Chapter 40 Oxygenation Factors Affecting Oxygenation Physiological factors




- Slides: 45
Chapter 40 Oxygenation
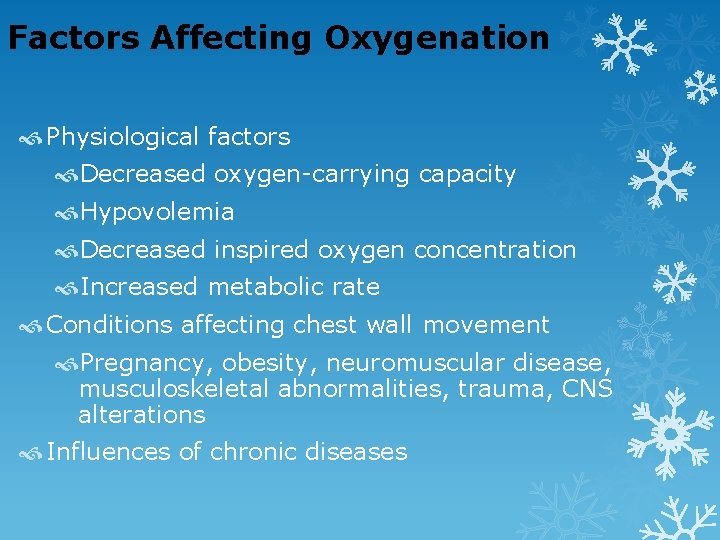
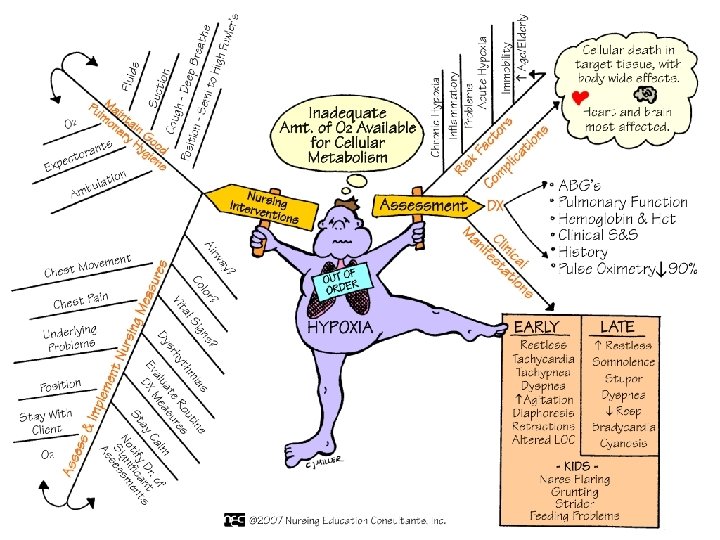
Factors Affecting Oxygenation Physiological factors Decreased oxygen-carrying capacity Hypovolemia Decreased inspired oxygen concentration Increased metabolic rate Conditions affecting chest wall movement Pregnancy, obesity, neuromuscular disease, musculoskeletal abnormalities, trauma, CNS alterations Influences of chronic diseases
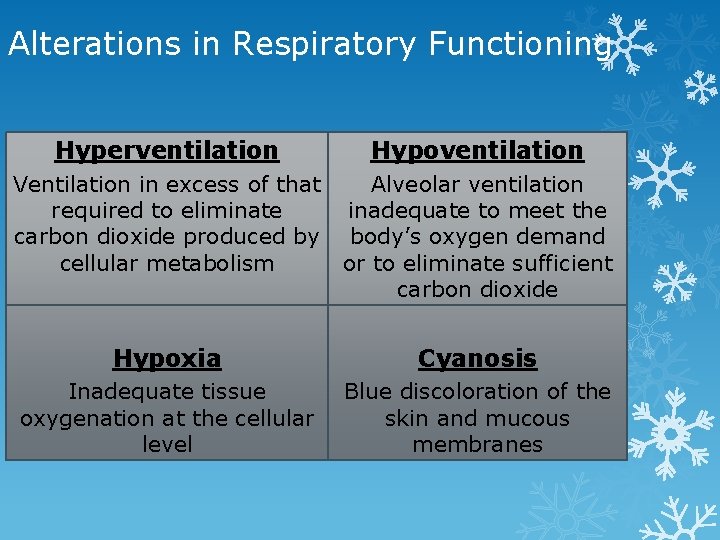
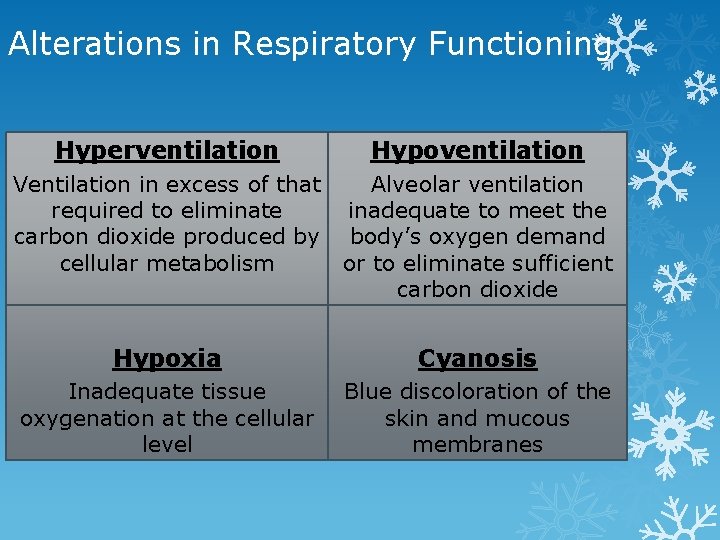
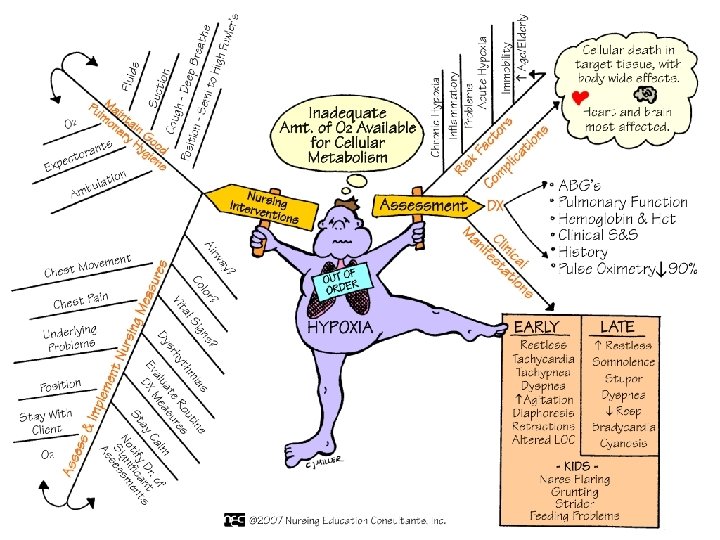
Alterations in Respiratory Functioning Hyperventilation Hypoventilation Ventilation in excess of that required to eliminate carbon dioxide produced by cellular metabolism Alveolar ventilation inadequate to meet the body’s oxygen demand or to eliminate sufficient carbon dioxide Hypoxia Cyanosis Inadequate tissue oxygenation at the cellular level Blue discoloration of the skin and mucous membranes
Nursing Knowledge Base Factors influencing oxygenation: Physiological Developmental Lifestyle Environmental

Developmental Factors Infants and toddlers School-aged children and adolescents Young and middle-aged adults Older adults

6
Changes Occurring with Aging Decreased elasticity of thorax and respiratory muscles Decrease in total body water, drier mucous membranes Loss of elastic recoil during exhalation Thickening of alveolar membrane; less efficient gas exchange Less respiratory reserve Slide 7 Copyright © 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Lifestyle Risk Factors Smoking Associated with heart disease, COPD, and lung cancer The risk of lung cancer is 10 times greater for a person who smokes than for a nonsmoker. Substance abuse Excessive use of alcohol and other drugs impairs tissue oxygenation. Stress A continuous state of stress or severe anxiety increases the metabolic rate and oxygen demand of the body.
Environmental Factors The incidence of pulmonary disease is higher in smoggy, urban areas than in rural areas. A patient’s workplace sometimes increases the risk for pulmonary disease. Coccidioidomycosis Asbestosis
10
Signs of Hypoxemia Restlessness, irritability, confusion Difficulty in breathing (dyspnea) Rapid breathing (tachypnea, stridor) Abnormal lung sounds Cyanosis, retractions, dysrhythmias Acid-base imbalance Decreased oxygen saturation Slide 11 Copyright © 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
Clearing Airway Secretions: The Effective Cough Most effective in the sitting position Two deep breaths and then inhale deeply again Breath rapidly and forcibly exhaled as quickly as possible with the mouth open This moves secretions up the bronchial tree Repeated forceful exhalation bring secretions up to where they can be more easily coughed up Slide 12 Copyright © 2014 by Elsevier Inc. All rights reserved.
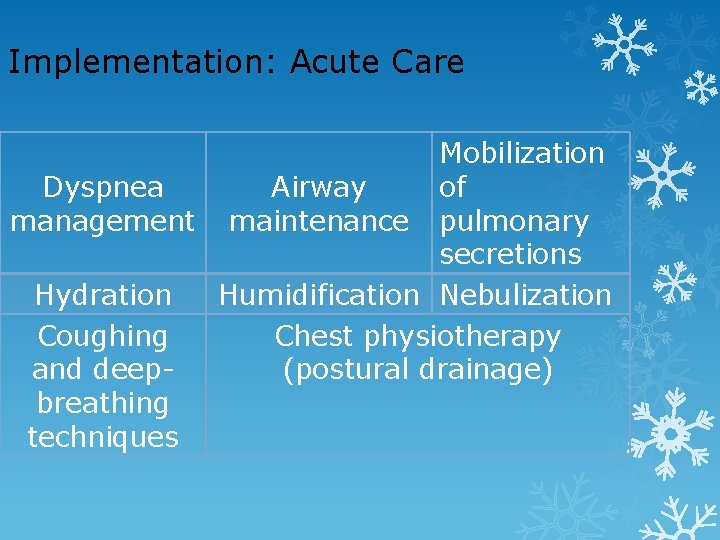
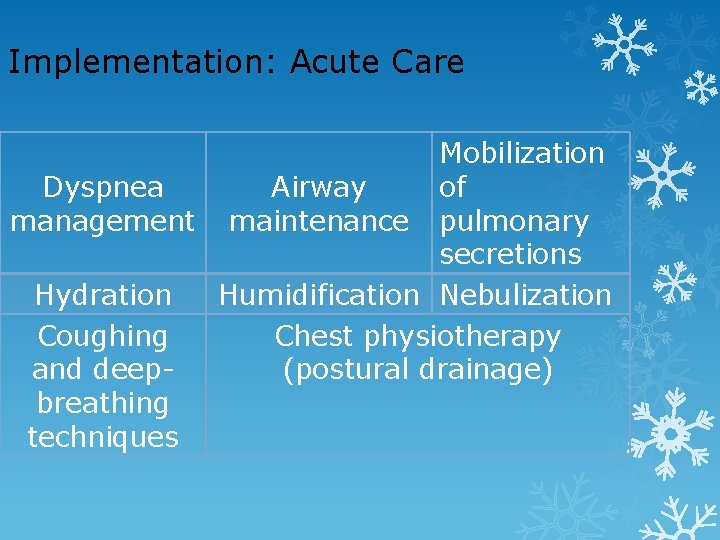
Implementation: Acute Care Mobilization Dyspnea Airway of management maintenance pulmonary secretions Hydration Humidification Nebulization Coughing Chest physiotherapy and deep(postural drainage) breathing techniques
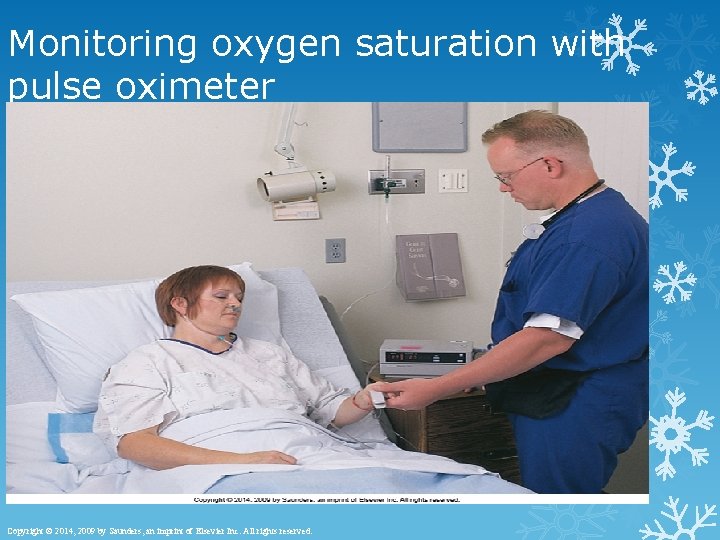
Pulse Oximetry Pulse oximeter Used to monitor any patient at risk for hypoxia Measures changes in serum oxygen continuously Sensor attached to fingers, toes, ears, or skin Helps track changes in oxygen therapy Slide 14 Copyright © 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
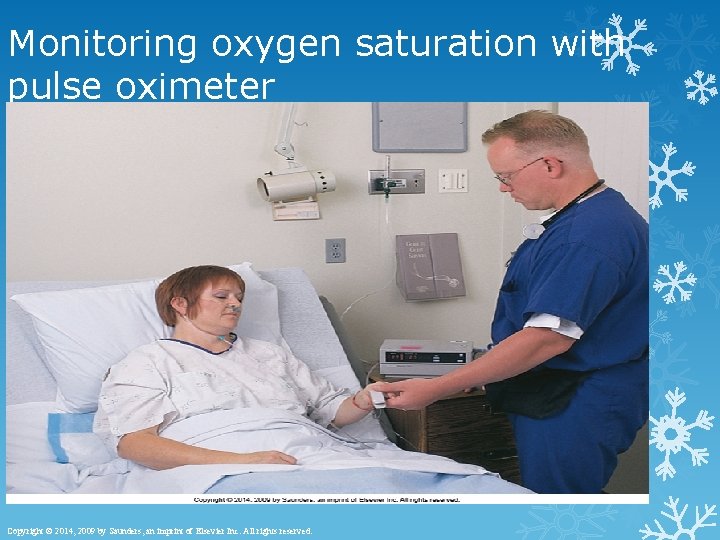
Monitoring oxygen saturation with pulse oximeter Slide 15 Copyright © 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.

Percussion
Implementation: Suctioning Techniques Oropharyngeal and nasopharyngeal Used when the patient can cough effectively but is not able to clear secretions Orotracheal and nasotracheal Used when the patient is unable to manage secretions Tracheal Used with an artificial airway
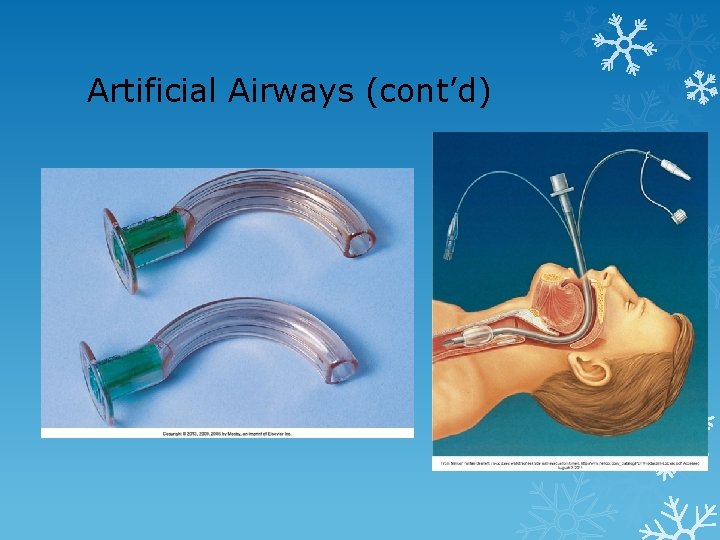
Artificial Airways Oral airway Prevents obstruction of the trachea by displacement of the tongue into the oropharynx Endotracheal and tracheal airways Short-term use to ventilate, relieve upper airway obstruction, protect against aspiration, clear secretions Tracheostomy Long-term assistance, surgical incision made into trachea
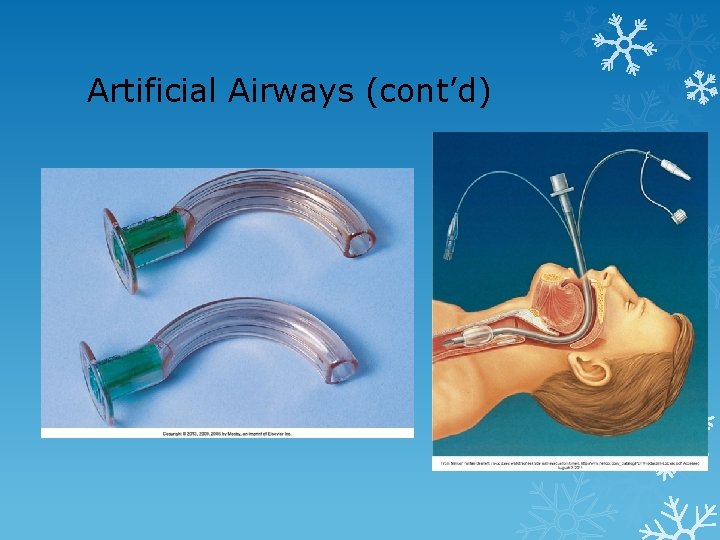
Artificial Airways (cont’d)

Types of airways Endotracheal Tube Nasopharyngeal Oropharyngeal Slide 20 Copyright © 2014, 2009 by Saunders, an imprint of Elsevier Inc. All rights reserved.
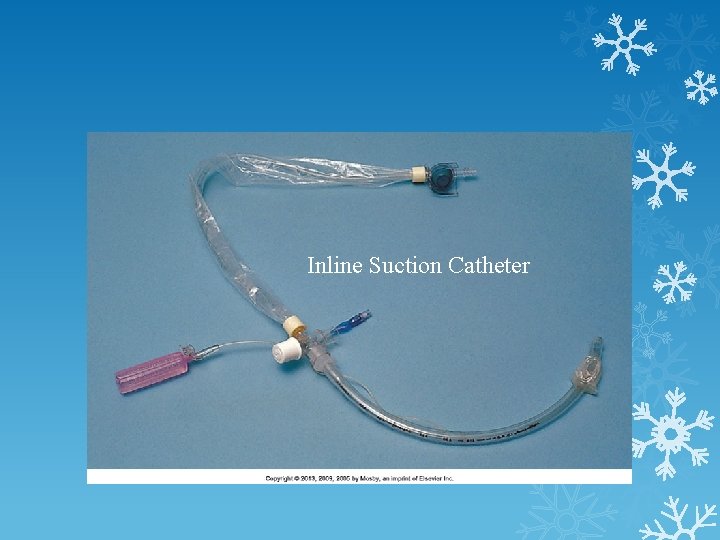
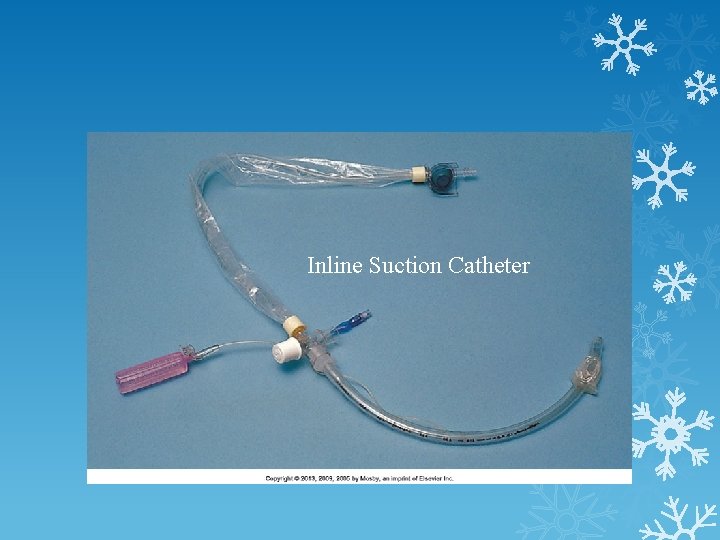
Inline Suction Catheter
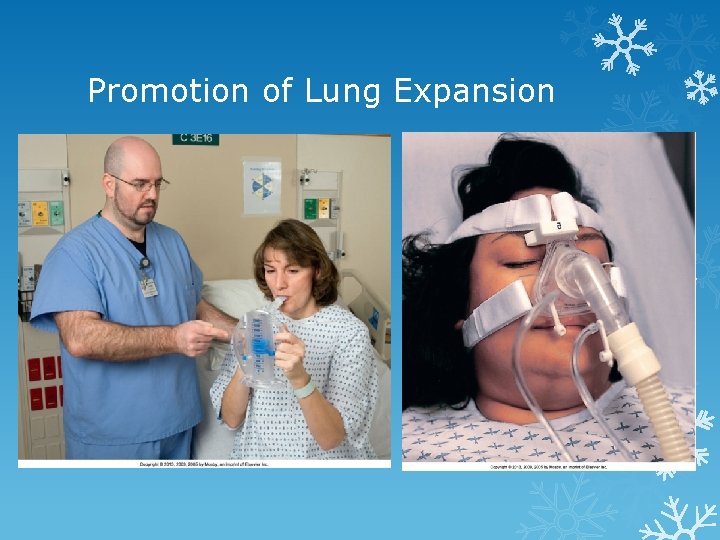
Maintenance and Promotion of Lung Expansion Ambulation Positioning Reduces pulmonary stasis, maintains ventilation and oxygenation Incentive spirometry Encourages voluntary deep breathing Noninvasive ventilation Maintains positive airway pressure and improves alveolar ventilation
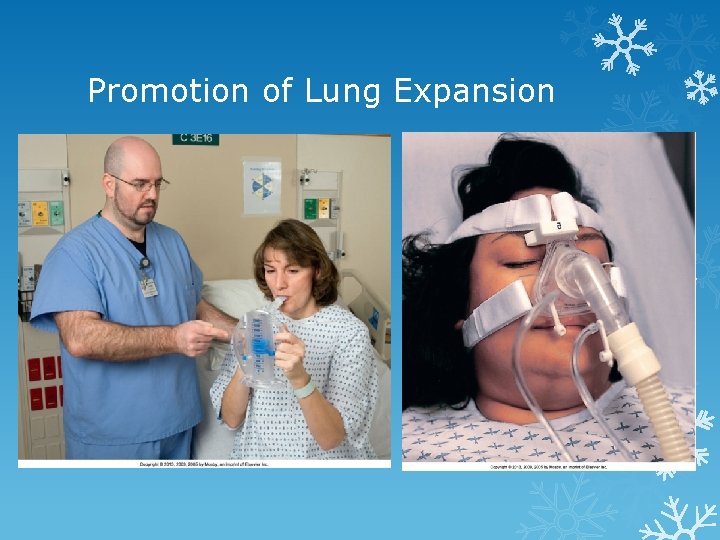
Promotion of Lung Expansion
Quick Quiz! 2. A patient with a tracheostomy has thick tenacious secretions. To maintain the airway, the most appropriate action for the nurse includes A. Tracheal suctioning. B. Oropharyngeal suctioning. C. Nasotracheal suctioning. D. Orotracheal suctioning.
Maintenance and Promotion of Lung Expansion Chest tube A catheter placed through the thorax to remove air and fluids from the pleural space, to prevent air from re-entering, or to reestablish intrapleural and intrapulmonic pressures Pneumothorax Hemothorax Special considerations
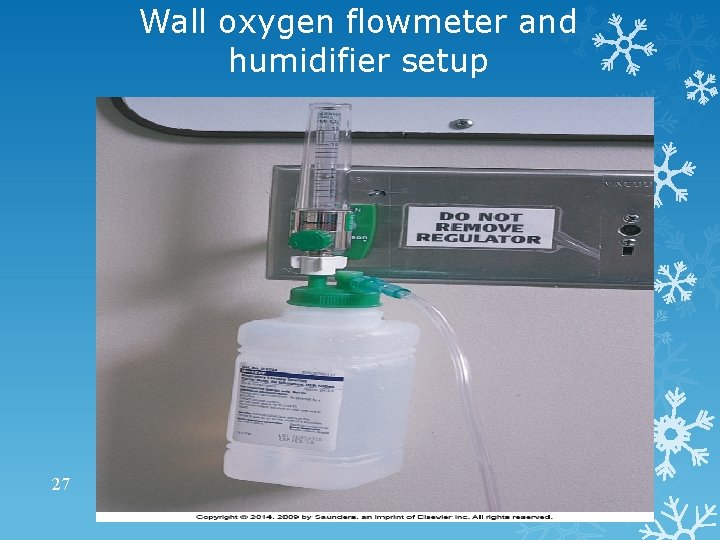
Oxygen Administration Oxygen: colorless, tasteless, odorless gas present in the air Although essential for life, use of oxygen is not without its disadvantages High concentrations cause fires to burn very rapidly Very drying to the tissues of the respiratory tract Equipment needed for oxygen therapy Oxygen source, the flowmeter, the humidifier, the tubing, and the appropriate appliance for the method ordered 26
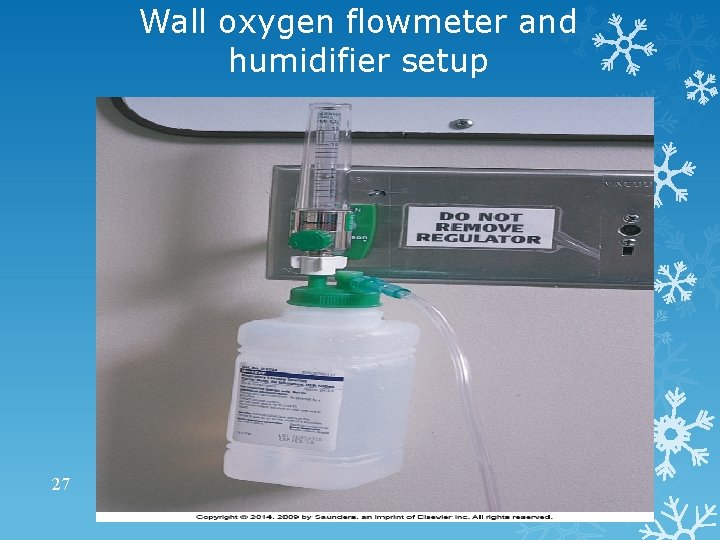
Wall oxygen flowmeter and humidifier setup 27
Oxygen Administration (cont’d) Used to supplement oxygen in inspired air Inspired air is 21% oxygen Can be delivered by nasal cannula, mask, tent, croupette, or catheter Requires humidification, flow rate prescribed by a physician Common flow rates are 4 -6 L/min COPD patients given only 2 to 3 L/min to prevent causing respiratory arrest 28
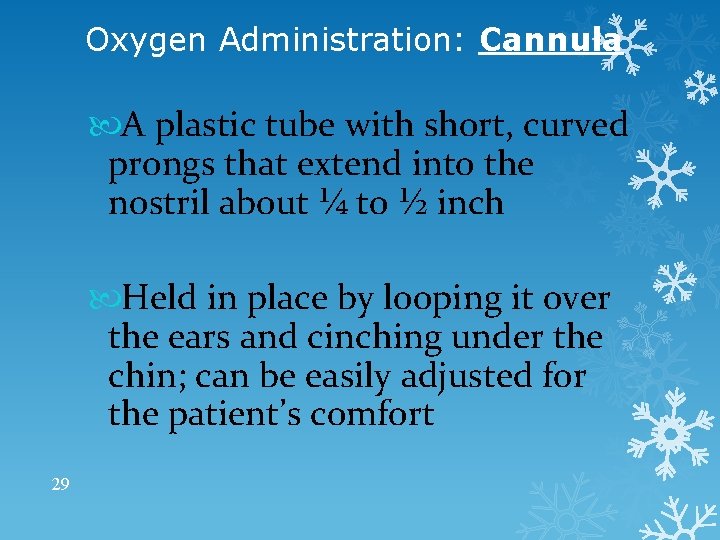
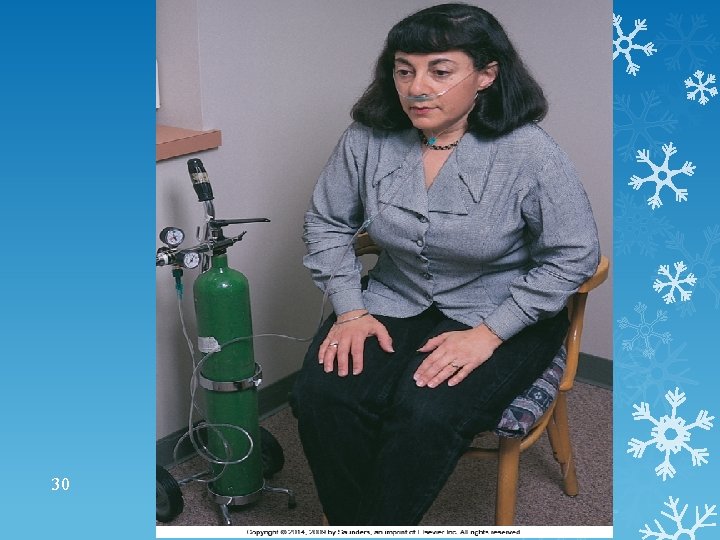
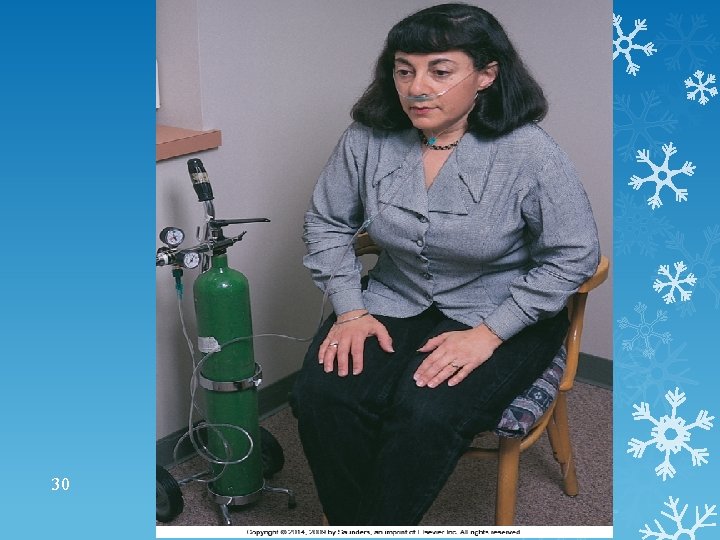
Oxygen Administration: Cannula A plastic tube with short, curved prongs that extend into the nostril about ¼ to ½ inch Held in place by looping it over the ears and cinching under the chin; can be easily adjusted for the patient’s comfort 29
30
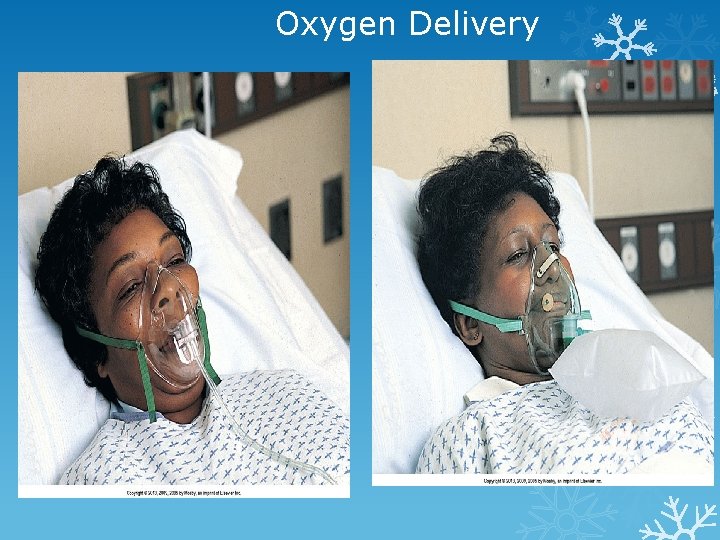
Oxygen Administration: Masks Various types available for administering oxygen in concentrations ranging from 24% to 55% at flows of 3 to 7 L/min Oxygen concentrations above 60% rarely used because of the danger of oxygen toxicity 31
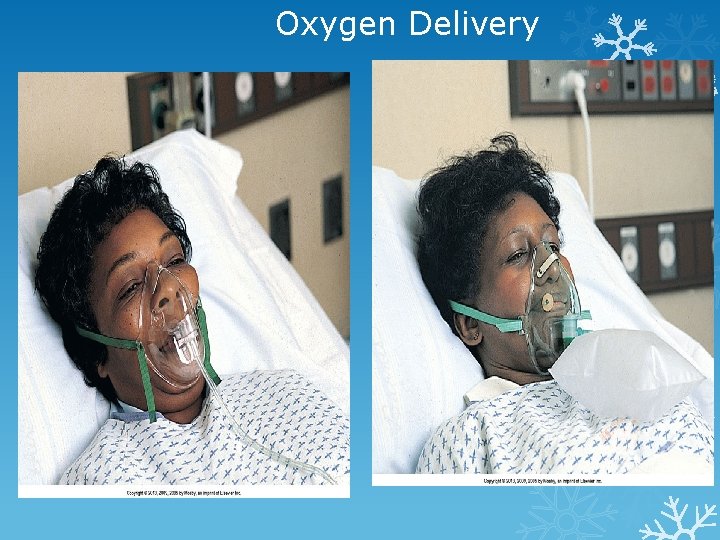
Oxygen Delivery
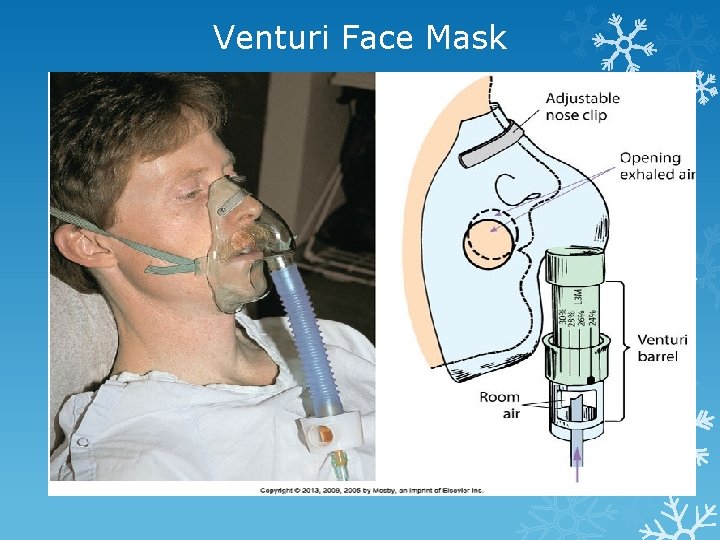
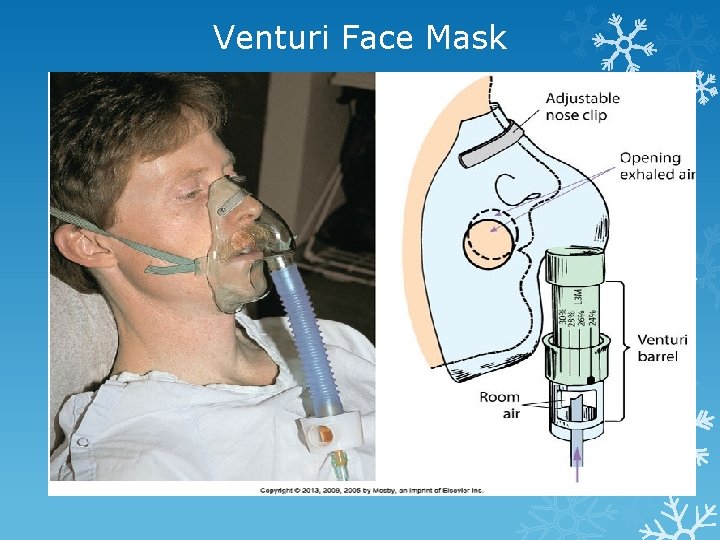
Venturi Face Mask
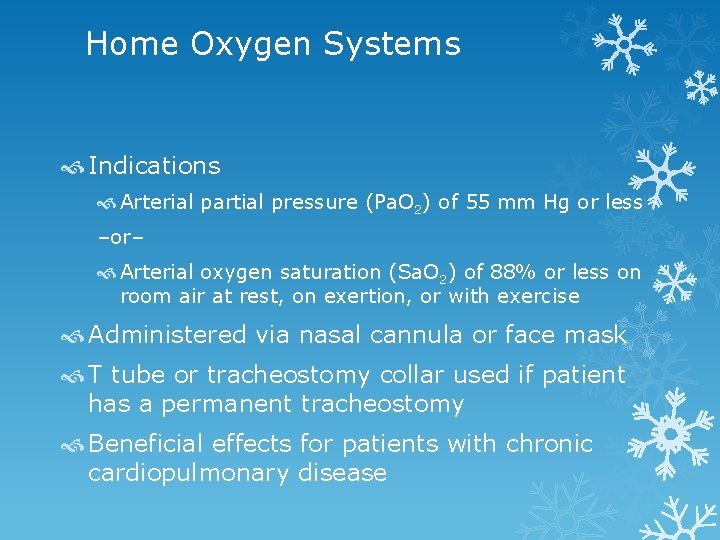
Home Oxygen Systems Indications Arterial partial pressure (Pa. O 2) of 55 mm Hg or less –or– Arterial oxygen saturation (Sa. O 2) of 88% or less on room air at rest, on exertion, or with exercise Administered via nasal cannula or face mask T tube or tracheostomy collar used if patient has a permanent tracheostomy Beneficial effects for patients with chronic cardiopulmonary disease
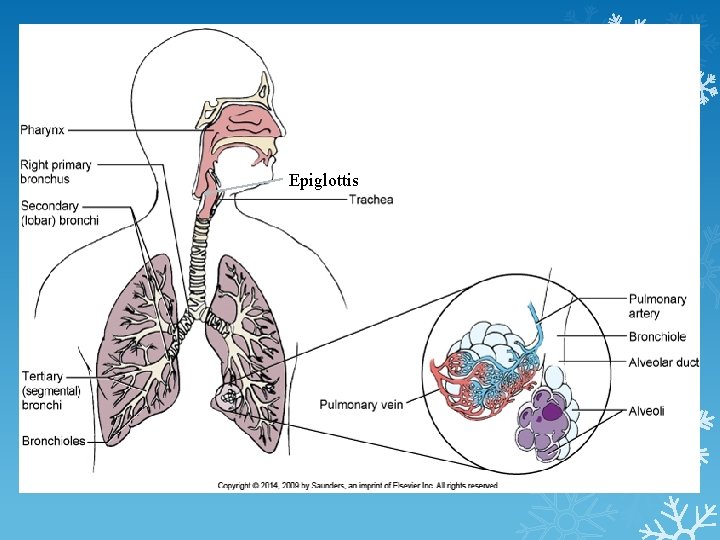
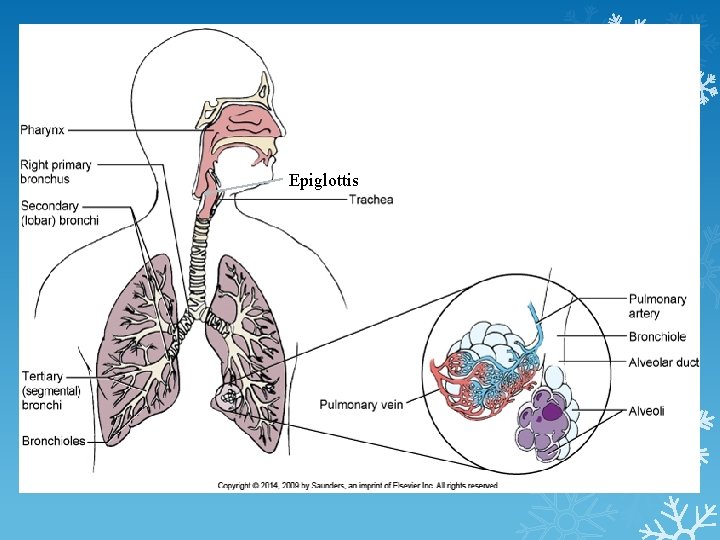
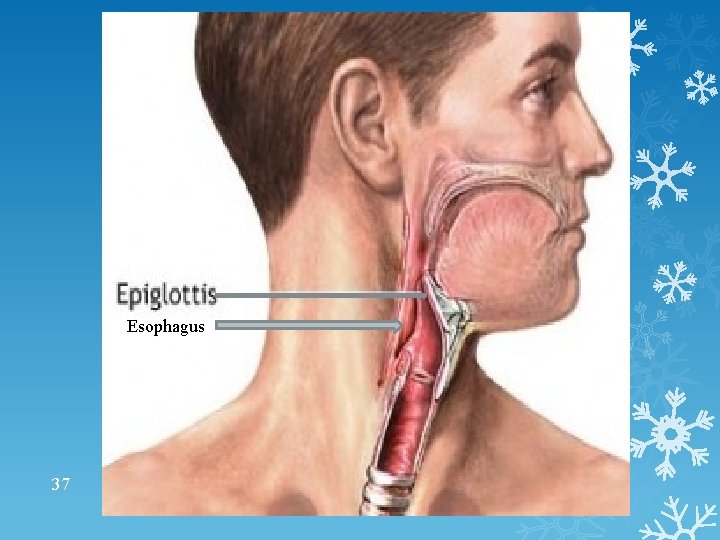
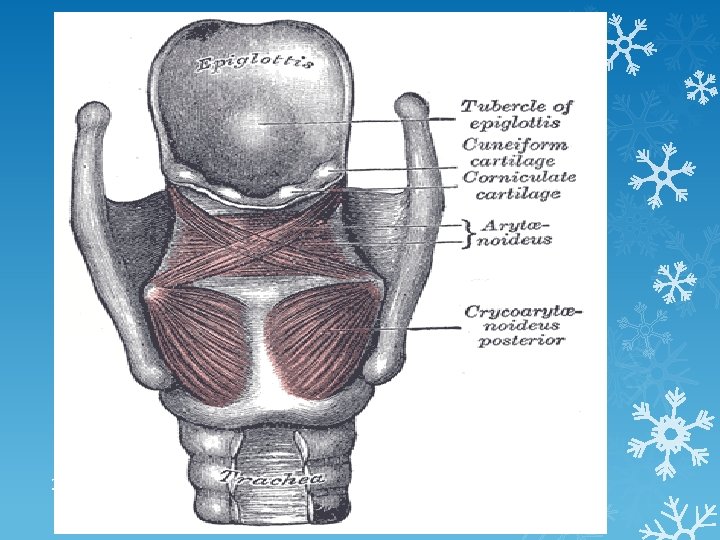
Epiglottis 35
36
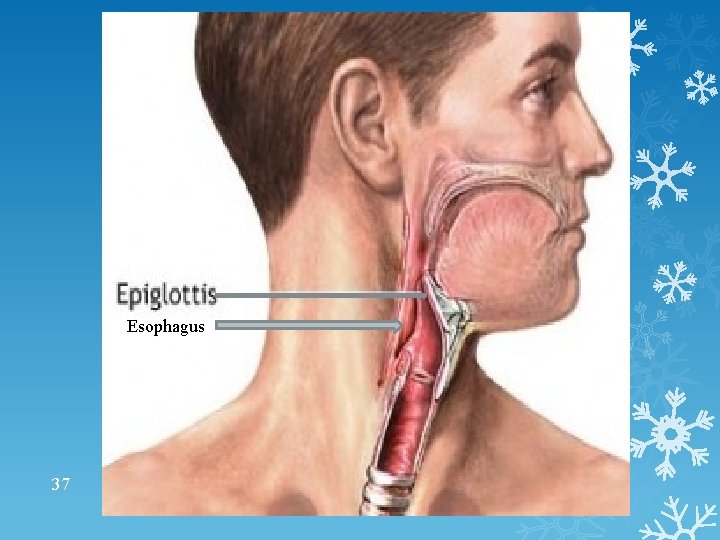
Esophagus 37
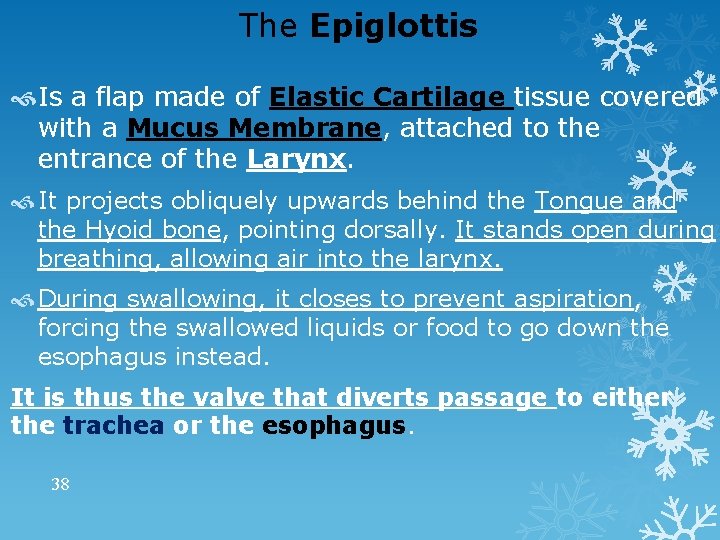
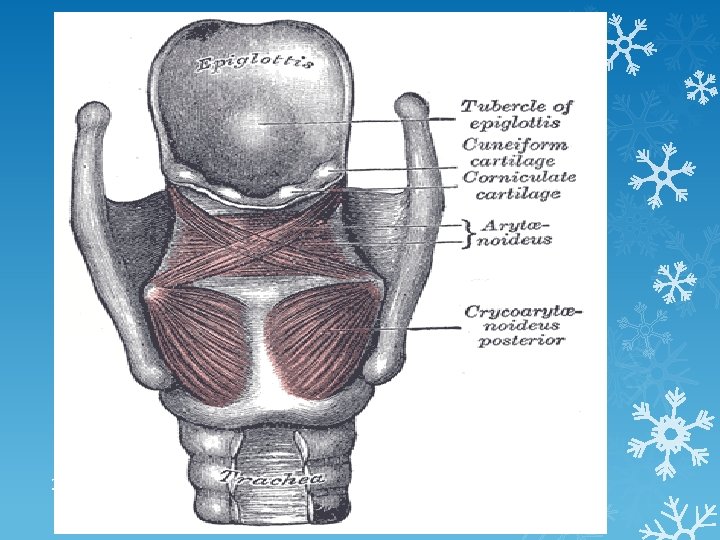
The Epiglottis Is a flap made of Elastic Cartilage tissue covered with a Mucus Membrane, attached to the entrance of the Larynx. It projects obliquely upwards behind the Tongue and the Hyoid bone, pointing dorsally. It stands open during breathing, allowing air into the larynx. During swallowing, it closes to prevent aspiration, forcing the swallowed liquids or food to go down the esophagus instead. It is thus the valve that diverts passage to either the trachea or the esophagus. 38
Assesment & Evaluation Perform Observe respiratory rate before, during, and after any activity. Assess any sputum produced. Auscultate lung sounds for improvement in adventitious sounds.
Suctioning Required for patients unable to clear secretions from their own airway effectively Nasopharyngeal Oral suction Can be performed with a Yankauer suction tip or with a 14 to 16 Fr. suction catheter attached to wall suction Negative pressure set between 80 and 120 mm Hg 40 Aseptic technique used for airway suctioning
WHEN TO SUCTION Suctioning is done only for patients who can’t clear their own airways. Its timing should be tailored to each patient rather than performed on a set schedule. Start with a complete assessment. Findings that suggest the need for suctioning include increased work of breathing, changes in respiratory rate, decreased oxygen saturation, copious secretions, wheezing, and the patient’s unsuccessful 41 attempts to clear secretions.
Nasopharyngeal Suctioning Maintain patent airway by removing accumulated secretions Involves upper air passages of nose, mouth, and pharynx Used most often for infants, gravely debilitated or unconscious patients, and those who have an ineffective cough Suction pressure set between 80 and 120 mm Hg 42
Tracheobronchial Suctioning Deep suctioning to remove secretions from the trachea and bronchi using sterile technique Most often performed on intubated patients or patients with a tracheostomy Patients need preoxygenation Sterile technique is mandatory Should be performed no longer than 10 seconds at a time, with oxygenation in between 43
Tracheostomy A surgical opening into the trachea to facilitate insertion of a cuffed tracheostomy tube Cuff enables controlling the airway and preventing aspiration Maintains a patent airway; facilitates suctioning and mechanical ventilation May be temporary or permanent 44
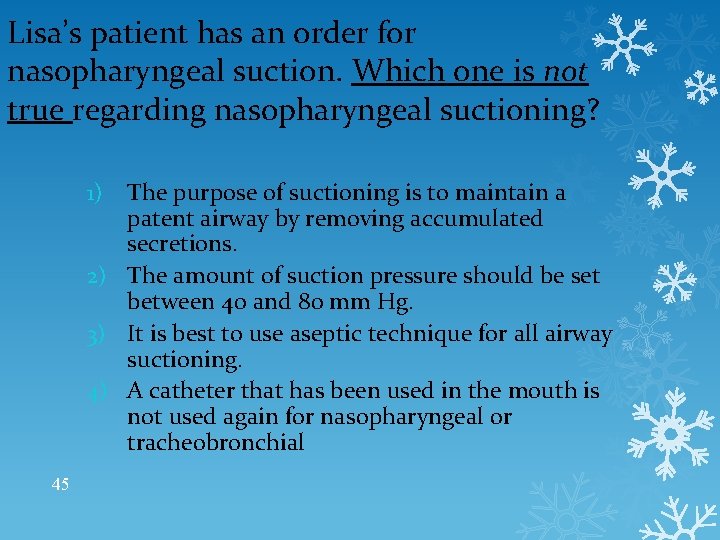
Lisa’s patient has an order for nasopharyngeal suction. Which one is not true regarding nasopharyngeal suctioning? The purpose of suctioning is to maintain a patent airway by removing accumulated secretions. 2) The amount of suction pressure should be set between 40 and 80 mm Hg. 3) It is best to use aseptic technique for all airway suctioning. 4) A catheter that has been used in the mouth is not used again for nasopharyngeal or tracheobronchial 1) 45