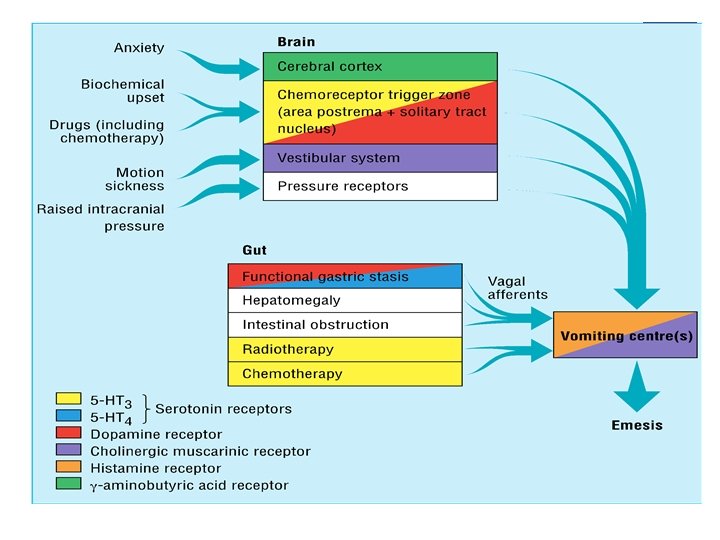
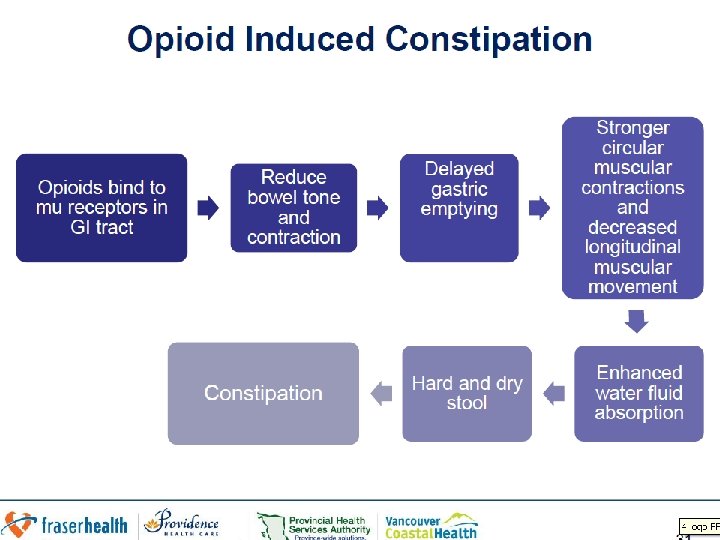
A mechanistic approach to Nausea Vomiting and Constipation


- Slides: 23
A mechanistic approach to Nausea Vomiting and Constipation in the ED Emergency/Palliative Medicine Workshop for UBC Emergency Medicine Residents Susanne Moadebi Pharm. D BCPS July 27 th, 2016 HOPE Centre
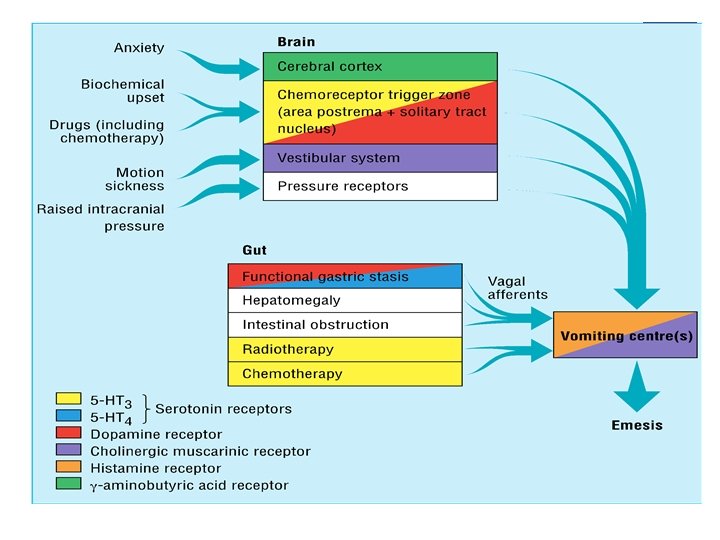
Outline n List common mechanisms which cause nausea and vomiting n Classify antiemetic agents based on major neurotransmitters and receptor targets n Review antiemetic use and new agents for treatment of constipation in the emergency department n Outline treatment principles for Malignant Bowel Obstruction n Cases 2
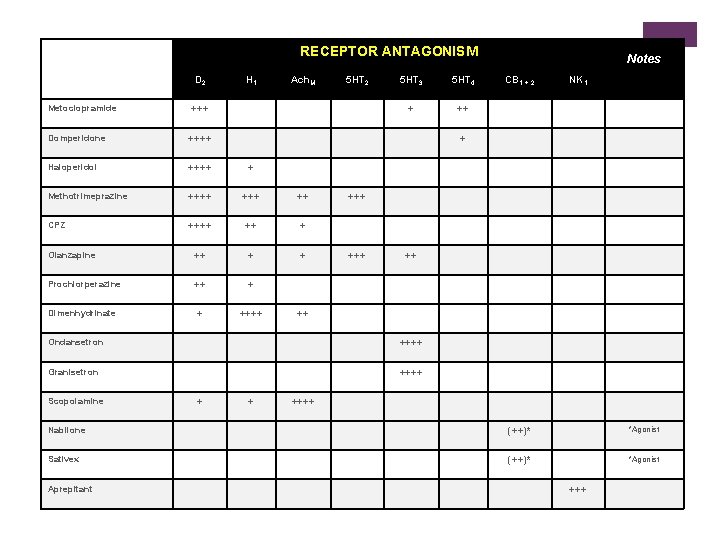
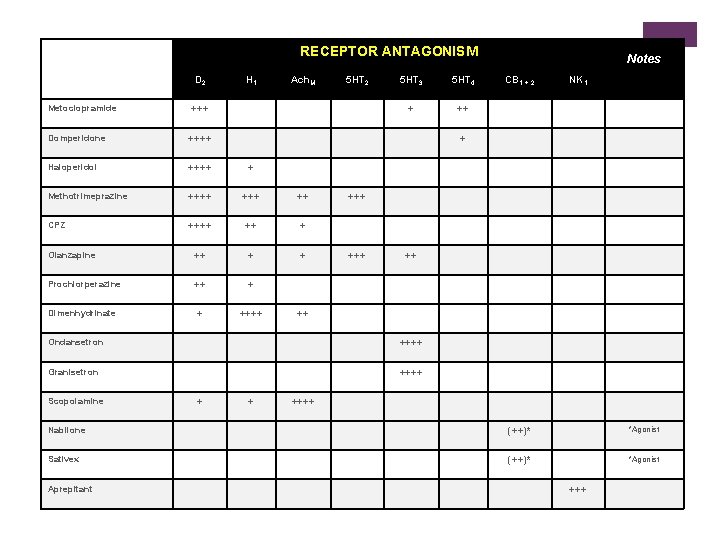
RECEPTOR ANTAGONISM D 2 Metoclopramide H 1 Ach. M +++ Domperidone ++++ Haloperidol ++++ + Methotrimeprazine ++++ ++ CPZ ++++ ++ + Olanzapine ++ + + Prochlorperazine ++ + + ++++ Dimenhydrinate 5 HT 2 5 HT 3 5 HT 4 + ++ NK 1 +++ ++++ Granisetron ++++ + CB 1 + 2 + Ondansetron Scopolamine Notes + ++++ Nabilone (++)* *Agonist Sativex (++)* *Agonist Aprepitant +++
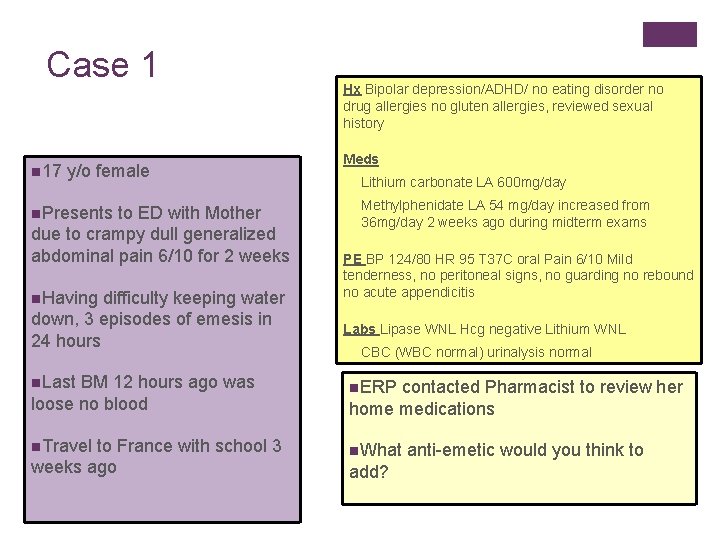
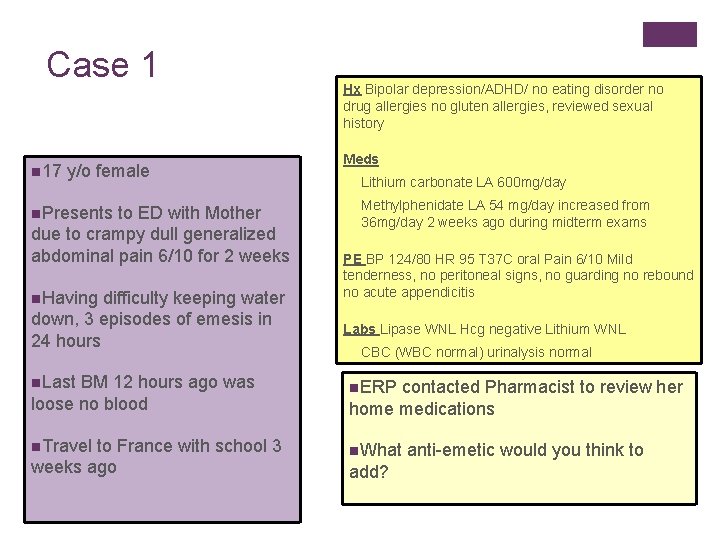
Case 1 n 17 y/o female n. Presents to ED with Mother due to crampy dull generalized abdominal pain 6/10 for 2 weeks n. Having difficulty keeping water down, 3 episodes of emesis in 24 hours n. Last BM 12 hours ago was loose no blood n. Travel to France with school 3 weeks ago Hx Bipolar depression/ADHD/ no eating disorder no drug allergies no gluten allergies, reviewed sexual history Meds Lithium carbonate LA 600 mg/day Methylphenidate LA 54 mg/day increased from 36 mg/day 2 weeks ago during midterm exams PE BP 124/80 HR 95 T 37 C oral Pain 6/10 Mild tenderness, no peritoneal signs, no guarding no rebound no acute appendicitis Labs Lipase WNL Hcg negative Lithium WNL CBC (WBC normal) urinalysis normal n. ERP contacted Pharmacist to review her home medications n. What anti-emetic would you think to add?
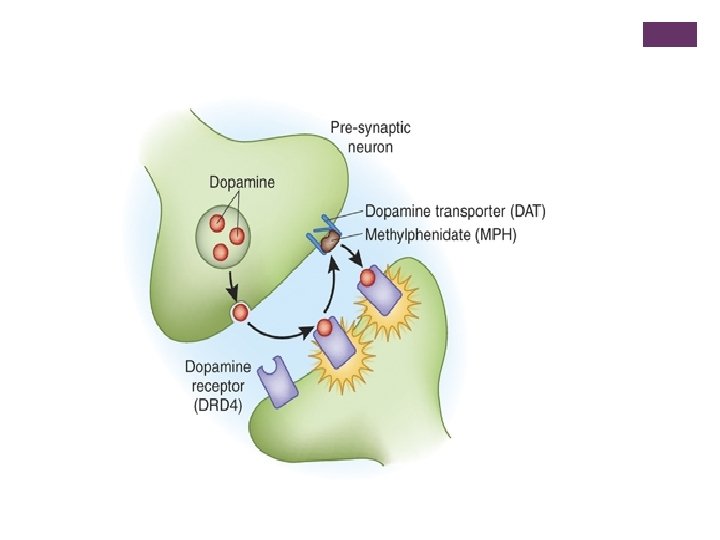
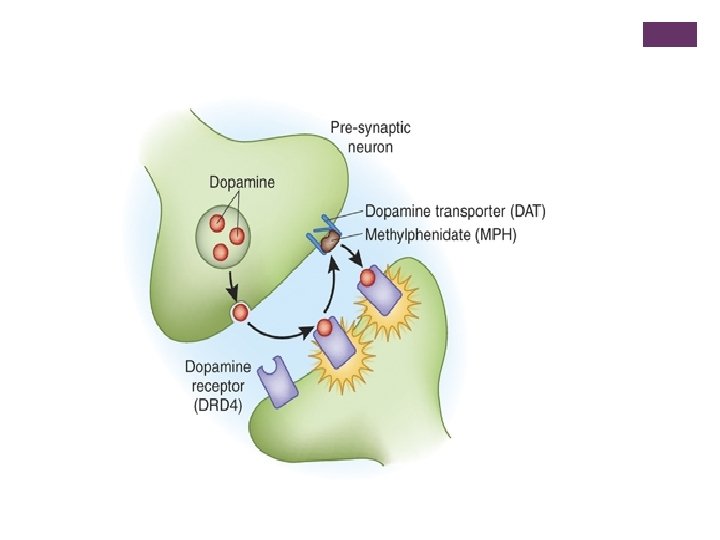
Case 1 continued n methylphenidate acts as a dopamine and norepinephrine reuptake inhibitor resulting in a prolongation of dopamine (D 1/D 2) receptor effects. It is believed that methylphenidate activates the brain stem arousal system and cortex. n The most common side effects associated with methylphenidate include headache, nausea, vomiting, anorexia, dizziness, and insomnia.
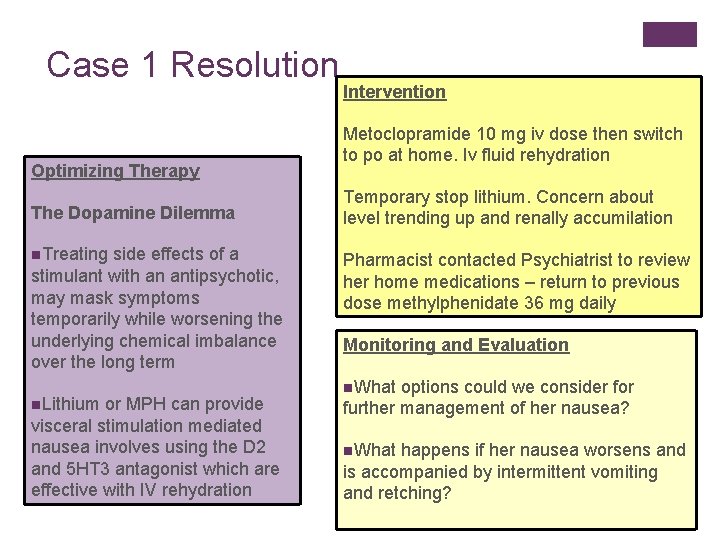
Case 1 Resolution Optimizing Therapy The Dopamine Dilemma n. Treating side effects of a stimulant with an antipsychotic, may mask symptoms temporarily while worsening the underlying chemical imbalance over the long term n. Lithium or MPH can provide visceral stimulation mediated nausea involves using the D 2 and 5 HT 3 antagonist which are effective with IV rehydration Intervention Metoclopramide 10 mg iv dose then switch to po at home. Iv fluid rehydration Temporary stop lithium. Concern about level trending up and renally accumilation Pharmacist contacted Psychiatrist to review her home medications – return to previous dose methylphenidate 36 mg daily Monitoring and Evaluation n. What options could we consider for further management of her nausea? n. What happens if her nausea worsens and is accompanied by intermittent vomiting and retching?
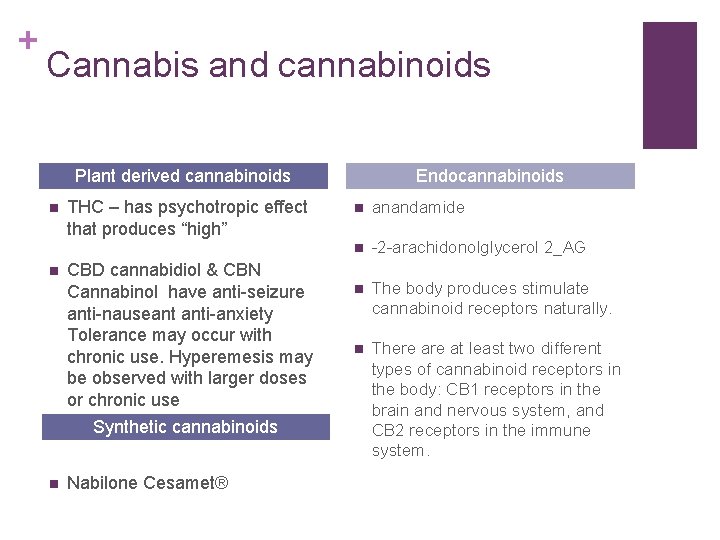
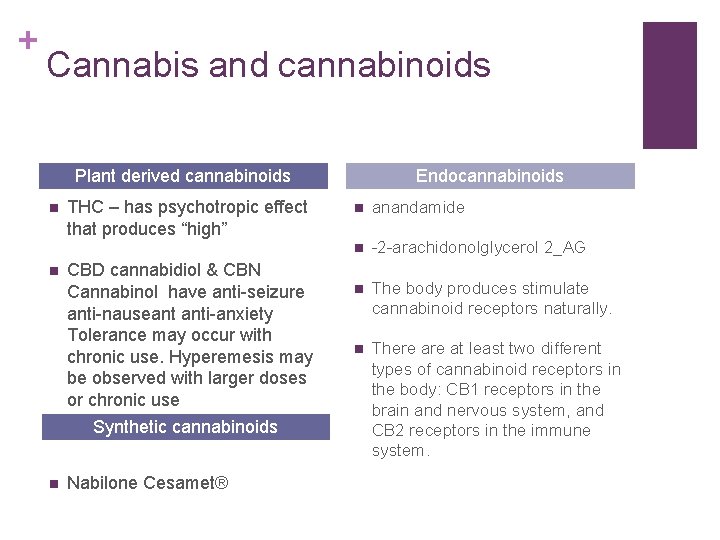
+ Cannabis and cannabinoids Plant derived cannabinoids n n THC – has psychotropic effect that produces “high” CBD cannabidiol & CBN Cannabinol have anti-seizure anti-nauseant anti-anxiety Tolerance may occur with chronic use. Hyperemesis may be observed with larger doses or chronic use Synthetic cannabinoids n Nabilone Cesamet® Endocannabinoids n anandamide n -2 -arachidonolglycerol 2_AG n The body produces stimulate cannabinoid receptors naturally. n There at least two different types of cannabinoid receptors in the body: CB 1 receptors in the brain and nervous system, and CB 2 receptors in the immune system.


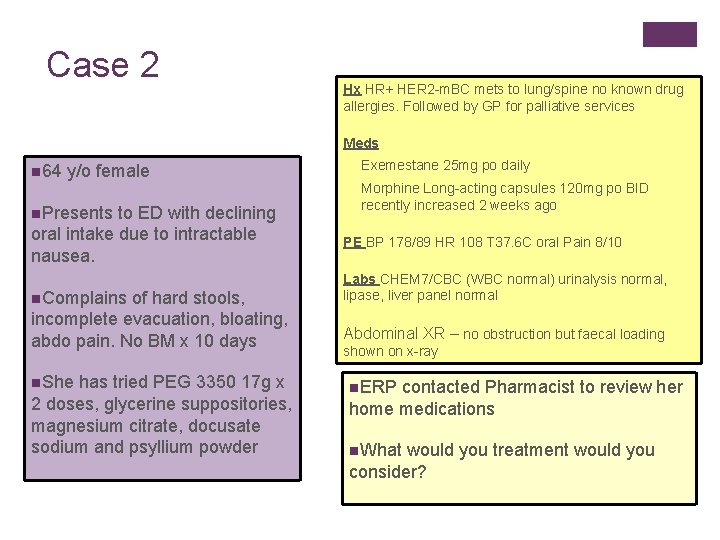
Case 2 Hx HR+ HER 2 -m. BC mets to lung/spine no known drug allergies. Followed by GP for palliative services Meds n 64 y/o female n. Presents to ED with declining oral intake due to intractable nausea. n. Complains of hard stools, incomplete evacuation, bloating, abdo pain. No BM x 10 days n. She has tried PEG 3350 17 g x 2 doses, glycerine suppositories, magnesium citrate, docusate sodium and psyllium powder Exemestane 25 mg po daily Morphine Long-acting capsules 120 mg po BID recently increased 2 weeks ago PE BP 178/89 HR 108 T 37. 6 C oral Pain 8/10 Labs CHEM 7/CBC (WBC normal) urinalysis normal, lipase, liver panel normal Abdominal XR – no obstruction but faecal loading shown on x-ray n. ERP contacted Pharmacist to review her home medications n. What would you treatment would you consider?
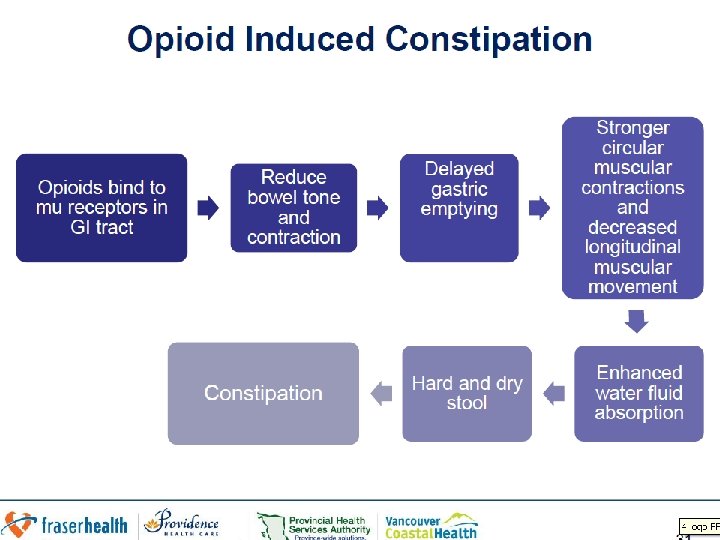
Case 2 Resolution Opioid induced constipation – how would you treat? n Intervention – use a peripherally acting mu-opioid receptor antagonist- 62 kg give Methylnaltrexone 8 mg sc n T 1/2 8 hours and T peak 30 minutes with no withdrawal of analagesia n Time to first laxation is 4 hours & will see appetite improve n Monitoring Watch for dizziness, abdo pain cramping start regular PEG and sennosides n PEG is more effective than lactulose for prevention
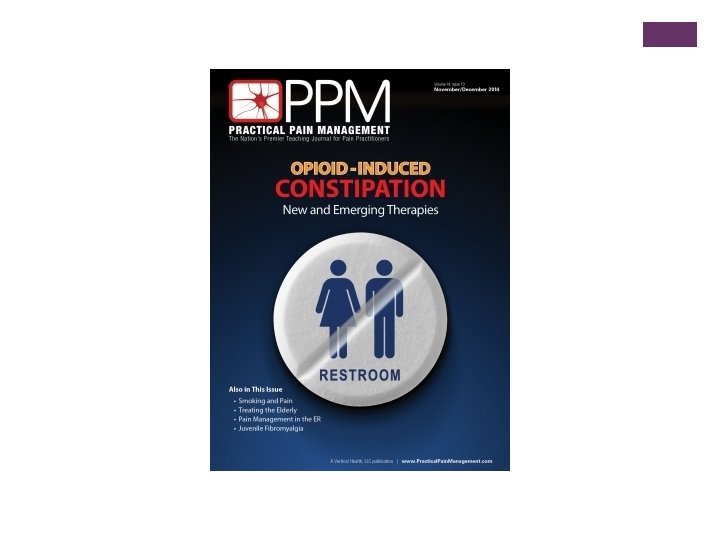
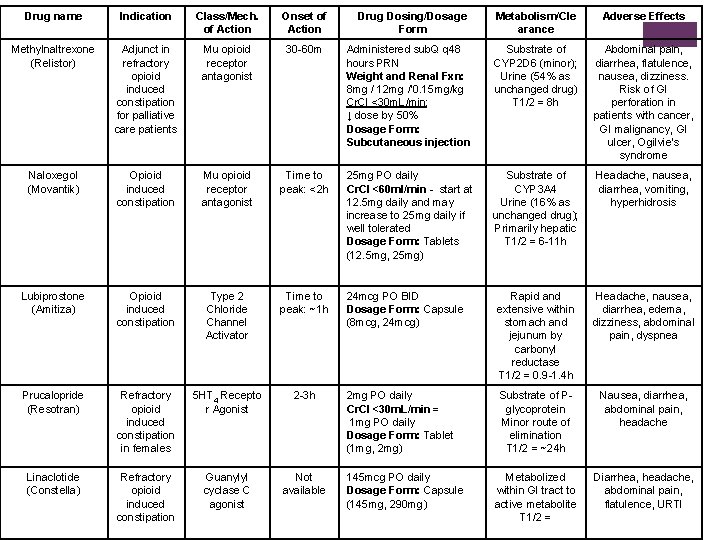
Drug name Indication Class/Mech. of Action Onset of Action Methylnaltrexone (Relistor) Adjunct in refractory opioid induced constipation for palliative care patients Mu opioid receptor antagonist 30 -60 m Naloxegol (Movantik) Opioid induced constipation Mu opioid receptor antagonist Lubiprostone (Amitiza) Opioid induced constipation Prucalopride (Resotran) Linaclotide (Constella) Drug Dosing/Dosage Form Metabolism/Cle arance Adverse Effects Administered sub. Q q 48 hours PRN Weight and Renal Fxn: 8 mg / 12 mg /‘ 0. 15 mg/kg Cr. Cl <30 m. L/min: ↓ dose by 50% Dosage Form: Subcutaneous injection Substrate of CYP 2 D 6 (minor); Urine (54% as unchanged drug) T 1/2 = 8 h Abdominal pain, diarrhea, flatulence, nausea, dizziness. Risk of GI perforation in patients with cancer, GI malignancy, GI ulcer, Ogilvie’s syndrome Time to peak: <2 h 25 mg PO daily Cr. Cl <60 ml/min - start at 12. 5 mg daily and may increase to 25 mg daily if well tolerated Dosage Form: Tablets (12. 5 mg, 25 mg) Substrate of CYP 3 A 4 Urine (16% as unchanged drug); Primarily hepatic T 1/2 = 6 -11 h Headache, nausea, diarrhea, vomiting, hyperhidrosis Type 2 Chloride Channel Activator Time to peak: ~1 h 24 mcg PO BID Dosage Form: Capsule (8 mcg, 24 mcg) Rapid and extensive within stomach and jejunum by carbonyl reductase T 1/2 = 0. 9 -1. 4 h Headache, nausea, diarrhea, edema, dizziness, abdominal pain, dyspnea Refractory opioid induced constipation in females 5 HT 4 Recepto r Agonist 2 -3 h 2 mg PO daily Cr. Cl <30 m. L/min = 1 mg PO daily Dosage Form: Tablet (1 mg, 2 mg) Substrate of Pglycoprotein Minor route of elimination T 1/2 = ~24 h Nausea, diarrhea, abdominal pain, headache Refractory opioid induced constipation Guanylyl cyclase C agonist Not available Metabolized within GI tract to active metabolite T 1/2 = Diarrhea, headache, abdominal pain, flatulence, URTI 145 mcg PO daily Dosage Form: Capsule (145 mg, 290 mg)
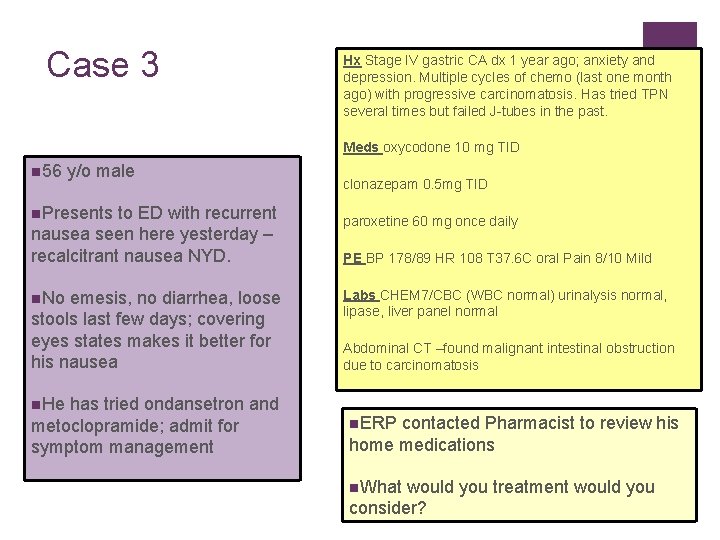
Case 3 Hx Stage IV gastric CA dx 1 year ago; anxiety and depression. Multiple cycles of chemo (last one month ago) with progressive carcinomatosis. Has tried TPN several times but failed J-tubes in the past. Meds oxycodone 10 mg TID n 56 y/o male n. Presents to ED with recurrent nausea seen here yesterday – recalcitrant nausea NYD. n. No emesis, no diarrhea, loose stools last few days; covering eyes states makes it better for his nausea n. He has tried ondansetron and metoclopramide; admit for symptom management clonazepam 0. 5 mg TID paroxetine 60 mg once daily PE BP 178/89 HR 108 T 37. 6 C oral Pain 8/10 Mild Labs CHEM 7/CBC (WBC normal) urinalysis normal, lipase, liver panel normal Abdominal CT –found malignant intestinal obstruction due to carcinomatosis n. ERP contacted Pharmacist to review his home medications n. What would you treatment would you consider?
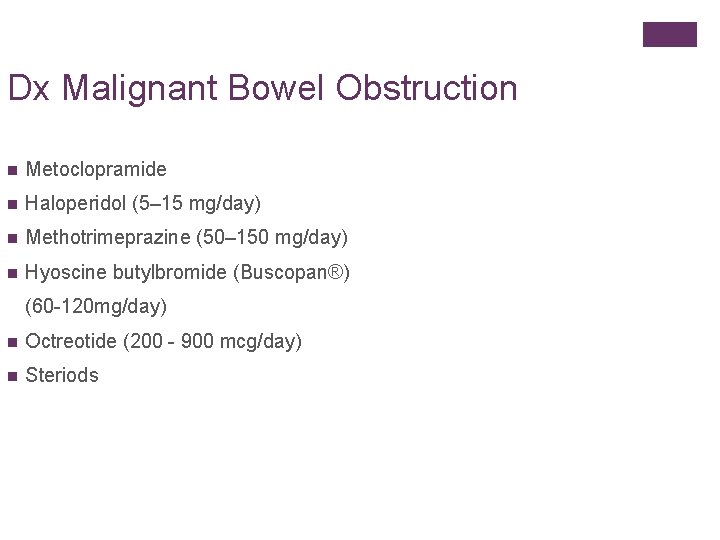
Dx Malignant Bowel Obstruction n Metoclopramide n Haloperidol (5– 15 mg/day) n Methotrimeprazine (50– 150 mg/day) n Hyoscine butylbromide (Buscopan®) (60 -120 mg/day) n Octreotide (200 - 900 mcg/day) n Steriods
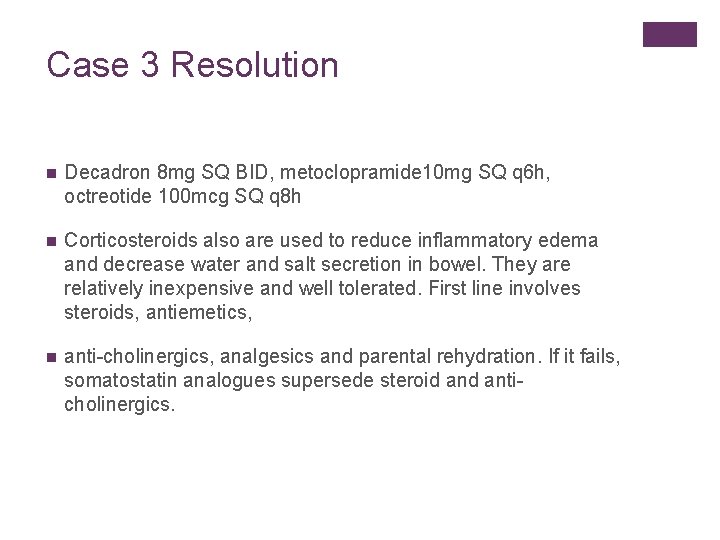
Case 3 Resolution n Decadron 8 mg SQ BID, metoclopramide 10 mg SQ q 6 h, octreotide 100 mcg SQ q 8 h n Corticosteroids also are used to reduce inflammatory edema and decrease water and salt secretion in bowel. They are relatively inexpensive and well tolerated. First line involves steroids, antiemetics, n anti-cholinergics, analgesics and parental rehydration. If it fails, somatostatin analogues supersede steroid anticholinergics.
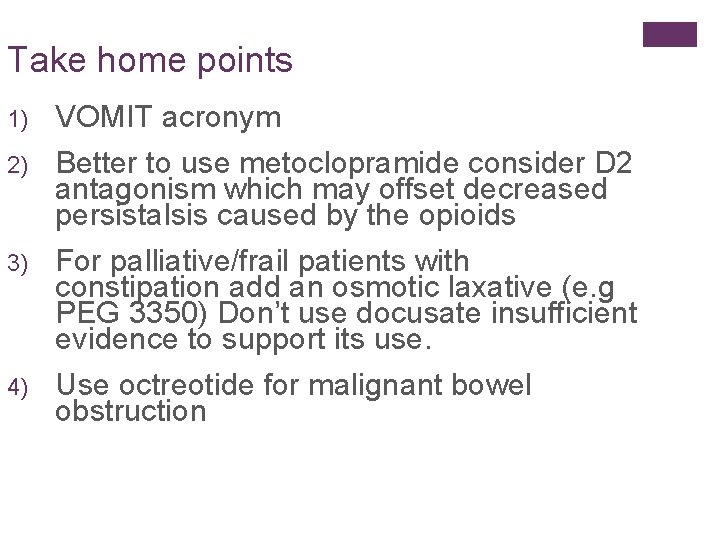
Take home points 1) 2) 3) 4) VOMIT acronym Better to use metoclopramide consider D 2 antagonism which may offset decreased persistalsis caused by the opioids For palliative/frail patients with constipation add an osmotic laxative (e. g PEG 3350) Don’t use docusate insufficient evidence to support its use. Use octreotide for malignant bowel obstruction
Questions?