SALIVARY GLAND DISEASES Yrd Do Dr Rasim Ylmazer

- Slides: 40
SALIVARY GLAND DISEASES Yrd. Doç. Dr. Rasim Yılmazer
Learning goal and objectives of the lesson Learning goal of the lesson: The learner should know the main clinical features and investigation of salivary gland disorders Learning objectives of the lesson the learner will be able to: n identify the most common etiologies of salivary masses based on history and physical exam n develop a clear concinse algorithm for use of diagnostic tests evaluation of salivary masses n describe available therapeutic options for malignant salivary gland masses n Understand how to approach the patient with “ a lump in the parotis or submandibular gland. Skill objectives of the lesson the learner will be able to take a directed history and perform a physical exam on a patient with salivary gland masses.
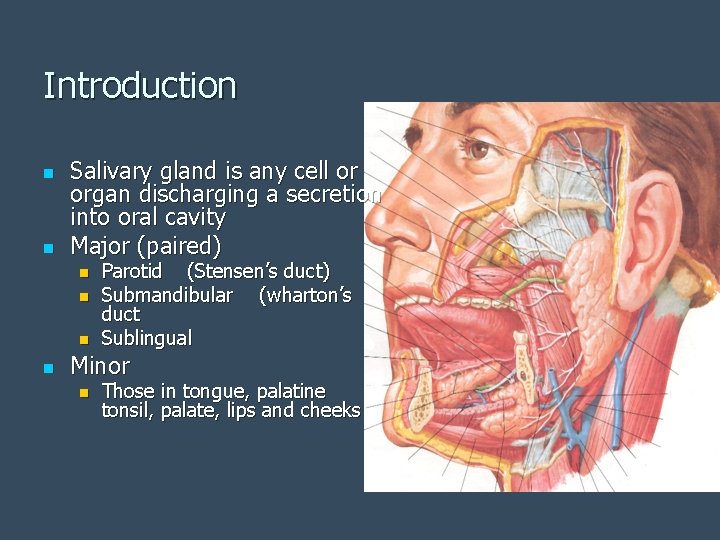
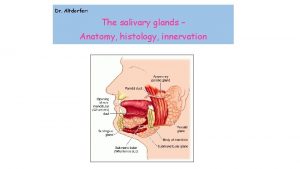
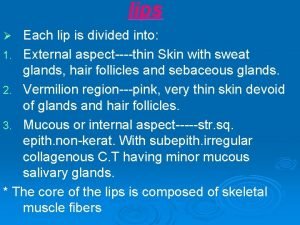
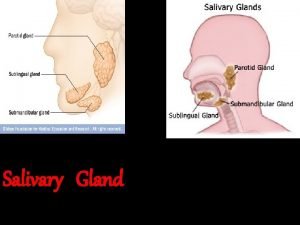
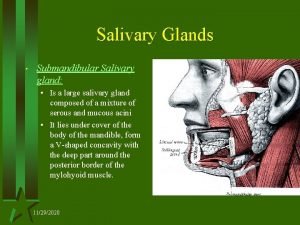
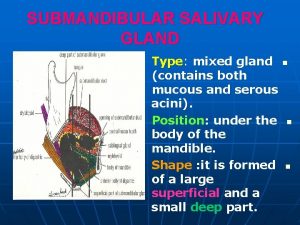
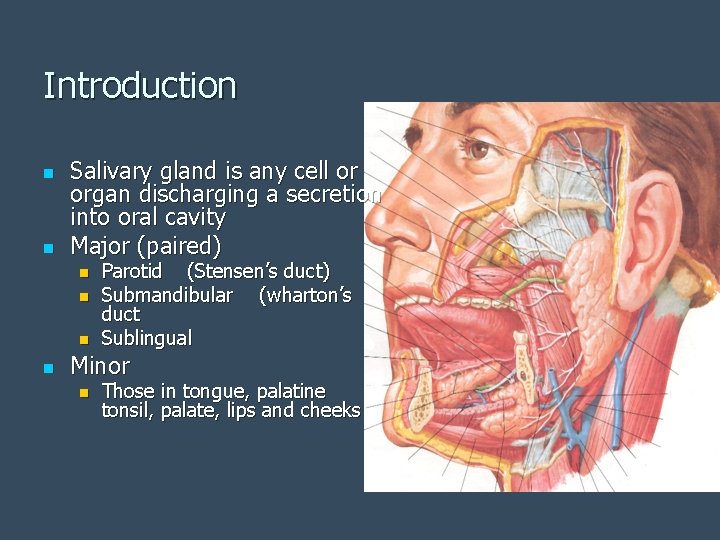
Introduction n n Salivary gland is any cell or organ discharging a secretion into oral cavity Major (paired) n n Parotid (Stensen’s duct) Submandibular (wharton’s duct Sublingual Minor n Those in tongue, palatine tonsil, palate, lips and cheeks
Nonneoplastic Diseases of the Salivary Glands
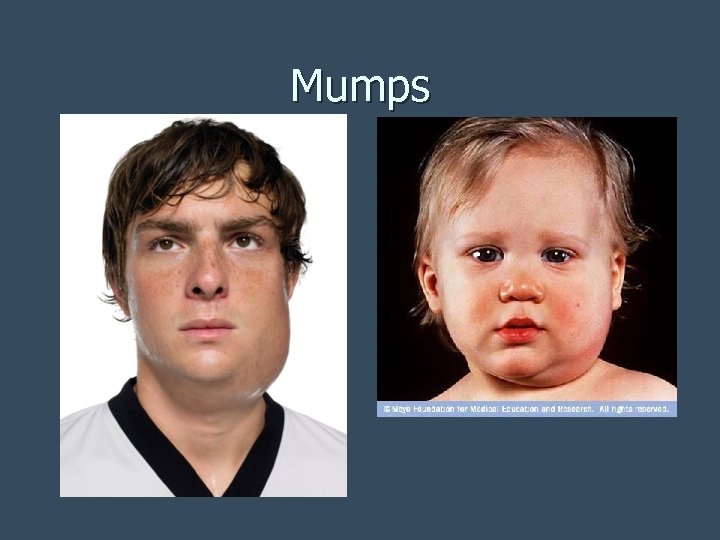
n Mumps Most common viral disorder of salivary glands n Peak age 4 -6 n Prodrome period is 2 -3 weeks n 1 or both parotid glandes can be involved n Contagious from approximately 6 days before the onset of symptoms until about 9 days after symptoms start n Diagnosis: diagnosed on clinical grounds n Serum amylase is often elevated n
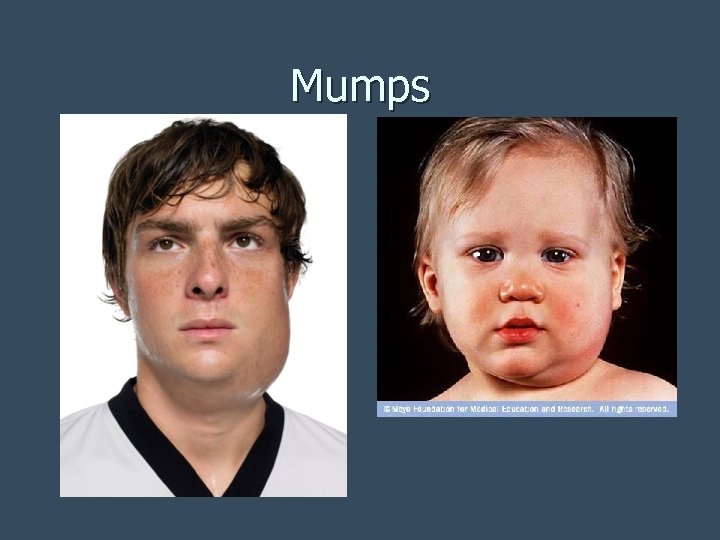
Mumps
n n Complications: deafness, pancreatitis, meningitis, encephalitis, orchitis or epididymitis, Oophoritis (inflammation of ovaries) Deafness generally unilateral rarely bilateral Profound (91 d. B or more) sensorineural hearing loss Acute unilateral deafness occurs in about 0. 005% of cases
n n n No specific treatment Paracetamol for pain relief Warm saltwater gargles, soft foods, and extra fluids may also help relieve symptoms Self-limiting, and general outcome is good Most common preventative measure against mumps is a vaccination with a mumps vaccine
n Other Viruses CMV, Coxsackievirus A, Echovirus, Influenza A, Lymphocytic choriomeningitis Virus n Treatment: symptomatic for all viral diseases n
n Acute bacterial parotitis most often caused by a bacterial infection of Staphylococcus aureus but may be caused by any commensal bacteria n Peak age 50’s-60’s n 30 -40% in post-op patients; most commonly gastrointestinal procedures n

Presentation: sudden, diffuse enlargement with associated induration and tenderness. Massage produces purulent saliva n 20% of cases bilateral n Treatment: hydration, improved oral hygiene, repeated massage of gland, IV antibiotics, warm compresses, sialogogues n If no significant improvement in 24 -48 h, then proceed to incision & drainage OR imageguided needle aspiration n
n Chronic Nonspecific Sialadenitis Most commonly parotid n Usually from permanent damage during acute infection; occasionally from recurrent parotitis of childhood n
n Recurrent Parotitis of Childhood n n n More common in males; peak age 5 -7 ¾ give role of Mumps; heredity plays no role Presentation: Usually unilateral; when bilateral, one side worse Severe pain, fever, malaise during attacks Recurs 55% of cases resolve with puberty 25% no improvement with puberty
n Sarcoidosis Parotid enlargement is a classic feature of sarcoidosis, but clinically apparent parotid involvement occurs in less than 10% of patients. n Bilateral involvement is the rule. n The gland is usually not tender, but firm and smooth. n Xerostomia can occur n Other exocrine glands are affected only rarely n
n Sjogren’s Syndrome: Sjögren syndrome also known as "Sicca syndrome" n Systemic autoimmune disease in which immune cells attack and destroy the exocrine glands that produce tears and saliva n Chronic, slowly progressive, benign; 2 nd most common autoimmune disease behind Rheumatoid arthritis n
n Although Sjögren's occurs in all age groups in both women and men n Nine out of ten Sjögren's patients are women n Average of onset is after menopause in women
Presentation Other exocrine gland involvement: dry nose, dry throat, xerotrachea, esophageal mucosal atrophy, atrophic gastritis, subclinical pancreatitis, vaginal dryness n 1/3 = fatigue, low grade fever, myalgias/arthralgias n Extraglandular involvement in ¼: Lungs, kidneys, vasculitis, nervous system n
Associated risks n Increased risk of 1) Non. Hodgkin’s Lymphoma 2) Multiple Myeloma
n Sialolithiasis n Formation of stones in the salivary glands n 80% submandibular gland, 20% parotid n Only 1 stone in ¾ cases n Presentation: recurrent swelling, pain worse with eating n Complications: sialadenitis, ductal ectasia, and stricture
Diagnosis is usually made by characteristic history and physical examination n Diagnosis can be confirmed by x-ray (80% of salivary gland calculi are visible on x-ray), or by sialogram or ultrasound. n 90% of submandibular stones radioopaque; 90% of parotid stones radiolucent n Treatment: Endoscopic excision, If near duct orifice transoral removal of stone with marsupialization, gland excision n
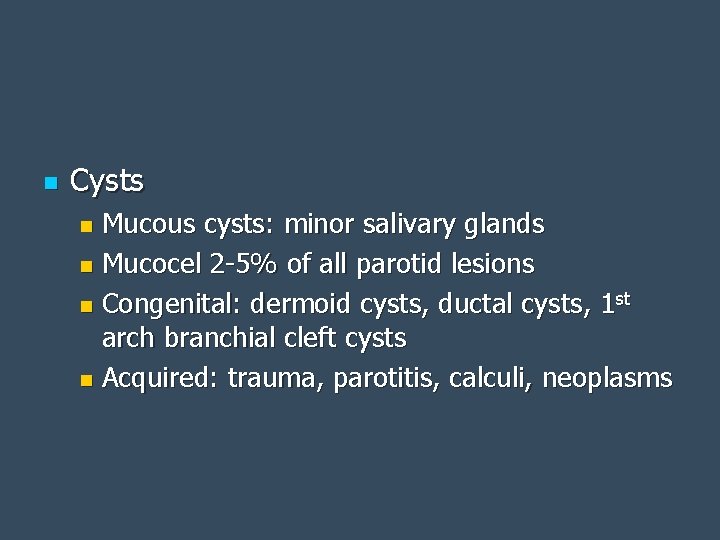
n Cysts Mucous cysts: minor salivary glands n Mucocel 2 -5% of all parotid lesions n Congenital: dermoid cysts, ductal cysts, 1 st arch branchial cleft cysts n Acquired: trauma, parotitis, calculi, neoplasms n
Neoplastic Diseases of the Salivary Glands
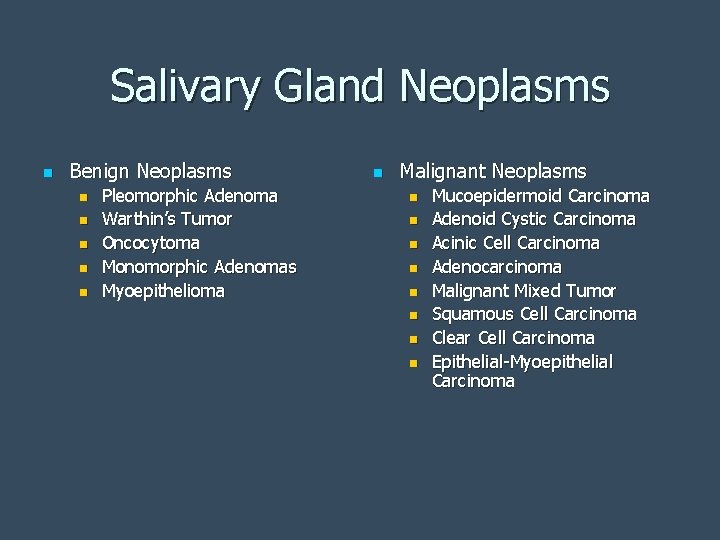
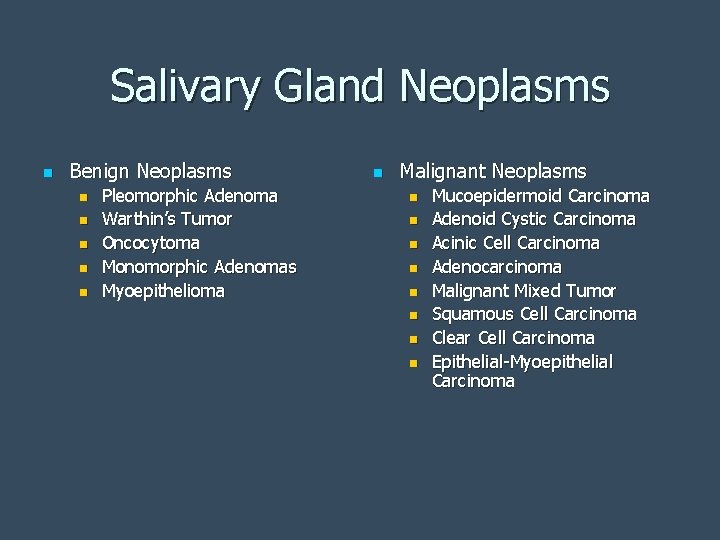
Salivary Gland Neoplasms n Benign Neoplasms n n n Pleomorphic Adenoma Warthin’s Tumor Oncocytoma Monomorphic Adenomas Myoepithelioma n Malignant Neoplasms n n n n Mucoepidermoid Carcinoma Adenoid Cystic Carcinoma Acinic Cell Carcinoma Adenocarcinoma Malignant Mixed Tumor Squamous Cell Carcinoma Clear Cell Carcinoma Epithelial-Myoepithelial Carcinoma
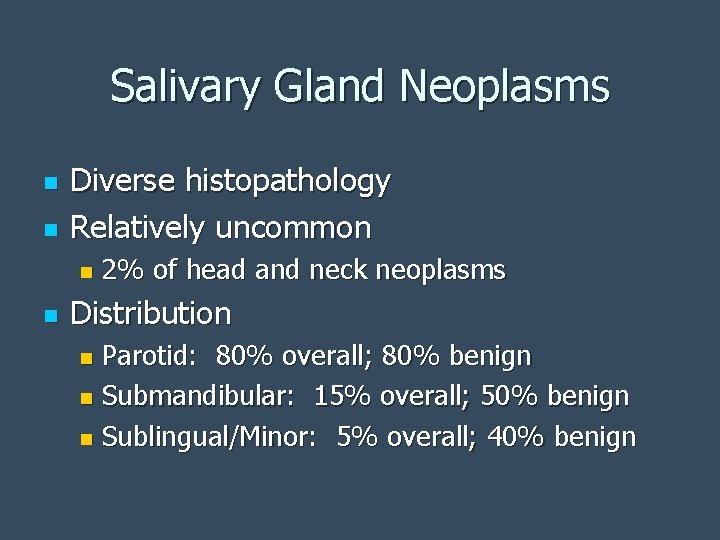
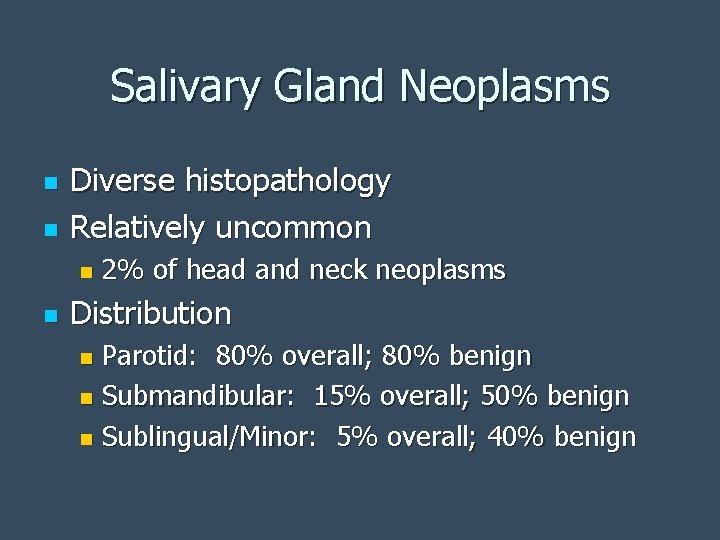
Salivary Gland Neoplasms n n Diverse histopathology Relatively uncommon n n 2% of head and neck neoplasms Distribution Parotid: 80% overall; 80% benign n Submandibular: 15% overall; 50% benign n Sublingual/Minor: 5% overall; 40% benign n
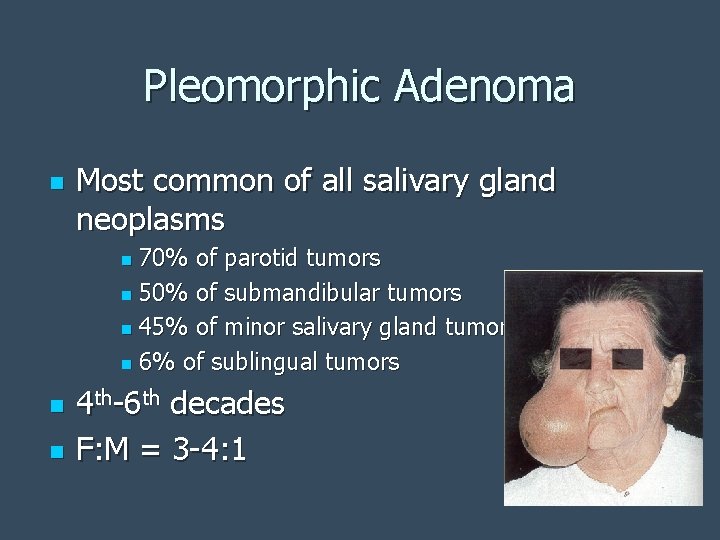
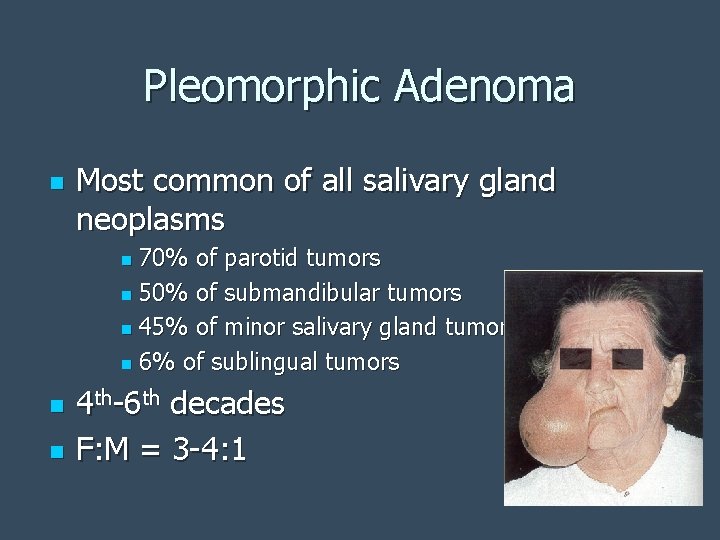
Pleomorphic Adenoma n Most common of all salivary gland neoplasms 70% of parotid tumors n 50% of submandibular tumors n 45% of minor salivary gland tumors n 6% of sublingual tumors n n n 4 th-6 th decades F: M = 3 -4: 1
Pleomorphic Adenoma n n n Slow-growing, painless mass Parotid: 90% in superficial lobe, most in tail of gland Minor salivary gland: lateral palate, submucosal mass
Pleomorphic Adenoma n Treatment: complete surgical excision Parotidectomy with facial nerve preservation n Submandibular gland excision n Wide local excision of minor salivary gland n n Avoid enucleation and tumor spill
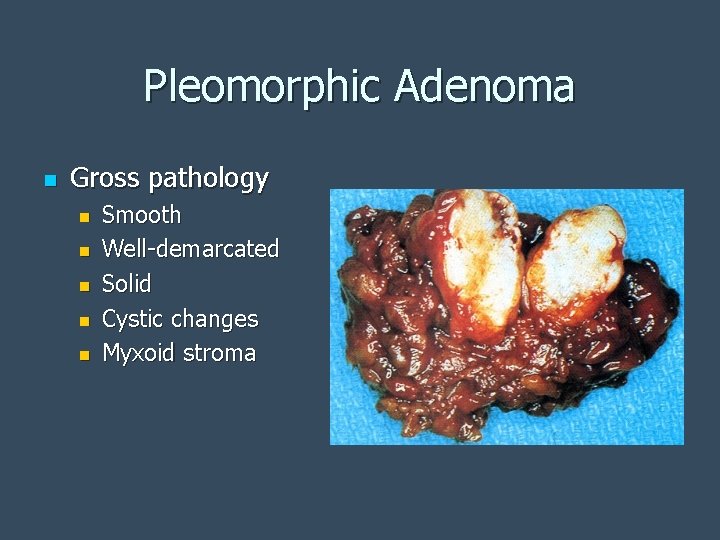
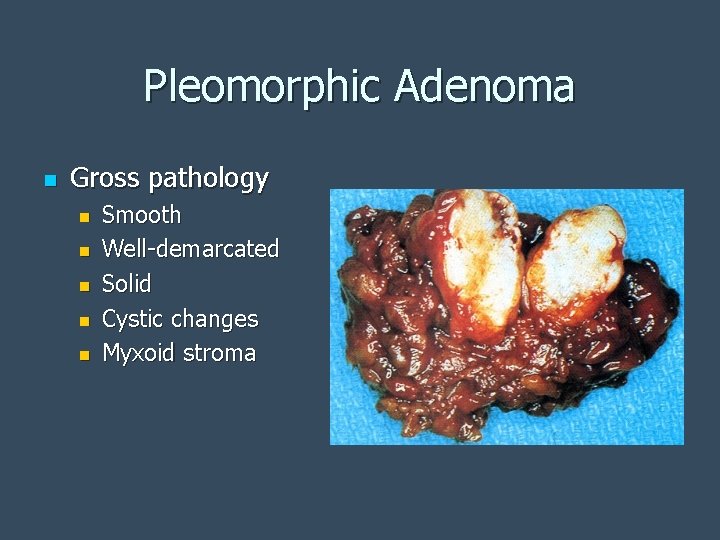
Pleomorphic Adenoma n Gross pathology n n n Smooth Well-demarcated Solid Cystic changes Myxoid stroma
Warthin’s Tumor n n n Papillary cystadenoma lymphomatosum 6 -10% of parotid neoplasms Older, caucasian, males 10% bilateral or multicentric 3% with associated neoplasms Presentation: slow-growing, painless mass
Oncocytoma n n n Rare: 2. 3% of benign salivary tumors 6 th decade M: F = 1: 1 Parotid: 78% Submandibular gland: 9% Minor salivary glands: palate, buccal mucosa, tongue
Monomorphic Adenomas n n n Basal cell, canalicular, sebaceous, glycogenrich, clear cell Basal cell is most common: 1. 8% of benign epithelial salivary gland neoplasms 6 th decade M: F = approximately 1: 1 Caucasian > African American Most common in parotid
Mucoepidermoid Carcinoma n n n n Most common salivary gland malignancy 5 -9% of salivary neoplasms Parotid 45 -70% of cases Palate 18% 3 rd-8 th decades, peak in 5 th decade F>M Caucasian > African American
Mucoepidermoid Carcinoma n Presentation n Low-grade: slow growing, painless mass n High-grade: rapidly enlarging, +/- pain
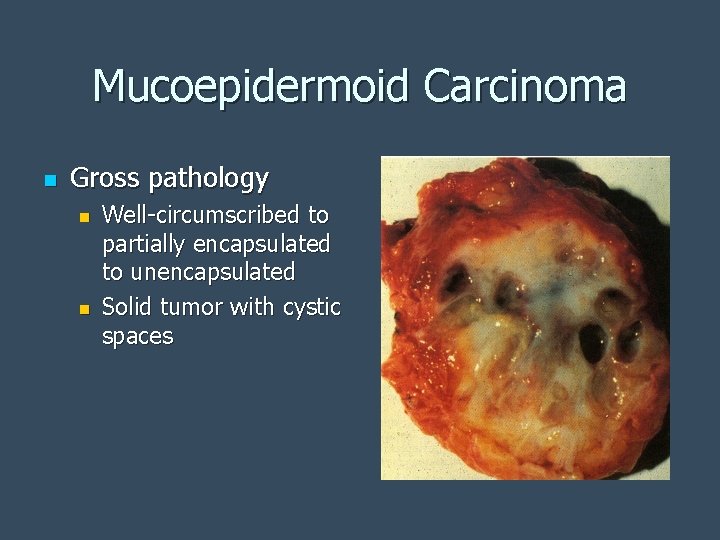
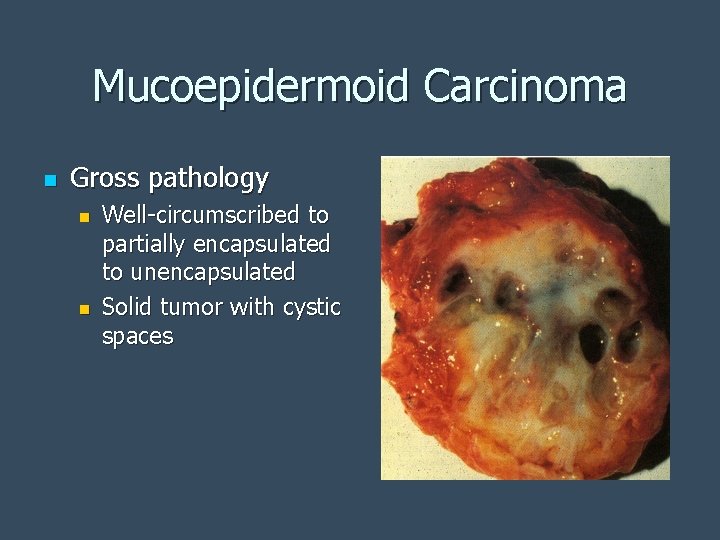
Mucoepidermoid Carcinoma n Gross pathology n n Well-circumscribed to partially encapsulated to unencapsulated Solid tumor with cystic spaces
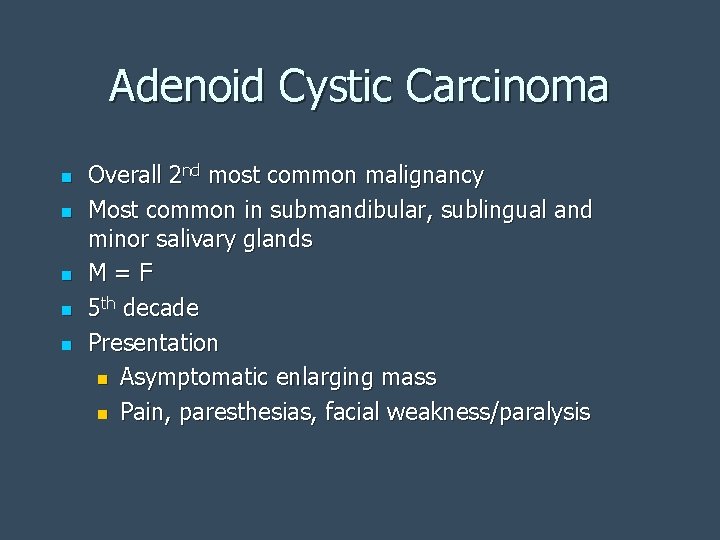
Adenoid Cystic Carcinoma n n n Overall 2 nd most common malignancy Most common in submandibular, sublingual and minor salivary glands M=F 5 th decade Presentation n Asymptomatic enlarging mass n Pain, paresthesias, facial weakness/paralysis
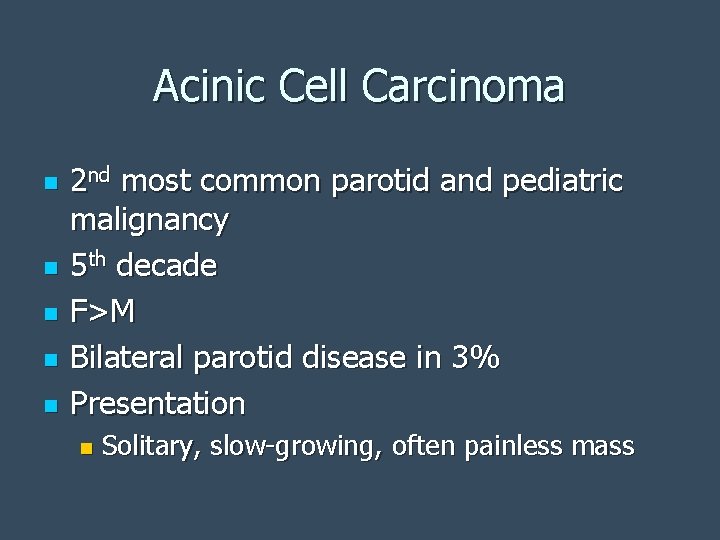
Acinic Cell Carcinoma n n n 2 nd most common parotid and pediatric malignancy 5 th decade F>M Bilateral parotid disease in 3% Presentation n Solitary, slow-growing, often painless mass
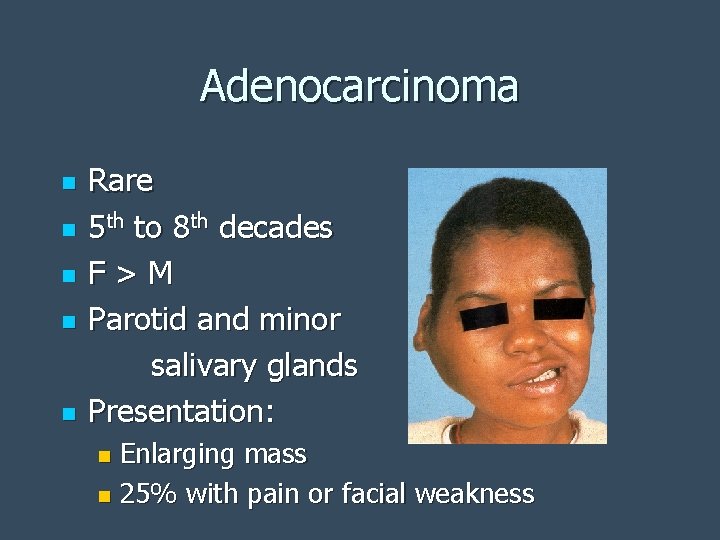
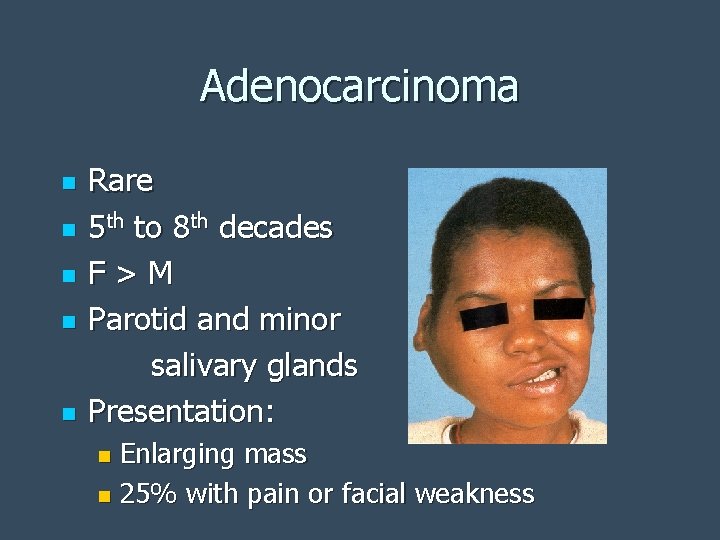
Adenocarcinoma n n n Rare 5 th to 8 th decades F>M Parotid and minor salivary glands Presentation: Enlarging mass n 25% with pain or facial weakness n
Malignant Mixed Tumors n n n Carcinoma ex-pleomorphic adenoma n Carcinoma developing in the epithelial component of preexisting pleomorphic adenoma Carcinosarcoma n True malignant mixed tumor—carcinomatous and sarcomatous components Metastatic mixed tumor n Metastatic deposits of otherwise typical pleomorphic adenoma
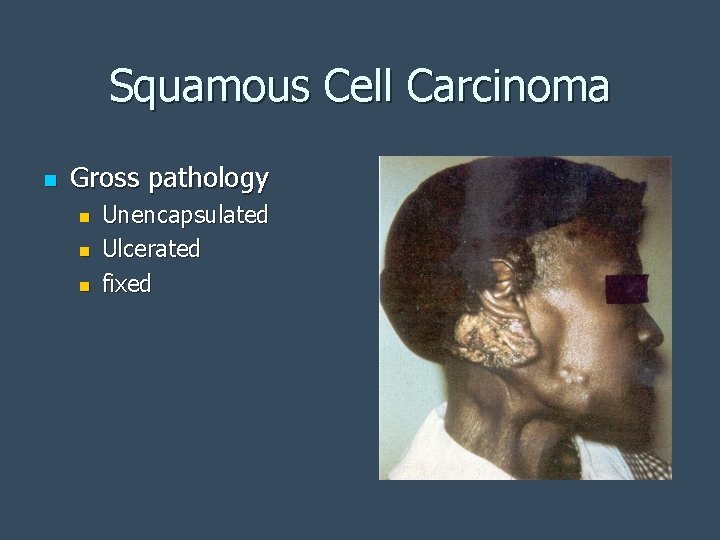
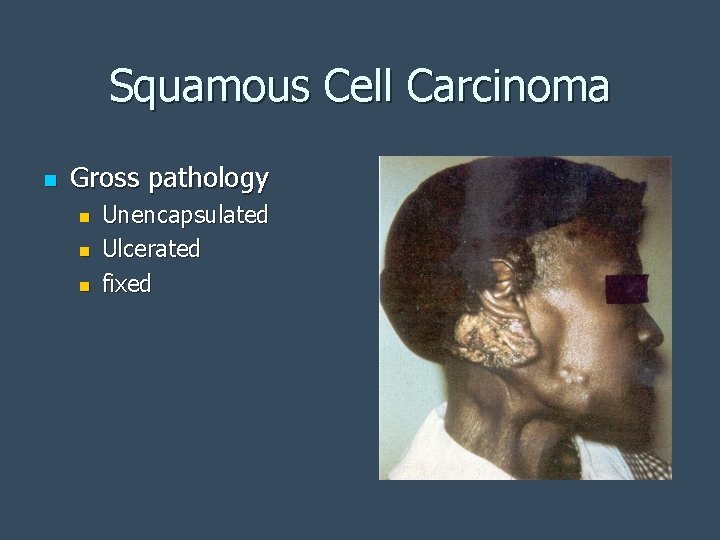
Squamous Cell Carcinoma n Gross pathology n n n Unencapsulated Ulcerated fixed
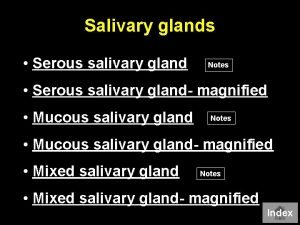
 Serous vs mucous glands
Serous vs mucous glands Basal cell adenoma
Basal cell adenoma Geniohyoid cat
Geniohyoid cat Git
Git Salivary gland disease classification
Salivary gland disease classification Pleomorphic adenoma
Pleomorphic adenoma Salivary gland pathology
Salivary gland pathology Salivary gland swelling
Salivary gland swelling Gastric glands
Gastric glands Warthin's tumor
Warthin's tumor Atresia of salivary gland
Atresia of salivary gland Types of exocrine glands
Types of exocrine glands Submadibular
Submadibular Oncocytoma salivary gland
Oncocytoma salivary gland Oncocytoma salivary gland
Oncocytoma salivary gland Mandicle
Mandicle Enes ylmazer
Enes ylmazer Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Pineal gland pituitary gland
Pineal gland pituitary gland Rasim temur mukavemet 1
Rasim temur mukavemet 1 Rasim temur mukavemet 1
Rasim temur mukavemet 1 Ahmet rasim edebi kişiliği
Ahmet rasim edebi kişiliği Rasim yılmazer
Rasim yılmazer Tek eksenli gerilme
Tek eksenli gerilme Aldasteron
Aldasteron Fosdick test
Fosdick test Minor salivary glands
Minor salivary glands Salivary amylase digestion of starch
Salivary amylase digestion of starch Types of salivary glands
Types of salivary glands Basal cell adenoma
Basal cell adenoma Dysphagia terminology
Dysphagia terminology Sublingual gland pig
Sublingual gland pig Git organs
Git organs Sialography
Sialography Function of salivary glands
Function of salivary glands Albans test is an example of
Albans test is an example of Minor salivary glands
Minor salivary glands Minor salivary glands
Minor salivary glands Public health entomology certificate
Public health entomology certificate Chapter 23 lesson 1 understanding communicable diseases
Chapter 23 lesson 1 understanding communicable diseases Chapter 24 lesson 1 sexually transmitted diseases
Chapter 24 lesson 1 sexually transmitted diseases