Nariman Sadeghi 1 Nariman sadeghi EMS educator MSc





















- Slides: 83

Nariman Sadeghi 1 Nariman sadeghi. EMS educator, MSc. N 10/25/2021 ADVANCED CARDIOVASCULAR LIFE SUPPORT ACLS
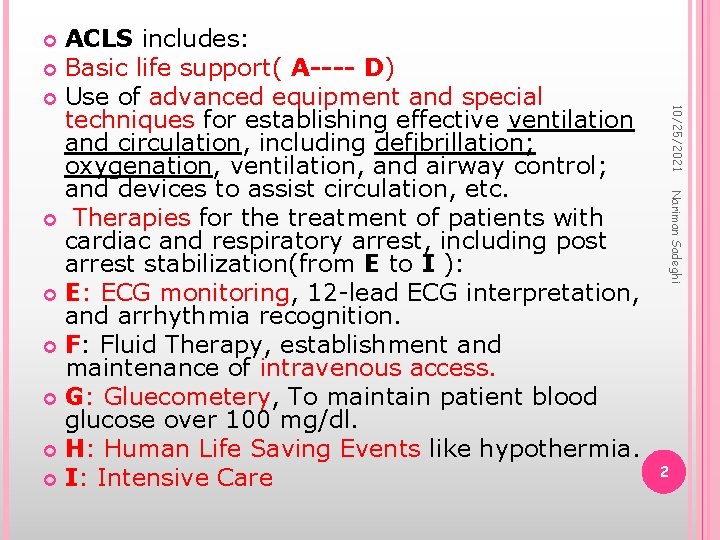
ACLS includes: Basic life support( A---- D) Use of advanced equipment and special techniques for establishing effective ventilation and circulation, including defibrillation; oxygenation, ventilation, and airway control; and devices to assist circulation, etc. Therapies for the treatment of patients with cardiac and respiratory arrest, including post arrest stabilization(from E to I ): E: ECG monitoring, 12 -lead ECG interpretation, and arrhythmia recognition. F: Fluid Therapy, establishment and maintenance of intravenous access. G: Gluecometery, To maintain patient blood glucose over 100 mg/dl. H: Human Life Saving Events like hypothermia. I: Intensive Care 10/25/2021 Nariman Sadeghi 2
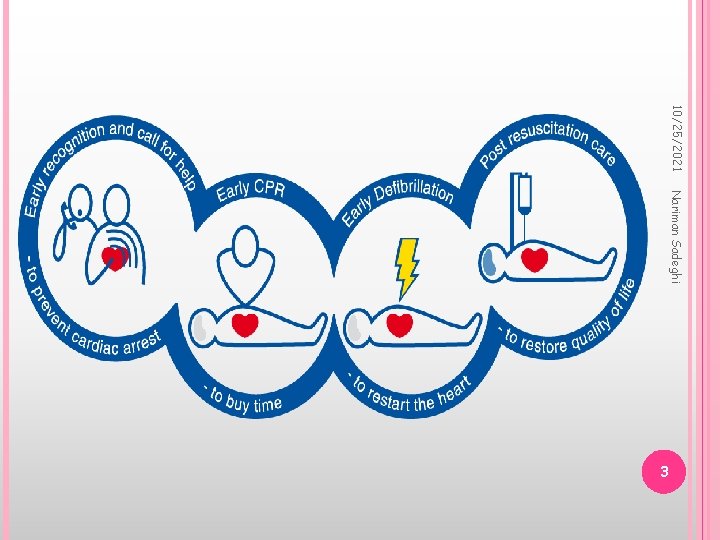
10/25/2021 Nariman Sadeghi 3
Nariman Sadeghi 4 10/25/2021 BLS
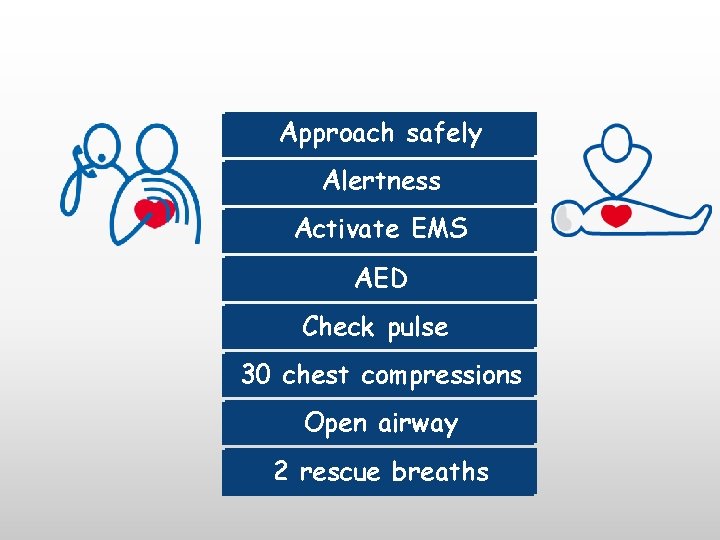
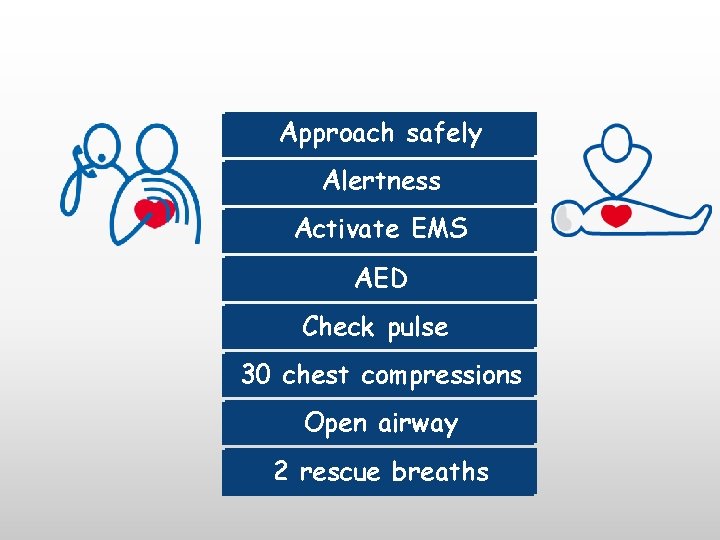
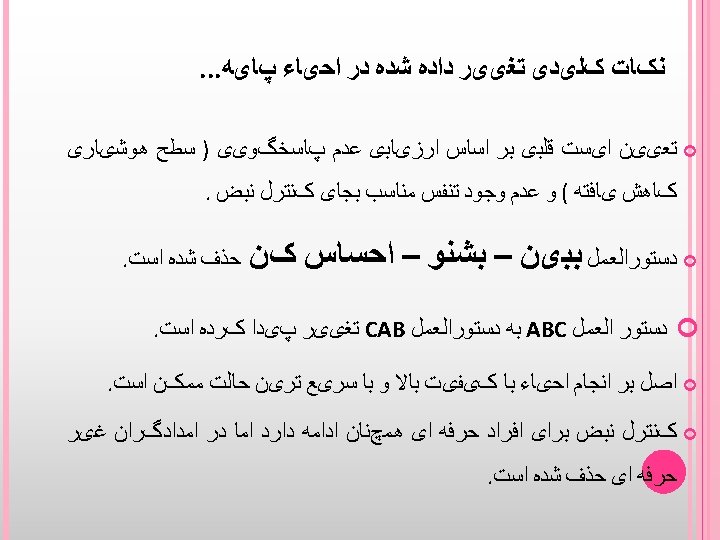
Approach safely Approach Alertness Check response Activate Call 115 -EMS AED Check pulse 30 chest Checkcompressions pulse 30 chest Opencompressions airway Open airway 2 rescue breaths

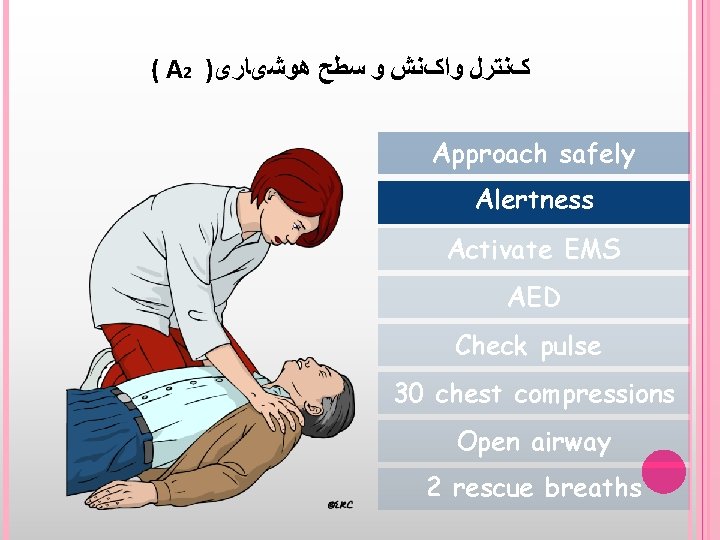
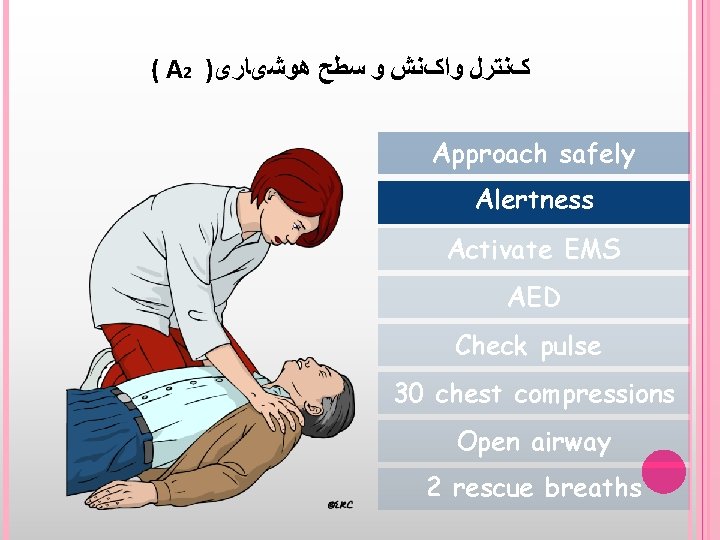
( A 2 ) کﻨﺘﺮﻝ ﻭﺍکﻨﺶ ﻭ ﺳﻄﺢ ﻫﻮﺷیﺎﺭی Approach safely Alertness Activate EMS AED Check pulse 30 chest compressions Open airway 2 rescue breaths



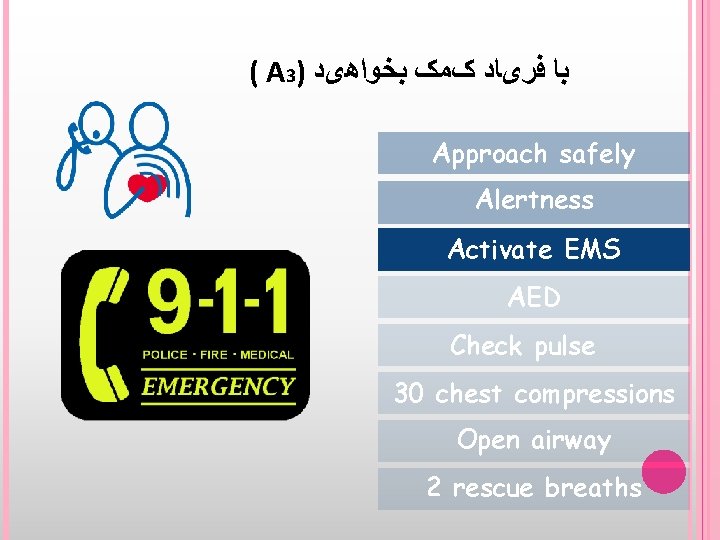
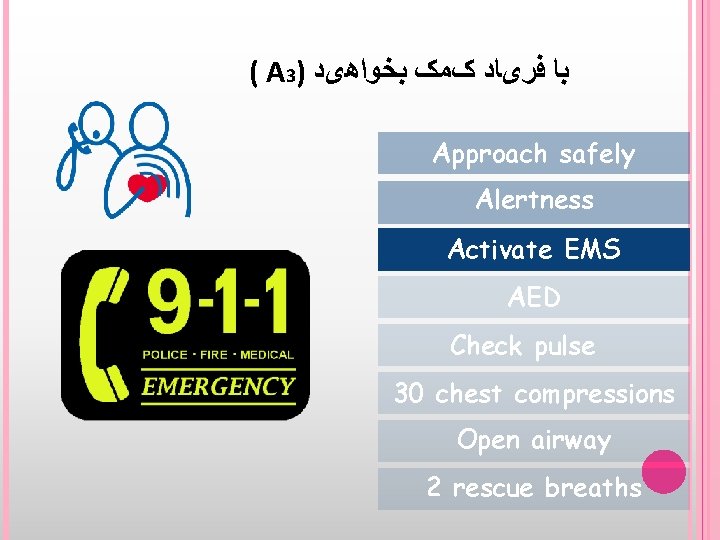
( A 3) ﺑﺎ ﻓﺮیﺎﺩ کﻤک ﺑﺨﻮﺍﻫیﺪ Approach safely Alertness Activate EMS AED Check pulse 30 chest compressions Open airway 2 rescue breaths
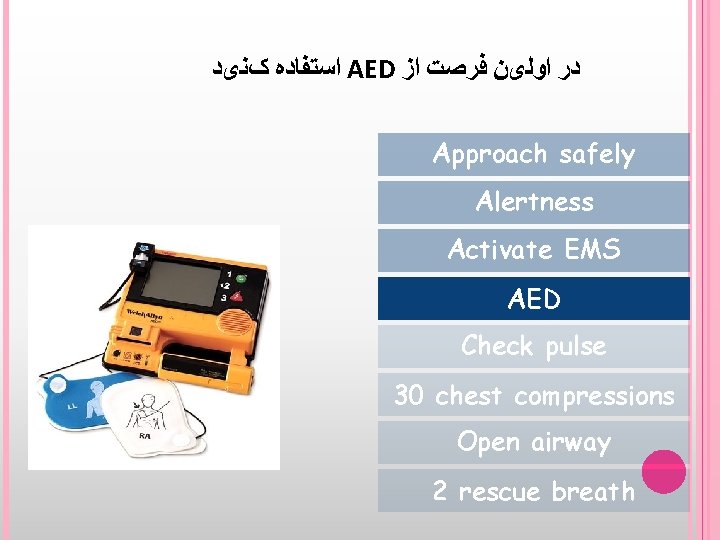
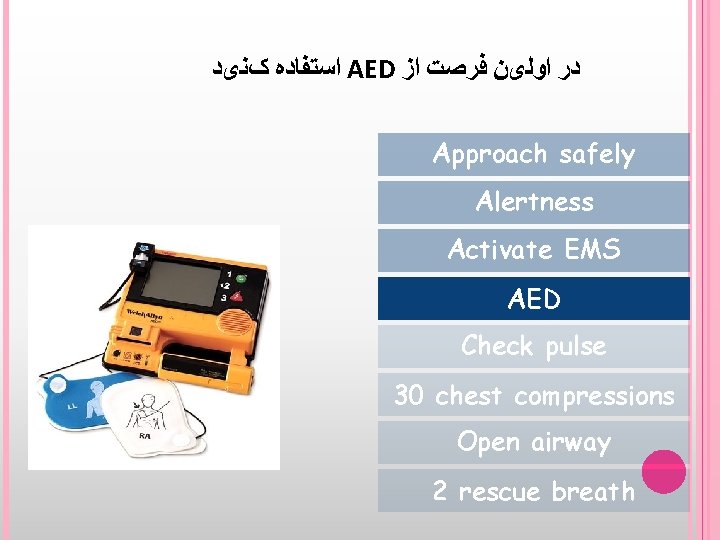
ﺍﺳﺘﻔﺎﺩﻩ کﻨیﺪ AED ﺩﺭ ﺍﻭﻟیﻦ ﻓﺮﺻﺖ ﺍﺯ Approach safely Alertness Activate EMS AED Check pulse 30 chest compressions Open airway 2 rescue breath
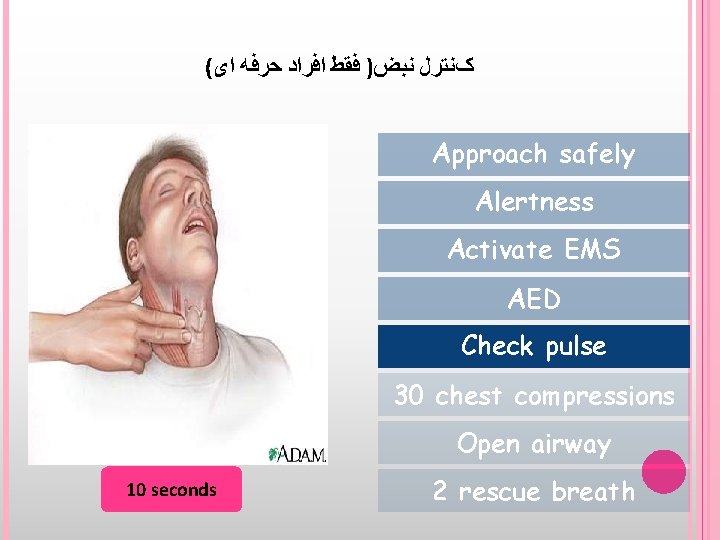
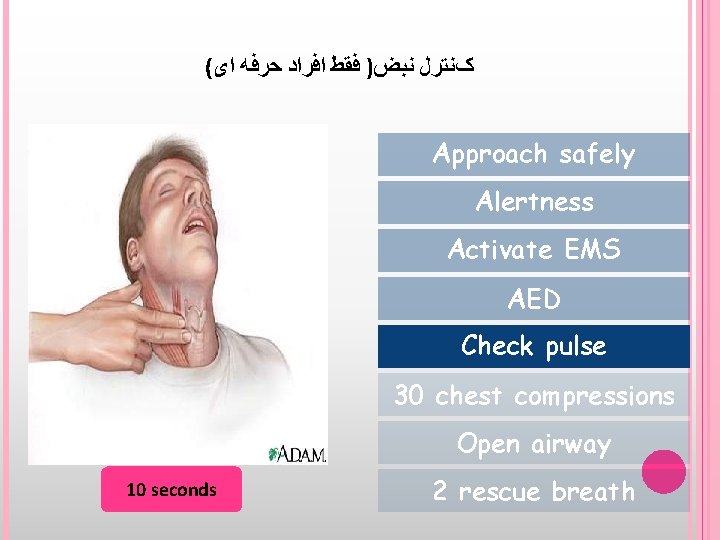
( کﻨﺘﺮﻝ ﻧﺒﺾ) ﻓﻘﻂ ﺍﻓﺮﺍﺩ ﺣﺮﻓﻪ ﺍی Approach safely Alertness Activate EMS AED Check pulse 30 chest compressions Open airway 10 seconds 2 rescue breath

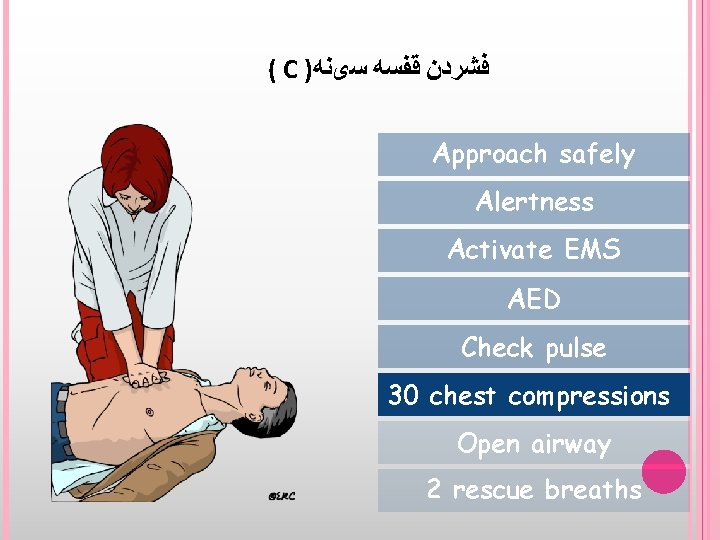
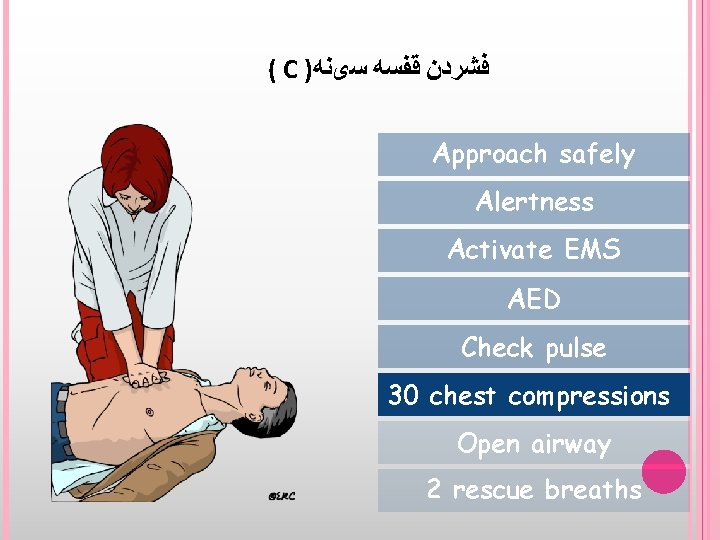
( C ) ﻓﺸﺮﺩﻥ ﻗﻔﺴﻪ ﺳیﻨﻪ Approach safely Alertness Activate EMS AED Check pulse 30 chest compressions Open airway 2 rescue breaths


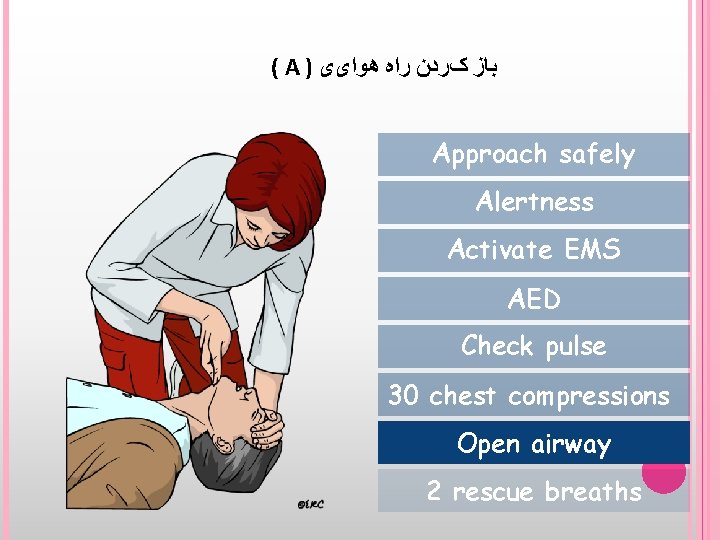
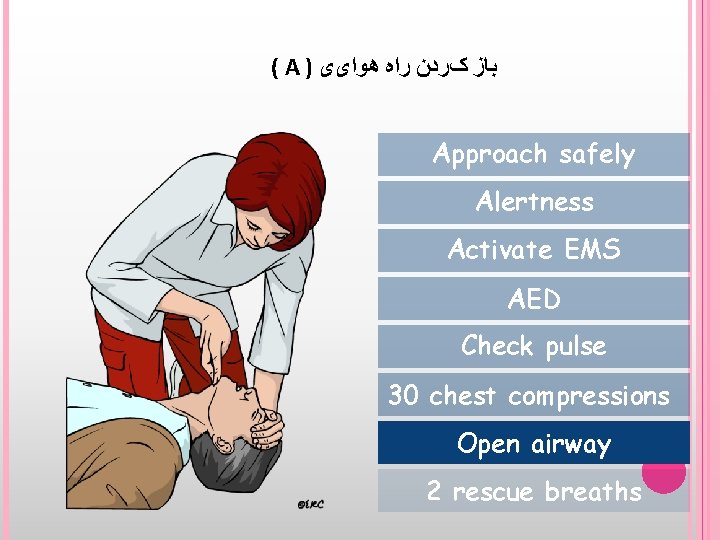
( A ) ﺑﺎﺯ کﺮﺩﻥ ﺭﺍﻩ ﻫﻮﺍیی Approach safely Alertness Activate EMS AED Check pulse 30 chest compressions Open airway 2 rescue breaths
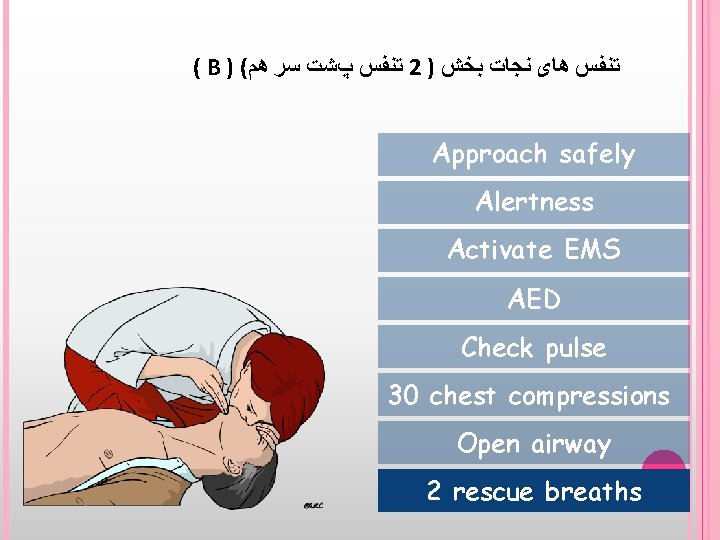
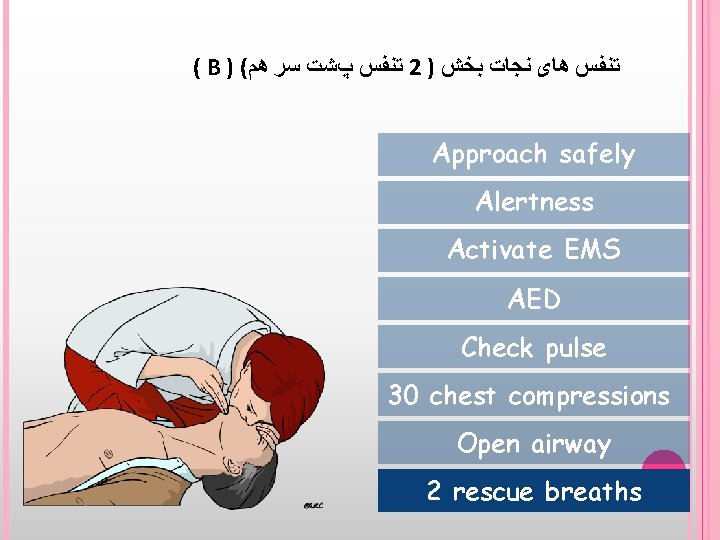
( B ) ( ﺗﻨﻔﺲ پﺸﺖ ﺳﺮ ﻫﻢ 2 ) ﺗﻨﻔﺲ ﻫﺎی ﻧﺠﺎﺕ ﺑﺨﺶ Approach safely Alertness Activate EMS AED Check pulse 30 chest compressions Open airway 2 rescue breaths








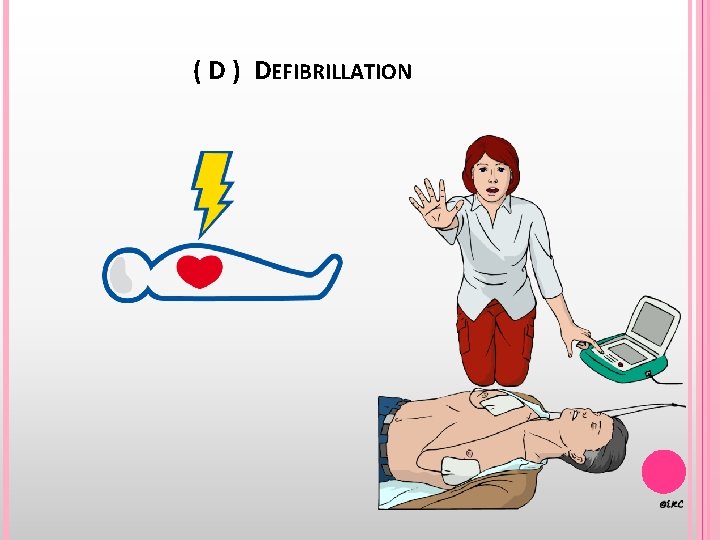
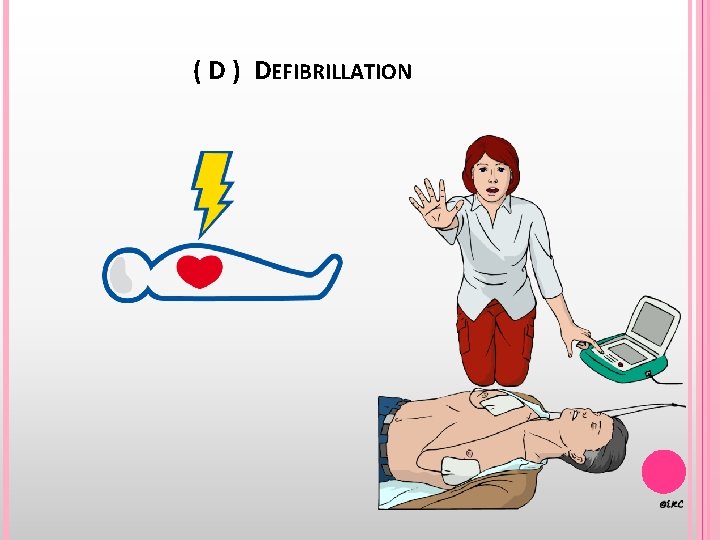
( D ) DEFIBRILLATION
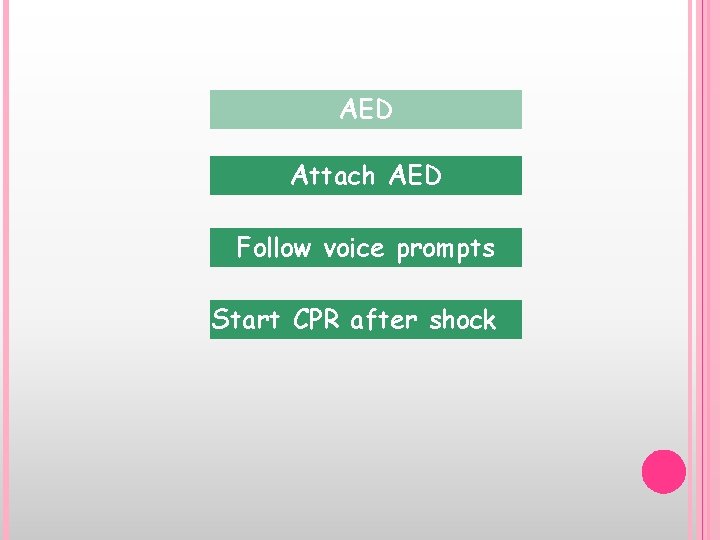
AED Attach AED Follow voice prompts Start CPR after shock
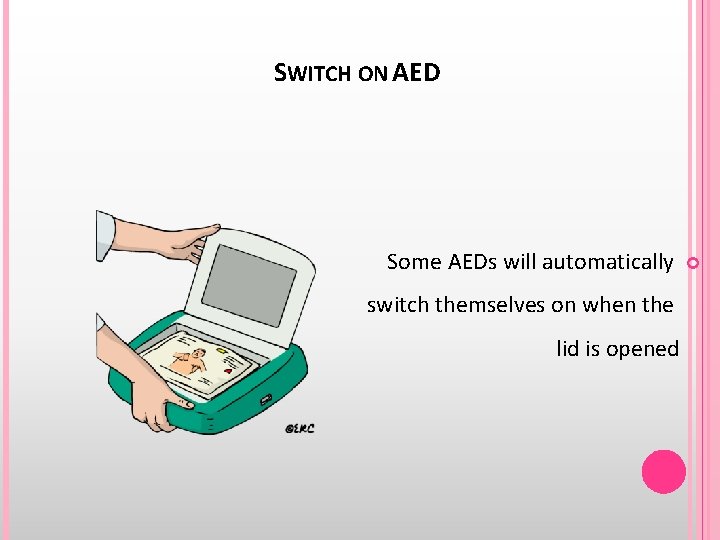
SWITCH ON AED Some AEDs will automatically switch themselves on when the lid is opened
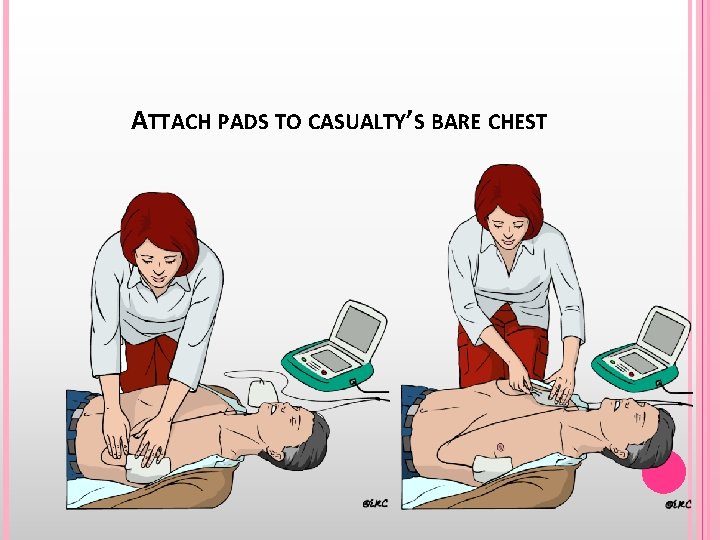
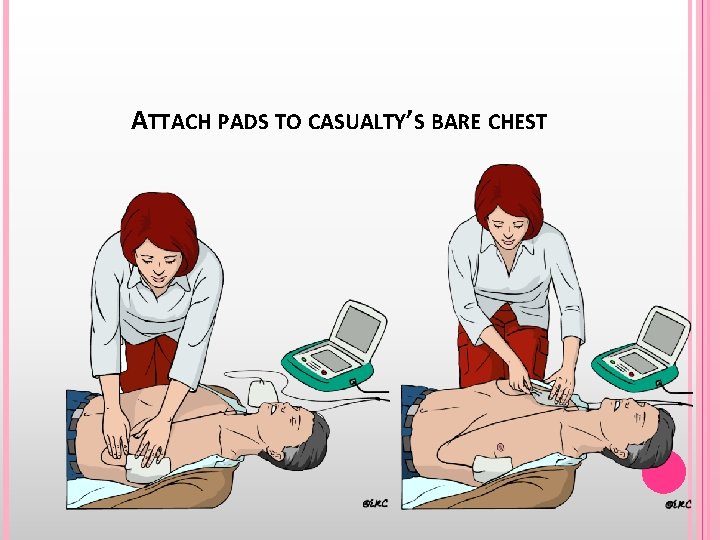
ATTACH PADS TO CASUALTY’S BARE CHEST
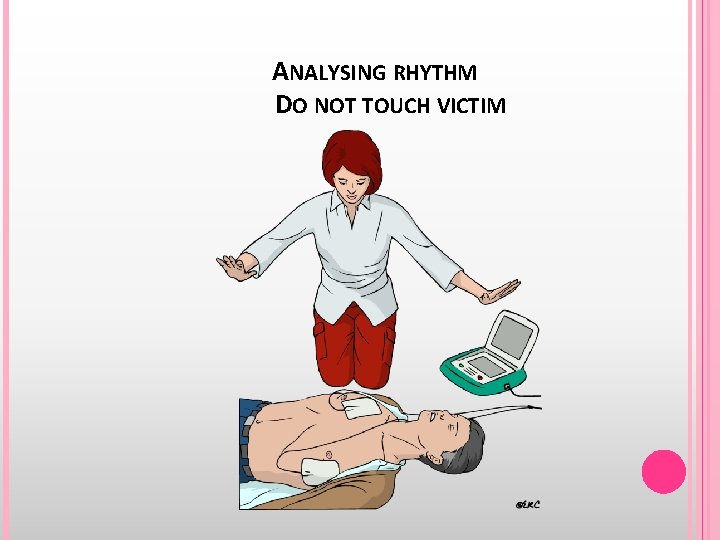
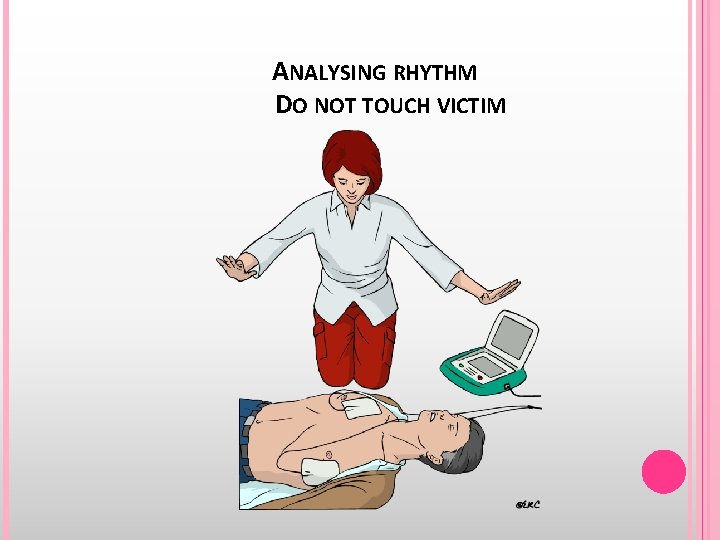
ANALYSING RHYTHM DO NOT TOUCH VICTIM
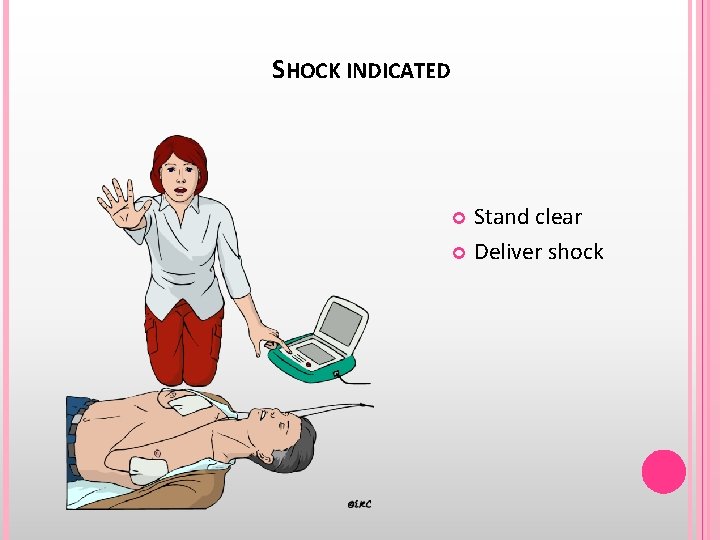
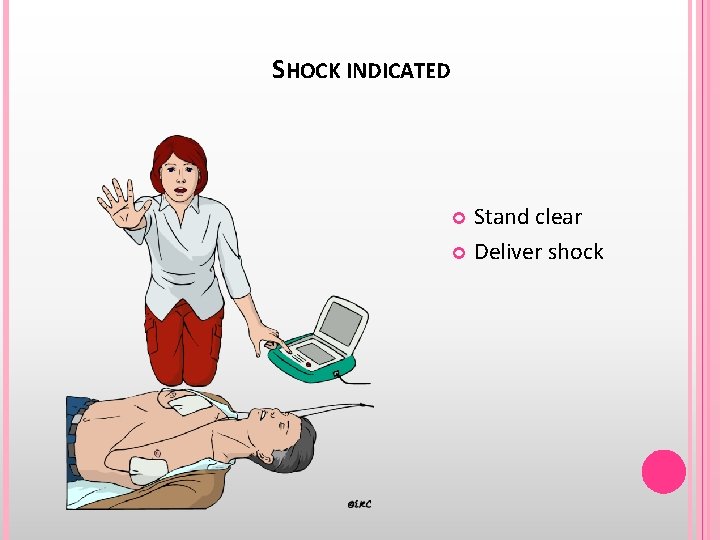
SHOCK INDICATED Stand clear Deliver shock
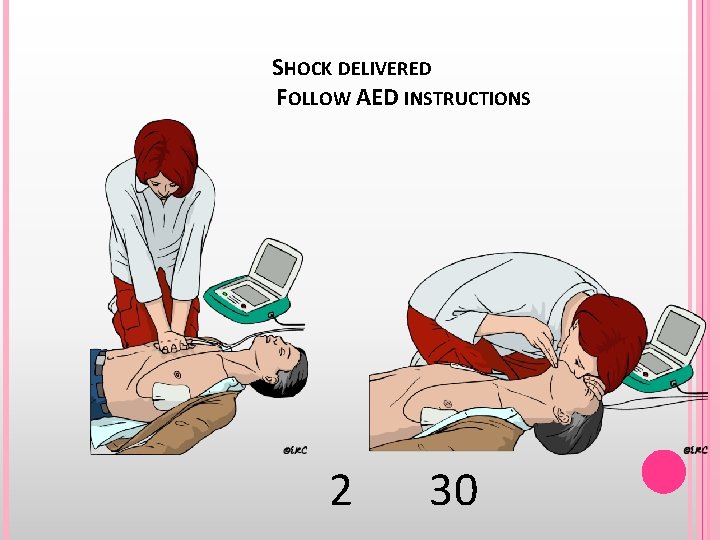
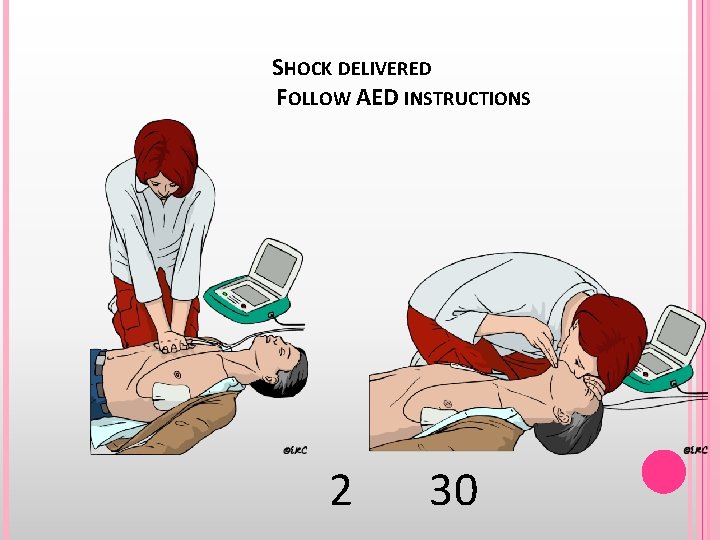
SHOCK DELIVERED FOLLOW AED INSTRUCTIONS 2 30
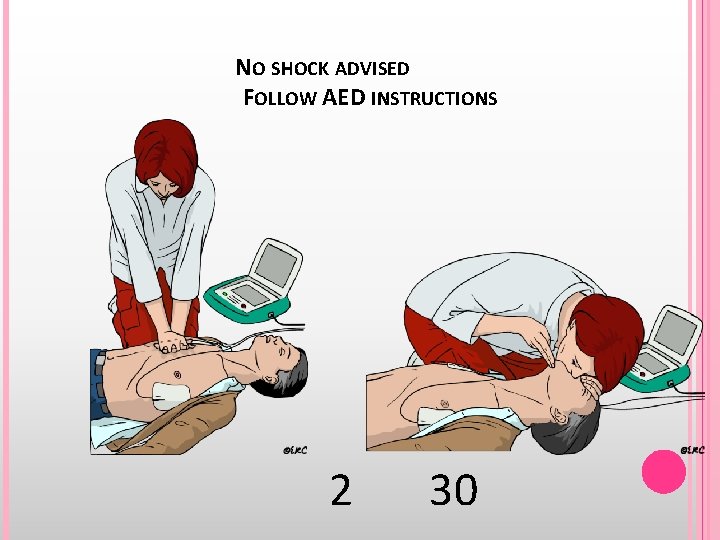
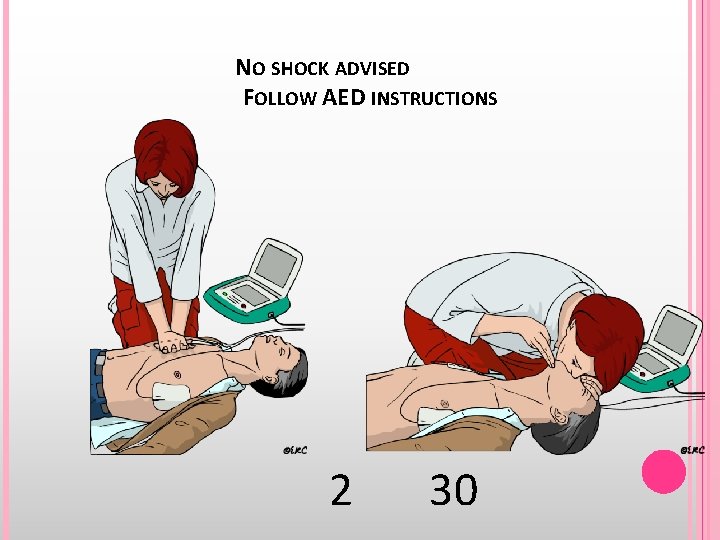
NO SHOCK ADVISED FOLLOW AED INSTRUCTIONS 2 30
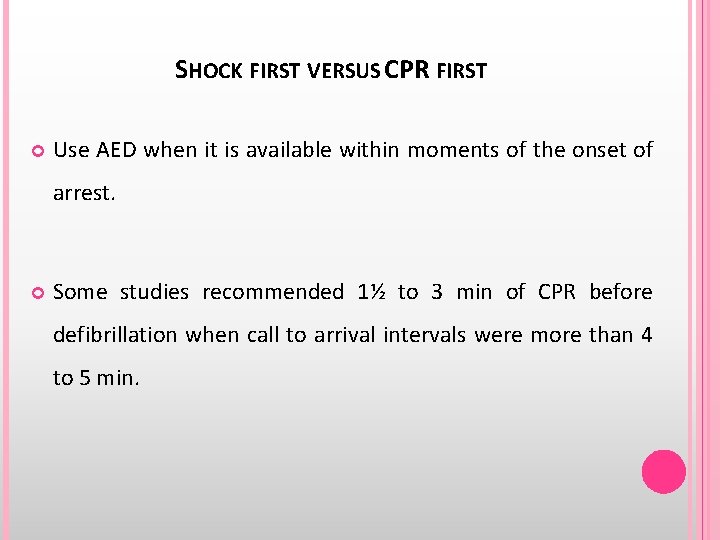
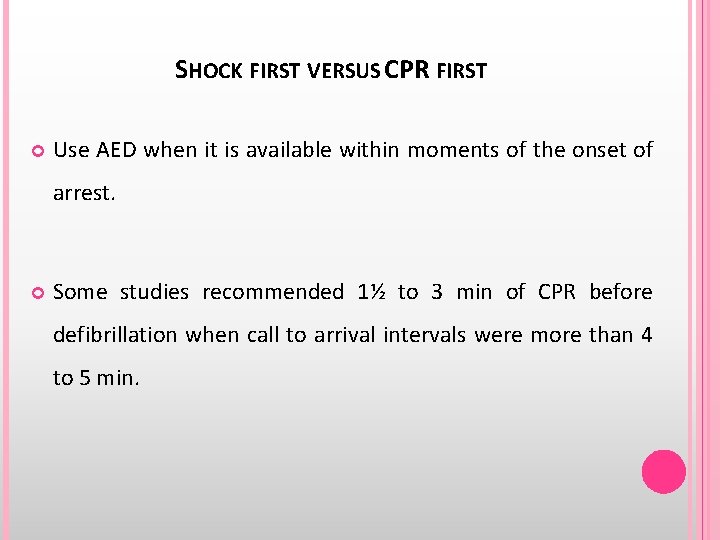
SHOCK FIRST VERSUS CPR FIRST Use AED when it is available within moments of the onset of arrest. Some studies recommended 1½ to 3 min of CPR before defibrillation when call to arrival intervals were more than 4 to 5 min.
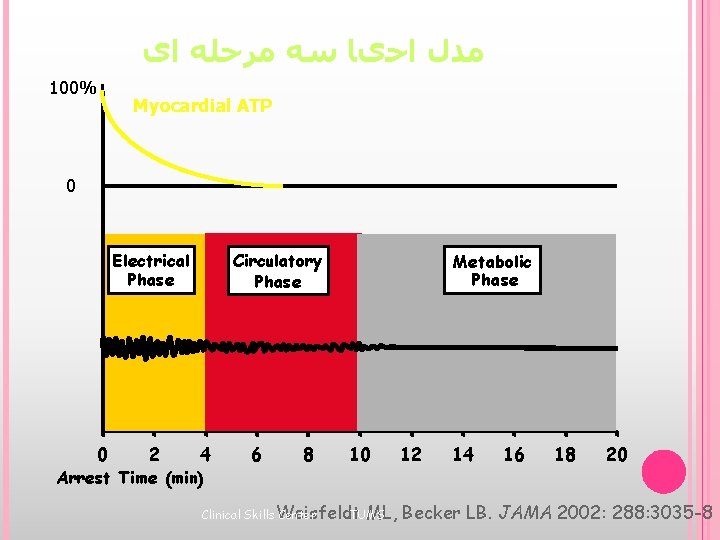
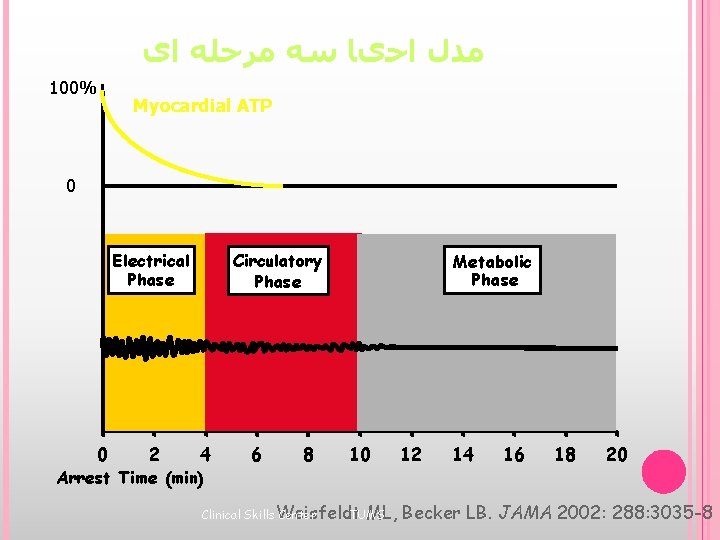
ﻣﺪﻝ ﺍﺣیﺎ ﺳﻪ ﻣﺮﺣﻠﻪ ﺍی 100% Myocardial ATP 0 Circulatory Phase Electrical Phase 0 2 4 Arrest Time (min) 6 8 Metabolic Phase 10 ML, Clinical Skills Weisfeldt Center TUMS 12 14 16 18 20 Becker LB. JAMA 2002: 288: 3035 -8



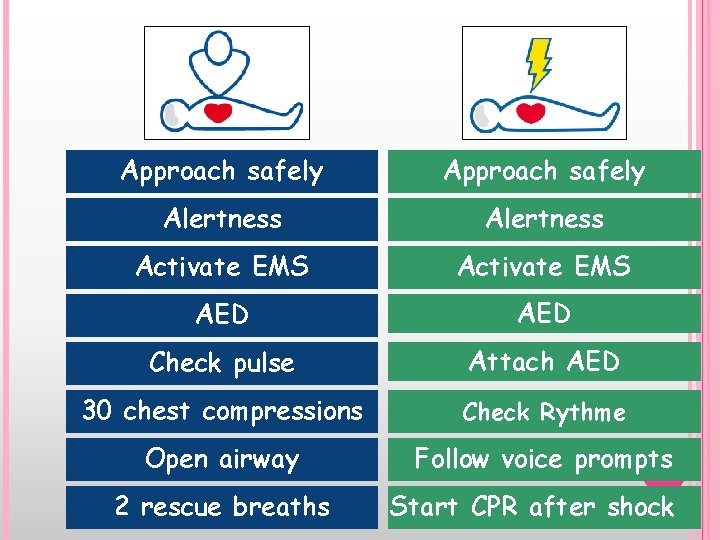
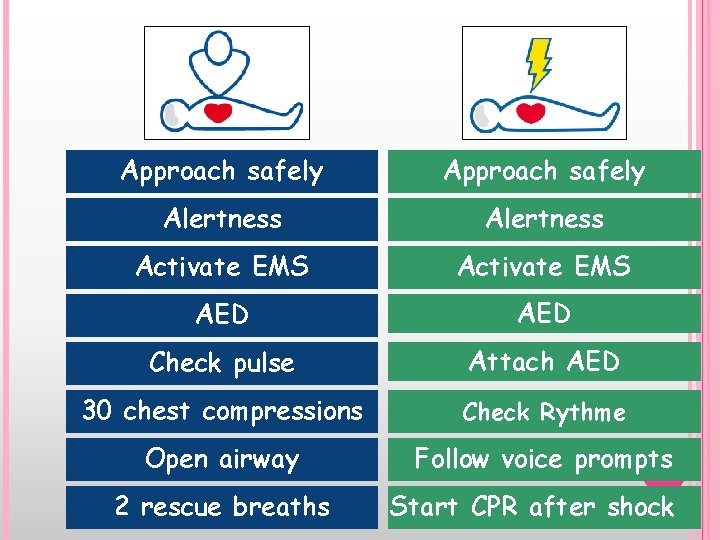
Approach safely Alertness Activate EMS AED Check pulse Attach AED 30 chest compressions Check Rythme Open airway Follow voice prompts 2 rescue breaths Start CPR after shock

Some challenges. . .
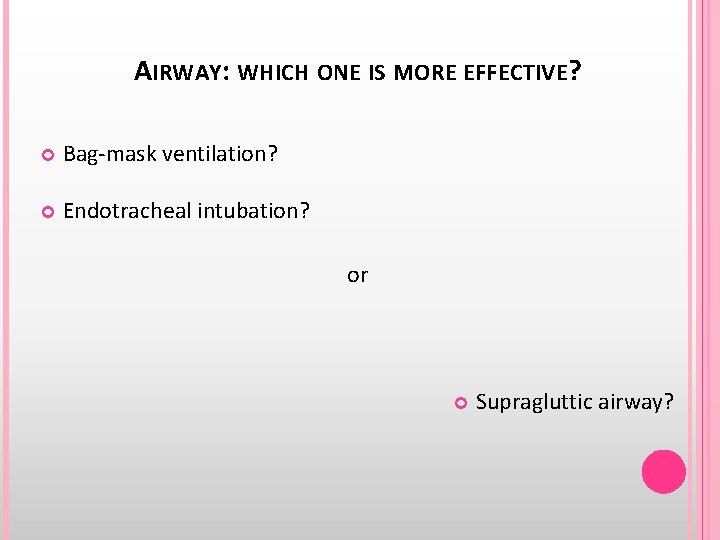
AIRWAY: WHICH ONE IS MORE EFFECTIVE? Bag-mask ventilation? Endotracheal intubation? or Supragluttic airway?
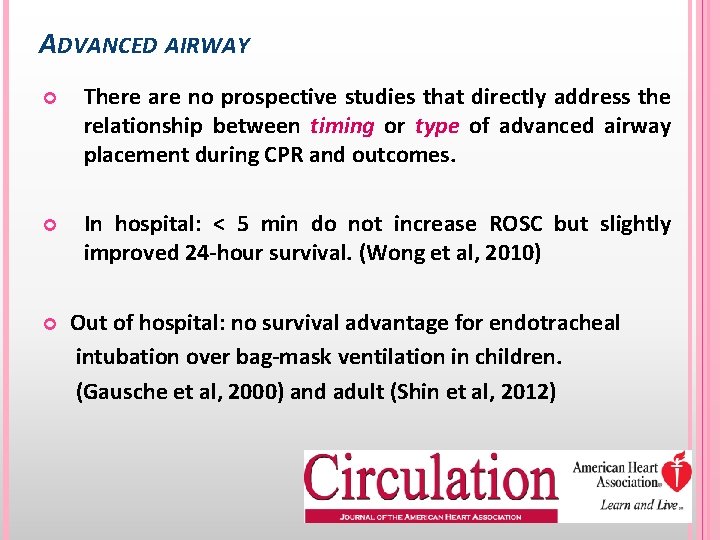
ADVANCED AIRWAY There are no prospective studies that directly address the relationship between timing or type of advanced airway placement during CPR and outcomes. In hospital: < 5 min do not increase ROSC but slightly improved 24 -hour survival. (Wong et al, 2010) Out of hospital: no survival advantage for endotracheal intubation over bag-mask ventilation in children. (Gausche et al, 2000) and adult (Shin et al, 2012)
Questions?
Nariman Sadeghi After using Advance Air Way the next step is ECG 12 lead ECG has to obtain for determining the arrhythmia. The most common kind of arrhythmia is VF or VT or Asystole. VT has two versions: Pulse VT and Pulseless VT 10/25/2021 E: ECG 47
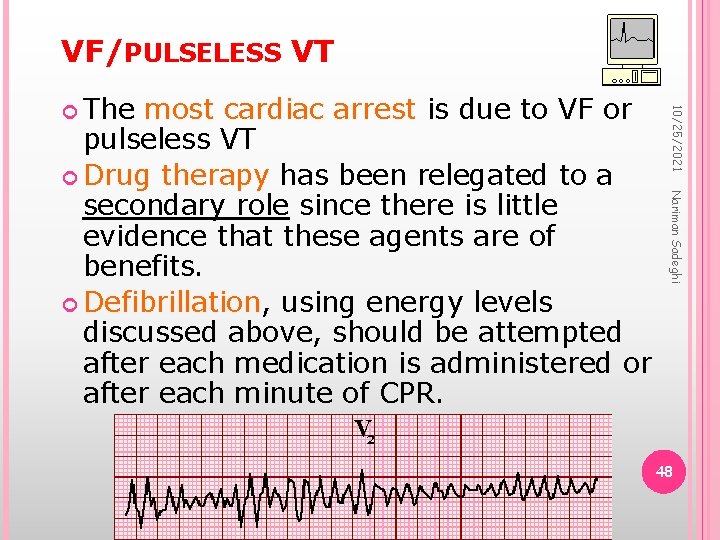
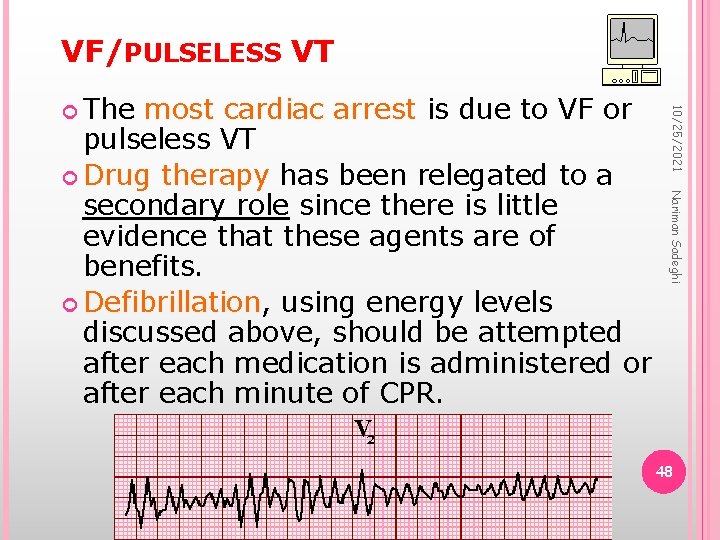
VF/PULSELESS VT Nariman Sadeghi most cardiac arrest is due to VF or pulseless VT Drug therapy has been relegated to a secondary role since there is little evidence that these agents are of benefits. Defibrillation, using energy levels discussed above, should be attempted after each medication is administered or after each minute of CPR. 10/25/2021 The 48
EPINEPHRINE 10/25/2021 Nariman Sadeghi Epinephrine (1 mg intravenous push) is administered if VF or pulseless VT persists after a second shock. It is repeated every three to five minutes thereafter if VF or pulseless VT persists. Higher doses of epinephrine (0. 2 mg/kg) is not suggested. 49
VASOPRESSIN Nariman Sadeghi is an acceptable alternative to epinephrine. It is recommended for asystole, VT, or VF; but not for PEA. A single intravenous dose of 40 U is given once (since the half life is 10 to 20 minutes compared to 3 to 5 minutes with epinephrine). 10/25/2021 Vasopressin 50
AMIODARONE Nariman Sadeghi is administered as a 300 mg intravenous push if VF or pulse less VT persists after three shocks. If VF or pulse less VT recurs or remains refractory, a further dose of 150 mg dose can be given immediately, followed by an infusion of 900 mg over 24 hours. 1 mg/min for the first 6 hours then 0. 5 mg/min for the next 18 hours 10/25/2021 Amiodarone 51
LIDOCAINE Nariman Sadeghi can be used as an alternative to amiodarone, but should not be administered if amiodarone has already been given. Lidocaine is administered at a dose of 1 mg/kg as an intravenous push and can be repeated every 3 to 5 minutes; it should not exceed a total dose of 3 mg/kg during the first hour. 10/25/2021 Lidocaine 52
PROCAINAMIDE Nariman Sadeghi Procainamide, administered at a dose of 30 mg/min intravenously up to a maximum dose of 17 mg/kg is acceptable but not recommended since the prolonged time for administration is unsuitable for a cardiac arrest. 10/25/2021 53
MAGNESIUM SULFATE Nariman Sadeghi Magnesium sulfate, 1 to 2 grams intravenously is recommended for the treatment of polymorphic VT (Torsade de Pointes) and suspected hypomagnesemic states. 10/25/2021 54
SODIUM BICARBONATE Nariman Sadeghi Sodium bicarbonate, 1 meq/kg intravenously, is indicated for severe conditions known to provoke sudden death, such as hyperkalemia, preexisting metabolic acidosis, or certain drug overdoses. 10/25/2021 55
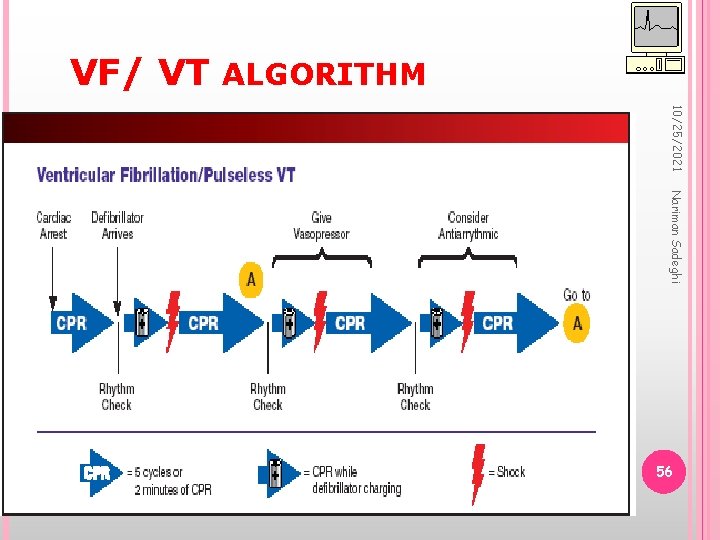
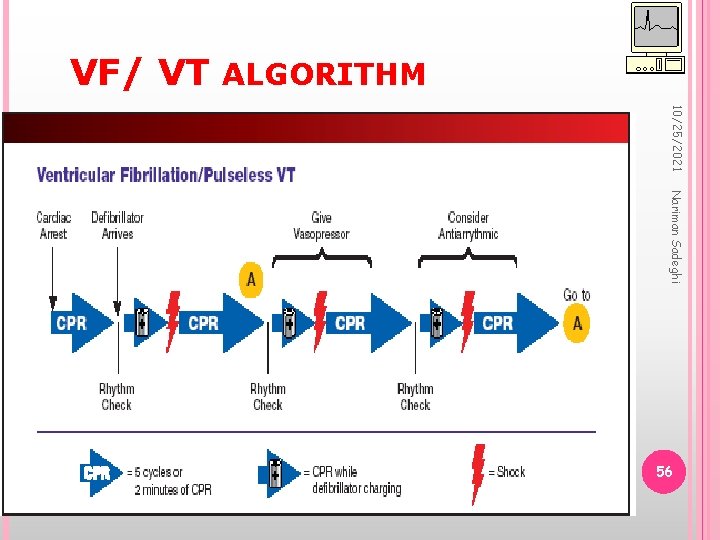
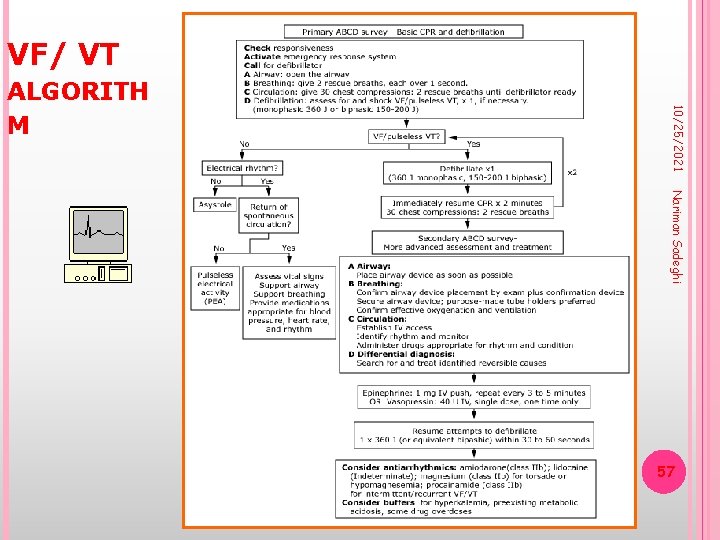
VF/ VT ALGORITHM 10/25/2021 Nariman Sadeghi 56
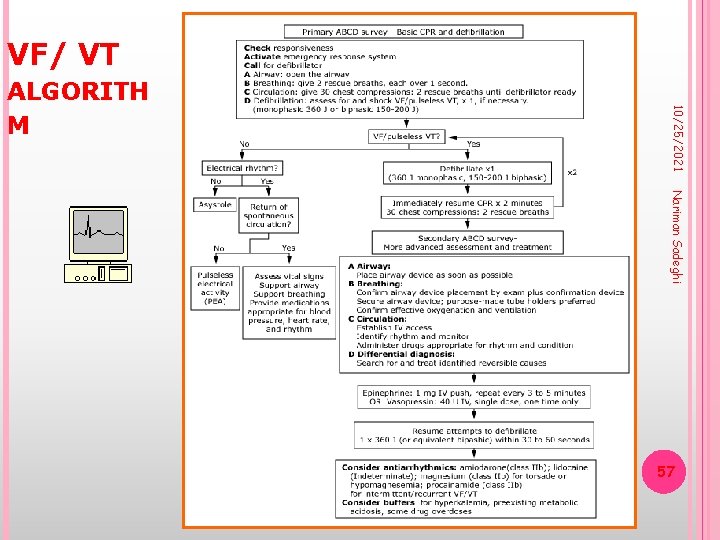
VF/ VT 10/25/2021 ALGORITH M Nariman Sadeghi 57

10/25/2021 Nariman Sadeghi 58
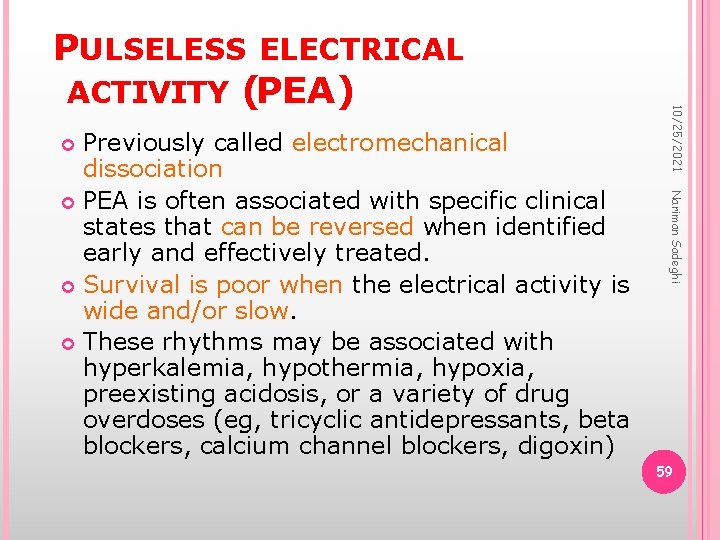
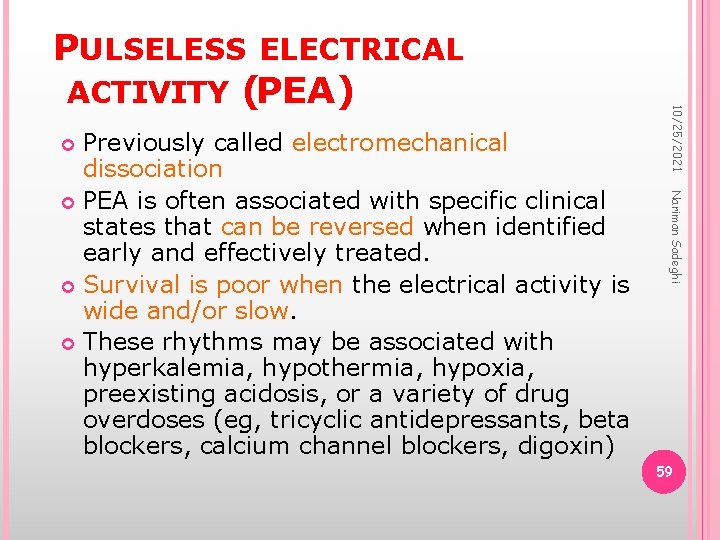
Nariman Sadeghi Previously called electromechanical dissociation PEA is often associated with specific clinical states that can be reversed when identified early and effectively treated. Survival is poor when the electrical activity is wide and/or slow. These rhythms may be associated with hyperkalemia, hypothermia, hypoxia, preexisting acidosis, or a variety of drug overdoses (eg, tricyclic antidepressants, beta blockers, calcium channel blockers, digoxin) 10/25/2021 PULSELESS ELECTRICAL ACTIVITY (PEA) 59
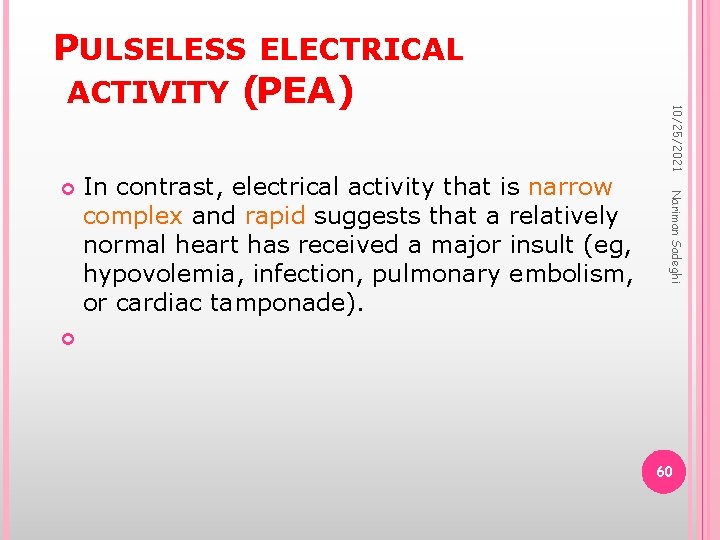
In contrast, electrical activity that is narrow complex and rapid suggests that a relatively normal heart has received a major insult (eg, hypovolemia, infection, pulmonary embolism, or cardiac tamponade). Nariman Sadeghi 10/25/2021 PULSELESS ELECTRICAL ACTIVITY (PEA) 60
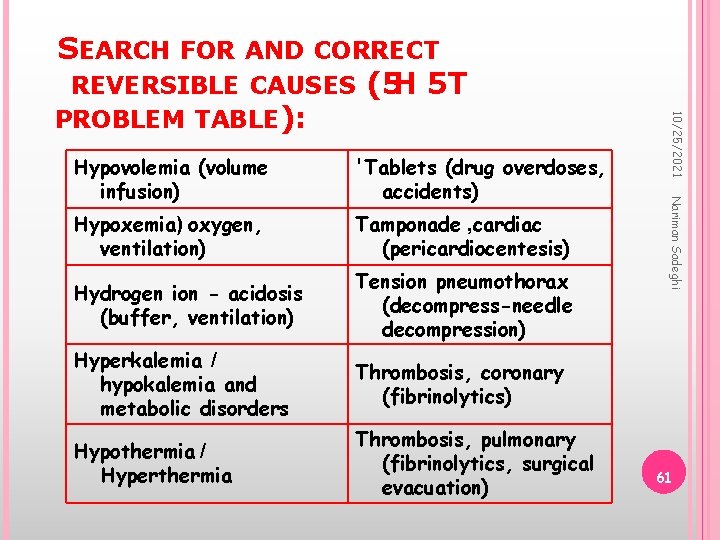
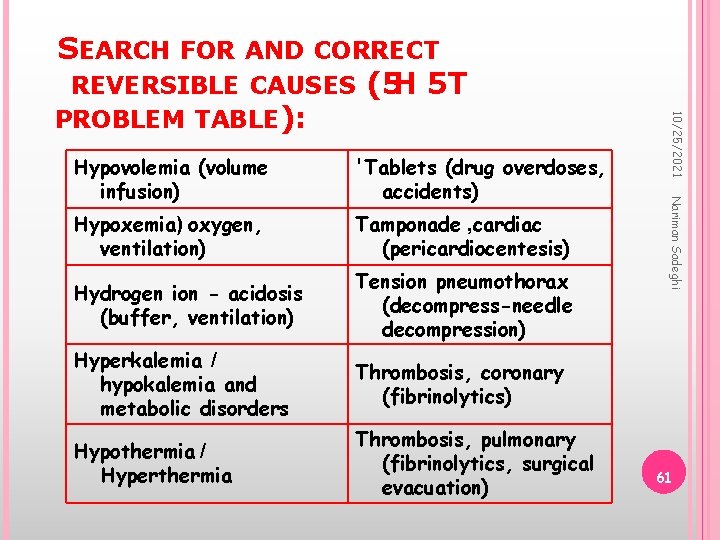
'Tablets (drug overdoses, accidents) Hypoxemia) oxygen, ventilation) Tamponade , cardiac (pericardiocentesis) Hydrogen ion - acidosis (buffer, ventilation) Tension pneumothorax (decompress-needle decompression) Hyperkalemia / hypokalemia and metabolic disorders Thrombosis, coronary (fibrinolytics) Hypothermia / Hyperthermia Thrombosis, pulmonary (fibrinolytics, surgical evacuation) Nariman Sadeghi Hypovolemia (volume infusion) 10/25/2021 SEARCH FOR AND CORRECT REVERSIBLE CAUSES (5 H 5 T PROBLEM TABLE): 61
EPINEPHRINE 10/25/2021 Nariman Sadeghi Epinephrine (1 mg intravenous push) should be given as soon as intravenous access is established and repeated every three to five minutes thereafter until return of spontaneous circulation is achieved. There is no evidence to support the routine use of vasopressin for PEA. 62
SODIUM BICARBONATE Nariman Sadeghi bicarbonate (1 meq/kg) has a role in the treatment of PEA due to specific causes: preexisting hyperkalemia preexisting bicarbonate-responsive acidosis treatment of tricyclic antidepressant overdose alkalinize the urine in aspirin or other drug overdoses. 10/25/2021 Sodium 63
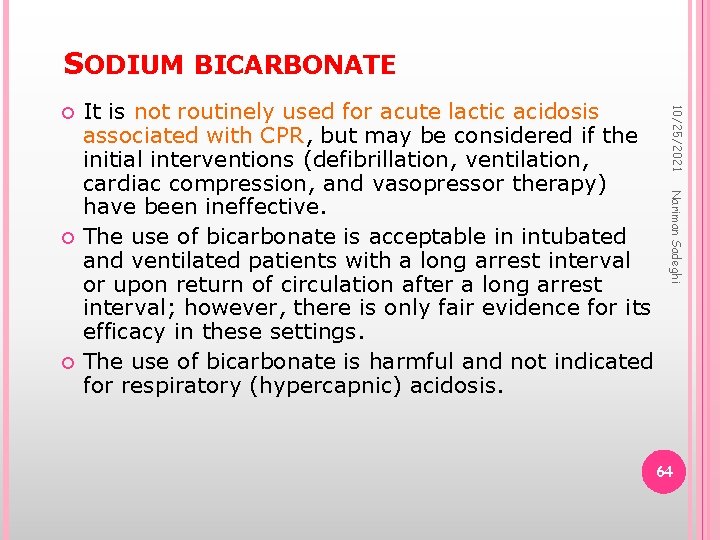
SODIUM BICARBONATE Nariman Sadeghi It is not routinely used for acute lactic acidosis associated with CPR, but may be considered if the initial interventions (defibrillation, ventilation, cardiac compression, and vasopressor therapy) have been ineffective. The use of bicarbonate is acceptable in intubated and ventilated patients with a long arrest interval or upon return of circulation after a long arrest interval; however, there is only fair evidence for its efficacy in these settings. The use of bicarbonate is harmful and not indicated for respiratory (hypercapnic) acidosis. 10/25/2021 64
ATROPINE Nariman Sadeghi The adaministration of atropine (1 mg every three to five minutes) is possibly helpful for PEA when the rate is slow (ie, absolute bradycardia with a rate <60 beats/min, or a heart rate less than expected relative to the underlying condition). 10/25/2021 65
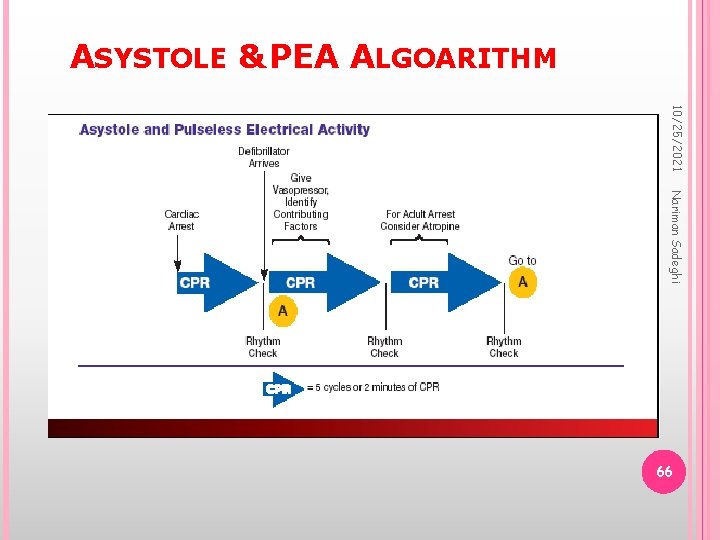
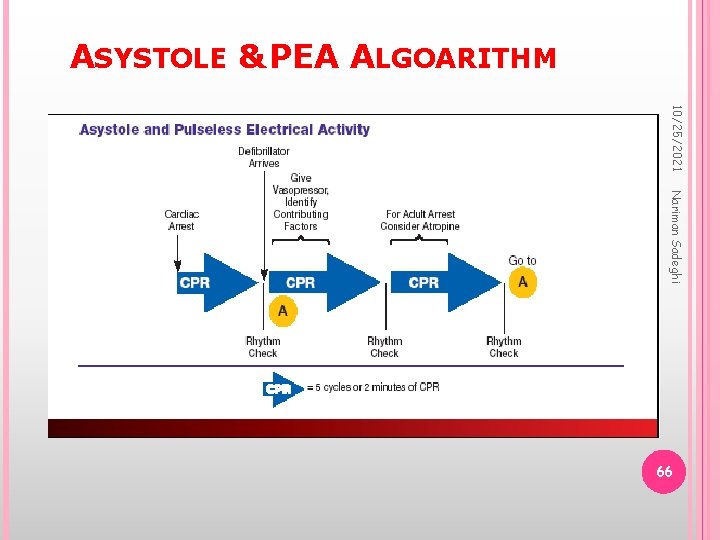
ASYSTOLE & PEA ALGOARITHM 10/25/2021 Nariman Sadeghi 66
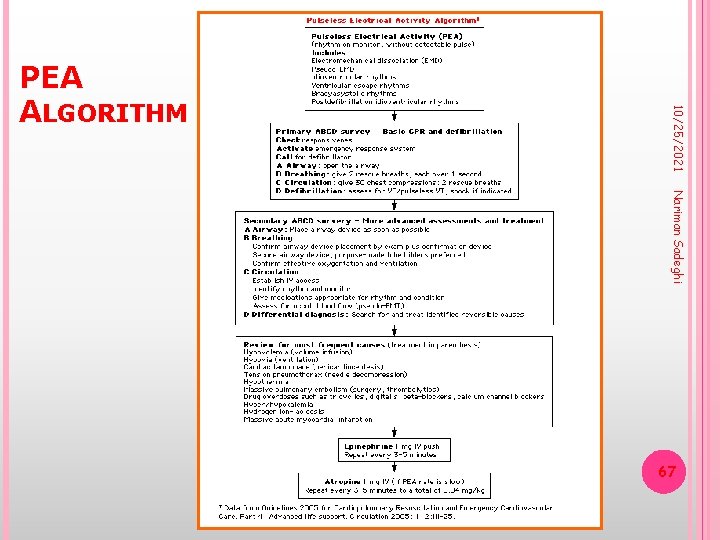
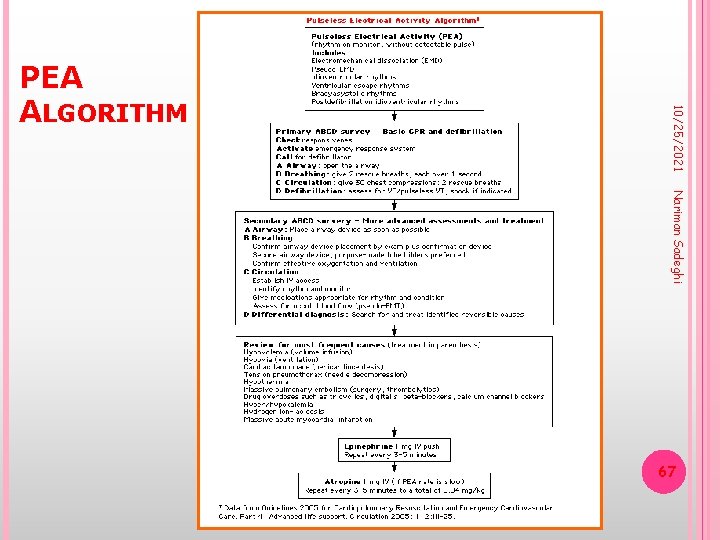
10/25/2021 PEA ALGORITHM Nariman Sadeghi 67
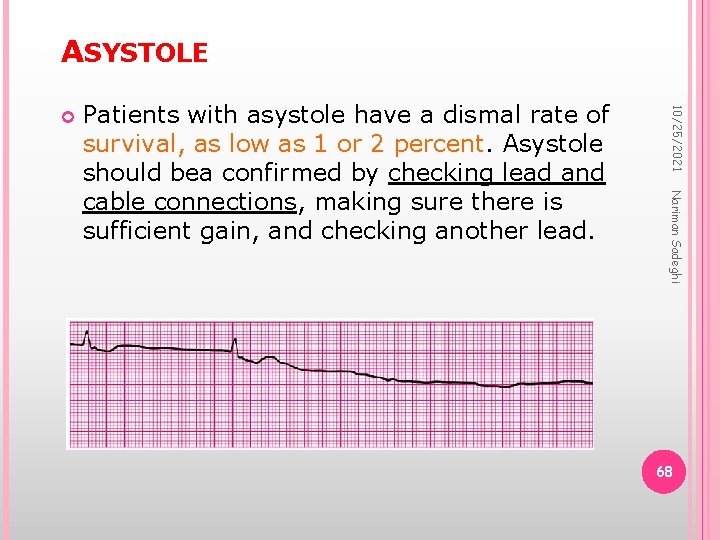
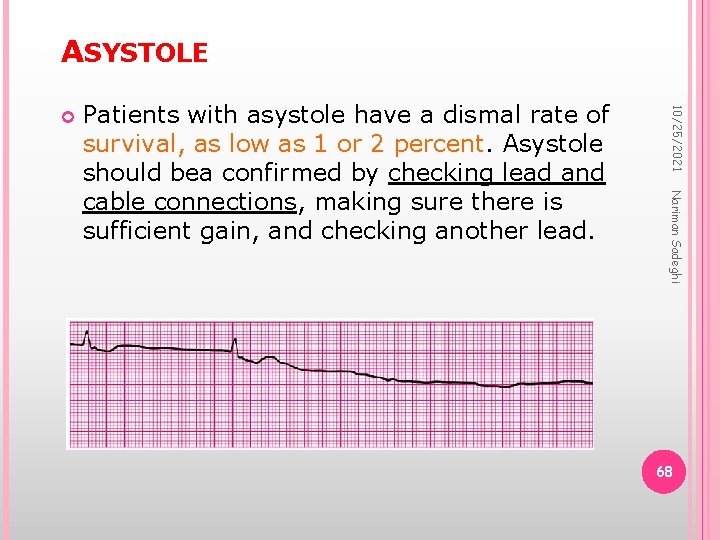
ASYSTOLE Nariman Sadeghi Patients with asystole have a dismal rate of survival, as low as 1 or 2 percent. Asystole should bea confirmed by checking lead and cable connections, making sure there is sufficient gain, and checking another lead. 10/25/2021 68
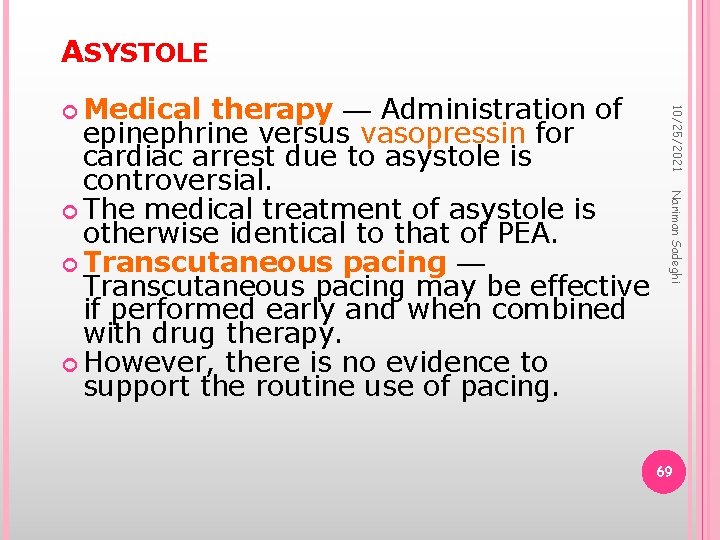
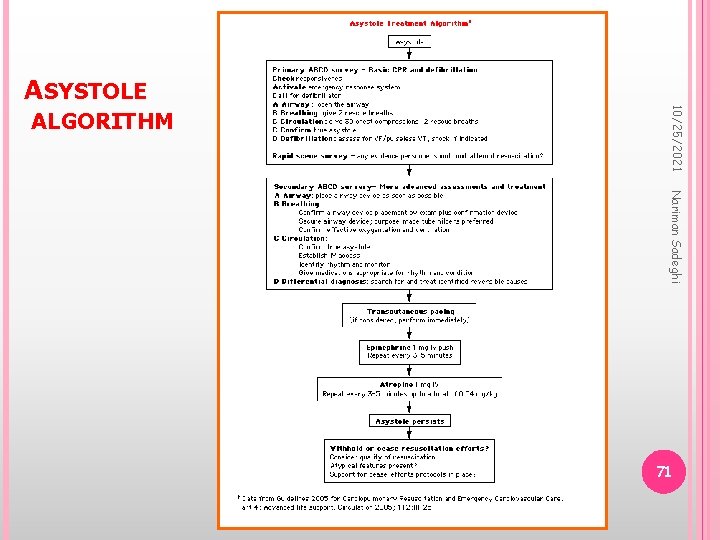
ASYSTOLE Nariman Sadeghi therapy — Administration of epinephrine versus vasopressin for cardiac arrest due to asystole is controversial. The medical treatment of asystole is otherwise identical to that of PEA. Transcutaneous pacing — Transcutaneous pacing may be effective if performed early and when combined with drug therapy. However, there is no evidence to support the routine use of pacing. 10/25/2021 Medical 69
PERSISTENT ASYSTOLE 10/25/2021 Nariman Sadeghi Was tracheal intubation performed? Was effective ventilation achieved? Was VF, if present, adequately shocked? Was intravenous access obtained? Were intravenous epinephrine and atropine given? Was a reversible cause ruled out or corrected, if identified? Was asystole continuously documented for more than 5 to 10 minutes after all of the above were accomplished? 70
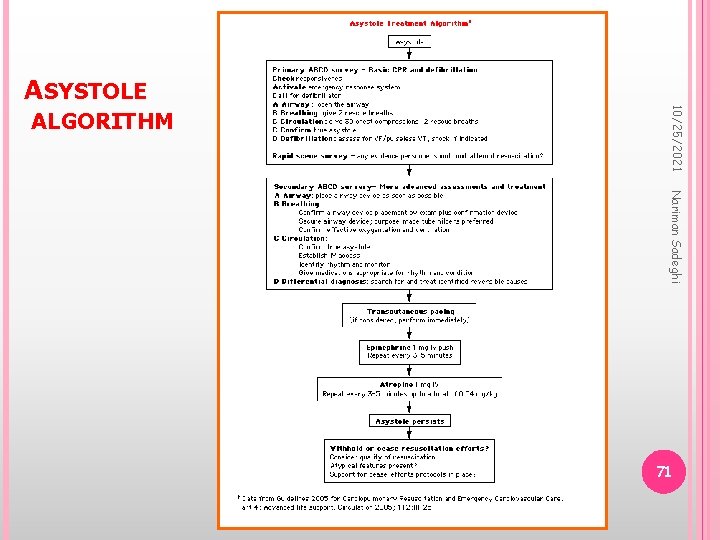
ASYSTOLE 10/25/2021 ALGORITHM Nariman Sadeghi 71
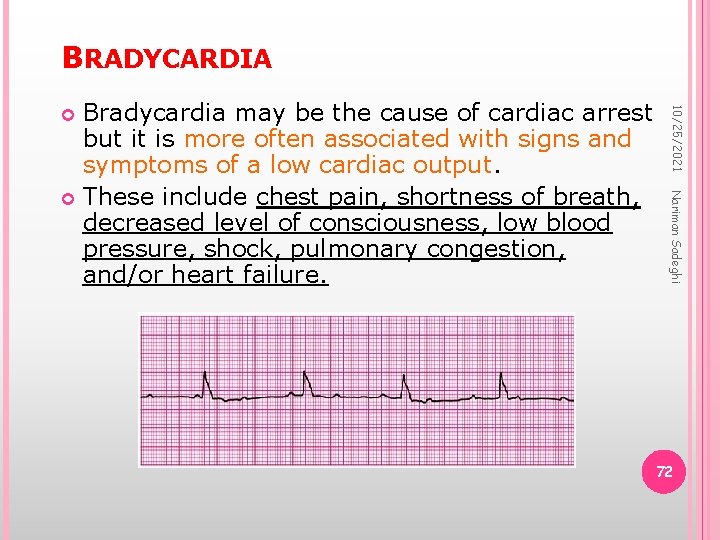
BRADYCARDIA 10/25/2021 Nariman Sadeghi Bradycardia may be the cause of cardiac arrest but it is more often associated with signs and symptoms of a low cardiac output. These include chest pain, shortness of breath, decreased level of consciousness, low blood pressure, shock, pulmonary congestion, and/or heart failure. 72
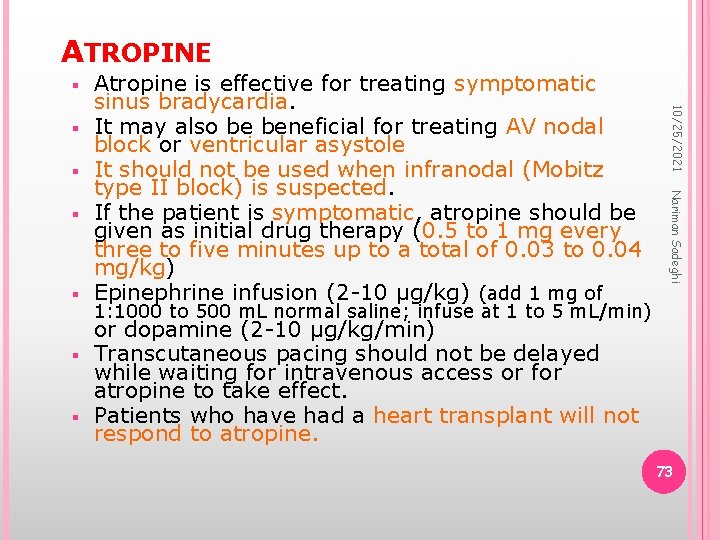
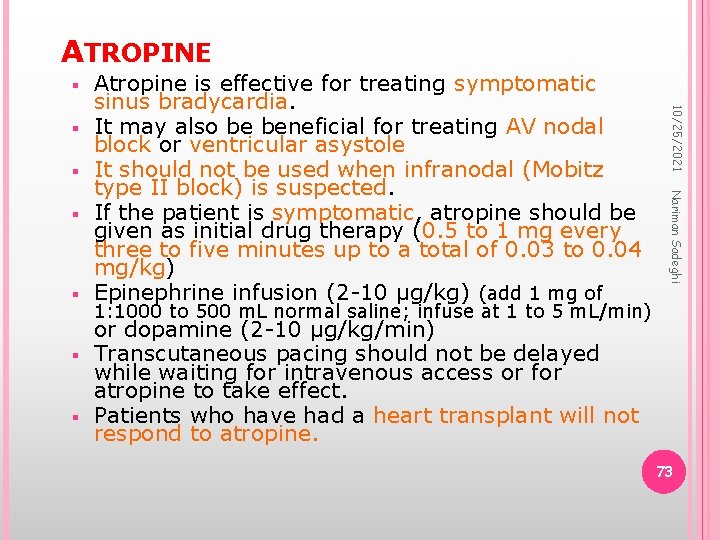
ATROPINE Nariman Sadeghi 10/25/2021 Atropine is effective for treating symptomatic sinus bradycardia. It may also be beneficial for treating AV nodal block or ventricular asystole It should not be used when infranodal (Mobitz type II block) is suspected. If the patient is symptomatic, atropine should be given as initial drug therapy (0. 5 to 1 mg every three to five minutes up to a total of 0. 03 to 0. 04 mg/kg) Epinephrine infusion (2 -10 µg/kg) (add 1 mg of 1: 1000 to 500 m. L normal saline; infuse at 1 to 5 m. L/min) or dopamine (2 -10 µg/kg/min) Transcutaneous pacing should not be delayed while waiting for intravenous access or for atropine to take effect. Patients who have had a heart transplant will not respond to atropine. 73
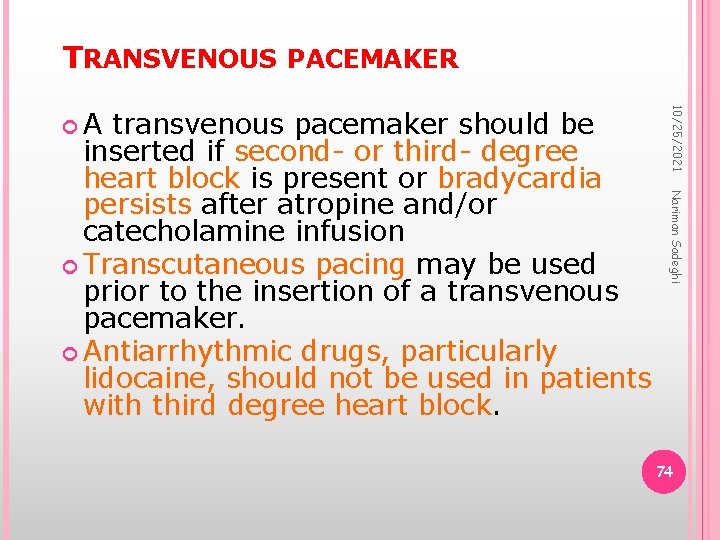
TRANSVENOUS PACEMAKER Nariman Sadeghi transvenous pacemaker should be inserted if second- or third- degree heart block is present or bradycardia persists after atropine and/or catecholamine infusion Transcutaneous pacing may be used prior to the insertion of a transvenous pacemaker. Antiarrhythmic drugs, particularly lidocaine, should not be used in patients with third degree heart block. 10/25/2021 A 74
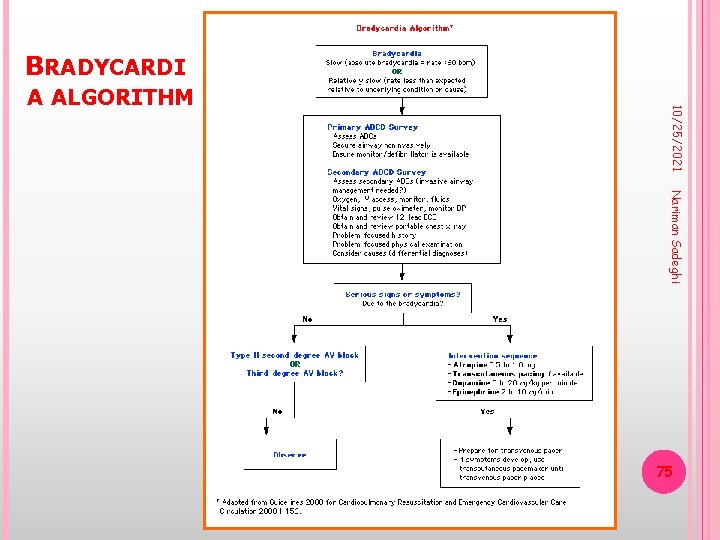
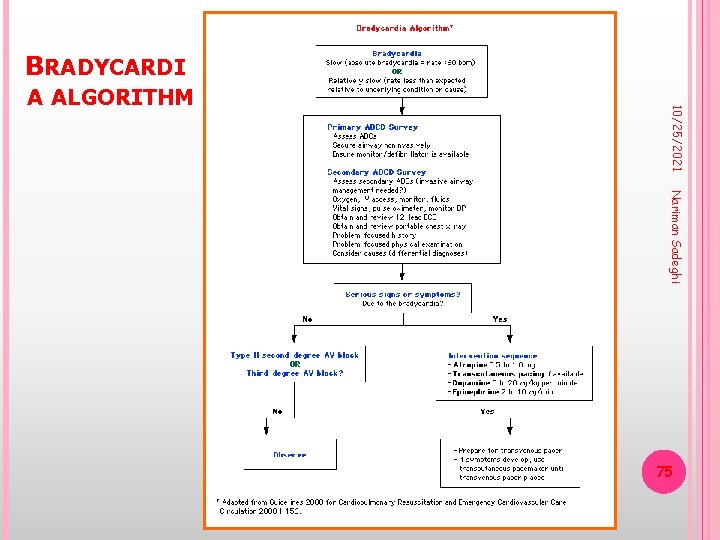
BRADYCARDI 10/25/2021 A ALGORITHM Nariman Sadeghi 75
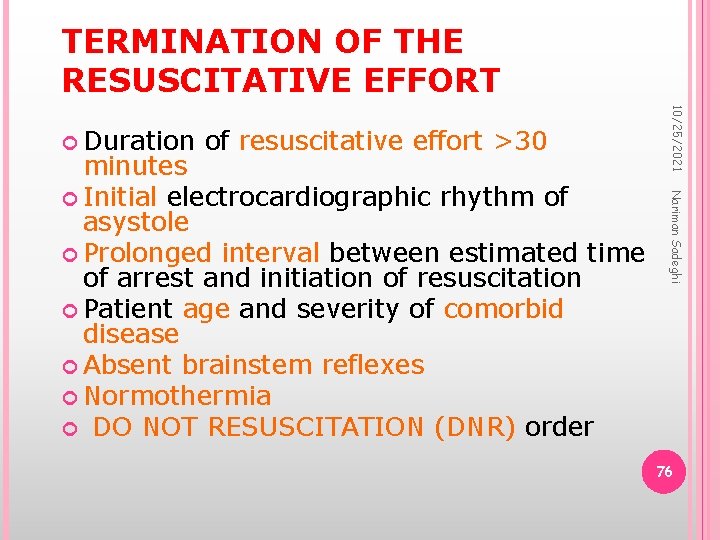
TERMINATION OF THE RESUSCITATIVE EFFORT of resuscitative effort >30 Nariman Sadeghi minutes Initial electrocardiographic rhythm of asystole Prolonged interval between estimated time of arrest and initiation of resuscitation Patient age and severity of comorbid disease Absent brainstem reflexes Normothermia DO NOT RESUSCITATION (DNR) order 10/25/2021 Duration 76
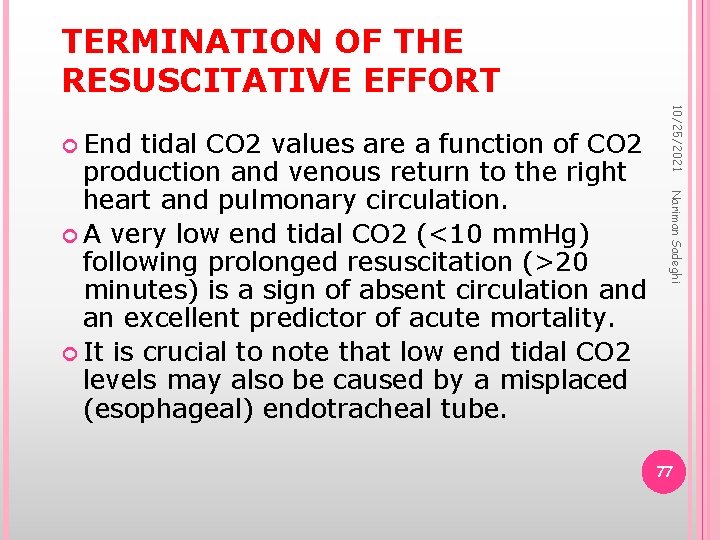
TERMINATION OF THE RESUSCITATIVE EFFORT Nariman Sadeghi tidal CO 2 values are a function of CO 2 production and venous return to the right heart and pulmonary circulation. A very low end tidal CO 2 (<10 mm. Hg) following prolonged resuscitation (>20 minutes) is a sign of absent circulation and an excellent predictor of acute mortality. It is crucial to note that low end tidal CO 2 levels may also be caused by a misplaced (esophageal) endotracheal tube. 10/25/2021 End 77
10/25/2021 Nariman Sadeghi 81
Nariman Sadeghi In ACLS the best fluid to resuscitate patient is Normal Saline. According to Patient: use 20 ml/kg or 250 ml stat if patient has no sign of CHF First of all, IV line must be determined. The best size is the large one. 10/25/2021 F: FLUID THERAPY 82
Nariman Sadeghi Be aware of Hypoglycemia. Use 50% DW if needed. 0/5 to 2 mg of glucose should be administrated in Pt with low glucose level. Recheck Pt BS after infusion glucose. Try to maintain PT BS about 100 mg/dl. 10/25/2021 G: GLUECOMETERY 84
Nariman Sadeghi According to PT, Hypothermia or Hyperthermia must be used. Position of PT Use of special ventilation mood ABG or VBG Check for Acidosis or Alkalosis Use of special drugs C-X ray Reassess PT Recheck IV line Use Antiarrhythmia which was used in CPR 10/25/2021 H: HUMAN LIFE SAVING EFFORT 85
Nariman Sadeghi After CPR: all the patients must be transferred to ICU for special purpose. Tracheal intubation must be remain for at least 24 h. Check peripheral pulse. Check for better ventilation. Pt must be NPO. Insert NGT and Foley cat. Check I. O. H. M at least for 24 h. 10/25/2021 I: INTENSIVE CARE 86
10/25/2021 Nariman Sadeghi THANK YOU FOR YOUR ATTENTION. 87 ANY QUESTIONS?