LEUCORRHOEA normal vaginal secretion Increased in amount Discharge

- Slides: 31
LEUCORRHOEA normal vaginal secretion Increased in amount
�Discharge is macroscopically and microscopically non-purulent �Permanent vulval moistness �Non irritant �Non offensive �Non pruritic
Physiological Leucorrhoea �At puberty �At ovulation �During premenstrual phase �During pregnancy
Classification of non pathogenic leucorrhoea �Cervical leucorrhoea �And Vaginal leucorrhoea
�Cervical leucorrhoea due to increased mucous secretion from endocervical glands �Chronic cervicitis �Cervical erosion �Mucous polypi �And ectropion.
Vaginal leucorrhoea �Originates in vagina. �Transudation through vaginal wall �Local congestive states like �Pregnancy state �Acquired retroversion �Prolapsed congestd ovaries �Chronic PID. , Chronic Constipation �Sedentary life
differentiated from vaginal infections �By a proper history taking �Complete medical examination A Per Speculum examination of vagina and Cx A Careful bimanual pelvic examination And a bacteriological examination.
Vaginal infections
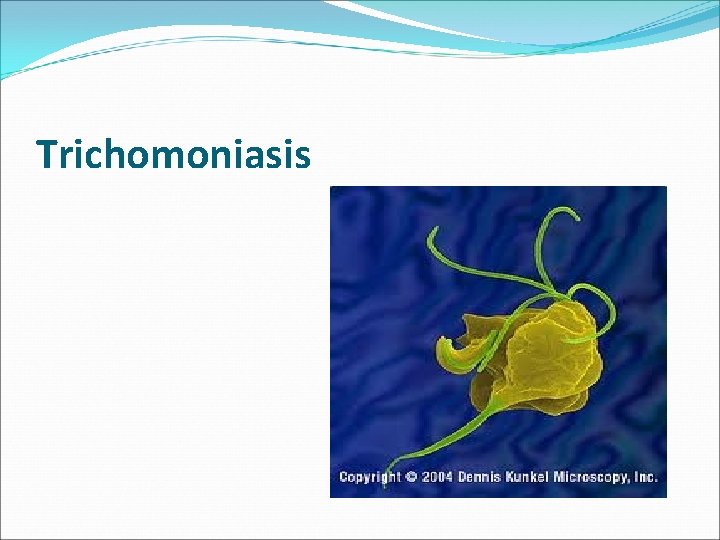
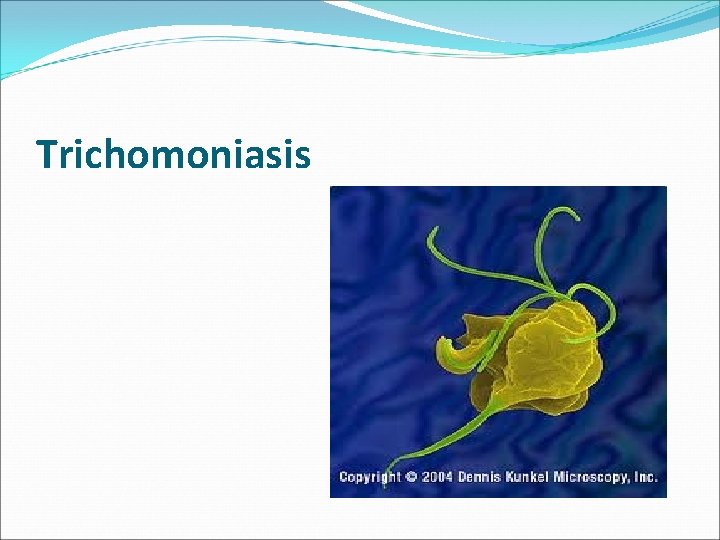
Trichomoniasis
Etiology �Most common form of vaginitis , seen in 50% women complaining of white discharge. �Can occur at any age but most commonly seen in young adults. �In vagina invariably accompanied by staphylococci , streptococci , enterococci etc.
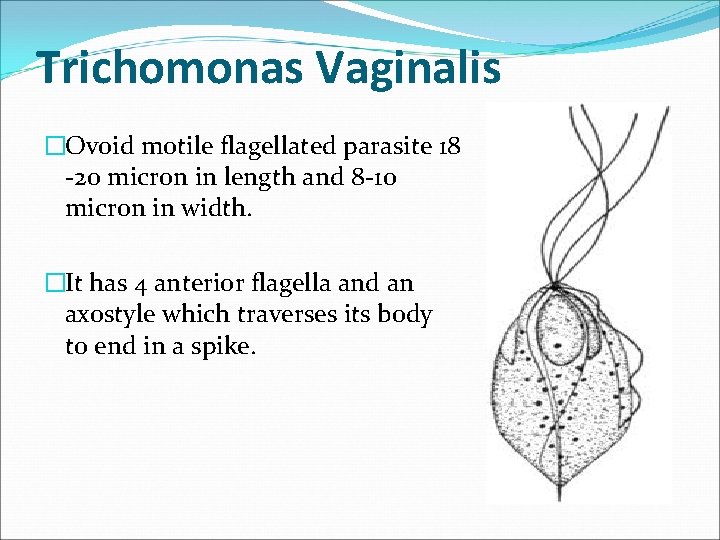
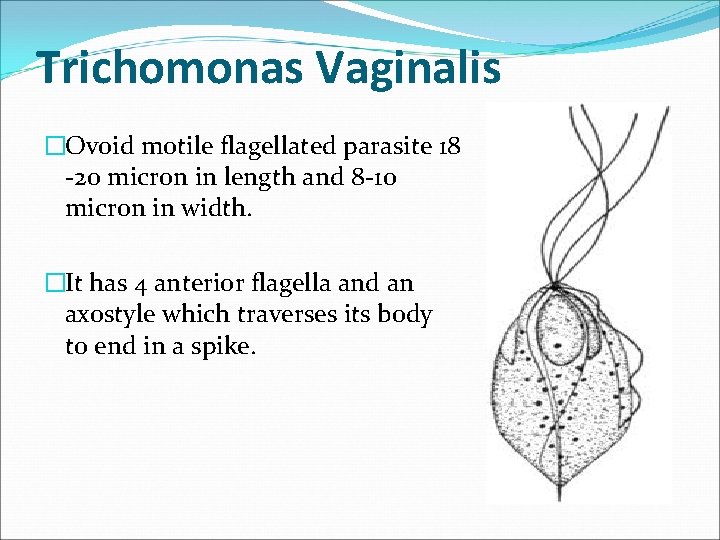
Trichomonas Vaginalis �Ovoid motile flagellated parasite 18 -20 micron in length and 8 -10 micron in width. �It has 4 anterior flagella and an axostyle which traverses its body to end in a spike.
Mode of infection �Sexual transmission from a infected asymptomatic male partner. �Indirect contact through bed linen , towels , improperly sterilized surgical instruments , contaminated swimming pools etc. �Hospital acquired.
Pathology �Essentially involve vaginal epithelium. � 70 -80 % cases cause acute or chronic urethritis. �Inflammation of Bartholin’s glands. �Involvement of endocervix to cause endocervicitis. �Optimal p. H for activity is 5. 5 -6. 5 which is seen immediately after menstruation.
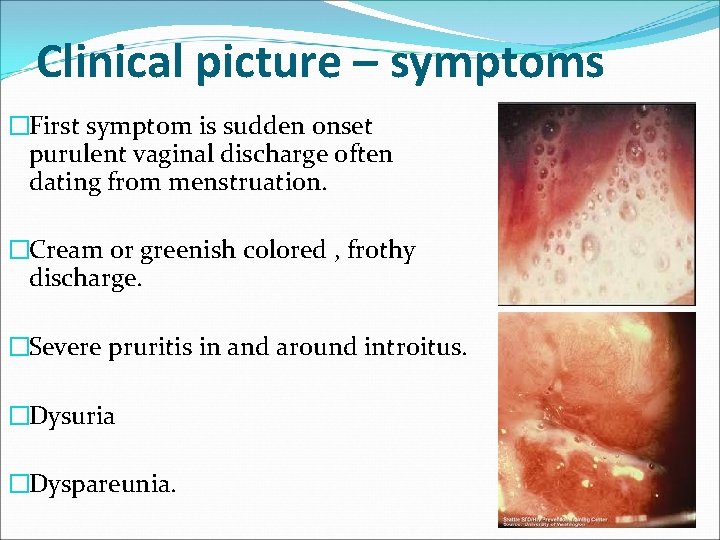
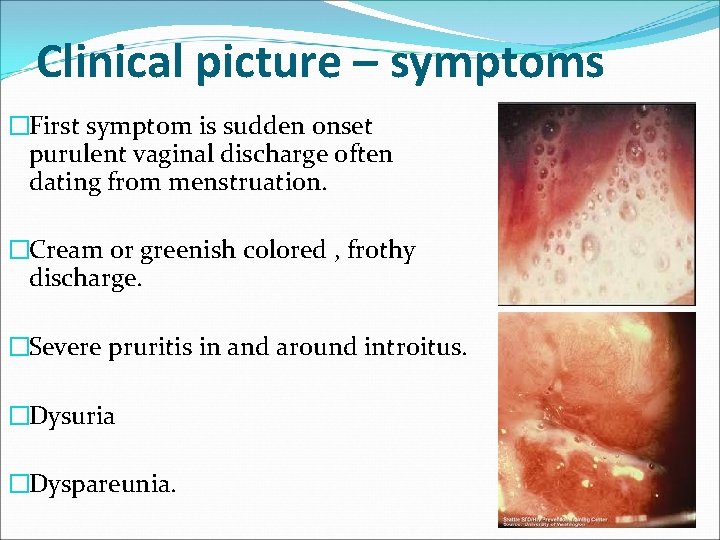
Clinical picture – symptoms �First symptom is sudden onset purulent vaginal discharge often dating from menstruation. �Cream or greenish colored , frothy discharge. �Severe pruritis in and around introitus. �Dysuria �Dyspareunia.
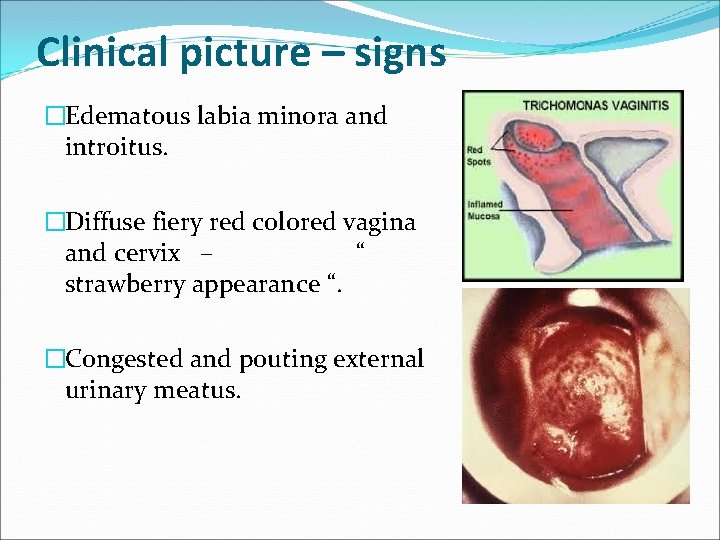
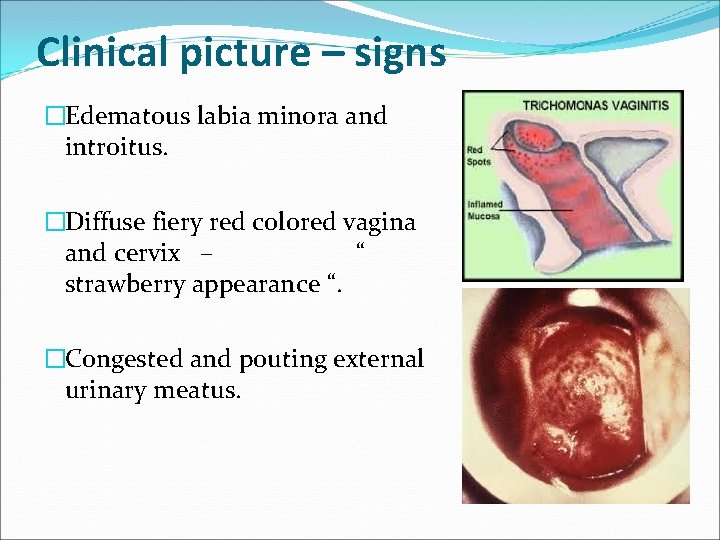
Clinical picture – signs �Edematous labia minora and introitus. �Diffuse fiery red colored vagina and cervix – “ strawberry appearance “. �Congested and pouting external urinary meatus.
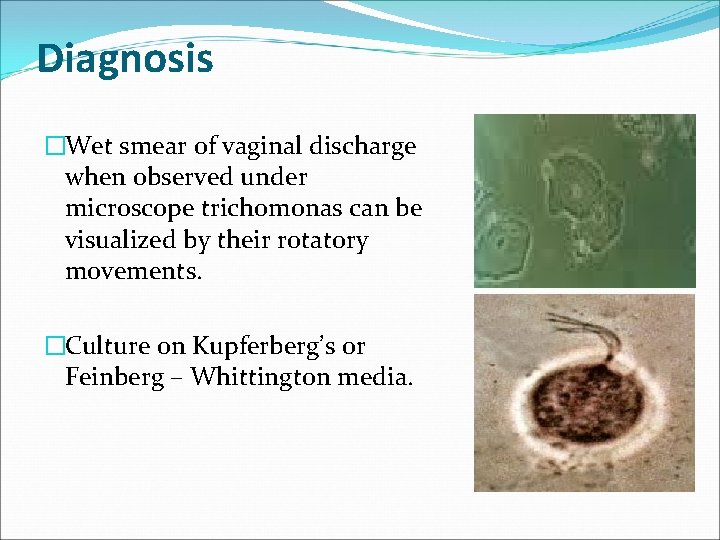
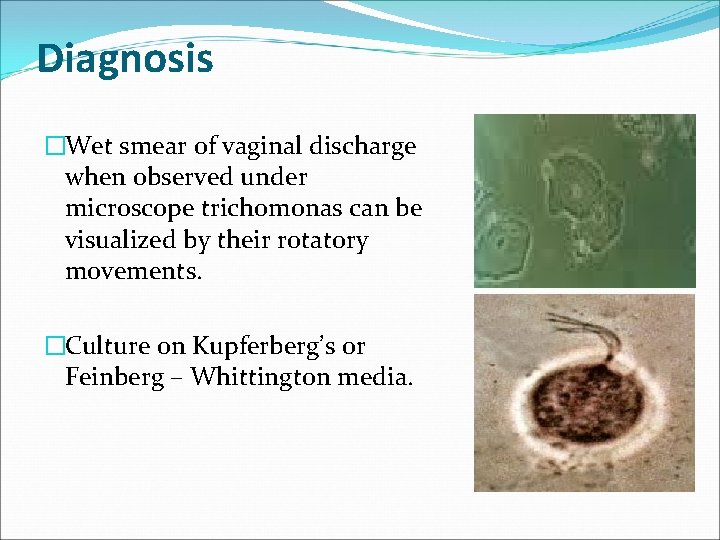
Diagnosis �Wet smear of vaginal discharge when observed under microscope trichomonas can be visualized by their rotatory movements. �Culture on Kupferberg’s or Feinberg – Whittington media.
Treatment �Metronidazole – tab 2 gm single dose for both husband wife / 400 mg twice daily for 1 week. �Secnidazole – 2 gm single dose orally equally effective with less side effects. �Metronidazole / clotrimazole – 100 mg pessary kept intravaginally for 3 -6 days. �Avoid sharing of personal clothing during treatment.

Candida vaginitis
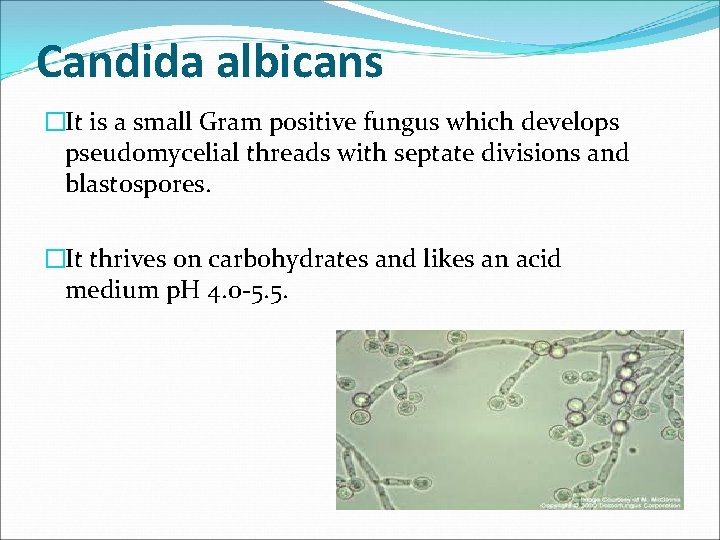
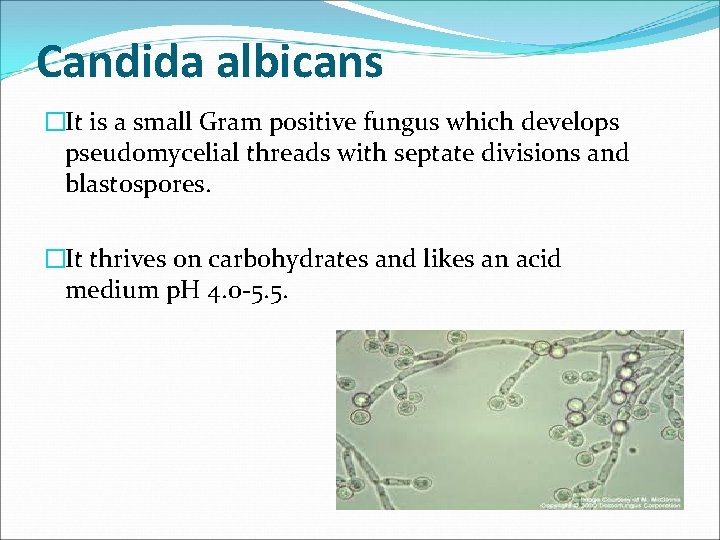
Candida albicans �It is a small Gram positive fungus which develops pseudomycelial threads with septate divisions and blastospores. �It thrives on carbohydrates and likes an acid medium p. H 4. 0 -5. 5.
Etiology �Caused by an organism called Candida albicans. �It usually has a wide distribution in the body. �It is demonstrated in the mouth (25%) , peri anal region (8%) and vagina (2025%) of all women.
Etiology �Active infection occurs in conditions like - Pregnancy - Diabetes mellitus - HIV - Anti cancer drugs - Long term use of OCPS - Prolonged antibiotic use
Mode of infection �Sexual transmission from an infected male partner. �Infection from other parts of the body- alimentary canal , hands , feet and peri anal skin. �From infected mother to the child during vaginal delivery.
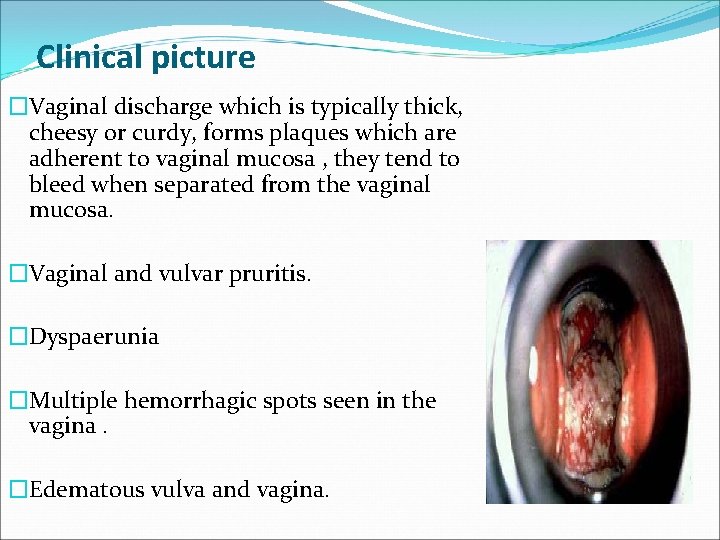
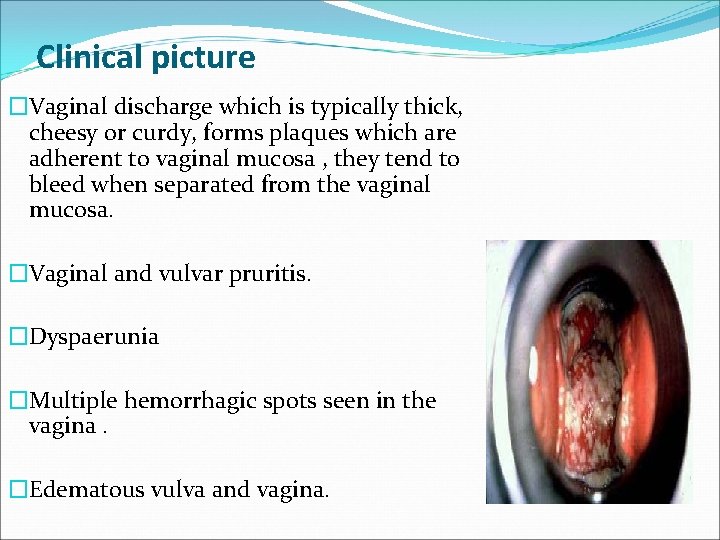
Clinical picture �Vaginal discharge which is typically thick, cheesy or curdy, forms plaques which are adherent to vaginal mucosa , they tend to bleed when separated from the vaginal mucosa. �Vaginal and vulvar pruritis. �Dyspaerunia �Multiple hemorrhagic spots seen in the vagina. �Edematous vulva and vagina.
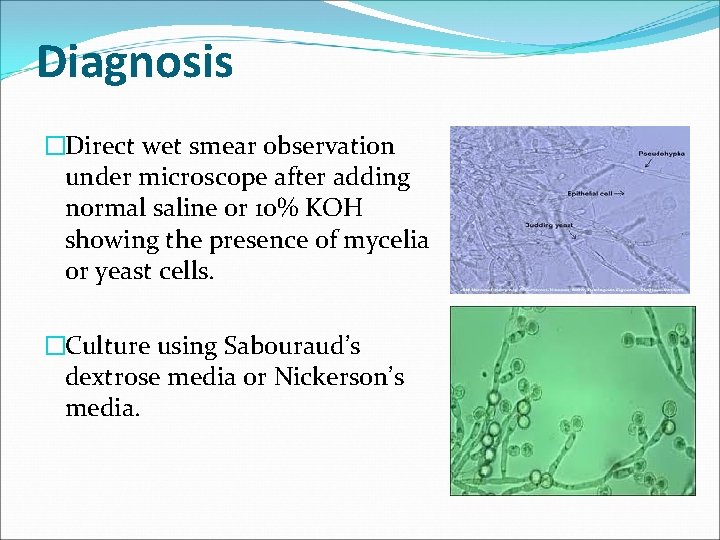
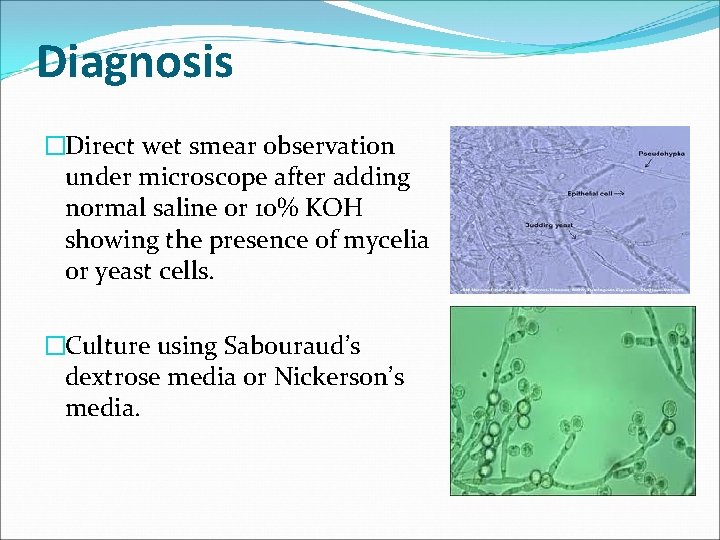
Diagnosis �Direct wet smear observation under microscope after adding normal saline or 10% KOH showing the presence of mycelia or yeast cells. �Culture using Sabouraud’s dextrose media or Nickerson’s media.
Treatment �Topical preparations – 1. Vaginal pessaries – miconazole 100 mg X 6 nights , clotrimazole 500 mg single dose , ticonazole 300 mg single dose. 2. Vaginal creams – 1% clotrimazole , 2 % miconazole , sertoconazole for 1 -5 nights. �Oral – ketoconazole 100 -200 mg BD X 5 days, itraconazole 200 mg BD X 1 day or fluconazole 150 mg single dose.
Bacterial Vaginosis
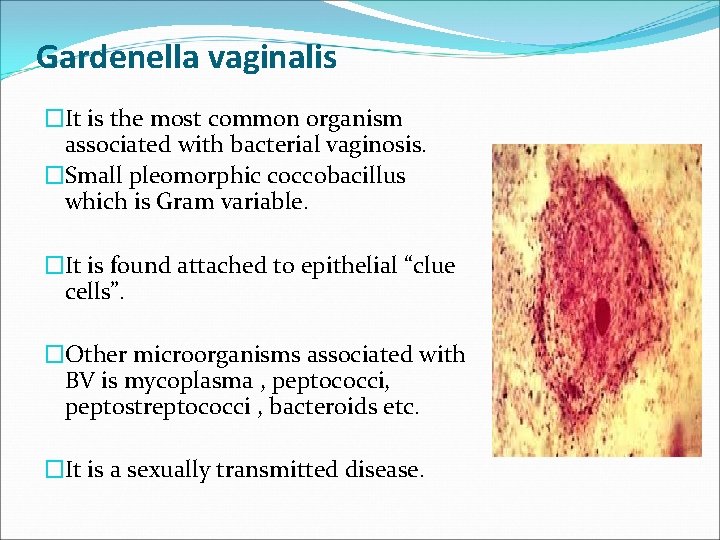
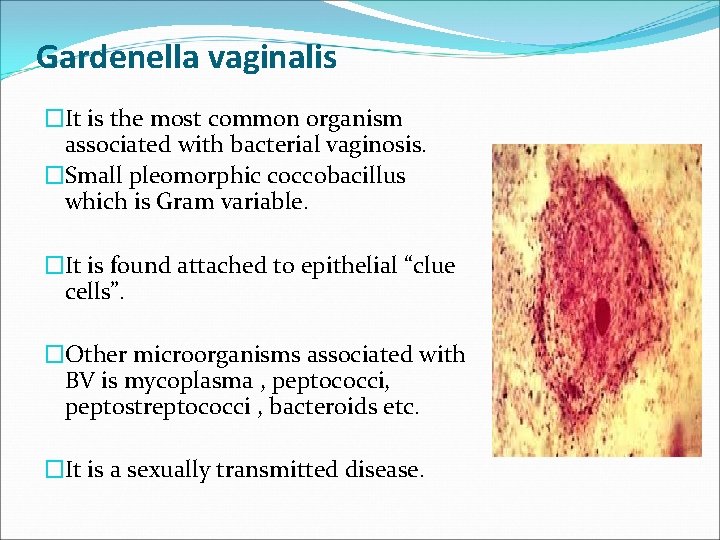
Gardenella vaginalis �It is the most common organism associated with bacterial vaginosis. �Small pleomorphic coccobacillus which is Gram variable. �It is found attached to epithelial “clue cells”. �Other microorganisms associated with BV is mycoplasma , peptococci, peptostreptococci , bacteroids etc. �It is a sexually transmitted disease.
Etiology �Commonly seen in patients with – - IUCD - Post partum endometritis - Post abortal PID - Post hysterectomy vaginal cuff cellulitis
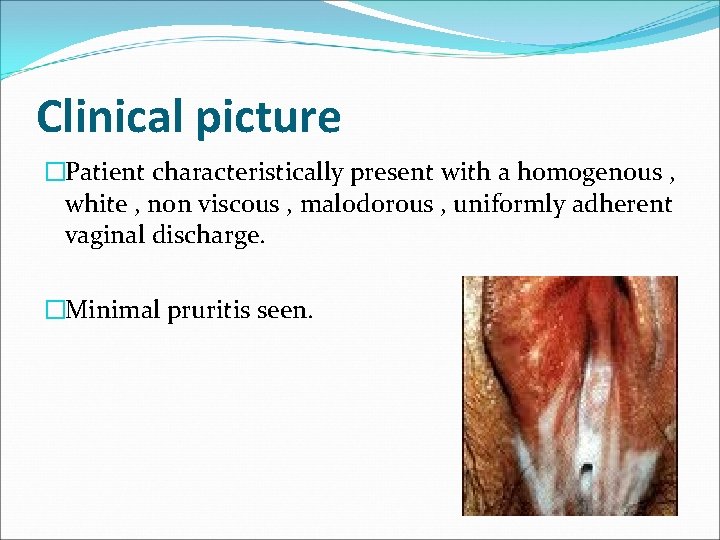
Clinical picture �Patient characteristically present with a homogenous , white , non viscous , malodorous , uniformly adherent vaginal discharge. �Minimal pruritis seen.
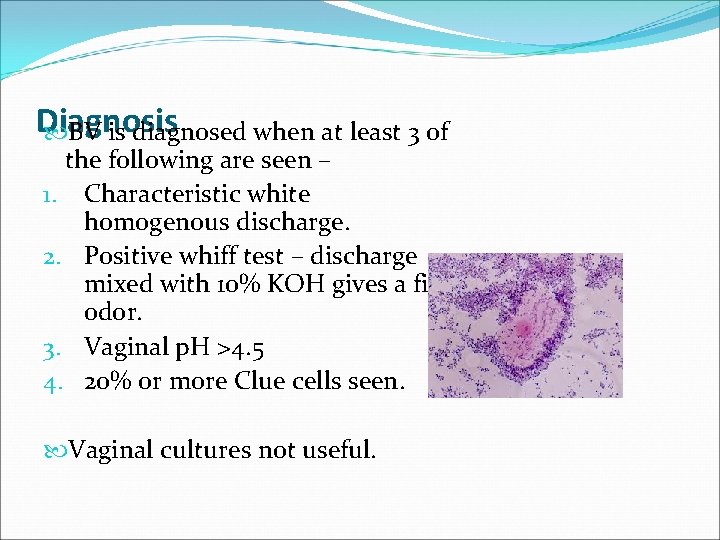
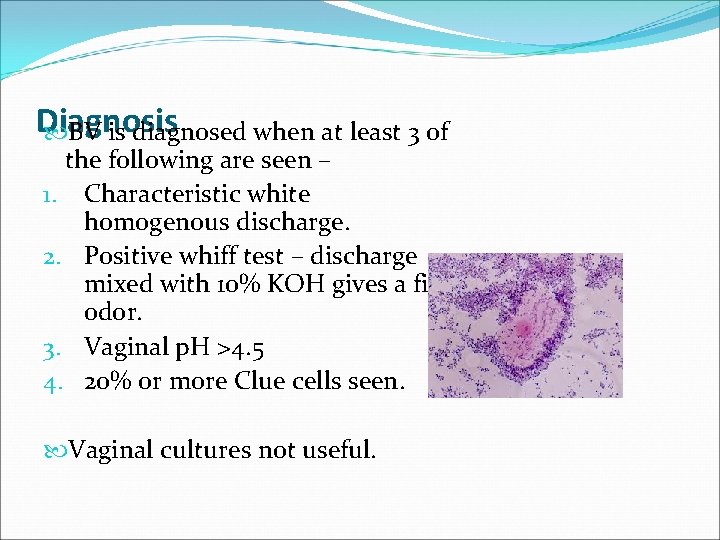
Diagnosis BV is diagnosed when at least 3 of the following are seen – 1. Characteristic white homogenous discharge. 2. Positive whiff test – discharge mixed with 10% KOH gives a fishy odor. 3. Vaginal p. H >4. 5 4. 20% or more Clue cells seen. Vaginal cultures not useful.
Treatment �Metronidazole 400 mg thrice daily for 5 -7 days. �Clindamycin 300 mg twice daily for 7 days.