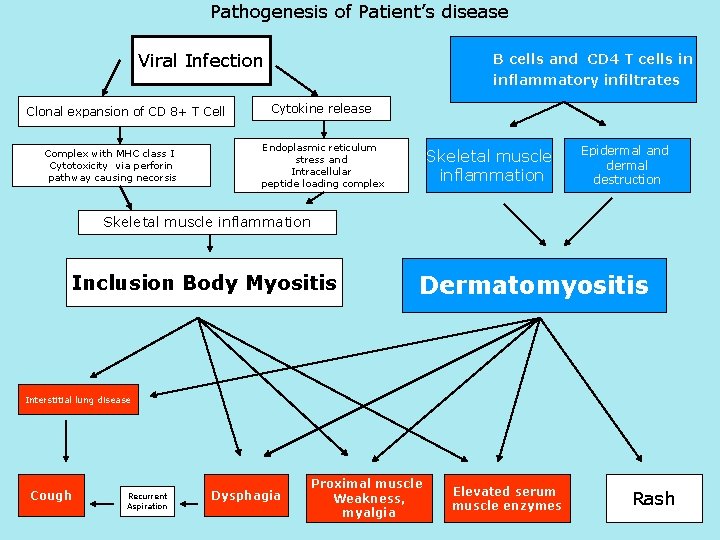
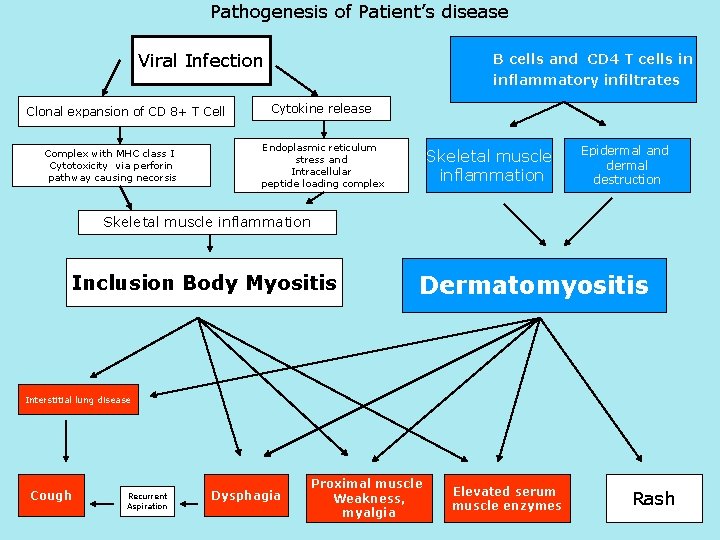
Pathogenesis of Patient’s disease Viral Infection Clonal expansion of CD 8+ T Cell Complex with MHC class I Cytotoxicity via perforin pathway causing necorsis B cells and CD 4 T cells in inflammatory infiltrates Cytokine release Endoplasmic reticulum stress and Intracellular peptide loading complex Skeletal muscle inflammation Epidermal and dermal destruction Skeletal muscle inflammation Inclusion Body Myositis Dermatomyositis Interstitial lung disease Cough Recurrent Aspiration Dysphagia Proximal muscle Weakness, myalgia Elevated serum muscle enzymes Rash
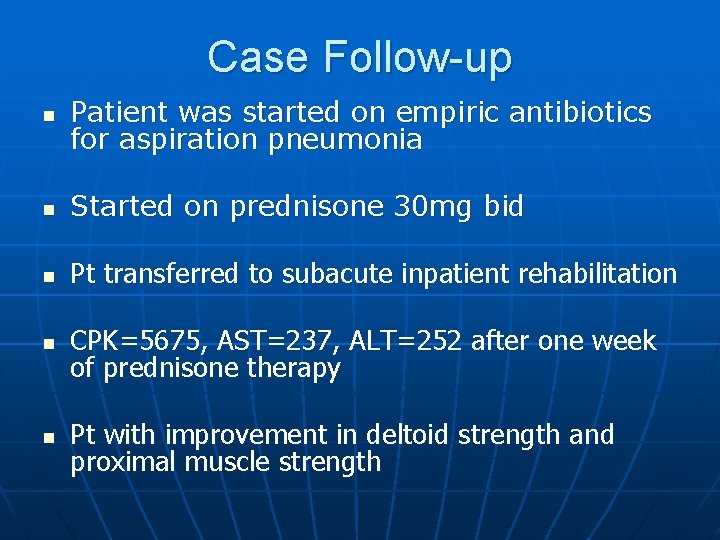
Case Follow-up n Patient was started on empiric antibiotics for aspiration pneumonia n Started on prednisone 30 mg bid n Pt transferred to subacute inpatient rehabilitation n CPK=5675, AST=237, ALT=252 after one week of prednisone therapy n Pt with improvement in deltoid strength and proximal muscle strength
Case Follow-up n n n Eventually discharged with outpatient rheumatology follow up Initially, clinical symptoms improved and patient was maintained on daily steroid for about 1 year Patient was found to have rising CK, and Azathioprine was added to his regimen Azathioprine did not improve his CK levels, and was switched to Mycophenolate mofetil Patient was electively admitted 2 weeks ago for IVIG as CK levels continue to be elevated
THANK YOU! n Medical Student Discussants Michael Goldman Juan Lado Megan Mcgill Nekee Pandya n Moderator: Martin Blaser, MD Faculty Discussant: Peter Izmirly, MD n Radiology Speaker: Dr. David Naidich , MD n Pathology Speaker: David Zagzag, MD n SPECIAL THANKS: Christina Yoon , MD, Harry n Shen, MD and Jean Park, M. D.
 2008 2008
2008 2008 Haney banks and zimbardo
Haney banks and zimbardo Physical composition of urine
Physical composition of urine Pathological jaundice workup
Pathological jaundice workup Murphy repertory rubrics
Murphy repertory rubrics Pathologic jaundice
Pathologic jaundice Introduction biomedical waste management
Introduction biomedical waste management Pathological demand avoidance test
Pathological demand avoidance test Pathological designs
Pathological designs Pathological designs
Pathological designs Inherent tone of ciliary muscle
Inherent tone of ciliary muscle Pathological analysis
Pathological analysis Pathological designs
Pathological designs Thanatology definition
Thanatology definition Pathological fractire
Pathological fractire Dutch north sea emergency medicine conference
Dutch north sea emergency medicine conference Unm internal medicine residency
Unm internal medicine residency Umass neurology residency
Umass neurology residency Total internal reflection in medicine
Total internal reflection in medicine William osler father of modern medicine
William osler father of modern medicine