COMPLICATED SKIN AND SKIN STRUCTURE INFECTIONS DR HUSAIN











- Slides: 70
COMPLICATED SKIN AND SKIN STRUCTURE INFECTIONS DR HUSAIN ALAWADHI Consultant Intensivist Department of Medicine King Faisal Specialist Hospital and Research Centre Riyadh, Saudi Arabia

PART ONE
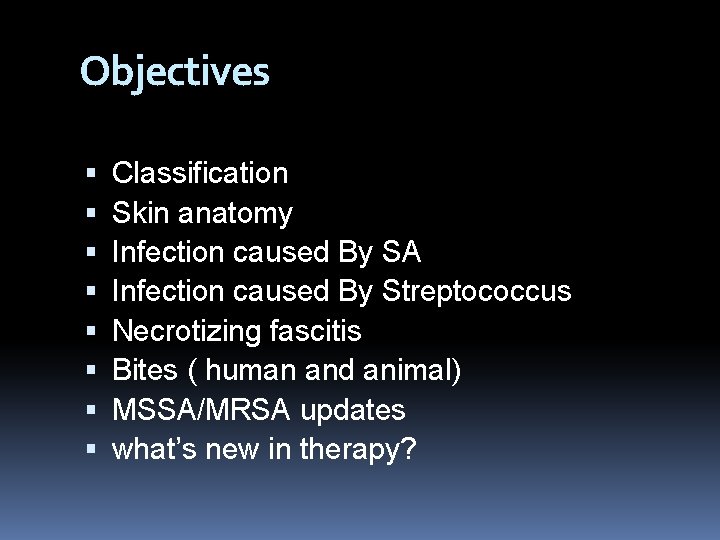
Objectives Classification Skin anatomy Infection caused By SA Infection caused By Streptococcus Necrotizing fascitis Bites ( human and animal) MSSA/MRSA updates what’s new in therapy?
CID, 2005, 41: 1373 -1406
What is Localized skin infection? Localized SSSIs include lesions such as furuncles, carbuncles, and abscesses, which would generally be treated by incision and debridement with drainage.
When to consider it complicated ? Surrounding cellulitis, immunocompromised, or the presence of potentially infectable prostheses, such as cardiac valves, orthopedic devises or vascular grafts, mandates antibiotic use and might well mean that the infection would be classed as complicated
In particular, there a number of underlying comorbidities that should be sought and excluded as being particularly relevant to the patient with an SSSI. Diabetes Vascular insufficiency in the area of the infection Chronic renal or hepatic disease Potentially infectable prostheses Immunosuppression Debilitation or advanced age Recent antimicrobial therapy Recent surgery; and Recent hospitalization
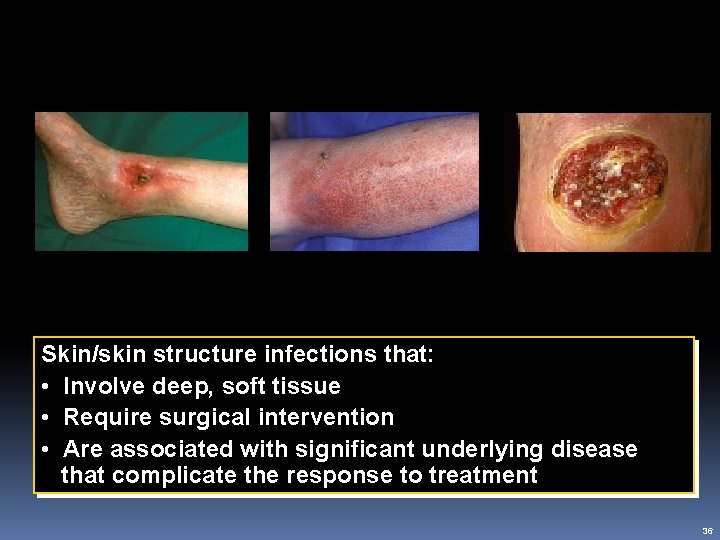
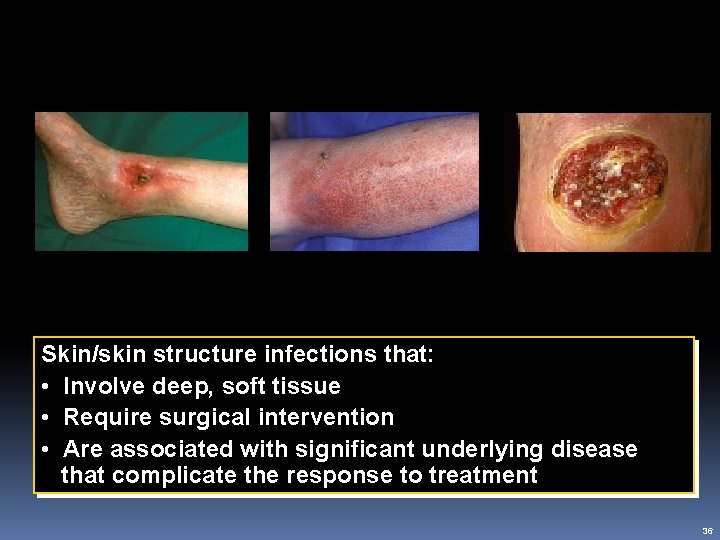
c. SSSI Definition Abscess Cellulitis Ulcer Skin/skin structure infections that: • Involve deep, soft tissue • Require surgical intervention • Are associated with significant underlying disease that complicate the response to treatment 36
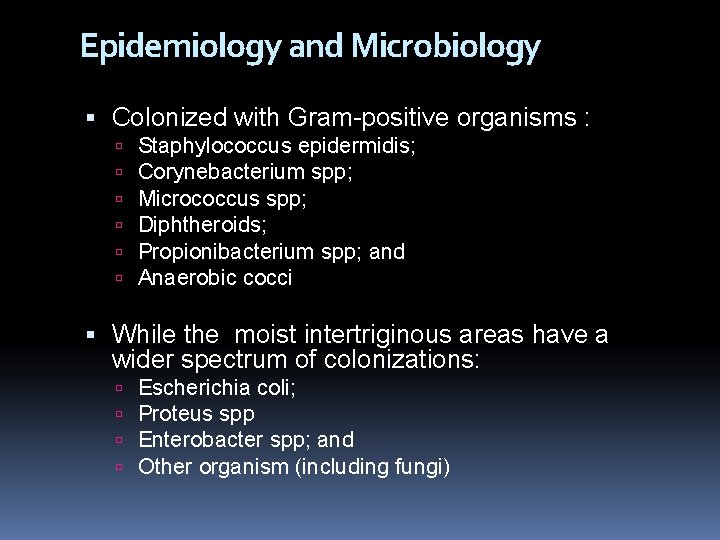
Epidemiology and Microbiology Colonized with Gram-positive organisms : Staphylococcus epidermidis; Corynebacterium spp; Micrococcus spp; Diphtheroids; Propionibacterium spp; and Anaerobic cocci While the moist intertriginous areas have a wider spectrum of colonizations: Escherichia coli; Proteus spp Enterobacter spp; and Other organism (including fungi)
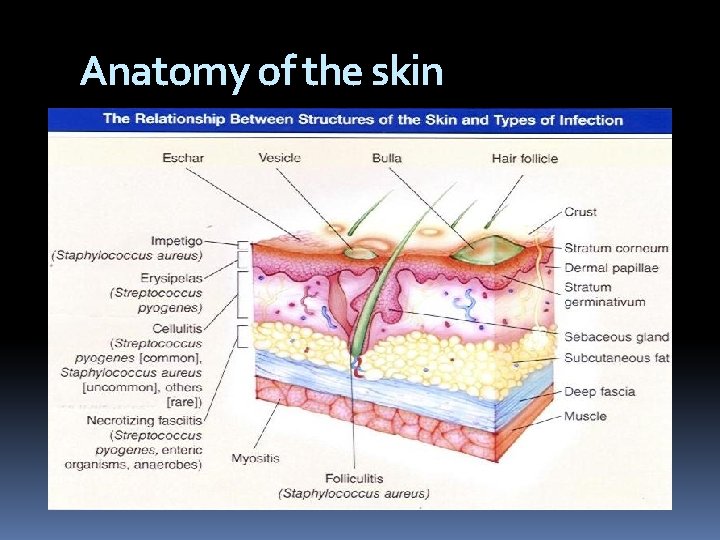
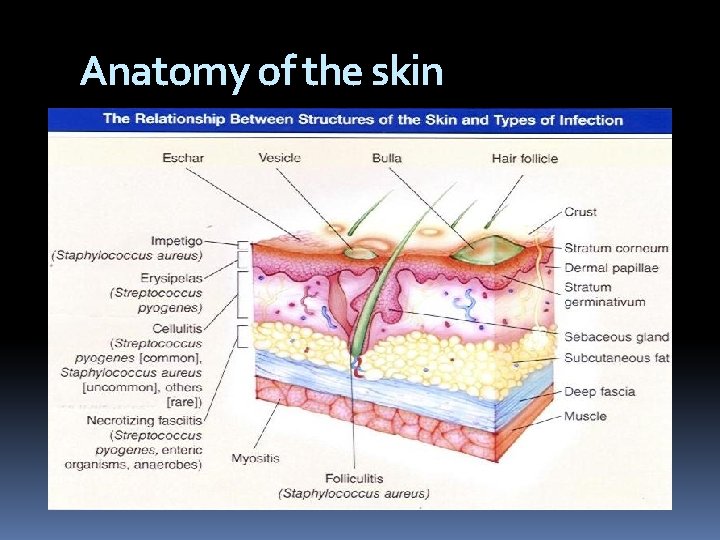
Anatomy of the skin
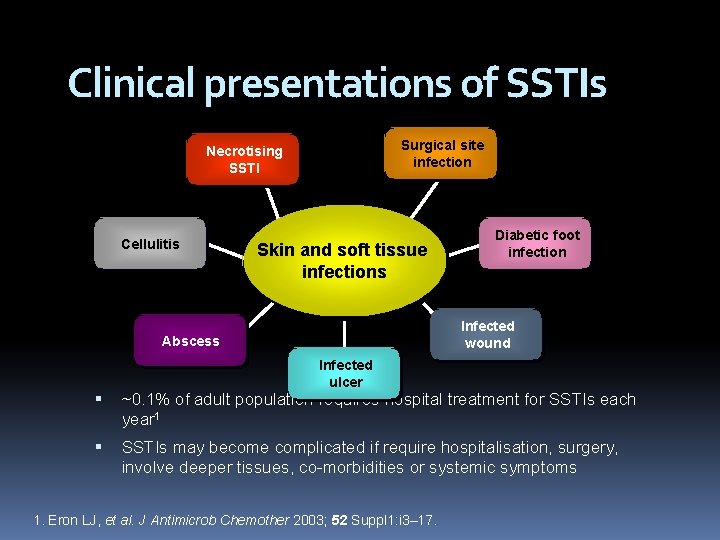
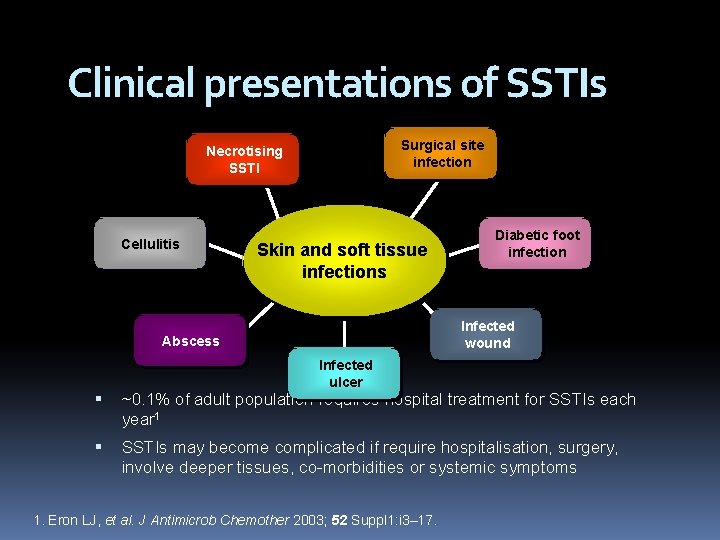
Clinical presentations of SSTIs Surgical site infection Necrotising SSTI Cellulitis Skin and soft tissue infections Diabetic foot infection Infected wound Abscess Infected ulcer ~0. 1% of adult population requires hospital treatment for SSTIs each year 1 SSTIs may become complicated if require hospitalisation, surgery, involve deeper tissues, co-morbidities or systemic symptoms 1. Eron LJ, et al. J Antimicrob Chemother 2003; 52 Suppl 1: i 3– 17.
What are the four main organisms? FIRST : S. aureus Is the commonest Two potent and clinically relevant exotoxins from S. aureus are the enterotoxins (responsible for food poisoning) and toxic shock syndrome toxin (TSST-1)
SECOND : Group A streptococci ( GAS) (S. pyogenes), much like S. aureus can produce a variety of virulence factors. Group A streptococci secrete an array of soluble exotoxins some of which are extremely potent causing systemic toxicity known as streptococcal toxic shock syndrome 9 STSS) and necrotizing fascitis. THIRD : Clostridium perfringens is the most frequently isolated, although isolates of C. septicum, C. histolyticum, C. bifermentans, and C. novyii can be equally pathogenics.

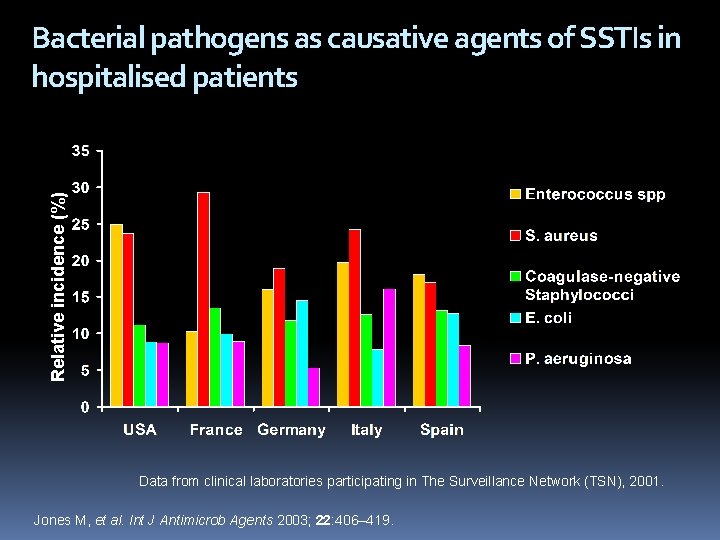
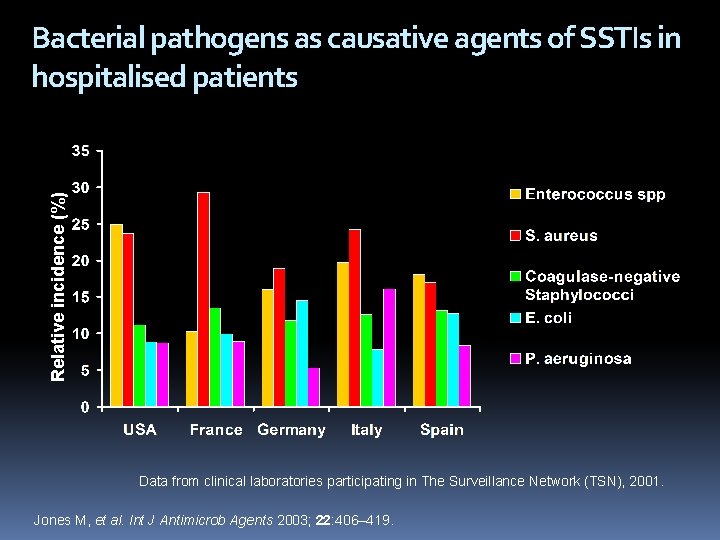
Relative incidence (%) Bacterial pathogens as causative agents of SSTIs in hospitalised patients Data from clinical laboratories participating in The Surveillance Network (TSN), 2001. Jones M, et al. Int J Antimicrob Agents 2003; 22: 406– 419.
What sort of skin structure infections are usually caused by staphylococci? It is often helpful to remember that localized SSSIs above the belt are more likely to be caused by S. aureus than those below the belt, belt which are more likely to be associated with mixed flora Furunculosis Cellulitis Abscesses
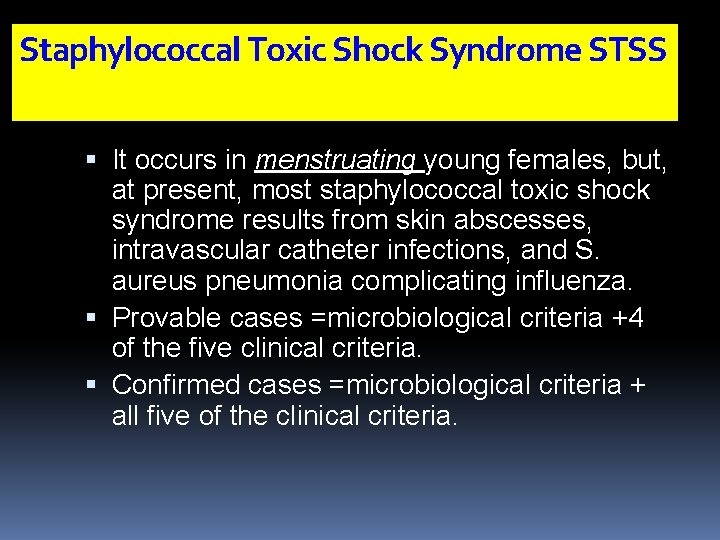
Staphylococcal Toxic Shock Syndrome STSS It occurs in menstruating young females, but, at present, most staphylococcal toxic shock syndrome results from skin abscesses, intravascular catheter infections, and S. aureus pneumonia complicating influenza. Provable cases =microbiological criteria +4 of the five clinical criteria. Confirmed cases =microbiological criteria + all five of the clinical criteria.
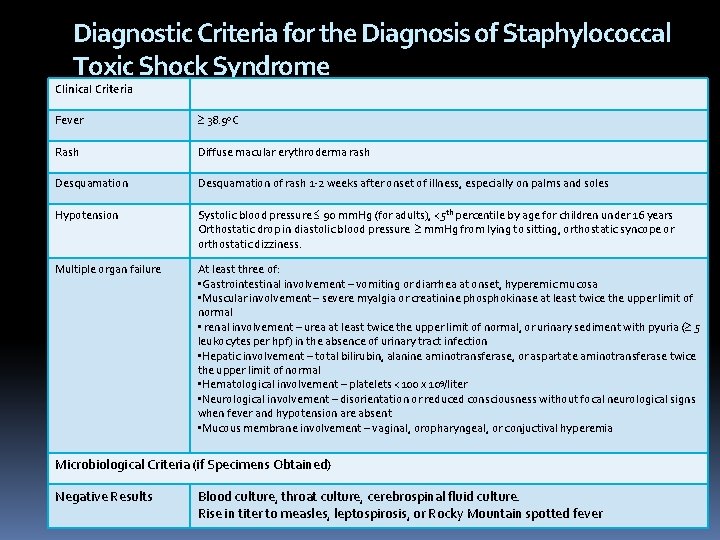
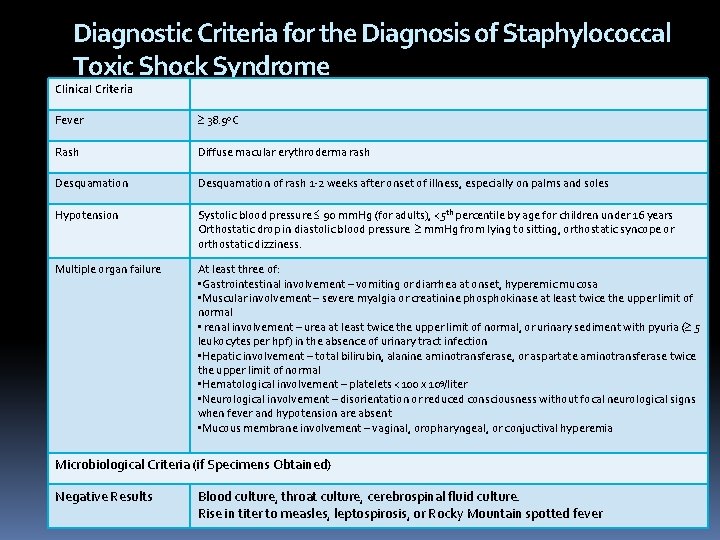
Diagnostic Criteria for the Diagnosis of Staphylococcal Toxic Shock Syndrome Clinical Criteria Fever 38. 9 o. C Rash Diffuse macular erythroderma rash Desquamation of rash 1 -2 weeks after onset of illness, especially on palms and soles Hypotension Systolic blood pressure 90 mm. Hg (for adults), <5 th percentile by age for children under 16 years Orthostatic drop in diastolic blood pressure mm. Hg from lying to sitting, orthostatic syncope or orthostatic dizziness. Multiple organ failure At least three of: • Gastrointestinal involvement – vomiting or diarrhea at onset, hyperemic mucosa • Muscular involvement – severe myalgia or creatinine phosphokinase at least twice the upper limit of normal • renal involvement – urea at least twice the upper limit of normal, or urinary sediment with pyuria ( 5 leukocytes per hpf) in the absence of urinary tract infection • Hepatic involvement – total bilirubin, alanine aminotransferase, or aspartate aminotransferase twice the upper limit of normal • Hematological involvement – platelets <100 x 109/liter • Neurological involvement – disorientation or reduced consciousness without focal neurological signs when fever and hypotension are absent • Mucous membrane involvement – vaginal, oropharyngeal, or conjuctival hyperemia Microbiological Criteria (if Specimens Obtained) Negative Results Blood culture, throat culture, cerebrospinal fluid culture. Rise in titer to measles, leptospirosis, or Rocky Mountain spotted fever
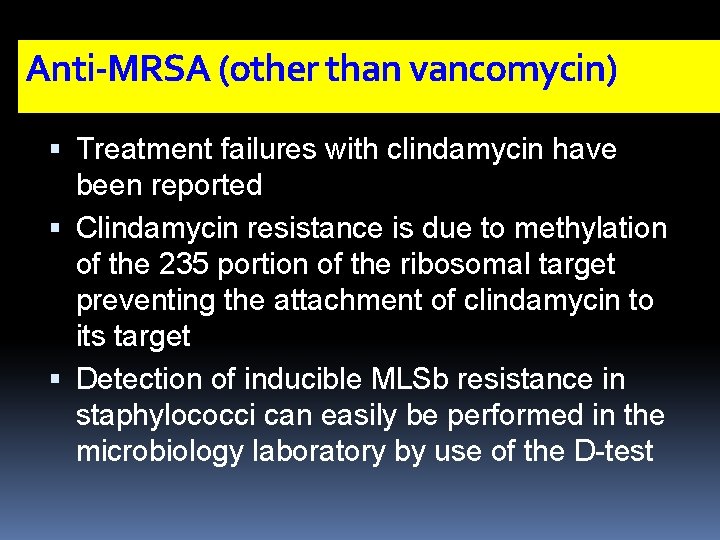
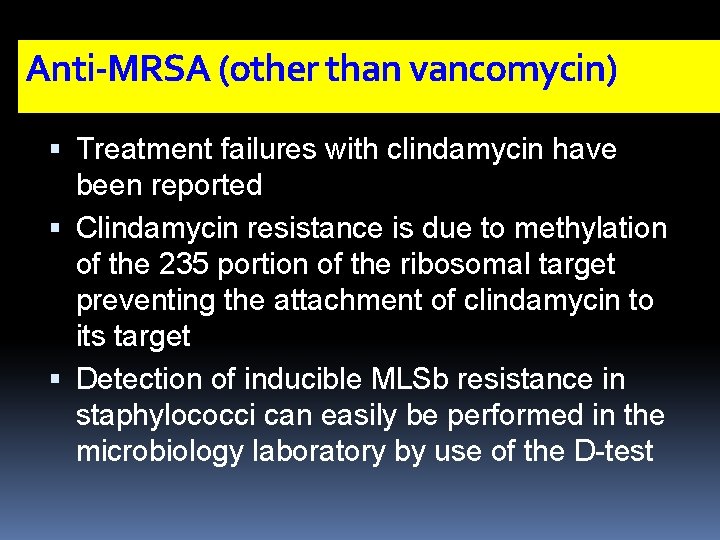
Anti-MRSA (other than vancomycin) Treatment failures with clindamycin have been reported Clindamycin resistance is due to methylation of the 235 portion of the ribosomal target preventing the attachment of clindamycin to its target Detection of inducible MLSb resistance in staphylococci can easily be performed in the microbiology laboratory by use of the D-test
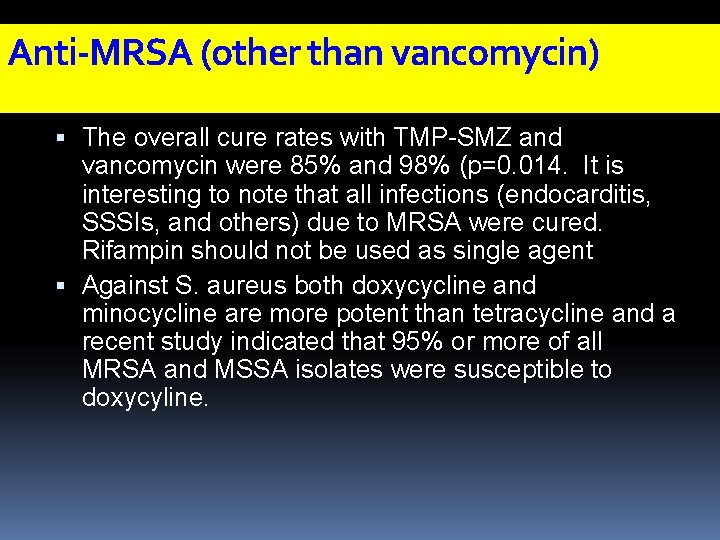
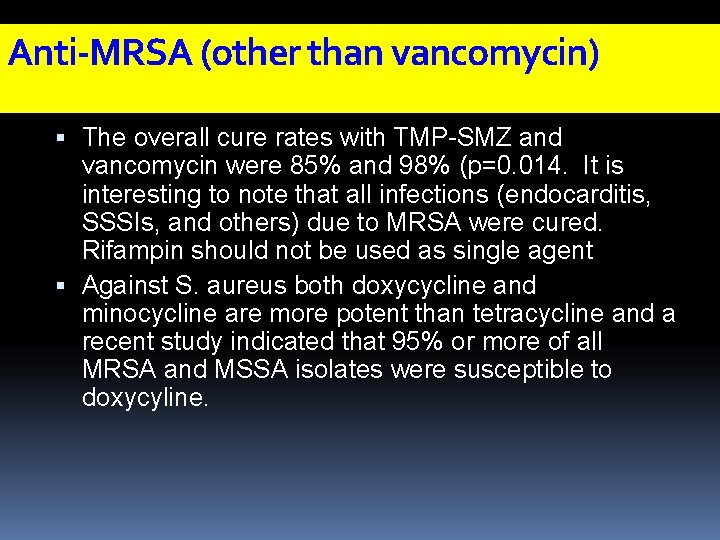
Anti-MRSA (other than vancomycin) The overall cure rates with TMP-SMZ and vancomycin were 85% and 98% (p=0. 014. It is interesting to note that all infections (endocarditis, SSSIs, and others) due to MRSA were cured. Rifampin should not be used as single agent Against S. aureus both doxycycline and minocycline are more potent than tetracycline and a recent study indicated that 95% or more of all MRSA and MSSA isolates were susceptible to doxycyline.
What infections are caused by sterptococci? Impetigo Cellulitis Erysipelas STSS Necrotizing fascitis
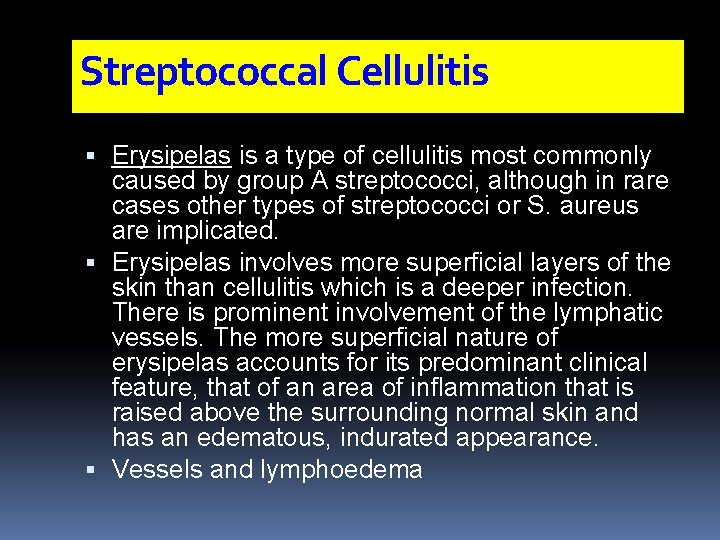
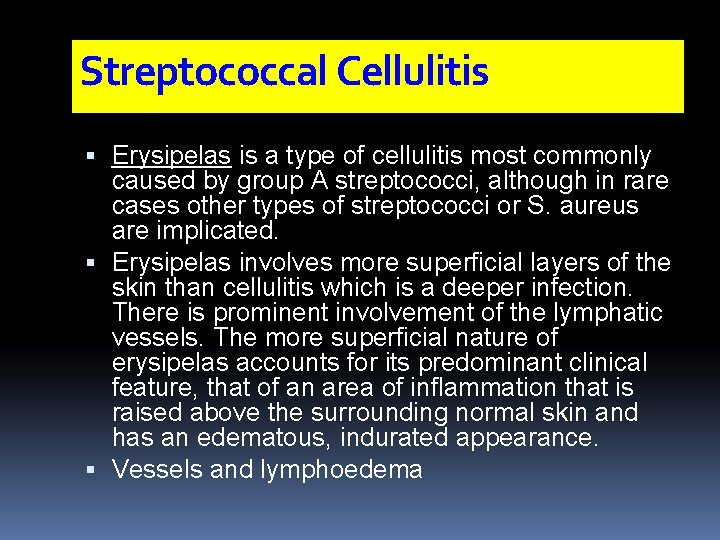
Streptococcal Cellulitis Erysipelas is a type of cellulitis most commonly caused by group A streptococci, although in rare cases other types of streptococci or S. aureus are implicated. Erysipelas involves more superficial layers of the skin than cellulitis which is a deeper infection. There is prominent involvement of the lymphatic vessels. The more superficial nature of erysipelas accounts for its predominant clinical feature, that of an area of inflammation that is raised above the surrounding normal skin and has an edematous, indurated appearance. Vessels and lymphoedema
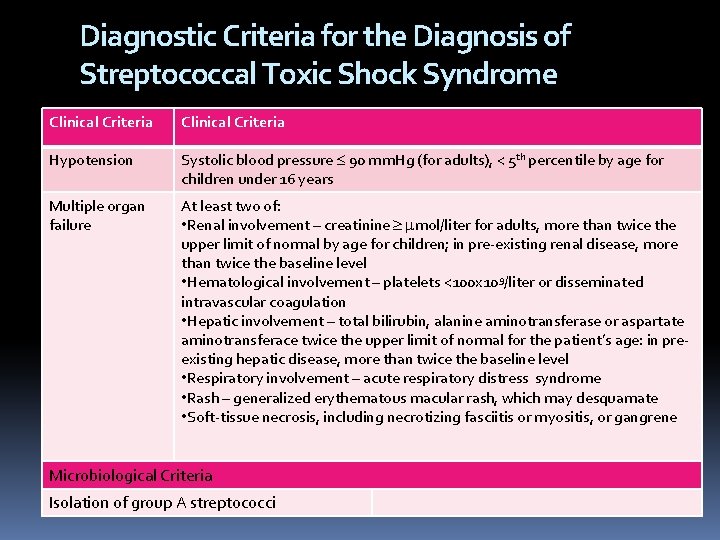
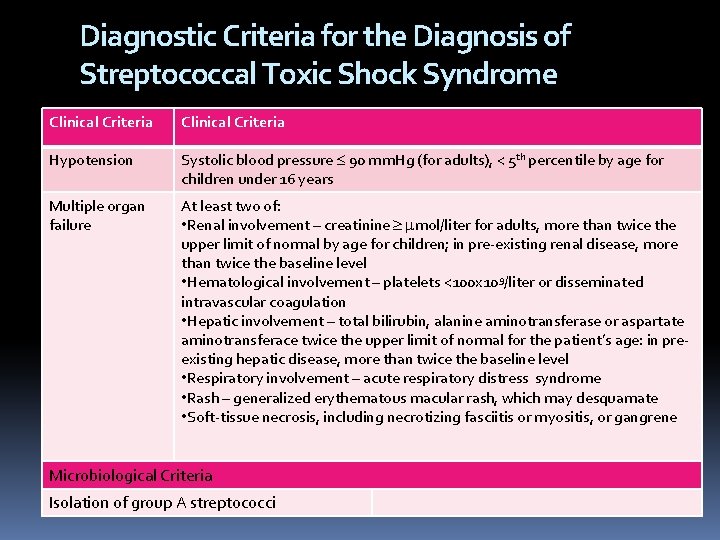
Diagnostic Criteria for the Diagnosis of Streptococcal Toxic Shock Syndrome Clinical Criteria Hypotension Systolic blood pressure 90 mm. Hg (for adults), < 5 th percentile by age for children under 16 years Multiple organ failure At least two of: • Renal involvement – creatinine mol/liter for adults, more than twice the upper limit of normal by age for children; in pre-existing renal disease, more than twice the baseline level • Hematological involvement – platelets <100 x 109/liter or disseminated intravascular coagulation • Hepatic involvement – total bilirubin, alanine aminotransferase or aspartate aminotransferace twice the upper limit of normal for the patient’s age: in preexisting hepatic disease, more than twice the baseline level • Respiratory involvement – acute respiratory distress syndrome • Rash – generalized erythematous macular rash, which may desquamate • Soft-tissue necrosis, including necrotizing fasciitis or myositis, or gangrene Microbiological Criteria Isolation of group A streptococci
Necrotizing Fascitis Necrotizing fascitis is a fulminating inflammation of the fascia that results in thrombosis of the subcutaneous blood vessels and necrosis of the underlying tissue Necrotizing fascitis itself is generally divided into two broad Type I, caused by mixed aerobic/anaerobic bacteria, including enterococci and non-group A streptococci (usually C or G); and Type 2, caused by group A streptococci, either alone or in combination with other organisms
What are the Clinical Features of Necrotizing Fasciitis? The most common site of infection is the distal lower limb, although fascial extension up the leg is common. The progression is often alarmingly rapid from a silent or apparently minor process to a fulminant condition with clinical features of systemic toxicity, extensive destruction with threat to the affected limb, and even imminent death. The first clue may be unexplained and rapidly worsening pain By the time the bullae have appeared, there is usually already extensive necrosis.
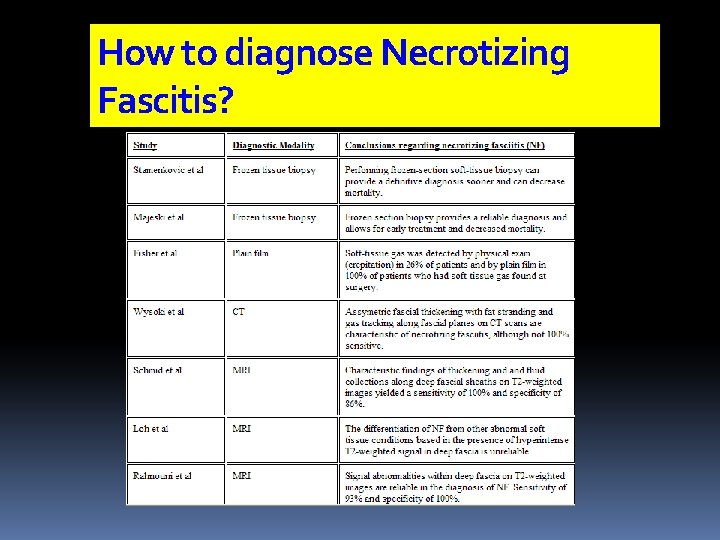
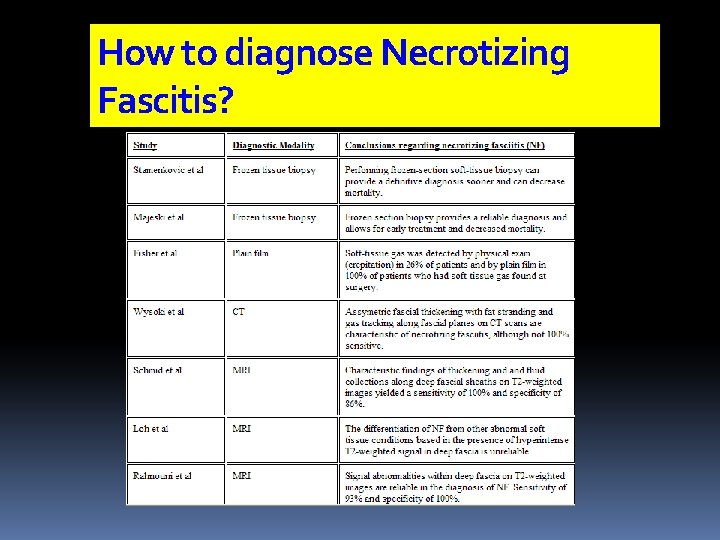
How to diagnose Necrotizing Fascitis?



Ncrotizing Facitis is LIMB + LIFE threatening Immediate extensive surgical debridement must be done ASAP CLINDAMYCIN must be give , it also has antitoxin action
Clostridial Infections Clostridia are large, anaerobic Grampositive, spore-forming bacilli. Clostridial infection cause myonecrosis, or gas gangrene, which can be divided into three major groups Post-traumatic; post-operative or non-traumatic; and spontaneous
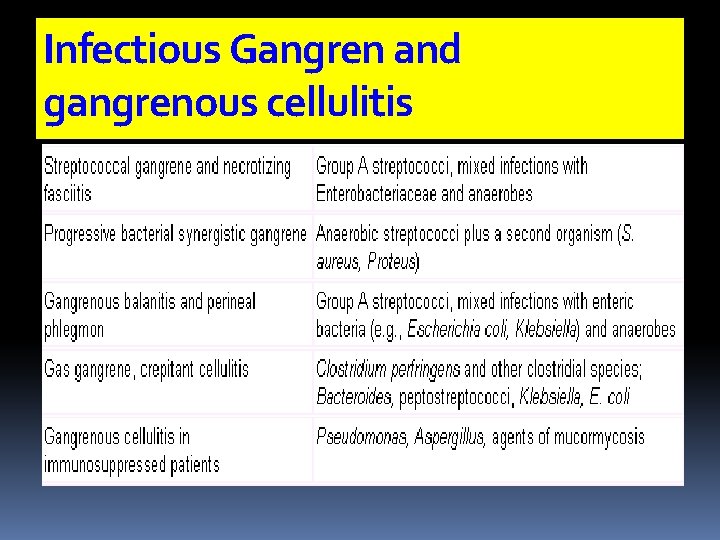
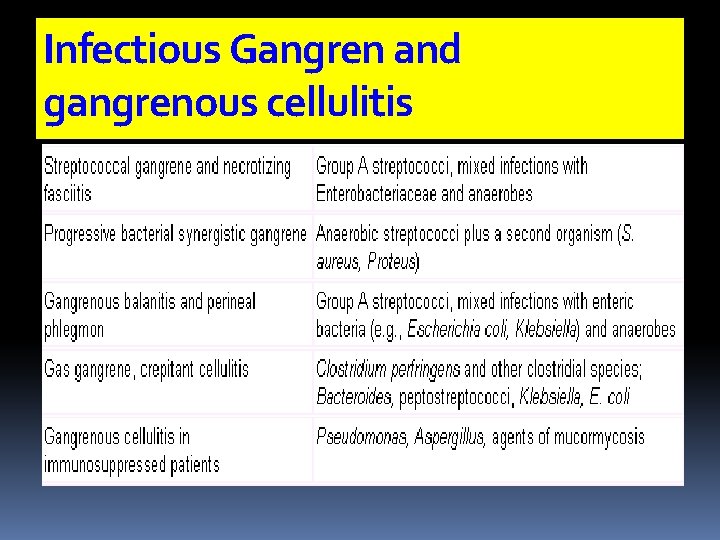
Infectious Gangren and gangrenous cellulitis
Clostridial Infections Clostridial myonecrosis is often associated with a traumatic event It can also develop in pre-existing wounds or infections such as skin ulcers and rhinocerebral or orbital mucormycosis. C. perfringens is the most frequent cause of clostridial myonecrosis but less frequent causes include C. septicum, C. novyii, C. histolyticum, and C. sordelli. ws
A case history A husband , which is not happy with his wife , became depressed and started to drink alcohol, and take some vitamins and iron ( for mood effects) he decided to take a break , he left hiswife, and went to a hotel to take a break, he was advised to take hot tub for relaxation, few days later he presented with sever cellulitis What is the organism to be covered ? A : Psedomonas Aerogenosa He received Treatment and improved
case 2 So he decided to travel to ladheqayya and do some fishing. His friend ( non alcoholic ) joined him. He later presented with cellulitis and necrotic ulcer, and within hours he developed severe septic shock. While his friend presented only with severe cellulitis. What is the organism ? A: Vibrio Vulnificus (Rx: doxycyclin +ceftazidim or FQ) , and in his friend Mycobacterim marinatum (Rx clarithromycin or minocyclin or bactrim or RIF+ETB x 3 months. or Erysipelothrix rhusiopathiae
case 3 He became more depressed, and was advised to have a second wife , which he did secretly But his first wife discovered that , and she attacked him , and she bitted him. And he developed an infected ulcer. What are the organism ? A : oral flora : anerobes and Eikenella Corrodes ( PCN, AUG or bactrim or FQ)
Case 4 The new wife , in a revenge , decided to through the first wife cat’s away, but the cat attacked her with a bite What organism to be covered ? A: Pasteurella Multicoda( AMP, DOXY, azithromax) The husband the new wife decided to leave to a small village , and have honey moon , and enjoy swimming in the river ( because of bas see experience) But both sustained a new celulitis
Case 5 What is the organism? A : Aeromonas Hydrophila( FQ or bactrim) The husband felt unlucky again with the second wife, so he was advised ( by his friend) to marry a third one. No body accepted him , except a middle aged lady , with DM and h/o speleenectomy at childhood after RTA When both the first & second wife new about it , they send a dog to attack them. The husband was able to run away , but the women sustained a dog bite , which was mild, within few hours she developed sever septic shock What is the organism A : Capnocytophagea canimoris( Rx augmnetin, FQ)
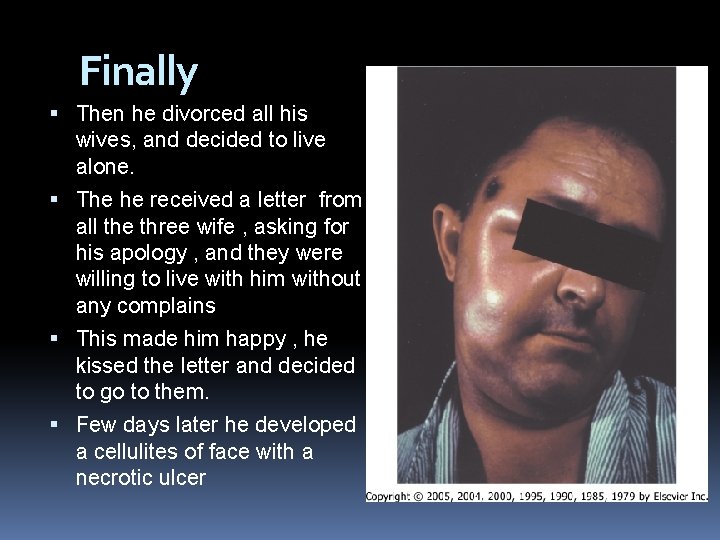
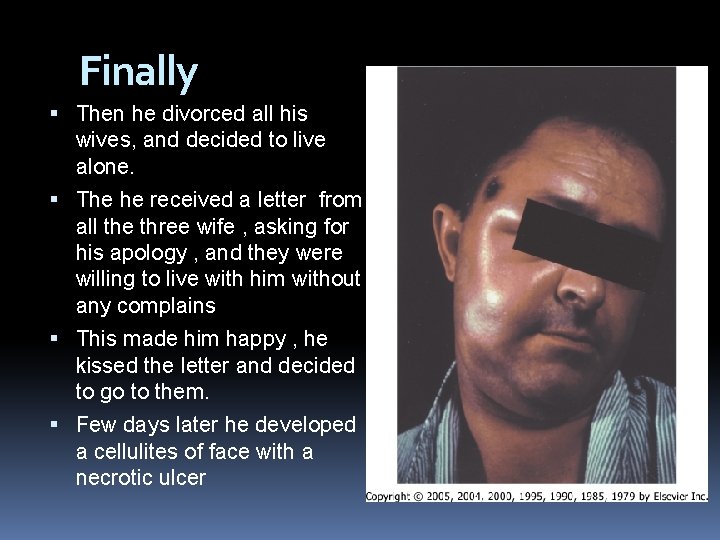
Finally Then he divorced all his wives, and decided to live alone. The he received a letter from all the three wife , asking for his apology , and they were willing to live with him without any complains This made him happy , he kissed the letter and decided to go to them. Few days later he developed a cellulites of face with a necrotic ulcer Cutanuous anthrax
PART TWO Community Associated MRSA
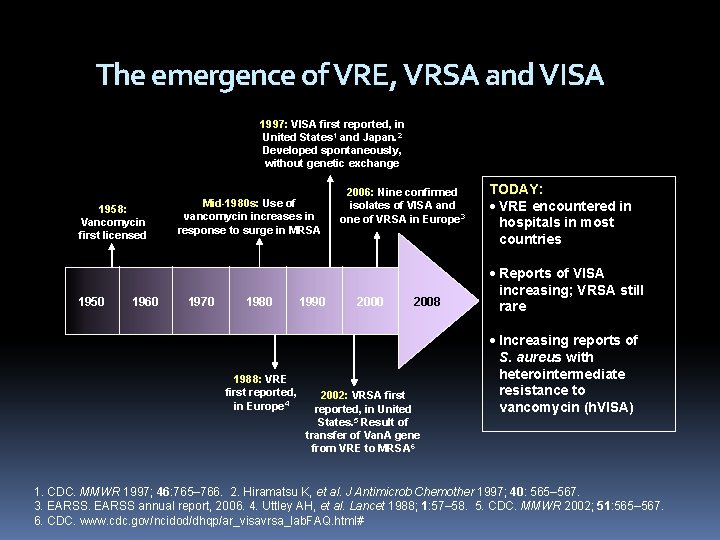
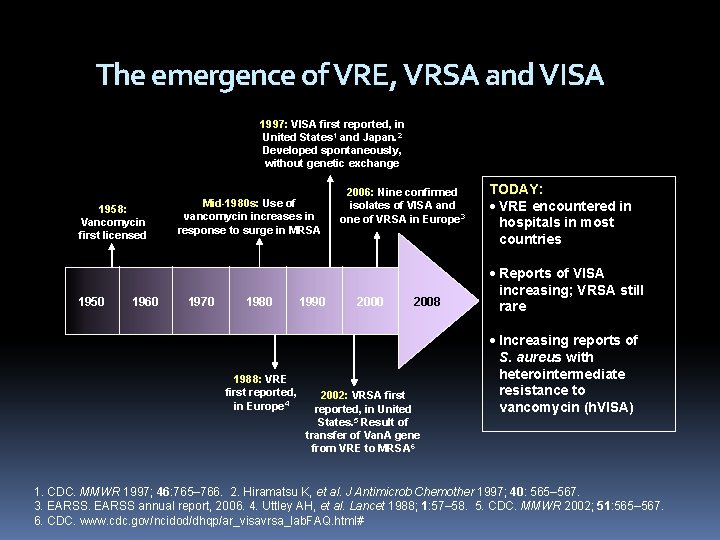
The emergence of VRE, VRSA and VISA 1997: VISA first reported, in United States 1 and Japan. 2 Developed spontaneously, without genetic exchange 1958: Vancomycin first licensed 1950 1960 Mid-1980 s: Use of vancomycin increases in response to surge in MRSA 1970 1988: VRE first reported, in Europe 4 1990 2006: Nine confirmed isolates of VISA and one of VRSA in Europe 3 2000 2008 2002: VRSA first reported, in United States. 5 Result of transfer of Van. A gene from VRE to MRSA 6 TODAY: VRE encountered in hospitals in most countries Reports of VISA increasing; VRSA still rare Increasing reports of S. aureus with heterointermediate resistance to vancomycin (h. VISA) 1. CDC. MMWR 1997; 46: 765– 766. 2. Hiramatsu K, et al. J Antimicrob Chemother 1997; 40: 565– 567. 3. EARSS annual report, 2006. 4. Uttley AH, et al. Lancet 1988; 1: 57– 58. 5. CDC. MMWR 2002; 51: 565– 567. 6. CDC. www. cdc. gov/ncidod/dhqp/ar_visavrsa_lab. FAQ. html#
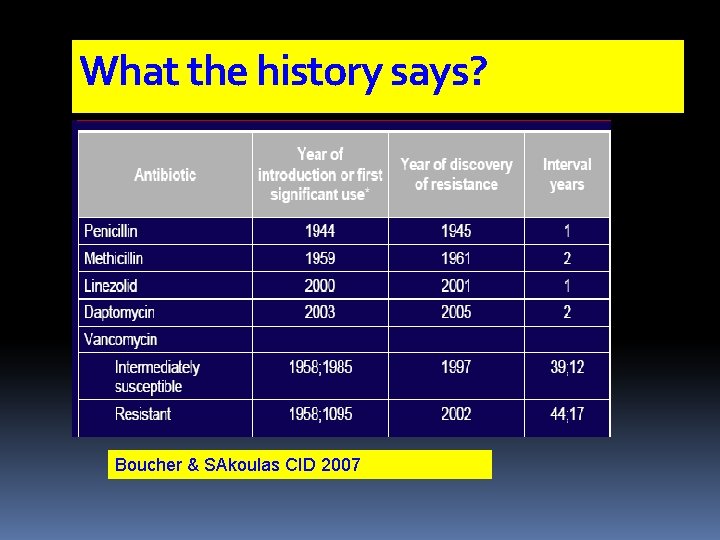
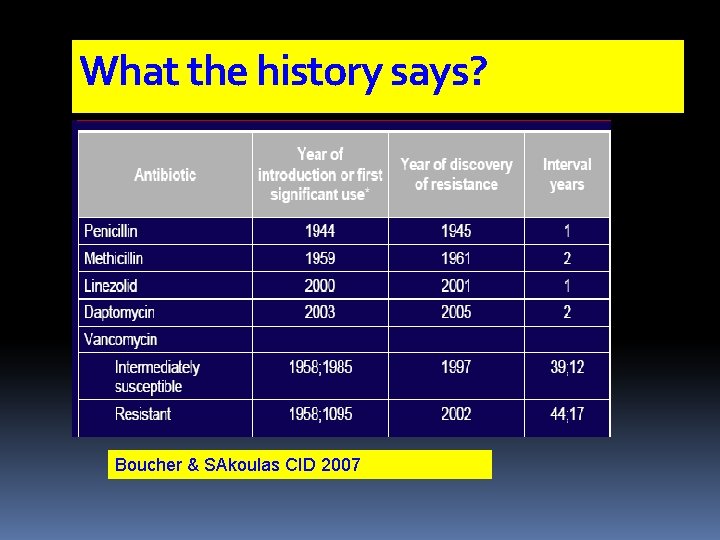
What the history says? Boucher & SAkoulas CID 2007
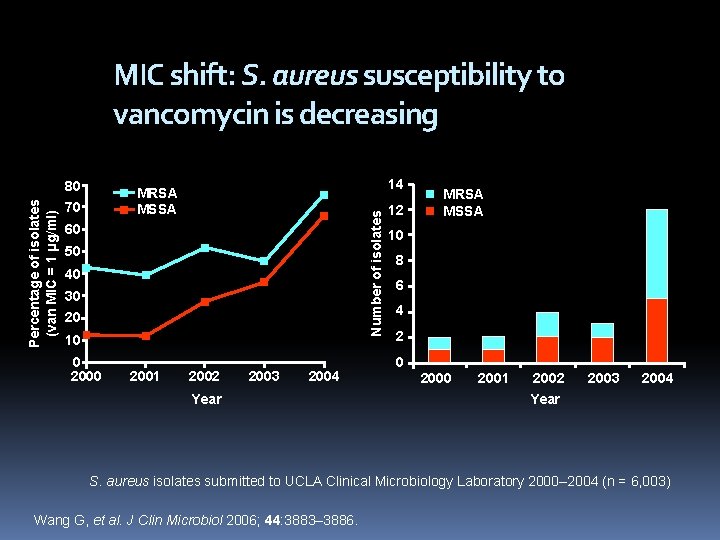
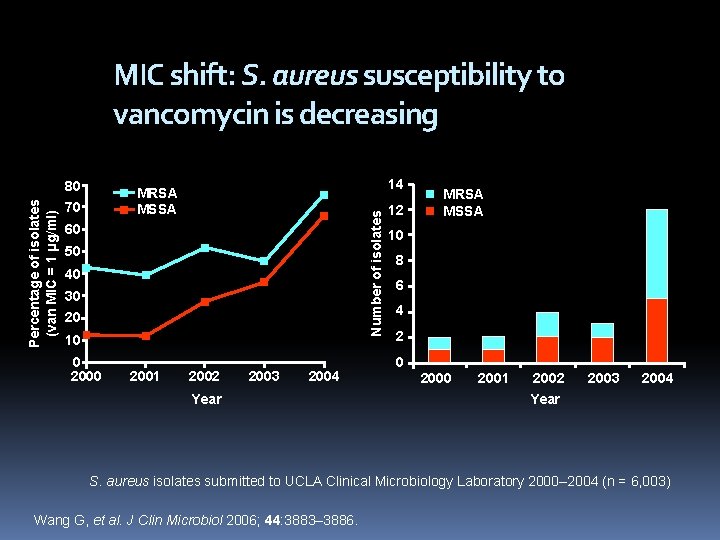
MIC shift: S. aureus susceptibility to vancomycin is decreasing 14 MRSA MSSA 70 Number of isolates Percentage of isolates (van MIC = 1 µg/ml) 80 60 50 40 30 20 10 0 2001 2002 2003 2004 Year 12 MRSA MSSA 10 8 6 4 2 0 2001 2002 2003 2004 Year S. aureus isolates submitted to UCLA Clinical Microbiology Laboratory 2000– 2004 (n = 6, 003) Wang G, et al. J Clin Microbiol 2006; 44: 3883– 3886.
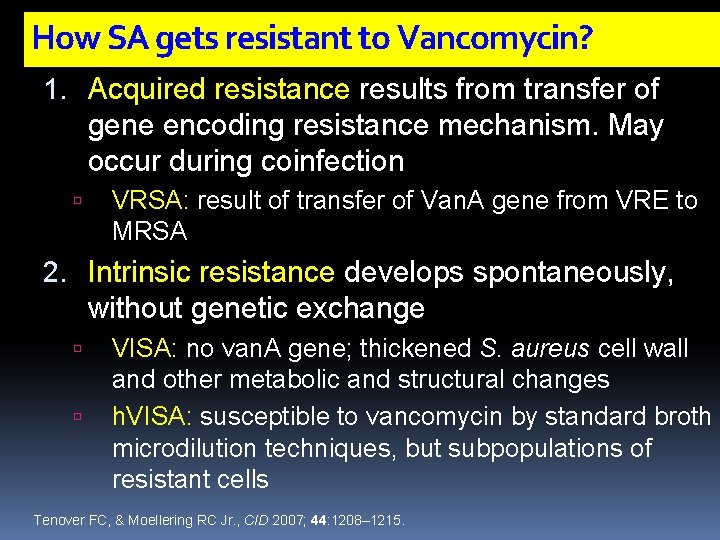
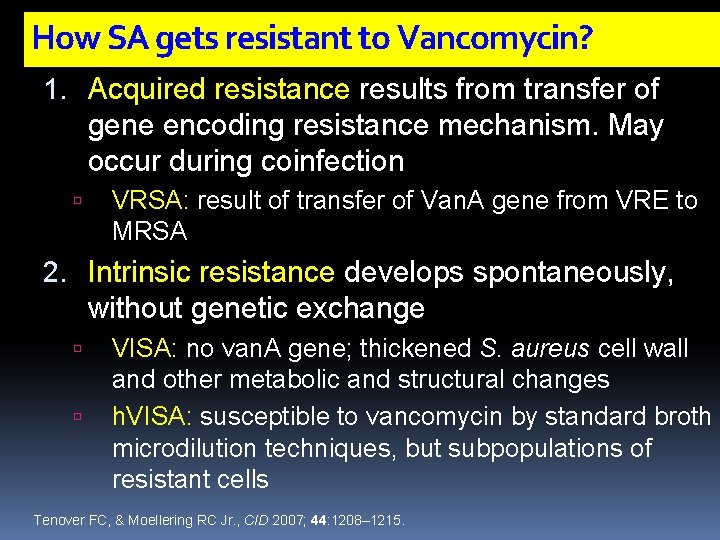
How SA gets resistant to Vancomycin? 1. Acquired resistance results from transfer of gene encoding resistance mechanism. May occur during coinfection VRSA: result of transfer of Van. A gene from VRE to MRSA 2. Intrinsic resistance develops spontaneously, without genetic exchange VISA: no van. A gene; thickened S. aureus cell wall and other metabolic and structural changes h. VISA: susceptible to vancomycin by standard broth microdilution techniques, but subpopulations of resistant cells Tenover FC, & Moellering RC Jr. , CID 2007; 44: 1208– 1215.
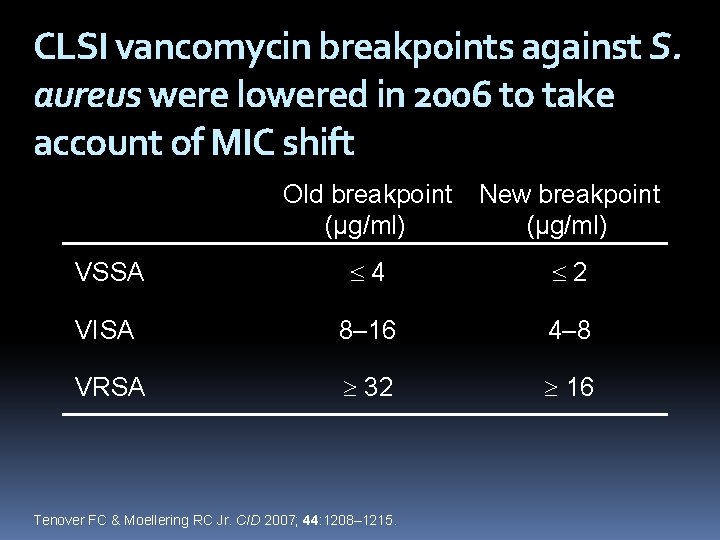
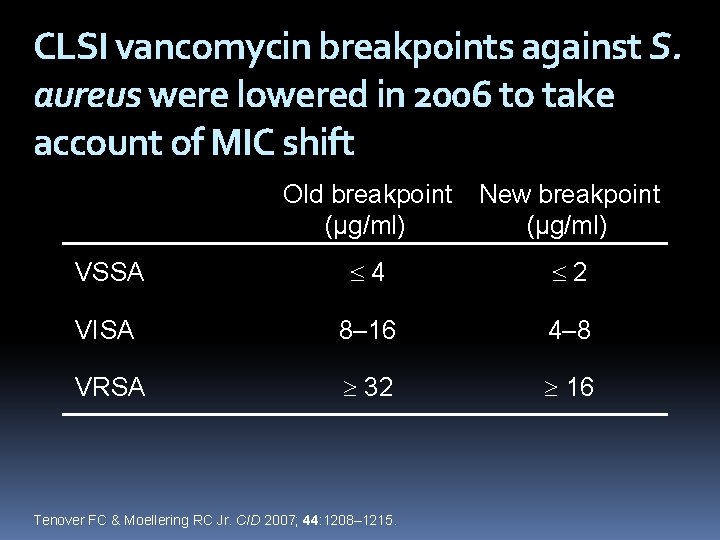
CLSI vancomycin breakpoints against S. aureus were lowered in 2006 to take account of MIC shift Old breakpoint (µg/ml) New breakpoint (µg/ml) VSSA 4 2 VISA 8– 16 4– 8 VRSA 32 16 Tenover FC & Moellering RC Jr. CID 2007; 44: 1208– 1215.

Why increasing ? ? Initially we thought it is pure Ping –Pong effects, i e, the same hospital acquired MRSA is now living in the community. But it is clear now that this is not the complete story There is emergence of new CA-MRSA

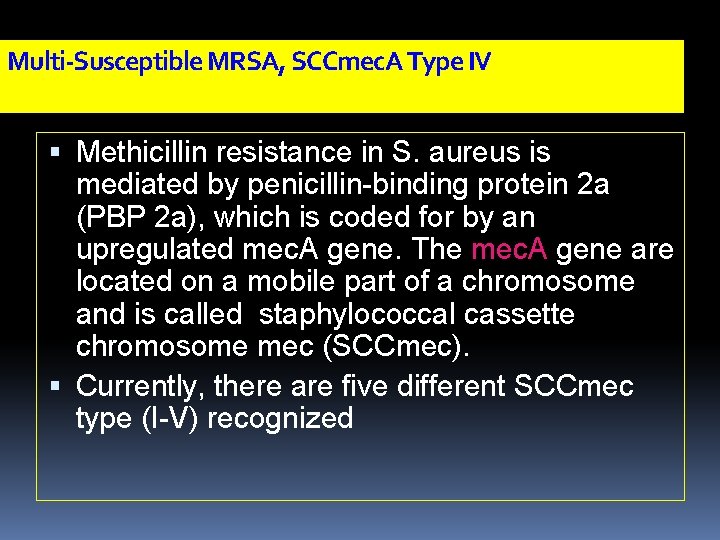
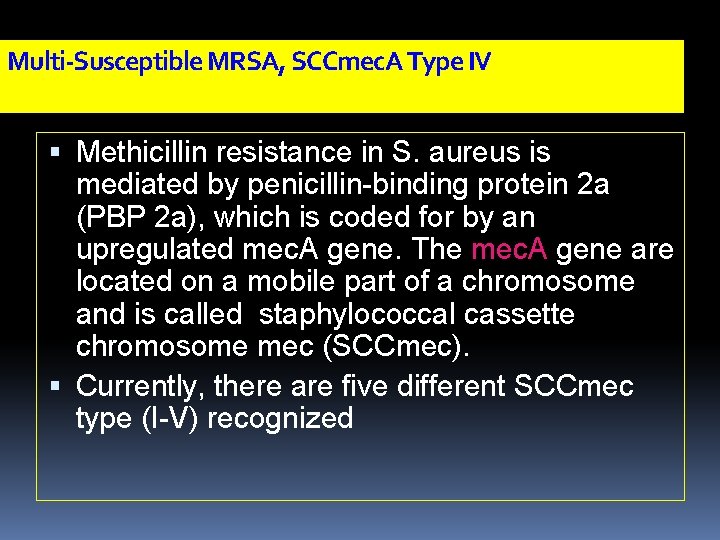
Multi-Susceptible MRSA, SCCmec. A Type IV Methicillin resistance in S. aureus is mediated by penicillin-binding protein 2 a (PBP 2 a), which is coded for by an upregulated mec. A gene. The mec. A gene are located on a mobile part of a chromosome and is called staphylococcal cassette chromosome mec (SCCmec). Currently, there are five different SCCmec type (I-V) recognized
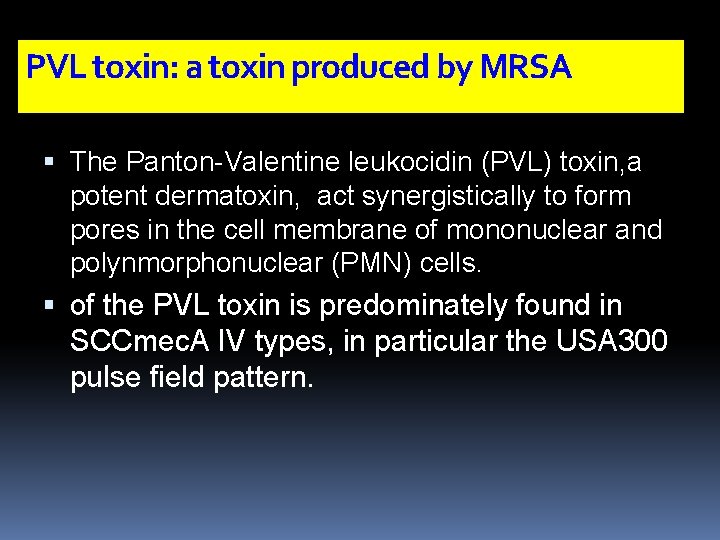
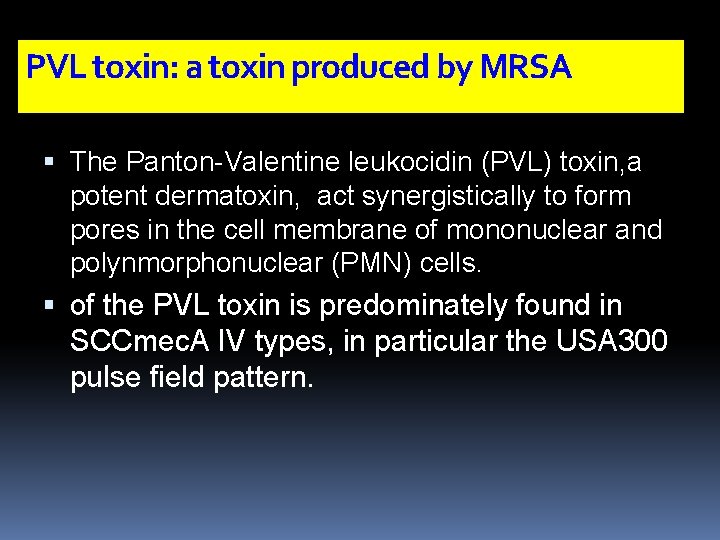
PVL toxin: a toxin produced by MRSA The Panton-Valentine leukocidin (PVL) toxin, a potent dermatoxin, act synergistically to form pores in the cell membrane of mononuclear and polynmorphonuclear (PMN) cells. of the PVL toxin is predominately found in SCCmec. A IV types, in particular the USA 300 pulse field pattern.
In Europe Now CA-MRSA USA-300 is increasing in Europe's, with outbreaks specially in pork farms Any patient coming from pork farm, MRSA infection should be considered

Emergence of a New Kind of MRSA The majority of CA-MRSA infections are SSSI and adequate drainage/debridement and/or antibiotics is sufficient therapy for cure these infections. Other reports of invasive CA-MRSA infections include necrotizing pneumonia and necrotizing fascitis CA-MRSA prevalence rate was 30. 2% (range 1. 9 -96%), whereas for the prospective studies 636 patients) the prevalence rate was 37. 3% (range 18. 2 -51. 2%).
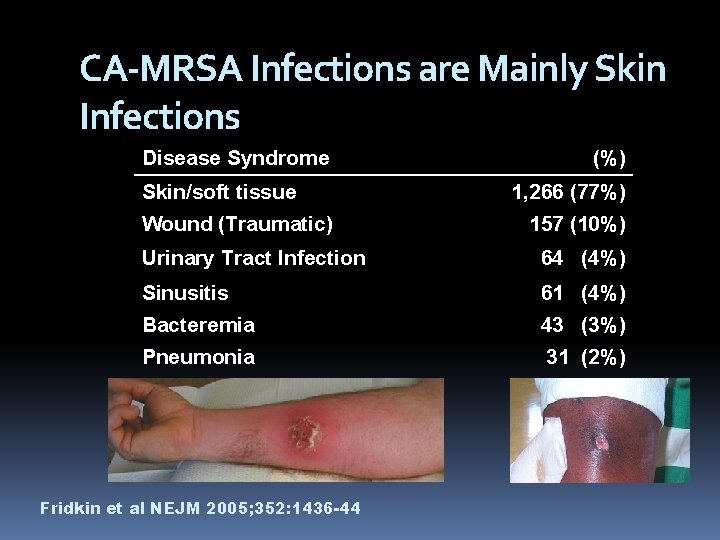
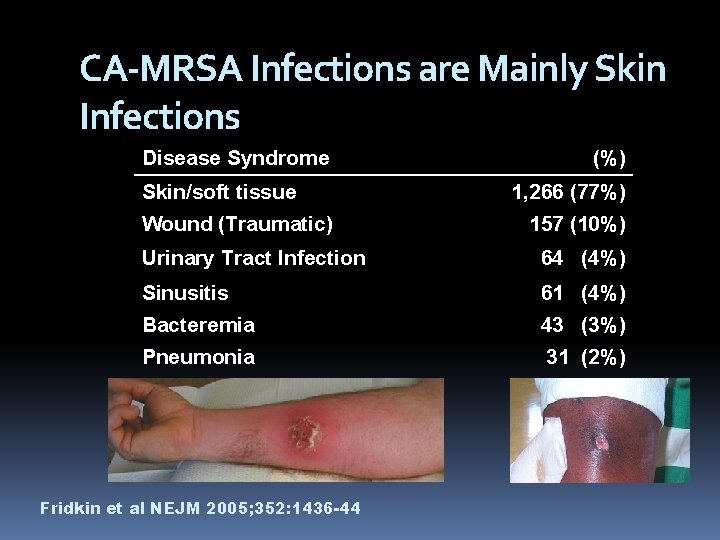
CA-MRSA Infections are Mainly Skin Infections Disease Syndrome Skin/soft tissue Wound (Traumatic) (%) 1, 266 (77%) 157 (10%) Urinary Tract Infection 64 (4%) Sinusitis 61 (4%) Bacteremia 43 (3%) Pneumonia 31 (2%) Fridkin et al NEJM 2005; 352: 1436 -44

CA-MRSA

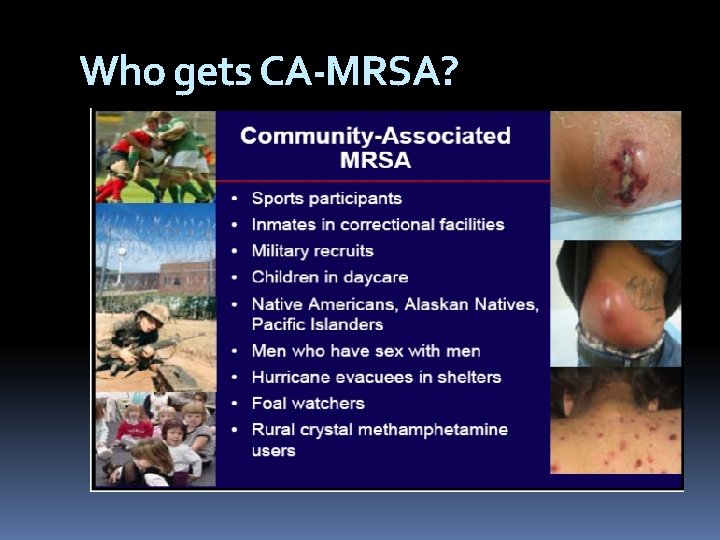
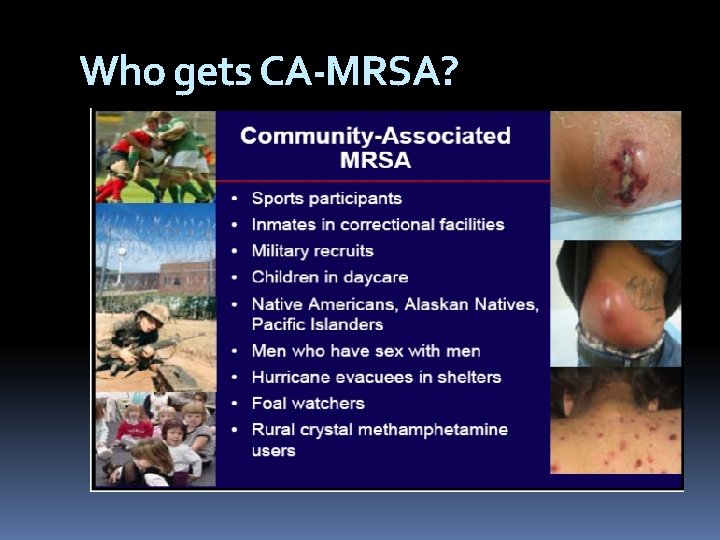
Who gets CA-MRSA?

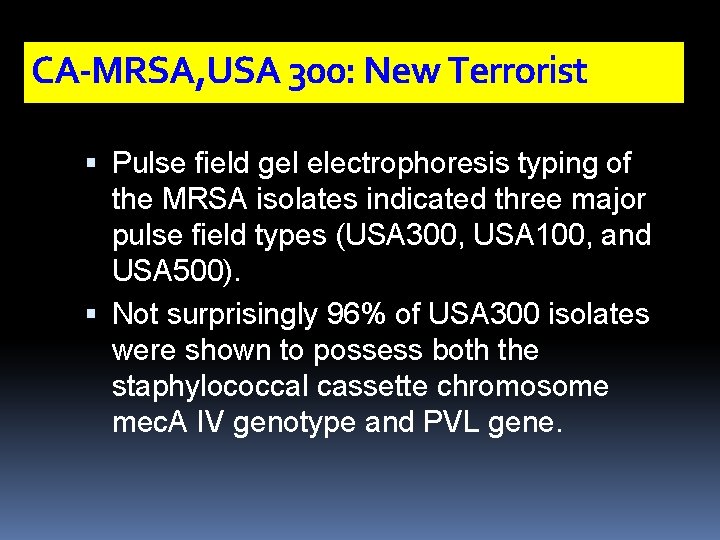
CA-MRSA, USA 300: New Terrorist Pulse field gel electrophoresis typing of the MRSA isolates indicated three major pulse field types (USA 300, USA 100, and USA 500). Not surprisingly 96% of USA 300 isolates were shown to possess both the staphylococcal cassette chromosome mec. A IV genotype and PVL gene.
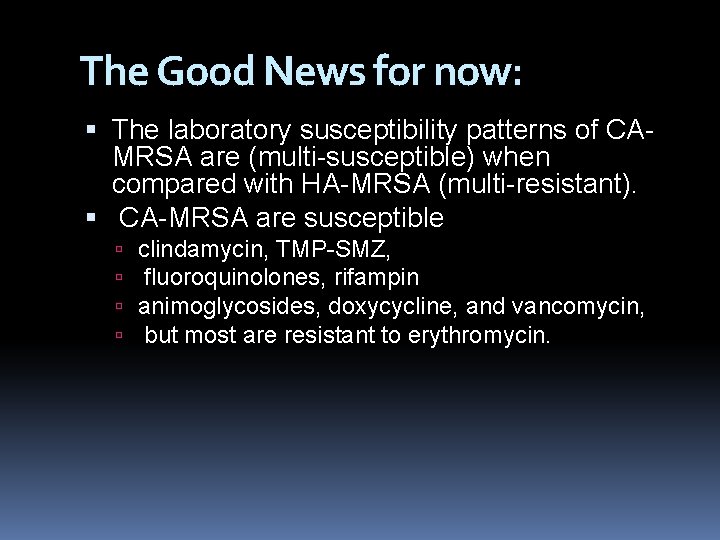
The Good News for now: The laboratory susceptibility patterns of CAMRSA are (multi-susceptible) when compared with HA-MRSA (multi-resistant). CA-MRSA are susceptible clindamycin, TMP-SMZ, fluoroquinolones, rifampin animoglycosides, doxycycline, and vancomycin, but most are resistant to erythromycin.
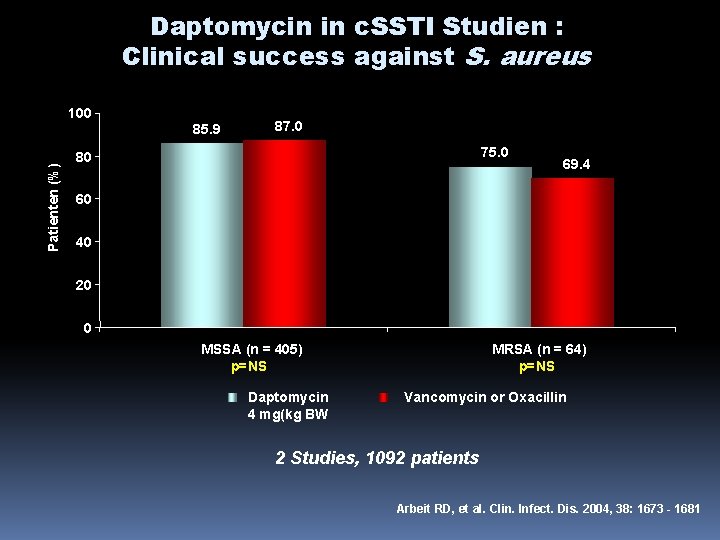
There was no difference in cure rates between linezolid (73%) and vancomycin (73%); MRSA eradication rates were 61% for linezolid and 63% for vancomycin Daptomycin clinical success rates were also equal to those of the comparator agents against Streptococcus spp. (SE. pyogenes, S. agalactiae, and S. dysgalactiae) and Enterococcus faecalis.
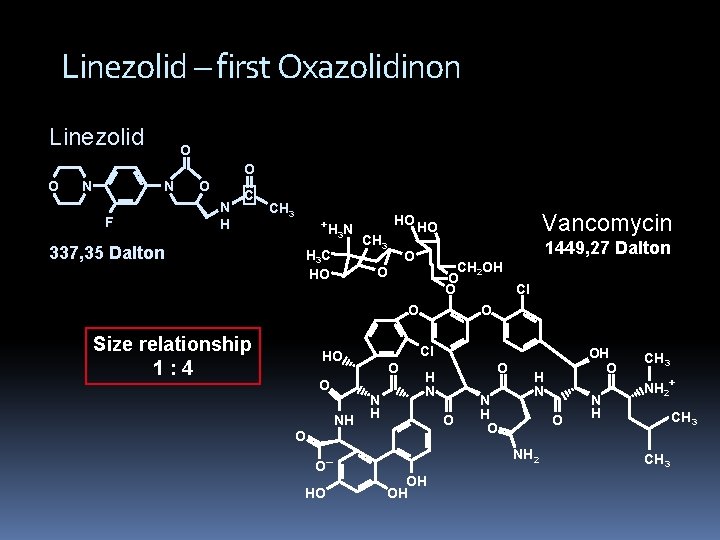
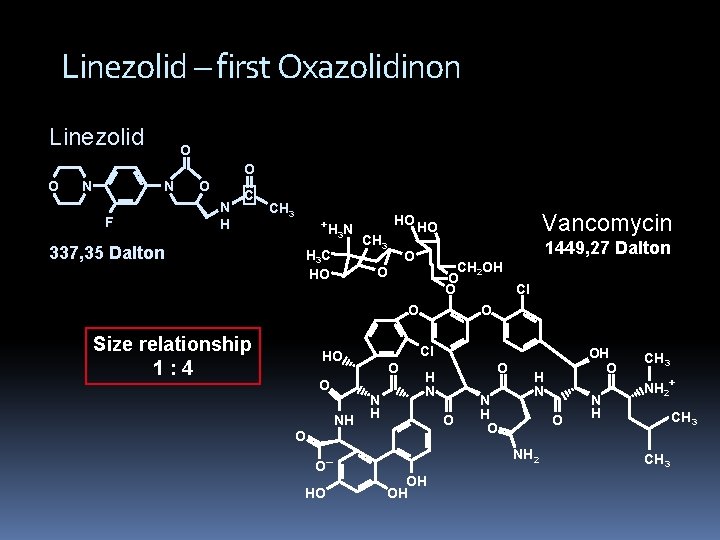
Linezolid – first Oxazolidinon Linezolid O O O N N F O N H C 337, 35 Dalton CH 3 +H N 3 H 3 C HO CH 3 1449, 27 Dalton O CH 2 OH O O Cl O O O Size relationship 1: 4 Cl HO O NH O N H HO O H N O O O– Vancomycin HO HO N H O H N O NH 2 OH OH OH O N H CH 3 NH 2+ CH 3
New Antibiotics against MRSA Tetracyclin Analoga (Glycylcycline) Tigecycline Lipopeptides Daptomycin New Glycopeptides Telavancin Oritavancin Dalbavancin MRSA Cephalosporines Ceftobiprole Anti-folate
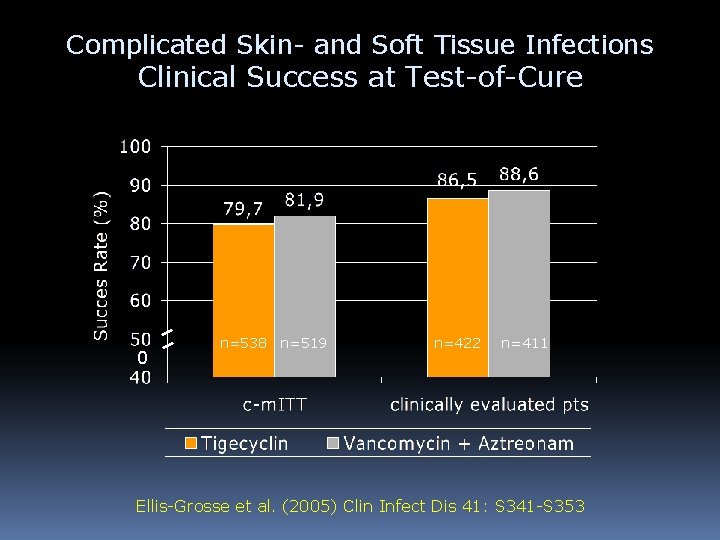
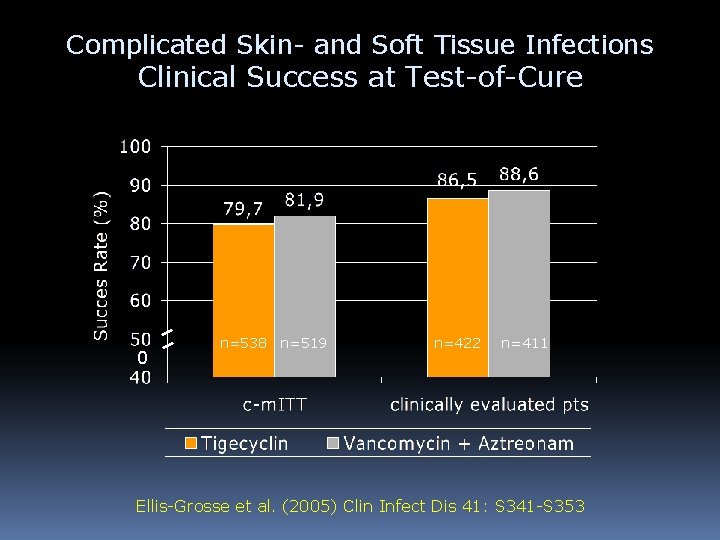
Complicated Skin- and Soft Tissue Infections Clinical Success at Test-of-Cure 0 n=538 n=519 n=422 n=411 Ellis-Grosse et al. (2005) Clin Infect Dis 41: S 341 -S 353
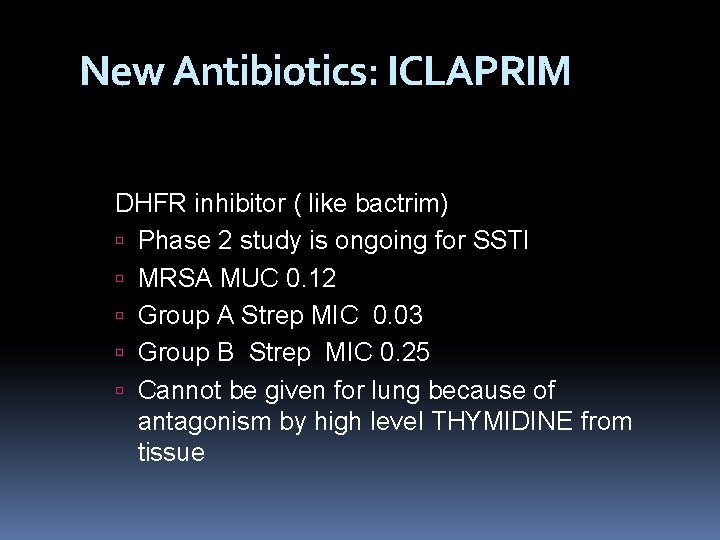
New Antibiotics: ICLAPRIM DHFR inhibitor ( like bactrim) Phase 2 study is ongoing for SSTI MRSA MUC 0. 12 Group A Strep MIC 0. 03 Group B Strep MIC 0. 25 Cannot be given for lung because of antagonism by high level THYMIDINE from tissue
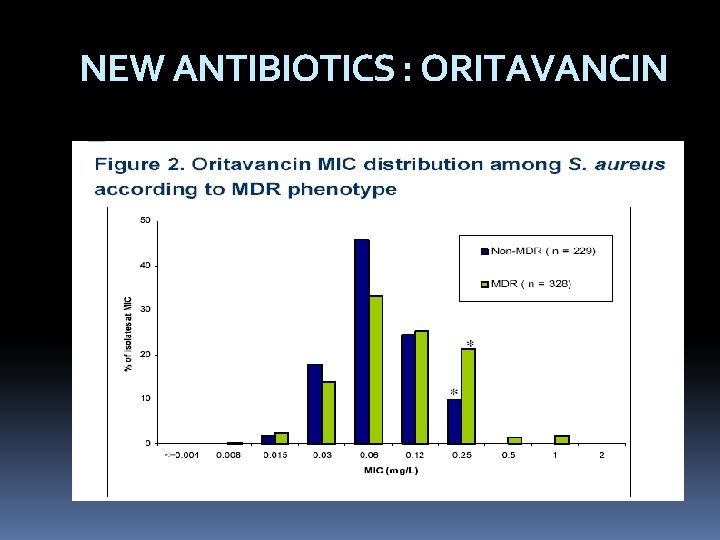
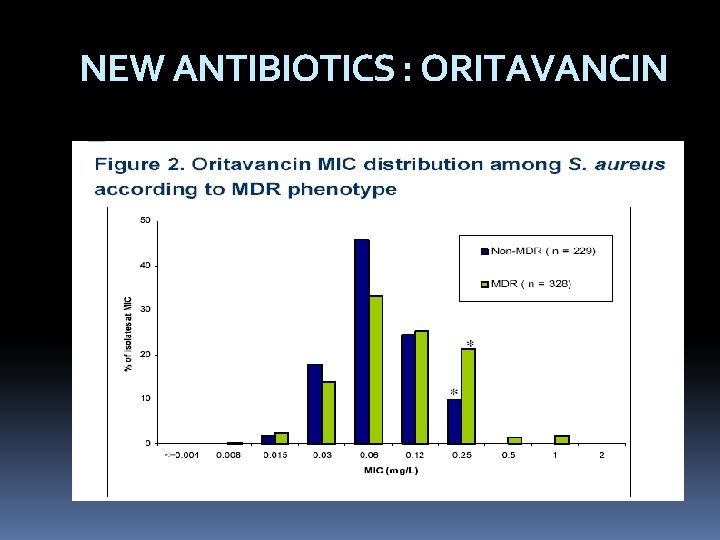
NEW ANTIBIOTICS : ORITAVANCIN
ORITAVANCIN Prolonged half life, may be given once weakly Minimal nephrotoxicity Active against VSE and VRE`
Daptomycin New bactercidal drug, cuasing calcium efflux and cell memebrane damge Approved for SSTI and Right sided bacterial endocarditis SE : elevated CK
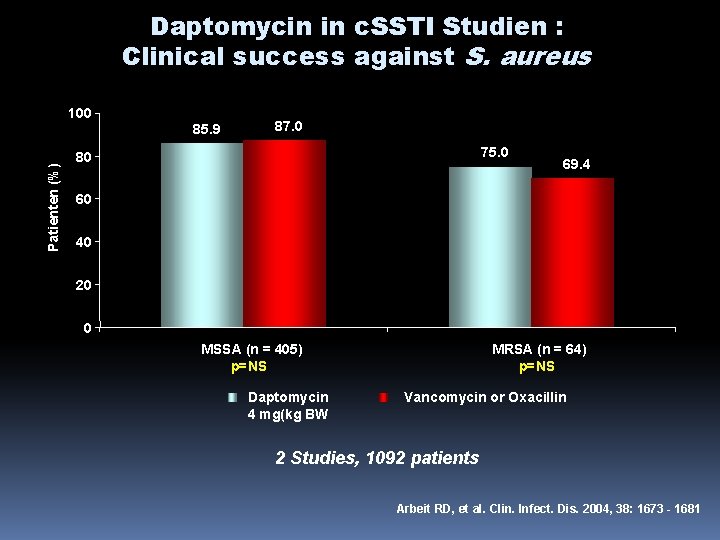
Daptomycin in c. SSTI Studien : Clinical success against S. aureus Patienten (%) 100 85. 9 87. 0 75. 0 80 69. 4 60 40 20 0 MSSA (n = 405) p=NS Daptomycin 4 mg(kg BW MRSA (n = 64) p=NS Vancomycin or Oxacillin 2 Studies, 1092 patients Arbeit RD, et al. Clin. Infect. Dis. 2004, 38: 1673 - 1681
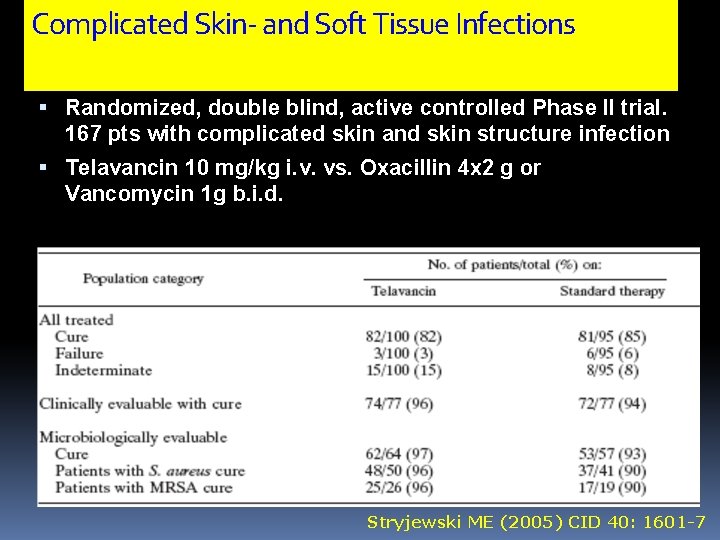
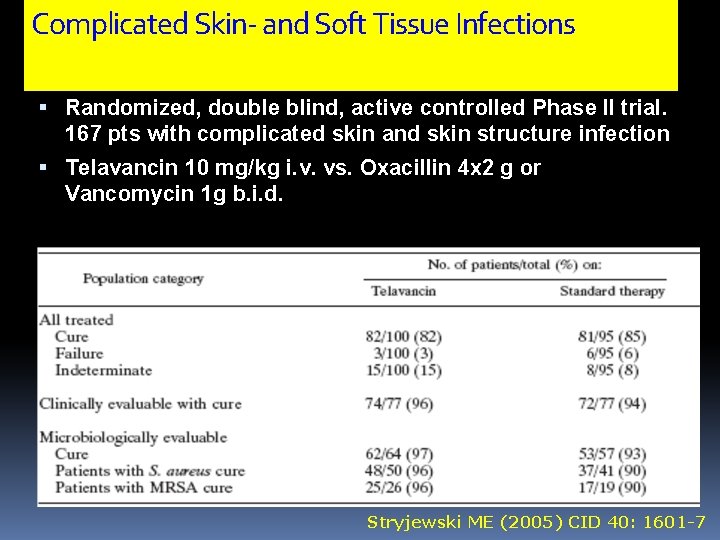
Complicated Skin- and Soft Tissue Infections Randomized, double blind, active controlled Phase II trial. 167 pts with complicated skin and skin structure infection Telavancin 10 mg/kg i. v. vs. Oxacillin 4 x 2 g or Vancomycin 1 g b. i. d. Stryjewski ME (2005) CID 40: 1601 -7
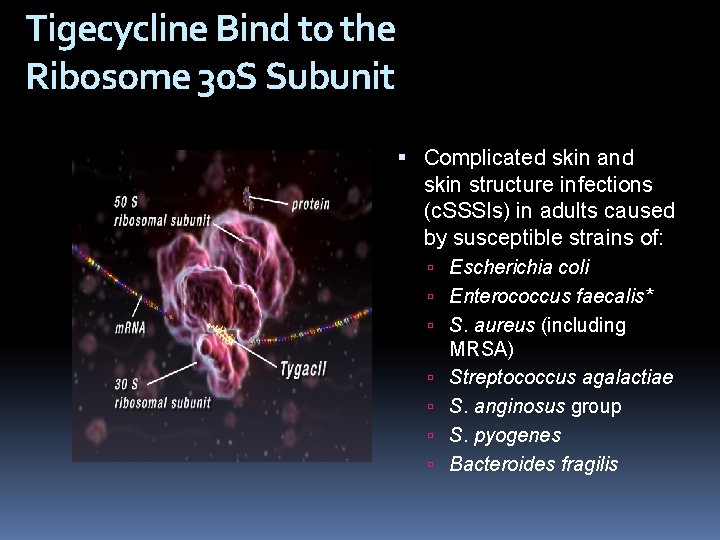
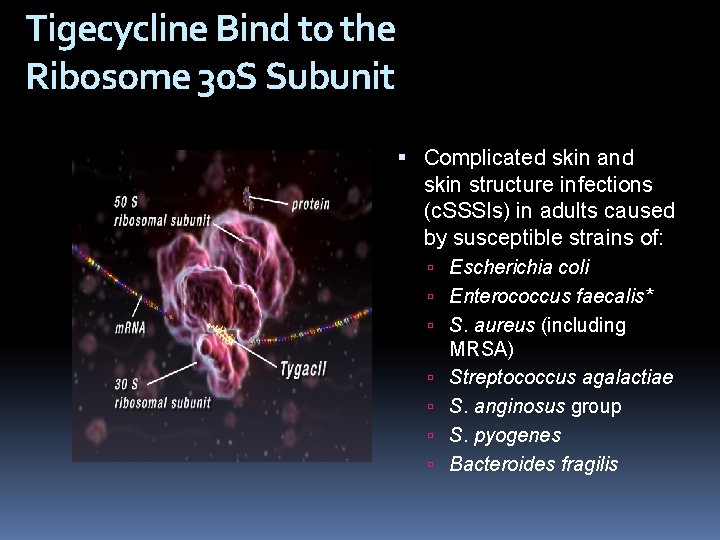
Tigecycline Bind to the Ribosome 30 S Subunit Complicated skin and skin structure infections (c. SSSIs) in adults caused by susceptible strains of: Escherichia coli Enterococcus faecalis* S. aureus (including MRSA) Streptococcus agalactiae S. anginosus group S. pyogenes Bacteroides fragilis
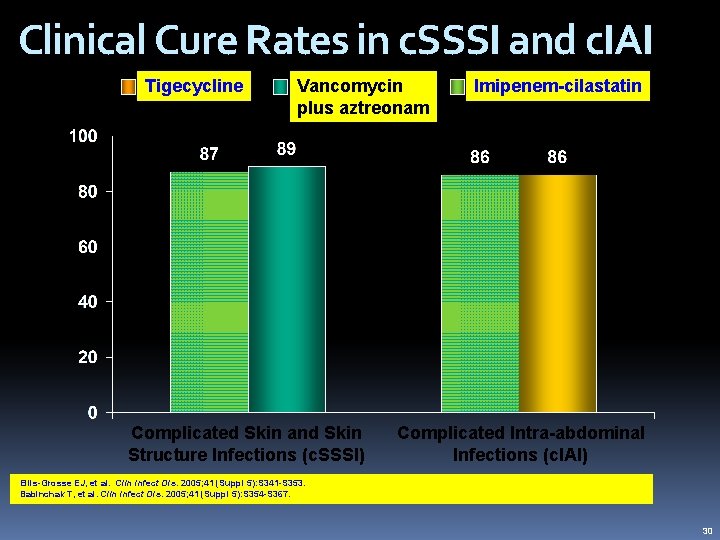
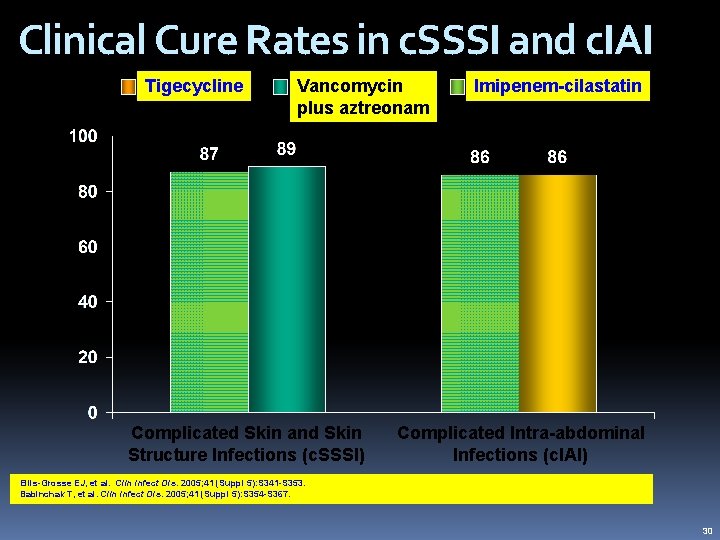
Clinical Cure Rates in c. SSSI and c. IAI Vancomycin plus aztreonam Imipenem-cilastatin Cure Rate (%) Tigecycline Complicated Skin and Skin Structure Infections (c. SSSI) Complicated Intra-abdominal Infections (c. IAI) Ellis-Grosse EJ, et al. Clin Infect Dis. 2005; 41 (Suppl 5): S 341 -S 353. Babinchak T, et al. Clin Infect Dis. 2005; 41 (Suppl 5): S 354 -S 367. 30
 Waris husain
Waris husain Ashraf husain
Ashraf husain Ashraf husain
Ashraf husain Mashkur husain md
Mashkur husain md Miss fatima husain
Miss fatima husain A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Understanding the mirai botnet
Understanding the mirai botnet Bone and joint infections
Bone and joint infections Methotrexate and yeast infections
Methotrexate and yeast infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Opportunistic infections
Opportunistic infections Opportunistic infections
Opportunistic infections Storch infections
Storch infections Storch infections
Storch infections Cryptosporidiose
Cryptosporidiose Bacterial vaginosis
Bacterial vaginosis Postpartum infections
Postpartum infections Genital infections
Genital infections Amber blumling
Amber blumling Salmonella life cycle
Salmonella life cycle Acute gingival infections
Acute gingival infections Stratum granulosum
Stratum granulosum Lifeline vi+
Lifeline vi+ Shapes that have smooth even edges and are measurable
Shapes that have smooth even edges and are measurable Enumerate the market forms of meat.
Enumerate the market forms of meat. Thin skin vs thick skin
Thin skin vs thick skin Modelage masks milady
Modelage masks milady Which language
Which language Conjunctions in paragraph
Conjunctions in paragraph Foam cells definition
Foam cells definition Polychromatic lustre complicated cataract
Polychromatic lustre complicated cataract Complicated software
Complicated software Why interpersonal communication is contextual
Why interpersonal communication is contextual Ocugen syock
Ocugen syock Tafjal
Tafjal Icd 10 malaria falciparum
Icd 10 malaria falciparum Complicated malaria
Complicated malaria Music of classical period 1750 to 1820
Music of classical period 1750 to 1820 Complicated urinary tract infection
Complicated urinary tract infection Complicated math
Complicated math Generally restful like the horizon
Generally restful like the horizon Complicated math
Complicated math Infinite
Infinite Complicated uti symptoms
Complicated uti symptoms Penicinilase
Penicinilase It is complicated because
It is complicated because Interpersonal communication principles
Interpersonal communication principles Complicated vs uncomplicated uti
Complicated vs uncomplicated uti Skin structure growth and nutrition
Skin structure growth and nutrition Accessory structure of the skin
Accessory structure of the skin Structure of thin skin
Structure of thin skin Skin diagram
Skin diagram Lexical ambiguity examples
Lexical ambiguity examples Transformational grammar
Transformational grammar Subject-dqrnghtp
Subject-dqrnghtp Static and dynamic queue in data structure
Static and dynamic queue in data structure Deep surface structure
Deep surface structure Dermatology morphology
Dermatology morphology Chapter 8 skin disorders and diseases review questions
Chapter 8 skin disorders and diseases review questions Nails assessment
Nails assessment Serosanguineous vs serous
Serosanguineous vs serous Skin care objectives
Skin care objectives Arctic wolf adaptation
Arctic wolf adaptation Fur turns white during the cold snowy winter months
Fur turns white during the cold snowy winter months How to make fake scars with vaseline
How to make fake scars with vaseline Kode icd 10 telogen effluvium
Kode icd 10 telogen effluvium Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases In what situation should a nail service not be performed?
In what situation should a nail service not be performed? Chapter 48 skin integrity and wound care
Chapter 48 skin integrity and wound care Chapter 4 skin and body membranes answer key
Chapter 4 skin and body membranes answer key Ch 4 skin and body membranes
Ch 4 skin and body membranes