Gonorrhea trichomoniasis chlamidiosis candidal and mycotic affection of
















- Slides: 58

Gonorrhea, trichomoniasis, chlamidiosis, candidal and mycotic affection of the skin. Lector: Shkilna M.
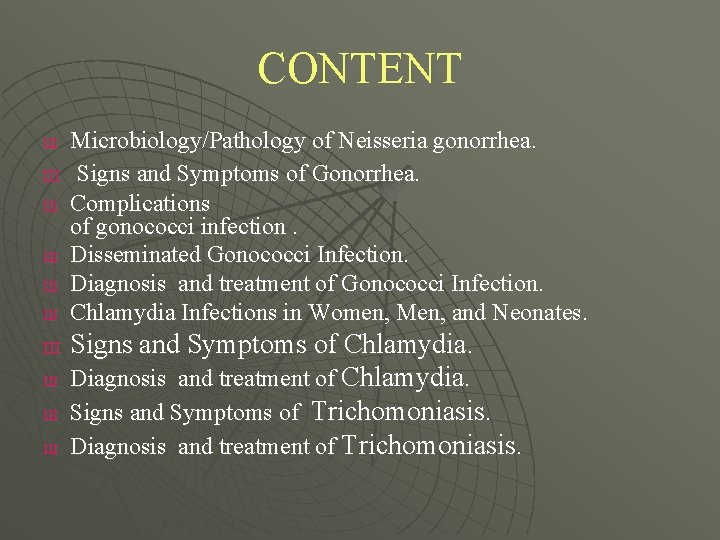
CONTENT Ш Ш Ш Ш Ш Microbiology/Pathology of Neisseria gonorrhea. Signs and Symptoms of Gonorrhea. Complications of gonococci infection. Disseminated Gonococci Infection. Diagnosis and treatment of Gonococci Infection. Chlamydia Infections in Women, Men, and Neonates. Signs and Symptoms of Chlamydia. Diagnosis and treatment of Chlamydia. Signs and Symptoms of Trichomoniasis. Diagnosis and treatment of Trichomoniasis.
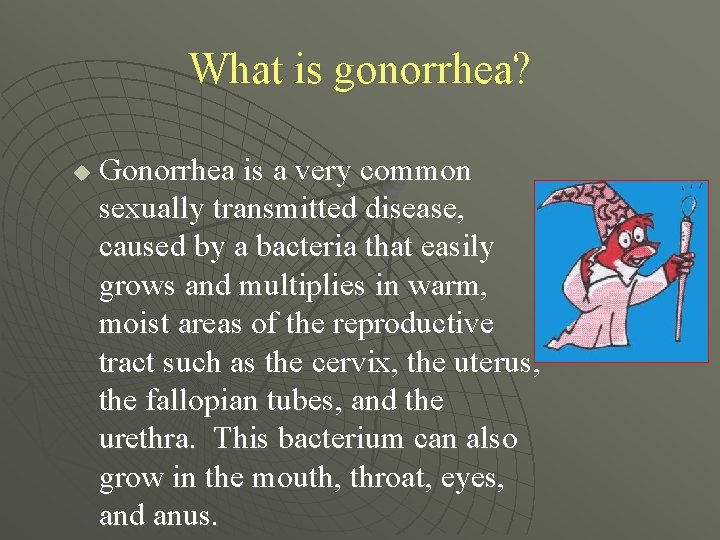
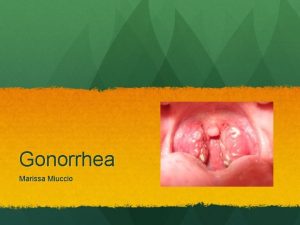
What is gonorrhea? u Gonorrhea is a very common sexually transmitted disease, caused by a bacteria that easily grows and multiplies in warm, moist areas of the reproductive tract such as the cervix, the uterus, the fallopian tubes, and the urethra. This bacterium can also grow in the mouth, throat, eyes, and anus.
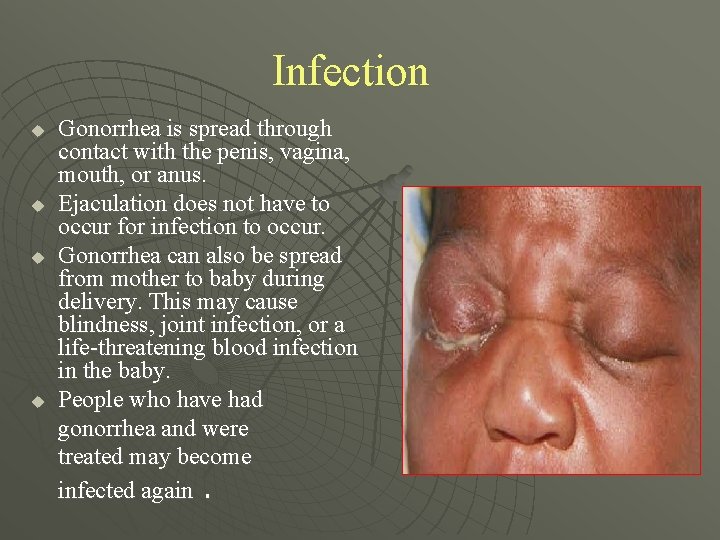
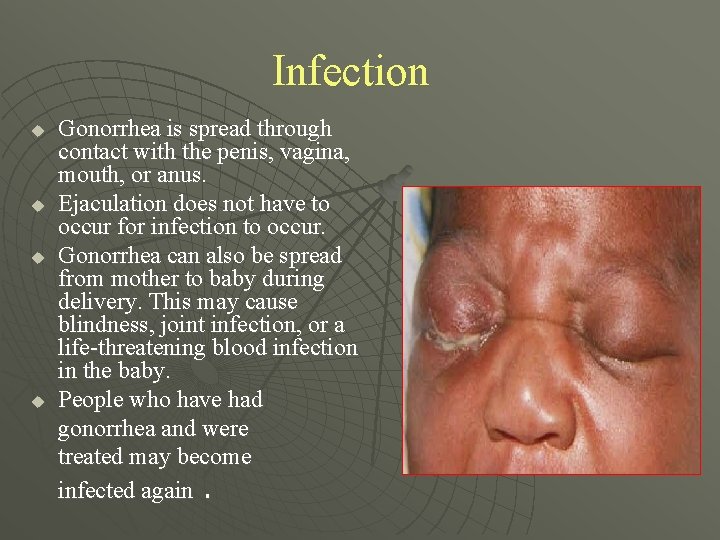
Infection u u Gonorrhea is spread through contact with the penis, vagina, mouth, or anus. Ejaculation does not have to occur for infection to occur. Gonorrhea can also be spread from mother to baby during delivery. This may cause blindness, joint infection, or a life-threatening blood infection in the baby. People who have had gonorrhea and were treated may become infected again.
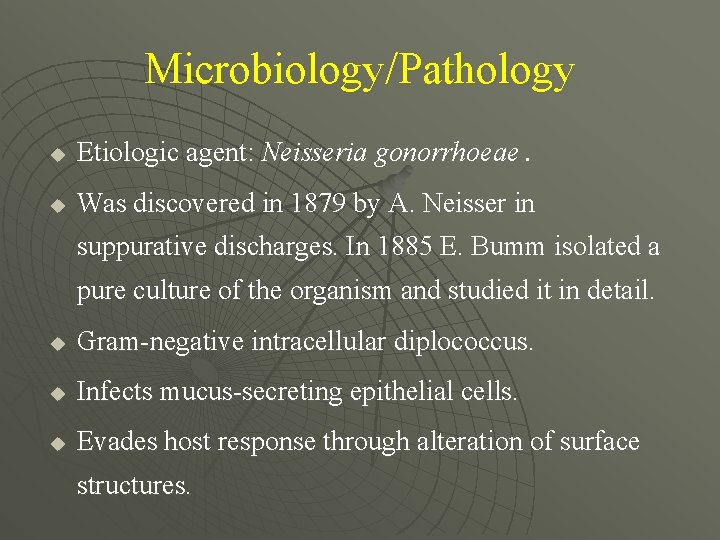
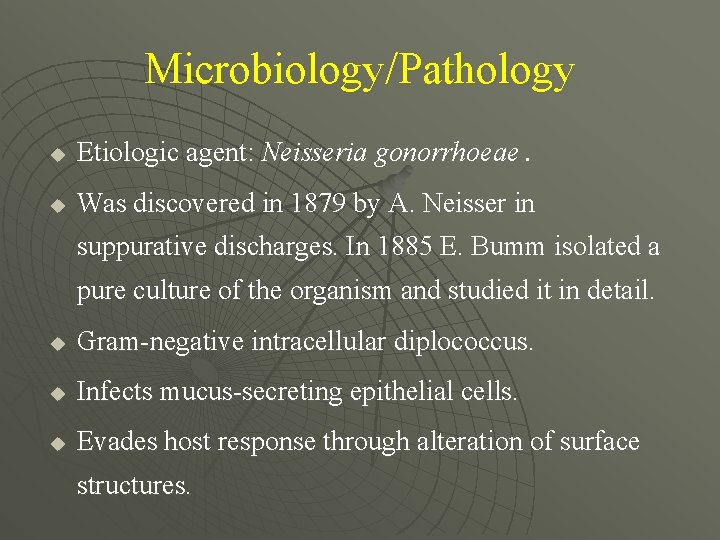
Microbiology/Pathology u Etiologic agent: Neisseria gonorrhoeae. u Was discovered in 1879 by A. Neisser in suppurative discharges. In 1885 E. Bumm isolated a pure culture of the organism and studied it in detail. u Gram-negative intracellular diplococcus. u Infects mucus-secreting epithelial cells. u Evades host response through alteration of surface structures.
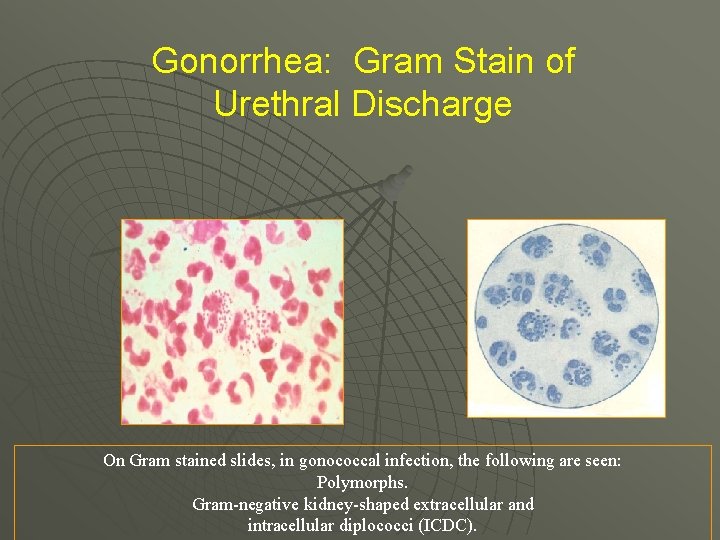
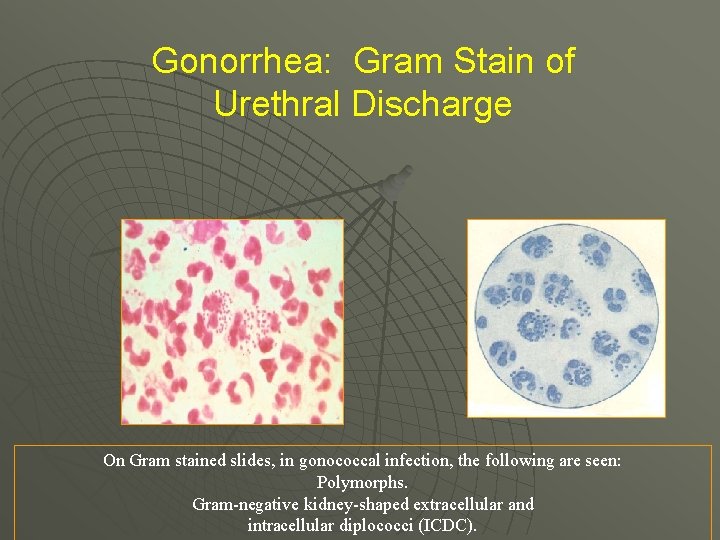
Gonorrhea: Gram Stain of Urethral Discharge On Gram stained slides, in gonococcal infection, the following are seen: Polymorphs. Gram-negative kidney-shaped extracellular and intracellular diplococci (ICDC).

Gram stain of urethral discharge showing gram negative, intracellular diplococci.
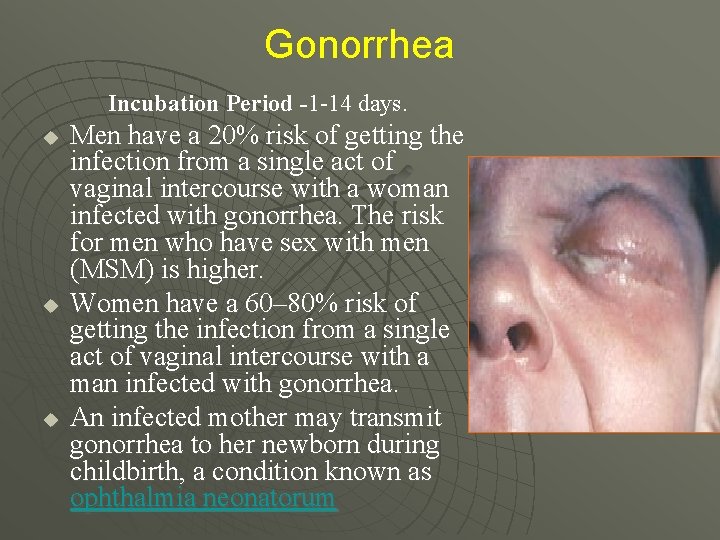
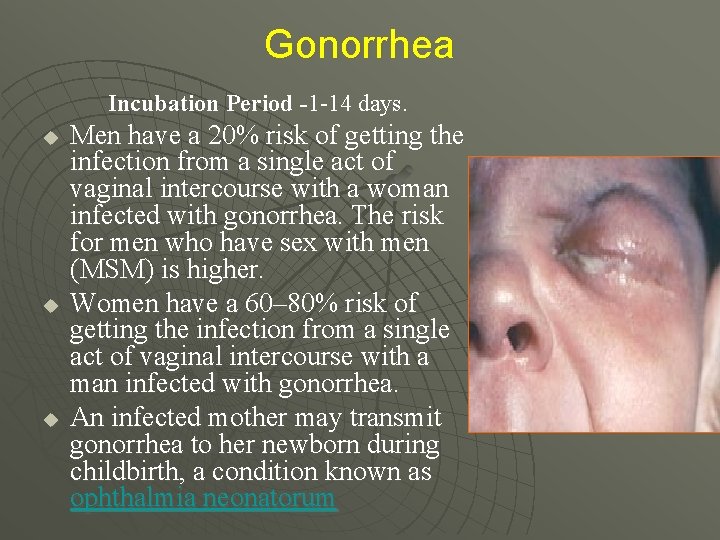
Gonorrhea Incubation Period -1 -14 days. u u u Men have a 20% risk of getting the infection from a single act of vaginal intercourse with a woman infected with gonorrhea. The risk for men who have sex with men (MSM) is higher. Women have a 60– 80% risk of getting the infection from a single act of vaginal intercourse with a man infected with gonorrhea. An infected mother may transmit gonorrhea to her newborn during childbirth, a condition known as ophthalmia neonatorum
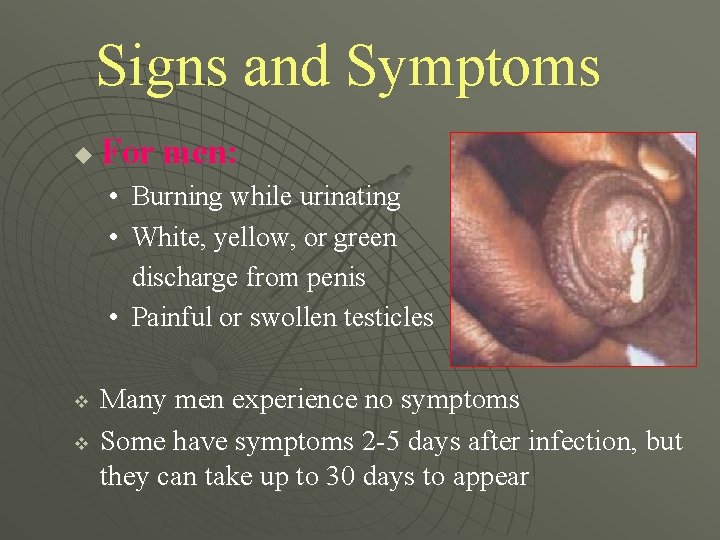
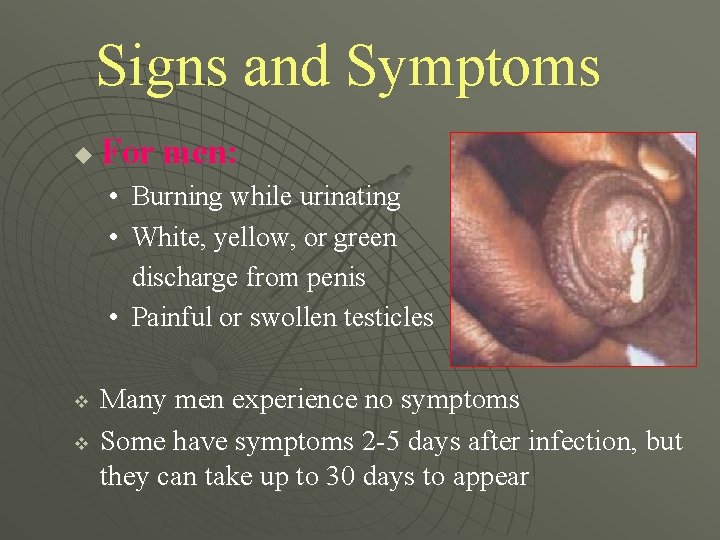
Signs and Symptoms u For men: • Burning while urinating • White, yellow, or green discharge from penis • Painful or swollen testicles v v Many men experience no symptoms Some have symptoms 2 -5 days after infection, but they can take up to 30 days to appear
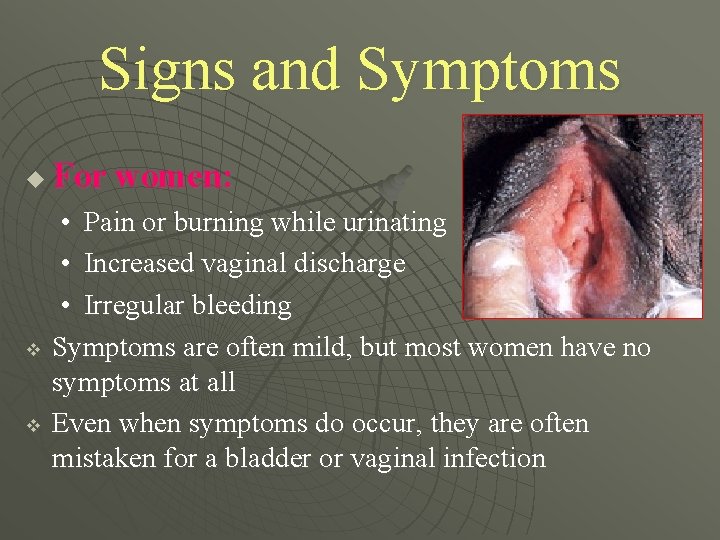
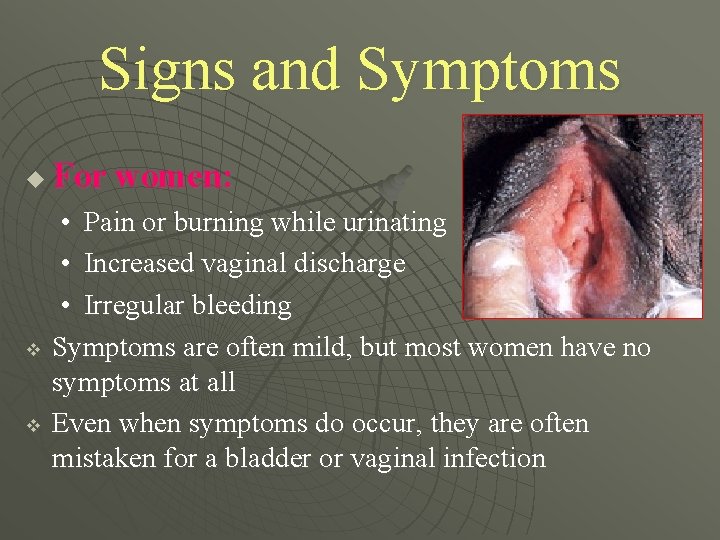
Signs and Symptoms u v v For women: • Pain or burning while urinating • Increased vaginal discharge • Irregular bleeding Symptoms are often mild, but most women have no symptoms at all Even when symptoms do occur, they are often mistaken for a bladder or vaginal infection

Gonococcal Bartholinitis n n Tender swollen Bartholin’s gland with purulent discharge Infection at other sites common

Bartholin’s Abscess n n n Painful swollen Bartholin’s glands Fluctuant, tender May have expressible purulent discharge
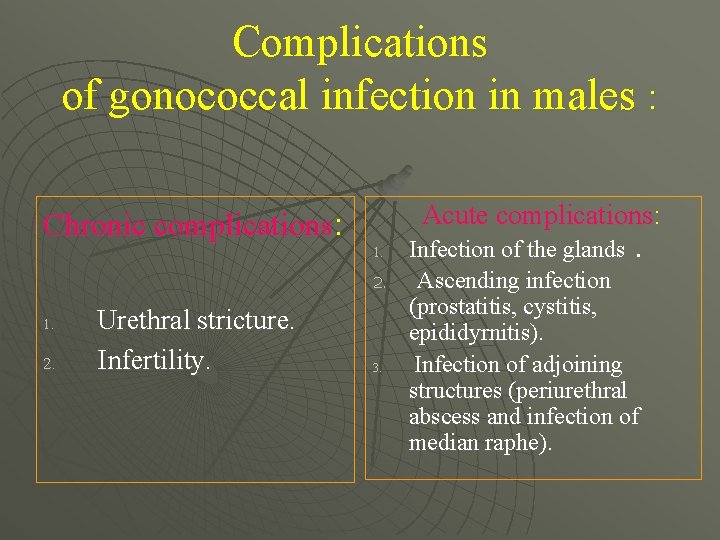
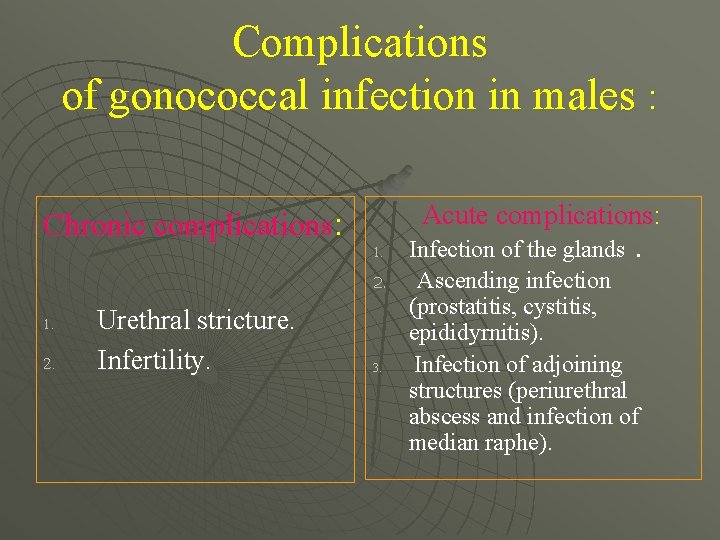
Complications of gonococcal infection in males : Chronic complications: Acute complications: 1. 2. 1. 2. Urethral stricture. Infertility. 3. Infection of the glands. Ascending infection (prostatitis, cystitis, epididyrnitis). Infection of adjoining structures (periurethral abscess and infection of median raphe).
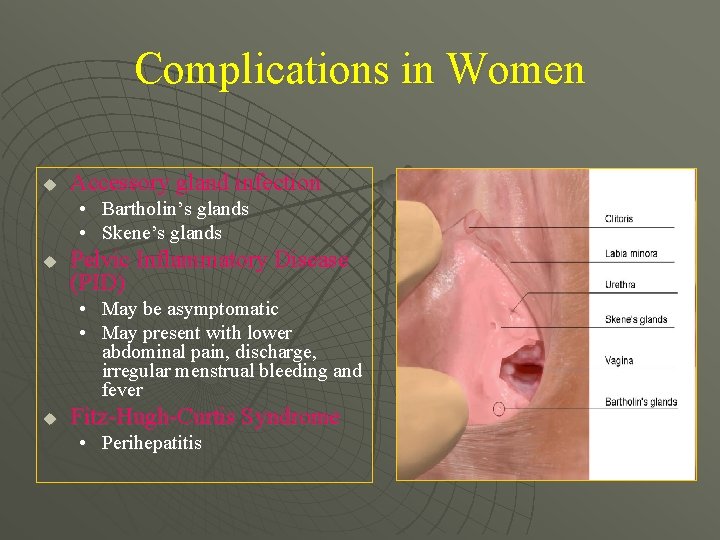
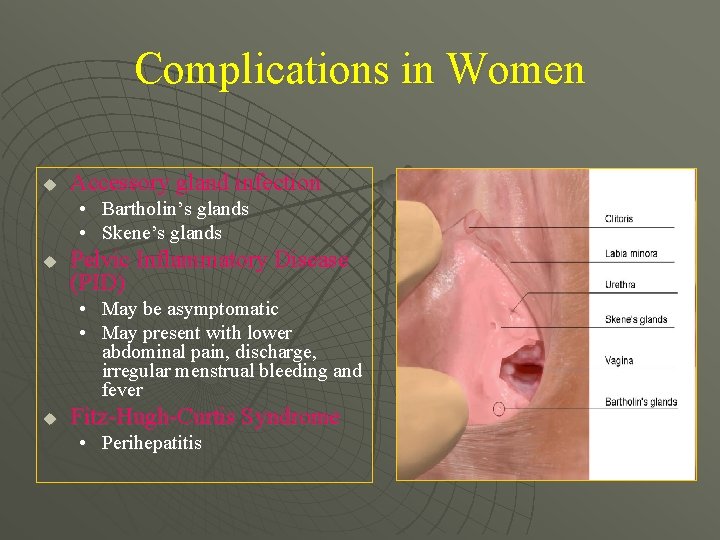
Complications in Women u Accessory gland infection • Bartholin’s glands • Skene’s glands u Pelvic Inflammatory Disease (PID) • May be asymptomatic • May present with lower abdominal pain, discharge, irregular menstrual bleeding and fever u Fitz-Hugh-Curtis Syndrome • Perihepatitis

DISSEMINATED GONORRHEA CLINICAL PRESENTATION
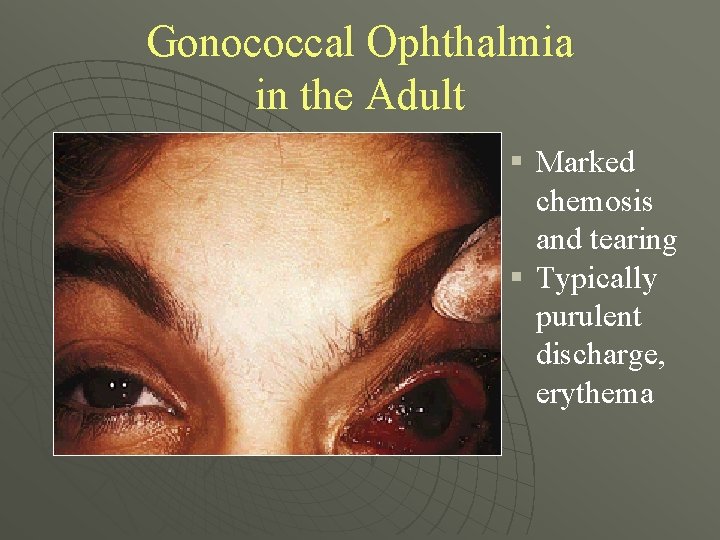
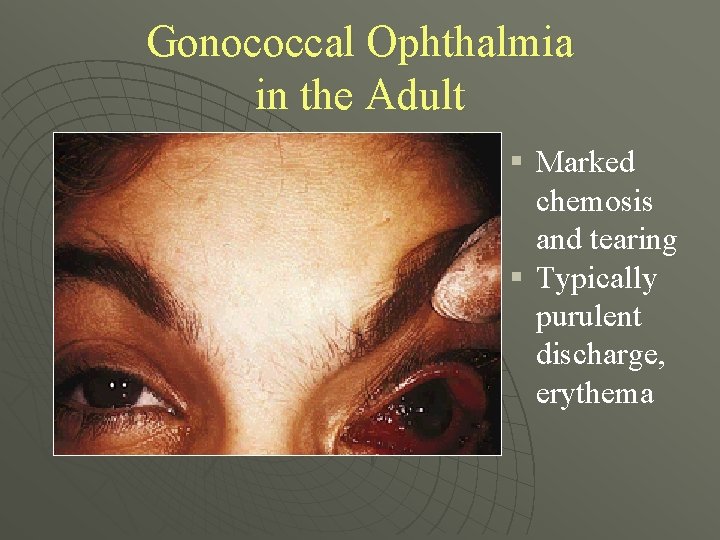
Gonococcal Ophthalmia in the Adult § Marked chemosis and tearing § Typically purulent discharge, erythema
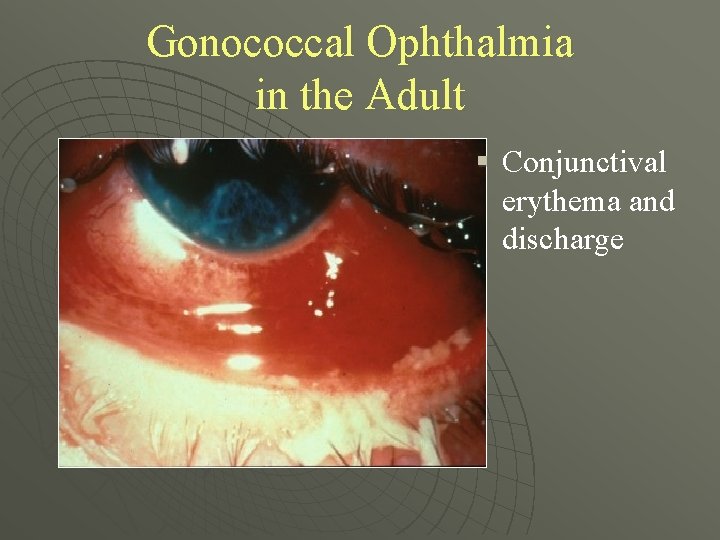
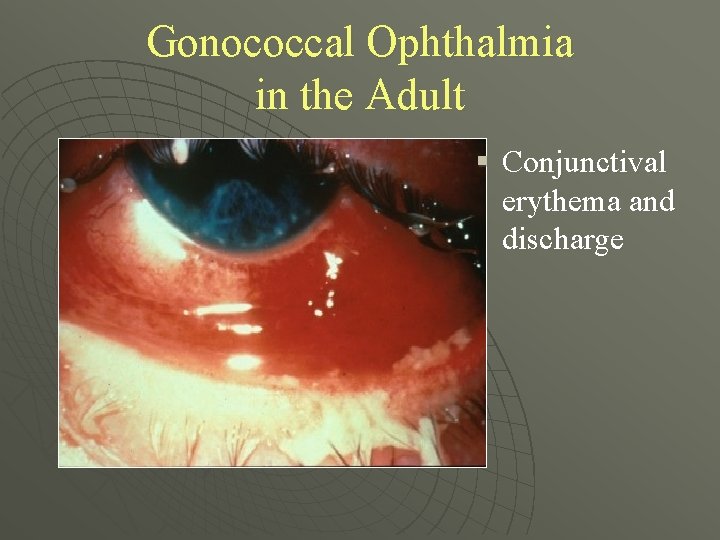
Gonococcal Ophthalmia in the Adult § Conjunctival erythema and discharge
Disseminated Gonococcal Infection Gonococcal bacteremia u Sources of infection include symptomatic and asymptomatic infections of pharynx, urethra, cervix u Occurs in < 5% of GC-infected patients u More common in females u
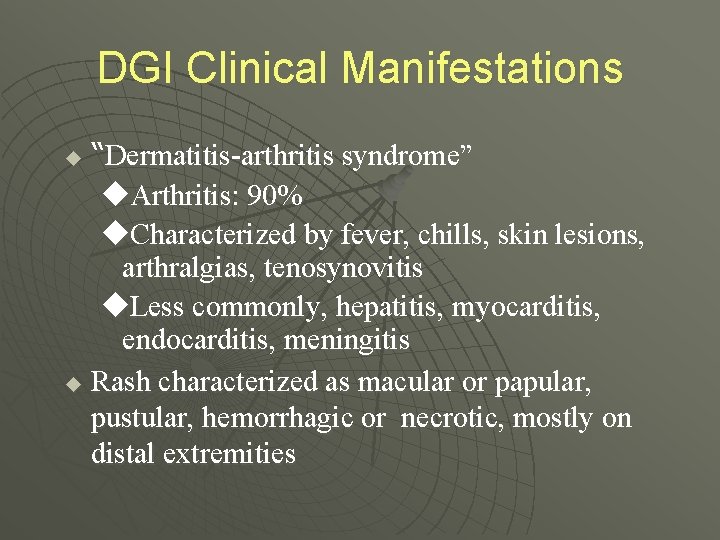
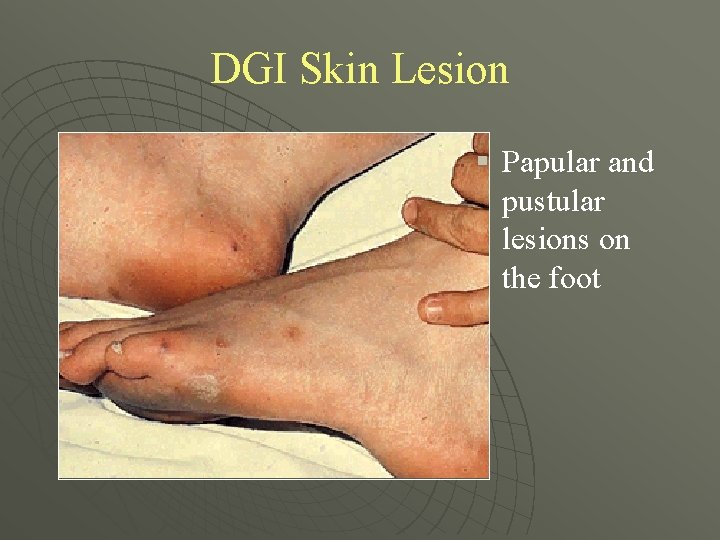
DGI Clinical Manifestations “Dermatitis-arthritis syndrome” u. Arthritis: 90% u. Characterized by fever, chills, skin lesions, arthralgias, tenosynovitis u. Less commonly, hepatitis, myocarditis, endocarditis, meningitis u Rash characterized as macular or papular, pustular, hemorrhagic or necrotic, mostly on distal extremities u

DGI Skin Lesion § Necrotic, grayish central lesion on erythematous base
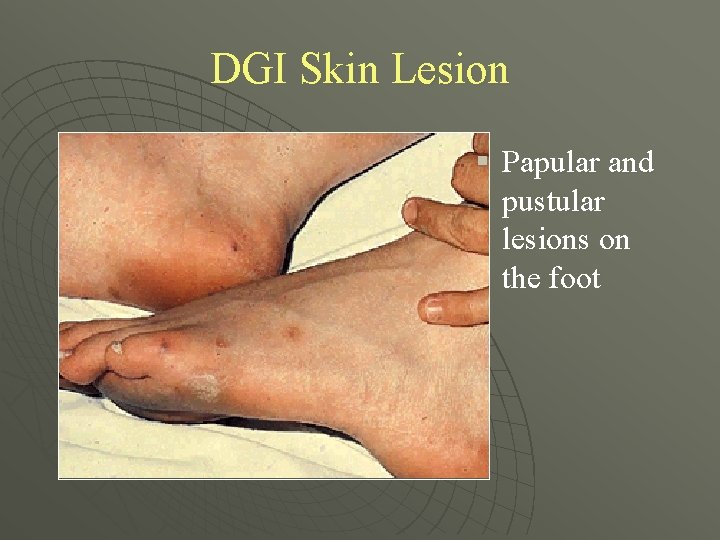
DGI Skin Lesion § Papular and pustular lesions on the foot

DGI Skin Lesion § Small painful midpalmar lesion on an erythematous base

DGI Skin Lesion § Pustular erythematous lesions
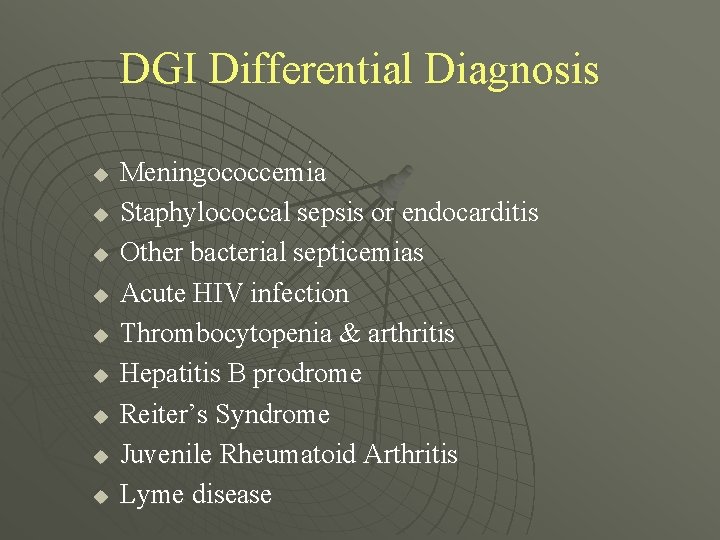
DGI Differential Diagnosis u u u u u Meningococcemia Staphylococcal sepsis or endocarditis Other bacterial septicemias Acute HIV infection Thrombocytopenia & arthritis Hepatitis B prodrome Reiter’s Syndrome Juvenile Rheumatoid Arthritis Lyme disease
Gonococcal Complications in Pregnancy Postpartum endometritis u Septic abortions u Post-abortal PID u Possible role in: § Gestational bleeding § Preterm labor and delivery § Premature rupture of membranes
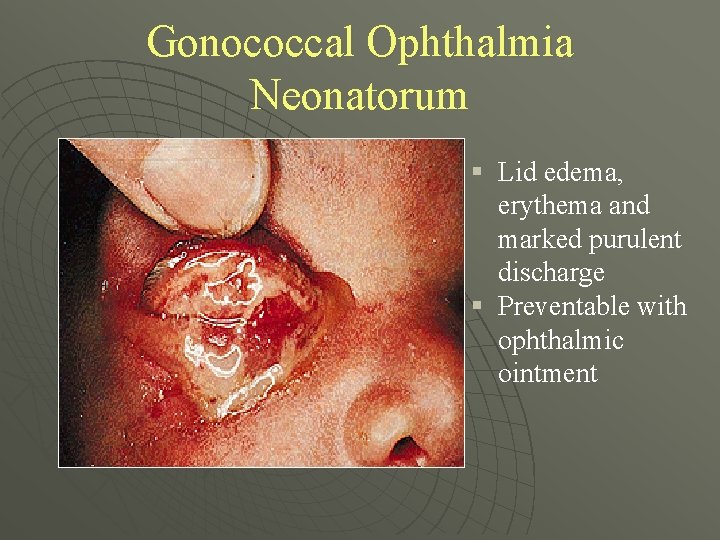
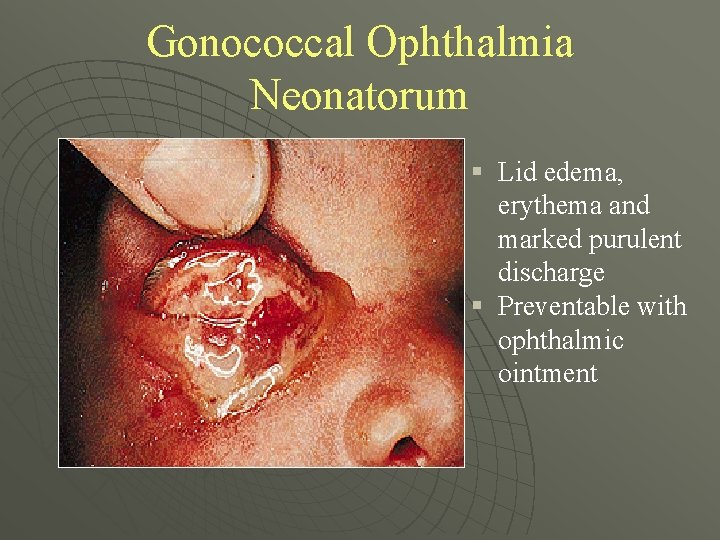
Gonococcal Ophthalmia Neonatorum § Lid edema, erythema and marked purulent discharge § Preventable with ophthalmic ointment
Diagnosis u u u A doctor or a nurse can obtain a sample from parts of the body likely to be infected, such as the cervix, urethra, rectum, or throat, and send it to a lab for analysis. Gonorrhea present in the cervix or urethra can be diagnosed through a urine sample. A Gram stain is a quick lab test that can be done in a clinic or doctor’s office. This test allows the doctor to see the gonorrhea bacterium under a microscope and can be done for men and women.
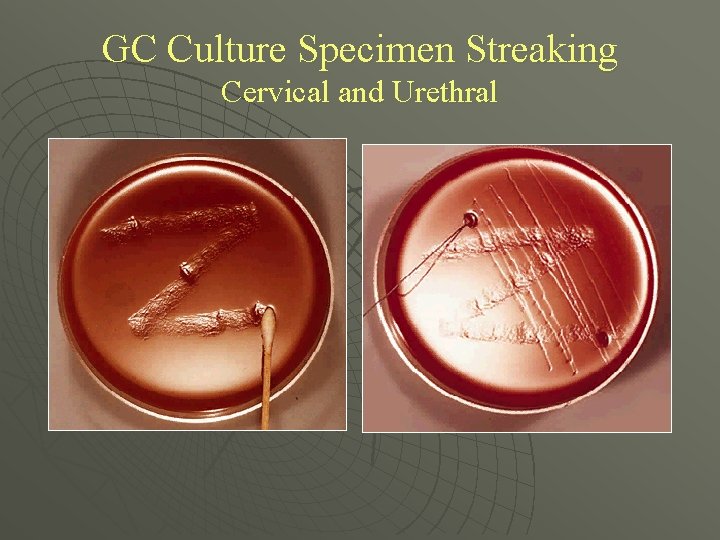
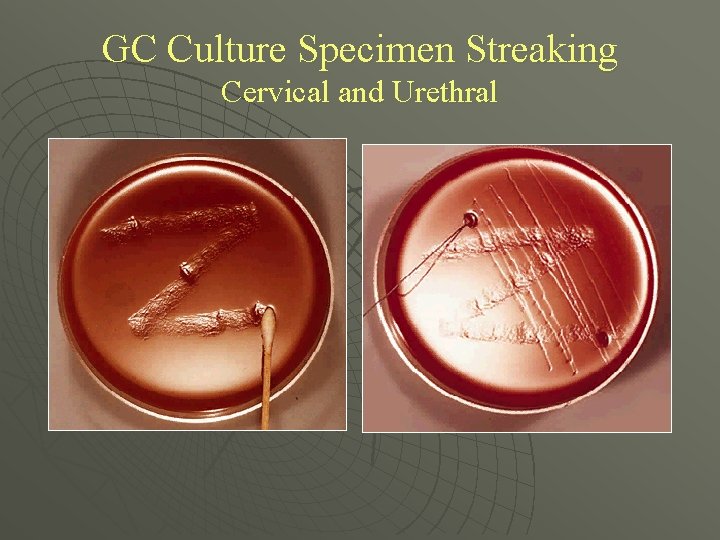
GC Culture Specimen Streaking Cervical and Urethral
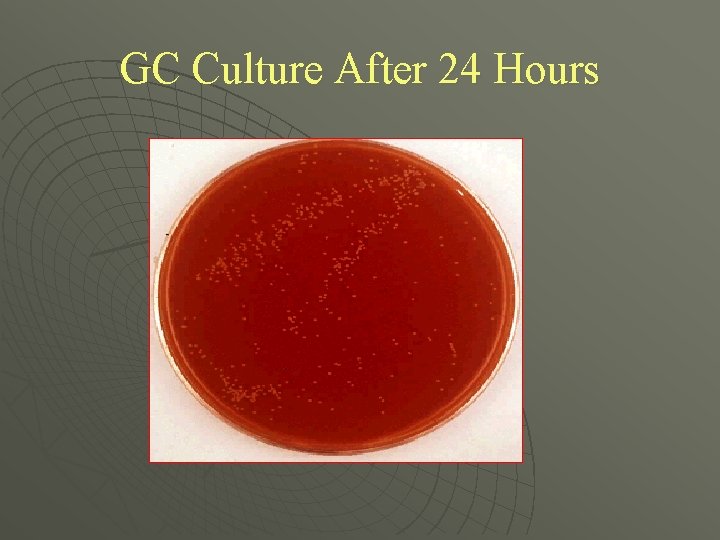
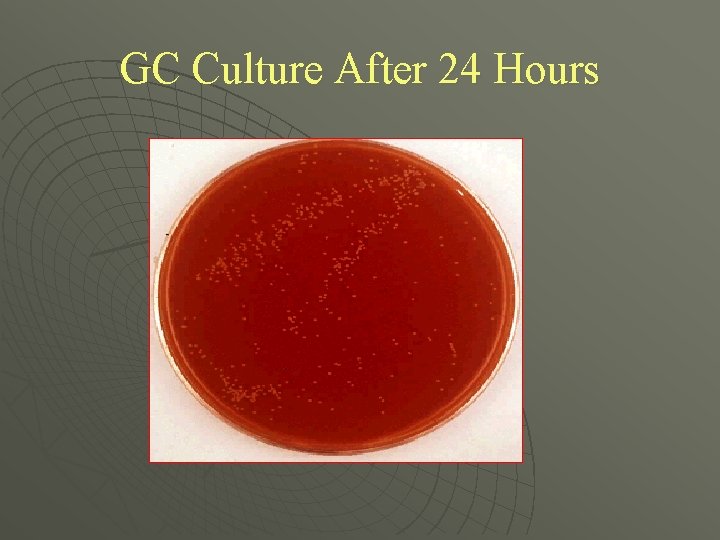
GC Culture After 24 Hours
Treatment u u v Several antibiotics can successfully cure gonorrhea However, drug-resistant strains of gonorrhea are increasing in many areas of the world, including the United States. Successful treatment is becoming more difficult. Because many people with gonorrhea also have Chlamydia, antibiotics for both infections are usually given together. In women, gonorrhea is a common cause of pelvic inflammatory disease (PID).
Chlamydia
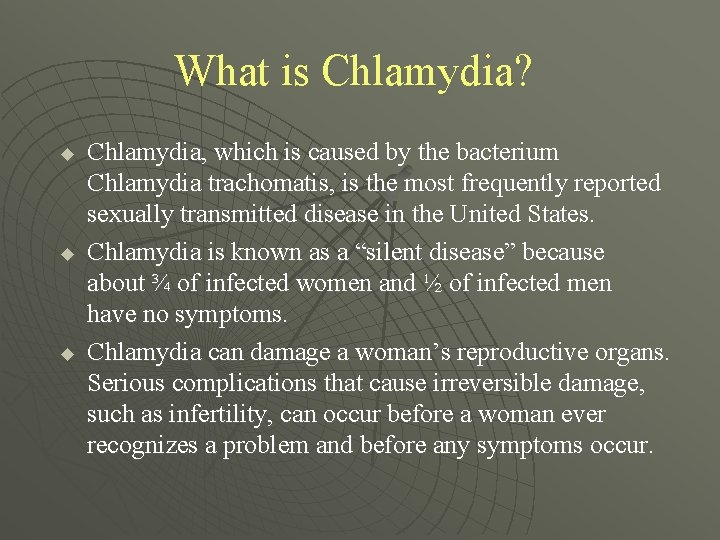
What is Chlamydia? u u u Chlamydia, which is caused by the bacterium Chlamydia trachomatis, is the most frequently reported sexually transmitted disease in the United States. Chlamydia is known as a “silent disease” because about ¾ of infected women and ½ of infected men have no symptoms. Chlamydia can damage a woman’s reproductive organs. Serious complications that cause irreversible damage, such as infertility, can occur before a woman ever recognizes a problem and before any symptoms occur.
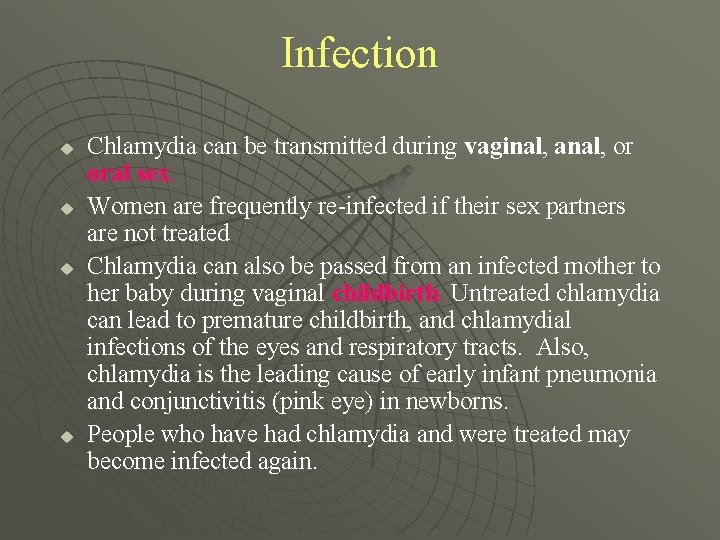
Infection u u Chlamydia can be transmitted during vaginal, anal, or oral sex. Women are frequently re-infected if their sex partners are not treated Chlamydia can also be passed from an infected mother to her baby during vaginal childbirth. Untreated chlamydia can lead to premature childbirth, and chlamydial infections of the eyes and respiratory tracts. Also, chlamydia is the leading cause of early infant pneumonia and conjunctivitis (pink eye) in newborns. People who have had chlamydia and were treated may become infected again.
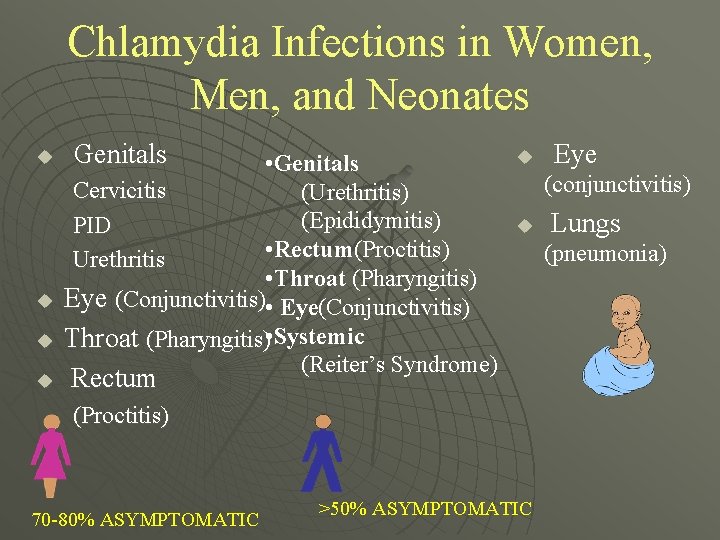
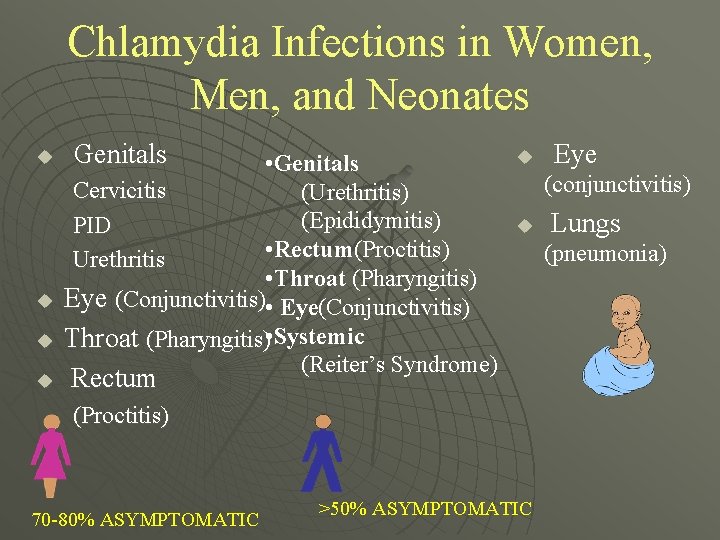
Chlamydia Infections in Women, Men, and Neonates u u Genitals • Genitals Cervicitis (Urethritis) (Epididymitis) PID • Rectum(Proctitis) Urethritis • Throat (Pharyngitis) Eye (Conjunctivitis) • Eye(Conjunctivitis) Throat (Pharyngitis) • Systemic (Reiter’s Syndrome) u (conjunctivitis) u Rectum (Proctitis) 70 -80% ASYMPTOMATIC Eye >50% ASYMPTOMATIC Lungs (pneumonia)
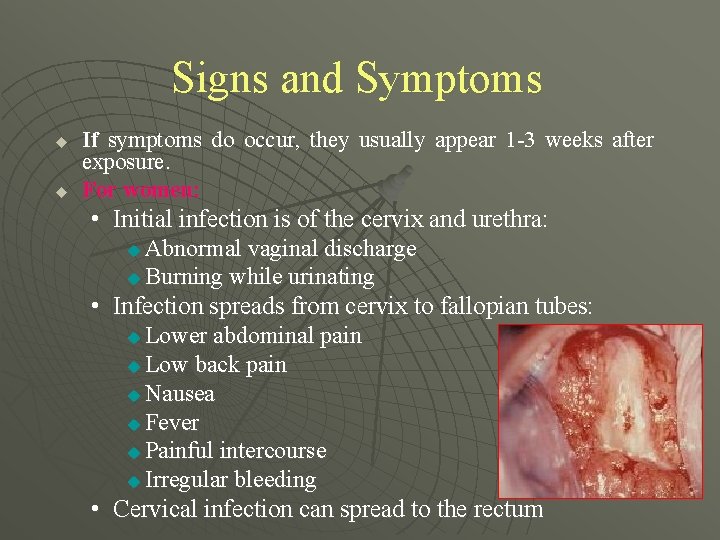
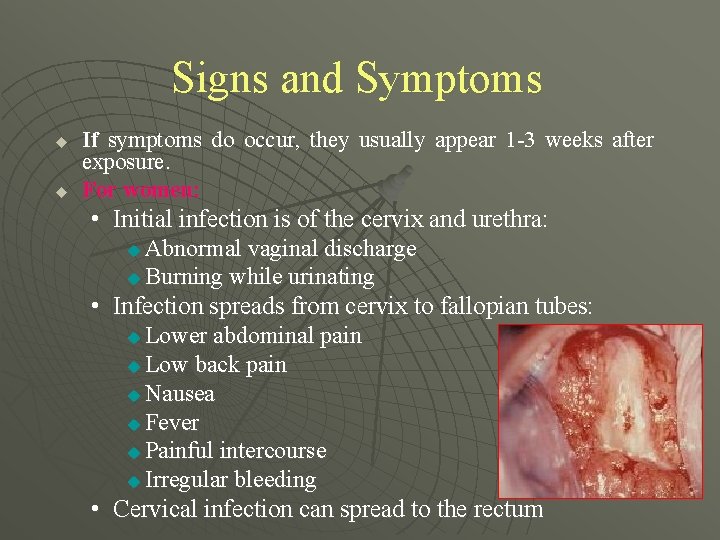
Signs and Symptoms u u If symptoms do occur, they usually appear 1 -3 weeks after exposure. For women: • Initial infection is of the cervix and urethra: Abnormal vaginal discharge u Burning while urinating • Infection spreads from cervix to fallopian tubes: u Lower abdominal pain u Low back pain u Nausea u Fever u Painful intercourse u Irregular bleeding • Cervical infection can spread to the rectum u

Signs and Symptoms u u u For men: • Discharge from penis • Burning while urinating • Burning and itching around opening of penis Rectal infection: • Rectal pain • Discharge • Bleeding Throat infections can also occur through oral sex
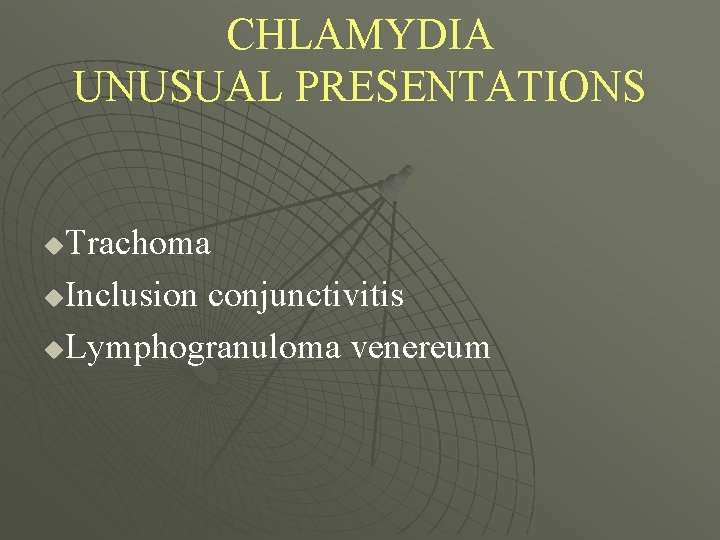
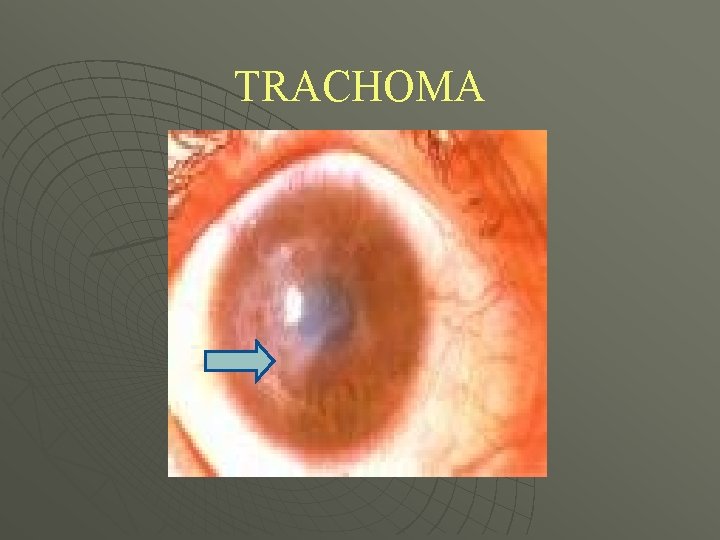
CHLAMYDIA UNUSUAL PRESENTATIONS Trachoma u. Inclusion conjunctivitis u. Lymphogranuloma venereum u
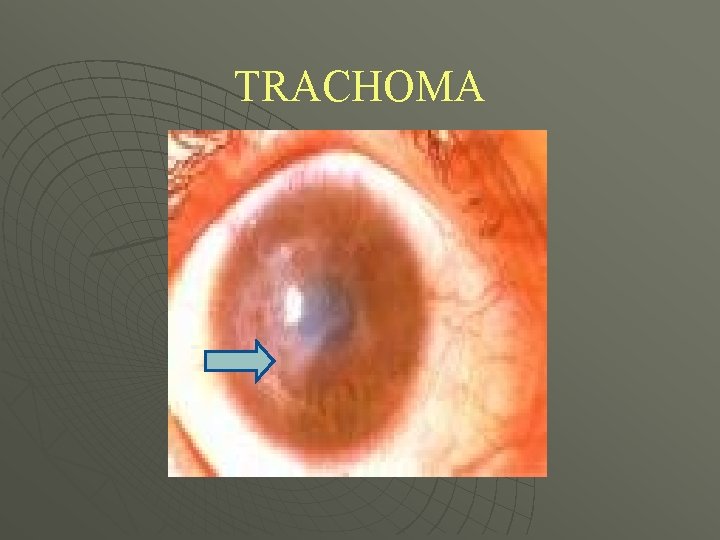
TRACHOMA

INCLUSION CONJUNCTIVITS
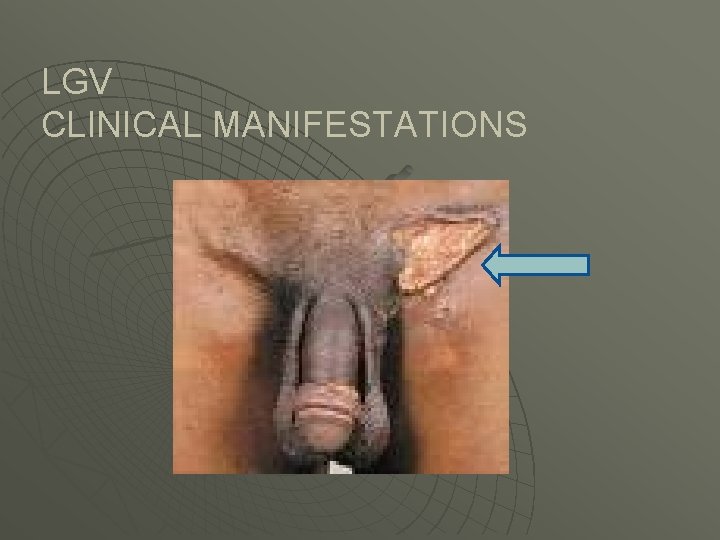
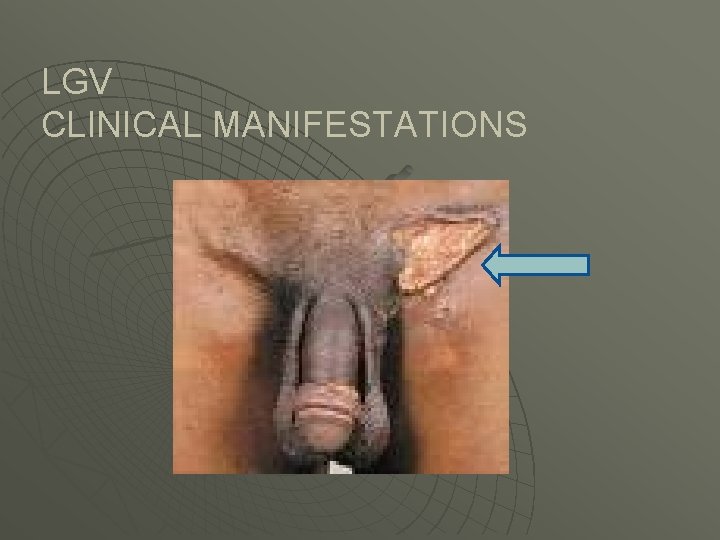
LGV CLINICAL MANIFESTATIONS
Diagnosis u Laboratory tests are done to diagnose chlamydia u Some are performed using a urine test u Other require a specimen from the penis or cervix

Complications
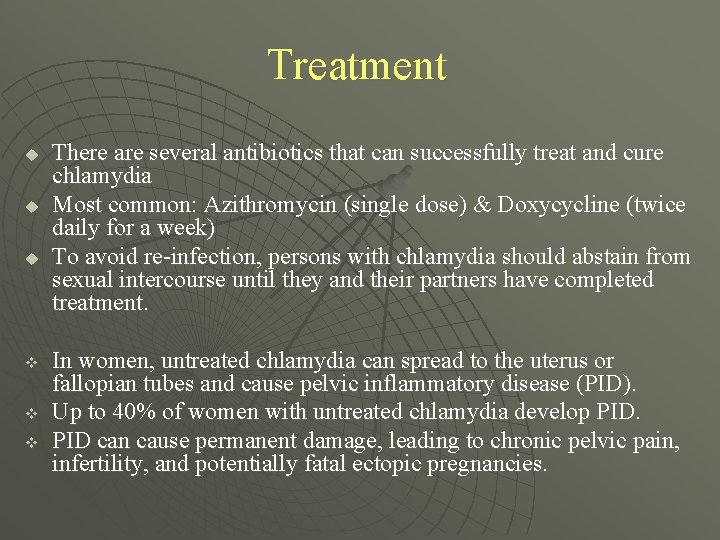
Treatment u u u v v v There are several antibiotics that can successfully treat and cure chlamydia Most common: Azithromycin (single dose) & Doxycycline (twice daily for a week) To avoid re-infection, persons with chlamydia should abstain from sexual intercourse until they and their partners have completed treatment. In women, untreated chlamydia can spread to the uterus or fallopian tubes and cause pelvic inflammatory disease (PID). Up to 40% of women with untreated chlamydia develop PID can cause permanent damage, leading to chronic pelvic pain, infertility, and potentially fatal ectopic pregnancies.
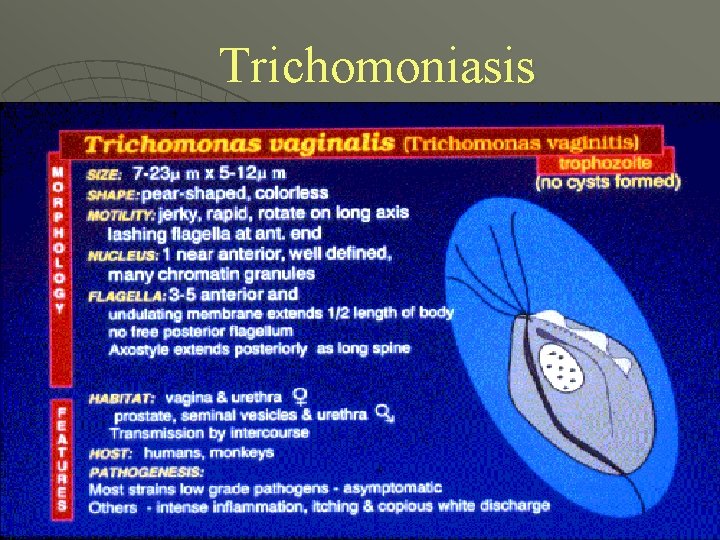
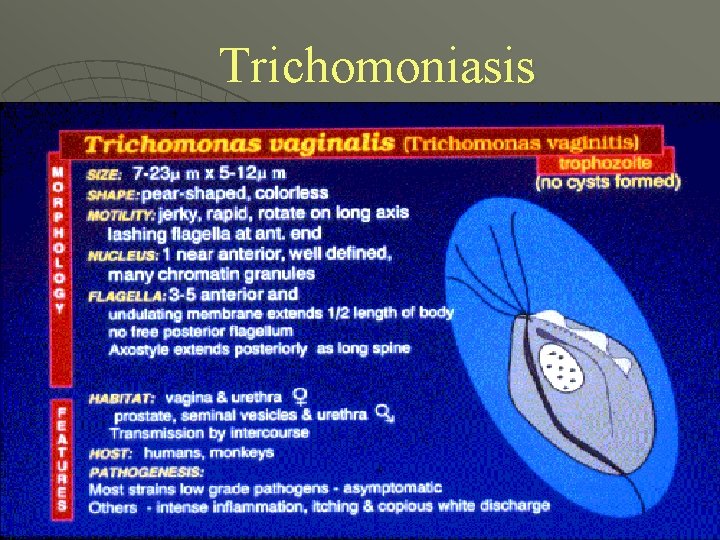
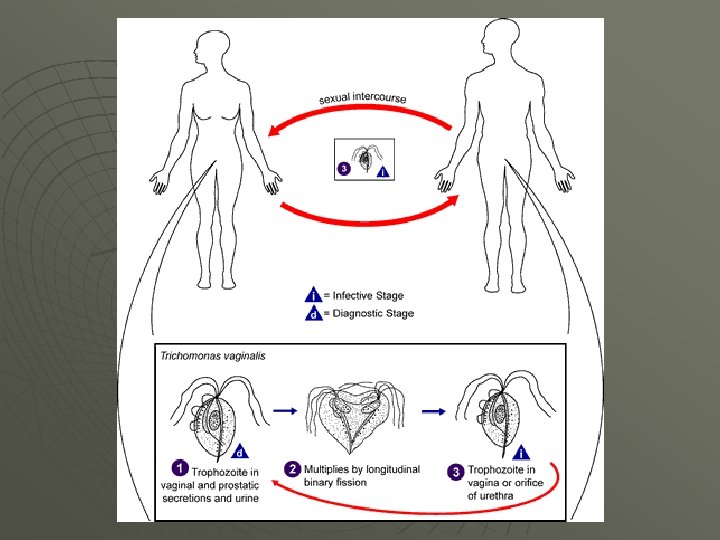
Trichomoniasis
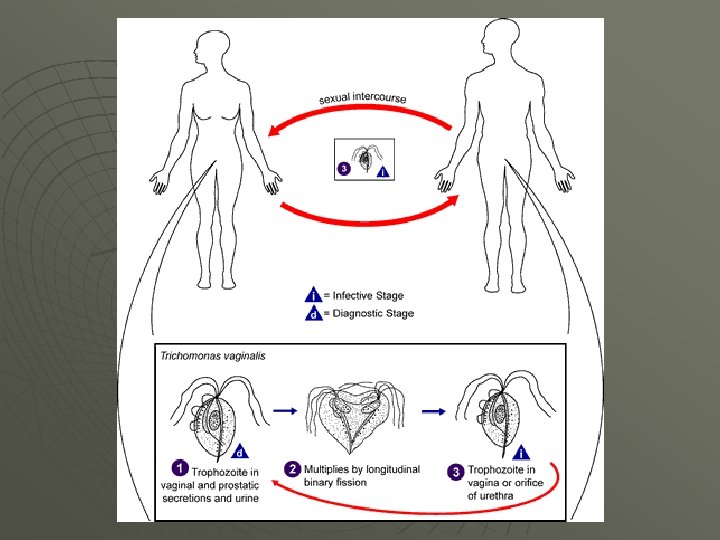

Symptoms u u Between 10% and 50% of women infected with T. Vaginalis are asymptomatic. Symptoms usually appear within 5 to 28 days of exposure. u Symptoms are nonspecific and cannot be used to differentiate trichomoniasis from other genital infections.
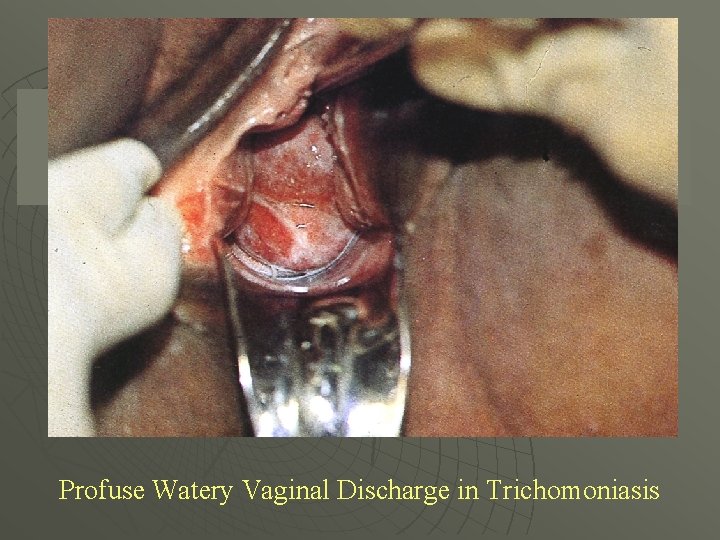
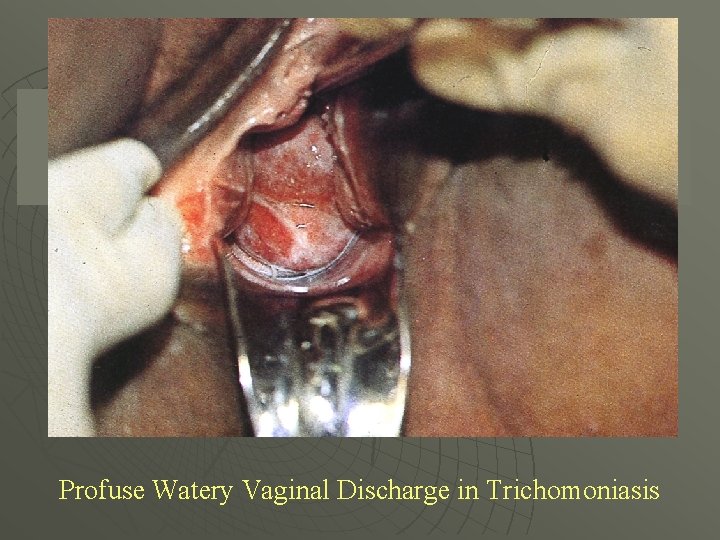
Profuse Watery Vaginal Discharge in Trichomoniasis
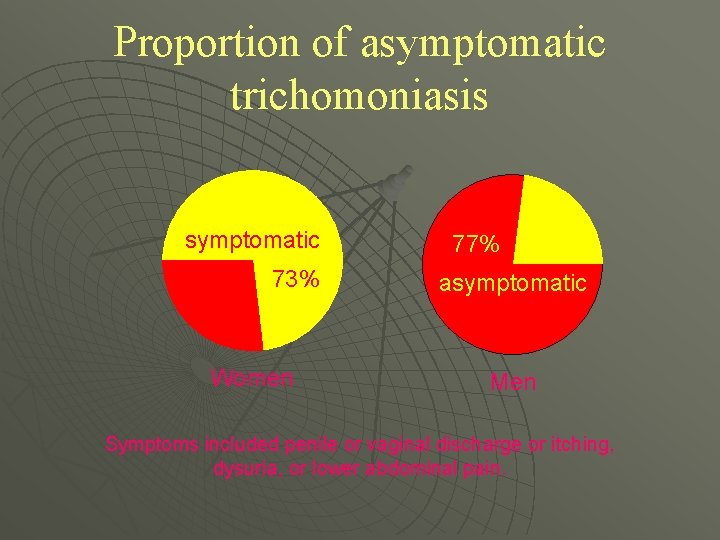
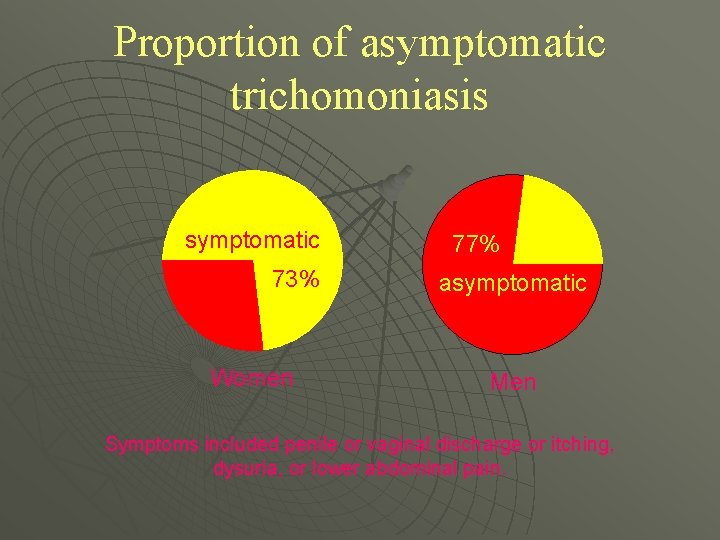
Proportion of asymptomatic trichomoniasis symptomatic 73% Women 77% asymptomatic Men Symptoms included penile or vaginal discharge or itching, dysuria, or lower abdominal pain.
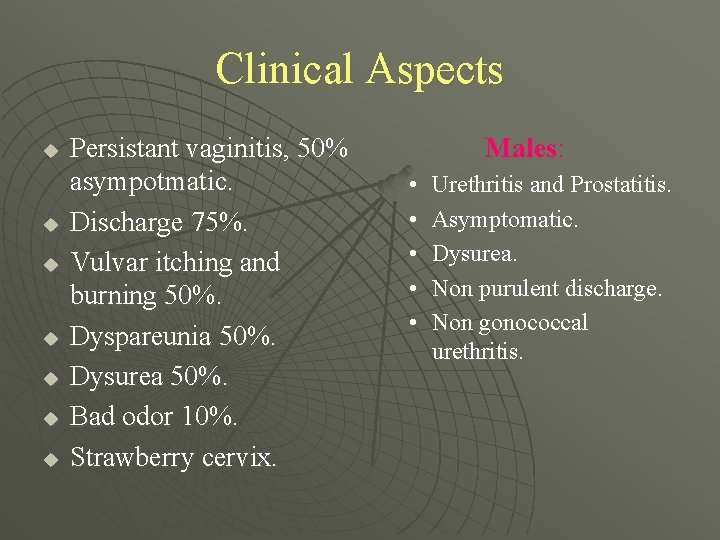
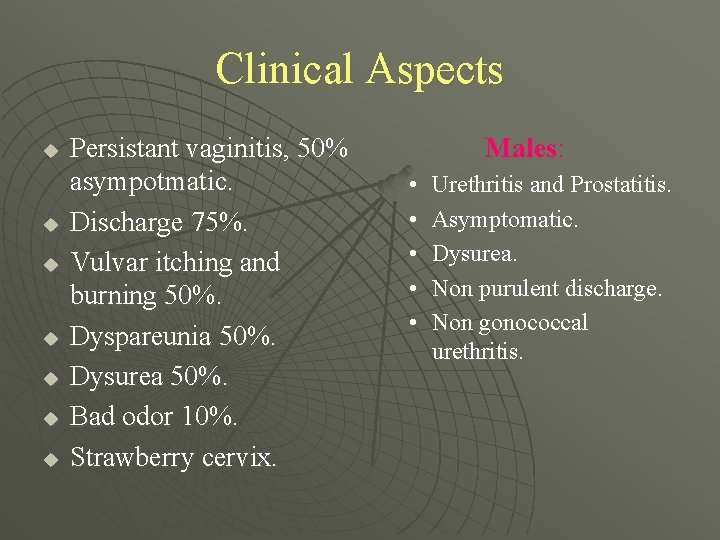
Clinical Aspects u u u u Persistant vaginitis, 50% asympotmatic. Discharge 75%. Vulvar itching and burning 50%. Dyspareunia 50%. Dysurea 50%. Bad odor 10%. Strawberry cervix. Males: • • • Urethritis and Prostatitis. Asymptomatic. Dysurea. Non purulent discharge. Non gonococcal urethritis.

Diagnosis Clinical picture. u Microscopic morphology (wet mount) u Male vs female. u Antigen detection. u Look for other venereal diseases. u

Wet mount microscopy u u Performed on vaginal swab specimens (or male urine sediment) resuspended in a drop or 2 of saline Organisms must be viable and motile Must be performed within 15 minutes of specimen collection 50 - 70% sensitivity with expert microscopist
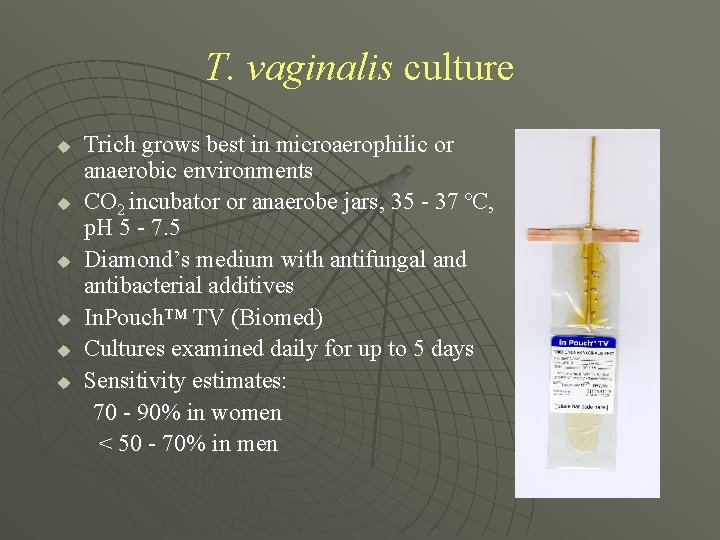
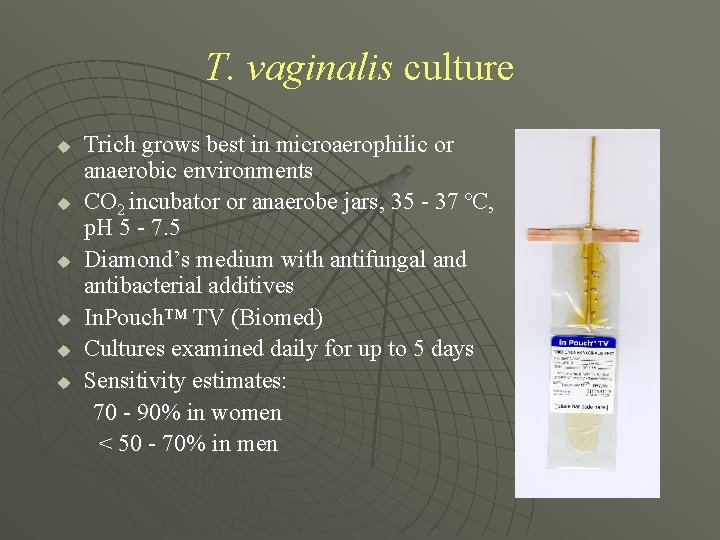
T. vaginalis culture u u u Trich grows best in microaerophilic or anaerobic environments CO 2 incubator or anaerobe jars, 35 - 37 ºC, p. H 5 - 7. 5 Diamond’s medium with antifungal and antibacterial additives In. Pouch™ TV (Biomed) Cultures examined daily for up to 5 days Sensitivity estimates: 70 - 90% in women < 50 - 70% in men
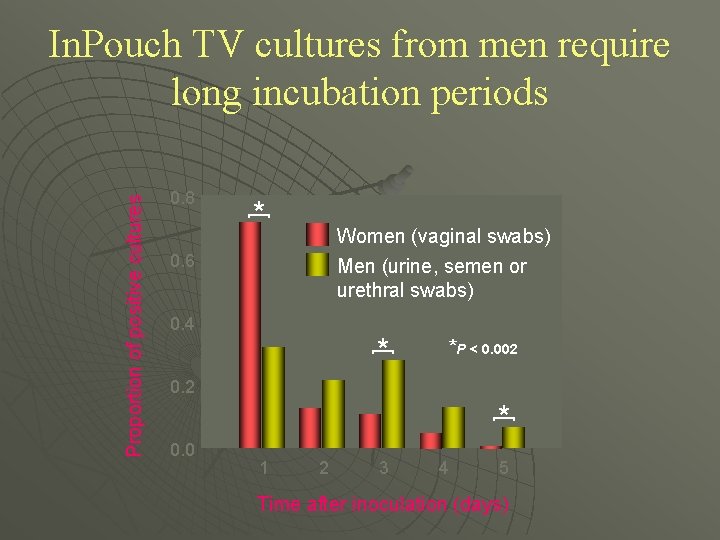
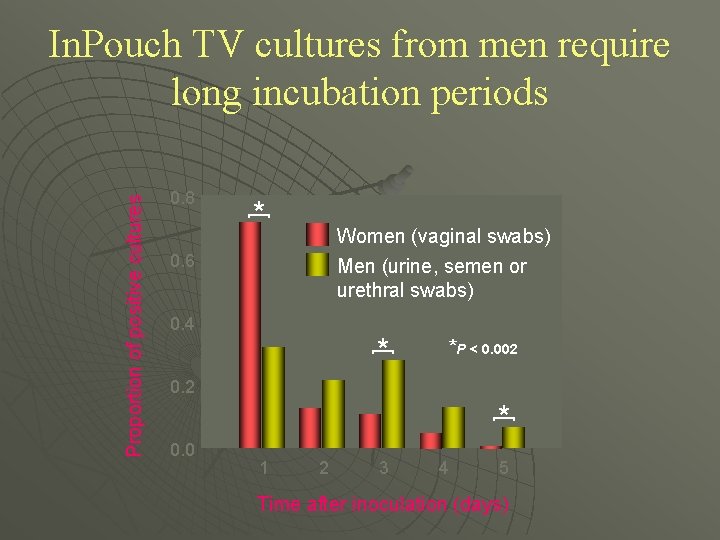
0. 8 * [ Women (vaginal swabs) Men (urine, semen or urethral swabs) 0. 6 0. 4 * [ * P < 0. 002 0. 2 * [ Proportion of positive cultures In. Pouch TV cultures from men require long incubation periods 0. 0 1 2 3 4 5 Time after inoculation (days)
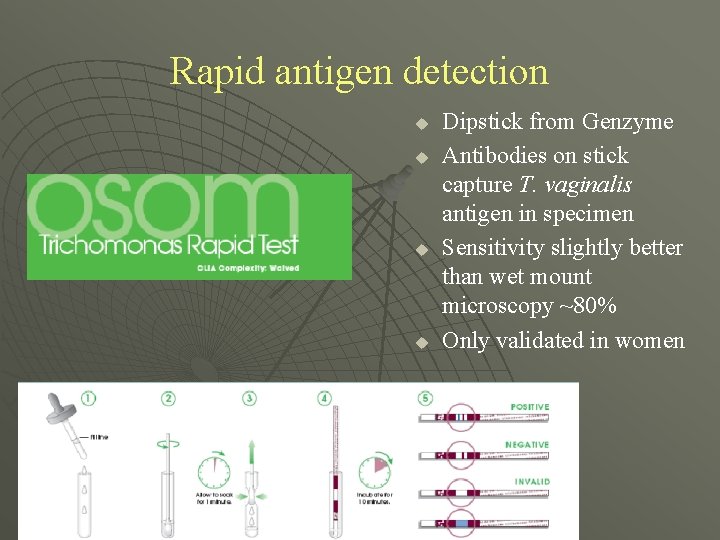
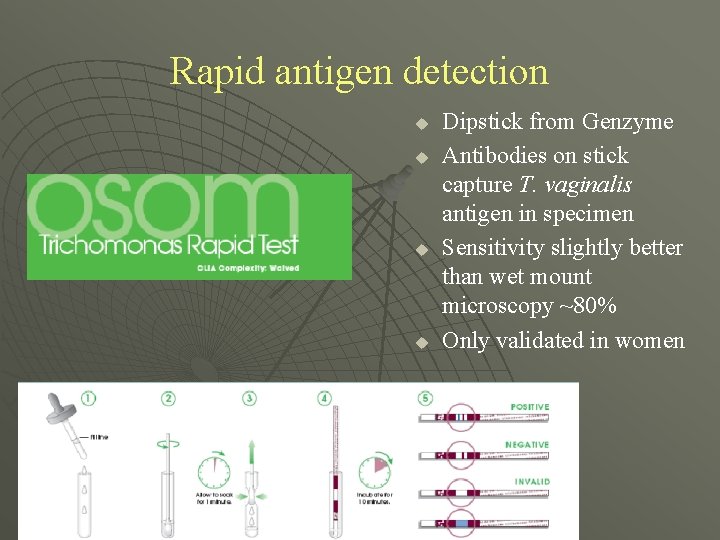
Rapid antigen detection u u Dipstick from Genzyme Antibodies on stick capture T. vaginalis antigen in specimen Sensitivity slightly better than wet mount microscopy ~80% Only validated in women
Treatment of Trichomoniasis • Metronidazole 2 gm orally once • Metronidazole 500 mg orally twice daily x 7 days • Metrogel NOT recommended; < 50% efficacious than oral regimens

Tinidazole u u u Tinidazole 2 gm orally once also recommended regimen Clinical trials found cure rates between 86 -100% in women, 83% in men. Compared to metronidazole, tinidazole has: • Higher clinical and microbiological cure rates • Less frequent side effects

Treatment during Pregnancy and Lactation u u Pregnancy • Metronidazole 2 gm orally once • Tinidazole safety NOT well evaluated (category C) Breast-feeding • Metronidazole - withhold breastfeeding during treatment and for 12 -24 hours after last dose • Tinidazole – withhold breastfeeding during treatment and for 3 days after last dose
! ! ! U O Y K N A TH “Nature did not have rewards and punishments. Only consequences are present. . .
 Mycotic infection rabbit
Mycotic infection rabbit Chlamidiosis
Chlamidiosis Can gonorrhea kill you
Can gonorrhea kill you Gonorrhea ophthalmia neonatorum
Gonorrhea ophthalmia neonatorum Boutonniere nodes
Boutonniere nodes Gonorrhea
Gonorrhea Chlamydia curable
Chlamydia curable Pictures of body lice and scabies
Pictures of body lice and scabies Gonorrhea
Gonorrhea Diplococcus gram negatif
Diplococcus gram negatif Epididymitis
Epididymitis Gonorrhea
Gonorrhea Gonorrhea
Gonorrhea Venereal granuloma
Venereal granuloma Trichomoniasis sores
Trichomoniasis sores The odds and ends kingdom
The odds and ends kingdom Trichomoniasis meaning
Trichomoniasis meaning Atrophic vaginitis
Atrophic vaginitis Trichomoniasis pictures
Trichomoniasis pictures Trichomoniasis pictures
Trichomoniasis pictures Orgasm disorder
Orgasm disorder Pid discharge pictures
Pid discharge pictures Trichomoniasis pictures
Trichomoniasis pictures Trichomoniasis treatment
Trichomoniasis treatment Trichomoniasis
Trichomoniasis The neurotic need for affection and approval
The neurotic need for affection and approval Verbal affection
Verbal affection Zone of affection
Zone of affection Strong affection
Strong affection Head strokes physical affection
Head strokes physical affection For a moment the last sunshine fell
For a moment the last sunshine fell Happy farmer candy bar
Happy farmer candy bar Set your affection on things above meaning
Set your affection on things above meaning Round flotation device candy
Round flotation device candy Psychology a journey
Psychology a journey Sample of lacreous affection
Sample of lacreous affection Schéma de wood
Schéma de wood Red blue yellow green orange pink purple
Red blue yellow green orange pink purple Willaim blake
Willaim blake Romeo and juliet vs west side story
Romeo and juliet vs west side story Younger shorter older old
Younger shorter older old How to write centavos
How to write centavos Red orange yellow green blue indigo violet pink
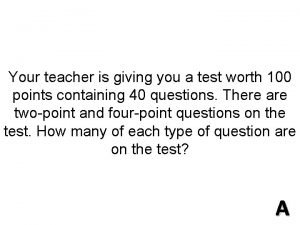
Red orange yellow green blue indigo violet pink Gabby and sydney bought some pens and pencils
Gabby and sydney bought some pens and pencils Young and dyslexic
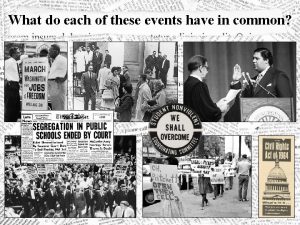
Young and dyslexic Us prior to brown map key
Us prior to brown map key West yorkshire health and care partnership
West yorkshire health and care partnership Whats a transverse wave
Whats a transverse wave Spring tide position
Spring tide position How to identify dependent and independent variable
How to identify dependent and independent variable Transitive intransitive and linking verbs
Transitive intransitive and linking verbs What are different life roles
What are different life roles Types of records and reports in nursing
Types of records and reports in nursing Prohibited route in transportation problem means
Prohibited route in transportation problem means Compare and contrast cold wave and wind chill factor
Compare and contrast cold wave and wind chill factor Vertical format of trading account
Vertical format of trading account Siop and tap have similar descriptors and indicators
Siop and tap have similar descriptors and indicators Tomorrow creeps in this petty pace
Tomorrow creeps in this petty pace Ritz carlton motto
Ritz carlton motto