SALIVARY TUMORS AND CALCULI Prof Yasser Hamza Professor















- Slides: 79
SALIVARY TUMORS AND CALCULI Prof. Yasser Hamza Professor of Surgery Faculty of Medicine, University of Alexandria

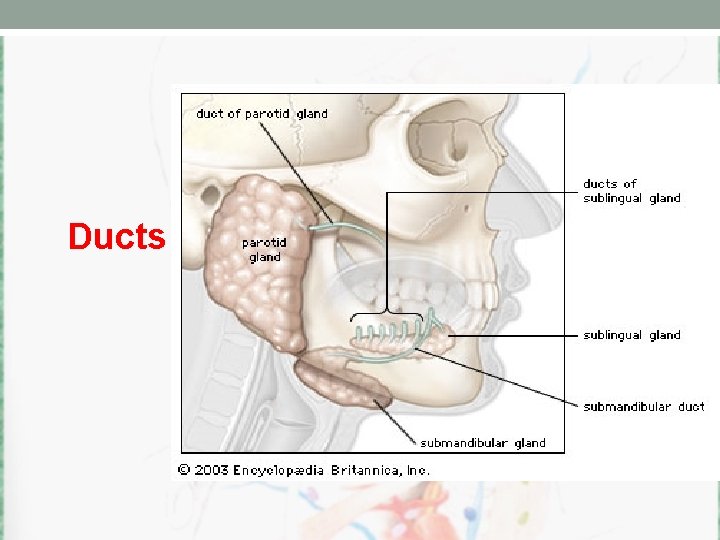
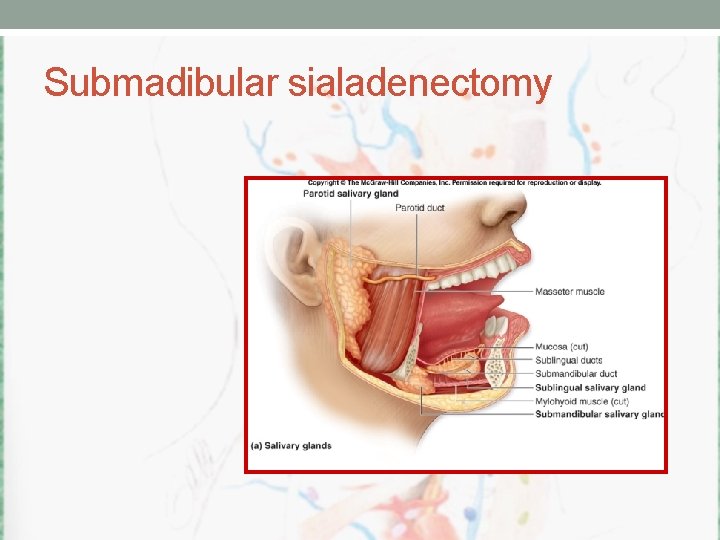
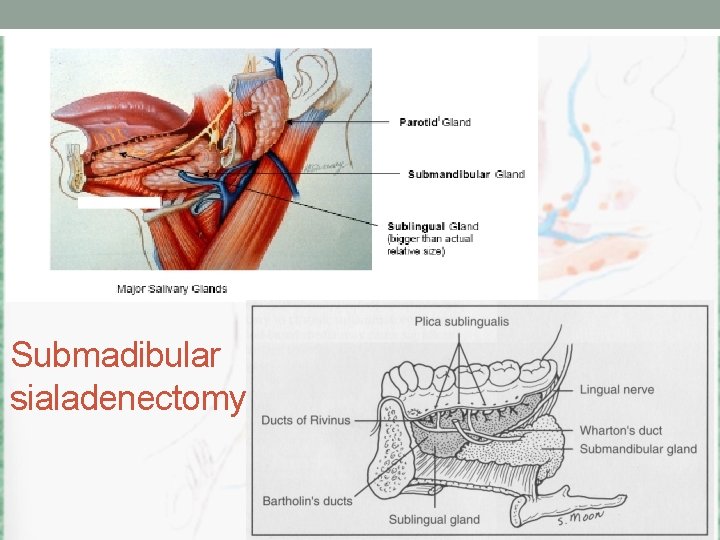
Anatomical Considerations • Two submandibular • Two Parotid • Two sublingual • > 400 minor salivary glands
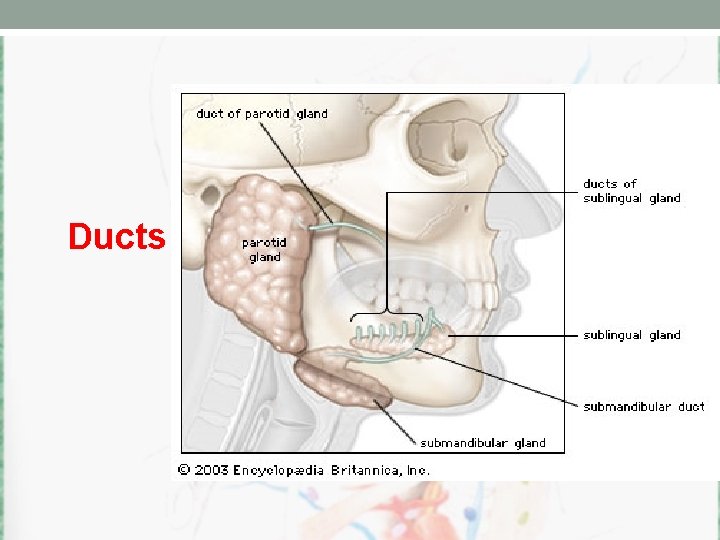
Ducts
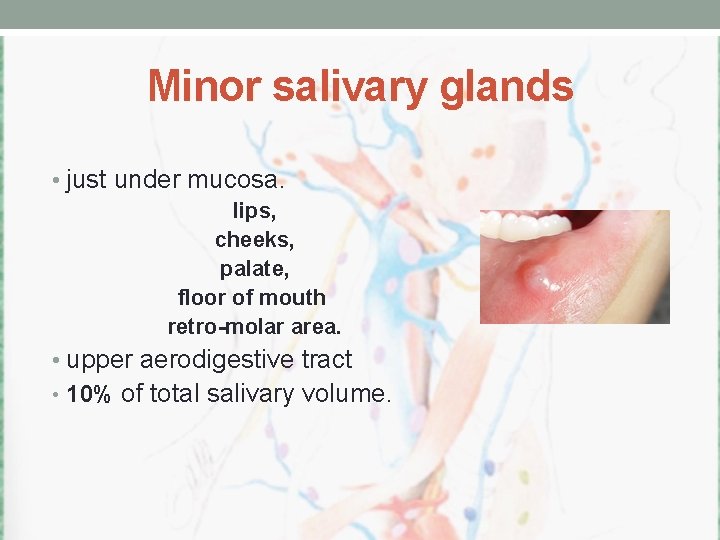
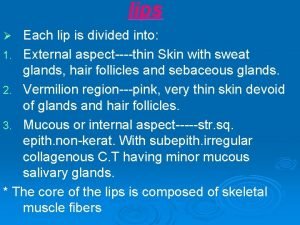
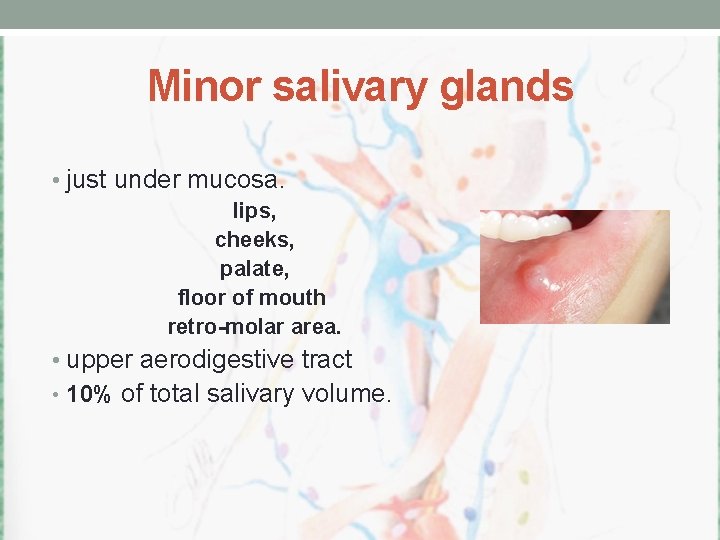
Minor salivary glands • just under mucosa. lips, cheeks, palate, floor of mouth retro-molar area. • upper aerodigestive tract • 10% of total salivary volume.
Clinical History • History of swellings / change over time • Trismus • Pain • Variation with meals • Bilateral • Dry mouth. dry eyes • Recent exposure to mumps • Radiation history • Current medications
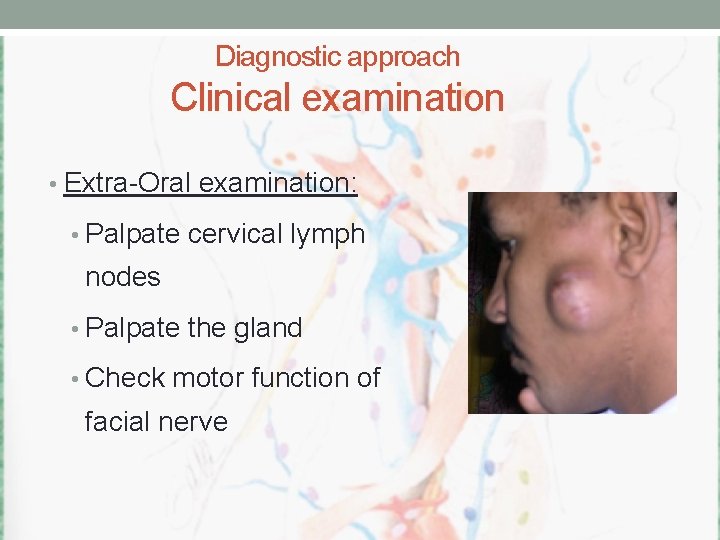
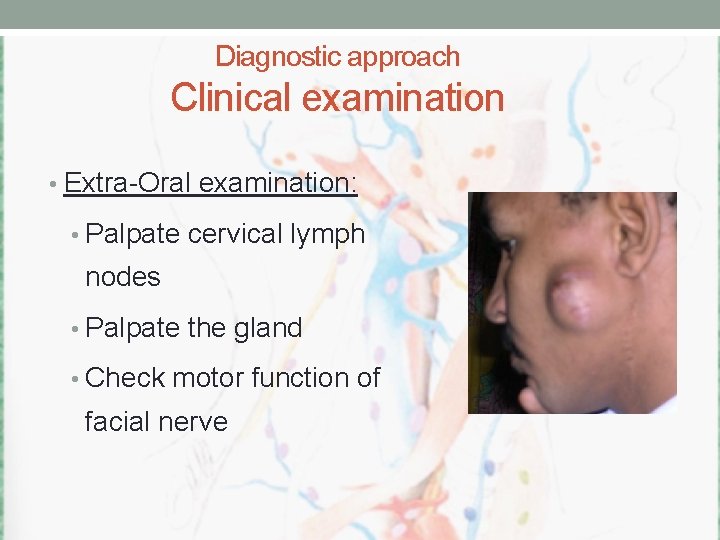
Diagnostic approach Clinical examination • Extra-Oral examination: • Palpate cervical lymph nodes • Palpate the gland • Check motor function of facial nerve
Diagnostic approach Clinical examination. • Intra-Oral examination: • Gland orifice • Teeth problems • Oral hyegene • Lemon test • Bi-digital palpaption
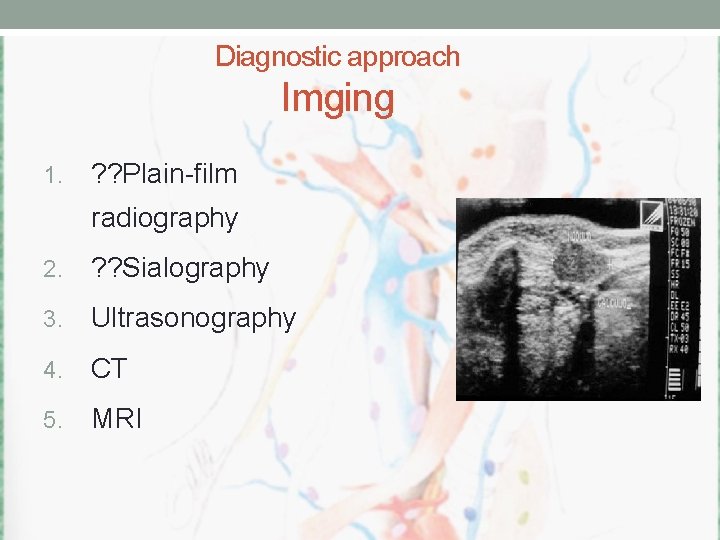
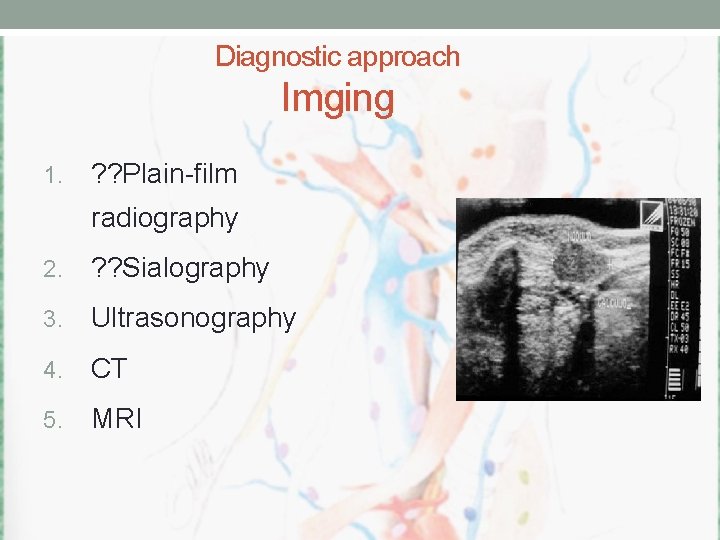
Diagnostic approach Imging 1. ? ? Plain-film radiography 2. ? ? Sialography 3. Ultrasonography 4. CT 5. MRI
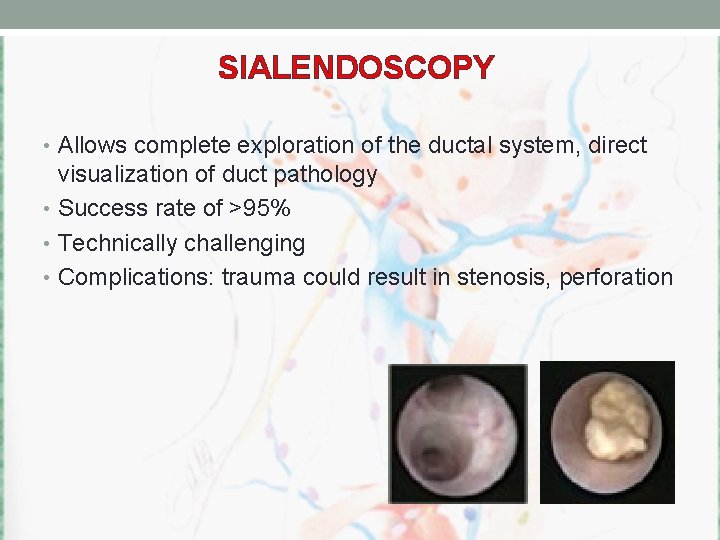
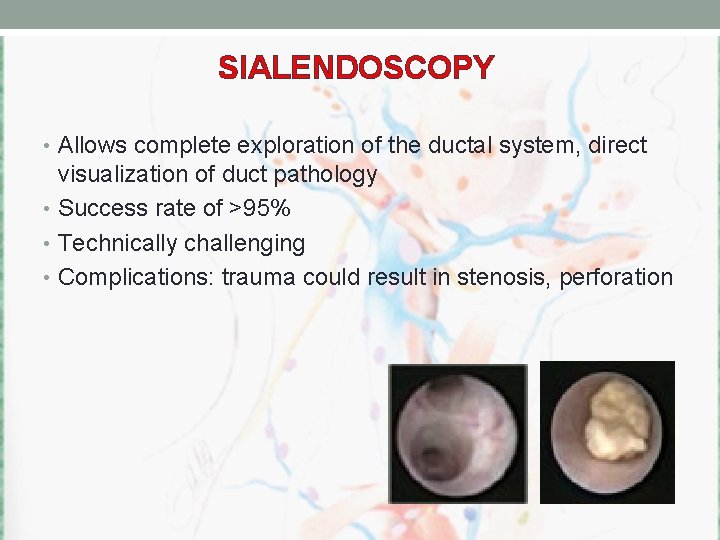
SIALENDOSCOPY • Allows complete exploration of the ductal system, direct visualization of duct pathology • Success rate of >95% • Technically challenging • Complications: trauma could result in stenosis, perforation
Obstructive Salivary Gland Disorders • Sialolithiasis • Mucous retention/extravasation
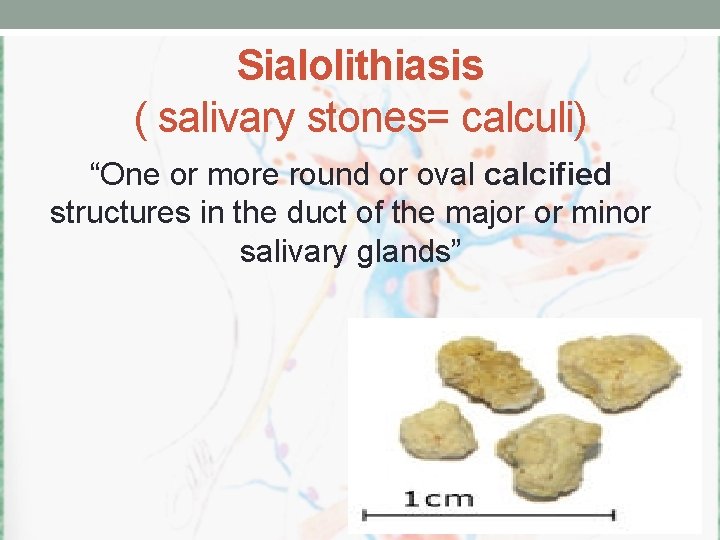
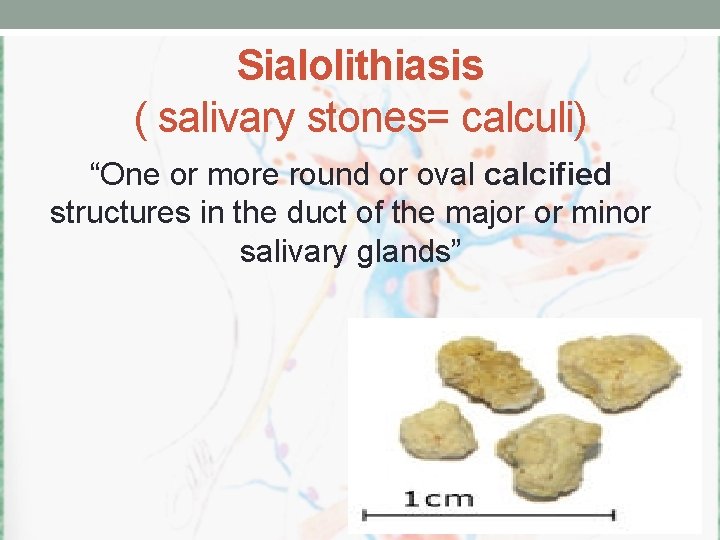
Sialolithiasis ( salivary stones= calculi) “One or more round or oval calcified structures in the duct of the major or minor salivary glands”
Salivary calculi • Submandibular Most common • Pain subsides before swelling. • Recurrent painful swelling at mealtime • Acute & subacute infection • Persistent obstruction leads to permanent damages to the gland.

Obstructive SG Disorders: Sialolithiasis • results in a mechanical obstuction of the salivary duct • Is the major cause of unilateral diffuse parotid or submandibular gland swelling
Sialolithiasis • exact pathogenesis unknown. • organic nidus that progressively grows by deposition of layers of inorganic and organic substances.
Etiology • Water hardness • Hypercalcemia • Xerostomia • Tobacco smoking • Gout.
Sialolithiasis Acute ductal obstruction may occur at meal time when saliva producing is at its maximum, the resultant swelling is sudden and can be painful.

Stone Composition • Organic; often predominate in the center • Glycoproteins • Mucopolysaccarides • Bacteria! • Cellular debris • Inorganic; often in the periphery • Calcium carbonates & calcium phosphates in the form of hydroxyapatite
Reasons sialolithiasis may occur more often in the submandibular gland • Saliva more alkaline • Higher concentration of calcium and phosphate in the saliva • Higher mucus content • Longer duct • Anti-gravity flow
Obstructive Salivary Gland Disorders • Sialolithiasis • Mucous retention/extravasation
Mucocele Extravasation is the leakage of fluid from the ducts or acini into the surrounding tissue. Retention: narrowed ductal opening that cannot adequately accommodate the exit of saliva produced, leading to ductal dilation and surface swelling. Less common phenomenon

Ranula • Is a term used for mucoceles that occur in the floor of the mouth. • The name is derived form the word rana, because the swelling may resemble the translucent underbelly of the frog.
Ranula • Although the source is usually the sublingual gland, • may also arise from the submandibular duct • or possibly the minor salivary glands in the floor of the mouth.
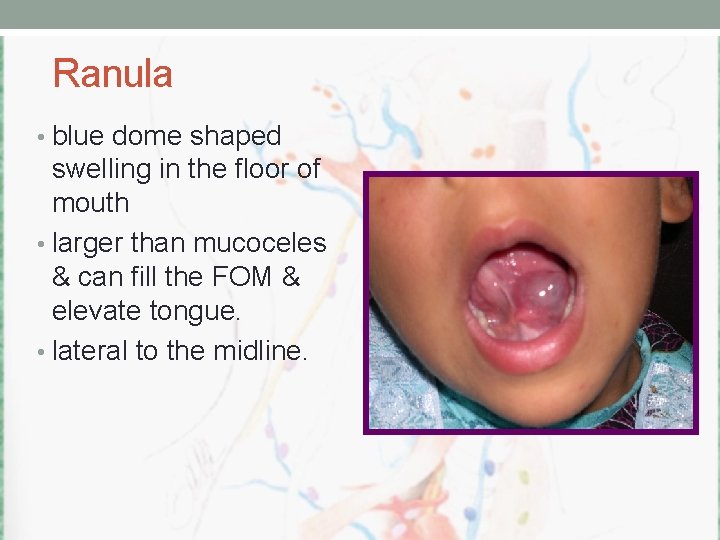
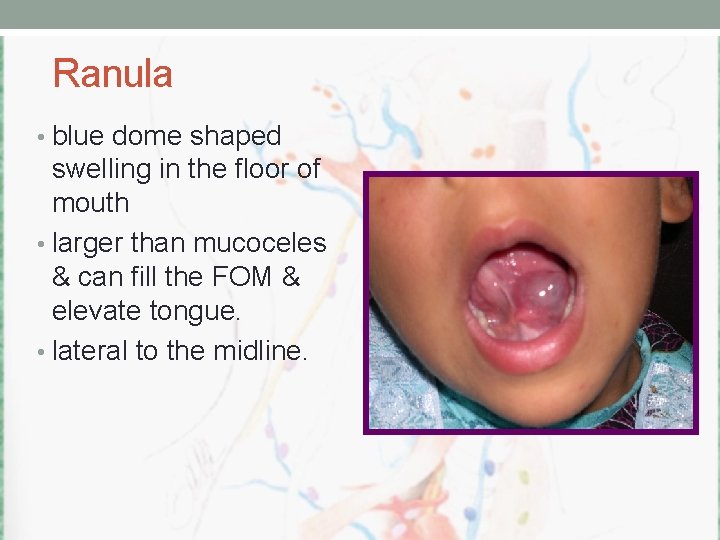
Ranula • blue dome shaped swelling in the floor of mouth • larger than mucoceles & can fill the FOM & elevate tongue. • lateral to the midline.
Plunging or Cervical Ranula • Occurs when spilled mucin dissects through the mylohyoid muscle and produces swelling in the neck. • Concomitant FOM swelling may or may not be visible.

Ranula Treatment • Marsupialization has fallen into disfavor due to the excessive recurrence rate of 60 -90% • Sublingual gland removal via intraoral approach
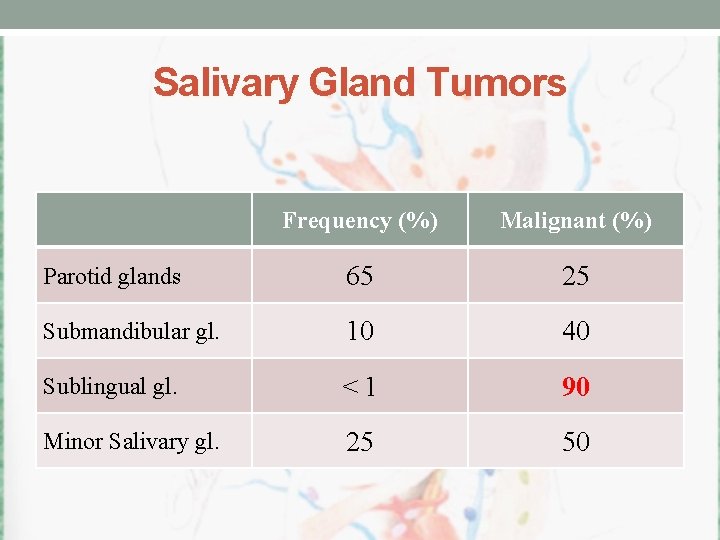
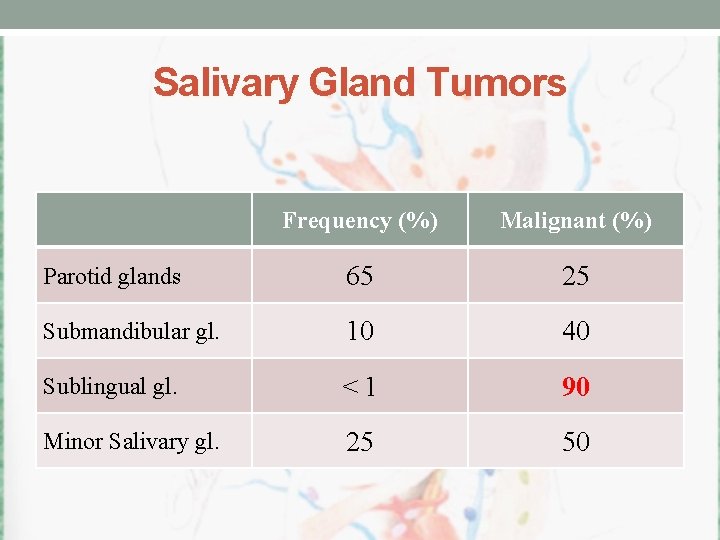
Salivary Gland Tumors Frequency (%) Malignant (%) Parotid glands 65 25 Submandibular gl. 10 40 Sublingual gl. < 1 90 Minor Salivary gl. 25 50
Benign tumors of the parotid Pleomorphic adenoma (benign mixed tumor). 2. Warthin’s tumor (papillary cyst adenoma lypmhomatosum). 3. Monomorphic adenoma a. Basal cell adenoma b. Canalicular adenomas c. Oncocytoma d. Myoepitheliomas 4. Granular cell tumor 5. ? ? Hemangioma 1.
Malignant neoplasm of the parotid gland 1. Mucoepidermoid carcinoma 40% 2. Adenoid cystic carcinoma 10% 3. Acinic cell carcinoma 10 – 15 % 4. Malignant mixed tumor 7% 5. Polymorphous low grade adenocarcinoma 10% 6. Adeno carcinoma 10% 7. Squamous cell carcinoma 4%
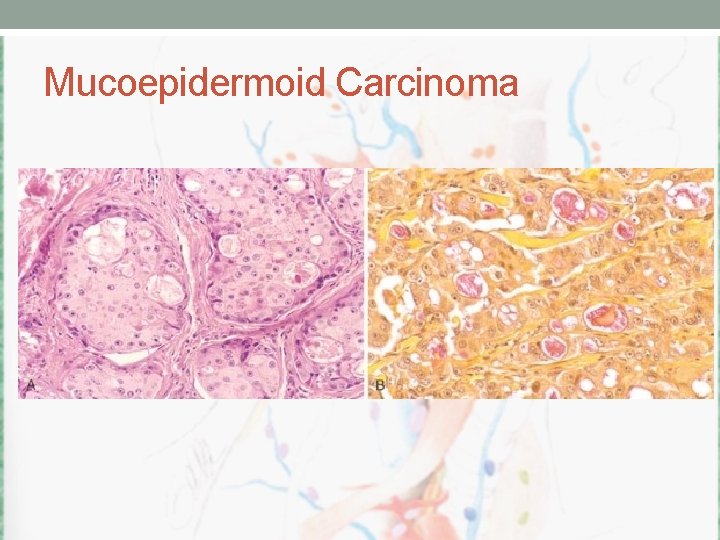
Malignant neoplasm of the parotid gland 1. Mucoepidermoid carcinoma – 40% Can be: high, intermediate, and low-grade based on the clinical behavior and the tumor differentiation which is related to the percentage of mucinous to epidermoid cell.
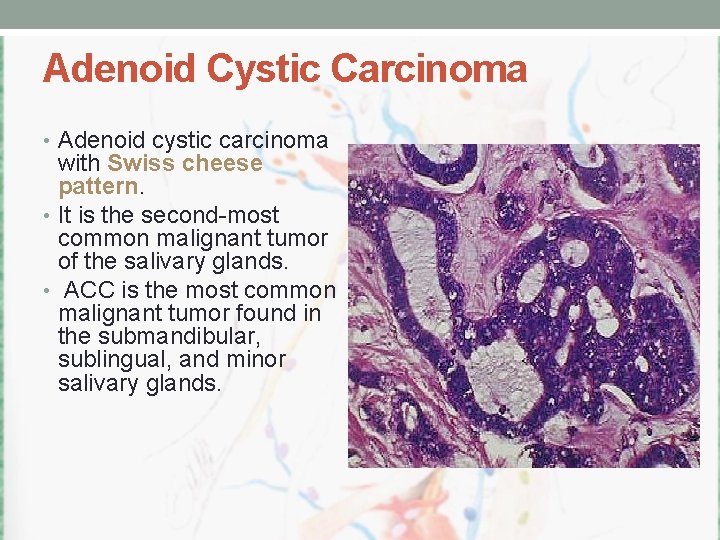
Malignant neoplasm of the parotid gland 2. Adenoid cystic carcinoma – 10% unique indolent preneural spread skip lesions. The disease thus specific survival continuous to declined for more than 20 years after initial treatment.
3. Acinic cell carcinoma – 10 – 15 % a low-grade tumor. 4. Malignant mixed tumor - 7% a high-grade malignancy. 5. Polymorphous low grade adenocarcinoma – 10% a low-grade variant of adenocarcinoma. 6. Adeno carcinoma – 10% high-grade with poor prognosis. 7. Squamous cell carcinoma – 4% It is high-grade more common in elderly patients can confused with high-grade mucoepidermoid carcinoma.
The malignant parotid tumor can be classified into: 1. High-grade: aggressive behavior, local invasion, and lymph node metastasis. - high grade mucoepidermoid carcinoma - adenoid cystic carcinoma - carcinoma ex phelomorphic adenoma - adenocarcinoma - aquamous cell carcinoma - undifferentiated carcinoma
The malignant parotid tumor can be classified into: 2. Intermediate grade - intermediate grade mucoepidermoid carcinoma - intermediate grade adenocarcinoma - oncocytic carcinoma
The malignant parotid tumor can be classified into: 3. Low-grade malignancy - low grade mucoepidermoid carcinoma - pholymorphous low grade adenocarcinoma - acinic cell carcinoma - low grade adenocarcinoma - basal cell carcinoma
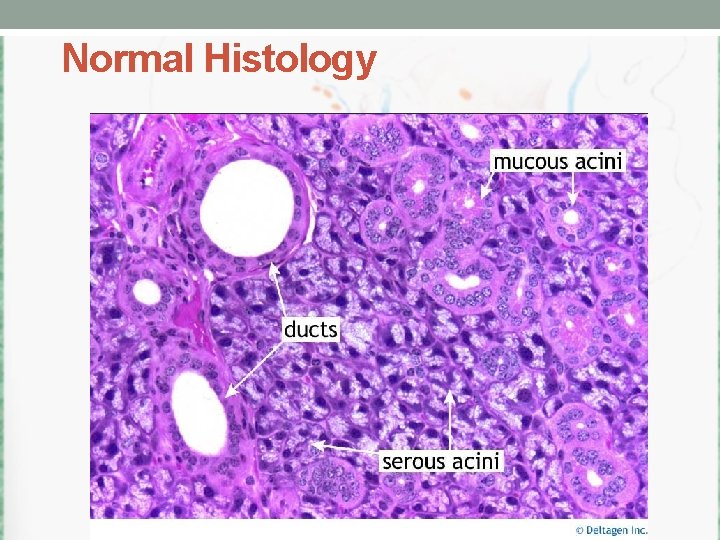
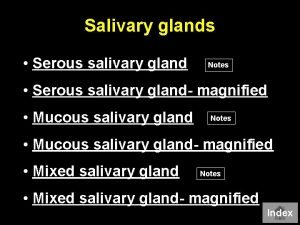
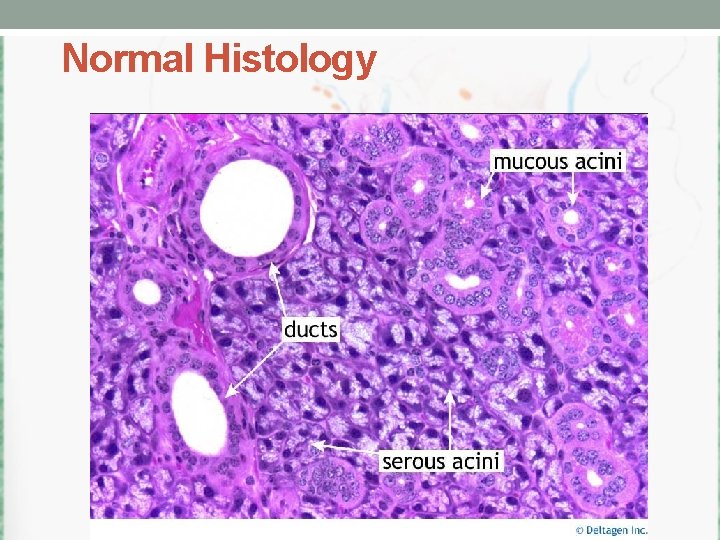
Normal Histology
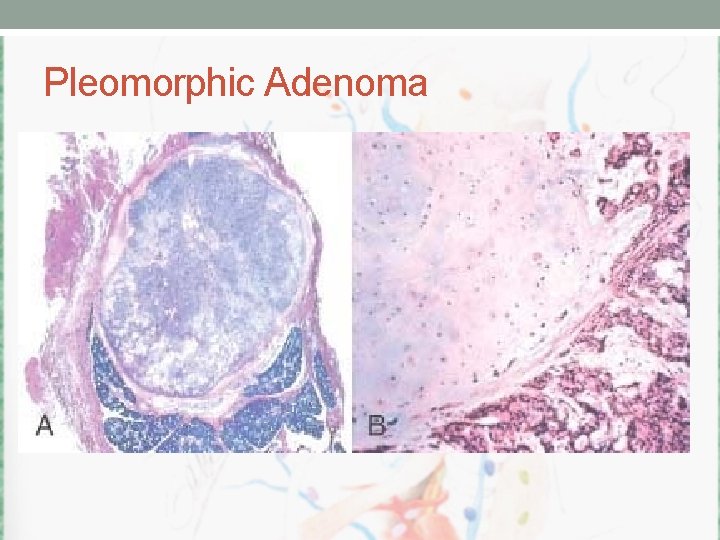
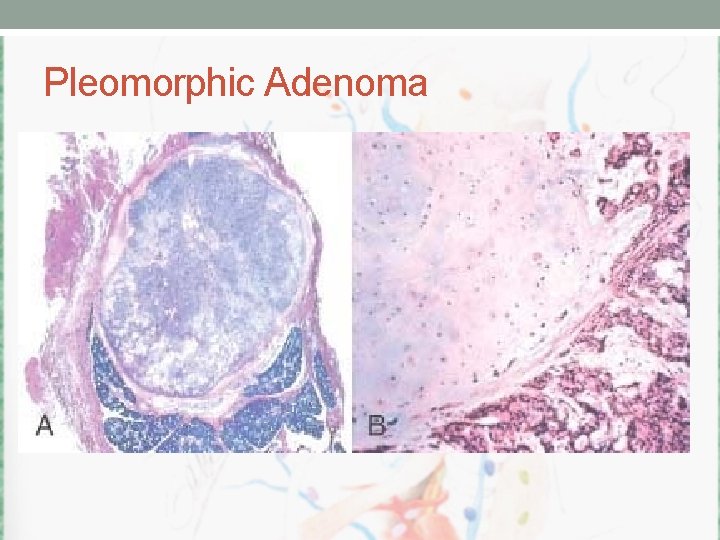
Pleomorphic Adenoma

Pleomorphic Adenoma • pleomorphic adenoma contains both epithelial (E) and stromal (S) components.
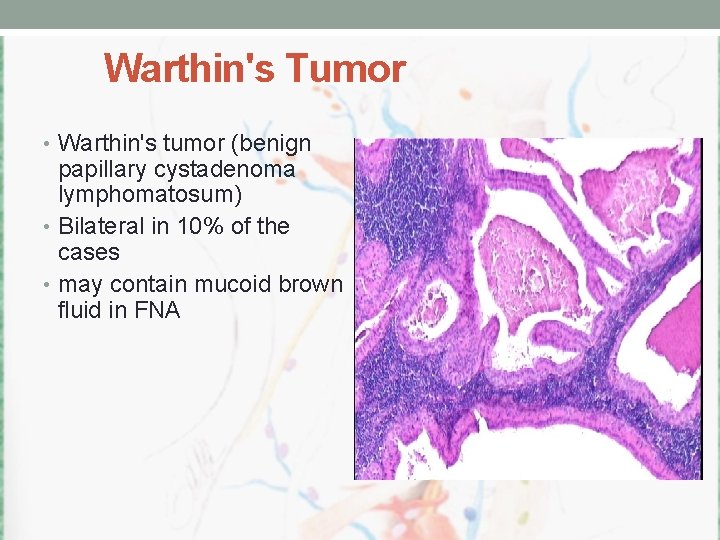
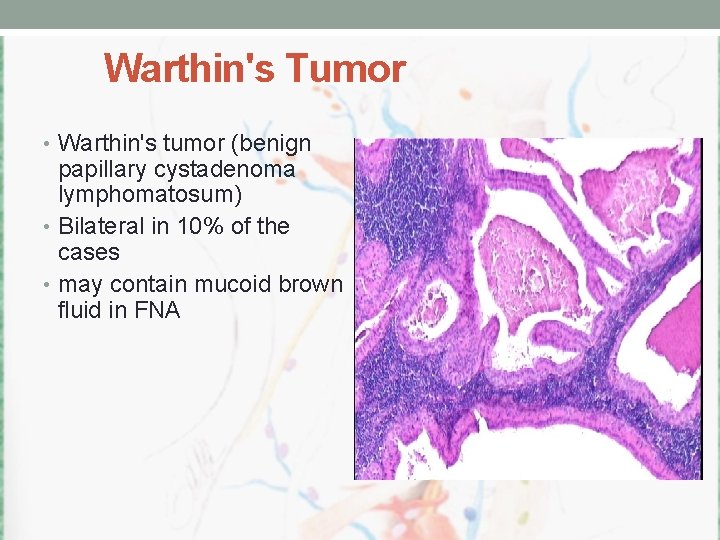
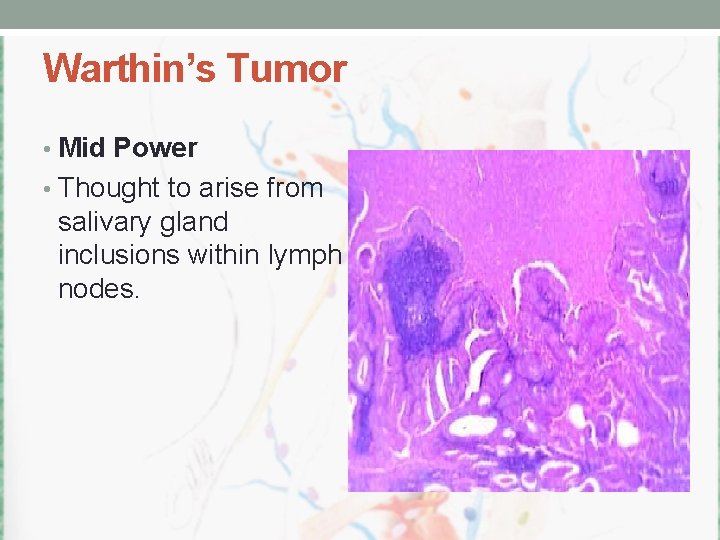
Warthin's Tumor • Warthin's tumor (benign papillary cystadenoma lymphomatosum) • Bilateral in 10% of the cases • may contain mucoid brown fluid in FNA
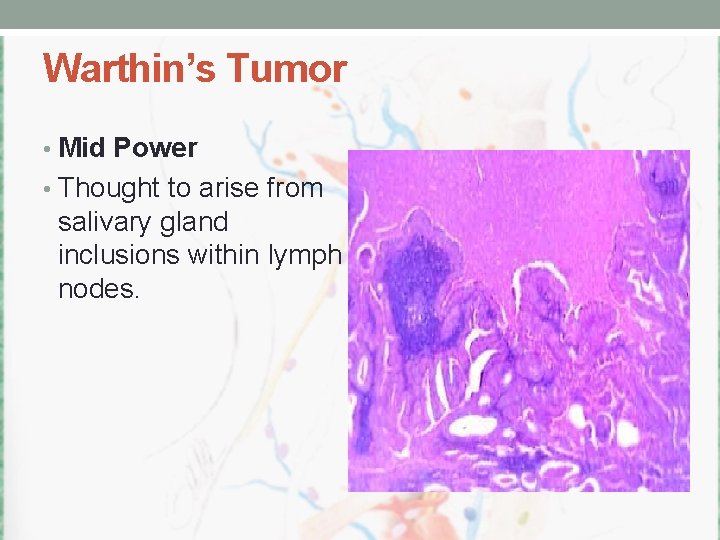
Warthin’s Tumor • Mid Power • Thought to arise from salivary gland inclusions within lymph nodes.
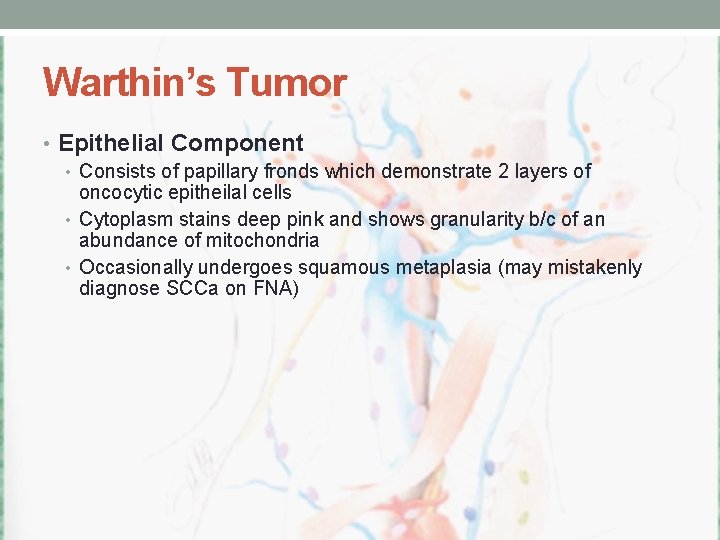
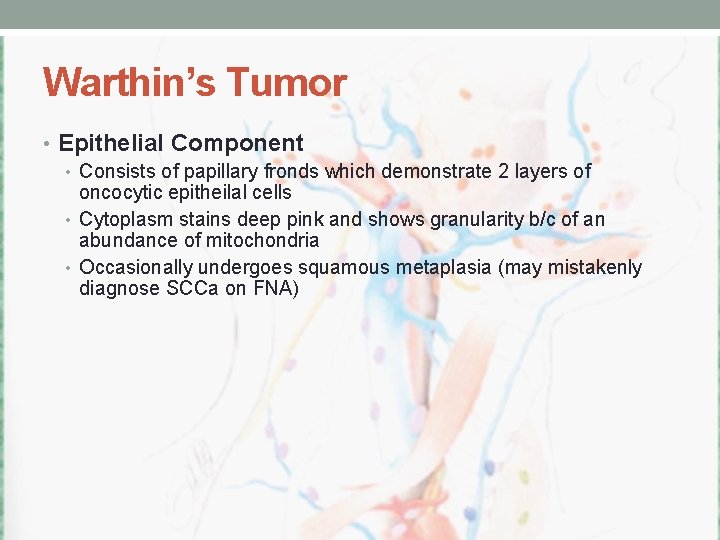
Warthin’s Tumor • Epithelial Component • Consists of papillary fronds which demonstrate 2 layers of oncocytic epitheilal cells • Cytoplasm stains deep pink and shows granularity b/c of an abundance of mitochondria • Occasionally undergoes squamous metaplasia (may mistakenly diagnose SCCa on FNA)

Warthin’s Tumor • Lymphoid Component • An abundance of this is present • Occasional germinal centres will be seen • Lymphoid tissue forms the core or papillary structures • Both lymphoid and oncocytic epithelial elements must be present to diagnose Warthin’s
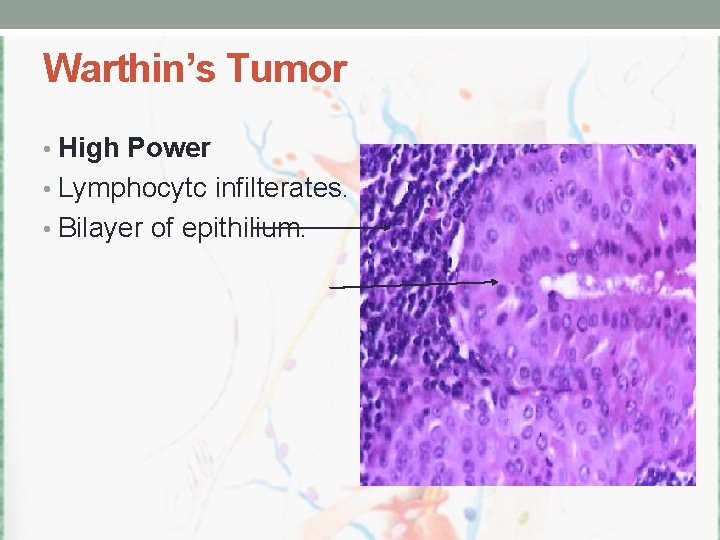
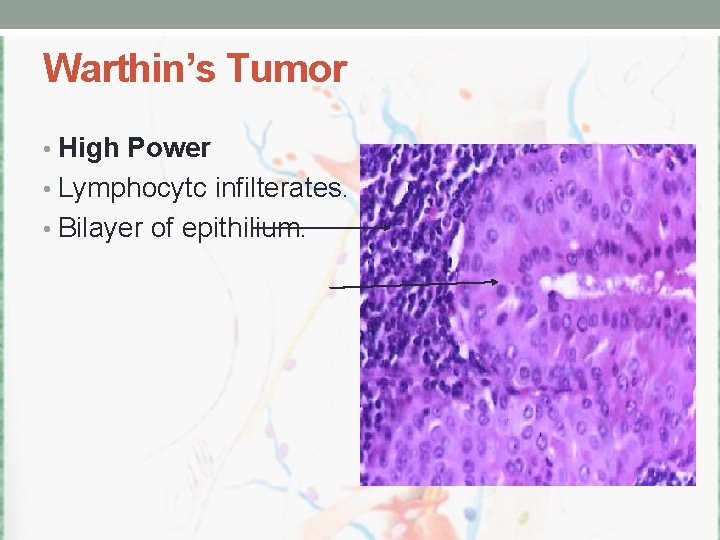
Warthin’s Tumor • High Power • Lymphocytc infilterates. • Bilayer of epithilium.
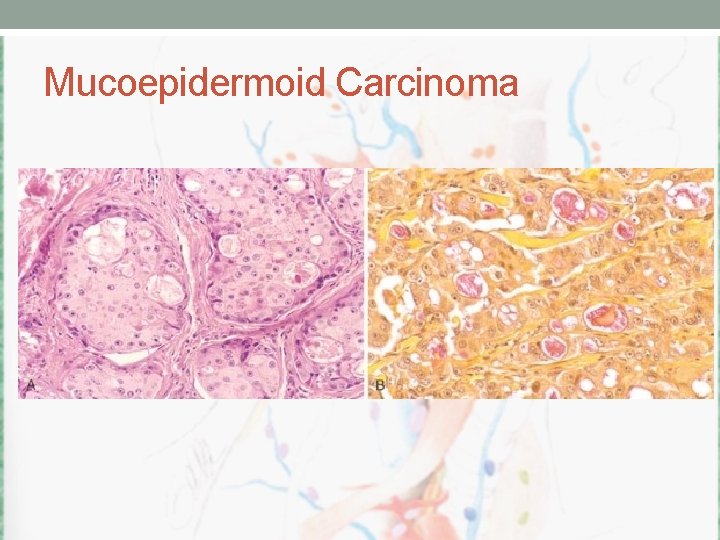
Mucoepidermoid Carcinoma
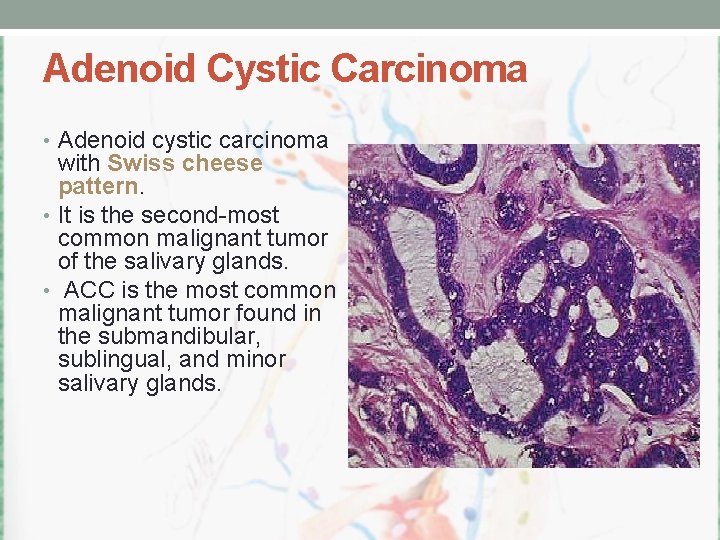
Adenoid Cystic Carcinoma • Adenoid cystic carcinoma with Swiss cheese pattern. • It is the second-most common malignant tumor of the salivary glands. • ACC is the most common malignant tumor found in the submandibular, sublingual, and minor salivary glands.

Acinic Cell Carcinoma • mainly in the parotid gland, also known as blue dot tumor. • Classic multicystic pattern. • Stained by PAS. • Cells heavily stained.
Treatment • Surgery – Total conservative – Total – Extended – +/- RND
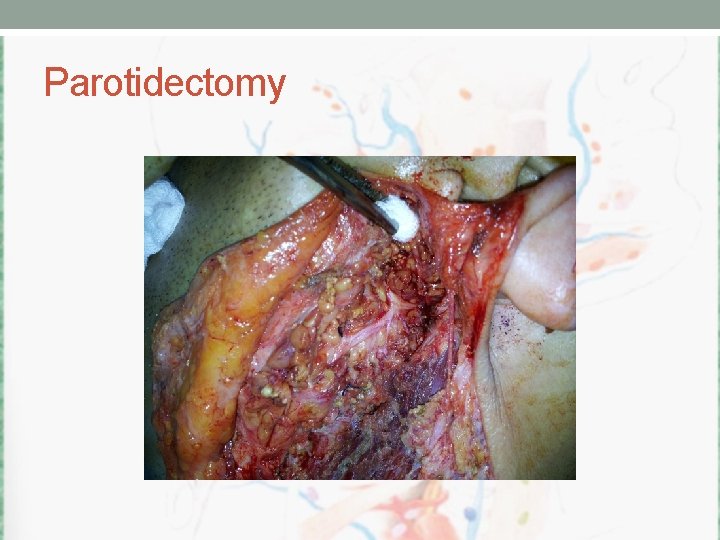
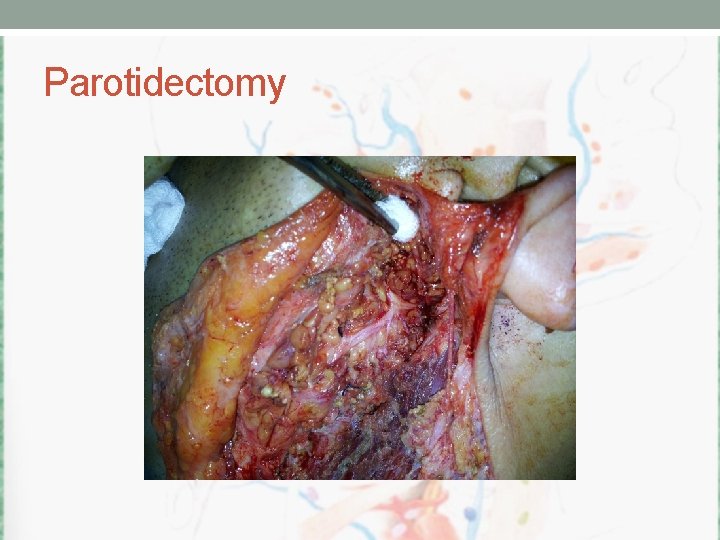
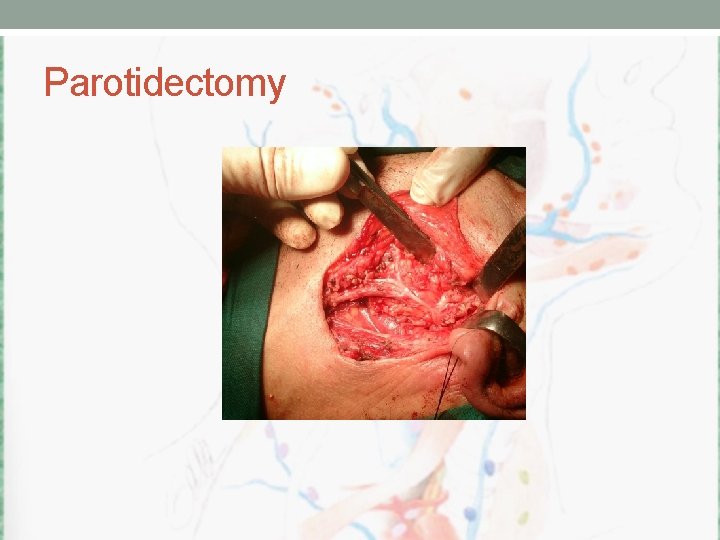
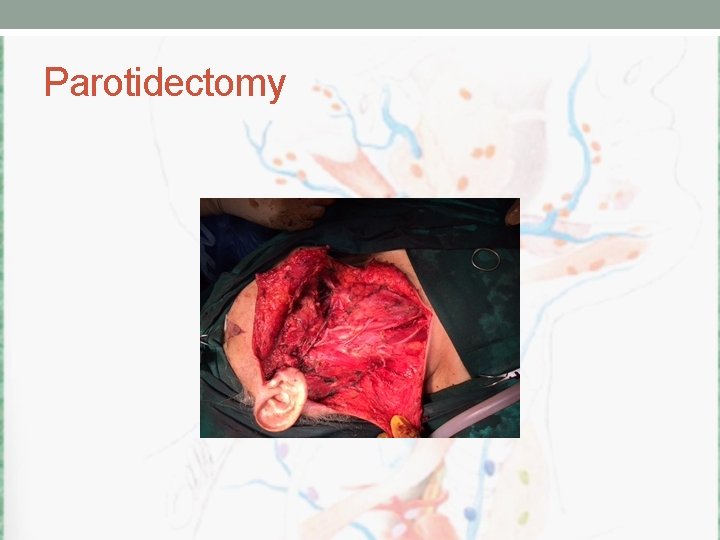
Parotidectomy
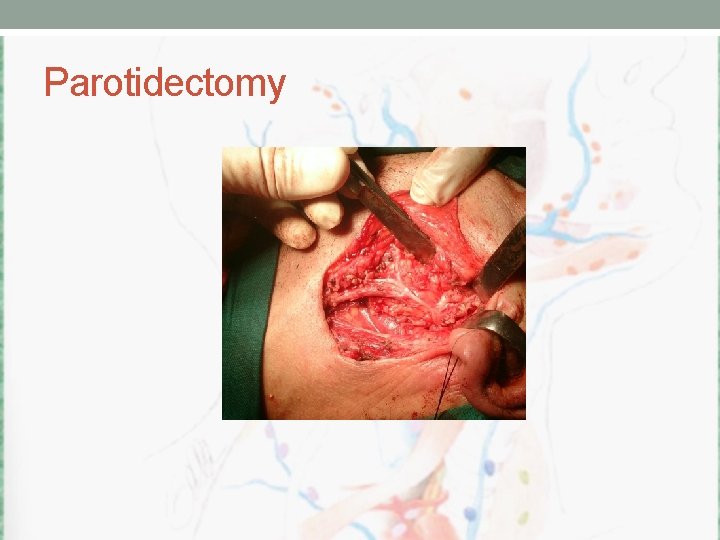
Parotidectomy
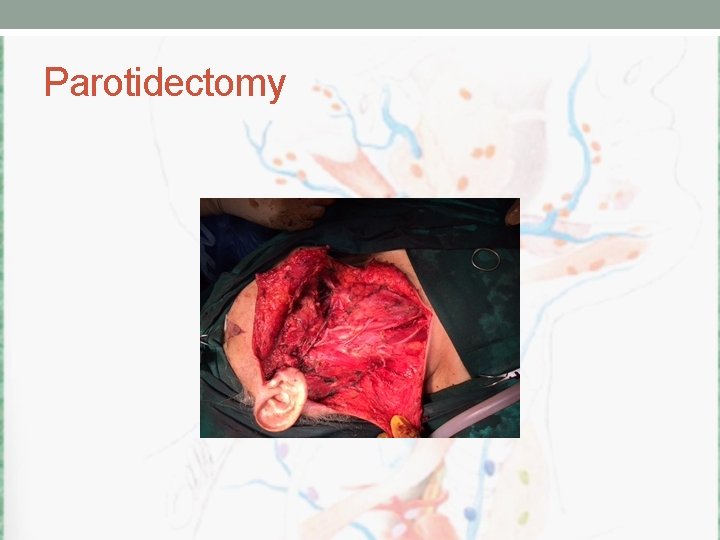
Parotidectomy

Parotidectomy
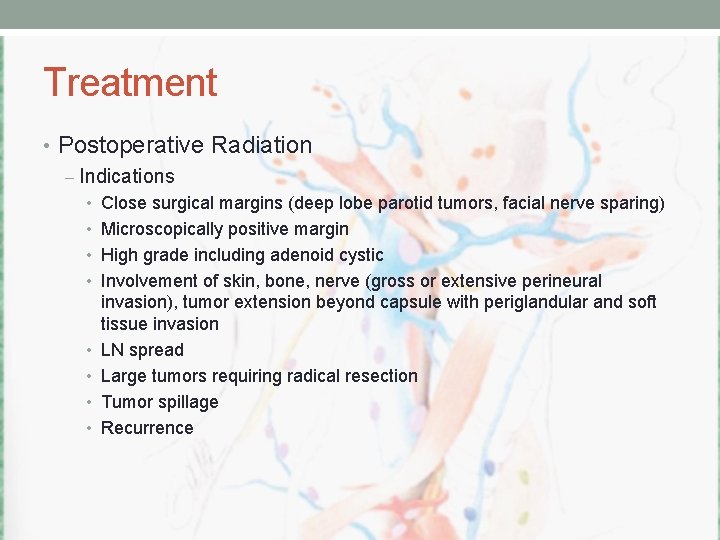
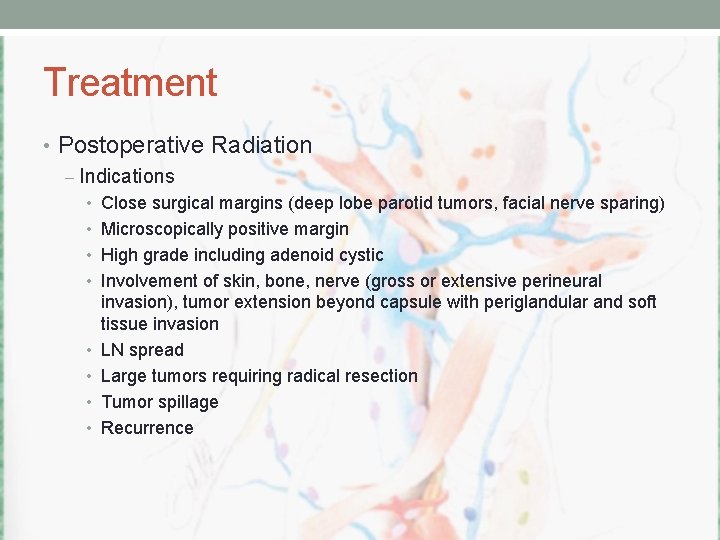
Treatment • Postoperative Radiation – Indications • Close surgical margins (deep lobe parotid tumors, facial nerve sparing) • Microscopically positive margin • High grade including adenoid cystic • Involvement of skin, bone, nerve (gross or extensive perineural • • invasion), tumor extension beyond capsule with periglandular and soft tissue invasion LN spread Large tumors requiring radical resection Tumor spillage Recurrence
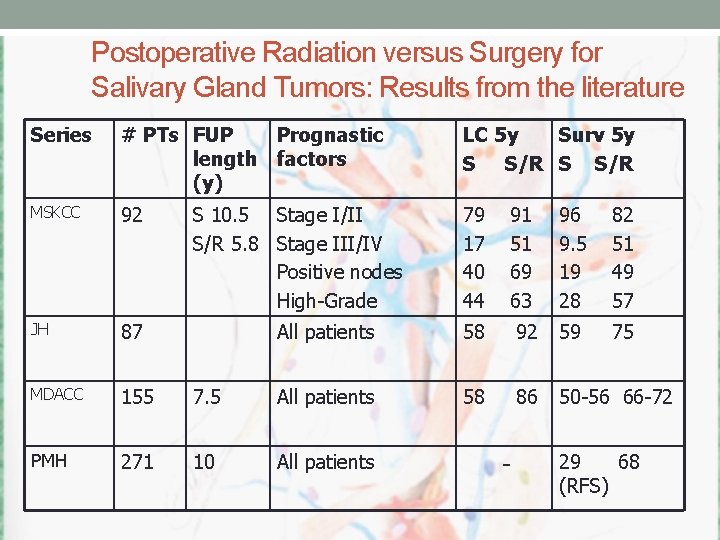
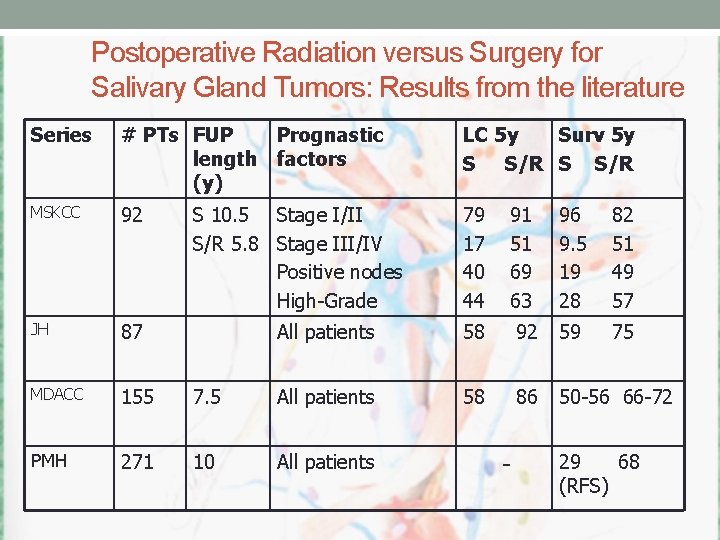
Postoperative Radiation versus Surgery for Salivary Gland Tumors: Results from the literature Series # PTs FUP Prognastic length factors (y) LC 5 y Surv 5 y S S/R MSKCC 92 79 17 40 44 JH 87 MDACC 155 PMH 271 S 10. 5 Stage I/II S/R 5. 8 Stage III/IV Positive nodes High-Grade 91 51 69 63 96 9. 5 19 28 82 51 49 57 75 All patients 58 92 59 7. 5 All patients 58 86 50 -56 66 -72 10 All patients - 29 68 (RFS)
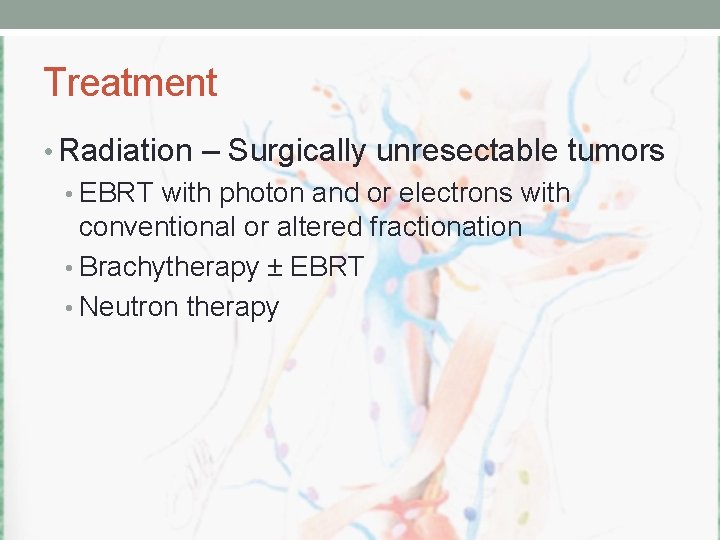
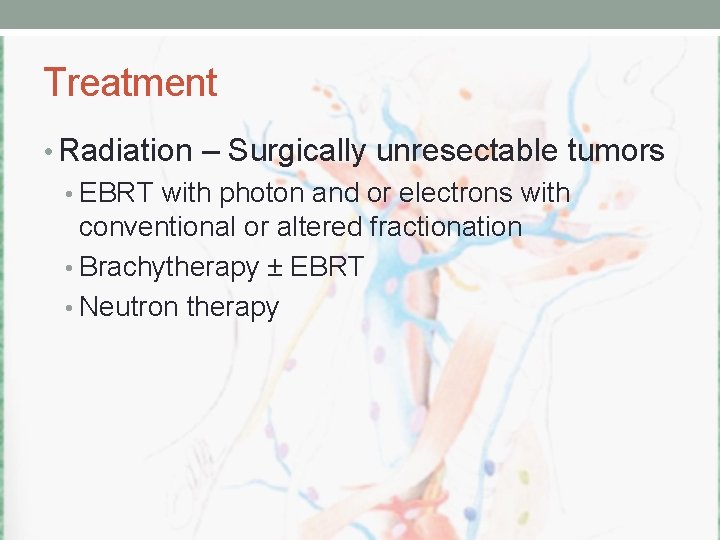
Treatment • Radiation – Surgically unresectable tumors • EBRT with photon and or electrons with conventional or altered fractionation • Brachytherapy ± EBRT • Neutron therapy
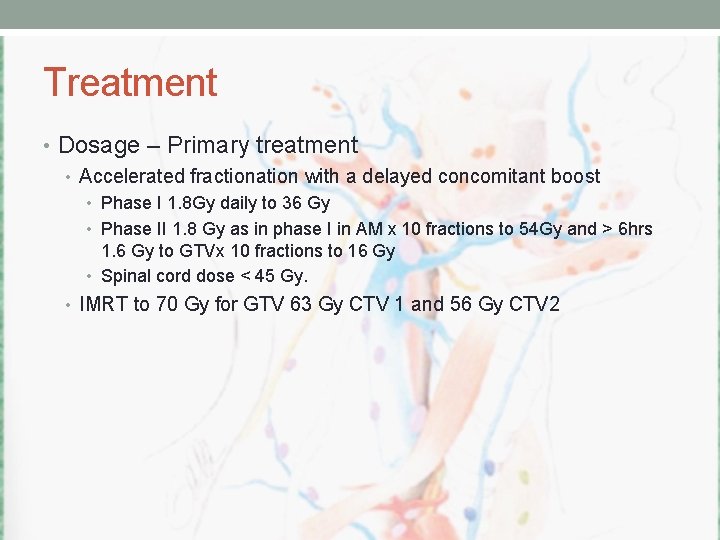
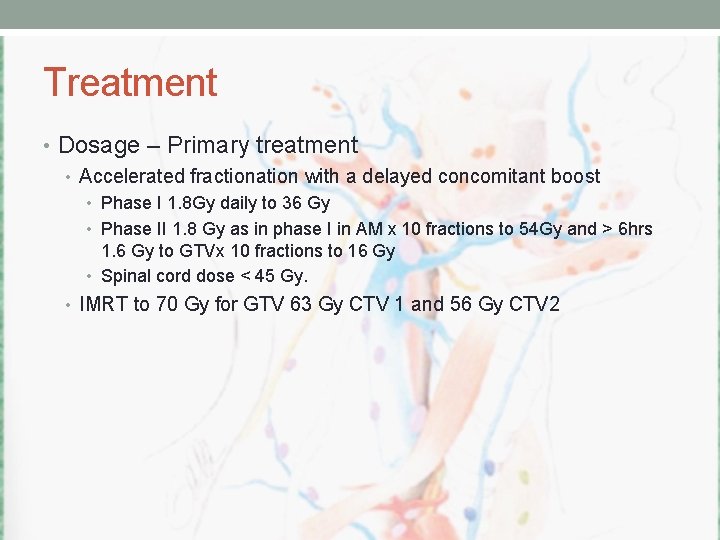
Treatment • Dosage – Primary treatment • Accelerated fractionation with a delayed concomitant boost • Phase I 1. 8 Gy daily to 36 Gy • Phase II 1. 8 Gy as in phase I in AM x 10 fractions to 54 Gy and > 6 hrs 1. 6 Gy to GTVx 10 fractions to 16 Gy • Spinal cord dose < 45 Gy. • IMRT to 70 Gy for GTV 63 Gy CTV 1 and 56 Gy CTV 2
Treatment • Dosage – Post op treatment • Administered within 6 weeks of surgery • High Risk 2. 0 Gy/fx to 60 Gy and 1. 8 Gy/fx to 63 Gy. • Small volume known microscopic disease 66 Gy. • Elective at risk 50 Gy (2. 0 Gy/fx) 54 Gy(1. 8 Gy/fx) • Gross residual 70 Gy.
Side effects • Salivary fxn • 80% of saliva produced by major salivary glands • Loss of salivary fxn complete >35 Gy • Dose limit to spare salivary function is 26 Gy. • Trismus • TMJ and masseter muscle < 50 Gy. PT during and after treatment
Adenoid Cystic Carcinoma • Post op RT always recommended • Post op RT of entire pathway of adjacent cranial nerve to base of skull always recommended • Regional LN spread is 15% and elective nodal irradiation is not standard • Surgery alone LCR 25 -40% +RT 75%-80%

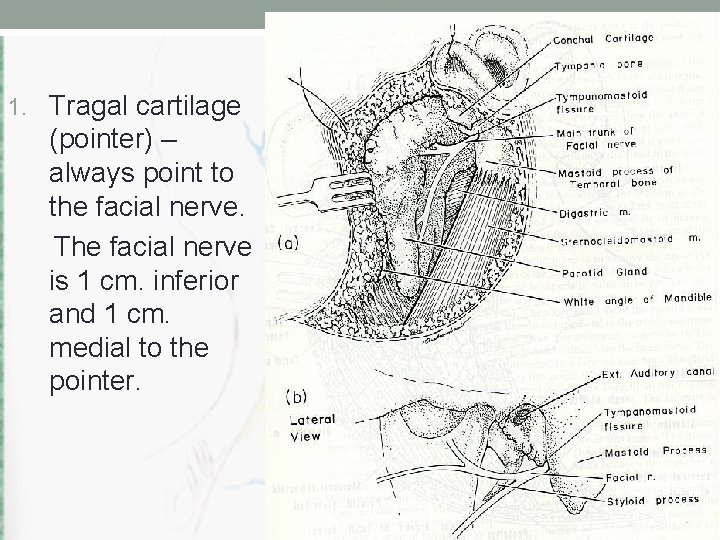
LOCALIZATION OF THE FACIAL NERVE
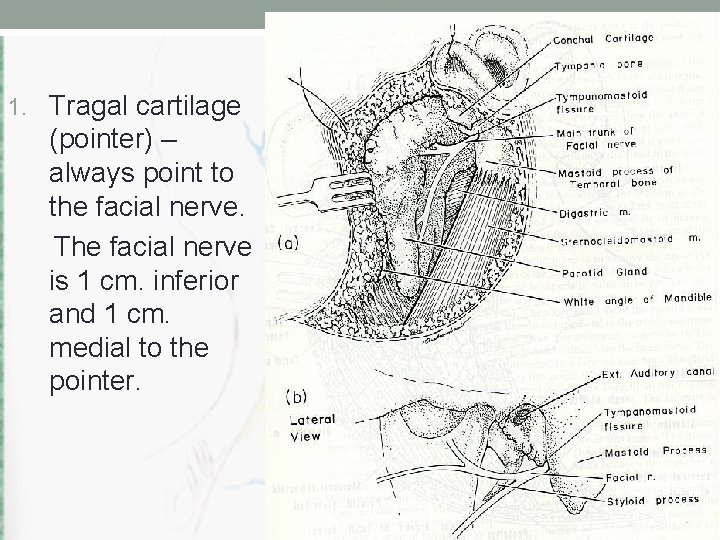
1. Tragal cartilage (pointer) – always point to the facial nerve. The facial nerve is 1 cm. inferior and 1 cm. medial to the pointer.

2. Tympanomastoid fissure – FN is 4 mm inferior to the tympano mastoid fissure as it exit from the stylo mastoid foramen.
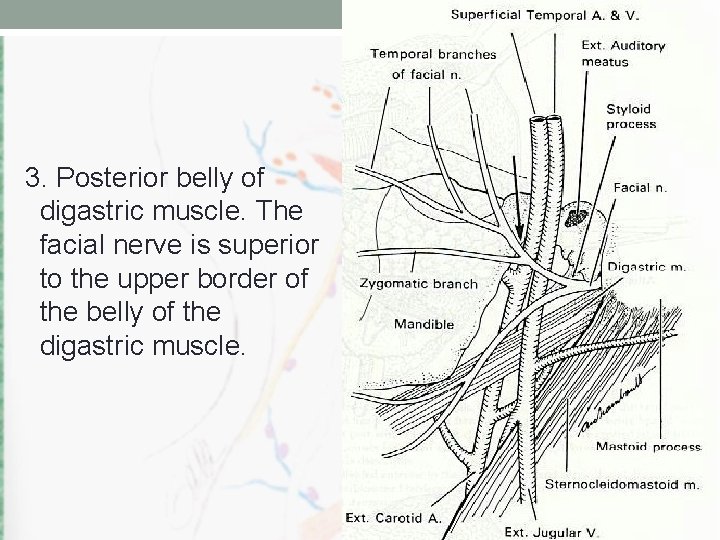
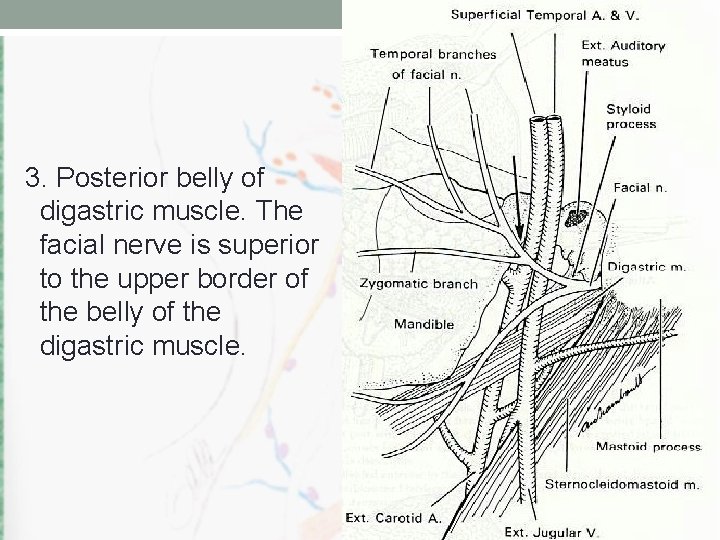
3. Posterior belly of digastric muscle. The facial nerve is superior to the upper border of the belly of the digastric muscle.
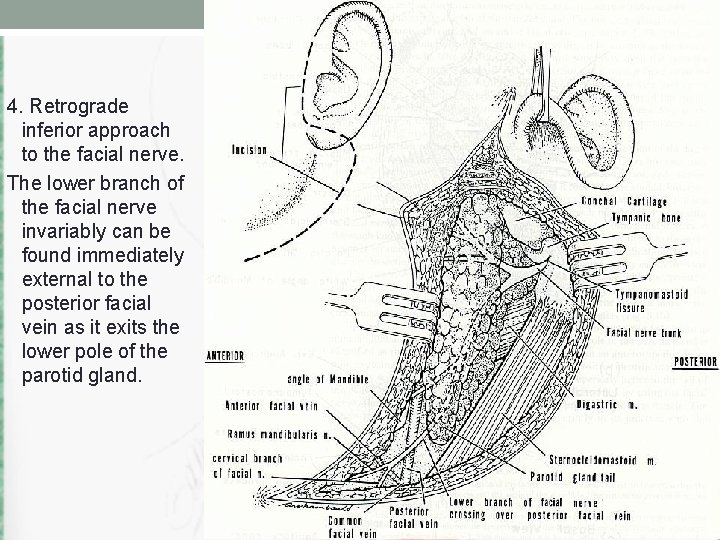
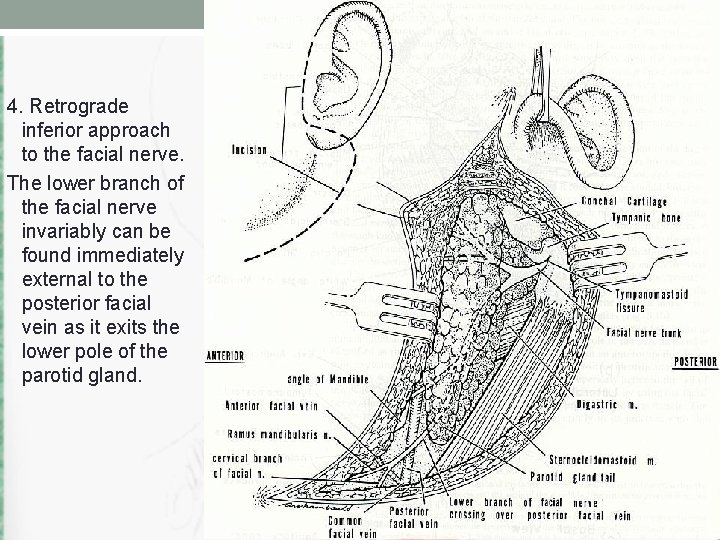
4. Retrograde inferior approach to the facial nerve. The lower branch of the facial nerve invariably can be found immediately external to the posterior facial vein as it exits the lower pole of the parotid gland.
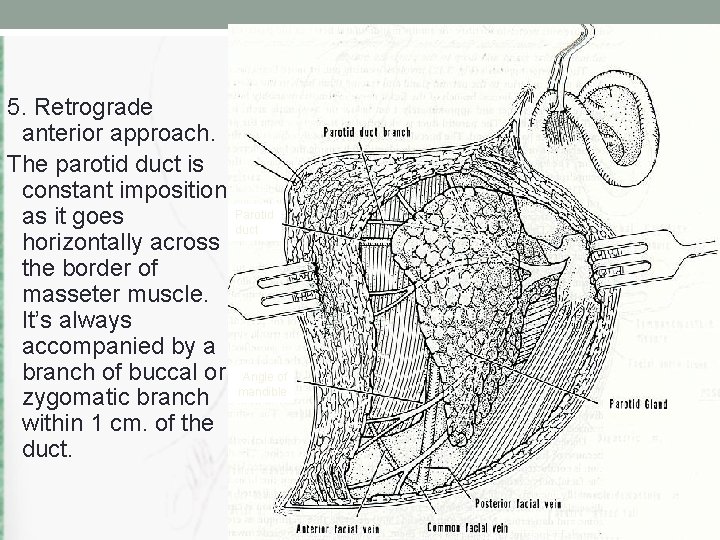
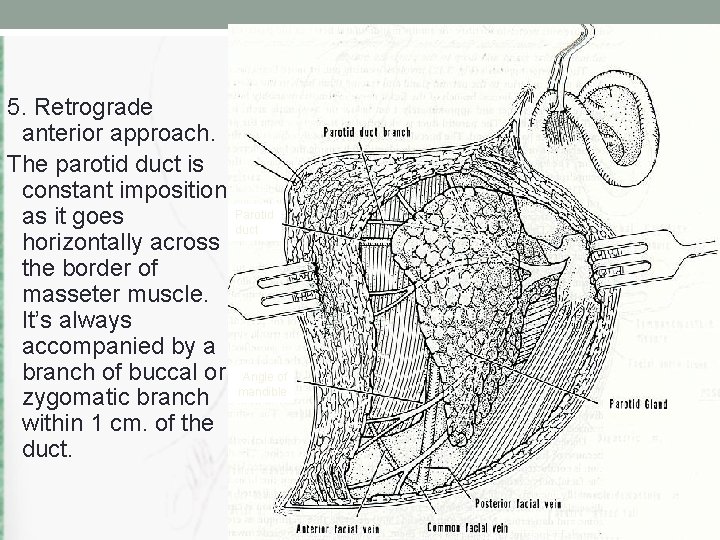
5. Retrograde anterior approach. The parotid duct is constant imposition Parotid as it goes duct horizontally across the border of masseter muscle. It’s always accompanied by a branch of buccal or Angle of zygomatic branch mandible within 1 cm. of the duct.
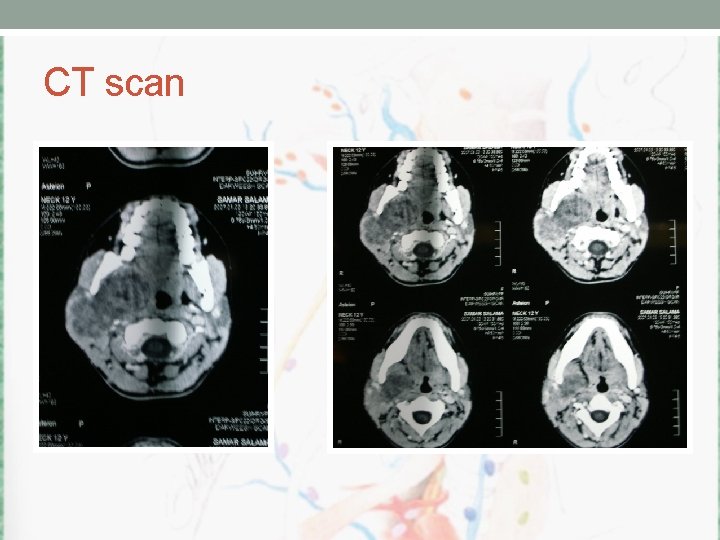
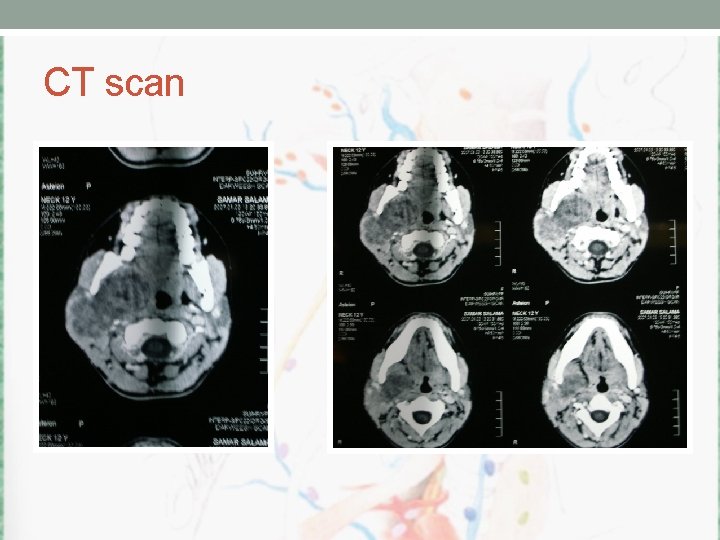
CT scan

CT scan
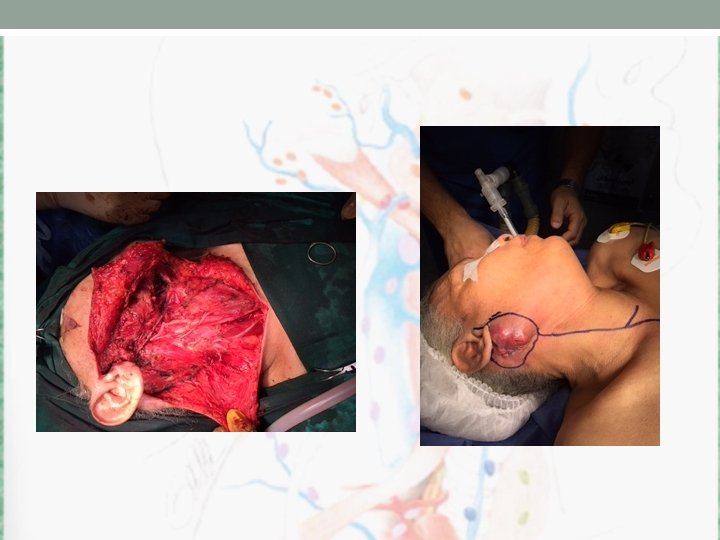
operation
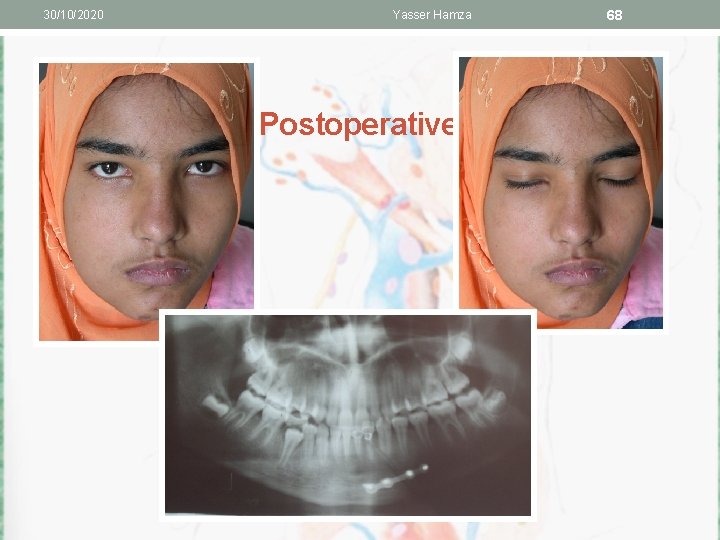
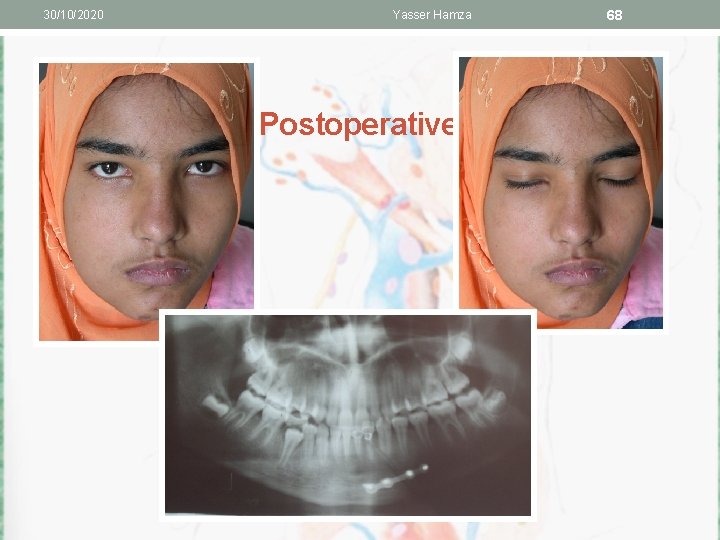
30/10/2020 Yasser Hamza Postoperative 68
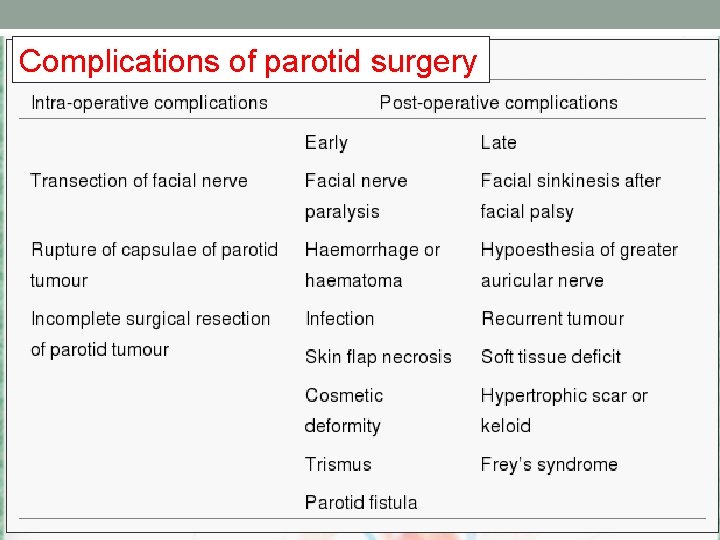
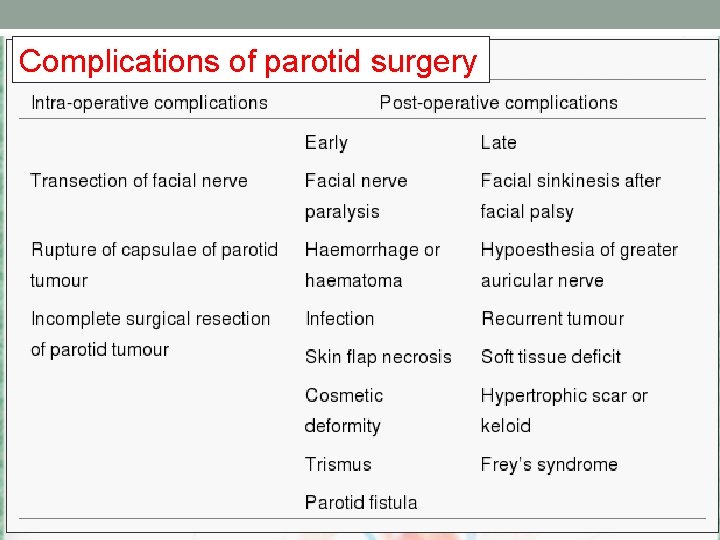
Complications of parotid surgery
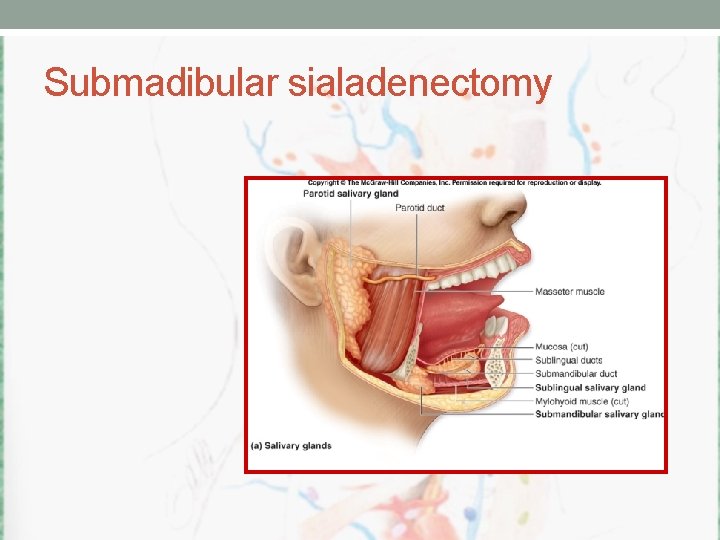
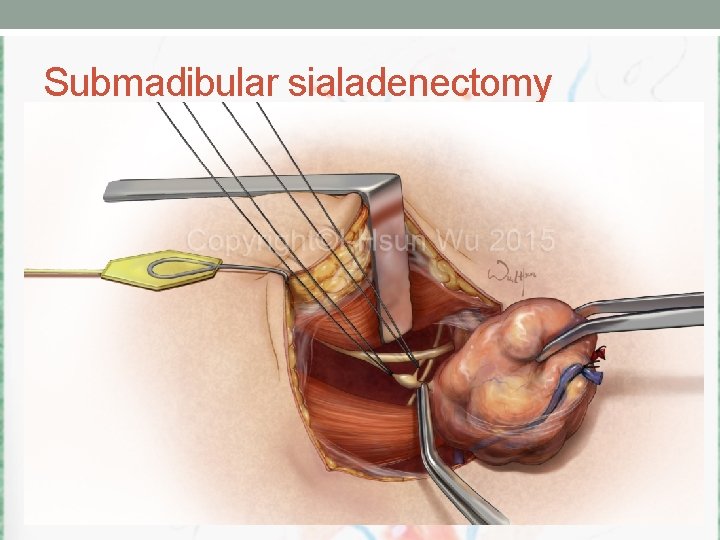
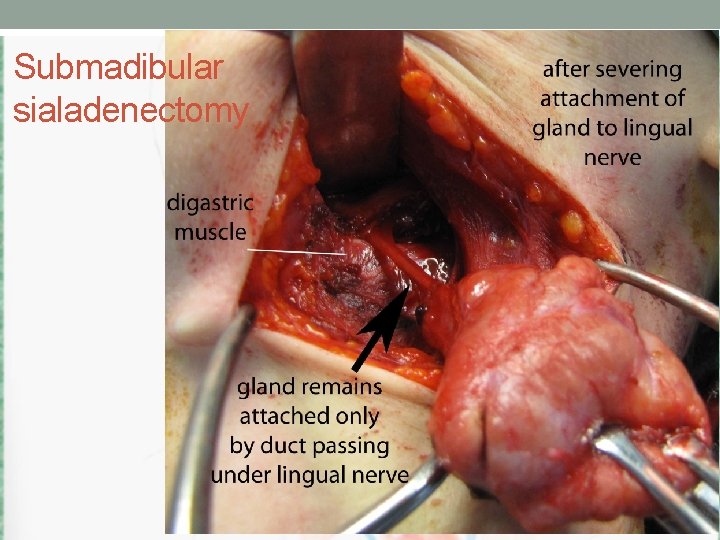
Submadibular sialadenectomy
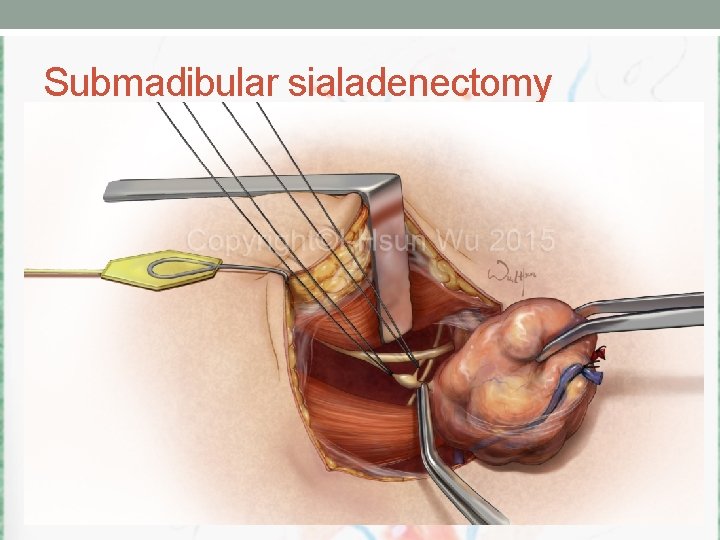
Submadibular sialadenectomy
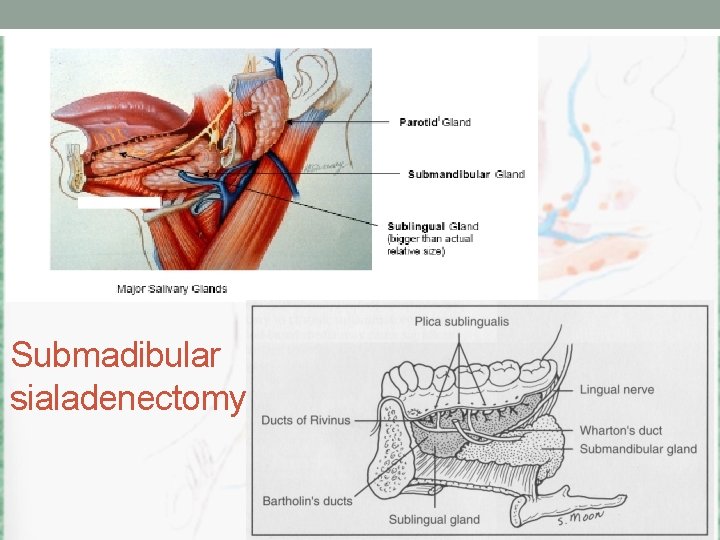
Submadibular sialadenectomy
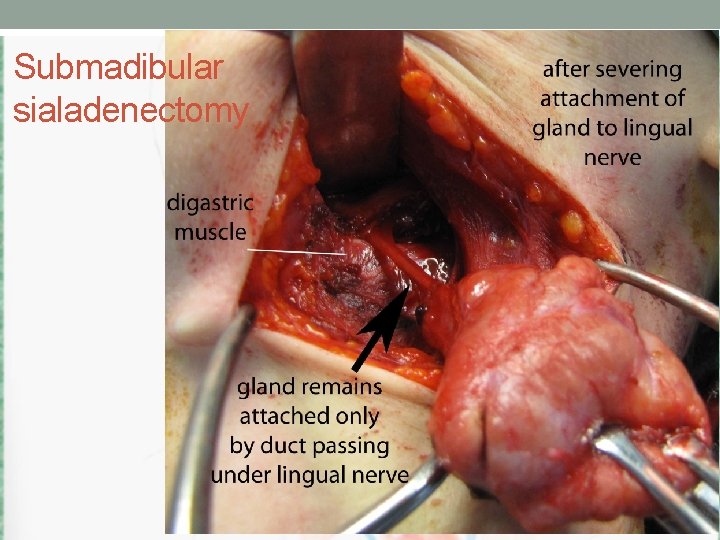
Submadibular sialadenectomy

Submadibular sialadenectomy
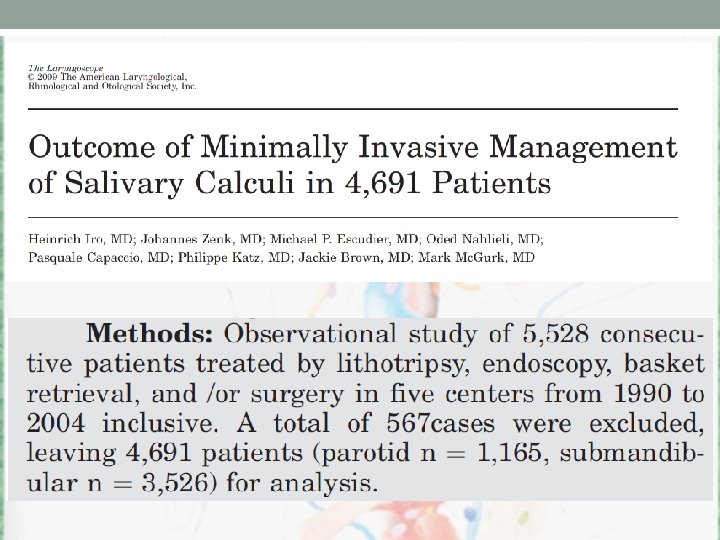
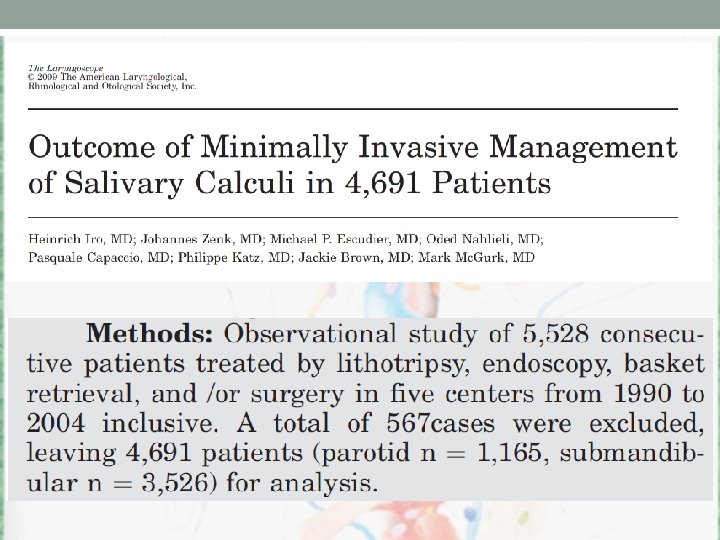
New techniques • Lithtrypsy • Sialoscopy • Min invasive • …
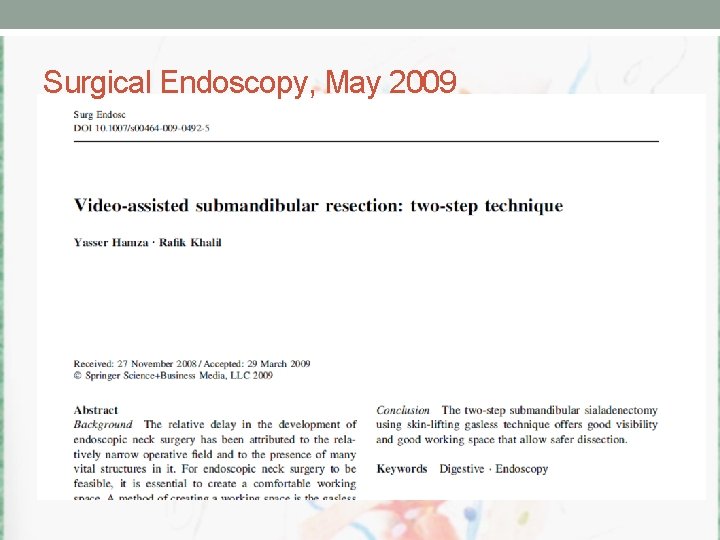
Surgical Endoscopy, May 2009


 Calculi sumeri
Calculi sumeri Calcium phosphate calculi
Calcium phosphate calculi Francis yasser
Francis yasser 2322008
2322008 Malignant and benign tumors
Malignant and benign tumors Prostatic adenocarcinoma
Prostatic adenocarcinoma Promotion from associate professor to professor
Promotion from associate professor to professor Teratoma
Teratoma Cervical ectropion
Cervical ectropion Response evaluation criteria in solid tumors (recist)
Response evaluation criteria in solid tumors (recist) Codman üçgeni
Codman üçgeni How many bones
How many bones Spinal cord tumors
Spinal cord tumors Brain tumors
Brain tumors Acromely
Acromely Radiothrapy
Radiothrapy Ipmn
Ipmn Local invasion
Local invasion Classification of tumors
Classification of tumors Odontogenic tumors classification
Odontogenic tumors classification Enneking staging
Enneking staging Odontogenic tumors
Odontogenic tumors Ameloblastoma rtg
Ameloblastoma rtg Ata thyroid
Ata thyroid Preapared
Preapared Ashwak hamza
Ashwak hamza Dr hamza jános
Dr hamza jános Hamza kashgari
Hamza kashgari Neighbours inner consultation model housekeeping
Neighbours inner consultation model housekeeping Hamza kashgari
Hamza kashgari Equação diferencial
Equação diferencial Hamza ameslek
Hamza ameslek Andreea hamza
Andreea hamza Heroes in turkey
Heroes in turkey Snow leopards diet
Snow leopards diet Hamza aftab
Hamza aftab Hamza hayat
Hamza hayat Dr. essam hamza
Dr. essam hamza Geniohyoid cat
Geniohyoid cat Incision for parotid abscess
Incision for parotid abscess Warthin tumor
Warthin tumor Nie wiem association
Nie wiem association Gland histology
Gland histology Histology
Histology Ginivitis
Ginivitis Cariostat test
Cariostat test Caries risk assessment form
Caries risk assessment form Salivary gland disorders classification
Salivary gland disorders classification Sublingua;
Sublingua; Salivary glands anatomy
Salivary glands anatomy Oncocytoma salivary gland
Oncocytoma salivary gland Basal cell adenoma
Basal cell adenoma Oncocytoma salivary gland
Oncocytoma salivary gland Oncocytoma salivary gland
Oncocytoma salivary gland Anatom
Anatom Minor salivary glands
Minor salivary glands Intercalated duct
Intercalated duct Oncocytoma salivary gland
Oncocytoma salivary gland Minor salivary glands
Minor salivary glands Submandibular gland excision
Submandibular gland excision Minor salivary glands
Minor salivary glands Salivary amylase digestion of starch
Salivary amylase digestion of starch Git
Git Submadibular
Submadibular Simple branched acinar
Simple branched acinar Salivary glands fetal pig
Salivary glands fetal pig Saliva formation
Saliva formation The professor and his beloved equation
The professor and his beloved equation Conclusion of growth and development
Conclusion of growth and development Prof ram meghe institute of technology and research
Prof ram meghe institute of technology and research Um balão de oxigênio contendo 3 01 x 1026
Um balão de oxigênio contendo 3 01 x 1026 How to write a formal email to teacher
How to write a formal email to teacher Proper adjective for java
Proper adjective for java Ppgea ufrrj
Ppgea ufrrj Ucf cheating scandal
Ucf cheating scandal Ruth guthrie rate my professor
Ruth guthrie rate my professor Professor mso afskaffes
Professor mso afskaffes Mattie is a new sociology professor
Mattie is a new sociology professor Paraphrase the following sentences.
Paraphrase the following sentences. Professor edley
Professor edley