Update Training on CIWA and COWS Clinical Institute
- Slides: 17
Update Training on CIWA and COWS
Clinical Institute Withdrawal Assessment of Alcohol Scale, Revised (CIWA-Ar) © 2008 Rush University Medical Center
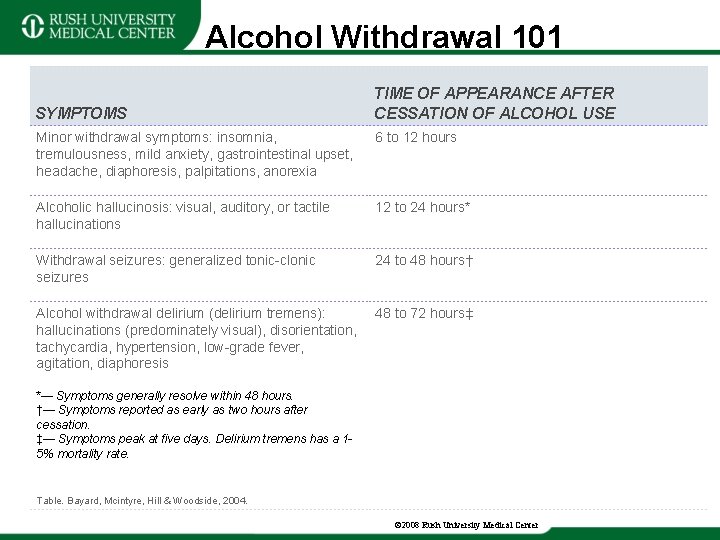
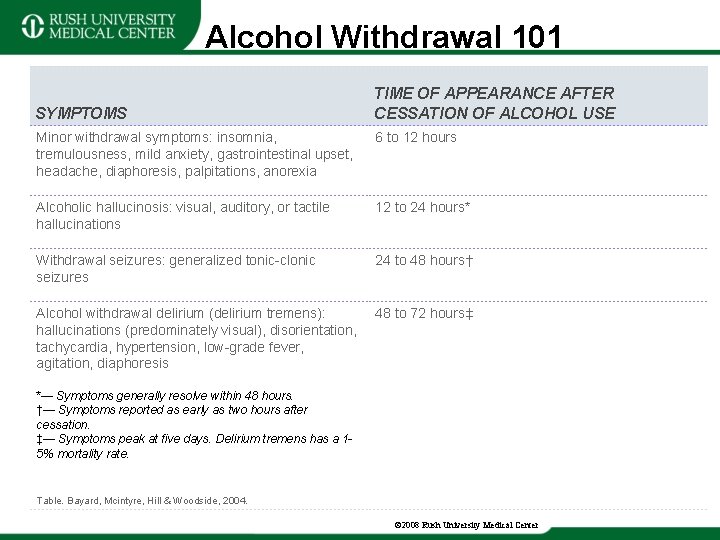
Alcohol Withdrawal 101 SYMPTOMS TIME OF APPEARANCE AFTER CESSATION OF ALCOHOL USE Minor withdrawal symptoms: insomnia, tremulousness, mild anxiety, gastrointestinal upset, headache, diaphoresis, palpitations, anorexia 6 to 12 hours Alcoholic hallucinosis: visual, auditory, or tactile hallucinations 12 to 24 hours* Withdrawal seizures: generalized tonic-clonic seizures 24 to 48 hours† Alcohol withdrawal delirium (delirium tremens): hallucinations (predominately visual), disorientation, tachycardia, hypertension, low-grade fever, agitation, diaphoresis 48 to 72 hours‡ *— Symptoms generally resolve within 48 hours. †— Symptoms reported as early as two hours after cessation. ‡— Symptoms peak at five days. Delirium tremens has a 15% mortality rate. Table. Bayard, Mcintyre, Hill & Woodside, 2004. © 2008 Rush University Medical Center
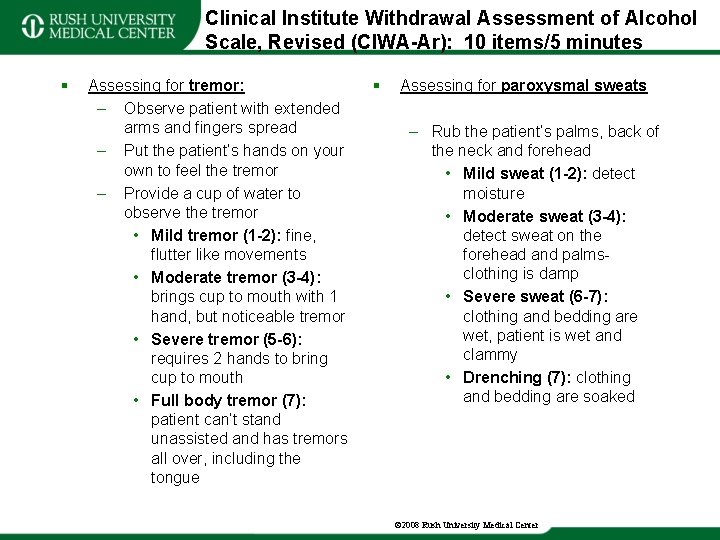
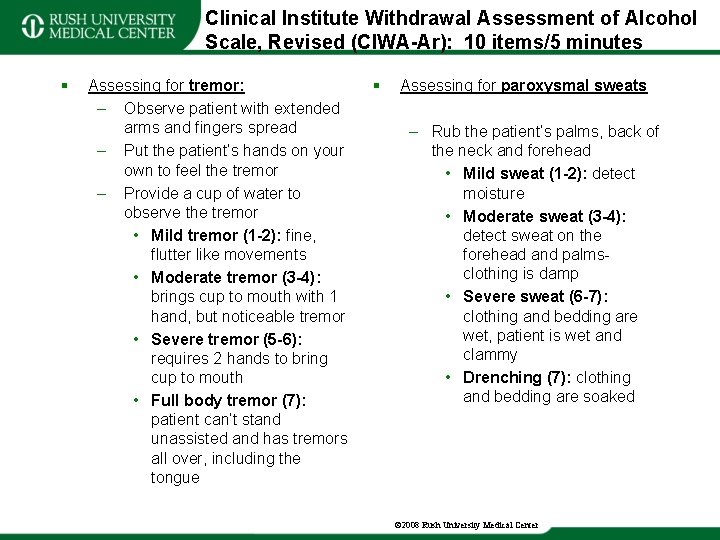
Clinical Institute Withdrawal Assessment of Alcohol Scale, Revised (CIWA-Ar): 10 items/5 minutes § Assessing for tremor: – Observe patient with extended arms and fingers spread – Put the patient’s hands on your own to feel the tremor – Provide a cup of water to observe the tremor • Mild tremor (1 -2): fine, flutter like movements • Moderate tremor (3 -4): brings cup to mouth with 1 hand, but noticeable tremor • Severe tremor (5 -6): requires 2 hands to bring cup to mouth • Full body tremor (7): patient can’t stand unassisted and has tremors all over, including the tongue § Assessing for paroxysmal sweats – Rub the patient’s palms, back of the neck and forehead • Mild sweat (1 -2): detect moisture • Moderate sweat (3 -4): detect sweat on the forehead and palms- clothing is damp • Severe sweat (6 -7): clothing and bedding are wet, patient is wet and clammy • Drenching (7): clothing and bedding are soaked © 2008 Rush University Medical Center
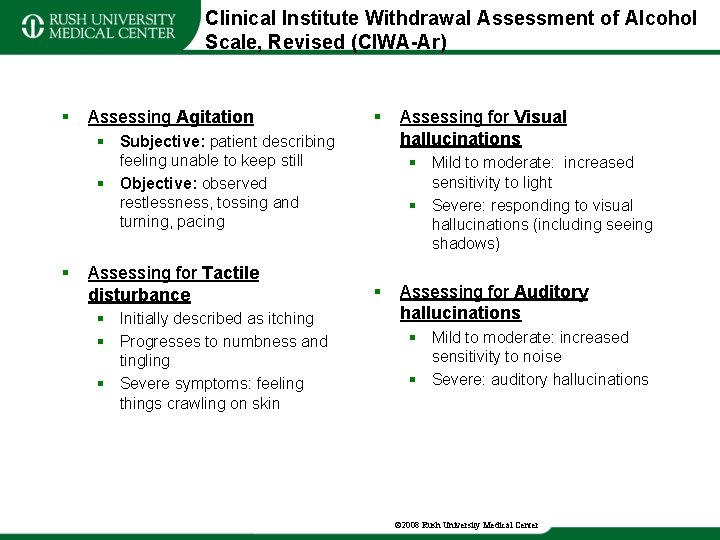
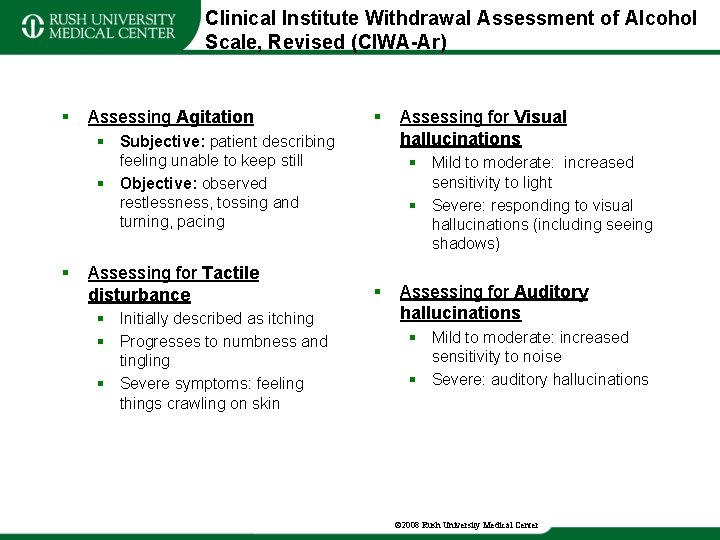
Clinical Institute Withdrawal Assessment of Alcohol Scale, Revised (CIWA-Ar) § Assessing Agitation § § Subjective: patient describing feeling unable to keep still § Objective: observed restlessness, tossing and turning, pacing § Assessing for Tactile disturbance § Initially described as itching § Progresses to numbness and tingling § Severe symptoms: feeling things crawling on skin Assessing for Visual hallucinations § Mild to moderate: increased sensitivity to light § Severe: responding to visual hallucinations (including seeing shadows) § Assessing for Auditory hallucinations § Mild to moderate: increased sensitivity to noise § Severe: auditory hallucinations © 2008 Rush University Medical Center
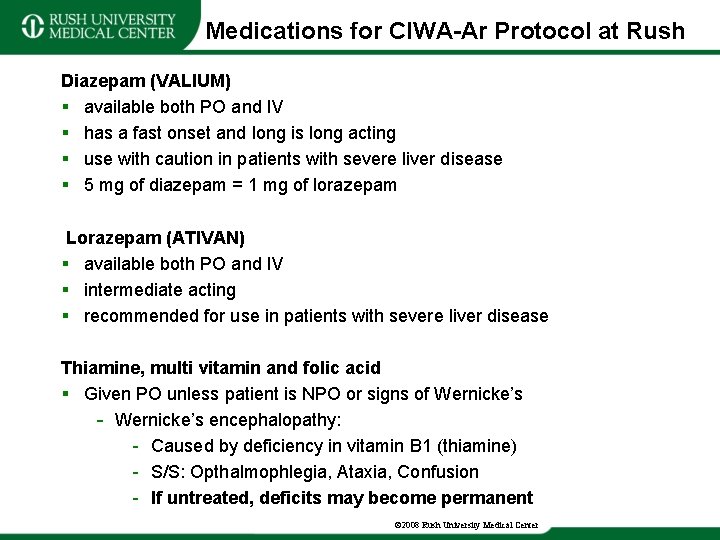
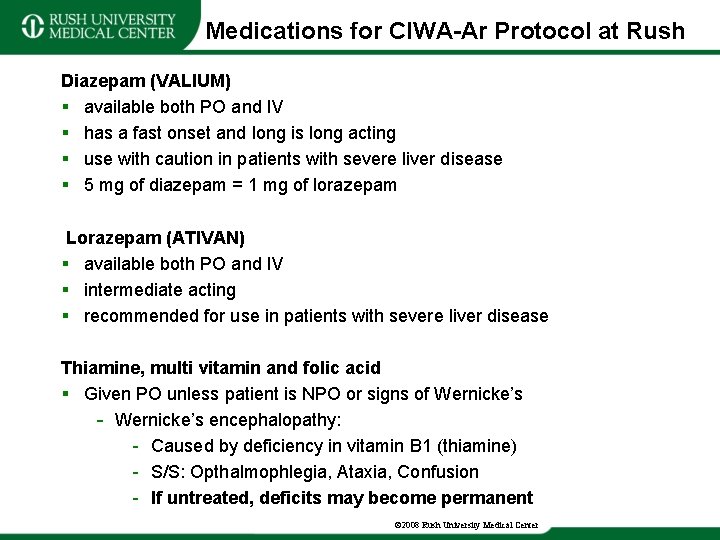
Medications for CIWA-Ar Protocol at Rush Diazepam (VALIUM) § available both PO and IV § has a fast onset and long is long acting § use with caution in patients with severe liver disease § 5 mg of diazepam = 1 mg of lorazepam Lorazepam (ATIVAN) § available both PO and IV § intermediate acting § recommended for use in patients with severe liver disease Thiamine, multi vitamin and folic acid § Given PO unless patient is NPO or signs of Wernicke’s - Wernicke’s encephalopathy: - Caused by deficiency in vitamin B 1 (thiamine) - S/S: Opthalmophlegia, Ataxia, Confusion - If untreated, deficits may become permanent © 2008 Rush University Medical Center
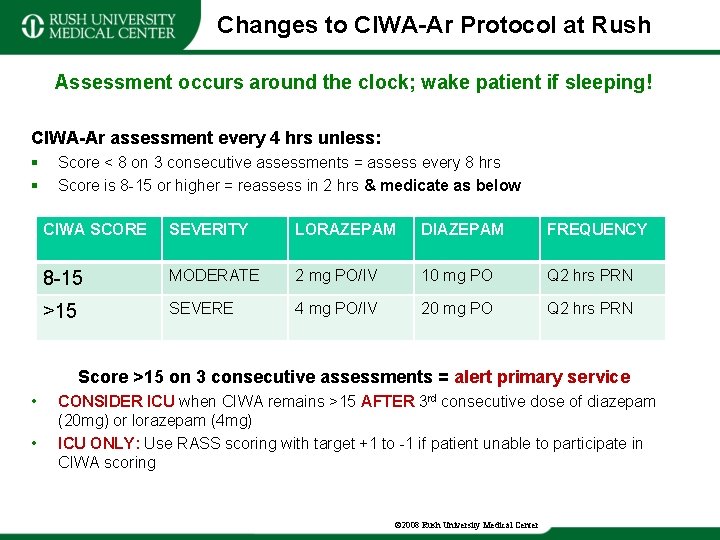
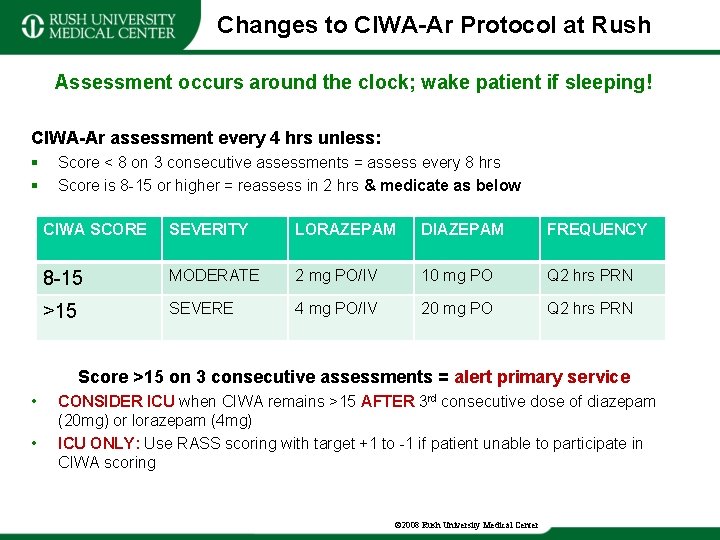
Changes to CIWA-Ar Protocol at Rush Assessment occurs around the clock; wake patient if sleeping! CIWA-Ar assessment every 4 hrs unless: § § Score < 8 on 3 consecutive assessments = assess every 8 hrs Score is 8 -15 or higher = reassess in 2 hrs & medicate as below CIWA SCORE SEVERITY LORAZEPAM DIAZEPAM FREQUENCY 8 -15 MODERATE 2 mg PO/IV 10 mg PO Q 2 hrs PRN >15 SEVERE 4 mg PO/IV 20 mg PO Q 2 hrs PRN Score >15 on 3 consecutive assessments = alert primary service • • CONSIDER ICU when CIWA remains >15 AFTER 3 rd consecutive dose of diazepam (20 mg) or lorazepam (4 mg) ICU ONLY: Use RASS scoring with target +1 to -1 if patient unable to participate in CIWA scoring © 2008 Rush University Medical Center
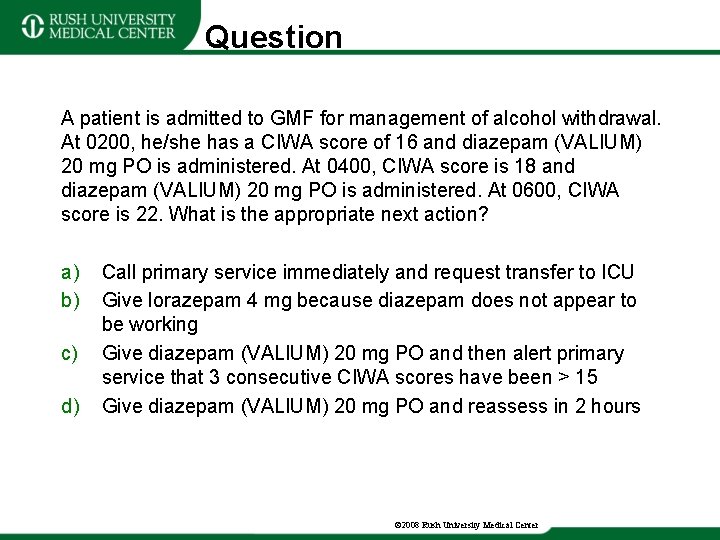
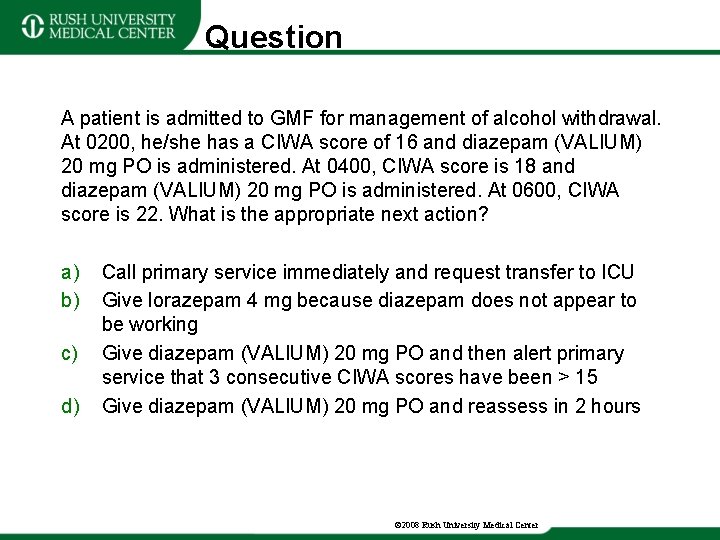
Question A patient is admitted to GMF for management of alcohol withdrawal. At 0200, he/she has a CIWA score of 16 and diazepam (VALIUM) 20 mg PO is administered. At 0400, CIWA score is 18 and diazepam (VALIUM) 20 mg PO is administered. At 0600, CIWA score is 22. What is the appropriate next action? a) b) c) d) Call primary service immediately and request transfer to ICU Give lorazepam 4 mg because diazepam does not appear to be working Give diazepam (VALIUM) 20 mg PO and then alert primary service that 3 consecutive CIWA scores have been > 15 Give diazepam (VALIUM) 20 mg PO and reassess in 2 hours © 2008 Rush University Medical Center
Clinical Opioid Withdrawal Scale (COWS) © 2008 Rush University Medical Center
Opioid Withdrawal 101 Onset of symptoms: – Heroin: begins within hours of last use & diminish by day 4 – Methadone: begins within days and diminish by day 10 – Prescription opioids: varies based on ½ life of opioid © 2008 Rush University Medical Center
Clinical Opioid Withdrawal Scale COWS – Previously referred to as the “CIWA Opioids Scale” – 2 - 10 minute to complete including observation and scoring © 2008 Rush University Medical Center
Clinical Opioid Withdrawal Scale § Items to assess: § Resting Pulse Rate § Recorded after the patient has been sitting or lying for 1 minute. § Sweating § Over the past ½ hour § Observation and patient report § Restlessness § If sitting still without obvious restlessness, ask “are you having difficulty sitting still? ” § Range from subjective report to clear observation of frequent movement § Pupil size § Observed in room light § Turn on the lights in the room for assessment and allow for adjustment § Bone or joint aches § Make a baseline assessment of pain (i. e does the patient have any chronic pain issues) § The assessment is based only on additional pain, outside of their baseline © 2008 Rush University Medical Center
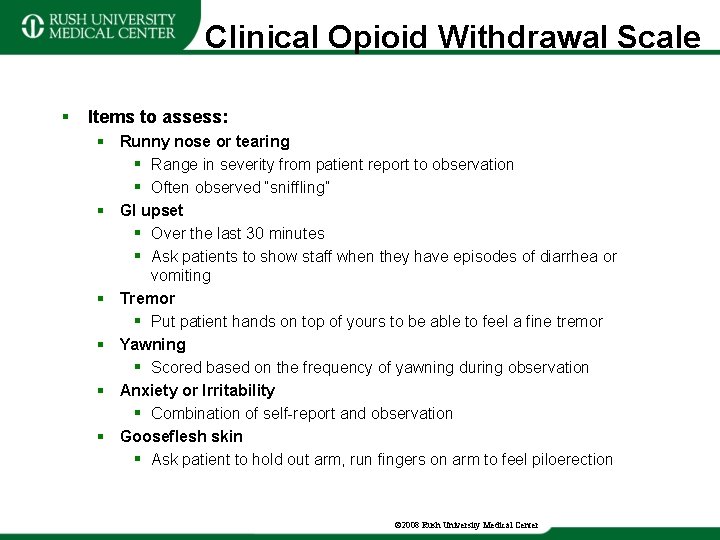
Clinical Opioid Withdrawal Scale § Items to assess: § Runny nose or tearing § Range in severity from patient report to observation § Often observed “sniffling” § GI upset § Over the last 30 minutes § Ask patients to show staff when they have episodes of diarrhea or vomiting § Tremor § Put patient hands on top of yours to be able to feel a fine tremor § Yawning § Scored based on the frequency of yawning during observation § Anxiety or Irritability § Combination of self-report and observation § Gooseflesh skin § Ask patient to hold out arm, run fingers on arm to feel piloerection © 2008 Rush University Medical Center
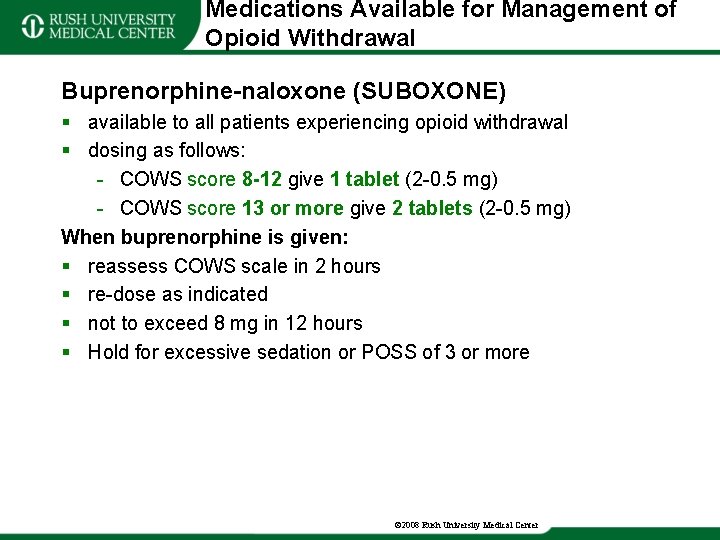
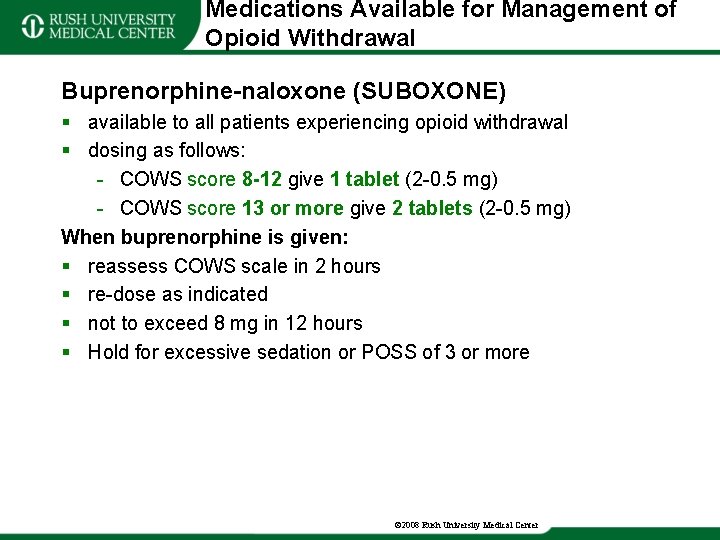
Medications Available for Management of Opioid Withdrawal Buprenorphine-naloxone (SUBOXONE) § available to all patients experiencing opioid withdrawal § dosing as follows: - COWS score 8 -12 give 1 tablet (2 -0. 5 mg) - COWS score 13 or more give 2 tablets (2 -0. 5 mg) When buprenorphine is given: § reassess COWS scale in 2 hours § re-dose as indicated § not to exceed 8 mg in 12 hours § Hold for excessive sedation or POSS of 3 or more © 2008 Rush University Medical Center
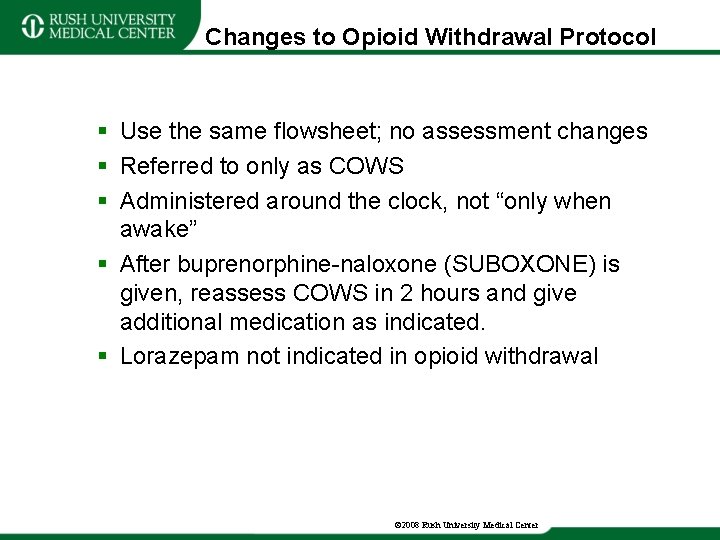
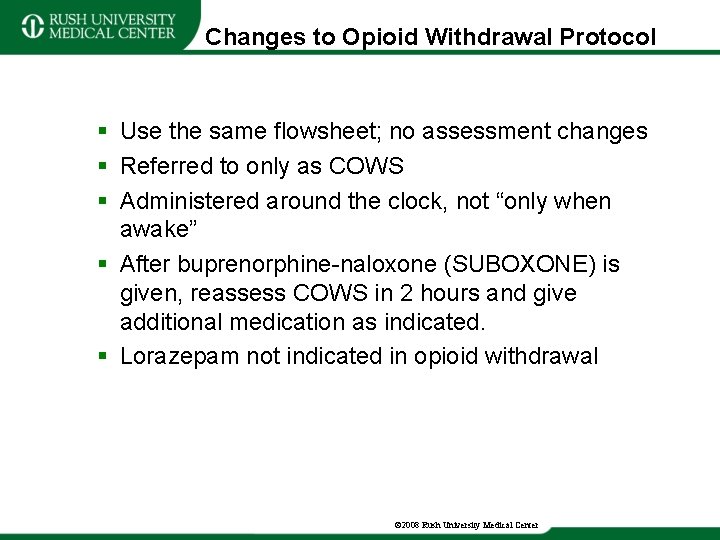
Changes to Opioid Withdrawal Protocol § Use the same flowsheet; no assessment changes § Referred to only as COWS § Administered around the clock, not “only when awake” § After buprenorphine-naloxone (SUBOXONE) is given, reassess COWS in 2 hours and give additional medication as indicated. § Lorazepam not indicated in opioid withdrawal © 2008 Rush University Medical Center
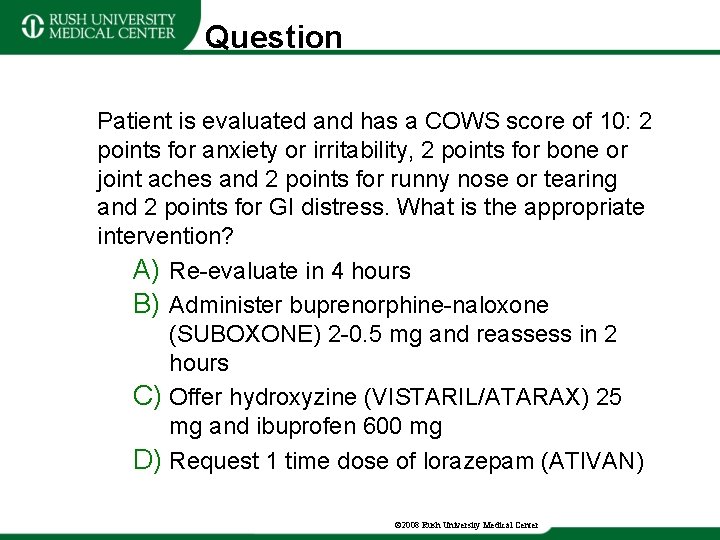
Question Patient is evaluated and has a COWS score of 10: 2 points for anxiety or irritability, 2 points for bone or joint aches and 2 points for runny nose or tearing and 2 points for GI distress. What is the appropriate intervention? A) Re-evaluate in 4 hours B) Administer buprenorphine-naloxone (SUBOXONE) 2 -0. 5 mg and reassess in 2 hours C) Offer hydroxyzine (VISTARIL/ATARAX) 25 mg and ibuprofen 600 mg D) Request 1 time dose of lorazepam (ATIVAN) © 2008 Rush University Medical Center
References • Bayard, M. , Mcintyre, J. , Hill, K. R. , & Woodside, J. Jr. (2004). Alcohol withdrawal syndrome. Am Fam Physician, 69(3), 1443 -1450. • Center for Substance Abuse Treatment. Detoxification and Substance Abuse Treatment Improvement Protocol (TIP) Series, No. 45. HHS Publication No. (SMA) 15 -4131. Rockville, MD: Center for Substance Abuse Treatment, 2006 • Hurst, G. B. (2012). Caring for patients in alcohol withdrawal. ) American Nurse Today, 7(6). Retrieved from https: //www. americannursetoday. com/caring-for-patients-in-alcoholwithdrawal/ • Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. (1989). Assessment of alcohol withdrawal: the revised Clinical Institute Withdrawal Assessment for alcohol scale (CIWA-Ar). Br J Addict, 84(11), 1353 -1357. • Wesson D. R. & Ling, W. (2003). The Clinical Opiate Withdrawal Scale [COWS]. J Psychoactive Drugs, 35(2), 253 -259. © 2008 Rush University Medical Center