First responder training MMH 15 F Emergency Department















































- Slides: 94
First responder training MMH 15 F Emergency Department Yu-Jang Su, M. D 95/6/22 13: 00— 13: 50 6/22/2006 First Responder Training 1
常見內科疾病處 置二 中毒 糖尿病急症 癲癇 6/22/2006 First Responder Training 2
中毒 Intoxication. 6/22/2006 First Responder Training 3

毒物途徑: • • 吸入, inhalation. 小於 5微米可以入肺泡 皮膚黏膜吸收, absorption. Ingestion, 攝食 (意外或自殺) 注射. (addiction) 6/22/2006 First Responder Training 5



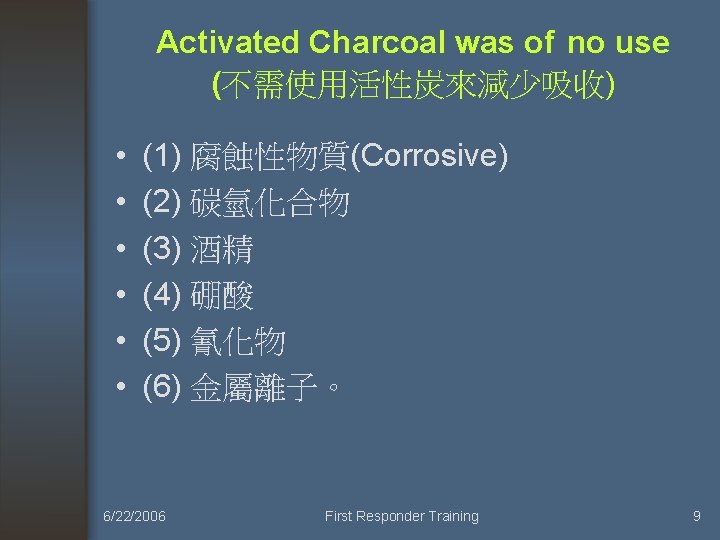
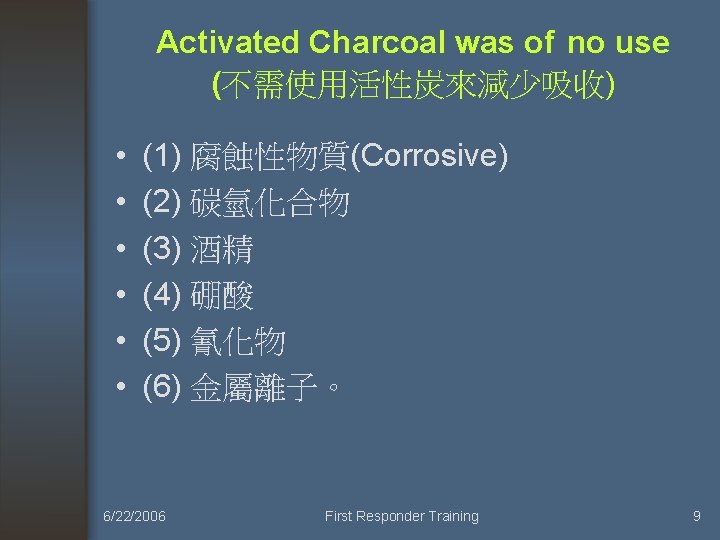
Activated Charcoal was of no use (不需使用活性炭來減少吸收) • • • (1) 腐蝕性物質(Corrosive) (2) 碳氫化合物 (3) 酒精 (4) 硼酸 (5) 氰化物 (6) 金屬離子。 6/22/2006 First Responder Training 9

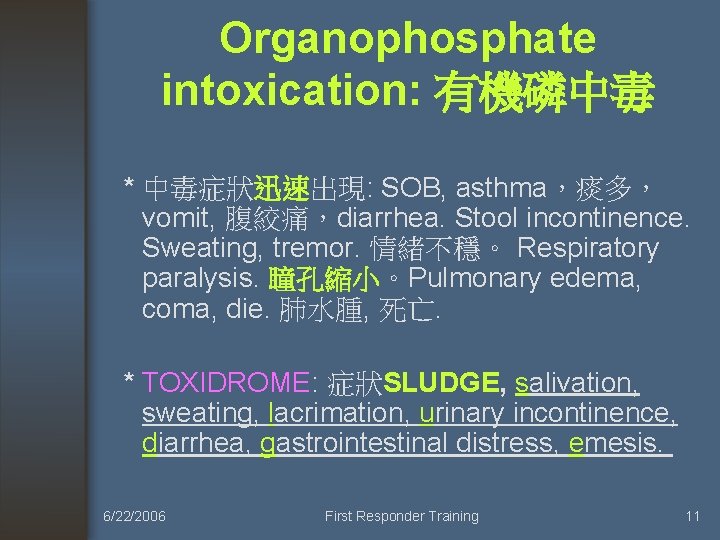
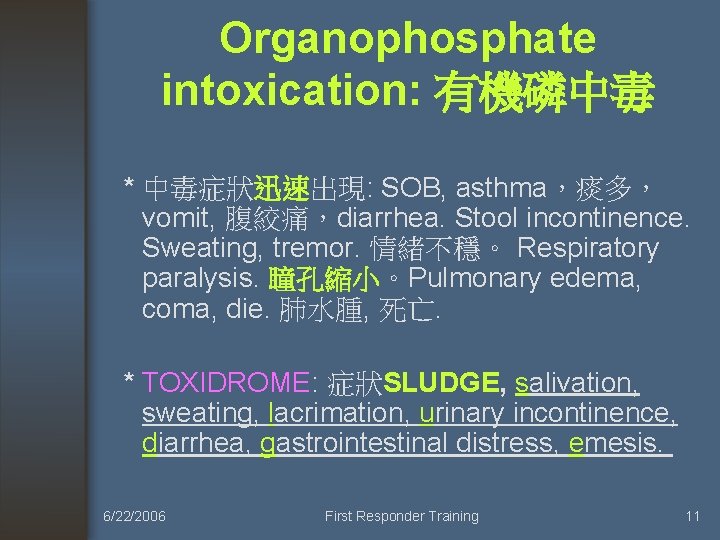
Organophosphate intoxication: 有機磷中毒 * 中毒症狀迅速出現: SOB, asthma,痰多, vomit, 腹絞痛,diarrhea. Stool incontinence. Sweating, tremor. 情緒不穩。 Respiratory paralysis. 瞳孔縮小。Pulmonary edema, coma, die. 肺水腫, 死亡. * TOXIDROME: 症狀SLUDGE, salivation, sweating, lacrimation, urinary incontinence, diarrhea, gastrointestinal distress, emesis. 6/22/2006 First Responder Training 11

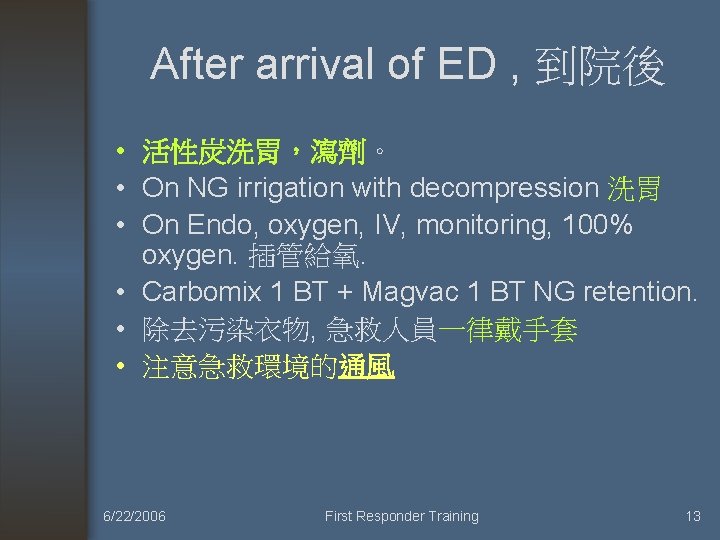
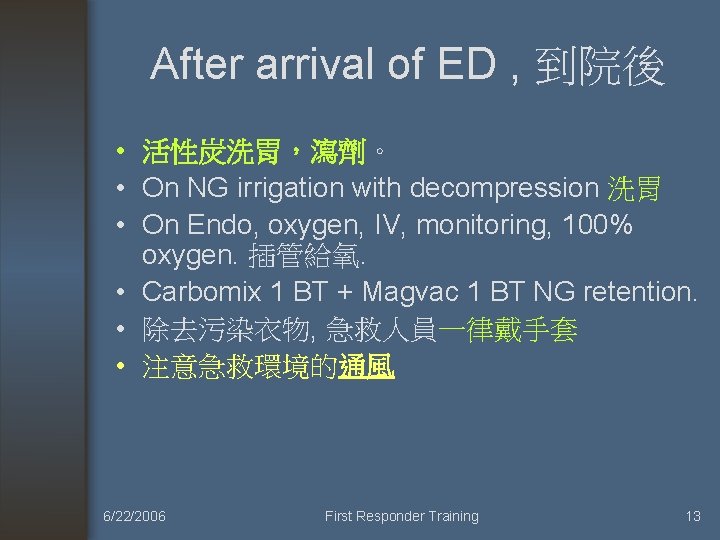
After arrival of ED , 到院後 • 活性炭洗胃,瀉劑。 • On NG irrigation with decompression 洗胃 • On Endo, oxygen, IV, monitoring, 100% oxygen. 插管給氧. • Carbomix 1 BT + Magvac 1 BT NG retention. • 除去污染衣物, 急救人員一律戴手套 • 注意急救環境的通風 6/22/2006 First Responder Training 13
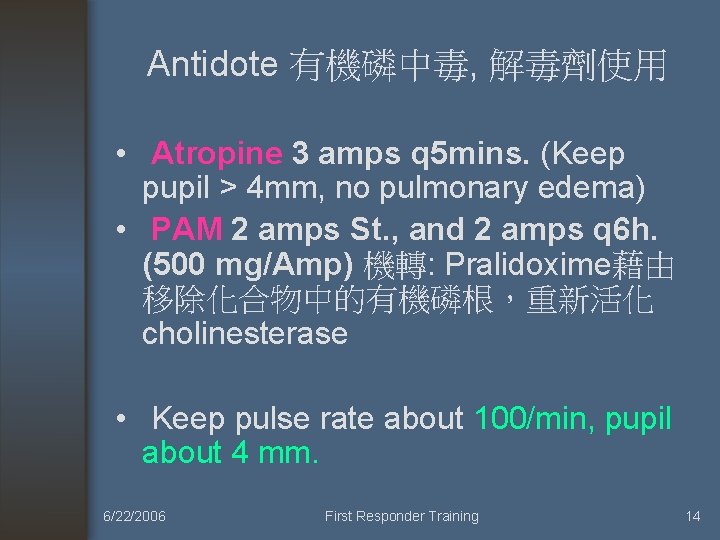
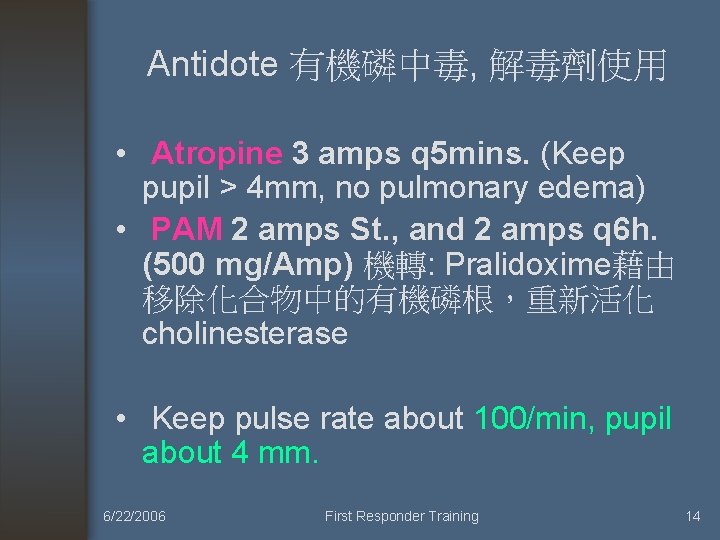
Antidote 有機磷中毒, 解毒劑使用 • Atropine 3 amps q 5 mins. (Keep pupil > 4 mm, no pulmonary edema) • PAM 2 amps St. , and 2 amps q 6 h. (500 mg/Amp) 機轉: Pralidoxime藉由 移除化合物中的有機磷根,重新活化 cholinesterase • Keep pulse rate about 100/min, pupil about 4 mm. 6/22/2006 First Responder Training 14
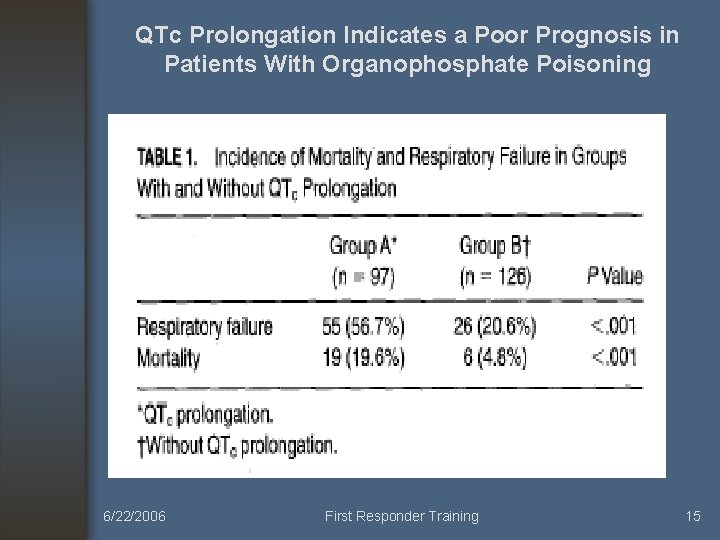
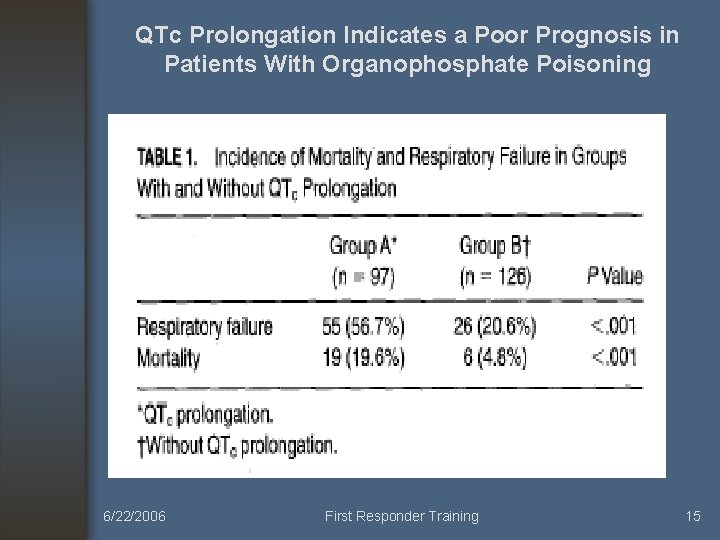
QTc Prolongation Indicates a Poor Prognosis in Patients With Organophosphate Poisoning 6/22/2006 First Responder Training 15

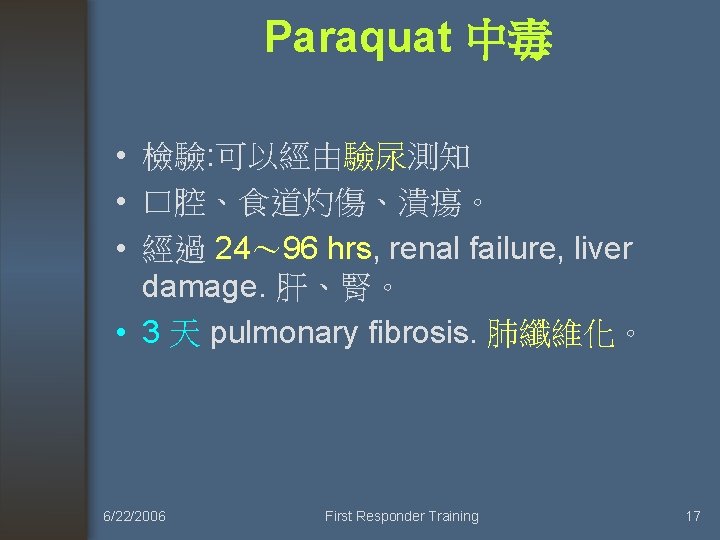
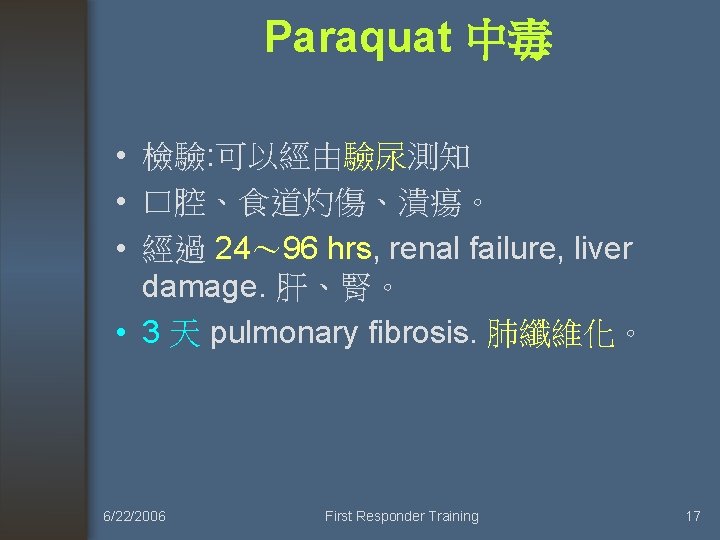
Paraquat 中毒 • 檢驗: 可以經由驗尿測知 • 口腔、食道灼傷、潰瘍。 • 經過 24~ 96 hrs, renal failure, liver damage. 肝、腎。 • 3 天 pulmonary fibrosis. 肺纖維化。 6/22/2006 First Responder Training 17
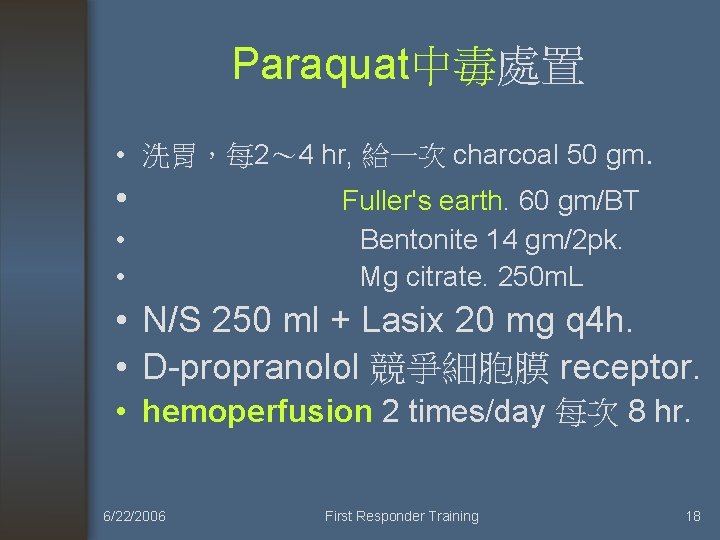
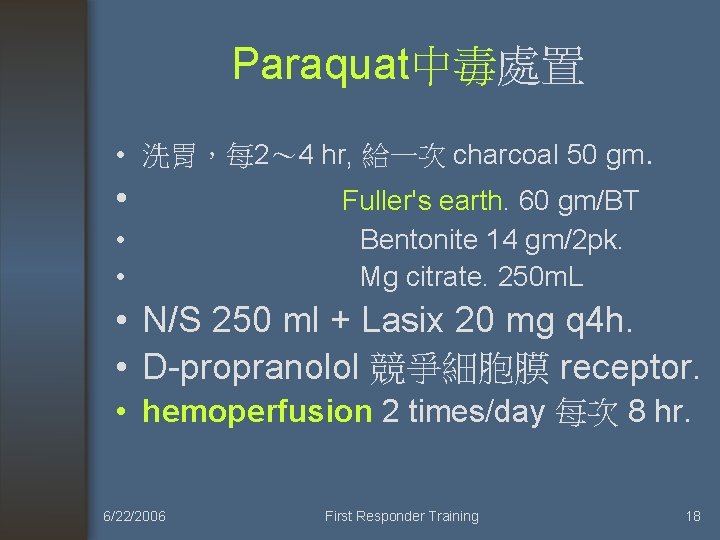
Paraquat中毒處置 • 洗胃,每 2~ 4 hr, 給一次 charcoal 50 gm. • Fuller's earth. 60 gm/BT • Bentonite 14 gm/2 pk. • Mg citrate. 250 m. L • N/S 250 ml + Lasix 20 mg q 4 h. • D-propranolol 競爭細胞膜 receptor. • hemoperfusion 2 times/day 每次 8 hr. 6/22/2006 First Responder Training 18



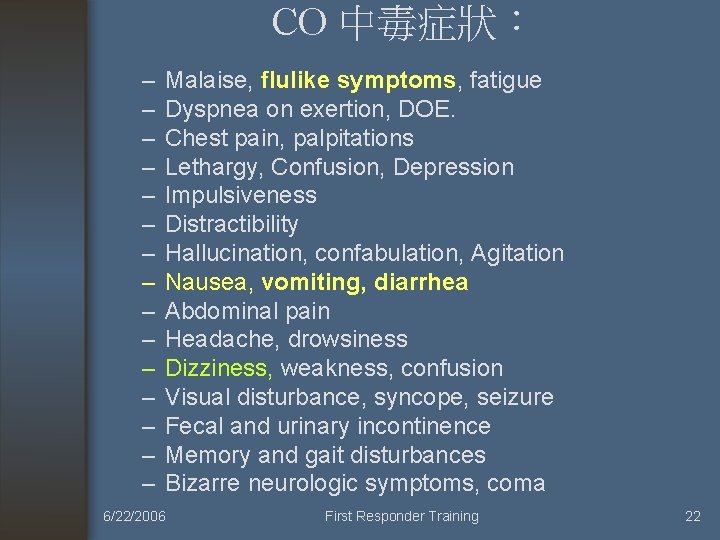
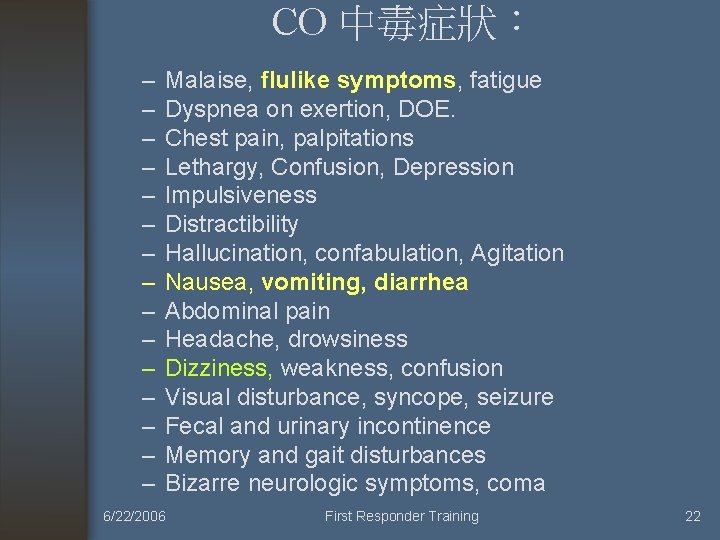
CO 中毒症狀: – – – – Malaise, flulike symptoms, fatigue Dyspnea on exertion, DOE. Chest pain, palpitations Lethargy, Confusion, Depression Impulsiveness Distractibility Hallucination, confabulation, Agitation Nausea, vomiting, diarrhea Abdominal pain Headache, drowsiness Dizziness, weakness, confusion Visual disturbance, syncope, seizure Fecal and urinary incontinence Memory and gait disturbances Bizarre neurologic symptoms, coma 6/22/2006 First Responder Training 22
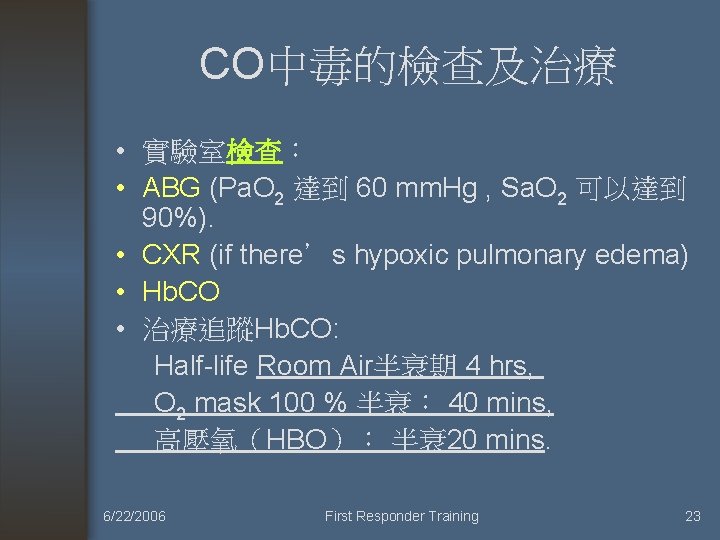
CO中毒的檢查及治療 • 實驗室檢查: • ABG (Pa. O 2 達到 60 mm. Hg , Sa. O 2 可以達到 90%). • CXR (if there’s hypoxic pulmonary edema) • Hb. CO • 治療追蹤Hb. CO: Half-life Room Air半衰期 4 hrs, O 2 mask 100 % 半衰: 40 mins, 高壓氧(HBO): 半衰 20 mins. 6/22/2006 First Responder Training 23








甲醇中毒 6/22/2006 First Responder Training 32
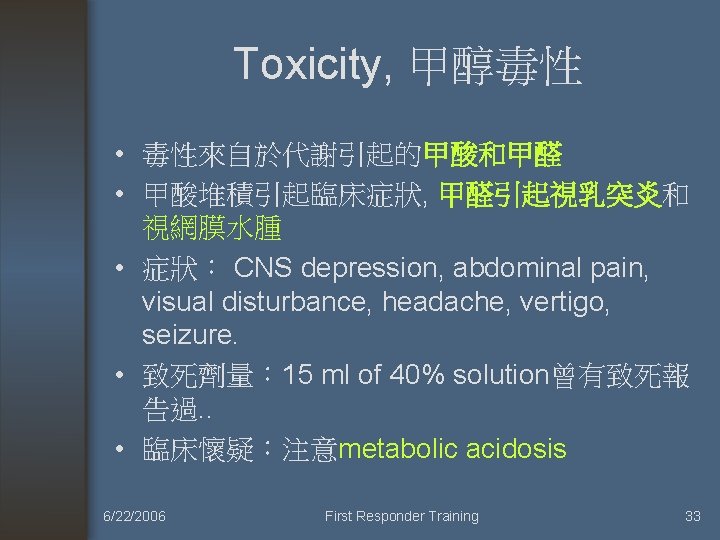
Toxicity, 甲醇毒性 • 毒性來自於代謝引起的甲酸和甲醛 • 甲酸堆積引起臨床症狀, 甲醛引起視乳突炎和 視網膜水腫 • 症狀: CNS depression, abdominal pain, visual disturbance, headache, vertigo, seizure. • 致死劑量: 15 ml of 40% solution曾有致死報 告過. . • 臨床懷疑:注意metabolic acidosis 6/22/2006 First Responder Training 33
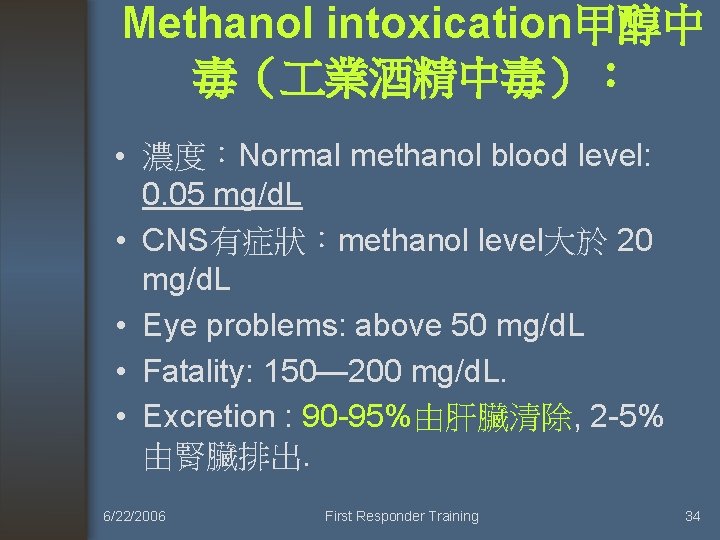
Methanol intoxication甲醇中 毒( 業酒精中毒): • 濃度:Normal methanol blood level: 0. 05 mg/d. L • CNS有症狀:methanol level大於 20 mg/d. L • Eye problems: above 50 mg/d. L • Fatality: 150— 200 mg/d. L. • Excretion : 90 -95%由肝臟清除, 2 -5% 由腎臟排出. 6/22/2006 First Responder Training 34
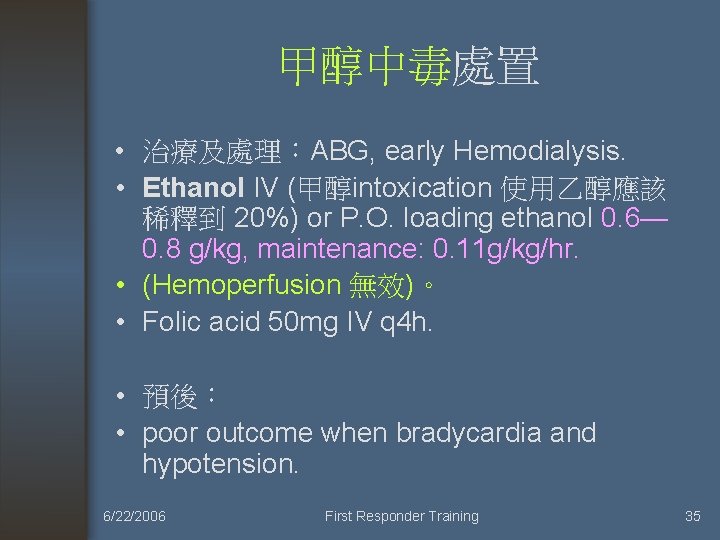
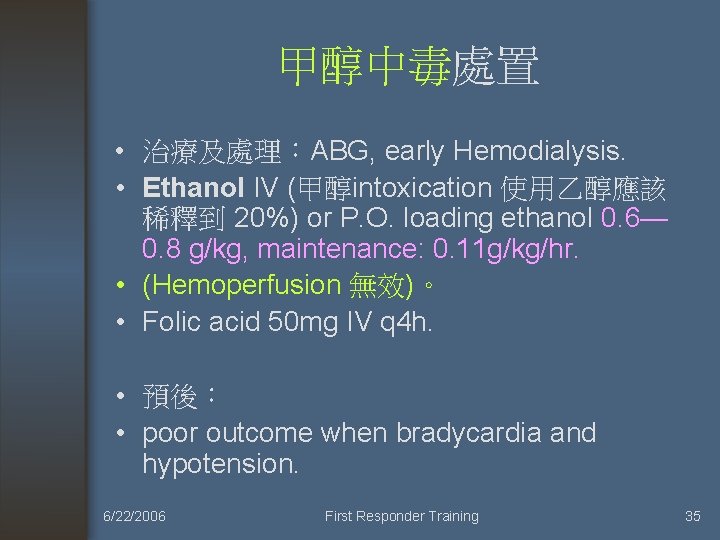
甲醇中毒處置 • 治療及處理:ABG, early Hemodialysis. • Ethanol IV (甲醇intoxication 使用乙醇應該 稀釋到 20%) or P. O. loading ethanol 0. 6— 0. 8 g/kg, maintenance: 0. 11 g/kg/hr. • (Hemoperfusion 無效)。 • Folic acid 50 mg IV q 4 h. • 預後: • poor outcome when bradycardia and hypotension. 6/22/2006 First Responder Training 35
毒蠻牛千面人王進展 被求死刑 • 2005. May. Taiwan台中 6/22/2006 First Responder Training 36




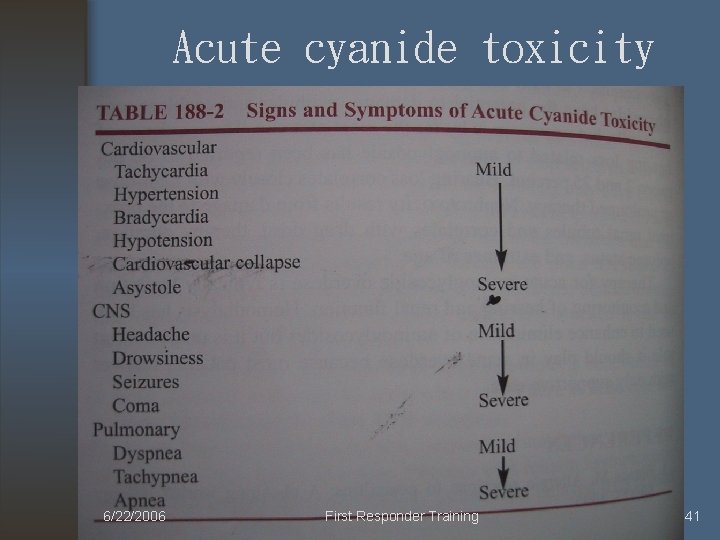
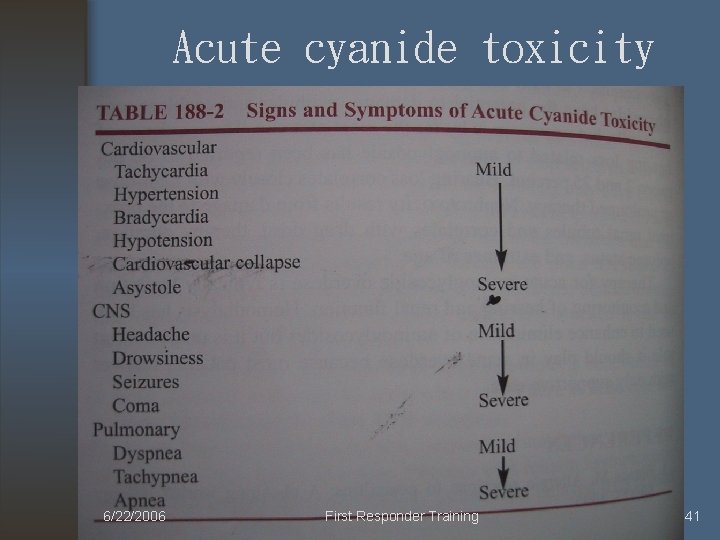
Acute cyanide toxicity 6/22/2006 First Responder Training 41


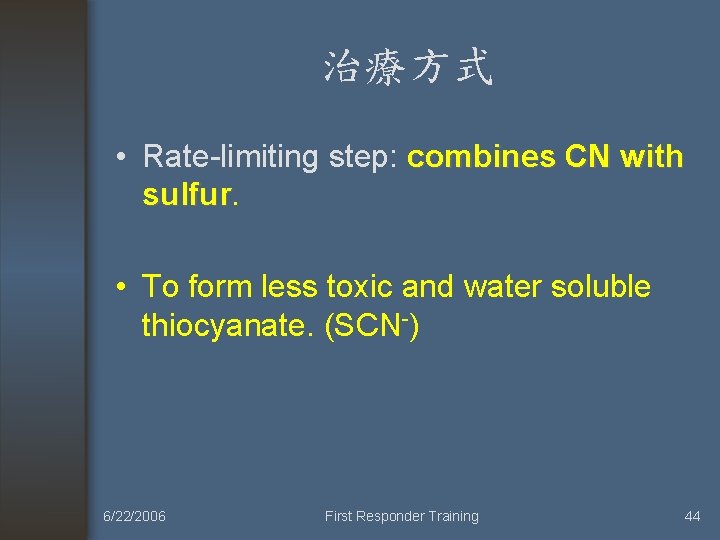
治療方式 • Rate-limiting step: combines CN with sulfur • To form less toxic and water soluble thiocyanate. (SCN-) 6/22/2006 First Responder Training 44

Cyanide antidote kit 6/22/2006 First Responder Training 46
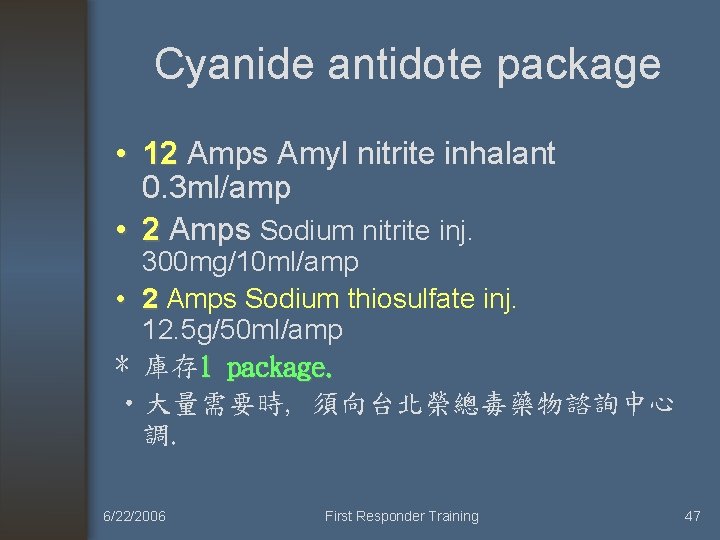
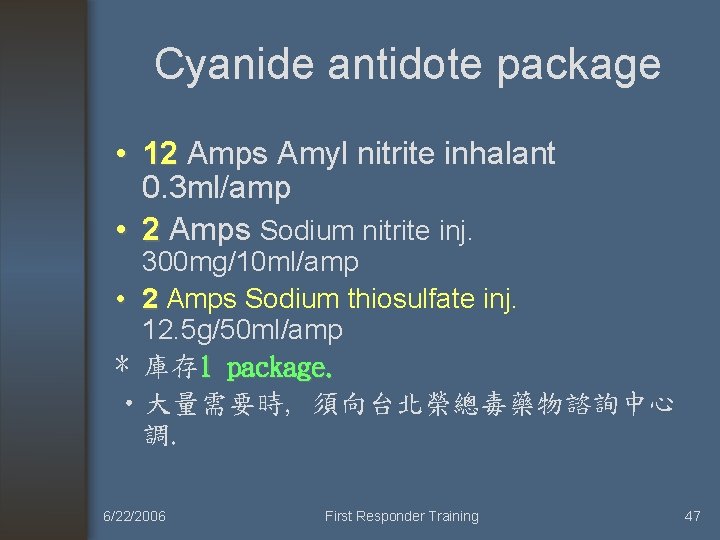
Cyanide antidote package • 12 Amps Amyl nitrite inhalant 12 0. 3 ml/amp • 2 Amps Sodium nitrite inj. 300 mg/10 ml/amp • 2 Amps Sodium thiosulfate inj. 12. 5 g/50 ml/amp * 庫存 1 package. • 大量需要時, 須向台北榮總毒藥物諮詢中心 調. 6/22/2006 First Responder Training 47



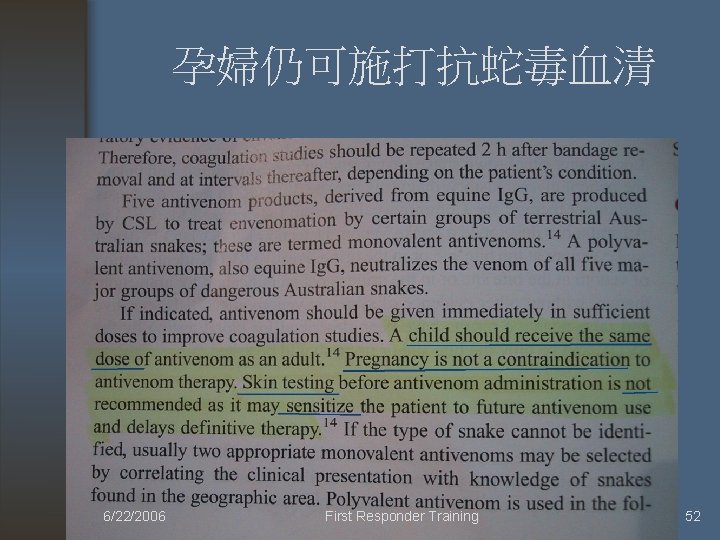
Anti-venom • Skin test? (not recommended) • Pregnancy? (not contraindicated) 6/22/2006 First Responder Training 51
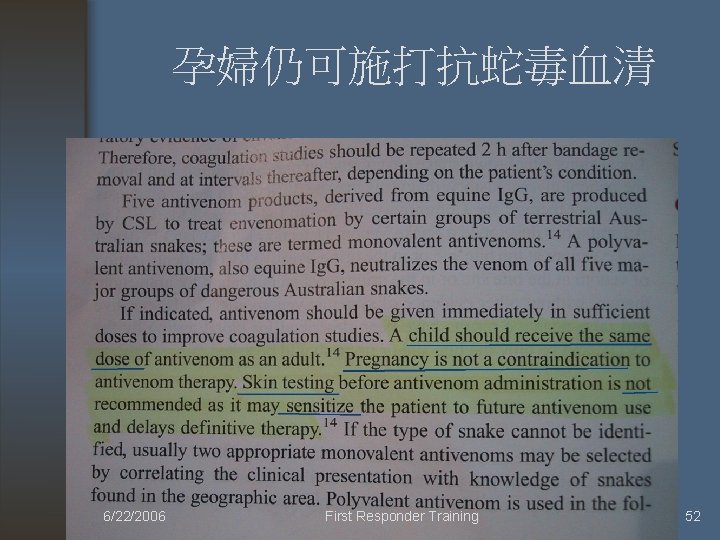
孕婦仍可施打抗蛇毒血清 6/22/2006 First Responder Training 52
Observation 需觀察多久? • How long ? 6/22/2006 First Responder Training 53
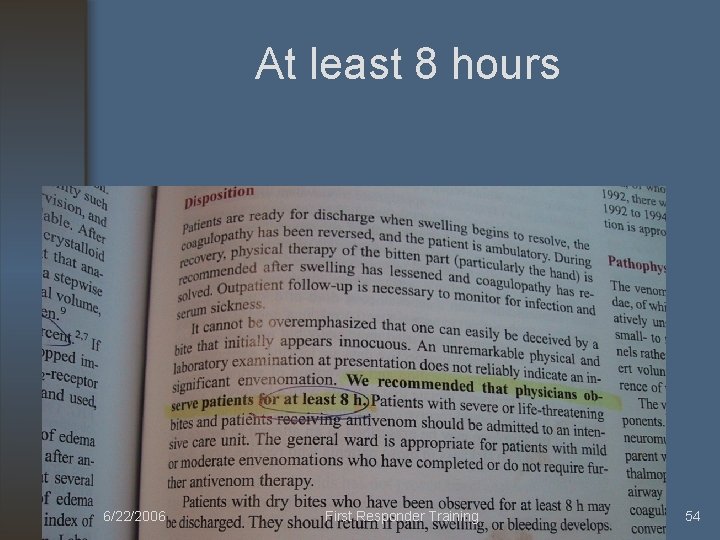
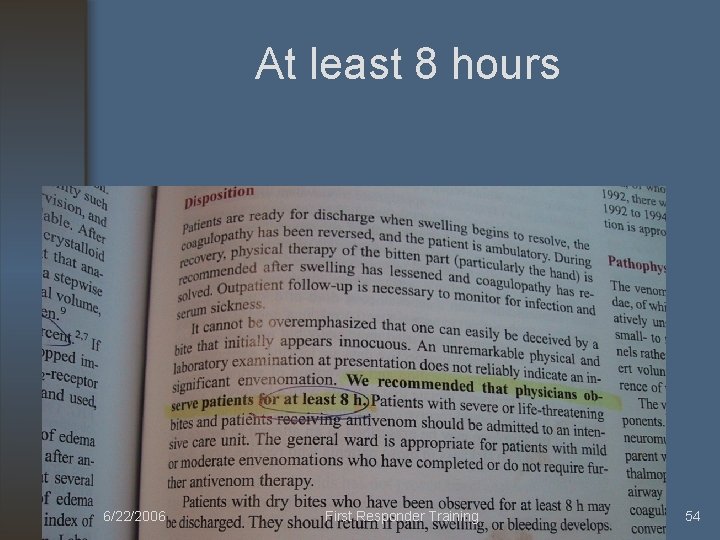
At least 8 hours 6/22/2006 First Responder Training 54

DKA (Diabetic ketoacidosis) • DKA主要發生於 Type I DM (Insulin dependent DM), 但也可以發生於 Type II DM 病人身上. • 有大約 20 --30 % 病人屬於 new onset diabetes. • 致病原因: • excess production of glucose. • Under-utilization of glucose. 葡萄糖利用不 足 6/22/2006 First Responder Training 56
Predisposing factors of DKA • Infection, pancreatitis 感染, 胰臟炎 • Stroke, myocardial infarction, pulmonary embolism • Trauma • Pregnancy • hyperthyroidism • Surgery • Steroid administration. 6/22/2006 First Responder Training 57
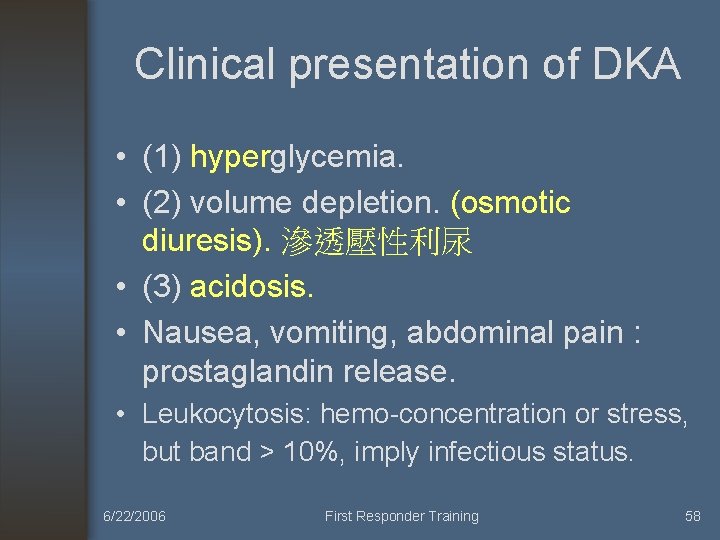
Clinical presentation of DKA • (1) hyperglycemia. • (2) volume depletion. (osmotic diuresis). 滲透壓性利尿 • (3) acidosis. • Nausea, vomiting, abdominal pain : prostaglandin release. • Leukocytosis: hemo-concentration or stress, but band > 10%, imply infectious status. 6/22/2006 First Responder Training 58
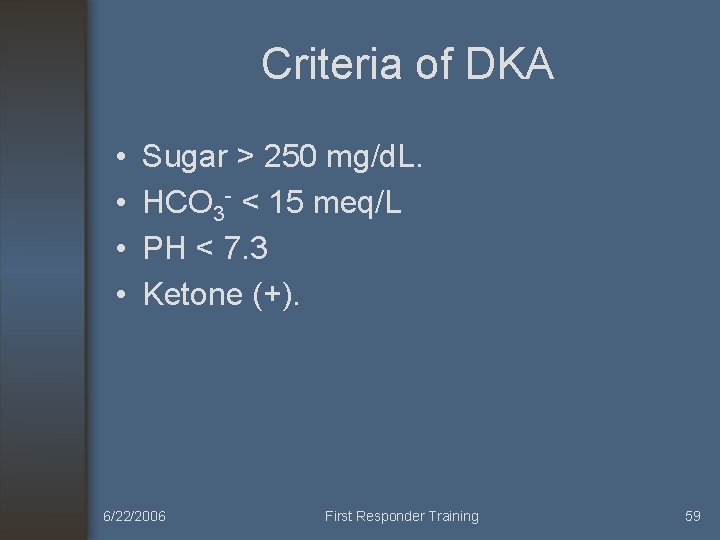
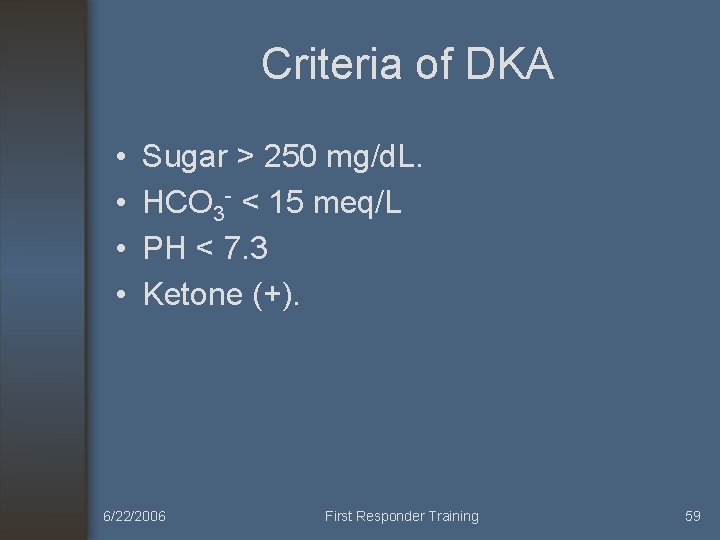
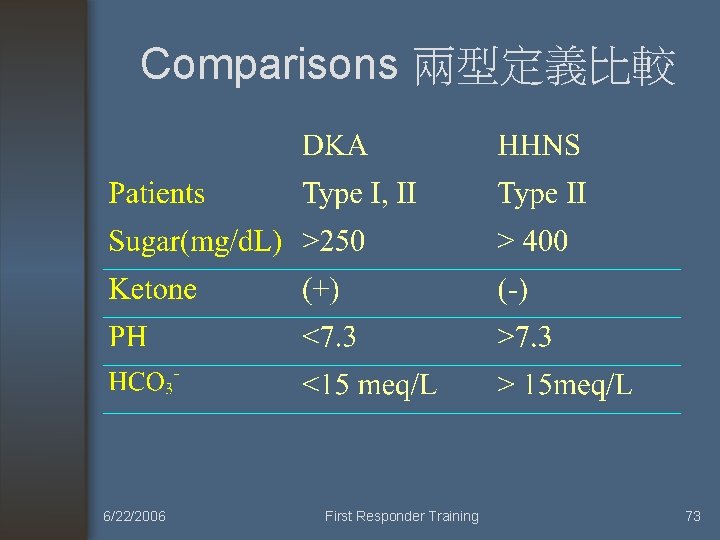
Criteria of DKA • • Sugar > 250 mg/d. L. HCO 3 - < 15 meq/L PH < 7. 3 Ketone (+). 6/22/2006 First Responder Training 59
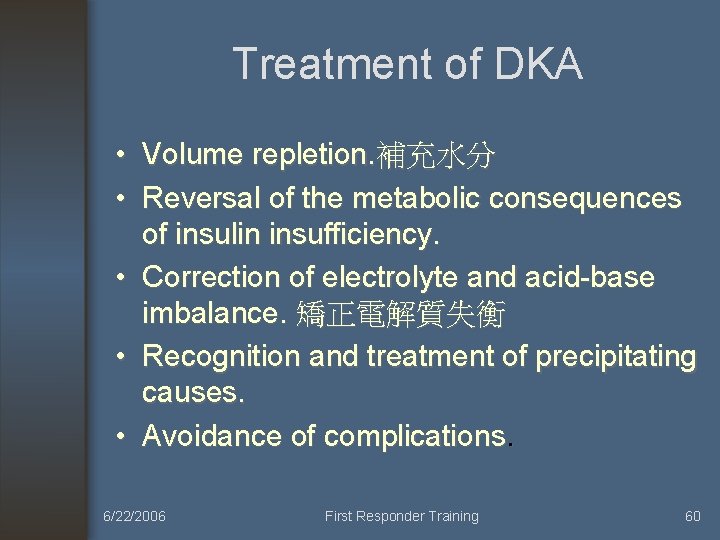
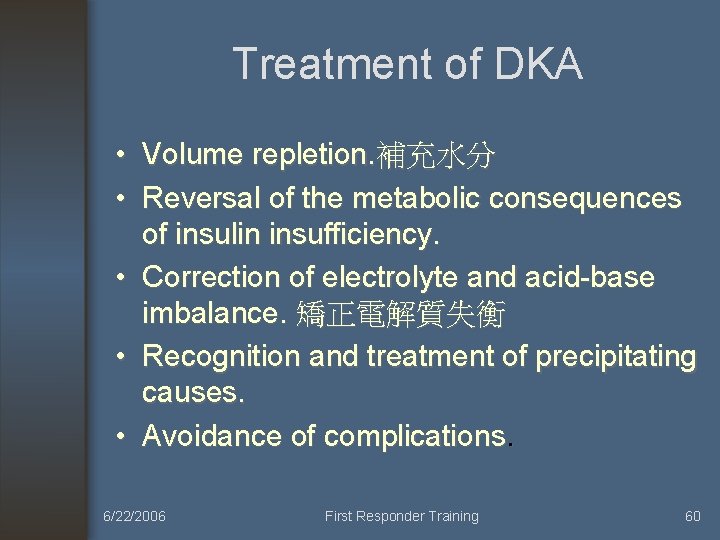
Treatment of DKA • Volume repletion. 補充水分 • Reversal of the metabolic consequences of insulin insufficiency. • Correction of electrolyte and acid-base imbalance. 矯正電解質失衡 • Recognition and treatment of precipitating causes. • Avoidance of complications. 6/22/2006 First Responder Training 60
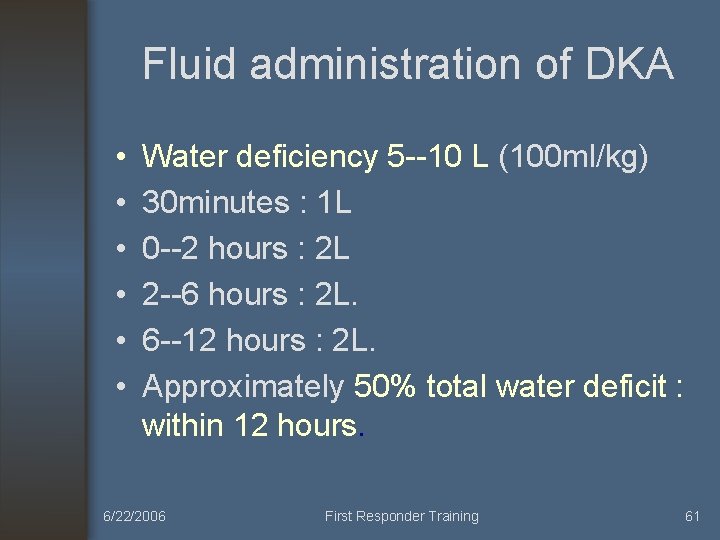
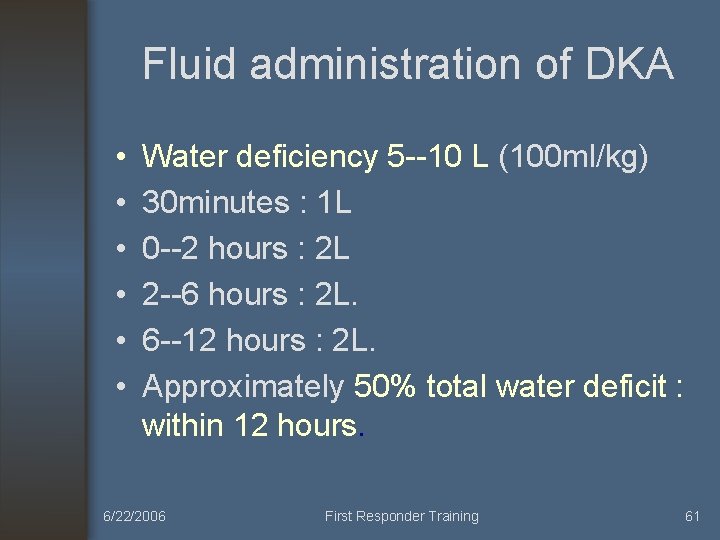
Fluid administration of DKA • • • Water deficiency 5 --10 L (100 ml/kg) 30 minutes : 1 L 0 --2 hours : 2 L 2 --6 hours : 2 L. 6 --12 hours : 2 L. Approximately 50% total water deficit : within 12 hours. 6/22/2006 First Responder Training 61
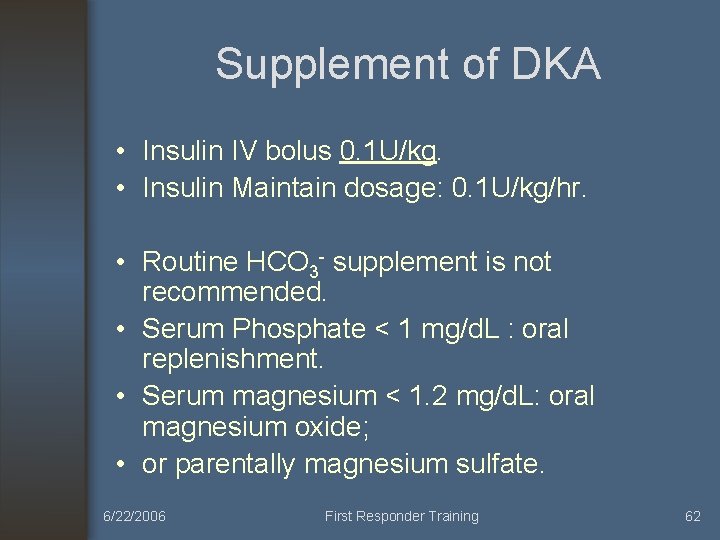
Supplement of DKA • Insulin IV bolus 0. 1 U/kg. • Insulin Maintain dosage: 0. 1 U/kg/hr. • Routine HCO 3 - supplement is not recommended. • Serum Phosphate < 1 mg/d. L : oral replenishment. • Serum magnesium < 1. 2 mg/d. L: oral magnesium oxide; • or parentally magnesium sulfate. 6/22/2006 First Responder Training 62
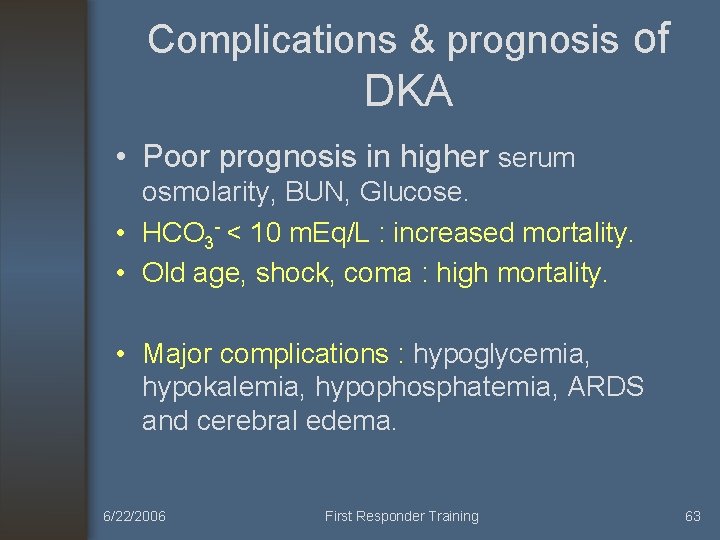
Complications & prognosis of DKA • Poor prognosis in higher serum osmolarity, BUN, Glucose. • HCO 3 - < 10 m. Eq/L : increased mortality. • Old age, shock, coma : high mortality. • Major complications : hypoglycemia, hypokalemia, hypophosphatemia, ARDS and cerebral edema. 6/22/2006 First Responder Training 63
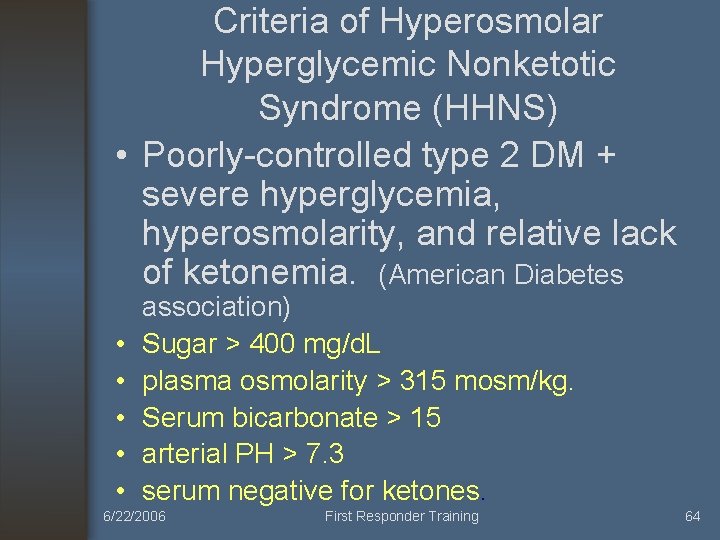
Criteria of Hyperosmolar Hyperglycemic Nonketotic Syndrome (HHNS) • Poorly-controlled type 2 DM + severe hyperglycemia, hyperosmolarity, and relative lack of ketonemia. (American Diabetes • • • association) Sugar > 400 mg/d. L plasma osmolarity > 315 mosm/kg. Serum bicarbonate > 15 arterial PH > 7. 3 serum negative for ketones. 6/22/2006 First Responder Training 64
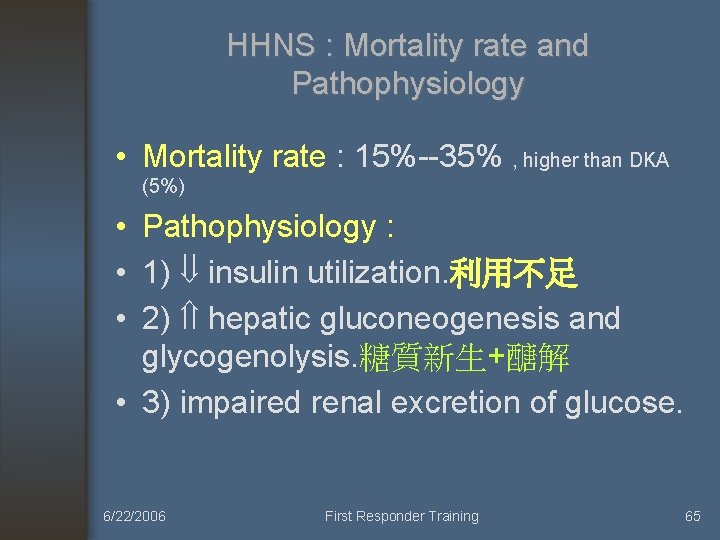
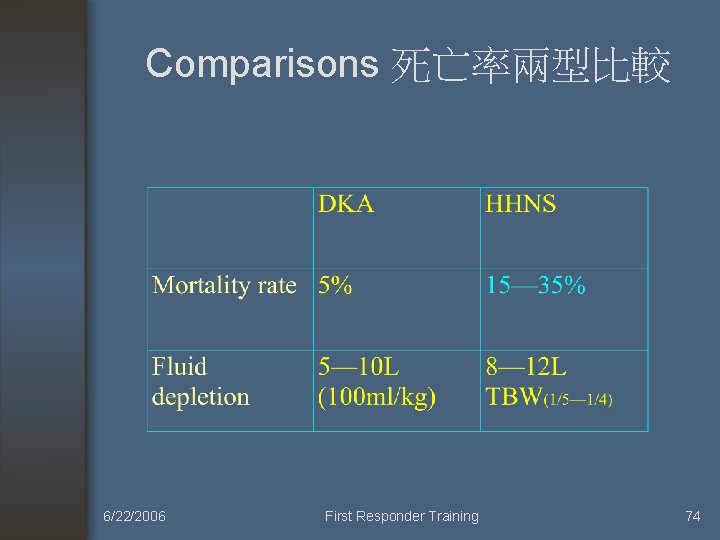
HHNS : Mortality rate and Pathophysiology • Mortality rate : 15%--35% , higher than DKA (5%) • Pathophysiology : • 1) insulin utilization. 利用不足 • 2) hepatic gluconeogenesis and glycogenolysis. 糖質新生+醣解 • 3) impaired renal excretion of glucose. 6/22/2006 First Responder Training 65
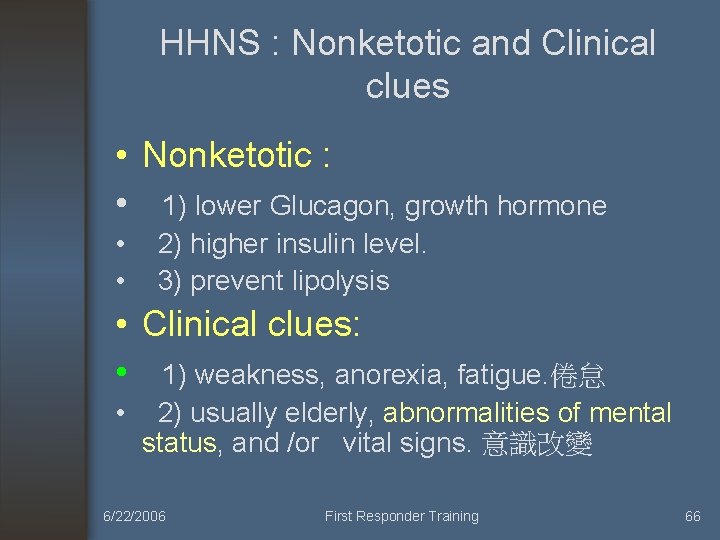
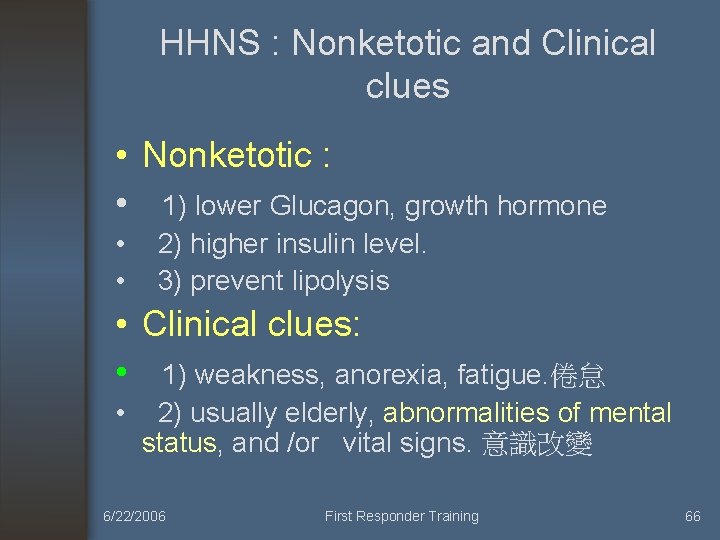
HHNS : Nonketotic and Clinical clues • Nonketotic : • 1) lower Glucagon, growth hormone • 2) higher insulin level. • 3) prevent lipolysis • Clinical clues: • 1) weakness, anorexia, fatigue. 倦怠 • 2) usually elderly, abnormalities of mental status, and /or vital signs. 意識改變 6/22/2006 First Responder Training 66
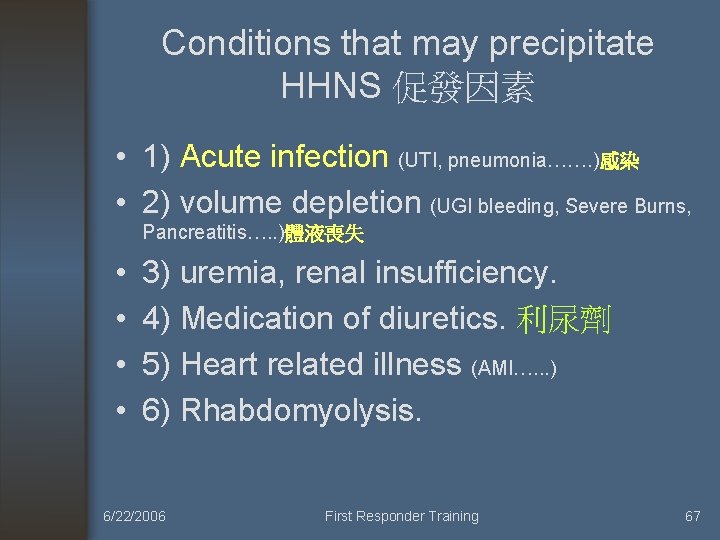
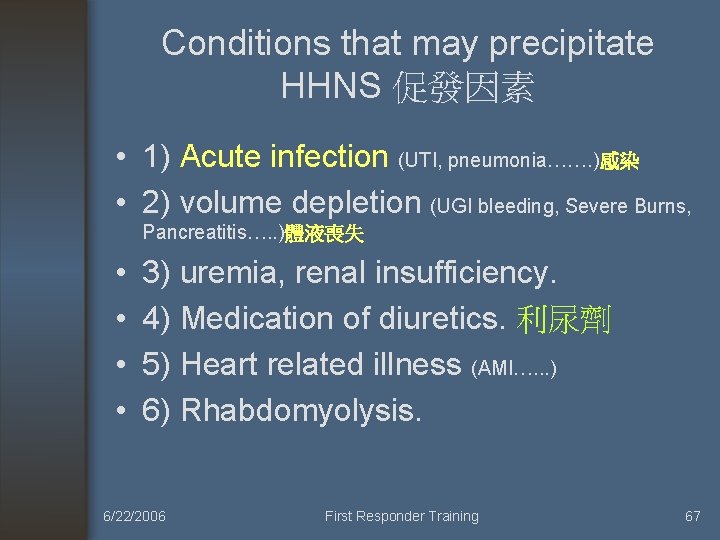
Conditions that may precipitate HHNS 促發因素 • 1) Acute infection (UTI, pneumonia……. )感染 • 2) volume depletion (UGI bleeding, Severe Burns, Pancreatitis…. . )體液喪失 • • 3) uremia, renal insufficiency. 4) Medication of diuretics. 利尿劑 5) Heart related illness (AMI…. . . ) 6) Rhabdomyolysis. 6/22/2006 First Responder Training 67
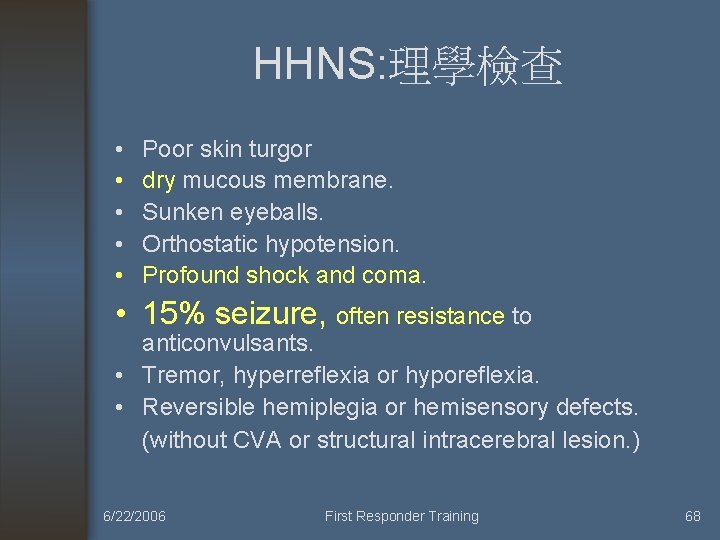
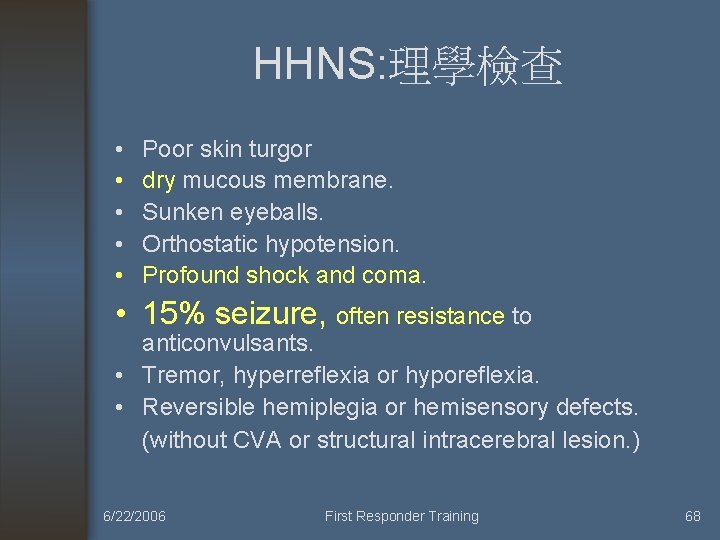
HHNS: 理學檢查 • • • Poor skin turgor dry mucous membrane. Sunken eyeballs. Orthostatic hypotension. Profound shock and coma. • 15% seizure, often resistance to anticonvulsants. • Tremor, hyperreflexia or hyporeflexia. • Reversible hemiplegia or hemisensory defects. (without CVA or structural intracerebral lesion. ) 6/22/2006 First Responder Training 68
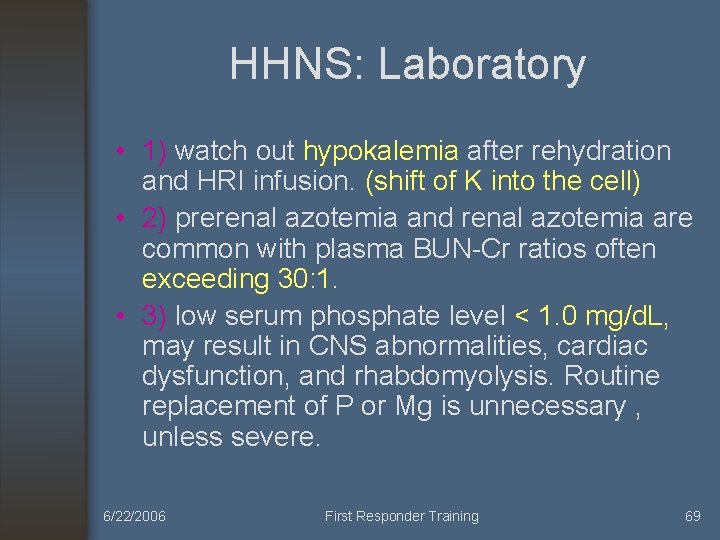
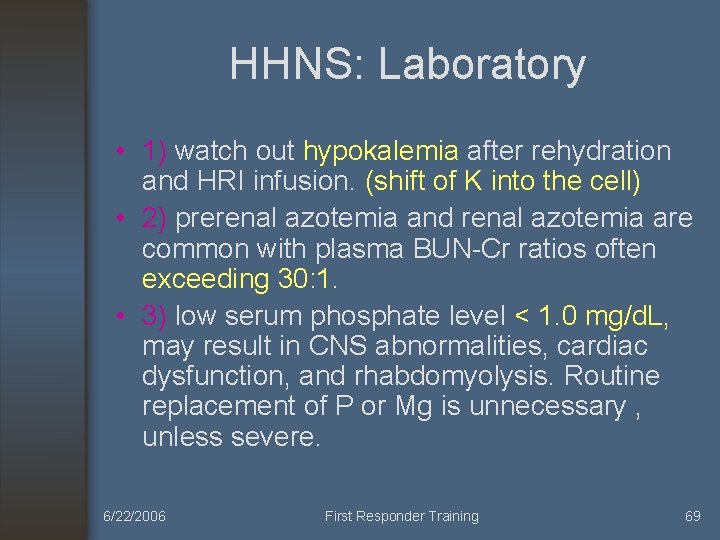
HHNS: Laboratory • 1) watch out hypokalemia after rehydration and HRI infusion. (shift of K into the cell) • 2) prerenal azotemia and renal azotemia are common with plasma BUN-Cr ratios often exceeding 30: 1. • 3) low serum phosphate level < 1. 0 mg/d. L, may result in CNS abnormalities, cardiac dysfunction, and rhabdomyolysis. Routine replacement of P or Mg is unnecessary , unless severe. 6/22/2006 First Responder Training 69
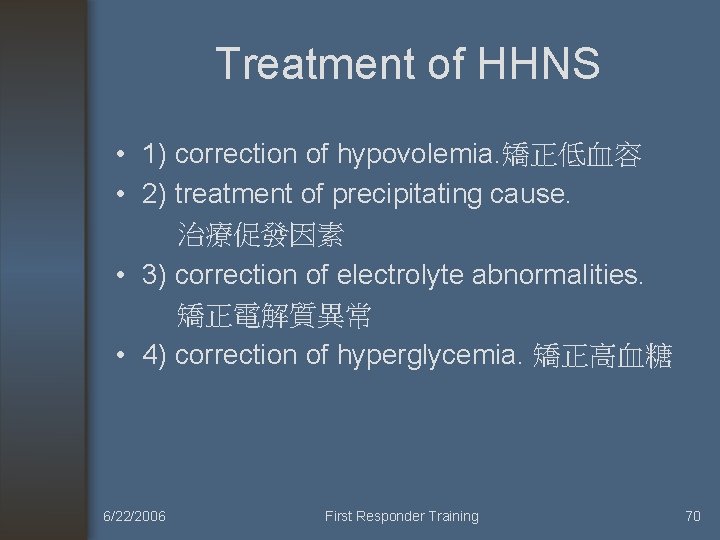
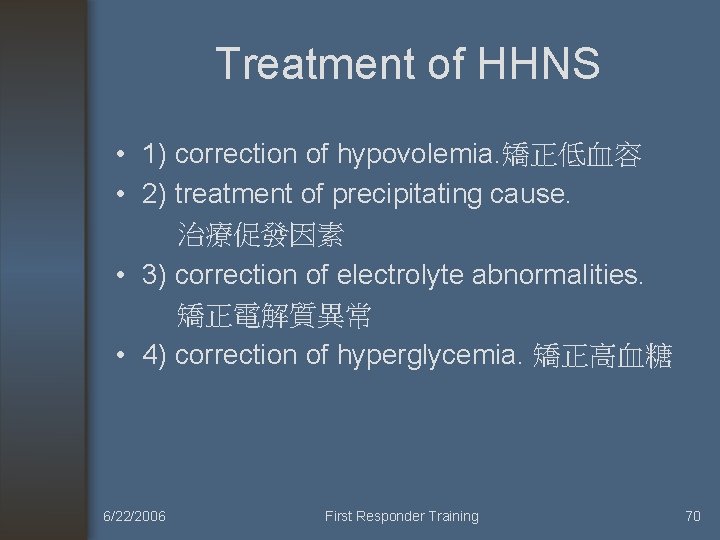
Treatment of HHNS • 1) correction of hypovolemia. 矯正低血容 • 2) treatment of precipitating cause. 治療促發因素 • 3) correction of electrolyte abnormalities. 矯正電解質異常 • 4) correction of hyperglycemia. 矯正高血糖 6/22/2006 First Responder Training 70
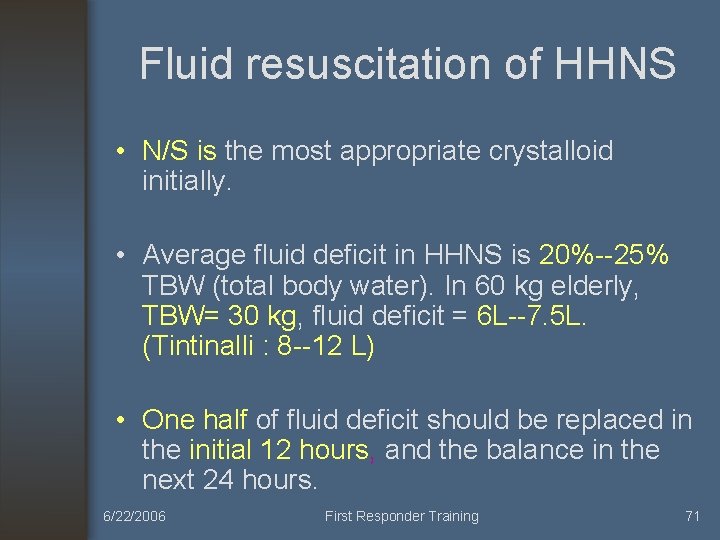
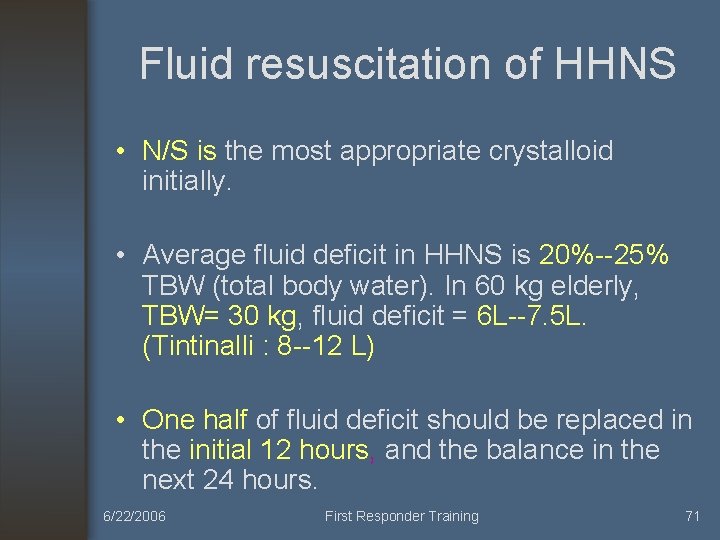
Fluid resuscitation of HHNS • N/S is the most appropriate crystalloid initially. • Average fluid deficit in HHNS is 20%--25% TBW (total body water). In 60 kg elderly, TBW= 30 kg, fluid deficit = 6 L--7. 5 L. (Tintinalli : 8 --12 L) • One half of fluid deficit should be replaced in the initial 12 hours, and the balance in the next 24 hours. 6/22/2006 First Responder Training 71
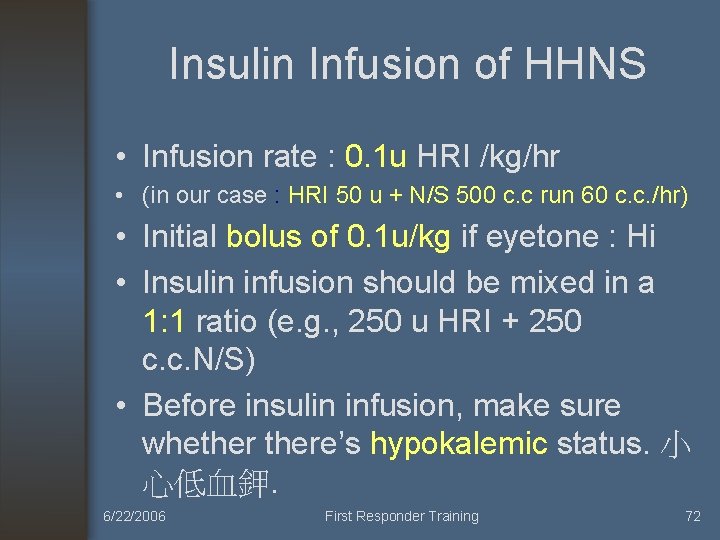
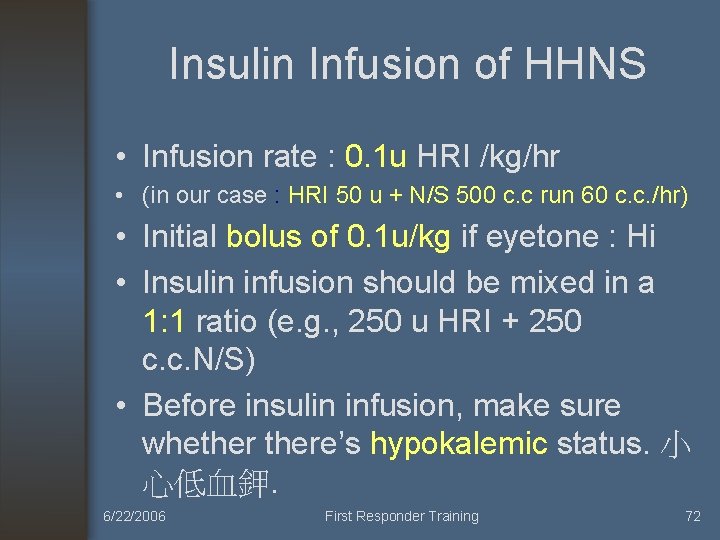
Insulin Infusion of HHNS • Infusion rate : 0. 1 u HRI /kg/hr • (in our case : HRI 50 u + N/S 500 c. c run 60 c. c. /hr) • Initial bolus of 0. 1 u/kg if eyetone : Hi • Insulin infusion should be mixed in a 1: 1 ratio (e. g. , 250 u HRI + 250 c. c. N/S) • Before insulin infusion, make sure whethere’s hypokalemic status. 小 心低血鉀. 6/22/2006 First Responder Training 72
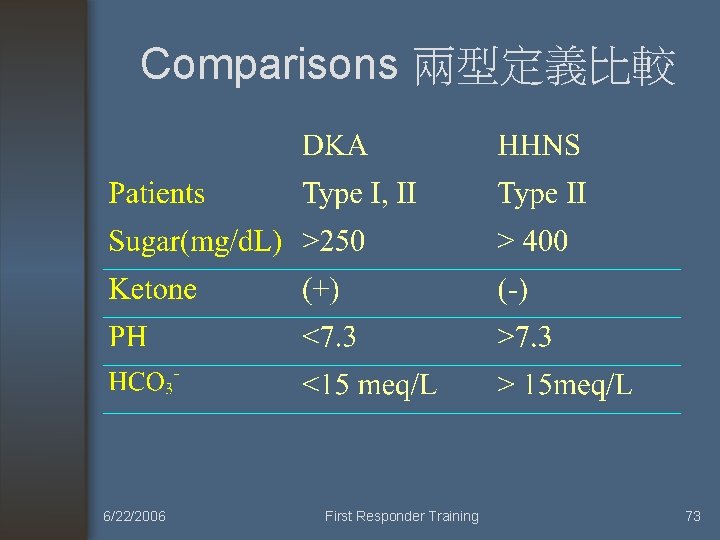
Comparisons 兩型定義比較 6/22/2006 First Responder Training 73
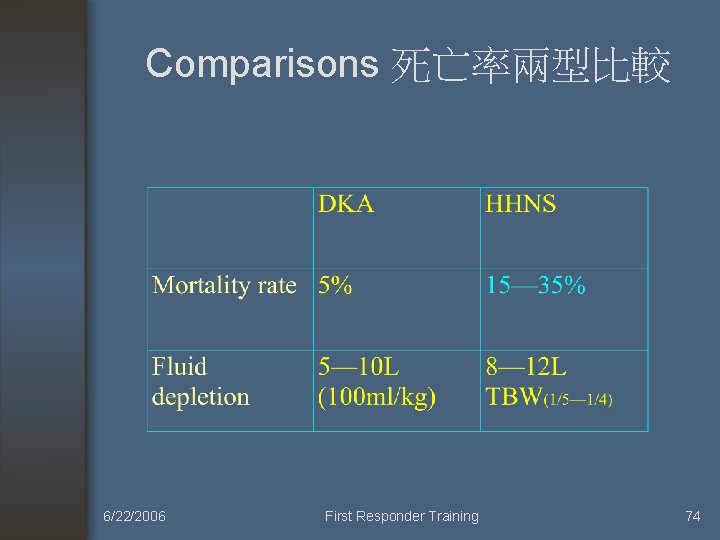
Comparisons 死亡率兩型比較 6/22/2006 First Responder Training 74






癲癇 6/22/2006 First Responder Training 81












References • Emerg. Med. J. , Mar 2006; 23: 183 - 185. • The American Journal of Emergency Medicine, Volume 14, Issue 5, September 1996, Pages 451 -453 • 蘇昱彰: 乙醯氨酚 (Acetaminophen) 服用過量。Taiwan Medical Journal 2004, Vol 47, No. 9, p. 423— 424. 6/22/2006 First Responder Training 94
 Emergency medical responder: first on scene
Emergency medical responder: first on scene Emergency medical responder first on scene 10th edition
Emergency medical responder first on scene 10th edition Emergency medical responder first on scene 11th edition
Emergency medical responder first on scene 11th edition American red cross first responder
American red cross first responder Antecubitsl
Antecubitsl Mmh radio thorax
Mmh radio thorax Mmh-015
Mmh-015 Mmh-015
Mmh-015 Lane designation terminology
Lane designation terminology National tim responder training test answers
National tim responder training test answers National tim responder training test answers
National tim responder training test answers Law enforcement first responder
Law enforcement first responder Emergency nursing orientation
Emergency nursing orientation Whittington emergency department
Whittington emergency department Emergency care harrow
Emergency care harrow Sfgh emergency department
Sfgh emergency department What is simultaneous evacuation
What is simultaneous evacuation The importance of training
The importance of training Chec certification
Chec certification Emergency evacuation training
Emergency evacuation training Pa wc bureau
Pa wc bureau Chapter 8 emergency care first aid and disasters
Chapter 8 emergency care first aid and disasters Como mandar un correo electronico formal
Como mandar un correo electronico formal Nwcg iqcs
Nwcg iqcs Responder
Responder Crisis responder
Crisis responder Esten siempre preparados para responder
Esten siempre preparados para responder Que responder a un bienvenido
Que responder a un bienvenido Adveischool opiniones
Adveischool opiniones Rescue breaths for child with pulse
Rescue breaths for child with pulse En qu
En qu Consecuencias de rechazar a cristo
Consecuencias de rechazar a cristo Valanti
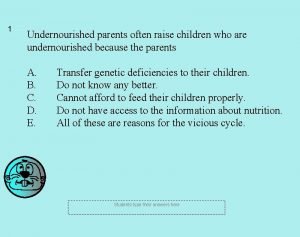
Valanti Undernourished parents often raise
Undernourished parents often raise Department of higher education and training
Department of higher education and training Department of labor and training
Department of labor and training Training design example
Training design example Training is expensive without training it is more expensive
Training is expensive without training it is more expensive Perbedaan on the job training dan off the job training
Perbedaan on the job training dan off the job training Aggression replacement training facilitator training
Aggression replacement training facilitator training Maturity continuum diagram
Maturity continuum diagram Recursive breadth first search
Recursive breadth first search Sdl first vs code first
Sdl first vs code first Put first things first activities
Put first things first activities Put first things first meaning
Put first things first meaning Entity framework 7 release date
Entity framework 7 release date First to file vs first to invent
First to file vs first to invent Stack declaration
Stack declaration Diketahui suatu stack dengan max_stack = 6
Diketahui suatu stack dengan max_stack = 6 First in first out
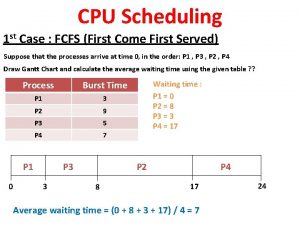
First in first out First come first serve
First come first serve Put first things first definition
Put first things first definition First come first serve gantt chart
First come first serve gantt chart Franklin covey maturity continuum
Franklin covey maturity continuum Habit 3 put first things first
Habit 3 put first things first Put first things first video
Put first things first video Put first things first activities
Put first things first activities First aid merit badge first aid kit
First aid merit badge first aid kit First aid in the first grade
First aid in the first grade Put first things first
Put first things first What is sems
What is sems Who emergency care system framework
Who emergency care system framework Svmc emergency room
Svmc emergency room Nethercutt emergency center
Nethercutt emergency center Pengertian emergency
Pengertian emergency Emergency purchasing
Emergency purchasing 7 tray in labour room
7 tray in labour room The standards of prehospital emergency care
The standards of prehospital emergency care Therapeutic communication techniques
Therapeutic communication techniques Pengertian emergency equipment
Pengertian emergency equipment Pdo emergency number
Pdo emergency number Pdo emergency number
Pdo emergency number Electric vehicle emergency field guide
Electric vehicle emergency field guide Module 12 emergency procedures
Module 12 emergency procedures Metropolitan fire and emergency services board
Metropolitan fire and emergency services board Abcde bundle
Abcde bundle Emergency management of maxillofacial trauma
Emergency management of maxillofacial trauma Htn emergency vs urgency
Htn emergency vs urgency The mutcd states all workers
The mutcd states all workers Egress flight
Egress flight Nn24 hour emergency dental
Nn24 hour emergency dental Emergency vehicle alert system
Emergency vehicle alert system Erg green section
Erg green section Emergency care enfield
Emergency care enfield Ercp emergency response
Ercp emergency response Hennepin county emergency management
Hennepin county emergency management Code grey hospital
Code grey hospital Emergency care 13th edition chapter 1
Emergency care 13th edition chapter 1 Emergency number estonia
Emergency number estonia List the emergency action steps
List the emergency action steps Emergency transmitter finder
Emergency transmitter finder Dialux emergency lighting tutorial
Dialux emergency lighting tutorial Emergency by denis johnson
Emergency by denis johnson Ham radio communications trailers
Ham radio communications trailers Thyristor applications and circuits
Thyristor applications and circuits