Haemostasis dr Sri Lestari Sulistyo Rini MSc Five













- Slides: 56
Haemostasis dr Sri Lestari Sulistyo Rini, MSc
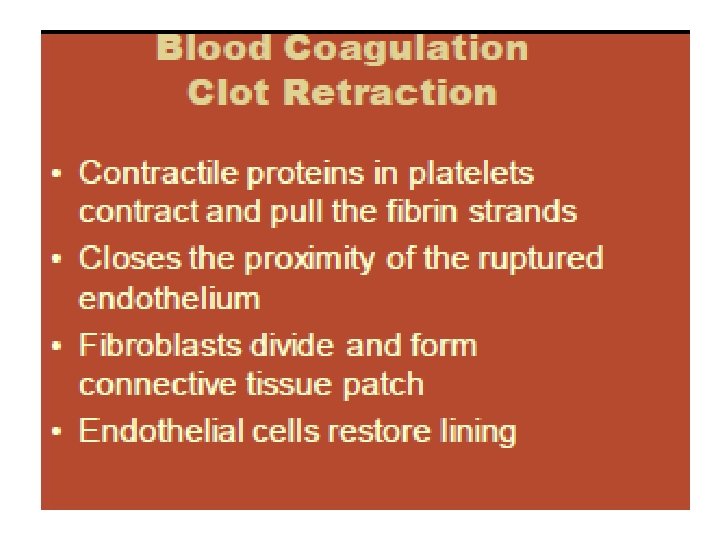
Five Stages of Hemostasis 1. Vessel spasm 2. Formation of the platelet plug 3. Blood coagulation or development of an insoluble fibrin clot 4. Clot retraction 5. Clot dissolution
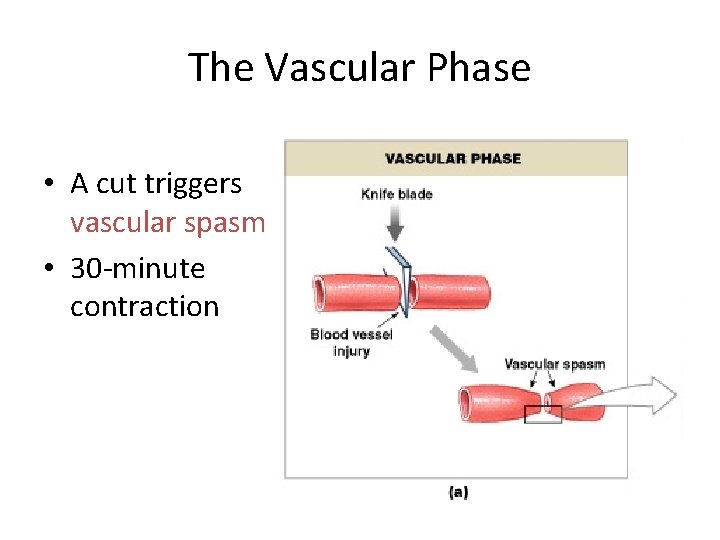
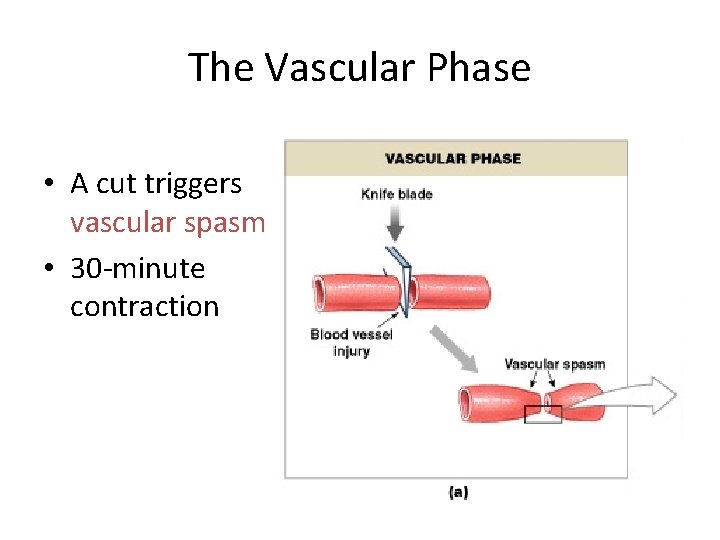
The Vascular Phase • A cut triggers vascular spasm • 30 -minute contraction Figure 19– 11 a
3 Steps of the Vascular Phase 1. Endothelial cells contract: – expose basal lamina to bloodstream 2. Endothelial cells release: – chemical factors: ADP, tissue factor, prostacyclin – local hormones: endothelins – stimulate smooth muscle contraction and cell division 3. Endothelial cell membranes become “sticky”: – seal off blood flow

Functions of Thrombin • Stimulates formation of tissue factor – stimulates release of PF-3: – forms positive feedback loop (intrinsic and extrinsic): • accelerates clotting
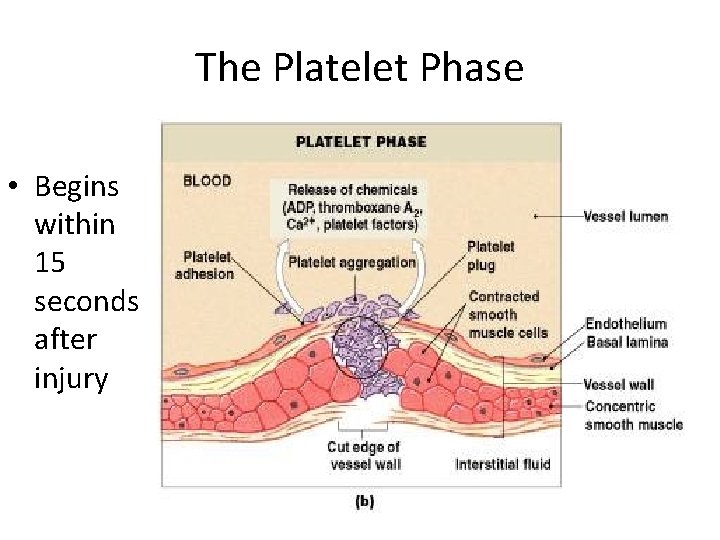
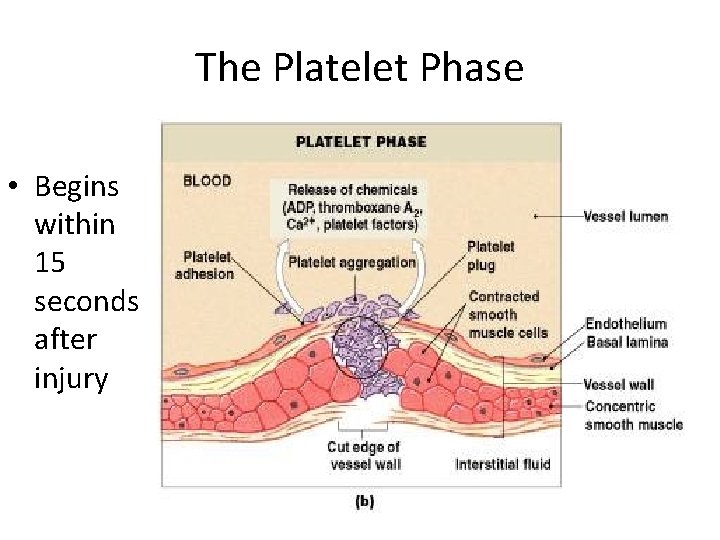
The Platelet Phase • Begins within 15 seconds after injury Figure 19– 11 b
Platelets • • Small fragments of megakaryocytes Formation is regulated by thrombopoietin Blue-staining outer region, purple granules Granules contain serotonin, Ca 2+, enzymes, ADP, and platelet-derived growth factor (PDGF)
Roles of Vessel Endothelial Cells in Physiological Hemostasis Roles are close related to its endocrine functions ①Vessel endothelium serves as barrier between underendothelial structure (namely, collagen) and blood. As soon as collagen expose to blood, hemostasis of platelet is immediately activated to form thrombus blocking wounded vessels.
②Platelet activation can releases constrictive factors (TXA 2, ET-1, 5 -HT, etc) making vessel convulsion, lasting about 60 sec. ③Stimulated vessel endothelial cells release coagulative factors and Promoting coagulative material to realize, speed up blood coagulation. At the same time, cells also release anticoagulative factors and fibrinolysis material to modify blood coagulation.
Endocrine functions of vessel endothelial cells ① Material related to hemostasis are basal membrane, collagen (III, IV), microfibril, elastin, laminin, ectonectin, fibronectin, von Willebrand factor (v. WF), protein enzyme inhibitor, adhesive amylose, etc. ② Anticoagulative material: They are prostacyclin (PGI 2), endothelium-derived relaxing factor (EDRF or nitric oxide, NO), tissue-type plasminogen activator (t. PA), u. PA, ADPase, ATIII, heparin sulfate, protein C, thrombomomodulin (TM), plasminogen activator (PA).

Endocrine functions of vessel endothelial cells ③Promoting coagulative material: Tissue factor, v. WF, blood clotting factor V, plasminogen activator inhibitor (PAI-1, PAI-2, ATIII), TNFα, interleukin-1 (IL-1). ④Vessel constricting and relaxing modulators: endothelin-1 (ET-1), EDRF (NO), PGI 2, etc.

Platelet • Normal value: 100× 109 ~ 300× 109, range from 6%~10% • Normal changes: more number in the afternoon than in the morning, more in winter than in spring, more in the venous blood than capillary, after sport↑, pregnacy↑.

Life- Span and Breakage of Platelet • Life-span: Averagely, 7~14 days in the blood. It can be consumed when it displays physiological functions. • Breakage: Aged platelet can be processed by phagocytosis in liver, spleen and lymphatic node.
Function of Platelet • Functions: 1. It maintains capillary endothelial cells smooth and integrated (repairing endothelium and providing nutrition). 2. It is involved in physiological hemostasis. • Platelet and clinic relation: decrease of platelet, abnormal immune reaction, will results in hemorrhage or bleeding, purpuric symptom.
Platelets • Form a temporary platelet plug that helps seal breaks in blood vessels • Circulating platelets are kept inactive and mobile by NO and prostacyclin from endothelial cells of blood vessels
Physiological Characteristics of Platelet • Thrombocyte adhesion: its membrane glycoprotein (GP, GPIb/IX and GPIIa/IIIb), collagen (underendothelial structure), v. WF (plasma component), fibrinogen are involved in adhesion. Mechanism: Exposed collagen + v. WF → v. WF changes → platelet membrane glycoprotein + changed v. WF → Thrombocyte adhesion.
• Thrombocyte aggregation: induced by physiological factors such as ADP, thromboxane A 2 (TXA 2), epinephrine, 5 -HT, histamine, collagen, thrombin, prostacyclin, etc and by pathological factors like bacteria, virus, immune complex, drugs, etc.
The process can be separated into two phases: phase one is reversible aggregation and phase two irreversible aggregation. Two phases require Ca 2+, fibrinogen and energy consumption • Mechanism : Various factors+corresponding receptors on the platelet →changes in the second messenger within platelet →c. AMP↓, Ip 3↑, Ca 2+↑, c. GMP↑→ platelet aggregation.
• Thrombocyte release: ADP, ATP, 5 -HT, Ca 2+ released from dense body, and β-platelet globin, PF 4, v. WF, fibrinogen, PFV, PDGF, thrombin sensitive protein from α-granule, and acid protein hydrolyzed enzyme, tissue hydrolyzed enzyme from lysosome.
• Thrombocyte contraction: Loose platelet thrombus could turn into compact platelet thrombus by Ca 2+ release and cytoskeleton movement (filament/canaliculus) within platelet.
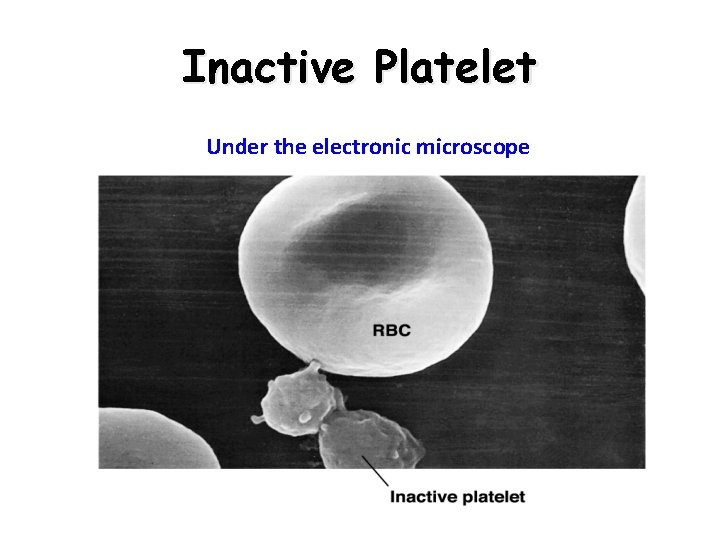
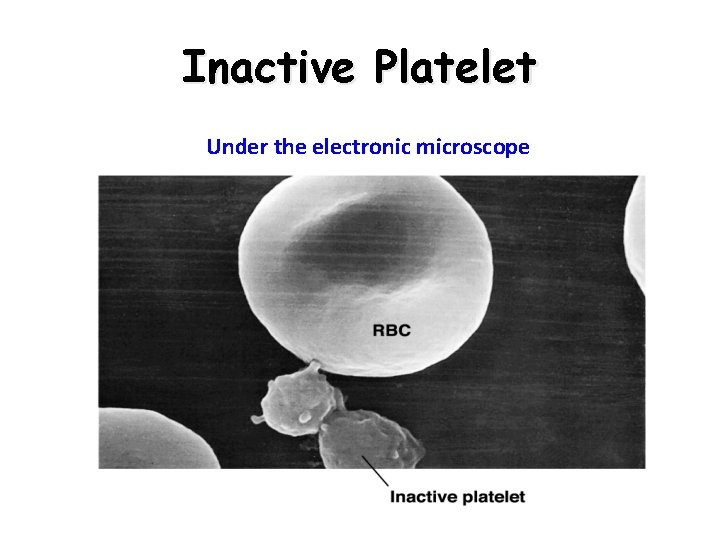
Inactive Platelet Under the electronic microscope

Activated Platelet for Hemostasis Under the electronic microscope
Roles of Platelet in Hemostasis 1. Activated platelets supply lecithoid (phospholipid) surface for blood clotting factor and involve in activating factor X and prothrombin. 2. Surface of platelet membrane combine with many blood clotting factor, such as fibrinogen, FV, FXIII to speed up coagulation.
Roles of Platelet in Hemostasis 3. Activated platelets release α-granule which contains fibrinogen to intensify fibrin forming and blood coagulation. 4. Activated platelets contract clot with its contractive protein to solidify blood coagulation.

Mechanism of Platelet in Hemostasis

Mechanism of Platelet in Hemostasis
Activated Platelets Release Clotting Compounds • • • Adenosine diphosphate (ADP) Thromboxane A 2 and serotonin Clotting factors Platelet-derived growth factor (PDGF) Calcium ions

Platelet Plug: Size Restriction • Prostacyclin: – released by endothelial cells – inhibits platelet aggregation • Inhibitory compounds: – released by other white blood cells • Circulating enzymes: break down ADP • Negative (inhibitory) feedback: from serotonin • Development of blood clot: isolates area
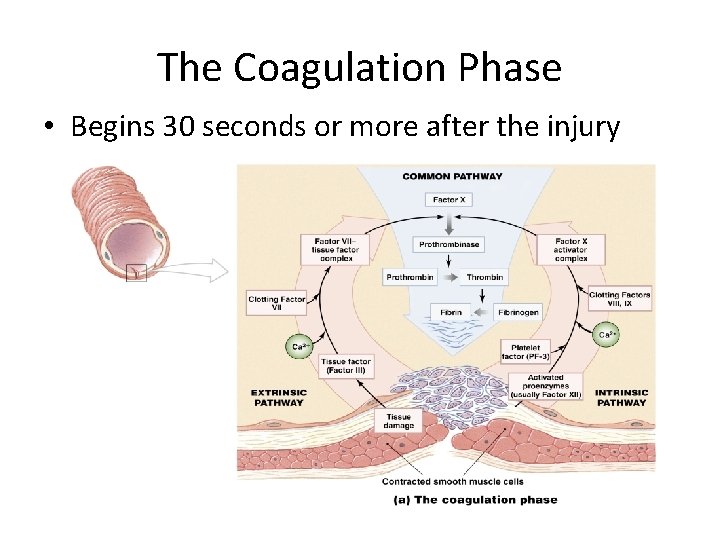
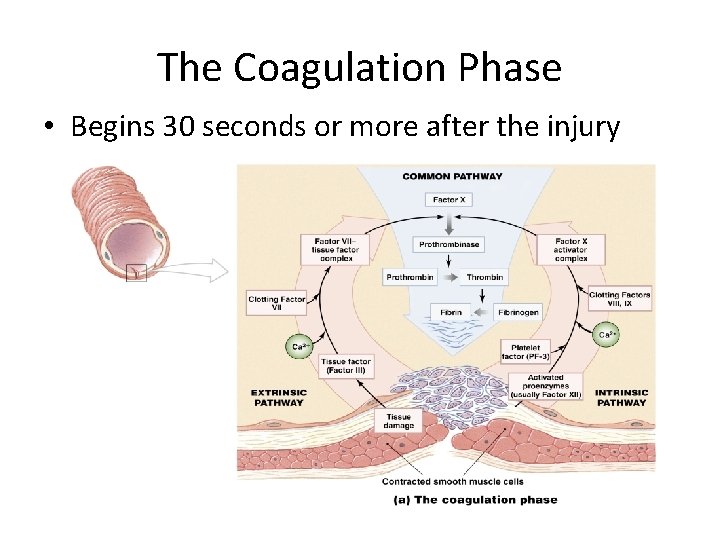
The Coagulation Phase • Begins 30 seconds or more after the injury Figure 19– 12 a


Blood Coagulation Blood Clotting Factor • Definition: The process of blood flow from flowing liquid to gel or gelatin. • Serum: Light yellow fluid after blood coagulation. • Difference between serum and plasma mainly consists in no fibrinogen in serum. • Blood coagulation is a series of complicated biochemical reactions with various enzymes.
• Blood clotting factor: Material which are directly involved in blood coagulation. There are 12 factors named Roman numerals, except Ca 2+, phospholipid,other factors being protein, and except FIII (TF), others are in fresh plasma synthesized by liver with Vit. K. • Blood clotting enzymes have two type: inactive and activated type [FII, FVII, FIX, Fx, FXII, FXIII].
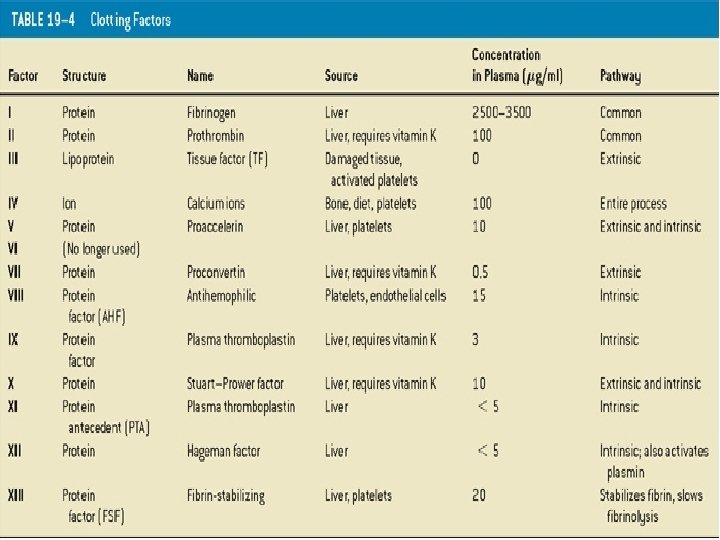
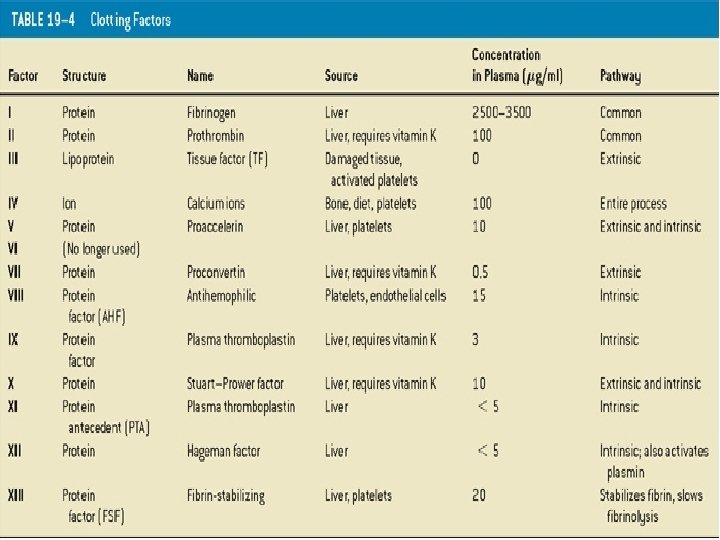
Table 19– 4
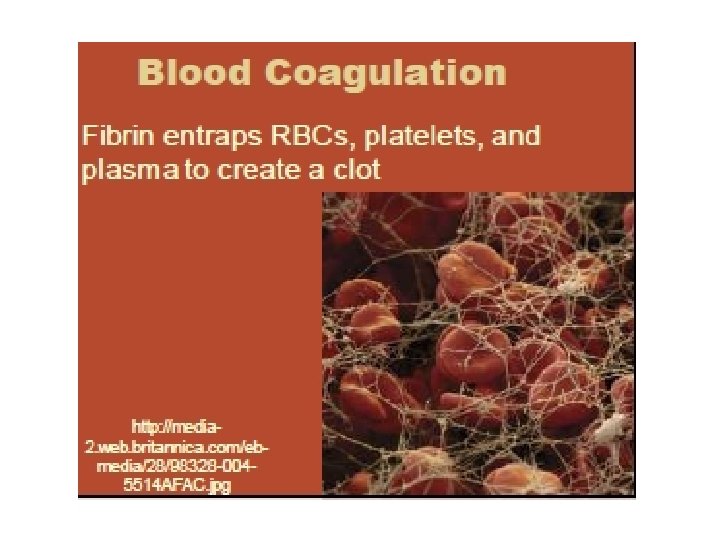
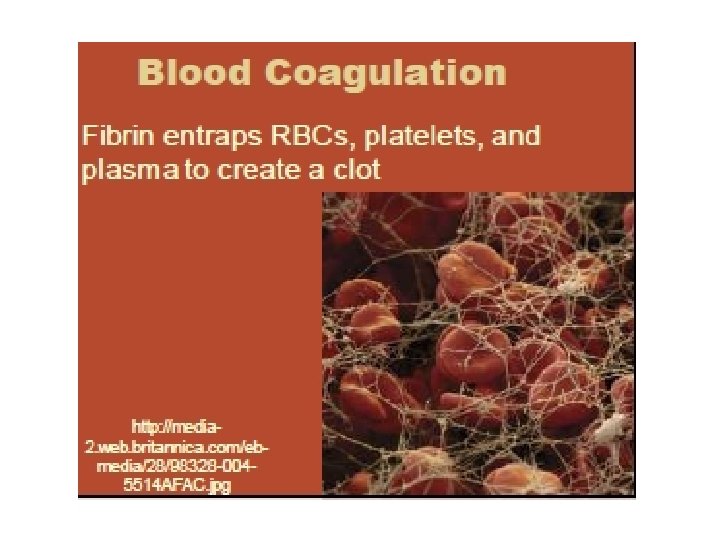
Clotting Factors • • Also called procoagulants Proteins or ions in plasma Required for normal clotting Fibrin network Covers platelet plug Traps blood cells Seals off area
Cascade Reactions • During coagulation phase • Chain reactions of enzymes and proenzymes • Form 3 pathways
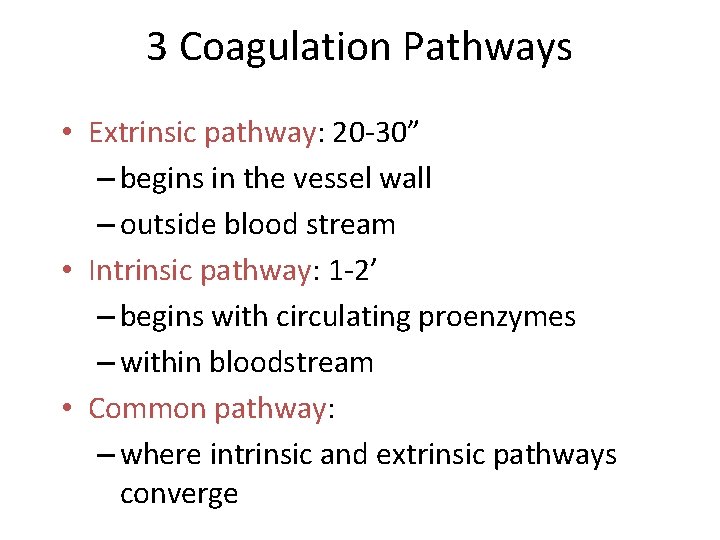
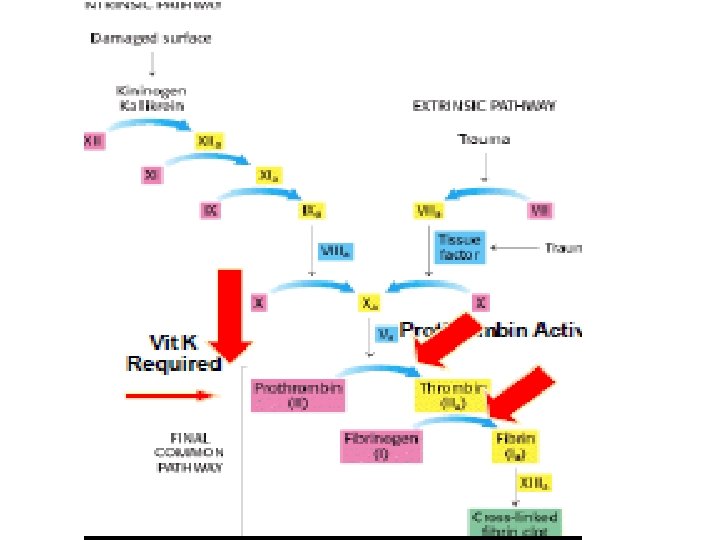
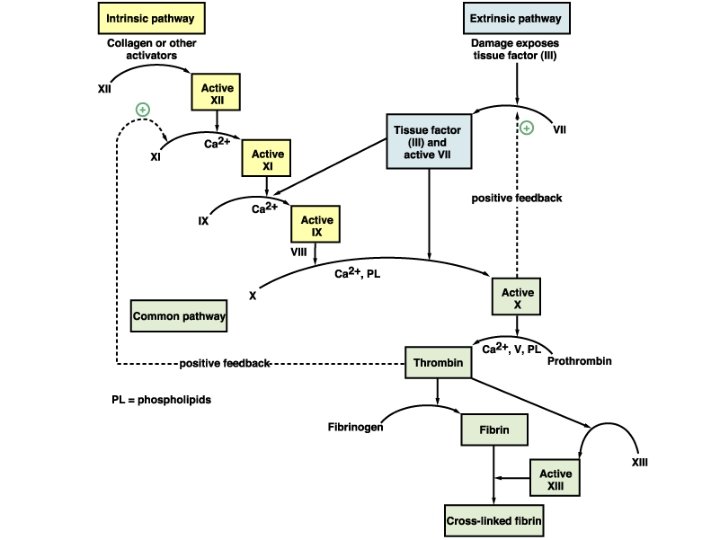
3 Coagulation Pathways • Extrinsic pathway: 20 -30” – begins in the vessel wall – outside blood stream • Intrinsic pathway: 1 -2’ – begins with circulating proenzymes – within bloodstream • Common pathway: – where intrinsic and extrinsic pathways converge
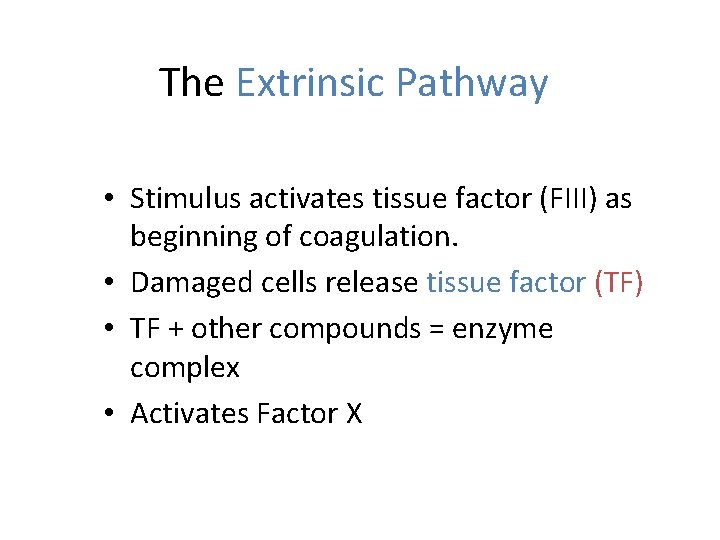
The Extrinsic Pathway • Stimulus activates tissue factor (FIII) as beginning of coagulation. • Damaged cells release tissue factor (TF) • TF + other compounds = enzyme complex • Activates Factor X
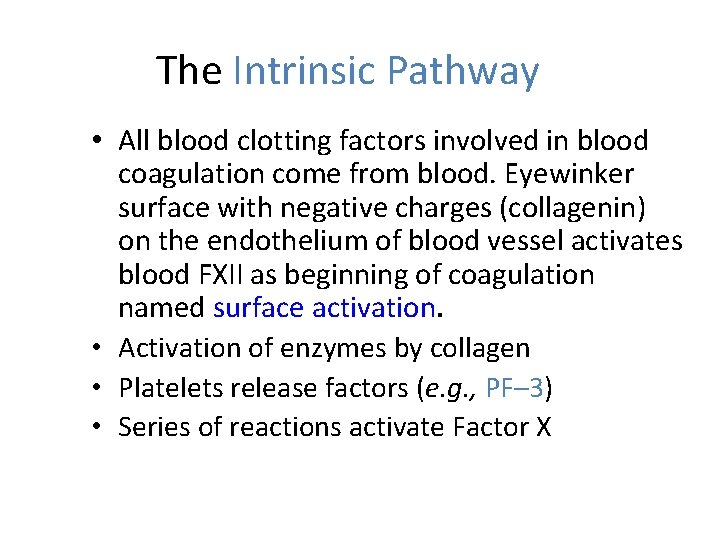
The Intrinsic Pathway • All blood clotting factors involved in blood coagulation come from blood. Eyewinker surface with negative charges (collagenin) on the endothelium of blood vessel activates blood FXII as beginning of coagulation named surface activation. • Activation of enzymes by collagen • Platelets release factors (e. g. , PF– 3) • Series of reactions activate Factor X
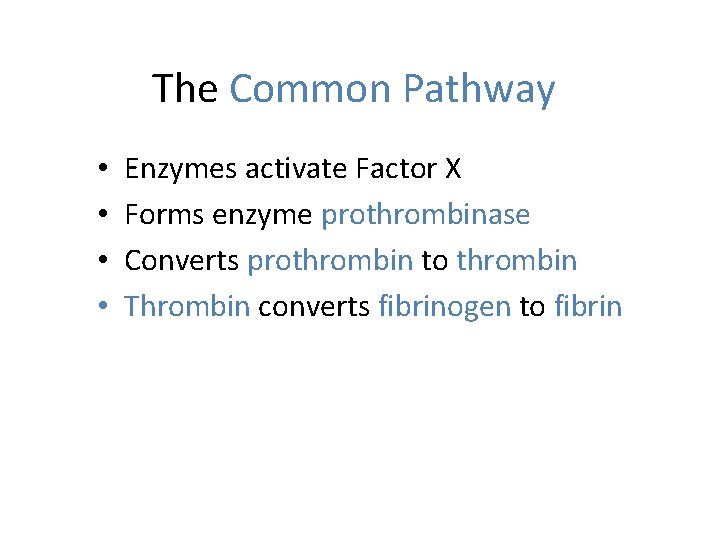
The Common Pathway • • Enzymes activate Factor X Forms enzyme prothrombinase Converts prothrombin to thrombin Thrombin converts fibrinogen to fibrin
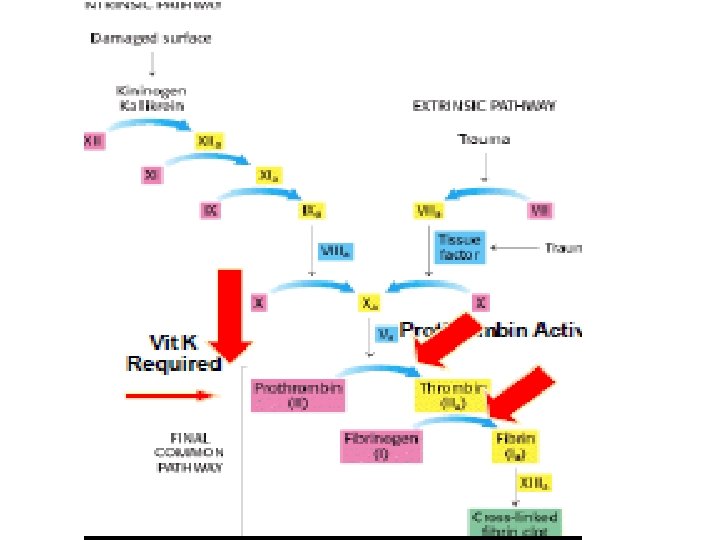
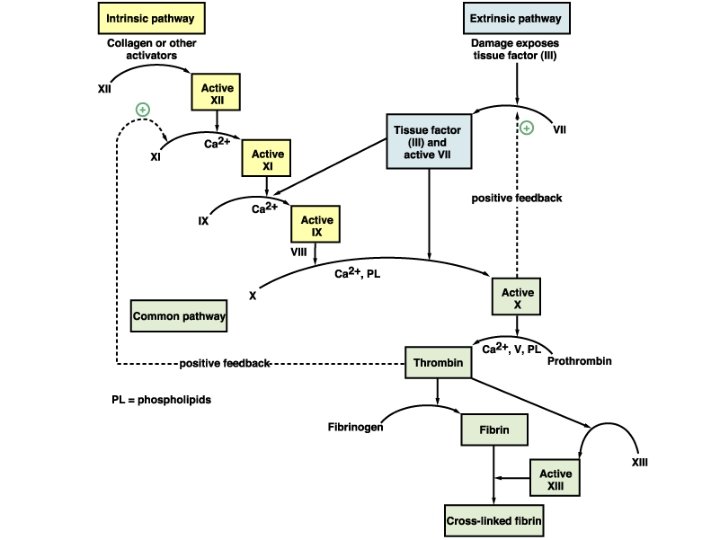
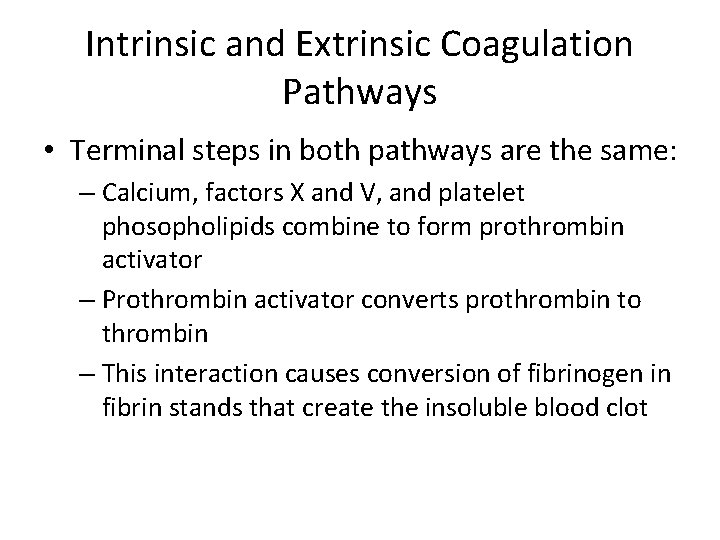
Intrinsic and Extrinsic Coagulation Pathways • Terminal steps in both pathways are the same: – Calcium, factors X and V, and platelet phosopholipids combine to form prothrombin activator – Prothrombin activator converts prothrombin to thrombin – This interaction causes conversion of fibrinogen in fibrin stands that create the insoluble blood clot
Regulation of Blood Coagulation • Antithrombin III inactivates coagulation factors and neutralizes thrombin • When antithrombin III is complexed with naturally occurring heparin, its action is accelerated and provides protection against uncontrolled thrombus formation on the endothelial surface • Protein C, a plasma protein, acts as an anticoagulant by inactivating factors V and VIII
• Humoral anticoagulative system: 1. Amino acid protease inhibitors in blood include antithrombin III, Cl-inhibitor, α 1 antitrypsin, α 2 antiplasmin, α 2 huge globin, heparin coenzyme II, protease nexin-1 (PN-1) to combine with FIXa, FXIa, FXIIa and thrombin and then inactivate them for anticoagulation. Heparin can intensify functions of antithrombin III.

2. Protein C system are protein C (PC), thrombomodulin (TM), protein S and Protein C inhibitors. Main functions of PC consist in ①It inactivates FVa, FVIIIa with phospholipid and Ca 2+; ②It blocks FXa combining with platelet phospholipid membrane to reduce prothrombin activation; ③It stimulates plasminogen activators release to trigger fibrinolysis; ④ Protein S is a coenzyme of PC and greatly intensify functions of PC.
3. Tissue factor pathway inhibitor (TFPI) mainly coming from vessel endothelial cells inhibits FXa and inactivates FVIIa-TF complex to block extrinsic pathway of coagulation with negative feed back. 4. Heparin used in the clinic widely is due to ①It combines with antithrombin III to increase functions of antithrombin III; ②It stimulates vessel endothelial cell greatlu releasing TFPI and other anticoagulative material; ③It intensifies PC activation and stimulates vessel endothelial cell releasing plasminogen activators to increase fibrinolysis. [lower molecular weight heparin is less hemorrhage]

Clotting: Area Restriction 1. Anticoagulants (plasma proteins): – antithrombin-III – alpha-2 -macroglobulin 2. Heparin” is a natural anticoagulant made by basophils & mast cells (activates Antithrombin III) 3. Protein C (activated by thrombomodulin) 4. Prostacyclin
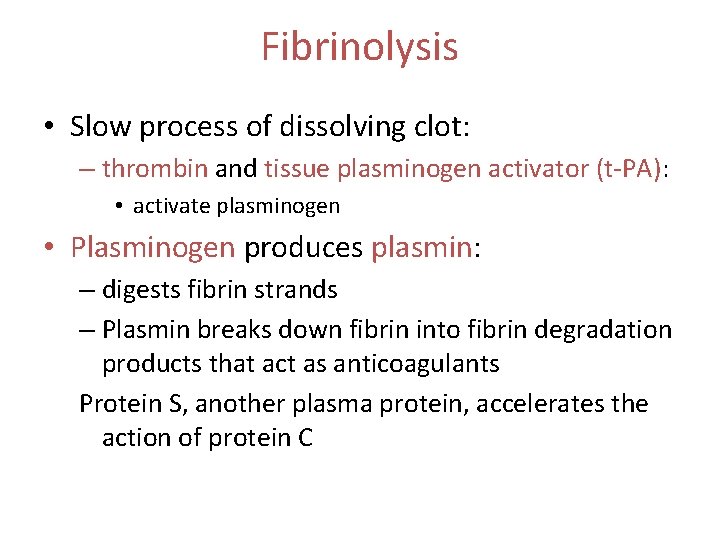
Fibrinolysis • Slow process of dissolving clot: – thrombin and tissue plasminogen activator (t-PA): • activate plasminogen • Plasminogen produces plasmin: – digests fibrin strands – Plasmin breaks down fibrin into fibrin degradation products that act as anticoagulants Protein S, another plasma protein, accelerates the action of protein C
• Two fibrinolytic systems: cellular one and plasma one. The former is leucocyte, macrophage, endothelial cell, mesothelial cell and platelet to engulf and digest fibrin. The latter is plasminogen activators (PA) and its inhibitors (PAI), plasminogen, plasmin.
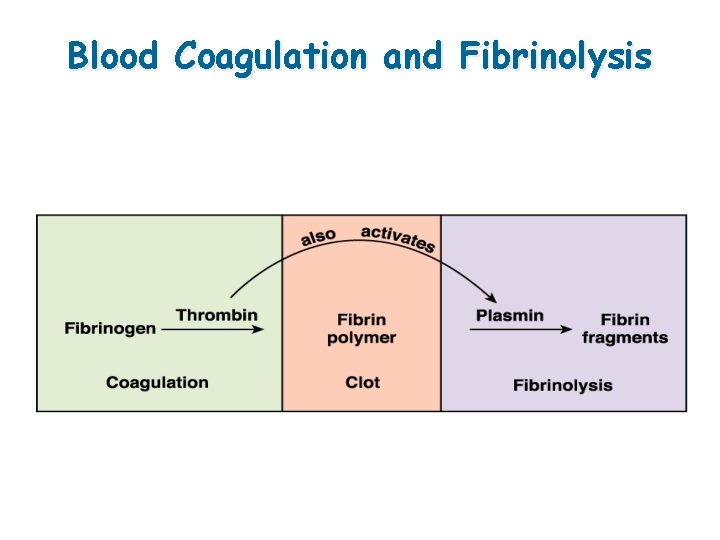
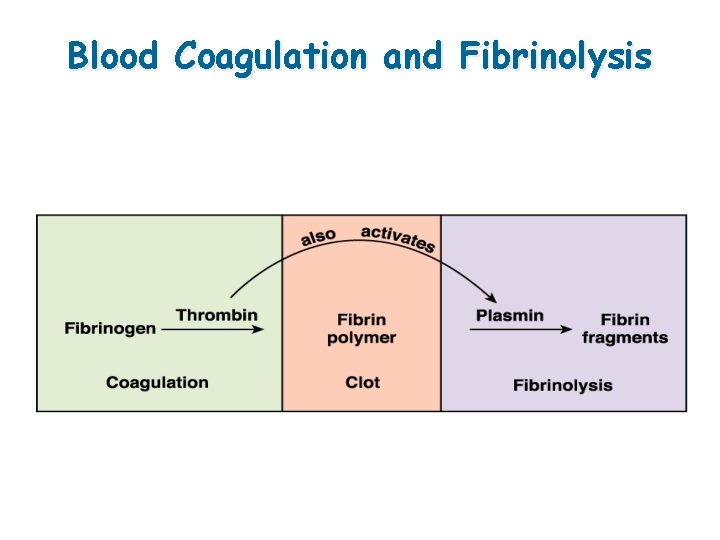
Blood Coagulation and Fibrinolysis
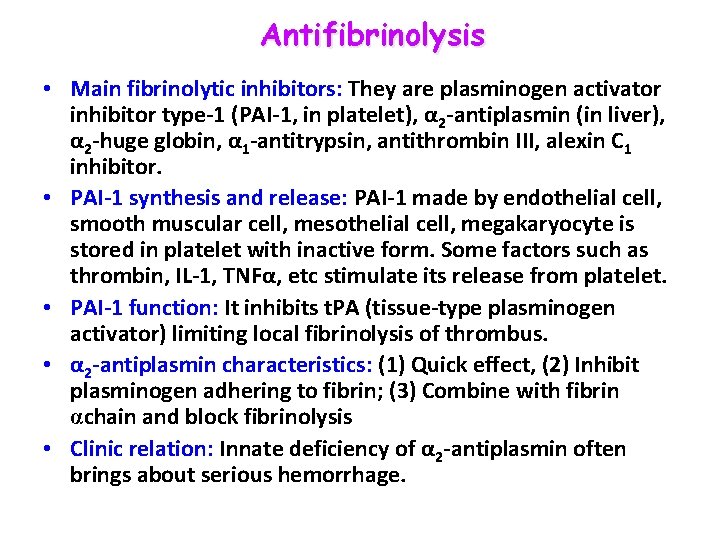
Antifibrinolysis • Main fibrinolytic inhibitors: They are plasminogen activator inhibitor type-1 (PAI-1, in platelet), α 2 -antiplasmin (in liver), α 2 -huge globin, α 1 -antitrypsin, antithrombin III, alexin C 1 inhibitor. • PAI-1 synthesis and release: PAI-1 made by endothelial cell, smooth muscular cell, mesothelial cell, megakaryocyte is stored in platelet with inactive form. Some factors such as thrombin, IL-1, TNFα, etc stimulate its release from platelet. • PAI-1 function: It inhibits t. PA (tissue-type plasminogen activator) limiting local fibrinolysis of thrombus. • α 2 -antiplasmin characteristics: (1) Quick effect, (2) Inhibit plasminogen adhering to fibrin; (3) Combine with fibrin αchain and block fibrinolysis • Clinic relation: Innate deficiency of α 2 -antiplasmin often brings about serious hemorrhage.

TERIMA KASIH
 Sri rama sri rama sri manoharama
Sri rama sri rama sri manoharama Promegakaryocyte
Promegakaryocyte Msc rini iii
Msc rini iii Laporan pkl di desa
Laporan pkl di desa The ivy method
The ivy method Clotting factors
Clotting factors Pt strawberindo lestari
Pt strawberindo lestari Pt asia pratama walindo
Pt asia pratama walindo Drg dwi imbang lestari
Drg dwi imbang lestari Pamuji lestari
Pamuji lestari Pt. indobamboo lestari
Pt. indobamboo lestari Amanah lestari alam
Amanah lestari alam Desi lestari
Desi lestari Dina ayu lestari
Dina ayu lestari Neurospora crassa dimanfaatkan dalam pembuatan
Neurospora crassa dimanfaatkan dalam pembuatan Dina lestari enterprise
Dina lestari enterprise Periklinal adalah
Periklinal adalah Desi lestari
Desi lestari Drg dwi imbang lestari
Drg dwi imbang lestari Praktek dr eka agustia rini
Praktek dr eka agustia rini Rini juni astuti
Rini juni astuti Dr eka agustia rini
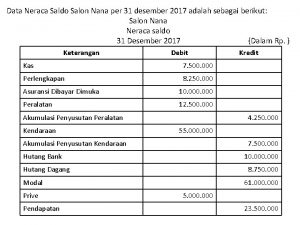
Dr eka agustia rini Kertas kerja usaha salon berdikari per 31 desember 2017
Kertas kerja usaha salon berdikari per 31 desember 2017 Osuksin
Osuksin Rini ratan
Rini ratan Rini nulis karangan
Rini nulis karangan Dr eka agustia rini
Dr eka agustia rini Rini nulis karangan
Rini nulis karangan 5 elements and 5 senses
5 elements and 5 senses These beauteous forms
These beauteous forms Macbeth act five scene five
Macbeth act five scene five One in five challenge
One in five challenge Msc agriculture
Msc agriculture Msc olga
Msc olga 2vision msc
2vision msc Amu msc
Amu msc Humánkineziológia msc
Humánkineziológia msc Msc marianna
Msc marianna Jma msc
Jma msc Tpc.msc
Tpc.msc Nsozvn
Nsozvn Msc ida ii
Msc ida ii Msc credit rating
Msc credit rating Msc nerissa current position
Msc nerissa current position Imo 645
Imo 645 Msc eir
Msc eir Msc i
Msc i Grenoble msc finance
Grenoble msc finance Msc gsm
Msc gsm Msc
Msc Msc direccionamiento
Msc direccionamiento Msc que significa
Msc que significa Ship construction file
Ship construction file Light refractive
Light refractive 7 aplikasi perdana msc
7 aplikasi perdana msc Msc joanna droga
Msc joanna droga Hapag qq
Hapag qq