Focal Peripheral Neuropathies Chapter 24 Alireza Ashraf M

- Slides: 52
Focal Peripheral Neuropathies Chapter 24 Alireza Ashraf, M. D. Professor of Physical Medicine & Rehabilitation Shiraz Medical school
Entrapment within a compartment of relatively fixed size, compression by an internal or external source, repetitive trauma and overuse, or some other etiology affecting a nerve over a finite segment is one of the most common lesions evaluated by an electrodiagnostic medicine consultant.
AXONAL LOSS n SNAP for approximately 9 -10 days n compound muscle action potential (CMAP) disappears by day 7 -8 because of neuromuscular junction transmission failure
SNAP n Preserved SNAP: n 1. PREGANGLIONIC LESION n 2. WITHIN FIRST 9 -10 DAYS n 3. PARTIAL LESION n MILD TO MODERATE lesions: side to side amplitude
CMAP may require about 7 -8 days to disappear following complete axonal Partial nerve injuries should stabilize within this time frame regarding a sequential decline in the CMAP amplitude. This implies the focal lesion is a static and not progressive type of disorder disruption.
collateral sprouting limits this parameter as a completely accurate predictor of axonal loss after several weeks.
EMG Helpful in delineating the lesion's extent when performed about 3 -4 weeks after the presumed neural insult. This 3 -4 week time frame is rather variable and depends upon the distance between the lesion site and muscle tissue voluntary motor units (reduced recruitment) within this short time frame may also be useful prior to the detectionof membrane instability.
n the presence of voluntary motor units is also important to document because it signifies that the lesion is incomplete and neural integrity is at least partially preserved
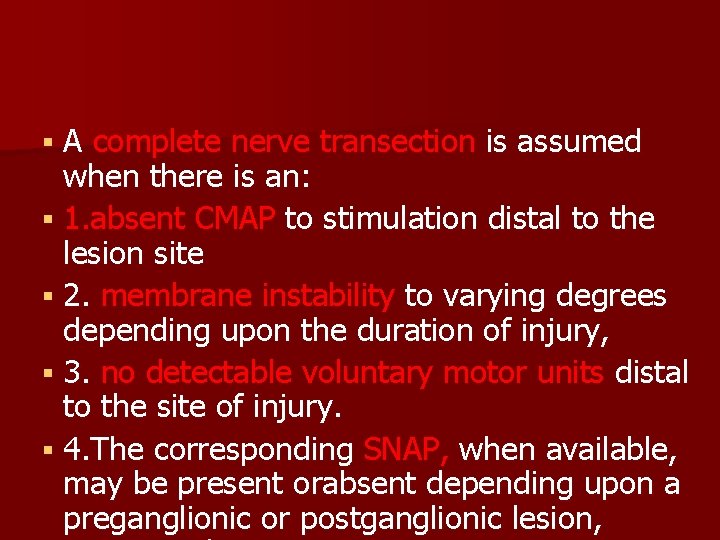
A complete nerve transection is assumed when there is an: 1. absent CMAP to stimulation distal to the lesion site 2. membrane instability to varying degrees depending upon the duration of injury, 3. no detectable voluntary motor units distal to the site of injury. 4. The corresponding SNAP, when available, may be present orabsent depending upon a preganglionic or postganglionic lesion,
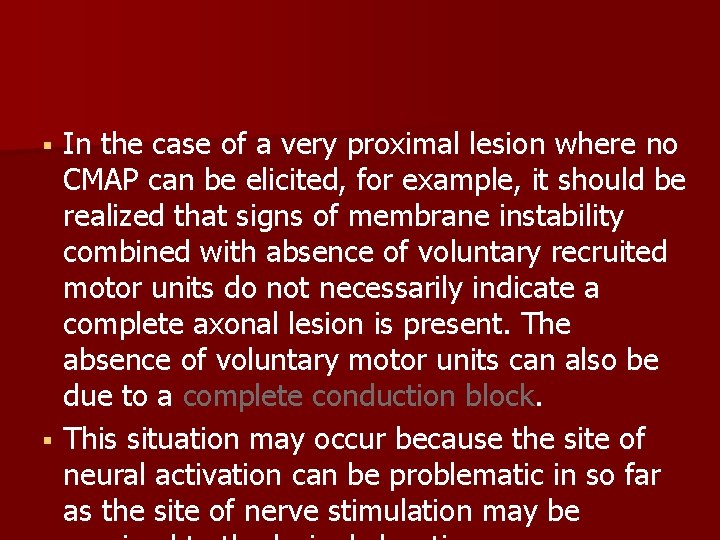
In the case of a very proximal lesion where no CMAP can be elicited, for example, it should be realized that signs of membrane instability combined with absence of voluntary recruited motor units do not necessarily indicate a complete axonal lesion is present. The absence of voluntary motor units can also be due to a complete conduction block. This situation may occur because the site of neural activation can be problematic in so far as the site of nerve stimulation may be
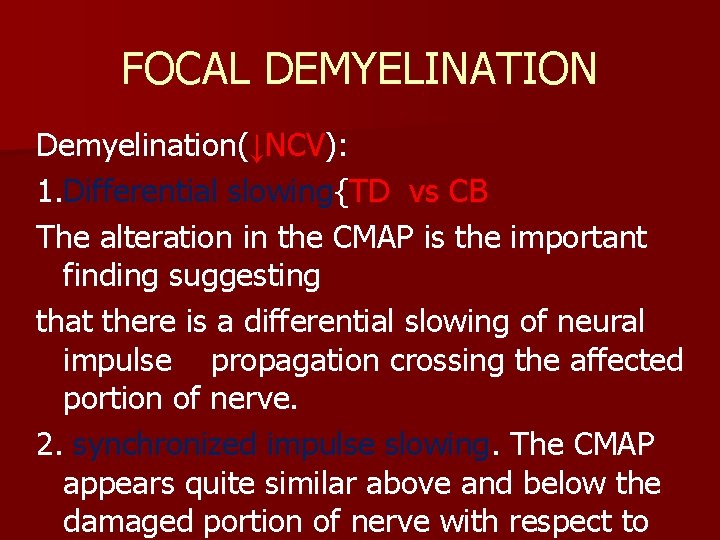
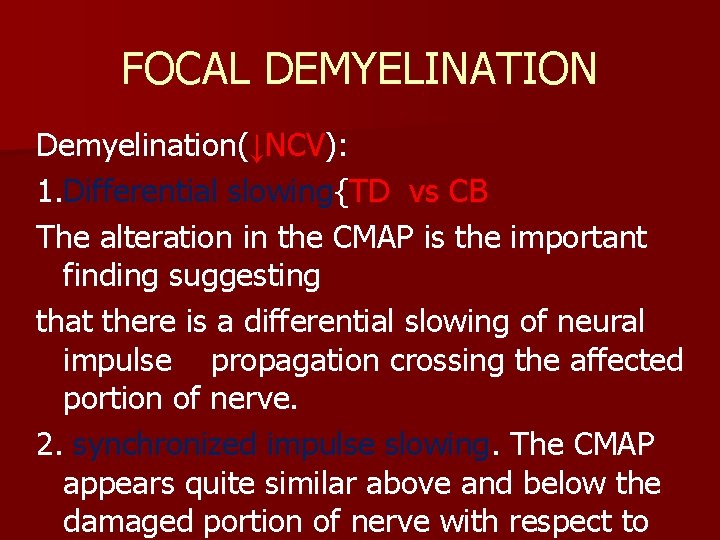
FOCAL DEMYELINATION Demyelination(↓NCV): 1. Differential slowing{TD vs CB The alteration in the CMAP is the important finding suggesting that there is a differential slowing of neural impulse propagation crossing the affected portion of nerve. 2. synchronized impulse slowing. The CMAP appears quite similar above and below the damaged portion of nerve with respect to
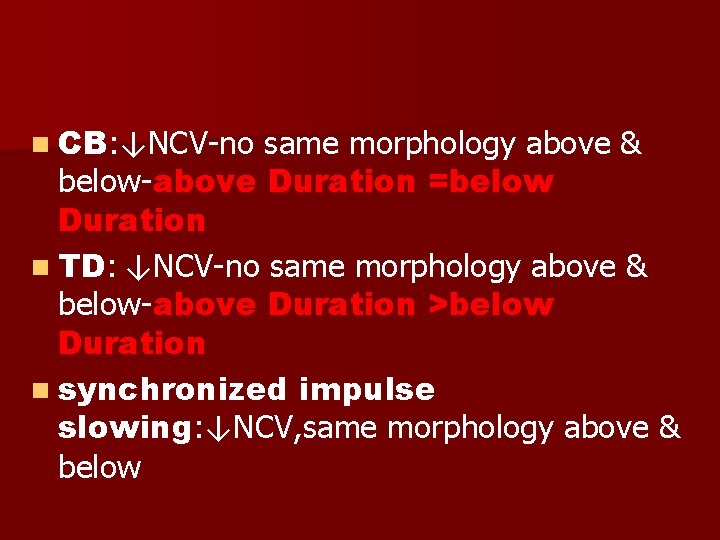
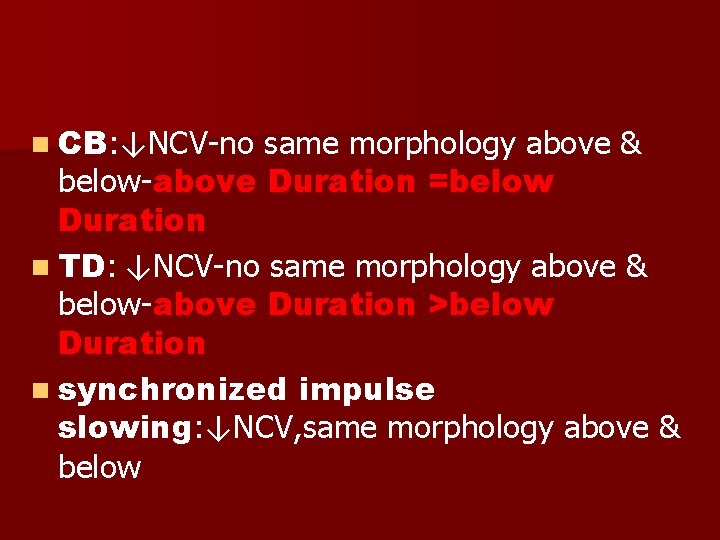
n CB: ↓NCV-no same morphology above & below-above Duration =below Duration n TD: ↓NCV-no same morphology above & below-above Duration >below Duration n synchronized impulse slowing: ↓NCV, same morphology above & below
HISTORY n acute or insidious n disease process. n All compressive nerve lesions that develop acutely should be treated conservatively, even if severe n work history, Dm, CTD
PHYSICAL EXAMINATION n pin prick, touch, vibration, and proprioception n muscle tone and deep tendon reflexes
NERVE CONDUCTION STUDIES n Nerve conduction studies are extremely important in evaluating focal peripheral neuropathies. n In addition to documenting segmental nerve conduction velocities, it is also necessary to determine the response's magnitude at various stimulation sites and distal latencies.
n SNAP amplitude across long body segments (elbow to wrist): phase cancellation secondary to temporal dispersive effects over long distances normally results in significant amplitude reductions. n Side-to-side SNAP amplitude comparisons over similar distances
Sensory Nerve Conduction Studies. The sensory fibers are usually, though not always, affected first and to a more significant degree(PNP). SNAPs from the lower limbs even with exclusively upper limb complaints whenever there is a clinical suspicion of a possible concomitant peripheral neuropathy. comparing a proximal and distal amplitude in the same limb is of less value because of the previously noted phase cancellation
Motor Nerve Conduction Studies The CMAP amp and nerve conduction velocity are perhaps the two most useful parameters The CMAP amplitude provides information regarding the number of functional axons especially when compared with the comparable response on the unaffected side The minor limitation of using velocities is the potential for inaccurate
The H-reflex is of little use in attempting to localize focal peripheral nerve lesions distal to the root level: n 1. The long pathway of impulse conduction renders it susceptible to compromise at any location along the afferent or efferent conduction course. n 2. the H-reflex is its limited distribution to primarily the tibial and median nerves. n
F-Wave. The most useful aspect of the F-wave is its long neural pathway in that it is capable of alerting one to the fact that a lesion is present at some location 1. The very nature of its long pathway renders this procedure nonspecific with respect to location 2. Also, most techniques use the shortest F-wave of multiple trials. This tends to predispose the results to a normal study, potentially missing subtle
Somatosensory Evoked Potentials (SEPs). n In the lower limb, the lateral femoral cutaneous and saphenous nerves may be more amenable to evaluation with SEPs, while the lower lateral cutaneousor posterior cutaneous nerve of the forearm in the upper limb n LATENCY ≥ AMPLITUDE
Mixed Nerve Stimulation. n The exact fiber population contributing to the potential's onset, fastest conducting fibers, is unclear and may be a mixture of motor and sensory axons, or pure sensory axons.
NEEDLE ELECTROMYOGRAPHY The most reliable finding : positive sharp waves and fibrillation potentials in a distribution compatible with an individual peripheral nerve as opposedto a root or plexus pattern. NL EMG: 1. peripheral nerve trunks contain multiple funiculi 2. Membrane instability also tends to be self-inhibiting 3. The needle electrode is placed in a partially denervated muscle and not located in the portion of this muscle containing the denervated fibers 4. Anomalous innervation
n MUAP morphologic changes and alterations in recruitment may also be of assistance in diagnosing focal peripheral neuropathies.
ANATOMY of median nerve and medial cords→each give off a major terminal branch, lateral and medial root of the median nerve, respectively, which fuse about the axillary artery to form the median nerve (C 5, C 6, and C 7, C 8 and T I) n lateral n 5 cm proximal to flex. retinaculom : Medial to FCR & LATERAL to P. long

carpal tunnel: Eight tendons of the superficial and deep finger flexors, and the flexor pollicis longus tendon and median nerve
Neural Branching The first muscular branch to arise from the median nerve is to the pronator teres 40 -58%, the branch to the pronator teres muscle originates proximal to the medial epicondyle. The next muscular branch off the median nerve is to the flexor carpi radialis Palmaris logus The flexor digitorum superficialis muscle is then innervated by either a separate branch from the main median nerve trunk, or from multiple branches supplying the flexor
n Approximately 2 -8 (mean 5. 1) cm distal to the medial epicondyle, the relatively large anterior interosseous nerve originates from the median nerve trunk to course distally and superficial to the FDP n The first muscle supplied by the A. I. O is the flexor digitorum profundus n Flexor pollicis longus And pronator quadratus
The last branch given off by the main trunk of the median nervein the forearm is the palmar cutaneous branch of the median nerve. cutaneous sensation to the bases of thenar and hypothenar eminencies as well as a small area of skin in the midpalm region. It may also be completely absent, in which case lateral antebrachial cutaneous (musculocutaneous) and superficial radial
n the carpal tunnel is bounded by four carpal bones and a tough transverse carpal ligament n Before entering the carpal tunnel, the median nerve is roughly cylindrical to oval in shape. n Just prior to reaching the distal edge of the transverse carpal ligament, the median nerve splits into lateral and medial limbs a thenar or recurrent (motor)
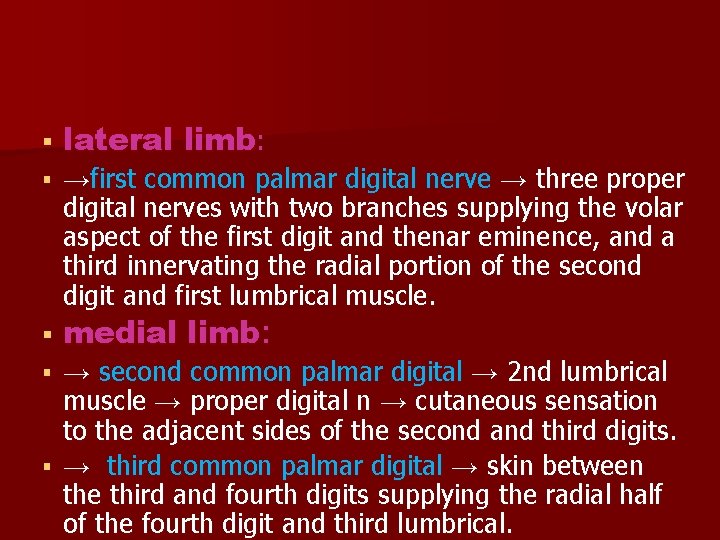
lateral limb: →first common palmar digital nerve → three proper digital nerves with two branches supplying the volar aspect of the first digit and thenar eminence, and a third innervating the radial portion of the second digit and first lumbrical muscle. medial limb: → second common palmar digital → 2 nd lumbrical muscle → proper digital n → cutaneous sensation to the adjacent sides of the second and third digits. → third common palmar digital → skin between the third and fourth digits supplying the radial half of the fourth digit and third lumbrical.
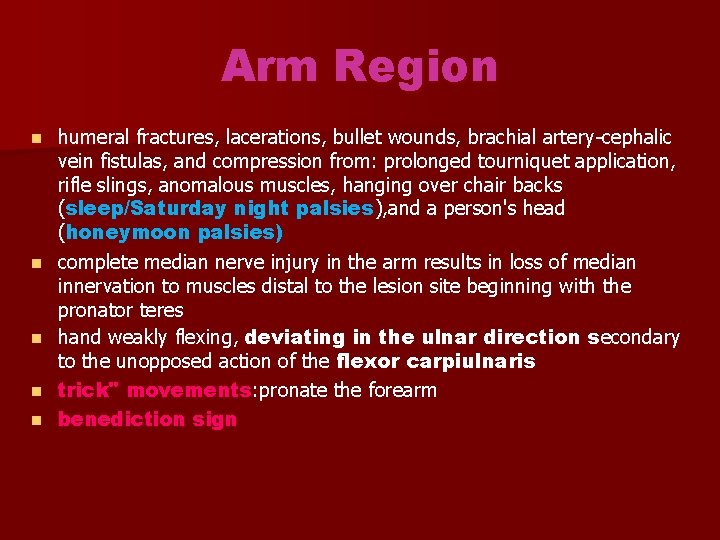
Arm Region n n humeral fractures, lacerations, bullet wounds, brachial artery-cephalic vein fistulas, and compression from: prolonged tourniquet application, rifle slings, anomalous muscles, hanging over chair backs (sleep/Saturday night palsies), and a person's head (honeymoon palsies) complete median nerve injury in the arm results in loss of median innervation to muscles distal to the lesion site beginning with the pronator teres hand weakly flexing, deviating in the ulnar direction secondary to the unopposed action of the flexor carpiulnaris trick" movements: pronate the forearm benediction sign
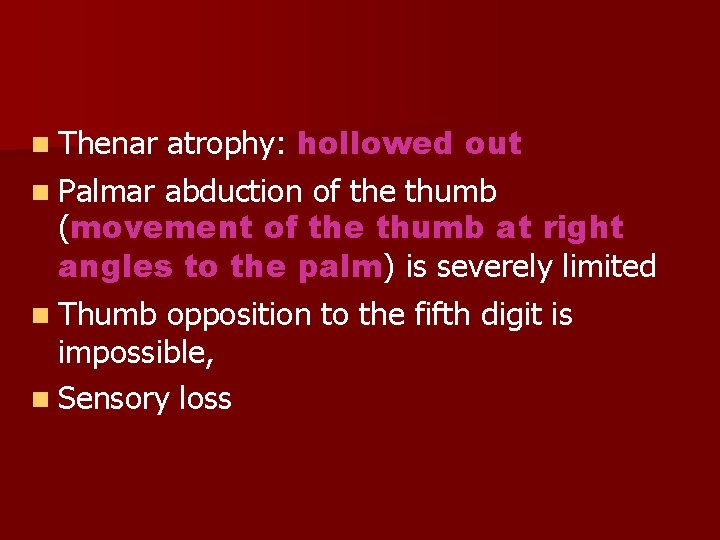
atrophy: hollowed out n Palmar abduction of the thumb (movement of the thumb at right angles to the palm) is severely limited n Thumb opposition to the fifth digit is impossible, n Sensory loss n Thenar
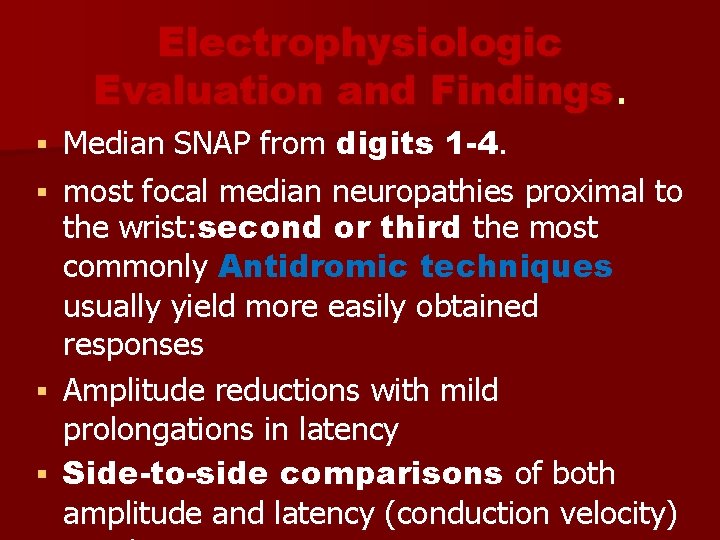
Electrophysiologic Evaluation and Findings. Median SNAP from digits 1 -4. most focal median neuropathies proximal to the wrist: second or third the most commonly Antidromic techniques usually yield more easily obtained responses Amplitude reductions with mild prolongations in latency Side-to-side comparisons of both amplitude and latency (conduction velocity)
n median SNAP from the second or third digit displaying a reduced amplitude and possibly prolonged latency. n ulnar and sup radial SNAP
CMAP from the APB is the most common median motor nerve technique. A lesion in the arm would be expected to result in a CMAP reduction when obtained from wrist stimulation and as compared with the contralateral side. In arm lesions, stimulate in the axilla as well as in the antecubital fossa or just proximal to this site, i. e. , the distal arm CMAP obtained with axilla stimulation is significantly less than 80% of that with elbow excitation, → conduction block→good prognosis A reduced amplitude at all stimulation sites, but no drop in NCV across the arm, is suggestive of an injury producing primarily axonal loss
n n n wait about 2 -4 weeks prior to performing the needle electromyographic examination depending upon the distance between the lesion and muscle tissue. membrane instability can be expected in all muscles innervated by the median nerve beginning with the pronator teres Performing the needle examination prior to the development of membrane instability only reveals recruitment abnormalities provided the lesion has affected a sufficient number of axons. motor conduction studies and needle electromyographic evaluation should be performed on more than just median-innervated muscles It is entirely possible to find positive sharp waves and fibrillation potentials in radial and ulnar innervated muscles despite corresponding "normal”CMAPs and SNAPs
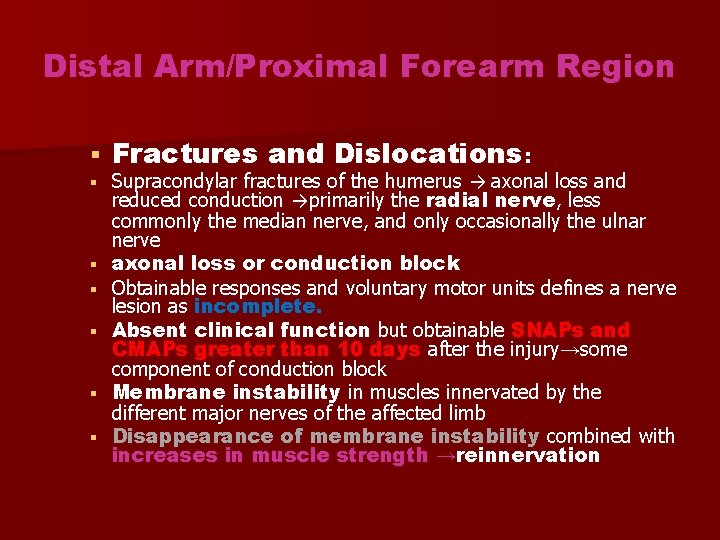
Distal Arm/Proximal Forearm Region Fractures and Dislocations: Supracondylar fractures of the humerus → axonal loss and reduced conduction →primarily the radial nerve, less commonly the median nerve, and only occasionally the ulnar nerve axonal loss or conduction block Obtainable responses and voluntary motor units defines a nerve lesion as incomplete. Absent clinical function but obtainable SNAPs and CMAPs greater than 10 days after the injury→some component of conduction block Membrane instability in muscles innervated by the different major nerves of the affected limb Disappearance of membrane instability combined with increases in muscle strength →reinnervation
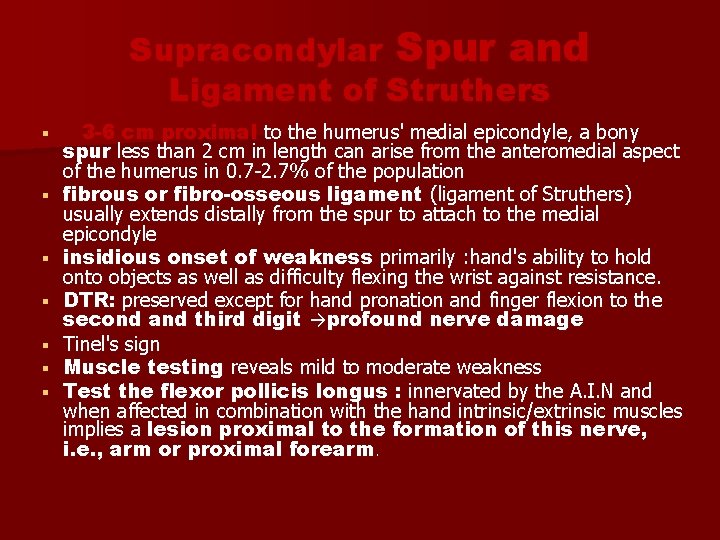
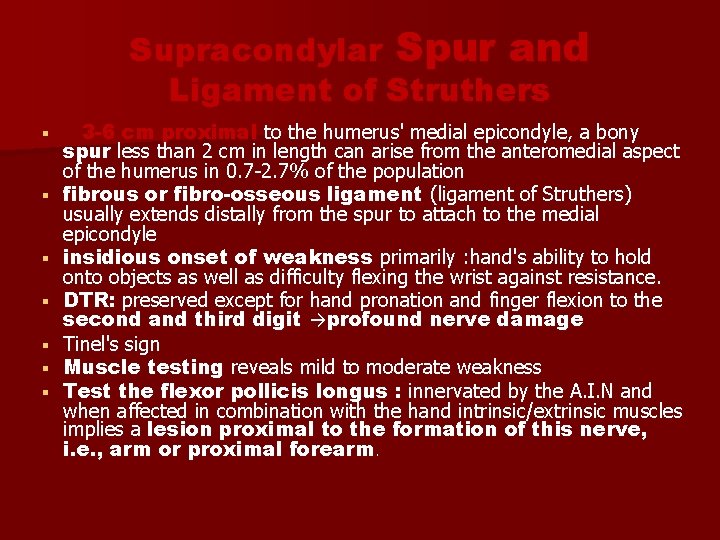
Supracondylar Spur and Ligament of Struthers 3 -6 cm proximal to the humerus' medial epicondyle, a bony spur less than 2 cm in length can arise from the anteromedial aspect of the humerus in 0. 7 -2. 7% of the population fibrous or fibro-osseous ligament (ligament of Struthers) usually extends distally from the spur to attach to the medial epicondyle insidious onset of weakness primarily : hand's ability to hold onto objects as well as difficulty flexing the wrist against resistance. DTR: preserved except for hand pronation and finger flexion to the second and third digit →profound nerve damage Tinel's sign Muscle testing reveals mild to moderate weakness Test the flexor pollicis longus : innervated by the A. I. N and when affected in combination with the hand intrinsic/extrinsic muscles implies a lesion proximal to the formation of this nerve, i. e. , arm or proximal forearm.
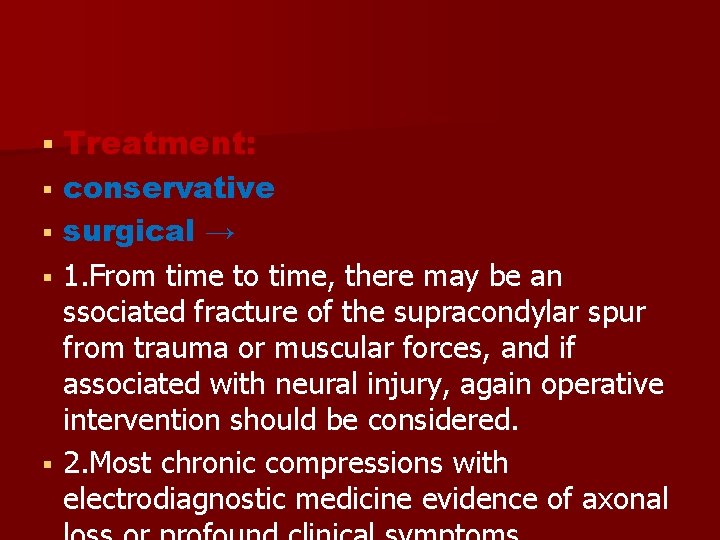
Treatment: conservative surgical → 1. From time to time, there may be an ssociated fracture of the supracondylar spur from trauma or muscular forces, and if associated with neural injury, again operative intervention should be considered. 2. Most chronic compressions with electrodiagnostic medicine evidence of axonal
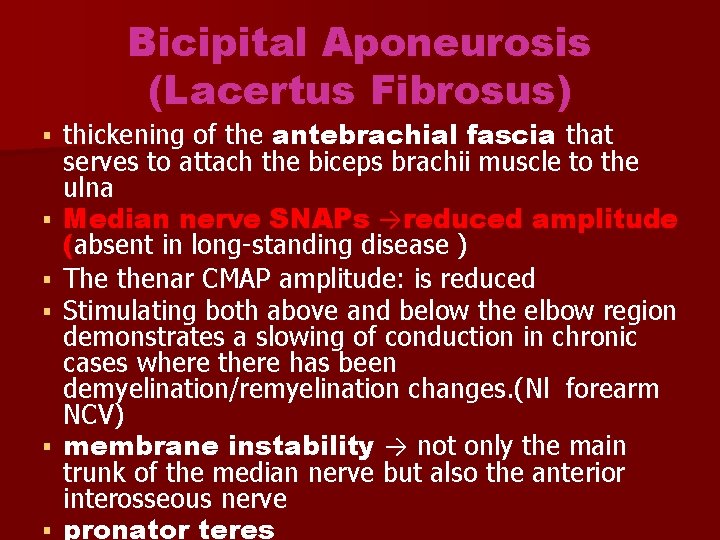
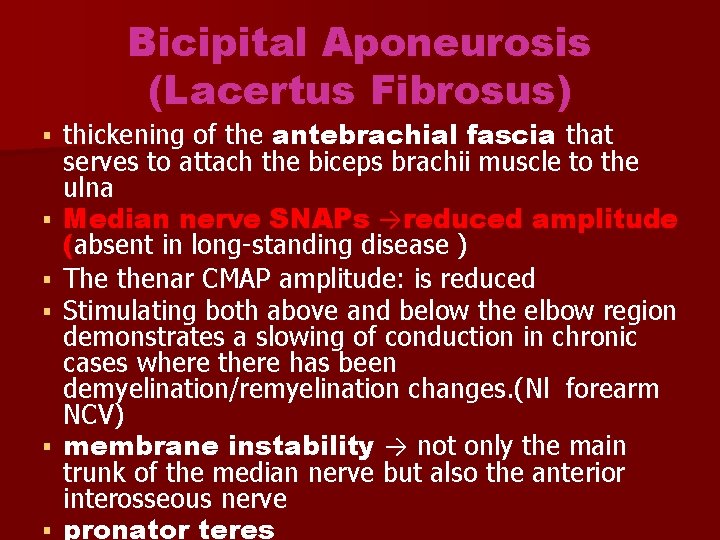
Bicipital Aponeurosis (Lacertus Fibrosus) thickening of the antebrachial fascia that serves to attach the biceps brachii muscle to the ulna Median nerve SNAPs →reduced amplitude (absent in long-standing disease ) The thenar CMAP amplitude: is reduced Stimulating both above and below the elbow region demonstrates a slowing of conduction in chronic cases where there has been demyelination/remyelination changes. (Nl forearm NCV) membrane instability → not only the main trunk of the median nerve but also the anterior interosseous nerve pronator teres
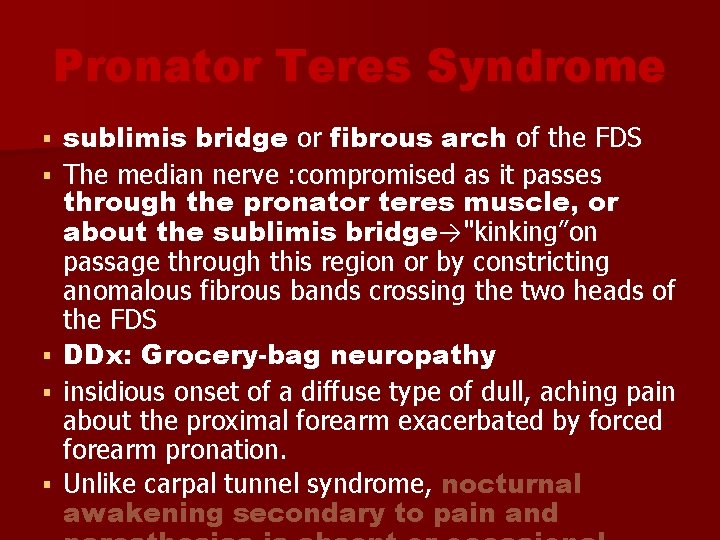
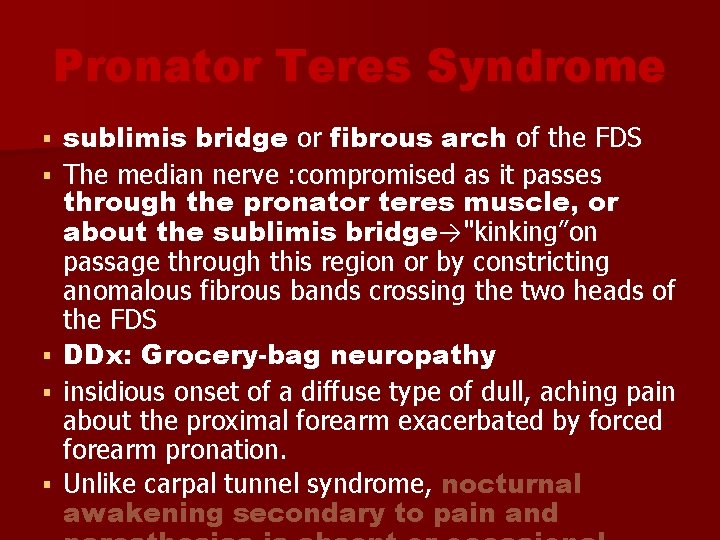
Pronator Teres Syndrome sublimis bridge or fibrous arch of the FDS The median nerve : compromised as it passes through the pronator teres muscle, or about the sublimis bridge→"kinking”on passage through this region or by constricting anomalous fibrous bands crossing the two heads of the FDS DDx: Grocery-bag neuropathy insidious onset of a diffuse type of dull, aching pain about the proximal forearm exacerbated by forced forearm pronation. Unlike carpal tunnel syndrome, nocturnal awakening secondary to pain and
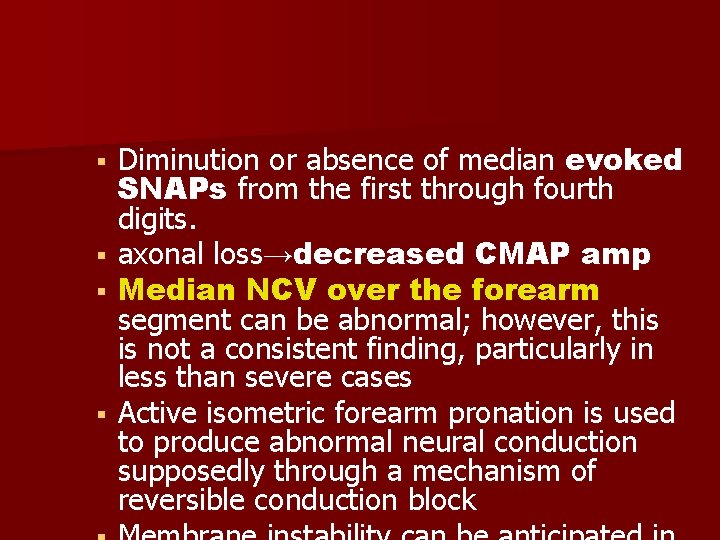
Diminution or absence of median evoked SNAPs from the first through fourth digits. axonal loss→decreased CMAP amp Median NCV over the forearm segment can be abnormal; however, this is not a consistent finding, particularly in less than severe cases Active isometric forearm pronation is used to produce abnormal neural conduction supposedly through a mechanism of reversible conduction block
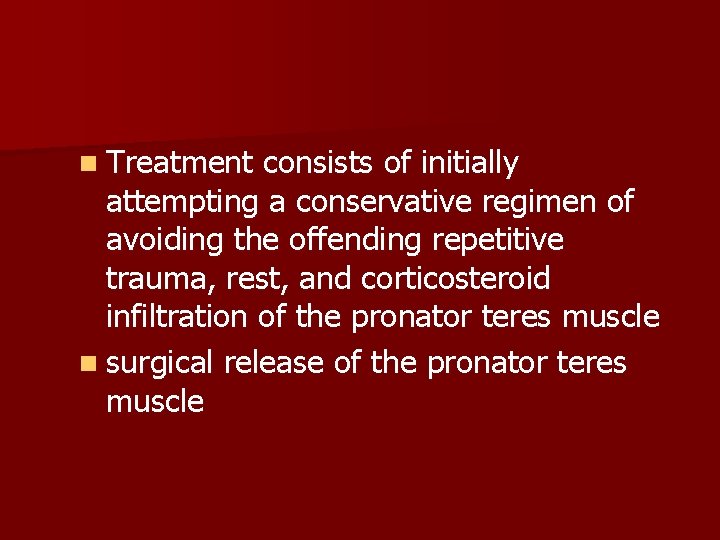
n Treatment consists of initially attempting a conservative regimen of avoiding the offending repetitive trauma, rest, and corticosteroid infiltration of the pronator teres muscle n surgical release of the pronator teres muscle
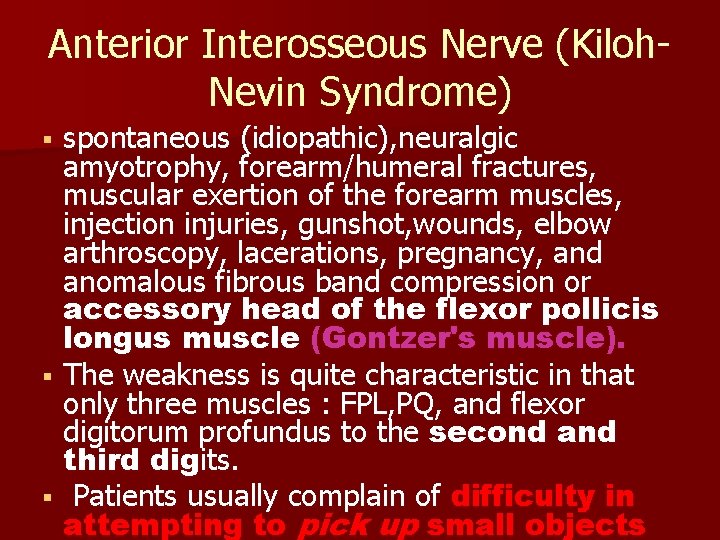
Anterior Interosseous Nerve (Kiloh. Nevin Syndrome) spontaneous (idiopathic), neuralgic amyotrophy, forearm/humeral fractures, muscular exertion of the forearm muscles, injection injuries, gunshot, wounds, elbow arthroscopy, lacerations, pregnancy, and anomalous fibrous band compression or accessory head of the flexor pollicis longus muscle (Gontzer's muscle). The weakness is quite characteristic in that only three muscles : FPL, PQ, and flexor digitorum profundus to the second and third digits. Patients usually complain of difficulty in attempting to pick up small objects
P/E Sensation : intact in the affected limb. MMT : must be properly performed to elicit weakness in the appropriate distribution For the first digit, the MCP joint is braced in extension by the examiner and the patient is asked to flex just the distal phalanx→FPL(MOST RELIABLE). A similar maneuver is performed for the remaining digits while also stabilizing the proximal IP joint. This procedure eliminates the flexor digitorum superficialis muscle and isolates the flexor digitorum profundus muscle's action on the terminal phalanx. A patient with a lesion to the anterior interosseous nerve will be unable to exert much in the way of terminal phalanx
The PQ’ clinical function is difficult to isolate from the pronator teres, but this can be attempted by flexing the forearm and asking the patient to resist supination. A useful clinical test is to ask the patient to forcefully approximate the finger pulps of the first and second digits in the "OK" sign weakness of the flexor pollicis longus and variable sparing of the pronator quadratus and profundi muscles suggesting a partial anterior interosseous syndrome long finger flexors were primarily innervated by the ulnar nerve pronator quadratus muscle is overwhelmed by the pronator teres muscle because of poor testing
Rarely, the fascicles destined to become the anterior interosseous nerve may be preferentially injured more proximally in the median nerve where they are tightly grouped. These cases present exactly like a lesion more distally affecting solely the anterior interosseous nerve despite an injury to the proximal median nerve trunk such as in humeral fractures. → (STIR) can reveal
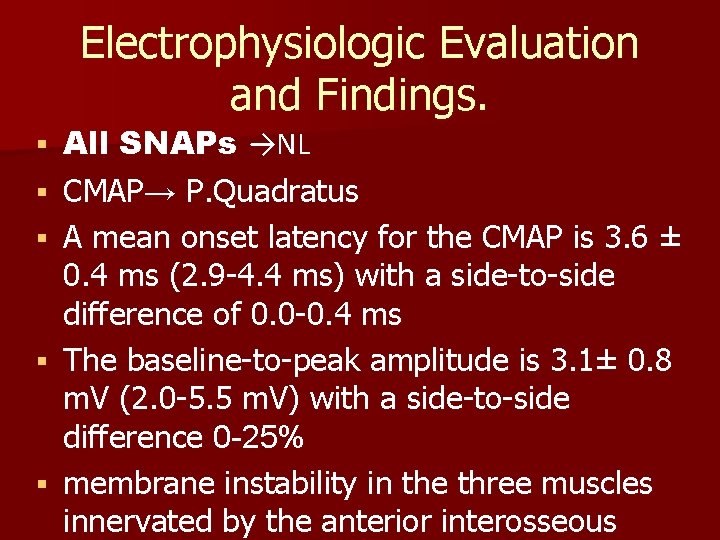
Electrophysiologic Evaluation and Findings. All SNAPs →NL CMAP→ P. Quadratus A mean onset latency for the CMAP is 3. 6 ± 0. 4 ms (2. 9 -4. 4 ms) with a side-to-side difference of 0. 0 -0. 4 ms The baseline-to-peak amplitude is 3. 1± 0. 8 m. V (2. 0 -5. 5 m. V) with a side-to-side difference 0 -25% membrane instability in the three muscles innervated by the anterior interosseous
A. I. N LESION with Martin-Gruber anastomosis conveys fibers to the ulnar nerve→innervate the first through third dorsal interossei , adductor pollicis and occasionally the abductor digiti minimi muscles Associated weakness of second and fifth digit abduction as well as adduction of the first digit. Membrane instability is observed not only in the anticipated three muscles innervated by the anterior interosseous nerve, but also in the ulnar-innervated hand intrinsic muscles. the ulnar nerve's palmar digital and dorsal ulnar cutaneous SNAPs are normal, as is conduction across the
n Rheumatoid arthritis → experience painless tendon ruptures of the flexor pollicis longus and flexor digitorum profundus muscles to the index finger, thus simulating an anterior interosseous nerve injury. n Treatment for the anterior interosseous entrapment syndrome is at first conservative.
Forearm Nerve lesions Elevated pressures in the flexor forearm compartment (Volkmann‘s ischemic contracture) secondary to hemorrhage in hemophiliacs from arterial/venous punctures, and generalized trauma, nerve entrapment in radius/ulna fracture fragments, direct needle injuries, and arteriovenous fistulas. Patients mayor may not complain of pain, but the motor and sensory consequences of median nerve insult are noted quite easily. Physical examination demonstrates diminished sensation in the hand consistent with a median nerve injury, as does weakness of thenar muscles innervated by this nerve Abnormalities in the median evoked SNAPs from the