Hemostasis Coagulation Modifying Agents Pathopharmacology Wanda Lovitz APRN
- Slides: 62
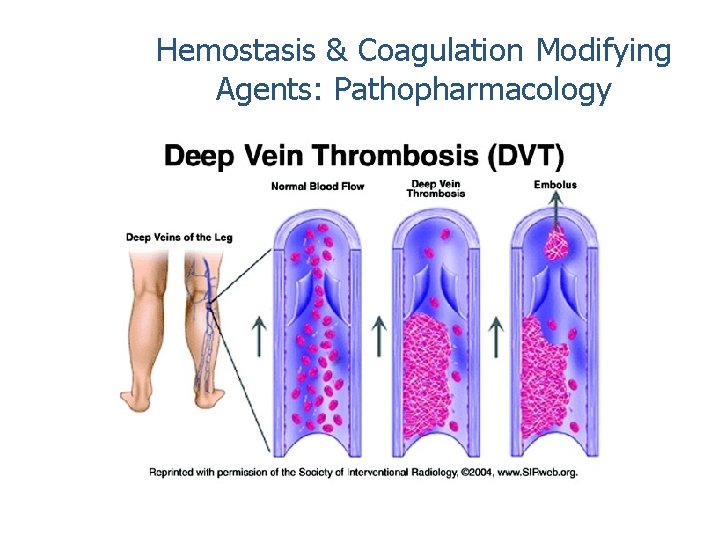
Hemostasis & Coagulation Modifying Agents: Pathopharmacology Wanda Lovitz, APRN
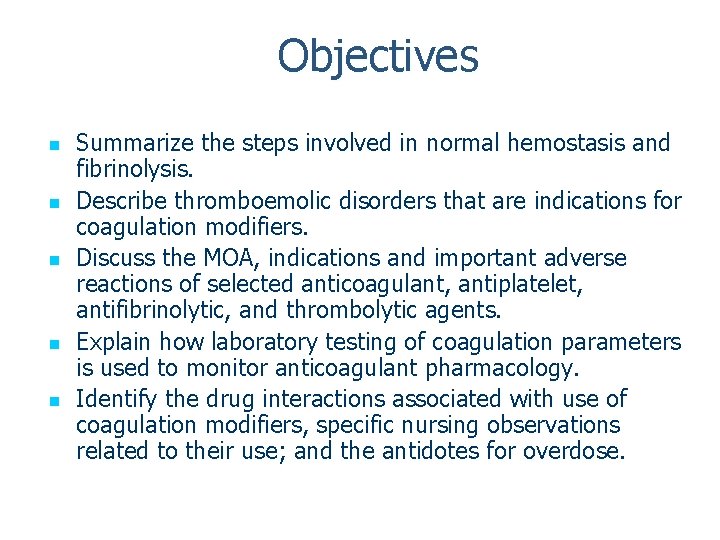
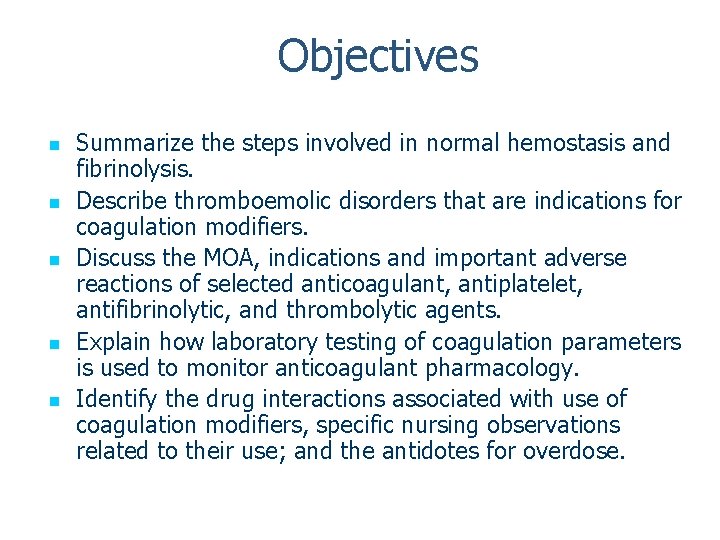
Objectives n n n Summarize the steps involved in normal hemostasis and fibrinolysis. Describe thromboemolic disorders that are indications for coagulation modifiers. Discuss the MOA, indications and important adverse reactions of selected anticoagulant, antiplatelet, antifibrinolytic, and thrombolytic agents. Explain how laboratory testing of coagulation parameters is used to monitor anticoagulant pharmacology. Identify the drug interactions associated with use of coagulation modifiers, specific nursing observations related to their use; and the antidotes for overdose.
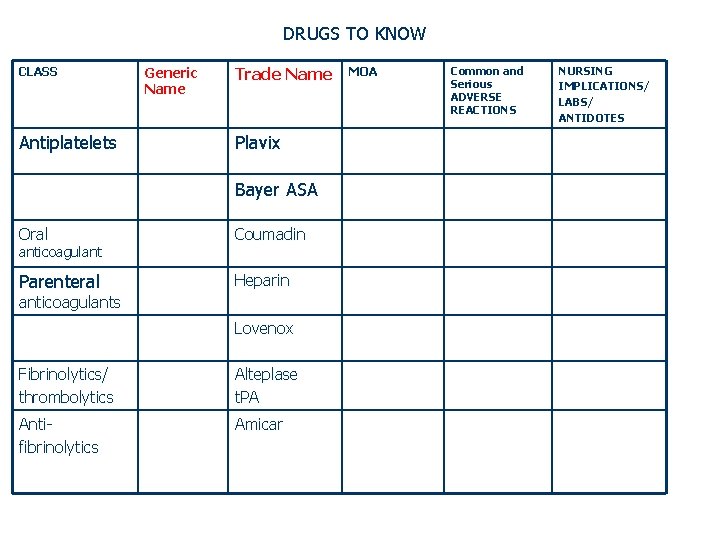
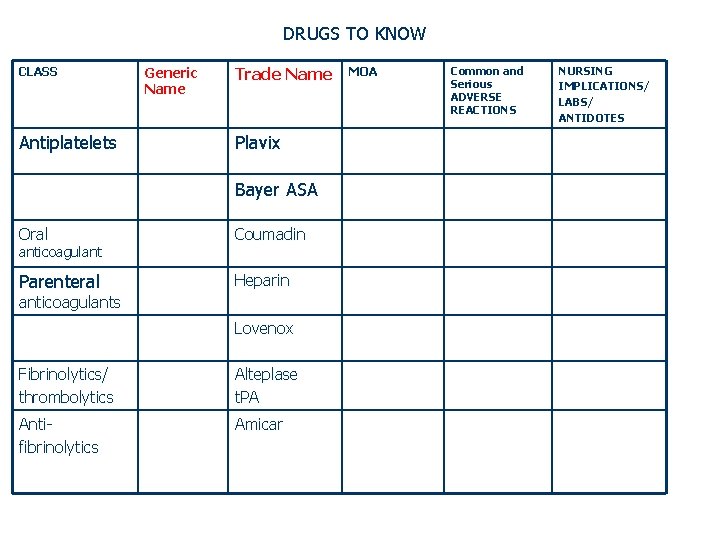
DRUGS TO KNOW CLASS Antiplatelets Generic Name Trade Name Plavix Bayer ASA Oral Coumadin Parenteral Heparin anticoagulants Lovenox Fibrinolytics/ thrombolytics Alteplase t. PA Antifibrinolytics Amicar MOA Common and Serious ADVERSE REACTIONS NURSING IMPLICATIONS/ LABS/ ANTIDOTES
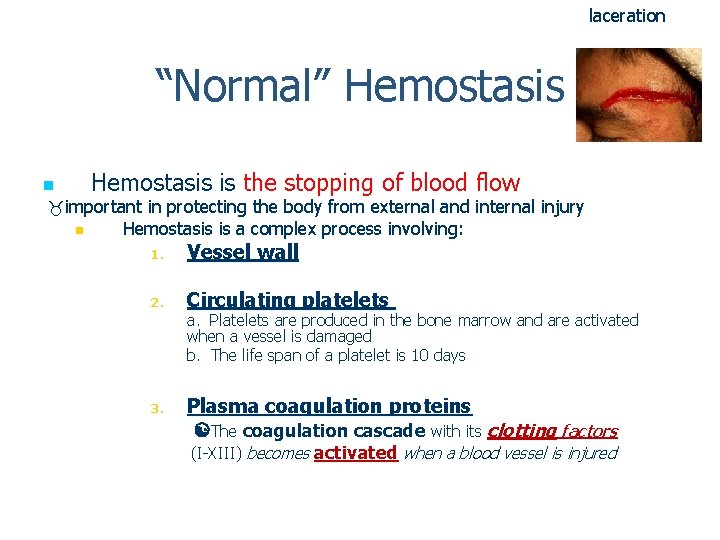
laceration “Normal” Hemostasis n Hemostasis is the stopping of blood flow important in protecting the body from external and internal injury n Hemostasis is a complex process involving: 1. Vessel wall 2. Circulating platelets a. Platelets are produced in the bone marrow and are activated when a vessel is damaged b. The life span of a platelet is 10 days 3. Plasma coagulation proteins The coagulation cascade with its clotting factors (I-XIII) becomes activated when a blood vessel is injured
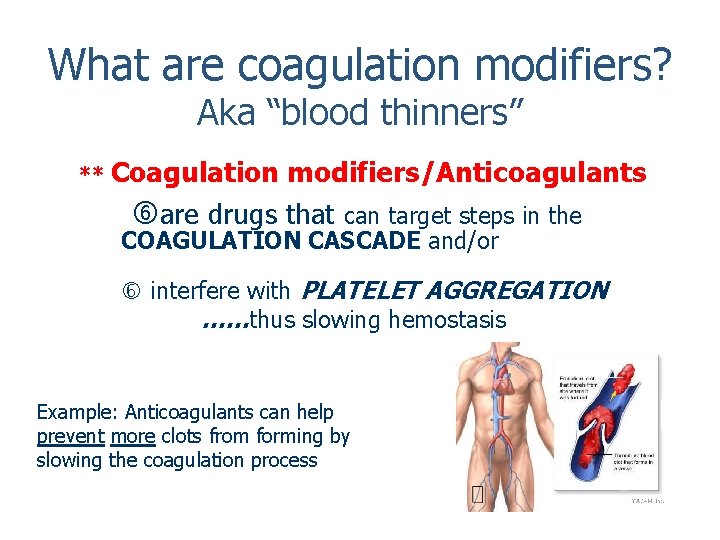
What are coagulation modifiers? Aka “blood thinners” ** Coagulation modifiers/Anticoagulants are drugs that can target steps in the COAGULATION CASCADE and/or interfere with PLATELET AGGREGATION ……thus slowing hemostasis Example: Anticoagulants can help prevent more clots from forming by slowing the coagulation process
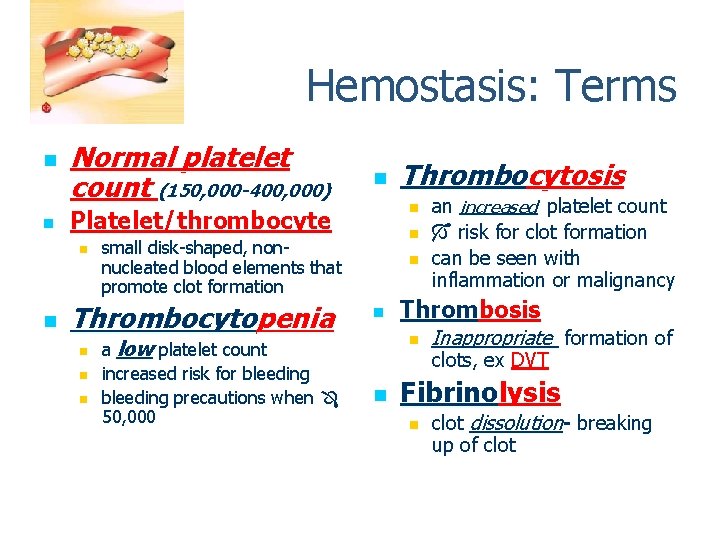
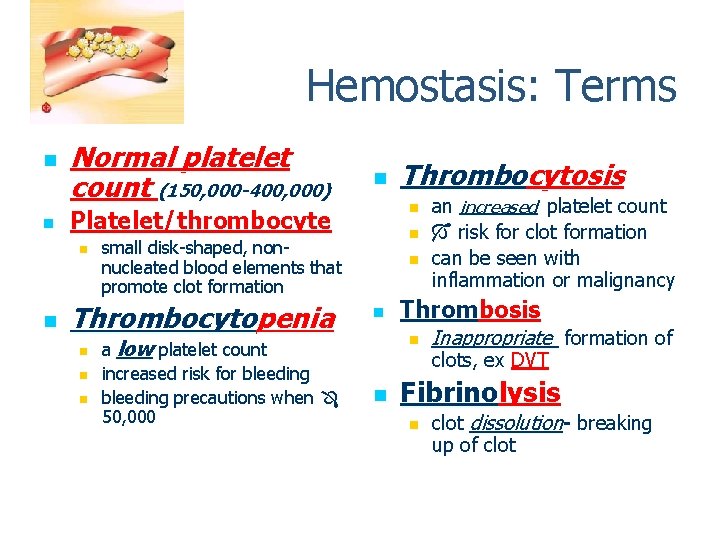
Hemostasis: Terms n n Normal platelet count (150, 000 -400, 000) n n small disk-shaped, nonnucleated blood elements that promote clot formation Thrombocytopenia a low platelet count increased risk for bleeding precautions when 50, 000 Thrombocytosis n Platelet/thrombocyte n n n Thrombosis n n an increased platelet count risk for clot formation can be seen with inflammation or malignancy Inappropriate formation of clots, ex DVT Fibrinolysis n clot dissolution- breaking up of clot
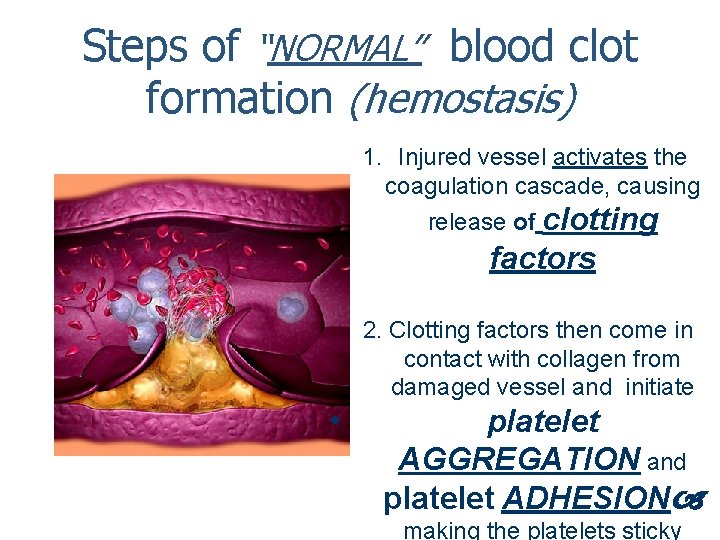
Steps of “NORMAL” blood clot formation (hemostasis) 1. Injured vessel activates the coagulation cascade, causing release of clotting factors 2. Clotting factors then come in contact with collagen from damaged vessel and initiate • platelet AGGREGATION and platelet ADHESION making the platelets sticky
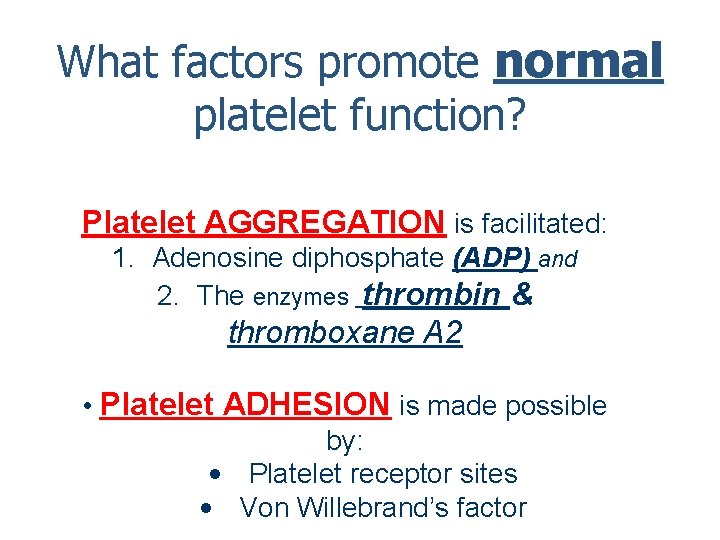
What factors promote normal platelet function? Platelet AGGREGATION is facilitated: 1. Adenosine diphosphate (ADP) and 2. The enzymes thrombin & thromboxane A 2 • Platelet ADHESION is made possible by: • Platelet receptor sites • Von Willebrand’s factor
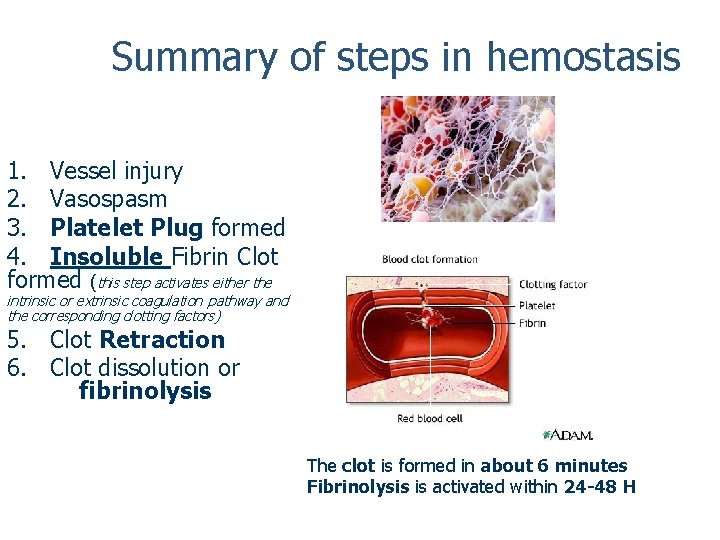
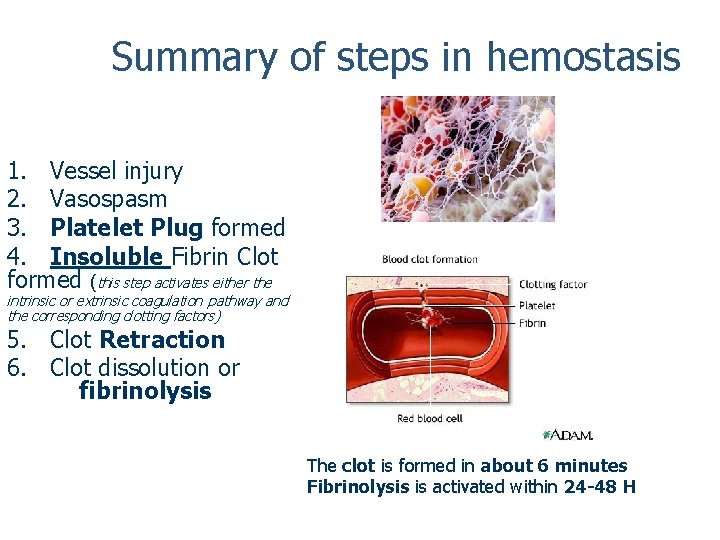
Summary of steps in hemostasis 1. Vessel injury 2. Vasospasm 3. Platelet Plug formed 4. Insoluble Fibrin Clot formed (this step activates either the intrinsic or extrinsic coagulation pathway and the corresponding clotting factors) 5. Clot Retraction 6. Clot dissolution or fibrinolysis The clot is formed in about 6 minutes Fibrinolysis is activated within 24 -48 H
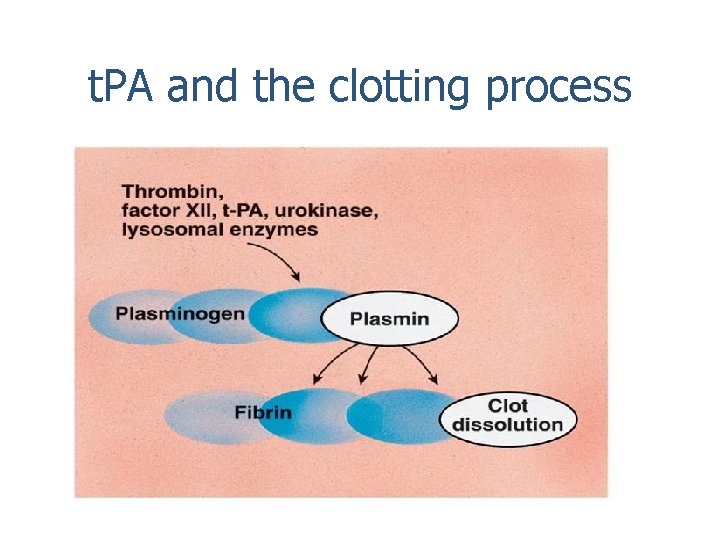
What role does t. PA play in fibrinolysis? Fibrinolysis requires the enzyme t. PA which converts plasminogen to plasmin Plasmin then digests the clot.
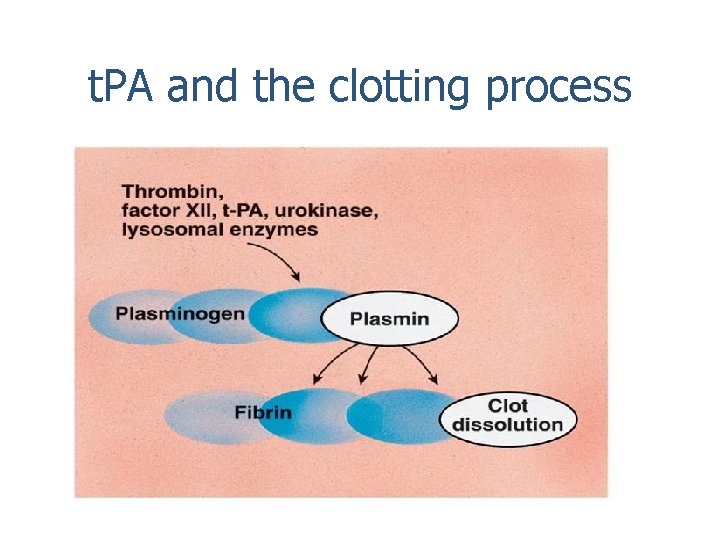
t. PA and the clotting process
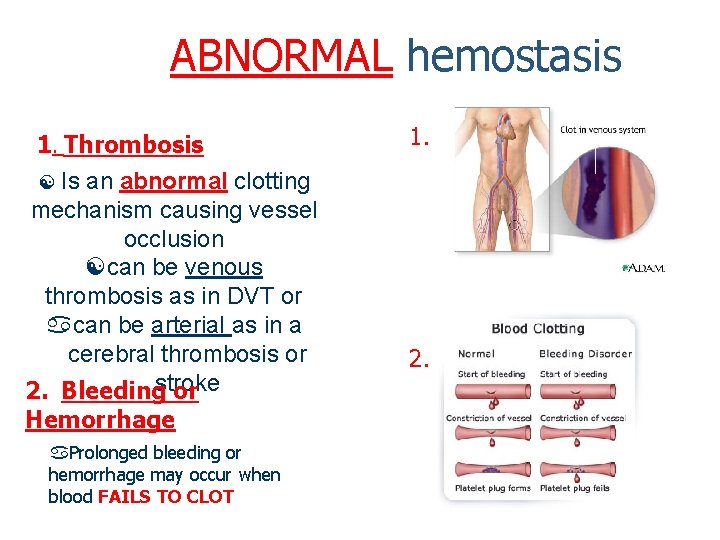
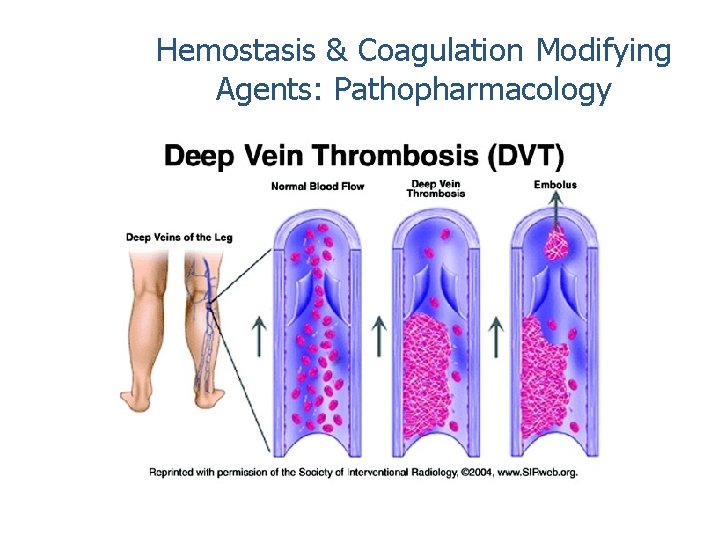
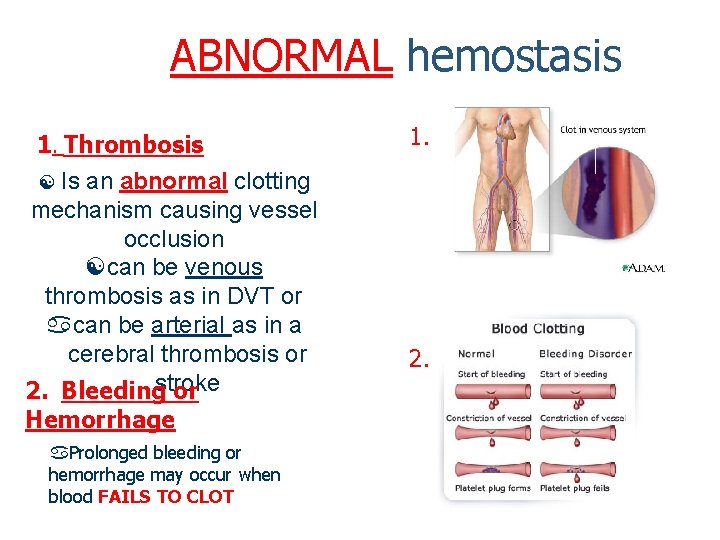
ABNORMAL hemostasis 1. Thrombosis Is an abnormal clotting mechanism causing vessel occlusion can be venous thrombosis as in DVT or can be arterial as in a cerebral thrombosis or 2. Bleedingstroke or Hemorrhage Prolonged bleeding or hemorrhage may occur when blood FAILS TO CLOT 1. 2.
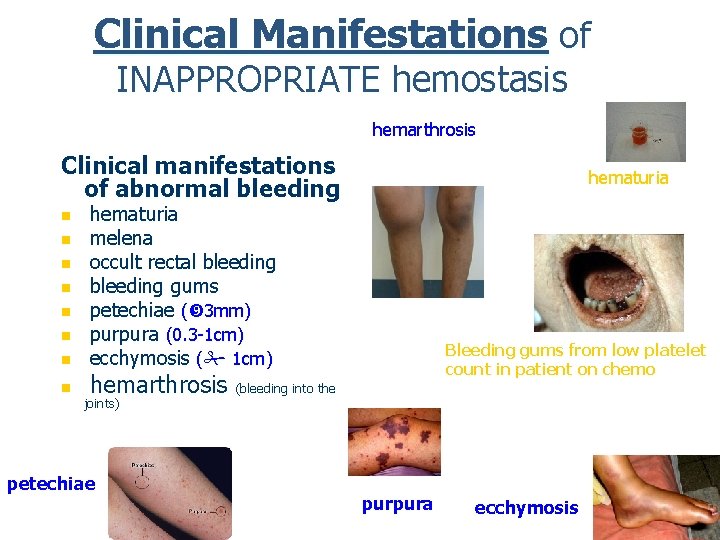
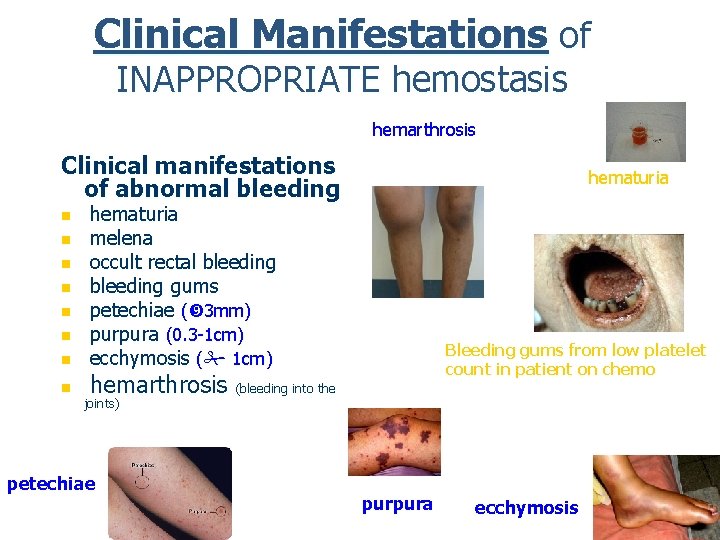
Clinical Manifestations of INAPPROPRIATE hemostasis hemarthrosis Clinical manifestations of abnormal bleeding n n n n hematuria melena occult rectal bleeding gums petechiae ( 3 mm) purpura (0. 3 -1 cm) ecchymosis ( 1 cm) Bleeding gums from low platelet count in patient on chemo hemarthrosis (bleeding into the joints) petechiae purpura ecchymosis
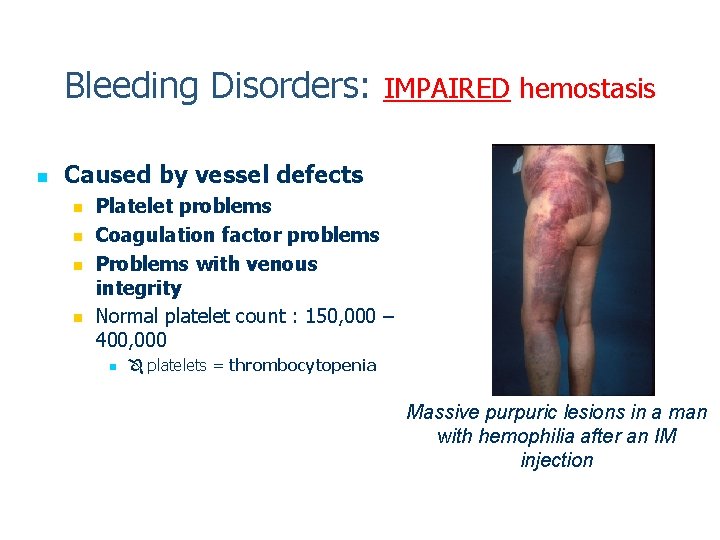
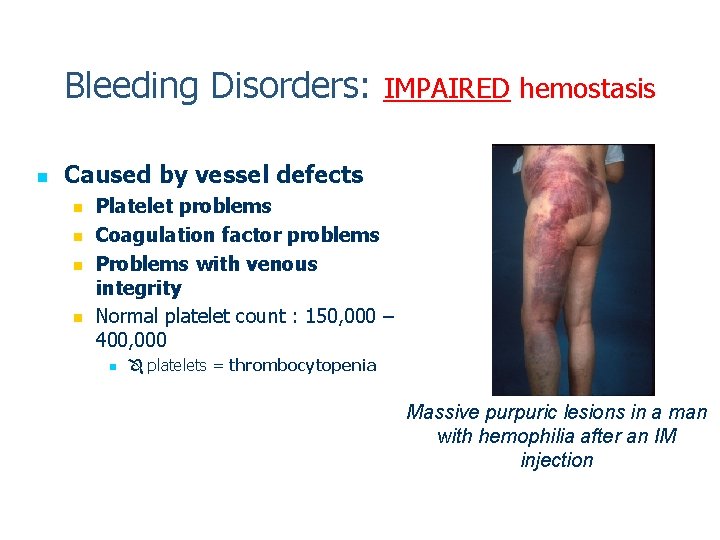
Bleeding Disorders: IMPAIRED hemostasis n Caused by vessel defects n n Platelet problems Coagulation factor problems Problems with venous integrity Normal platelet count : 150, 000 – 400, 000 n platelets = thrombocytopenia Massive purpuric lesions in a man with hemophilia after an IM injection
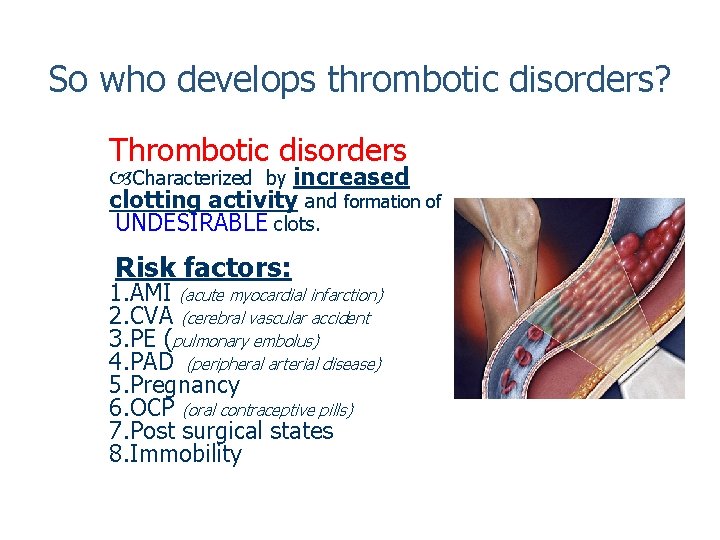
So who develops thrombotic disorders? Thrombotic disorders Characterized by increased clotting activity and formation of UNDESIRABLE clots. Risk factors: 1. AMI (acute myocardial infarction) 2. CVA (cerebral vascular accident 3. PE (pulmonary embolus) 4. PAD (peripheral arterial disease) 5. Pregnancy 6. OCP (oral contraceptive pills) 7. Post surgical states 8. Immobility
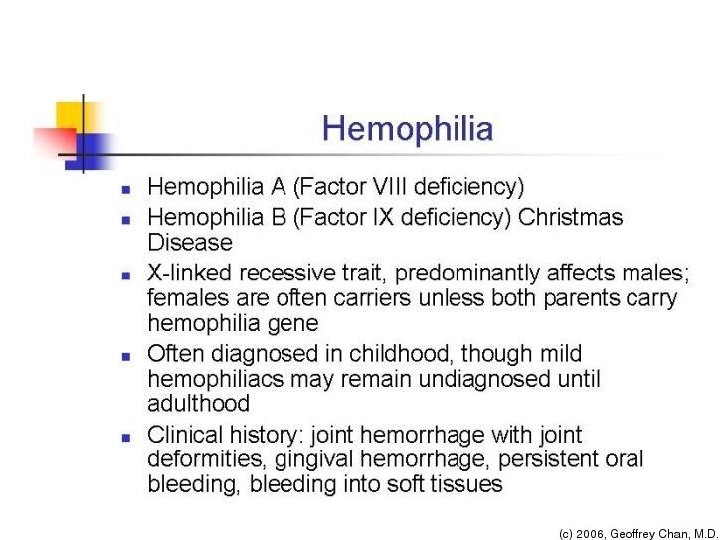
Common Diseases of hemostasis: n Bleeding disorders Characterized by ABNORMAL clot formation. n Thrombocytopenia n a common bleeding disorder resulting form a deficiency of platelets. Can result from any conditions that suppresses bone marrow function n Liver n n disorders impaired synthesis of clotting factors may occur Decreased levels of vit K can impair hemostasis n Hemophilia n bleeding disorders caused by genetic deficiencies in certain clotting factors
Platelet Defect: thrombocytopenia n Thrombocytopenia results from: n A decrease in platelet production by the bone marrow A pooling of platelets in the spleen Decreased platelet survival n CAN BE AN ADVERSE EFFECT OF DRUGS n Can be genetic n n n CAN BE IDIOPATHIC (idiopathic thrombocytopenia purpura) (ITP)
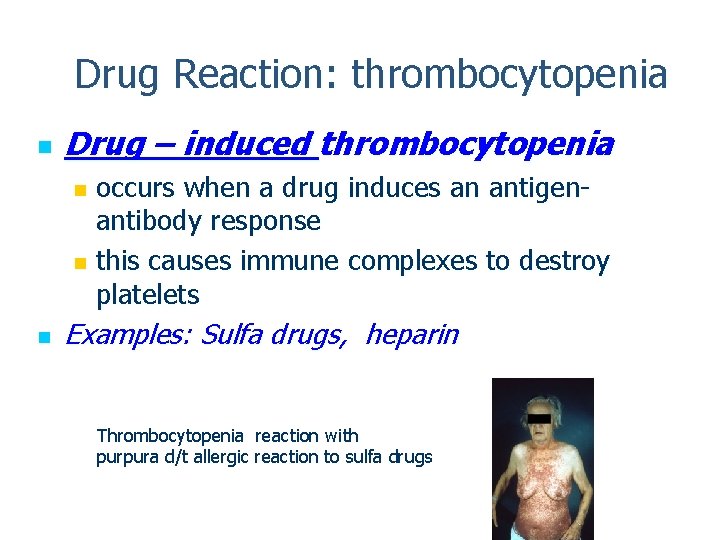
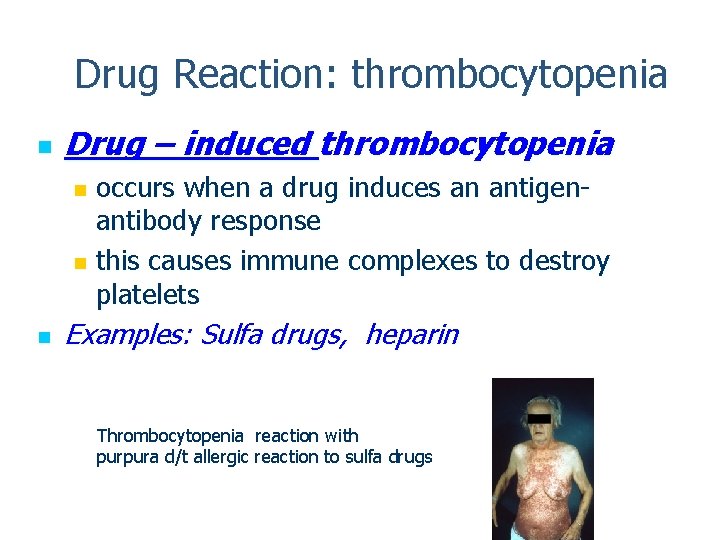
Drug Reaction: thrombocytopenia n Drug – induced thrombocytopenia occurs when a drug induces an antigenantibody response n this causes immune complexes to destroy platelets n n Examples: Sulfa drugs, heparin Thrombocytopenia reaction with purpura d/t allergic reaction to sulfa drugs
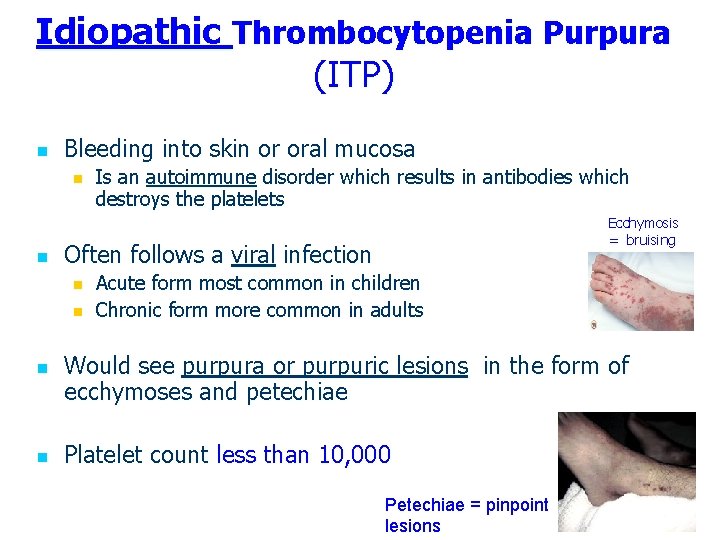
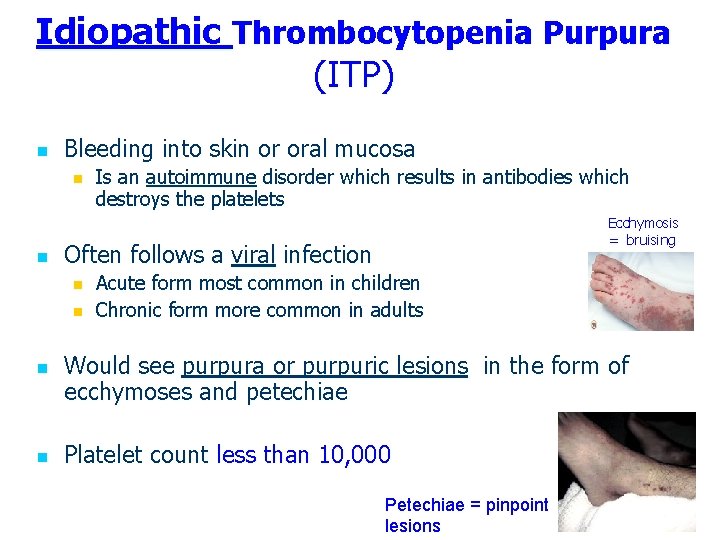
Idiopathic Thrombocytopenia Purpura (ITP) n Bleeding into skin or oral mucosa n n Ecchymosis = bruising Often follows a viral infection n n Is an autoimmune disorder which results in antibodies which destroys the platelets Acute form most common in children Chronic form more common in adults Would see purpura or purpuric lesions in the form of ecchymoses and petechiae Platelet count less than 10, 000 Petechiae = pinpoint lesions
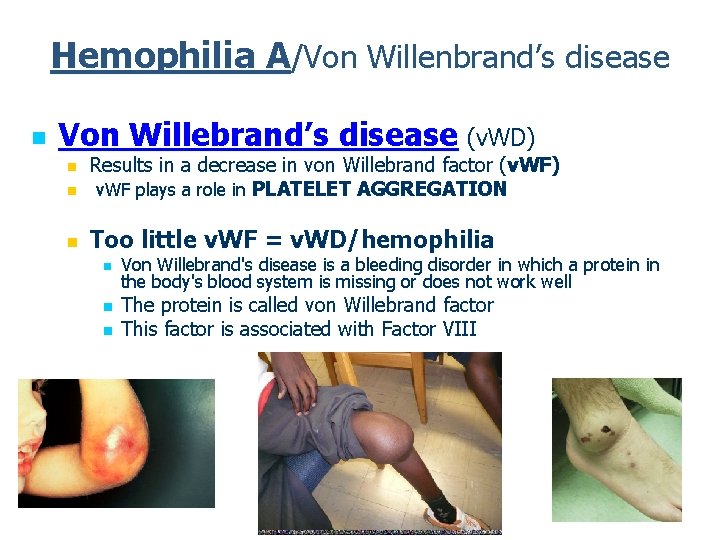
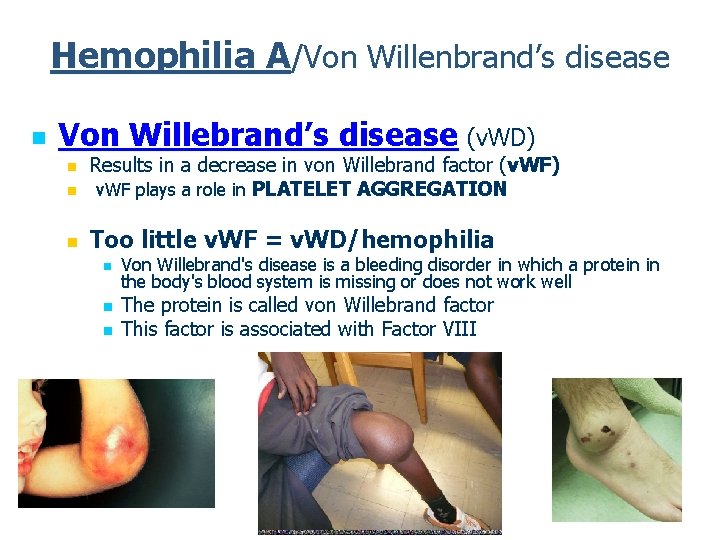
Hemophilia A/Von Willenbrand’s disease n Von Willebrand’s disease (v. WD) n Results in a decrease in von Willebrand factor (v. WF) v. WF plays a role in PLATELET AGGREGATION n Too little v. WF = v. WD/hemophilia n n Von Willebrand's disease is a bleeding disorder in which a protein in the body's blood system is missing or does not work well The protein is called von Willebrand factor This factor is associated with Factor VIII
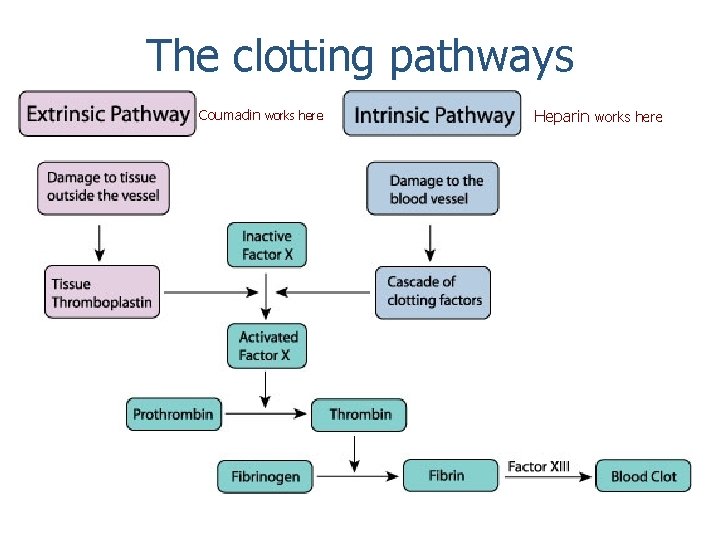
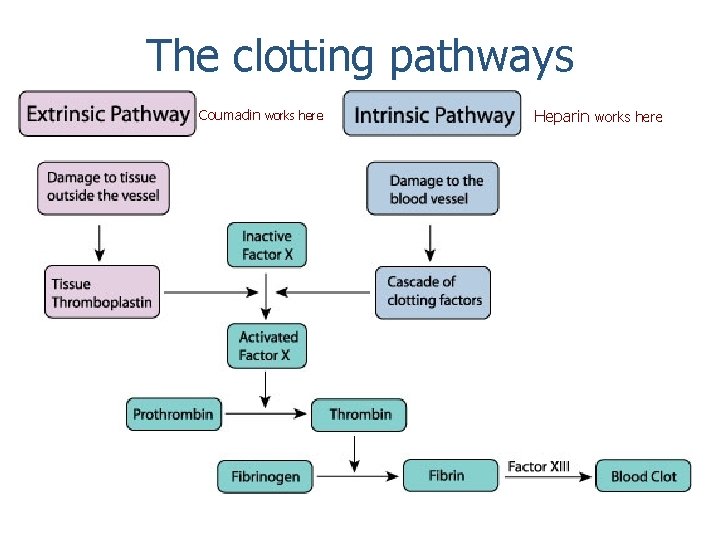
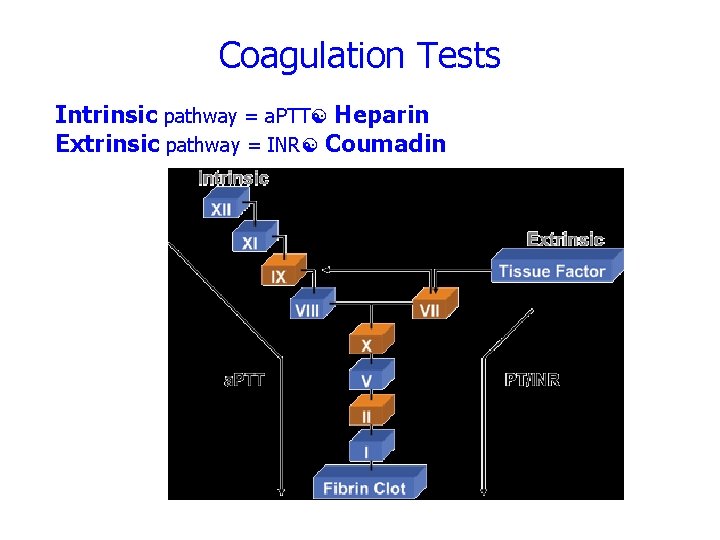
The clotting pathways Coumadin works here Heparin works here
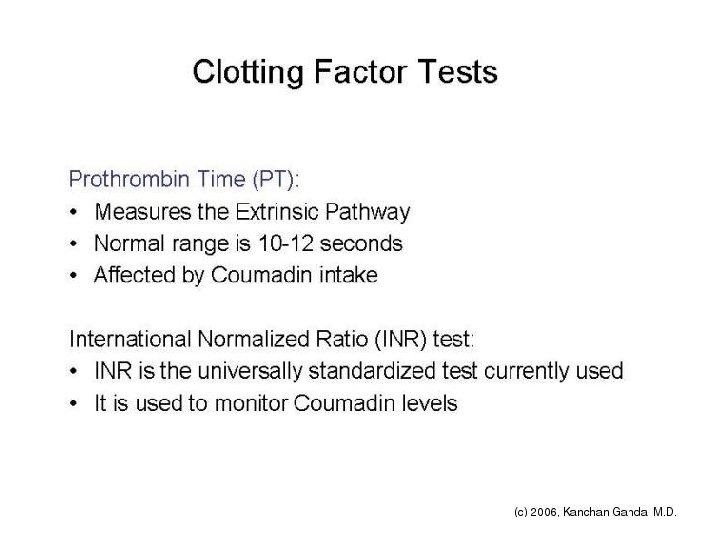
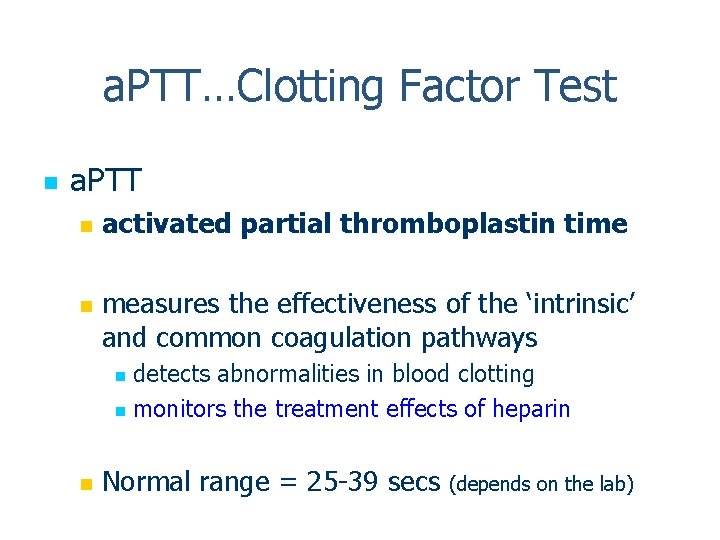
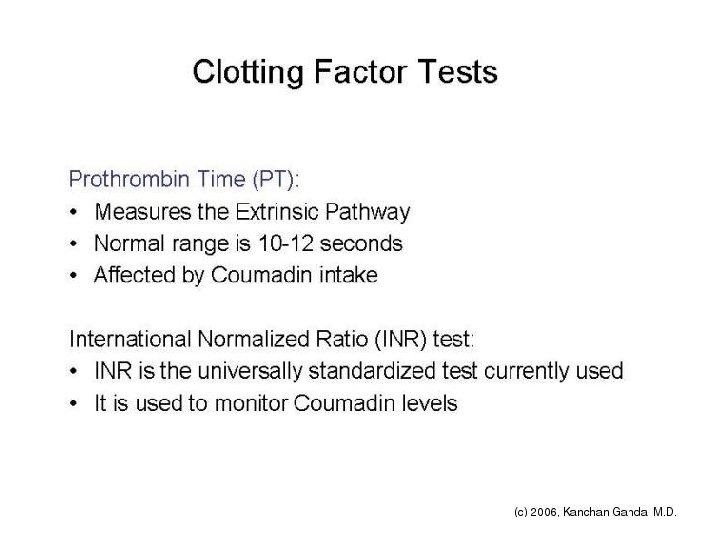
a. PTT…Clotting Factor Test n a. PTT n n activated partial thromboplastin time measures the effectiveness of the ‘intrinsic’ and common coagulation pathways detects abnormalities in blood clotting n monitors the treatment effects of heparin n n Normal range = 25 -39 secs (depends on the lab)
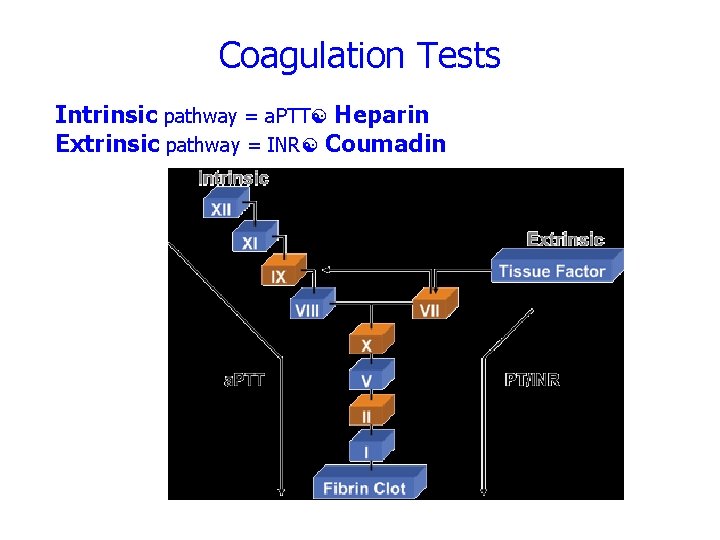
Coagulation Tests Intrinsic pathway = a. PTT Heparin Extrinsic pathway = INR Coumadin
Summary Slide: Heparin n HEPARIN n n Heparin PRIMARILY works by inactivating thrombin and factor Xa to ultimately suppress formation of fibrin Since fibrin forms the framework of thrombi in VEINS, of venous thrombi (DVT, PE) Works quickly (within minutes of IV administration) Used primarily in the acute care for treatment of DVT, PE, and to achieve quick anticoagulation prior to long term coumadin use
SUMMARY SLIDE: COUMADIN Coumadin PRIMARILY works by decreasing the production of certain clotting factors (VII, IX, X, and prothrombin) These clotting factors are dependent on Vitamin K "vitamin K dependent clotting factors“ Coumadin decreases the production of vitamin K -dependent clotting factors by 30 -50% It takes DAYS for the full effect of Coumadin to be seen because Coumadin does not affect clotting factors already in circulation Coumadin is used for long-term prophylaxis of thrombosis
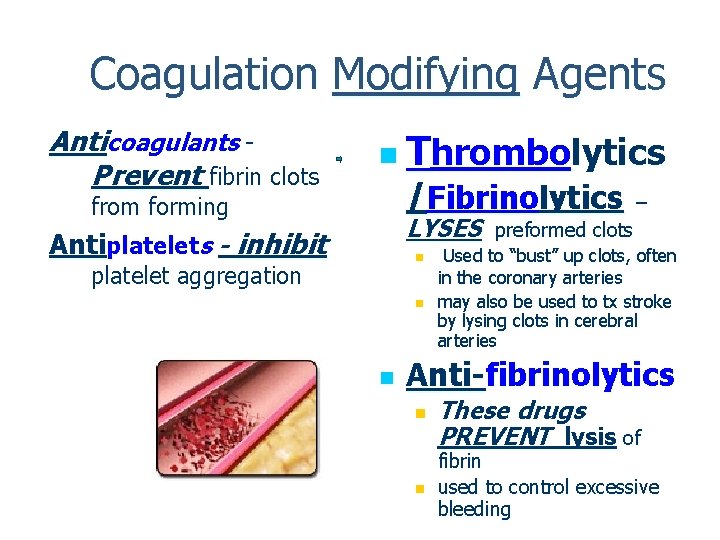
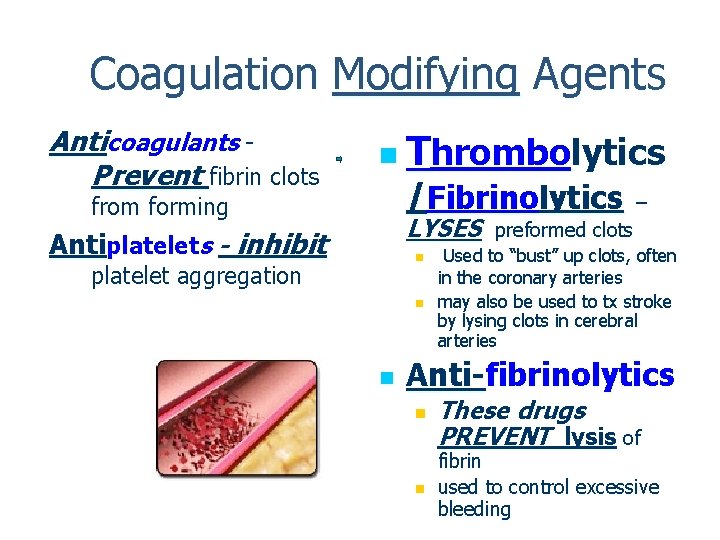
Coagulation Modifying Agents Anticoagulants Prevent fibrin clots n Thrombolytics /Fibrinolytics from forming LYSES Antiplatelets - inhibit n platelet aggregation n n – preformed clots Used to “bust” up clots, often in the coronary arteries may also be used to tx stroke by lysing clots in cerebral arteries Anti-fibrinolytics n n These drugs PREVENT lysis of fibrin used to control excessive bleeding
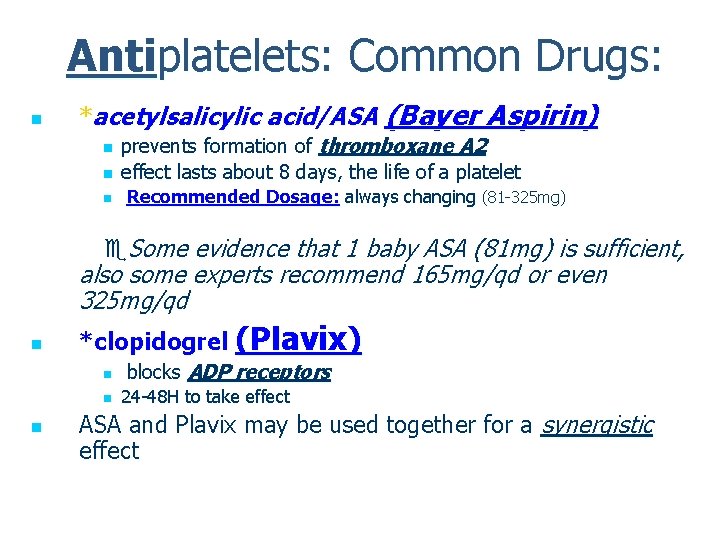
Antiplatelets: Common Drugs: n *acetylsalicylic acid/ASA (Bayer Aspirin) n n n prevents formation of thromboxane A 2 effect lasts about 8 days, the life of a platelet Recommended Dosage: always changing (81 -325 mg) Some evidence that 1 baby ASA (81 mg) is sufficient, also some experts recommend 165 mg/qd or even 325 mg/qd n *clopidogrel (Plavix) n n n blocks ADP receptors 24 -48 H to take effect ASA and Plavix may be used together for a synergistic effect
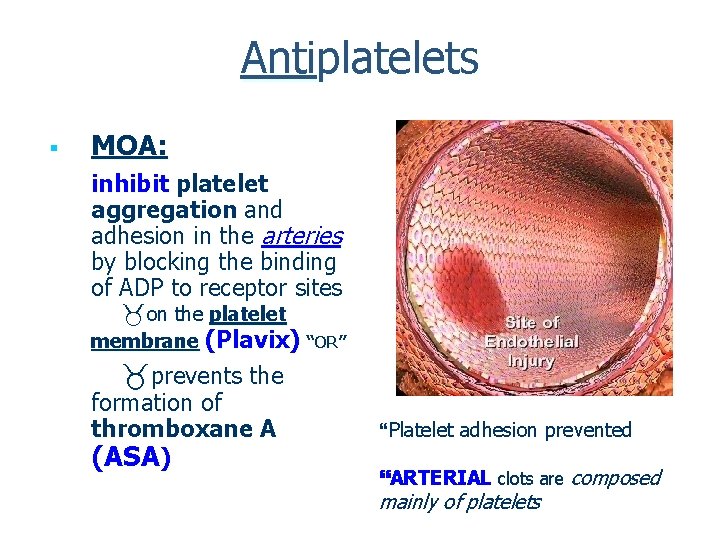
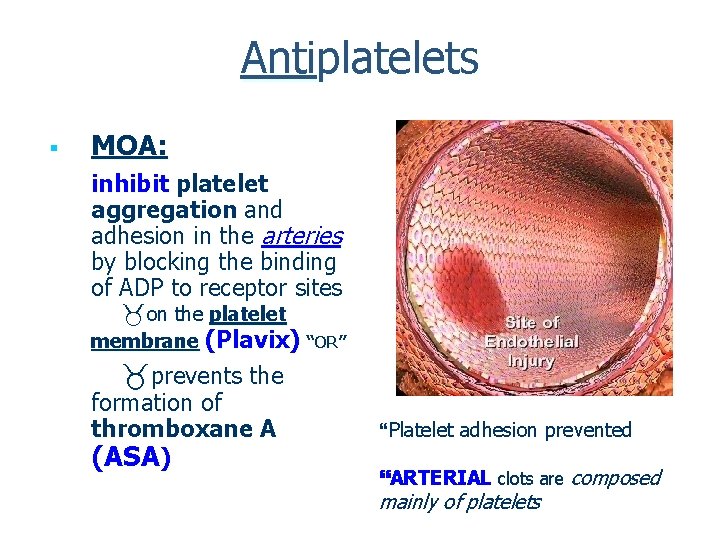
Antiplatelets § MOA: inhibit platelet aggregation and adhesion in the arteries by blocking the binding of ADP to receptor sites on the platelet membrane (Plavix) “OR” prevents the formation of thromboxane A (ASA) Platelet adhesion prevented ARTERIAL clots are composed mainly of platelets
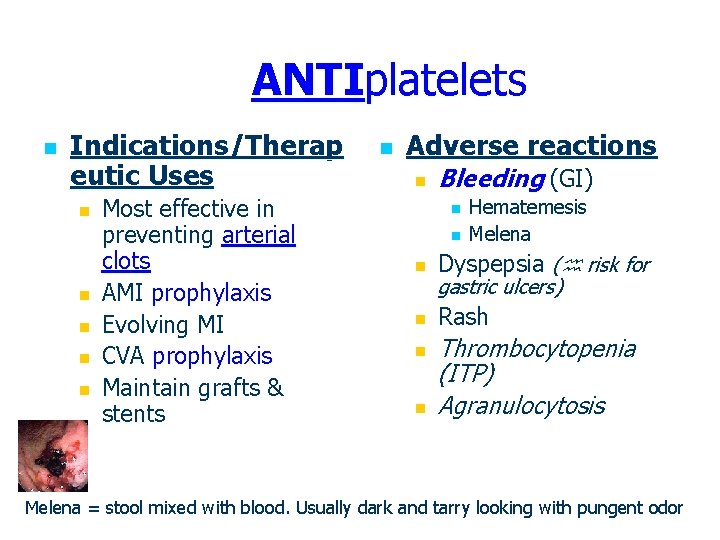
ANTIplatelets n Indications/Therap eutic Uses n n n Most effective in preventing arterial clots AMI prophylaxis Evolving MI CVA prophylaxis Maintain grafts & stents n Adverse reactions n Bleeding (GI) n n Hematemesis Melena n Dyspepsia ( risk for n Rash n n gastric ulcers) Thrombocytopenia (ITP) Agranulocytosis Melena = stool mixed with blood. Usually dark and tarry looking with pungent odor
Antiplatelets n Interactions n n n risk of bleeding if combined with other drugs affecting clotting ASA and NSAIDS can potentiate bleeding absorption with antacids n Contraindications n Allergy Pregnancy/lactation n Vit K deficiency n PUD (peptic ulcer disease) n Asthma n n Children under 12 yrs with flu-like sx ( risk for Reye’s syndrome) Nursing Alert – hold for 7 days before surgery or dental procedure unless ordered otherwise by MD
Anticoagulants n n Drugs which prevent the formation of a clot Anticoagulants are only given PROPHYLACTICALLY n They have no affect on already formed clots, but can prevent new clots from forming or prevent the extension of an already formed clot or thrombus
Contraindications for anticoagulants Ø Any condition that could be compromised by bleeding tendencies: recent trauma, GI ulcers, recent surgery: Ø Renal disease ( erythropoietin = RBCs) Ø Hepatic disease ( vitamin K = bleeding) Ø Peptic Ulcer Ø Hemophilia ( v. WF = bleeding) Ø Client should not take concurrent ASA unless Rx by MD
Oral Anticoagulants n MOA: Interferes with the formation of vitamin K dependent clotting factors in the liver n n **Prototype drug – n n The eventual effect is a depletion of clotting factors and a prolongation of clotting times warfarin (Coumadin) Half-life 0. 5 – 3 days Remember: it takes 3 -5 half-lives to reach a steady state (therapeutic level) n So therapeutic level not achieved for 3 -5 days with coumadin
Coumadin: Therapeutic Uses n n Most effective against venous thrombosis Prevent clot (prophylaxis) or prevent the extension of a blood clot 1. 2. 3. 4. 5. 6. 7. DVT PE CAD/AMI A-fib Prophylaxis in patients with artificial heart valves Major surgery (orthopedic) Immobilized patients
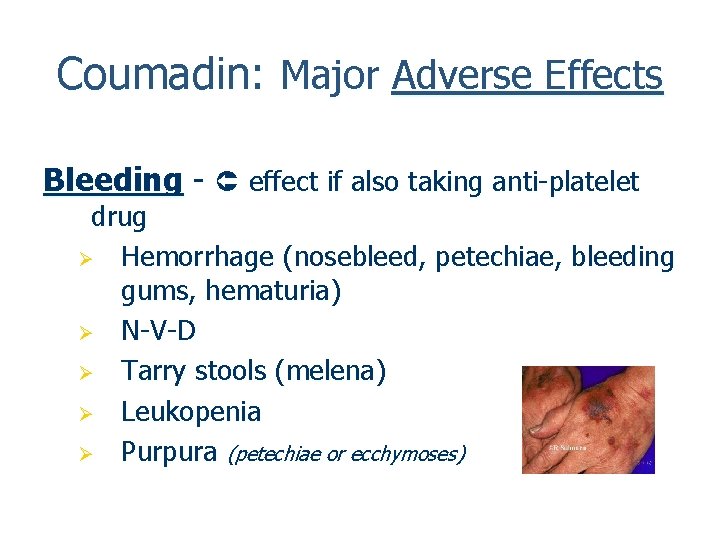
Coumadin: Major Adverse Effects Bleeding - effect if also taking anti-platelet drug Ø Hemorrhage (nosebleed, petechiae, bleeding gums, hematuria) Ø N-V-D Ø Tarry stools (melena) Ø Leukopenia Ø Purpura (petechiae or ecchymoses)
Coumadin: Interactions n *Coumadin has documented drug-drug interactions with a vast number of other drugs! n n n It is very highly protein bound (99%) HAS A VERY NARROW THERAPEUTIC INDEX Requires lab monitoring to establish safe and effective dose (INR) n n Known to interact with herbs ginkgo and ginseng causing increased bleeding times Cranberry juice risk of bleeding
Coumadin: Nursing Implications n n Assess for bleeding Monitor prothrombin time (PT) & international normalized ratio (INR)= PT/INR n Normally the GOAL is for the INR to be 2 -3 X normal to achieve the desired anticoagulation effect (see handout) n The effect of coumadin may last for up to 10 days after discontinuation of therapy
Coumdin: Nursing Implications/ Patient Teaching n Instruct the clients to: n Do not take ASA, ibuprofen or other NSAIDS (unless directed by their physician) n Acetaminophen/Tylenol OK n Avoid trauma n Wear medical alert bracelet n Consult MD prior to OTC drugs n Avoid dietary changes of foods high in Vit K (leafy green veggies) n VITAMIN K CONSISTENT DIET
Coumadin: Nursing Implications/ Patient Teaching n Avoid ASA unless Rx by MD n Report S & S of bleeding n Monitor PT/INR (get routine labs drawn!) n Continue bleeding precautions for appox 10 days after last dose n n Avoid IM injections if possible Antidote = vitamin n n K /Aqua Mephyton (po or IM) May be ordered if INR is too high (more than 3 times normal) and bleeding is present It takes about 6 H for the antidote to have an effect on bleeding
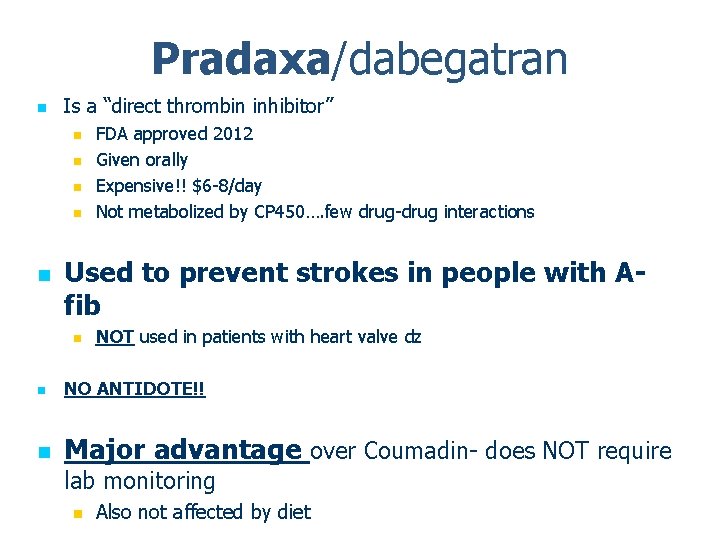
Pradaxa/dabegatran n Is a “direct thrombin inhibitor” n n n FDA approved 2012 Given orally Expensive!! $6 -8/day Not metabolized by CP 450…. few drug-drug interactions Used to prevent strokes in people with Afib n NOT used in patients with heart valve dz n NO ANTIDOTE!! n Major advantage over Coumadin- does NOT require lab monitoring n Also not affected by diet
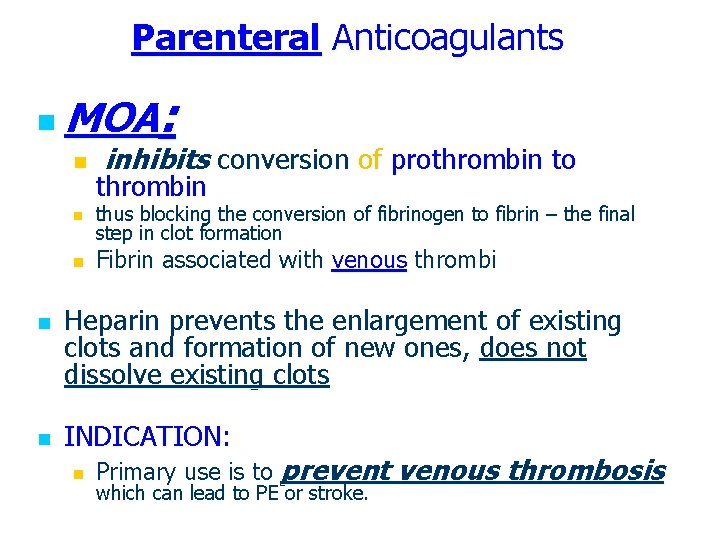
Parenteral Anticoagulants : n MOA n n n inhibits conversion of prothrombin to thrombin thus blocking the conversion of fibrinogen to fibrin – the final step in clot formation Fibrin associated with venous thrombi Heparin prevents the enlargement of existing clots and formation of new ones, does not dissolve existing clots INDICATION: n Primary use is to prevent venous thrombosis which can lead to PE or stroke.
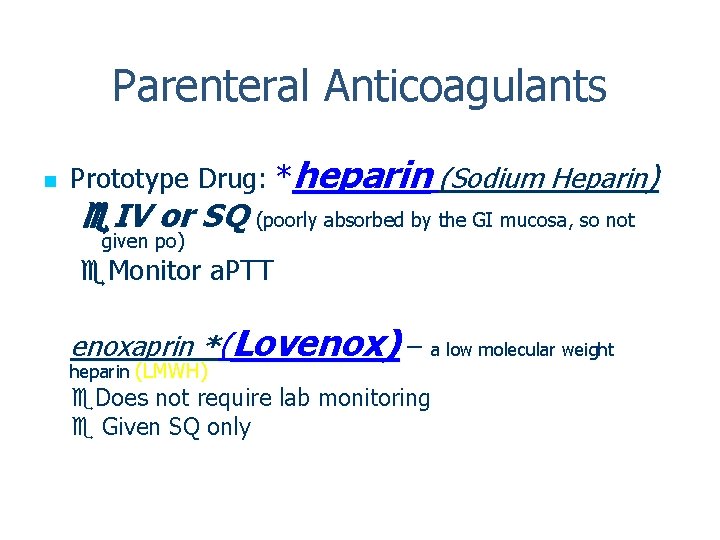
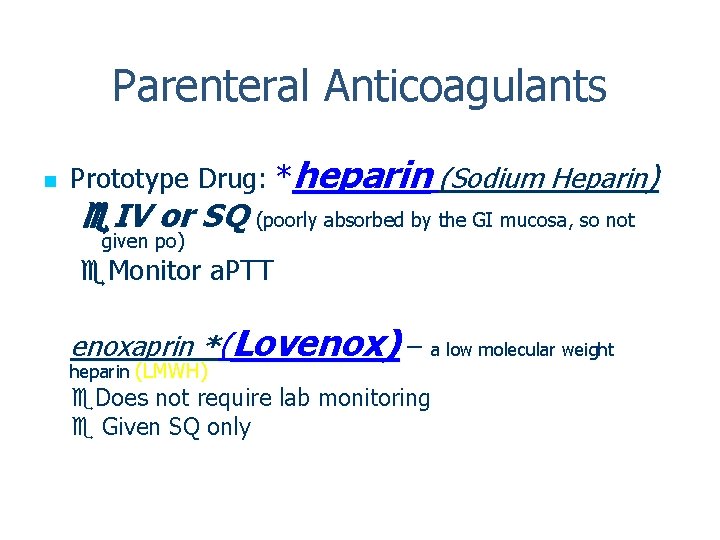
Parenteral Anticoagulants n Prototype Drug: *heparin (Sodium Heparin) IV or SQ (poorly absorbed by the GI mucosa, so not given po) Monitor a. PTT enoxaprin *(Lovenox) – a low molecular weight heparin (LMWH) Does not require lab monitoring Given SQ only
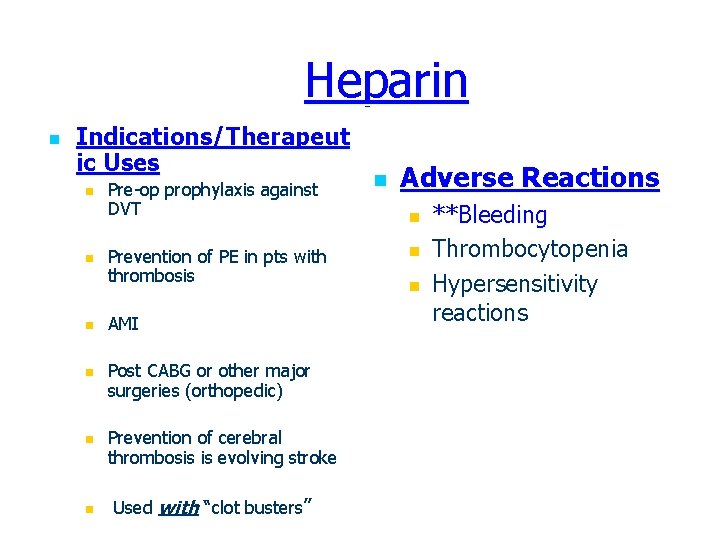
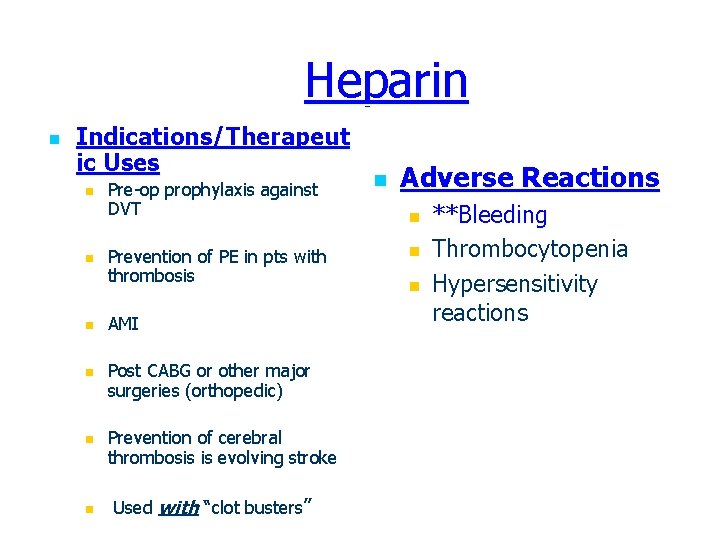
Heparin n Indications/Therapeut ic Uses n n n Pre-op prophylaxis against DVT Prevention of PE in pts with thrombosis AMI Post CABG or other major surgeries (orthopedic) Prevention of cerebral thrombosis is evolving stroke Used with “clot busters” n Adverse Reactions n n n **Bleeding Thrombocytopenia Hypersensitivity reactions
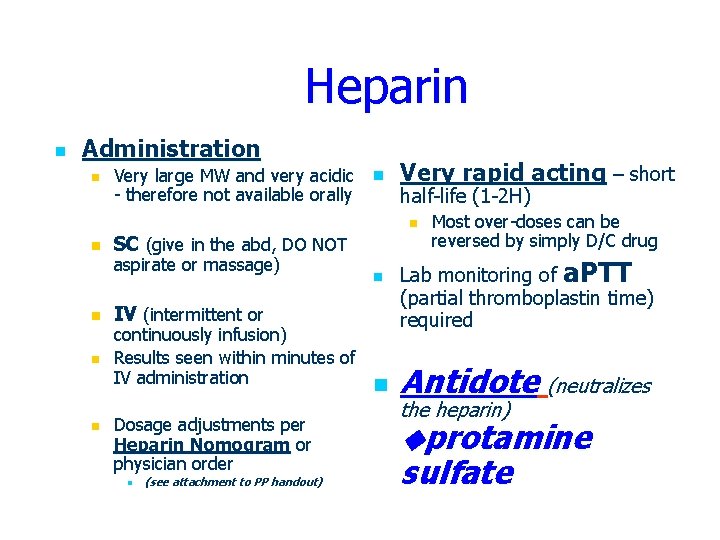
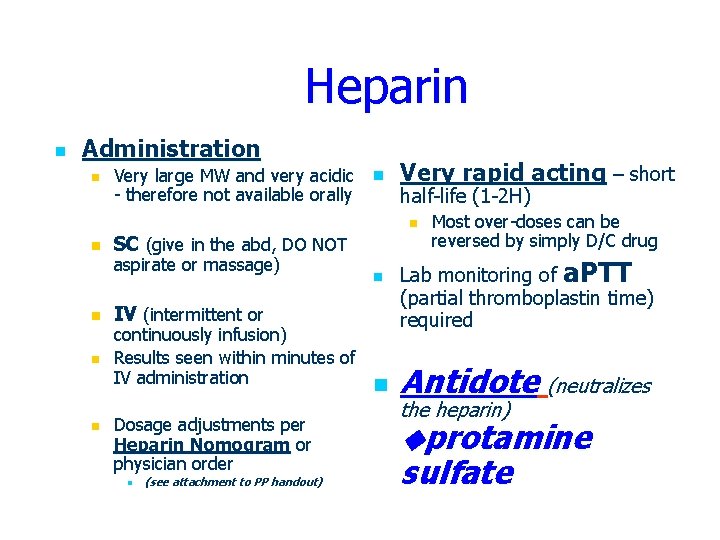
Heparin n Administration n Very large MW and very acidic - therefore not available orally n Very rapid acting – short half-life (1 -2 H) n n n SC (give in the abd, DO NOT aspirate or massage) IV (intermittent or n continuously infusion) Results seen within minutes of IV administration n Dosage adjustments per Heparin Nomogram or physician order n (see attachment to PP handout) Most over-doses can be reversed by simply D/C drug Lab monitoring of a. PTT (partial thromboplastin time) required Antidote (neutralizes the heparin) protamine sulfate
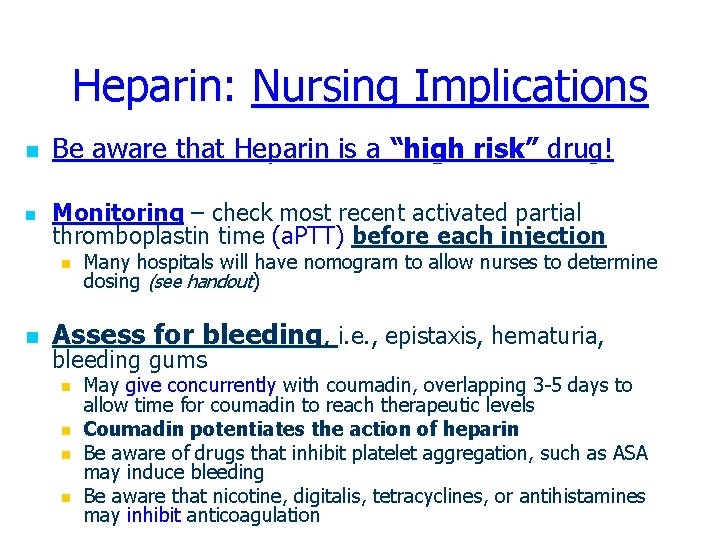
Heparin: Nursing Implications n Be aware that Heparin is a “high risk” drug! n Monitoring – check most recent activated partial thromboplastin time (a. PTT) before each injection n n Many hospitals will have nomogram to allow nurses to determine dosing (see handout) Assess for bleeding, i. e. , epistaxis, hematuria, bleeding gums n n May give concurrently with coumadin, overlapping 3 -5 days to allow time for coumadin to reach therapeutic levels Coumadin potentiates the action of heparin Be aware of drugs that inhibit platelet aggregation, such as ASA may induce bleeding Be aware that nicotine, digitalis, tetracyclines, or antihistamines may inhibit anticoagulation
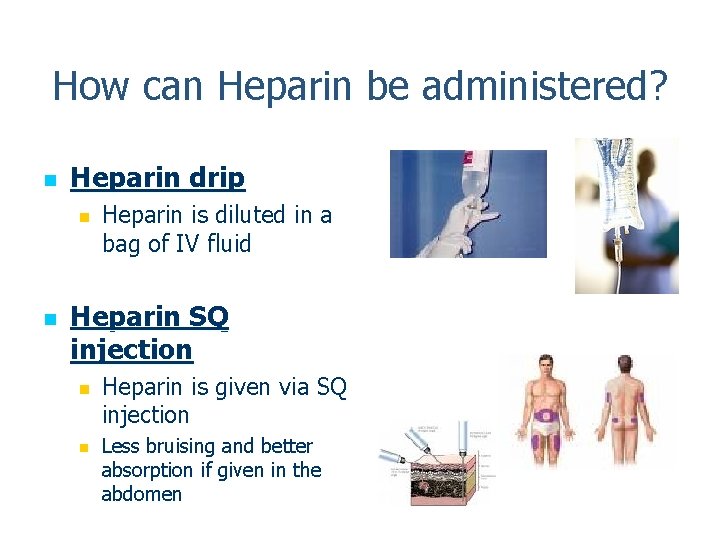
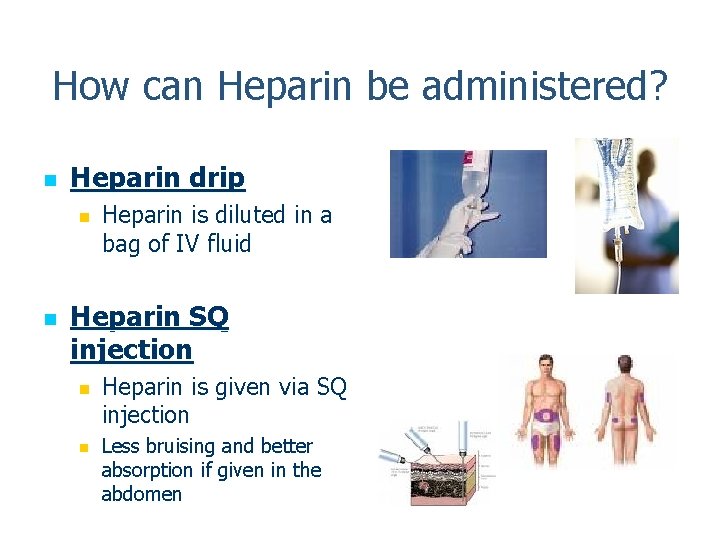
How can Heparin be administered? n Heparin drip n n Heparin is diluted in a bag of IV fluid Heparin SQ injection n n Heparin is given via SQ injection Less bruising and better absorption if given in the abdomen
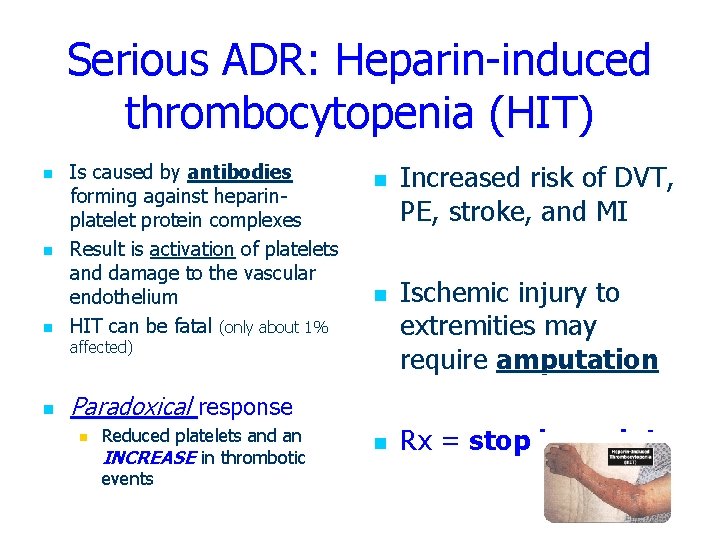
Serious ADR: Heparin-induced thrombocytopenia (HIT) n n n Is caused by antibodies forming against heparinplatelet protein complexes Result is activation of platelets and damage to the vascular endothelium HIT can be fatal (only about 1% n n affected) n Increased risk of DVT, PE, stroke, and MI Ischemic injury to extremities may require amputation Paradoxical response n Reduced platelets and an INCREASE in thrombotic events n Rx = stop heparin!
enoxaprin (Lovenox). . . a heparin derivative drug n MOA: same as heparin/ prevention of thrombus formation. Prevention of extension of existing thrombi n n Advantage: Is a low molecular weight form of heparin and does not require monitoring of PTT Antidote: protamine sulfate
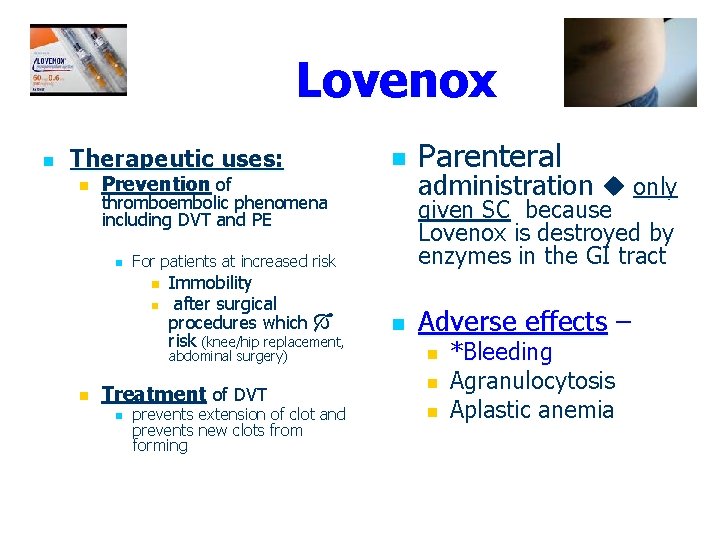
Lovenox n Therapeutic uses: n Prevention of thromboembolic phenomena including DVT and PE n n Immobility after surgical procedures which risk (knee/hip replacement, abdominal surgery) Treatment of DVT n prevents extension of clot and prevents new clots from forming Parenteral administration only given SC because Lovenox is destroyed by enzymes in the GI tract For patients at increased risk n n Adverse effects – n n n *Bleeding Agranulocytosis Aplastic anemia
Thrombolytic/Fibrinolytic Agents n MOA: n n DISSOLVES the clot by converting plaminogen to plasmin this lyses the thrombi and fibrinogen, destroying the fibrin clot n n n first used to re-establish blood to starved heart muscle in clients having an AMI Also known as “Clot Busters” Fibrinolysis – the process by which a clot dissovles n Plasmin “digests” the clot
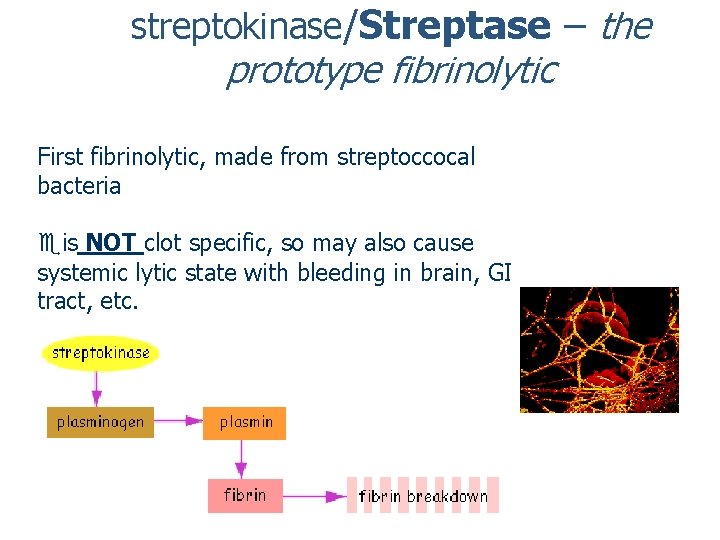
streptokinase/Streptase – the prototype fibrinolytic First fibrinolytic, made from streptoccocal bacteria is NOT clot specific, so may also cause systemic lytic state with bleeding in brain, GI tract, etc.
Fibrinolytics n Common drugs: n t. PA (tissue plasminogen activator) =(Alteplase ) (from recombinant DNA) Therapeutic uses: n n n AMI (window of less than 6 H from SX onset) CVA (window 3 H from sx onset) DVT PE Occluded central venous access devices (PICC) Widely used since 1980’s to Rx acute MI with decrease in morality rate by 50%
Tissue Plasminogen Activator n t. PA also known as Alteplase n A naturally ocurring plasminogen activator secreted by vascular n n n Much more expensive than streptokinase ($2, 750 vs $540) Given via IV infusion OR directly into occluded coronary or cerebral artery n n endothelial cells Now made through recombinant DNA Approved (FDA 1996) for treatment of ischemic stroke (streptokinase is not) 3 H window after onset of sx for CVA and 6 H for MI
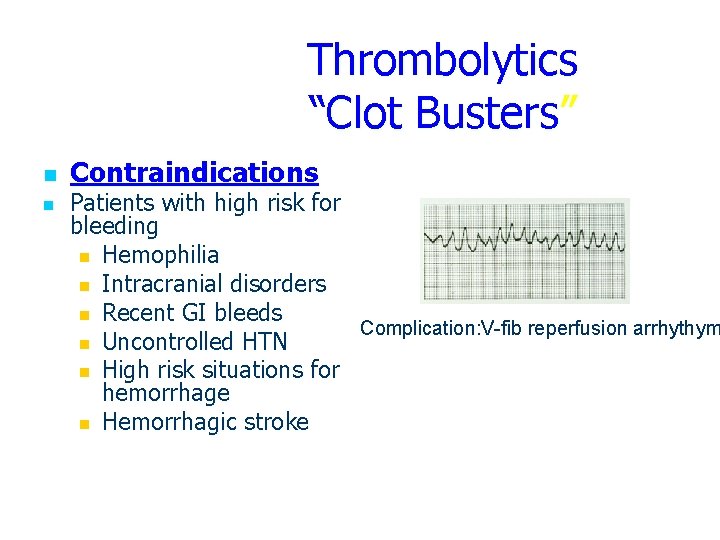
Thrombolytics “Clot Busters” n n Contraindications Patients with high risk for bleeding n Hemophilia n Intracranial disorders n Recent GI bleeds Complication: V-fib reperfusion arrhythym n Uncontrolled HTN n High risk situations for hemorrhage n Hemorrhagic stroke
SE: Thrombolytics n Side Effects/Nursing implications n Screen patients before thrombolytic therapy n * MONITOR FOR BLEEDING n Monitor for anaphylaxis Administer with IV pump n IV bolus followed by drip n Assess for reperfusion arrhythmias n n n Always put pt on heart monitor Monitor B/P – hypotension may occur n Avoid noncompressible IV sites n Give adjunctive therapy (ASA and heparin) n n Usually given with heparin d/t very short half-life Hold pressure for 10 min. after IV D/C n Avoid IM injections
Thrombolytics: nsg implications n n Bleeding risk may persist for 24 H after the infusion is stopped! Antitdote = (aminocaproic acid (Amicar) this drug is an anti-fibriolytic agent
Anti-fibrinolytics n MOA n Prevents the lysis of fibrin promoting clot formation and restoring hemostasis n STOPS THE BLEEDING n * aminocaproic acid (Amicar) n Indications/Therapeutic Uses n Prevent and treat excessive bleeding from surgical complications n n n To stop excessive bleeding from chest tubes and after heart bypass surgery As adjunct therapy in hemophilia ANTIDOTE for fibrinolytics
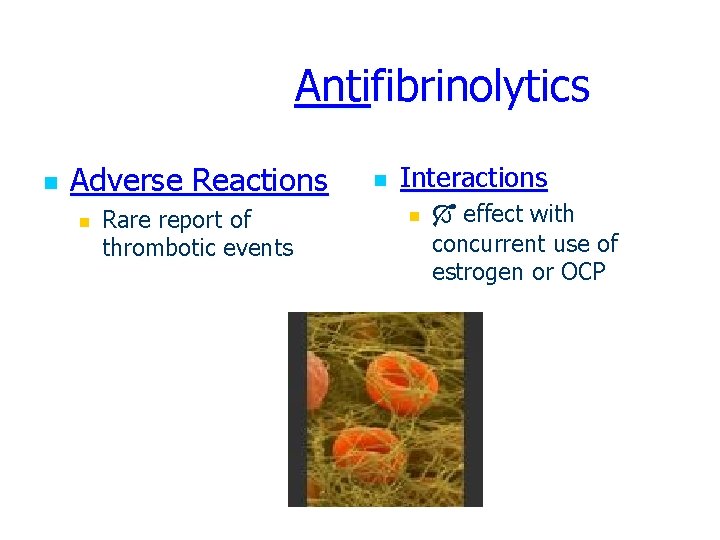
Antifibrinolytics n Adverse Reactions n Rare report of thrombotic events n Interactions n effect with concurrent use of estrogen or OCP
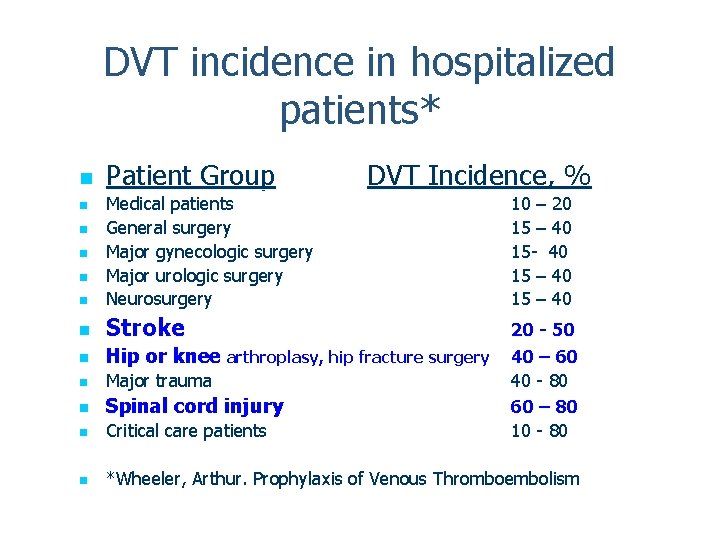
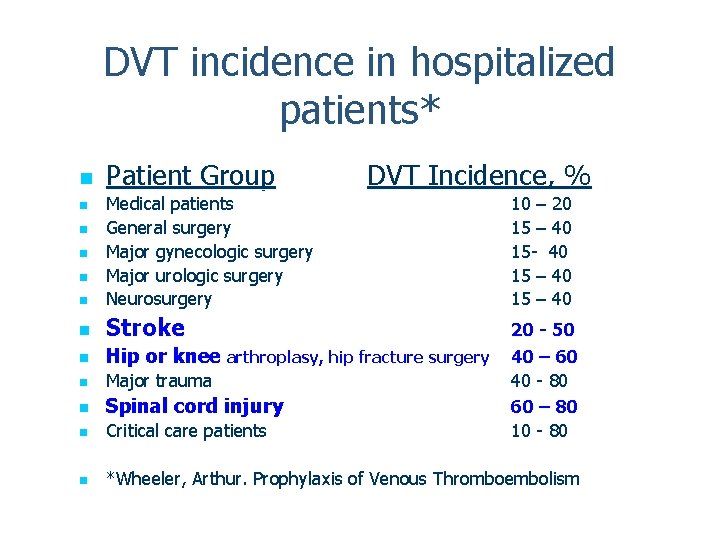
DVT incidence in hospitalized patients* n Patient Group DVT Incidence, % n Medical patients General surgery Major gynecologic surgery Major urologic surgery Neurosurgery 10 – 20 15 – 40 15 - 40 15 – 40 n Stroke n Hip or knee arthroplasy, hip fracture surgery n Major trauma n Spinal cord injury n Critical care patients 20 - 50 40 – 60 40 - 80 60 – 80 10 - 80 n *Wheeler, Arthur. Prophylaxis of Venous Thromboembolism n n