Atherosclerosis CVS 1 Hisham Al Khalidi Atherosclerosis wmv












- Slides: 28
Atherosclerosis CVS 1 Hisham Al Khalidi
Atherosclerosis. wmv
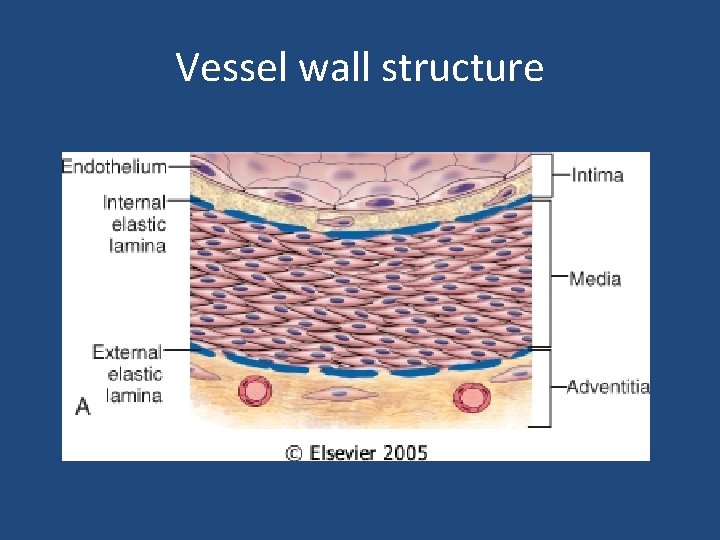
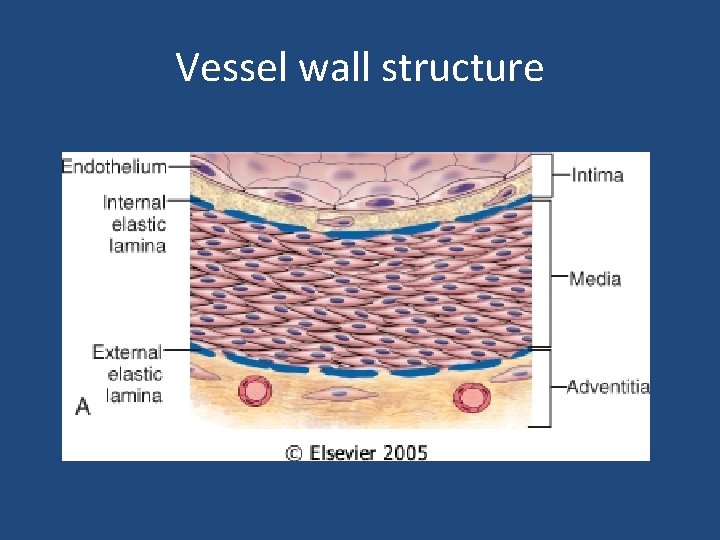
Vessel wall structure


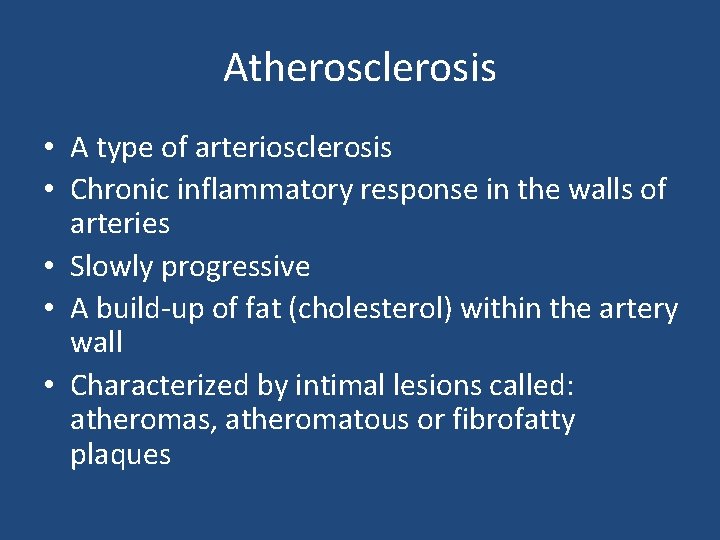
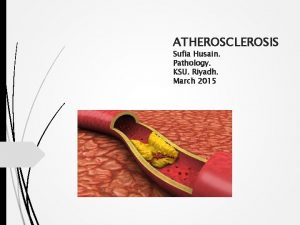
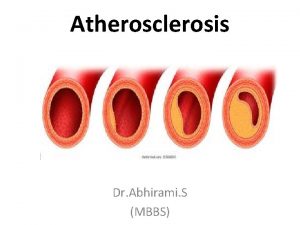
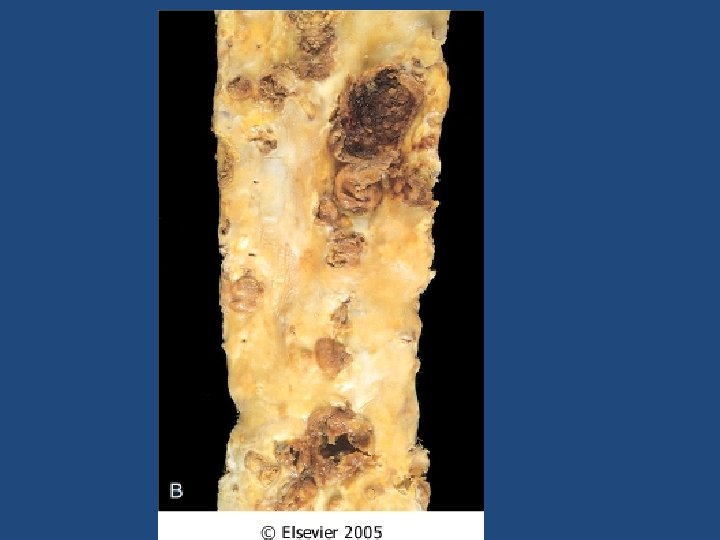
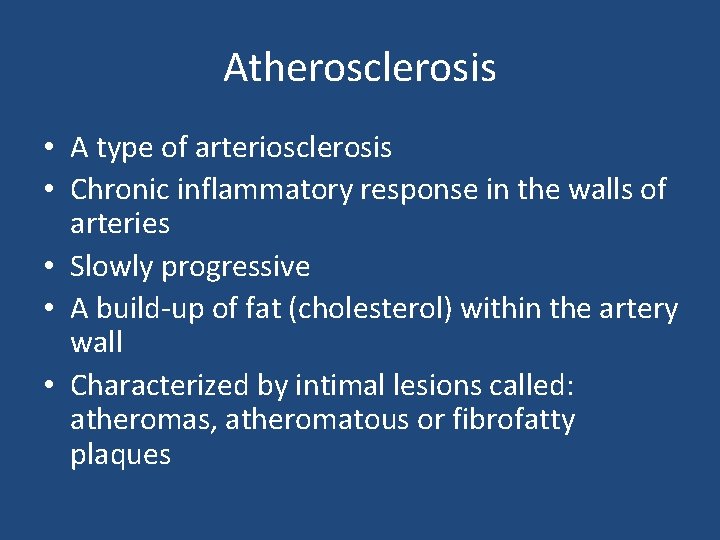
Atherosclerosis • A type of arteriosclerosis • Chronic inflammatory response in the walls of arteries • Slowly progressive • A build-up of fat (cholesterol) within the artery wall • Characterized by intimal lesions called: atheromas, atheromatous or fibrofatty plaques

Atherosclerosis Common sites • • • Abdominal aorta Coronaries Popliteal artery The internal carotid arteries The vessels of the circle of Willis
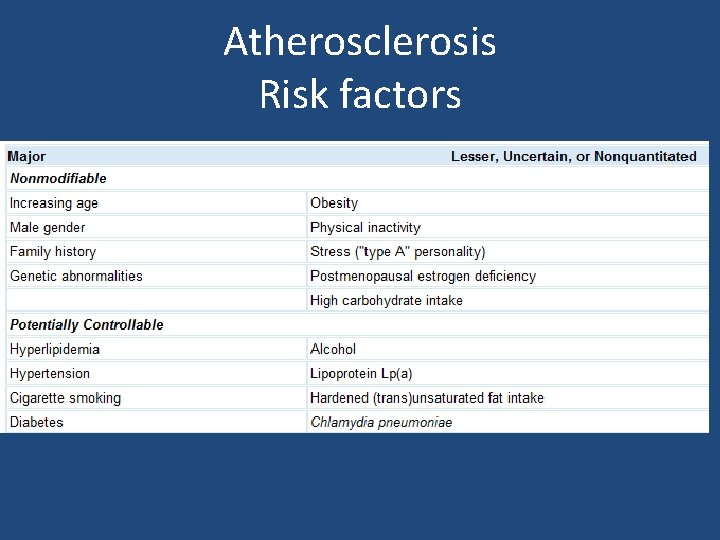
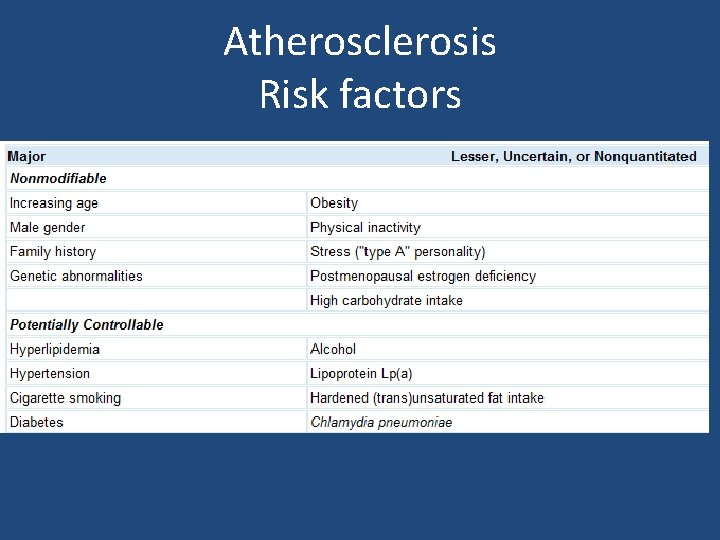
Atherosclerosis Risk factors
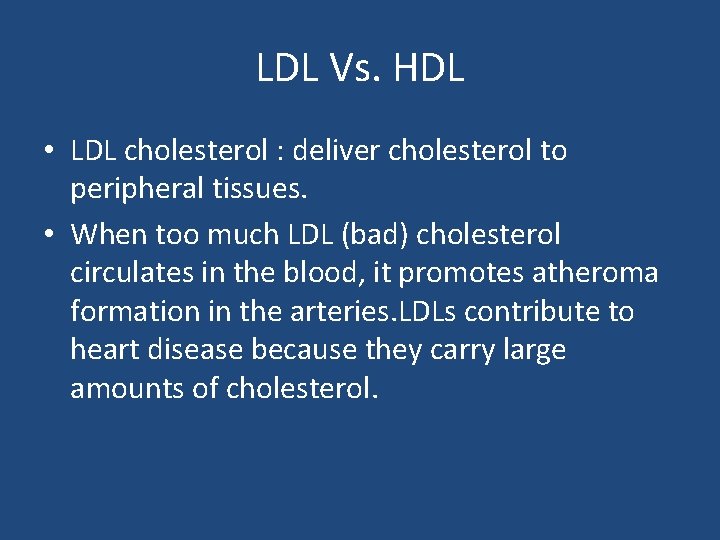
LDL Vs. HDL • LDL cholesterol : deliver cholesterol to peripheral tissues. • When too much LDL (bad) cholesterol circulates in the blood, it promotes atheroma formation in the arteries. LDLs contribute to heart disease because they carry large amounts of cholesterol.
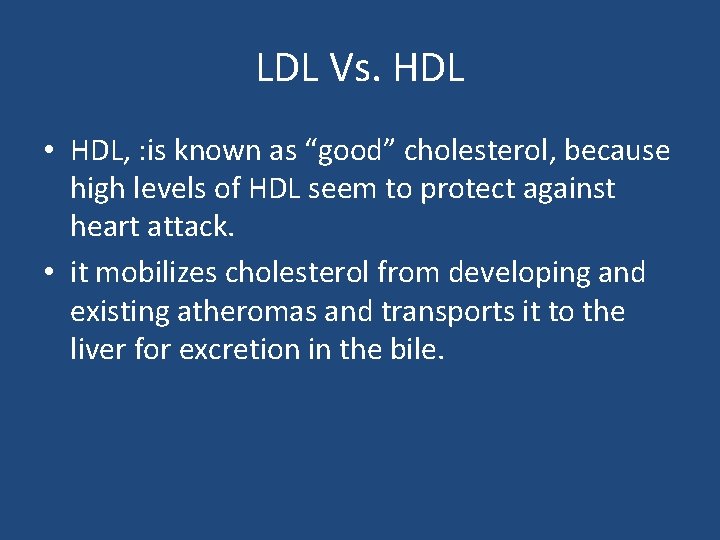
LDL Vs. HDL • HDL, : is known as “good” cholesterol, because high levels of HDL seem to protect against heart attack. • it mobilizes cholesterol from developing and existing atheromas and transports it to the liver for excretion in the bile.
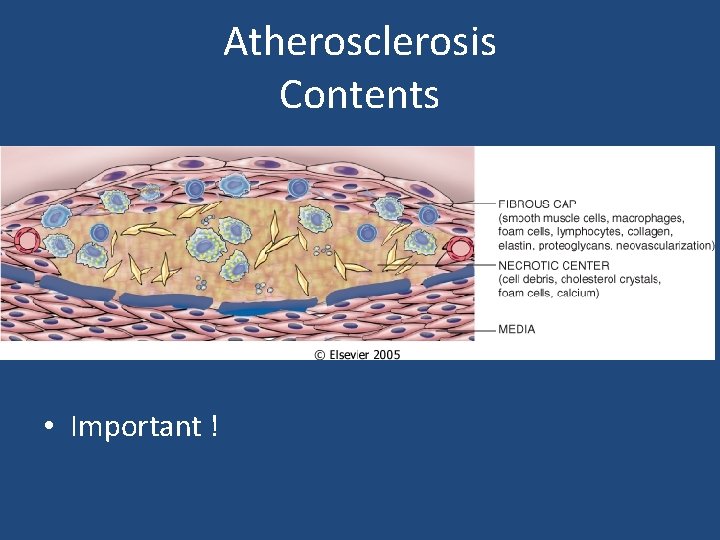
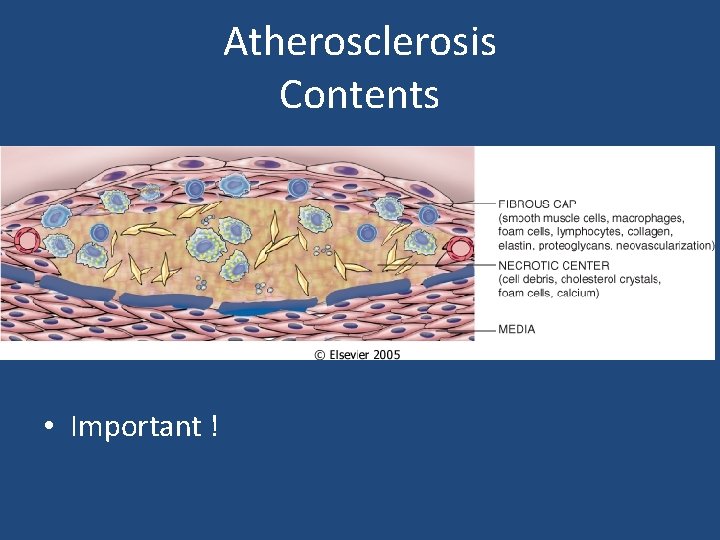
Atherosclerosis Contents • Important !
Atherosclerosis Pathogenesis • The main components of a fibrofatty plaques: – Lipids – Extracellular matrix – Cells, Proliferating smooth muscle cells
Atherosclerosis Pathogenesis response-to-injury hypothesis • Endothelial injury – Not completely understood – Nevertheless, the two most important causes of endothelial dysfunction are: • Hemodynamic disturbances • Hypercholesterolemia – Inflammation is also an important contributor. • Smooth muscle cell proliferation
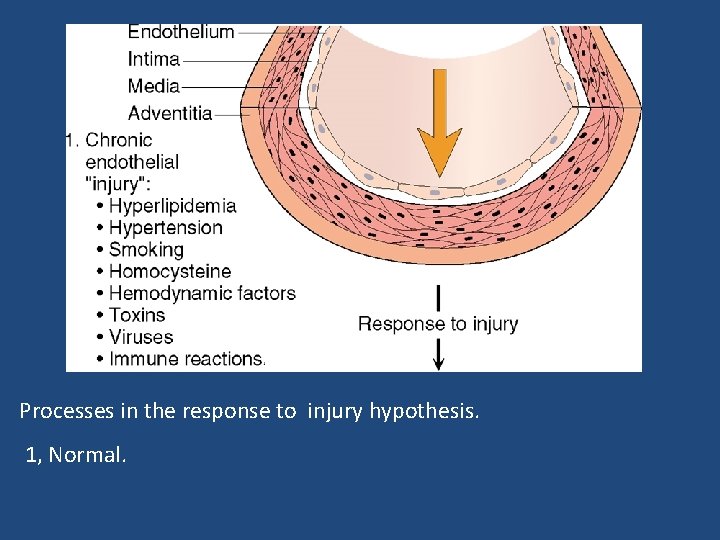
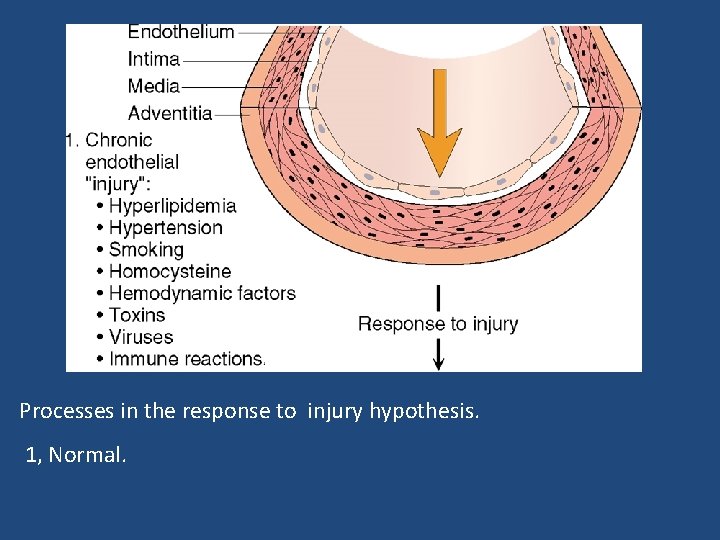
Processes in the response to injury hypothesis. 1, Normal.
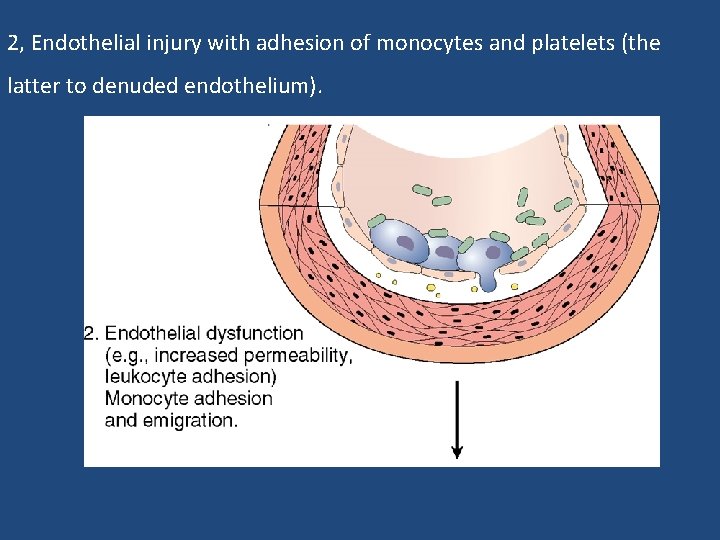
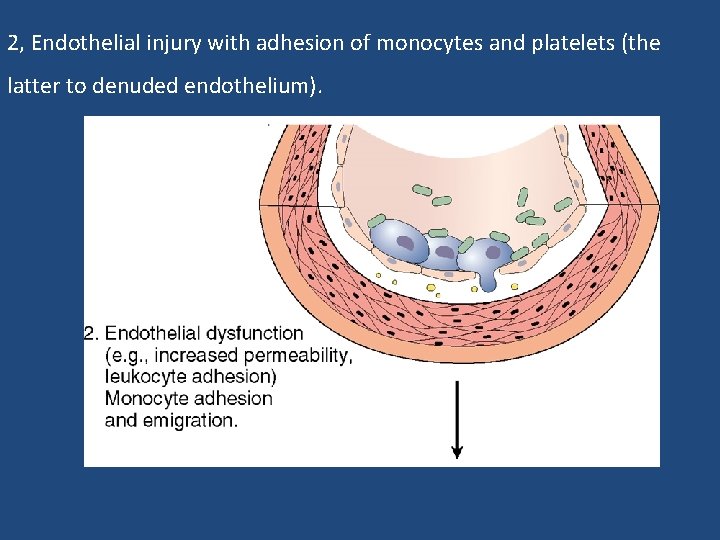
2, Endothelial injury with adhesion of monocytes and platelets (the latter to denuded endothelium).

3, Migration of monocytes (from the lumen) and smooth muscle cells (from the media) into the intima.

4, Smooth muscle cell proliferation in the intima.
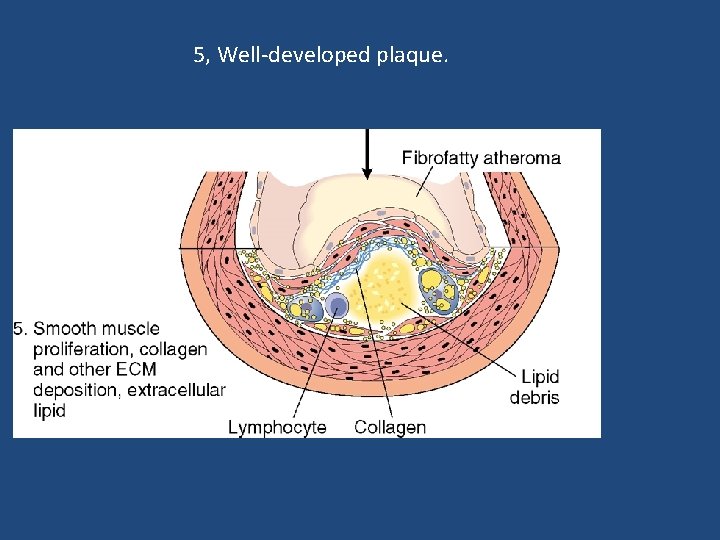
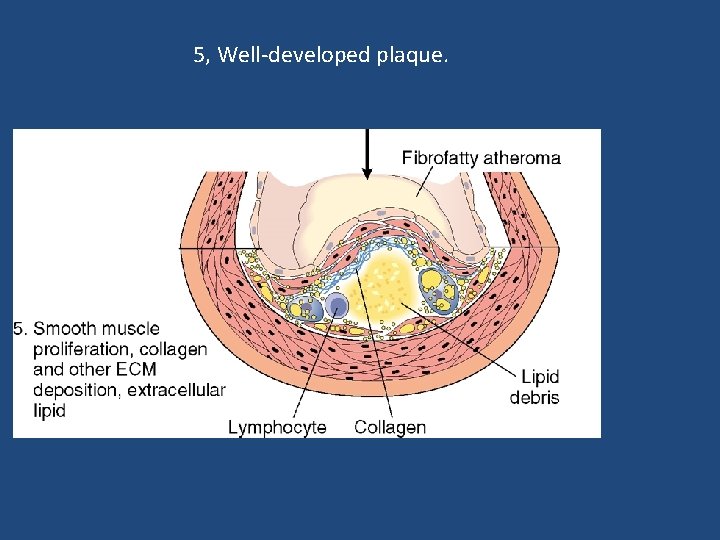
5, Well-developed plaque.

Atherosclerosis Consequences

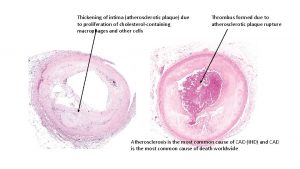
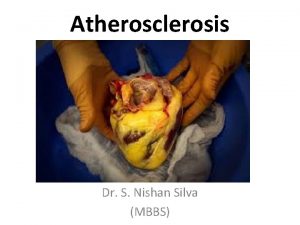
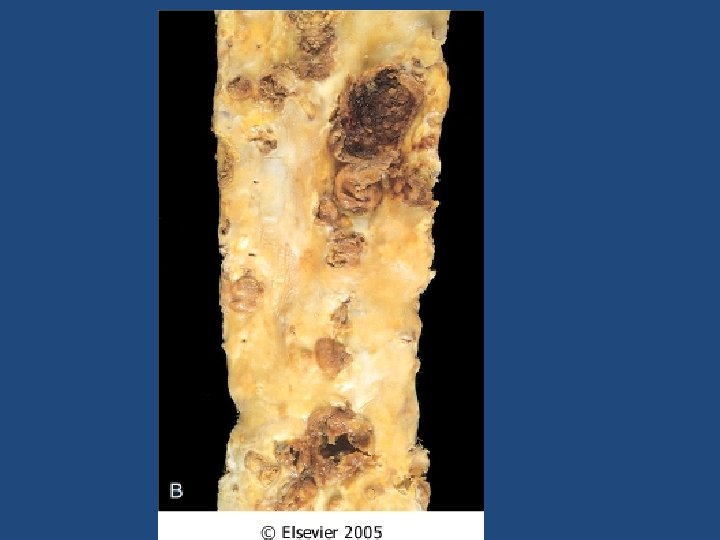
Atherosclerosis Complications The advanced lesion of atherosclerosis is at risk for the following pathological changes that have clinical significance: 1) Focal rupture, ulceration, or erosion of the luminal surface of atheromatous plaques may result in exposure of highly thrombogenic substances that induce thrombus formation or discharge of debris into the bloodstream, producing microemboli composed of lesion contents (cholesterol emboli or atheroemboli).

Atherosclerosis Complications • 2) Hemorrhage into a plaque, especially in the coronary arteries, may be initiated by rupture of either the overlying fibrous cap or the thinwalled capillaries that vascularize the plaque. A contained hematoma may expand the plaque or induce plaque rupture.
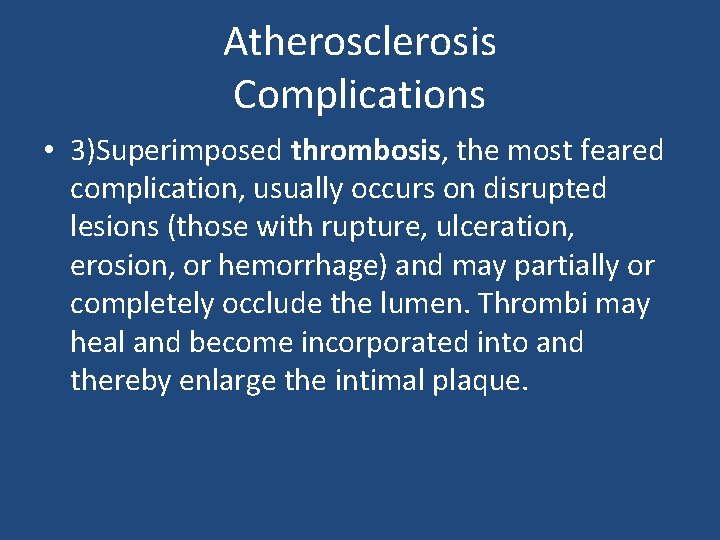
Atherosclerosis Complications • 3)Superimposed thrombosis, the most feared complication, usually occurs on disrupted lesions (those with rupture, ulceration, erosion, or hemorrhage) and may partially or completely occlude the lumen. Thrombi may heal and become incorporated into and thereby enlarge the intimal plaque.

Atherosclerosis Complications 4)Aneurysmal dilation may result from ATHinduced atrophy of the underlying media, with loss of elastic tissue, causing weakness and potential rupture 5) Calcifications.

Atherosclerosis Clinical Complications • • • Myocardial infarction (heart attack) Cerebral infarction (stroke) Aortic aneurysms Mesentric occlusion Peripheral vascular disease (gangrene of the legs)
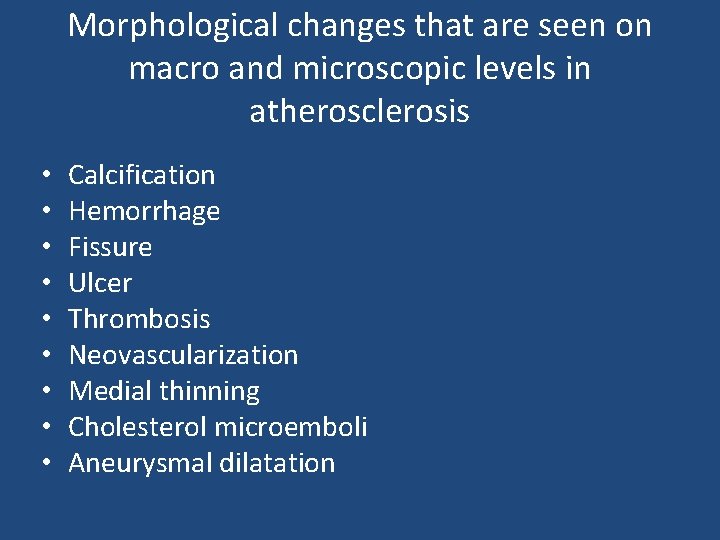
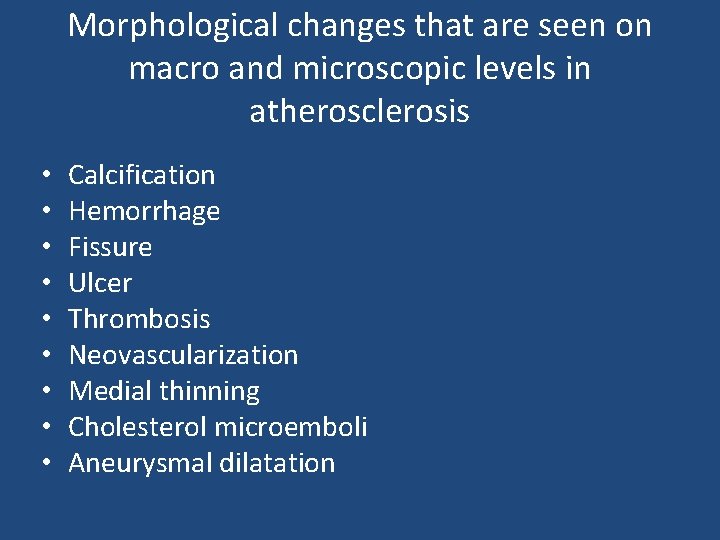
Morphological changes that are seen on macro and microscopic levels in atherosclerosis • • • Calcification Hemorrhage Fissure Ulcer Thrombosis Neovascularization Medial thinning Cholesterol microemboli Aneurysmal dilatation


 Dr. hisham khalil
Dr. hisham khalil Heart disease
Heart disease Atherosclerosis
Atherosclerosis Atherosclerosis
Atherosclerosis Atherosclerosis
Atherosclerosis Major branches of abdominal aorta
Major branches of abdominal aorta Atherosclerosis
Atherosclerosis Atherosclerosis tunica intima
Atherosclerosis tunica intima Variant angina
Variant angina Atherosclerosis
Atherosclerosis Atherosclerosis
Atherosclerosis Eclipse cvs repository
Eclipse cvs repository Netbeans cvs
Netbeans cvs Cvs steel libido
Cvs steel libido Cvs 4057
Cvs 4057 Cvs vs amniocentesis venn diagram
Cvs vs amniocentesis venn diagram Samantha cervantes
Samantha cervantes Michael hewitt gleeson
Michael hewitt gleeson Riluzole moa
Riluzole moa Cvs agenda
Cvs agenda Cvs wireless charger
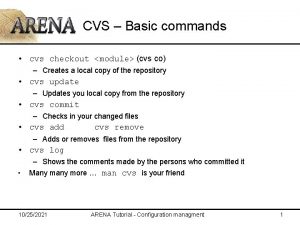
Cvs wireless charger Concurrent version system
Concurrent version system Cvs generic epipen
Cvs generic epipen Aloe cadabra target
Aloe cadabra target Tortoisecvs download
Tortoisecvs download Sterno pericardial ligament
Sterno pericardial ligament Cvs poinsettia
Cvs poinsettia Picto cvs
Picto cvs Costco pharmacy huntington
Costco pharmacy huntington