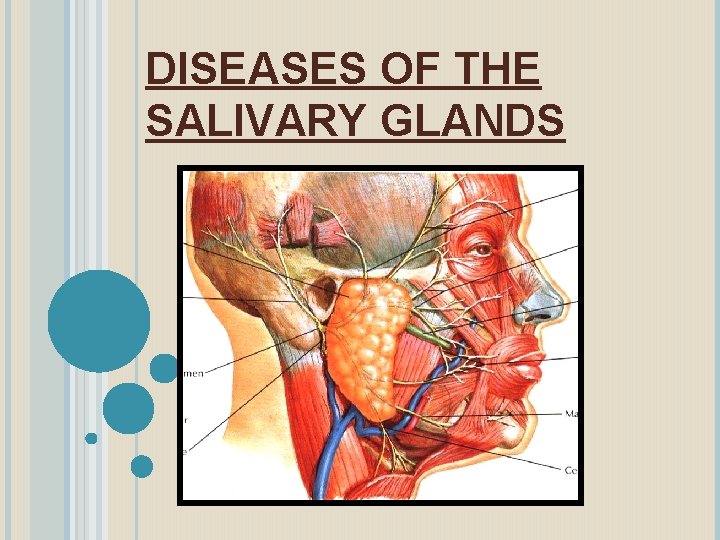
DISEASES OF THE SALIVARY GLANDS THE SALIVARY GLANDS



















- Slides: 95
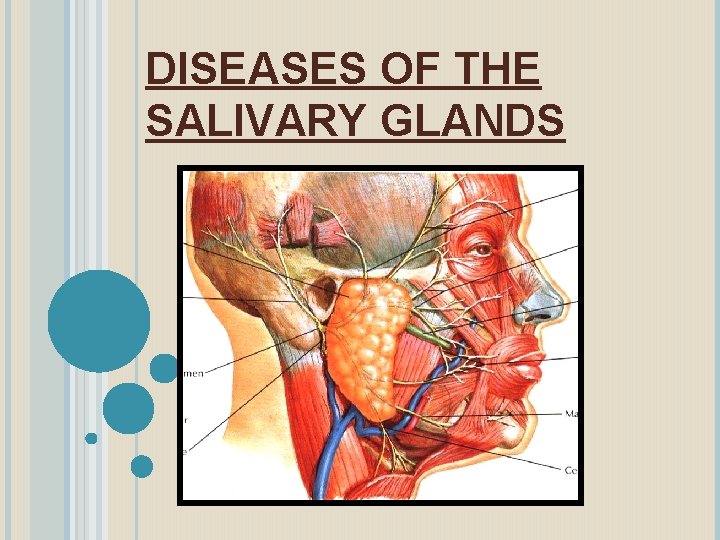
DISEASES OF THE SALIVARY GLANDS
THE SALIVARY GLANDS May be classified as Major and Minor glands. Major glands are paired glands. They are: (i) Parotid (ii) Sub-mandibular and (iii) Sub-lingual glands. There are numerous minor salivary glands which are widely distributed in the oral cavity.
BASED ON THE TYPE OF SECRETION Salivary glands may be grouped as: (i) Serous, (ii) Mucous and (iii) Mixed. Parotid gland secretion is serous in nature, The sublingual secretes both serous and mucous but predominantly mucous Submandibular secretion is also mixed with predominantly serous. The minor glands secrete mucous saliva.
CLASSIFICATION OF SALIVARY GLAND DISEASES I. DEVELOPMENTAL Aplasia – Absence of the gland Atresia – Absence of the duct. Aberrancy – Ectopic gland.
II. ENLARGEMENT OF THE GLAND A. Inflammatory � Viral: Mumps, Coxsackie A, CMV, Echovirus, Parainfluenza virus I and Influenza virus. � Bacterial � Allergic � Sarcoidosis � Obstructive
B. Non-inflammatory Autoimmune : Sjogren’s Syndrome & Mickulicz’s disease. Alcoholic cirrhosis Diabetes Mellitus Nutritional Deficiency HIV associated III. CYSTS Extravasation cysts Retention Cysts Ranula
IV. TUMORS OF SALIVARY GLANDS Benign Tumors: Pleomorphic Adenoma Warthin’s Tumor Basal cell adenoma Myoepithelioma Canalicular adenoma Ductal papilloma
Malignant Tumors: Mucoepidermoid carcinoma Adenoid Cystic carcinoma Malignant pleomorphic adenoma Epidermoid carcinoma. V. NECROTIZING SIALO METAPLASIA VI. SALIVARY GLAND DYSFUNCTION Xerostomia Sialorrhoea.
SIALOLITHIASIS Sialolithiasis is the formation of sialolith (salivary calculi, salivary stone) in the salivary duct or the gland resulting in the obstruction of the salivary flow. Sialolith is a calcareous substance, which may form in the parenchyma or the duct of the major or minor salivary glands.
About 90% of the sialoliths is formed in the submandibular gland because the long, curved Wharton’s duct has increased chance of entrapment of organic debris, plus the secretion of this gland is higher in calcium content and thick in consistency and the position of the gland increases the chances for the stagnation of the saliva.
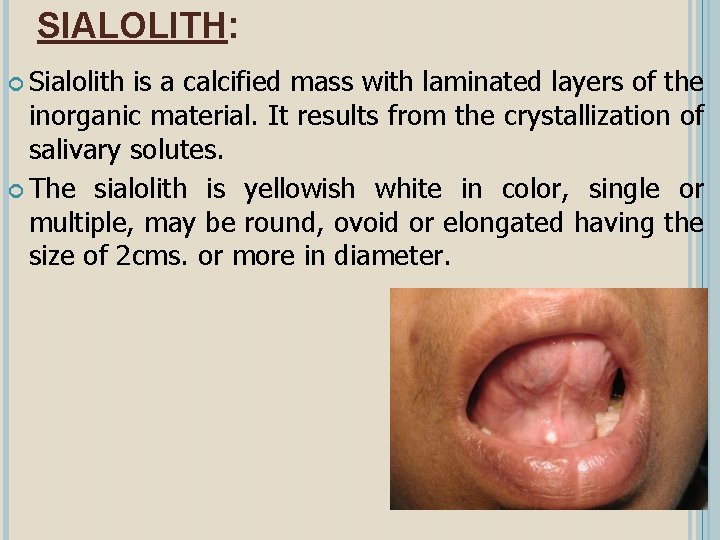
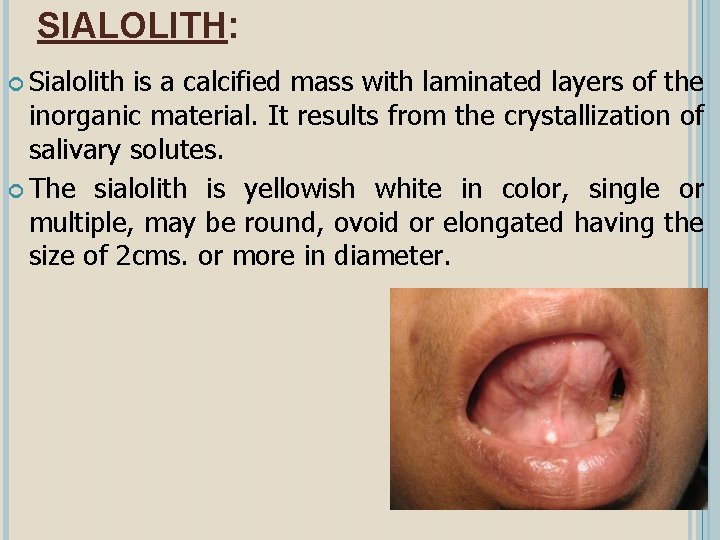
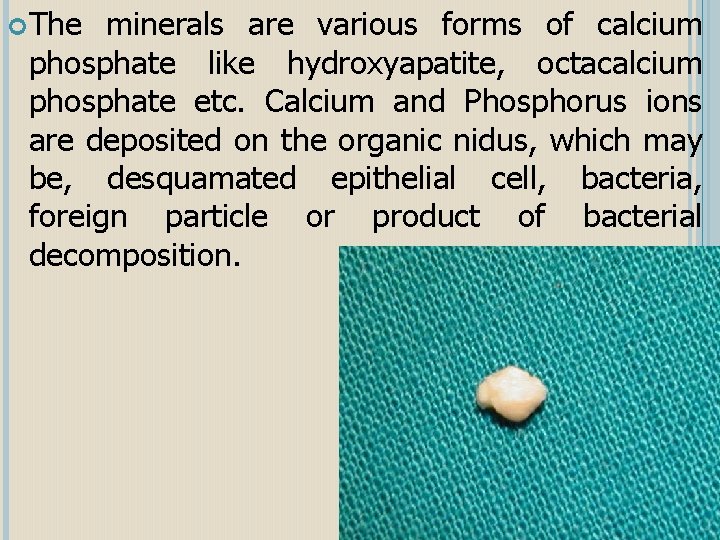
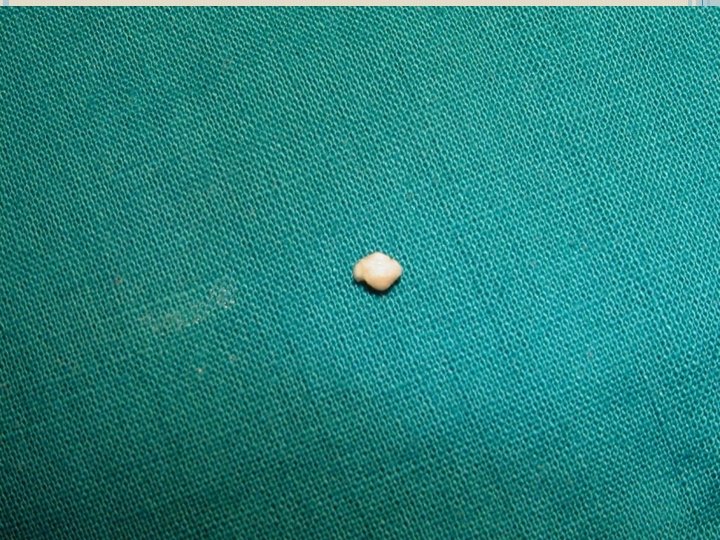
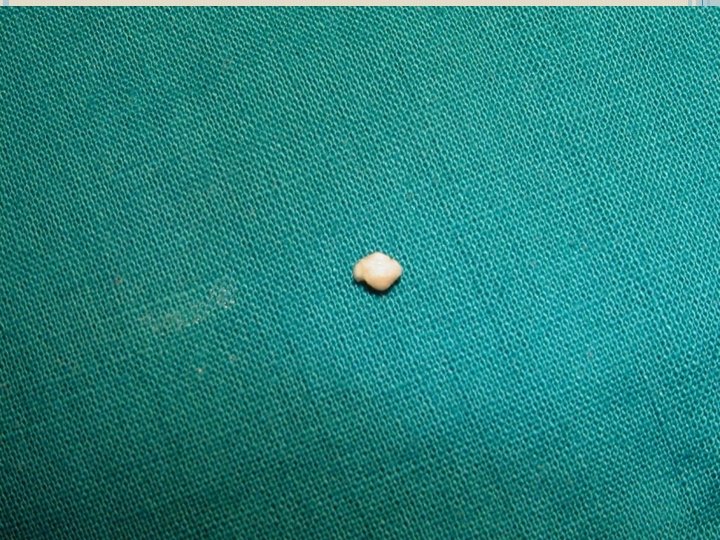
SIALOLITH: Sialolith is a calcified mass with laminated layers of the inorganic material. It results from the crystallization of salivary solutes. The sialolith is yellowish white in color, single or multiple, may be round, ovoid or elongated having the size of 2 cms. or more in diameter.
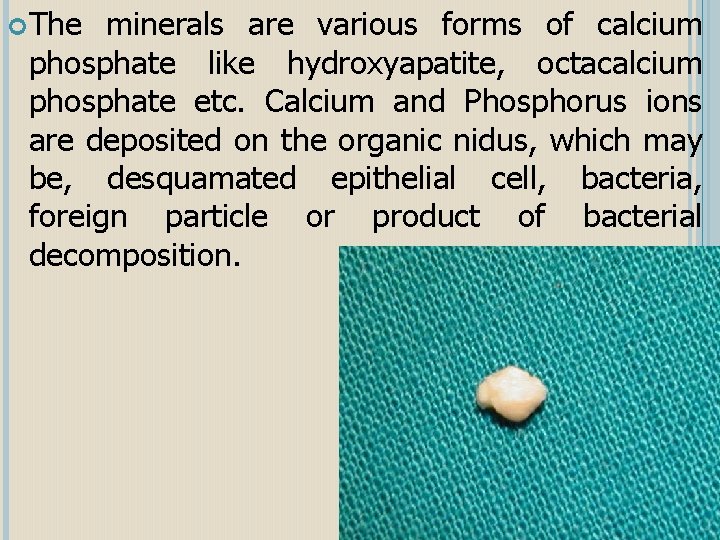
The minerals are various forms of calcium phosphate like hydroxyapatite, octacalcium phosphate etc. Calcium and Phosphorus ions are deposited on the organic nidus, which may be, desquamated epithelial cell, bacteria, foreign particle or product of bacterial decomposition.
CLINICAL FEATURES: Sialolithiasis may occur at any age; common in the middle aged adults. When a duct of the major gland is involved, there is pain with the psychic stimulation of the salivary flow. Patients complain of pain and swelling during and after having the food. The obstruction of the duct by the sialolith causes prevents salivary flow and increase pressure producing the pain. On examination, the stone may be palpated especially if present at the peripheral aspect of the duct.
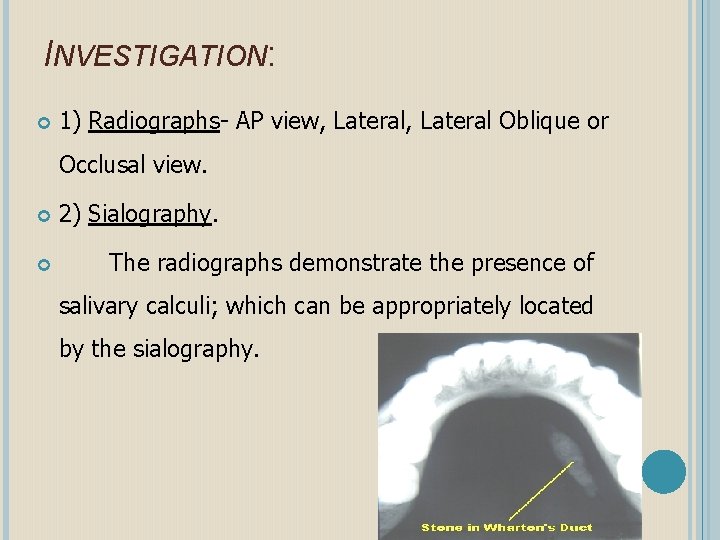
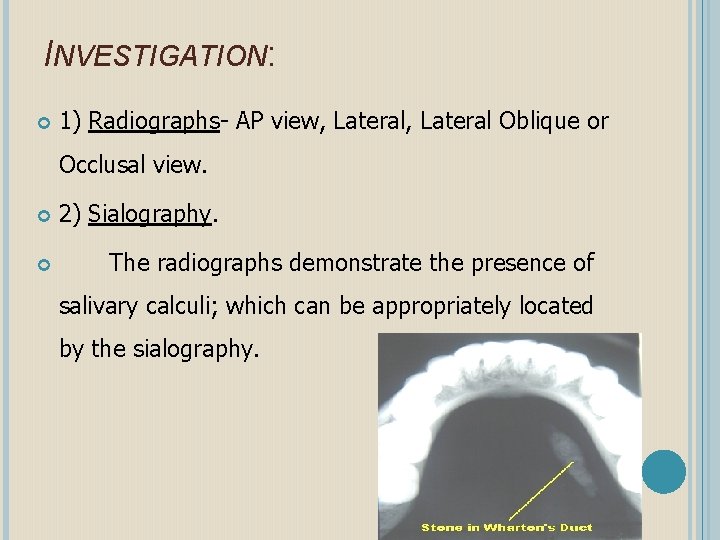
INVESTIGATION: 1) Radiographs- AP view, Lateral Oblique or Occlusal view. 2) Sialography. The radiographs demonstrate the presence of salivary calculi; which can be appropriately located by the sialography.
COMPLICATIONS: 1) Bacterial infection of the gland may result in the obstruction of long duration. 2) Sialoangiectasis: Dilatation of the gland the duct system can happen because of the stasis of the saliva. It may be due to a sialolith, a stricture or chronic infection of the gland. 3) The retention of the saliva may result in the formation of mucoceles especially the mucous retention phenomenon. 4) Rarely, the complete obstruction of the duct may result in the atrophy of the glands.
MANAGEMENT: There are several techniques available for the removal of the sialolith. A suitable procedure is selected depending upon the no. Size, placement of the stone in the duct or the gland, age of the patient etc. The smaller sialoliths, which are located peripherally near the ductal opening may be removed by manipulation. (Called milking the gland)





Larger sialoliths are surgically removed Sometimes, the stones, which are not impacted, may be extracted through the intubation of the duct with fine soft plastic catheter and application of the suction to the tube. Multiple stones or stones near the gland require the removal of the gland.





Some investigators have successfully used modern techniques like Piezo electric shockwave lithotripsy to fragment the salivary stones. The fragments will pass through the duct as the salivary flow is stimulated which can be enhanced by the use of sialogogues.
TRANSORAL SIALOLITHOTOMY OF THE SUBMANDIBULAR DUCT is the best procedure to surgically remove the submandibular duct stones. This procedure can be carried out under local anaesthesia. The exact site of the stone is located by palpation. Following this a suture may be placed behind the stone to prevent its backward movement. The tongue is lifted and held with the help of a gauze. Incision is made in the mucosa parallel to the duct taking care not to injure the structures like the lingual nerve and the sublingual glands
After this , blunt dissection is carried out. The tissues are displaced to locate the duct. Once that part of the duct lodging the stone is identified, a longitudinal incision is made over the stone. The stone is removed using small forceps, in case the stone is large, its crushed with the help of the forceps. Following this a cannula may be passed to aspirate the pieces of stone, mucin etc. The patency of the duct anterior to the surgical area should be ensured by passing a probe. Sutures are placed at the level of the mucosa.
SIALADENITIS: Inflammation of the salivary glands is known as sialadenitis. Viral infections, bacterial infections, allergic reactions and systemic diseases are the major causes for sialadenitis. It may be acute or chronic.
Viral Infections: Mumps (epidemic parotitis) is the most common viral infection affecting the salivary glands; which is caused by a paramyxovirus. It is an acute, contagious disease usually affecting the parotid gland. Occasionally, the submandibular or the sublingual glands may also be involved. This disease is not dangerous, self-limiting one. In these days, the number of cases is reduced because of the Mumps vaccine. It is a disease of the childhood but in case affects the adults leads to greater complications.
CLINICAL FEATURES: Initially, the patient may suffer from mild fever, headache, chills, vomiting etc. followed by pain below the ear and sudden onset of firm rubbery or elastic swelling of the salivary glands, frequently elevating the ear lobe. In viral parotitis, the glands of both the sides enlarge, which may be simultaneous or one following the other in 24 -48 hrs.
There is extruciating ear pain during mastication. Xerostomia, trismus, cervical lymphadenitis, tender glands, edema of the overlying skin may also be present. These symptoms usually last for a week. The disease spreads through droplet dissemination as the virus is present in the saliva. Because of the inflammation of the glands, the salivary flow decreases, the viscosity and turbidity increases which increase the chance of ascending infections.
COMPLICATIONS 1) In adults, this viral disease may lead to the inflammation of gonads and central nervous system resulting in meningitis, encephalitis, orchitis, epididymitis, deafness, myocarditis, thyroiditis, pancreatitis, oophoritis etc. 2) In case of secondary infection leads to bacterial sialdenitis.
INVESTIGATIONS In acute phase, the serum amylase level is increased. Demonstration of the antibodies may confirm the disease. Differential diagnosis: l Because the swelling can be near the angle of the mandible, one should not confuse Mumps for a infectious swelling from lower molars.
MANAGEMENT It is self limiting. Symptomatic relief can be given by the antipyretics; antibiotics can be given to prevent the secondary infections.
BACTERIAL INFECTIONS: Bacterial infections can lead to the inflammation of major salivary glands. Depending on the onset it may be acute or chronic / recurrent. The bacterial sialadenitis affect the parotid glands more commonly, the submandibular glands are rarely affected because of its increased bacteriostatic activity.
ACUTE The BACTERIAL SIALADENITIS commensal organisms such as Staphylococcus aureus, Staph. pyogenes, Strep. viridans, Pnuemococcus, Actinomycosis etc. can cause the bacterial sialadenitis. It affects either the neonate & children or debilitated adults with poor oral hygiene. Some drugs like tranquilizers, antiparkinson drugs, diueretics, anti- histamines, tricyclic anti depressants etc. decrease the salivary flow which increases the chance of infection of salivary glands.
CLINICAL FEATURES: The disease is characterized by sudden onset of pain at the angle of the jaw, which is unilateral. The affected gland is enlarged and tender and extremely painful. The inflammatory swelling is very tense and doesn’t show much fluctuation. The overlying skin is warm and red. There is purulent discharge from Stenson’s duct, which can be seen upon pressing the papilla. Patient might suffer from fever and other symptoms of acute inflammation.
D. D: - Bacterial sialadenitis can be differentiated from mumps by the discharge of pus at ductal opening. Investigation: - The lecuocyte count is high – leucocytosis. Sialography should not be performed in the presence of acute suppuration. The pus is collected form Stenson’s duct taking care not to contaminate the swab with oral microfloa, for the culture & sensitivity test.
MANAGEMENT: Antibiotics. Palliative- a) Hydrating the patient with electrolytes. b) Stimulate the salivation by chewing. c) Improve the oral hygiene by debridement & irrigation. If there is no improvement, Surgical drainage may be done using needle aspiration guided by CT scan or ultra sonography.
CHRONIC BACTERIAL SIALADENITIS The chronic or the recurrent type of bacterial sialadenitis may be seen in children & adults. It may be idiopathic or with factors like duct obstruction, congenital stenosis, Sjogrens syndrome, viral infection. All these factors except the duct obstruction by stone are seen commonly in the parotid glands. The microorganism may be Strep. viridans, Escherichia coli, Proteus, Pneumococci. Because these are with low virulence, the changes are not sudden.
CLINICAL FEATURES: The disease starts as an unilateral swelling at the angle of the jaw. The recurrent sialedenitis shows periods of remissions. The gland may under go atrophy, which results in decreased flow.
MANAGEMENT: 1) Antibiotics Intraductal infusion of erythromycin, tetracycline Occluding ductal system with a protein solution In intractable cases, removal of the gland.
CYSTS OF THE SALIVARY GLANDS MUCOCELE: Cysts of the salivary gland is known as Mucocele is a clinical term that describes swelling caused by the accumulation of saliva at the site of a traumatized or obstructed minor salivary gland duct. TYPES 1. Extravasation type 2. Retention type
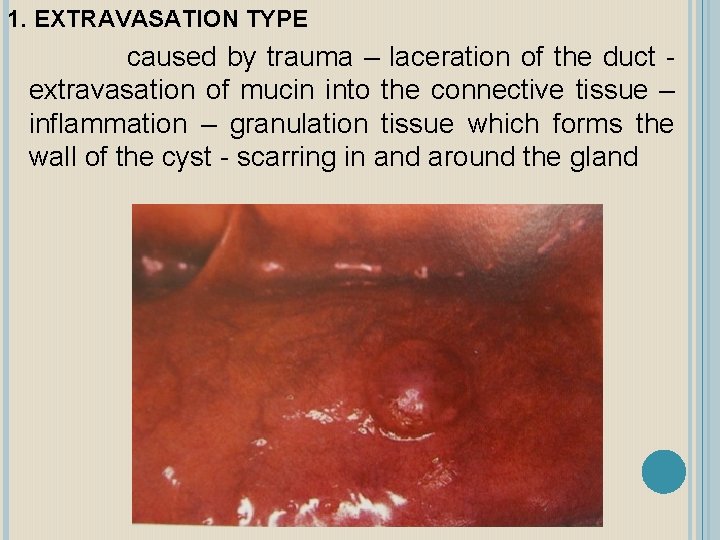
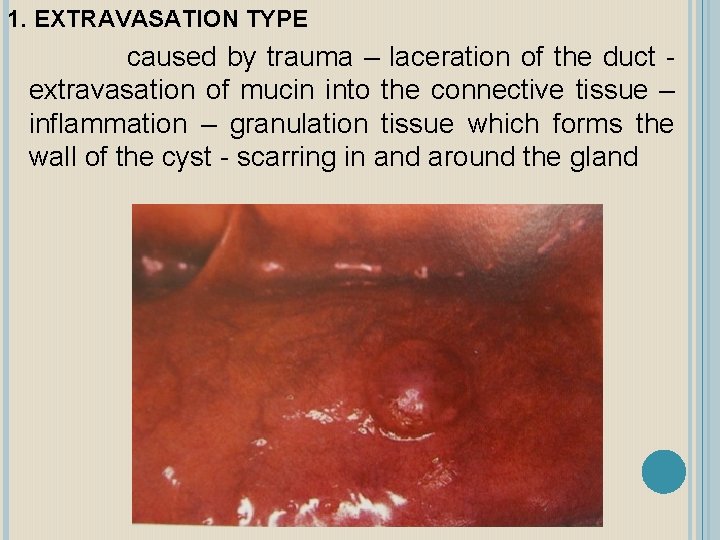
1. EXTRAVASATION TYPE caused by trauma – laceration of the duct extravasation of mucin into the connective tissue – inflammation – granulation tissue which forms the wall of the cyst - scarring in and around the gland
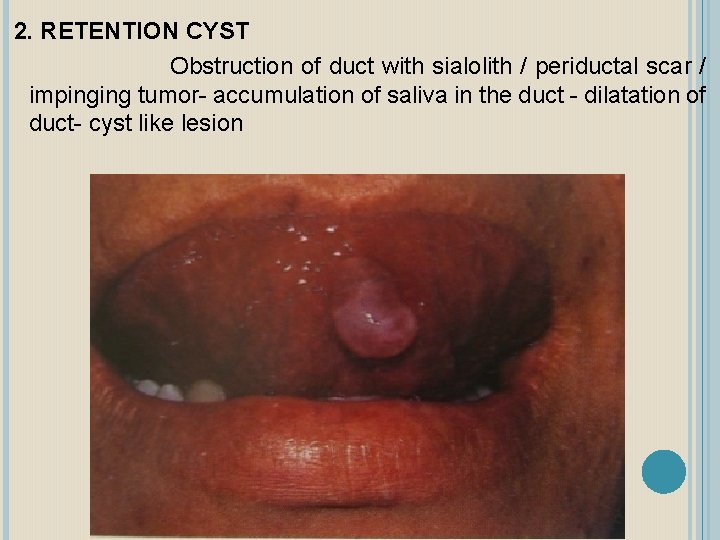
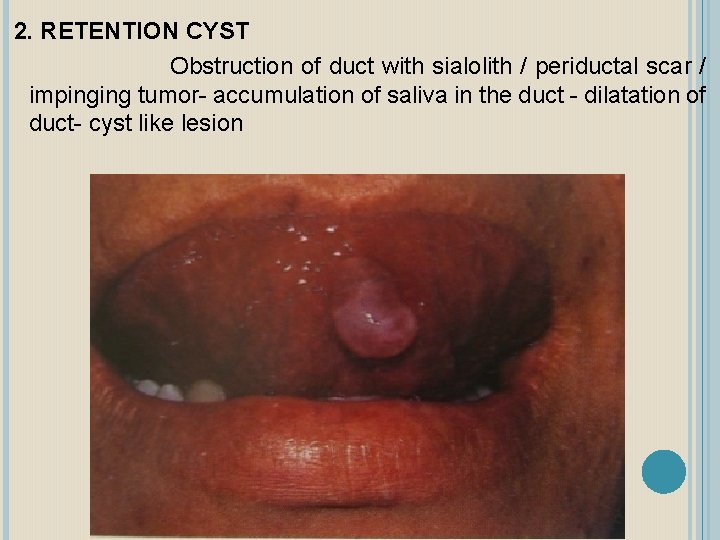
2. RETENTION CYST Obstruction of duct with sialolith / periductal scar / impinging tumor- accumulation of saliva in the duct - dilatation of duct- cyst like lesion
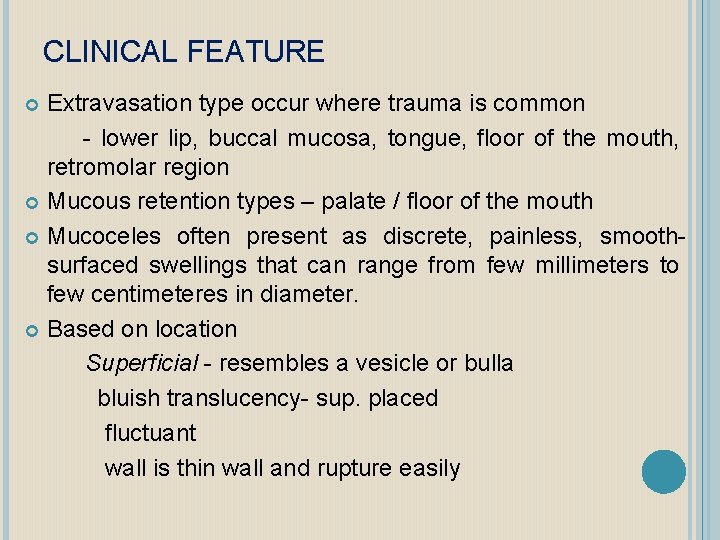
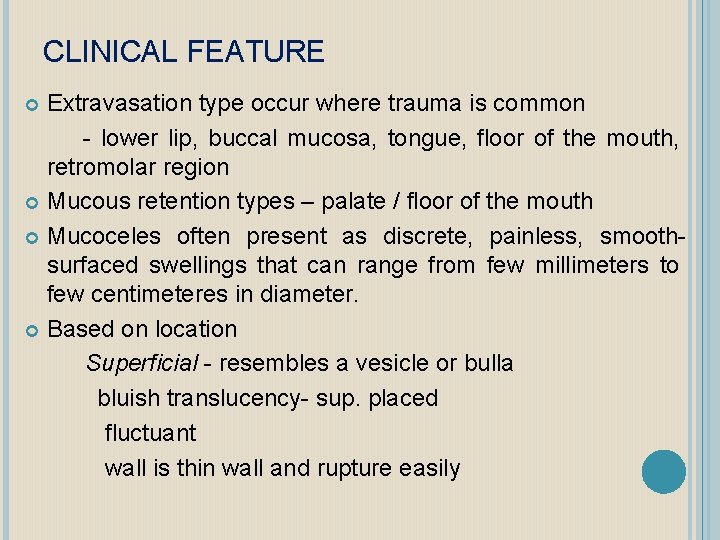
CLINICAL FEATURE Extravasation type occur where trauma is common - lower lip, buccal mucosa, tongue, floor of the mouth, retromolar region Mucous retention types – palate / floor of the mouth Mucoceles often present as discrete, painless, smoothsurfaced swellings that can range from few millimeters to few centimeteres in diameter. Based on location Superficial - resembles a vesicle or bulla bluish translucency- sup. placed fluctuant wall is thin wall and rupture easily
-Deep more diffuse covered by normal appearing mucosa firm & well circumscribed present for longer period some regress and enlarge periodically D/D salivary gland neoplasm, vascular malformation, neurofibroma, lipoma
MANAGEMENT Surgical excision recurrence is common. Can be minimized if acini is also removed cryosurgery




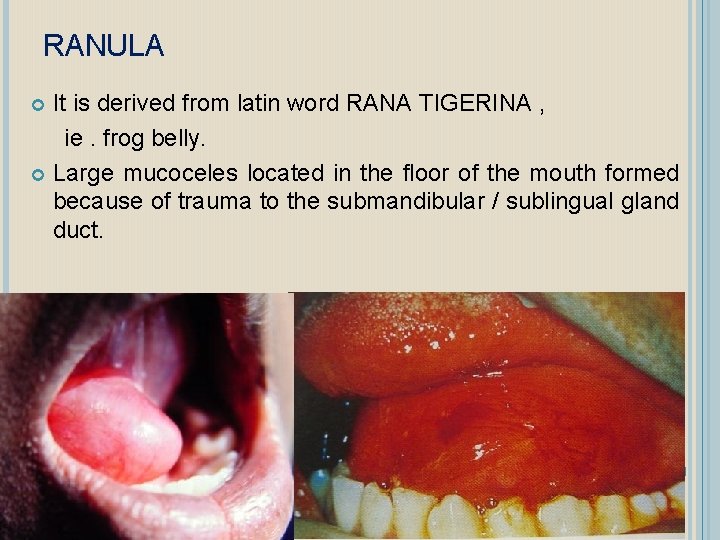
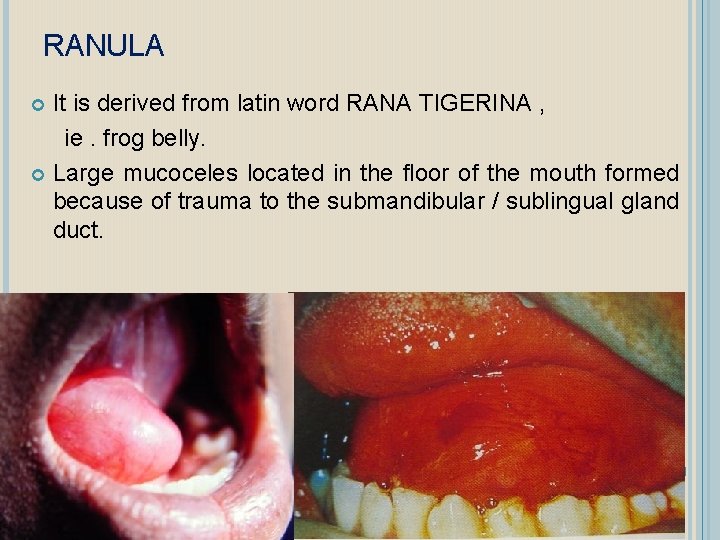
RANULA It is derived from latin word RANA TIGERINA , ie. frog belly. Large mucoceles located in the floor of the mouth formed because of trauma to the submandibular / sublingual gland duct.
TYPES Superficial - develop as a retention or extravasation phenomenon associated with trauma to the duct Plunging ranula – a rare variety which herniates thru mylohyoid muscle resulting as swelling of the neck.
CLINICAL FEATURE Usually unilateral Occurs usually in children and young adults Seen on floor of the mouth , below the tongue and on side of the frenum Produce blue swelling like a frog’s belly. The overlying mucosa appear normal if the lesion is deeply seated to the mylohyoid muscle Develops as slowly enlarging painless mass on one side of the floor of the mouth. Larger lesions – deviation and superior elevation of tongue , difficulty in speech / eating Size is smaller in early morning and largest just before meals, due increased secretory activity.
Soft in consistency and fluctuant. Non pitting on pressure D/D -Angioma -Lipoma -Dermoid cyst TREATMENT Marsupilization
NECROTIZING SIALOMETAPLASIA Benign , Self limiting reactive inflammatory disorder Minor salivary glands Mimics malignancy
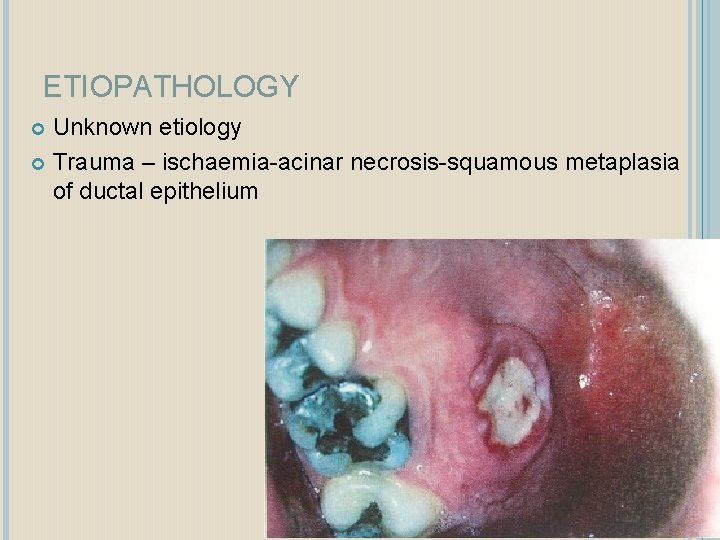
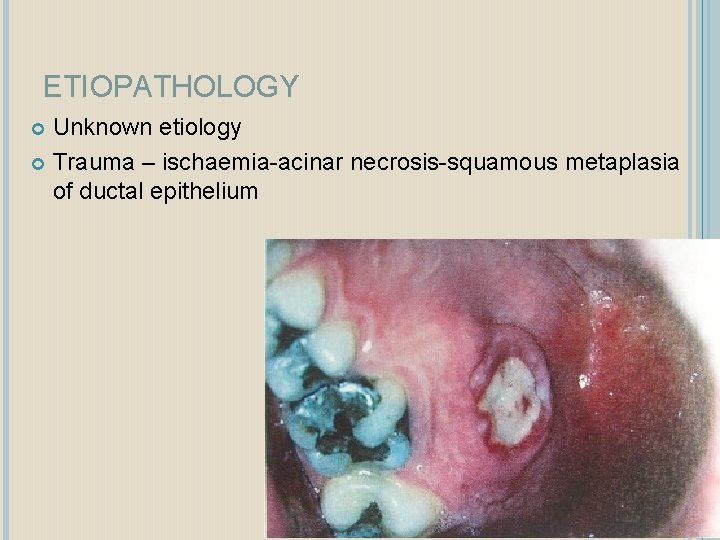
ETIOPATHOLOGY Unknown etiology Trauma – ischaemia-acinar necrosis-squamous metaplasia of ductal epithelium
CLINICAL FEATURE Commonly occurs in men in 5 th and 6 th decade. Site- palate, lip, retromolar pad Rapid onset Initially tender erythematous nodule Deep ulceration yellow base forms Dull pain Occur after oral procedures Vomiting episodes in bulimia
MANAGEMENT Self limiting , heals in 6 -8 weeks Debridement by hydrogen peroxide and saline rinses
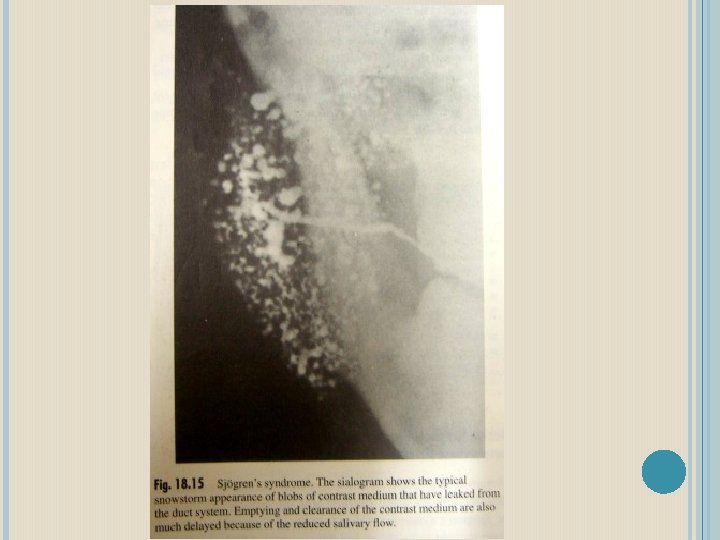
SJOGREN’S SYNDROME Most common immunologic disorder associated with salivary gland disease. Characterized by a lymphocyte-mediated destruction of the exocrine glands leading to xerostomia and keratoconjunctivitis sicca ETIOLOGY Unknown Suggested hormonal immunologic genetic
CLINICAL FEATURES � Above 40 yrs 90% cases occur in women Average of onset is 50 y � Predominantly women � Dry eyes leads to pain , burning sensation and ulceration � Dry mouth � Rhematoid arthritis

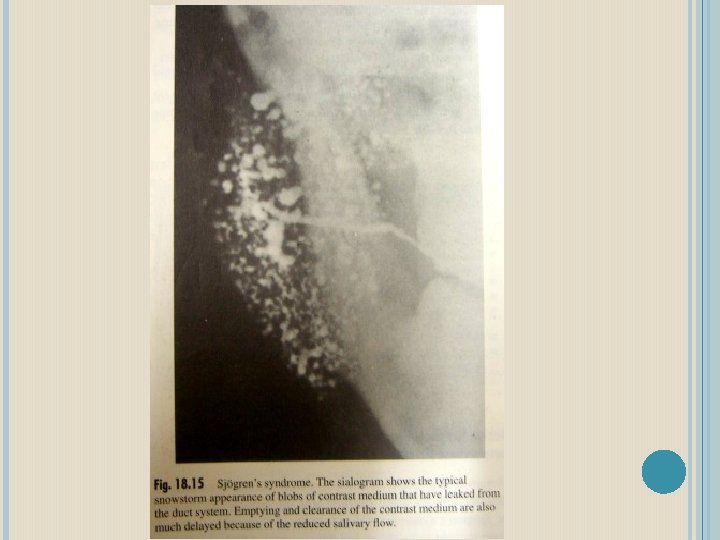
Two forms: Primary: involves the exocrine glands only Secondary: associated with a definable autoimmune disease, usually rheumatoid arthritis. 80% of primary and 30 -40% of secondary involves unilateral or bilateral salivary glands swelling
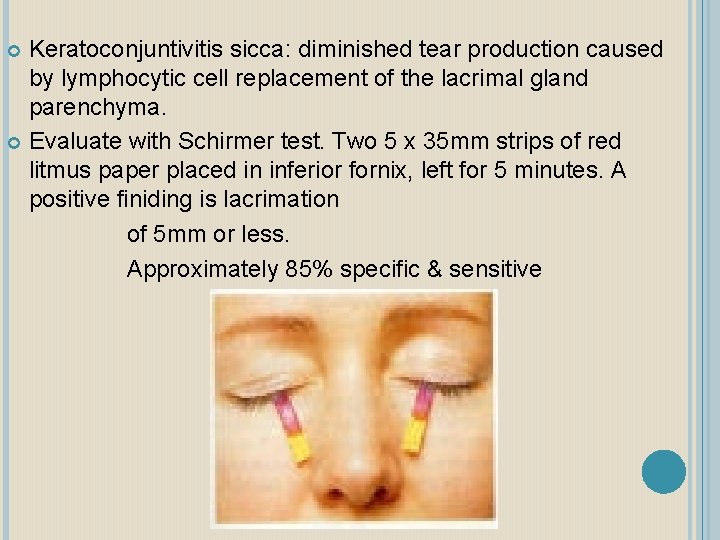
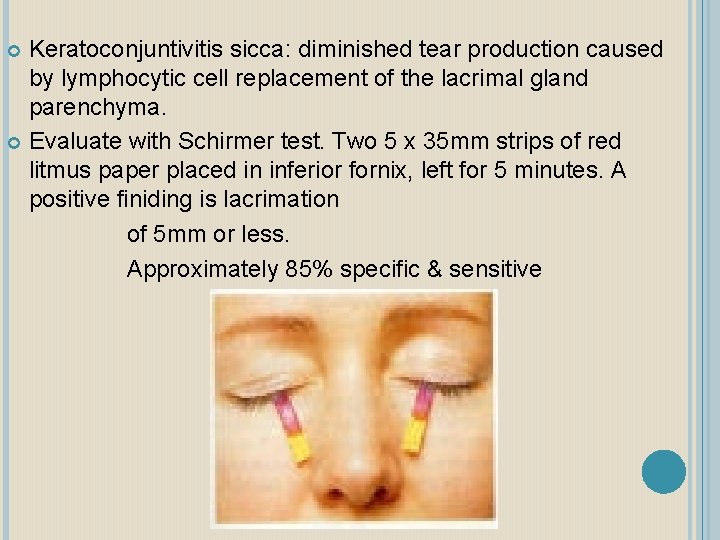
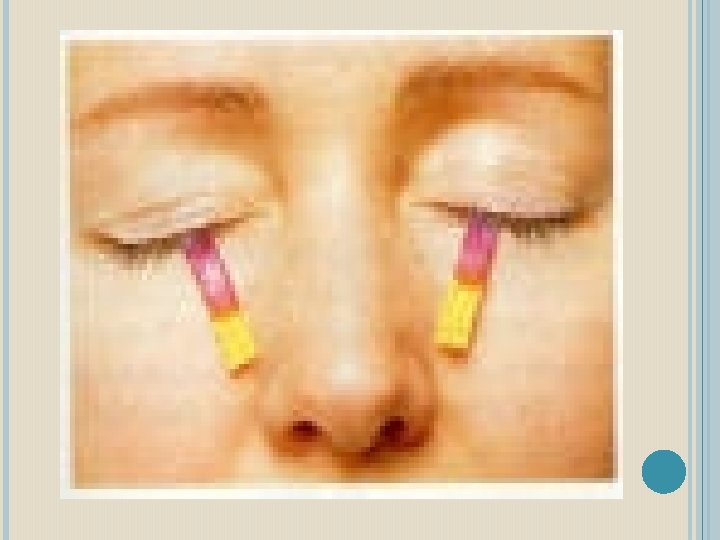
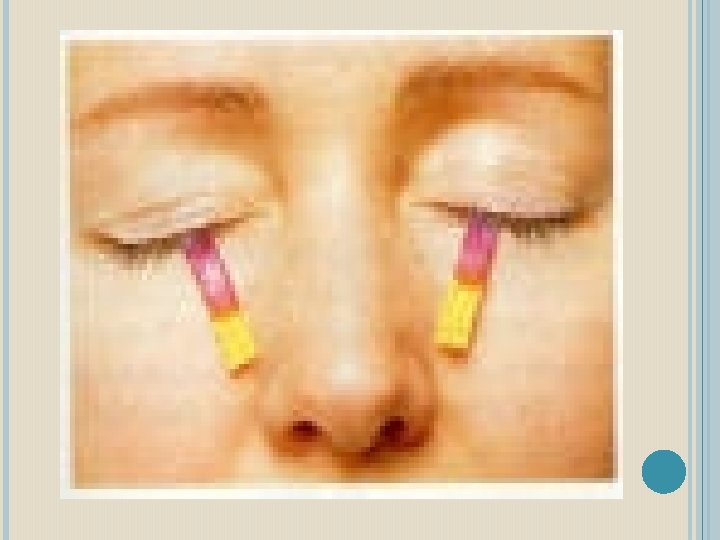
Keratoconjuntivitis sicca: diminished tear production caused by lymphocytic cell replacement of the lacrimal gland parenchyma. Evaluate with Schirmer test. Two 5 x 35 mm strips of red litmus paper placed in inferior fornix, left for 5 minutes. A positive finiding is lacrimation of 5 mm or less. Approximately 85% specific & sensitive
MANAGEMENT Symptomatic therapy for xerostomia artificial saliva gels water sipping chewing sugar free gum parasympathomimetic secretogogues -pilocarpine-4 mg qid -cevimeline-30 mg qid
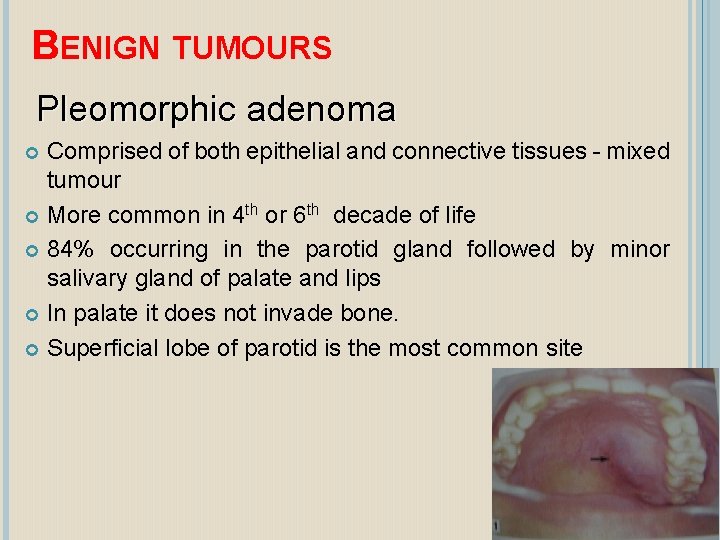
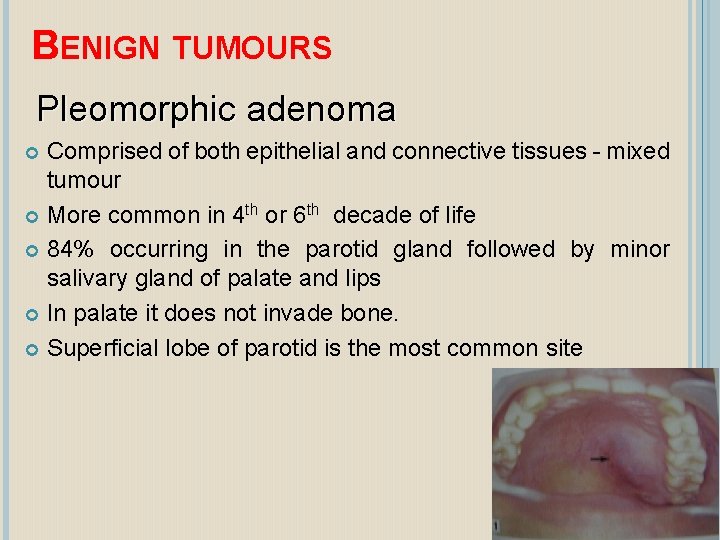
BENIGN TUMOURS Pleomorphic adenoma Comprised of both epithelial and connective tissues - mixed tumour More common in 4 th or 6 th decade of life 84% occurring in the parotid gland followed by minor salivary gland of palate and lips In palate it does not invade bone. Superficial lobe of parotid is the most common site
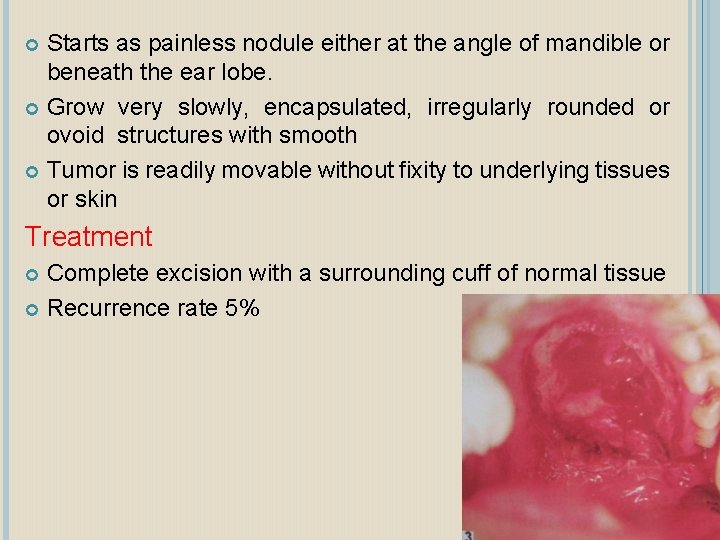
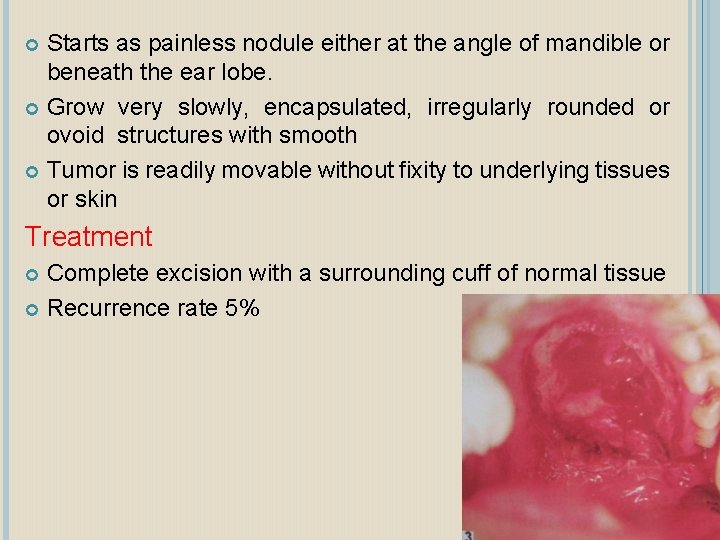
Starts as painless nodule either at the angle of mandible or beneath the ear lobe. Grow very slowly, encapsulated, irregularly rounded or ovoid structures with smooth Tumor is readily movable without fixity to underlying tissues or skin Treatment Complete excision with a surrounding cuff of normal tissue Recurrence rate 5%
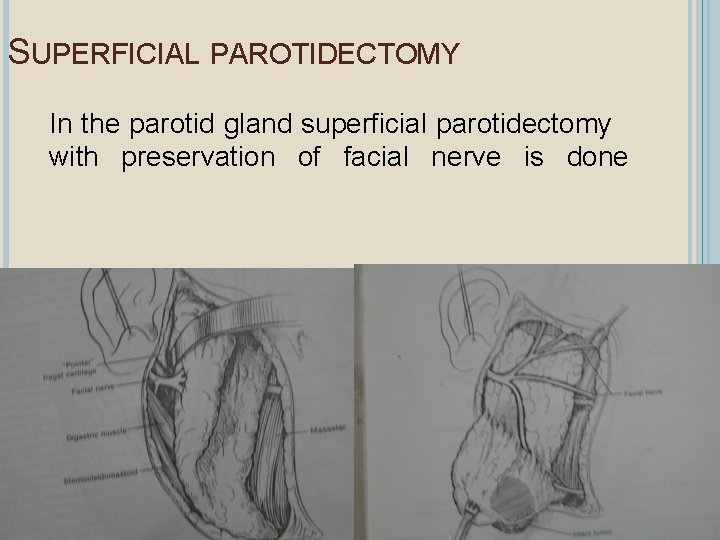
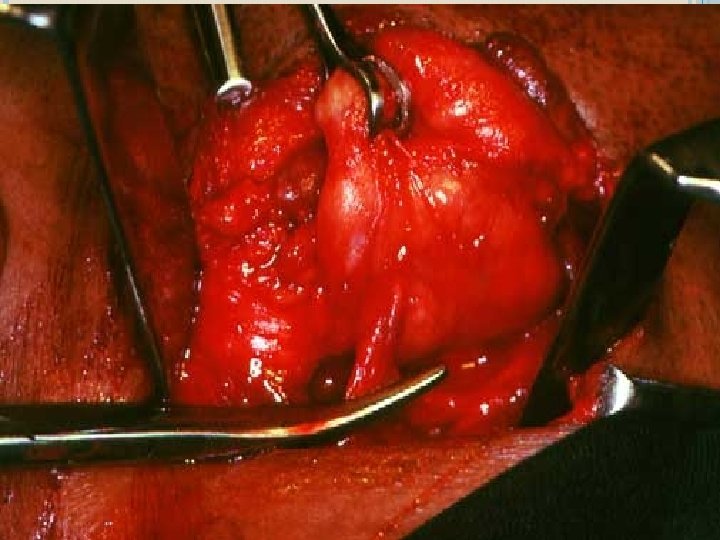
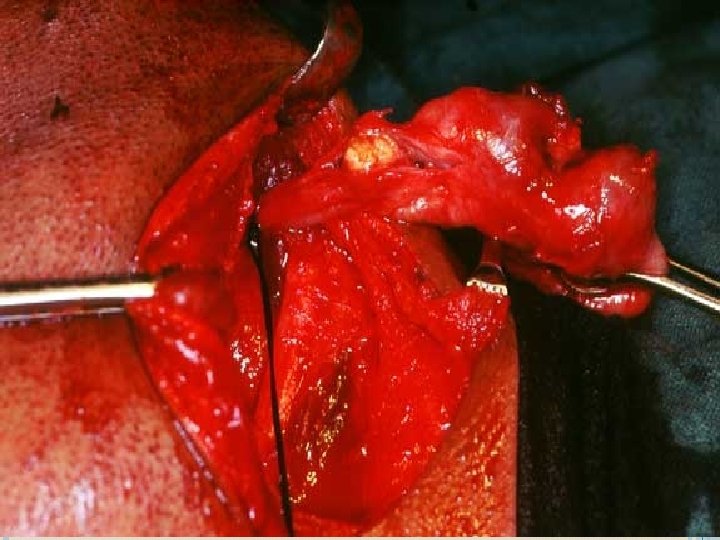
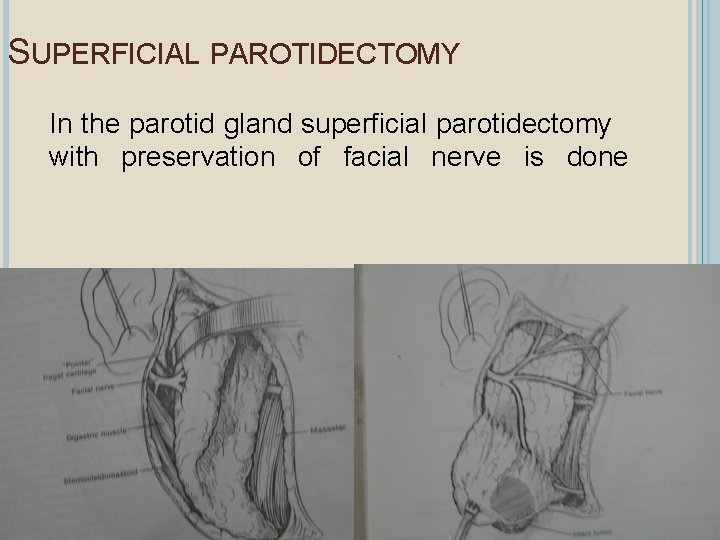
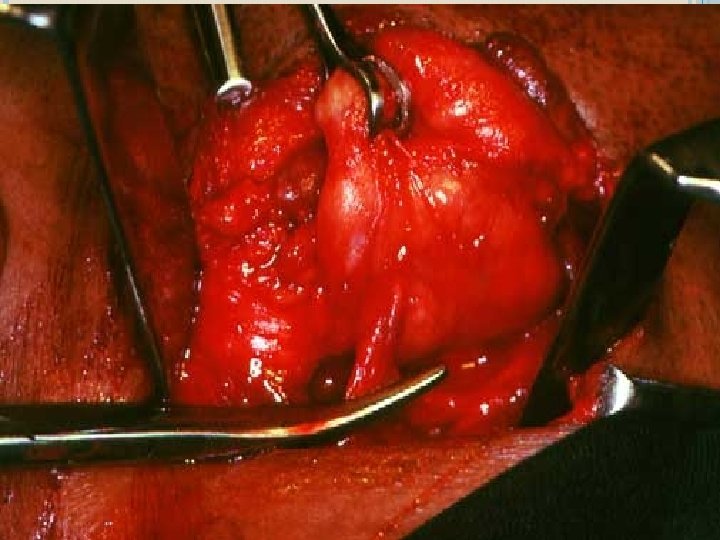
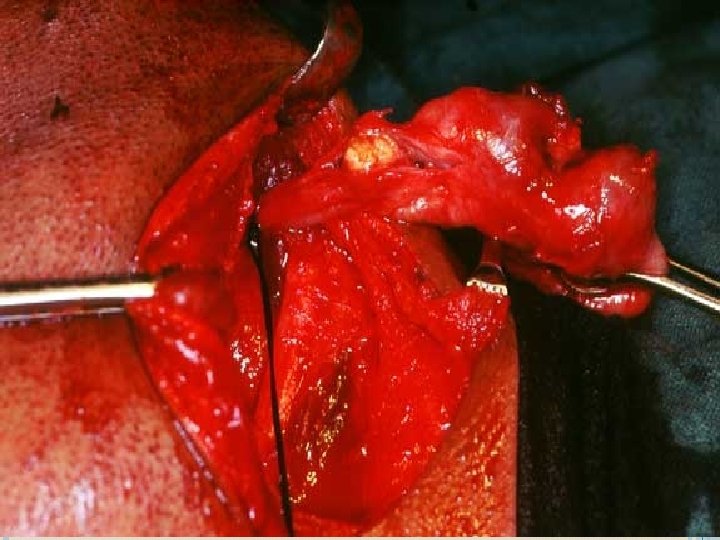
SUPERFICIAL PAROTIDECTOMY In the parotid gland superficial parotidectomy with preservation of facial nerve is done
WARTHIN’S TUMOUR This tumour is seen exclusively in parotid gland. Very rare in submandibular & minor glands. Males are more effected in 5 th decade It is firm, non tender, circumscribed mass seen in region of angle or ramus of mandible beneath the ear lobe. Diagnosis is confirmed by biopsy Treatment Surgical excision
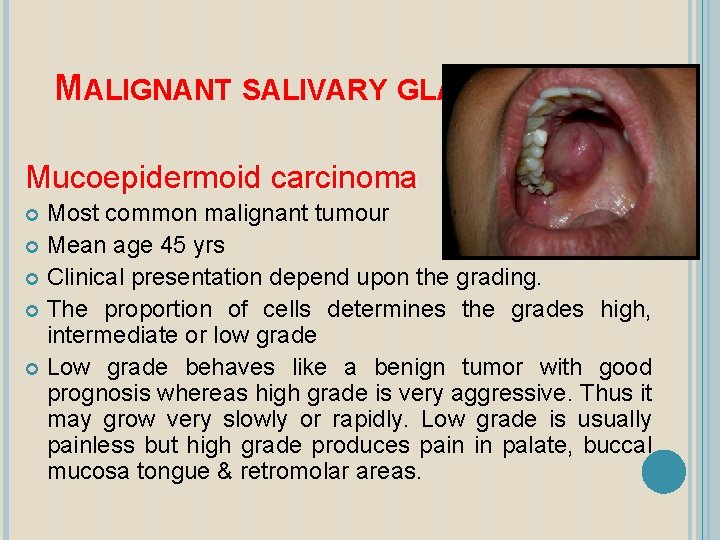
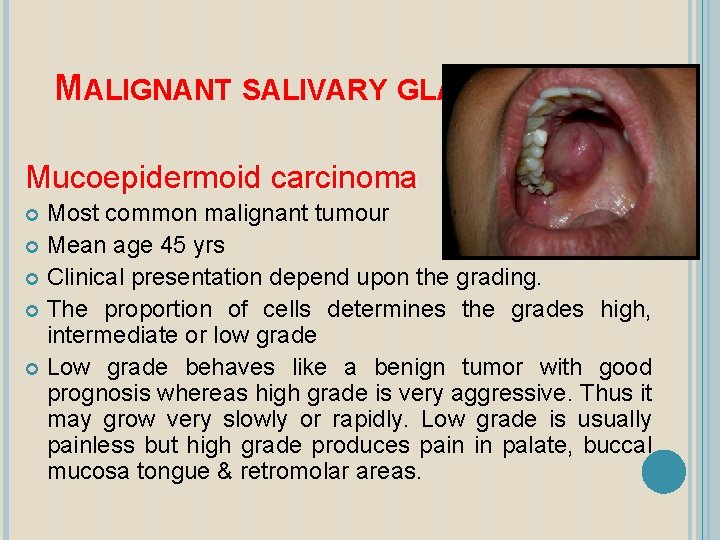
MALIGNANT SALIVARY GLAND TUMOURS Mucoepidermoid carcinoma Most common malignant tumour Mean age 45 yrs Clinical presentation depend upon the grading. The proportion of cells determines the grades high, intermediate or low grade Low grade behaves like a benign tumor with good prognosis whereas high grade is very aggressive. Thus it may grow very slowly or rapidly. Low grade is usually painless but high grade produces pain in palate, buccal mucosa tongue & retromolar areas.
Intraosseous mucoepidermiod carcinoma Mucoepidermiod carcinoma can occur within jaw bones, commonly in mandible. Entrapped mucous glands, epithelial cells may undergo neoplastic malformatio. These tumors are similar to extraosseous varity. Treatment: More radical surgical excision.

MUCOEPIDERMOID CARCINOMA
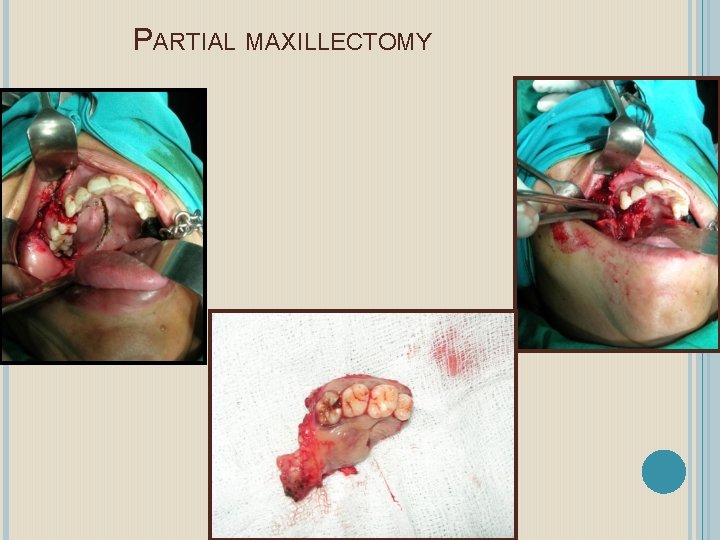
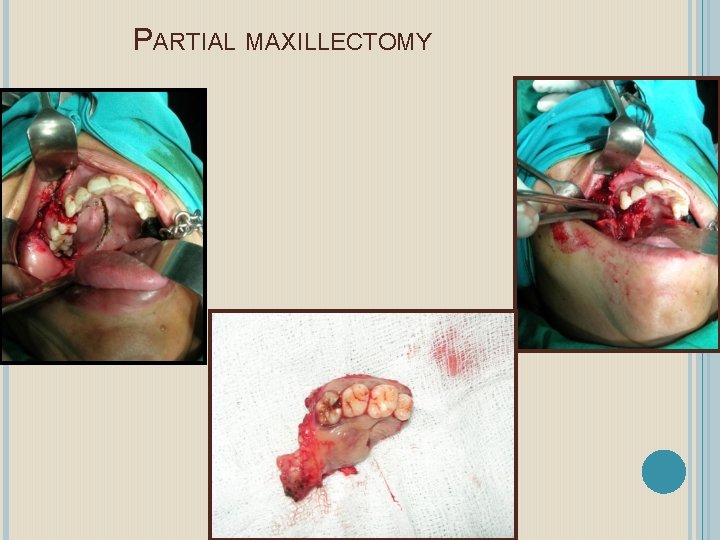
PARTIAL MAXILLECTOMY

POST OPERATIVE
ADENO CARCINOMA Second common Common site is junction of hard and soft palate Male to female ratio 3: 1 Slow growing , asymptomatic masses Predilection for invasion of the surrounding nerves Treatment –wide surgical excision
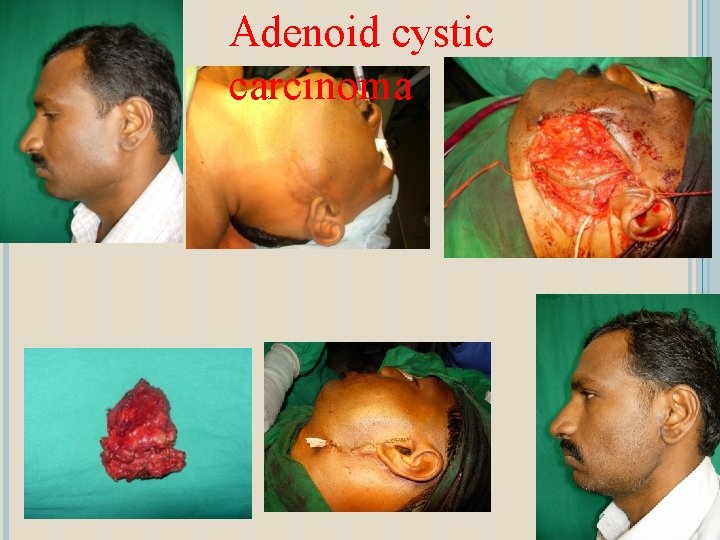
ADENOID CYSTIC CARCINOMA Also called Cylindroma because of its histological appearance Slow growing swelling mimics benign tumour clinically and histologically It has high potential for local distruction & invasiveness Treatment : Radical excision This tumour is radio resistance, irridation is not a mode of primary treatment
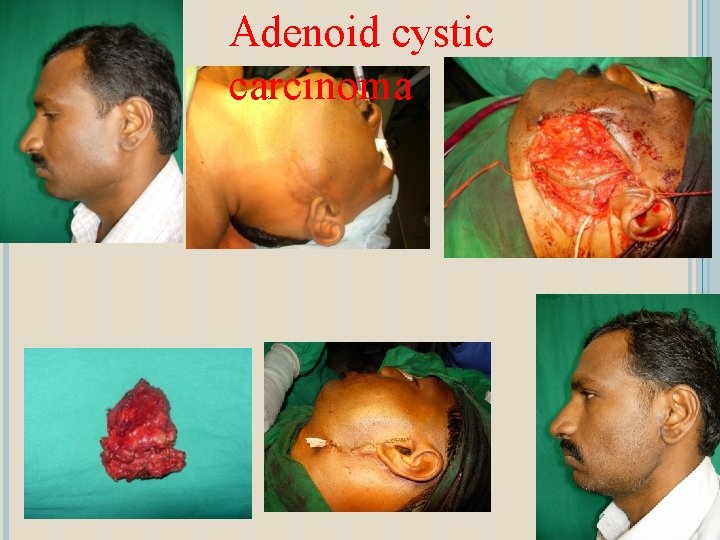
Adenoid cystic carcinoma
PAROTID GLAND: Largest salivary gland, the secretion of which is serous in nature. It is pyramidal in shape; the apex is towards the angle of the mandible, the base at the external acoustic meatus. Anteriorly the gland extends up to the buccal pad of fat and posteriorly encircles the posterior border of the mandible. Parotid gland has 2 lobes: (i) the Superficial and (ii) the Deep. They are connected by an isthmus at the posterior part of the gland. The entire gland is covered by a fibrous capsule.
The parotid duct (Stenson’s Duct) emerges at the anterior part of the gland. It passes horizontally across the masseter muscle, then pierces through the buccinator, to turn at right angles to reach the oral cavity. Stenson’s duct opening is seen as a papilla in the buccal mucosa opposite to the maxillary second molar. Parotid gland has close association with external carotid artery, the Retromandibular vein and the Facial nerve. The facial nerve emerges from the stylomastoid foramen, branches out from anterior and inferior margins of the gland.
SUB-MANDIBULAR GLAND: The sub-mandibular gland secretion is both serous and mucous in nature. This gland is located in the sub-mandibular space, extending inferiorly up to the digastric muscle, superiorly the mylohyoid muscle, posteriorly up to the angle of the mandible and anteriorly till the mid portion of the body of the mandible.
The sub-mandibular duct (Wharton’s Duct) starts from the deep part of the gland, turns sharply at the posterior border of the mylohyoid muscle anteriorly and superiorly, crosses the hyoglossus muscle then reaches the oral cavity. It opens at the sub-lingual papilla in the floor of the mouth. The sub-mandibular gland is in close association with the facial artery, facial vein, branch of the facial nerve and lingual nerve.
SUB-LINGUAL GLAND: The sub-lingual glands secrete predominantly mucous saliva. This gland is located in the sublingual space. The gland is present in association with the sub-lingual folds below the tongue. This gland is divided into anterior and posterior parts. It has got many small ducts. In the posterior part, these ducts open though the sublingual folds. The ducts of the anterior part may join to form a large main duct called Bartholin’s duct. This either opens though the sub-lingual papilla or joins with the Wharton’s duct.
MINOR SALIVARY GLANDS More than 700 minor salivary glands may be present in the oral cavity. These are in groups scattered all over the mouth. The minor glands secrete mucous secretions. These glands have numerous small ducts.


MONOMORPHIC ADENOMA (CANALICULAR ADENOMA , BASAL CELL ADENOMA AND CYSTIC ADENOMA) Benign salivary gland tumors composed predominantly of epithelium Basaloid, membraneous, salivary duct, sebaceous, oncocytomas, mucinous, myoepithelial and epidermoid papillary. Clinical feature- sub mucosal nodular mass, freely movable, firm mass Treatment-conservative extracapsular excision