Management Conference Young girl with RUQ mass and






















- Slides: 60

Management Conference Young girl with RUQ mass and pain Raika Jamali MD Digestive Disease Research Center Tehran University of Medical Sciences
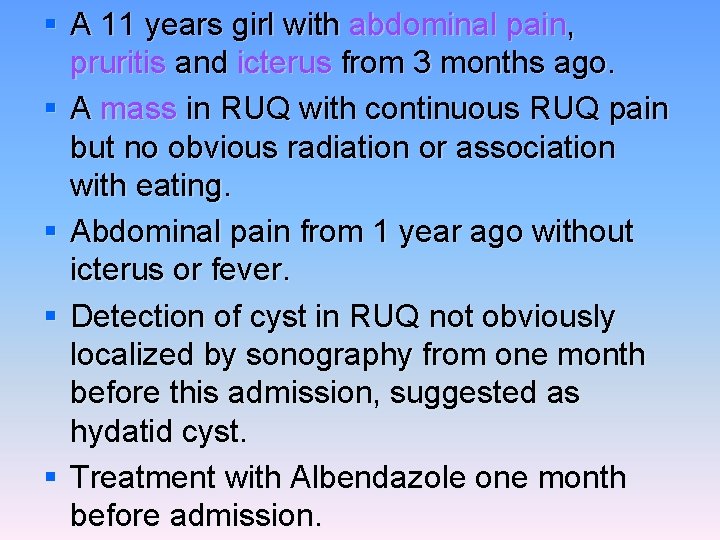
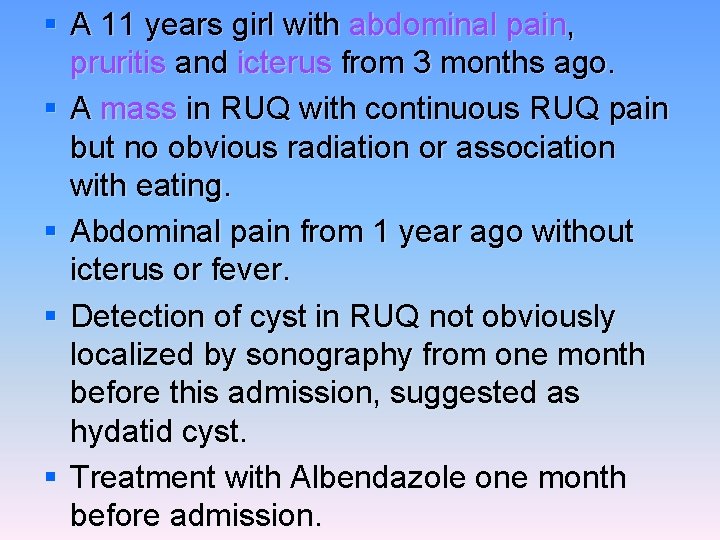
§ A 11 years girl with abdominal pain, pruritis and icterus from 3 months ago. § A mass in RUQ with continuous RUQ pain but no obvious radiation or association with eating. § Abdominal pain from 1 year ago without icterus or fever. § Detection of cyst in RUQ not obviously localized by sonography from one month before this admission, suggested as hydatid cyst. § Treatment with Albendazole one month before admission.
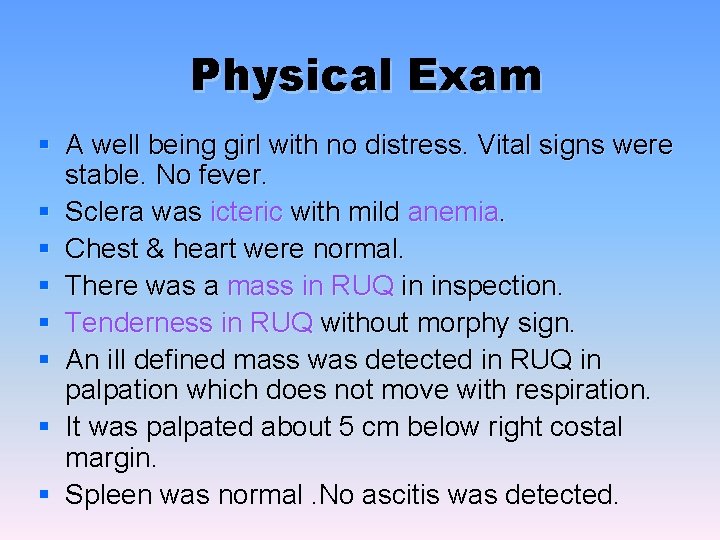
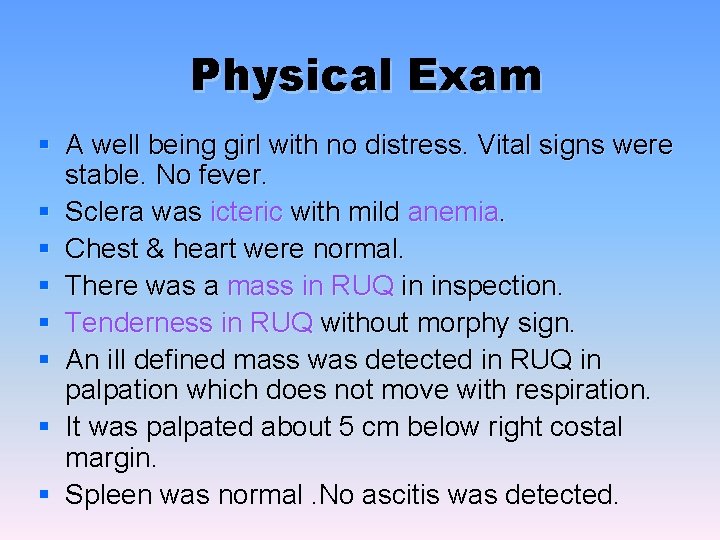
Physical Exam § A well being girl with no distress. Vital signs were stable. No fever. § Sclera was icteric with mild anemia. § Chest & heart were normal. § There was a mass in RUQ in inspection. § Tenderness in RUQ without morphy sign. § An ill defined mass was detected in RUQ in palpation which does not move with respiration. § It was palpated about 5 cm below right costal margin. § Spleen was normal. No ascitis was detected.
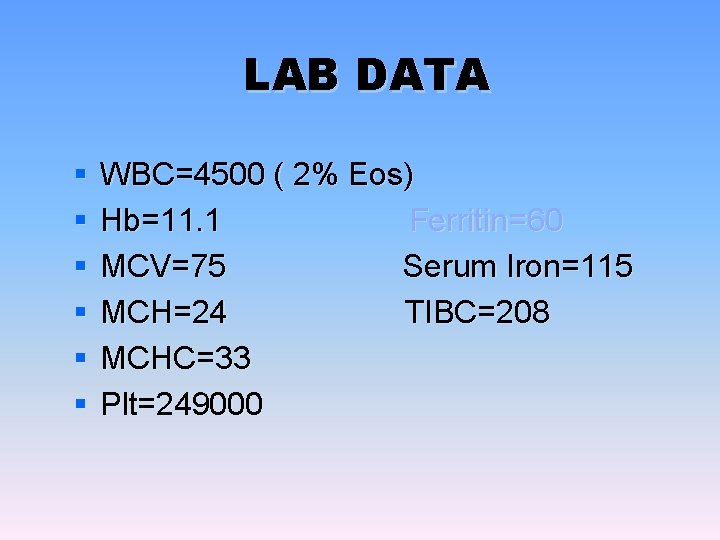
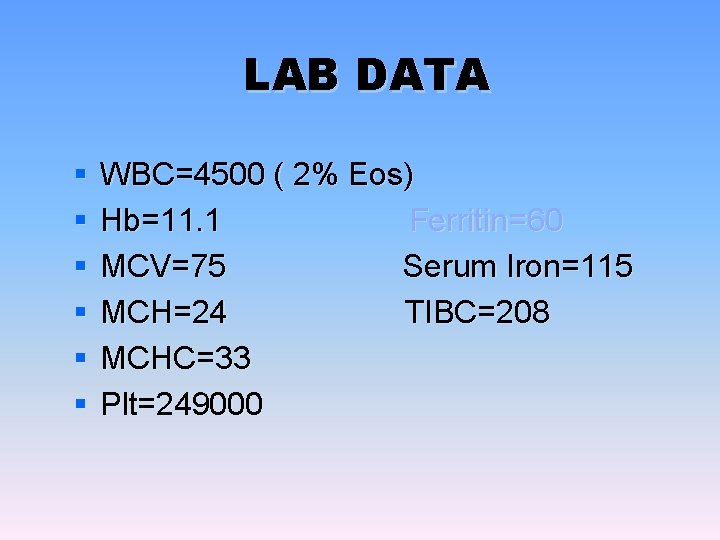
LAB DATA § § § WBC=4500 ( 2% Eos) Hb=11. 1 Ferritin=60 MCV=75 Serum Iron=115 MCH=24 TIBC=208 MCHC=33 Plt=249000
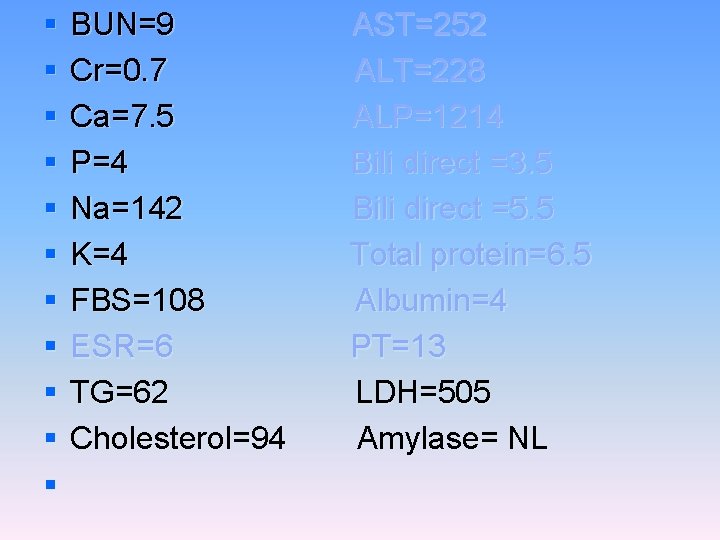
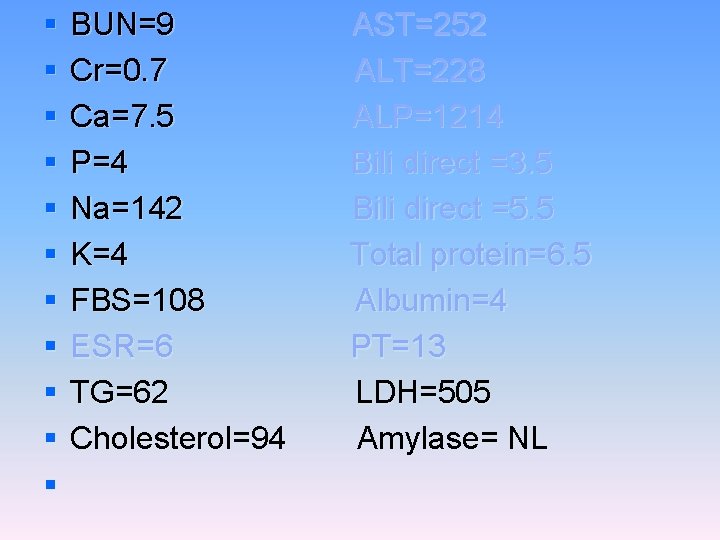
§ § § BUN=9 Cr=0. 7 Ca=7. 5 P=4 Na=142 K=4 FBS=108 ESR=6 TG=62 Cholesterol=94 AST=252 ALT=228 ALP=1214 Bili direct =3. 5 Bili direct =5. 5 Total protein=6. 5 Albumin=4 PT=13 LDH=505 Amylase= NL
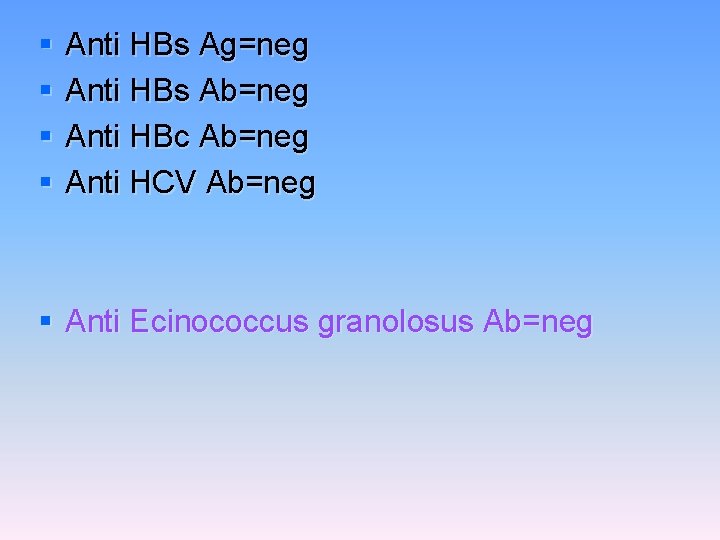
§ § Anti HBs Ag=neg Anti HBs Ab=neg Anti HBc Ab=neg Anti HCV Ab=neg § Anti Ecinococcus granolosus Ab=neg

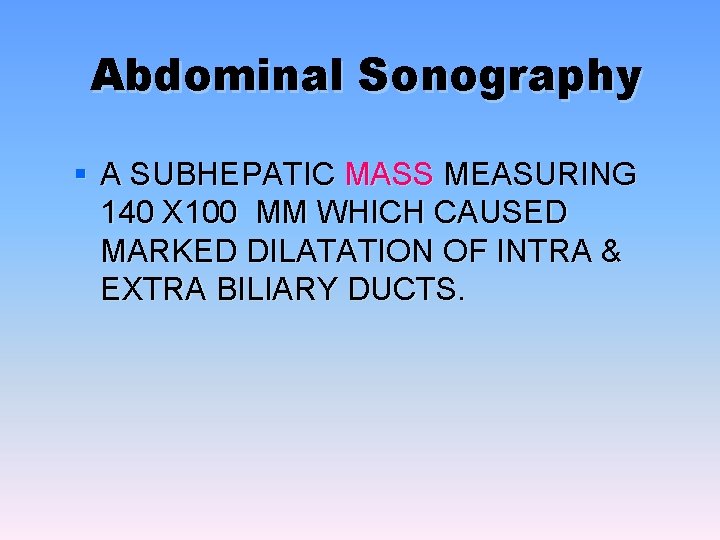
Abdominal Sonography § A SUBHEPATIC MASS MEASURING 140 X 100 MM WHICH CAUSED MARKED DILATATION OF INTRA & EXTRA BILIARY DUCTS.
Abdominal CT Scan § A regular lobulated cystic mass in right lobe of liver (120 x 120) without calcification causing dilatation of intra & extra biliary ducts.









MRCP & MRI § Huge thicked wall cystic mass (140 x 120 mm), at the portahepatis that seems connected to biliary tree and gall bladder, resulted in severe dilatation of intra hepatic bile ducts and displaced right kidney posteriorly. § Spleen, kidneys, bowel loops and abdominal wall are normal. § Finding could be due to congenital anomalies like choledocal cyst, Duplication cyst, mesenteric cyst and hydatid cyst are in DDx.







Surgery report § There was a mass(10 x 20 cm) in hilum of liver which had compressed the duodenum anteroinferiorly. It was not resectable because of extension and adhesion to the mesocolon & stomach. § Gall bladder was bilobulated. § Stomach , intestine & uterus were normal. § Cyst was draineged which was full of bile. § Cystodoudenostomy to D 2 was done.



Pathology § Microscopic Description: Sections show fibrotic cyst wall with columnar epithelial lining, inflammation and ulceration area. § Diagnosis: Choledocal cyst wall, resection: - Cyst wall with fibrosis, hemorrhage, acute & chronic inflammation and ulceration.
Biliary cysts § Biliary cysts are cystic dilatations, which may occur singly or in multiples throughout the bile ducts. § They were originally termed choledochal cysts (involving the extrahepatic bile duct) but the clinical classification was revised in 1977 to include intrahepatic cysts.
§ The incidence of biliary cysts has been estimated to be 1: 100, 000 to 150, 000. § The incidence is higher in some Asian countries (Japan). § The female to male ratio is about 3: 1. § In the past, the majority of cases were reported in children, although more recent series report equal numbers in adults and children.
§ Pathologic features of choledochal cysts are variable, ranging from normal bile duct mucosa to carcinoma. § More commonly in children there is a densely fibrotic cyst wall with evidence of chronic and acute inflammation. § In adults, there are frequently inflammatory changes, erosions, sparse distribution of mucin glands, and not infrequently metaplasia.
§ In the case of type III cysts (see below), the cyst is most often lined by duodenal mucosa, and less commonly by bile duct epithelium. § Cysts may be congenital or acquired and have been associated with a variety of anatomic abnormalities. § Familial occurrence of cysts has been described.
§ Congenital biliary cysts may be diagnosed prenatally and can be associated with biliary atresia. § Fetal viral infection may also have a role; reovirus RNA has been isolated from biliary tissue of neonates with infantile biliary obstruction and choledochal cysts. § Cyst formation may be the result of ductal obstruction or distension during the prenatal or neonatal period.
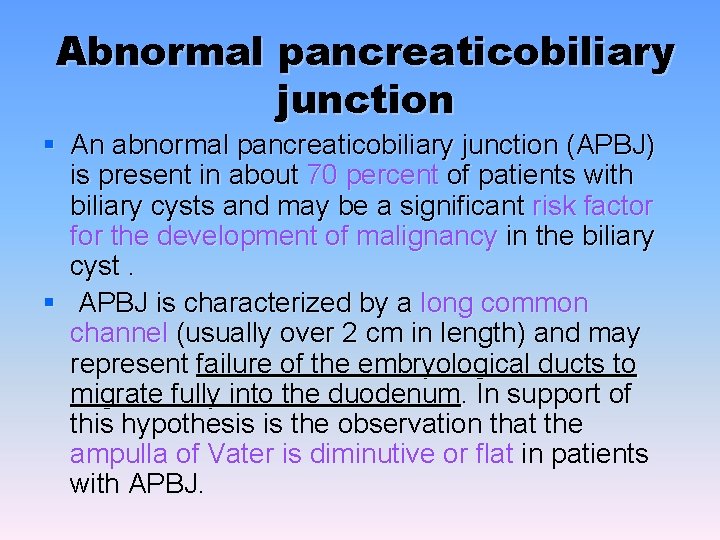
Abnormal pancreaticobiliary junction § An abnormal pancreaticobiliary junction (APBJ) is present in about 70 percent of patients with biliary cysts and may be a significant risk factor for the development of malignancy in the biliary cyst. § APBJ is characterized by a long common channel (usually over 2 cm in length) and may represent failure of the embryological ducts to migrate fully into the duodenum. In support of this hypothesis is the observation that the ampulla of Vater is diminutive or flat in patients with APBJ.
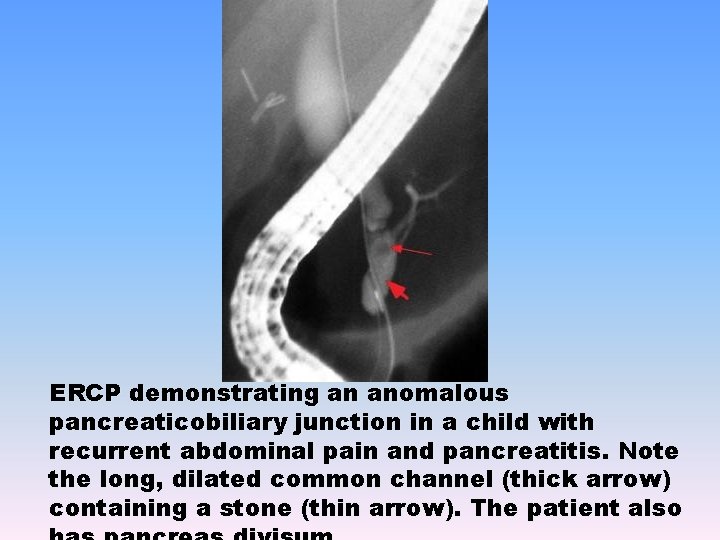
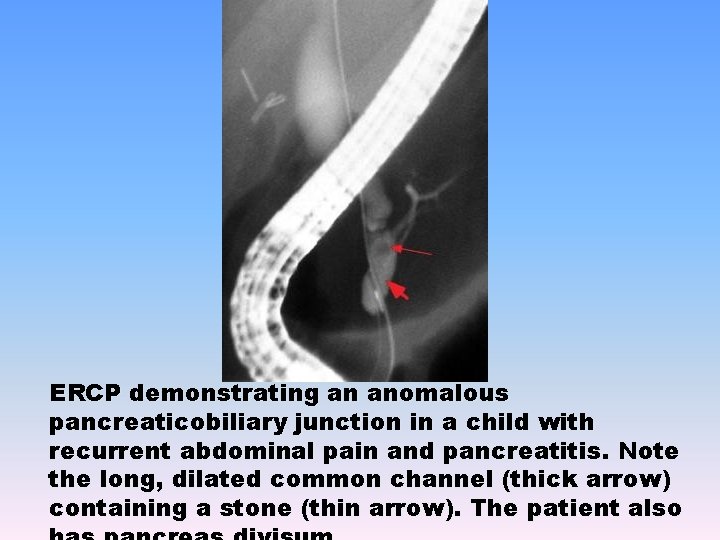
ERCP demonstrating an anomalous pancreaticobiliary junction in a child with recurrent abdominal pain and pancreatitis. Note the long, dilated common channel (thick arrow) containing a stone (thin arrow). The patient also
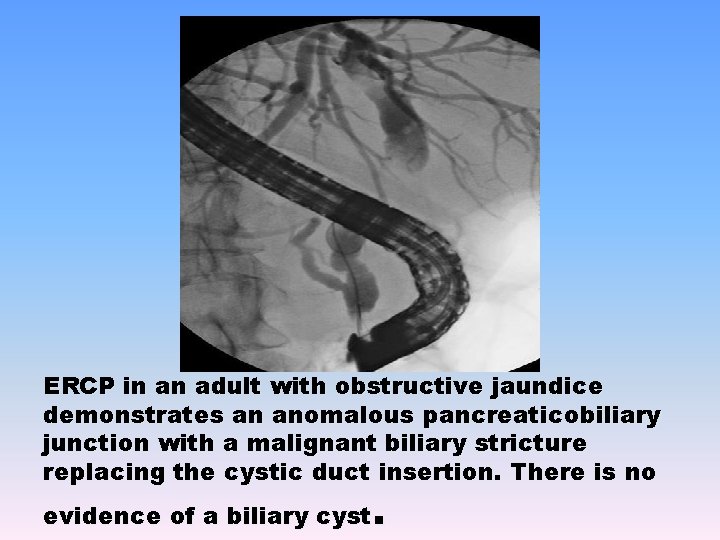
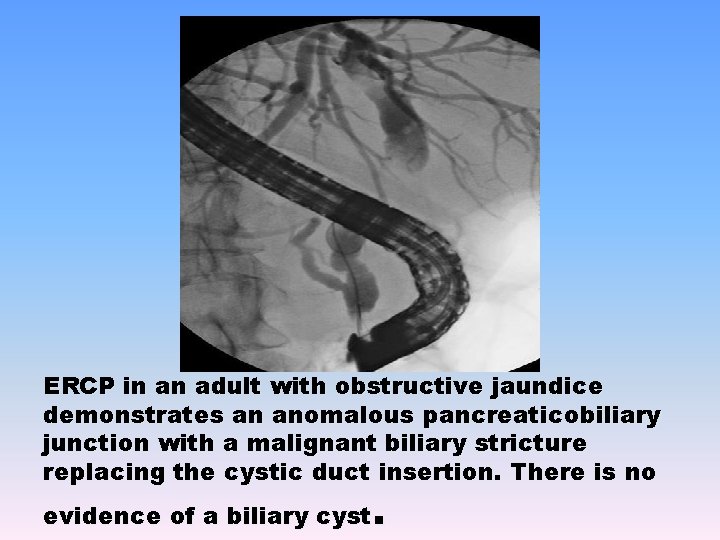
ERCP in an adult with obstructive jaundice demonstrates an anomalous pancreaticobiliary junction with a malignant biliary stricture replacing the cystic duct insertion. There is no . evidence of a biliary cyst

§ A long common channel may predispose to reflux of pancreatic juice into the biliary tree, since the ductal junction lies outside of the sphincter of Oddi. § This can result in increased amylase levels in bile , intraductal activation of proteolytic enzymes, alterations in bile composition, and theoretically biliary epithelial damage, inflammation, ductal distension, and cyst formation. § Elevated sphincter of Oddi pressures have been documented in APBJ and could promote pancreaticobiliary reflux.
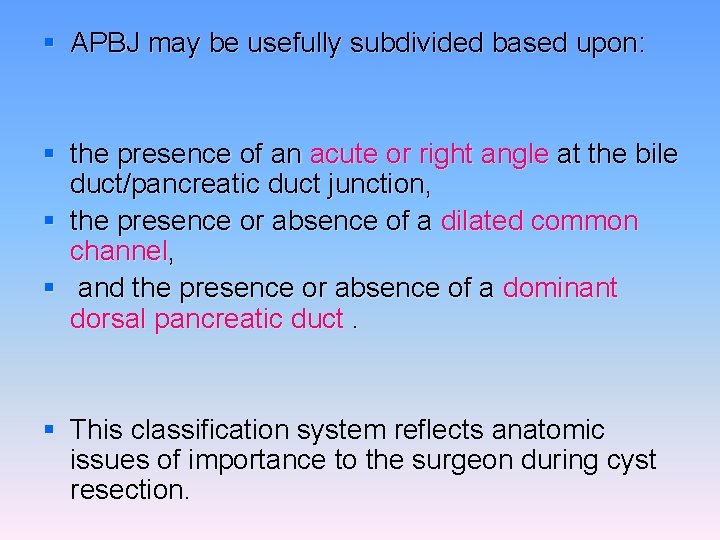
§ APBJ may be usefully subdivided based upon: § the presence of an acute or right angle at the bile duct/pancreatic duct junction, § the presence or absence of a dilated common channel, § and the presence or absence of a dominant dorsal pancreatic duct. § This classification system reflects anatomic issues of importance to the surgeon during cyst resection.
§ Proteinaceous plugs or stones within a dilated common channel ( figure 1) may cause ductal obstruction and pancreatitis, and cyst resection alone may not resolve the patient's symptoms. § Surgical sphincteroplasty or endoscopic sphincterotomy may be required in the treatment of such patients.
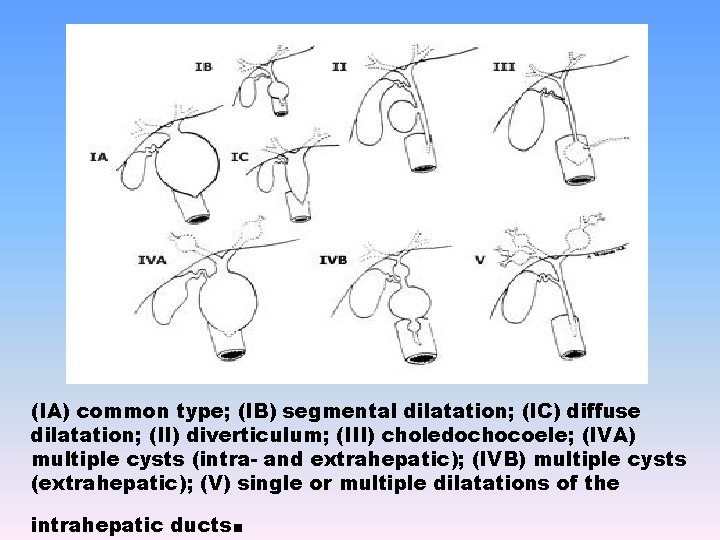
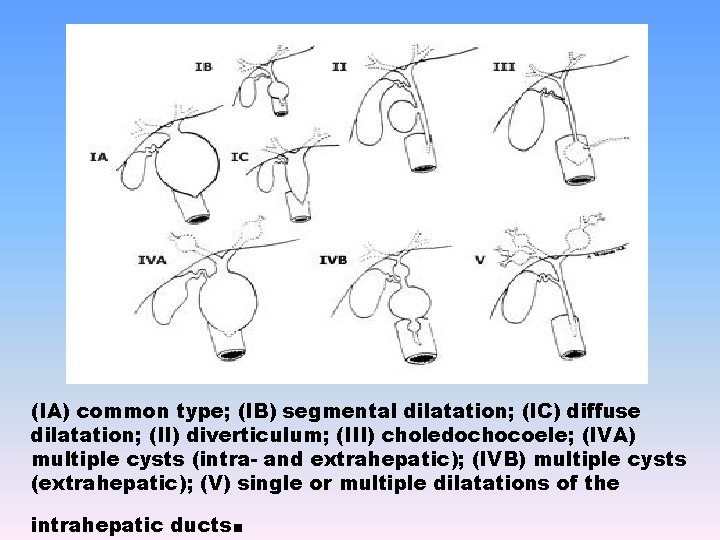
(IA) common type; (IB) segmental dilatation; (IC) diffuse dilatation; (II) diverticulum; (III) choledochocoele; (IVA) multiple cysts (intra- and extrahepatic); (IVB) multiple cysts (extrahepatic); (V) single or multiple dilatations of the . intrahepatic ducts
CLINICAL MANIFESTATIONS Infants: § conjugated hyperbilirubinemia (80 %), § failure to thrive, or an abdominal mass (30 to 60 %). § The triad of pain, jaundice, and abdominal mass is found in (11 to 63 %).
patients older than two: § chronic and intermittent abdominal pain (50 to 96 %). § Intermittent jaundice and recurrent cholangitis (34 to 55%). § Abdominal mass is less common(10 to 20%). § Pancreatitis (20%) § Biliary lithiasis (8%) § Rarely, intraperitoneal rupture, bleeding due to erosion into adjacent vessels, or portal hypertension and cirrhosis.
DIAGNOSIS § A diagnosis of biliary cyst should be considered in adults when a dilated portion of the bile ducts or ampulla is identified, especially in the absence of overt obstruction. § A high level of suspicion is required for diagnosis, particularly for Type I cysts, which may go undiagnosed unless considered in the differential diagnosis of patients found to have ductal dilation.
§ Acute or chronic biliary obstruction may cause marked biliary dilation that mimics a Type I cyst. § Such patients usually present with jaundice or markedly elevated serum alkaline phosphatase, have a readily identifiable obstructing lesion such as a stone or stricture, and their biliary dilation often improves after appropriate treatment. § Careful evaluation for APBJ may help with diagnosis in indeterminate cases.
§ Utrasound or CT may suggest the presence of a biliary cyst. § Direct cholangiography (whether intraoperative, percutaneous, or endoscopic) has long been considered the best test for diagnosis and evaluation. § Cholangiography demonstrates areas of cystic dilation, excludes overt obstruction of the bile duct, and delineates the presence of an APBJ. It may also demonstrate stones or malignancy in the cyst.
§ MRCP also appears to be useful for diagnosis. It accurately demonstrates cystically dilated segments of the biliary tree, and identifies APBJ in over 75 percent of cases. § However, MR is less sensitive than direct cholangiography for excluding obstruction.
§ Endoscopic ultrasound (EUS) can also demonstrate extrahepatic biliary cysts and provide detailed images of the cyst wall and pancreaticobiliary junction. § Intraductal ultrasound (IDUS) has been used for diagnosis of early malignant changes in a biliary cyst. § This technique is likely to be more sensitive than direct cholangiography for detection of early malignancy in the cyst wall.
CANCER RISK § Biliary cysts are associated with an increased risk of cancer, particularly cholangiocarcinoma. § The incidence of malignancy increases with age. § § 0. 7 percent in patients under 10 years of age, 6. 8 percent in patients 11 to 20 years of age, 14. 3 percent in patients over 20 years of age 50 percent has been reported in older patients.
§ The risk of malignancy is best studied in Type I and IV cysts, § although Type V cysts (Caroli's disease) have also been associated with a 7 percent risk of malignancy. § Cancer is an uncommon complication of Type III cysts, and may be limited to those choledochoceles lined by biliary rather than duodenal epithelium.
§ The cited statistics likely overestimate the risk of cancer in biliary cysts, because most series include only symptomatic patients presenting with complications of their cyst, including malignancy. § To calculate the true risk of malignant degeneration, the incidence of asymptomatic biliary cysts in the population should be used as the denominator, a parameter that is unknown. § If patients who developed malignancy at least two years after initial diagnosis of their cyst are studied, the incidence in adults appears lower (4. 5 percent rather than 14. 3 percent).
§ Evidence clearly points to a markedly increased risk of cholangiocarcinoma in biliary cysts compared to the general population. § This evidence includes the occurrence of cholangiocarcinoma in patients as young as 10 years of age , the occurrence of synchronous and metachronous biliary cancers, and the subsequent development of cancer in patients with incompletely resected cysts. § The possibility of cancer should always be considered in a newly diagnosed adult with a biliary cyst.
§ Patients previously treated with biliary bypass rather than cyst resection have a risk of subsequent malignancy that seems higher than the risk in unoperated patients. § Patients who have previously undergone cyst resection continue to have an increased risk of carcinoma. § Malignancy may develop in portions of cysts that were left behind at surgery, at the anastomotic site, or in the pancreas.
§ In one study, the increased incidence of cholangiocarcinoma in biliary cysts was confined to patients with an APBJ. § APBJ appears to increase the risk of biliary and pancreatic malignancy even in patients without a biliary cyst or ductal dilation. § K-ras mutations and p 53 overexpression have been demonstrated in the biliary mucosa of such patients. § Gallbladder cancer is the most common malignancy seen in patients with APBJ and no bile duct cyst. § Thus, prophylactic cholecystectomy in patients with APBJ has been advised.
MANAGEMENT § Because of the risk of malignant degeneration of the cyst, the current standard is surgical excision. § In addition to decreasing the risk of malignant degeneration, excision of cysts can reduce complications such as recurrent cholangitis, choledocholithiasis, and pancreatitis, which were frequently seen following the older surgical strategy of cyst drainage by choledochojejunostomy, without resection.
§ In the case of extrahepatic cysts, resection is usually followed by hepaticojejunostomy for reconstruction. § Some surgeons have advocated leaving the posterior cyst wall intact and performing mucosectomy if dissection of an extrahepatic cyst from the portal vein or hepatic artery is technically difficult. § The intrapancreatic portion of Type I cysts can generally be treated with an intramural dissection down to the pancreaticobiliary junction, without pancreatic head resection. § If left in place, the intrapancreatic portion of a Type I cyst can be associated with subsequent malignancy or stone formation in the cyst remnant. § A partial hepatectomy may be indicated if intrahepatic cysts are present and resectable.
§ Surgical resection effectively treats symptoms and appears to decrease, although not eliminate, cancer risk. § The most frequent long-term complication of hepaticojejunostomy is stenosis of the biliary-enteric anastomosis leading to cholangitis, jaundice, or cirrhosis. (25%) § After surgery, patients should have yearly serum liver tests looking for biochemical evidence of partial biliary obstruction. § Significant elevations of the serum alkaline phosphatase merit investigation and treatment, even in asymptomatic patients, to prevent secondary biliary cirrhosis.
§ When an APBJ is present with a dilated common channel, surgical or endoscopic removal of stones or protein plugs from the common channel may be necessary in patients with recurrent pain or pancreatitis. § Cholecystectomy should be considered in patients with APBJ and no bile duct cyst because of the increased risk of gallbladder cancer. § Patients with Caroli's disease may eventually require liver transplantation.
§ Type IIIA cysts (choledochoceles) are often amenable to endoscopic sphincterotomy. § Type IIIB cysts (diverticular choledochoceles) may be resected surgically or endoscopically. § In patients with a biliary cyst who refuse resective surgery or are poor surgical candidates, lesser interventions (such as laparoscopic cholecystectomy and ERCP) may treat symptoms caused by gallstones or sludge. § If screening is attempted, intraductal ultrasound is probably the most sensitive available test for early malignancy in the cyst wall
 Ruq mass
Ruq mass The right hypochondriac region is in the ruq
The right hypochondriac region is in the ruq Ruq pain
Ruq pain Tpr pharmacy abbreviation
Tpr pharmacy abbreviation Once upon a time there was a girl who said
Once upon a time there was a girl who said Stone girl bone girl
Stone girl bone girl Xxxx boy and girl
Xxxx boy and girl What is the shape of dr. jekyll’s house?
What is the shape of dr. jekyll’s house? Is atomic mass and relative atomic mass the same
Is atomic mass and relative atomic mass the same Differentiate between atomic number and mass number
Differentiate between atomic number and mass number Mass of oxygen
Mass of oxygen What makes up the atomic mass
What makes up the atomic mass Stoichiometry examples
Stoichiometry examples Percentage composition of propane
Percentage composition of propane Inertial mass vs gravitational mass
Inertial mass vs gravitational mass Convert grams to moles
Convert grams to moles Molar mass unit
Molar mass unit Molar mass def
Molar mass def Mol to mol conversion
Mol to mol conversion Mol from mass
Mol from mass Mass/mass problems
Mass/mass problems Gravitational mass vs inertial mass
Gravitational mass vs inertial mass Formula mass vs molecular mass
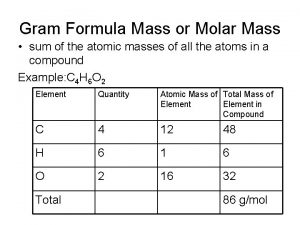
Formula mass vs molecular mass Molecular mass
Molecular mass Formula mass vs molecular mass
Formula mass vs molecular mass Formula mass vs molar mass
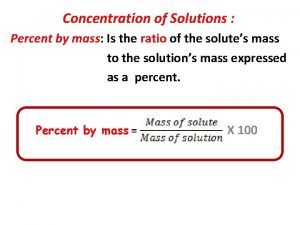
Formula mass vs molar mass How to get percent concentration
How to get percent concentration Inertial mass vs gravitational mass
Inertial mass vs gravitational mass Formula mass vs molecular mass
Formula mass vs molecular mass Atomic mass vs molar mass
Atomic mass vs molar mass Stoichiometry worksheet #2 (mole-mass mass-mole problems)
Stoichiometry worksheet #2 (mole-mass mass-mole problems) N n avogadro
N n avogadro A rocket of mass 12000 kg accelerates vertically
A rocket of mass 12000 kg accelerates vertically Mass mole
Mass mole Formula mass vs gram formula mass
Formula mass vs gram formula mass Cold air mass overtakes warm air mass
Cold air mass overtakes warm air mass Time management conference
Time management conference Enterprise content management conference
Enterprise content management conference Anser
Anser Customer experience management conference 2011
Customer experience management conference 2011 Third party risk management conference 2019 new york
Third party risk management conference 2019 new york Cboe risk management conference
Cboe risk management conference Financial risk management conference 2018
Financial risk management conference 2018 Local government asset management software
Local government asset management software Conference management middlesbrough
Conference management middlesbrough Top management middle management first line management
Top management middle management first line management Top management middle management first line management
Top management middle management first line management Basic concepts of management
Basic concepts of management Young and dyslexic analysis
Young and dyslexic analysis What did the sibley commission do
What did the sibley commission do A boy and a girl are balanced on a massless seesaw
A boy and a girl are balanced on a massless seesaw Lucy liu my girl drew
Lucy liu my girl drew Yes i think it was simply a piece of gross impertinence
Yes i think it was simply a piece of gross impertinence Once upon a time jack
Once upon a time jack Boy and girl
Boy and girl Israel boy and girl scouts federation
Israel boy and girl scouts federation Nmeninges
Nmeninges Girl scout law and promise
Girl scout law and promise Cranial nerve function mnemonic
Cranial nerve function mnemonic Geko girl
Geko girl This is only for young people
This is only for young people