Interpretasi hasil pemeriksaan skrining hemostasis Departemen Patologi Klinik




- Slides: 25
Interpretasi hasil pemeriksaan skrining hemostasis Departemen Patologi Klinik UNTAD
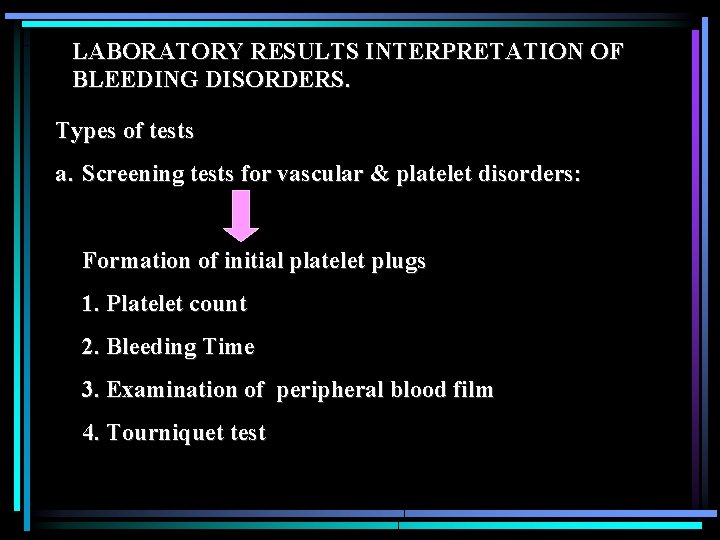
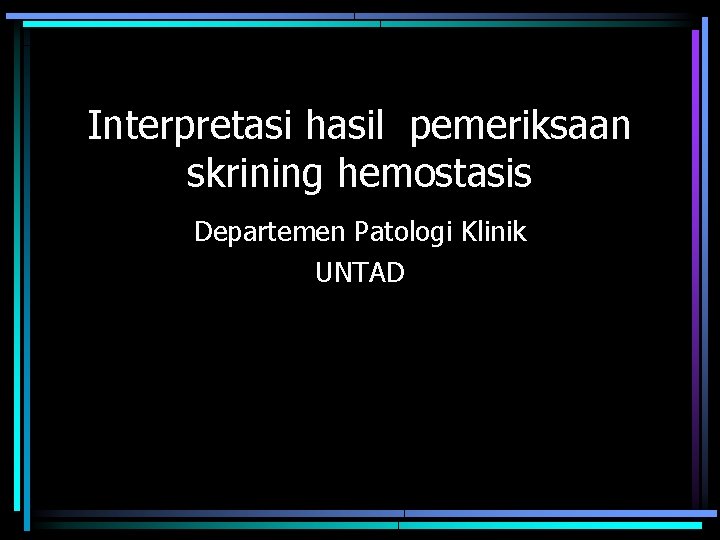
LABORATORY RESULTS INTERPRETATION OF BLEEDING DISORDERS. Types of tests a. Screening tests for vascular & platelet disorders: Formation of initial platelet plugs 1. Platelet count 2. Bleeding Time 3. Examination of peripheral blood film 4. Tourniquet test
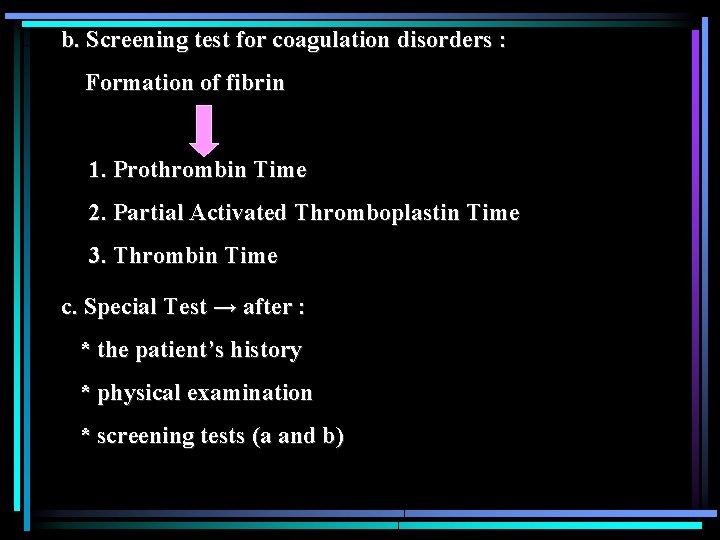
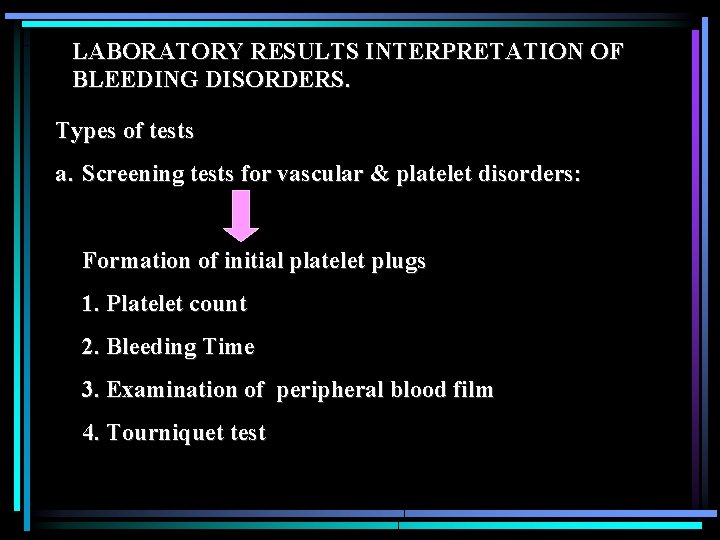
b. Screening test for coagulation disorders : Formation of fibrin 1. Prothrombin Time 2. Partial Activated Thromboplastin Time 3. Thrombin Time c. Special Test → after : * the patient’s history * physical examination * screening tests (a and b)
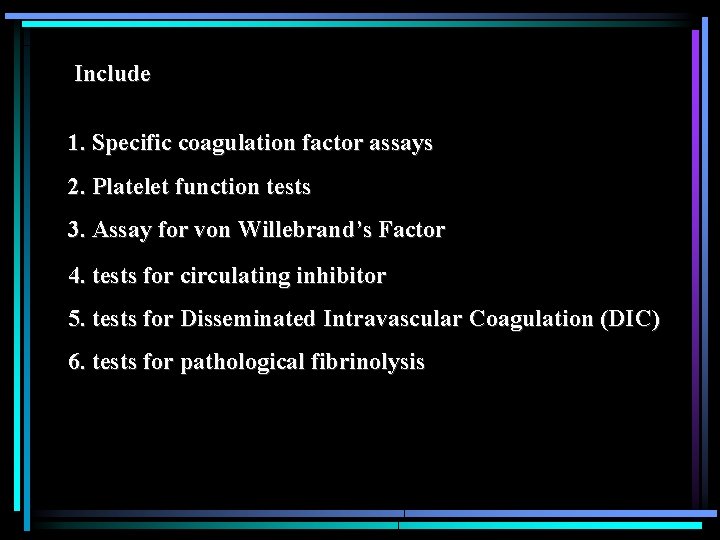
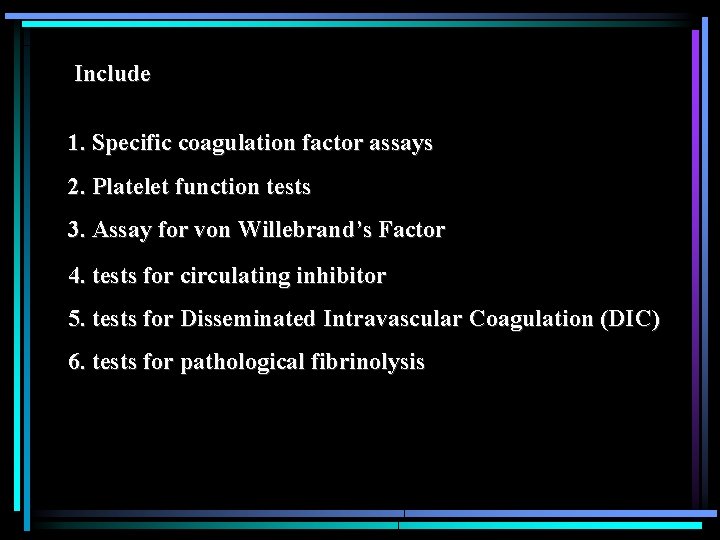
Include 1. Specific coagulation factor assays 2. Platelet function tests 3. Assay for von Willebrand’s Factor 4. tests for circulating inhibitor 5. tests for Disseminated Intravascular Coagulation (DIC) 6. tests for pathological fibrinolysis
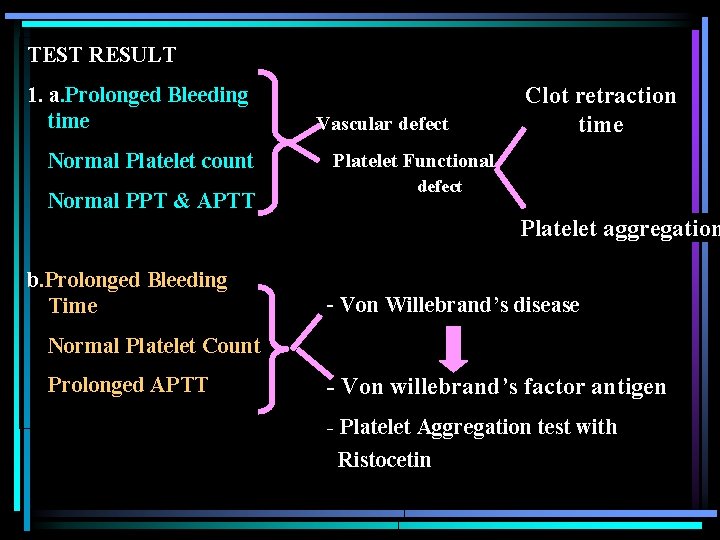
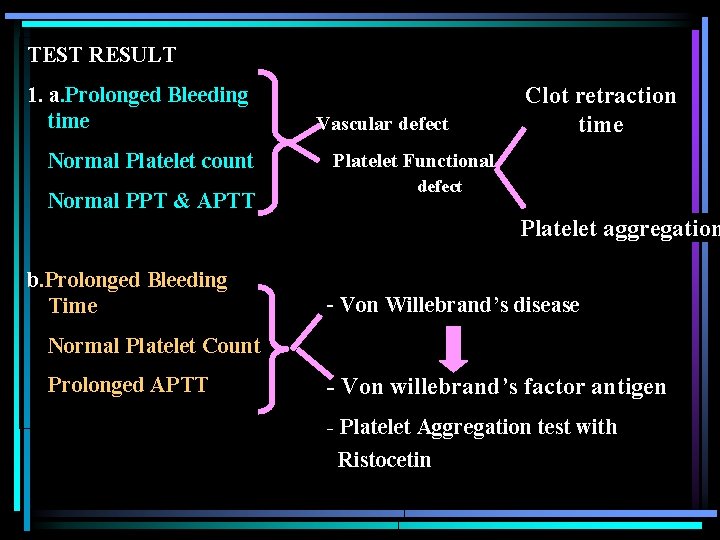
TEST RESULT 1. a. Prolonged Bleeding time Normal Platelet count Normal PPT & APTT Vascular defect Clot retraction time Platelet Functional defect Platelet aggregation b. Prolonged Bleeding Time - Von Willebrand’s disease Normal Platelet Count Prolonged APTT - Von willebrand’s factor antigen - Platelet Aggregation test with Ristocetin
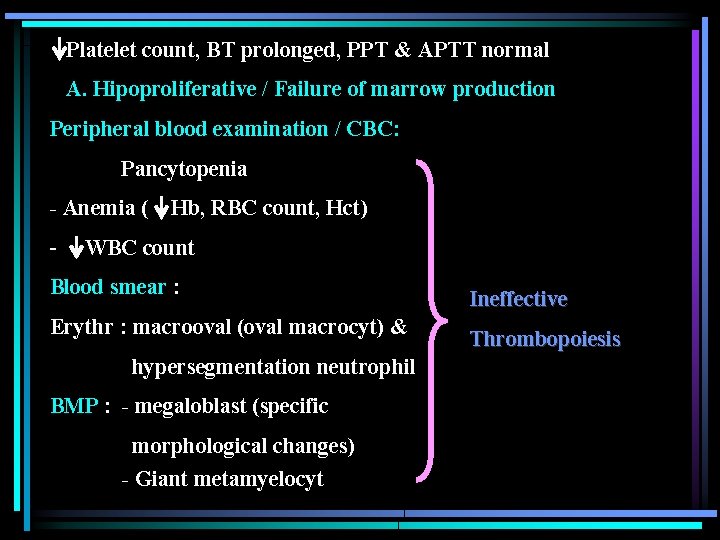
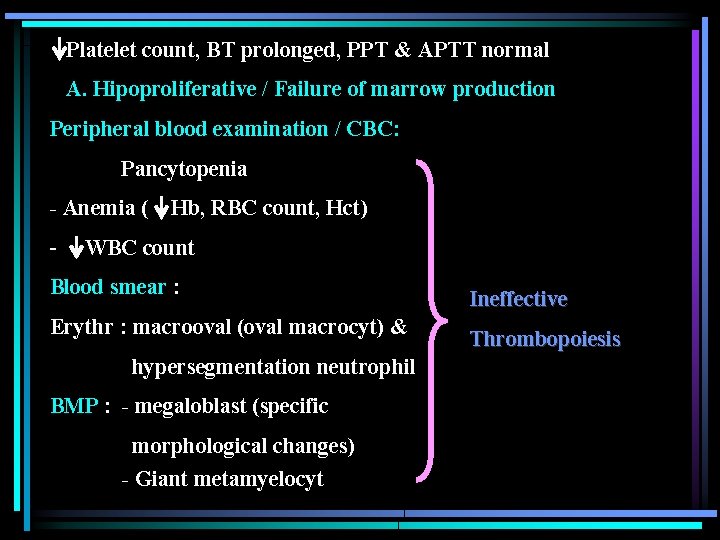
Platelet count, BT prolonged, PPT & APTT normal A. Hipoproliferative / Failure of marrow production Peripheral blood examination / CBC: Pancytopenia - Anemia ( - Hb, RBC count, Hct) WBC count Blood smear : Erythr : macrooval (oval macrocyt) & hypersegmentation neutrophil BMP : - megaloblast (specific morphological changes) - Giant metamyelocyt Ineffective Thrombopoiesis
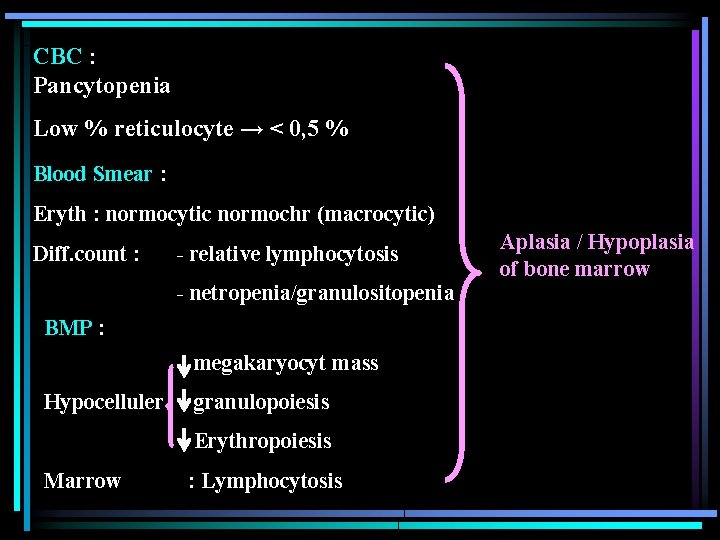
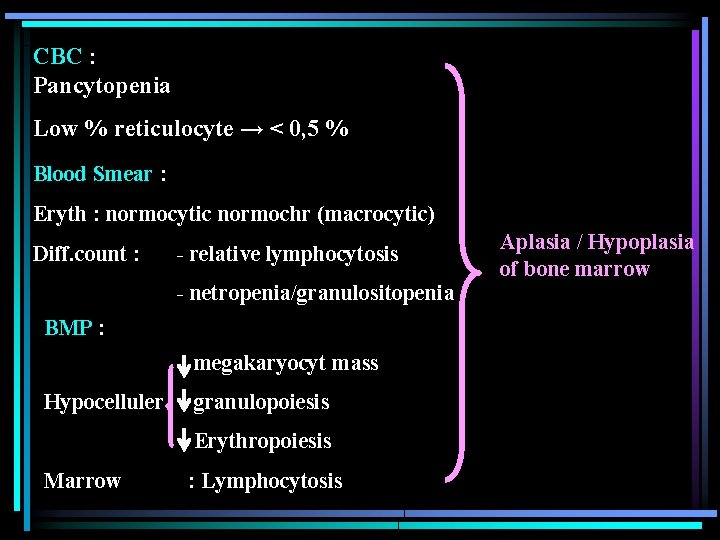
CBC : Pancytopenia Low % reticulocyte → < 0, 5 % Blood Smear : Eryth : normocytic normochr (macrocytic) Diff. count : - relative lymphocytosis - netropenia/granulositopenia BMP : megakaryocyt mass Hypocelluler granulopoiesis Erythropoiesis Marrow : Lymphocytosis Aplasia / Hypoplasia of bone marrow
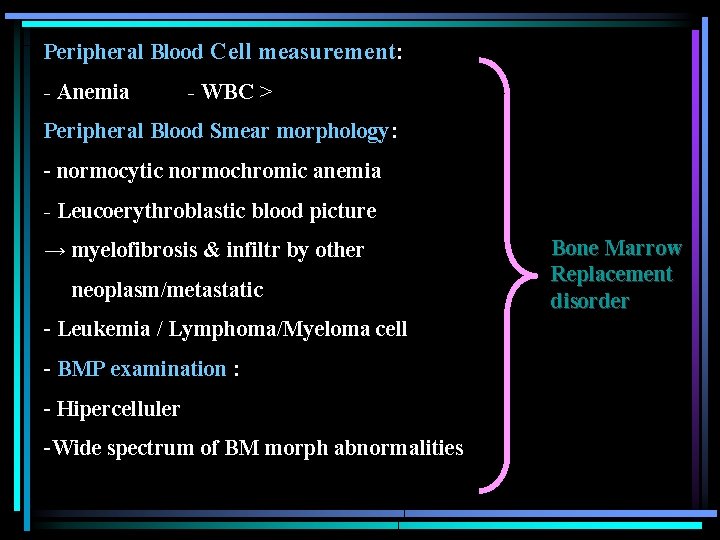
Peripheral Blood Cell measurement: - Anemia - WBC > Peripheral Blood Smear morphology: - normocytic normochromic anemia - Leucoerythroblastic blood picture → myelofibrosis & infiltr by other neoplasm/metastatic - Leukemia / Lymphoma/Myeloma cell - BMP examination : - Hipercelluler -Wide spectrum of BM morph abnormalities Bone Marrow Replacement disorder
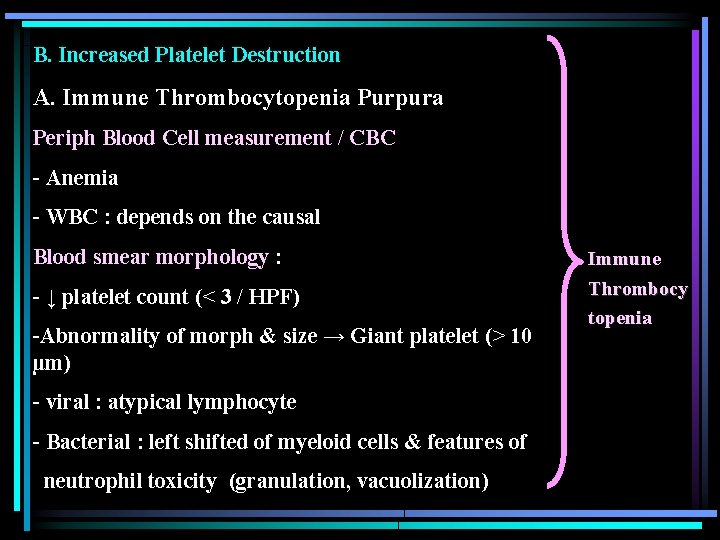
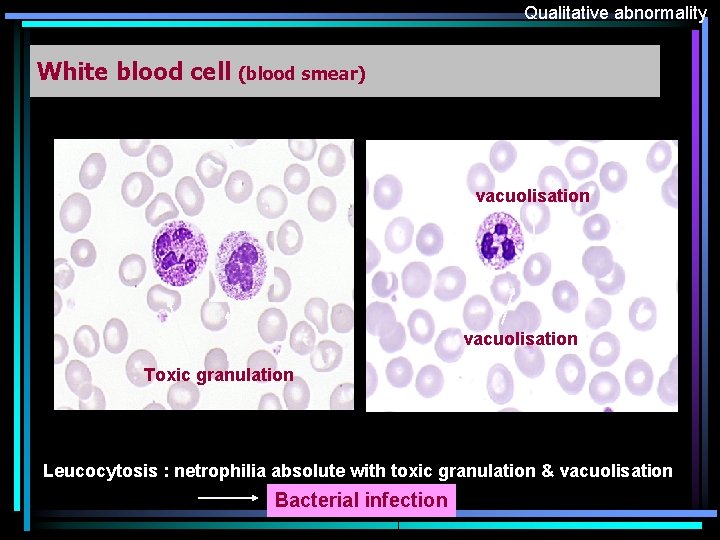
B. Increased Platelet Destruction A. Immune Thrombocytopenia Purpura Periph Blood Cell measurement / CBC - Anemia - WBC : depends on the causal Blood smear morphology : - ↓ platelet count (< 3 / HPF) -Abnormality of morph & size → Giant platelet (> 10 µm) - viral : atypical lymphocyte - Bacterial : left shifted of myeloid cells & features of neutrophil toxicity (granulation, vacuolization) Immune Thrombocy topenia
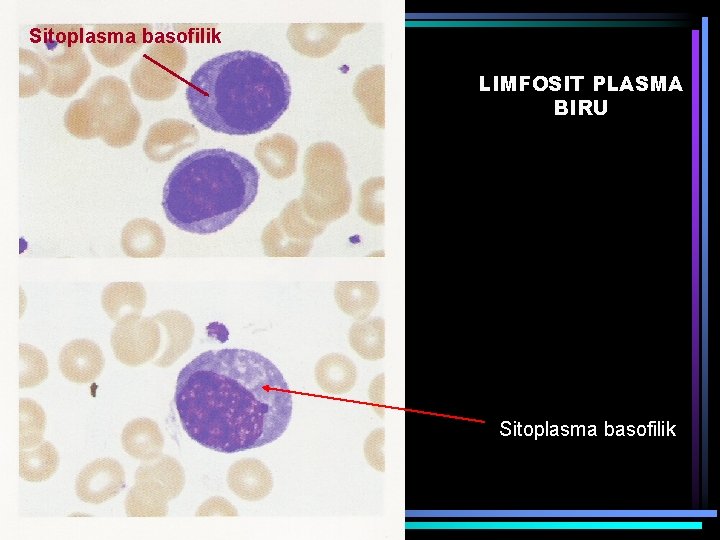
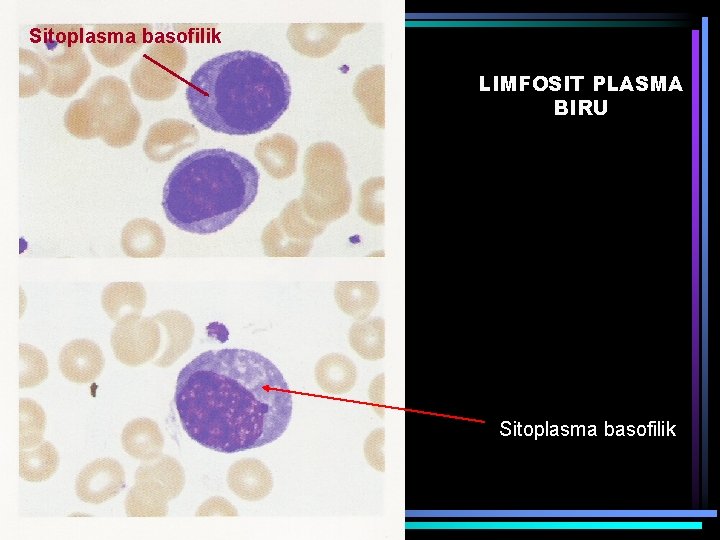
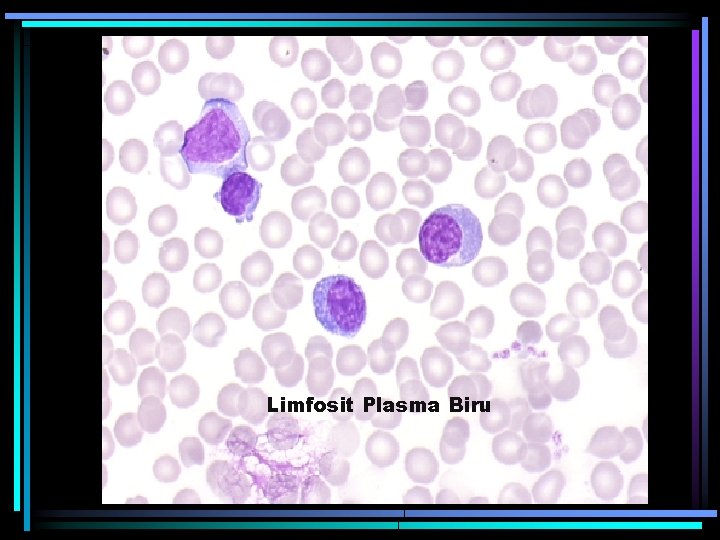
Sitoplasma basofilik LIMFOSIT PLASMA BIRU Sitoplasma basofilik
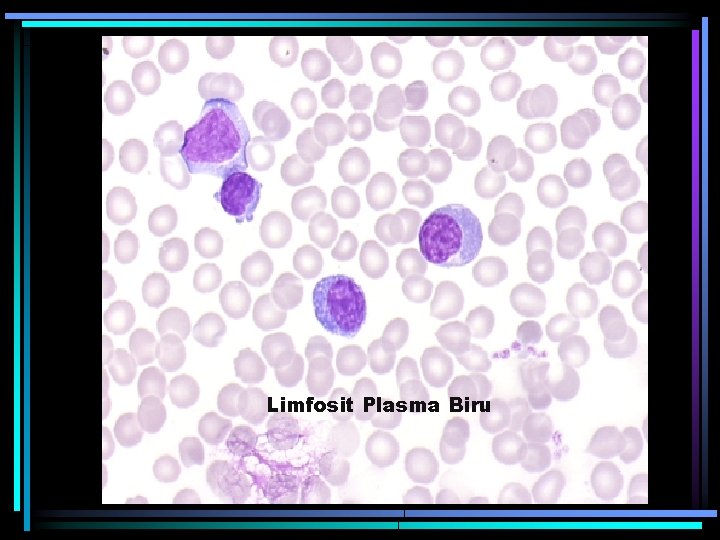
Limfosit Plasma Biru
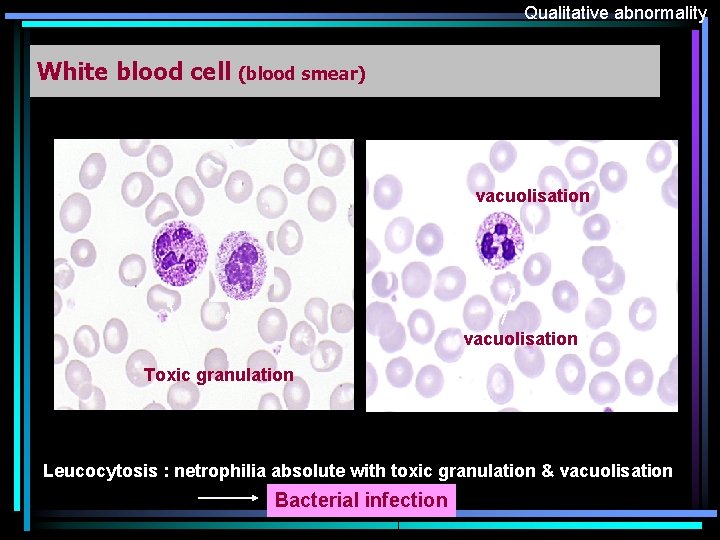
Qualitative abnormality White blood cell (blood smear) vacuolisation Toxic granulation Leucocytosis : netrophilia absolute with toxic granulation & vacuolisation Bacterial infection

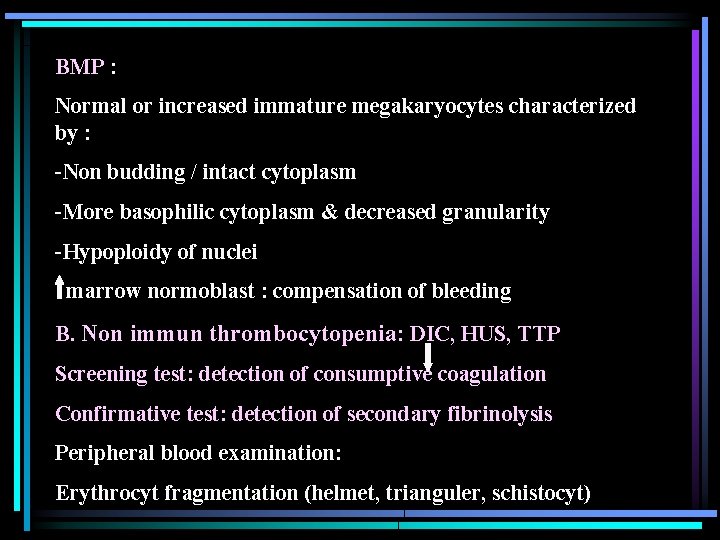
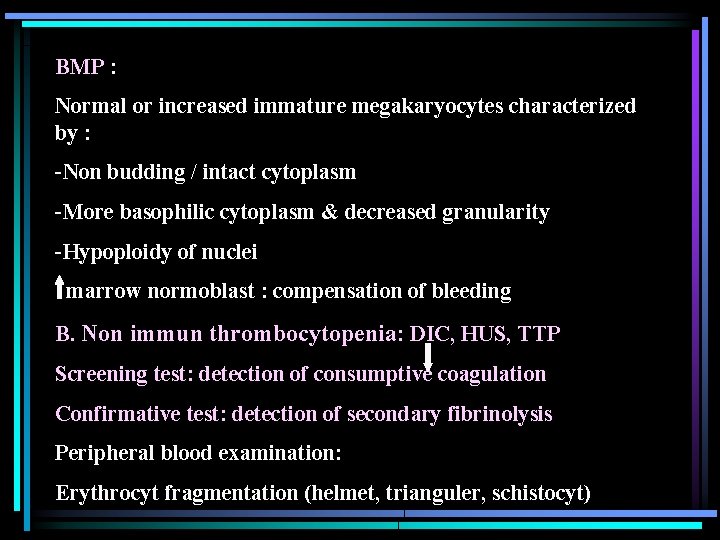
BMP : Normal or increased immature megakaryocytes characterized by : -Non budding / intact cytoplasm -More basophilic cytoplasm & decreased granularity -Hypoploidy of nuclei marrow normoblast : compensation of bleeding B. Non immun thrombocytopenia: DIC, HUS, TTP Screening test: detection of consumptive coagulation Confirmative test: detection of secondary fibrinolysis Peripheral blood examination: Erythrocyt fragmentation (helmet, trianguler, schistocyt)
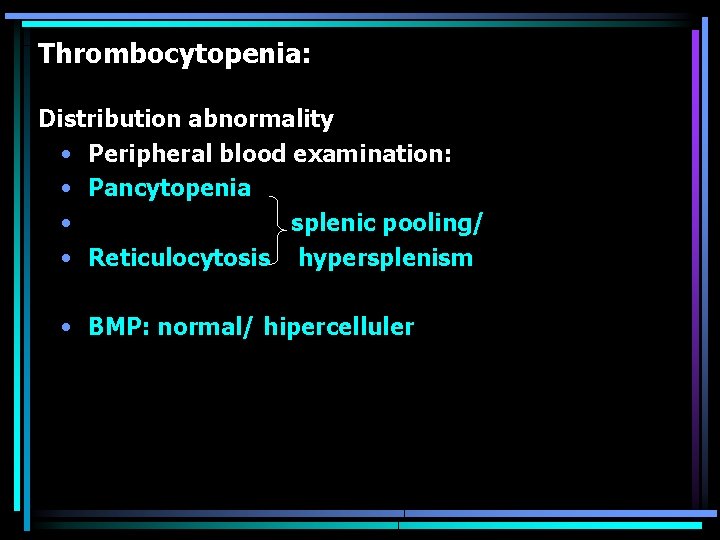
Thrombocytopenia: Distribution abnormality • Peripheral blood examination: • Pancytopenia • splenic pooling/ • Reticulocytosis hypersplenism • BMP: normal/ hipercelluler
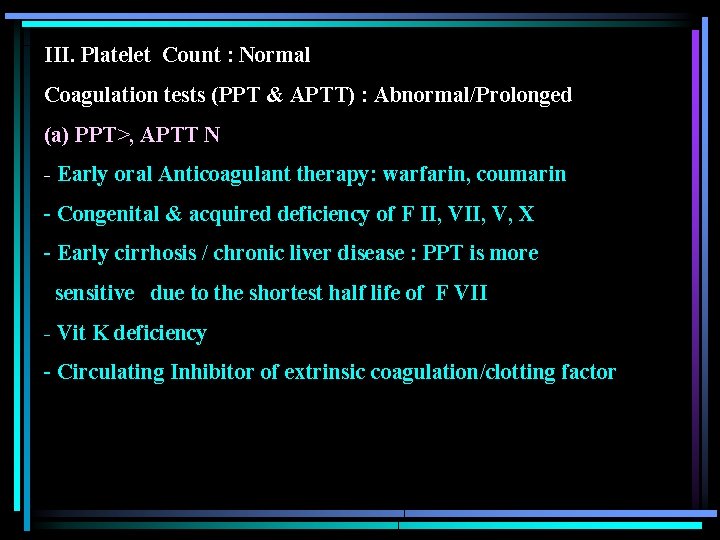
III. Platelet Count : Normal Coagulation tests (PPT & APTT) : Abnormal/Prolonged (a) PPT>, APTT N - Early oral Anticoagulant therapy: warfarin, coumarin - Congenital & acquired deficiency of F II, V, X - Early cirrhosis / chronic liver disease : PPT is more sensitive due to the shortest half life of F VII - Vit K deficiency - Circulating Inhibitor of extrinsic coagulation/clotting factor

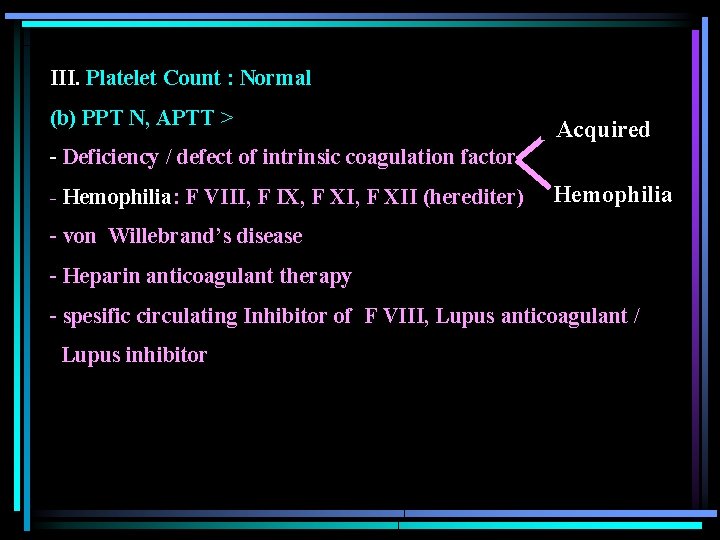
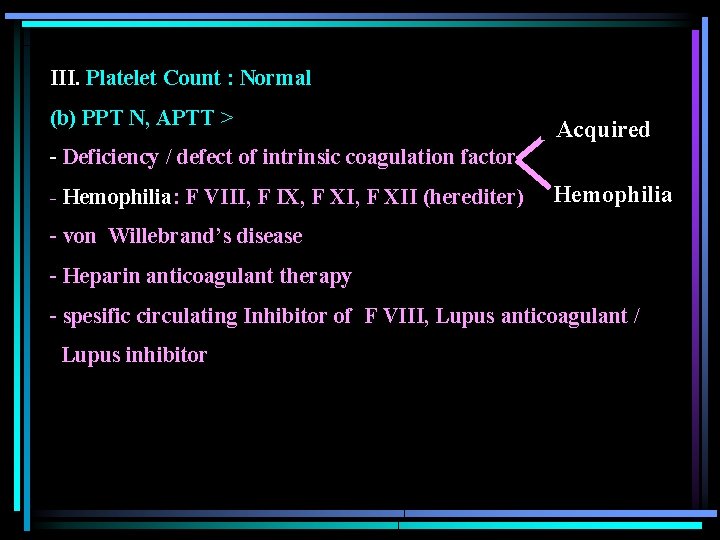
III. Platelet Count : Normal (b) PPT N, APTT > Acquired - Deficiency / defect of intrinsic coagulation factor - Hemophilia: F VIII, F IX, F XII (herediter) Hemophilia - von Willebrand’s disease - Heparin anticoagulant therapy - spesific circulating Inhibitor of F VIII, Lupus anticoagulant / Lupus inhibitor

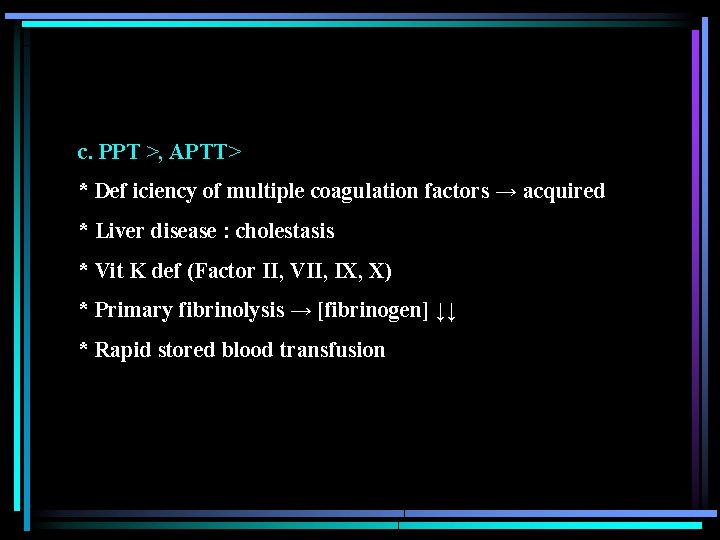
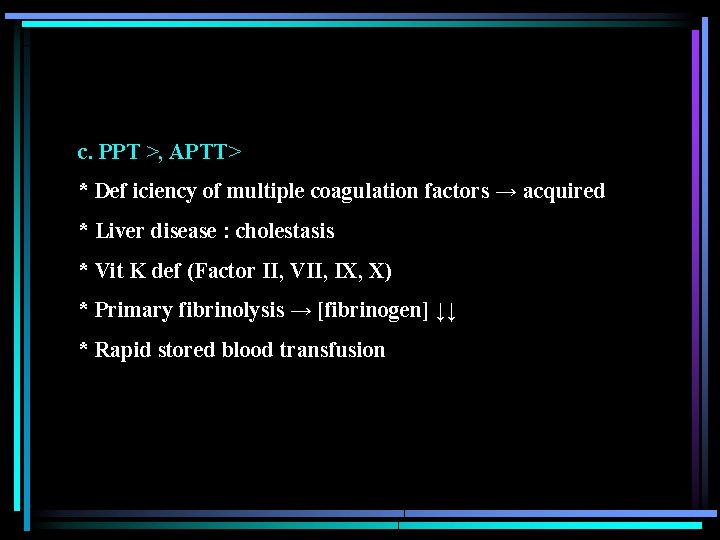
c. PPT >, APTT> * Def iciency of multiple coagulation factors → acquired * Liver disease : cholestasis * Vit K def (Factor II, VII, IX, X) * Primary fibrinolysis → [fibrinogen] ↓↓ * Rapid stored blood transfusion
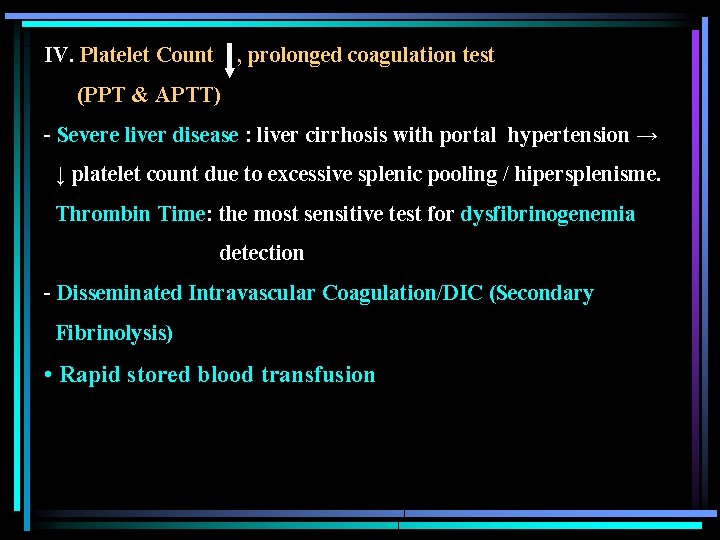
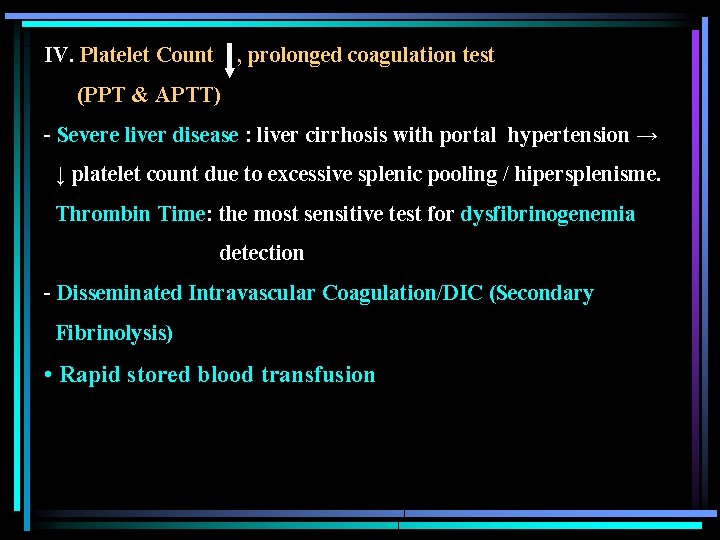
IV. Platelet Count , prolonged coagulation test (PPT & APTT) - Severe liver disease : liver cirrhosis with portal hypertension → ↓ platelet count due to excessive splenic pooling / hipersplenisme. Thrombin Time: the most sensitive test for dysfibrinogenemia detection - Disseminated Intravascular Coagulation/DIC (Secondary Fibrinolysis) • Rapid stored blood transfusion
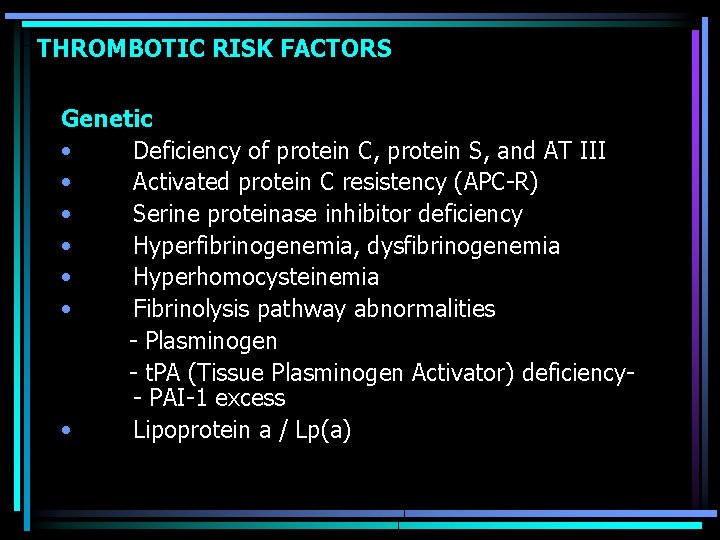
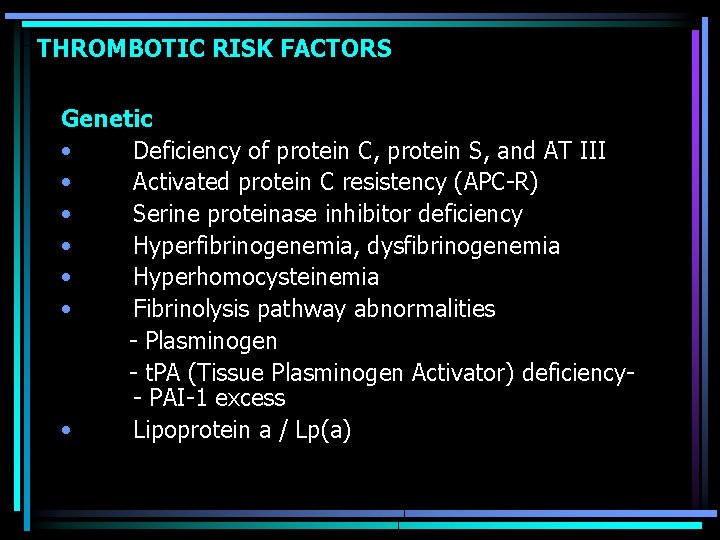
THROMBOTIC RISK FACTORS Genetic • Deficiency of protein C, protein S, and AT III • Activated protein C resistency (APC-R) • Serine proteinase inhibitor deficiency • Hyperfibrinogenemia, dysfibrinogenemia • Hyperhomocysteinemia • Fibrinolysis pathway abnormalities - Plasminogen - t. PA (Tissue Plasminogen Activator) deficiency- PAI-1 excess • Lipoprotein a / Lp(a)
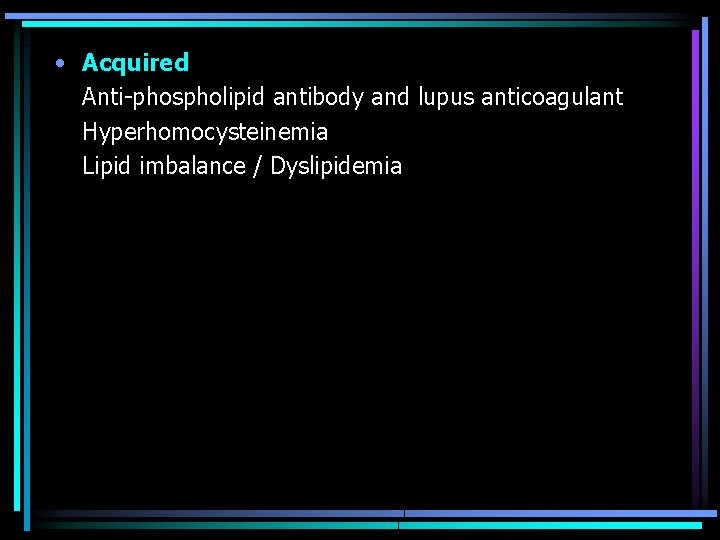
• Acquired Anti-phospholipid antibody and lupus anticoagulant Hyperhomocysteinemia Lipid imbalance / Dyslipidemia

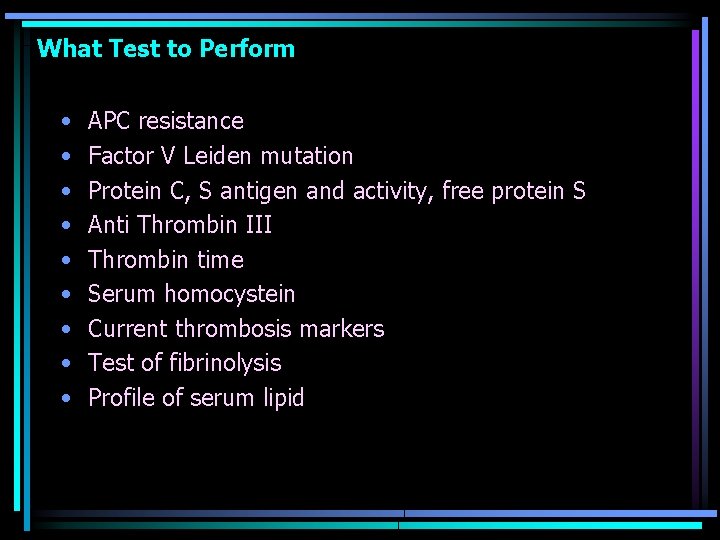
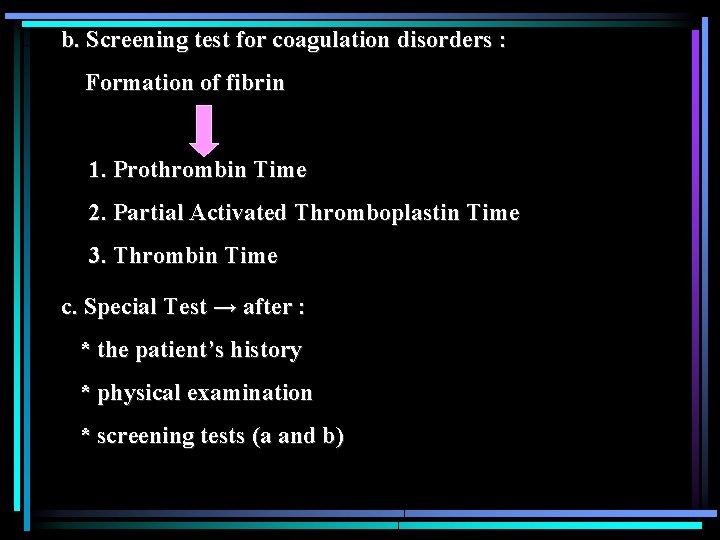
What Test to Perform • • • APC resistance Factor V Leiden mutation Protein C, S antigen and activity, free protein S Anti Thrombin III Thrombin time Serum homocystein Current thrombosis markers Test of fibrinolysis Profile of serum lipid
 Nilai normal lcs
Nilai normal lcs Subsequent event dan penyelesaian pemeriksaan
Subsequent event dan penyelesaian pemeriksaan Tindakan menempatkan testes masuk ke scrotum disebut
Tindakan menempatkan testes masuk ke scrotum disebut Skrining sinonim
Skrining sinonim Materi skrining epidemiologi
Materi skrining epidemiologi Teoae skrining sluha
Teoae skrining sluha Interpretasi agd adalah
Interpretasi agd adalah Interpretasi hasil asesmen
Interpretasi hasil asesmen Definisi patologi sosial
Definisi patologi sosial Patologi rehabilitasi sosial
Patologi rehabilitasi sosial Uhthoffs fenomen
Uhthoffs fenomen Haemophilia types
Haemophilia types Saddle blood clot
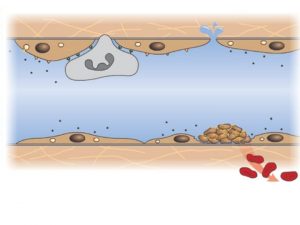
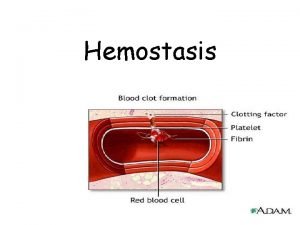
Saddle blood clot Hemostasis
Hemostasis Hemostasis
Hemostasis Nama ami
Nama ami Primary hemostasis
Primary hemostasis 13 blood clotting factors list pdf
13 blood clotting factors list pdf Primary hemostasis
Primary hemostasis Bleeding time
Bleeding time 1ry hemostasis prescribed by:
1ry hemostasis prescribed by: Hemostasis
Hemostasis Hemostasis process
Hemostasis process Vasoconstriction
Vasoconstriction Interpretasi ddst
Interpretasi ddst Tarif bop per dmh untuk setiap departemen produksi
Tarif bop per dmh untuk setiap departemen produksi