Inflammatory Bowel Disease Samantha Fish MD Andrew Grossman
Inflammatory Bowel Disease Samantha Fish, MD Andrew Grossman, MD Children’s Hospital of Philadelphia 2013 Resident Education Series Reviewed by Edward Hoffenberg, MD of the Professional Education Committee
Case Presentation • 13 yo female presents with 2 mo history of abdominal pain, diarrhea with intermittent blood and 10 lb weight loss • Examination reveals soft abdomen with fullness appreciated in the RLQ, pain on palpation of RLQ, otherwise normal exam • Laboratory evaluation reveals WBC 7, Hgb 11, Plt 517, Alb 3. 1, ESR 50, CRP 3. 2. Remainder of CBC and CMP normal
Background: Inflammatory Bowel Disease • Chronic inflammatory disease of the intestinal tract • Usually characterized by progressive damage to the gastrointestinal tract • Pediatrics: risk for complications in growth, malnutrition, bone disease, psychosocial issues • Pathogenesis poorly defined • IBD is being identified more frequently in the US
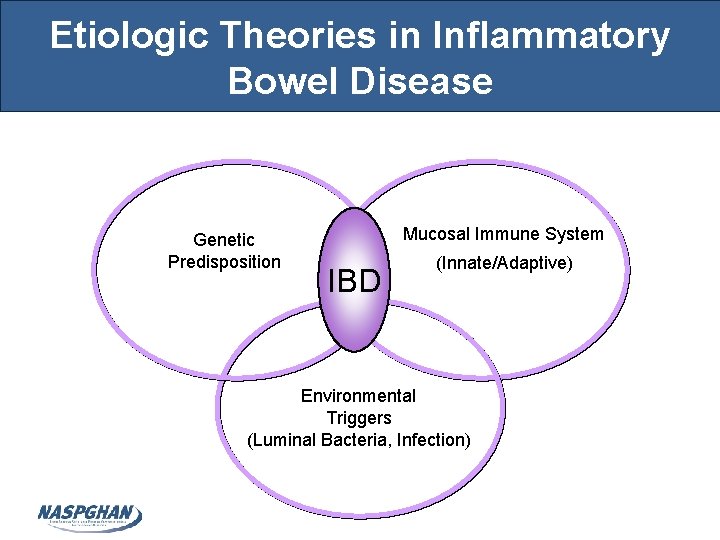
Etiologic Theories in Inflammatory Bowel Disease Genetic Predisposition Mucosal Immune System IBD (Innate/Adaptive) Environmental Triggers (Luminal Bacteria, Infection)
IBD in Pediatric Patients • Similarities with adults – Disease and therapy are generally the same – Differential diagnosis is commonly similar for patients over the age of 5 years • Differences with adults – Lack of specific pediatric data – Lack of child-appropriate formulations – Unique growth and development problems
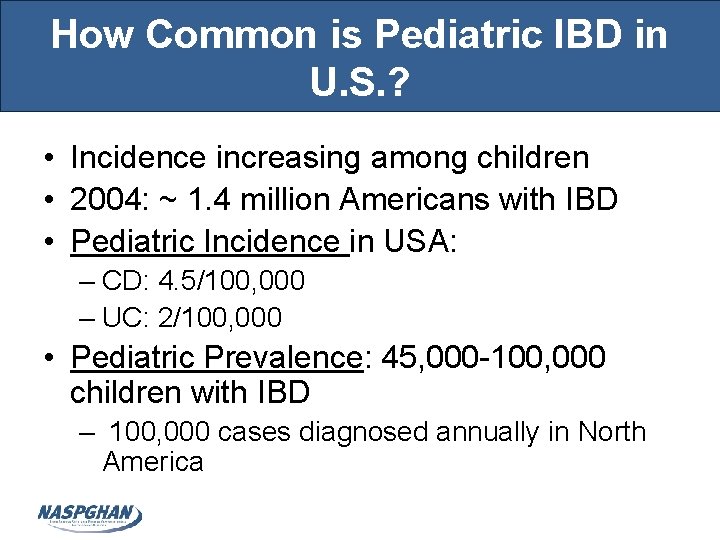
How Common is Pediatric IBD in U. S. ? • Incidence increasing among children • 2004: ~ 1. 4 million Americans with IBD • Pediatric Incidence in USA: – CD: 4. 5/100, 000 – UC: 2/100, 000 • Pediatric Prevalence: 45, 000 -100, 000 children with IBD – 100, 000 cases diagnosed annually in North America
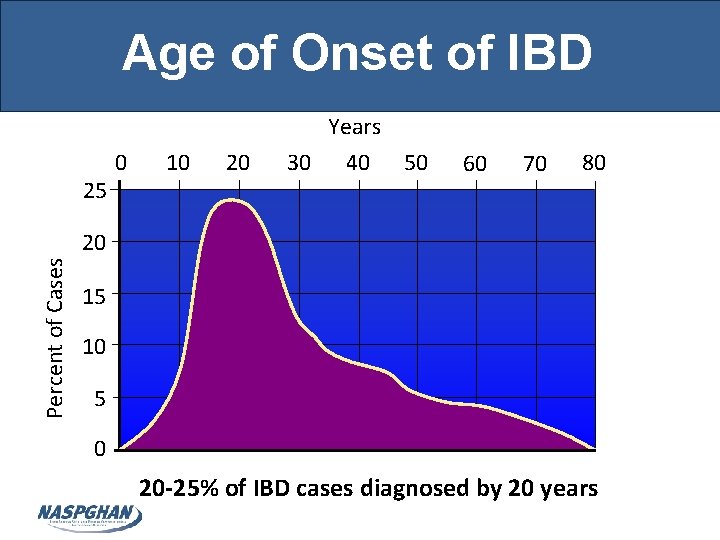
Age of Onset of IBD Years 25 0 10 20 30 40 50 60 70 80 Percent of Cases 20 15 10 5 0 20 -25% of IBD cases diagnosed by 20 years Loftus, Gastroenterology 2003, abstract
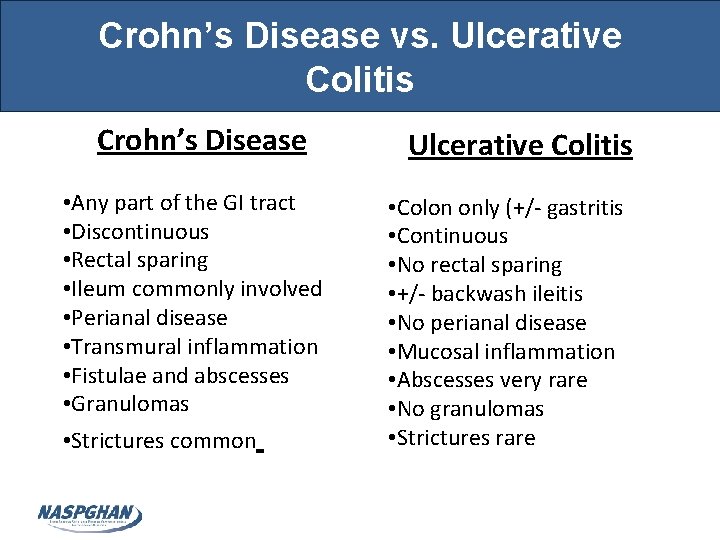
Crohn’s Disease vs. Ulcerative Colitis Crohn’s Disease • Any part of the GI tract • Discontinuous • Rectal sparing • Ileum commonly involved • Perianal disease • Transmural inflammation • Fistulae and abscesses • Granulomas • Strictures common Ulcerative Colitis • Colon only (+/- gastritis • Continuous • No rectal sparing • +/- backwash ileitis • No perianal disease • Mucosal inflammation • Abscesses very rare • No granulomas • Strictures rare
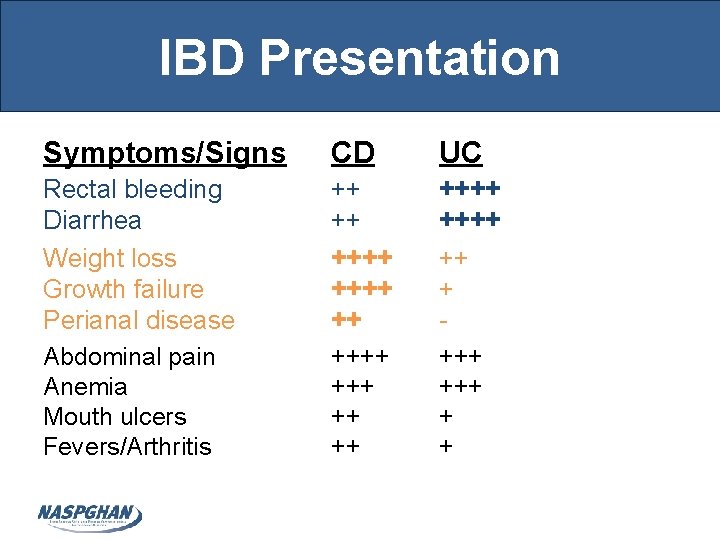
IBD Presentation Symptoms/Signs CD UC Rectal bleeding Diarrhea Weight loss Growth failure Perianal disease Abdominal pain Anemia Mouth ulcers Fevers/Arthritis ++ ++ ++++ +++ ++++ +++ + +
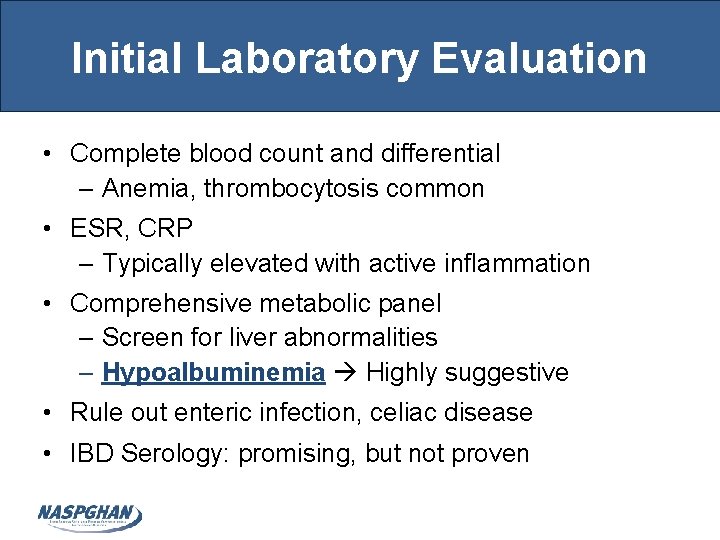
Initial Laboratory Evaluation • Complete blood count and differential – Anemia, thrombocytosis common • ESR, CRP – Typically elevated with active inflammation • Comprehensive metabolic panel – Screen for liver abnormalities – Hypoalbuminemia Highly suggestive • Rule out enteric infection, celiac disease • IBD Serology: promising, but not proven
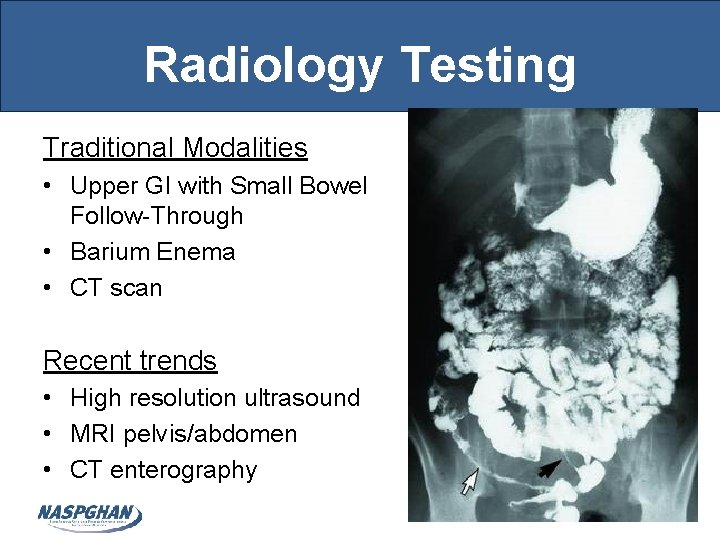
Radiology Testing Traditional Modalities • Upper GI with Small Bowel Follow-Through • Barium Enema • CT scan Recent trends • High resolution ultrasound • MRI pelvis/abdomen • CT enterography
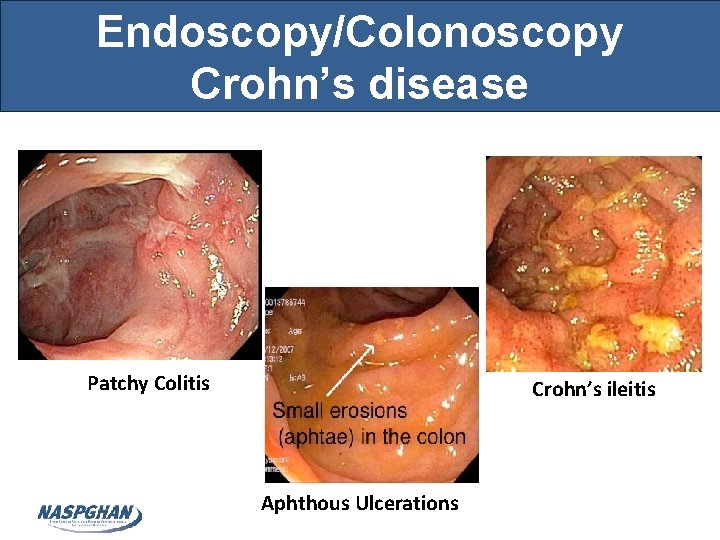
Endoscopy/Colonoscopy Crohn’s disease Patchy Colitis Crohn’s ileitis Aphthous Ulcerations
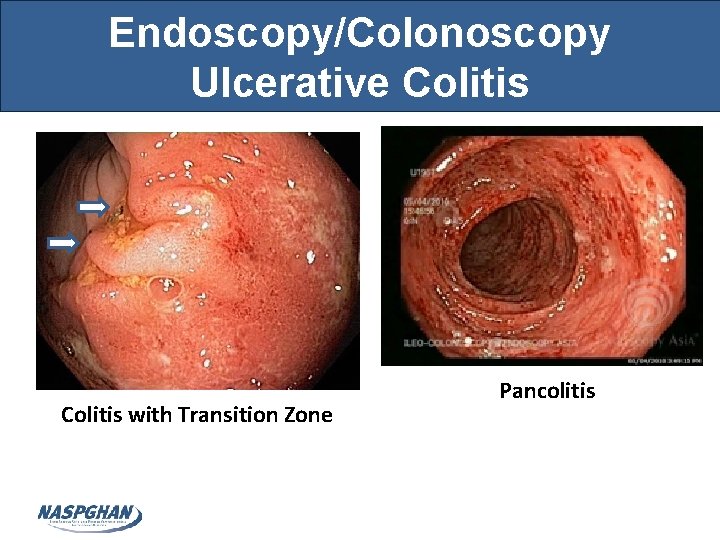
Endoscopy/Colonoscopy Ulcerative Colitis with Transition Zone Pancolitis
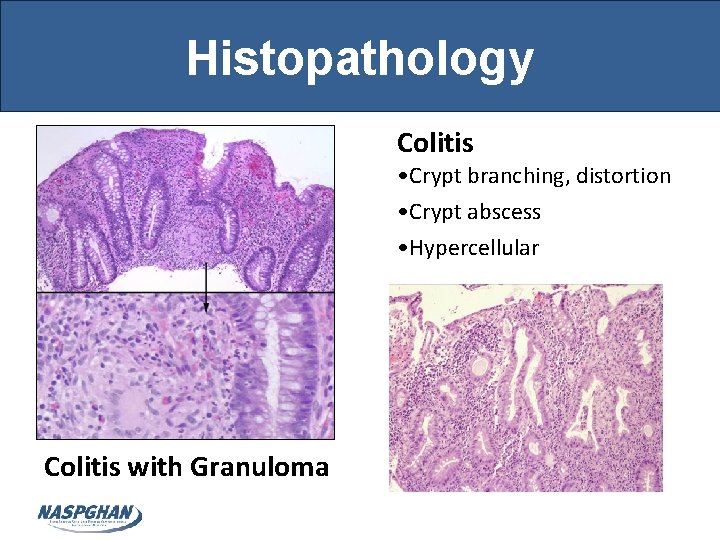
Histopathology Colitis • Crypt branching, distortion • Crypt abscess • Hypercellular Colitis with Granuloma
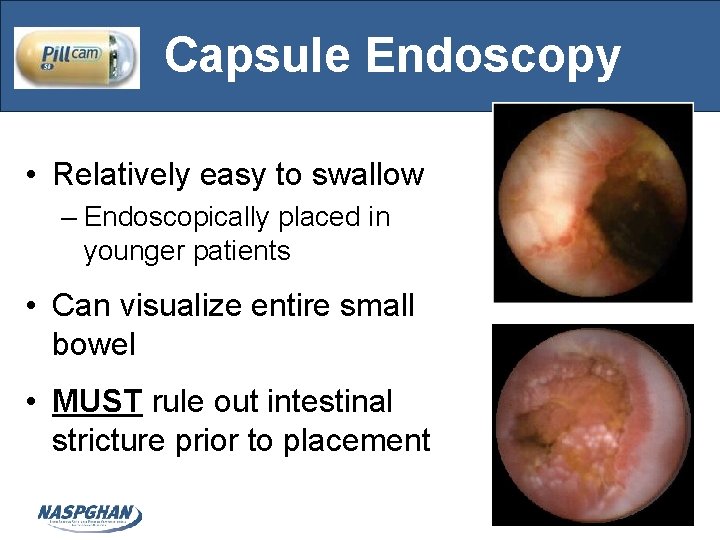
Capsule Endoscopy • Relatively easy to swallow – Endoscopically placed in younger patients • Can visualize entire small bowel • MUST rule out intestinal stricture prior to placement

Treatment of Pediatric IBD Goals • Improve growth and nutrition • Improve quality of life • Maximize therapeutic response • Minimize toxicity • Prevent disease complications • Maximize adherence • Promote psychological health
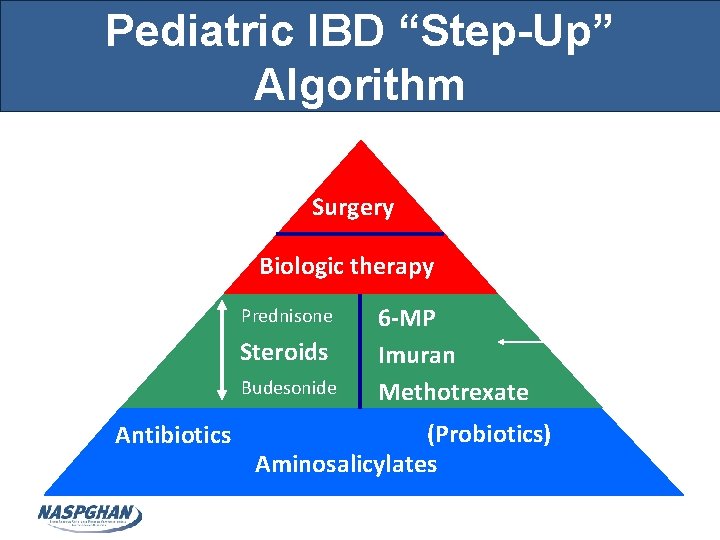
Pediatric IBD “Step-Up” Algorithm Severe Surgery Biologic therapy Moderate Prednisone Steroids Budesonide Mild Antibiotics 6 -MP Imuran Methotrexate (Probiotics) Aminosalicylates Enteral Nutrition
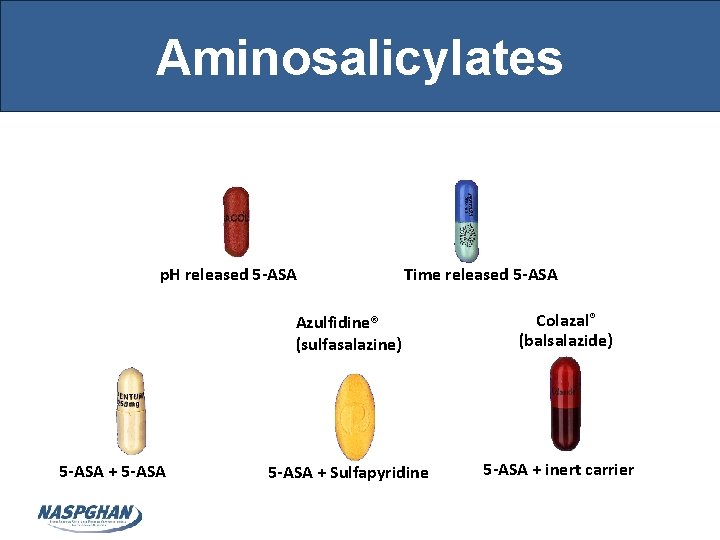
Aminosalicylates Pentasa® (mesalamine) Asacol® (mesalamine) p. H released 5 -ASA Time released 5 -ASA Dipentum® (olsalazine) Azulfidine® (sulfasalazine) 5 -ASA + Sulfapyridine Colazal® (balsalazide) 5 -ASA + inert carrier
Aminosalicylates (5 -ASA) • Locally reduce inflammation in the bowel – Inhibition of arachidonic metabolism • Oral and rectal preparations available • Often a first-line therapy for UC and Crohn’s • Role in decreasing risk of colon cancer • Well tolerated – Headaches, GI complaints most common – 3 -5% with allergy to medicine • Adherence can be an issue with large number of pills to be taken multiple times daily
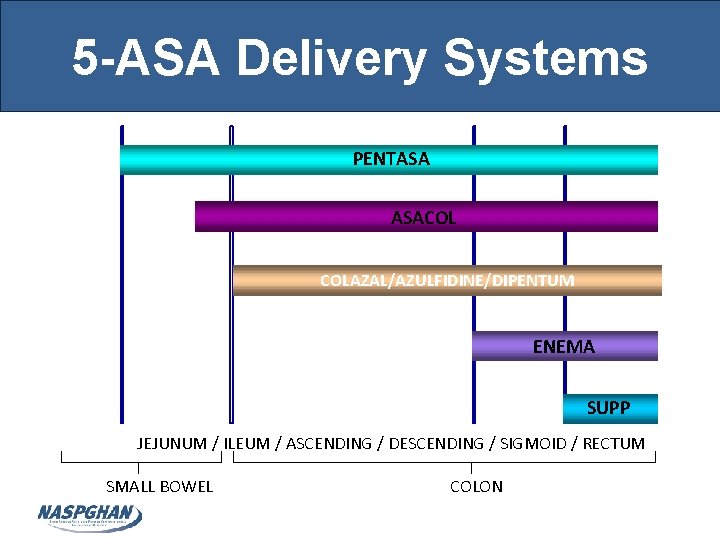
5 -ASA Delivery Systems PENTASA ASACOL COLAZAL/AZULFIDINE/DIPENTUM ENEMA SUPP JEJUNUM / ILEUM / ASCENDING / DESCENDING / SIGMOID / RECTUM SMALL BOWEL COLON
Efficacy of 5 -ASA’s Ulcerative Colitis • Oral and rectal forms • Oral therapy effective for induction and maintenance of remission • Rectal + oral More effective than just oral for distal disease Crohn’s disease • Efficacy unclear for induction or maintenance of remission
Antibiotics • Decrease inflammation by changing or eliminating bacteria in GI tract Flagyl (metronidazole) • Multiple indications for Crohn’s – Perianal disease – Abscess – Prevent post-operative recurrence – Treatment of mild or moderate disease • Not proven effective for UC Cipro (ciprofloxacin)
Systemic Corticosteroids • Oral (prednisone), IV (Solumedrol), or rectal • Suppress active inflammation • Indication: Crohn’s flare • Provide immediate symptomatic relief – Do not promote GI tract mucosal healing • Not indicated for maintenance therapy
Entocort (Budesonide) • Rapid hepatic clearance formulation – Released in the terminal ileum • Considerably less steroid side effects • Effective for ileocolonic Crohn’s disease • Not effective for UC, Crohn’s colitis or gastritis • Role as maintenance therapy unclear – Evidence of some steroid side effects (growth suppression)
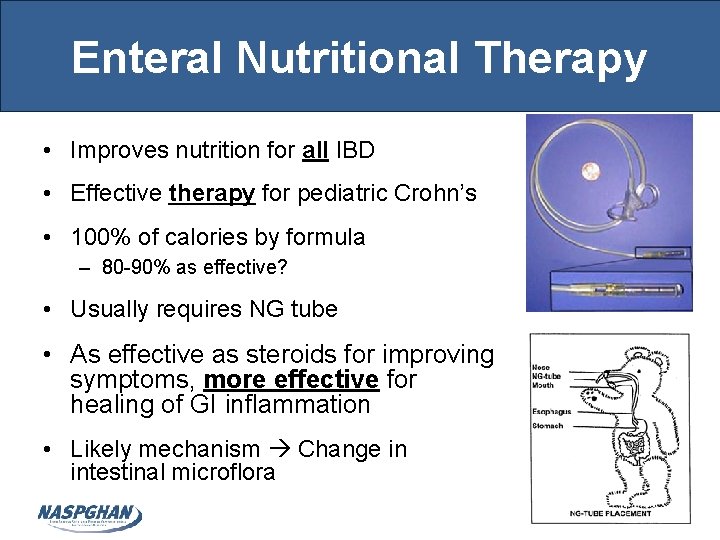
Enteral Nutritional Therapy • Improves nutrition for all IBD • Effective therapy for pediatric Crohn’s • 100% of calories by formula – 80 -90% as effective? • Usually requires NG tube • As effective as steroids for improving symptoms, more effective for healing of GI inflammation • Likely mechanism Change in intestinal microflora
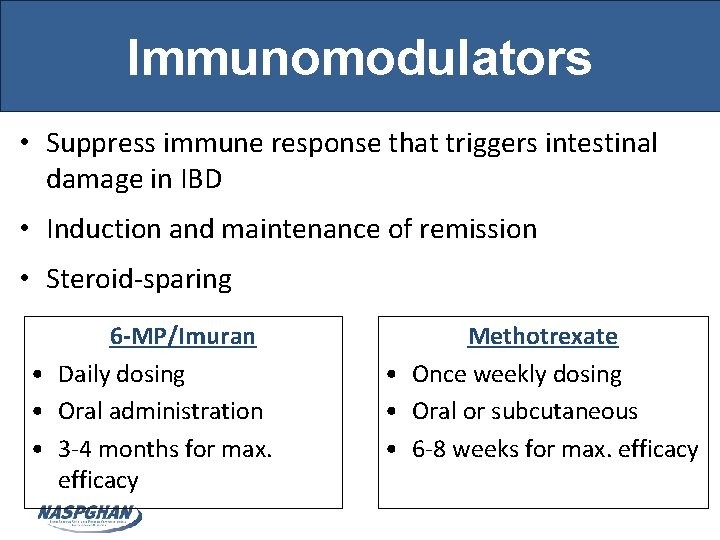
Immunomodulators • Suppress immune response that triggers intestinal damage in IBD • Induction and maintenance of remission • Steroid-sparing 6 -MP/Imuran • Daily dosing • Oral administration • 3 -4 months for max. efficacy Methotrexate • Once weekly dosing • Oral or subcutaneous • 6 -8 weeks for max. efficacy

Biologic Therapies • Pro-inflammatory cytokines contribute to inflammation in IBD Remicade (infliximab) – TNFα is elevated in IBD patients • Biologics block and neutralize cytokines • Used to treat moderate to severe IBD not responding to otherapy 75% Human Humira (adalimumab) – Infusion (Infliximab = Remicade) – Injectable (Adalimumab = Humira) 100% Human
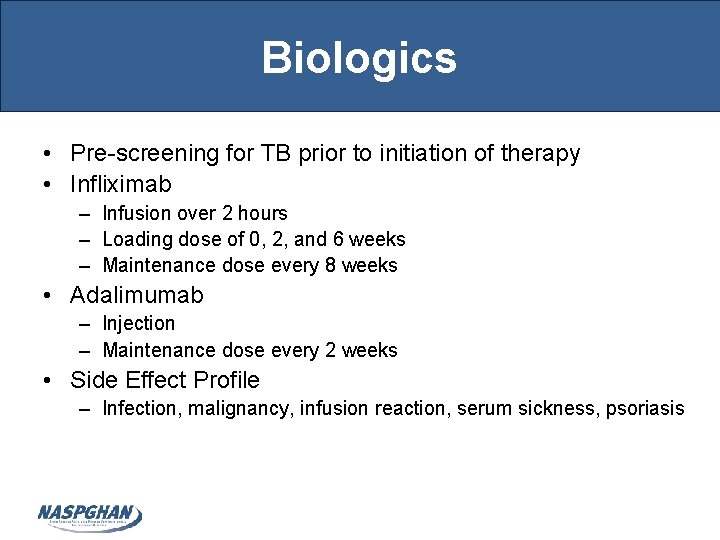
Biologics • Pre-screening for TB prior to initiation of therapy • Infliximab – Infusion over 2 hours – Loading dose of 0, 2, and 6 weeks – Maintenance dose every 8 weeks • Adalimumab – Injection – Maintenance dose every 2 weeks • Side Effect Profile – Infection, malignancy, infusion reaction, serum sickness, psoriasis
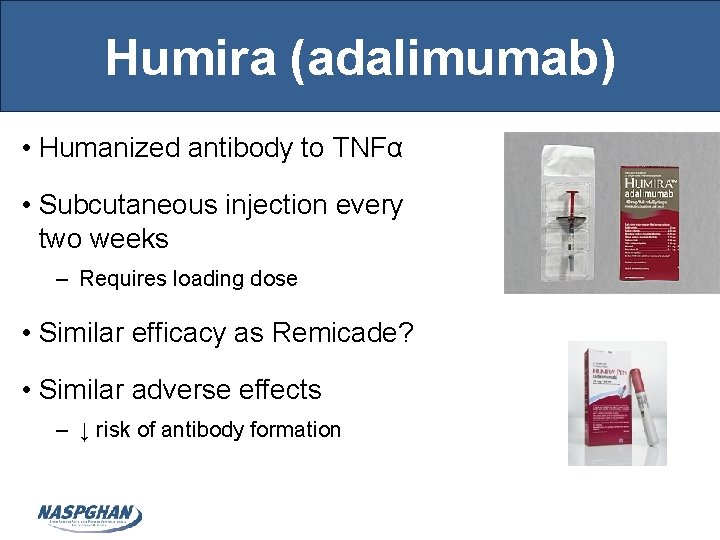
Humira (adalimumab) • Humanized antibody to TNFα • Subcutaneous injection every two weeks – Requires loading dose • Similar efficacy as Remicade? • Similar adverse effects – ↓ risk of antibody formation
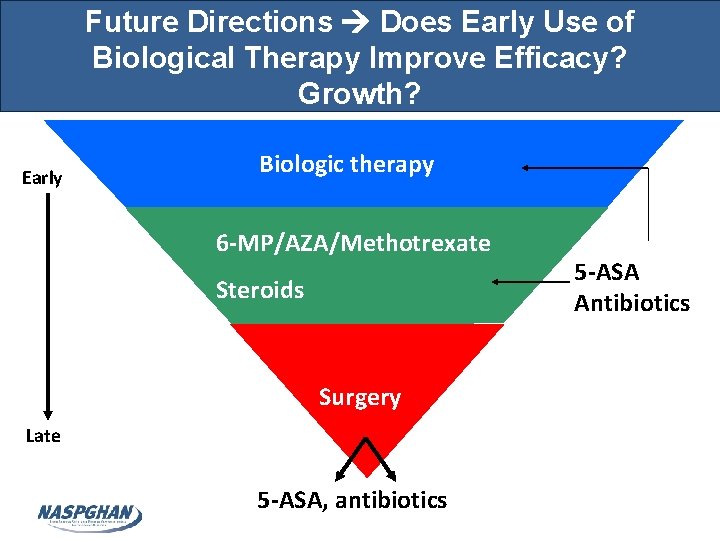
Future Directions Does Early Use of Biological Therapy Improve Efficacy? Growth? Early Biologic therapy 6 -MP/AZA/Methotrexate Steroids Surgery Late 5 -ASA, antibiotics 5 -ASA Antibiotics
Case Conclusion • Colonoscopy showed gross pancolitis confirmed by histology • Patient started on oral and rectal 5 -ASA as well as an immunomodulator with symptom improvement
- Slides: 31