CPANCAPA Certification Test Taking Preoperative Assessment Education Discharge








































- Slides: 126

CPAN/CAPA Certification Test Taking Preoperative Assessment, Education & Discharge Speaker: Lois Schick MN, MBA, CPAN. CAPAPA

Disclosure • I Currently have No conflict of interest • This presentation will not provide any commercial support of products or supplies. • I Currently have no sponsorship for this presentation.
Objectives • Describe Certified Post. Anesthesia Nurse (CPAN®) /Certified Ambulatory Peri. Anesthesia (CAPA®) certification test taking strategies. • Identify effective methods of patient education. • Identify recommended practices in preparing patients for surgery.
Benefits of CPAN & CAPA Certification ABPANC Website www. cpancapa. org • Join an elite group of experienced nursing colleagues who collectively serve to promote quality patient care while enhancing the awareness and respect of Perianesthesia Nursing. • Reflects commitment to perianesthesia nursing and quality patient care. • Increased professional credibility with patients and their loved ones. • Validation of current knowledge, experience and commitment to life-long learning. • Strong sense of achievement, personal pride and increased self esteem. • Gives a competitive edge in the job market.

CPAN / CAPA Blueprint Based on Role Delineation 2015 -2016 Percentage of Exam Questions Patient Needs CPAN CAPA Physiological 57% 50% Behavioral/Cognitive 18% 21% Safety 25% 29%

Which Test Should I Take? • What is most relevant to your practice? • ASPAN’s Scope of Practice of Peri. Anesthesia Care • Phase I – CPAN • Preanesthesia, Day of Surgery/Procedure, Phase II, &/or Extended Care – CAPA
CPAN/CAPA Differentiation • Patient care priorities differ d/t acuity, surgical intervention, behavioral responses • Differ regarding patient education, discharge teaching, care transitions • Both require same level of critical thinking
• 185 questions The Test Itself – 140 questions are scored • 3 hours to complete • Questions have been verified for accuracy, currency and reliability • Questions referenced to a source published within the last 5 years • Questions written by practicing perianesthesia nurses • Mark questions to come back to • Easily change your answers • View a list at end of exam that shows questions not answered

Costs Regular Continual Learning for Recertification ASPAN Non. Member $314 $424 $194 $315

ASPAN Membership National membership $80. 00/year State membership – varies $20 -45/year Membership includes Journal of Perianesthesia Nursing Joanna Briggs Institute membership Discounts to ASPAN publications Note: Price subject to change
Computer Based Testing • • Apply on-line No prior computer experience is necessary 6 week test windows Can take both CPAN AND CAPA in the same test window
Locations for CBT • Prometric test sites – hundreds of sites nationwide • Testing offered 5 days a week, many offer 6 days a week
Test Results CBT offers immediate preliminary test scores • Preliminary /unofficial score before leaving test site. Official score 2 -3 weeks later • must obtain a total scale score of 450 or higher • The scale range for the CPAN® and CAPA® examination is 200 to 800, with 450 set as the passing point

STUDY TECHNIQUES • Start with a positive attitude • Establish routine – try to study each day ( Review what you have learned each day) • Set short term and long term goals • Control distracters • Practice test taking • Make flash cards • Allow time for family and FUN!
TEST TAKING STRATEGIES • • Old tests make good study guides Take ABPANC tests online (www. cpancapa. org) Taking tests is a skill Practice makes perfect Practice Relaxation Read Question Carefully Do Not Read Into Question
TEST TAKING STRATEGIES • • • Consider usual situations Eliminate Incorrect Choices Only One answer is correct Identify “WHAT” is Question Asking Observe Patterns and relationships in questions
TEST TAKING STRATEGIES • • • First Response is usually right Answers may “POP UP” in other questions Break question down into components Identify options Correct answer: only one choice Distracters: designed to distract from the answer

TEST TAKING STRATEGIES • Non -Answers (Zero, None of the above) are usually poor guesses • Limiting terms used (All, Never Always, Must) False is best Answer • General terms used (Most, some, usually, could, might) True is best answer
TEST TAKING STRATEGIES • “ALL OF THE ABOVE” Good Guess • Look at Stem of Question: Which answer emphasizes the same thing • Read ALL Choices even though you might think the first or second answer is correct • If two answers mean the same , both are, Both are probably incorrect unless there is the option of “All of the above”
TEST TAKING STRATEGIES • There are usually No Patterns to answers- They are usually arranged randomly • Concentrate on basic principles: National examinations will not be specific to your state or clinical facility • The Broader the statement, The more likely it is untrue.
TEST TAKING STRATEGIES • If Question asks for a Plural (or Singular) answer, make sure you pick the Plural (or Singular) Answer • Exaggerated or complex answers are generally “FALSE” • When in doubt, Follow the rules for the best educated guess

TEST TAKING STRATEGIES • Commit things to memory only when you are well rested • If a question is difficult to visualize, draw it • Several short study sessions are generally better than one long one
TEST TAKING STRATEGIES • Certain vitamins can improve our Memory – Vitamin C – Vitamin B-1 (Thiamin) – Vitamin B-3 (Niacin) – Vitamin B-6 – Vitamin B-12 (Folic Acid & Iron) – Lecithin and Choline – Tryosine
TEST TAKING STRATEGIES • Generic terms used throughout: Know Generic names for drugs, equipment and procedures • Use multiple sources for review: Jo. PAN, perianesthesia/ambulatory nursing texts, physiology texts, ASPAN standards • Check ABPANC website (www. cpancapa. org) for reference list to use
TEST TAKING STRATEGIES • Eat Pasta at least one meal each day for one week before taking the test. • Last week, review – do not try to learn new info. • Review the content outline provided in the exam packet • Questions on qualifications for taking the exam and maintaining certification may be a test question. • Useless to cram the night before - Relax and get a good night sleep
TEST TAKING STRATEGIES • The exam is a normative examination - Not everyone is expected to pass. Do not give up -Time and efforts spent in preparation makes one a better nurse • This is a national exam, not specific to your state or practice area

Percentage of Candidates Passing the CPAN and CAPA Examinations: • October/November 2016: 61% passed CPAN; 66% passed CAPA • April/May 2016: 66% passed CPAN; 64% passed CAPA • October/November: 67% passed CPAN; 66% passed CAPA • April/May 2015: 69% passed CPAN; 68% passed CAPA • October/November 2014: 68% passed CPAN; 61% passed CAPA • April/May 2014: 65% passed CPAN; 61% passed CAPA • October/November 2013: 61% passed CPAN; 55% passed CAPA • April/May 2013: 69% passed CPAN; 67% passed CAPA • October/November 2012: 68% passed CPAN; 68% passed CAPA • April/May 2012: 74% passed CPAN; 65% passed CAPA
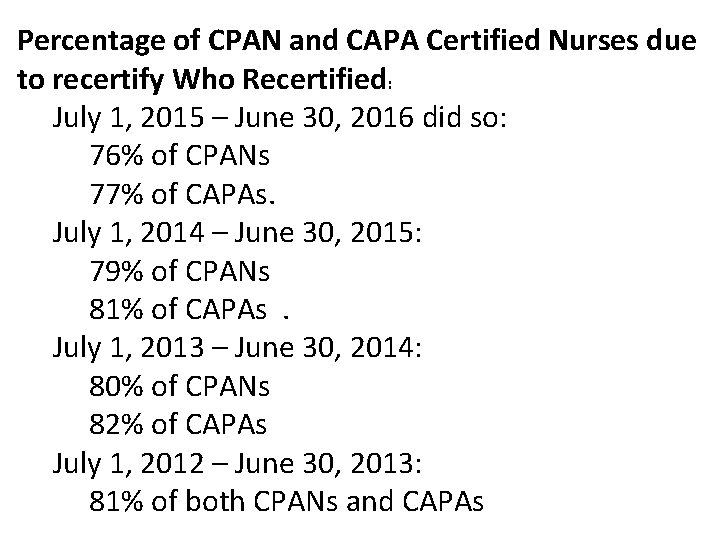
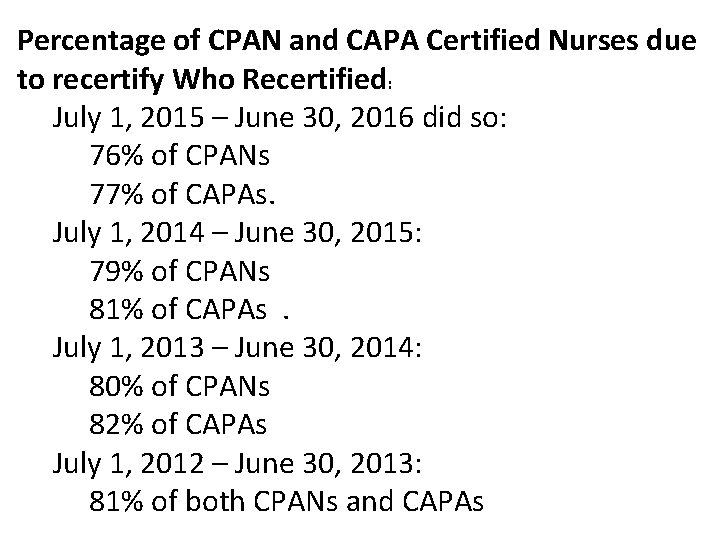
Percentage of CPAN and CAPA Certified Nurses due to recertify Who Recertified: July 1, 2015 – June 30, 2016 did so: 76% of CPANs 77% of CAPAs. July 1, 2014 – June 30, 2015: 79% of CPANs 81% of CAPAs. July 1, 2013 – June 30, 2014: 80% of CPANs 82% of CAPAs July 1, 2012 – June 30, 2013: 81% of both CPANs and CAPAs
TEST TAKING STRATEGIES • Eat a good breakfast the morning of the exam • Allow sufficient time to get to the exam site • Dress comfortable - Remember to dress in layers as the room may be too hot or too cold • Wear Bright Yellow or Bright Red on the day of the examination
Learning opportunity • Spend more time on – those subjects that are your weakness – those patients you do not work with. (i. e. OB, Pediatrics, Geriatrics) • HAVE FUN!!!
Preoperative Nursing • • • Assessment Data collection/documentation Physiologic assessment Psychosocial assessment Spiritual/cultural assessment Education
Preoperative Nursing Assessment components Patient questionnaires Individual interviews/Assessment History & Physical Testing Teaching/Education Consents – Surgical – Anesthesia • Evaluation • • •

Importance of Patient Preparation • Contributes to: – Decreased length of stay – Decreased cost of hospitalization – Decreased patient anxiety therefore decreased need for sedation – Increased customer satisfaction
Telephone Interview • Telephone call the day before surgery by nurse, anesthesiologist • • Arrival time given Instructions reviewed Directions reinforced Questions answered

Anesthesiologists meeting with Patients • Educate about anesthesia, periop care and pain management • Obtain pertinent info about medical history, physical and mental conditions • Determine tests & consultations needed • Choice of care plans guided by patient choices & risk factors • Obtain informed anesthesia consent • Minimize resource utilization yet achieve good outcome
American Society of Anesthesiologists (ASA) states: • No routine lab or diagnostic screening of patients is necessary, but should instead be based upon the patient’s specific clinical risk factors. • Tests should be ordered when the results may influence decisions regarding risks and management of anesthesia or surgery during the course of the operation.
Preadmission Testing • What’s necessary? • When is it done? • Does Patient have significant systemic disease?

Test Taking • Hemoglobin • Blood Glucose: all diabetics • Basic Metabolic Panel (NA, K, CL, BUN, CR, Glucose, CA) • Comprehensive Metabolic Panel • PT, PTT, Platelets • Pregnancy • Type and Screen/Type and Hold/Type and Crossmatch • EKG • Chest X-Ray • Cervical Spine
Obesity 1. 2. 3. 4. Common physical finding Morbid obesity is a total body disease Determine ideal body weight and the body mass index Even the easy things are difficult in the morbidly obese patient
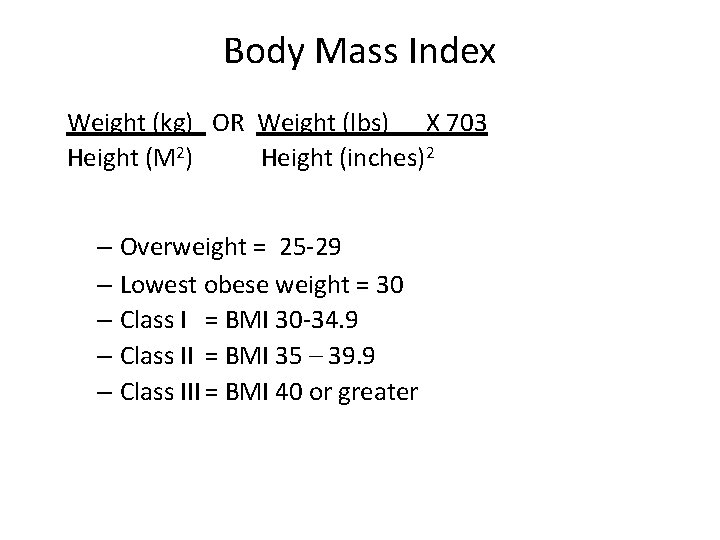
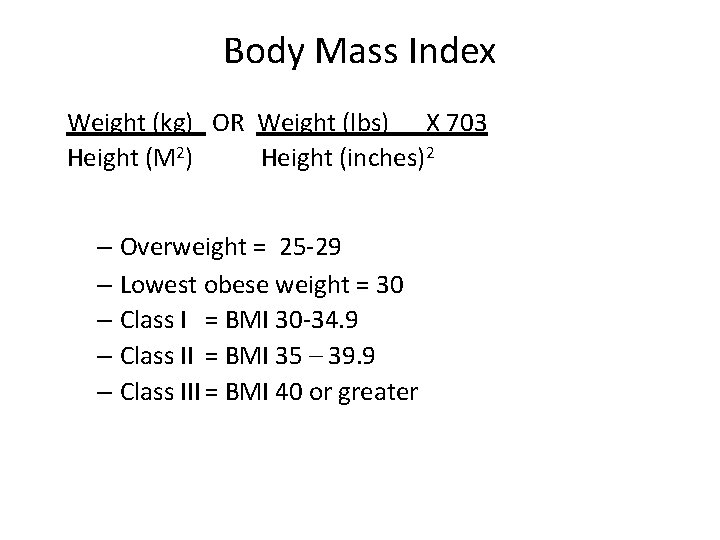
Body Mass Index Weight (kg) OR Weight (lbs) X 703 Height (M 2) Height (inches)2 – Normal = <25 – Overweight = 25 -29 – Lowest obese weight = 30 – Class I = BMI 30 -34. 9 – Class II = BMI 35 – 39. 9 – Class III = BMI 40 or greater
Morbid Obesity 1. 2. Twice the ideal body weight Physiologic changes – Altered blood volume • Increased total volume • Decreased ml / kg – Increased O 2 demand
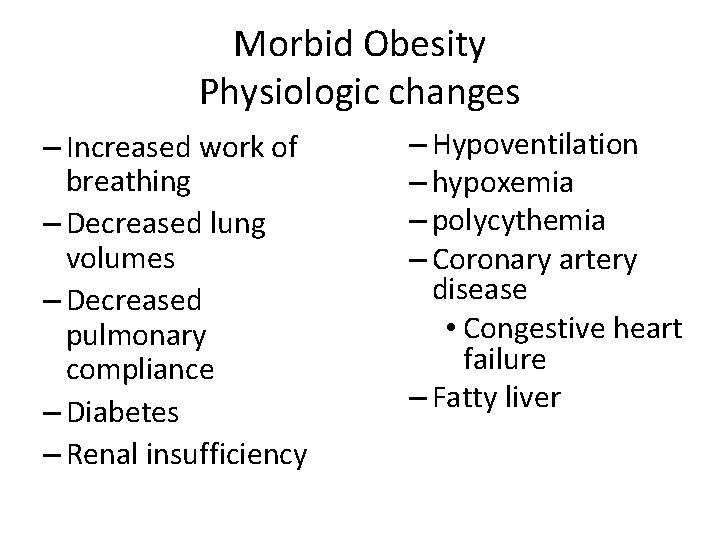
Morbid Obesity Physiologic changes – Increased work of breathing – Decreased lung volumes – Decreased pulmonary compliance – Diabetes – Renal insufficiency – Hypoventilation – hypoxemia – polycythemia – Coronary artery disease • Congestive heart failure – Fatty liver
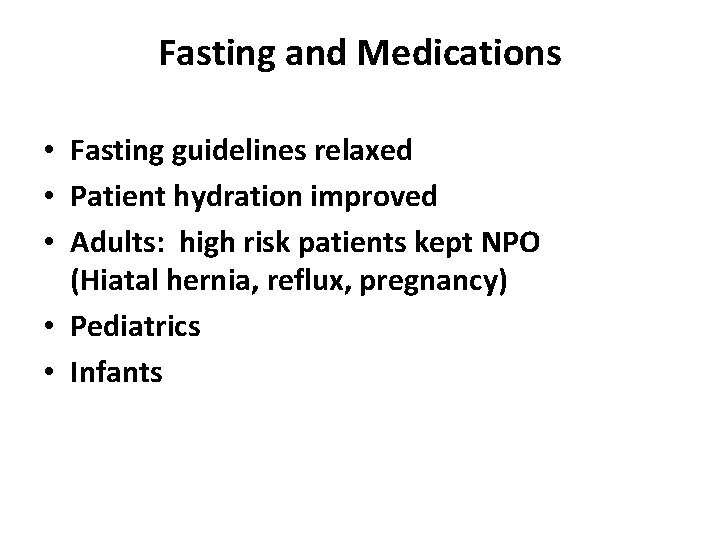
Fasting and Medications • Fasting guidelines relaxed • Patient hydration improved • Adults: high risk patients kept NPO (Hiatal hernia, reflux, pregnancy) • Pediatrics • Infants

Fasting Instructions • AGE MILK/SOLID • 0 -6 months 4 hours • 6 -36 months 6 hours • > 36 months 8 hours CLEAR LIQUIDS 2 hours 3 hours • (European Society of Anesthesiologist recommend Solid food be prohibited 6 hr before elective surgery in adults & children. )
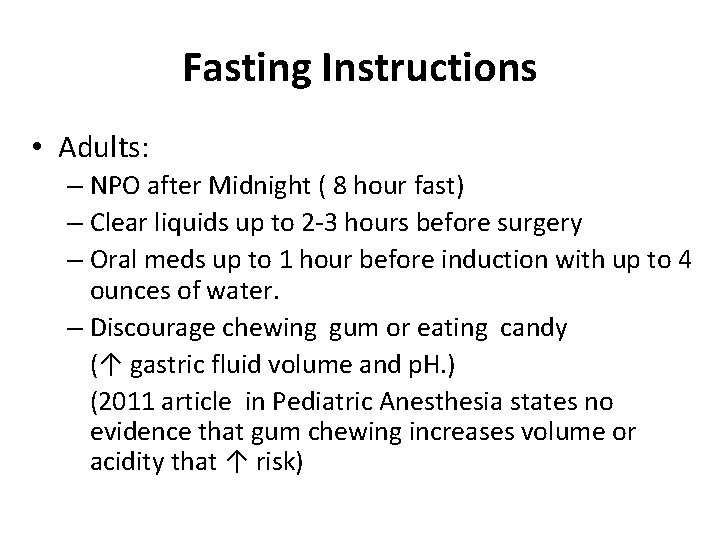
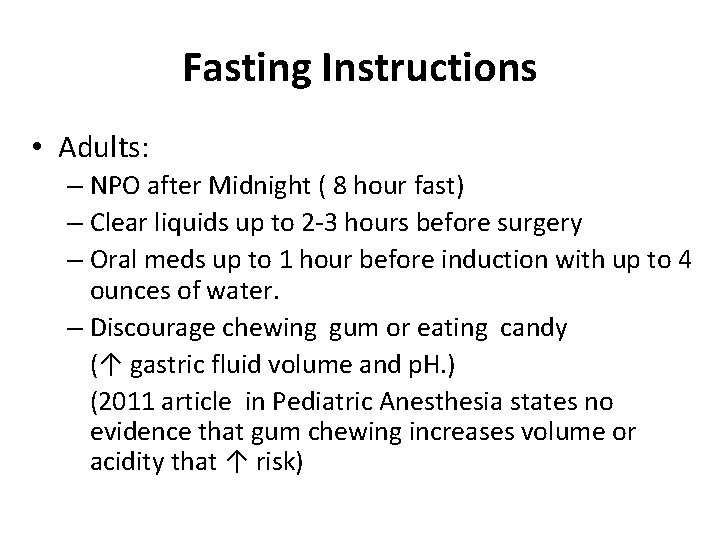
Fasting Instructions • Adults: – NPO after Midnight ( 8 hour fast) – Clear liquids up to 2 -3 hours before surgery – Oral meds up to 1 hour before induction with up to 4 ounces of water. – Discourage chewing gum or eating candy (↑ gastric fluid volume and p. H. ) (2011 article in Pediatric Anesthesia states no evidence that gum chewing increases volume or acidity that ↑ risk)
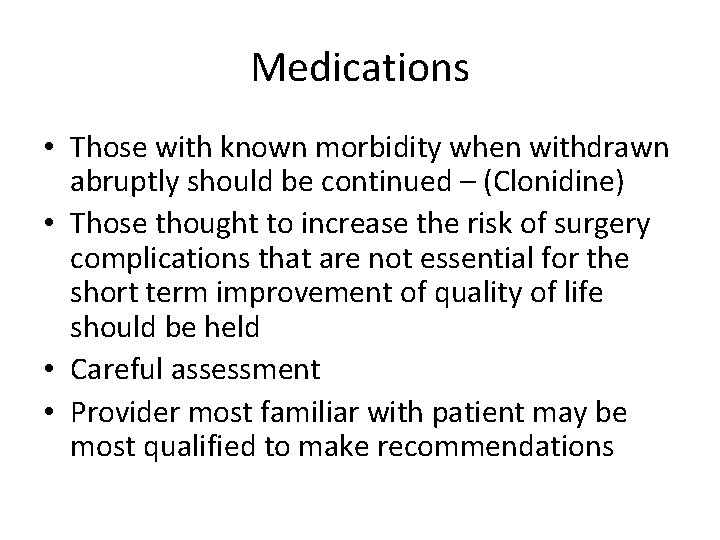
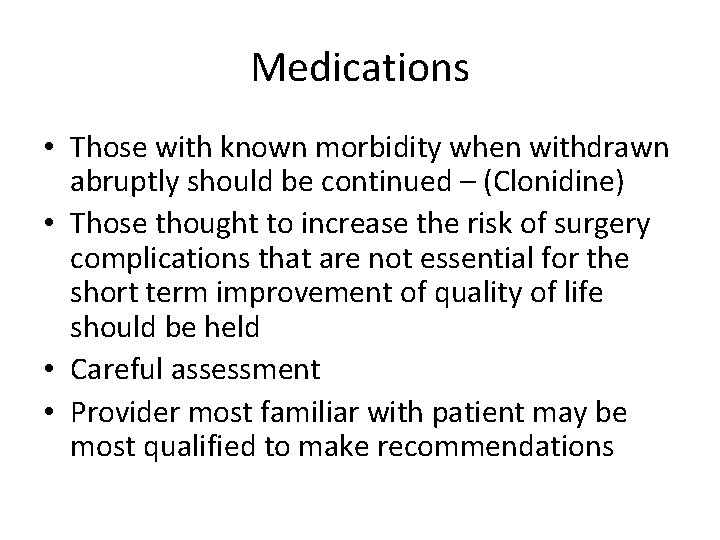
Medications • Those with known morbidity when withdrawn abruptly should be continued – (Clonidine) • Those thought to increase the risk of surgery complications that are not essential for the short term improvement of quality of life should be held • Careful assessment • Provider most familiar with patient may be most qualified to make recommendations

Cardiac Meds • Continue up to and including day of surgery – Beta Blockers – Clonidine – Nitrates – Digoxin – Calcium channel blockers – Antidysrhythmics – Statins
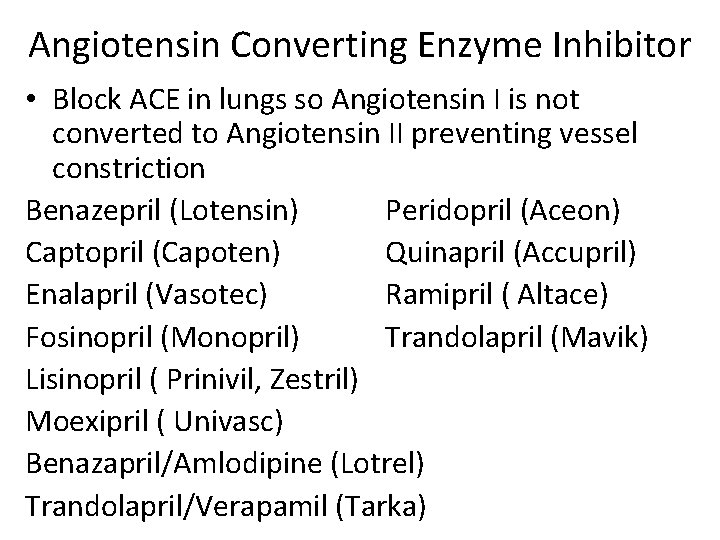
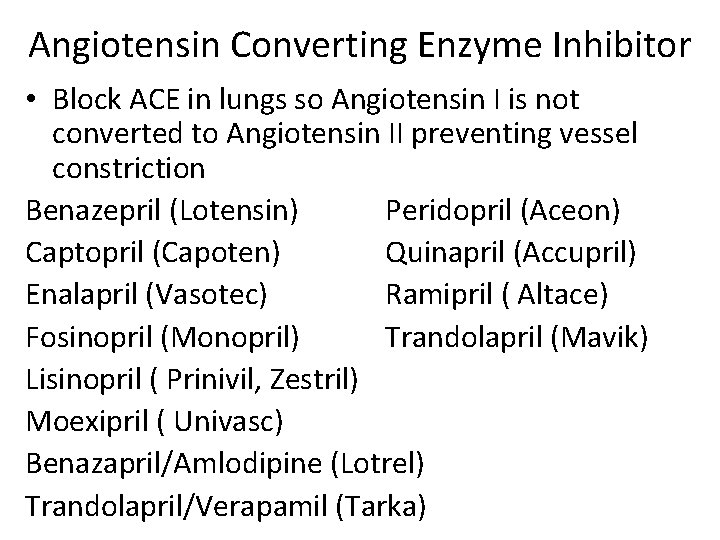
Angiotensin Converting Enzyme Inhibitor • Block ACE in lungs so Angiotensin I is not converted to Angiotensin II preventing vessel constriction Benazepril (Lotensin) Peridopril (Aceon) Captopril (Capoten) Quinapril (Accupril) Enalapril (Vasotec) Ramipril ( Altace) Fosinopril (Monopril) Trandolapril (Mavik) Lisinopril ( Prinivil, Zestril) Moexipril ( Univasc) Benazapril/Amlodipine (Lotrel) Trandolapril/Verapamil (Tarka)

Angiotensin Receptor Blockers (ARBs) • Block chemical receptors for Angiotensin II on small arteries therefore arteries cannot constrict Cozaar (Losartan) Hyzaar (Losartan/hctz) Diovan (Valsartan) Avapro ( Irbesartan) Atacand (Candesartan) Micardis (Telmisartan) Benicar (Olmesartan) Teveten (Eprosartan) Exforge(Amlodipine/Valsartan) Avalide (Irbesartan/HCTZ) Azor (Olmesartan/Amlodipine) Valturna (Aliskiren/Valsartan)
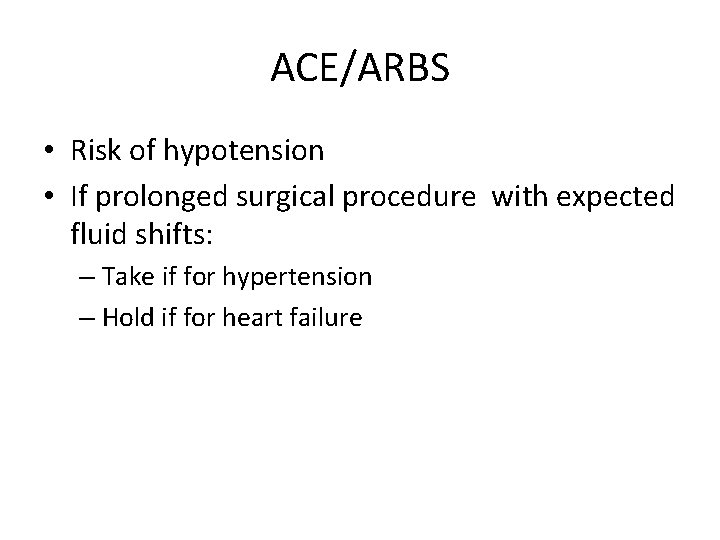
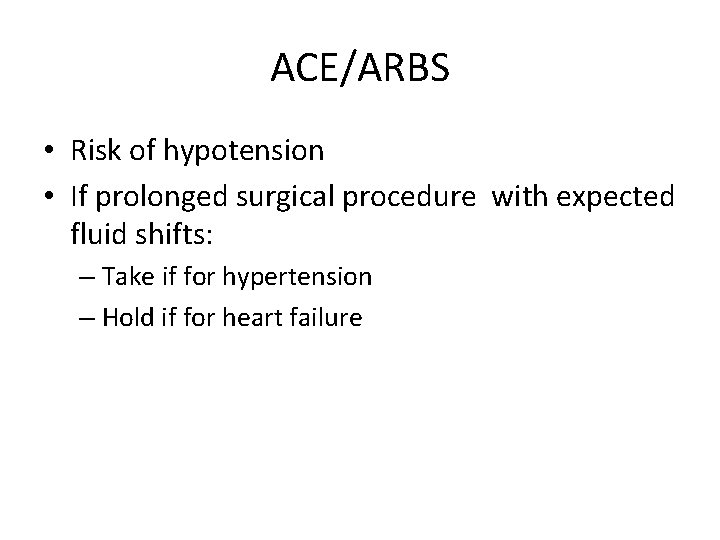
ACE/ARBS • Risk of hypotension • If prolonged surgical procedure with expected fluid shifts: – Take if for hypertension – Hold if for heart failure
Medications • Statins – Continue • Diuretics: Hold at least the morning of surgery • MAO Inhibitors: Nardil, Parnate, & Marplan Stop 2 weeks preoperatively for elective surgery.

Meds • Reflux meds: continue • Pain Meds: continue as long as they do not contain NSAID. Oxycontin – continue • Thyroid: Continue • Seizure/Parkinson meds: Continue unless neurology instructs to hold • Antidepressants/Psych meds: continue • MAO Inhibitors: continue and alert Anesthesia • Diuretics: Withhold AM dose to avoid dehydration and low blood volume
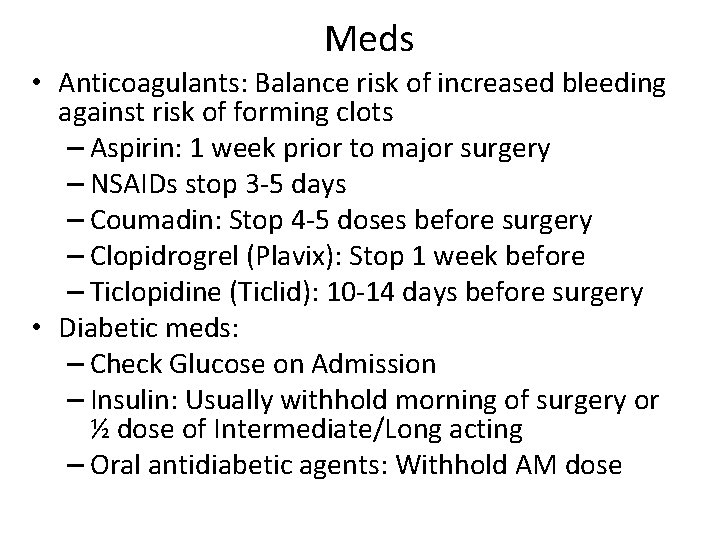
Meds • Anticoagulants: Balance risk of increased bleeding against risk of forming clots – Aspirin: 1 week prior to major surgery – NSAIDs stop 3 -5 days – Coumadin: Stop 4 -5 doses before surgery – Clopidrogrel (Plavix): Stop 1 week before – Ticlopidine (Ticlid): 10 -14 days before surgery • Diabetic meds: – Check Glucose on Admission – Insulin: Usually withhold morning of surgery or ½ dose of Intermediate/Long acting – Oral antidiabetic agents: Withhold AM dose
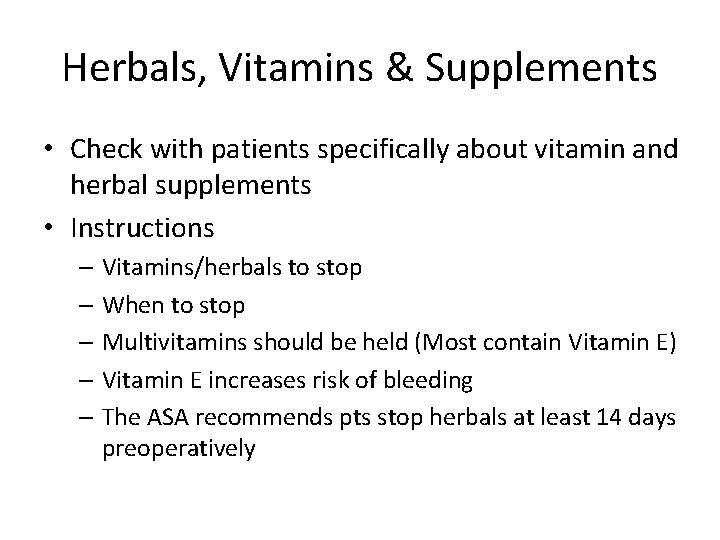
Herbals, Vitamins & Supplements • Check with patients specifically about vitamin and herbal supplements • Instructions – Vitamins/herbals to stop – When to stop – Multivitamins should be held (Most contain Vitamin E) – Vitamin E increases risk of bleeding – The ASA recommends pts stop herbals at least 14 days preoperatively
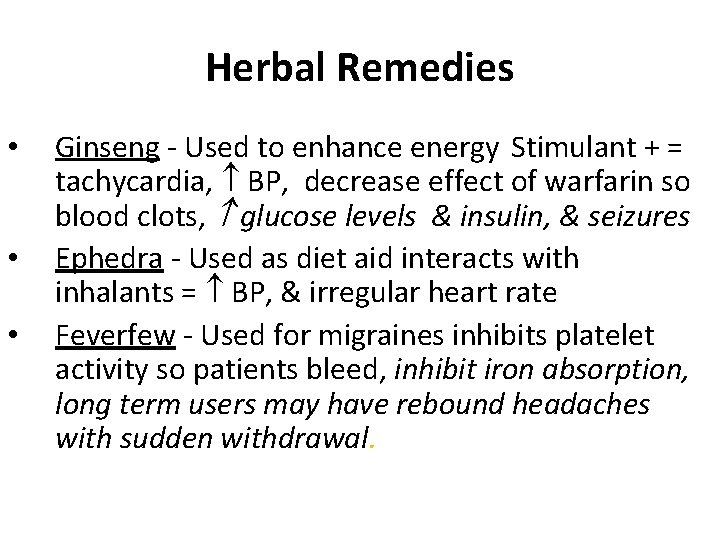
Herbal Remedies • • • Ginseng - Used to enhance energy Stimulant + = tachycardia, BP, decrease effect of warfarin so blood clots, glucose levels & insulin, & seizures Ephedra - Used as diet aid interacts with inhalants = BP, & irregular heart rate Feverfew - Used for migraines inhibits platelet activity so patients bleed, inhibit iron absorption, long term users may have rebound headaches with sudden withdrawal.
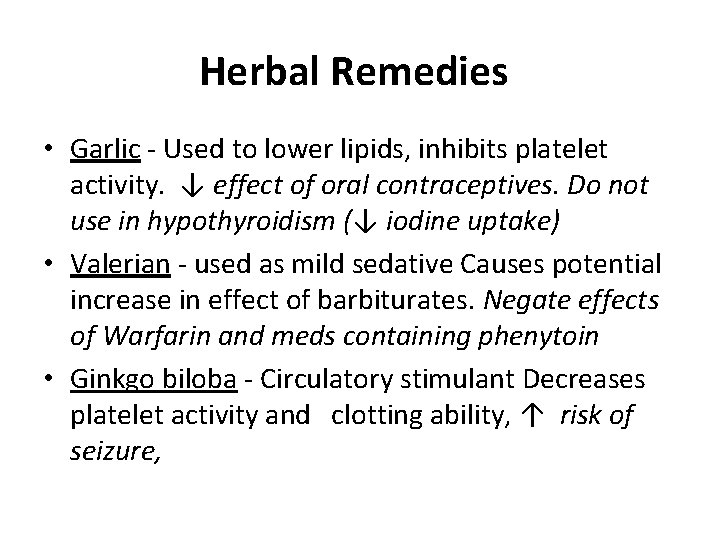
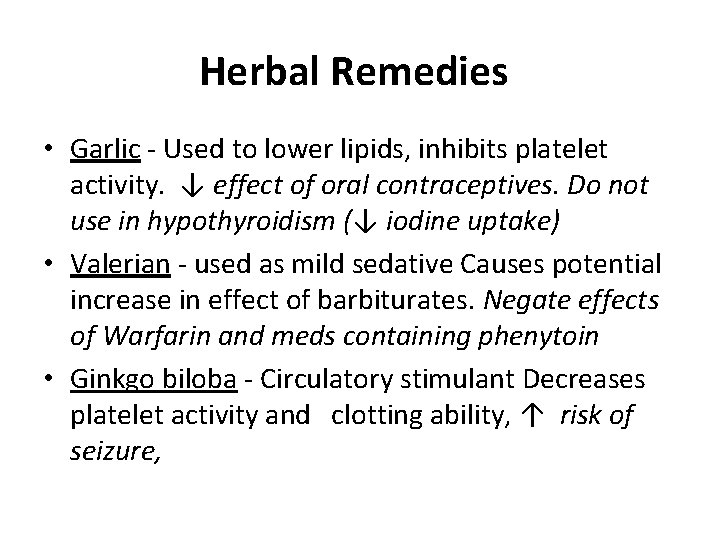
Herbal Remedies • Garlic - Used to lower lipids, inhibits platelet activity. ↓ effect of oral contraceptives. Do not use in hypothyroidism (↓ iodine uptake) • Valerian - used as mild sedative Causes potential increase in effect of barbiturates. Negate effects of Warfarin and meds containing phenytoin • Ginkgo biloba - Circulatory stimulant Decreases platelet activity and clotting ability, ↑ risk of seizure,
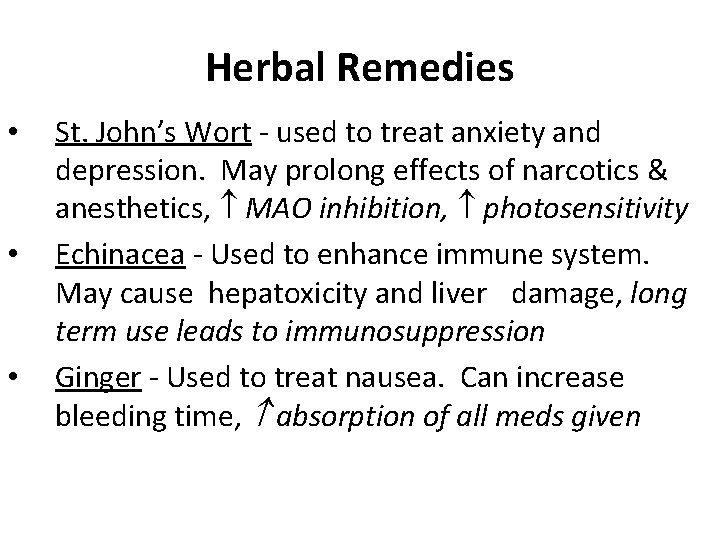
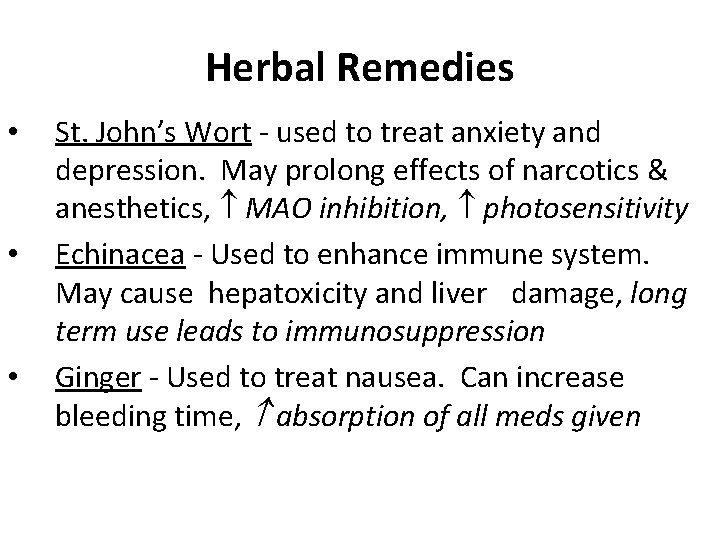
Herbal Remedies • • • St. John’s Wort - used to treat anxiety and depression. May prolong effects of narcotics & anesthetics, MAO inhibition, photosensitivity Echinacea - Used to enhance immune system. May cause hepatoxicity and liver damage, long term use leads to immunosuppression Ginger - Used to treat nausea. Can increase bleeding time, absorption of all meds given
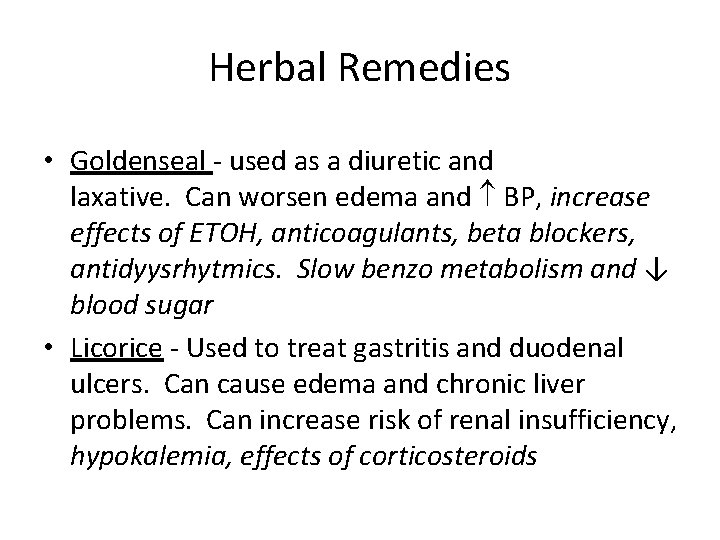
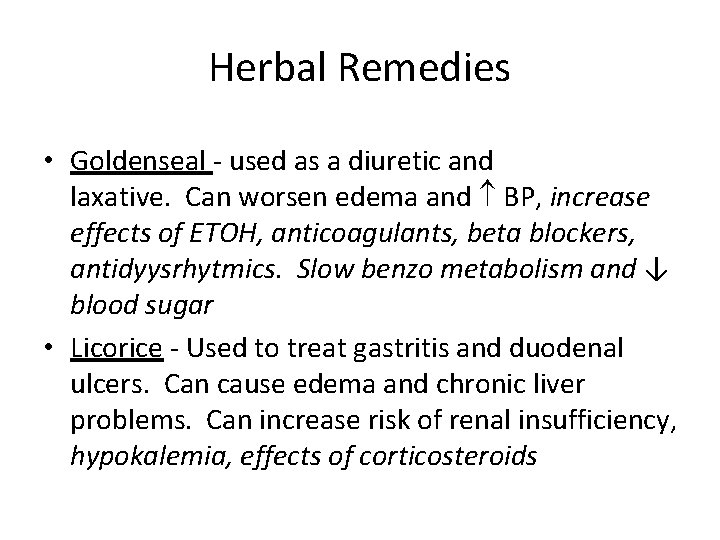
Herbal Remedies • Goldenseal - used as a diuretic and laxative. Can worsen edema and BP, increase effects of ETOH, anticoagulants, beta blockers, antidyysrhytmics. Slow benzo metabolism and ↓ blood sugar • Licorice - Used to treat gastritis and duodenal ulcers. Can cause edema and chronic liver problems. Can increase risk of renal insufficiency, hypokalemia, effects of corticosteroids

Herbal Remedies • Fish oil: Hyperlipidemia, hypertension, Diabetes, CAD, decrease aggregation of platelets • Kava: Use for anxiety, stress, insomnia • Quease Ease: Aromatherapy using essential oils (peppermint, ginger, spearmint) to treat nausea & vomiting. Lavender added as anxiolytic and antispasmodic.
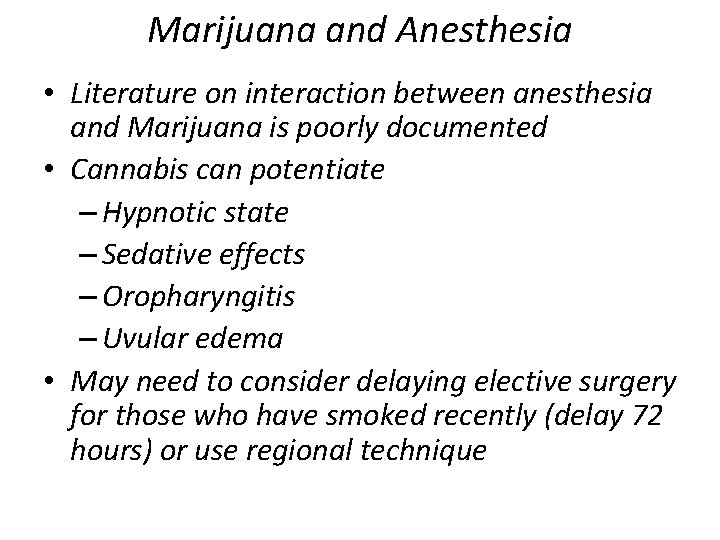
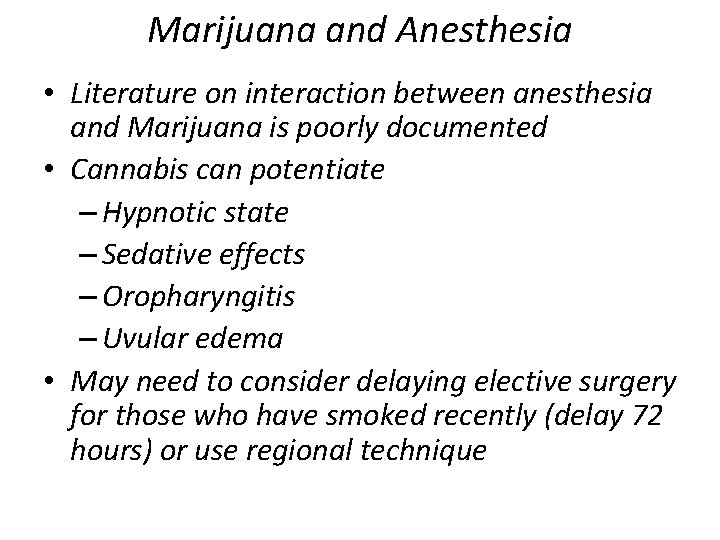
Marijuana and Anesthesia • Literature on interaction between anesthesia and Marijuana is poorly documented • Cannabis can potentiate – Hypnotic state – Sedative effects – Oropharyngitis – Uvular edema • May need to consider delaying elective surgery for those who have smoked recently (delay 72 hours) or use regional technique
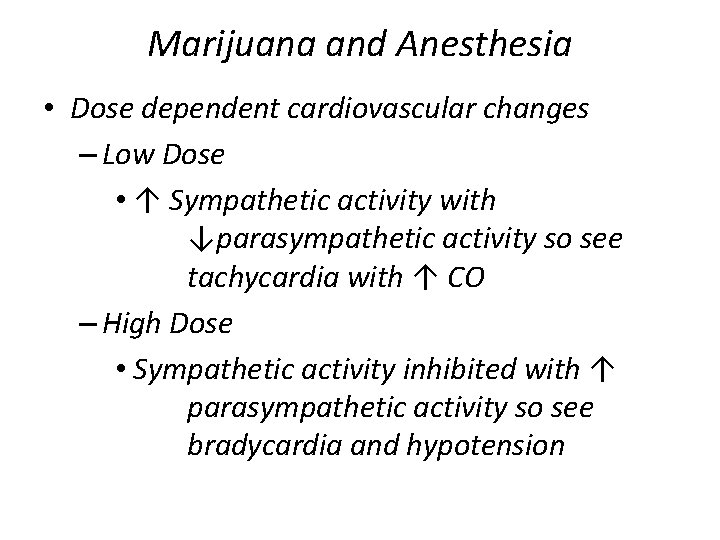
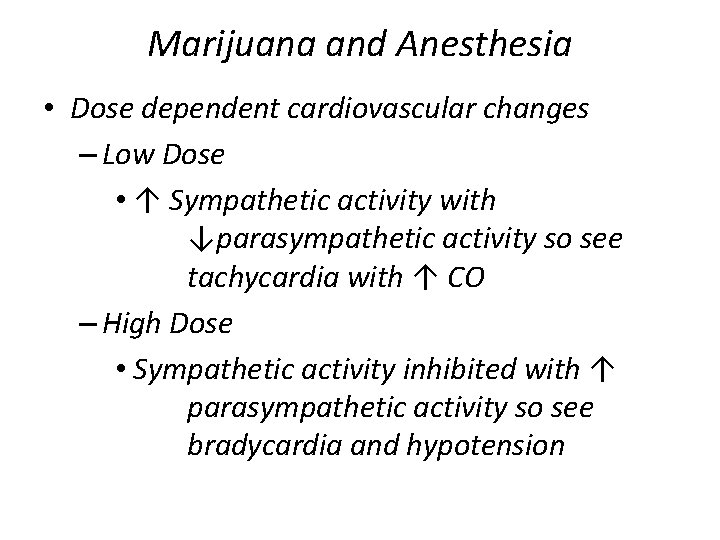
Marijuana and Anesthesia • Dose dependent cardiovascular changes – Low Dose • ↑ Sympathetic activity with ↓parasympathetic activity so see tachycardia with ↑ CO – High Dose • Sympathetic activity inhibited with ↑ parasympathetic activity so see bradycardia and hypotension

Marijuana and Anesthesia • Acute consumption – More anesthetic may be required due to greater catecholamine release • Chronic consumption – Less anesthetic because of catecholamine depletion • Consider psychiatric side-effects or withdrawal in patients during induction and emergence.

Cultural Diversity • Members of ethnic • Cultural Assessment includes information groups share similar – Cultural health beliefs – History – Communication – Language methods – Customs – Cultural restrictions – Characteristics – Social networks – Nutritional status – Religion – Values & beliefs

Cultural Sensitivity • Ethnic norms influence – Diet ( no porcine or bovine products) – Responses to pain – Compliance with self care activities & medical treatments – Trust in health care providers • Cultural Considerations – Assault & Battery – Respect patient’s cultural values & beliefs regarding touching

Cultural awareness of touch • Hispanics • African Americans – Highly tactile-may embrace & – May not like to be touched without permission shake hands – May exercise level of distrust – Very modest; May request health initially care provider of same gender – Touching another’s hair may – Illness/pain may be seen as be viewed as offensive punishment for misdeeds • Native Americans – May not like to be touched – May use home remedies without permission (touch of • Asians/Pacific Islanders dead baby prohibited) – Nonverbal communication is – Avoid touching important; Shake hands – Touching during an argument = lightly loss of control (shame) – Illness disruption of balance – Oneness; Balance Yin & Yang – Respect for elders; strong sense of family – 5 elements; Fire, Earth, Metal, Water, Wood – Agrees even if do not understand
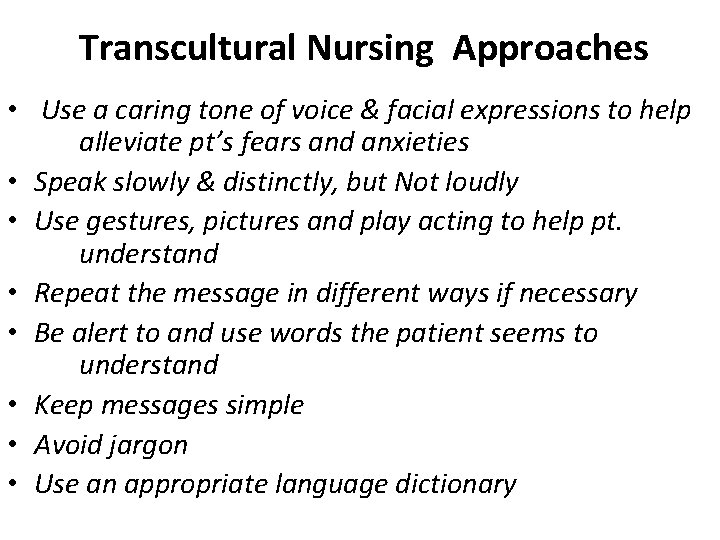
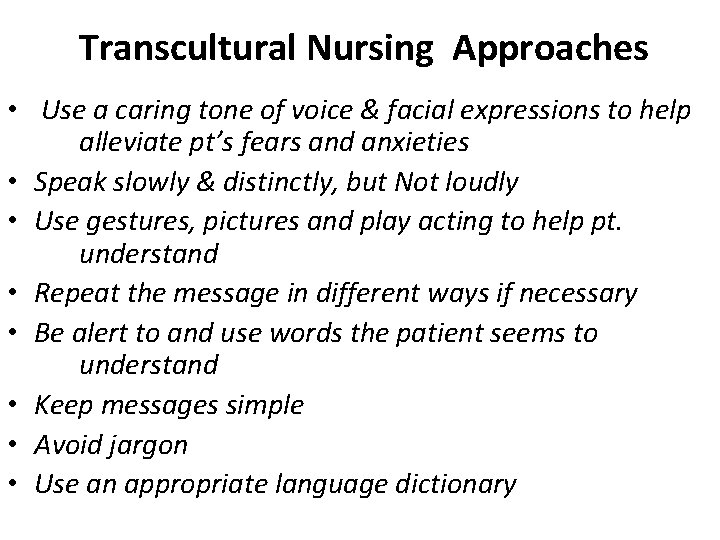
Transcultural Nursing Approaches • Use a caring tone of voice & facial expressions to help alleviate pt’s fears and anxieties • Speak slowly & distinctly, but Not loudly • Use gestures, pictures and play acting to help pt. understand • Repeat the message in different ways if necessary • Be alert to and use words the patient seems to understand • Keep messages simple • Avoid jargon • Use an appropriate language dictionary
To offer patients the BEST in preoperative care, nurses need to create an environment in which = patients are free to identify their fears and anxieties

Hurried environment leaves patients feeling confused and rushed through the system jeopardizing the essence of patient focused preoperative care

Preoperative Education benefit for nurses and institution • • • Prepared patient Increased job satisfaction Reduced potential for litigation Decreased complaints about care Decreased Length of Stay Compliance with TJC requirements

Learner Characteristics Demographics Primary language Special learning considerations – Reading level – Sensory limitations – Preferred level of learning – Physical condition • Developmental level – Mental, emotional, educational limitations – Motivation & attitude • • •
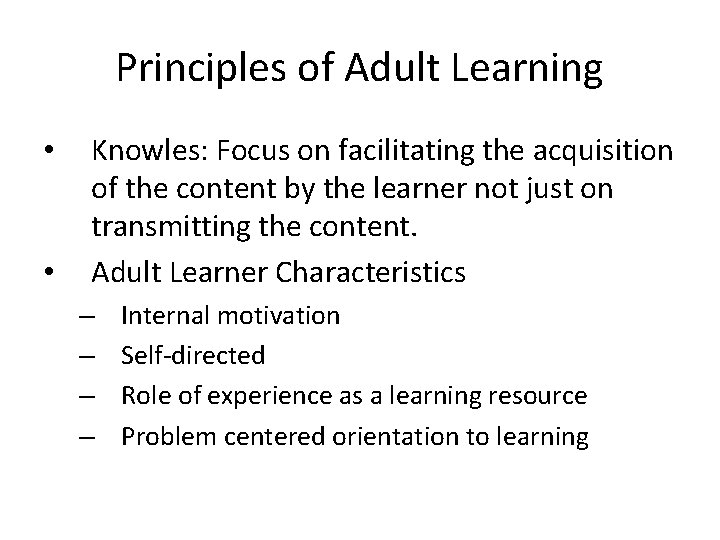
Principles of Adult Learning • • Knowles: Focus on facilitating the acquisition of the content by the learner not just on transmitting the content. Adult Learner Characteristics – – Internal motivation Self-directed Role of experience as a learning resource Problem centered orientation to learning

Trust vs Mistrust (0 – 1 year) • • Consider Growth & Development Anxiety & stranger anxiety Spend time getting acquainted Encourage use of new or familiar play objects Allow child to use transitional objects ( blanket, pacifier) Teach parents to participate in care Handle child gently & speak in soft tones
Autonomy vs. Shame & Doubt (1 -3 years) • • • Children strive to maintain autonomy Give simple, direct and honest explanations Strong fear of abandonment Psychosocial skills are developing Play can be useful to anxiety (puppets, coloring books Toddlers need to play with medical equipment

Autonomy vs. Shame & Doubt (1 -3 years) • Let child make appropriate choices i. e. choose side of body for injection • Explain things in brief nonthreatening terms; simple neutral words child understands • Sitting at child’s level is helpful • Invite parents to join in play • Use play therapy as an emotional outlet to test child’s sense of reality • Use words child understands
Initiative vs. Guilt (3 -5 Years) • • • Strives for sense of control, purpose, independence Body integrity is major issue Fear of bleeding and punctures Imagination consumes child’s thinking Magical thinking (Assumption reality & fantasy are the same; Child can magically influence) Information must be factual, nonthreatening, direct and related in simple terms
Initiative vs. Guilt (3 -5 Years) • Child masters experiences through – use of imagination – Role modeling – Opportunities to make choices – Play • Let child handle equipment before procedure • Use dolls to show anatomic sites and procedures

Industry vs. Inferiority (6 -12 years) • • • Skill acquisition characterizes this development stage Choices - allow child measure of control ( walk or ride; flavored anesthesia mask) Thinking is concrete - children tend to be quite literal – “put to sleep” may be associated with pet euthanasia • “Fear loss of control, bodily injury and pain, death, dismemberment, body mutilation and failure to live up to expectations of important others. ”
Industry vs. Inferiority (6 -12 years) • • • Use body models to explain Explain logically why a procedure is necessary Describe sensations to anticipate Encourage active participation Praise for cooperating with a procedure

Identity vs. Role Confusion (12 -18 years) • Adolescents seek identity in midst of physical & emotional changes • Feelings of low self-esteem & self-consciousness typical • Give scientific explanations, using body diagrams, models or videotapes • Provide privacy • Personal questions (I. e. drugs, MJ, ETOH, sexual activity) should be done in absence of parents if honest answers expected
Identity vs. Role Confusion (12 -18 years) • • • Encourage patient to express concerns about surgery especially as it relates to body image and peer conformity (encourage artwork, writing) Use books, diagrams Offer appropriate praise

• Even with preparation, separation anxiety for both child and parent is real See an increased trend for parents with child during induction especially ages 1 -5 • Having parent dress in OR attire in front of child is important for child to be able to recognize parent
Child’s Experience • • • Behavior can be altered for days, weeks or months after surgery. More positive the experience the less likely the child will have negative behavioral response. Some negative behavioral response include: nightmares, eating problems, separation anxiety, withdrawal, apathy, escalated fear of physicians; increased rebelliousness toward parents and guardians Providing a sedative can reduce the incidence of negative behavior in children
Elderly Patients Less formal education Sensory deficits can interfere with ability to learn • Barriers to Learning – Physiological – Emotional – Cultural – Environmental – Language barriers – Inadequate or poor teaching • •

Present Knowledge • • • Previous experience Prior education Patient perception and expectations Potential misinformation Psychosocial – Health beliefs – Attitudes – Stress – Coping Skills – Social support – Anxiety
Learning Environment • • • Conducive to learning Quiet, private Decrease anxiety Facilitate learning Family oriented Lack of physical/mental barriers
Teaching Characteristics & Domains of Learning • • Knowledge of teaching-learning characteristics Use Common language Anxiety & pain impede learning Adult learning is goal directed Reinforce learning Knowledge of teaching tools and content Domains of Learning – Cognitive (understanding) – Psychomotor (motor skills) – Affective (attitudes)
Cognitive • • • Recall facts, information Understand concepts Apply learned ideas, facts Analyze Problem solve Intellectual abilities
Psychomotor • • • Use muscular action Use control Demonstrate a skill Perform an action Manipulate objects Ability to perform
Affective • • • Change Attitudes, beliefs, values Develop Specific feelings, interests Involves emotions & attitudes
Sequence of Events • • What’s going to happen when Timing Research Immediately before for children
Expected Behaviors • • • NPO Medications Leave valuables, jewelry at home Ride home Responsible caregiver
Postoperative Behaviors • • Passive exercises Ambulation Deep breathing & coughing Dressing care Diet Signs & symptoms Emergency contacts
Alterations in Comfort Level • • Pain Sore throat Strategies to reduce pain Nausea & Vomiting
Education Materials • • Written: handouts, booklets Teaching models: joints, ear, eye, devices, etc. Demonstration: physical skills Audiovisual programs: videotapes, slides, photographs

Teaching Methods/Materials • • • Individual Group Tours (4 -12 year olds) Play Therapy (3 -7 years of age) Written (5 -6 th grade level) Models ( 3 -6 year olds) Films – Videos (7 – 12 years old) Demonstrations Teleconferencing
The patient receives education and training specific to patient’s needs and as appropriate to care and services provided by the organization. • The assessment of learning needs addresses – Cultural and religious beliefs – Emotional barriers – Desire and motivation to learn – Physical or cognitive limitations – Barriers to communication – The content is presented in an understandable manner. – Comprehension is evaluated
Discharge Teaching Identify the Regulatory agencies expectations regarding patient discharge teaching. Describe topics that need to be addressed in patient discharge teaching.
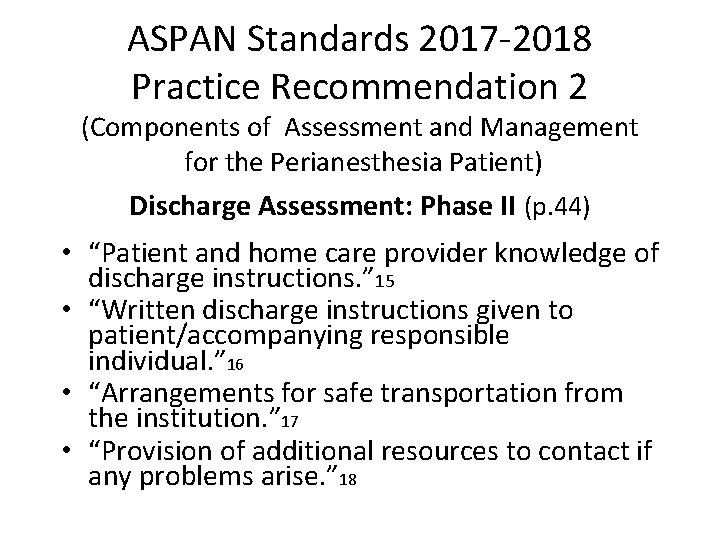
ASPAN Standards 2017 -2018 Practice Recommendation 2 (Components of Assessment and Management for the Perianesthesia Patient) Discharge Assessment: Phase II (p. 44) • “Patient and home care provider knowledge of discharge instructions. ” 15 • “Written discharge instructions given to patient/accompanying responsible individual. ” 16 • “Arrangements for safe transportation from the institution. ” 17 • “Provision of additional resources to contact if any problems arise. ” 18
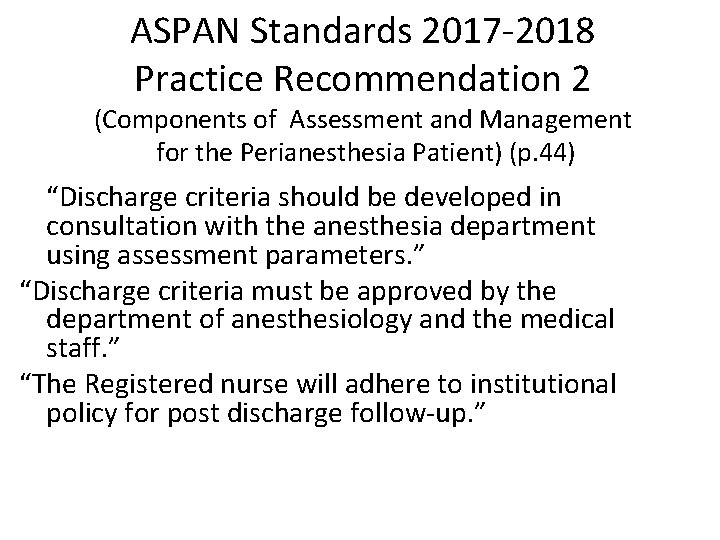
ASPAN Standards 2017 -2018 Practice Recommendation 2 (Components of Assessment and Management for the Perianesthesia Patient) (p. 44) “Discharge criteria should be developed in consultation with the anesthesia department using assessment parameters. ” “Discharge criteria must be approved by the department of anesthesiology and the medical staff. ” “The Registered nurse will adhere to institutional policy for post discharge follow-up. ”
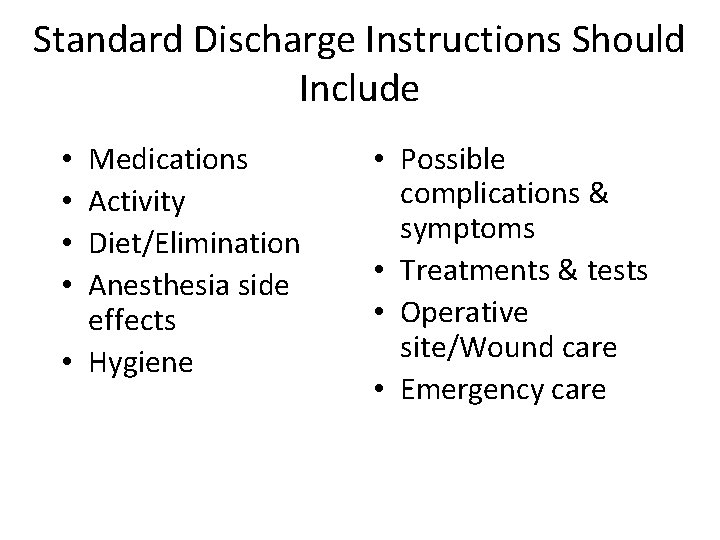
Standard Discharge Instructions Should Include Medications Activity Diet/Elimination Anesthesia side effects • Hygiene • • • Possible complications & symptoms • Treatments & tests • Operative site/Wound care • Emergency care

Medications • Previously prescribed meds – When to resume • Newly prescribed meds – Name, dose, purpose, time ‘Next dose due’ should be written on Discharge Instruction sheet (antibiotics, pain meds)
Newly Prescribed Analgesic Medications • Drug name, dose, purpose • Proper usage according to onset and duration of action and physician prescription • Self medication using pain scale • Acetaminophen warning if appropriate • What to do if pain is not relieved • Driving/alcohol use while taking pain medications
Activity Restrictions • Next 24 hours – Light activity/no important decisions/no driving • • Dizziness/drowsiness expected Restrictions depend on surgical procedure Lifting/weight bearing Be in the care of a responsible adult for first 24 hours
Diet/Elimination • Any restrictions ordered by MD • Foods to avoid – May cause PONV (spicy/greasy) • Laxatives/stool softeners – Due to opioids or procedure – Diet alterations to minimize constipation • Voiding – By when and what to do if unable
Anesthesia Side Effects General Anesthesia/Sedation • Dizziness/drowsiness – Rise slowly, limit activity • • PONV, myalgia Sore throat Impaired psychomotor and cognitive skills General malaise

Anesthesia Side Effects Regional / Blocks • Motor function may return before sensory – Protect limb • Careful positioning and protection • Signs and symptoms that should be reported and who to contact
Hygiene • When patient can bathe and shower • How to protect dressings or incision • What to do with drains while bathing

Possible Complications • Signs and symptoms indicative of postop complications – Fever > 38. 3°C (101°F) – Breathing problems – Bleeding – dressing saturated with continually increasing amount of blood – Pain unrelieved by medication
Possible Complications • Urinary retention or inability to void within defined time frame • Persistent PDNV • Extreme swelling/redness around surgical wound • Drainage change to yellow or green • Change in pain: increase in or change in location or characteristic

Treatments or Tests • Procedures – Dressing changes, ice/heat treatment • • List supplies needed Follow-up tests if ordered Postop follow-up with surgeon Teaching about – Use of crutches, incentive spirometer, antiembolic stockings, drain/catheter care
Operative Site/Wound Care • Instructions for care – Dressing changes • Prevention of infection – Including hand washing & dressing disposal • Sexual activity – Clarify physician’s instructions if appropriate • Extremity care – Swelling, numbness or tingling • Ice/elevation as ordered
Emergency Care • When to seek treatment • Whom to contact • Where to go
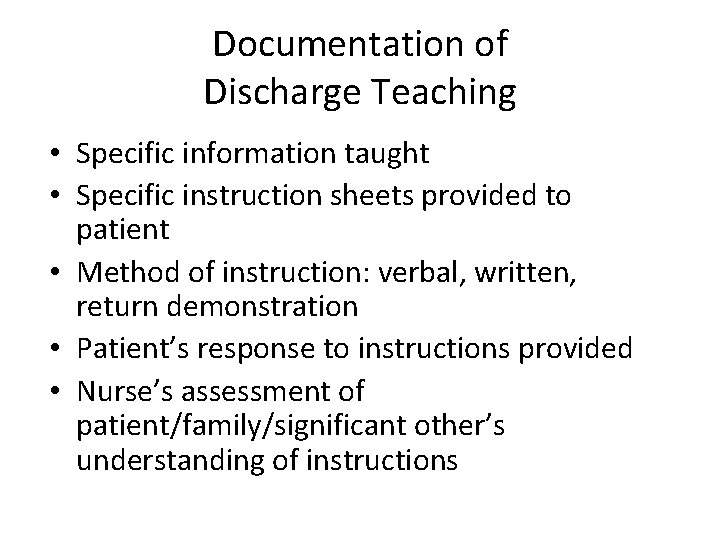
Documentation of Discharge Teaching • Specific information taught • Specific instruction sheets provided to patient • Method of instruction: verbal, written, return demonstration • Patient’s response to instructions provided • Nurse’s assessment of patient/family/significant other’s understanding of instructions
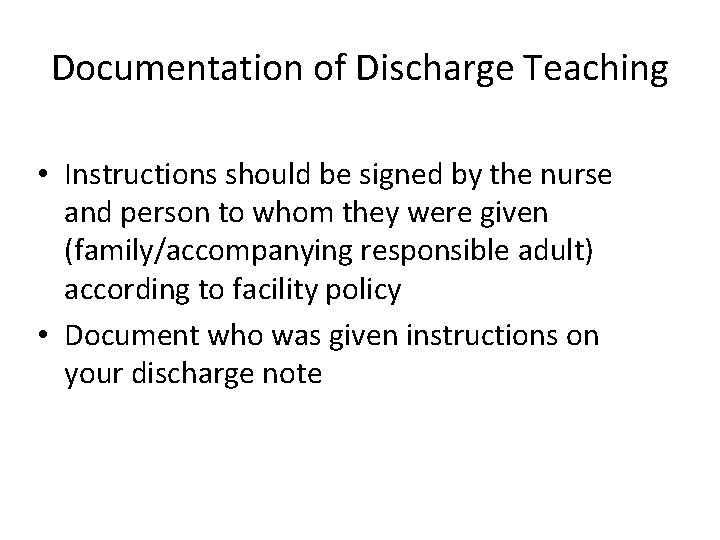
Documentation of Discharge Teaching • Instructions should be signed by the nurse and person to whom they were given (family/accompanying responsible adult) according to facility policy • Document who was given instructions on your discharge note

PACU Discharge Criteria • Awake with muscle strength • Patent airway / good respiratory function • Stable vital signs • Patency of tubes, catheters, IV’s • Condition of surgical site • Comfort / anxiety
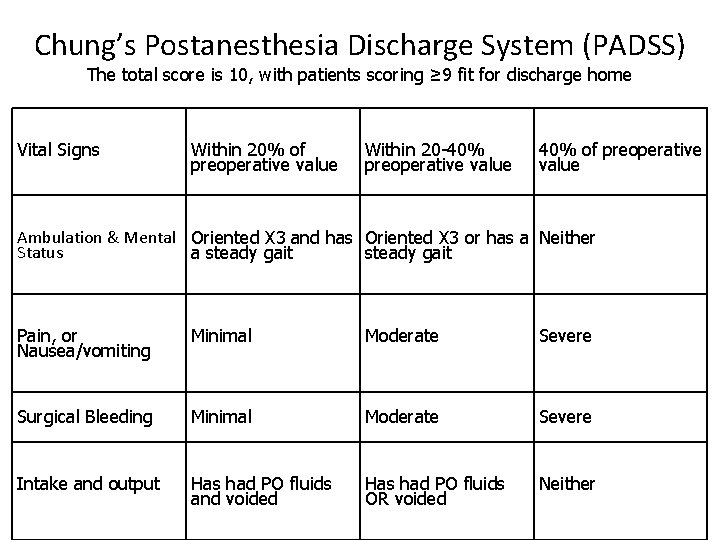
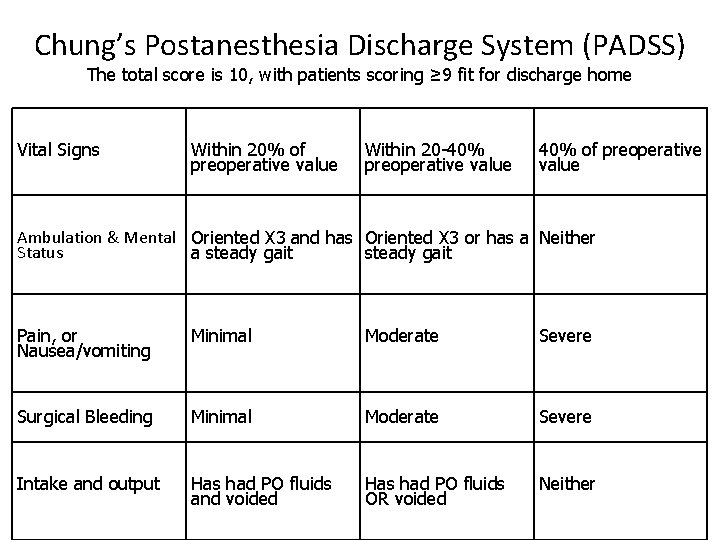
Chung’s Postanesthesia Discharge System (PADSS) The total score is 10, with patients scoring ≥ 9 fit for discharge home Vital Signs Within 20% of preoperative value Within 20 -40% preoperative value 40% of preoperative value Ambulation & Mental Oriented X 3 and has Oriented X 3 or has a Neither Status a steady gait Pain, or Nausea/vomiting Minimal Moderate Severe Surgical Bleeding Minimal Moderate Severe Intake and output Has had PO fluids and voided Has had PO fluids OR voided Neither

Modified Postanesthesia Discharge Scoring System (MPADSS) The total score is 10, with patients scoring ≥ 9 fit for discharge home Vital Signs Within 20% of preoperative value Within 20 -40% preoperative value 40% of preoperative value Ambulation Steady gait/No dizziness With assistance None/Dizziness Pain Minimal Moderate Severe Nausea/ vomiting Minimal Moderate Severe Surgical Bleeding Minimal Moderate Severe

Aldrete’s Modified Postanesthesia Scoring System A minimum score of 9/10 (and/or return to similar preop status) is achieved prior to transferring the patient to a Phase II recovery area Category Score =2 Score = 1 Score = 0 Respirations Breathes and coughs freely Dyspnea Apnea O 2 Saturation Sp. O 2 > 92% on Room air Supplemental O 2 Sp. O 2 < 92% on O 2 Circulation BP +/- 20 mm Hg preop value BP +/- 20 -50 mm Hg preop value BP +/- 50 mm Hg preop value Level Of Consciousness Awake and oriented Wakens with stimulation Non-responsive Movement Moves 4 limbs spontaneously Moves 0 limbs spontaneously Moves 2 limbs spontaneously
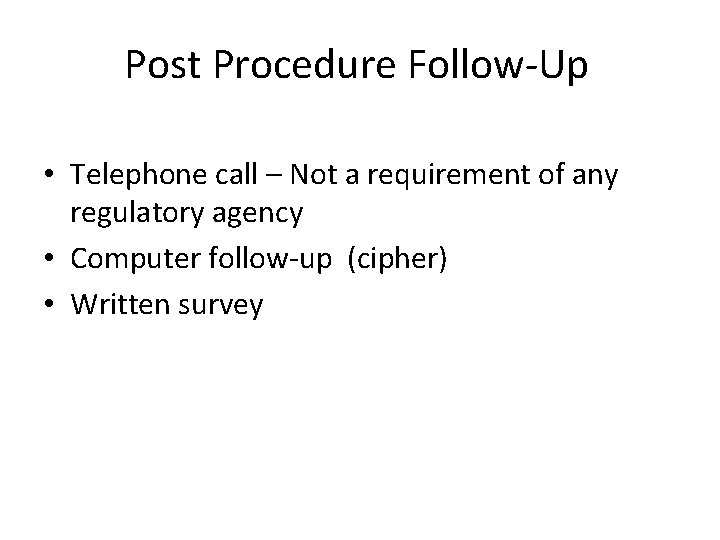
Post Procedure Follow-Up • Telephone call – Not a requirement of any regulatory agency • Computer follow-up (cipher) • Written survey
Purpose of Phone Call Evaluate patient’s general condition Assess patient satisfaction Provide positive marketing for facility Provides nurse with completion; adds to nurse satisfaction • Legally • • – Potential liabilities addressed ASAP, may avoid lawsuit if problem identified/corrected early • Performance Improvement
Postop Phone Calls • Ideally should be done 24 to 48 hours after visit - follow facility policy • Should be done by Perianesthesia nurse (to address patient teaching needs) • Facility policy addresses how many attempts should be made to contact patient
Patient Privacy • Do not call patient at work unless patient requests • Do not divulge to family members who is calling • In Preop ask patient: for an accurate phone number to call and best time to call

Questions to Ask • Do you have any problems related to your procedure or anesthesia? • Are you – Eating, drinking, voiding without difficulty? • Is your pain controlled? • What level of pain are you experiencing? (0 – 10) • Is there anything we could have done to make your stay better? • Did you understand discharge instructions?
Documentation • In patient’s record – Problems identified or statement of patient’s well being – Any issues related to compliance with DC Instructions – Any referrals made to patient
One Last Word About Postop Phone Calls… Share any positive comments from patients to the staff responsible
QUESTIONS
 Pre op certification
Pre op certification Pre operative care
Pre operative care Nursing care plan of patients with cataract
Nursing care plan of patients with cataract Chapter 17 preoperative nursing management
Chapter 17 preoperative nursing management 3 phases of perioperative nursing
3 phases of perioperative nursing Define perioperative nursing
Define perioperative nursing Post operative nursing management
Post operative nursing management Preoperative care ppt
Preoperative care ppt Nursing assessment of glaucoma
Nursing assessment of glaucoma Preoperative medical evaluation of the healthy patient
Preoperative medical evaluation of the healthy patient Cushing's triad
Cushing's triad Taking flight disc
Taking flight disc Pirates test taking strategy
Pirates test taking strategy While taking a difficult test cindy muscles
While taking a difficult test cindy muscles Anxiety symptoms
Anxiety symptoms Staar testing strategies
Staar testing strategies Eog strategies
Eog strategies Test taking skills for middle school
Test taking skills for middle school Test taking strategies for nursing students
Test taking strategies for nursing students Prayer before a big exam
Prayer before a big exam Math multiple choice test taking strategies
Math multiple choice test taking strategies Rubies test taking strategy
Rubies test taking strategy Sol test taking strategies
Sol test taking strategies Michigan department of education teacher certification
Michigan department of education teacher certification Cg-10 application form
Cg-10 application form Educational diagnostician (253)
Educational diagnostician (253) Cpss certification
Cpss certification What is afip certification
What is afip certification Acm case management
Acm case management Indiana teacher certification exams
Indiana teacher certification exams Cris certification test
Cris certification test Airs certification practice test
Airs certification practice test Serosanguineous exudate
Serosanguineous exudate Yellow cottage cheese discharge
Yellow cottage cheese discharge Vaginal discharge meaning
Vaginal discharge meaning Homan's sign
Homan's sign Gonorrhea
Gonorrhea Oral sex
Oral sex Discharge messages
Discharge messages Subcool and superheat explained
Subcool and superheat explained Physalia symmetry
Physalia symmetry Xray van
Xray van Nematocyst discharge
Nematocyst discharge Phyllodes tumor mammogram
Phyllodes tumor mammogram Modified aldrete score
Modified aldrete score Aldrete scoring
Aldrete scoring Uti discharge pictures
Uti discharge pictures Partial discharge in medium voltage switchgear
Partial discharge in medium voltage switchgear 1/2 diagonal rule egress
1/2 diagonal rule egress Candida albicans blastospores
Candida albicans blastospores Aba discharge summary example
Aba discharge summary example What does foamy discharge look like
What does foamy discharge look like What does foamy discharge look like
What does foamy discharge look like White cottage cheese discharge
White cottage cheese discharge Discharge from penis
Discharge from penis Manning formula for discharge
Manning formula for discharge Leiomyomas
Leiomyomas Exit exit access and exit discharge
Exit exit access and exit discharge Glow discharge tem grids
Glow discharge tem grids Discharge abstract database
Discharge abstract database Liquid pipe thermistor
Liquid pipe thermistor Premenstrual discharge
Premenstrual discharge Chapter 11 admission transfer and discharge
Chapter 11 admission transfer and discharge Discharging capacitor equation
Discharging capacitor equation Grey discharge no smell
Grey discharge no smell Grey white discharge
Grey white discharge Unilateral nipple discharge
Unilateral nipple discharge Partial discharge survey
Partial discharge survey Grey cloudy discharge
Grey cloudy discharge Vaginal discharge
Vaginal discharge Bacterial vaginosis
Bacterial vaginosis Grey cloudy discharge
Grey cloudy discharge Premenstrual syndrome discharge
Premenstrual syndrome discharge Reva rubin
Reva rubin Pid discharge pictures
Pid discharge pictures Dark grey discharge
Dark grey discharge Streptococcus pneumoniae csf
Streptococcus pneumoniae csf What is discharge fluid mechanics
What is discharge fluid mechanics Terminal method of family planning
Terminal method of family planning Discharge by performance
Discharge by performance Discharge letter from mental health services
Discharge letter from mental health services Chapter 11 admission transfer and discharge
Chapter 11 admission transfer and discharge What is percussion welding
What is percussion welding Design discharge for bridge
Design discharge for bridge Fertile discharge
Fertile discharge Admission of patients in hospital
Admission of patients in hospital Chapter 9 admission transfer discharge and physical exams
Chapter 9 admission transfer discharge and physical exams Mental health discharge planning checklist
Mental health discharge planning checklist Mental health discharge planning checklist
Mental health discharge planning checklist Two types of transferable discharge permits
Two types of transferable discharge permits A very dramatic electric discharge
A very dramatic electric discharge Exit interview process flowchart
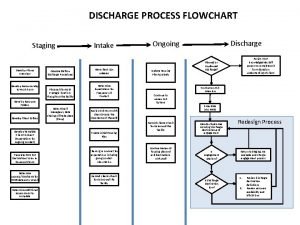
Exit interview process flowchart Discharge by breach
Discharge by breach Chapter 14 discharge
Chapter 14 discharge Chapter 10 discharge
Chapter 10 discharge Admission transfer discharge and physical exams
Admission transfer discharge and physical exams Std with white discharge
Std with white discharge Site:slidetodoc.com
Site:slidetodoc.com Discharge by performance
Discharge by performance Electrical discharge
Electrical discharge Esd awareness
Esd awareness The phrase “quantum meruit” literally means
The phrase “quantum meruit” literally means Depth of discharge
Depth of discharge Capacitor discharge circuit schematic
Capacitor discharge circuit schematic What is a river discharge
What is a river discharge Gray discharge
Gray discharge Terumo same day discharge
Terumo same day discharge Lighting discharge
Lighting discharge Signs of chlamydia
Signs of chlamydia Uti discharge pictures
Uti discharge pictures Vaginal discharge chart
Vaginal discharge chart 2021 involuntary separation pay chart
2021 involuntary separation pay chart Peak discharge
Peak discharge Cms-r-193
Cms-r-193 Manning formula
Manning formula Black fungus mucus color
Black fungus mucus color Discharge certificate from hospital
Discharge certificate from hospital Salpingitis
Salpingitis Plasma discharge
Plasma discharge Plasma discharge
Plasma discharge Starpower srl
Starpower srl Criteria led discharge
Criteria led discharge Ldeq
Ldeq Discharge clipart
Discharge clipart Discharge pathways
Discharge pathways Disease synonym
Disease synonym Product principle in portfolio assessment
Product principle in portfolio assessment