FOCAL ACTIVE COLITIS PATTERN Focal active colitis FAC










- Slides: 39
FOCAL ACTIVE COLITIS PATTERN
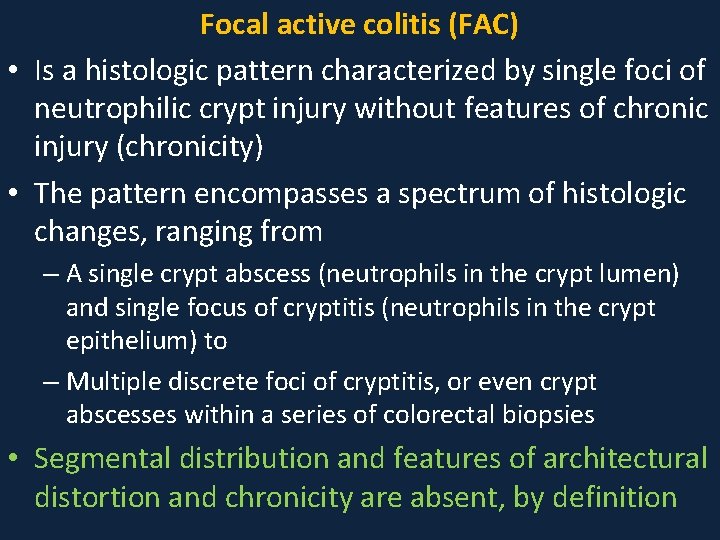
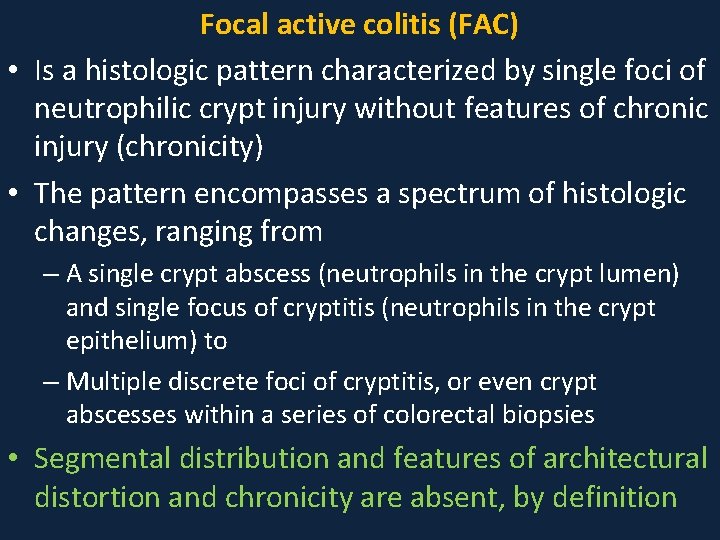
Focal active colitis (FAC) • Is a histologic pattern characterized by single foci of neutrophilic crypt injury without features of chronic injury (chronicity) • The pattern encompasses a spectrum of histologic changes, ranging from – A single crypt abscess (neutrophils in the crypt lumen) and single focus of cryptitis (neutrophils in the crypt epithelium) to – Multiple discrete foci of cryptitis, or even crypt abscesses within a series of colorectal biopsies • Segmental distribution and features of architectural distortion and chronicity are absent, by definition
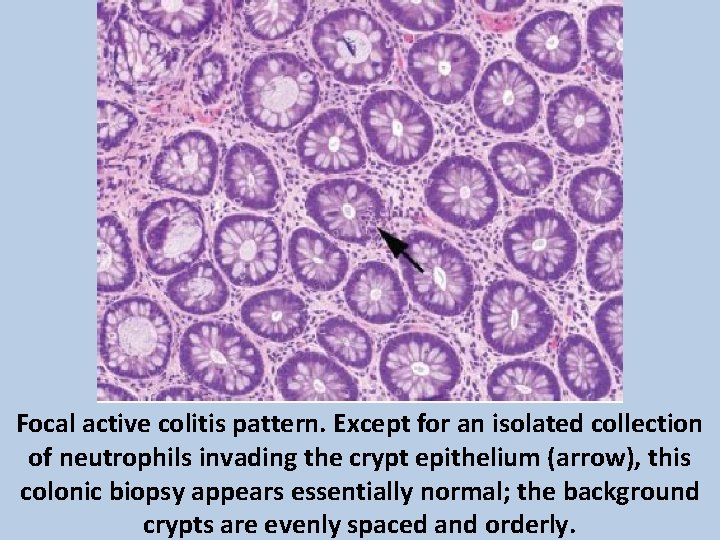
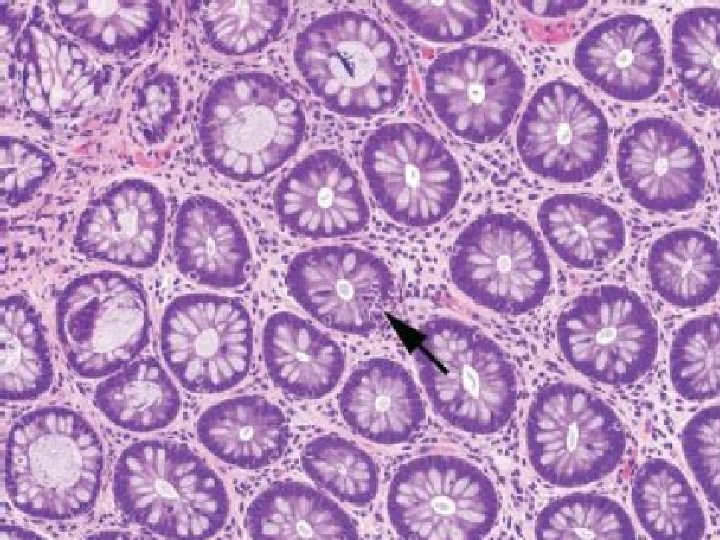
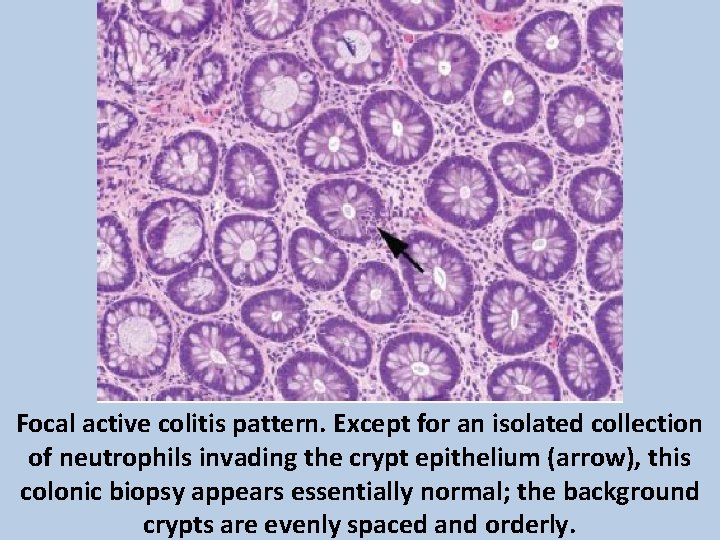
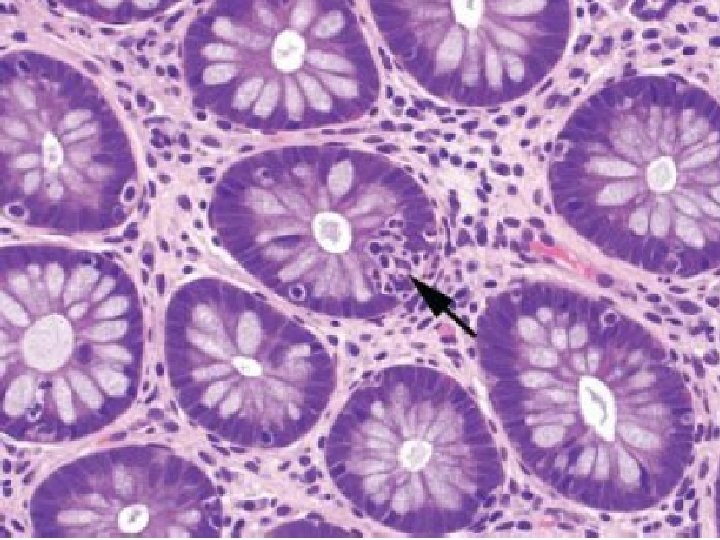
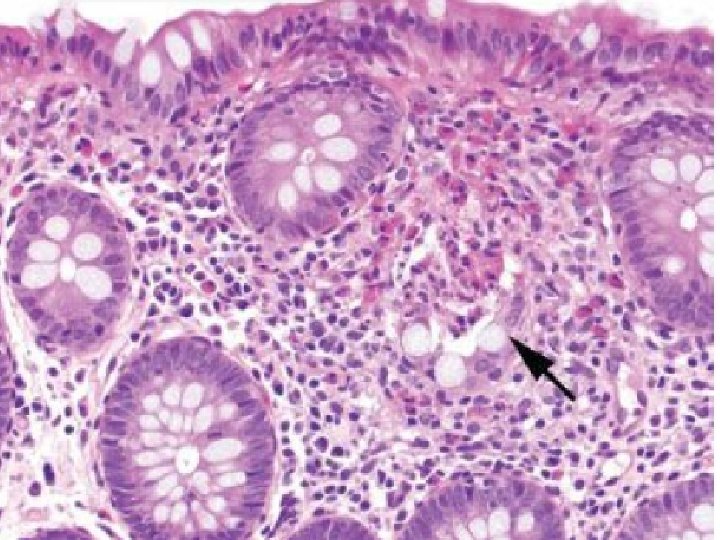
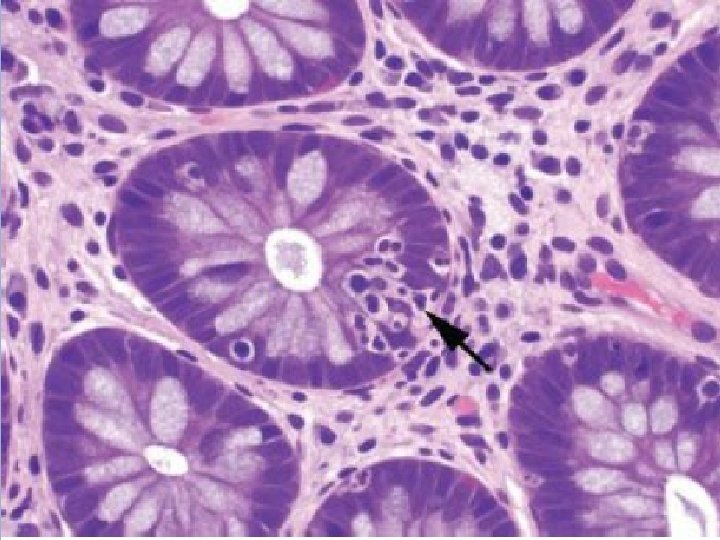
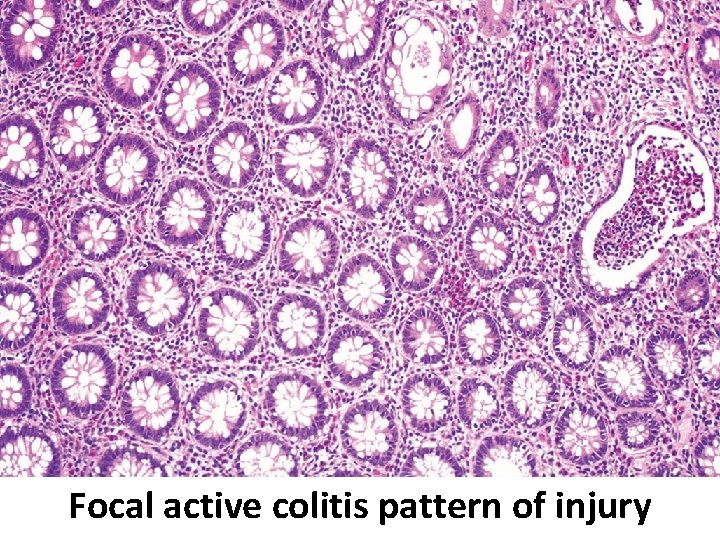
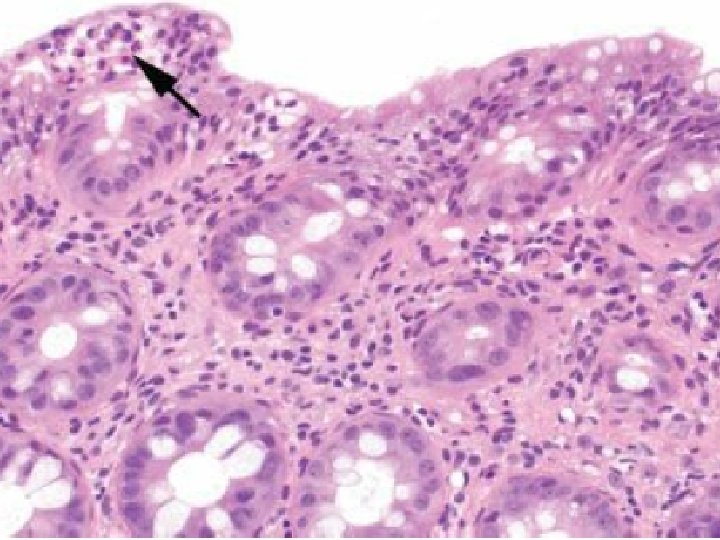
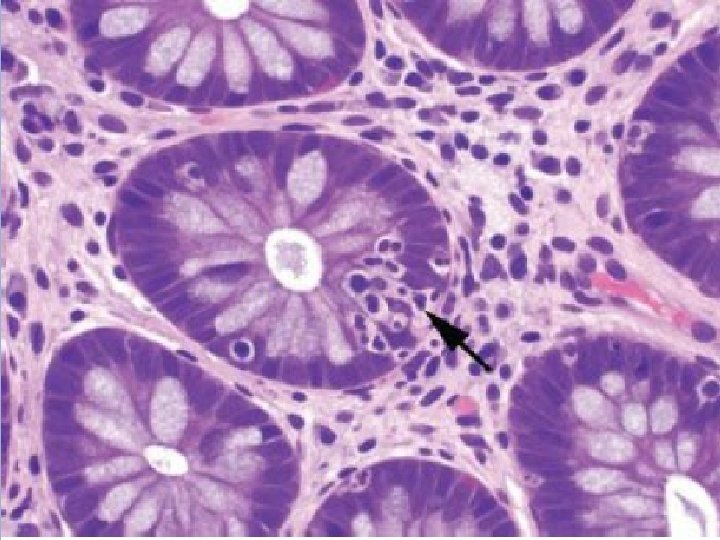
Focal active colitis pattern. Except for an isolated collection of neutrophils invading the crypt epithelium (arrow), this colonic biopsy appears essentially normal; the background crypts are evenly spaced and orderly.
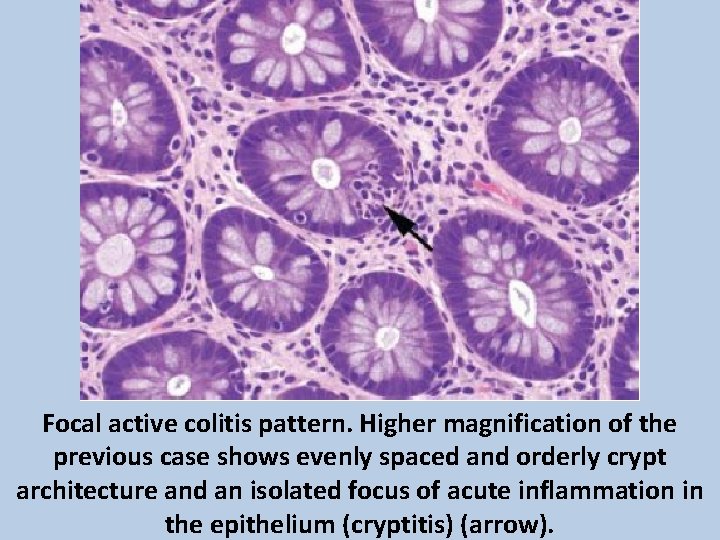
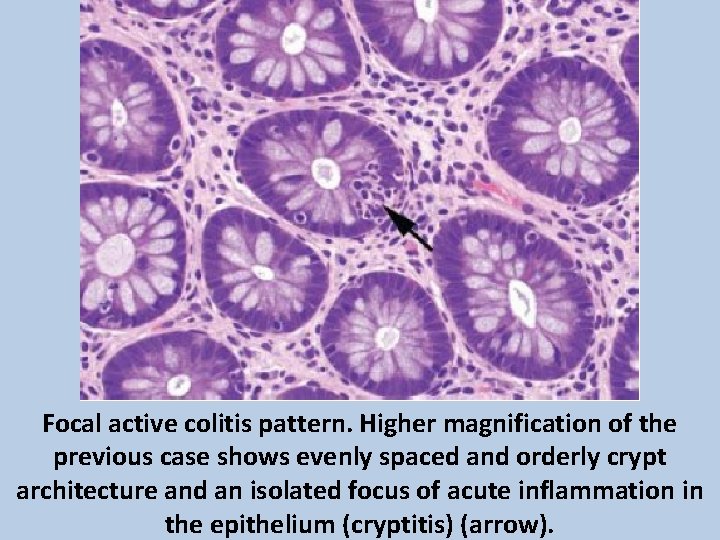
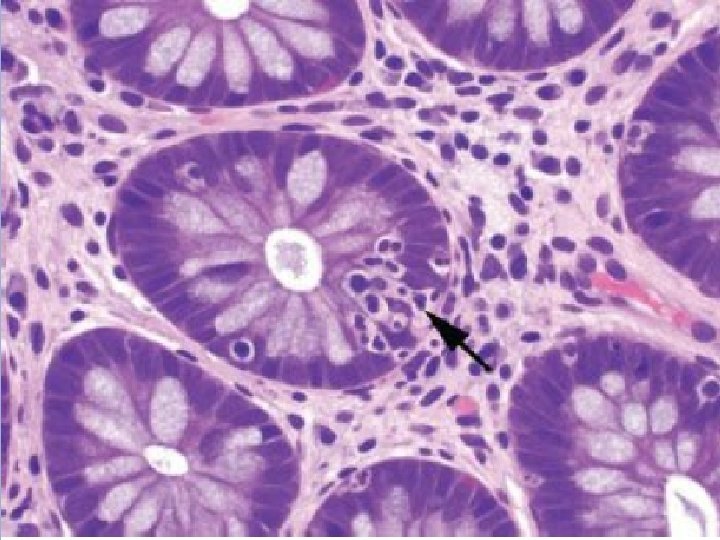
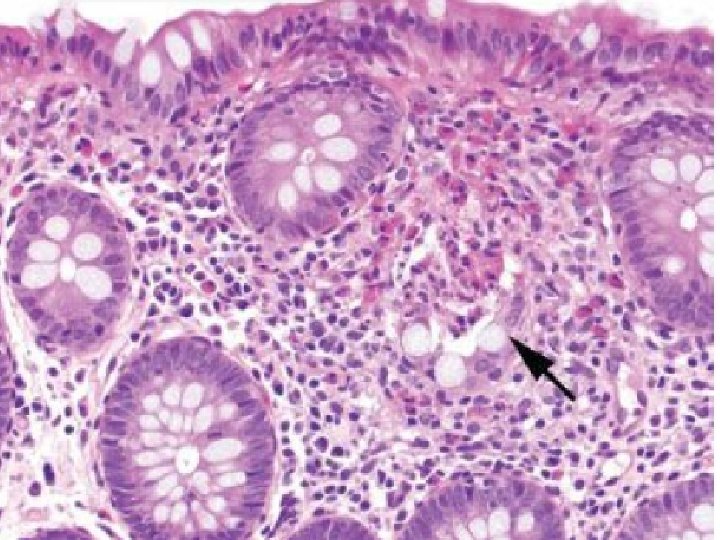
Focal active colitis pattern. Higher magnification of the previous case shows evenly spaced and orderly crypt architecture and an isolated focus of acute inflammation in the epithelium (cryptitis) (arrow).
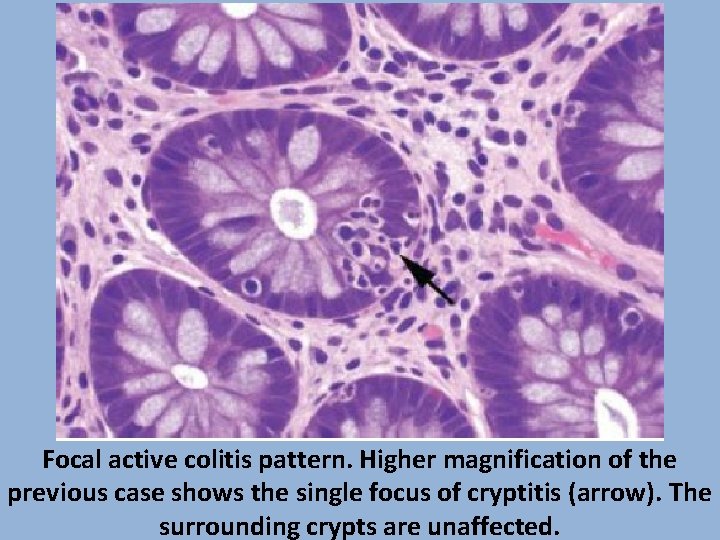
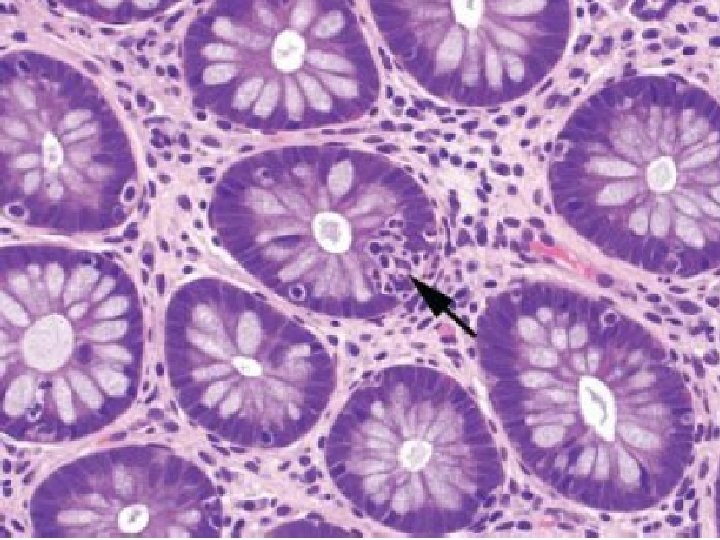
Focal active colitis pattern. Higher magnification of the previous case shows the single focus of cryptitis (arrow). The surrounding crypts are unaffected.
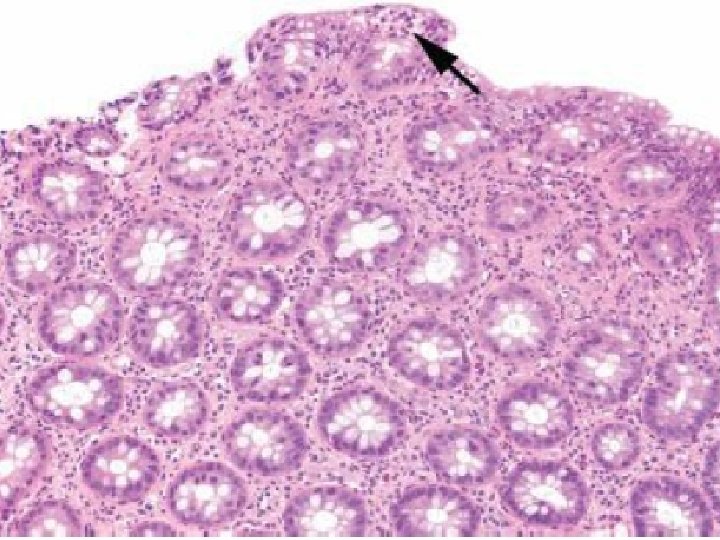
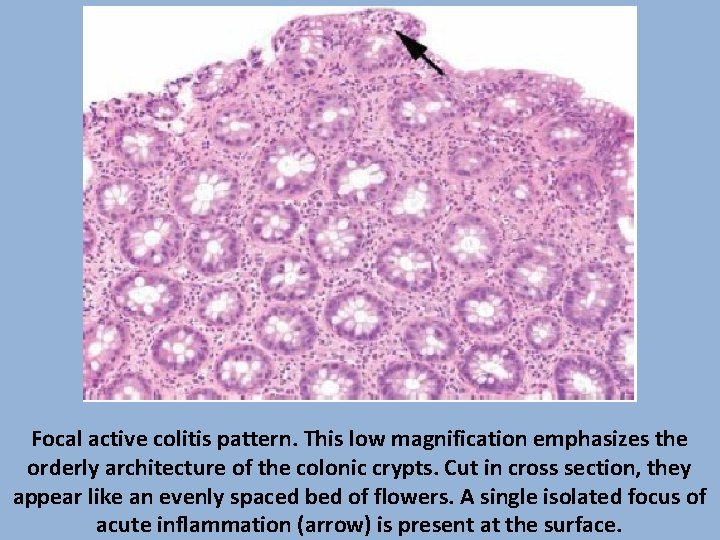
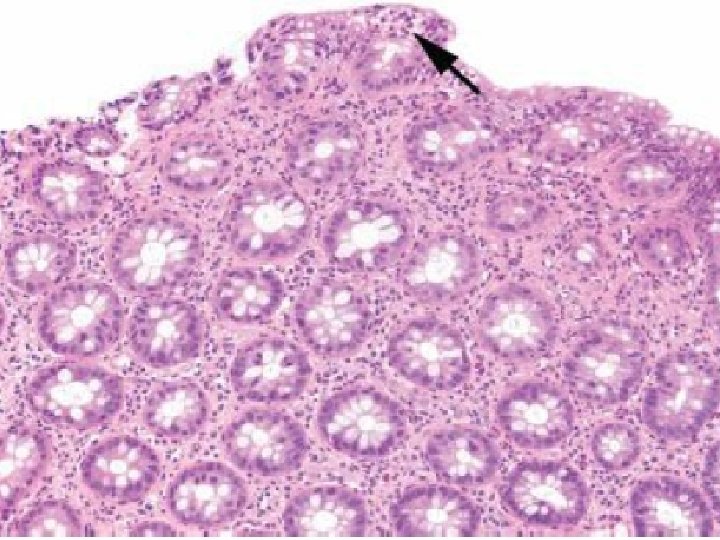
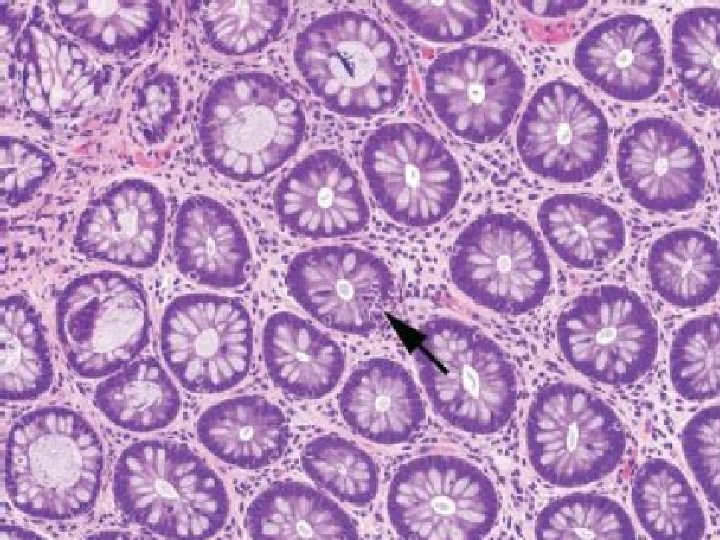
Focal active colitis pattern. This low magnification emphasizes the orderly architecture of the colonic crypts. Cut in cross section, they appear like an evenly spaced bed of flowers. A single isolated focus of acute inflammation (arrow) is present at the surface.
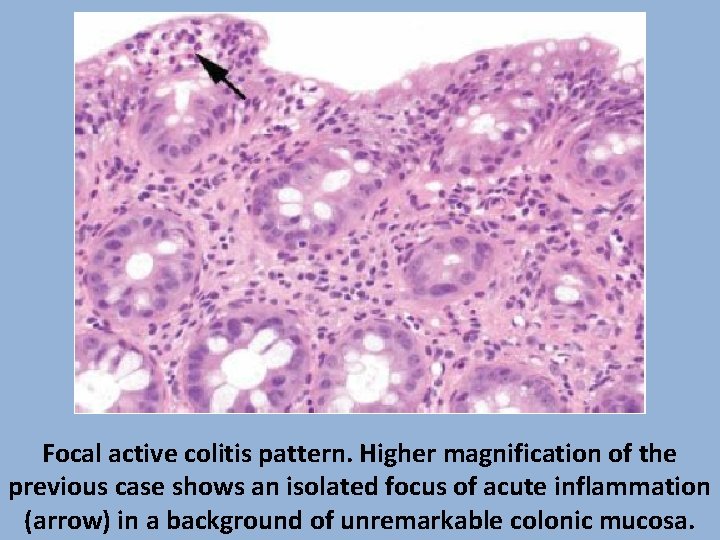
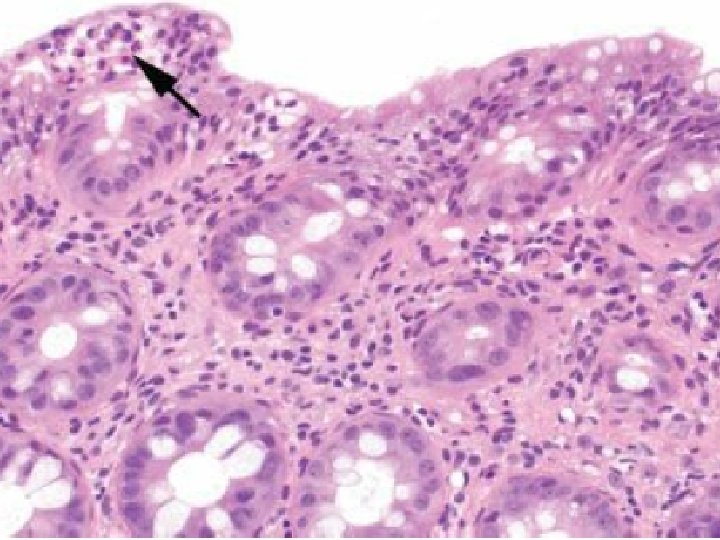
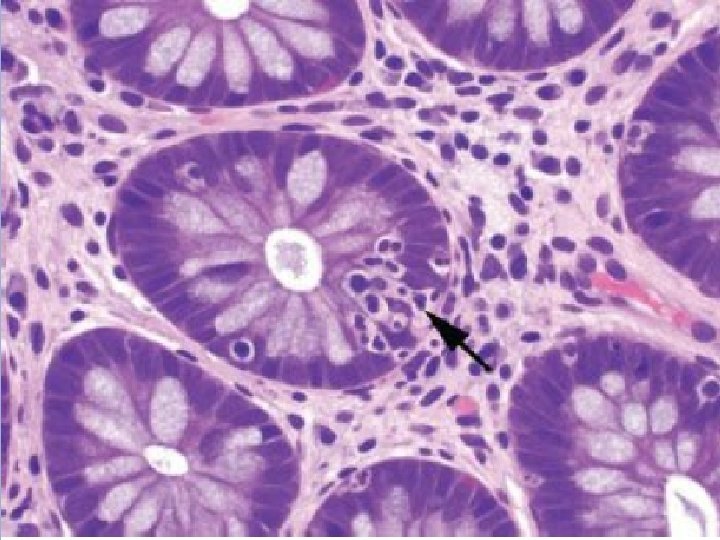
Focal active colitis pattern. Higher magnification of the previous case shows an isolated focus of acute inflammation (arrow) in a background of unremarkable colonic mucosa.
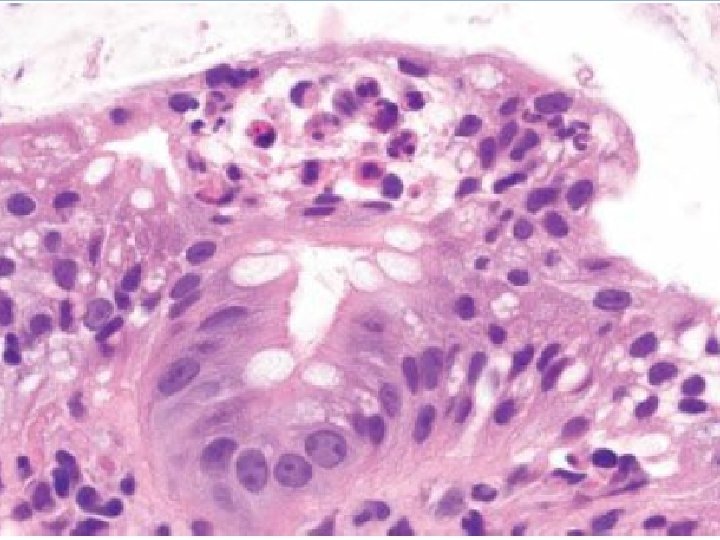
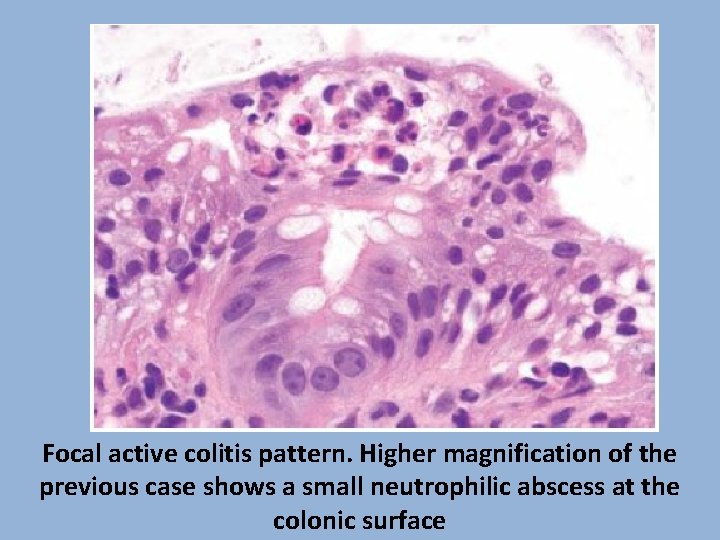
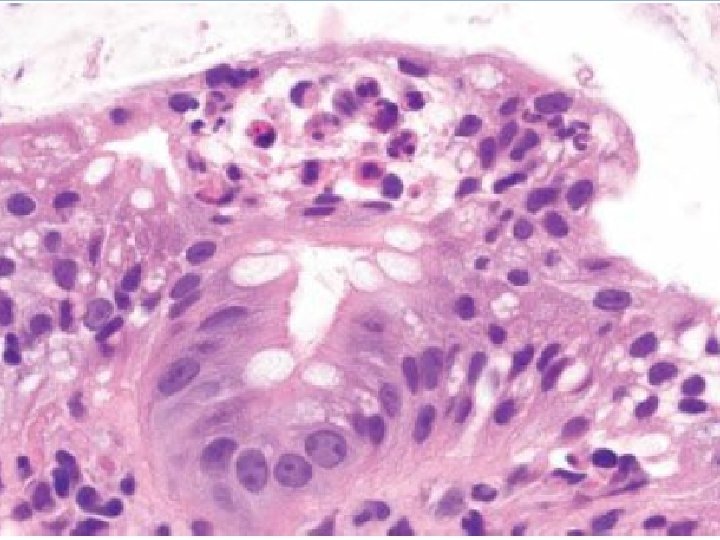
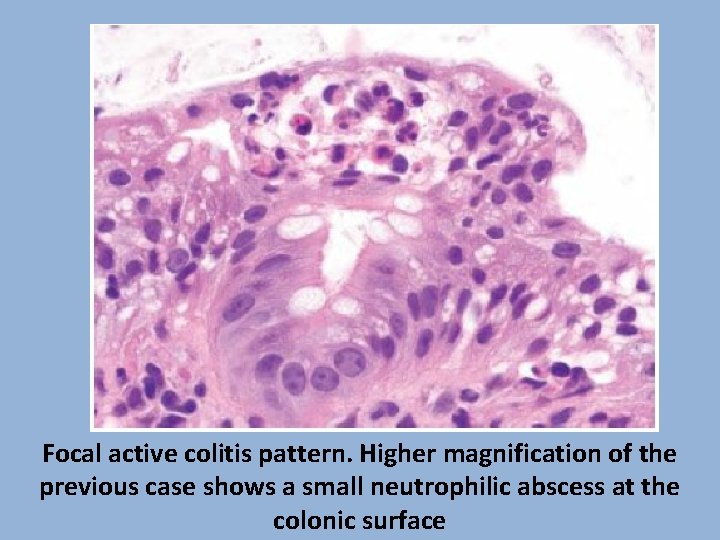
Focal active colitis pattern. Higher magnification of the previous case shows a small neutrophilic abscess at the colonic surface
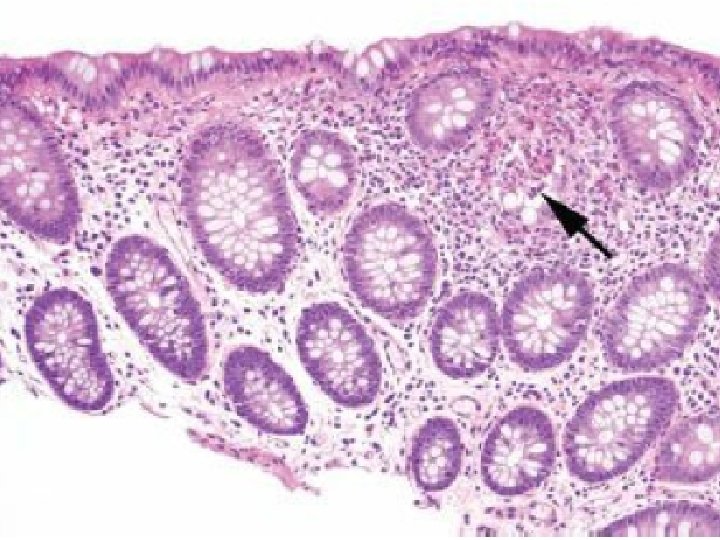
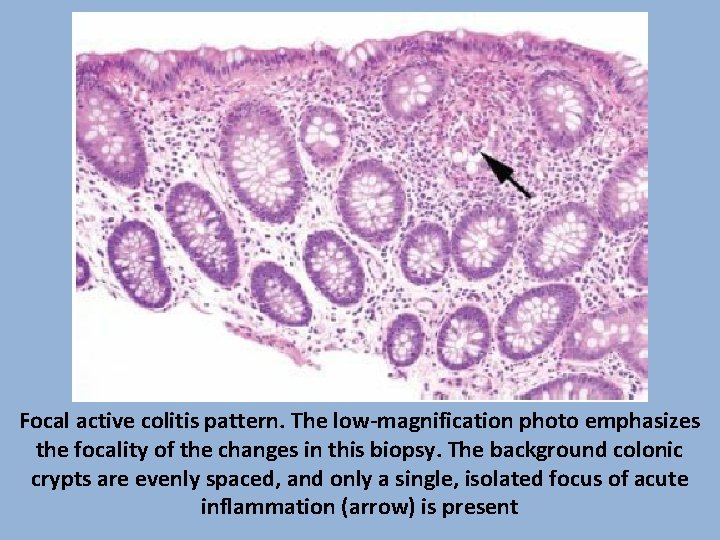
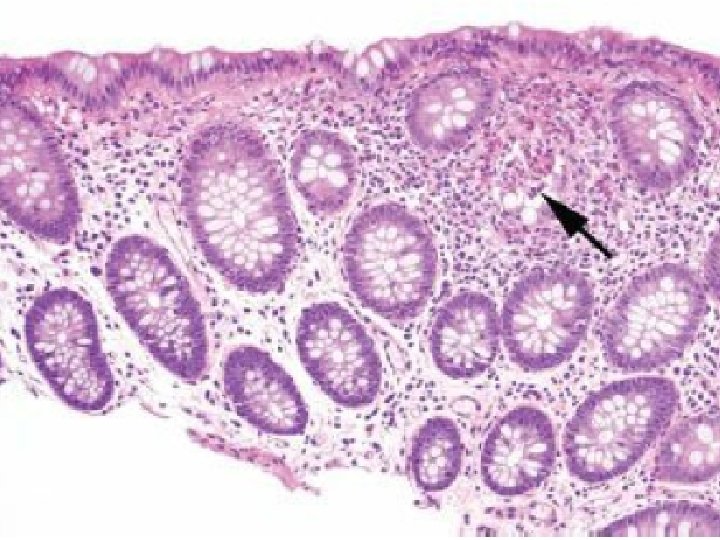
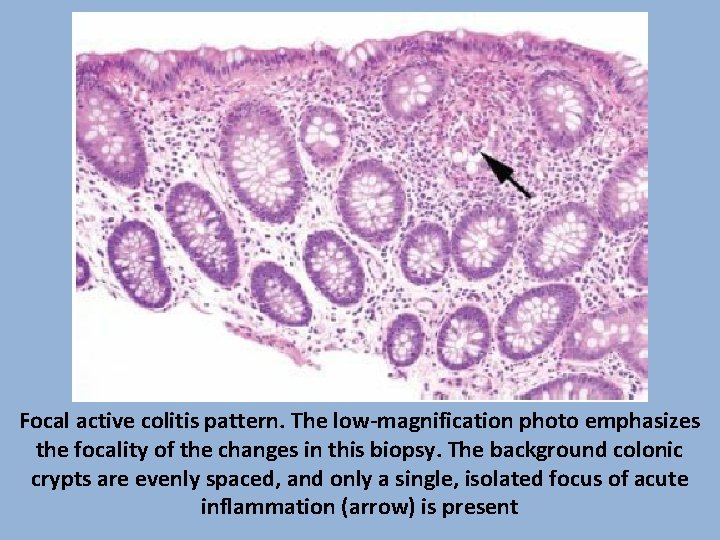
Focal active colitis pattern. The low-magnification photo emphasizes the focality of the changes in this biopsy. The background colonic crypts are evenly spaced, and only a single, isolated focus of acute inflammation (arrow) is present
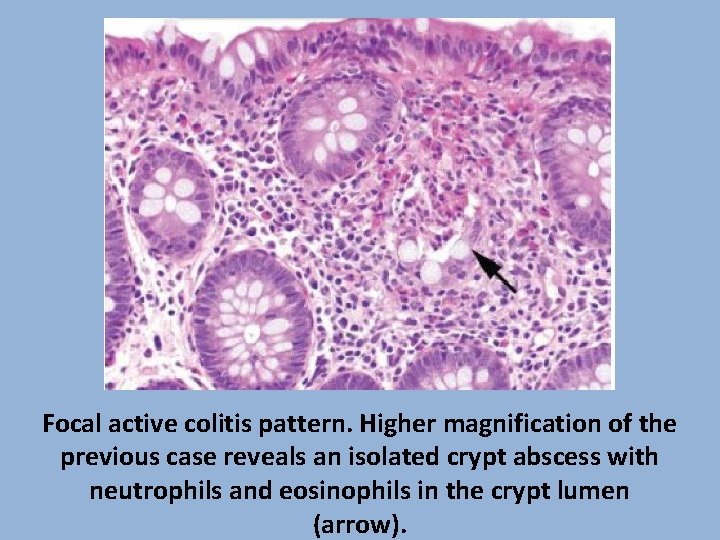
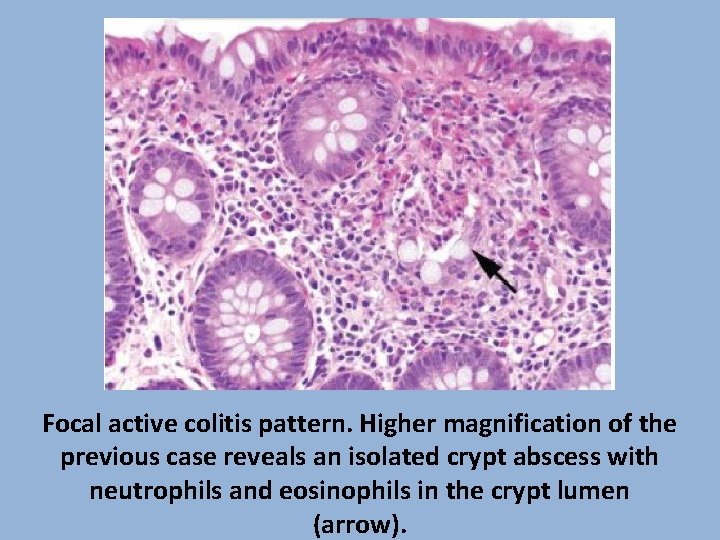
Focal active colitis pattern. Higher magnification of the previous case reveals an isolated crypt abscess with neutrophils and eosinophils in the crypt lumen (arrow).
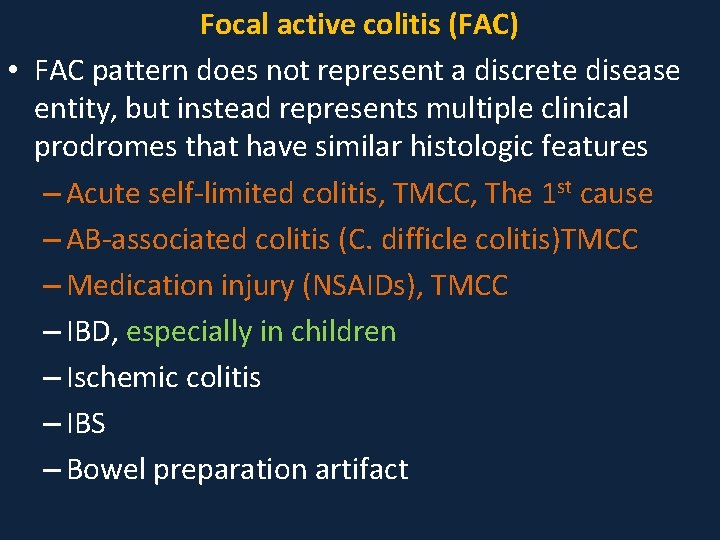
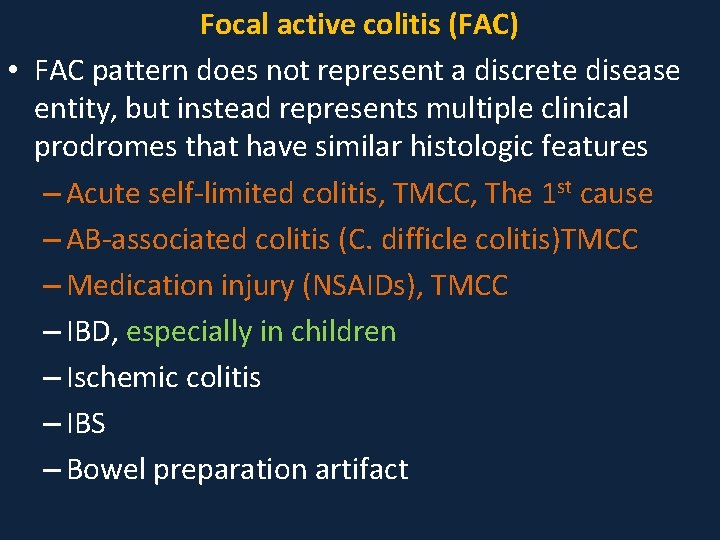
Focal active colitis (FAC) • FAC pattern does not represent a discrete disease entity, but instead represents multiple clinical prodromes that have similar histologic features – Acute self-limited colitis, TMCC, The 1 st cause – AB-associated colitis (C. difficle colitis)TMCC – Medication injury (NSAIDs), TMCC – IBD, especially in children – Ischemic colitis – IBS – Bowel preparation artifact
Focal active colitis (FAC) • Among these patients, clinically significant diarrhea is the most common indication for colonoscopy • FAC is also an incidental finding in asymptomatic patients undergoing routine cancer surveillance colonoscopy • Determining the significance of FAC requires correlation with clinical and microbiologic information
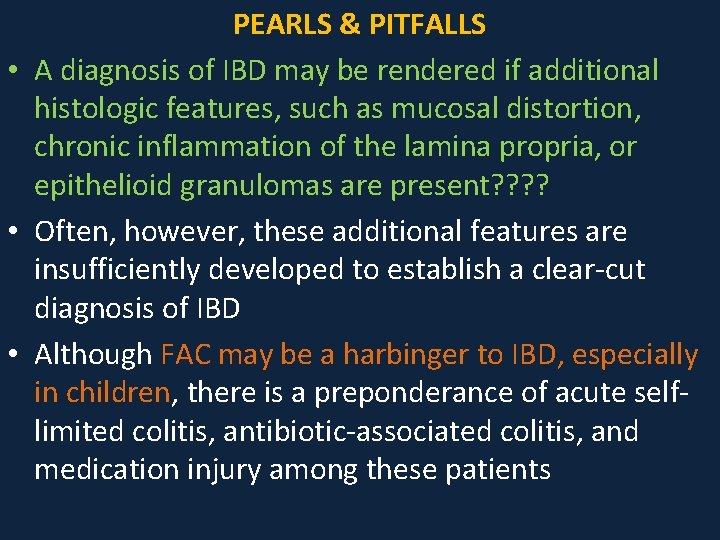
PEARLS & PITFALLS • A diagnosis of IBD may be rendered if additional histologic features, such as mucosal distortion, chronic inflammation of the lamina propria, or epithelioid granulomas are present? ? • Often, however, these additional features are insufficiently developed to establish a clear-cut diagnosis of IBD • Although FAC may be a harbinger to IBD, especially in children, there is a preponderance of acute selflimited colitis, antibiotic-associated colitis, and medication injury among these patients
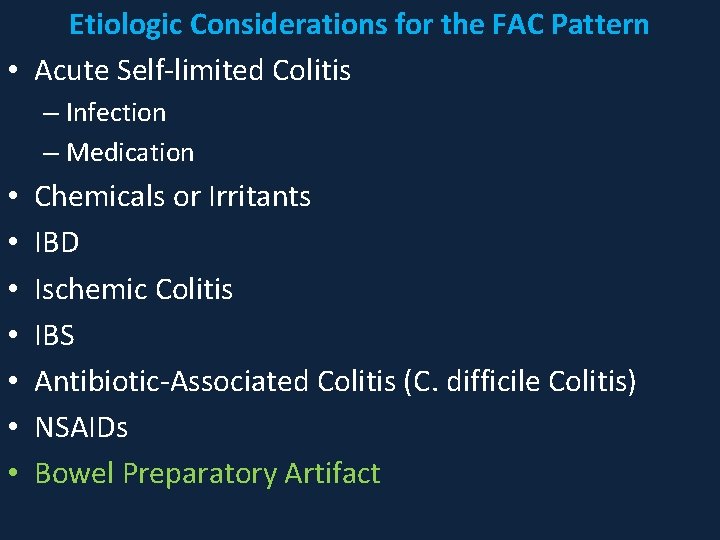
Etiologic Considerations for the FAC Pattern • Acute Self-limited Colitis – Infection – Medication • • Chemicals or Irritants IBD Ischemic Colitis IBS Antibiotic-Associated Colitis (C. difficile Colitis) NSAIDs Bowel Preparatory Artifact
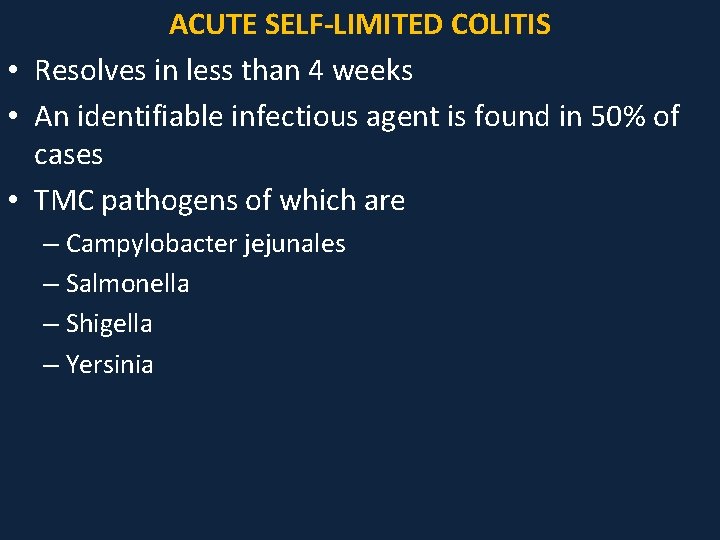
ACUTE SELF-LIMITED COLITIS • Resolves in less than 4 weeks • An identifiable infectious agent is found in 50% of cases • TMC pathogens of which are – Campylobacter jejunales – Salmonella – Shigella – Yersinia
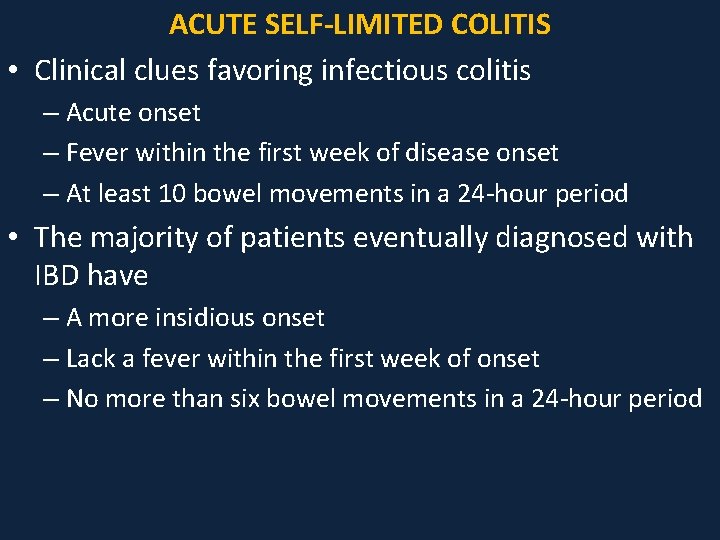
ACUTE SELF-LIMITED COLITIS • Clinical clues favoring infectious colitis – Acute onset – Fever within the first week of disease onset – At least 10 bowel movements in a 24 -hour period • The majority of patients eventually diagnosed with IBD have – A more insidious onset – Lack a fever within the first week of onset – No more than six bowel movements in a 24 -hour period
ACUTE SELF-LIMITED COLITIS • The remaining cases of acute self-limited colitis for which stool cultures are negative are the result of viral infection, parasitic infection, medication reaction, or other chemical irritants • Histologically, biopsies show a predominantly acute inflammation restricted to the mucosa in either a patchy or diffuse fashion • Erosions, ulcerations, and neutrophilic involvement of crypt epithelium (cryptitis) and crypt lumens (crypt abscesses) may be seen, but features of chronicity (e. g. , crypt distortion, crypt dropout, crypt shortfall, increased lamina propria chronic inflammation) are absent
• • • KEY FEATURES of the Focal Active Colitis Pattern FAC refers to individual foci of neutrophilic inflammation in the absence of chronicity The most common etiology is acute self-limited colitis Acute self-limited colitis is defined as a diarrheal illness less than 4 weeks in duration, and is most commonly attributed to infection even though half of these patients have negative stool cultures Other associations with FAC include IBD, ischemic colitis, IBS, AB-associated colitis, NSAIDs FAC in asymptomatic patients undergoing surveillance endoscopy is likely of no clinical significance and may be related to bowel preparation artifact
• Focal active colitis refers to a pattern of injury commonly seen in colorectal biopsy specimens characterized by focal crypt and surface epithelial injury mediated by neutrophils associated with a focal increase of inflammatory cells in the lamina propria • It represents a pattern of injury rather than a specific diagnosis; most cases correlate clinically with infectious-type colitis, but other causes include bowel preparation, medication-induced injury, ischemia, and even Crohn disease, especially when this pattern is seen in children
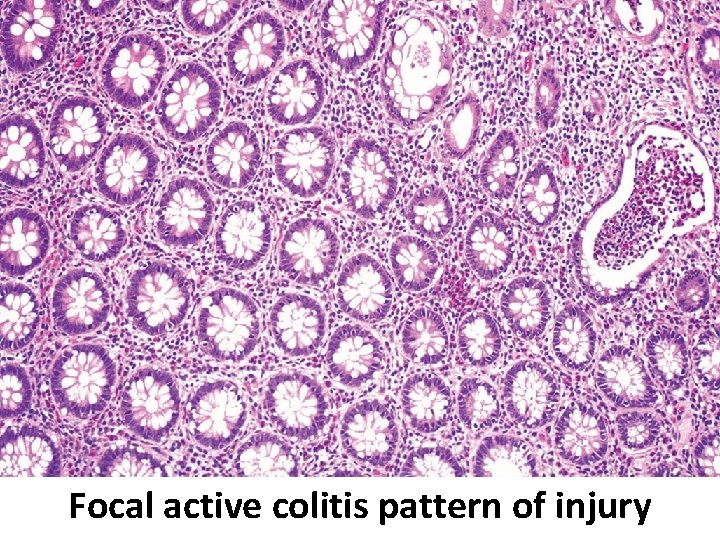
Focal active colitis pattern of injury









