Atherosclerosis is the condition in which an artery

- Slides: 25
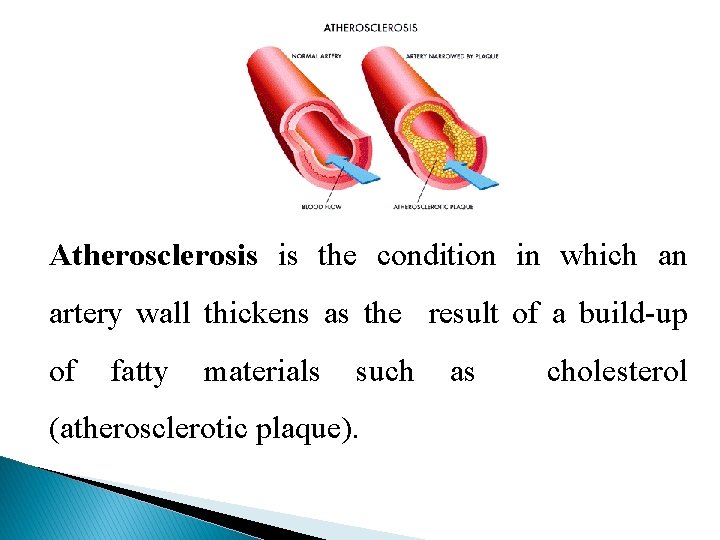
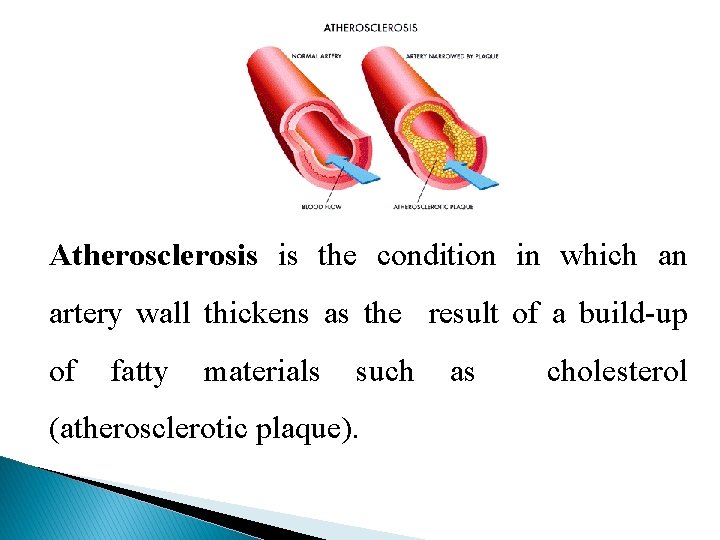
Atherosclerosis is the condition in which an artery wall thickens as the result of a build-up of fatty materials such (atherosclerotic plaque). as cholesterol
• It is caused by the formation of multiple plaques within the arteries. • It can restrict blood flow. These plaques can also burst, causing a blood clot. • Although atherosclerosis is often considered a heart problem, it can affect arteries anywhere in your body. • Atherosclerosis is a preventable and treatable condition.
TERMS • Arteriosclerosis is a general term describing any hardening (and loss of elasticity) of medium or large arteries • Arteriolosclerosis is any hardening (and loss of elasticity) of arterioles (small arteries); • Atherosclerosis is a hardening of an artery specifically due to an atheromatous plaque. • Atherogenic is used for substances or processes that cause atherosclerosis. • Atherogenesis is atheromatous plaques the developmental process of
CAUSES Atherosclerosis starts with damage or injury to the inner layer of an artery. The damage may be caused by: • High blood pressure • High cholesterol • An irritant, such as nicotine • Certain diseases, such as diabetes • Family history • Lack of exercise • Unhealthy diet
Pathophysiology • Atherosclerosis develops as a chronic inflammatory response of the arterial wall to endothelial injury. • Lesion progression occurs through interactions lipoproteins, monocyte-derived of modified macrophages, T-lymphocytes, and the normal cellular constituent of the arterial wall. • The contemporary view of atherosclerosis is response-to-injury hypothesis. expressed by the
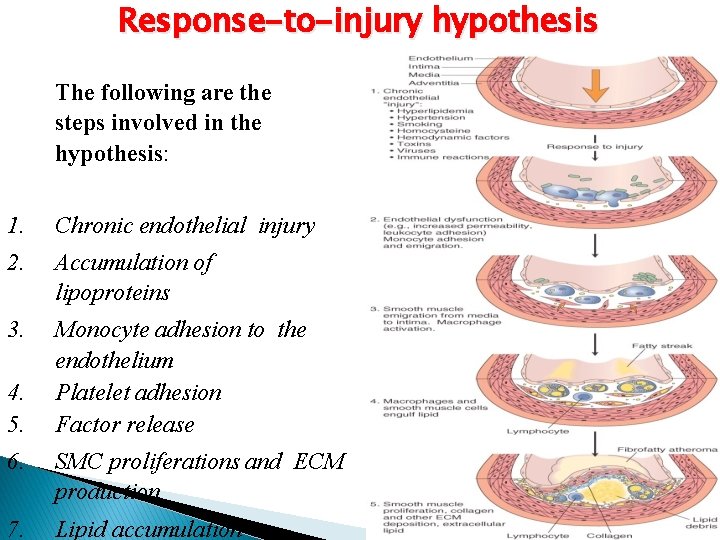
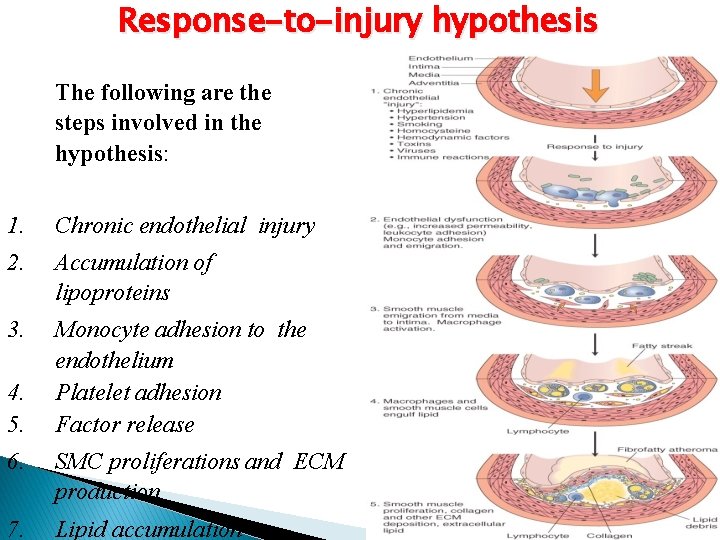
Response-to-injury hypothesis The following are the steps involved in the hypothesis: 1. Chronic endothelial injury 2. Accumulation of lipoproteins 3. Monocyte adhesion to the endothelium Platelet adhesion Factor release 4. 5. 6. SMC proliferations and ECM production 7. Lipid accumulation
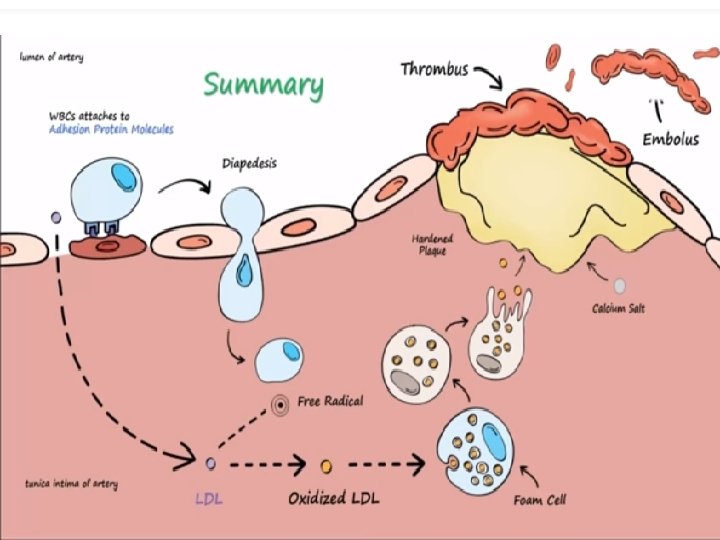
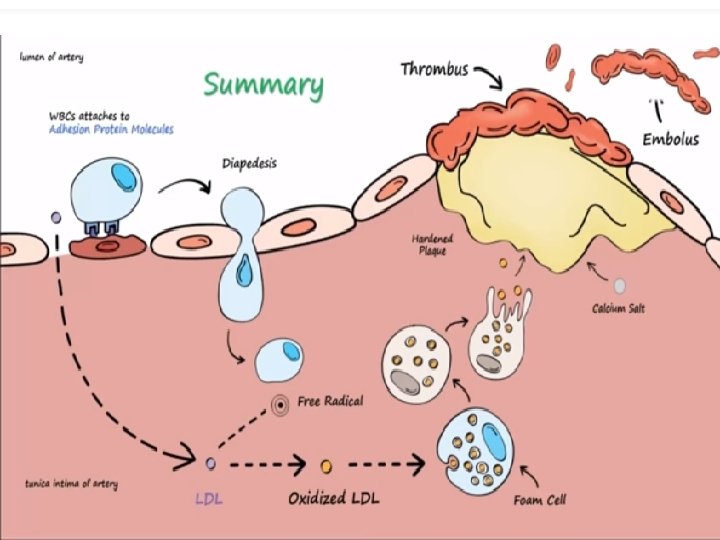
Response-to-injury hypothesis 1. Chronic endothelial injury With resultant endothelial dysfunction, causing increased permeability, leukocyte adhesion, and thrombosis. 2. Accumulation of lipoproteins Mainly LDL (Low density lipoproteins) & its oxidised forms (ldl-ox) by free radicals. When oxidized LDL comes in contact with an artery wall, a series of reactions occur to repair the damage to the artery wall caused by oxidized LDL
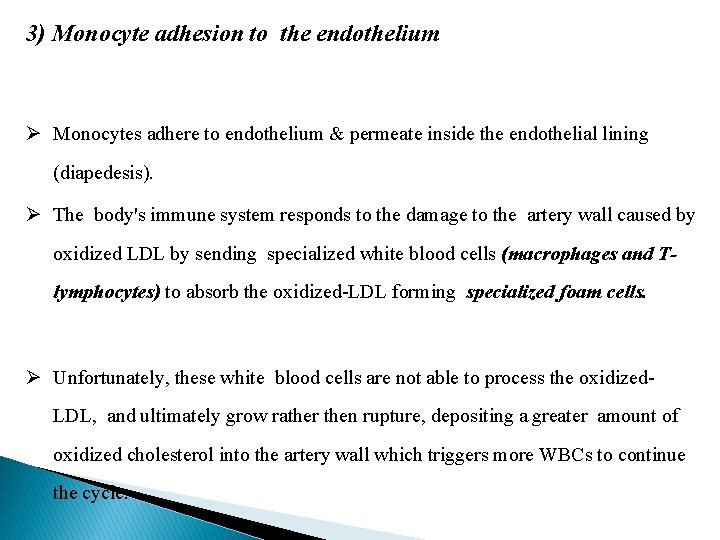
3) Monocyte adhesion to the endothelium Ø Monocytes adhere to endothelium & permeate inside the endothelial lining (diapedesis). Ø The body's immune system responds to the damage to the artery wall caused by oxidized LDL by sending specialized white blood cells (macrophages and Tlymphocytes) to absorb the oxidized-LDL forming specialized foam cells. Ø Unfortunately, these white blood cells are not able to process the oxidized. LDL, and ultimately grow rather then rupture, depositing a greater amount of oxidized cholesterol into the artery wall which triggers more WBCs to continue the cycle.
4. Platelet adhesion 5. Factor release From activated platelet & macrophages, factors are released inducing SMC (smooth muscle cell) recruitment from the media. 6. SMC proliferations and ECM (Extracellular matrix) production. Eventually, the artery becomes inflamed. The cholesterol plaque causes the smooth muscle cells to enlarge and form a hard cover the affected area. This hard cover is what causes a narrowing of the artery, reduces the blood flow and increases blood pressure.
7. Lipid accumulation • Lipids are accumulated in macrophages, T- lymphocytes & smooth muscle cells giving rising to fatty streaks which on further evolution gives rise to atheromatic plaques.
Symptoms Develops gradually Begins in early adolescence Found in major arteries
Atherosclerosis symptoms depend on which arteries are affected v Atherosclerosis in heart arteries - chest pain (angina). v Atherosclerosis in the arteries leading to brain - sudden numbness or weakness in arms or legs, difficulty in speaking or slurred speech. v Atherosclerosis in the arteries in arms and legs - leg pain when walking
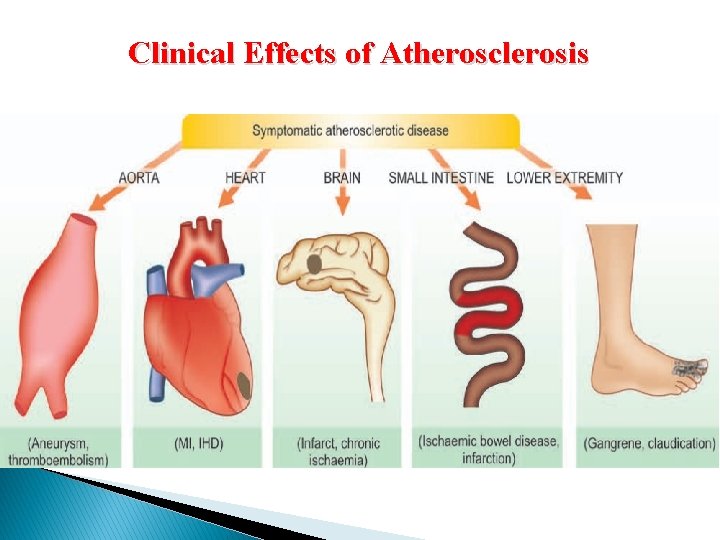
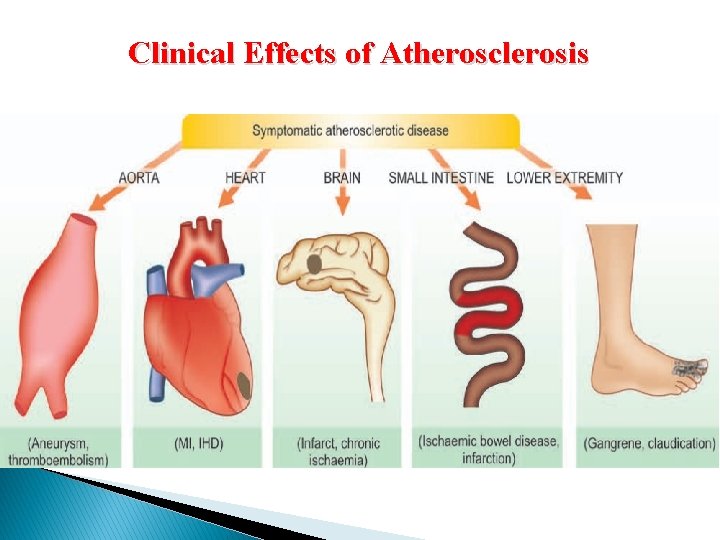
Clinical Effects of Atherosclerosis
Complications The complications of atherosclerosis depend on the location of the blocked arteries. For example: • Coronary artery disease - When atherosclerosis narrows the arteries close to heart that can cause chest pain (angina) or a heart attack. • Carotid artery disease - When atherosclerosis narrows the arteries close to brain that can cause a transient ischemic attack (TIA) or stroke.
• Peripheral artery disease. When atherosclerosis narrows the arteries in arms or legs it may develop circulation problems. This can increase the risk of burns or frostbite. In rare cases it can cause tissue death (gangrene). • Aneurysms. Atherosclerosis can also cause aneurysms which can occur anywhere in the body. An aneurysm is a bulge in the wall of the artery. If an aneurysm bursts it may cause life-threatening internal bleeding.
Tests and diagnosis 1) Blood tests- Lab tests can detect increased levels of cholesterol and blood sugar that may increase the risk of atherosclerosis. 2) Doppler ultrasound- Is a special ultrasound device to measure blood pressure at various points along arm or leg.
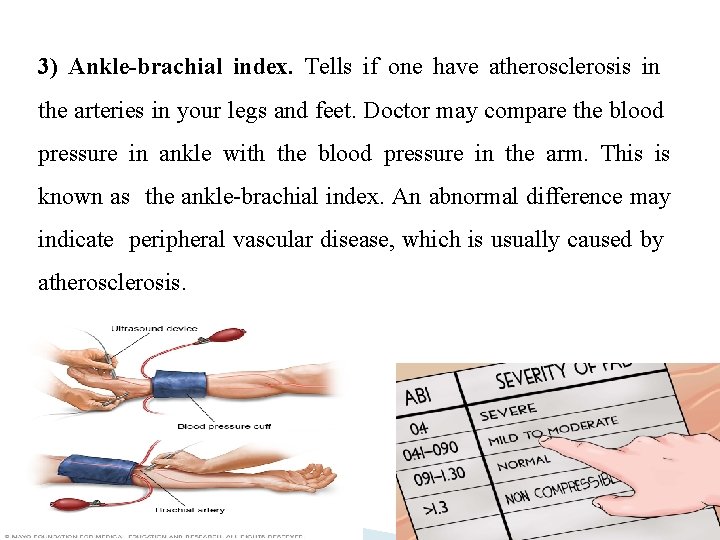
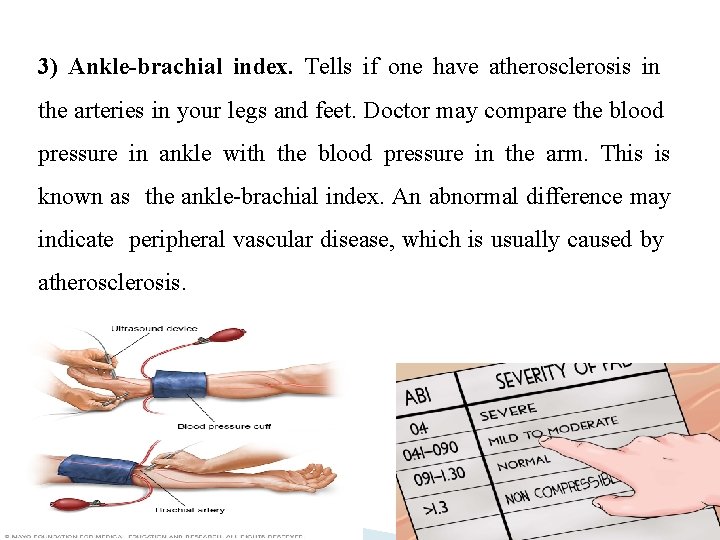
3) Ankle-brachial index. Tells if one have atherosclerosis in the arteries in your legs and feet. Doctor may compare the blood pressure in ankle with the blood pressure in the arm. This is known as the ankle-brachial index. An abnormal difference may indicate peripheral vascular disease, which is usually caused by atherosclerosis.
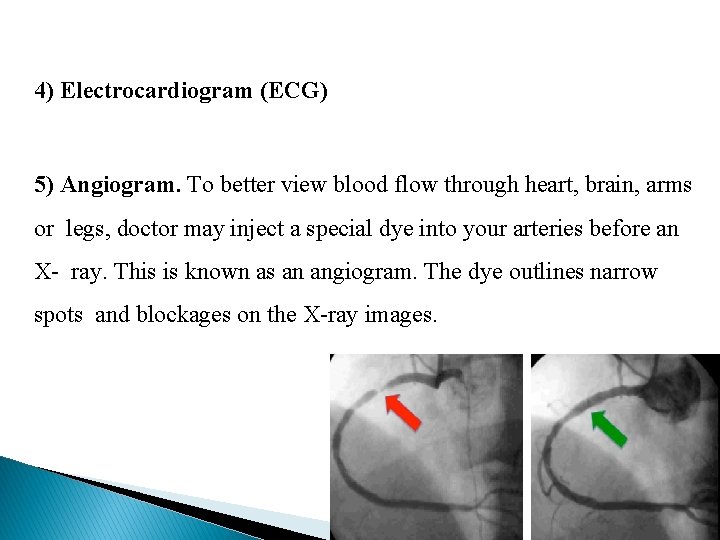
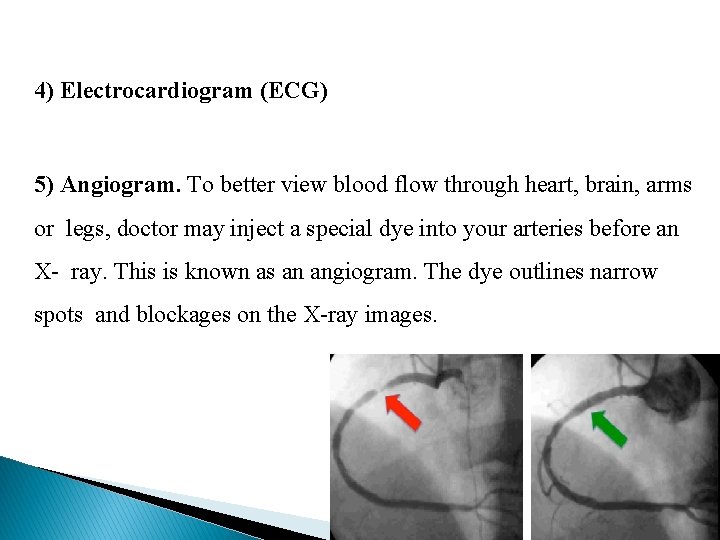
4) Electrocardiogram (ECG) 5) Angiogram. To better view blood flow through heart, brain, arms or legs, doctor may inject a special dye into your arteries before an X- ray. This is known as an angiogram. The dye outlines narrow spots and blockages on the X-ray images.
Treatment of Atherosclerosis 1) Cholesterol lowering medications – statins & fibrates 2) Anti-platelet medications – e. g. aspirin to reduce the likelihood that platelets will clump in narrowed arteries, form a blood clot and cause further blockage. 3) Anticoagulants – e. g. heparin or warfarin can help thin blood to prevent clots from forming. 4) Blood pressure medications - Medications to control blood pressure, such as beta blockers, ACE inhibitors and calcium channel blockers, can slow the progression of atherosclerosis
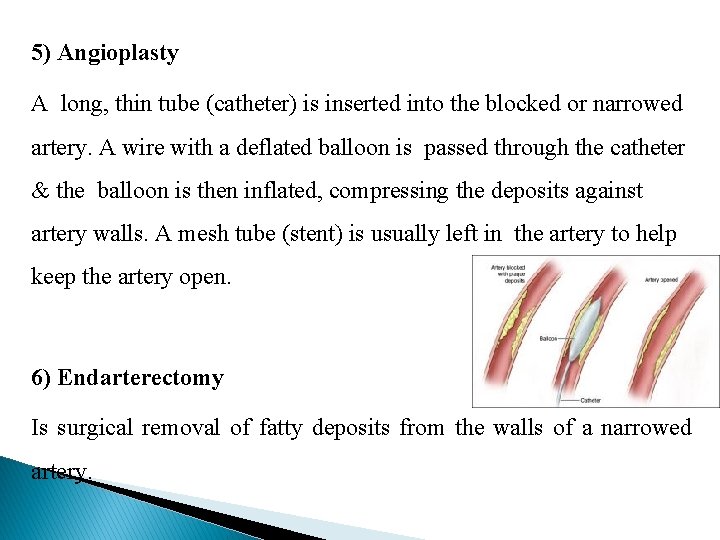
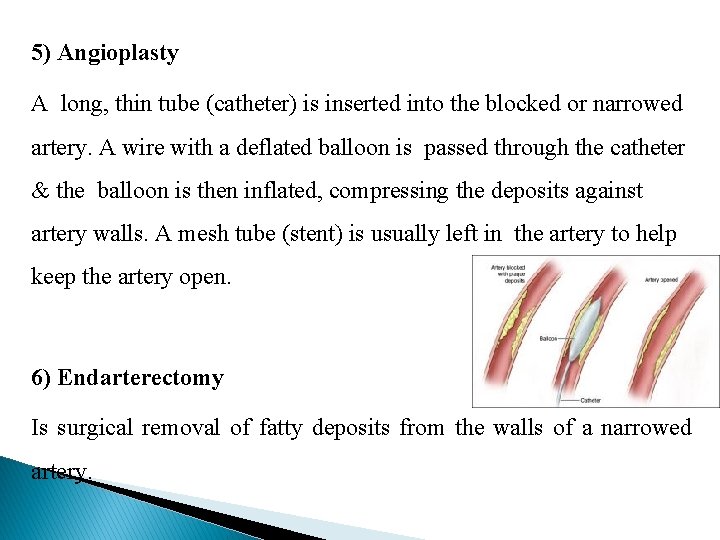
5) Angioplasty A long, thin tube (catheter) is inserted into the blocked or narrowed artery. A wire with a deflated balloon is passed through the catheter & the balloon is then inflated, compressing the deposits against artery walls. A mesh tube (stent) is usually left in the artery to help keep the artery open. 6) Endarterectomy Is surgical removal of fatty deposits from the walls of a narrowed artery.
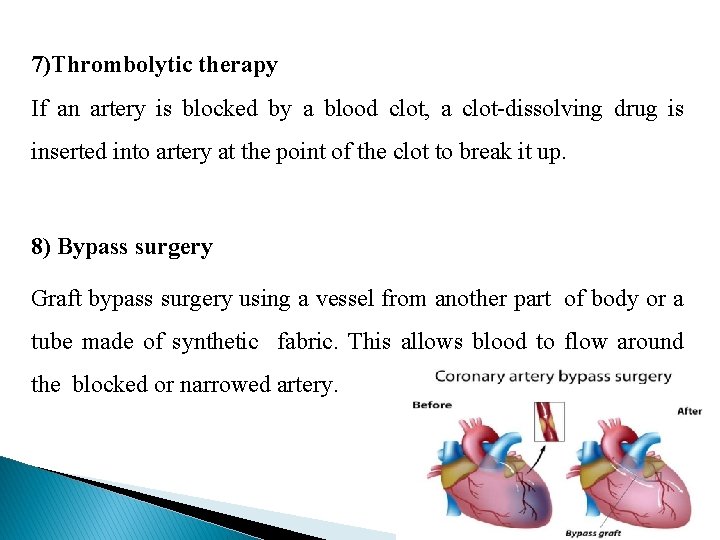
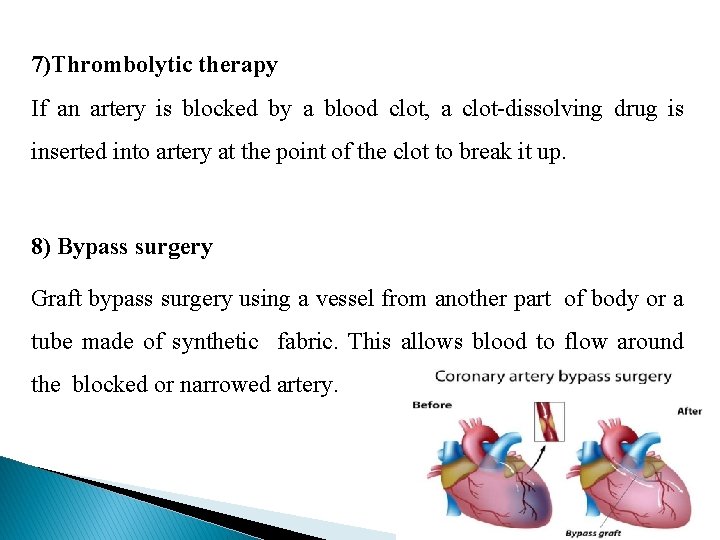
7)Thrombolytic therapy If an artery is blocked by a blood clot, a clot-dissolving drug is inserted into artery at the point of the clot to break it up. 8) Bypass surgery Graft bypass surgery using a vessel from another part of body or a tube made of synthetic fabric. This allows blood to flow around the blocked or narrowed artery.
Lifestyle and home remedies Lifestyle changes can help prevent or slow the progression of atherosclerosis • Stop smoking. • Exercise most days of the week. • Eat healthy foods • Manage stress • Manage the condition of high cholesterol, high blood pressure, diabetes or other chronic disease
