Atherosclerosis Coronary heart disease Angina pectoris Myocardial infarction





- Slides: 49
Atherosclerosis Coronary heart disease Angina pectoris Myocardial infarction
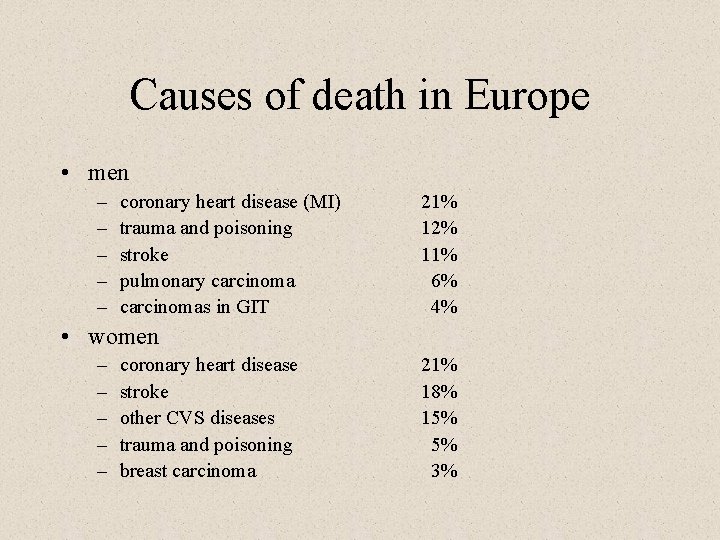
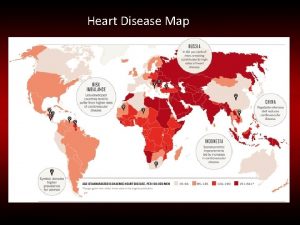
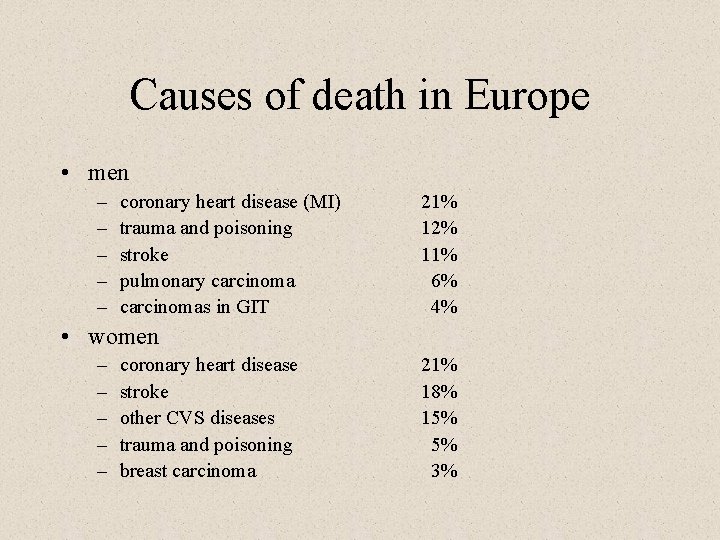
Causes of death in Europe • men – – – coronary heart disease (MI) trauma and poisoning stroke pulmonary carcinomas in GIT 21% 12% 11% 6% 4% • women – – – coronary heart disease stroke other CVS diseases trauma and poisoning breast carcinoma 21% 18% 15% 5% 3%
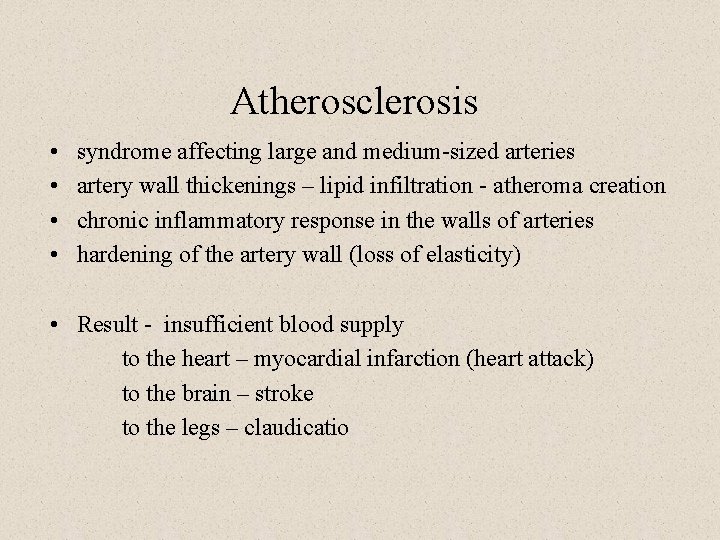
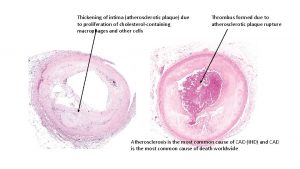
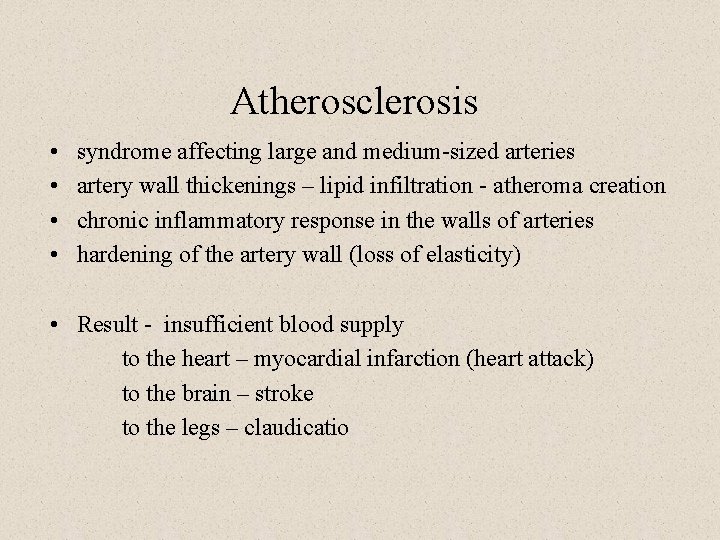
Atherosclerosis • • syndrome affecting large and medium-sized arteries artery wall thickenings – lipid infiltration - atheroma creation chronic inflammatory response in the walls of arteries hardening of the artery wall (loss of elasticity) • Result - insufficient blood supply to the heart – myocardial infarction (heart attack) to the brain – stroke to the legs – claudicatio
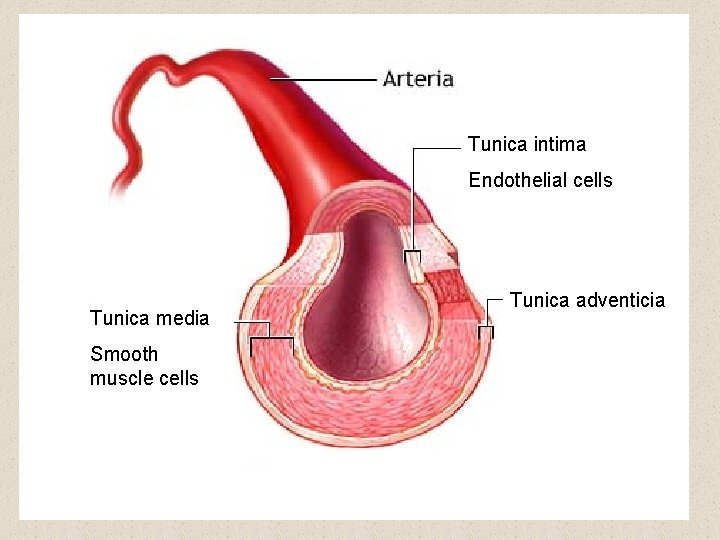
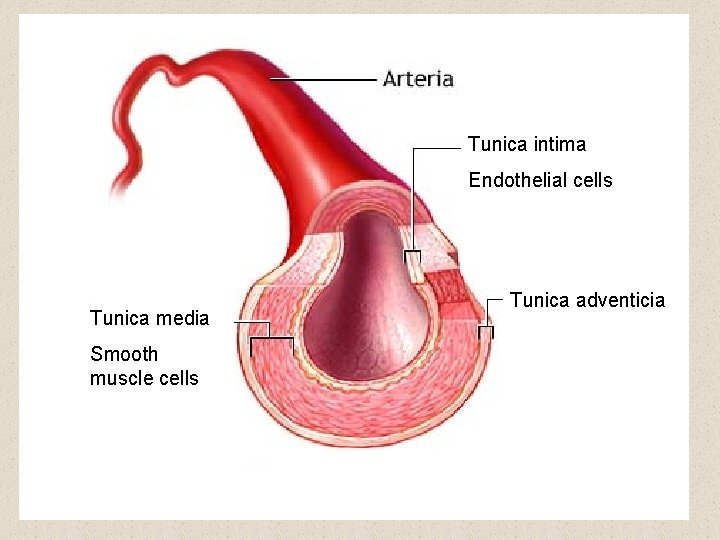
Tunica intima Endothelial cells Tunica media Smooth muscle cells Tunica adventicia
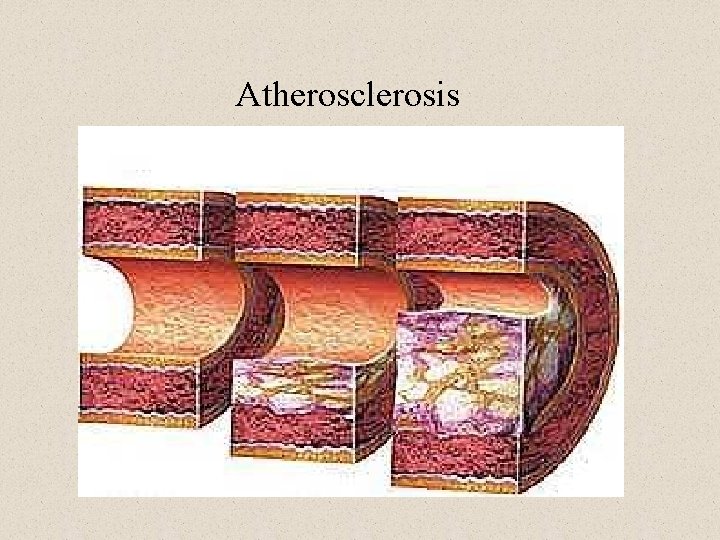
Atherosclerosis
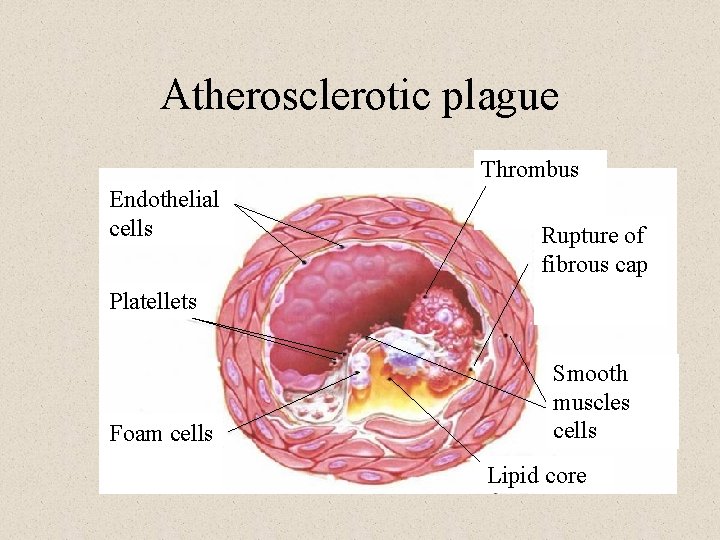
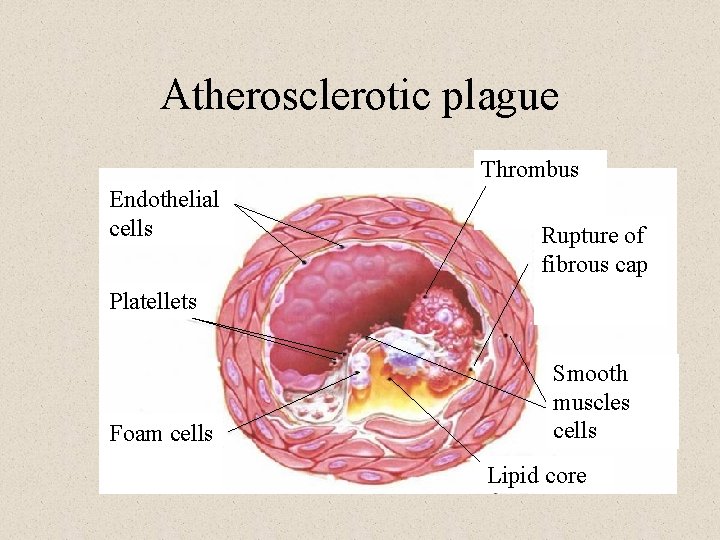
Atherosclerotic plague Thrombus Endothelial cells Rupture of fibrous cap Platellets Foam cells Smooth muscles cells Lipid core

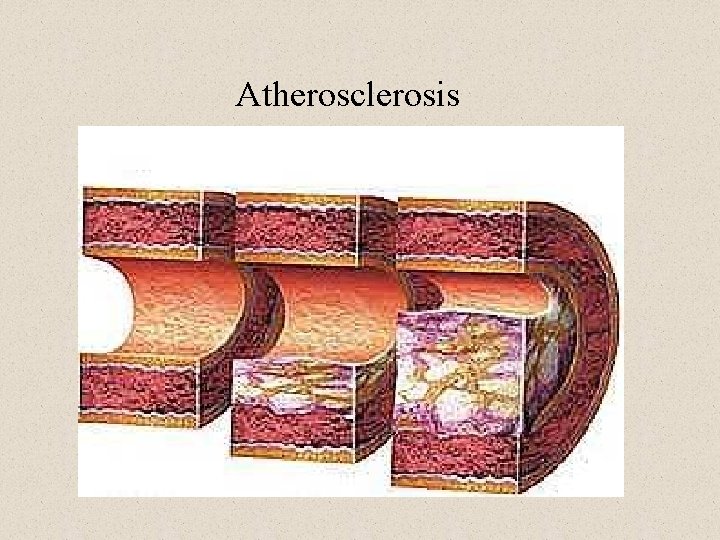
Stages of atherosclerotic plaque development • Type I – isolated foam cells – macrophages with a droplet of fat in intima • Type II – fatty streaks – foam cells layer • Type III – higher amount of lipids under the foam cells layer • Type IV – atheroma – lipid core, fibrous cap • Type V – more collagen and smooth muscle cells in fibrous cap • Type VI – atheroma with complications - thrombosis

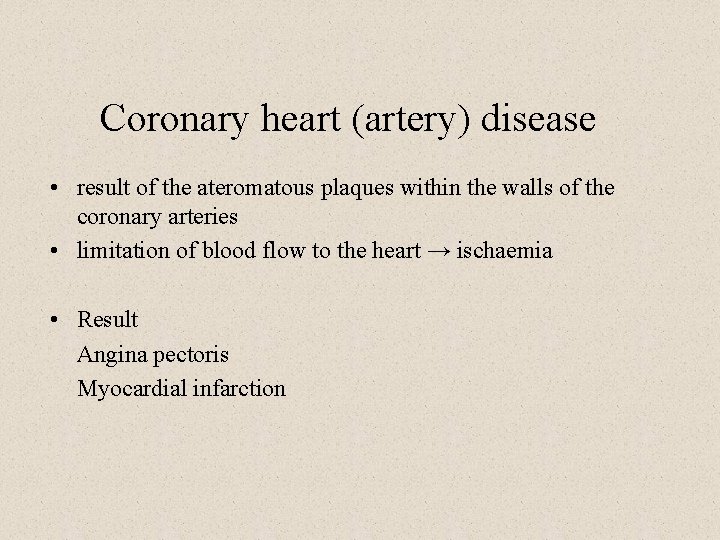
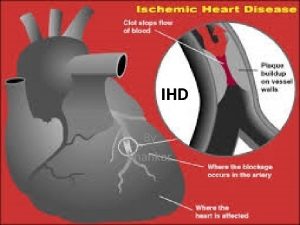
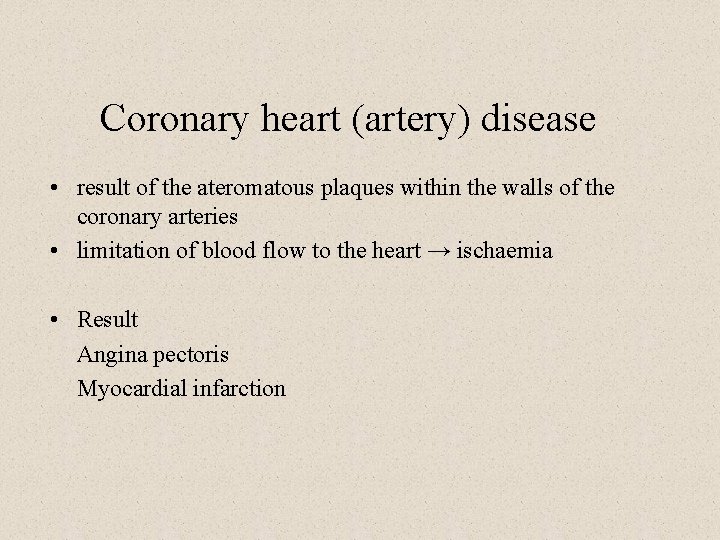
Coronary heart (artery) disease • result of the ateromatous plaques within the walls of the coronary arteries • limitation of blood flow to the heart → ischaemia • Result Angina pectoris Myocardial infarction
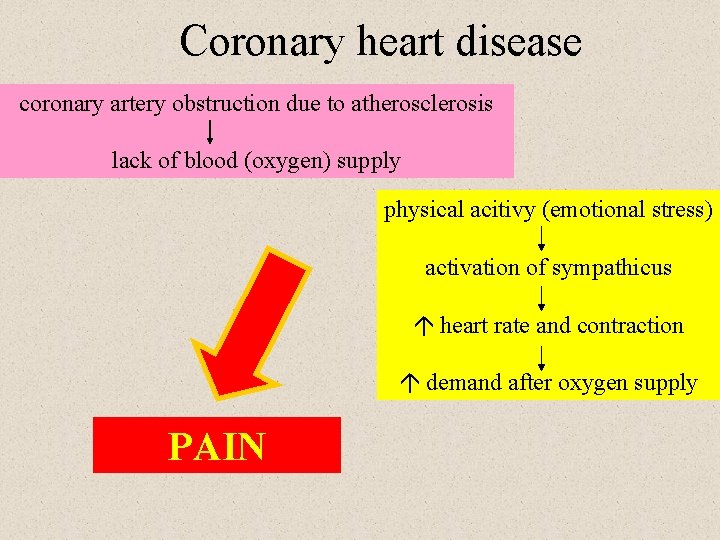
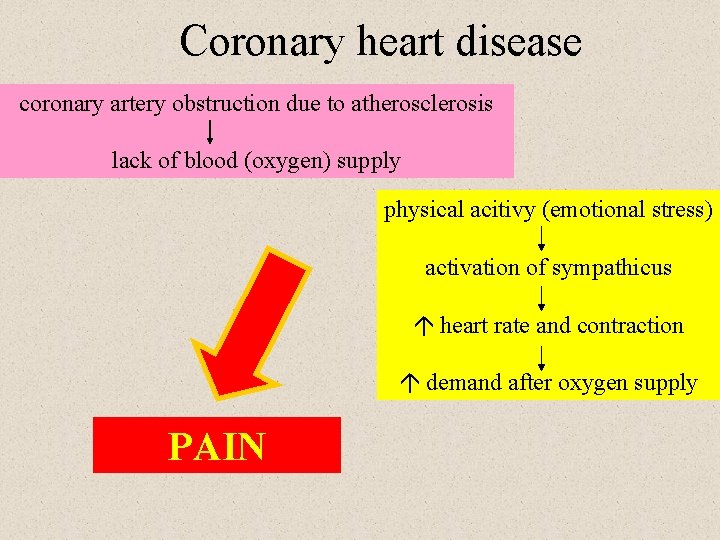
Coronary heart disease coronary artery obstruction due to atherosclerosis lack of blood (oxygen) supply physical acitivy (emotional stress) activation of sympathicus heart rate and contraction demand after oxygen supply PAIN
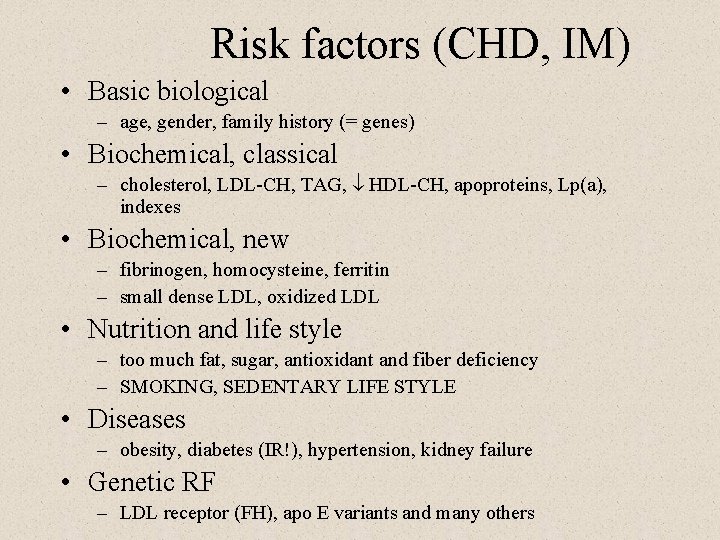
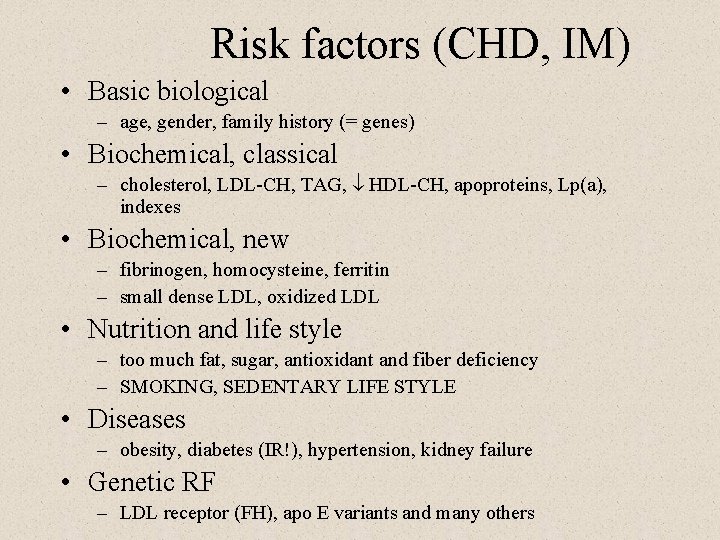
Risk factors (CHD, IM) • Basic biological – age, gender, family history (= genes) • Biochemical, classical – cholesterol, LDL-CH, TAG, ¯ HDL-CH, apoproteins, Lp(a), indexes • Biochemical, new – fibrinogen, homocysteine, ferritin – small dense LDL, oxidized LDL • Nutrition and life style – too much fat, sugar, antioxidant and fiber deficiency – SMOKING, SEDENTARY LIFE STYLE • Diseases – obesity, diabetes (IR!), hypertension, kidney failure • Genetic RF – LDL receptor (FH), apo E variants and many others
Basic biological factors • age – men > 45 years – women after menopause • gender – men > women
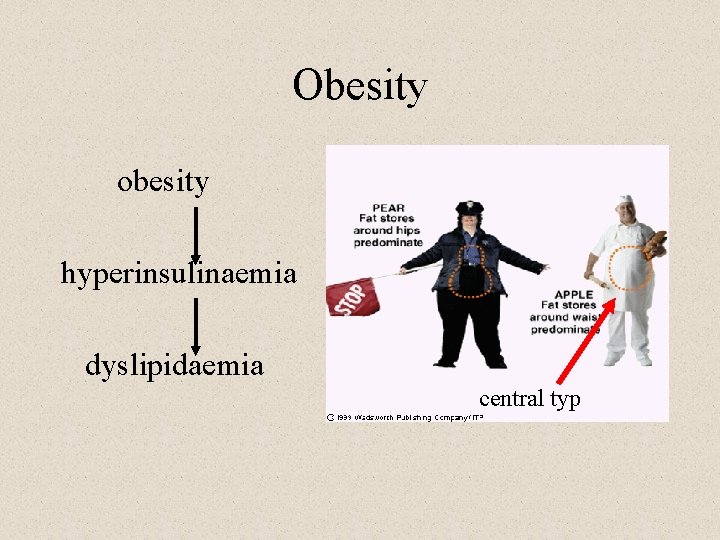
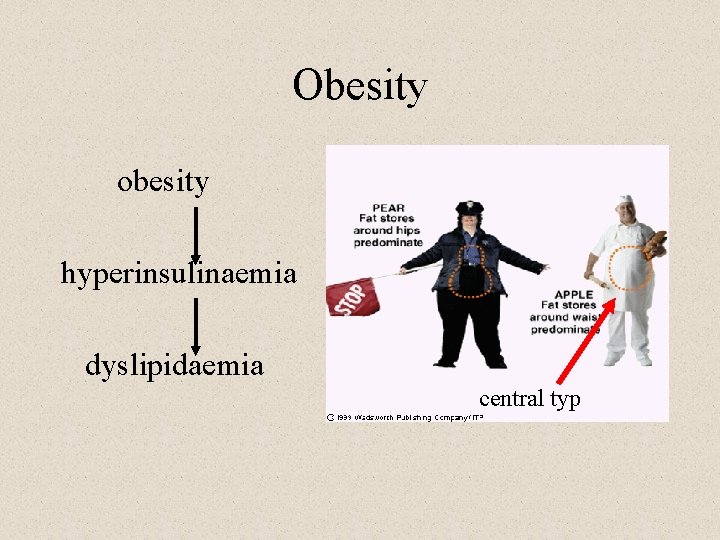
Obesity obesity hyperinsulinaemia dyslipidaemia central typ
Hypertension • endothelium damage
Smoking • nicotine – effect on lipid metabolism – vasoconstriction • CO – carboxyhaemoglobin • increased coagulation cascade activity
Endothel • Intelligent interface between blood and vessel wall/tissues • 1500 g, football field (1000 m 2) • Endocrine, paracrine and autocrine functions – vessel tonus, coagulation, adhesion, cell replication • Organ specificity, differences in arteries, capillaries a venes • Dysfunction in hypertension, diabetes, dyslipidemia. . .
Lipoproteins
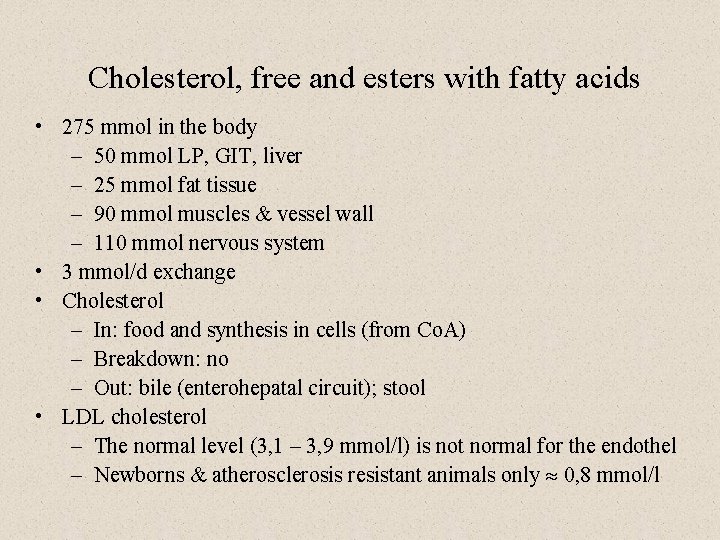
Cholesterol, free and esters with fatty acids • 275 mmol in the body – 50 mmol LP, GIT, liver – 25 mmol fat tissue – 90 mmol muscles & vessel wall – 110 mmol nervous system • 3 mmol/d exchange • Cholesterol – In: food and synthesis in cells (from Co. A) – Breakdown: no – Out: bile (enterohepatal circuit); stool • LDL cholesterol – The normal level (3, 1 – 3, 9 mmol/l) is not normal for the endothel – Newborns & atherosclerosis resistant animals only » 0, 8 mmol/l
Triacylglycerols & fatty acids TAG & FFA • • • 15 kg in nonobese subjects 570 000 k. J; enough for 3 months Thermal isolation, fertility, body shape Intake & synthesis: 80 – 170 mmol/d Different fatty acids – saturated, unsaturated, polyunsaturated (eikosanoids), shorter and longer chain • Rapid turnover dependent on diet and alcohol intake, breakdown through physical activity (FFA – minutes)
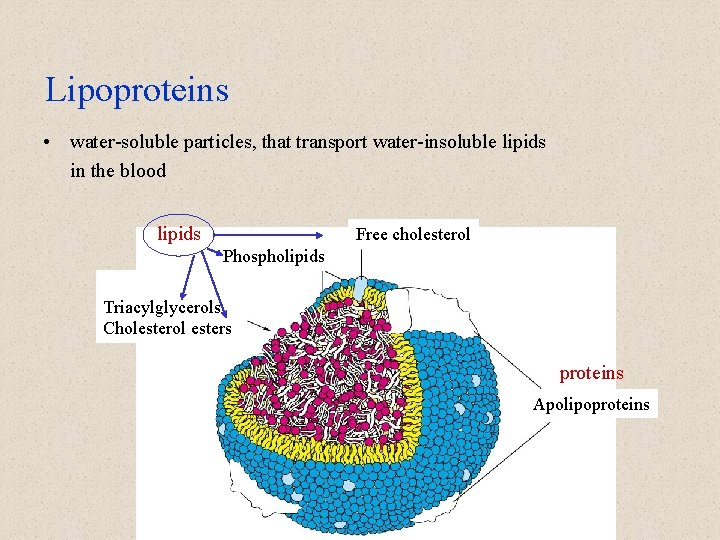
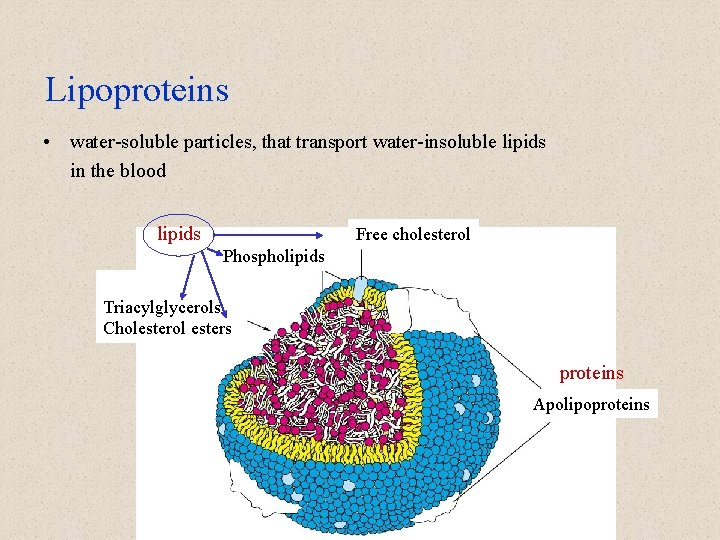
Lipoproteins • water-soluble particles, that transport water-insoluble lipids in the blood lipids Free cholesterol Phospholipids Triacylglycerols Cholesterol esters proteins Apolipoproteins

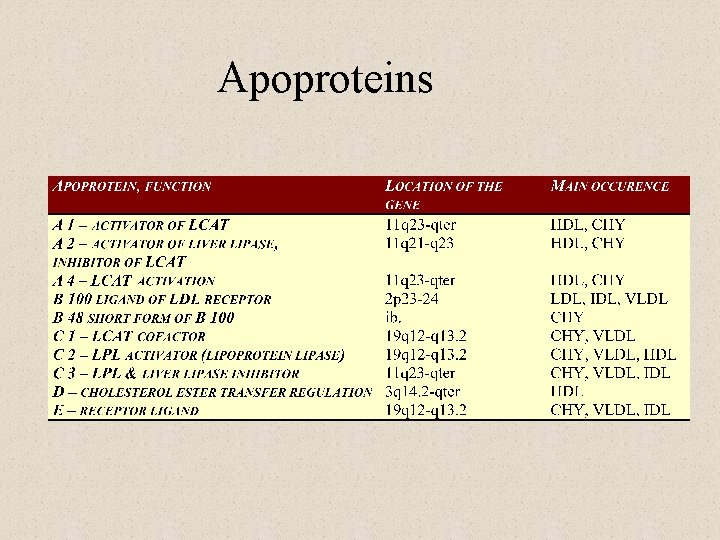
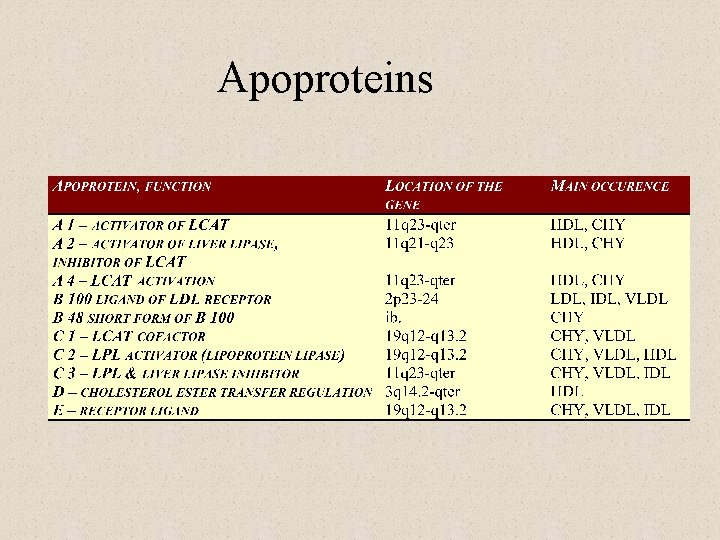
Apoproteins
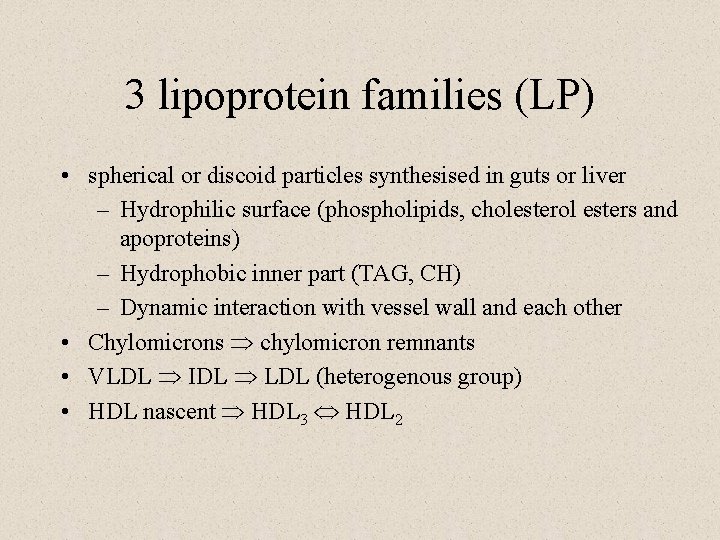
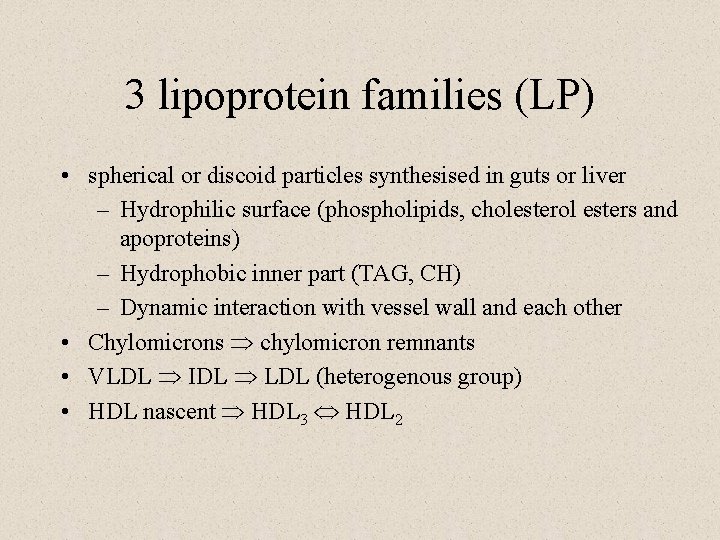
3 lipoprotein families (LP) • spherical or discoid particles synthesised in guts or liver – Hydrophilic surface (phospholipids, cholesterol esters and apoproteins) – Hydrophobic inner part (TAG, CH) – Dynamic interaction with vessel wall and each other • Chylomicrons Þ chylomicron remnants • VLDL Þ IDL Þ LDL (heterogenous group) • HDL nascent Þ HDL 3 Û HDL 2
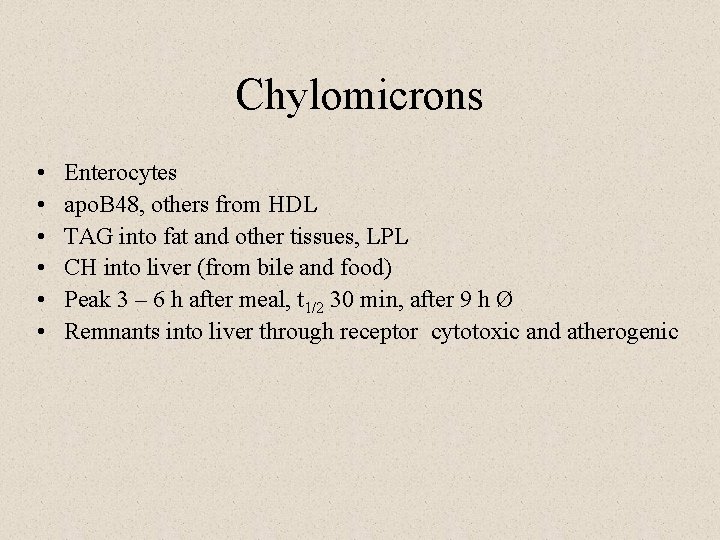
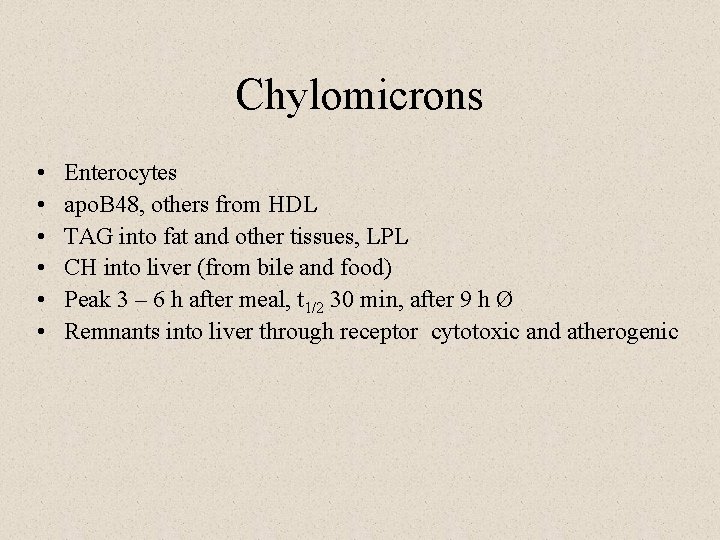
Chylomicrons • • • Enterocytes apo. B 48, others from HDL TAG into fat and other tissues, LPL CH into liver (from bile and food) Peak 3 – 6 h after meal, t 1/2 30 min, after 9 h Ø Remnants into liver through receptor cytotoxic and atherogenic

VLDL – LDL family • • • Liver, endogeneous TAG, CH B 100 and others functions and metabolism similar to CHY VLDL t 1/2 2 – 4 hod, transformation to IDL, LDL has a slow turnover, can be modified – oxidation, glycation • small dense LDL • Receptor and scavenger receptor
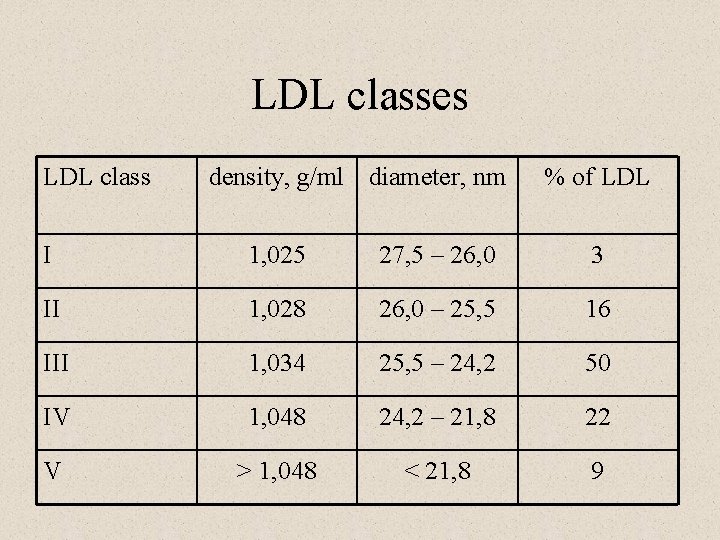
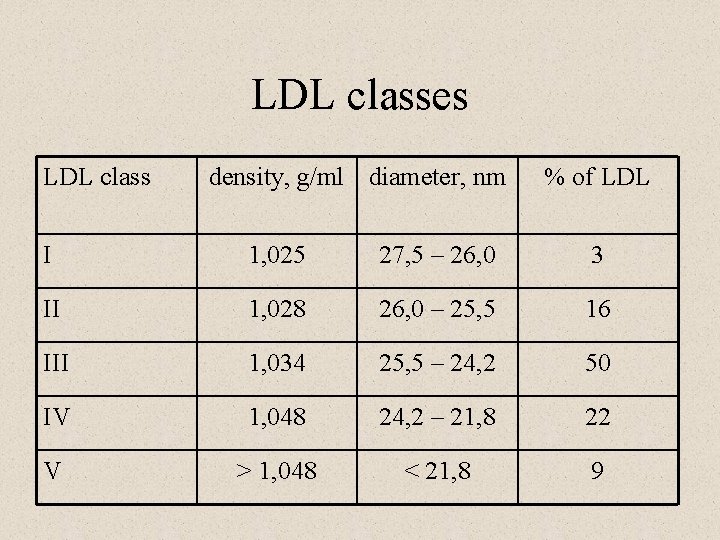
LDL classes LDL class density, g/ml diameter, nm % of LDL I 1, 025 27, 5 – 26, 0 3 II 1, 028 26, 0 – 25, 5 16 III 1, 034 25, 5 – 24, 2 50 IV 1, 048 24, 2 – 21, 8 22 V > 1, 048 < 21, 8 9
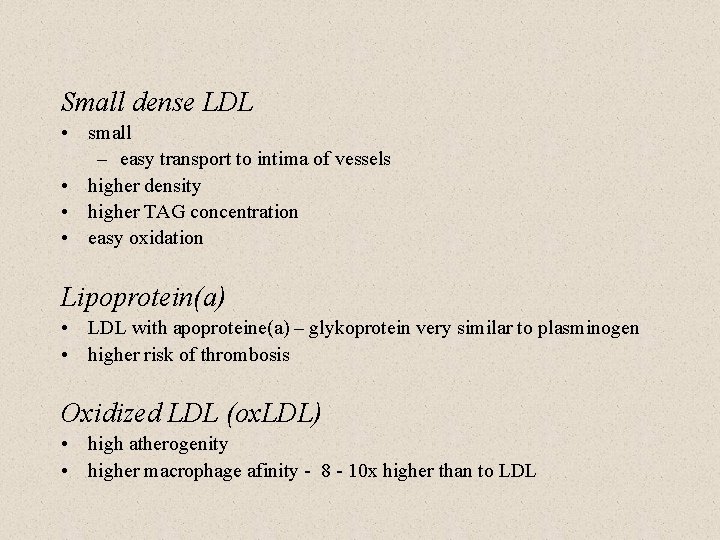
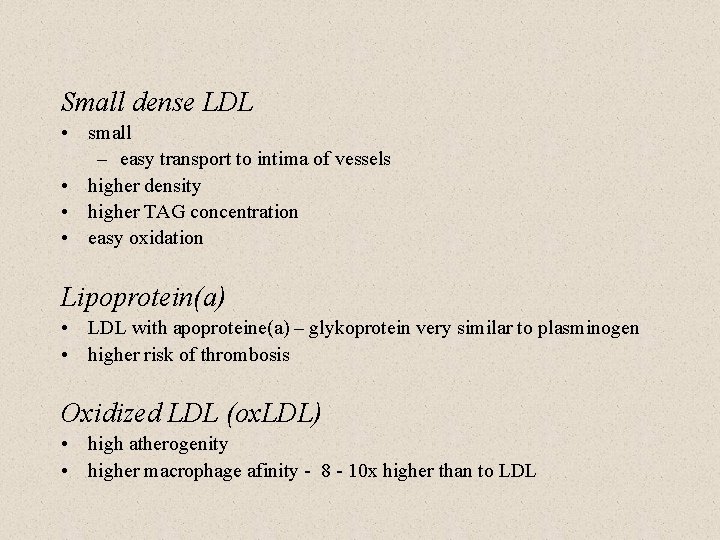
Small dense LDL • small – easy transport to intima of vessels • higher density • higher TAG concentration • easy oxidation Lipoprotein(a) • LDL with apoproteine(a) – glykoprotein very similar to plasminogen • higher risk of thrombosis Oxidized LDL (ox. LDL) • high atherogenity • higher macrophage afinity - 8 - 10 x higher than to LDL
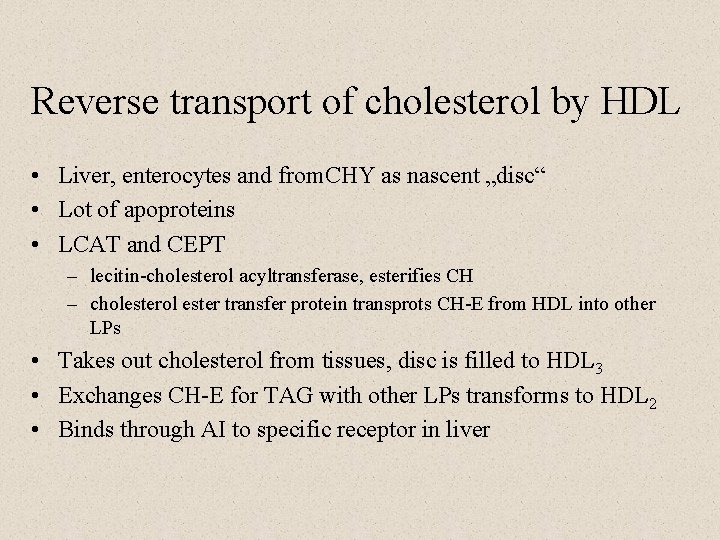
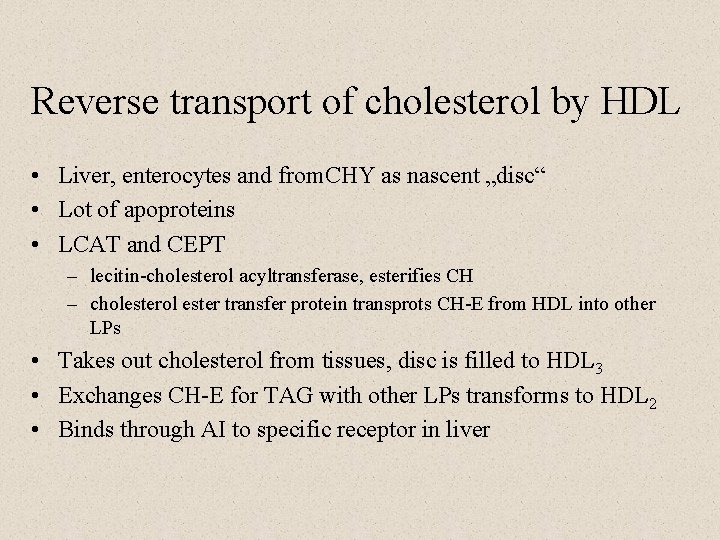
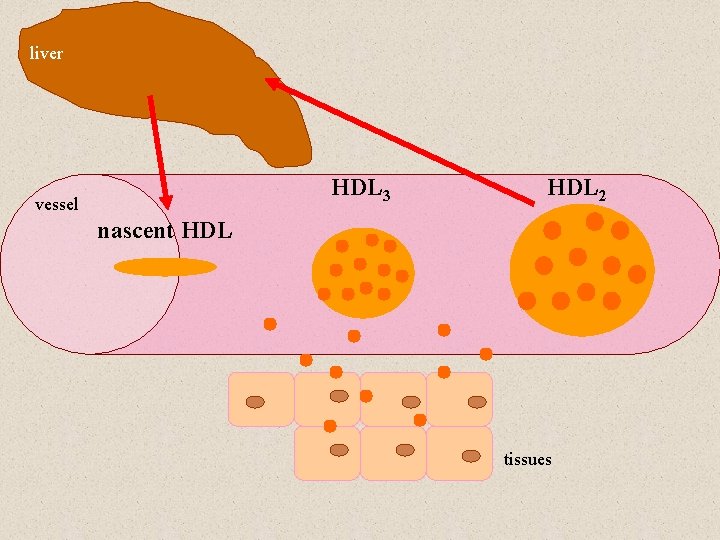
Reverse transport of cholesterol by HDL • Liver, enterocytes and from. CHY as nascent „disc“ • Lot of apoproteins • LCAT and CEPT – lecitin-cholesterol acyltransferase, esterifies CH – cholesterol ester transfer protein transprots CH-E from HDL into other LPs • Takes out cholesterol from tissues, disc is filled to HDL 3 • Exchanges CH-E for TAG with other LPs transforms to HDL 2 • Binds through AI to specific receptor in liver
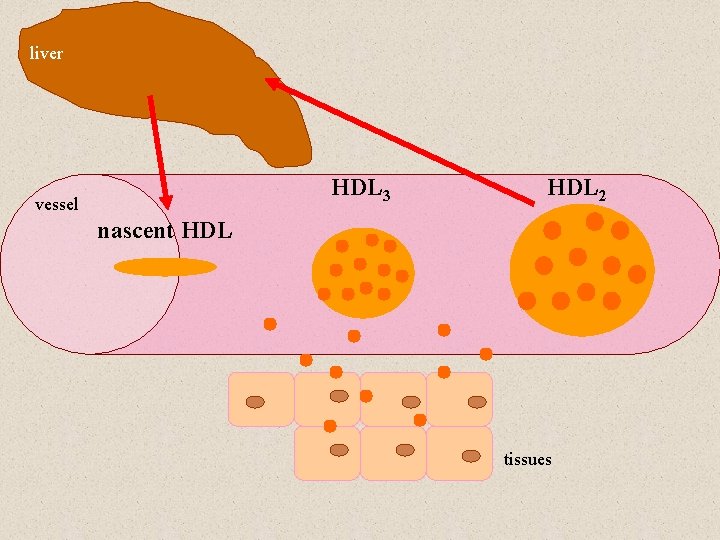
liver HDL 3 vessel HDL 2 nascent HDL tissues
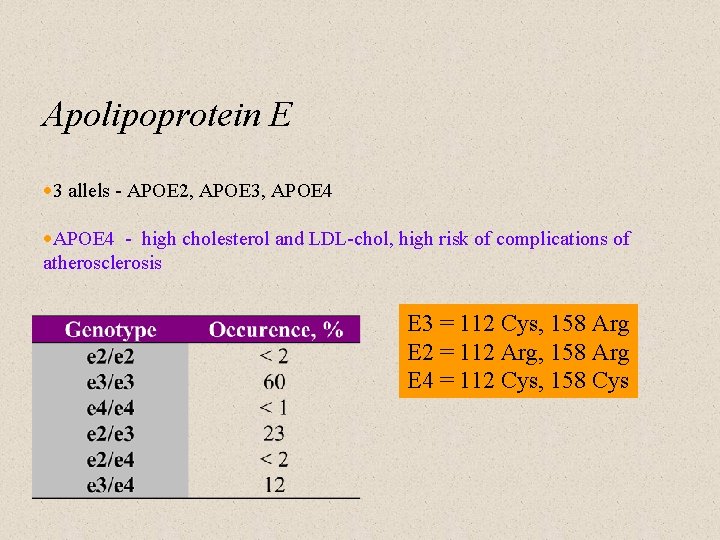
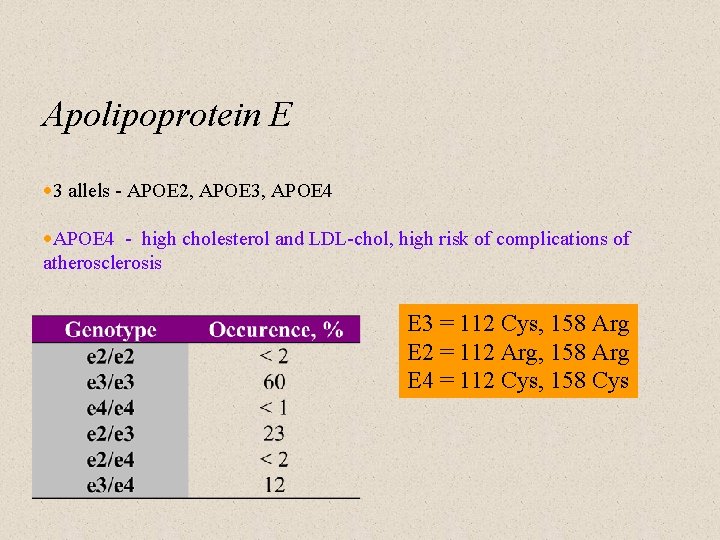
Apolipoprotein E · 3 allels - APOE 2, APOE 3, APOE 4 ·APOE 4 - high cholesterol and LDL-chol, high risk of complications of atherosclerosis E 3 = 112 Cys, 158 Arg E 2 = 112 Arg, 158 Arg E 4 = 112 Cys, 158 Cys
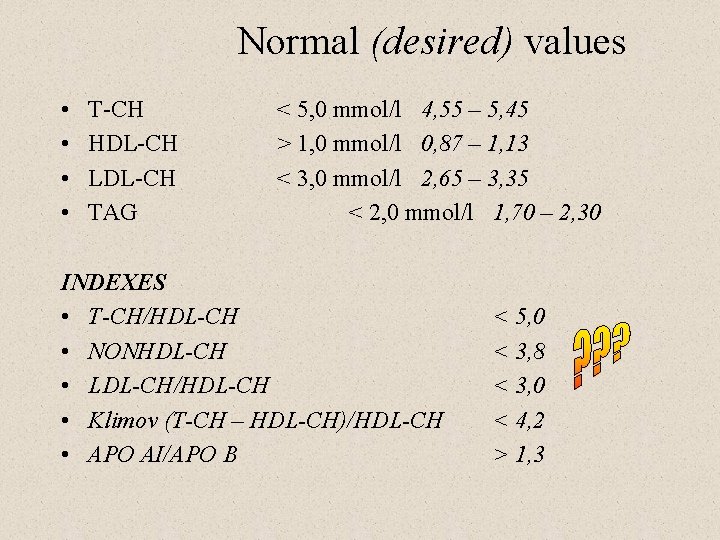
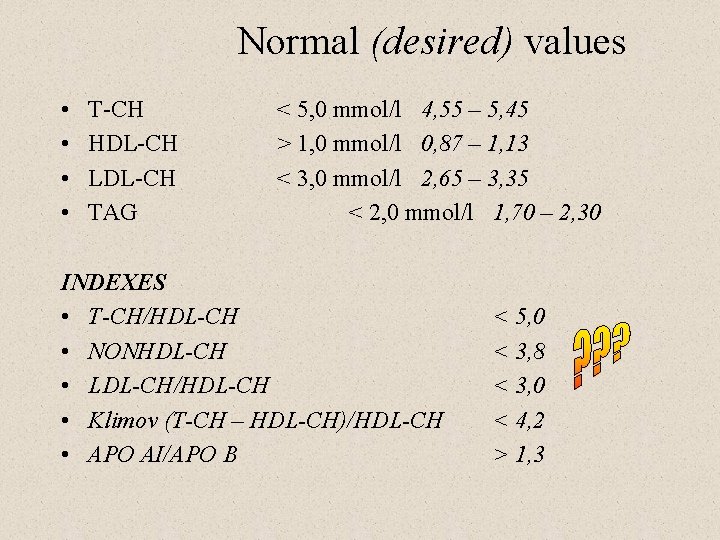
Normal (desired) values • • T-CH HDL-CH LDL-CH TAG < 5, 0 mmol/l 4, 55 – 5, 45 > 1, 0 mmol/l 0, 87 – 1, 13 < 3, 0 mmol/l 2, 65 – 3, 35 < 2, 0 mmol/l 1, 70 – 2, 30 INDEXES • T-CH/HDL-CH • NONHDL-CH • LDL-CH/HDL-CH • Klimov (T-CH – HDL-CH)/HDL-CH • APO AI/APO B < 5, 0 < 3, 8 < 3, 0 < 4, 2 > 1, 3
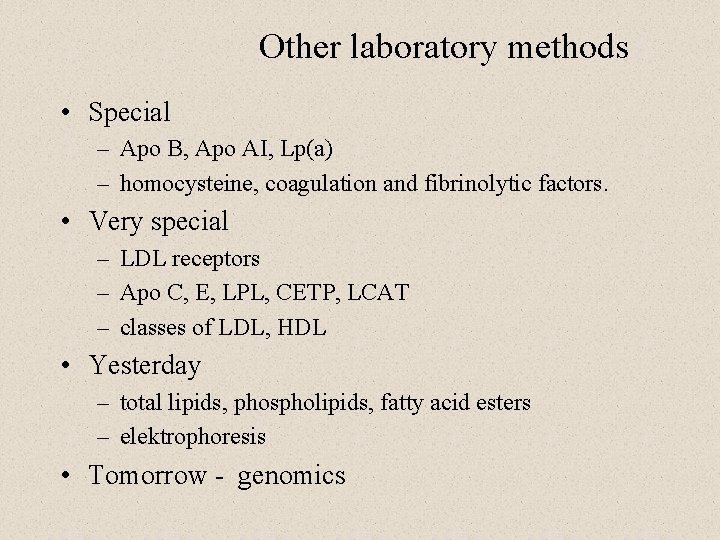
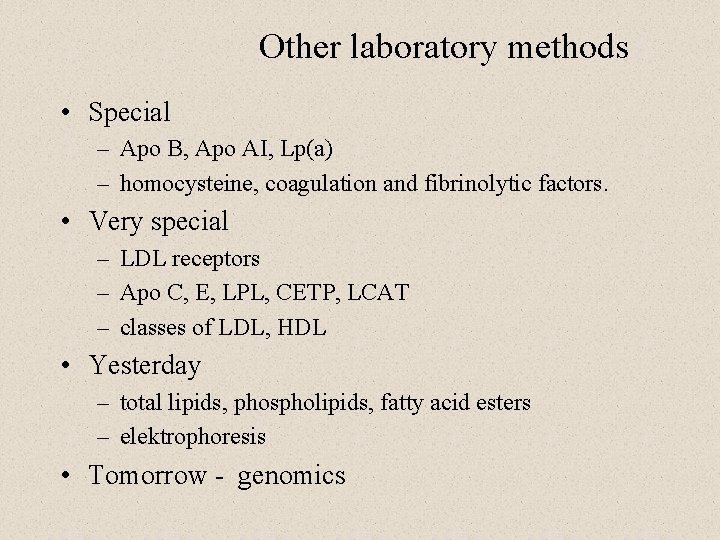
Other laboratory methods • Special – Apo B, Apo AI, Lp(a) – homocysteine, coagulation and fibrinolytic factors. • Very special – LDL receptors – Apo C, E, LPL, CETP, LCAT – classes of LDL, HDL • Yesterday – total lipids, phospholipids, fatty acid esters – elektrophoresis • Tomorrow - genomics
Hyperlipoproteinemias
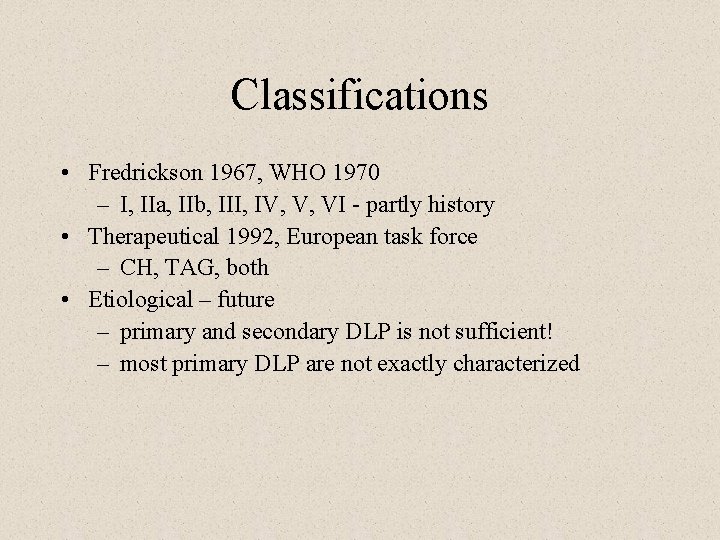
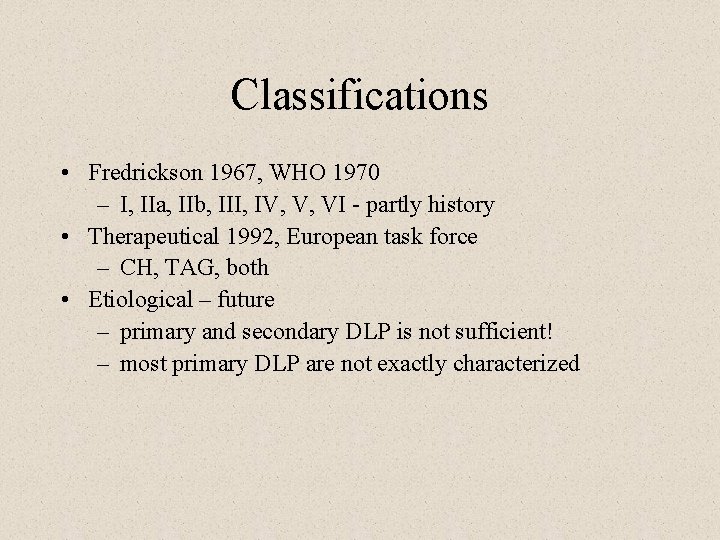
Classifications • Fredrickson 1967, WHO 1970 – I, IIa, IIb, III, IV, V, VI - partly history • Therapeutical 1992, European task force – CH, TAG, both • Etiological – future – primary and secondary DLP is not sufficient! – most primary DLP are not exactly characterized
“Primary DLP” ü ü ? ? Familiar hypercholesterolemia (LDL rec. ) Familiar defect of Apo. B 100 (FDB) Polygenous hypercholesterolemia Polygeneous hypertriglcyceridemia Dysbetalipoproteinemia (IDL) Familiar type V hyperlipidemia
“Secondary DLP” • Nutrition and lifestyle – including smoking, alcohol and micronutrient deficiency • Obesity • Diabetes mellitus – type 2 usually, decompensated type 1 (BG 20 – extreme TAG) • Kidney failure • Liver disease • Endocrine diseases – ß thyroid function • Drugs • Hormones – anticonception, gravidity, postmenopausal, anabolics
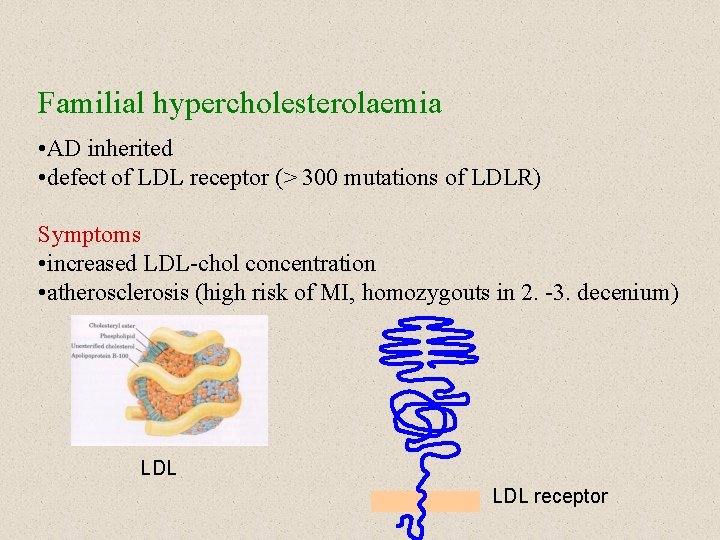
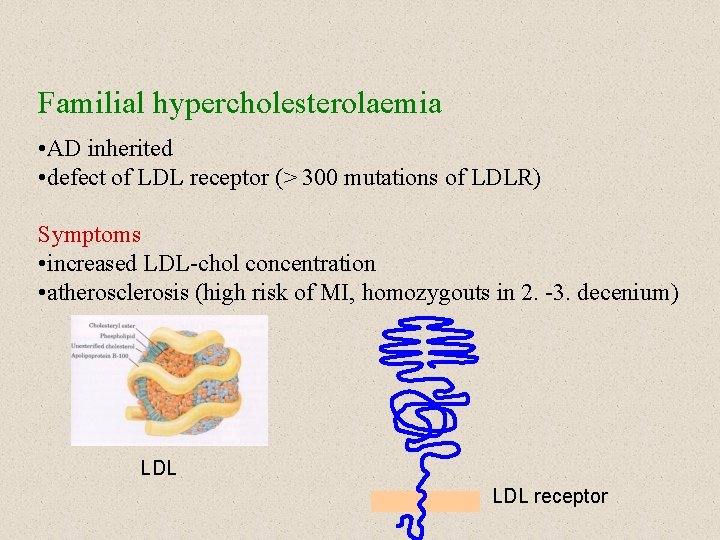
Familial hypercholesterolaemia • AD inherited • defect of LDL receptor (> 300 mutations of LDLR) Symptoms • increased LDL-chol concentration • atherosclerosis (high risk of MI, homozygouts in 2. -3. decenium) LDL receptor
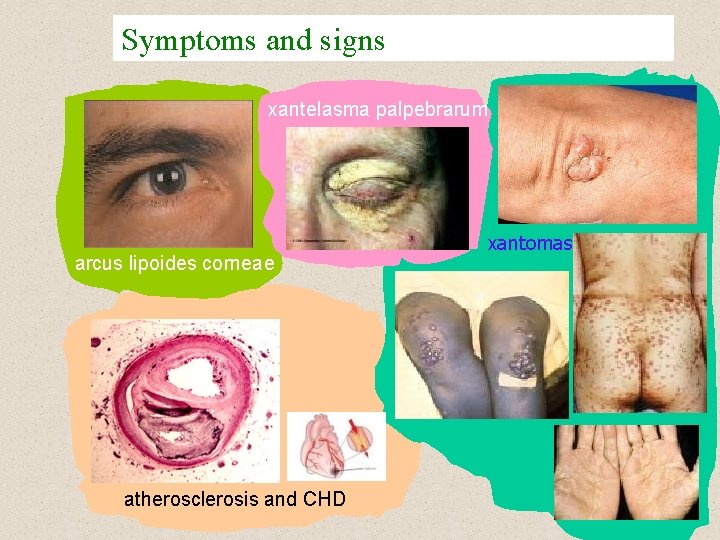
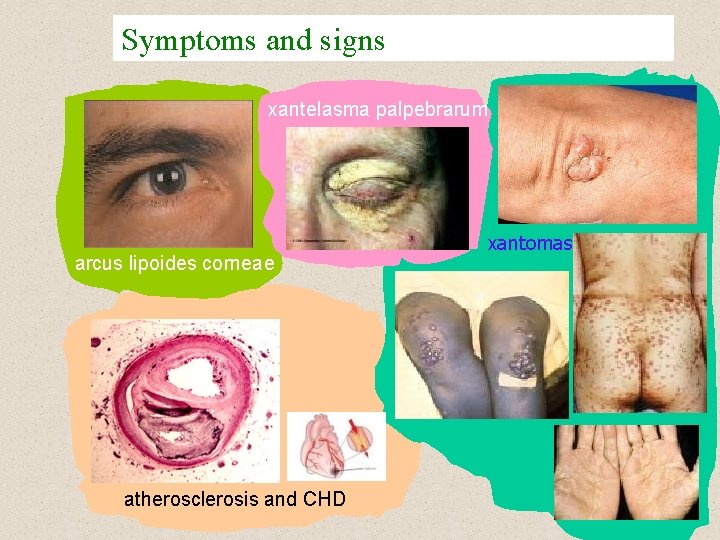
Symptoms and signs xantelasma palpebrarum arcus lipoides corneae atherosclerosis and CHD xantomas
Angina pectoris • severe chest pain due to ischaemia of the heart muscle, due to obstruction of the coronary arteria • Symptoms – after exertion, emotional stress, in the rest – chest pain (or discomfort) – lasting several minutes – referred pain to the arms, shoulders, neck, chin – exacerbated by full stomach or cold temperature – breathlessness, sweating, nausea – pain relieved by nitroglycerin
Types of angina pectoris • Stable AP – stable atherosclerotic plaque – retrosternal pain precipitaded by activity (walking, running) – no pain in rest – 3 – 5 min – referred pain to the arms, shoulders, back. . . • Unstable AP – „crescendo“ angina – unstable atherosclerotic plaque – at rest – > 10 min. – more serious symptoms • Variant (Prinzmetal´s, vasospastic) AP – caused by vasospasm – unknown mechanism (dysfunction of endothelium? ) – atherosclerotic changes – not necessary – at rest (at night, early morning)
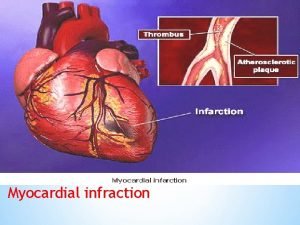
Myocardial infarction • Acute myocardial infarction • Heart attack • Necrosis of the heart cells due to interruption of blood supply to the part of the heart Causes • rupture of the ustable atherosclerotic plaque → trombosis • coronary artery obstruction by the stable plaque
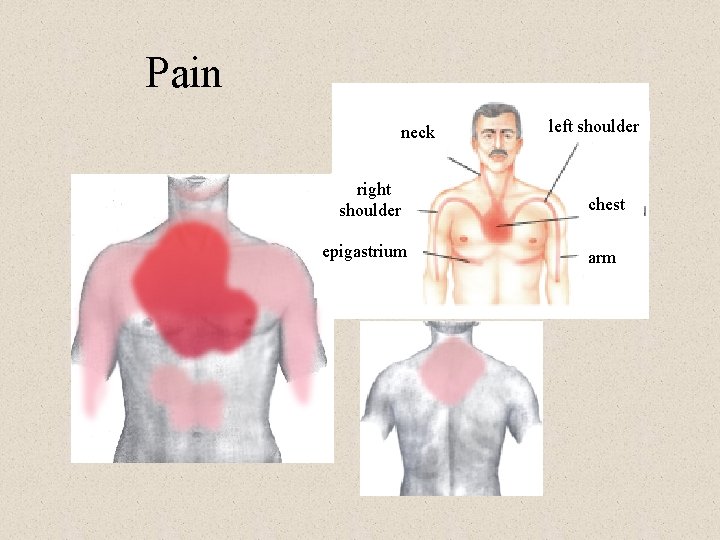
• Signs and symptoms – sudden chest pain radiating to the left arm, shoulder, neck, chin. . . – pain not relieved by nitroglycerin – anxiety – nausea, vomiting, sweating – dyspnea – pale, cold skin – cardiogenic shock symptoms • arterial pressure decrease • tachycardia – sometimes silent ischaemia – without pain (e. g. diabetic neuropathy)
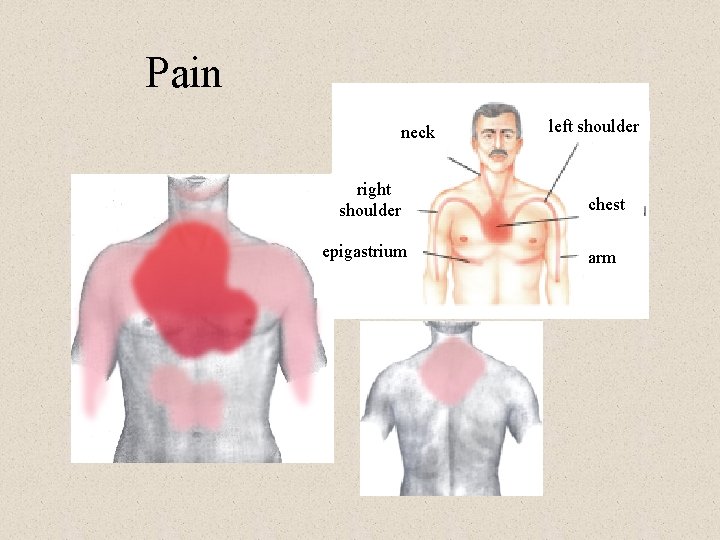
Pain neck right shoulder epigastrium left shoulder chest arm

ECG diagnosis T wave inverion ST segment elevation patological Q wave
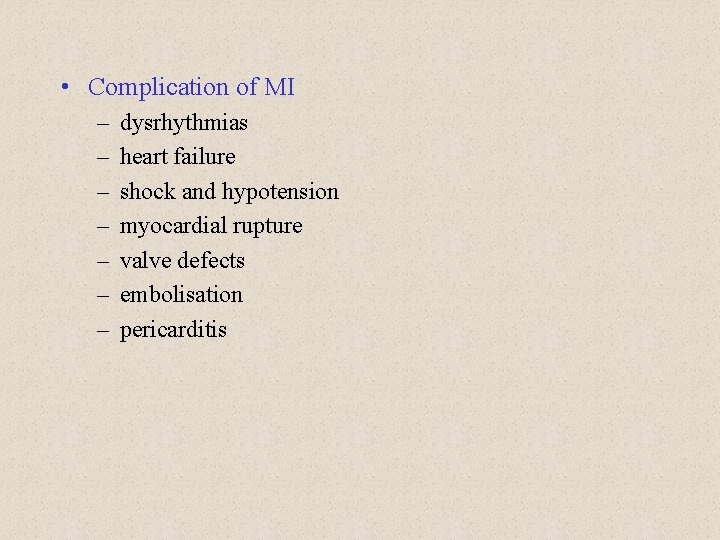
• Complication of MI – – – – dysrhythmias heart failure shock and hypotension myocardial rupture valve defects embolisation pericarditis
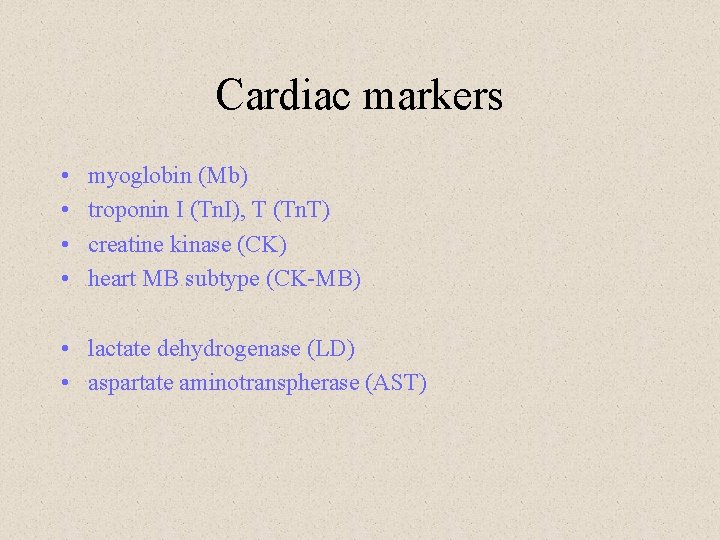
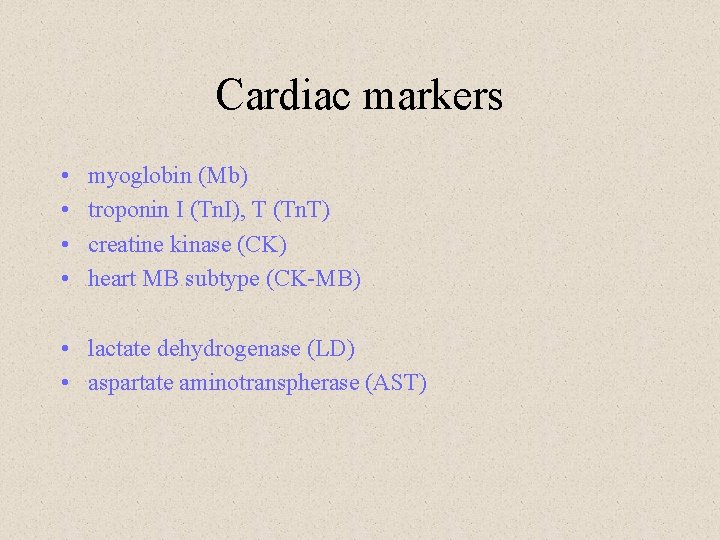
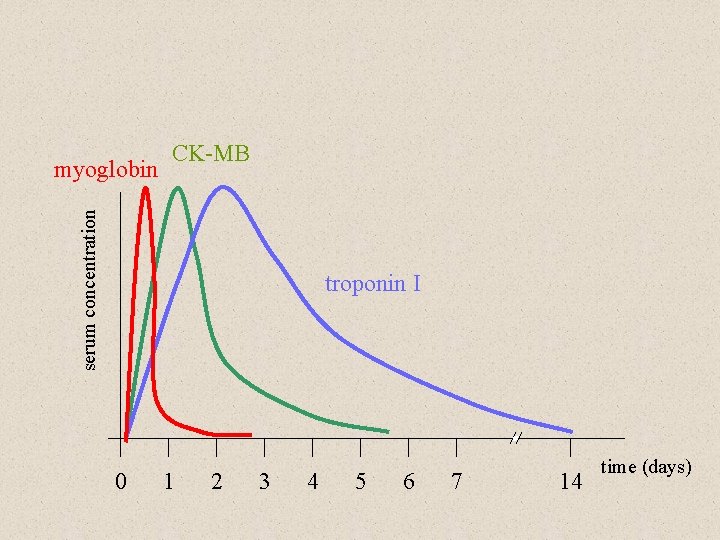
Cardiac markers • • myoglobin (Mb) troponin I (Tn. I), T (Tn. T) creatine kinase (CK) heart MB subtype (CK-MB) • lactate dehydrogenase (LD) • aspartate aminotranspherase (AST)
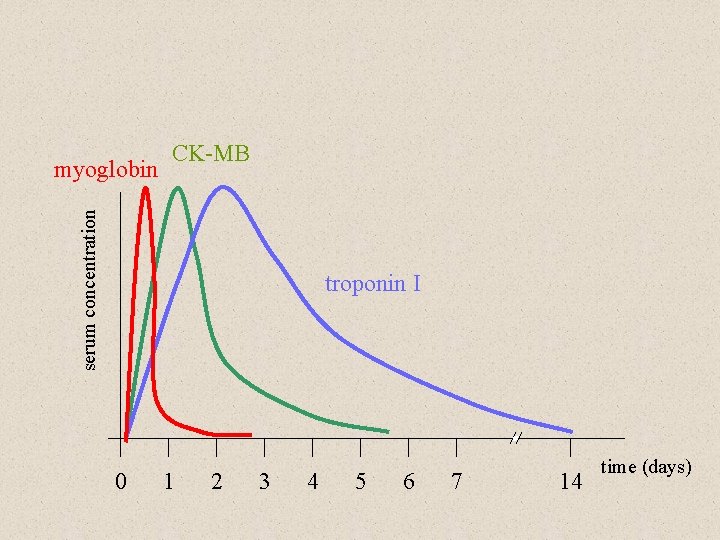
serum concentration myoglobin CK-MB troponin I 0 1 2 3 4 5 6 7 14 time (days)
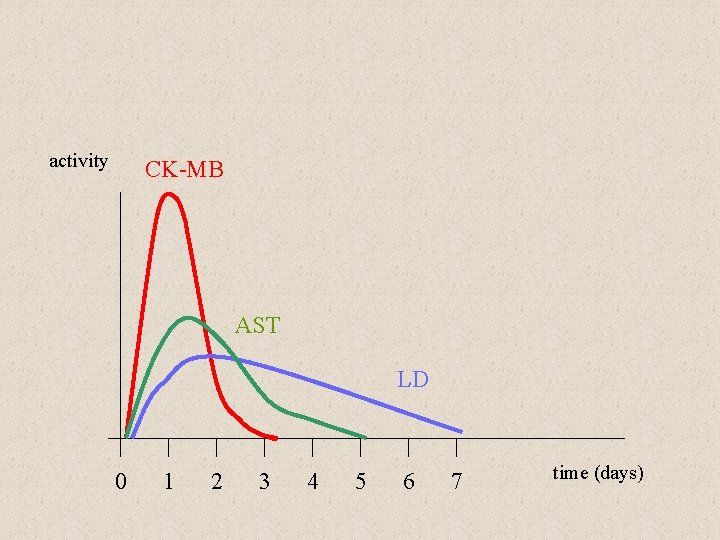
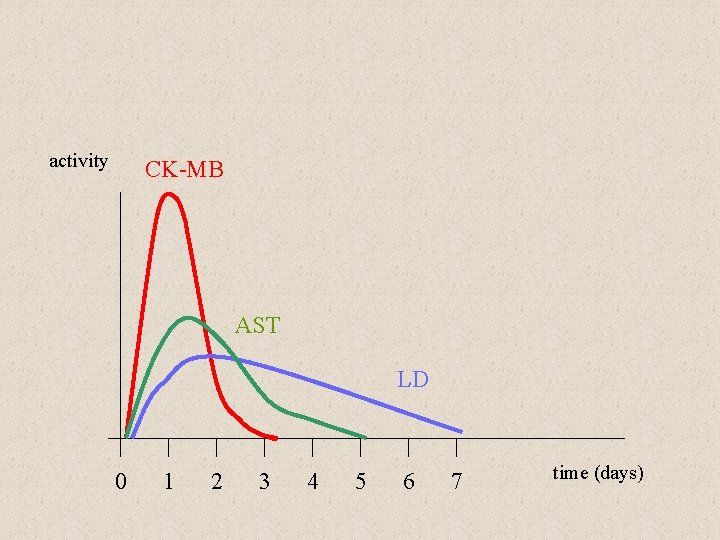
activity CK-MB AST LD 0 1 2 3 4 5 6 7 time (days)
• Complication of MI – – – – dysrhythmias heart failure shock and hypotension myocardial rupture valve defects embolisation pericarditis
 Wall stemi
Wall stemi Pancreas wiki
Pancreas wiki Pico question myocardial infarction
Pico question myocardial infarction Acute pericarditis
Acute pericarditis Myocardial infarction
Myocardial infarction Heart disease
Heart disease Coronary heart disease
Coronary heart disease Nitroglycerin srdce
Nitroglycerin srdce Angina pectoris
Angina pectoris Nursing care plan on angina pectoris
Nursing care plan on angina pectoris Angina pectoris pathophysiology
Angina pectoris pathophysiology Unstable angina vs stable angina
Unstable angina vs stable angina Coronary artery disease
Coronary artery disease Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Circulatory system crash course
Circulatory system crash course Cardiac plexus
Cardiac plexus Coronary circulation of heart
Coronary circulation of heart Gross
Gross Unifocal pvc
Unifocal pvc Os cuboideus
Os cuboideus Myocardial ischemia meaning
Myocardial ischemia meaning Atherosclerosis
Atherosclerosis Radial pulse
Radial pulse Atherosclerosis
Atherosclerosis Atherosclerosis tunica intima
Atherosclerosis tunica intima Variant angina
Variant angina Atherosclerosis
Atherosclerosis Atherosclerosis
Atherosclerosis Dna structure
Dna structure Atherosclerosis
Atherosclerosis Bharathi viswanathan
Bharathi viswanathan Medici antiqui pectoris
Medici antiqui pectoris Medici antiqui pectoris
Medici antiqui pectoris Medici antiqui pectoris
Medici antiqui pectoris Body mekanik
Body mekanik Where is the pulmonary semilunar valve located
Where is the pulmonary semilunar valve located Flow of coronary circulation
Flow of coronary circulation Coronary sinus opening
Coronary sinus opening Qfr coronary
Qfr coronary Glisson capsule
Glisson capsule Coronary circulatory routes
Coronary circulatory routes Global registry of acute coronary events
Global registry of acute coronary events Dipyrimadole
Dipyrimadole 3 main functions heart
3 main functions heart Mesa coronary calcium score
Mesa coronary calcium score Acute coronary syndrome
Acute coronary syndrome Coronary sinusoids
Coronary sinusoids Coronary circulation
Coronary circulation Mesa coronary calcium score
Mesa coronary calcium score Chronic coronary syndrome
Chronic coronary syndrome