DISEASES OF SALIVARY GLAND SALIVARY GLANDS There are





- Slides: 56
DISEASES OF SALIVARY GLAND
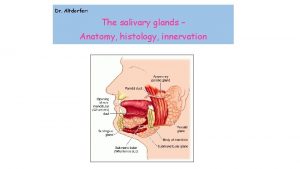
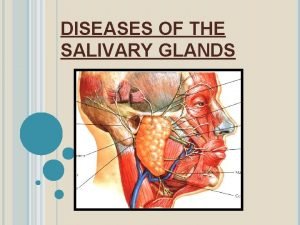
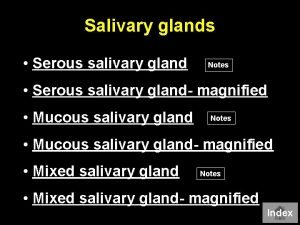
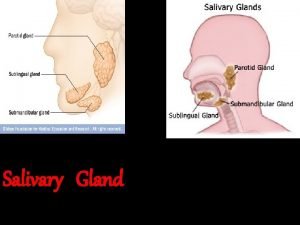
SALIVARY GLANDS • There are two main groups of salivary glands— major minor. • The major salivary glands are three paired glands • parotid • Submandibular • sublingual The minor salivary glands are numerous and are widely distributed in the mucosa of oral cavity The main duct of the parotid gland drains into the oral cavity opposite the second maxillary molar,
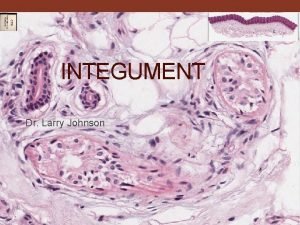
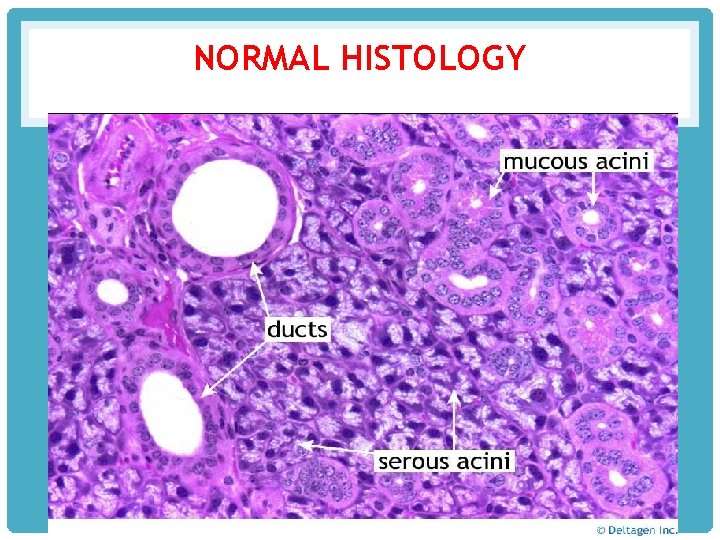
HISTOLOGY • ducts of submandibular and sublingual glands empty in the floor of the mouth. • the salivary glands are tubuloalveolar glands may contain mucous cells, serous cells, or both • parotid gland is purely serous submandibular gland is mixed type sublingual gland is predominantly mucous type.
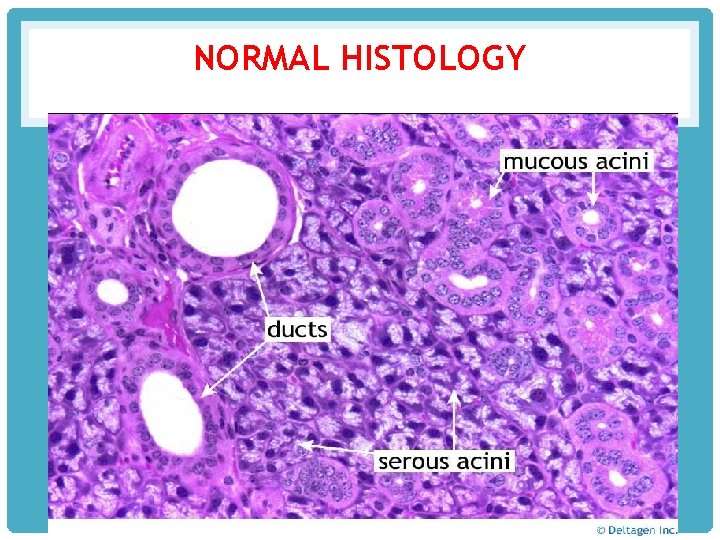
NORMAL HISTOLOGY
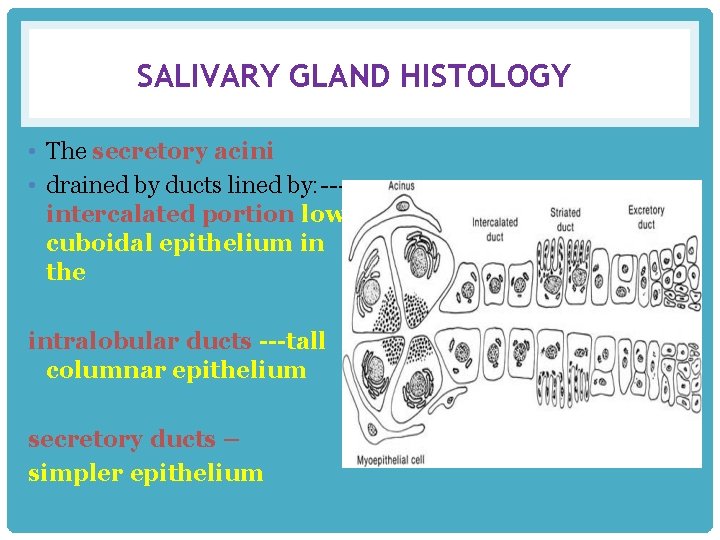
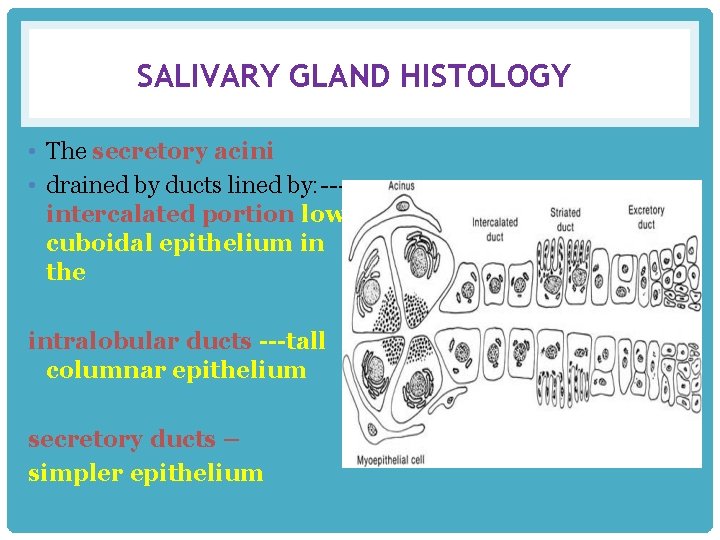
SALIVARY GLAND HISTOLOGY • The secretory acini • drained by ducts lined by: --intercalated portion low cuboidal epithelium in the intralobular ducts ---tall columnar epithelium secretory ducts – simpler epithelium
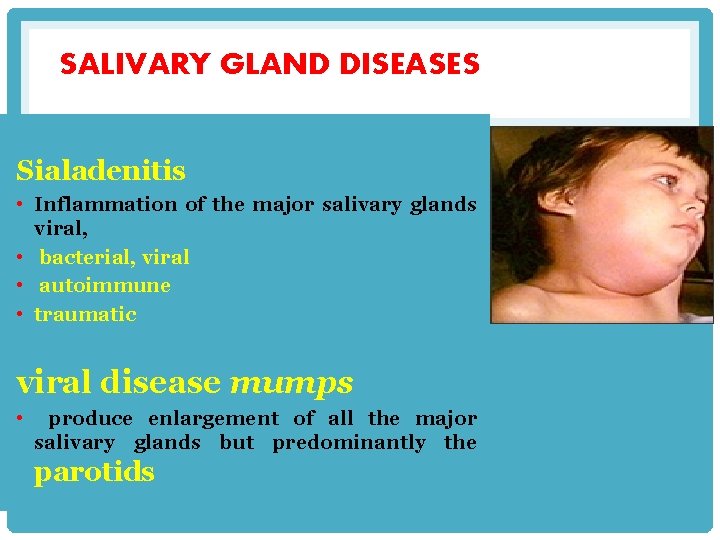
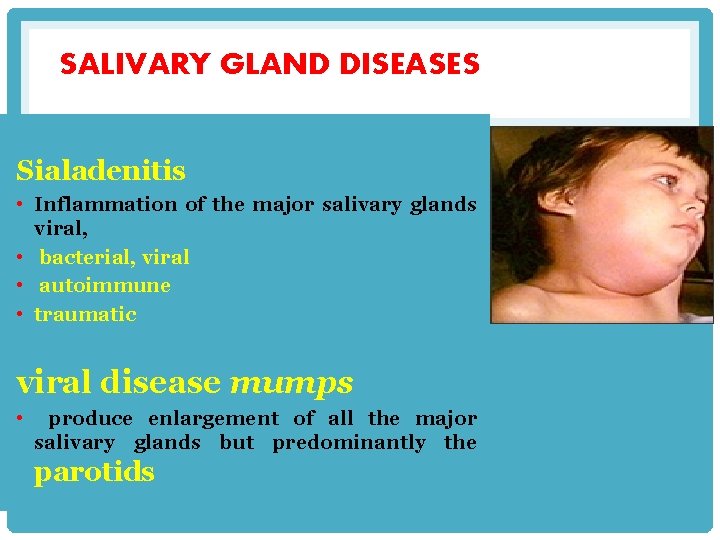
SALIVARY GLAND DISEASES Sialadenitis • Inflammation of the major salivary glands viral, • bacterial, viral • autoimmune • traumatic viral disease mumps • produce enlargement of all the major salivary glands but predominantly the parotids
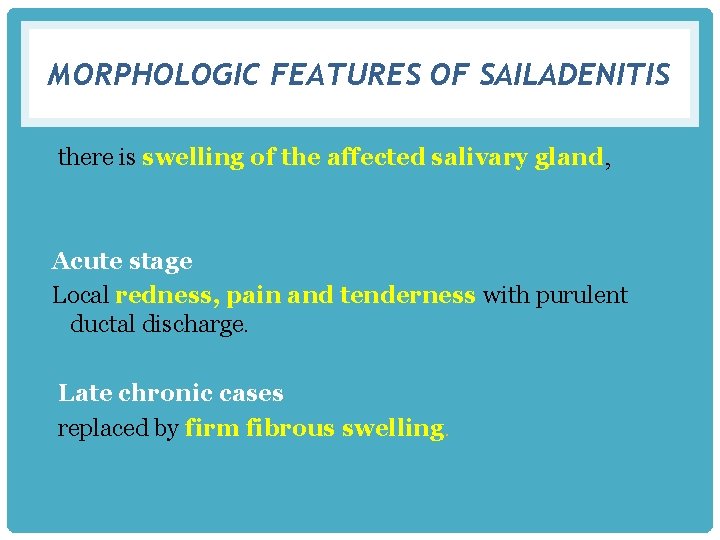
MORPHOLOGIC FEATURES OF SAILADENITIS there is swelling of the affected salivary gland, Acute stage Local redness, pain and tenderness with purulent ductal discharge. Late chronic cases replaced by firm fibrous swelling.
MUMPS • occurring in children of school-age. characterized by triad of pathological involvement— • epidemic parotitis(mumps) • orchitis-oophoritis • pancreatitis • testis and pancreas -----atrophy.
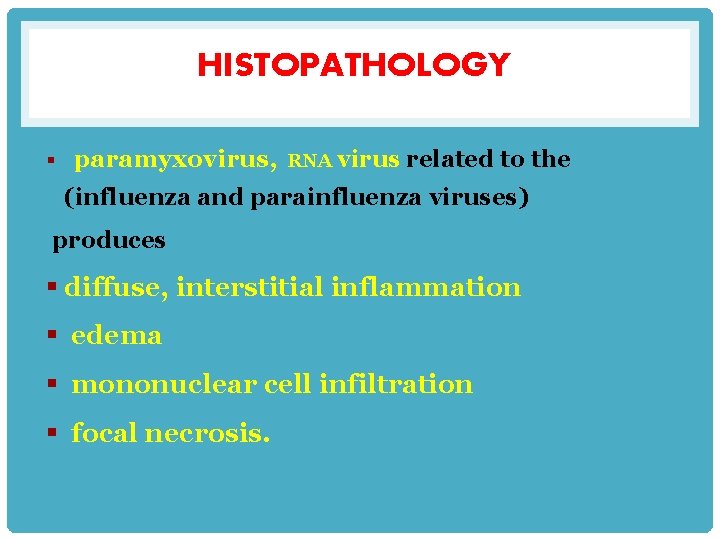
HISTOPATHOLOGY § paramyxovirus, RNA virus related to the (influenza and parainfluenza viruses) produces § diffuse, interstitial inflammation § edema § mononuclear cell infiltration § focal necrosis.
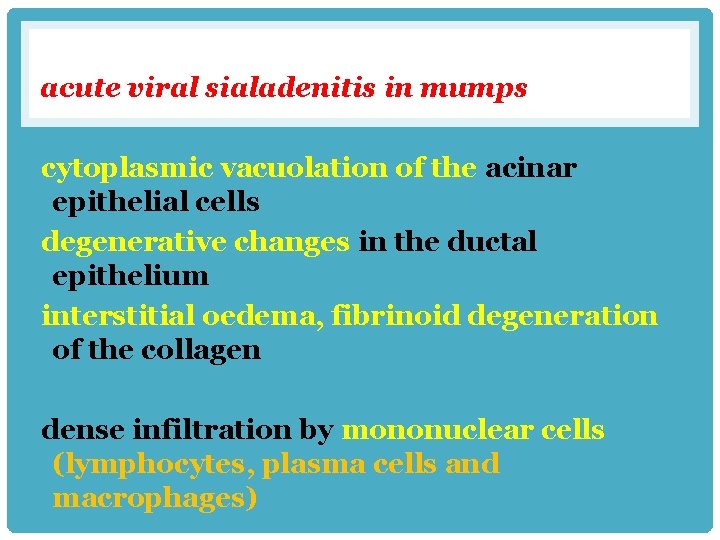
acute viral sialadenitis in mumps cytoplasmic vacuolation of the acinar epithelial cells degenerative changes in the ductal epithelium interstitial oedema, fibrinoid degeneration of the collagen dense infiltration by mononuclear cells (lymphocytes, plasma cells and macrophages)
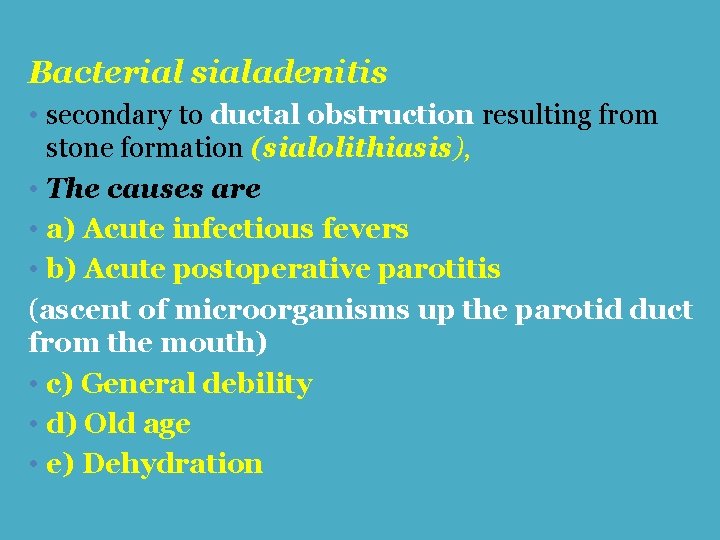
Bacterial sialadenitis • secondary to ductal obstruction resulting from stone formation (sialolithiasis), • The causes are • a) Acute infectious fevers • b) Acute postoperative parotitis (ascent of microorganisms up the parotid duct from the mouth) • c) General debility • d) Old age • e) Dehydration
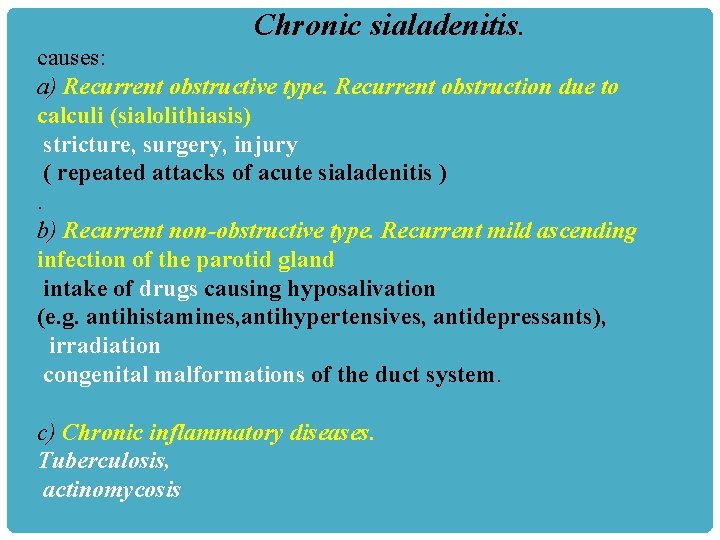
Chronic sialadenitis. causes: a) Recurrent obstructive type. Recurrent obstruction due to calculi (sialolithiasis) stricture, surgery, injury ( repeated attacks of acute sialadenitis ). b) Recurrent non-obstructive type. Recurrent mild ascending infection of the parotid gland intake of drugs causing hyposalivation (e. g. antihistamines, antihypertensives, antidepressants), irradiation congenital malformations of the duct system. c) Chronic inflammatory diseases. Tuberculosis, actinomycosis
The sialadenitis may be § interstitial § suppurative necrosis § abscess formation. Pathogenesis • Chronic sialadenitis arises from • decreased production of saliva with inflammation. • increased lymphoid tissue in the interstitium, loss of secretory tissue and replacement by fibrosis.
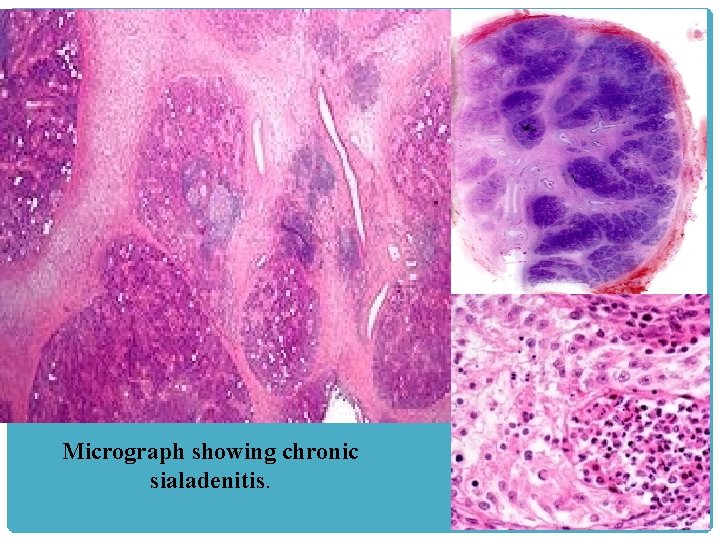
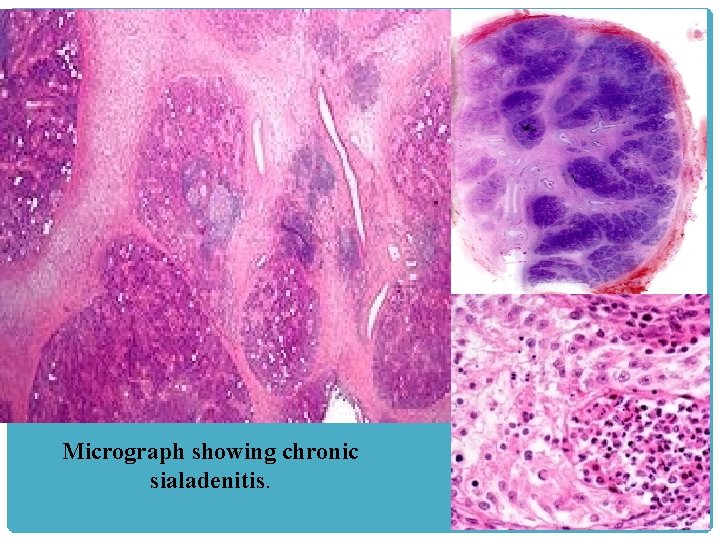
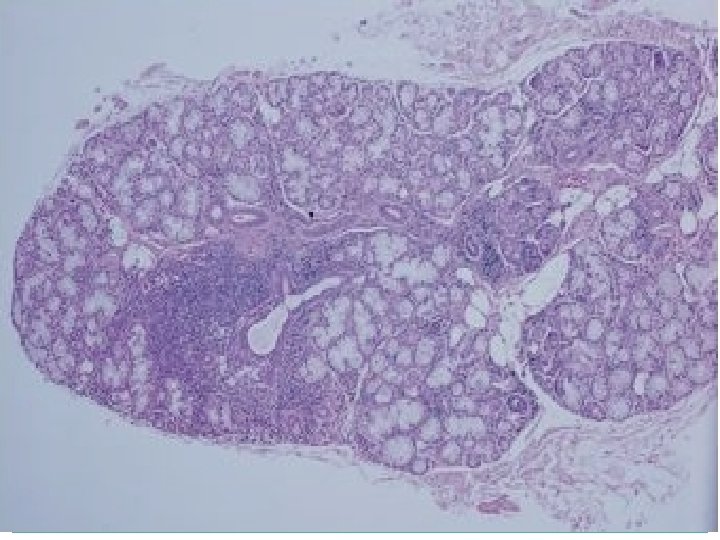
Micrograph showing chronic sialadenitis.
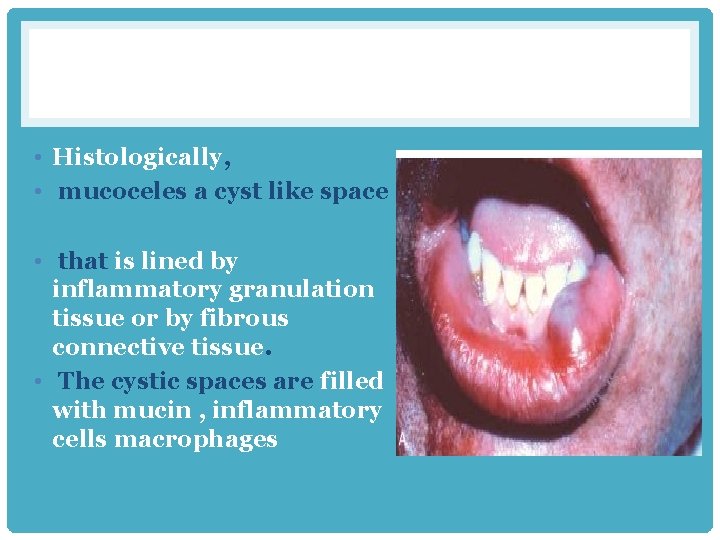
Mucoceles • most common type of inflammatory salivary gland lesion • found on the lower lip • result of trauma • toddlers and young adults history of changes in the size of the lesion, in association with meals • results from either blockage or rupture of a salivary gland duct, • leakage of saliva into the surrounding connective tissue stroma. present as fluctuant swellings of the lower lip and have a blue translucent hue
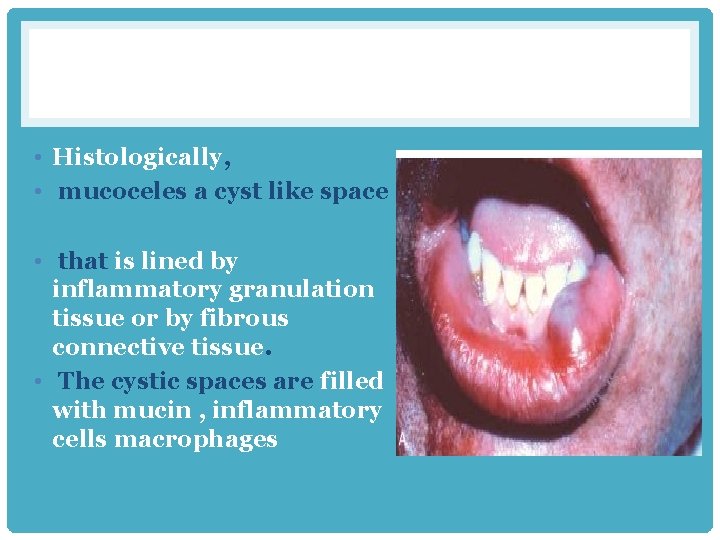
• Histologically, • mucoceles a cyst like space • that is lined by inflammatory granulation tissue or by fibrous connective tissue. • The cystic spaces are filled with mucin , inflammatory cells macrophages
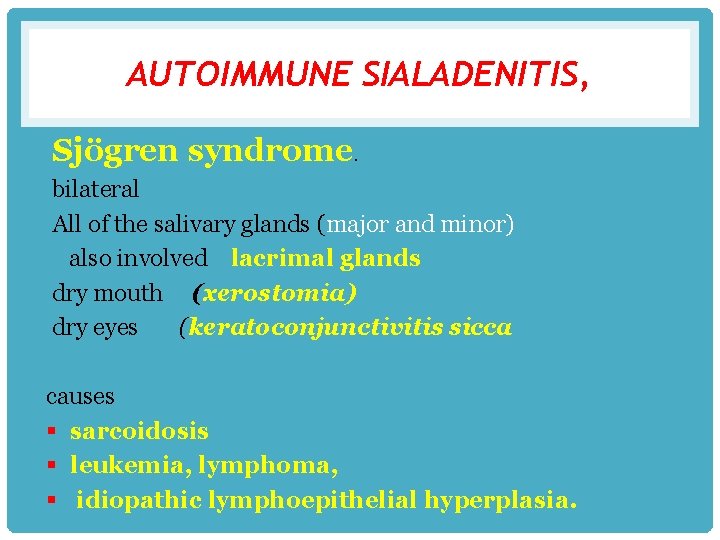
AUTOIMMUNE SIALADENITIS, Sjögren syndrome. bilateral All of the salivary glands (major and minor) also involved lacrimal glands dry mouth (xerostomia) dry eyes (keratoconjunctivitis sicca causes § sarcoidosis § leukemia, lymphoma, § idiopathic lymphoepithelial hyperplasia.
SJÖGREN SYNDROME: CLINICAL FEATURES • Two forms of Sjögren syndrome are recognized: • Primary (sicca syndrome sicca means dry (dry eyes and dry mouth • no other autoimmune disorder) Secondary where the patient manifest dry eyes and mouth plus, associated autoimmune disease such as (rheumatoid arthritis SLE, scleroderma)
CLINICAL FEATURES • The swelling may be painful or slightly tender • . • The patient may have dry skin and nasal and vaginal dryness • Fatigue and depressed. • sialography often reveals punctate sialectasia with a • “fruit-laden, branchless tree” pattern.
XEROSTOMIA: CLINICAL FEATURES q. Mastication and swallowing may be difficult. q. The incidence of oral candidiasis increases q dental decay especially cervical and root caries “radiation” caries (xerostomia-related caries).


• Salivary gland tumours
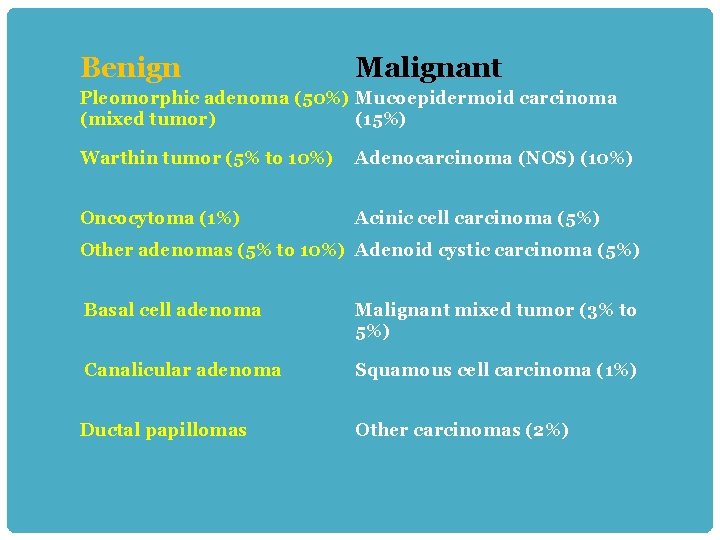
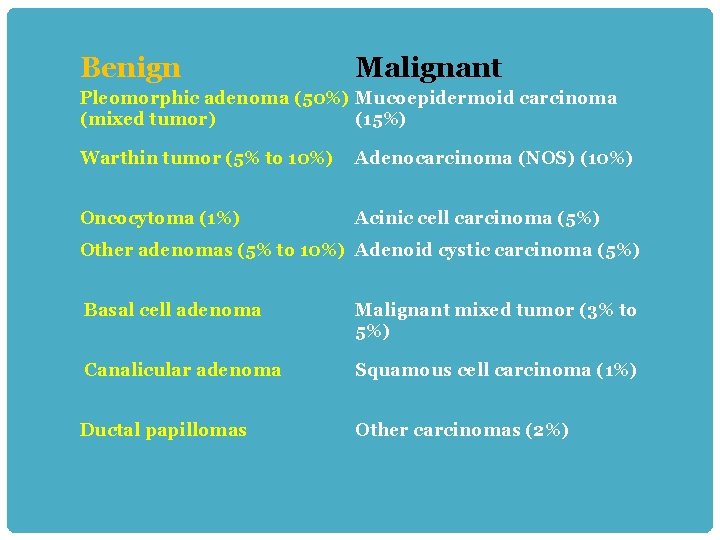
Benign Malignant Pleomorphic adenoma (50%) Mucoepidermoid carcinoma (mixed tumor) (15%) Warthin tumor (5% to 10%) Adenocarcinoma (NOS) (10%) Oncocytoma (1%) Acinic cell carcinoma (5%) Other adenomas (5% to 10%) Adenoid cystic carcinoma (5%) Basal cell adenoma Malignant mixed tumor (3% to 5%) Canalicular adenoma Squamous cell carcinoma (1%) Ductal papillomas Other carcinomas (2%)
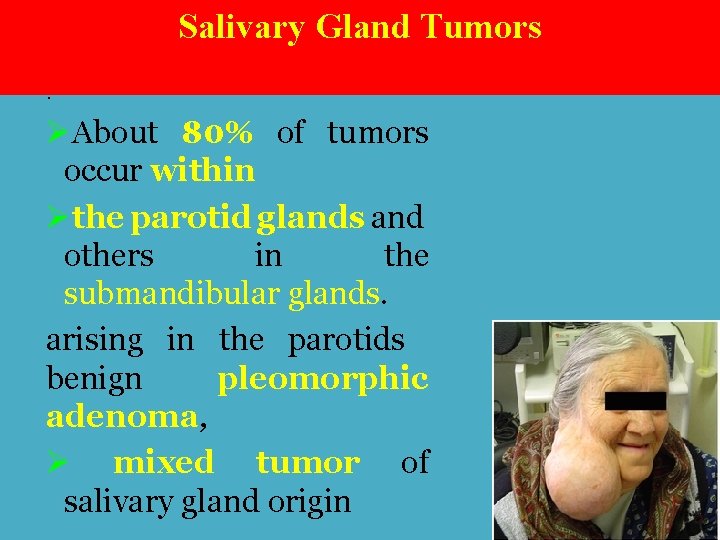
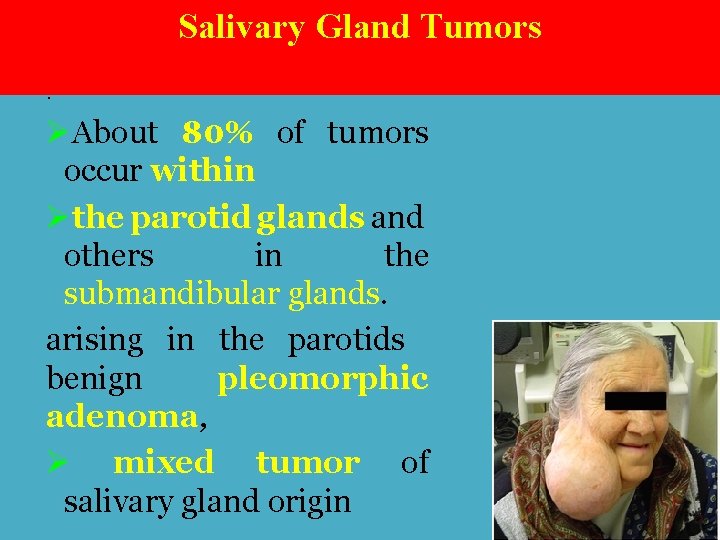
Salivary Gland Tumors. ØAbout 80% of tumors occur within Øthe parotid glands and others in the submandibular glands. arising in the parotids benign pleomorphic adenoma, Ø mixed tumor of salivary gland origin
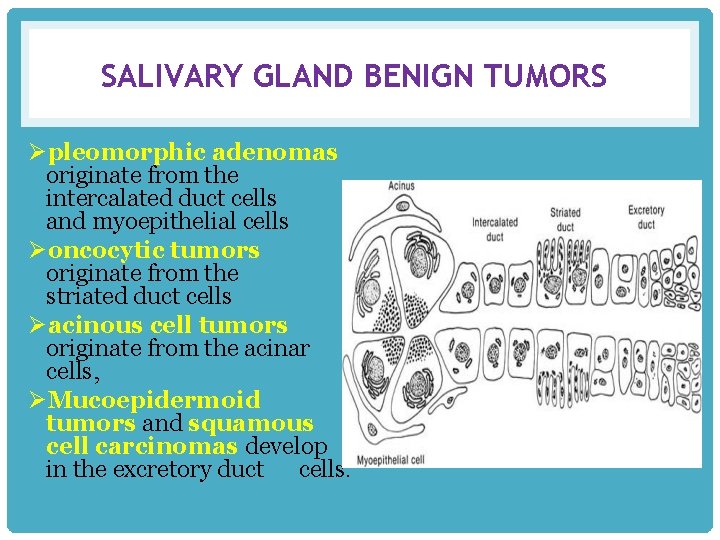
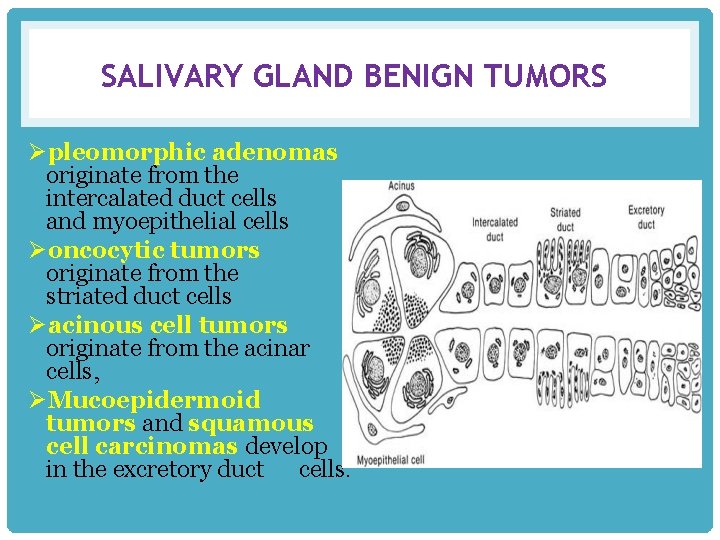
SALIVARY GLAND BENIGN TUMORS Øpleomorphic adenomas originate from the intercalated duct cells and myoepithelial cells Øoncocytic tumors originate from the striated duct cells Øacinous cell tumors originate from the acinar cells, ØMucoepidermoid tumors and squamous cell carcinomas develop in the excretory duct cells.
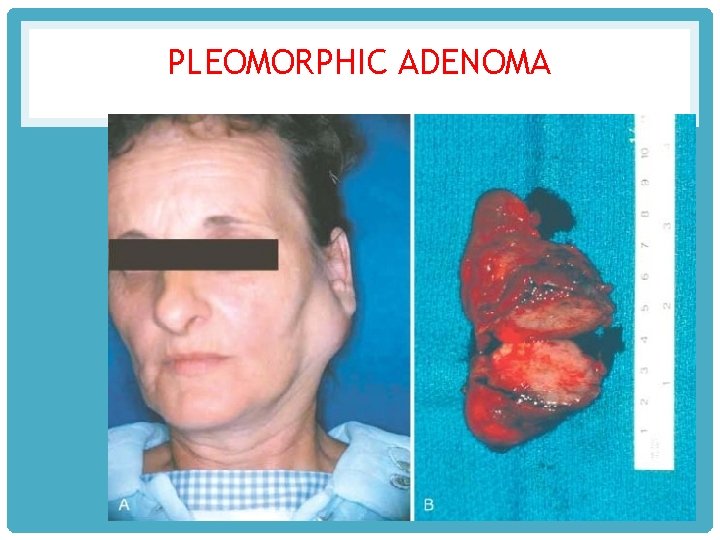
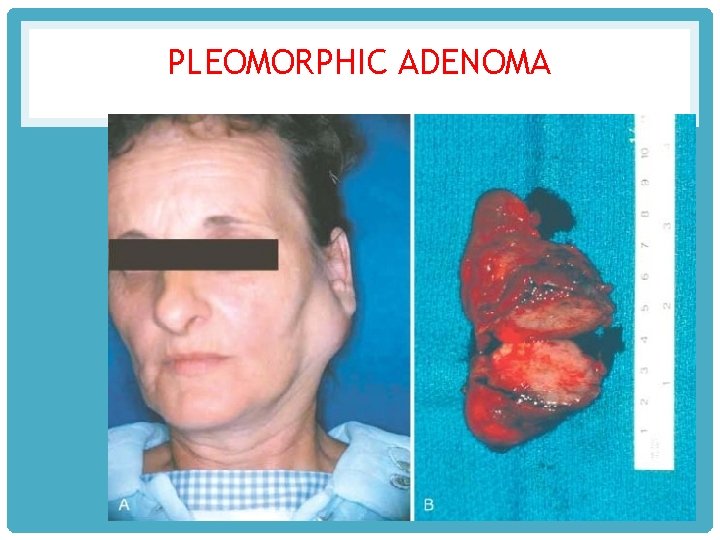
PLEOMORPHIC ADENOMA
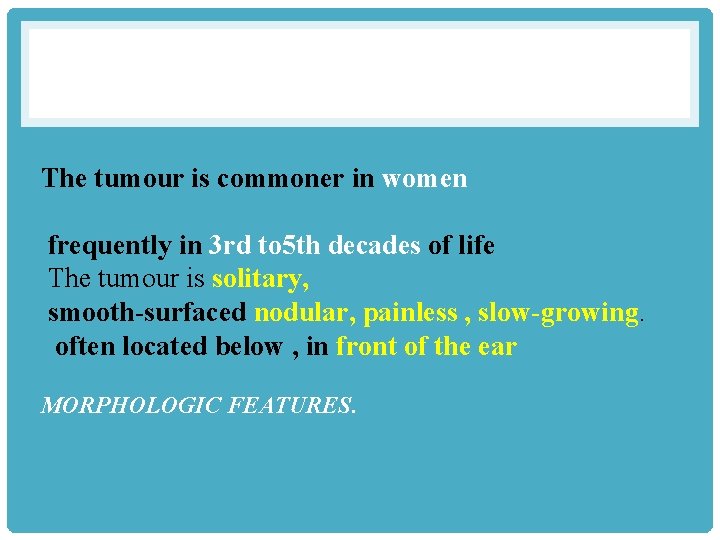
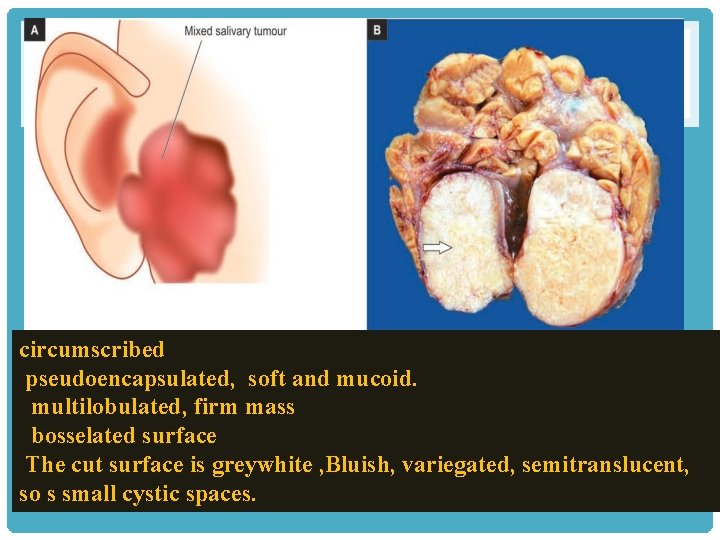
The tumour is commoner in women frequently in 3 rd to 5 th decades of life The tumour is solitary, smooth-surfaced nodular, painless , slow-growing. often located below , in front of the ear MORPHOLOGIC FEATURES.
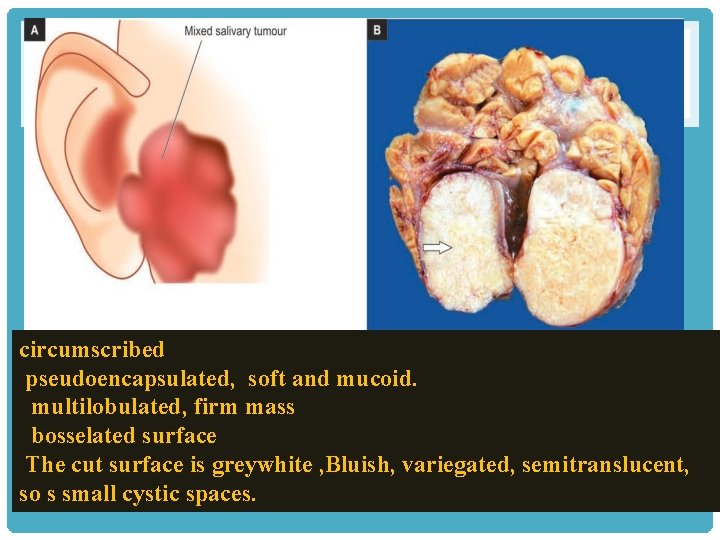
circumscribed pseudoencapsulated, soft and mucoid. multilobulated, firm mass bosselated surface The cut surface is greywhite , Bluish, variegated, semitranslucent, so s small cystic spaces.
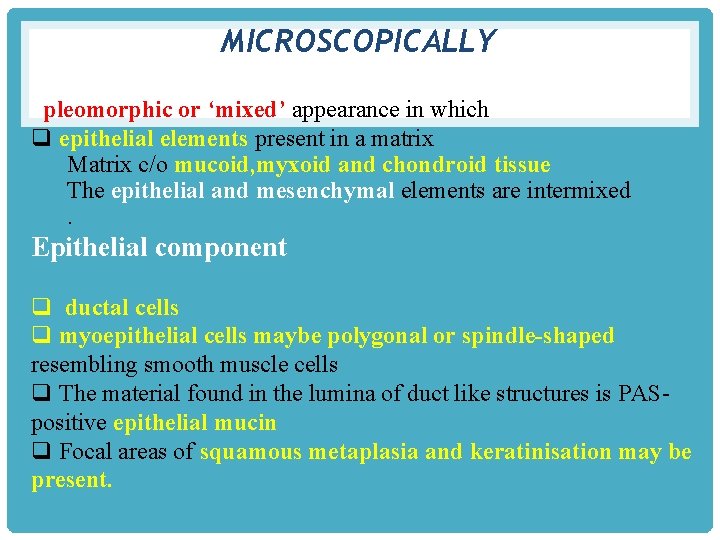
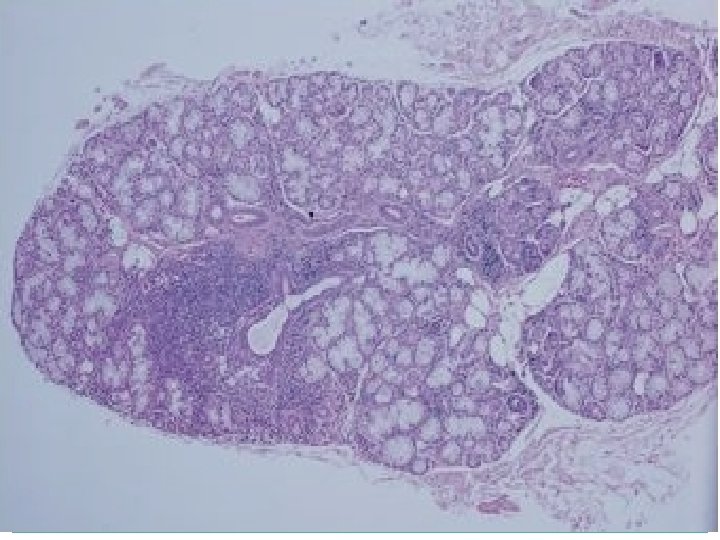
MICROSCOPICALLY pleomorphic or ‘mixed’ appearance in which q epithelial elements present in a matrix Matrix c/o mucoid, myxoid and chondroid tissue The epithelial and mesenchymal elements are intermixed. Epithelial component q ductal cells q myoepithelial cells maybe polygonal or spindle-shaped resembling smooth muscle cells q The material found in the lumina of duct like structures is PASpositive epithelial mucin q Focal areas of squamous metaplasia and keratinisation may be present.
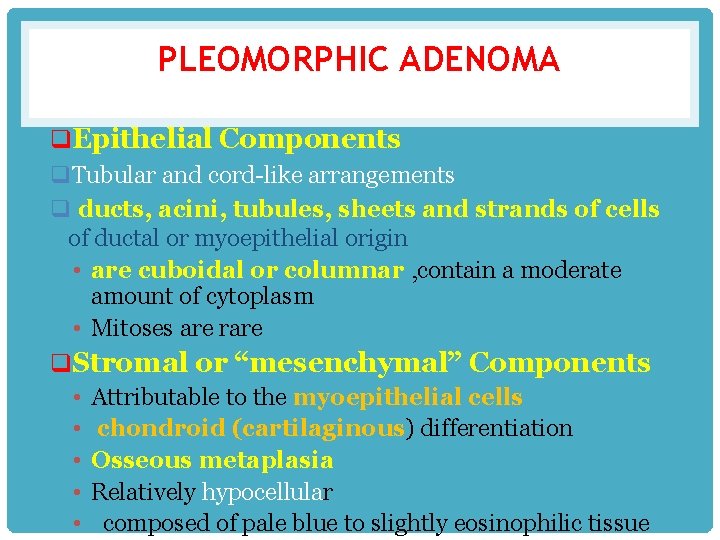
PLEOMORPHIC ADENOMA q. Epithelial Components q. Tubular and cord-like arrangements q ducts, acini, tubules, sheets and strands of cells of ductal or myoepithelial origin • are cuboidal or columnar , contain a moderate amount of cytoplasm • Mitoses are rare q. Stromal or “mesenchymal” Components • Attributable to the myoepithelial cells • chondroid (cartilaginous) differentiation • Osseous metaplasia • Relatively hypocellular • composed of pale blue to slightly eosinophilic tissue
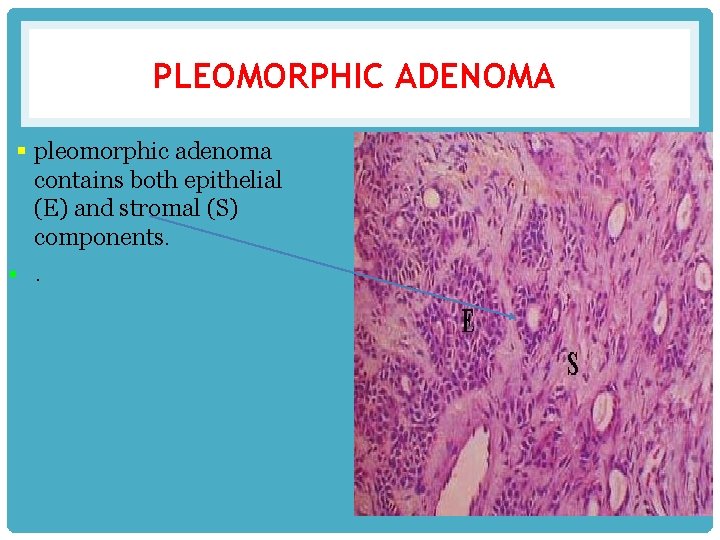
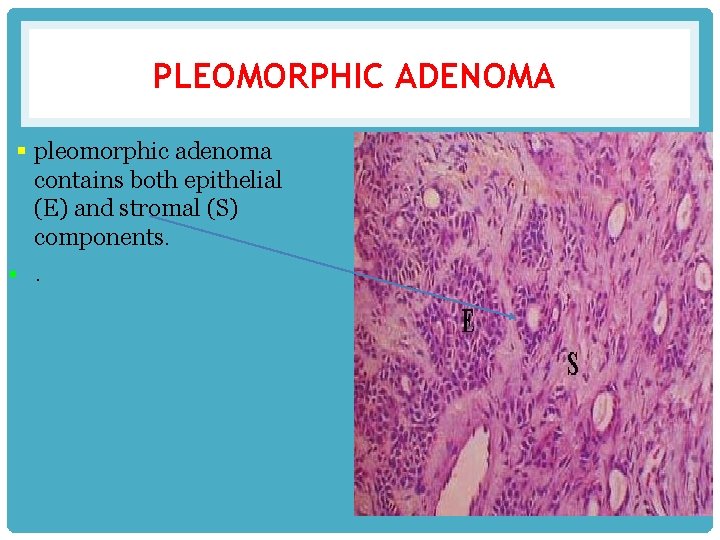
PLEOMORPHIC ADENOMA § pleomorphic adenoma contains both epithelial (E) and stromal (S) components. §.
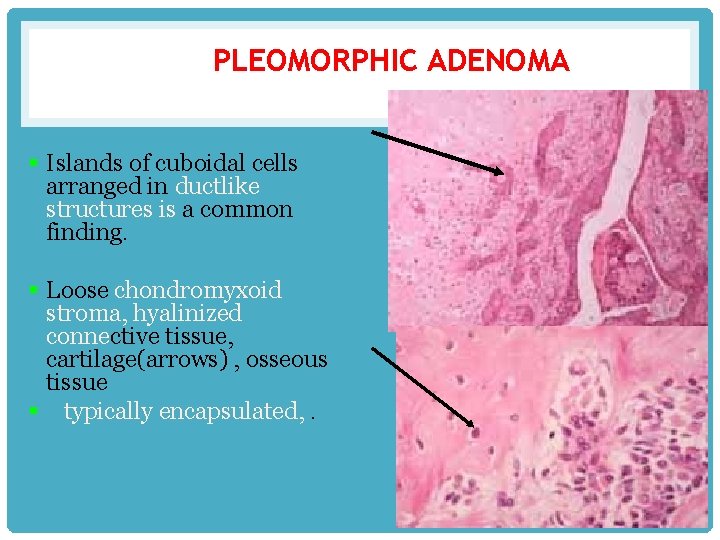
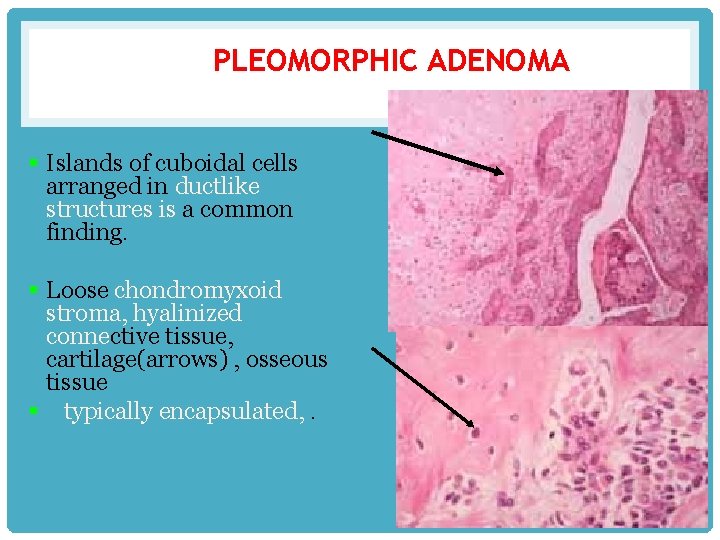
PLEOMORPHIC ADENOMA § Islands of cuboidal cells arranged in ductlike structures is a common finding. § Loose chondromyxoid stroma, hyalinized connective tissue, cartilage(arrows) , osseous tissue § typically encapsulated, .
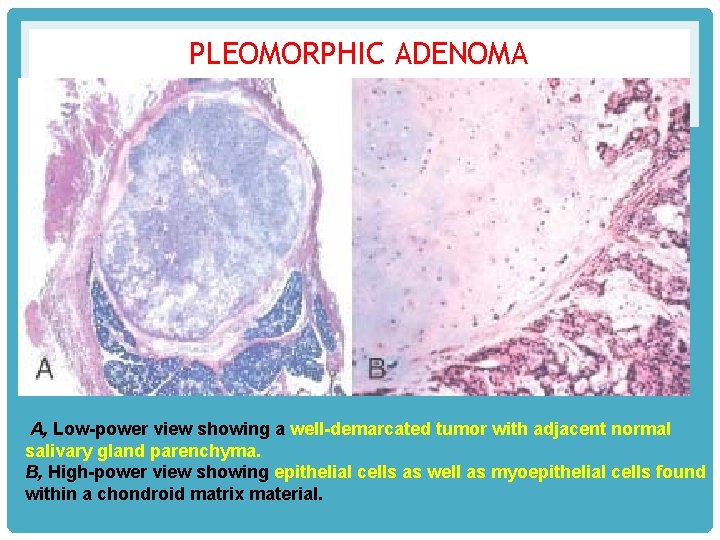
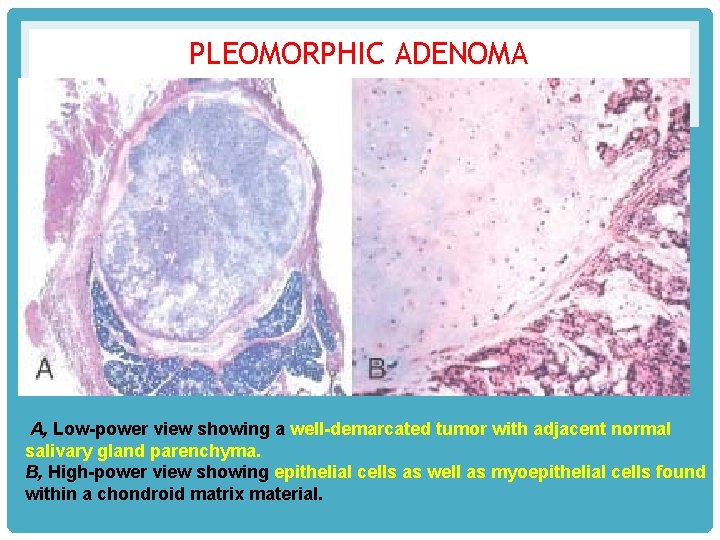
PLEOMORPHIC ADENOMA A, Low-power view showing a well-demarcated tumor with adjacent normal salivary gland parenchyma. B, High-power view showing epithelial cells as well as myoepithelial cells found within a chondroid matrix material.
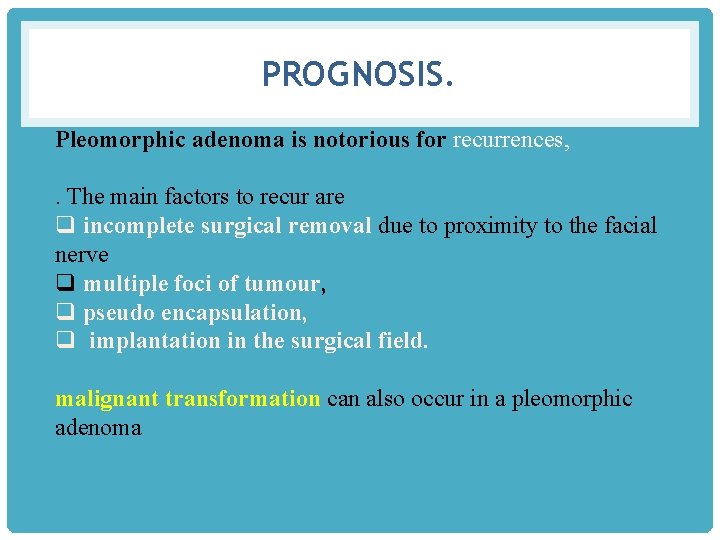
PROGNOSIS. Pleomorphic adenoma is notorious for recurrences, . The main factors to recur are q incomplete surgical removal due to proximity to the facial nerve q multiple foci of tumour, q pseudo encapsulation, q implantation in the surgical field. malignant transformation can also occur in a pleomorphic adenoma
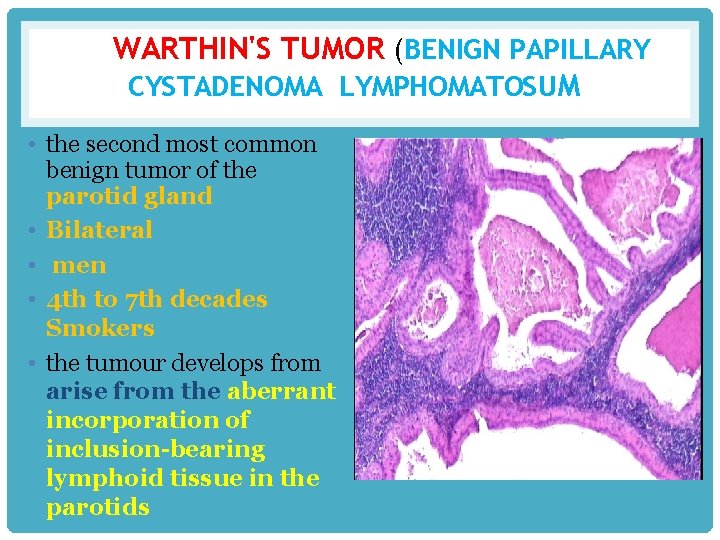
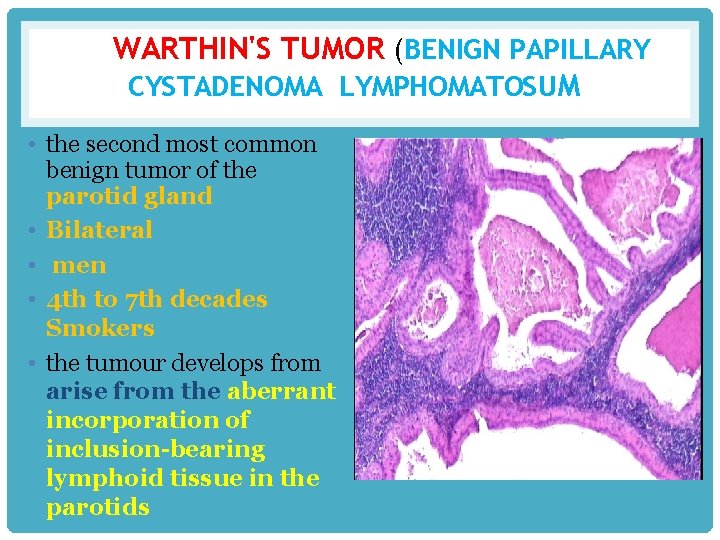
WARTHIN'S TUMOR (BENIGN PAPILLARY CYSTADENOMA LYMPHOMATOSUM • the second most common benign tumor of the parotid gland • Bilateral • men • 4 th to 7 th decades Smokers • the tumour develops from arise from the aberrant incorporation of inclusion-bearing lymphoid tissue in the parotids
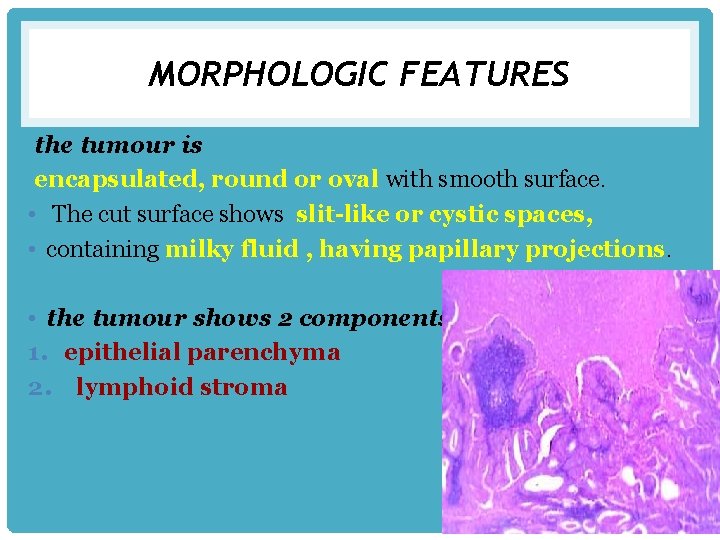
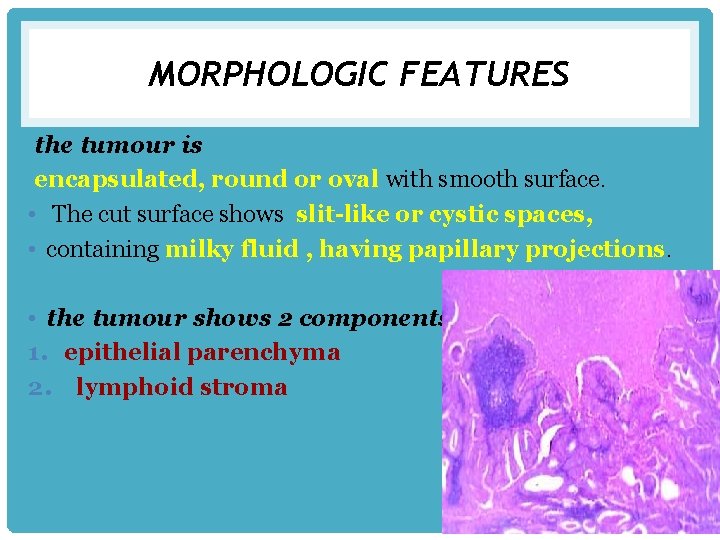
MORPHOLOGIC FEATURES the tumour is encapsulated, round or oval with smooth surface. • The cut surface shows slit-like or cystic spaces, • containing milky fluid , having papillary projections. • the tumour shows 2 components: 1. epithelial parenchyma 2. lymphoid stroma
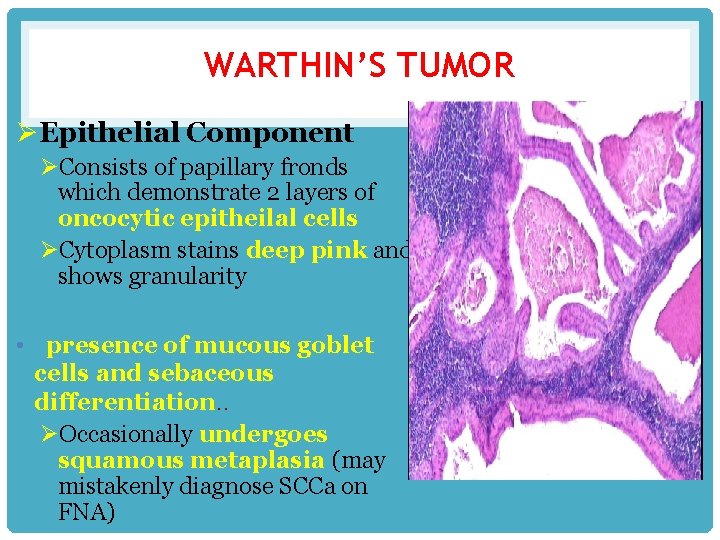
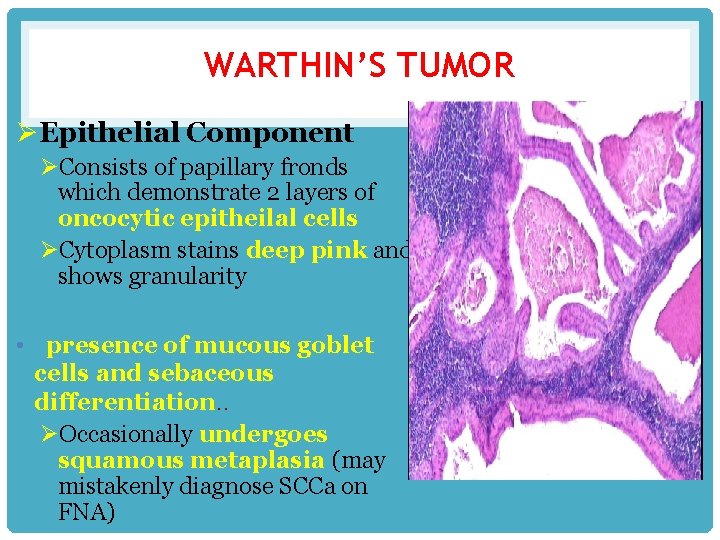
WARTHIN’S TUMOR ØEpithelial Component ØConsists of papillary fronds which demonstrate 2 layers of oncocytic epitheilal cells ØCytoplasm stains deep pink and shows granularity • presence of mucous goblet cells and sebaceous differentiation. . ØOccasionally undergoes squamous metaplasia (may mistakenly diagnose SCCa on FNA)
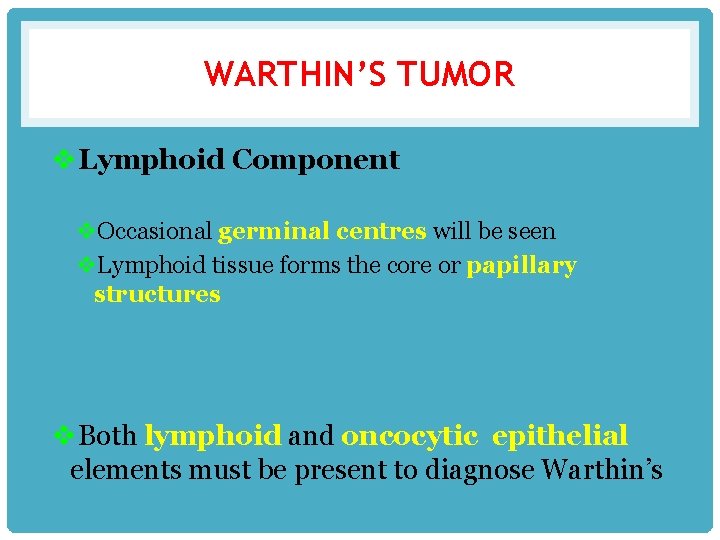
WARTHIN’S TUMOR v. Lymphoid Component v. Occasional germinal centres will be seen v. Lymphoid tissue forms the core or papillary structures v. Both lymphoid and oncocytic epithelial elements must be present to diagnose Warthin’s
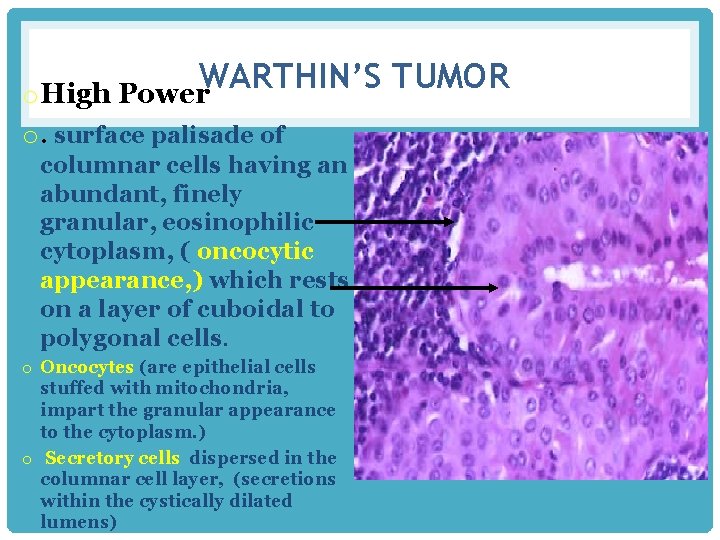
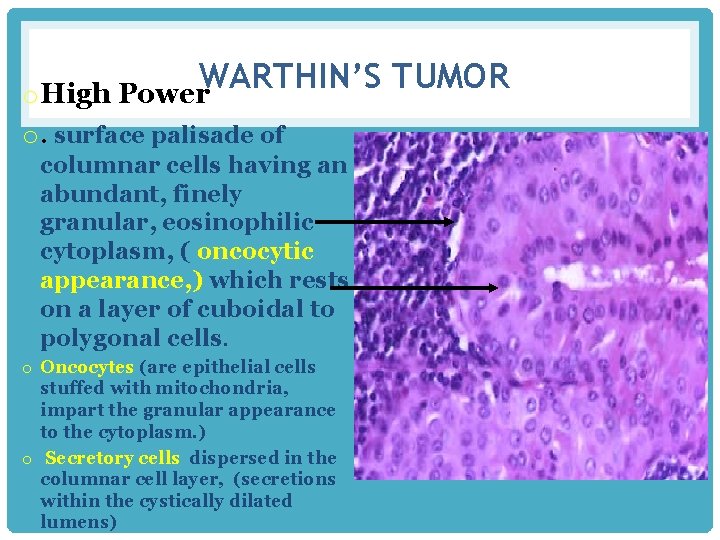
WARTHIN’S TUMOR o High Power o. surface palisade of columnar cells having an abundant, finely granular, eosinophilic cytoplasm, ( oncocytic appearance, ) which rests on a layer of cuboidal to polygonal cells. o Oncocytes (are epithelial cells stuffed with mitochondria, impart the granular appearance to the cytoplasm. ) o Secretory cells dispersed in the columnar cell layer, (secretions within the cystically dilated lumens)
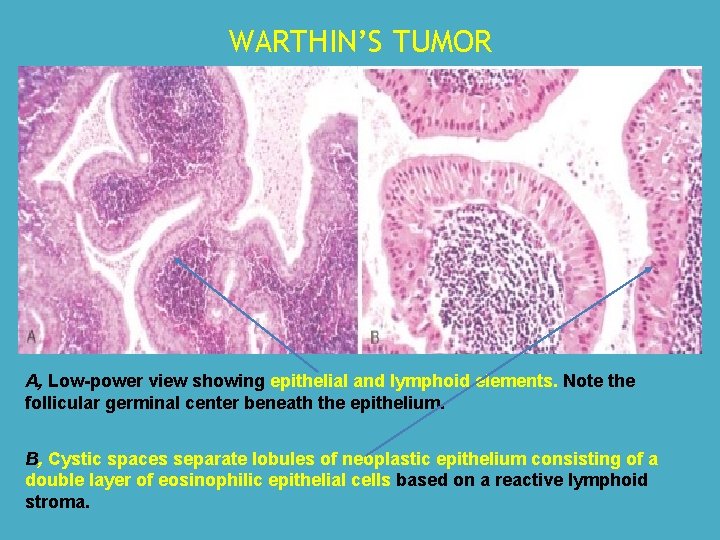
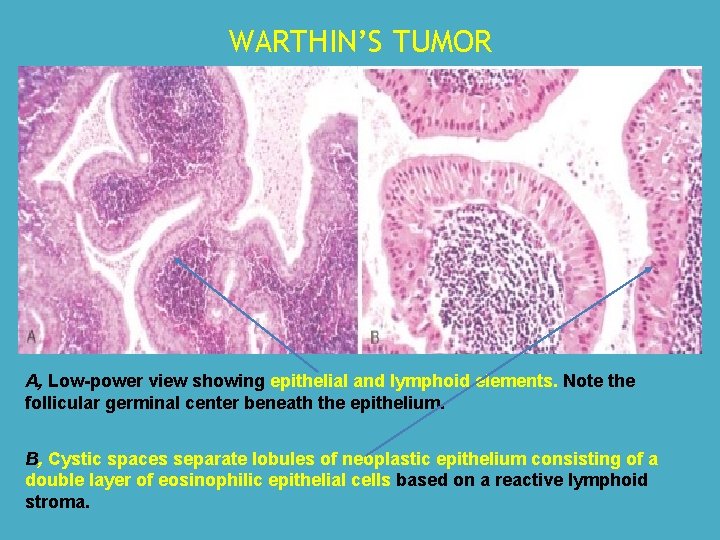
WARTHIN’S TUMOR A, Low-power view showing epithelial and lymphoid elements. Note the follicular germinal center beneath the epithelium. B, Cystic spaces separate lobules of neoplastic epithelium consisting of a double layer of eosinophilic epithelial cells based on a reactive lymphoid stroma.
MONOMORPHIC ADENOMA ØSimilar to Pleomorphic Adenoma except no mesenchymal stromal component • Predominantly an epithelial component ØMore common in minor salivary glands (upper lip) Ø 12% bilateral ØRare malignant potential ØTypes: • • • Basal Cell Adenoma Canicular Adenoma Myoepithelioma Adenoma Clear Cell Adenoma Membranous Adenoma Glycogen-Rich Adenoma
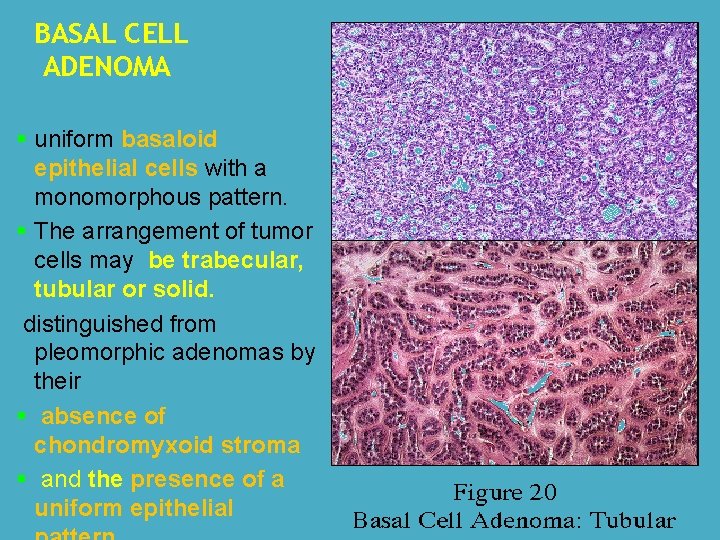
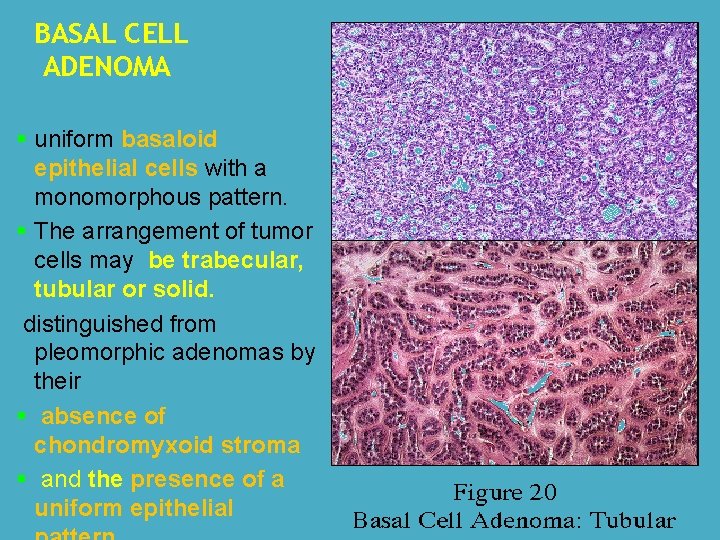
BASAL CELL ADENOMA § uniform basaloid epithelial cells with a monomorphous pattern. § The arrangement of tumor cells may be trabecular, tubular or solid. distinguished from pleomorphic adenomas by their § absence of chondromyxoid stroma § and the presence of a uniform epithelial
MALIGNANT SALIVARY GLAND TUMORS
MUCOEPIDERMOID CARCINOMA Mucoepidermoid carcinoma (MEC) 1. most common malignant tumor of the parotid gland 2. second-most common malignancy (adenoid cystic carcinoma is more common) of the submandibular and minor salivary glands 3. most common malignant salivary gland tumour in children and adolescents. 4 most common example of radiationinduced malignant tumour.

MOST COMMON SITES. The major salivary glands -----parotid gland minor salivary glands ----- palate Common age group ---- 30 -60 years.
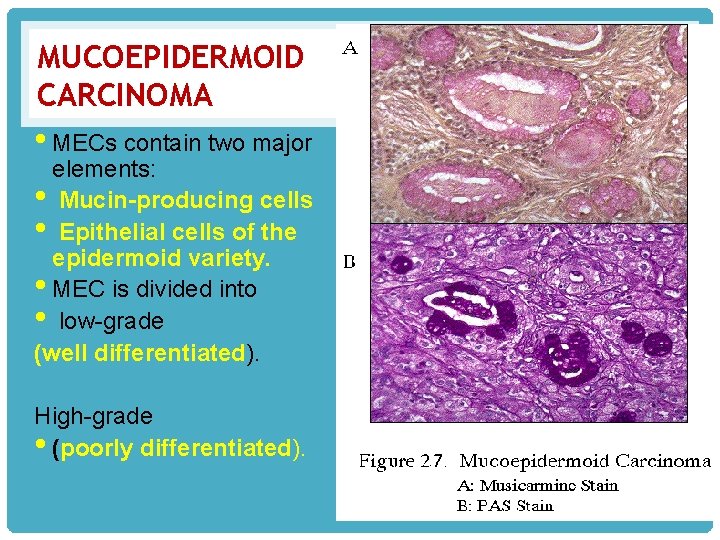
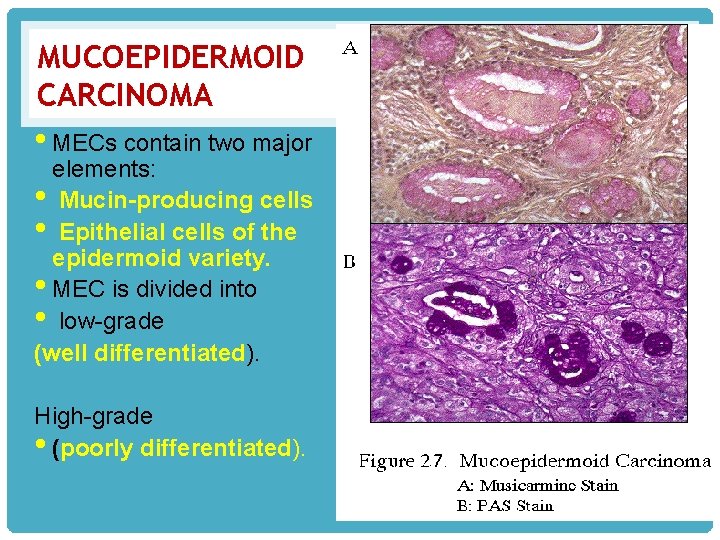
MUCOEPIDERMOID CARCINOMA • MECs contain two major elements: • Mucin-producing cells • Epithelial cells of the epidermoid variety. • MEC is divided into • low-grade (well differentiated). High-grade • (poorly differentiated).
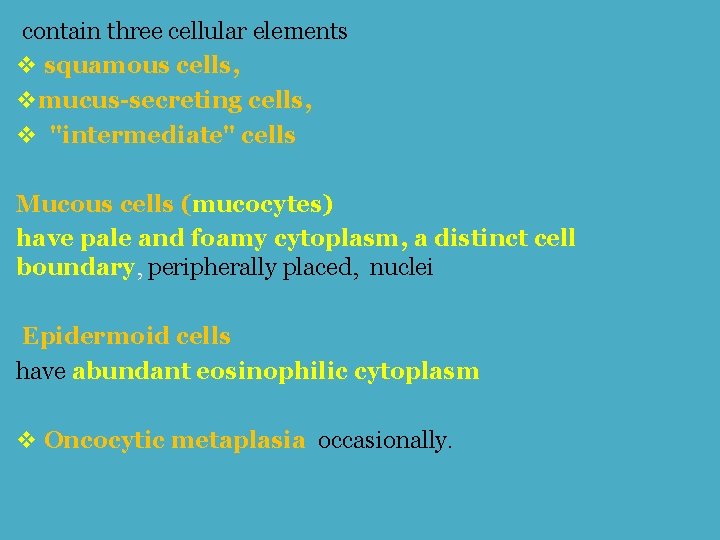
contain three cellular elements v squamous cells, vmucus-secreting cells, v "intermediate" cells Mucous cells (mucocytes) have pale and foamy cytoplasm, a distinct cell boundary, peripherally placed, nuclei Epidermoid cells have abundant eosinophilic cytoplasm v Oncocytic metaplasia occasionally.

MUCOEPIDERMOID CARCINOMA A, Mucoepidermoid carcinoma showing islands having squamous cells as well as clear cells containing mucin. B, Mucicarmine stains the mucin reddish-pink.
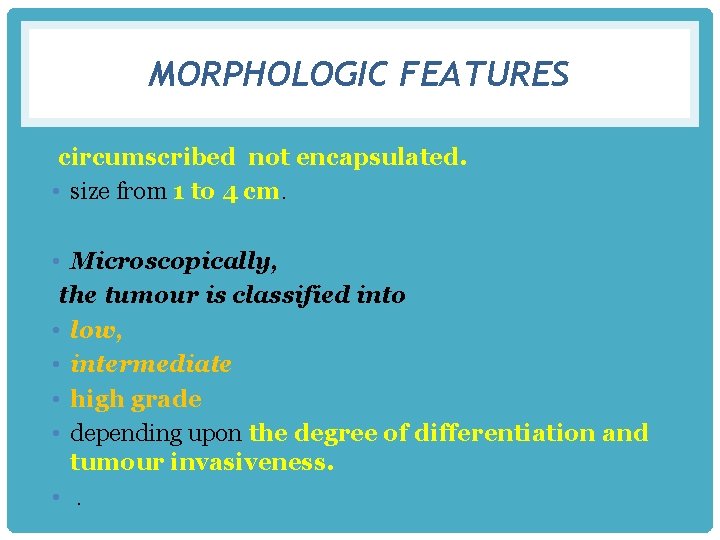
MORPHOLOGIC FEATURES circumscribed not encapsulated. • size from 1 to 4 cm. • Microscopically, the tumour is classified into • low, • intermediate • high grade • depending upon the degree of differentiation and tumour invasiveness. • .
• Well differentiated tumours • predominance of mucinous cells, • poorly differentiated have more solid and infiltrative pattern
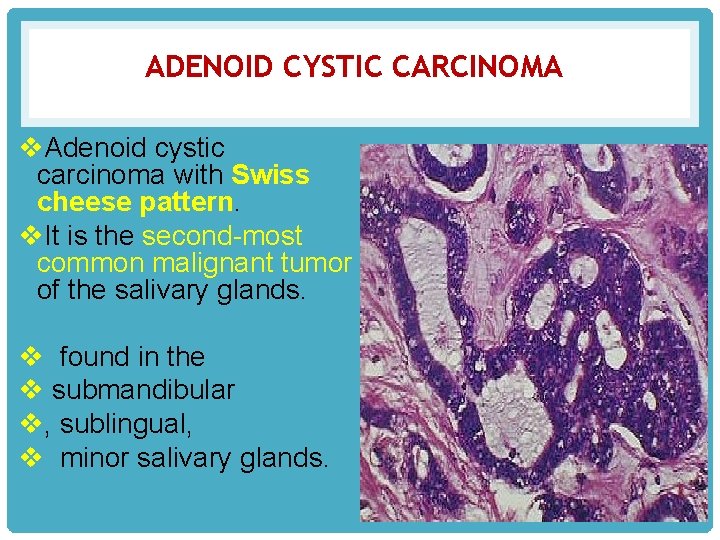
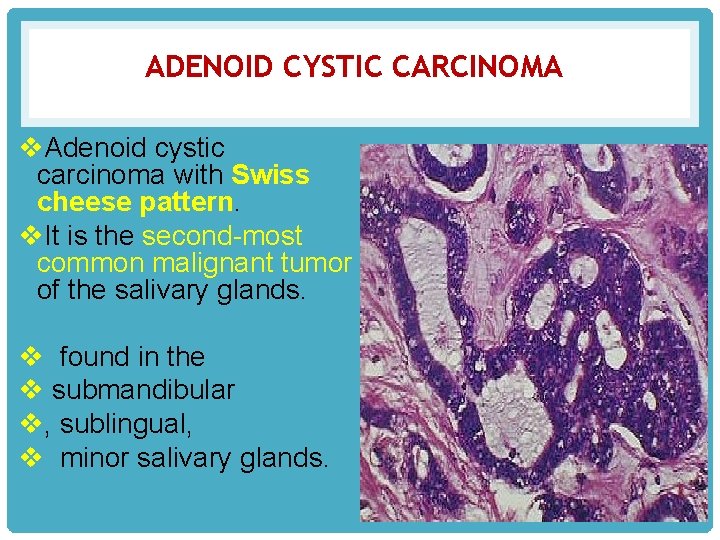
ADENOID CYSTIC CARCINOMA v. Adenoid cystic carcinoma with Swiss cheese pattern. v. It is the second-most common malignant tumor of the salivary glands. v found in the v submandibular v, sublingual, v minor salivary glands.

• Adenoid Cystic Carcinoma (Cylindroma) • • highly malignant tumour • typical infiltrative nature, along the nerve sheaths. • cribriform appearance i. e. • the epithelial tumour cells of duct-lining and myoepithelial cells are arranged in duct-like structures or • masses of cells, • having typical fenestrations or cyst-like spaces and hence the name ‘adenoid cystic’. • These cystic spaces contain PAS-positive basophilic material
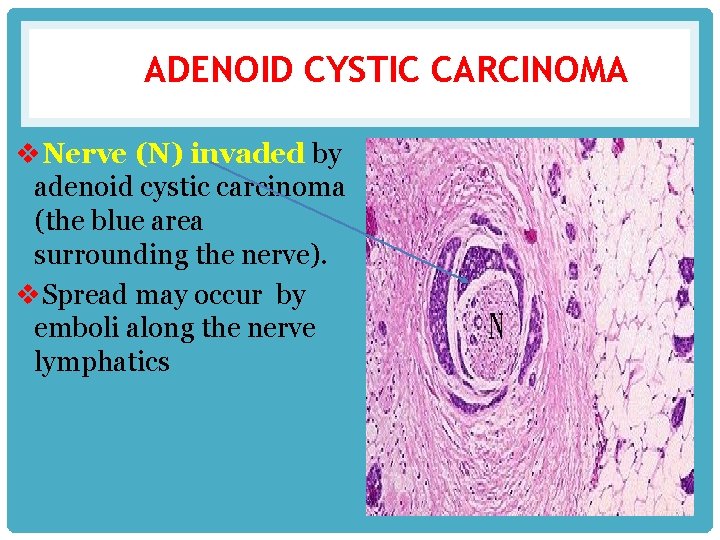
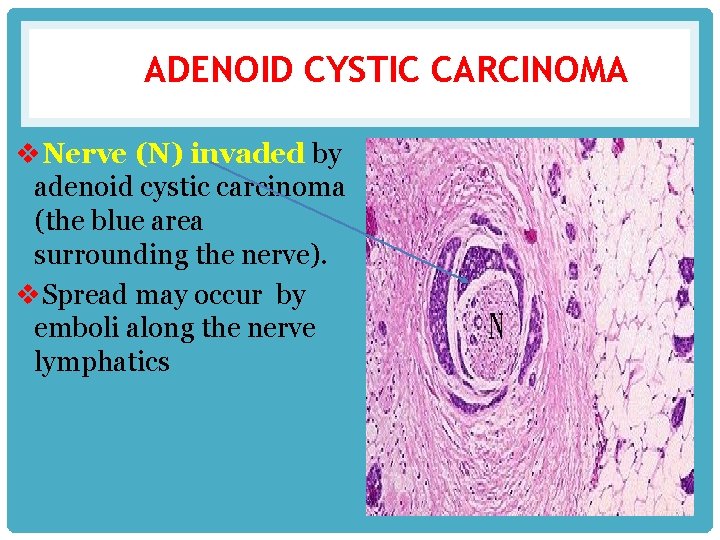
ADENOID CYSTIC CARCINOMA v. Nerve (N) invaded by adenoid cystic carcinoma (the blue area surrounding the nerve). v. Spread may occur by emboli along the nerve lymphatics
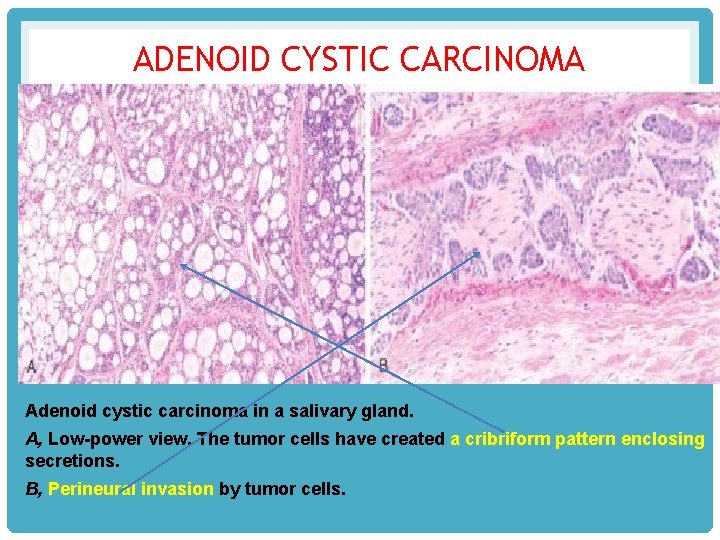
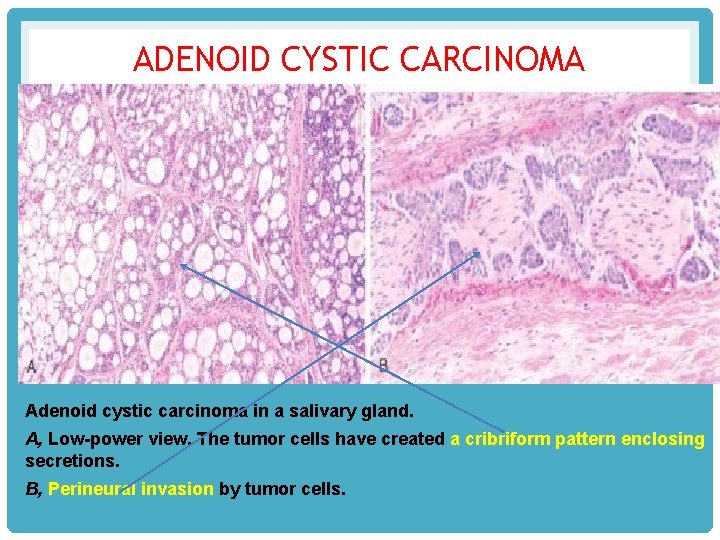
ADENOID CYSTIC CARCINOMA Adenoid cystic carcinoma in a salivary gland. A, Low-power view. The tumor cells have created a cribriform pattern enclosing secretions. B, Perineural invasion by tumor cells.
 Mikael ferm
Mikael ferm Nie wiem association
Nie wiem association Glands of weber
Glands of weber Minor salivary glands
Minor salivary glands Minor salivary glands
Minor salivary glands Ts of liver
Ts of liver Gruczoł
Gruczoł Gall bladder function
Gall bladder function Submandibular gland excision
Submandibular gland excision Testing cranial nerves
Testing cranial nerves Incision for parotid abscess
Incision for parotid abscess Saliva formation
Saliva formation Minor salivary glands
Minor salivary glands Submandibular gland excision
Submandibular gland excision Pseudostratified columnar epithelium
Pseudostratified columnar epithelium Basal cell adenoma
Basal cell adenoma Function of bile
Function of bile Salivary gland disease classification
Salivary gland disease classification Oncocytoma salivary gland
Oncocytoma salivary gland Nasal concha cadaver
Nasal concha cadaver Salivary gland tumor
Salivary gland tumor Sublingua;
Sublingua; Cylindroma slideshare
Cylindroma slideshare Party wall appearance seen in
Party wall appearance seen in Crypts of lieberkuhn
Crypts of lieberkuhn Oncocytoma salivary gland
Oncocytoma salivary gland Oncocytoma salivary gland
Oncocytoma salivary gland Simple acinar gland histology
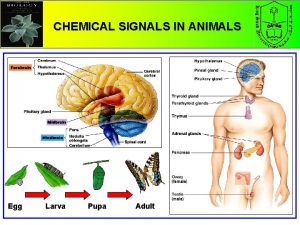
Simple acinar gland histology Pineal gland pituitary gland
Pineal gland pituitary gland Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Salivary amylase digestion of starch
Salivary amylase digestion of starch Dentocult lb test
Dentocult lb test Dentobuff test
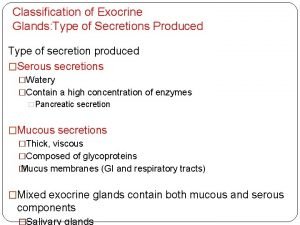
Dentobuff test Classification of exocrine glands
Classification of exocrine glands Whats the difference between endocrine and exocrine glands
Whats the difference between endocrine and exocrine glands Glands secrete what in reflex actions
Glands secrete what in reflex actions Merocrine glands
Merocrine glands Where is the sperm produced
Where is the sperm produced Labia minora glands
Labia minora glands Endocrine system
Endocrine system Spermatocytogenesis
Spermatocytogenesis Exocrine glands
Exocrine glands Stratum basale
Stratum basale Pea size glands flanking the vagina
Pea size glands flanking the vagina Endocrine glands
Endocrine glands Rat internal organs
Rat internal organs Follicular adenoma
Follicular adenoma Ptostate gland
Ptostate gland Human body systems images
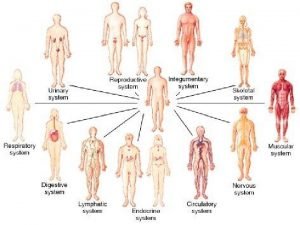
Human body systems images Thyroid
Thyroid Endocrine glands secrete
Endocrine glands secrete Gastric glands
Gastric glands Gastric gland
Gastric gland The only example of unicellular exocrine glands are
The only example of unicellular exocrine glands are Hypothal
Hypothal Exocrine glands
Exocrine glands The purified lymph with lymphocytes and antibodies added
The purified lymph with lymphocytes and antibodies added