Hemophagocytic Lympho Histiocytosis Case presentation 11 yr old


























- Slides: 79

Hemophagocytic Lympho Histiocytosis
Case presentation 11 yr old boy with CC: §Fever & Headache since 2 wks ago §
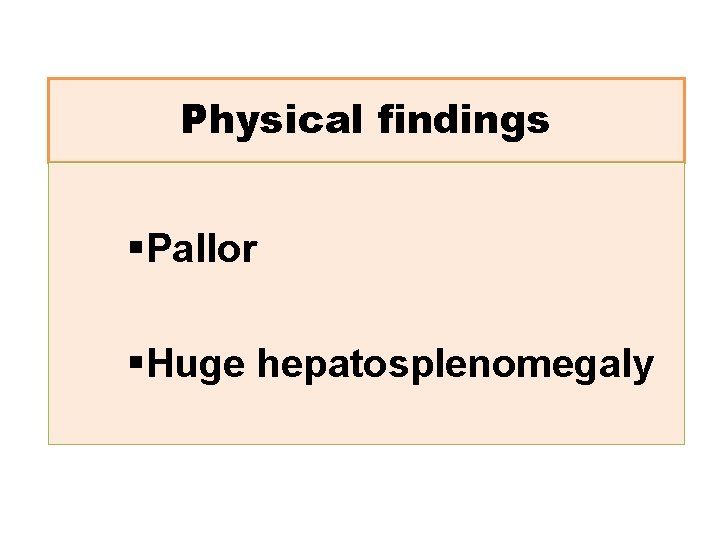
Physical findings §Pallor §Huge hepatosplenomegaly

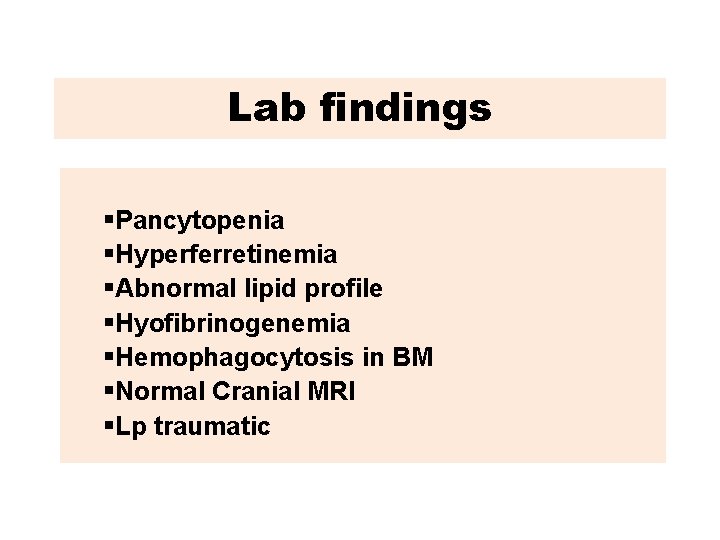
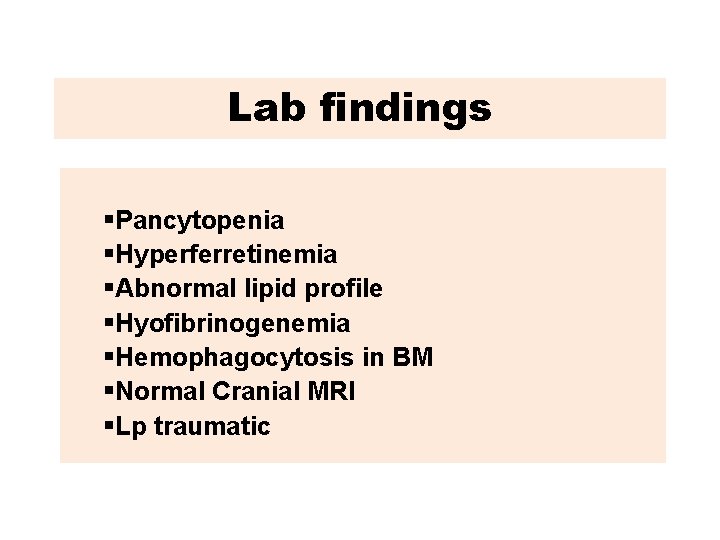
Lab findings §Pancytopenia §Hyperferretinemia §Abnormal lipid profile §Hyofibrinogenemia §Hemophagocytosis in BM §Normal Cranial MRI §Lp traumatic
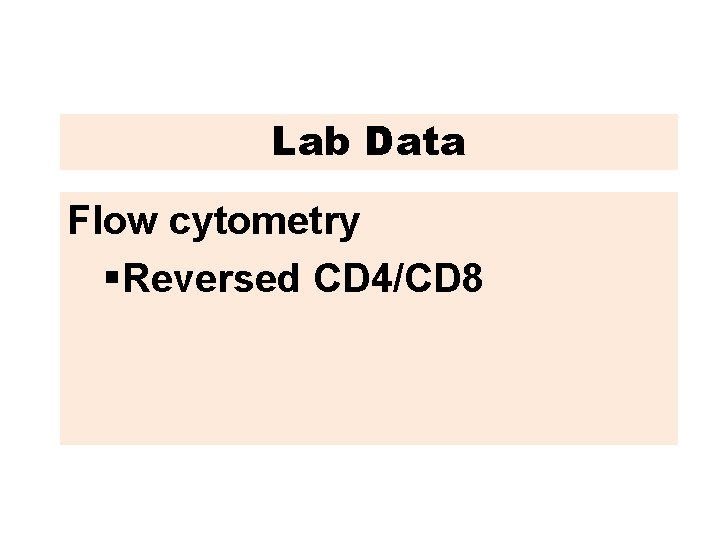
Lab Data Flow cytometryl §Reversed CD 4/CD 8
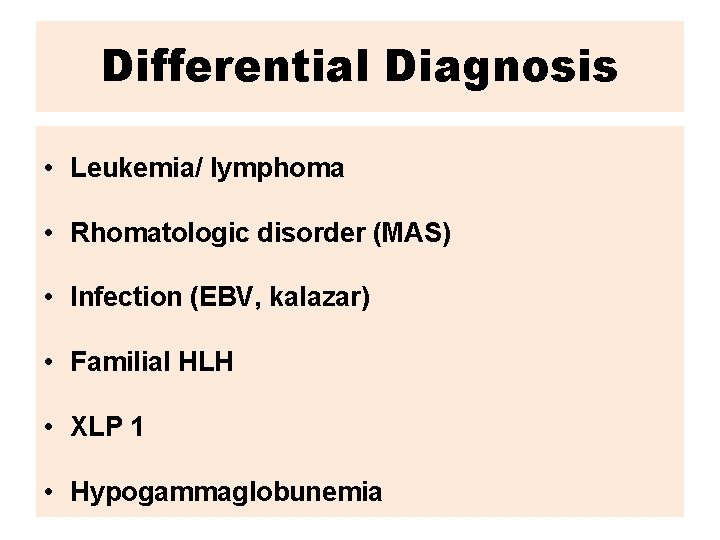
Differential Diagnosis • Leukemia/ lymphoma • Rhomatologic disorder (MAS) • Infection (EBV, kalazar) • Familial HLH • XLP 1 • Hypogammaglobunemia

Diagnosis
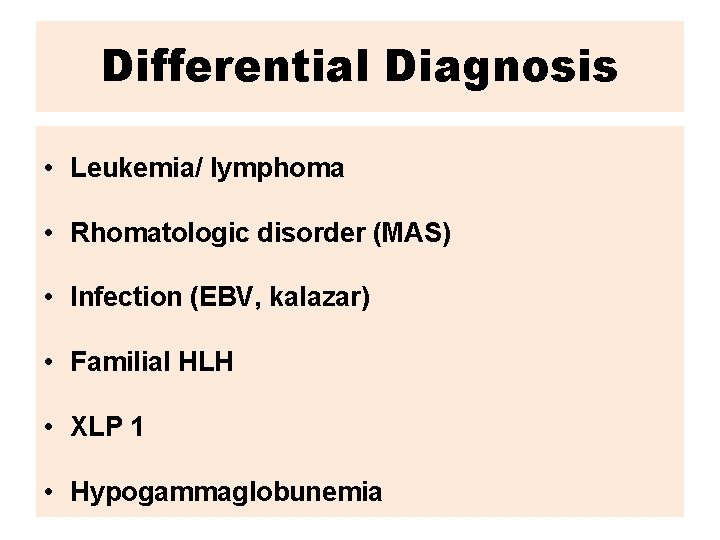
Differential Diagnosis • Leukemia/ lymphoma • Rhomatologic disorder (MAS) • Infection (EBV, kalazar) • Familial HLH • XLP 1 • Hypogammaglobunemia
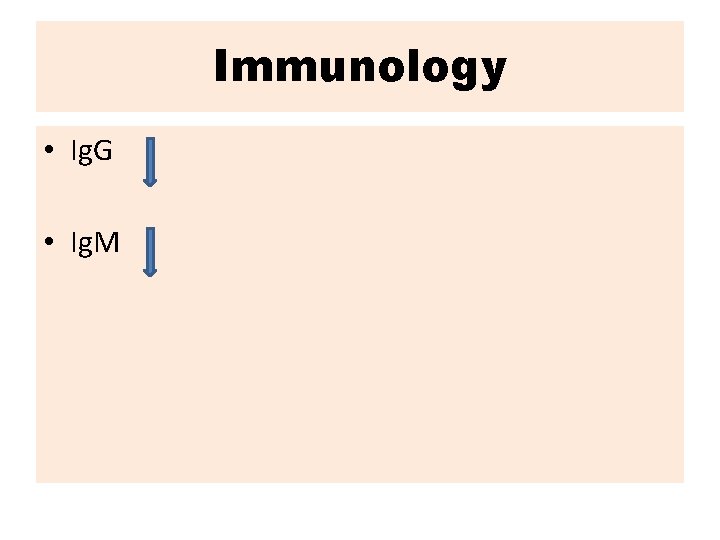
Immunology • Ig. G • Ig. M
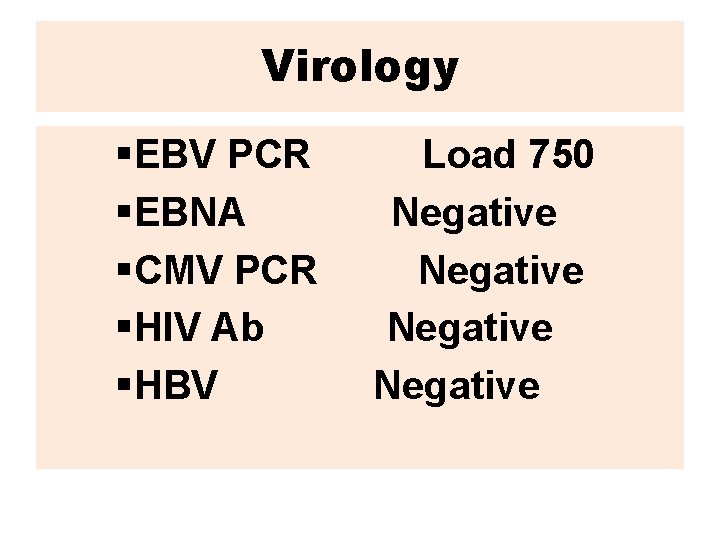
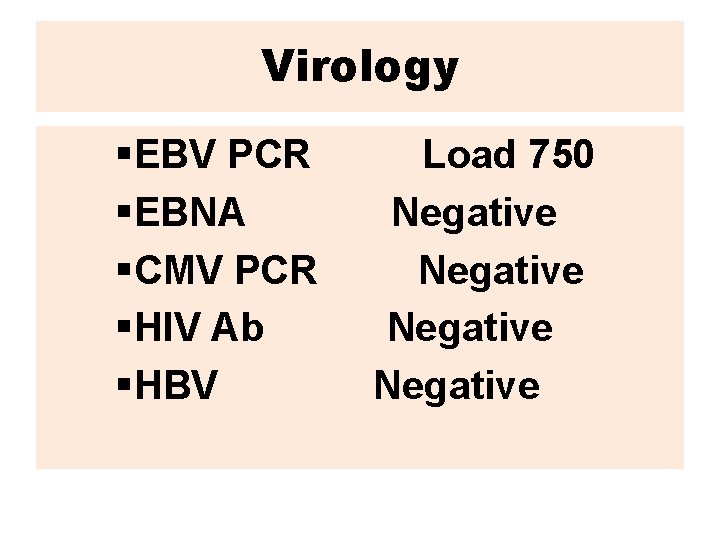
Virology §EBV PCR §EBNA §CMV PCR §HIV Ab §HBV Load 750 Negative
Kalazar • BM Negative • Serology Negative
Rheumatology panel • Negative RF • Negative Anti DNA
Genetic • Not ready
Supportive therapy • Irradiated blood products • Broad spectrum AB • IV IG • PCP and fungal prophylaxia
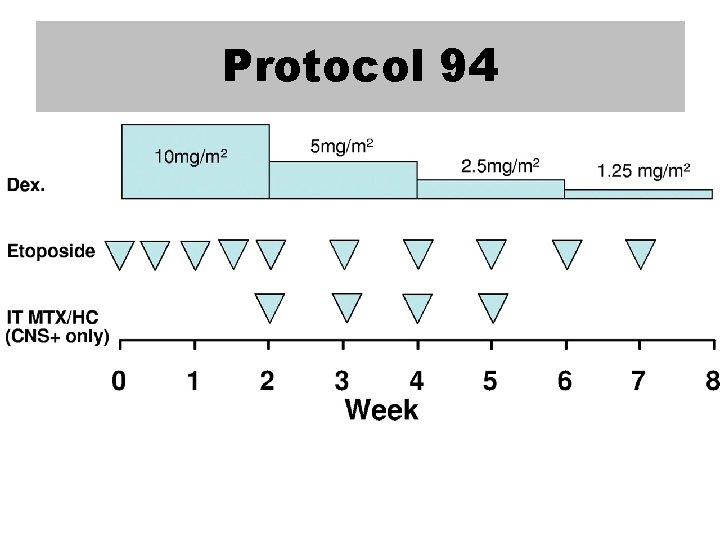
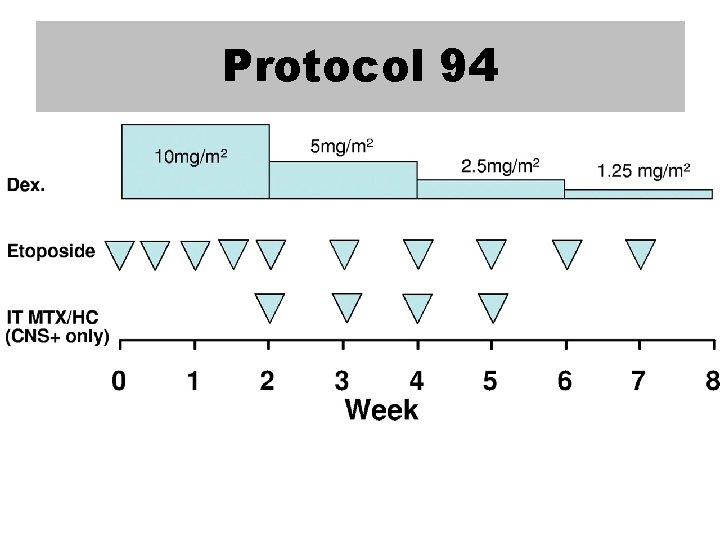
Protocol 94
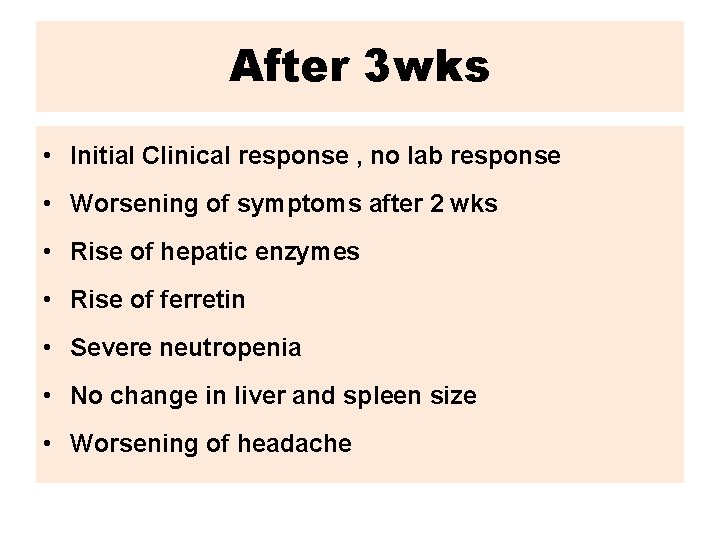
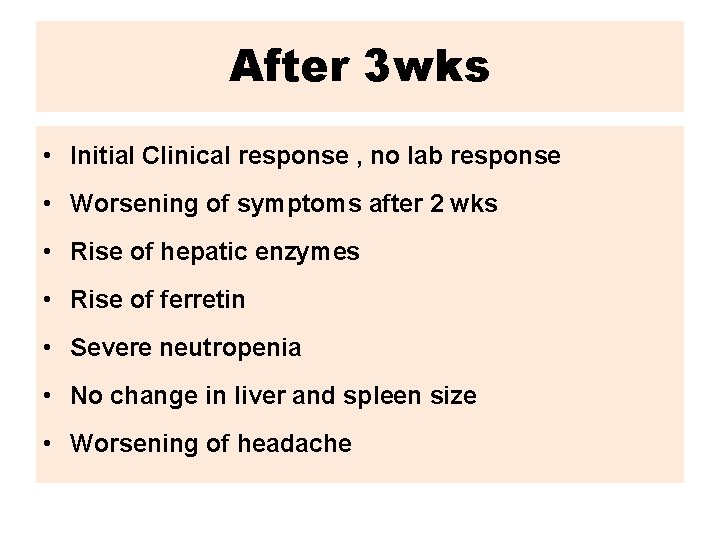
After 3 wks • Initial Clinical response , no lab response • Worsening of symptoms after 2 wks • Rise of hepatic enzymes • Rise of ferretin • Severe neutropenia • No change in liver and spleen size • Worsening of headache
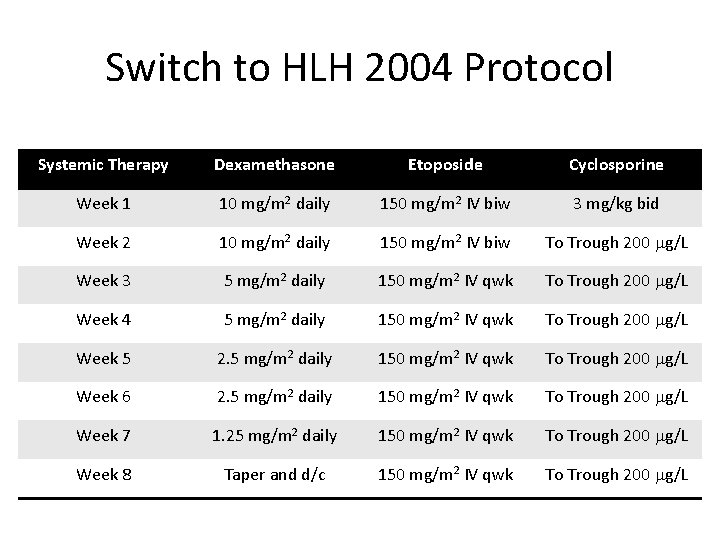
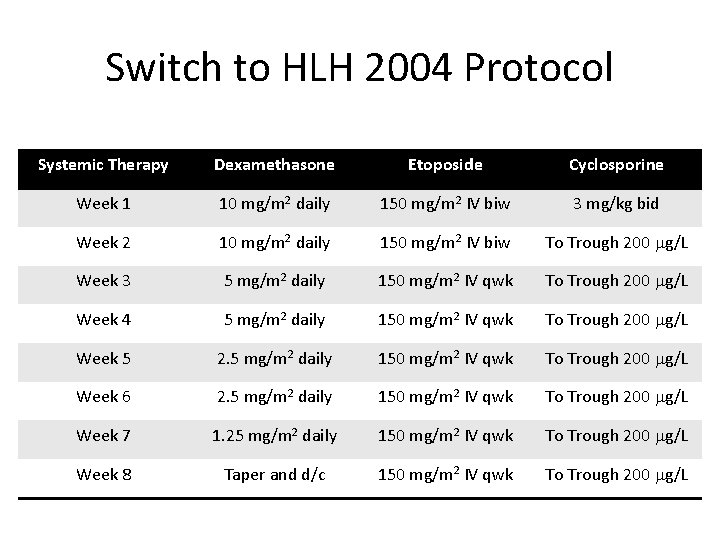
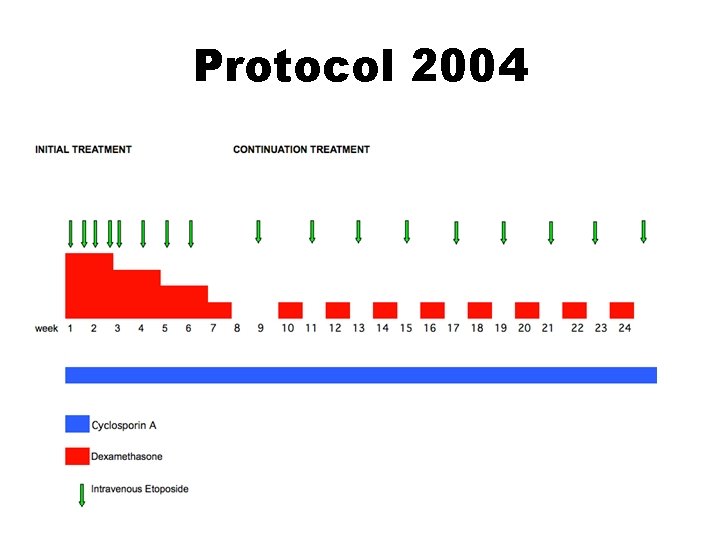
Switch to HLH 2004 Protocol Systemic Therapy Dexamethasone Etoposide Cyclosporine Week 1 10 mg/m 2 daily 150 mg/m 2 IV biw 3 mg/kg bid Week 2 10 mg/m 2 daily 150 mg/m 2 IV biw To Trough 200 g/L Week 3 5 mg/m 2 daily 150 mg/m 2 IV qwk To Trough 200 g/L Week 4 5 mg/m 2 daily 150 mg/m 2 IV qwk To Trough 200 g/L Week 5 2. 5 mg/m 2 daily 150 mg/m 2 IV qwk To Trough 200 g/L Week 6 2. 5 mg/m 2 daily 150 mg/m 2 IV qwk To Trough 200 g/L Week 7 1. 25 mg/m 2 daily 150 mg/m 2 IV qwk To Trough 200 g/L Week 8 Taper and d/c 150 mg/m 2 IV qwk To Trough 200 g/L
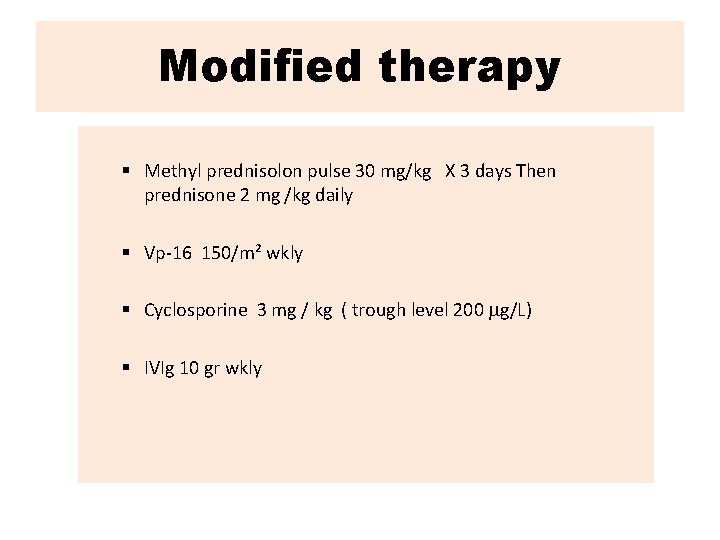
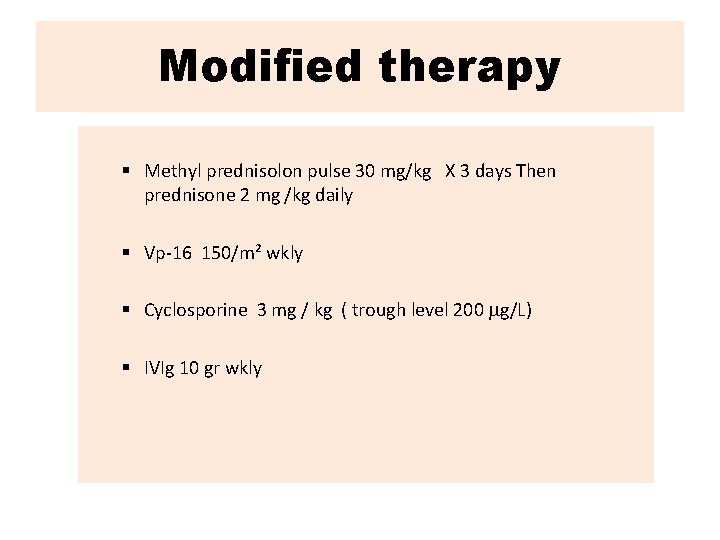
Modified therapy § Methyl prednisolon pulse 30 mg/kg X 3 days Then prednisone 2 mg /kg daily § Vp-16 150/m² wkly § Cyclosporine 3 mg / kg ( trough level 200 g/L) § IVIg 10 gr wkly
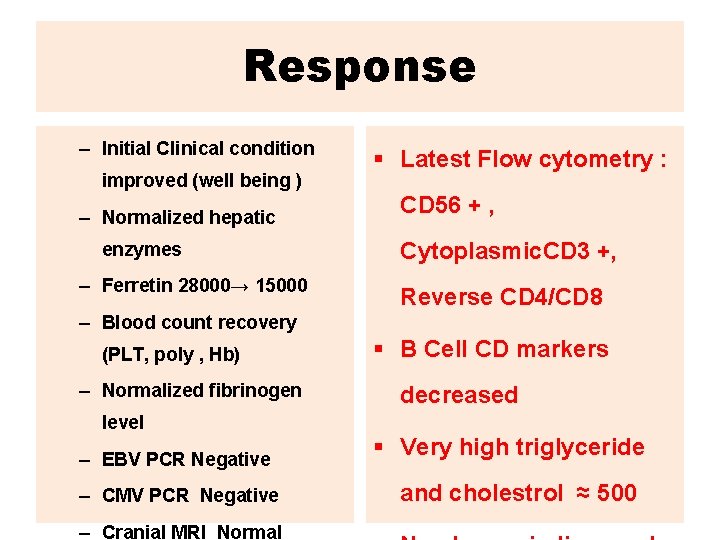
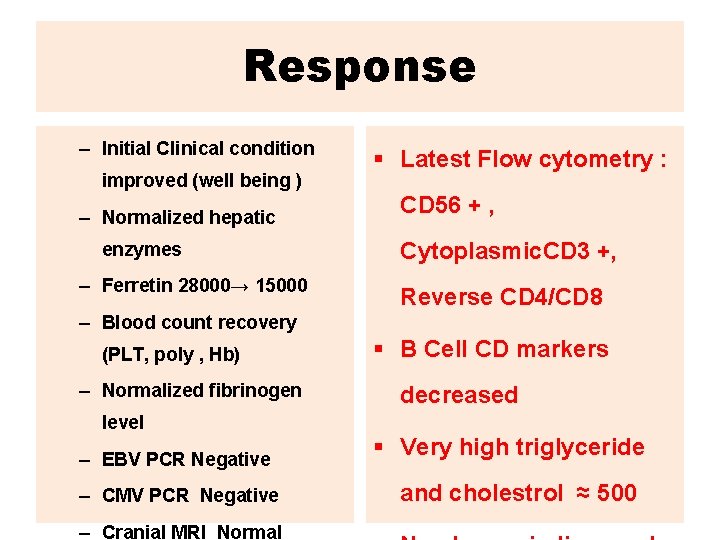
Response – Initial Clinical condition improved (well being ) – Normalized hepatic enzymes – Ferretin 28000→ 15000 § Latest Flow cytometry : CD 56 + , Cytoplasmic. CD 3 +, Reverse CD 4/CD 8 – Blood count recovery (PLT, poly , Hb) – Normalized fibrinogen level – EBV PCR Negative – CMV PCR Negative – Cranial MRI Normal § B Cell CD markers decreased § Very high triglyceride and cholestrol ≈ 500


HLH

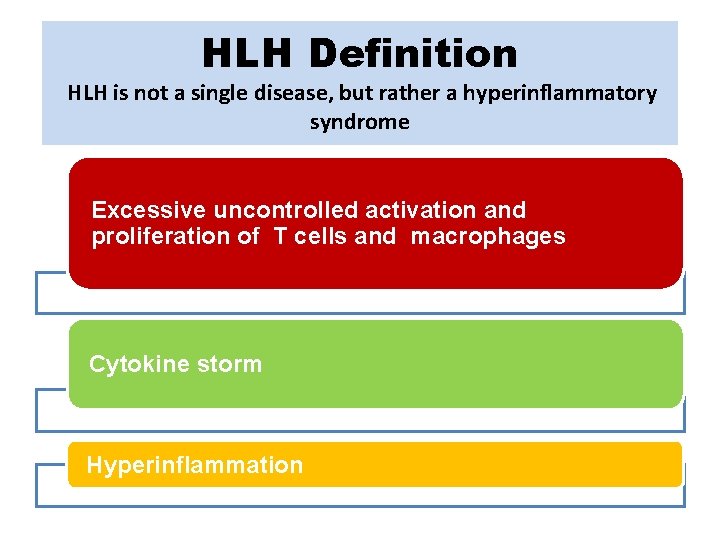
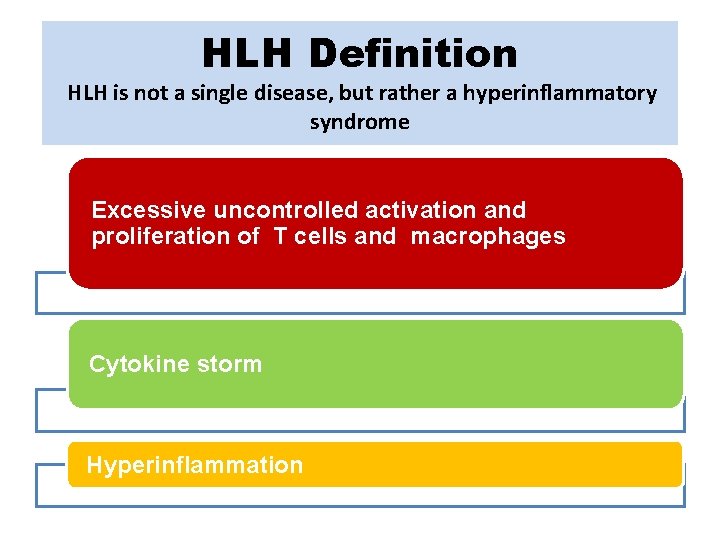
HLH Definition HLH is not a single disease, but rather a hyperinflammatory syndrome Excessive uncontrolled activation and proliferation of T cells and macrophages Cytokine storm Hyperinflammation


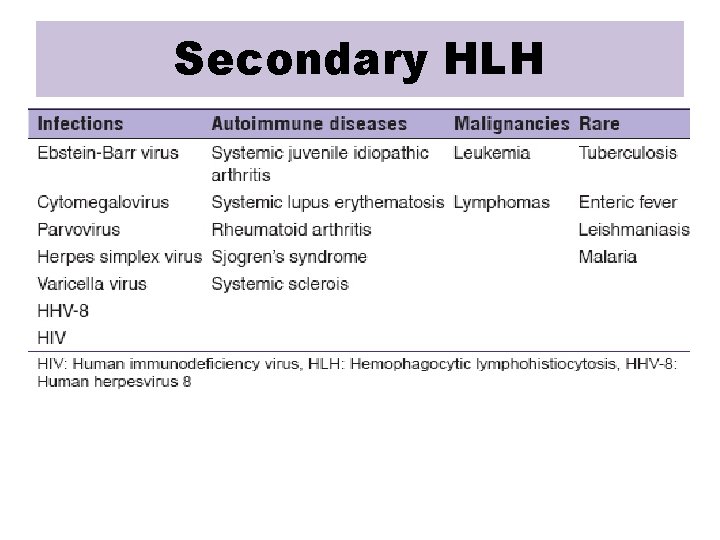
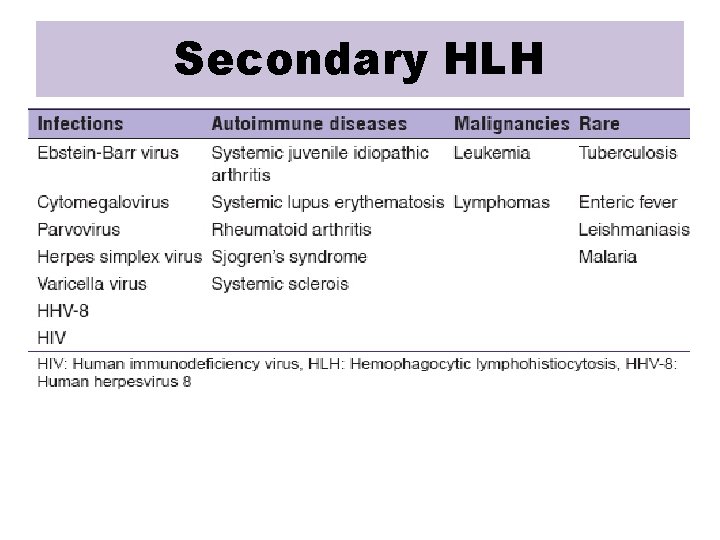
Secondary HLH
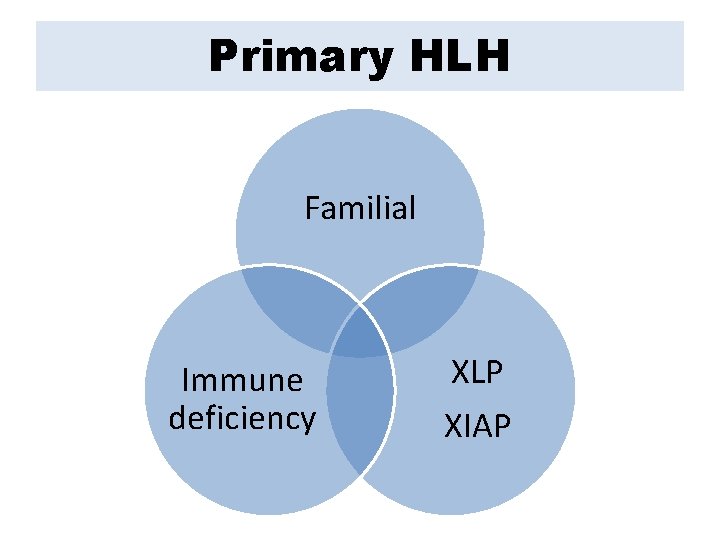
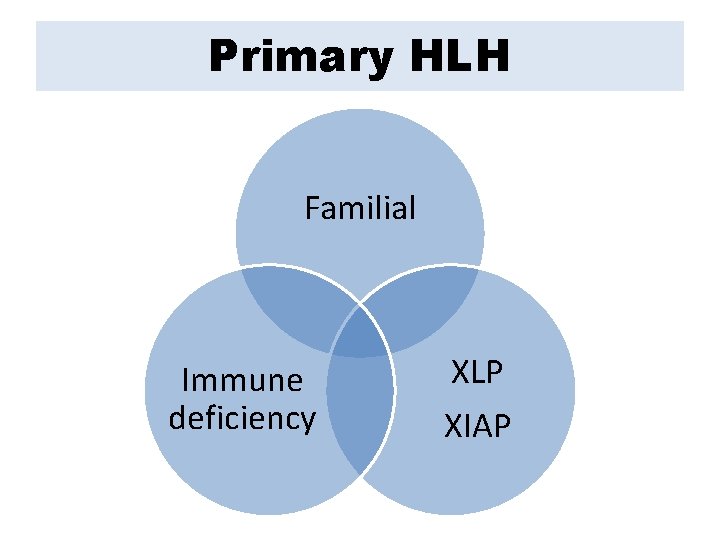
Primary HLH Familial Immune deficiency XLP XIAP
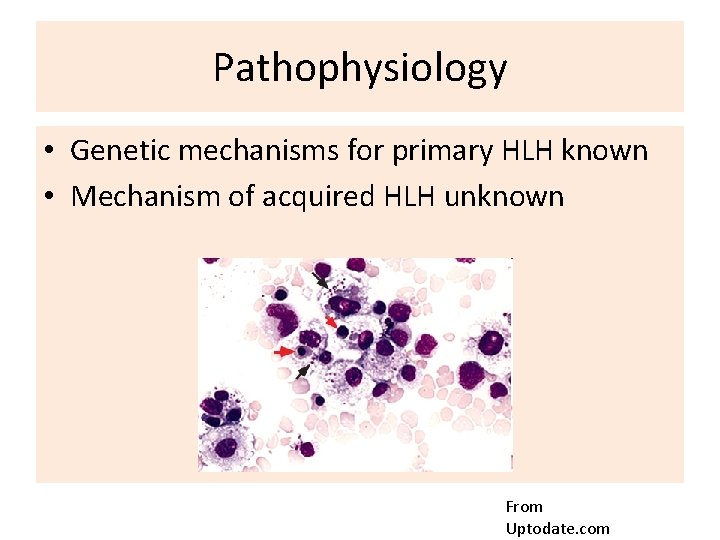
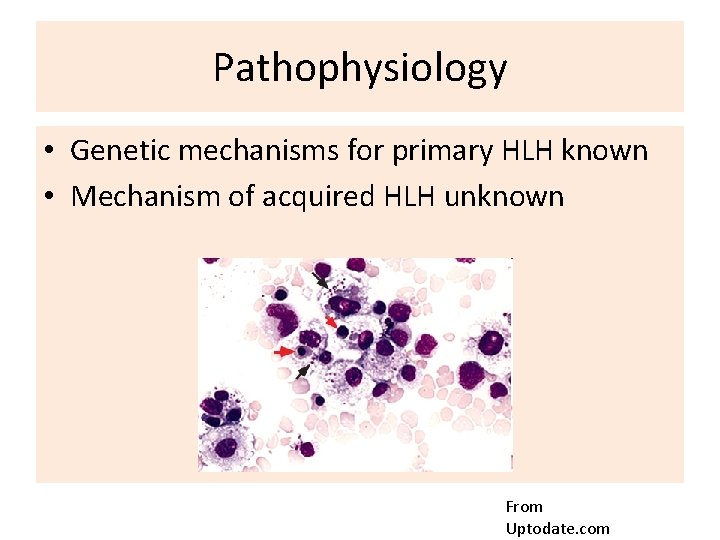
Pathophysiology • Genetic mechanisms for primary HLH known • Mechanism of acquired HLH unknown From Uptodate. com
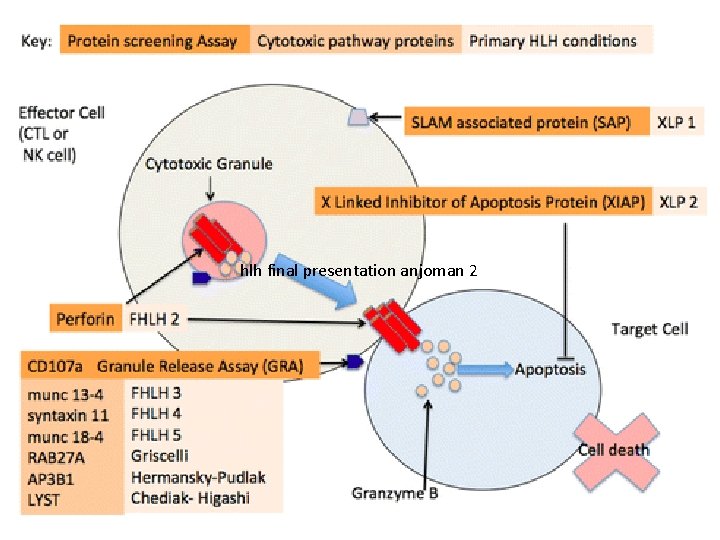
Pathophysiology Primary HLH
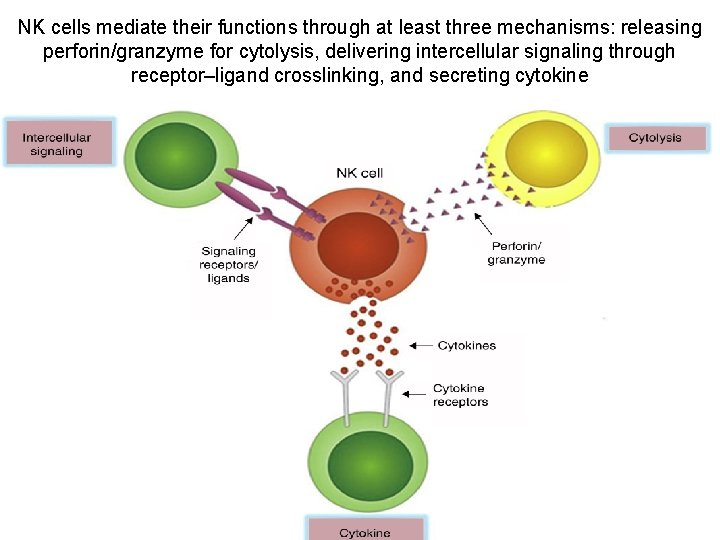
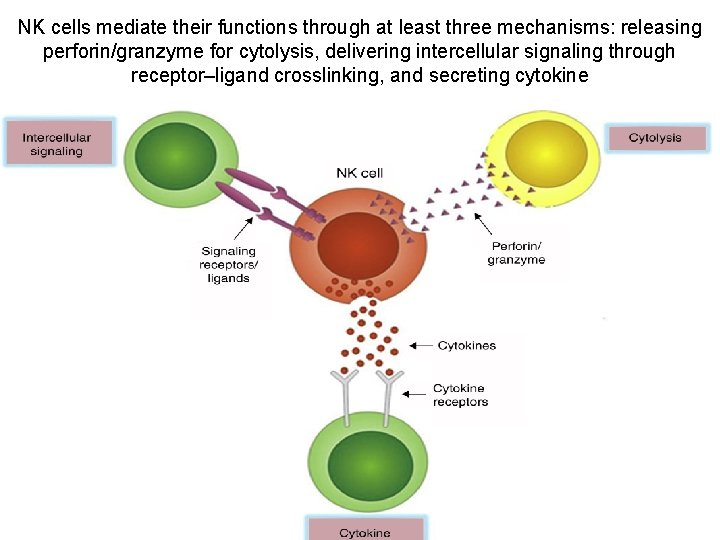
NK cells mediate their functions through at least three mechanisms: releasing perforin/granzyme for cytolysis, delivering intercellular signaling through receptor–ligand crosslinking, and secreting cytokine







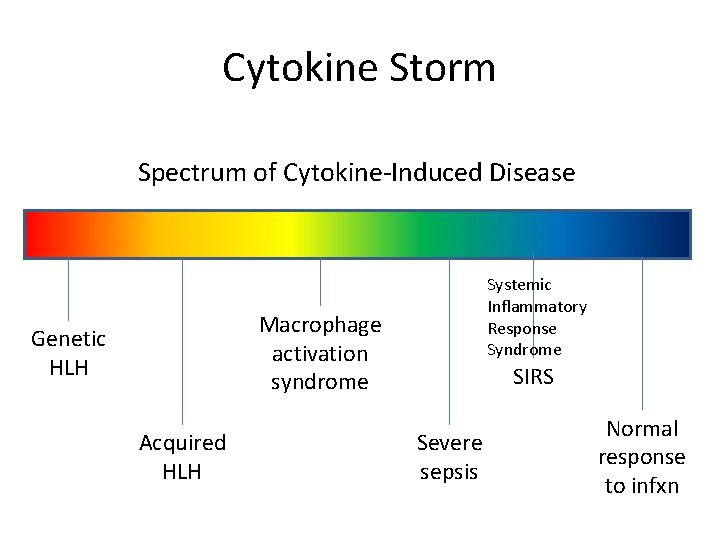
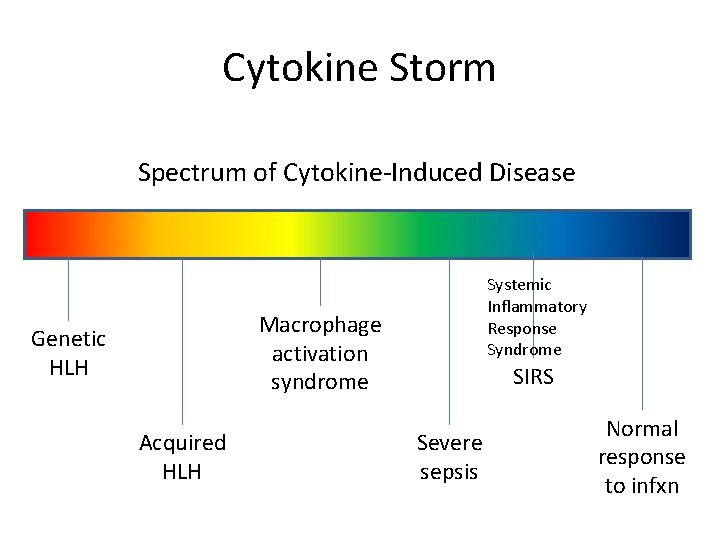
Cytokine Storm Spectrum of Cytokine-Induced Disease Systemic Inflammatory Response Syndrome Macrophage activation syndrome Genetic HLH Acquired HLH SIRS Severe sepsis Normal response to infxn
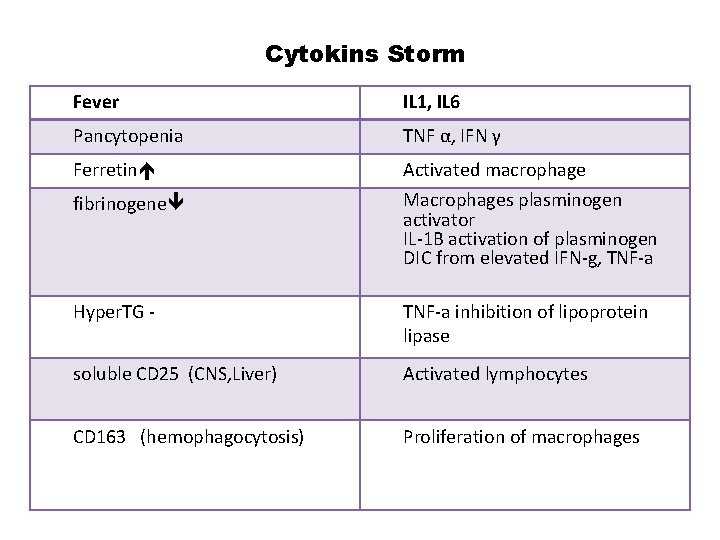
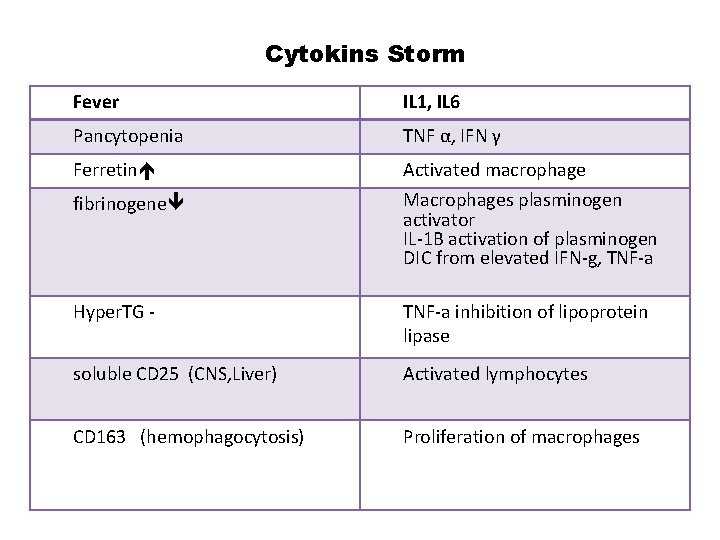
Cytokins Storm Fever IL 1, IL 6 Pancytopenia TNF α, IFN γ Ferretin Activated macrophage fibrinogene Macrophages plasminogen activator IL-1 B activation of plasminogen DIC from elevated IFN-g, TNF-a Hyper. TG - TNF-a inhibition of lipoprotein lipase soluble CD 25 (CNS, Liver) Activated lymphocytes CD 163 (hemophagocytosis) Proliferation of macrophages



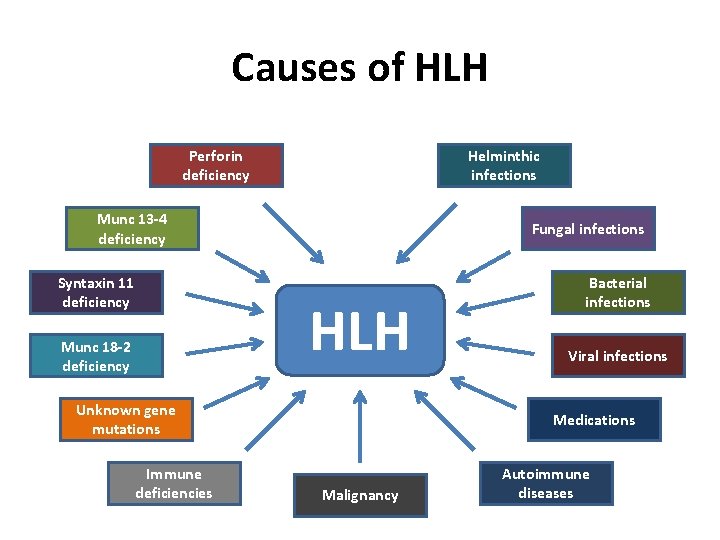
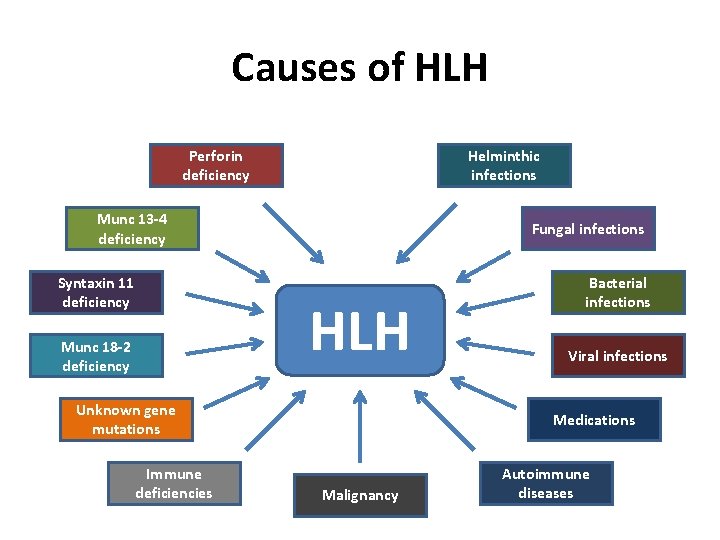
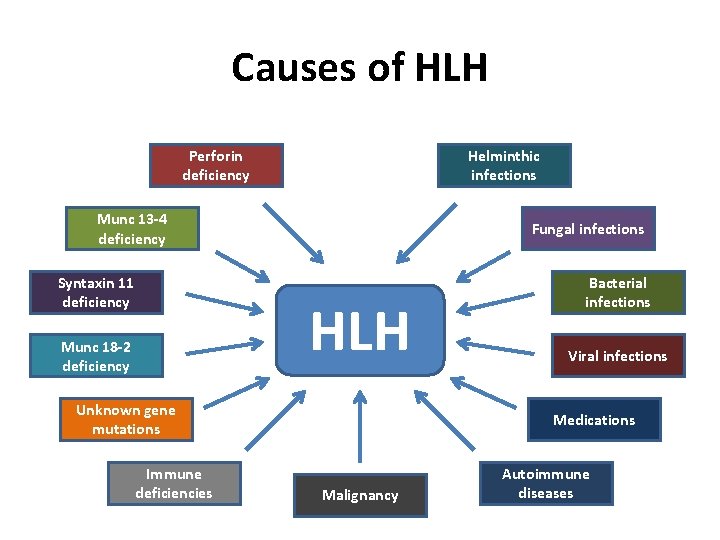
Causes of HLH Perforin deficiency Helminthic infections Munc 13 -4 deficiency Syntaxin 11 deficiency Fungal infections HLH Munc 18 -2 deficiency Unknown gene mutations Immune deficiencies Bacterial infections Viral infections Medications Malignancy Autoimmune diseases
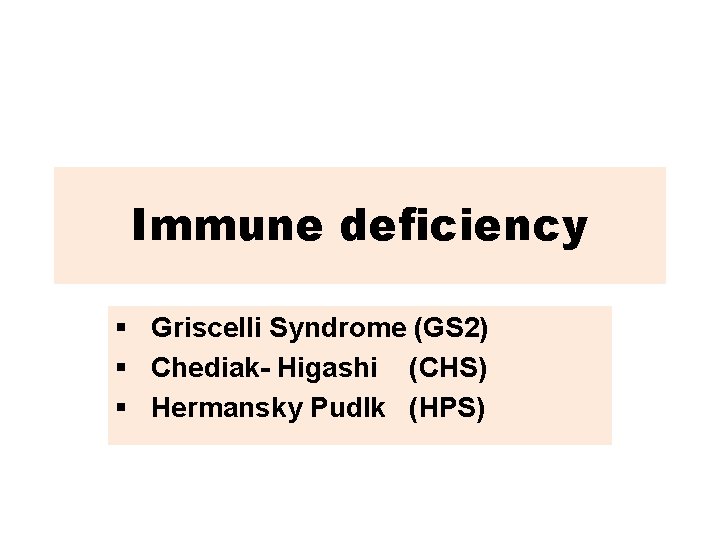
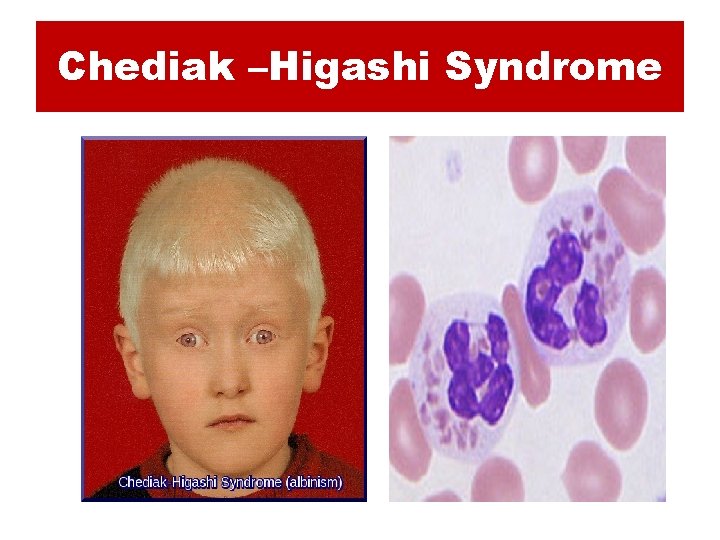
Immune deficiency § Griscelli Syndrome (GS 2) § Chediak- Higashi (CHS) § Hermansky Pudlk (HPS)
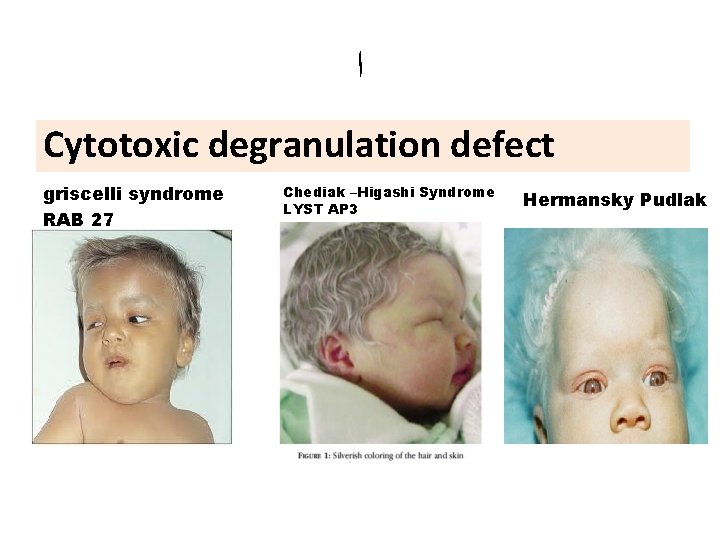
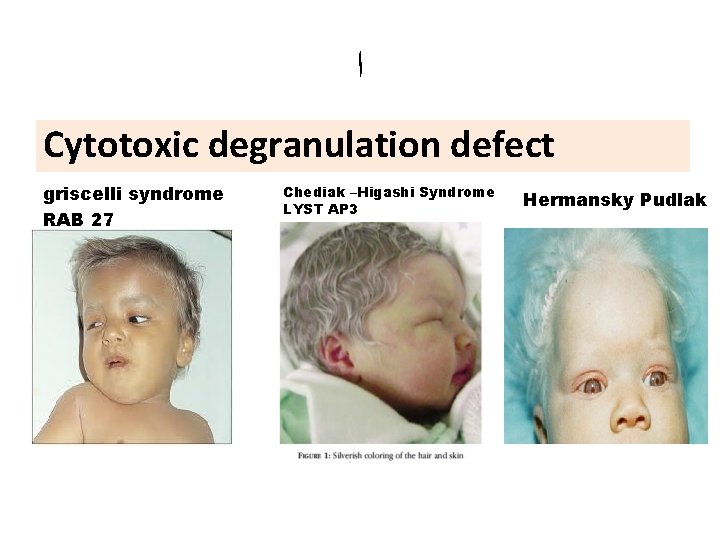
ﺍ Cytotoxic degranulation defect griscelli syndrome RAB 27 Chediak –Higashi Syndrome LYST AP 3 Hermansky Pudlak
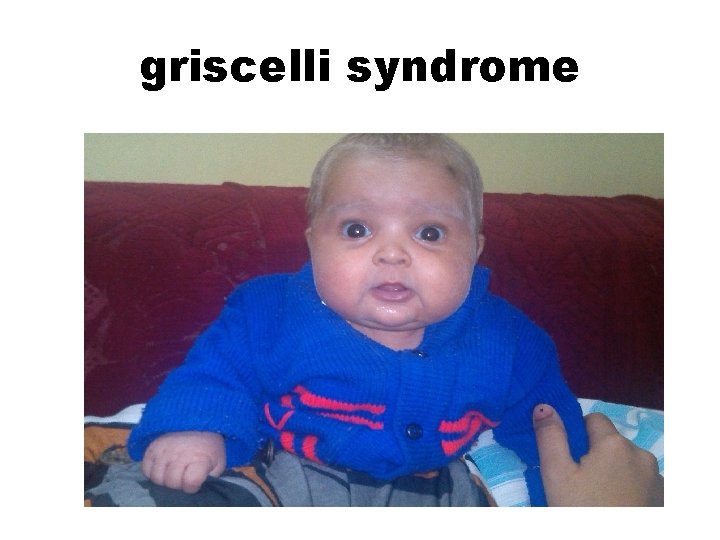
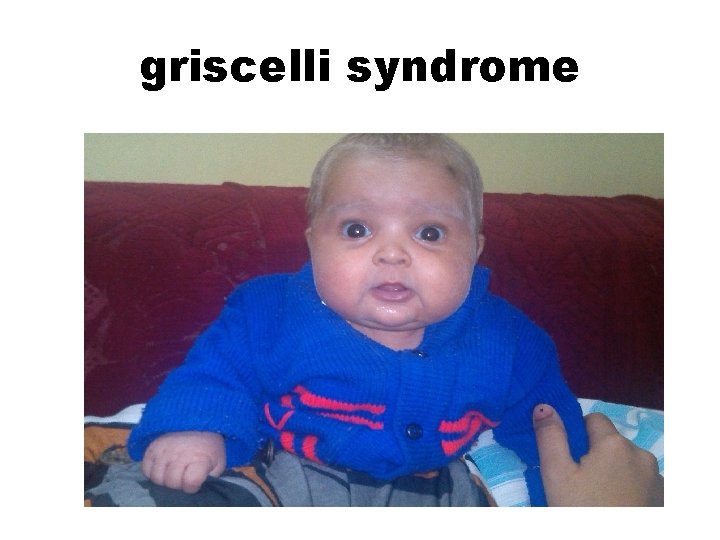
griscelli syndrome
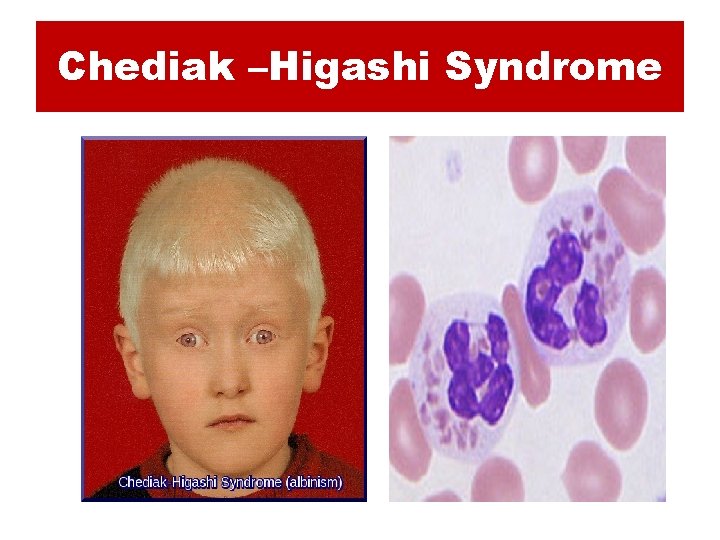
Chediak –Higashi Syndrome

Hermansky Pudlak
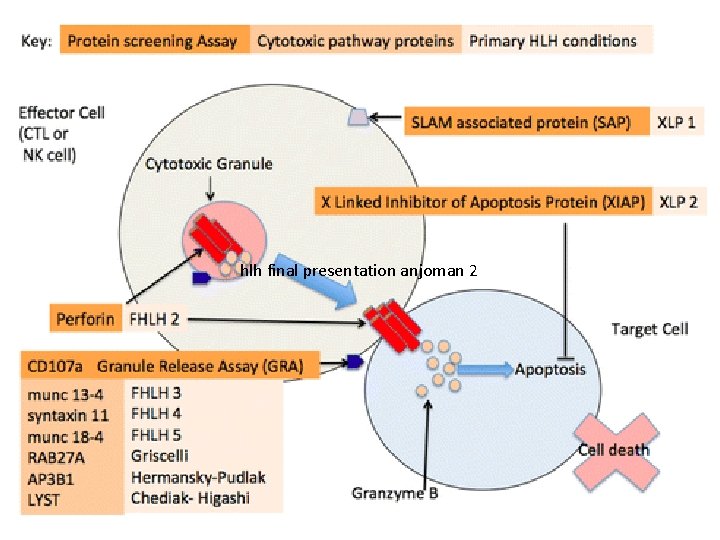
X -Linked Lymphoproliferative Disorders 1. XLP 2. XIAP
XLP • X-linked lymphoproliferative disorder—characterized by hypogammaglobulinemia or lymphoproliferation • Caused by mutations in SLAM-associated protein (SAP) or X-linked inhibitor of apoptosis (XIAP) • Epstein-Barr virus infection results in fulminant and fatal mononucleosis • HLH is almost always associated with EBV infection • SAP deficiency results in a partial cytotoxic defect; no observable cytotoxic defect in XIAP deficiency
XLP • • In XLP, 60– 70% of patients have mutations in the gene SAP (SLAMassociated protein), also termed SH 2 DIA (SH 2 -domain containing gene 1 A) or DSHP. This gene, located at Xq 25, regulates a protein involved in signal transduction in T and NK cells. In T cells, the protein binds to the Signaling Lymphocyte Activation Molecule (SLAM, known as CDw 150) and in NK
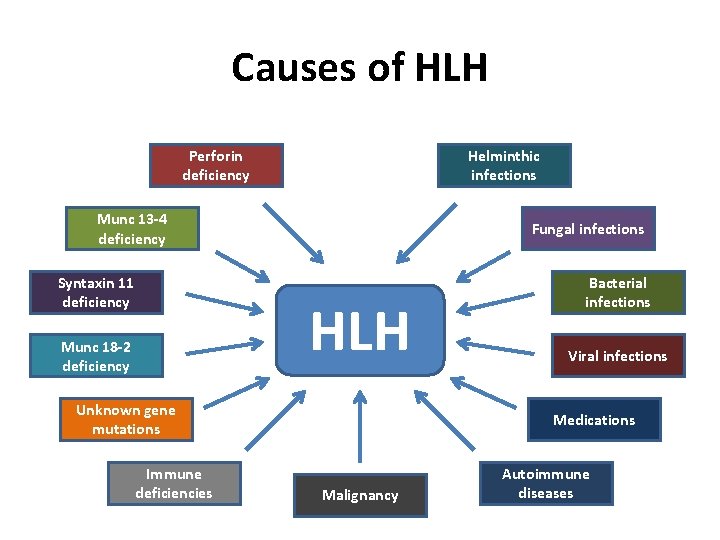
Causes of HLH Perforin deficiency Helminthic infections Munc 13 -4 deficiency Syntaxin 11 deficiency Fungal infections HLH Munc 18 -2 deficiency Unknown gene mutations Immune deficiencies Bacterial infections Viral infections Medications Malignancy Autoimmune diseases

Diagnosis
Timely Diagnosis – Timely diagnosis is critical to start therapy before damage by hypercytokinemia becomes irreversible. – There is no single feature that is specific for HLH.
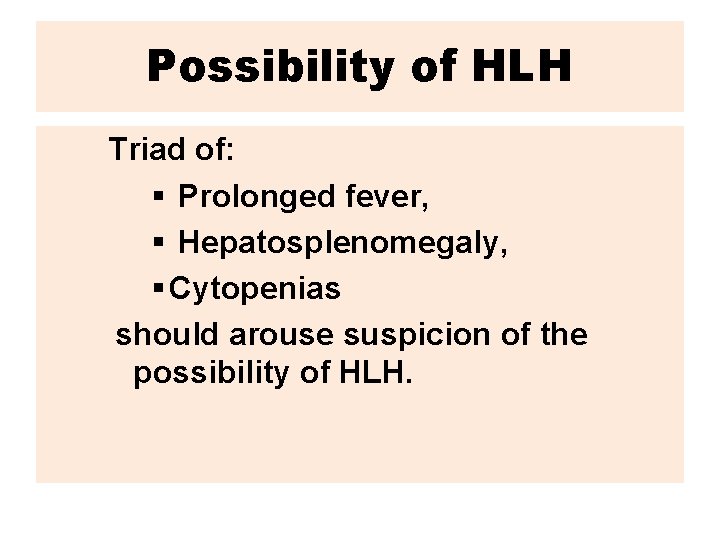
Possibility of HLH Triad of: § Prolonged fever, § Hepatosplenomegaly, § Cytopenias should arouse suspicion of the possibility of HLH.
Primary HLH vs. Secondary HLH – Severity of disease and the identification of an infectious agent do not discriminate between genetic and acquired forms of HLH. – Age is helpful to some extent: a minority of children 1 year of age will have
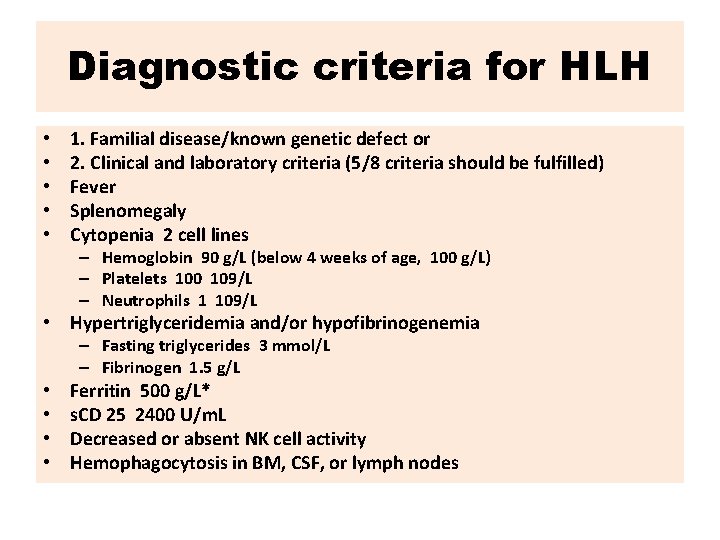
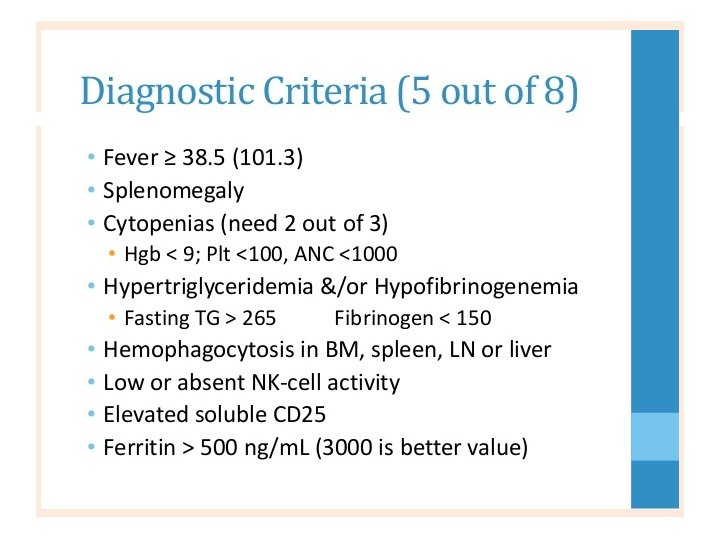
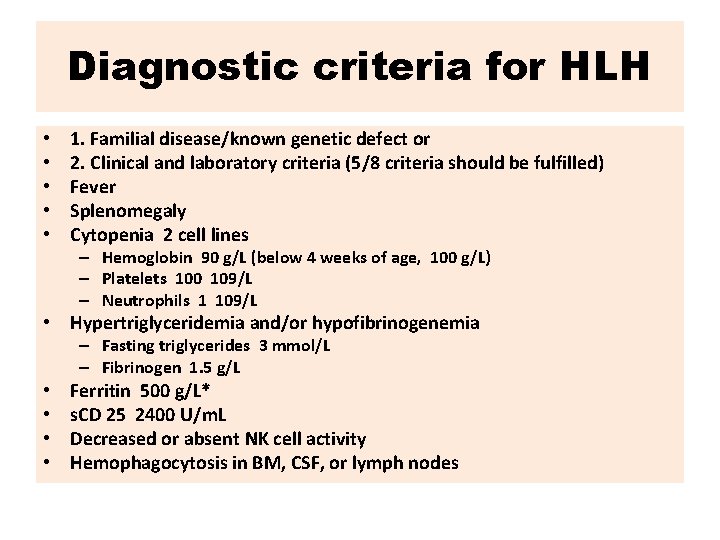
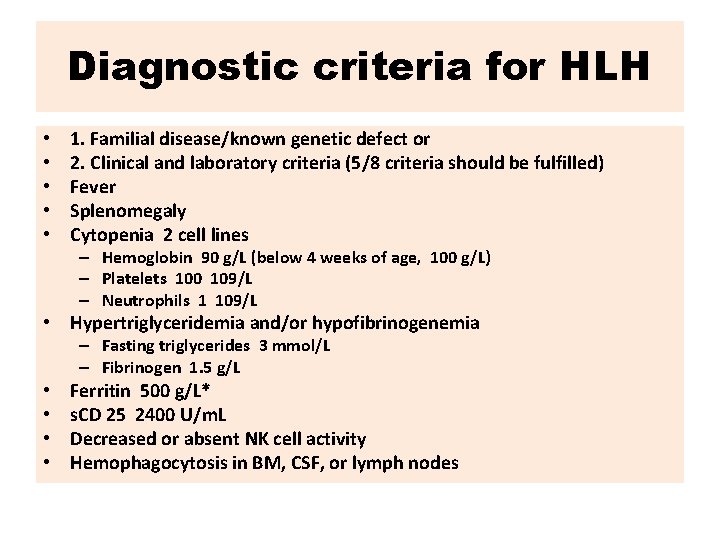
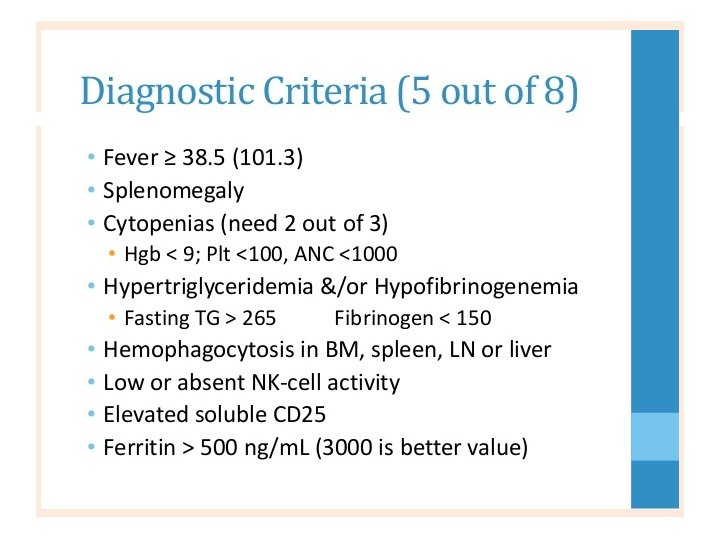
Diagnostic criteria for HLH • • • 1. Familial disease/known genetic defect or 2. Clinical and laboratory criteria (5/8 criteria should be fulfilled) Fever Splenomegaly Cytopenia 2 cell lines – Hemoglobin 90 g/L (below 4 weeks of age, 100 g/L) – Platelets 100 109/L – Neutrophils 1 109/L • Hypertriglyceridemia and/or hypofibrinogenemia – Fasting triglycerides 3 mmol/L – Fibrinogen 1. 5 g/L • • Ferritin 500 g/L* s. CD 25 2400 U/m. L Decreased or absent NK cell activity Hemophagocytosis in BM, CSF, or lymph nodes
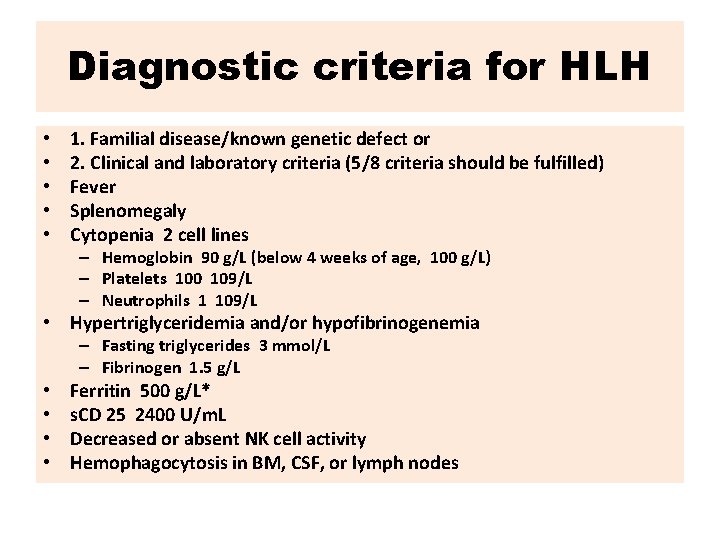
Diagnostic criteria for HLH • • • 1. Familial disease/known genetic defect or 2. Clinical and laboratory criteria (5/8 criteria should be fulfilled) Fever Splenomegaly Cytopenia 2 cell lines – Hemoglobin 90 g/L (below 4 weeks of age, 100 g/L) – Platelets 100 109/L – Neutrophils 1 109/L • Hypertriglyceridemia and/or hypofibrinogenemia – Fasting triglycerides 3 mmol/L – Fibrinogen 1. 5 g/L • • Ferritin 500 g/L* s. CD 25 2400 U/m. L Decreased or absent NK cell activity Hemophagocytosis in BM, CSF, or lymph nodes
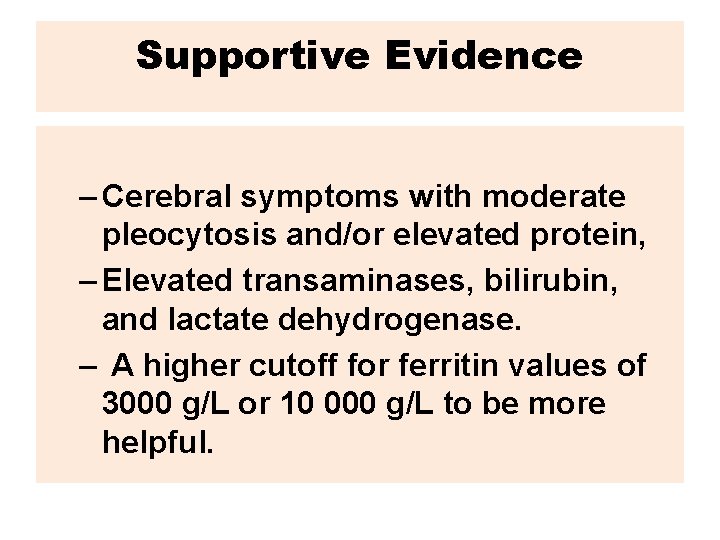
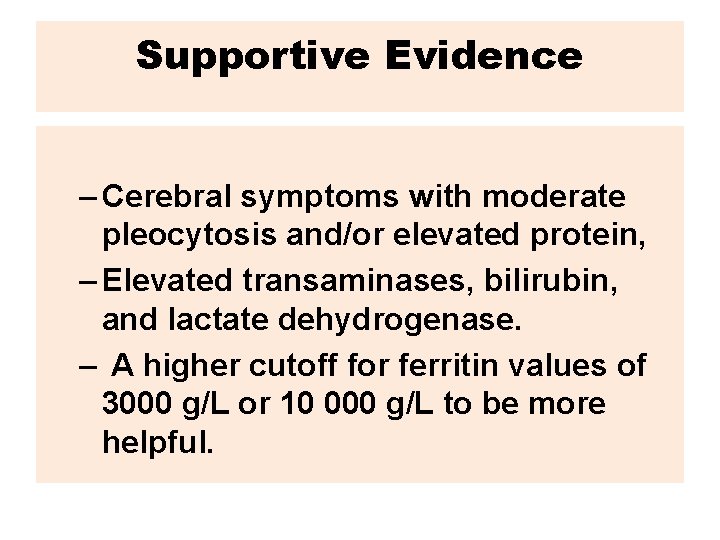
Supportive Evidence – Cerebral symptoms with moderate pleocytosis and/or elevated protein, – Elevated transaminases, bilirubin, and lactate dehydrogenase. – A higher cutoff for ferritin values of 3000 g/L or 10 000 g/L to be more helpful.

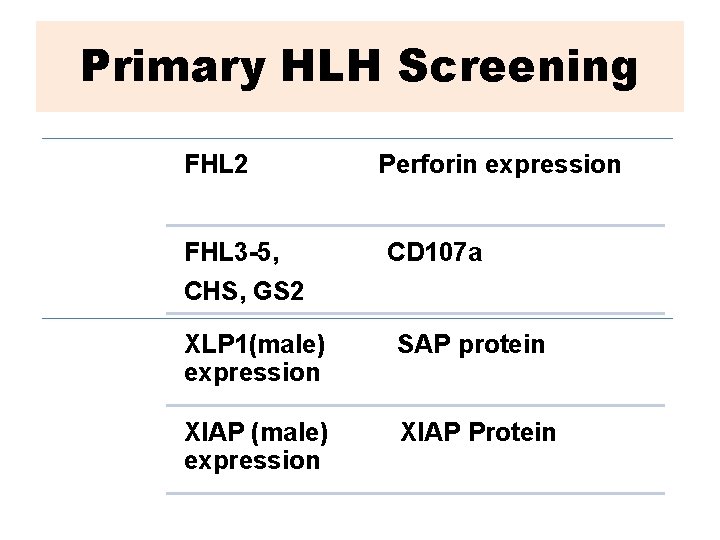
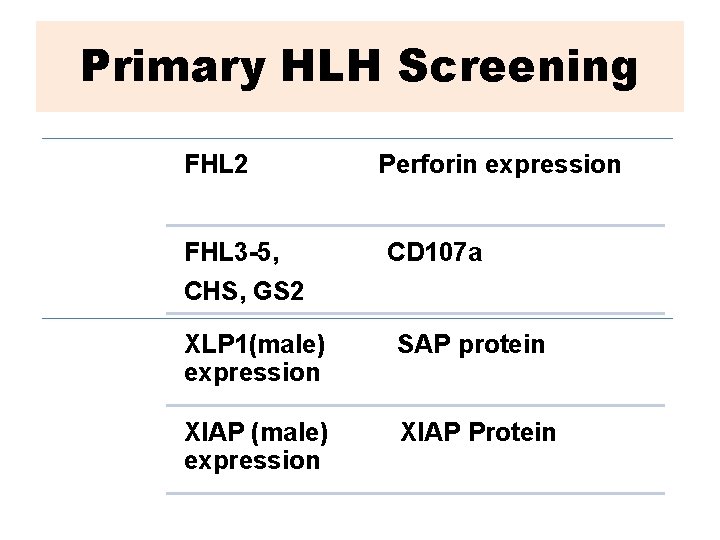
Primary HLH Screening FHL 2 FHL 3 -5, CHS, GS 2 Perforin expression CD 107 a XLP 1(male) expression SAP protein XIAP (male) expression XIAP Protein
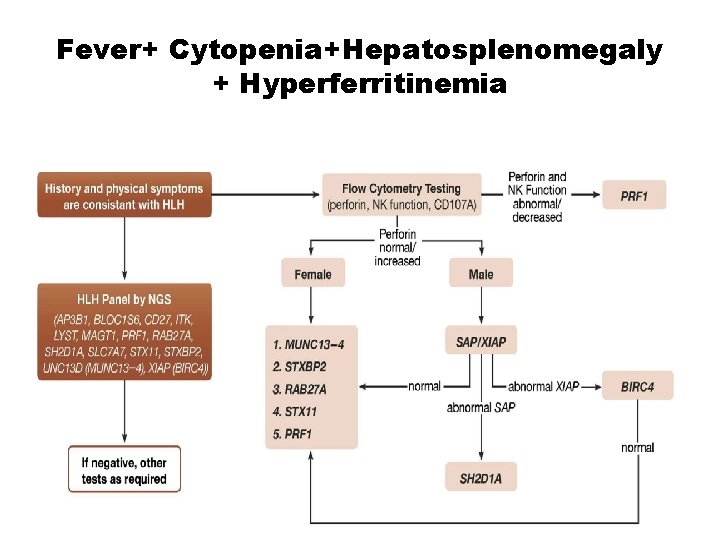
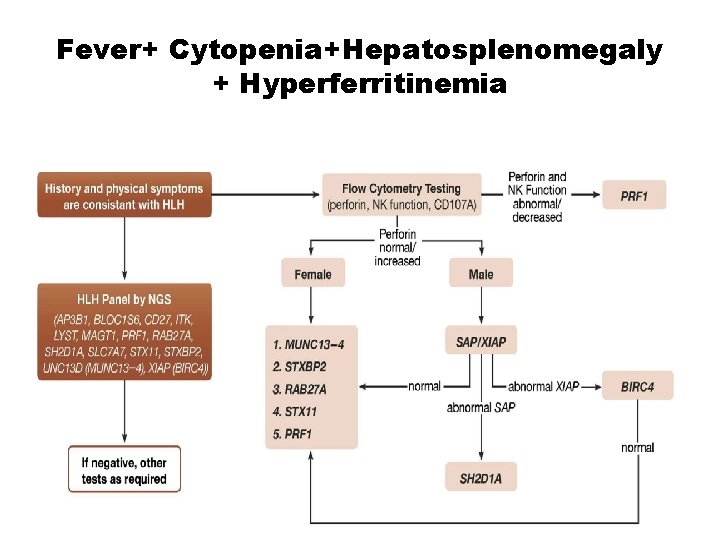
Fever+ Cytopenia+Hepatosplenomegaly + Hyperferritinemia
hlh final presentation anjoman 2
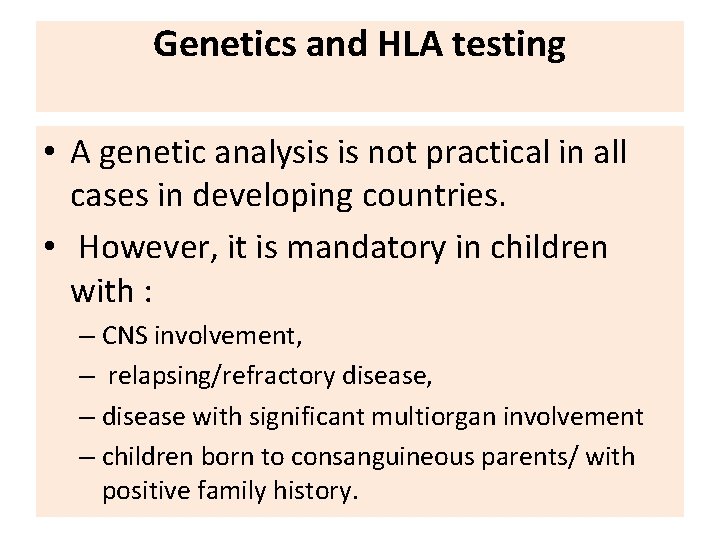
Genetics and HLA testing • A genetic analysis is not practical in all cases in developing countries. • However, it is mandatory in children with : – CNS involvement, – relapsing/refractory disease, – disease with significant multiorgan involvement – children born to consanguineous parents/ with positive family history.

Immunology & HLH



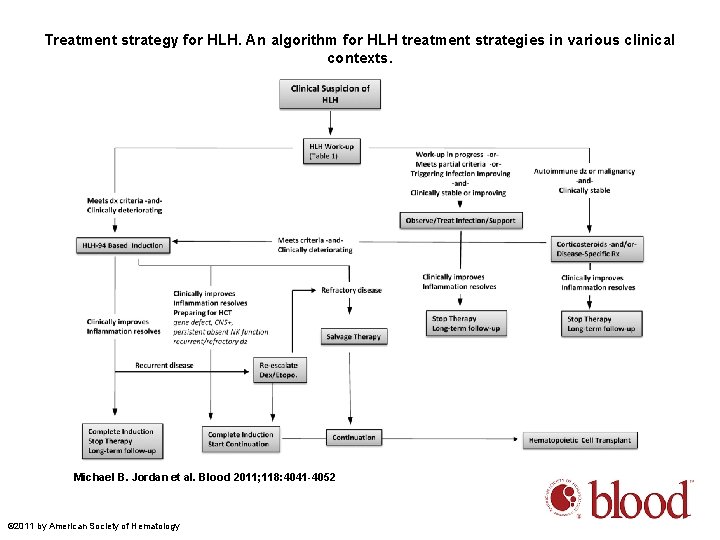
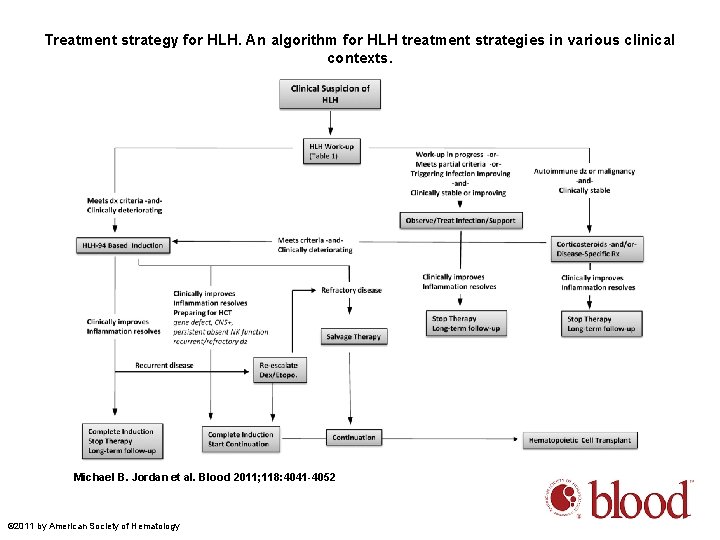
Treatment strategy for HLH. An algorithm for HLH treatment strategies in various clinical contexts. Michael B. Jordan et al. Blood 2011; 118: 4041 -4052 © 2011 by American Society of Hematology
• Once these functional tests suggest a genetic basis for HLH, molecular analysis should follow, including for parents and siblings.
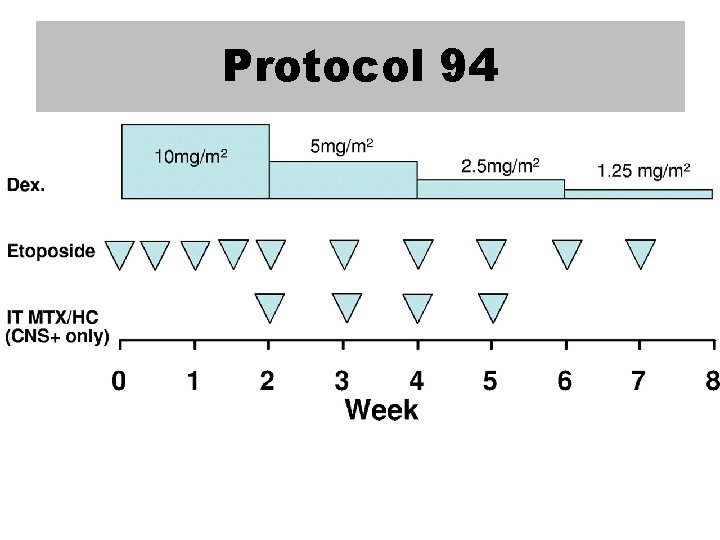
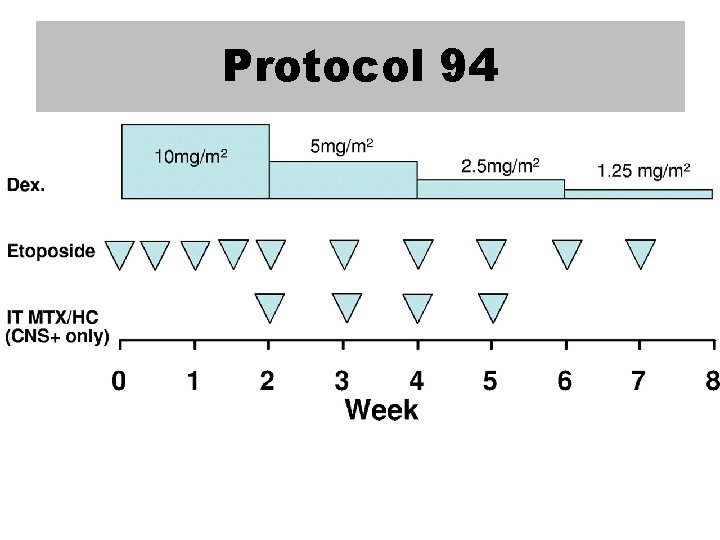
Protocol 94
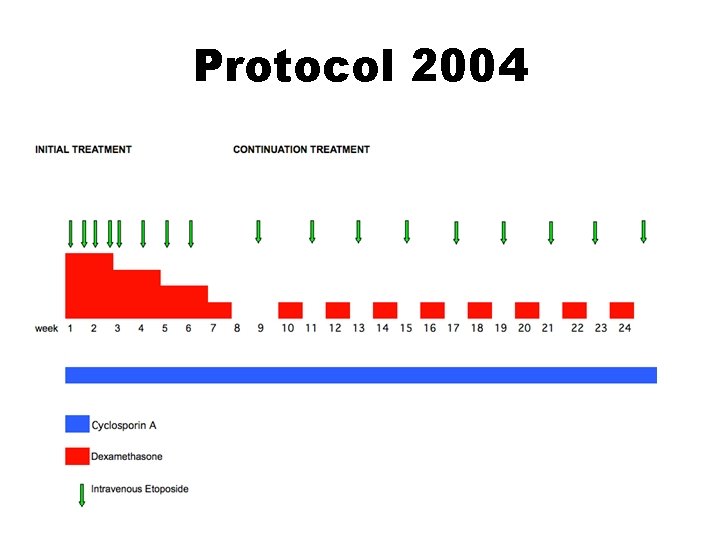
Protocol 2004
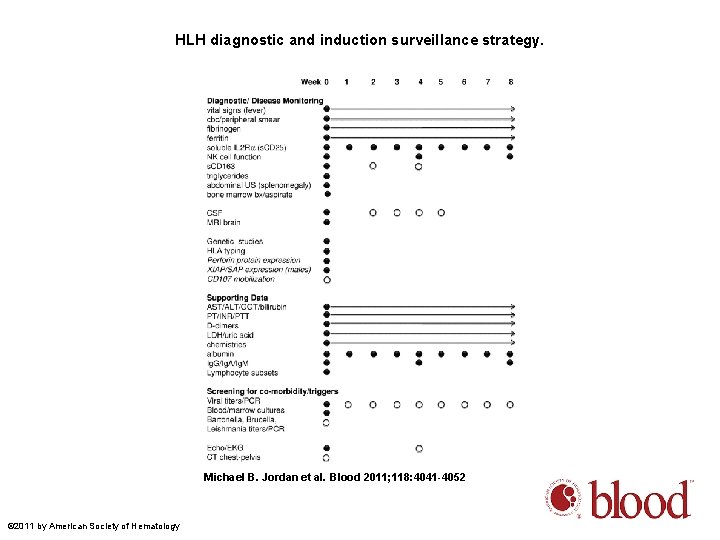
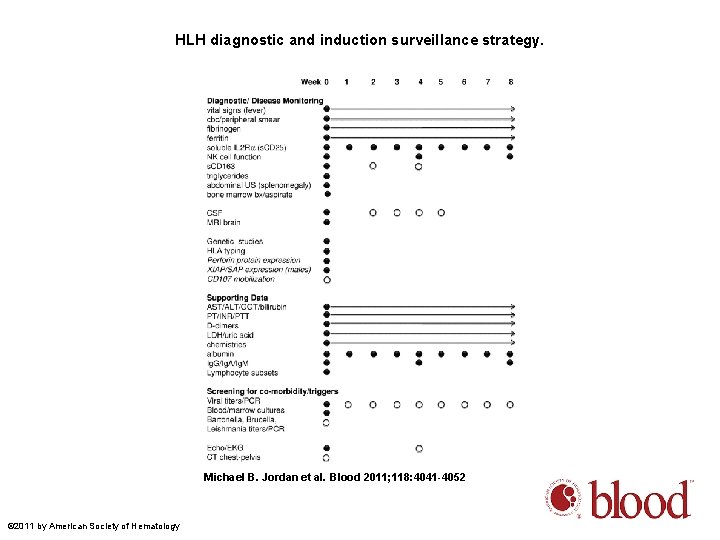
HLH diagnostic and induction surveillance strategy. Michael B. Jordan et al. Blood 2011; 118: 4041 -4052 © 2011 by American Society of Hematology

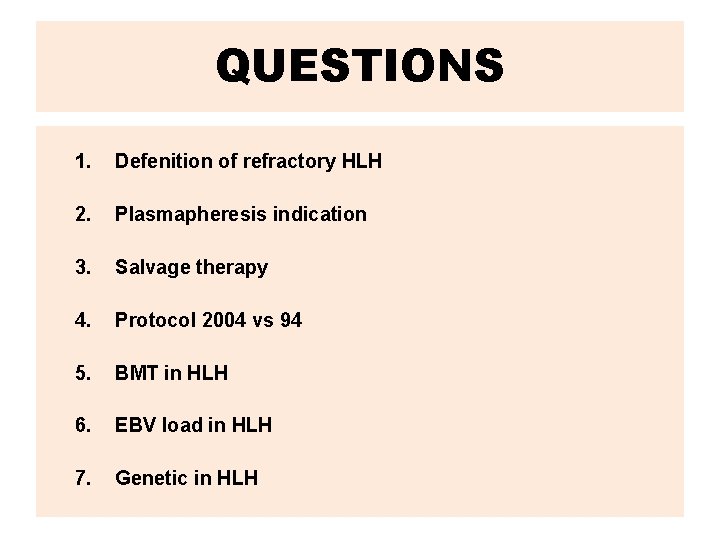
QUESTIONS 1. Defenition of refractory HLH 2. Plasmapheresis indication 3. Salvage therapy 4. Protocol 2004 vs 94 5. BMT in HLH 6. EBV load in HLH 7. Genetic in HLH
 Wbc ip message blasts/abn lympho
Wbc ip message blasts/abn lympho Cat histiocytosis
Cat histiocytosis Feline histiocytosis
Feline histiocytosis Pankreas stent
Pankreas stent Best case worst case average case
Best case worst case average case And how old are you
And how old are you Once upon a time there lived a boy
Once upon a time there lived a boy Once upon a time there lived an old man and an old woman
Once upon a time there lived an old man and an old woman Once upon a time there lived a very poor boy
Once upon a time there lived a very poor boy Old english literature presentation
Old english literature presentation Old spice case study
Old spice case study Occipital brow presentation
Occipital brow presentation 4 maneuvers of leopold
4 maneuvers of leopold Sheryl fleisch
Sheryl fleisch Lbo model test
Lbo model test Yelp core values
Yelp core values Malnutrition case
Malnutrition case Case presentation template
Case presentation template Emergency medicine case presentation
Emergency medicine case presentation Case presentation medicine
Case presentation medicine Vomiting case presentation
Vomiting case presentation Case presentation introduction
Case presentation introduction Icu case presentation
Icu case presentation Icu case presentation
Icu case presentation Wpvr-230
Wpvr-230 Vomiting case presentation
Vomiting case presentation Radiology case presentation
Radiology case presentation Dka case presentation ppt
Dka case presentation ppt Orthopedic case presentation
Orthopedic case presentation Orthopedic case presentation
Orthopedic case presentation Delirium case presentation
Delirium case presentation Dr grace ng
Dr grace ng Evaluation criteria for case study presentation
Evaluation criteria for case study presentation Gbs case presentation
Gbs case presentation Jaundice case presentation
Jaundice case presentation Chatecholamine
Chatecholamine Brozodex
Brozodex Surgery case presentation
Surgery case presentation Hematological malignancies
Hematological malignancies Geriatric case presentation
Geriatric case presentation Nephrology case presentation
Nephrology case presentation Candida albicans blastospores
Candida albicans blastospores Asmita karandikar
Asmita karandikar Creek 2003 occupational therapy process
Creek 2003 occupational therapy process Family case presentation
Family case presentation Short case vs long case
Short case vs long case Binary search complexity
Binary search complexity Case western reserve university case school of engineering
Case western reserve university case school of engineering Bubble sort algorithm pseudocode
Bubble sort algorithm pseudocode It project failure case study
It project failure case study Bubble sort best case and worst case
Bubble sort best case and worst case Bubble sort best case and worst case
Bubble sort best case and worst case Ssa ambiguous case
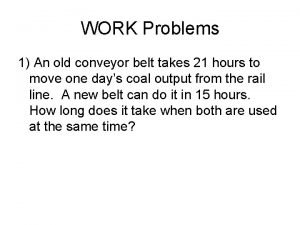
Ssa ambiguous case An old conveyor belt takes 21
An old conveyor belt takes 21 To thee old cause
To thee old cause What is your name how old are you
What is your name how old are you There once was a woman from china
There once was a woman from china What is the difference between the old and new covenant
What is the difference between the old and new covenant Grandpa family tree
Grandpa family tree The courtyard of the old residency in munich
The courtyard of the old residency in munich Heart rates for women
Heart rates for women Old man's cloth el anatsui
Old man's cloth el anatsui The old grandfather and his little grandson
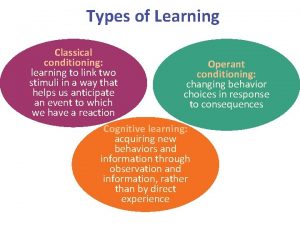
The old grandfather and his little grandson Operant conditioning vs classical conditioning
Operant conditioning vs classical conditioning Aunt alexandra quotes chapter 13
Aunt alexandra quotes chapter 13 Tin history
Tin history Ikemefuna personality
Ikemefuna personality Religious symbolism in the old man and the sea
Religious symbolism in the old man and the sea Old age physical changes
Old age physical changes Young and old prophet
Young and old prophet Food chart
Food chart Questions for tell tale heart
Questions for tell tale heart The secret of old age
The secret of old age Renaissance is a french word meaning
Renaissance is a french word meaning Soft shoe tap dance
Soft shoe tap dance The old guitarist painting
The old guitarist painting Old england kingdoms
Old england kingdoms Doreen lioy 2017
Doreen lioy 2017 The band the night they drove old dixie down
The band the night they drove old dixie down Old ucas points calculator
Old ucas points calculator