Cows Milk Protein Allergy CMPA Road to Management


- Slides: 66
Cows Milk Protein Allergy (CMPA) Road to Management 1

Dedication JNMC SGPGIMS Late Dr S K BHATNAGAR
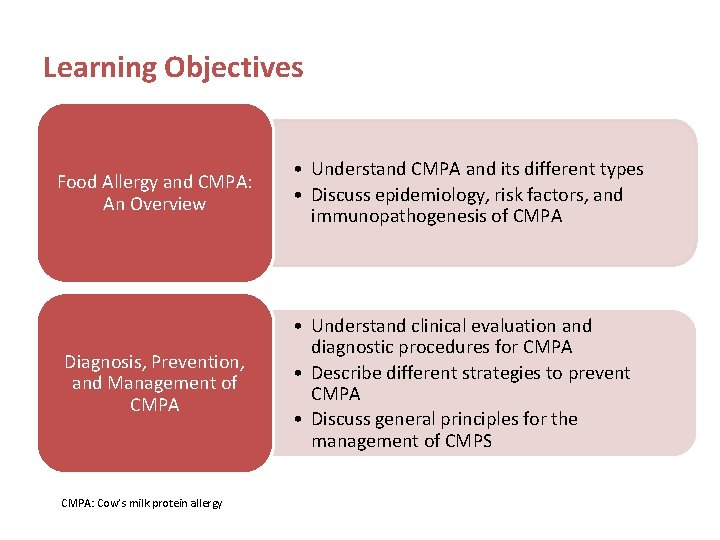
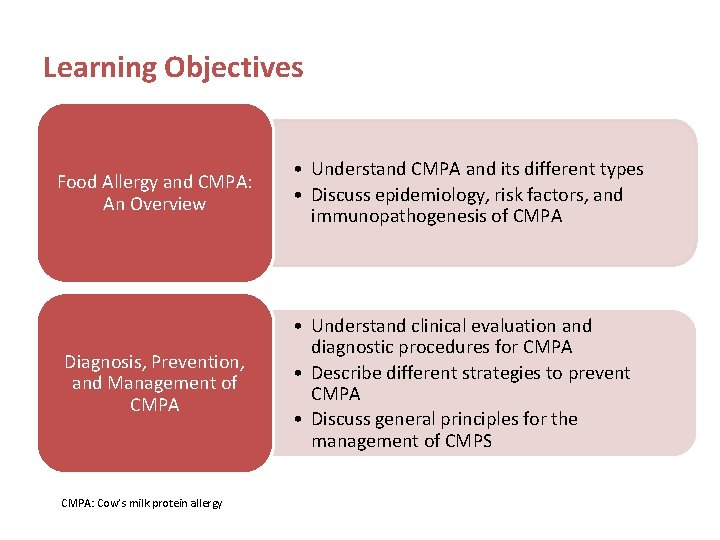
Learning Objectives Food Allergy and CMPA: An Overview Diagnosis, Prevention, and Management of CMPA: Cow’s milk protein allergy • Understand CMPA and its different types • Discuss epidemiology, risk factors, and immunopathogenesis of CMPA • Understand clinical evaluation and diagnostic procedures for CMPA • Describe different strategies to prevent CMPA • Discuss general principles for the management of CMPS
Case presentation I
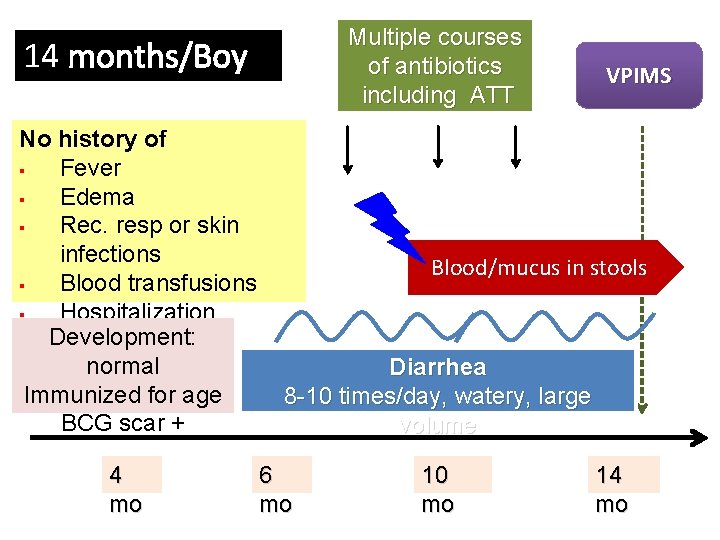
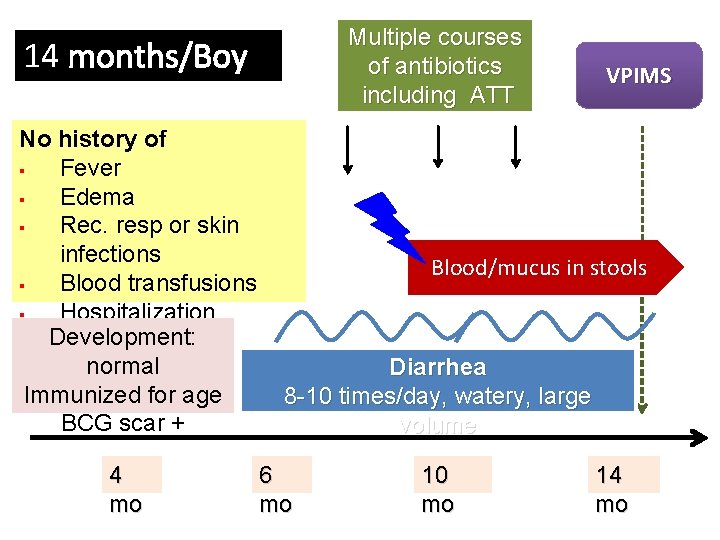
Multiple courses of antibiotics including ATT 14 months/Boy No history of § Fever § Edema § Rec. resp or skin infections § Blood transfusions § Hospitalization Development: normal Immunized for age BCG scar + 4 mo VPIMS Blood/mucus in stools Diarrhea 8 -10 times/day, watery, large volume 6 mo 10 mo 14 mo
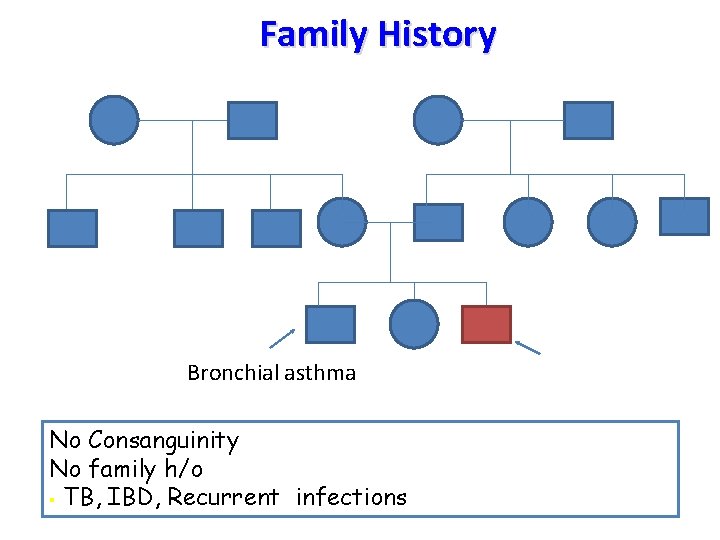
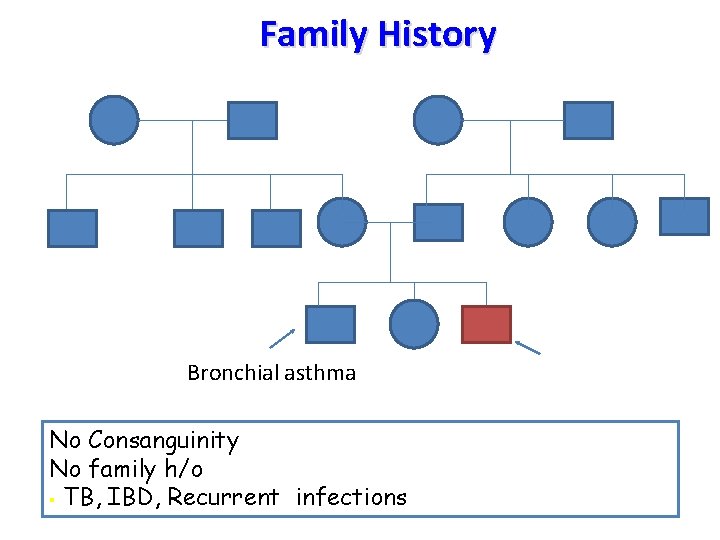
Family History Bronchial asthma No Consanguinity No family h/o § TB, IBD, Recurrent infections
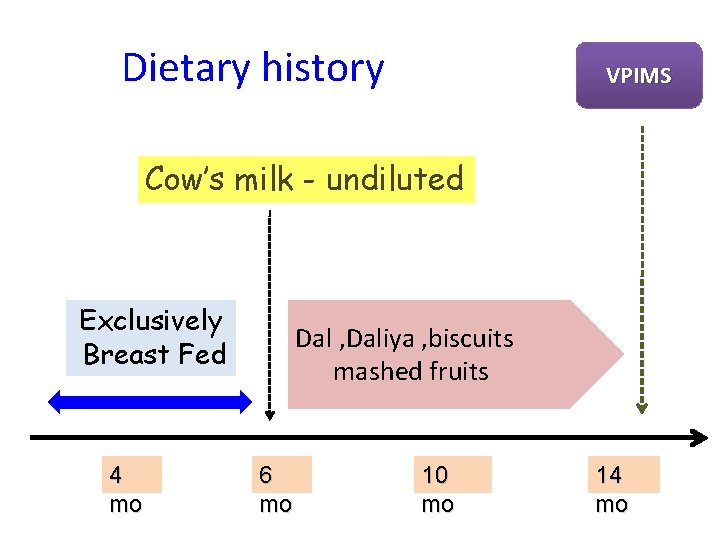
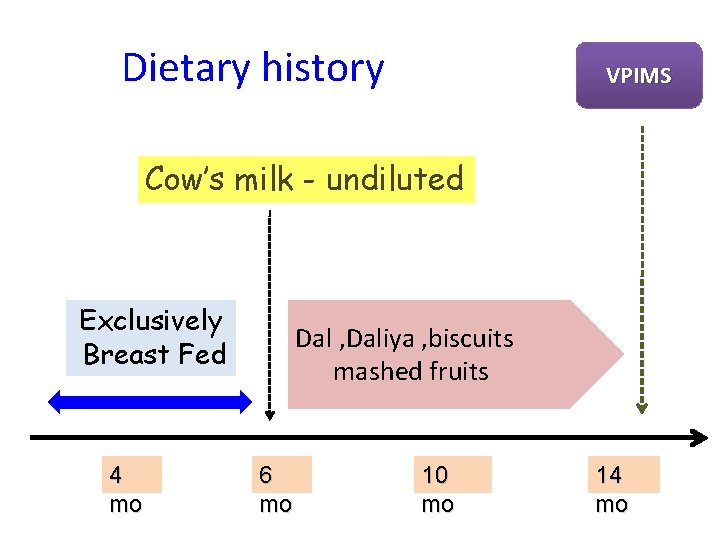
Dietary history VPIMS Cow’s milk - undiluted Exclusively Breast Fed 4 mo Dal , Daliya , biscuits mashed fruits 6 mo 10 mo 14 mo
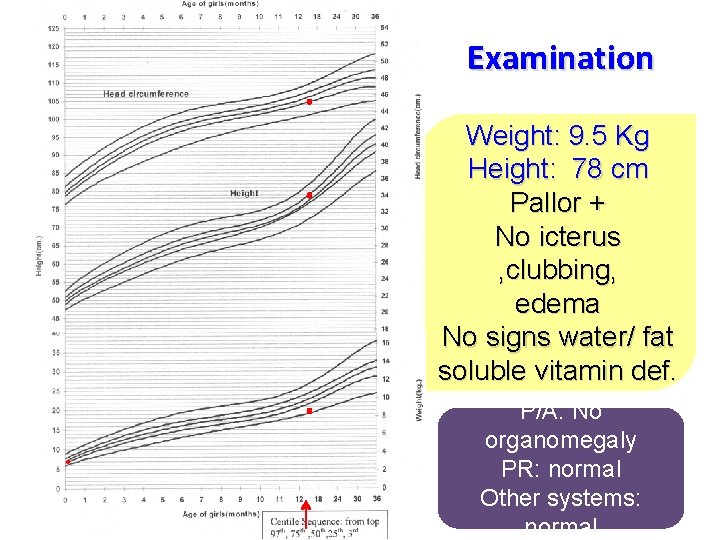
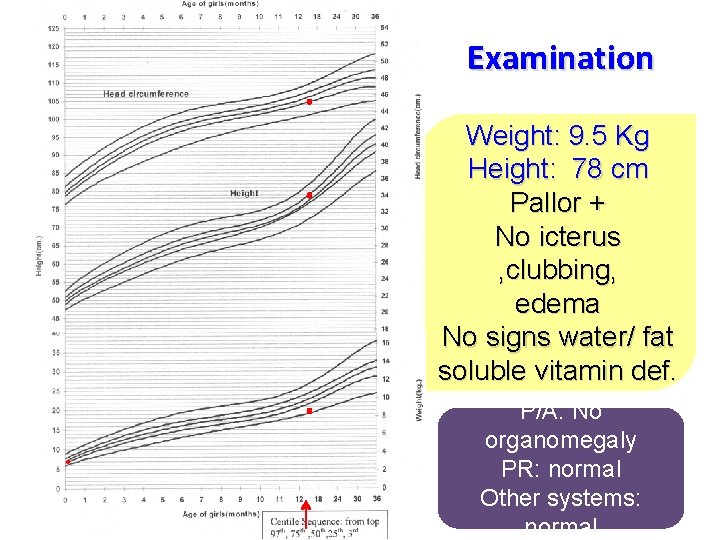
Examination Weight: 9. 5 Kg Height: 78 cm Pallor + No icterus , clubbing, edema No signs water/ fat soluble vitamin def. P/A: No organomegaly PR: normal Other systems: normal
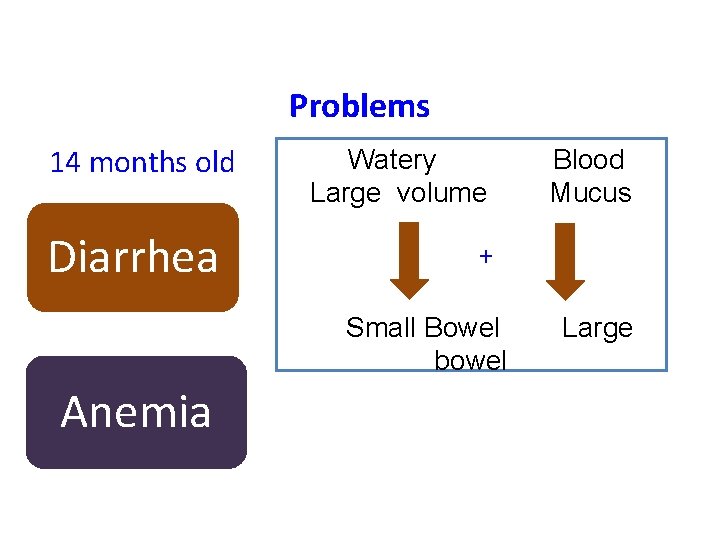
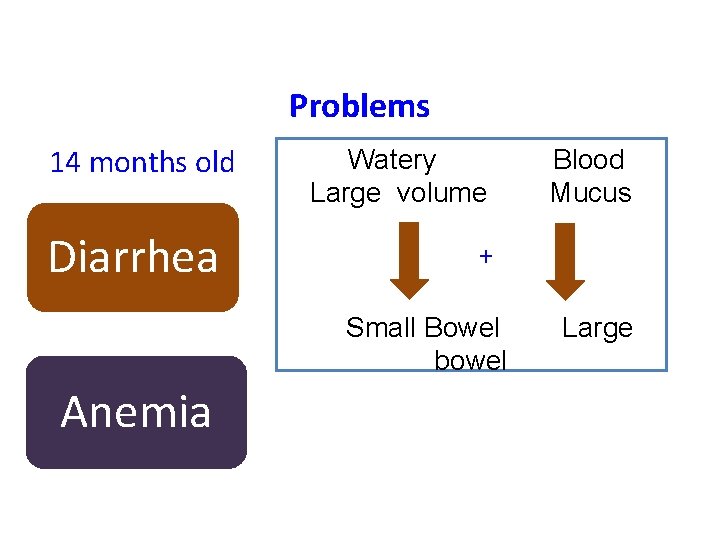
Problems 14 months old Diarrhea Watery Large volume + Small Bowel bowel Anemia Blood Mucus Large
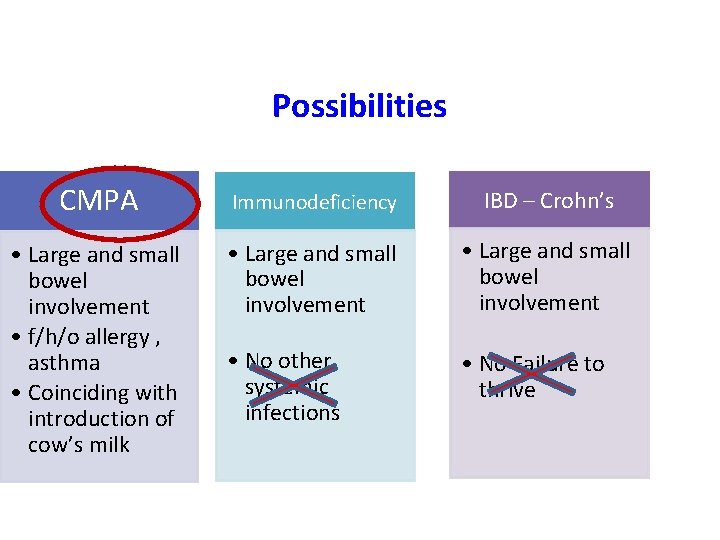
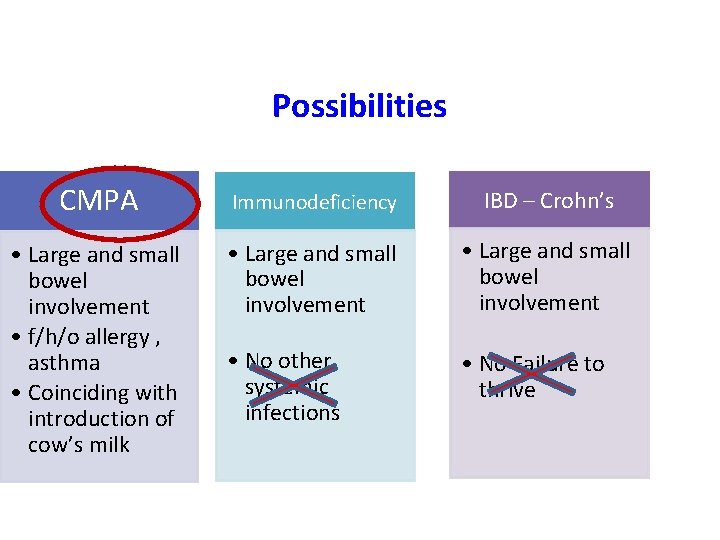
Possibilities CMPA Immunodeficiency IBD – Crohn’s • Large and small bowel involvement • f/h/o allergy , asthma • Coinciding with introduction of cow’s milk • Large and small bowel involvement • No other systemic infections • No Failure to thrive
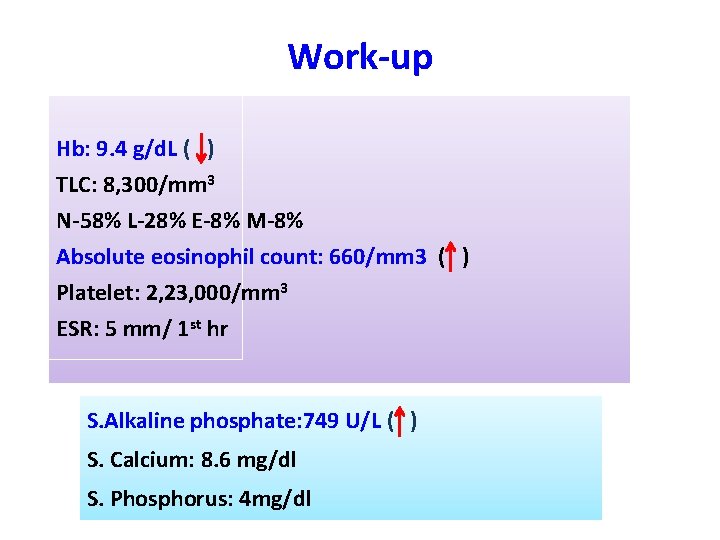
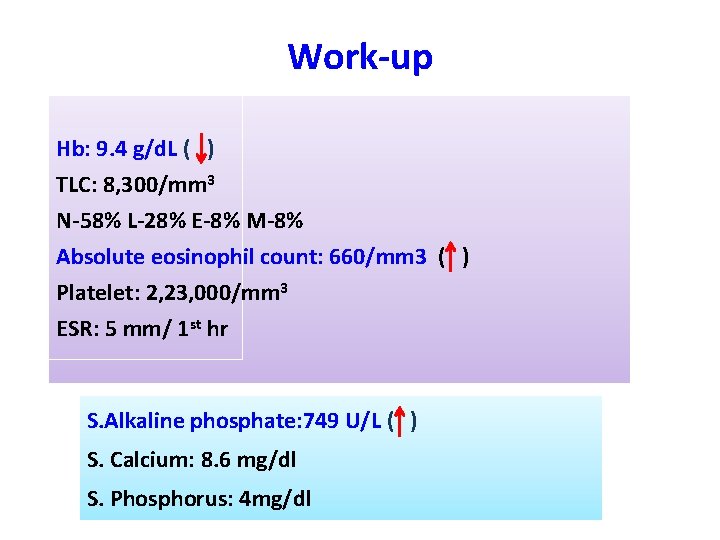
Work-up Hb: 9. 4 g/d. L ( ) TLC: 8, 300/mm 3 N-58% L-28% E-8% M-8% Absolute eosinophil count: 660/mm 3 ( ) Platelet: 2, 23, 000/mm 3 ESR: 5 mm/ 1 st hr S. Alkaline phosphate: 749 U/L ( ) S. Calcium: 8. 6 mg/dl S. Phosphorus: 4 mg/dl
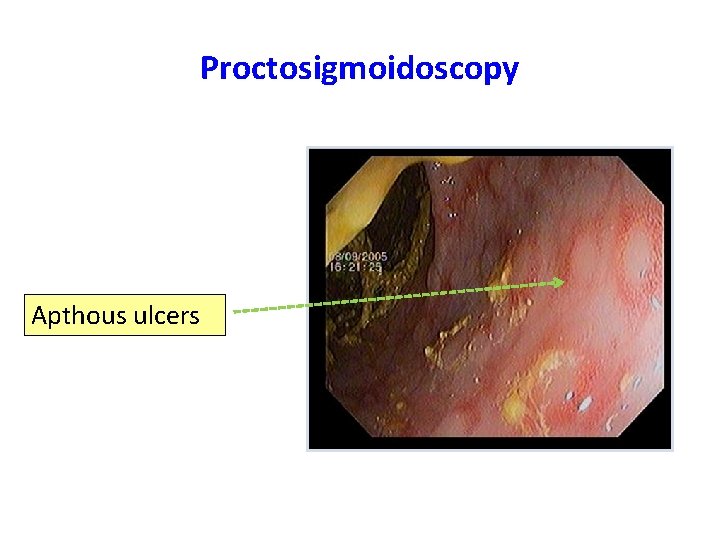
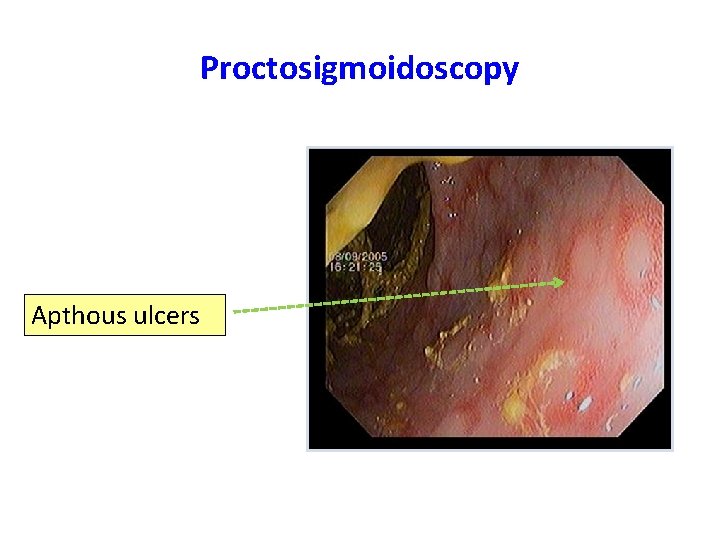
Proctosigmoidoscopy Apthous ulcers
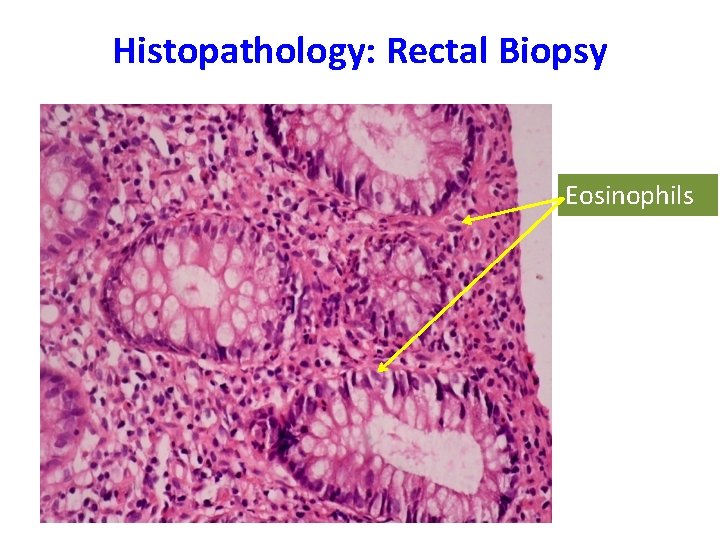
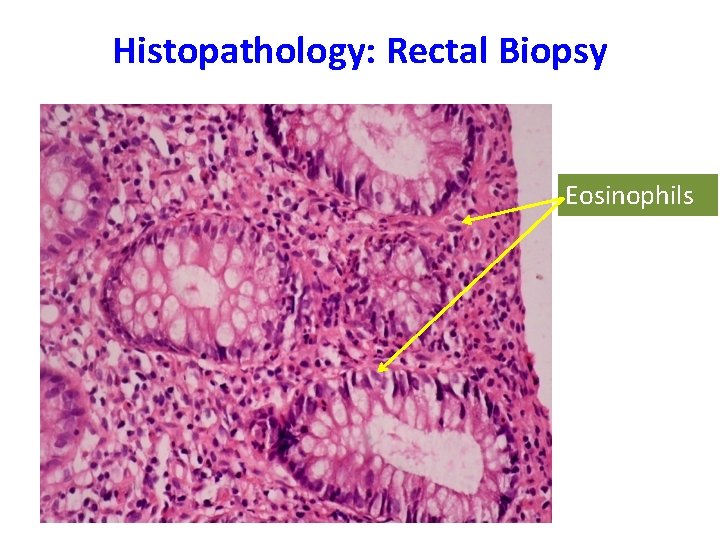
Histopathology: Rectal Biopsy Eosinophils
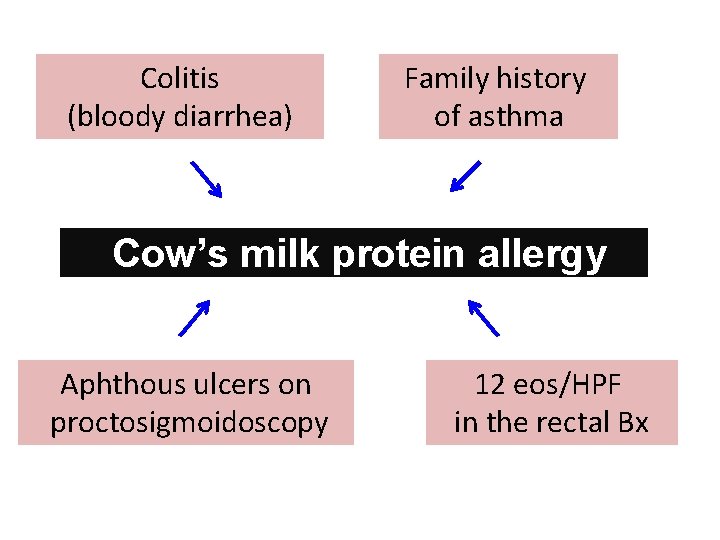
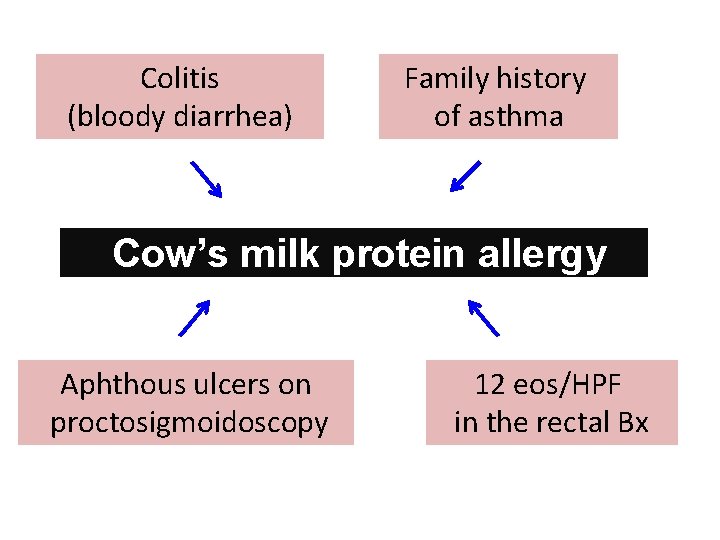
Colitis (bloody diarrhea) Family history of asthma Cow’s milk protein allergy Aphthous ulcers on proctosigmoidoscopy 12 eos/HPF in the rectal Bx
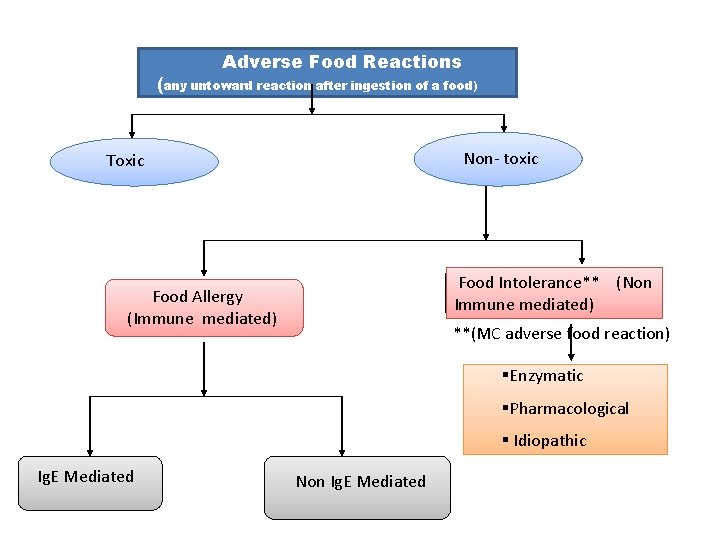
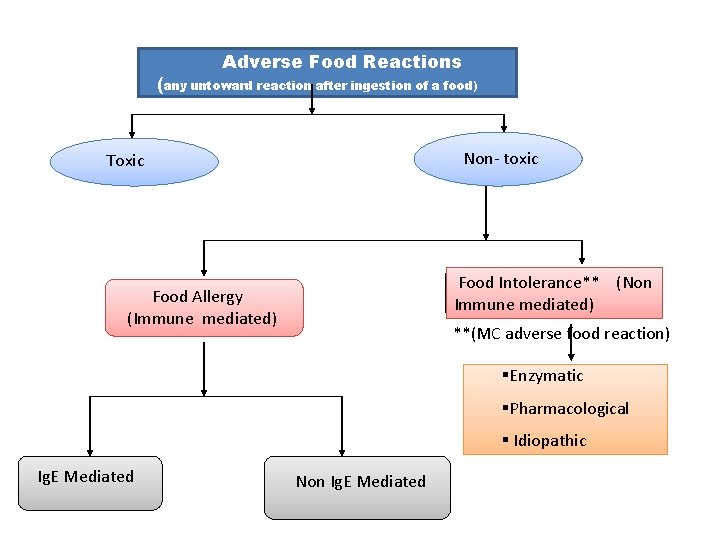
Adverse Food Reactions (any untoward reaction after ingestion of a food) Non- toxic Toxic Food Allergy (Immune mediated) Food Intolerance** (Non Immune mediated) **(MC adverse food reaction) §Enzymatic §Pharmacological § Idiopathic Ig. E Mediated Non Ig. E Mediated
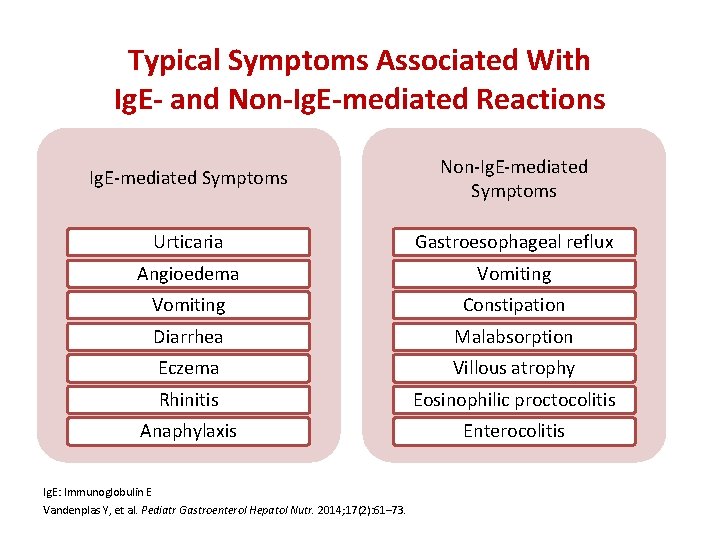
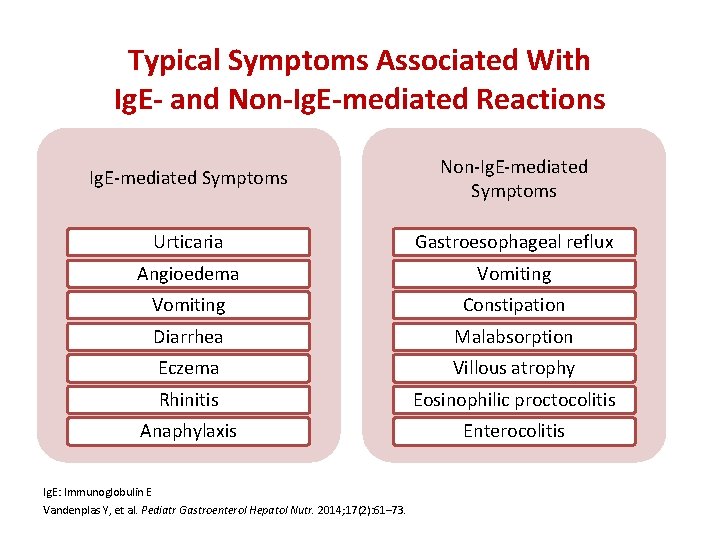
Typical Symptoms Associated With Ig. E- and Non-Ig. E-mediated Reactions Ig. E-mediated Symptoms Non-Ig. E-mediated Symptoms Urticaria Gastroesophageal reflux Angioedema Vomiting Constipation Diarrhea Malabsorption Eczema Villous atrophy Rhinitis Eosinophilic proctocolitis Anaphylaxis Enterocolitis Ig. E: Immunoglobulin E Vandenplas Y, et al. Pediatr Gastroenterol Hepatol Nutr. 2014; 17(2): 61– 73.
Myth 1 Lactose intolerance is same as CMPA
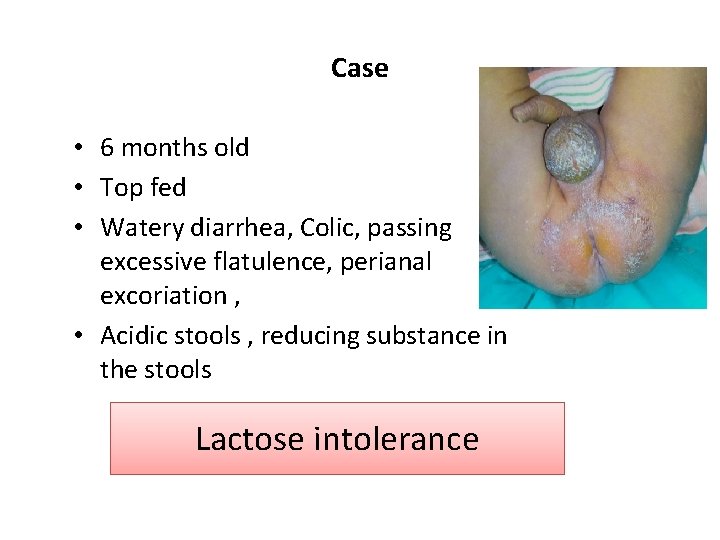
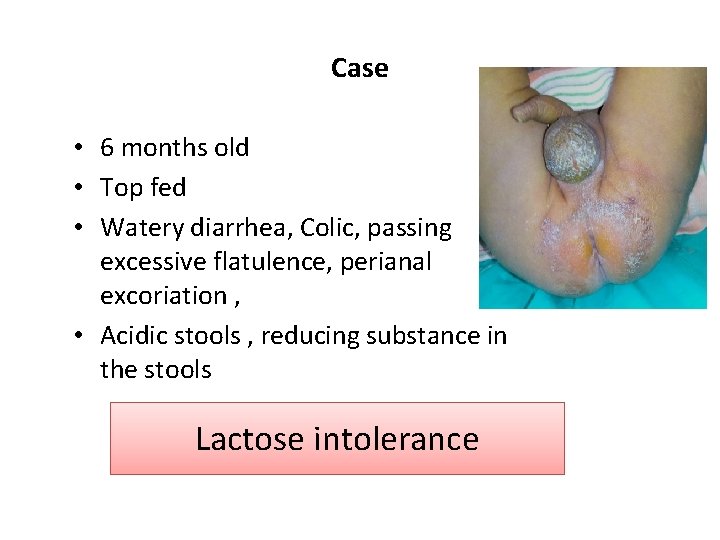
Case • 6 months old • Top fed • Watery diarrhea, Colic, passing excessive flatulence, perianal excoriation , • Acidic stools , reducing substance in the stools Lactose intolerance
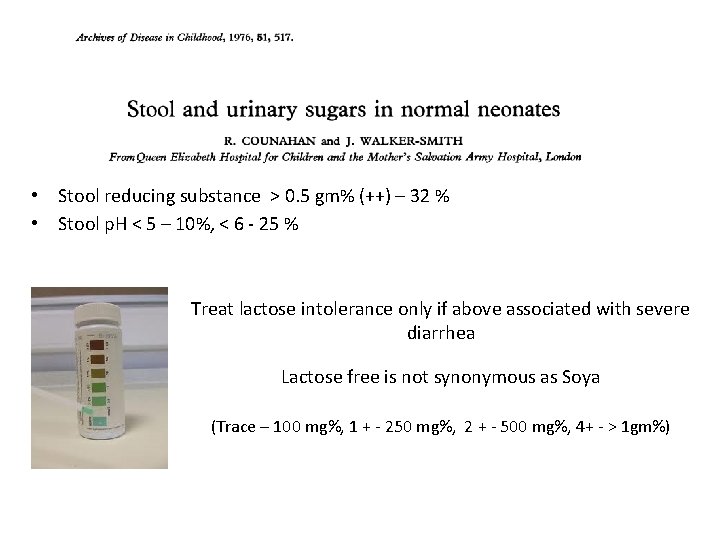
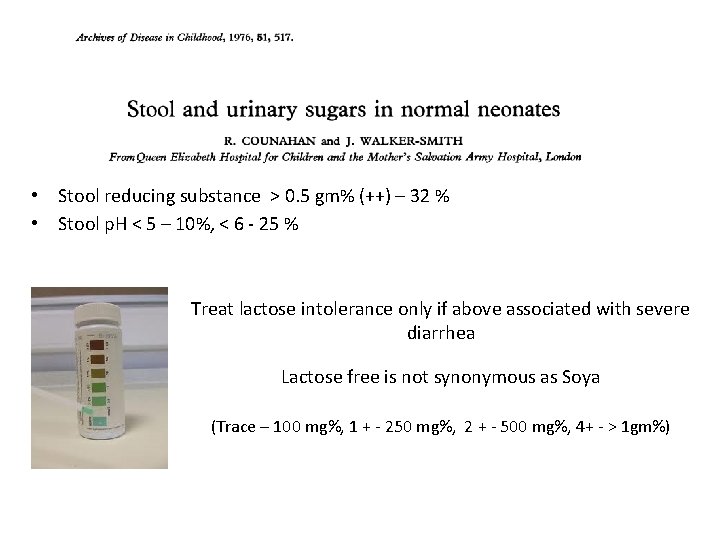
• Stool reducing substance > 0. 5 gm% (++) – 32 % • Stool p. H < 5 – 10%, < 6 - 25 % Treat lactose intolerance only if above associated with severe diarrhea Lactose free is not synonymous as Soya (Trace – 100 mg%, 1 + - 250 mg%, 2 + - 500 mg%, 4+ - > 1 gm%)
Myth 1 Lactose intolerance is same as CMPA • Both are entirely different entities • CMPA being immune mediated requiring complete avoidance of milk and milk products for varying duration • Lactose intolerance is non-immune mediated (enzymatic) and is transient.
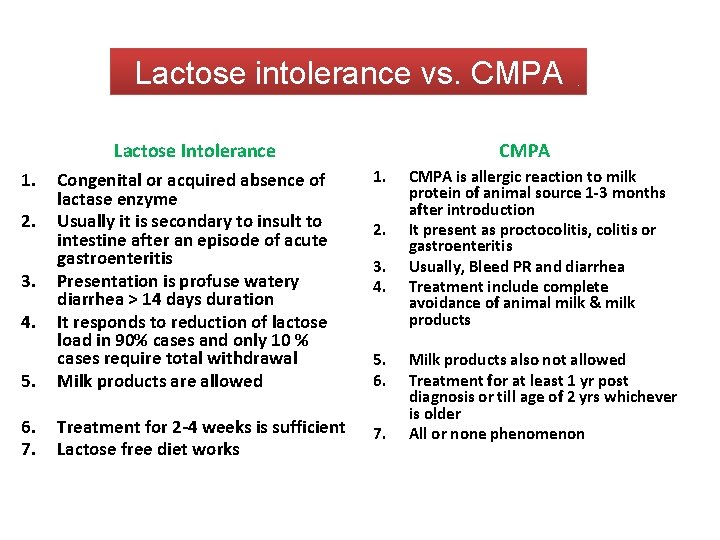
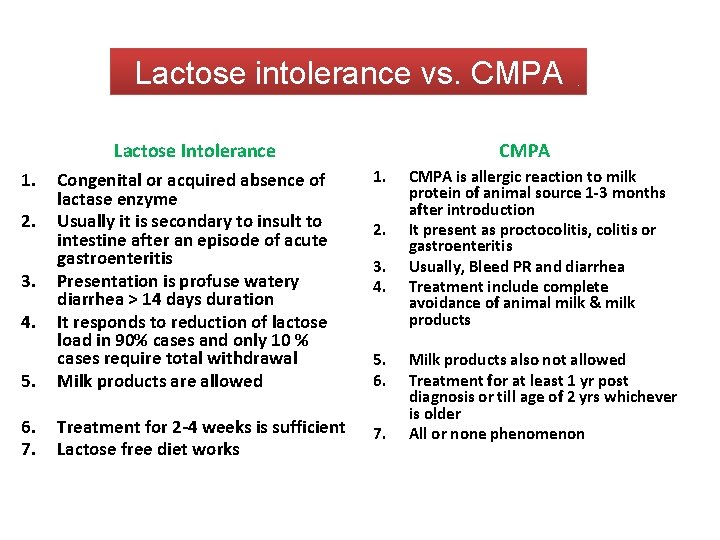
Lactose intolerance vs. CMPA Lactose Intolerance CMPA 1. 5. Congenital or acquired absence of lactase enzyme Usually it is secondary to insult to intestine after an episode of acute gastroenteritis Presentation is profuse watery diarrhea > 14 days duration It responds to reduction of lactose load in 90% cases and only 10 % cases require total withdrawal Milk products are allowed 6. 7. Treatment for 2 -4 weeks is sufficient Lactose free diet works 7. 1. 2. 3. 4. 5. 6. CMPA is allergic reaction to milk protein of animal source 1 -3 months after introduction It present as proctocolitis, colitis or gastroenteritis Usually, Bleed PR and diarrhea Treatment include complete avoidance of animal milk & milk products Milk products also not allowed Treatment for at least 1 yr post diagnosis or till age of 2 yrs whichever is older All or none phenomenon
What makes CMPA challenging ?
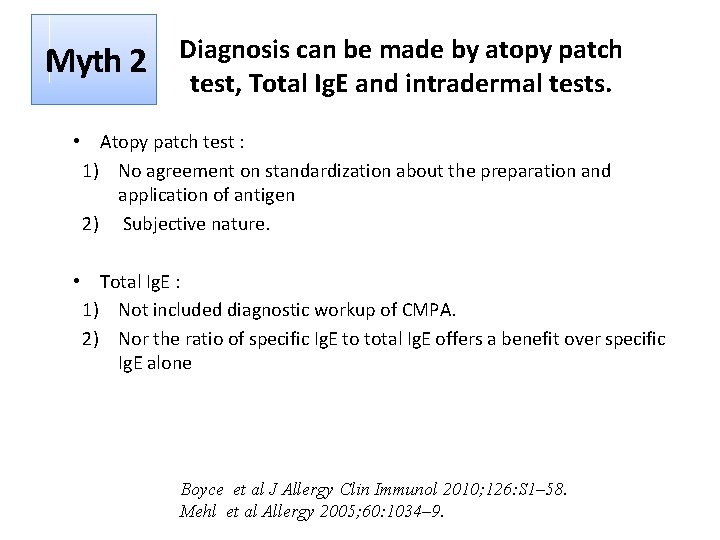
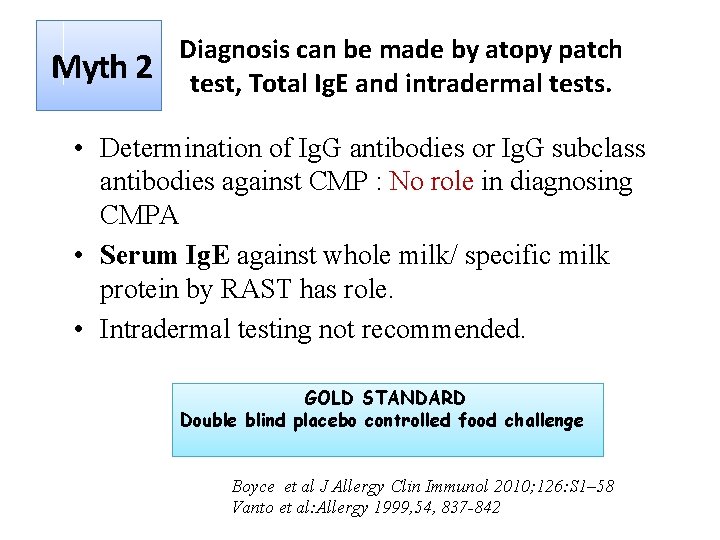
Myth 2 Diagnosis can be made by atopy patch test, Total Ig. E and intradermal tests.
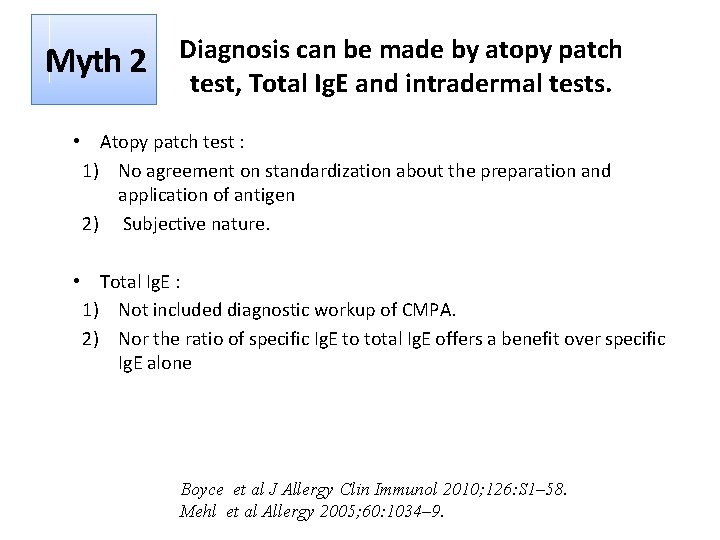
Myth 2 Diagnosis can be made by atopy patch test, Total Ig. E and intradermal tests. • Atopy patch test : 1) No agreement on standardization about the preparation and application of antigen 2) Subjective nature. • Total Ig. E : 1) Not included diagnostic workup of CMPA. 2) Nor the ratio of specific Ig. E to total Ig. E offers a benefit over specific Ig. E alone Boyce et al J Allergy Clin Immunol 2010; 126: S 1– 58. Mehl et al Allergy 2005; 60: 1034– 9.
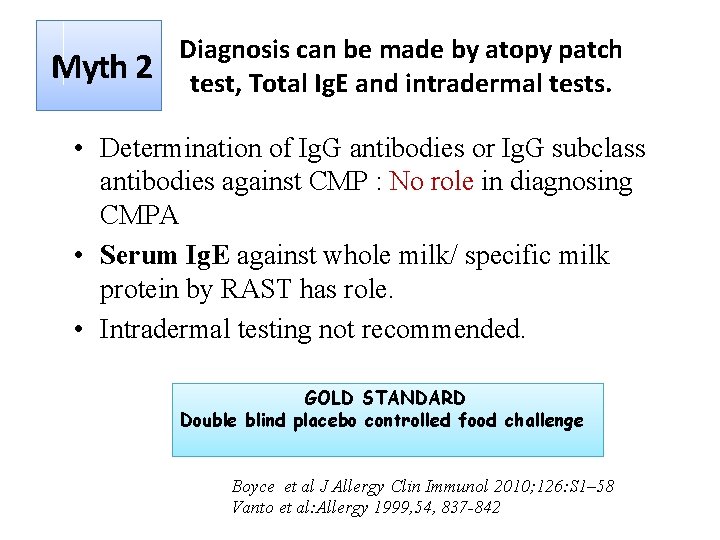
Myth 2 Diagnosis can be made by atopy patch test, Total Ig. E and intradermal tests. • Determination of Ig. G antibodies or Ig. G subclass antibodies against CMP : No role in diagnosing CMPA • Serum Ig. E against whole milk/ specific milk protein by RAST has role. • Intradermal testing not recommended. GOLD STANDARD Double blind placebo controlled food challenge Boyce et al J Allergy Clin Immunol 2010; 126: S 1– 58 Vanto et al: Allergy 1999, 54, 837 -842
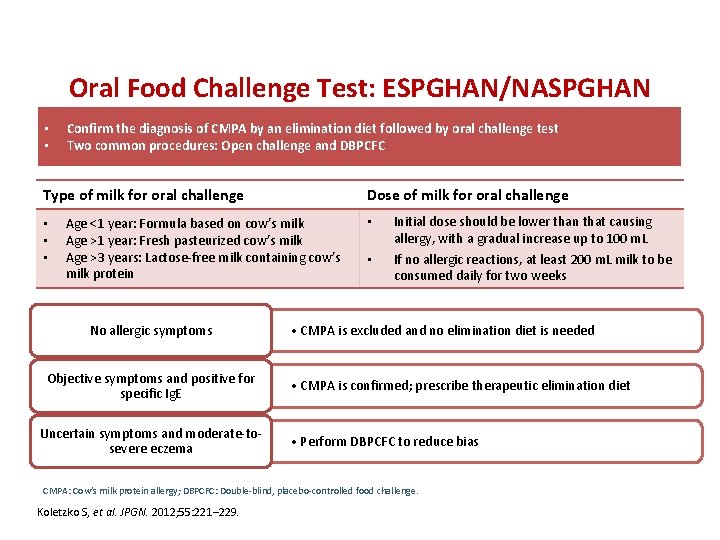
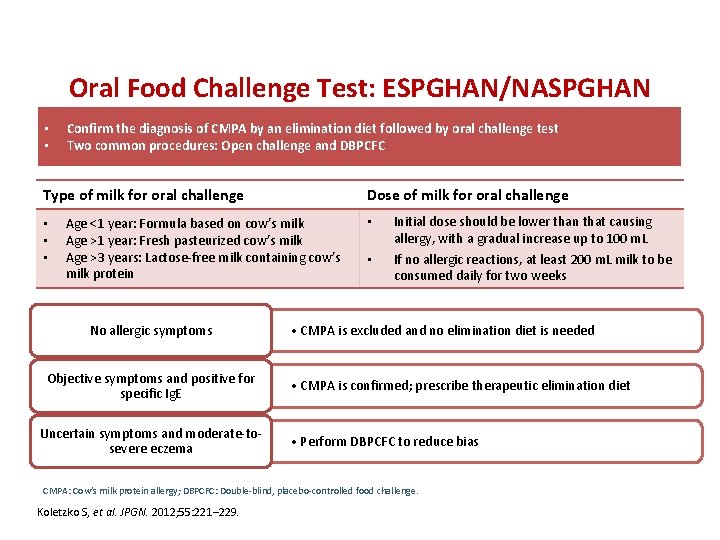
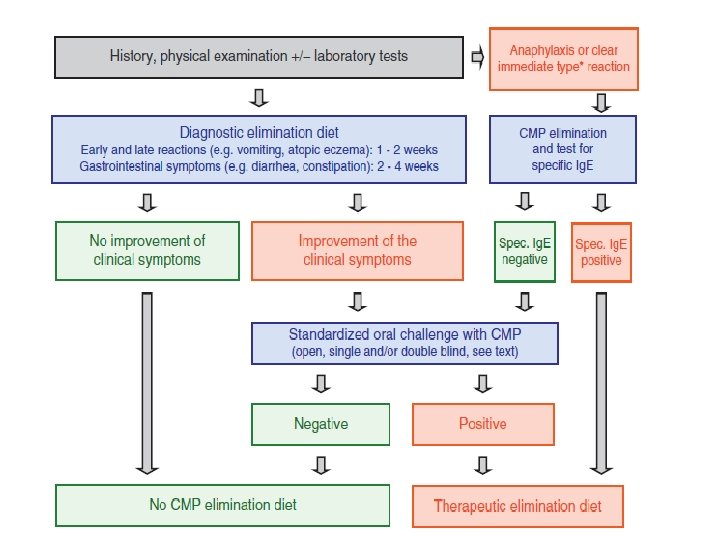
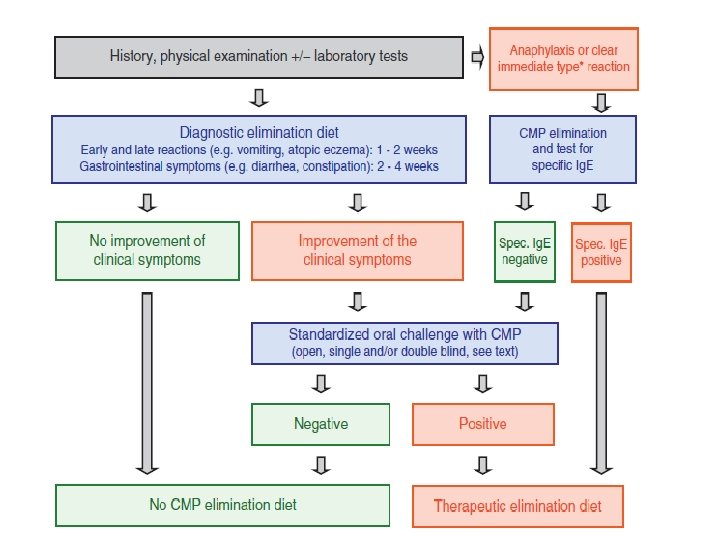
• • Oral Food Challenge Test: ESPGHAN/NASPGHAN Guideline Recommendations Confirm the diagnosis of CMPA by an elimination diet followed by oral challenge test Two common procedures: Open challenge and DBPCFC Type of milk for oral challenge • • • Dose of milk for oral challenge Age <1 year: Formula based on cow’s milk Age >1 year: Fresh pasteurized cow’s milk Age >3 years: Lactose-free milk containing cow’s milk protein No allergic symptoms Objective symptoms and positive for specific Ig. E Uncertain symptoms and moderate-tosevere eczema • • Initial dose should be lower than that causing allergy, with a gradual increase up to 100 m. L If no allergic reactions, at least 200 m. L milk to be consumed daily for two weeks • CMPA is excluded and no elimination diet is needed • CMPA is confirmed; prescribe therapeutic elimination diet • Perform DBPCFC to reduce bias CMPA: Cow’s milk protein allergy; DBPCFC: Double-blind, placebo-controlled food challenge. Koletzko S, et al. JPGN. 2012; 55: 221– 229.
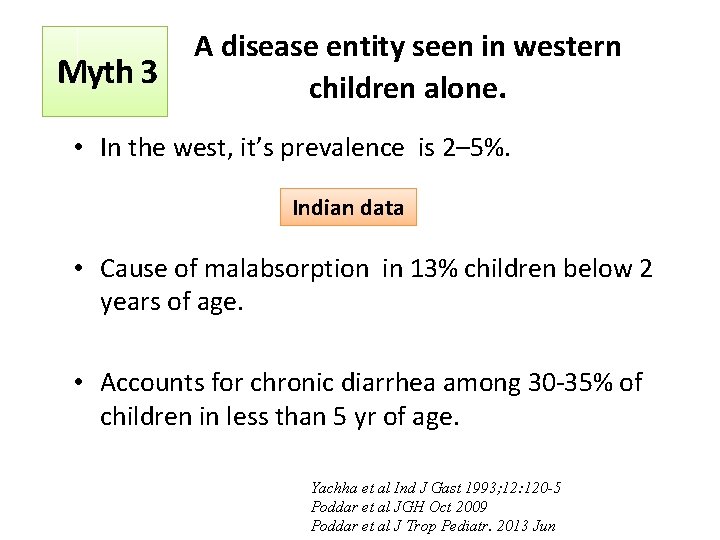
Myth 3 A disease entity seen in western children alone.
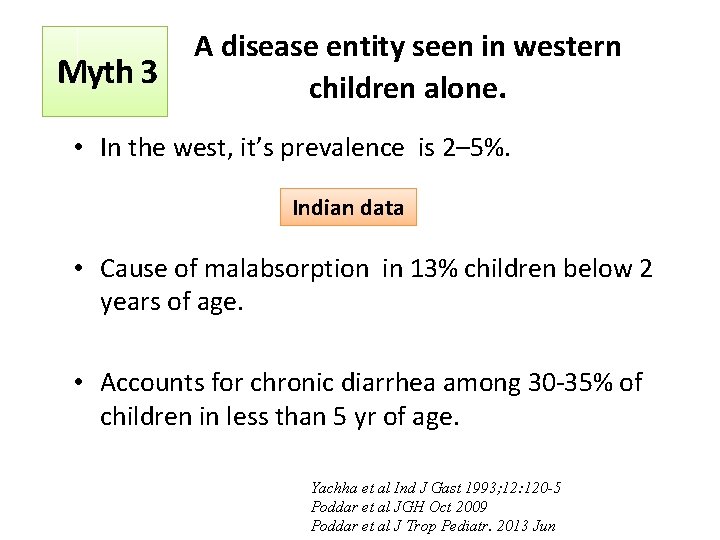
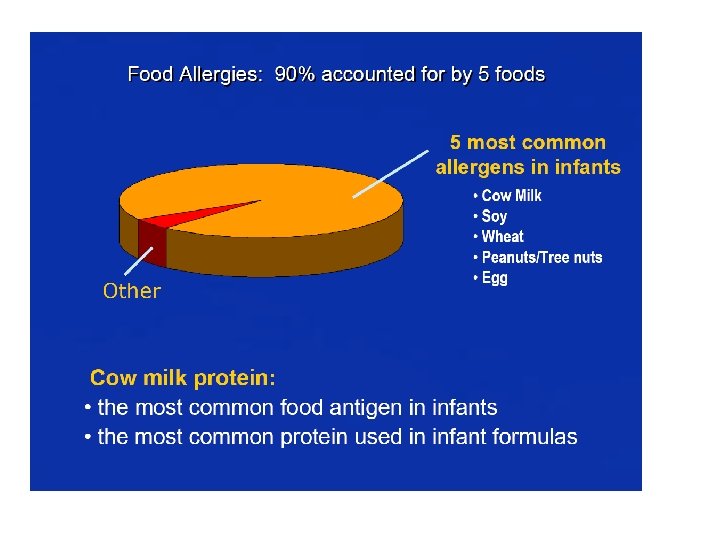
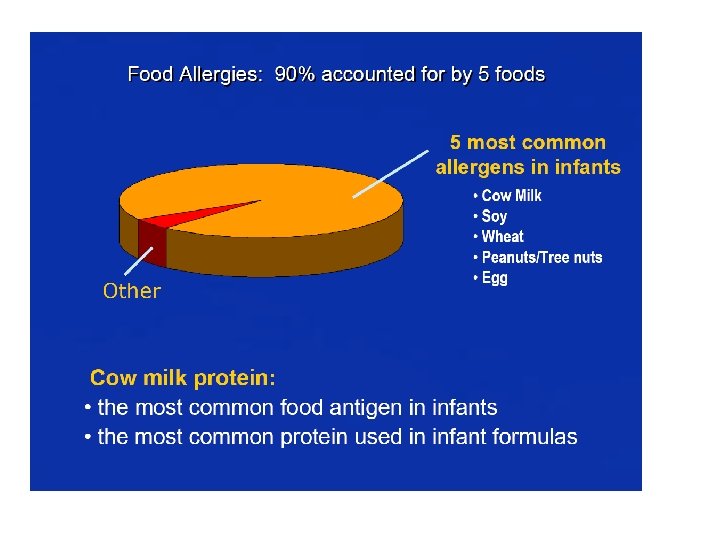
Myth 3 A disease entity seen in western children alone. • In the west, it’s prevalence is 2– 5%. Indian data • Cause of malabsorption in 13% children below 2 years of age. • Accounts for chronic diarrhea among 30 -35% of children in less than 5 yr of age. Yachha et al Ind J Gast 1993; 12: 120 -5 Poddar et al JGH Oct 2009 Poddar et al J Trop Pediatr. 2013 Jun

An : f n e O r d ate l i h C t S In The In a e h r r a i D ectrum ; 4 1 p 0 c 2 i. S r t n a i o d l e r P p m Ch logica esh e t n o. C 1 J 4 t d o n 7 I i 3 a : Et ar Pr 1(1) Utt Authors Dr Shrish Bhatnagar, Dr Romesh Gauttam Received DR J. R. SRIVASTAVA AWARD at UP Pedicon 2011
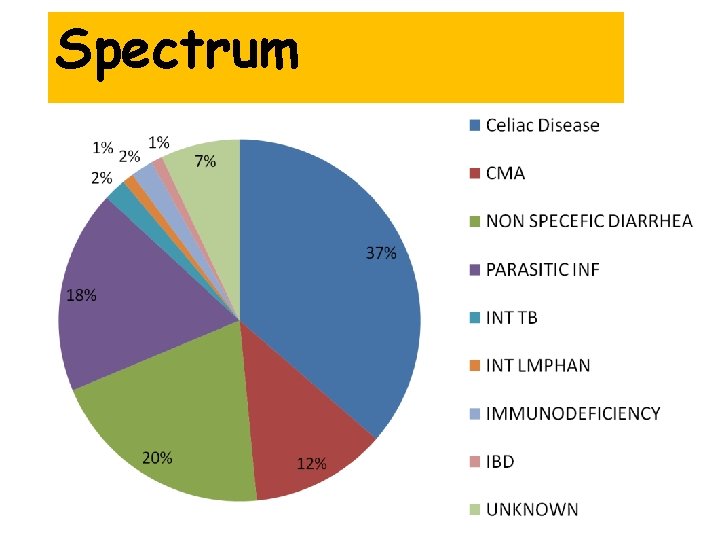
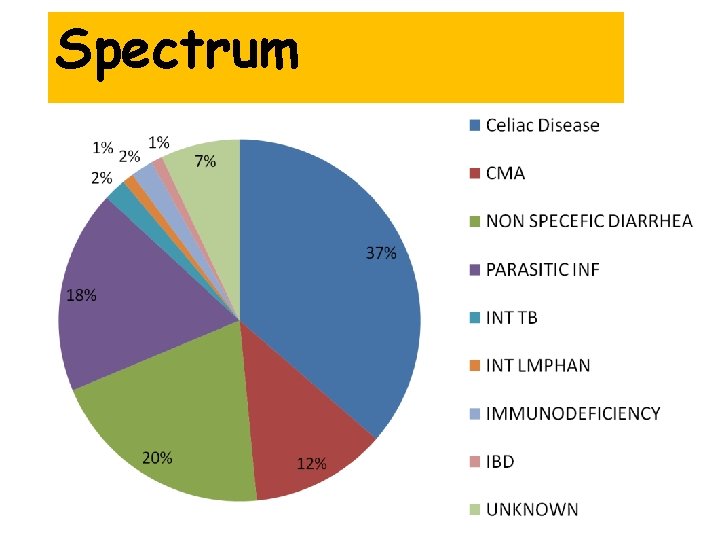
Spectrum
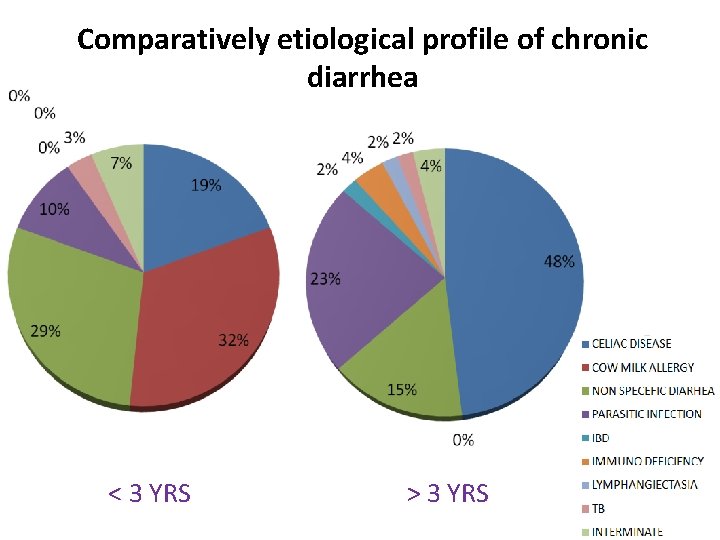
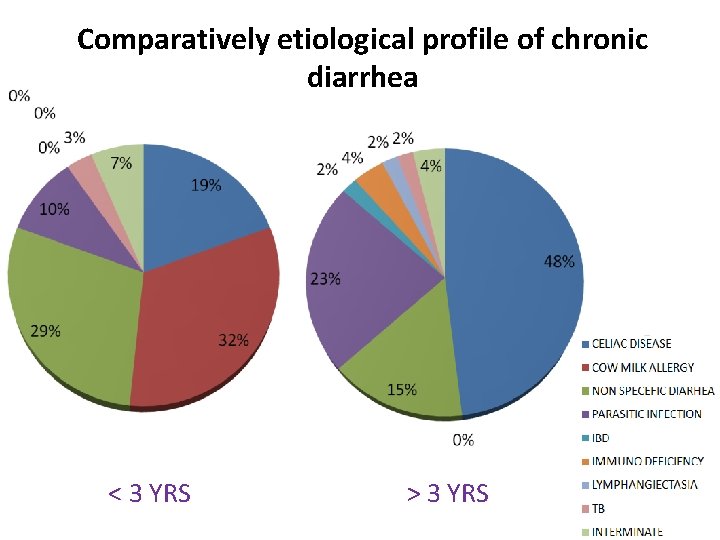
Comparatively etiological profile of chronic diarrhea < 3 YRS > 3 YRS
Myth 4 Onset of cow milk allergy can occur after 5 yr of age.
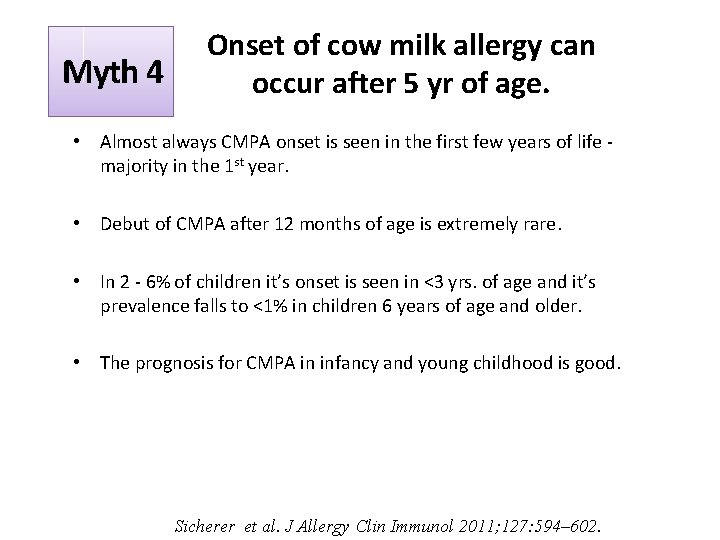
Myth 4 Onset of cow milk allergy can occur after 5 yr of age. • Almost always CMPA onset is seen in the first few years of life - majority in the 1 st year. • Debut of CMPA after 12 months of age is extremely rare. • In 2 - 6% of children it’s onset is seen in <3 yrs. of age and it’s prevalence falls to <1% in children 6 years of age and older. • The prognosis for CMPA in infancy and young childhood is good. Sicherer et al. J Allergy Clin Immunol 2011; 127: 594– 602.
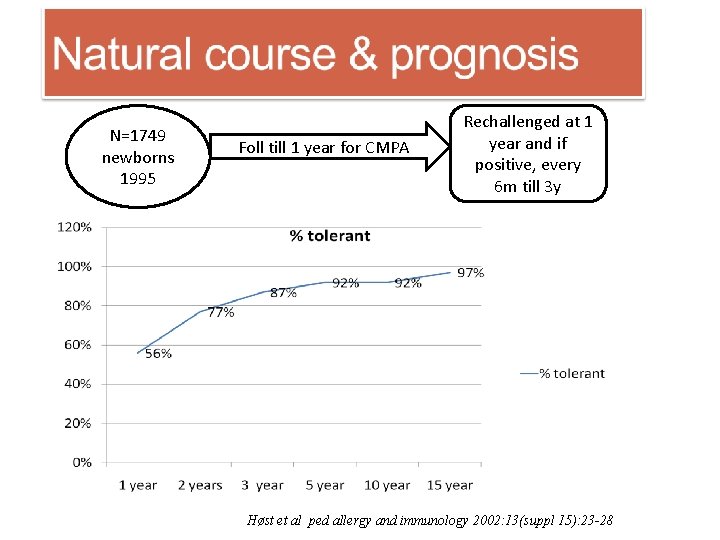
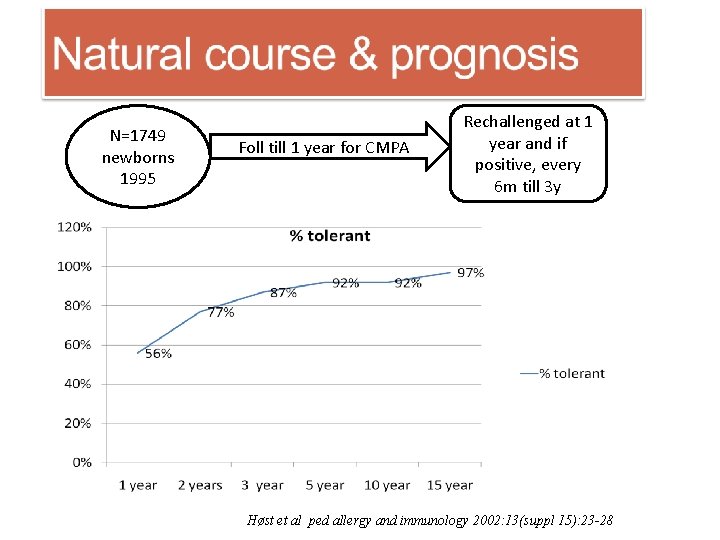
N=1749 newborns 1995 Foll till 1 year for CMPA Rechallenged at 1 year and if positive, every 6 m till 3 y Høst et al ped allergy and immunology 2002: 13(suppl 15): 23 -28
Myth 4 Onset of cow milk allergy can occur after 5 yr of age. • Inappropriate or overly long dietary eliminations should be avoided. • Such restrictions : 1) Impair the quality of life of both child and family, 2) Induce improper growth, and 3) Incur unnecessary health care costs. Sicherer et al. J Allergy Clin Immunol 2011; 127: 594– 602.
Myth 5 Milk from other animal sources can be given in a child with CMPA. • Cross-reactivity is present among milk proteins obtained from cows, goats and sheep. • Strong structural homology between milk proteins from different mammals. • Only the whey fraction in the goat's milk differs from that in the cow's milk. • Goat's milk is tolerated by only 40% of children who are allergic to cow's milk. All animal milk are to be avoided Bellioni et al J Allergy Clin Immunol. 1999; 103: 1191– 1194
General Principles for Management of CMPA Dietary elimination of CMP and replacement with hypoallergenic or soy formula Maternal CMP elimination CMPA: Cow’s milk protein allergy Allen K, Davidson G, Day A et al. Journal of Paediatrics and Child Health. 2009; (45): 481– 486
Case scenario- 2 • 3 month old infant c/o visible specks of blood with mucus. • Exclusively breast fed • Non sick baby, wt gain acceptable • Stool examination – Blood present • What next?
Case scenario-3 • 11 month old infant with on and off minor blood mixed with loose stools for 4 months. • Not otherwise pale, growth satisfactory • Diet – On cows milk at onset, changed to lactose free soya milk, multiple antibiotics, • NO RESPONSE
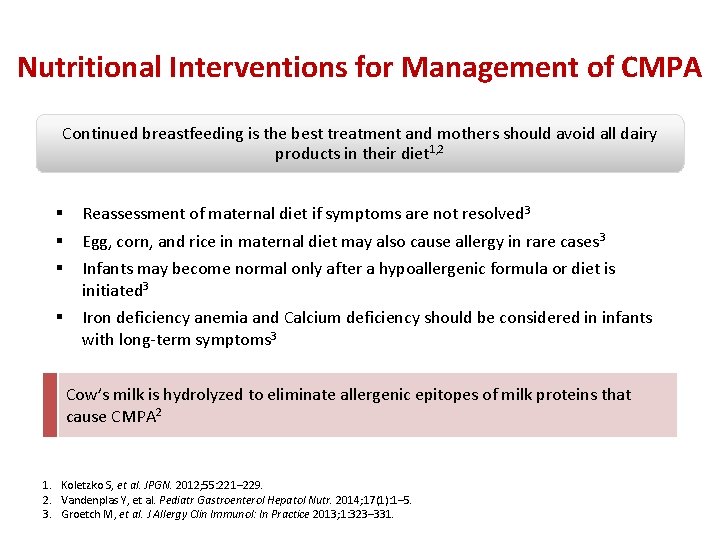
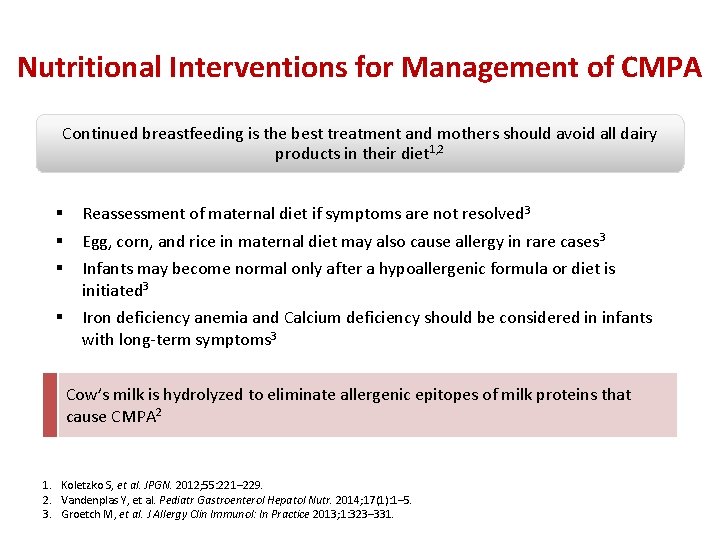
Nutritional Interventions for Management of CMPA Continued breastfeeding is the best treatment and mothers should avoid all dairy products in their diet 1, 2 § § § Reassessment of maternal diet if symptoms are not resolved 3 § Iron deficiency anemia and Calcium deficiency should be considered in infants with long-term symptoms 3 Egg, corn, and rice in maternal diet may also cause allergy in rare cases 3 Infants may become normal only after a hypoallergenic formula or diet is initiated 3 Cow’s milk is hydrolyzed to eliminate allergenic epitopes of milk proteins that cause CMPA 2 1. Koletzko S, et al. JPGN. 2012; 55: 221– 229. 2. Vandenplas Y, et al. Pediatr Gastroenterol Hepatol Nutr. 2014; 17(1): 1– 5. 3. Groetch M, et al. J Allergy Clin Immunol: In Practice 2013; 1: 323– 331.
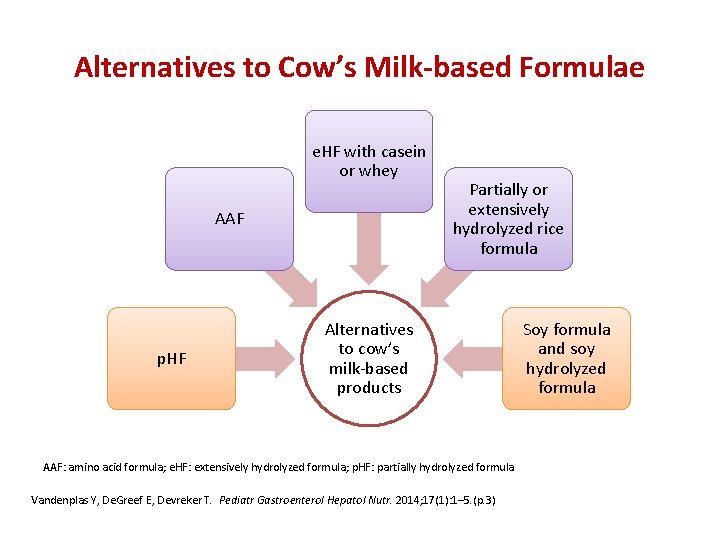
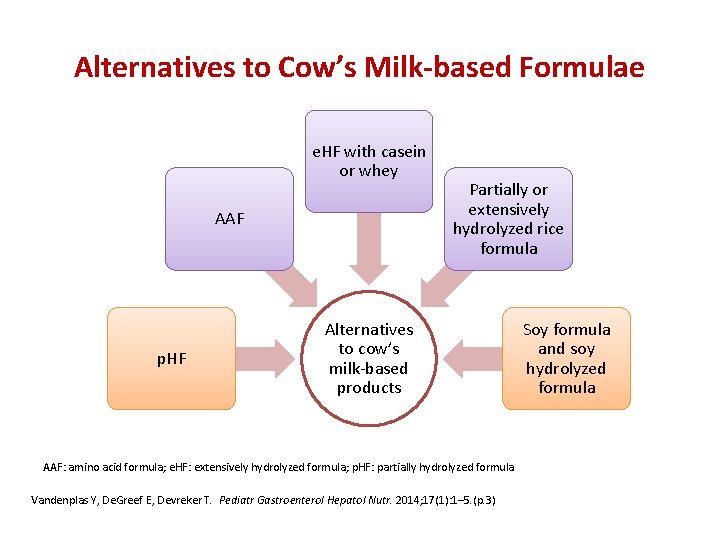
Alternatives to Cow’s Milk-based Formulae e. HF with casein or whey AAF p. HF Partially or extensively hydrolyzed rice formula Alternatives to cow’s milk-based products AAF: amino acid formula; e. HF: extensively hydrolyzed formula; p. HF: partially hydrolyzed formula Vandenplas Y, De. Greef E, Devreker T. Pediatr Gastroenterol Hepatol Nutr. 2014; 17(1): 1– 5. (p. 3) Soy formula and soy hydrolyzed formula
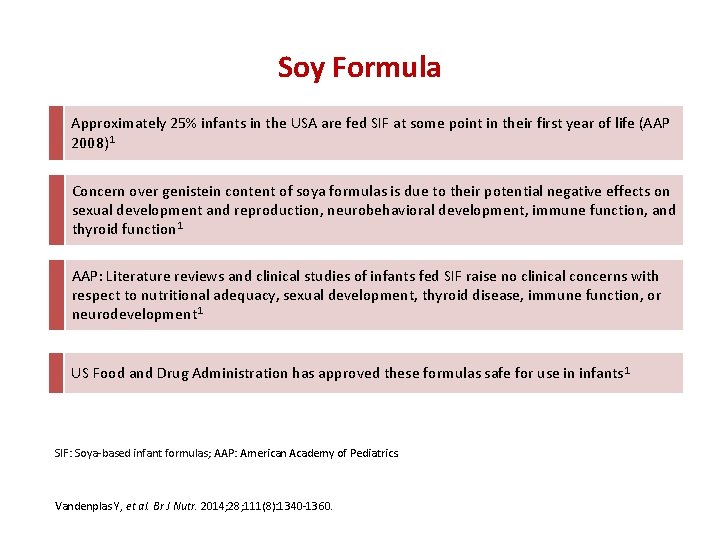
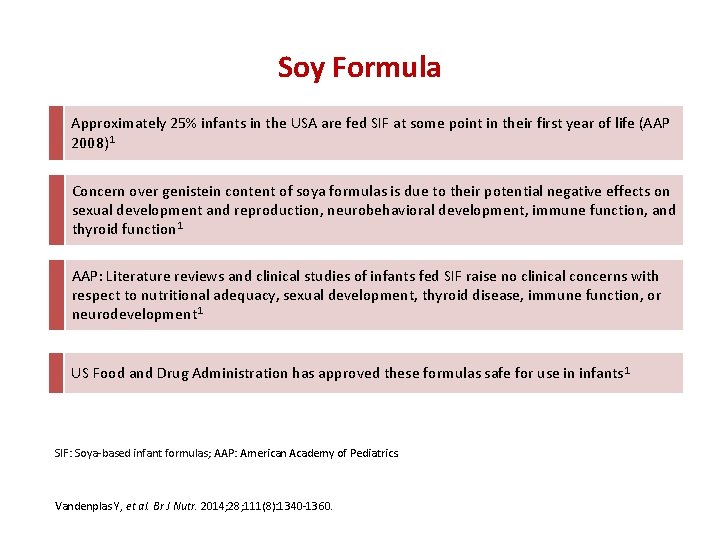
Soy Formula Approximately 25% infants in the USA are fed SIF at some point in their first year of life (AAP 2008)1 Concern over genistein content of soya formulas is due to their potential negative effects on sexual development and reproduction, neurobehavioral development, immune function, and thyroid function 1 AAP: Literature reviews and clinical studies of infants fed SIF raise no clinical concerns with respect to nutritional adequacy, sexual development, thyroid disease, immune function, or neurodevelopment 1 US Food and Drug Administration has approved these formulas safe for use in infants 1 SIF: Soya-based infant formulas; AAP: American Academy of Pediatrics. Vandenplas Y, et al. Br J Nutr. 2014; 28; 111(8): 1340 -1360.
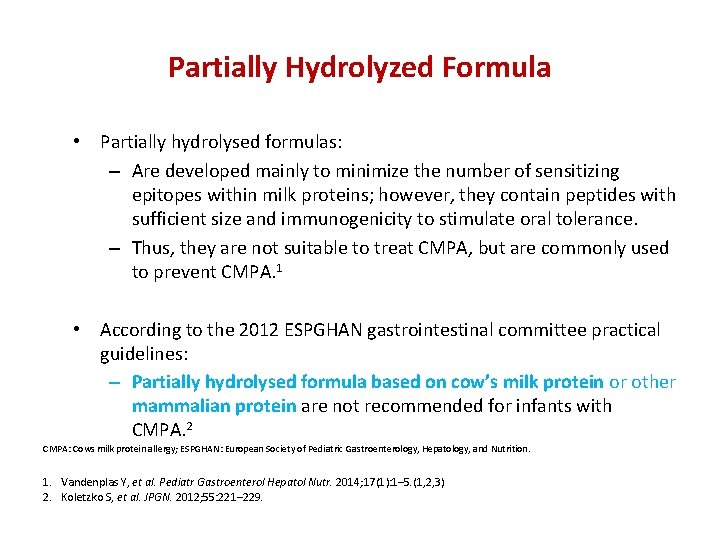
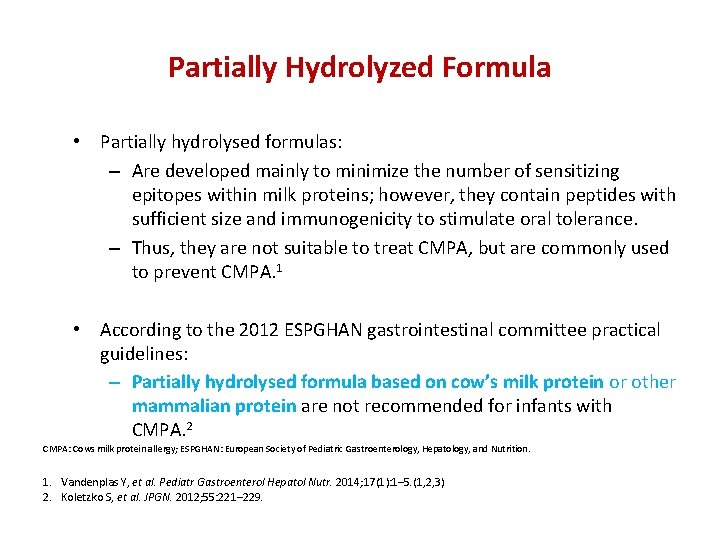
Partially Hydrolyzed Formula • Partially hydrolysed formulas: – Are developed mainly to minimize the number of sensitizing epitopes within milk proteins; however, they contain peptides with sufficient size and immunogenicity to stimulate oral tolerance. – Thus, they are not suitable to treat CMPA, but are commonly used to prevent CMPA. 1 • According to the 2012 ESPGHAN gastrointestinal committee practical guidelines: – Partially hydrolysed formula based on cow’s milk protein or other mammalian protein are not recommended for infants with CMPA. 2 CMPA: Cows milk protein allergy; ESPGHAN: European Society of Pediatric Gastroenterology, Hepatology, and Nutrition. 1. Vandenplas Y, et al. Pediatr Gastroenterol Hepatol Nutr. 2014; 17(1): 1– 5. (1, 2, 3) 2. Koletzko S, et al. JPGN. 2012; 55: 221– 229.
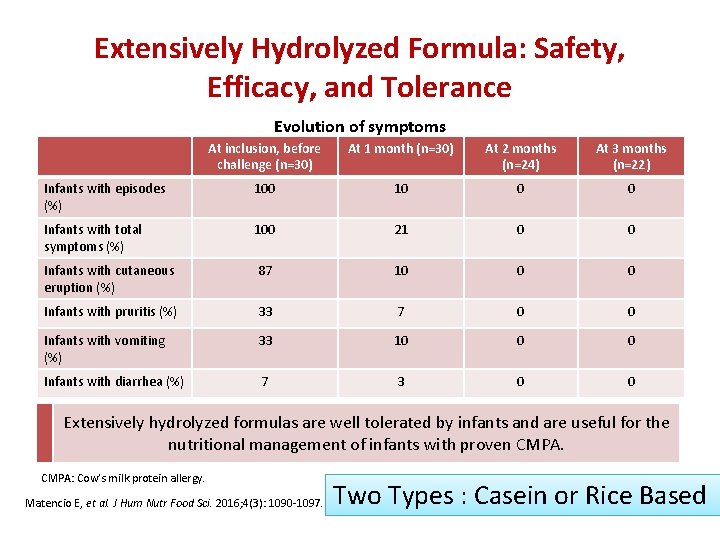
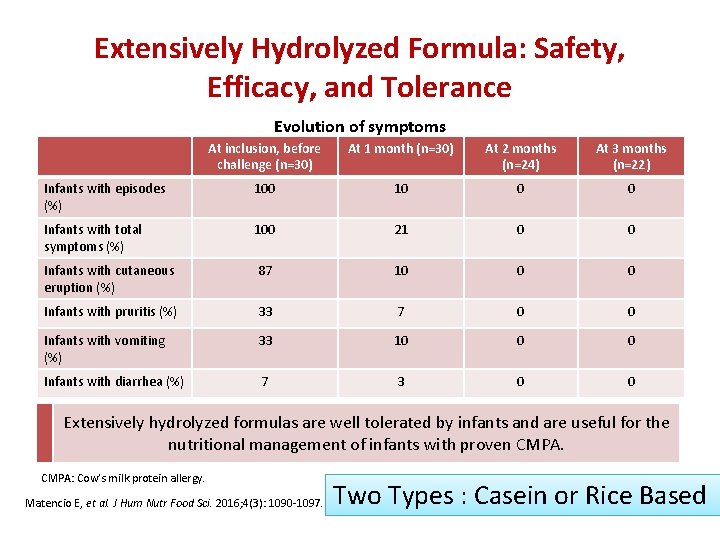
Extensively Hydrolyzed Formula: Safety, Efficacy, and Tolerance Evolution of symptoms At inclusion, before challenge (n=30) At 1 month (n=30) At 2 months (n=24) At 3 months (n=22) Infants with episodes (%) 100 10 0 0 Infants with total symptoms (%) 100 21 0 0 Infants with cutaneous eruption (%) 87 10 0 0 Infants with pruritis (%) 33 7 0 0 Infants with vomiting (%) 33 10 0 0 Infants with diarrhea (%) 7 3 0 0 Extensively hydrolyzed formulas are well tolerated by infants and are useful for the nutritional management of infants with proven CMPA: Cow’s milk protein allergy. Matencio E, et al. J Hum Nutr Food Sci. 2016; 4(3): 1090 -1097. Two Types : Casein or Rice Based
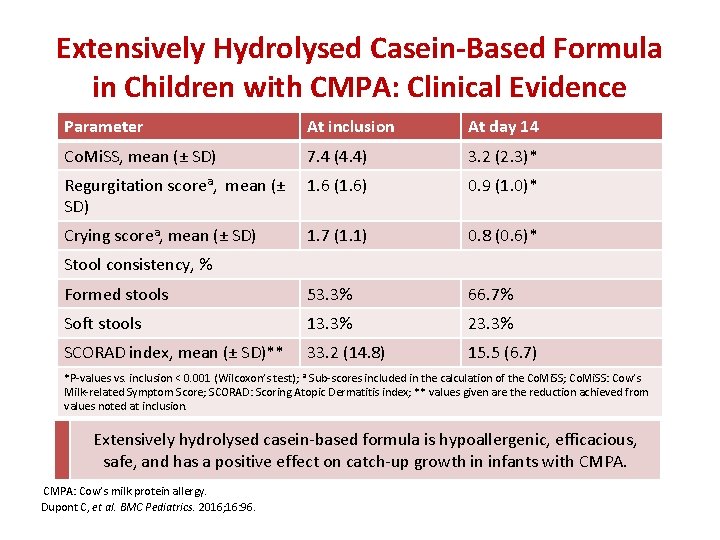
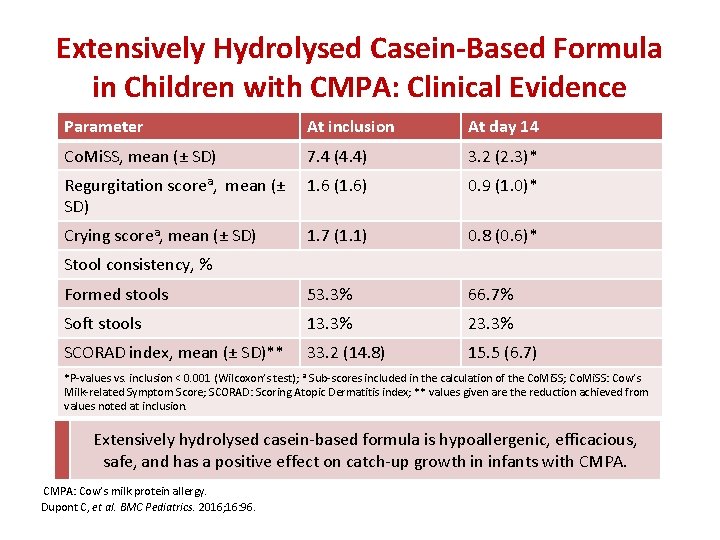
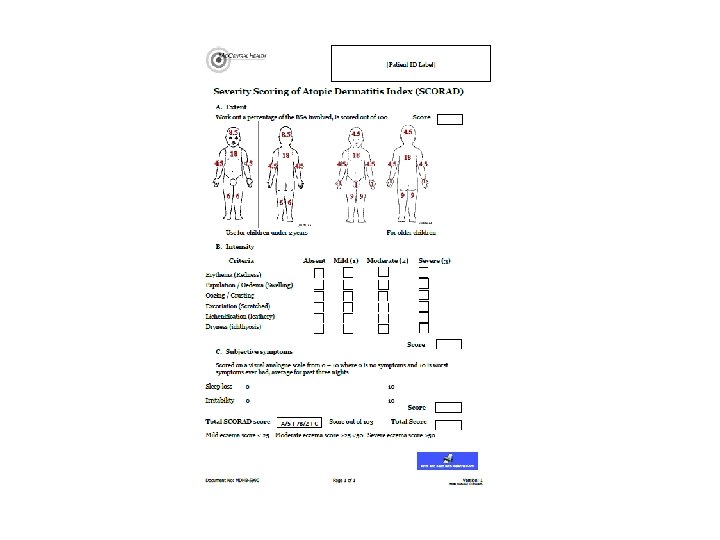
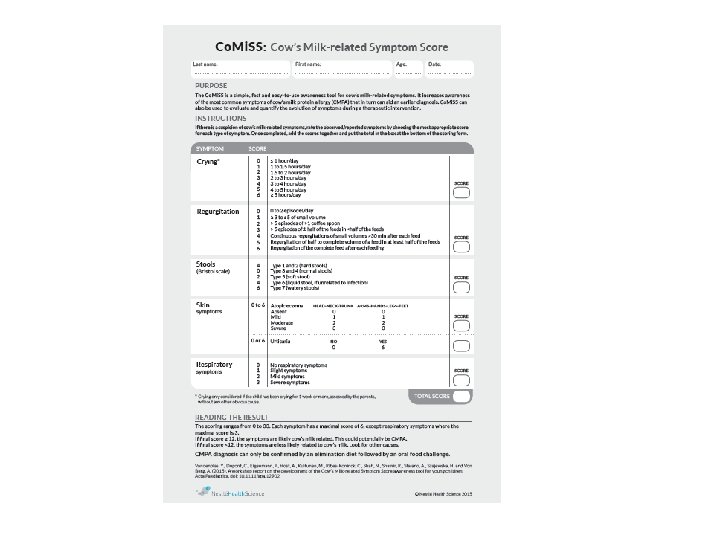
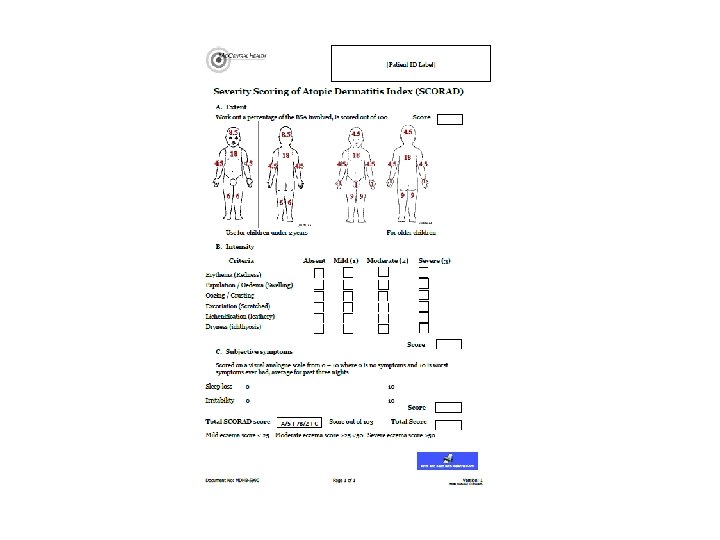
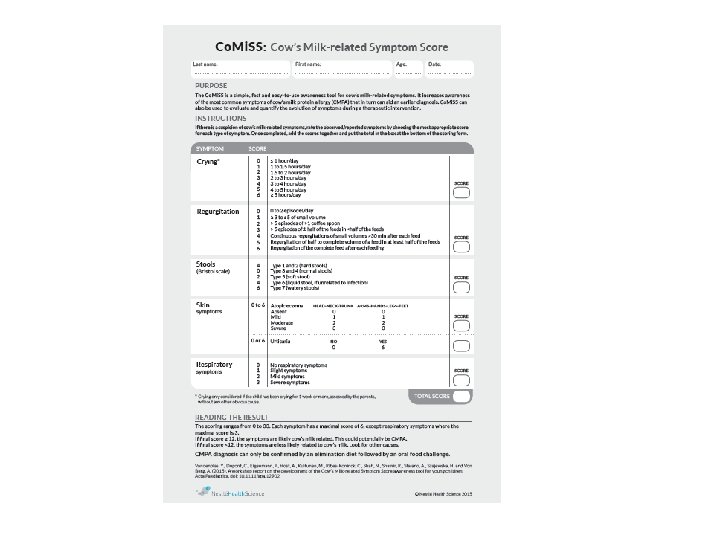
Extensively Hydrolysed Casein-Based Formula in Children with CMPA: Clinical Evidence Parameter At inclusion At day 14 Co. Mi. SS, mean (± SD) 7. 4 (4. 4) 3. 2 (2. 3)* Regurgitation scorea, mean (± 1. 6 (1. 6) SD) 0. 9 (1. 0)* Crying scorea, mean (± SD) 1. 7 (1. 1) 0. 8 (0. 6)* Formed stools 53. 3% 66. 7% Soft stools 13. 3% 23. 3% SCORAD index, mean (± SD)** 33. 2 (14. 8) 15. 5 (6. 7) Stool consistency, % *P-values vs. inclusion < 0. 001 (Wilcoxon’s test); a Sub-scores included in the calculation of the Co. Mi. SS; Co. Mi. SS: Cow’s Milk-related Symptom Score; SCORAD: Scoring Atopic Dermatitis index; ** values given are the reduction achieved from values noted at inclusion. Extensively hydrolysed casein-based formula is hypoallergenic, efficacious, safe, and has a positive effect on catch-up growth in infants with CMPA: Cow’s milk protein allergy. Dupont C, et al. BMC Pediatrics. 2016; 16: 96.
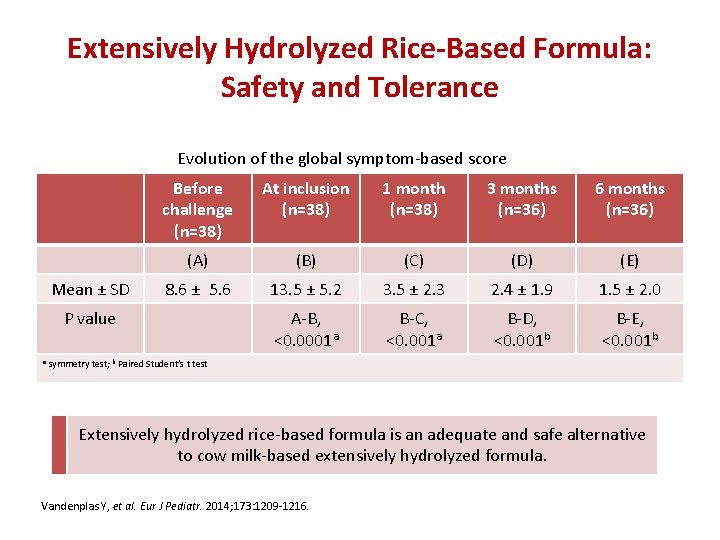
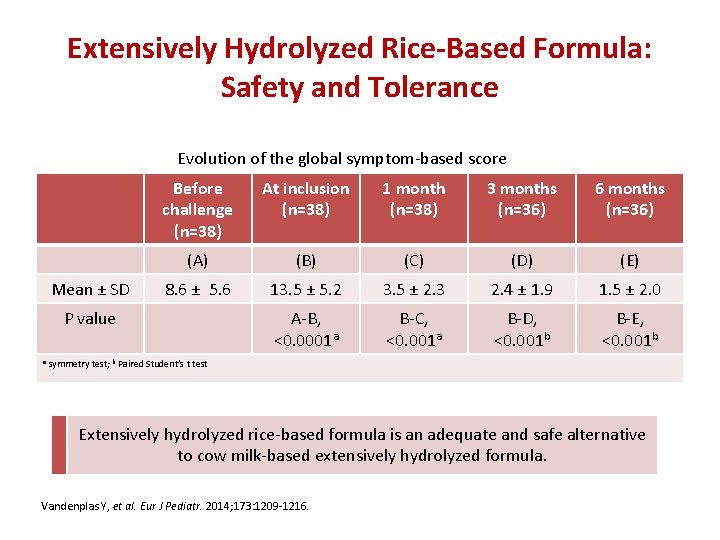
Extensively Hydrolyzed Rice-Based Formula: Safety and Tolerance Evolution of the global symptom-based score Mean ± SD Before challenge (n=38) At inclusion (n=38) 1 month (n=38) 3 months (n=36) 6 months (n=36) (A) (B) (C) (D) (E) 8. 6 ± 5. 6 13. 5 ± 5. 2 3. 5 ± 2. 3 2. 4 ± 1. 9 1. 5 ± 2. 0 A-B, <0. 0001 a B-C, <0. 001 a B-D, <0. 001 b B-E, <0. 001 b P value a symmetry test; b Paired Student’s t test Extensively hydrolyzed rice-based formula is an adequate and safe alternative to cow milk-based extensively hydrolyzed formula. Vandenplas Y, et al. Eur J Pediatr. 2014; 173: 1209 -1216.
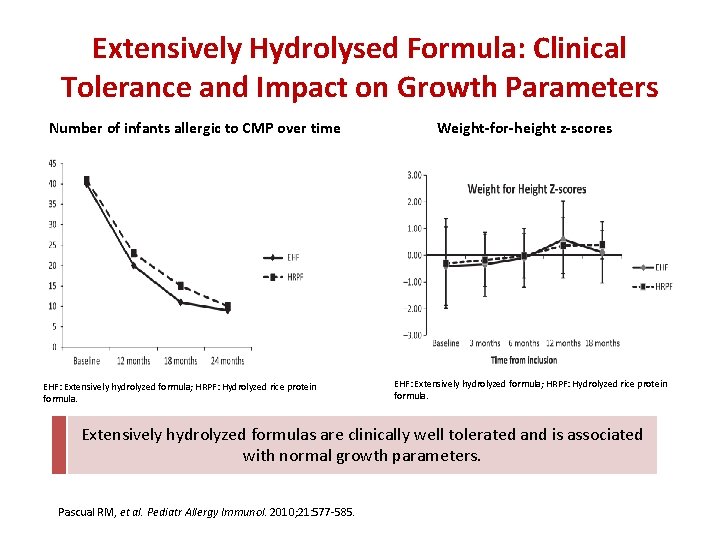
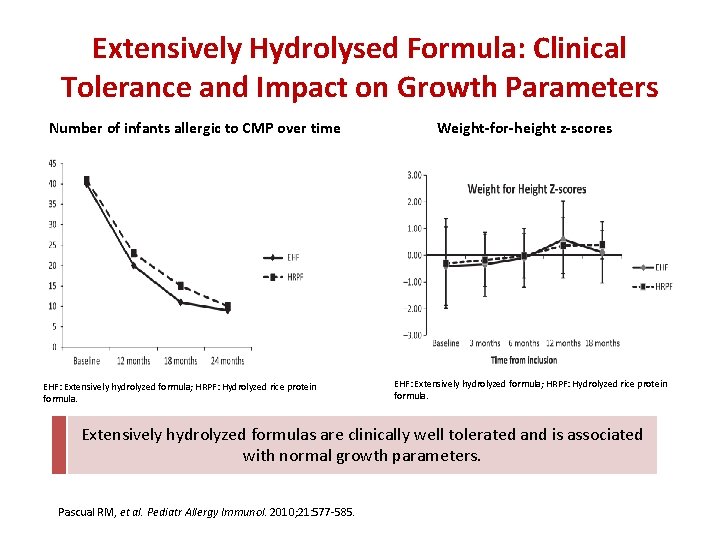
Extensively Hydrolysed Formula: Clinical Tolerance and Impact on Growth Parameters Number of infants allergic to CMP over time EHF: Extensively hydrolyzed formula; HRPF: Hydrolyzed rice protein formula. Weight-for-height z-scores EHF: Extensively hydrolyzed formula; HRPF: Hydrolyzed rice protein formula. Extensively hydrolyzed formulas are clinically well tolerated and is associated with normal growth parameters. Pascual RM, et al. Pediatr Allergy Immunol. 2010; 21: 577 -585.
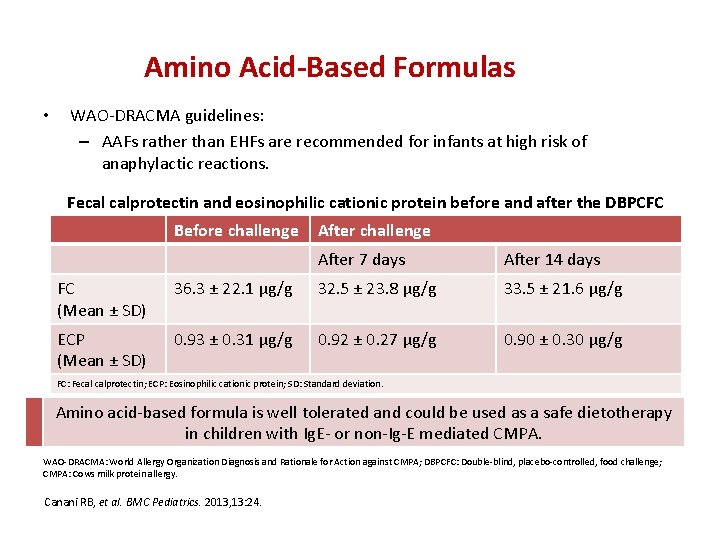
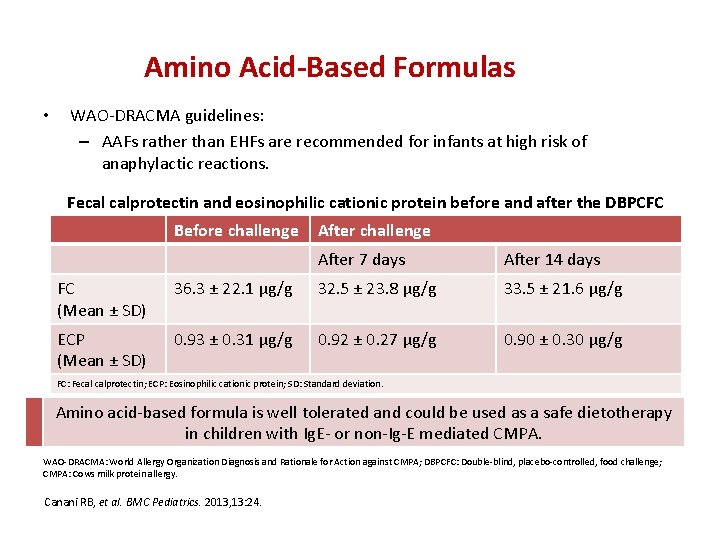
Amino Acid-Based Formulas • WAO-DRACMA guidelines: – AAFs rather than EHFs are recommended for infants at high risk of anaphylactic reactions. Fecal calprotectin and eosinophilic cationic protein before and after the DBPCFC Before challenge After 7 days After 14 days FC (Mean ± SD) 36. 3 ± 22. 1 μg/g 32. 5 ± 23. 8 μg/g 33. 5 ± 21. 6 μg/g ECP (Mean ± SD) 0. 93 ± 0. 31 μg/g 0. 92 ± 0. 27 μg/g 0. 90 ± 0. 30 μg/g FC: Fecal calprotectin; ECP: Eosinophilic cationic protein; SD: Standard deviation. Amino acid-based formula is well tolerated and could be used as a safe dietotherapy in children with Ig. E- or non-Ig-E mediated CMPA. WAO-DRACMA: World Allergy Organization Diagnosis and Rationale for Action against CMPA; DBPCFC: Double-blind, placebo-controlled, food challenge; CMPA: Cows milk protein allergy. Canani RB, et al. BMC Pediatrics. 2013, 13: 24.
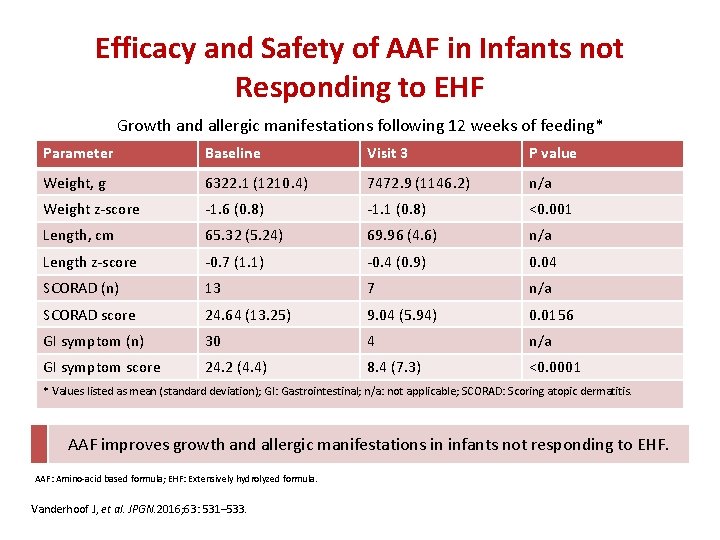
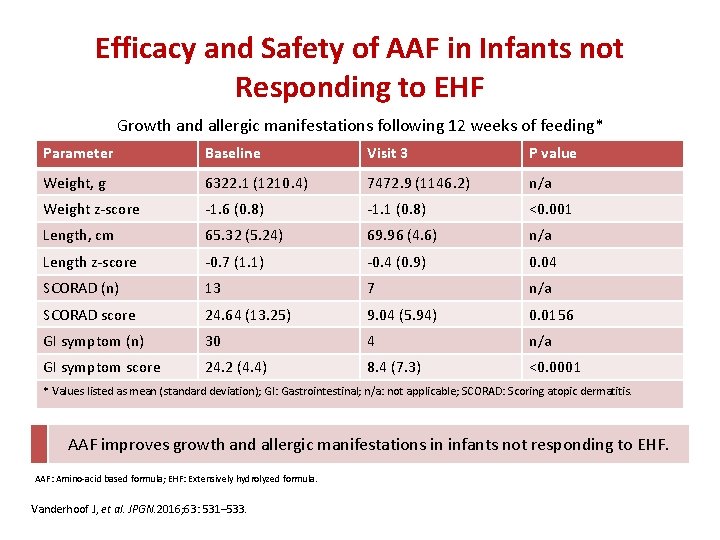
Efficacy and Safety of AAF in Infants not Responding to EHF Growth and allergic manifestations following 12 weeks of feeding* Parameter Baseline Visit 3 P value Weight, g 6322. 1 (1210. 4) 7472. 9 (1146. 2) n/a Weight z-score -1. 6 (0. 8) -1. 1 (0. 8) <0. 001 Length, cm 65. 32 (5. 24) 69. 96 (4. 6) n/a Length z-score -0. 7 (1. 1) -0. 4 (0. 9) 0. 04 SCORAD (n) 13 7 n/a SCORAD score 24. 64 (13. 25) 9. 04 (5. 94) 0. 0156 GI symptom (n) 30 4 n/a GI symptom score 24. 2 (4. 4) 8. 4 (7. 3) <0. 0001 * Values listed as mean (standard deviation); GI: Gastrointestinal; n/a: not applicable; SCORAD: Scoring atopic dermatitis. AAF improves growth and allergic manifestations in infants not responding to EHF. AAF: Amino-acid based formula; EHF: Extensively hydrolyzed formula. Vanderhoof J, et al. JPGN. 2016; 63: 531– 533.
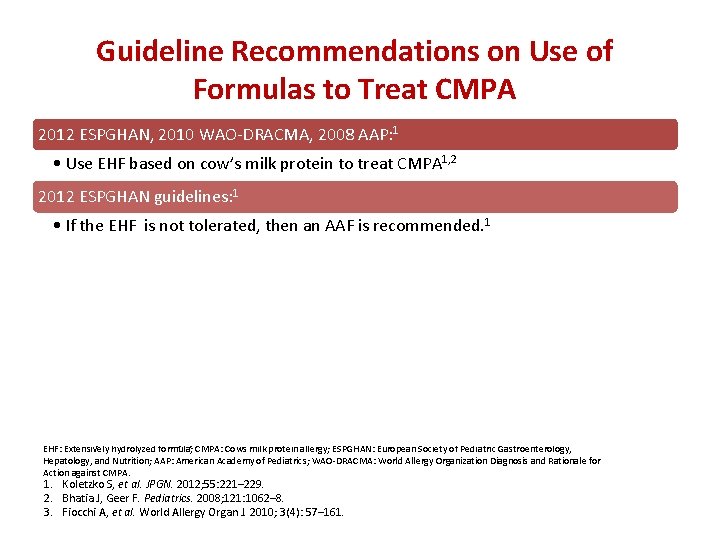
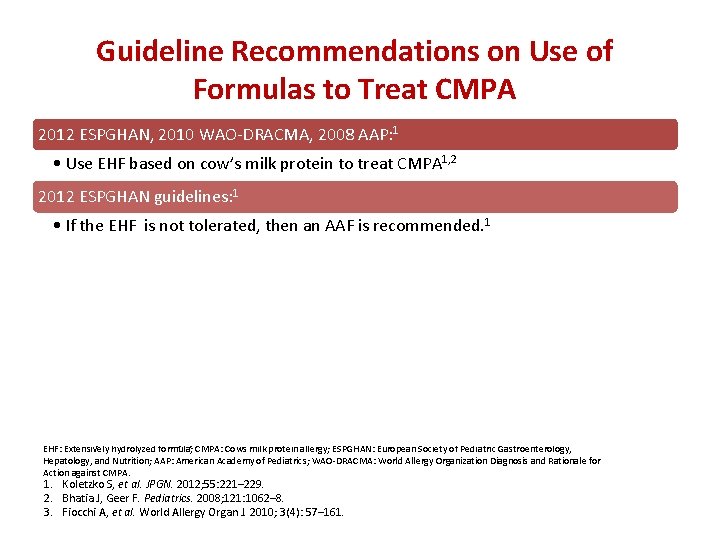
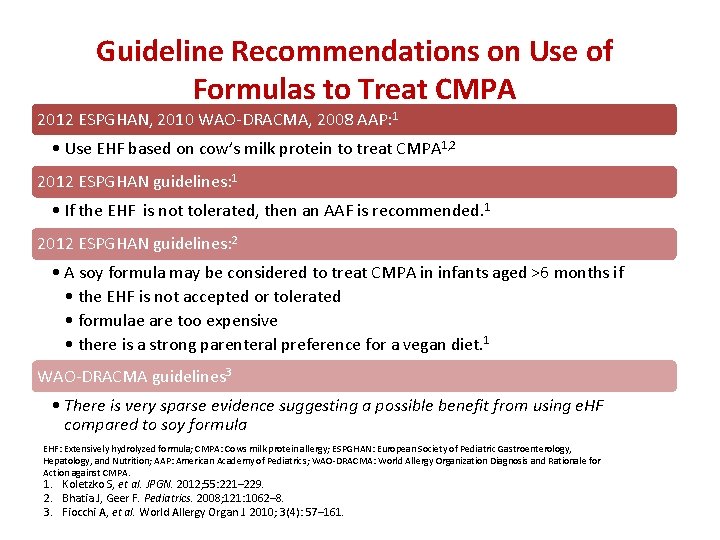
Guideline Recommendations on Use of Formulas to Treat CMPA 2012 ESPGHAN, 2010 WAO-DRACMA, 2008 AAP: 1 • Use EHF based on cow’s milk protein to treat CMPA 1, 2 2012 ESPGHAN guidelines: 1 • If the EHF is not tolerated, then an AAF is recommended. 1 2012 ESPGHAN guidelines: 2 • A soy formula may be considered to treat CMPA in infants aged >6 months if • the EHF is not accepted or tolerated • formulae are too expensive • there is a strong parenteral preference for a vegan diet. 1 WAO-DRACMA guidelines 3 • There is very sparse evidence suggesting a possible benefit from using e. HF compared to soy formula EHF: Extensively hydrolyzed formula; CMPA: Cows milk protein allergy; ESPGHAN: European Society of Pediatric Gastroenterology, Hepatology, and Nutrition; AAP: American Academy of Pediatrics; WAO-DRACMA: World Allergy Organization Diagnosis and Rationale for Action against CMPA. 1. Koletzko S, et al. JPGN. 2012; 55: 221– 229. 2. Bhatia J, Geer F. Pediatrics. 2008; 121: 1062– 8. 3. Fiocchi A, et al. World Allergy Organ J. 2010; 3(4): 57– 161.
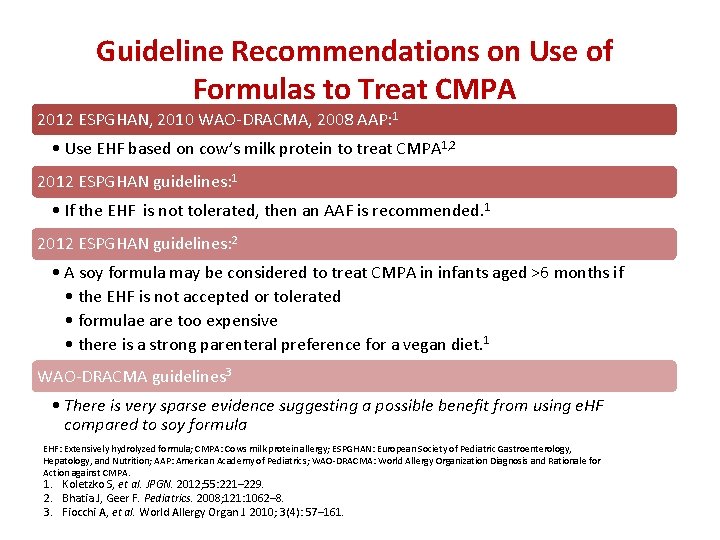
Guideline Recommendations on Use of Formulas to Treat CMPA 2012 ESPGHAN, 2010 WAO-DRACMA, 2008 AAP: 1 • Use EHF based on cow’s milk protein to treat CMPA 1, 2 2012 ESPGHAN guidelines: 1 • If the EHF is not tolerated, then an AAF is recommended. 1 2012 ESPGHAN guidelines: 2 • A soy formula may be considered to treat CMPA in infants aged >6 months if • the EHF is not accepted or tolerated • formulae are too expensive • there is a strong parenteral preference for a vegan diet. 1 WAO-DRACMA guidelines 3 • There is very sparse evidence suggesting a possible benefit from using e. HF compared to soy formula EHF: Extensively hydrolyzed formula; CMPA: Cows milk protein allergy; ESPGHAN: European Society of Pediatric Gastroenterology, Hepatology, and Nutrition; AAP: American Academy of Pediatrics; WAO-DRACMA: World Allergy Organization Diagnosis and Rationale for Action against CMPA. 1. Koletzko S, et al. JPGN. 2012; 55: 221– 229. 2. Bhatia J, Geer F. Pediatrics. 2008; 121: 1062– 8. 3. Fiocchi A, et al. World Allergy Organ J. 2010; 3(4): 57– 161.
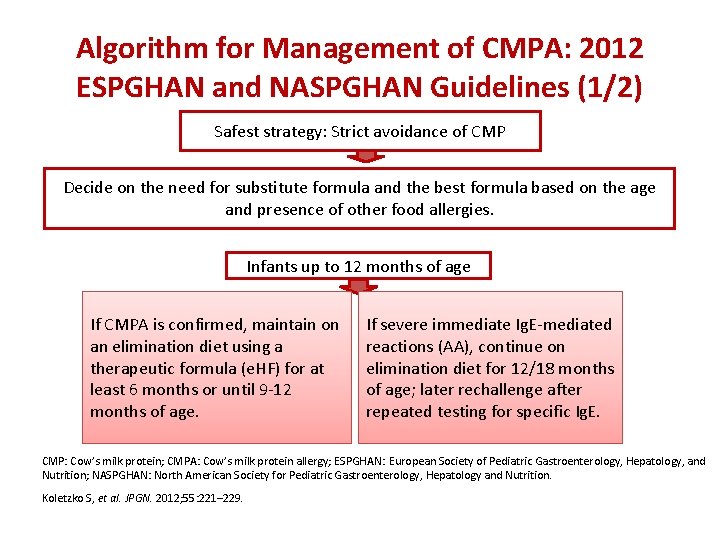
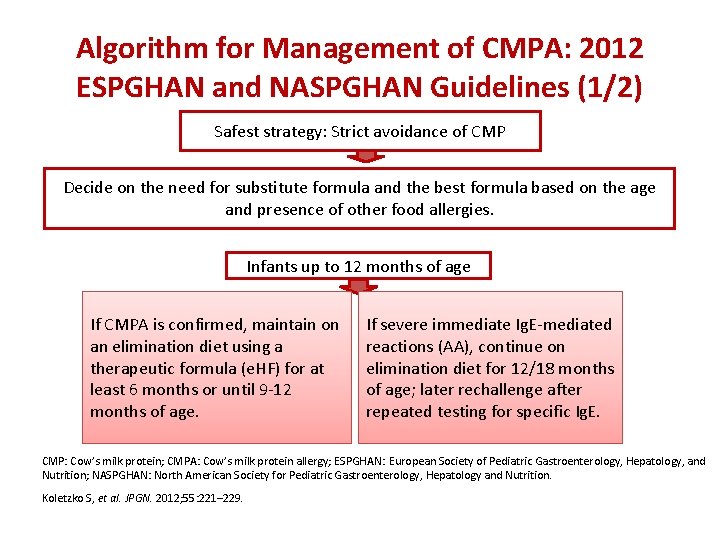
Algorithm for Management of CMPA: 2012 ESPGHAN and NASPGHAN Guidelines (1/2) Safest strategy: Strict avoidance of CMP Decide on the need for substitute formula and the best formula based on the age and presence of other food allergies. Infants up to 12 months of age If CMPA is confirmed, maintain on an elimination diet using a therapeutic formula (e. HF) for at least 6 months or until 9 -12 months of age. If severe immediate Ig. E-mediated reactions (AA), continue on elimination diet for 12/18 months of age; later rechallenge after repeated testing for specific Ig. E. CMP: Cow’s milk protein; CMPA: Cow’s milk protein allergy; ESPGHAN: European Society of Pediatric Gastroenterology, Hepatology, and Nutrition; NASPGHAN: North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. Koletzko S, et al. JPGN. 2012; 55: 221– 229.
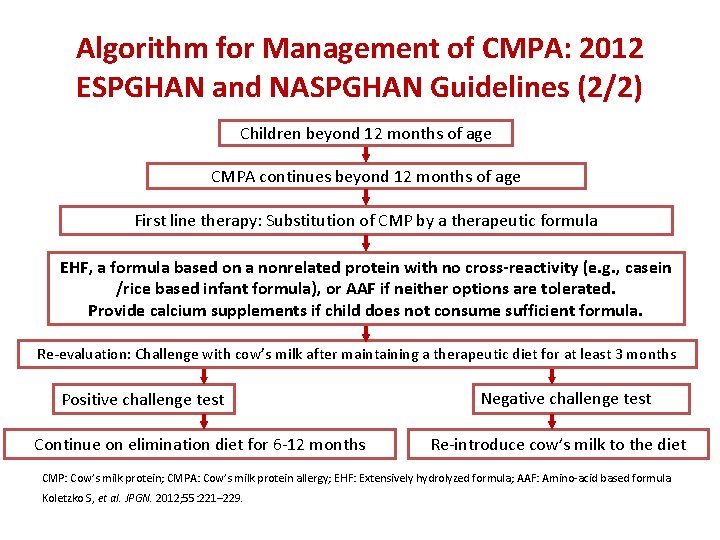
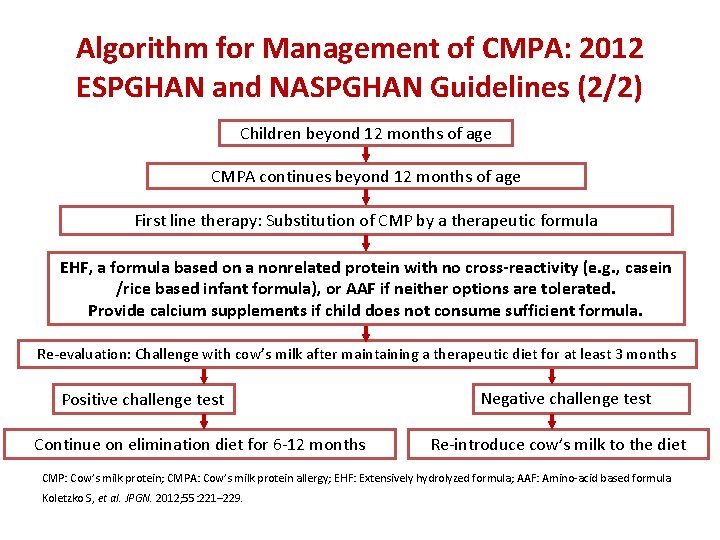
Algorithm for Management of CMPA: 2012 ESPGHAN and NASPGHAN Guidelines (2/2) Children beyond 12 months of age CMPA continues beyond 12 months of age First line therapy: Substitution of CMP by a therapeutic formula EHF, a formula based on a nonrelated protein with no cross-reactivity (e. g. , casein /rice based infant formula), or AAF if neither options are tolerated. Provide calcium supplements if child does not consume sufficient formula. Re-evaluation: Challenge with cow’s milk after maintaining a therapeutic diet for at least 3 months Positive challenge test Continue on elimination diet for 6 -12 months Negative challenge test Re-introduce cow’s milk to the diet CMP: Cow’s milk protein; CMPA: Cow’s milk protein allergy; EHF: Extensively hydrolyzed formula; AAF: Amino-acid based formula. Koletzko S, et al. JPGN. 2012; 55: 221– 229.
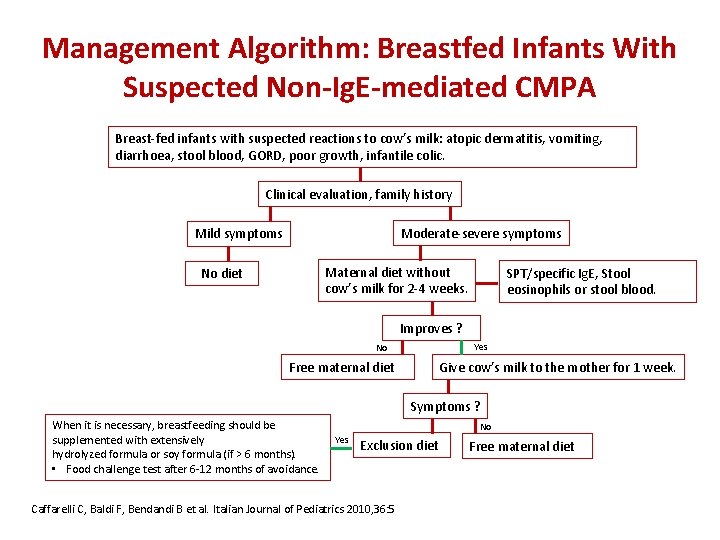
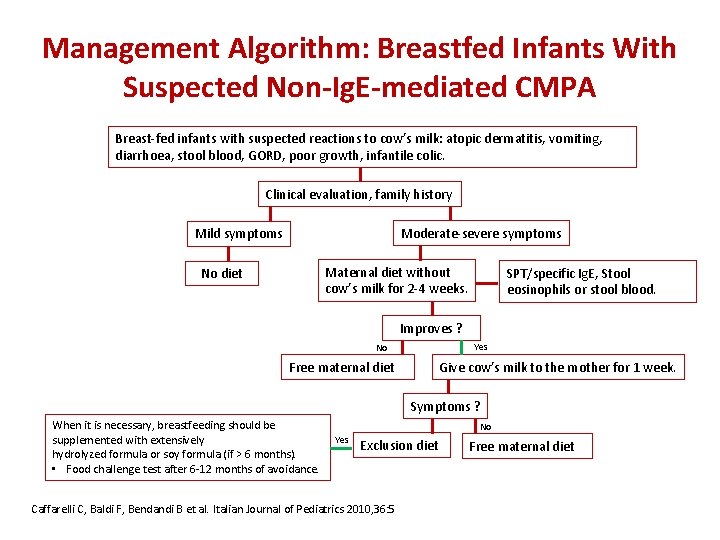
Management Algorithm: Breastfed Infants With Suspected Non-Ig. E-mediated CMPA Breast-fed infants with suspected reactions to cow’s milk: atopic dermatitis, vomiting, diarrhoea, stool blood, GORD, poor growth, infantile colic. Clinical evaluation, family history Moderate-severe symptoms Mild symptoms Maternal diet without cow’s milk for 2 -4 weeks. No diet SPT/specific Ig. E, Stool eosinophils or stool blood. Improves ? Yes No Free maternal diet Give cow’s milk to the mother for 1 week. Symptoms ? When it is necessary, breastfeeding should be supplemented with extensively hydrolyzed formula or soy formula (if > 6 months). • Food challenge test after 6 -12 months of avoidance. No Yes Exclusion diet Caffarelli C, Baldi F, Bendandi B et al. Italian Journal of Pediatrics 2010, 36: 5 Free maternal diet
Is there any way I could have prevented it? (Primary Prevention) • No evidence to restrict dairy avoidance during pregnancy • At risk individuals – Maternal avoidance of dairy products – need more RCT • Evidence of using hydrolyzed formula compared cows milk at high risk individuals – there is lot of evidence
Natural history of FA • Most children with FA will eventually tolerate milk, egg, soy and wheat; far fewer will tolerate tree nuts and peanut. • A higher initial level of Ig. E is associated with a lower rate of resolution of clinical allergy over time • Earlier the age of intolerance, more is the chances of remission
Prognosis – CMPA • Virtually all children manifest in first year • 50 % tolerance by 1 year, 80 % tolerance by 5 years of age. Children with non-Ig. E-mediated CMPI have a good prognosis • 35 % developed allergies to other food • Ig. E mediated allergy may last longer
Protocol in CMPA - nutshell • Dairy free diet for child and mother(if being breastfed) for 4 -8 weeks • If improvement - rechallange with cows milk after 2 months • If symptoms recur, confirms diagnosis. Rechallange after 1 year of age or after 6 mths of the reaction.
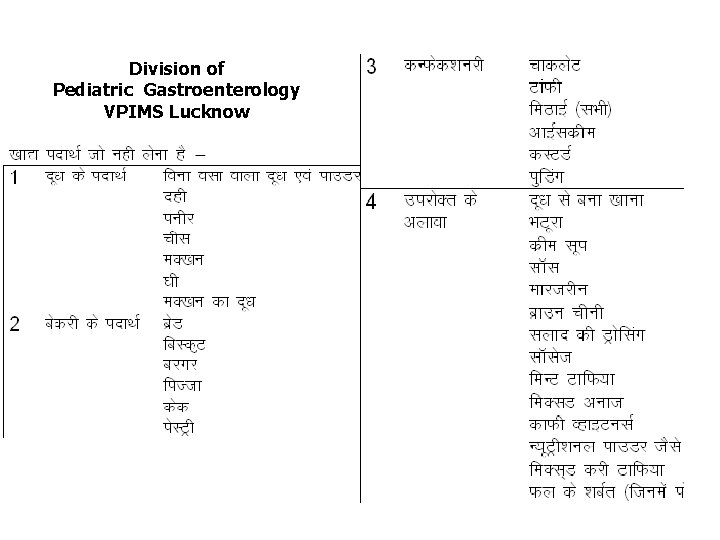
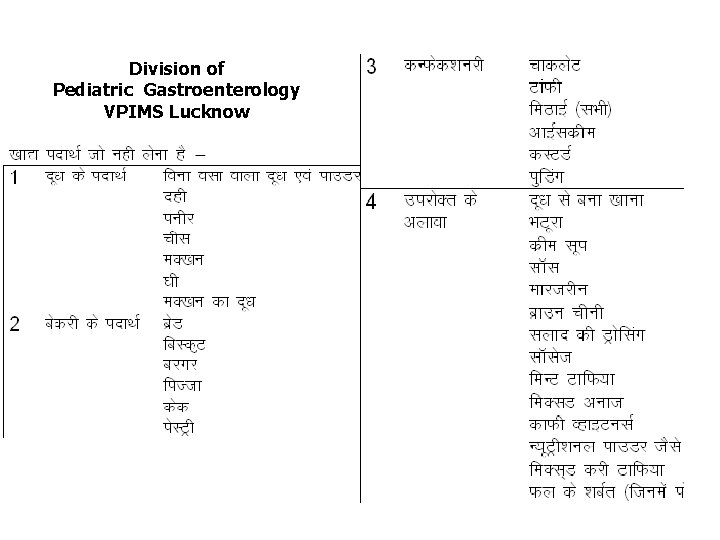
Division of Pediatric Gastroenterology VPIMS Lucknow
Summary Cow’ s milk is the major cause of food allergy in children aged <3 years CMPA may be due to Ig. E- or non-Ig. E-mediated reactions and is the result of impaired oral tolerance For the prevention of allergies, breastfeeding without maternal allergen elimination is recommended as long as the infant is devoid of symptoms Clinical assessment with the elimination diet and challenge within four weeks are fundamental strategies for the accurate diagnosis of CMPA Continued breastfeeding is the best treatment for CMPA and the mother should avoid all dairy products in her diet e. HF based on cow’s milk protein or AAF is a better choice over soy protein-based formula AAF: Amino acid formula; CMPA: Cow milk protein allergy; p. HF: Partially hydrolyzed formula; e. HF: Extensively hydrolyzed formula; Ig. E: Immunoglobulin E
 Milk yield and composition in dairy cows ppt
Milk yield and composition in dairy cows ppt Sensory evaluation of milk and milk products
Sensory evaluation of milk and milk products Milk for toddlers with milk allergynon dairy
Milk for toddlers with milk allergynon dairy Human milk vs cow milk
Human milk vs cow milk Contamination of milk and milk products
Contamination of milk and milk products Difference between cow milk and human milk
Difference between cow milk and human milk Disaccharide found in milk and milk products
Disaccharide found in milk and milk products Protein in buffalo milk
Protein in buffalo milk Protein pump vs protein channel
Protein pump vs protein channel Protein-protein docking
Protein-protein docking Paved road vs unpaved road
Paved road vs unpaved road You have 2 cows
You have 2 cows Romberg rest
Romberg rest Cows flowsheet
Cows flowsheet Nystagmus cows
Nystagmus cows Hawk d'onofrio
Hawk d'onofrio Cow give
Cow give Bull reproductive system parts and functions
Bull reproductive system parts and functions Tale of two cows
Tale of two cows Every good boy does fine all cows eat grass
Every good boy does fine all cows eat grass What is codominance
What is codominance Click clack reading glasses
Click clack reading glasses Parts of a cows stomach
Parts of a cows stomach Casting of cattle
Casting of cattle Two cows theory
Two cows theory Jamaica hope
Jamaica hope Drsabcd worksheet
Drsabcd worksheet How do cows grow
How do cows grow Cow eye retina
Cow eye retina Cows near an electric fence einstein
Cows near an electric fence einstein Political ideologies cows
Political ideologies cows Cows
Cows You have two cows
You have two cows Cows scoring
Cows scoring Polyinheritance
Polyinheritance Cows are omnivores
Cows are omnivores Narayana's cows sequence
Narayana's cows sequence Dr adam fox allergy
Dr adam fox allergy Surgical prep guidelines
Surgical prep guidelines Latex allergy
Latex allergy ü latex
ü latex Allergy wise
Allergy wise Ounces of ice cream in a large milkshake
Ounces of ice cream in a large milkshake Fruit latex allergy
Fruit latex allergy Macaulay allergy
Macaulay allergy Allergic rhinitis treatment guidelines
Allergic rhinitis treatment guidelines Allergy shiners
Allergy shiners Allergic rhinitis treatment guidelines
Allergic rhinitis treatment guidelines Allergy
Allergy Allergy
Allergy Allergy
Allergy Icd 10 code for seasonal allergic rhinitis
Icd 10 code for seasonal allergic rhinitis Allergy rates
Allergy rates Rhinitis allergy
Rhinitis allergy Allergy board review course
Allergy board review course Rhinitis allergy
Rhinitis allergy Allergy
Allergy Acr contrast reaction card
Acr contrast reaction card Hypersensitivity
Hypersensitivity Penicillin allergy cme
Penicillin allergy cme World allergy organ j
World allergy organ j Keva immunorich
Keva immunorich Maia brewerton
Maia brewerton Food information for consumers regulation
Food information for consumers regulation Capers allergy
Capers allergy American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 Allergy asthma immunol res impact factor
Allergy asthma immunol res impact factor