The post natal care Faculty of nursing Islamic



- Slides: 34

The post natal care Faculty of nursing Islamic university of Gaza 2018 - 2019

The post natal care Postpartum care begins immediately after childbirth. During this time, the nurse assists the new mother in learning how to care for herself and her baby. This 6 -week period of time, also known as the puerperium.
Early Maternal Assessment VITAL SIGNS: - Blood pressure - Temp - Pulse - Respiration During the postpartum period, vital signs can alert the nurse to the presence of hemorrhage or infection and should be monitored according to hospital policy. Vital signs are typically monitored every 15 minutes during the first hour after childbirth, then every 30 minutes during the second hour, once during the third hour, and then every 8 hours until discharge or until they are stable.
Temperature During the first 24 hours postpartum, some women experience an increase in body temperature up to (38°C). High temperature at this time may be indicative of infection. Pulse Heart rates of 50 to 70 beats per minute (bradycardia) commonly occur during the first 6 to 10 days of the postpartum period. During pregnancy, the weight of the gravid uterus causes a decreased flow of venous blood to the heart. The elevated stroke volume leads to a decreased heart rate. Postpartal tachycardia may result from a complication, prolonged labor, blood loss, temperature elevation, or infection.
Blood Pressure Decreased blood pressure may result from the physiological changes associated with the decrease in intrapelvic pressure, or it may be indicative of uterine hemorrhage. An increase in the systolic blood pressure of 30 mm Hg or 5 mm Hg in the diastolic blood pressure, especially when associated with headaches or visual changes, may be a sign of gestational hypertension. Orthostatic hypotension may occur when the patient moves from a supine to a sitting position. Respirations The respiratory rate normal range of 12 to 20 respirations per minute. Elevated respirations may occur due to pain, fear, excitement, exertion, or excessive blood loss. Tachypnea, abnormal lung sounds, shortness of breath, chest pain, anxiety, or restlessness are abnormal findings that must be reported immediately. These signs and symptoms may be indicative of pulmonary edema or emboli.
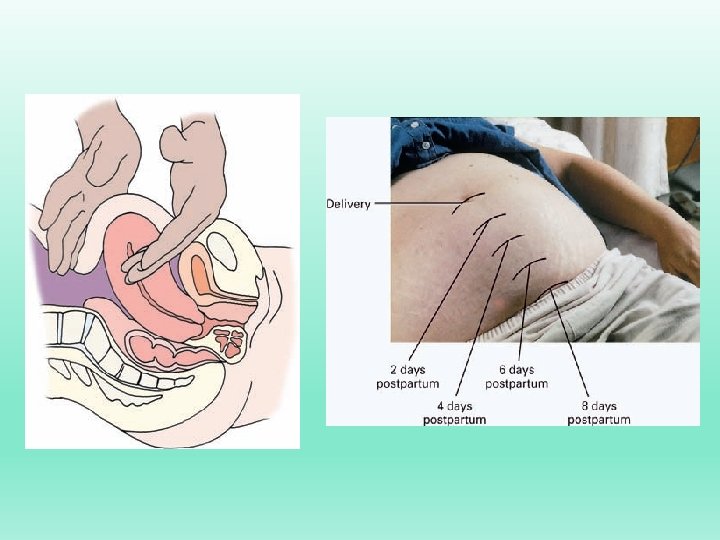
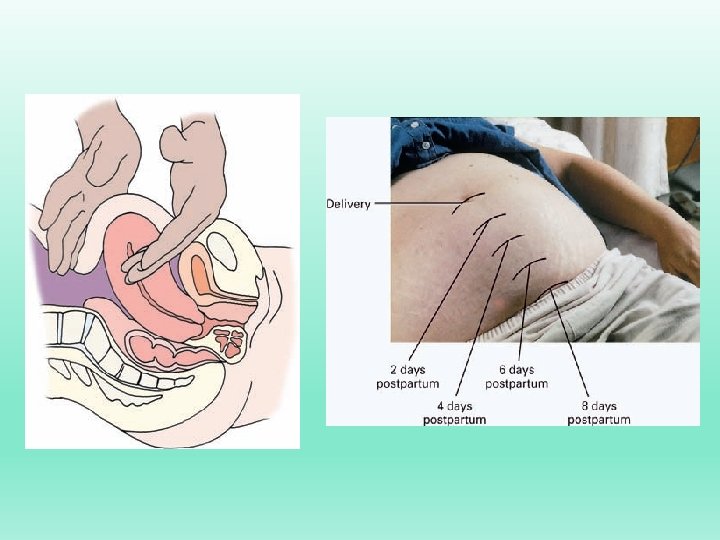
FUNDUS, LOCHIA, PERINEUM Within a few minutes after birth, the firmly contracted uterine fundus should be palpable through the abdominal wall halfway between the umbilicus and the symphysis pubis. Approximately 1 hour later, the fundus should have risen to the level of the umbilicus, where it remains for the following 24 hours. [Uterine assessment crucial during the first hour postpartum] Because the first post-partal hour represents the most dangerous time for the patient, it is essential that the nurse conduct frequent uterine assessments during this time. Relaxation of the uterus (a tony) results in rapid, life threatening blood loss because no permanent thrombi have yet formed at the placental site.
- perineum need to be assessed every 15 minutes during the immediate postpartum period. - To facilitate the perineal assessment, the nurse assists the patient into a Sim’s (side-lying) position with her back facing the nurse. Use of the acronym REEDA guides the nurse to assess for Redness, Edema, Ecchymosis, Drainage or discharge, and Approximation of the episiotomy if present. - The episiotomy and/or laceration repairs should appear intact with the tissue edges closely approximated. - Episiotomy: is a surgical incision of the perineum is performed to enlarge the vaginal orifice during labor.
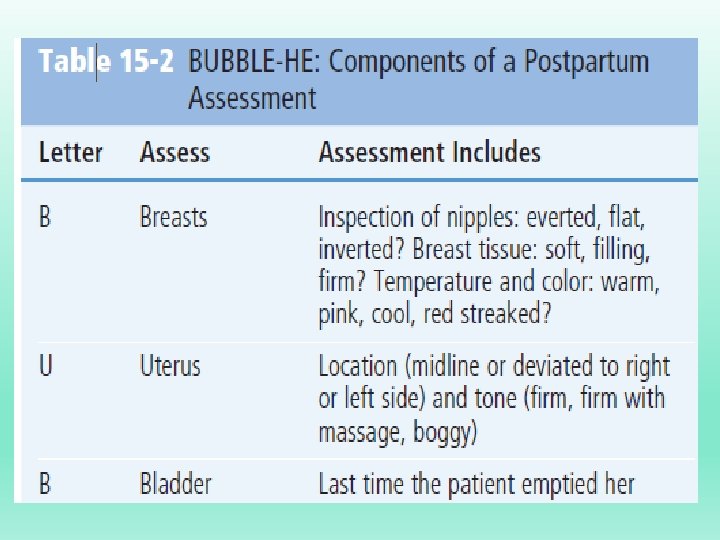
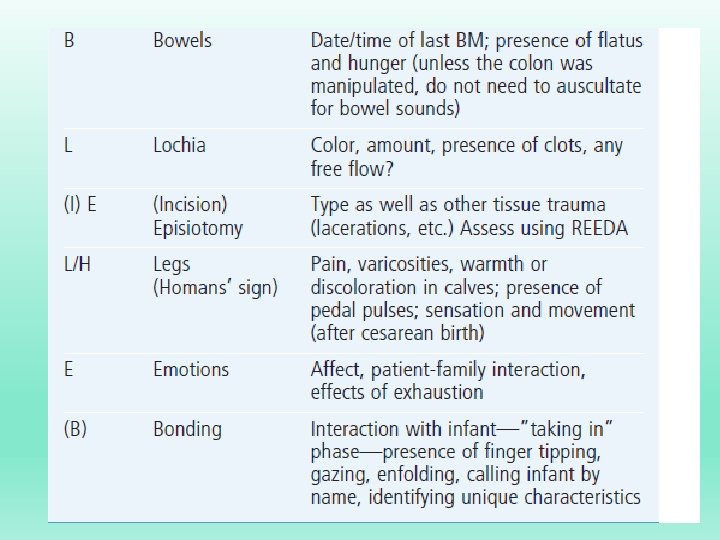
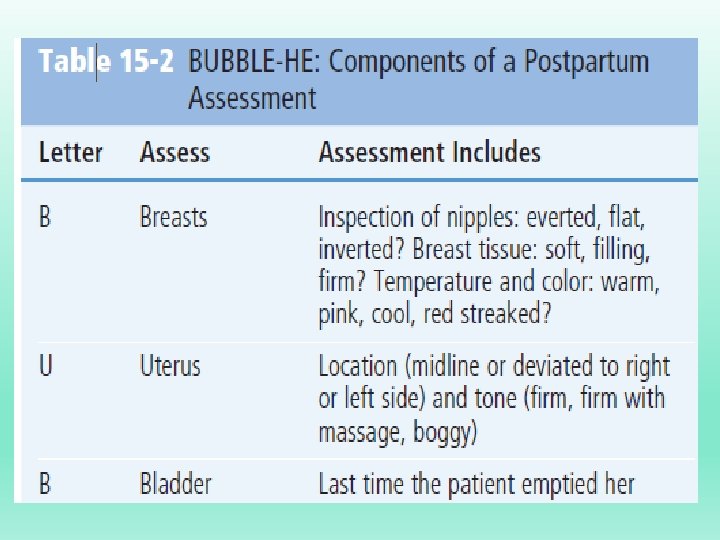
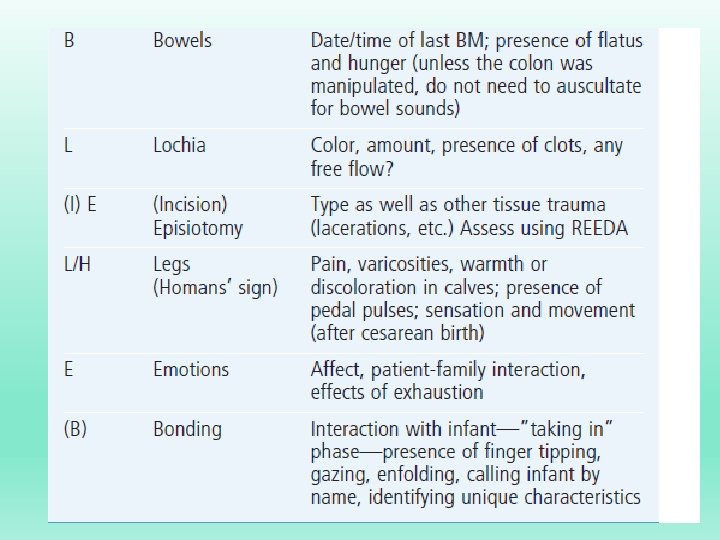
Postpartum Assessment Guide to Facilitate Nursing Care THE BUBBLE-HE MNEMONIC To assist with the postpartum assessment, the mnemonic BUBBLE-HE is commonly used to guide nursing practice. BUBBLE-HE reminds the nurse to assess the breasts, uterus, bladder, bowel, lochia, and episiotomy. Assessment of maternal pain, Homans’ sign, the patient’s emotional status and initiation of infant bonding are other important components to be included in the postpartum evaluation (Table below).
Uterus Involution: is a term that describes the process whereby the uterus returns to the non-pregnant state. - Immediately after expulsion of the placenta, the uterus rapidly contracts to prevent hemorrhage. - The uterus weighs approximately 1000 g in the immediate pos-tpartal period and by the end of the first week, its weight has diminished to 500 g. Uterine size and weight continue to decrease and on average, the uterus weighs 300 g by the end of the second week
Subinvolution: is the failure of the uterus to return to the non-pregnant state. - Uterine involution may be inhibited by multiple births, hydramnios, prolonged labor or difficult birth, infection, grand multiparity, or excessive maternal analgesia. - In addition, a full bladder or retained placental tissue may prevent the uterus from sustaining the contractions needed to prevent hemorrhage or to facilitate involution.
FUNDUS: The uterine fundus can be palpated midline, midway between the umbilicus and symphysis pubis. - Within an hour, the uterus settles in the midline at the level of the umbilicus. Over the course of days, the uterus descends into the pelvis at a rate of about 1 cm/day (one fingerbreadth. - After 10 days, the uterus has descended into the pelvis and is no longer palpable. The fundus is assessed for consistency (firm, soft, or boggy), location (should be midline), and height (measured in finger breadths).
Breasts: - with loss of the placenta, circulating level of estrogen and progesterone will decrease, while increase level of prolactine thus initiating lactation in the postpartum woman. - Colostrum: a yellowish fluid containing more minerals and protin but less sugar and fats than mature breast milk, is secreted for the first 2 day postpartum. - Mature milk secretion: is usually present by the 3 rd day. - Breast engorgement with milk, venous and lymphatic stasis and swollen, tender breast tissue may occur between day 3 -5 postpartum.
Afterpains (afterbirth pains): are intermittent uterine contractions that occur during the process of involution describe as a discomfort similar to menstrual cramps. - The primiparous woman typically has mild afterpains, if she notices them at all, because her uterus is able to maintain a contracted state. - Multiparas and patients with uterine overdistention (e. g. , large baby, multifetal gestation, hydramnios) are more likely to experience afterpains, due to the continuous pattern of uterine relaxation and vigorous contractions.
Breastfeeding and the administration of exogenous oxytocin usually produce pronounced afterpains because both cause powerful uterine contractions. Afterbirth pain is often severe for 2 to 3 days after childbirth. Nursing interventions Øassisting the patient into a prone position Øa small pillow placed under her abdomen Ø initiating sitz baths (for warmth) Øencouraging ambulation Øand administrating mild analgesics.
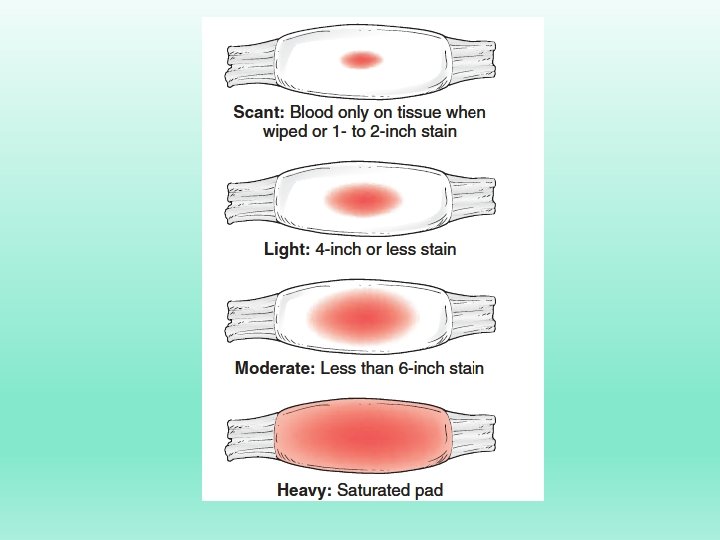
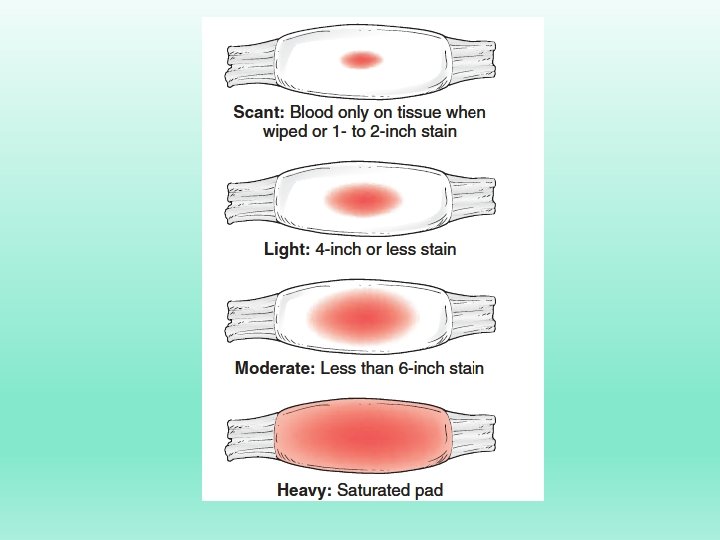
Lochia is composed of erythrocytes; epithelial cells; blood; and fragments of decidua, mucus, and bacteria (Cunningham et al. , 2005). lochia consists : 1) lochia rubra (it a characteristic red color). 2) lochia serosa (3 to 4 days, the lochia becomes the pinkish brownish. 3) Lochia alba (after approximately 10 to 14 days, the uterine. discharge has a reduced fluid content and is largely composed of leukocytes. This combination produces a white or yellow-white thick discharge known as lochia alba. also contains decidual cells, mucus, bacteria, and epithelial cells. It is present until about the third week after childbirth but may persist for 6 weeks.
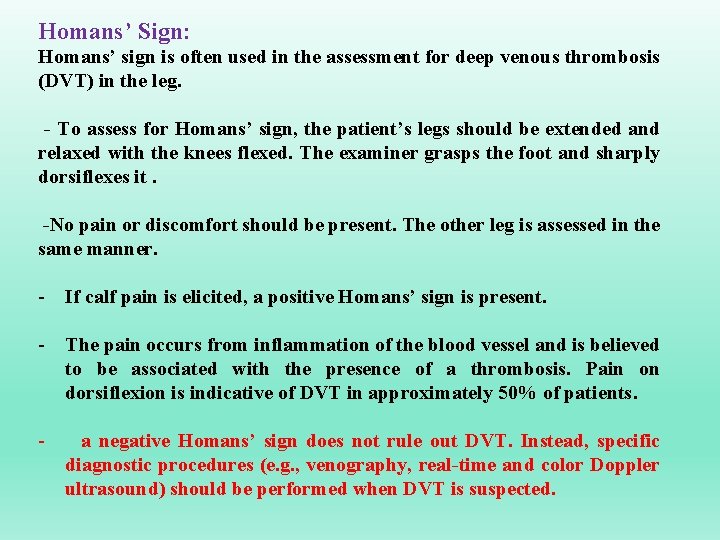
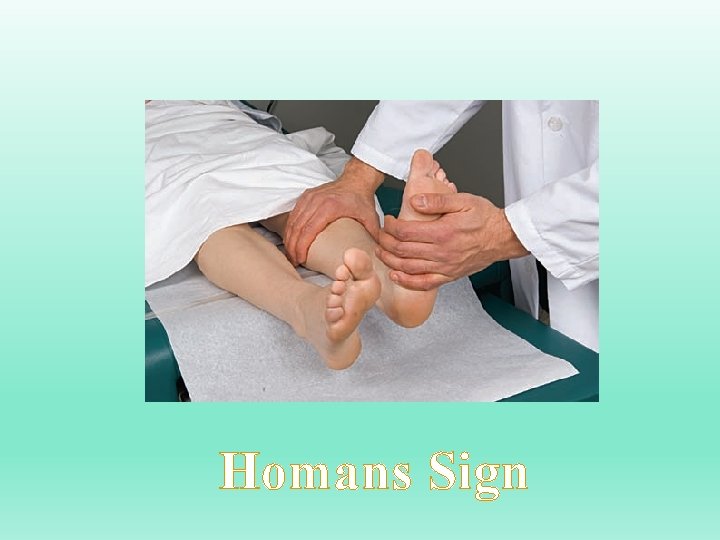
Homans’ Sign: Homans’ sign is often used in the assessment for deep venous thrombosis (DVT) in the leg. - To assess for Homans’ sign, the patient’s legs should be extended and relaxed with the knees flexed. The examiner grasps the foot and sharply dorsiflexes it. -No pain or discomfort should be present. The other leg is assessed in the same manner. - If calf pain is elicited, a positive Homans’ sign is present. - The pain occurs from inflammation of the blood vessel and is believed to be associated with the presence of a thrombosis. Pain on dorsiflexion is indicative of DVT in approximately 50% of patients. - a negative Homans’ sign does not rule out DVT. Instead, specific diagnostic procedures (e. g. , venography, real-time and color Doppler ultrasound) should be performed when DVT is suspected.
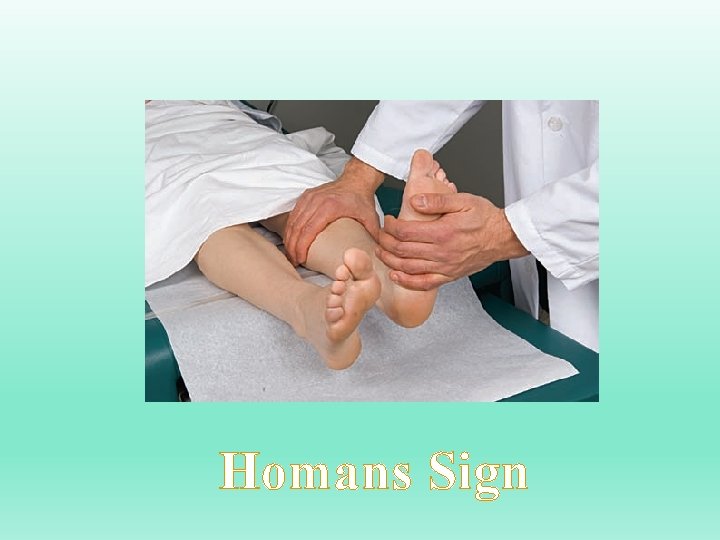
Homans Sign
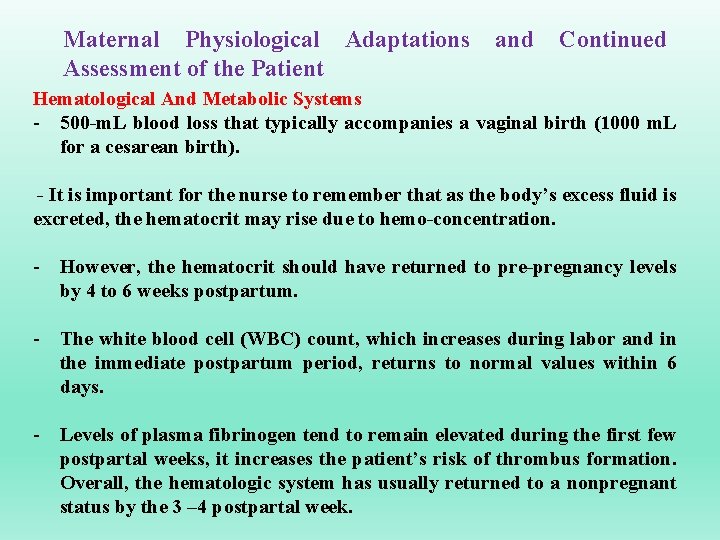
Maternal Physiological Adaptations Assessment of the Patient and Continued Hematological And Metabolic Systems - 500 -m. L blood loss that typically accompanies a vaginal birth (1000 m. L for a cesarean birth). - It is important for the nurse to remember that as the body’s excess fluid is excreted, the hematocrit may rise due to hemo-concentration. - However, the hematocrit should have returned to pre-pregnancy levels by 4 to 6 weeks postpartum. - The white blood cell (WBC) count, which increases during labor and in the immediate postpartum period, returns to normal values within 6 days. - Levels of plasma fibrinogen tend to remain elevated during the first few postpartal weeks, it increases the patient’s risk of thrombus formation. Overall, the hematologic system has usually returned to a nonpregnant status by the 3 – 4 postpartal week.
NEUROLOGICAL SYSTEM (Common Sign) ØFatigue and discomfort are common complaints after childbirth. Øaltered sleep patterns that contribute to increased maternal fatigue. Ø during labor and birth may cause transient maternal neurological changes such as numbness in the legs or dizziness. ØWhen these changes are present, the nursing priority is to safeguard the patient and her infant and prevent injury from falls. Ø Complaints of headaches require further nursing assessment. Ø Patients who received epidural or spinal anesthesia may experience headaches, especially when they assume an upright position. ØAfter spinal or epidural anesthesia, headaches may result from the leakage of cerebrospinal fluid into the extradural space.
IMMUNE SYSTEM The WBC count is increased during labor and birth and remains elevated during the early postpartum period, gradually returning to normal values within 4 to 7 days after childbirth. Women who are rubella susceptible during pregnancy should receive the MMR (measles–mumps– rubella) vaccine at the time of hospital discharge; varicella vaccine should also be encouraged (American College of Obstetricians and Gynecologists [ACOG], 2003).
CARDIOVASCULAR SYSTEM - Despite the usual blood loss (500 m. L with a vaginal birth; 1000 m. L with a cesarean birth), the maternal cardiac output is significantly elevated above pre labor levels for 1 to 2 hours postpartum and remains high for 48 hours postpartum. - The cardiac output returns to pre-pregnant levels within 2 to 4 weeks after childbirth.
GASTROINTESTINAL SYSTEM - Abdominal discomfort results from gaseous distention related to decreased motility and abdominal muscle relaxation. Constipation, a common nursing diagnosis for the pos-tpartal patient, is associated with abdominal discomfort and decreased hunger. - Straining to pass hard stool can cause hemorrhoids and tear episiotomy sutures. Although spontaneous bowel movements usually resume by the second or third day after childbirth, it is important to educate the patient about strategies to prevent constipation. Stool softeners may be necessary
MUSCULOSKELETAL SYSTEM - During the first few days after childbirth, the woman may experience muscle fatigue and general body aches from the exertion of labor and delivery of the baby. - The progressive stretching causes a decrease in the muscle tone of the rectus muscles of the abdomen and results in the soft, flabby, and weak muscles experienced after birth. - Women should be aware that during the early postpartal period, the abdominal wall may not be sufficiently protected to withstand additional stress from increased activities. - Nurses should teach them to maintain correct posture when performing activities such as lifting, carrying, and bathing the baby for at least 12 weeks after birth.
Postpartum Psychosis Postpartum psychosis develops in approximately one or two women for every 1000 births and is unlikely to manifest itself during the early postpartum period. Symptoms include delusions; hallucinations; agitation; inability to sleep; and bizarre, irrational behavior. Before hospital discharge, patients with a history of mood disorders or depression should be referred to appropriate resources for community support and followup
Nursig diagnosis: - potential bleeding related to vaginal delivery, episiotomy, complication. - Discomfort (backache, uterine cramping, breast engrogement…. ) related to process of labor. - Urinary retention related to bladder trauma. - Constipation related to episiotomy, decreased muscle tone of the intestine. - Risk for infection related to prolonged labor, vaginal delivery, laceration. - Knowledge deficit related to inadequate childbirth, parenting preparation, lack of self-confidence. - Anxiety related chronic fatigue, adapting a new family member, inability to integrate that with labor experience.
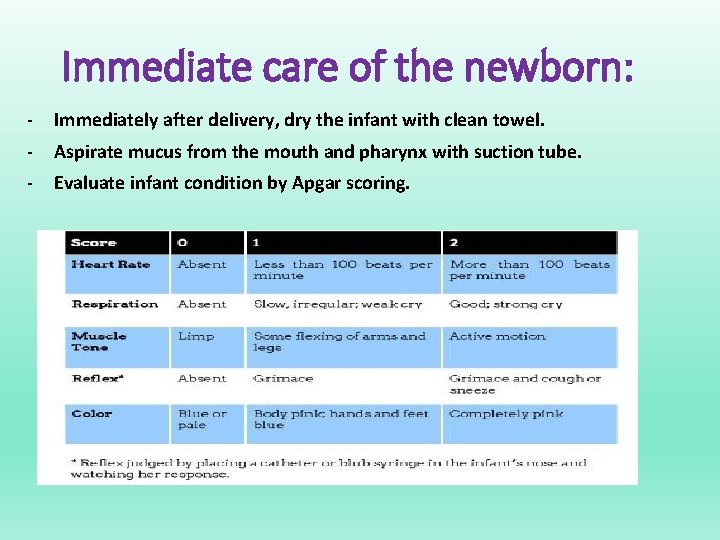
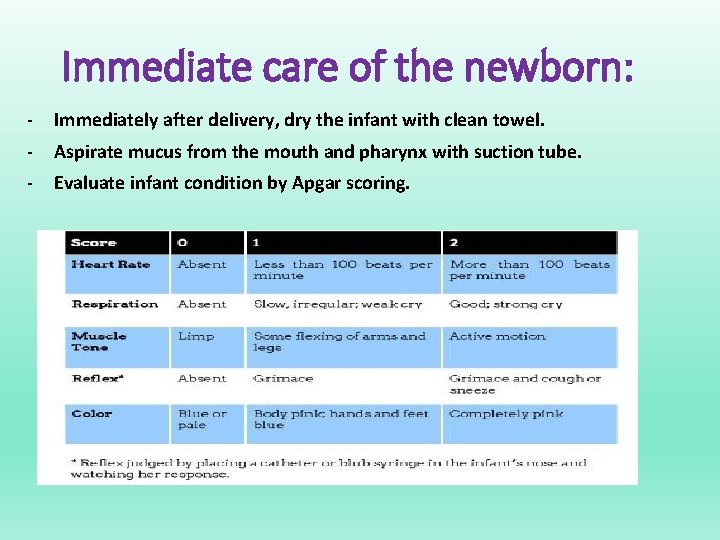
Immediate care of the newborn: - Immediately after delivery, dry the infant with clean towel. - Aspirate mucus from the mouth and pharynx with suction tube. - Evaluate infant condition by Apgar scoring.
*Infants scoring(7 -10) : are free of immediate stresses. *Infants scoring(4 -6 ) : are moderately depressed. *Infants scoring(0 -3 ) : are severely depressed. - Tie off the umblical cord approximately 2. 5 cm from abdominal wall using a plastic clamp. - Administer 1 mg of vit K. - Apply ID band include mother name, infant sex , time and date of the birth. - Weight and measure the infant.
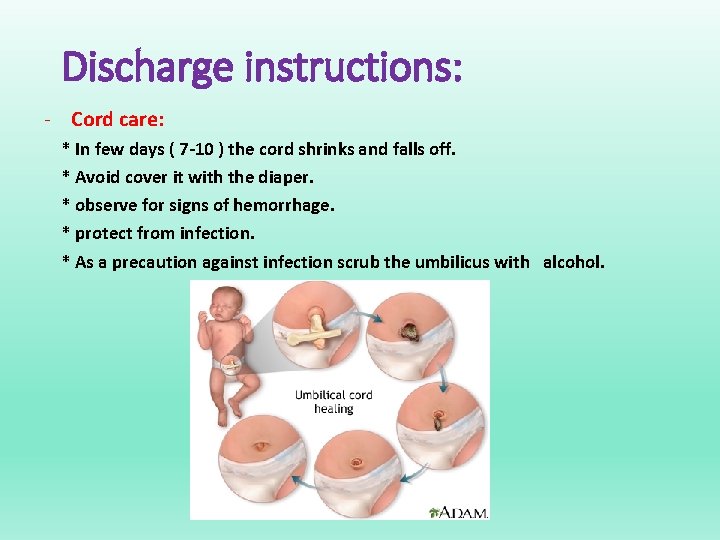
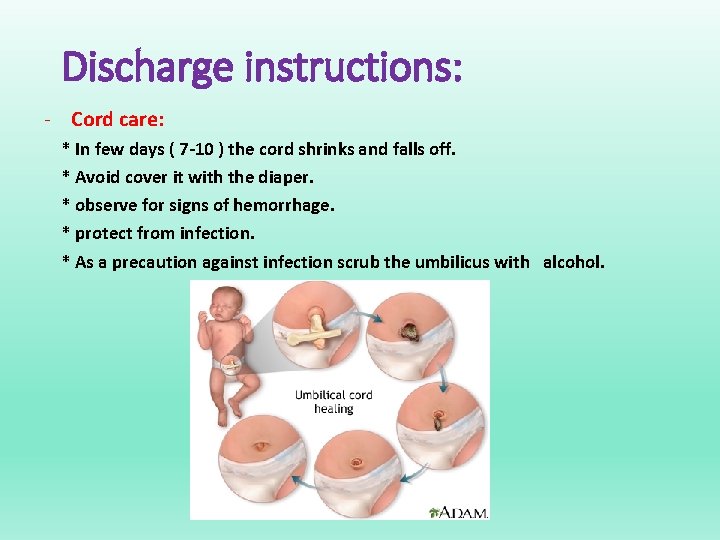
Discharge instructions: - Cord care: * In few days ( 7 -10 ) the cord shrinks and falls off. * Avoid cover it with the diaper. * observe for signs of hemorrhage. * protect from infection. * As a precaution against infection scrub the umbilicus with alcohol.
- Follow up. Bathing and diapering. Breast and formula feeding. Measuring body temp. Recognizing reportable signs and symptoms “ pallor, cyanosis, vomiting, diarrhea, abdominal respiration, fever, hypothermia…”

THANKS A LOT