Oxygen Needs Interference with O 2 Transport Case
- Slides: 77
Oxygen Needs Interference with O 2 Transport
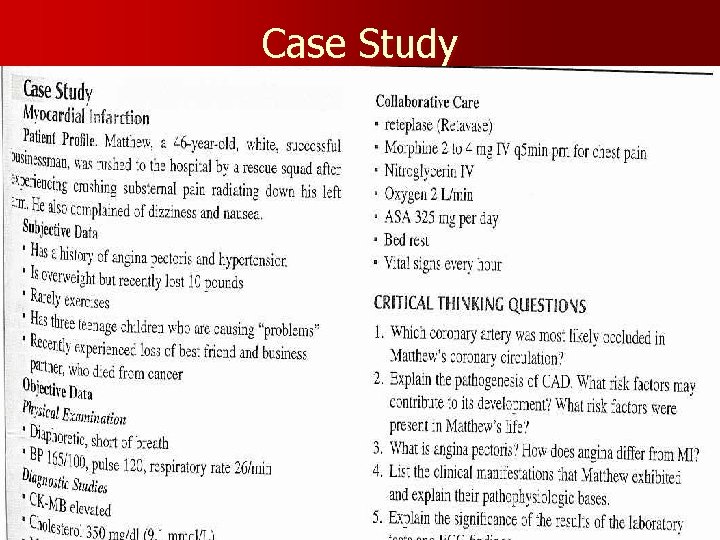
Case Study
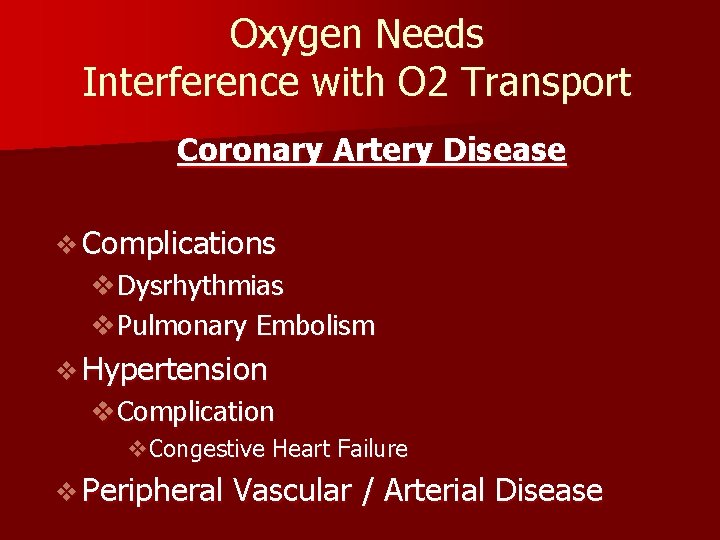
Oxygen Needs Interference with O 2 Transport Coronary Artery Disease v Complications v. Dysrhythmias v. Pulmonary Embolism v Hypertension v. Complication v. Congestive Heart Failure v Peripheral Vascular / Arterial Disease
Oxygen Needs Interference with O 2 Transport v Care of Patients with: v. Coronary Artery Disease v. Risk Factors v. Myocardial Infarction v. Alterations in: v. Rate & Rhythm (Cardiac Conduction) v. Effect on Cardiac Output
Content Approach v Anatomy & Physiology Review v Demographics/occurrence v Pathophysiology v Clinical Manifestation v Medical / Surgical Management v Nursing Process (APIE) v Assessment - Nursing Actions - Education
Anatomy & Physiology v Right Heart v Left Heart v Systole v. Valve Closure: v Diastole v. Valve Closure:
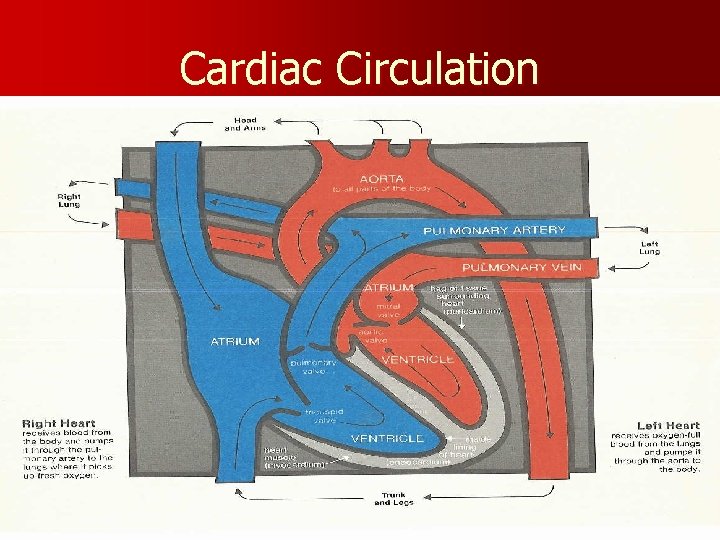
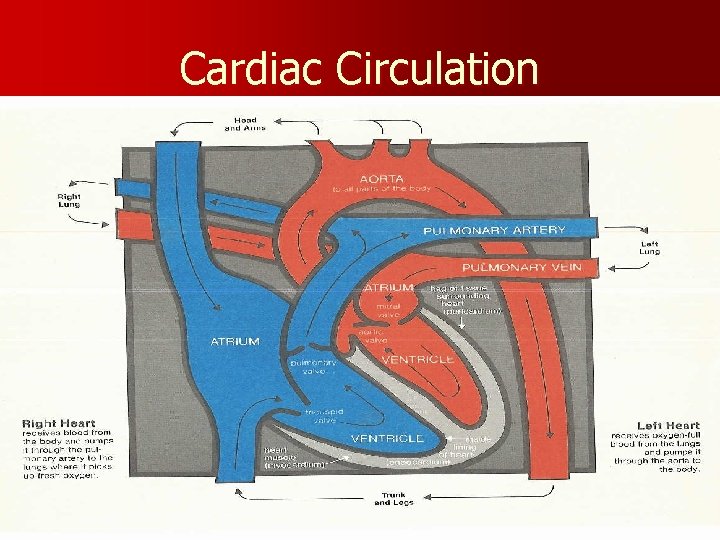
Cardiac Circulation
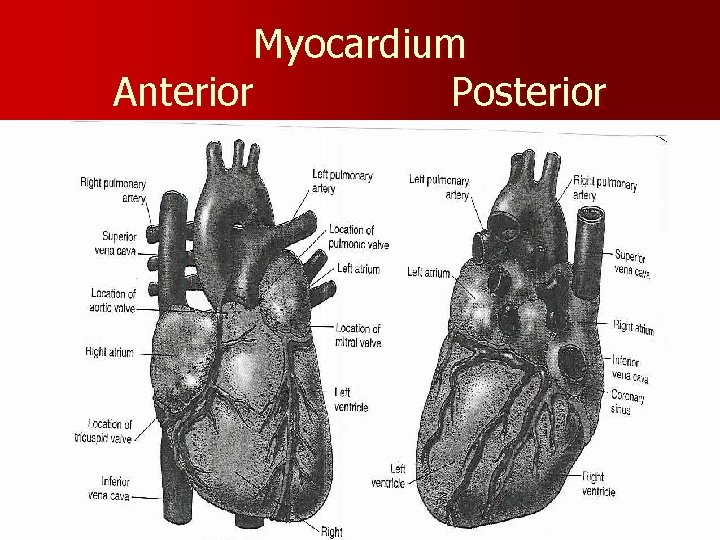
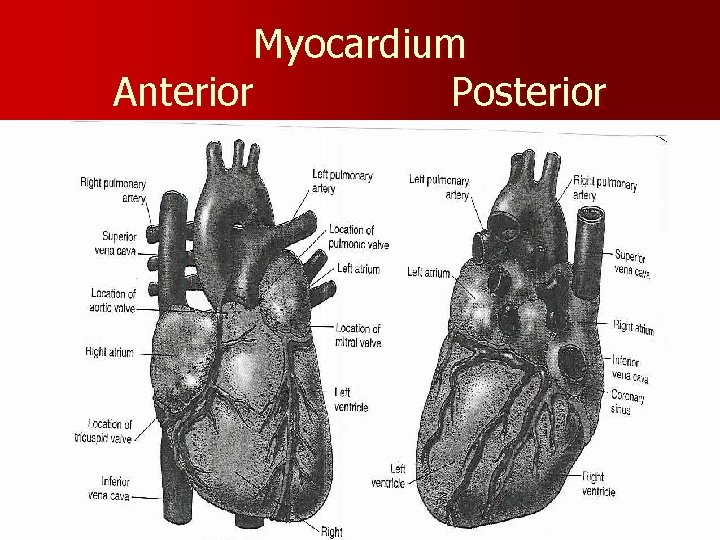
Myocardium Anterior Posterior
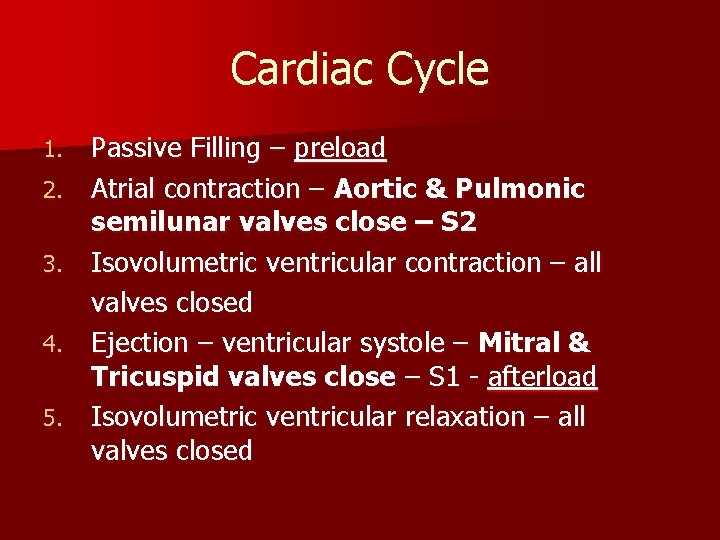
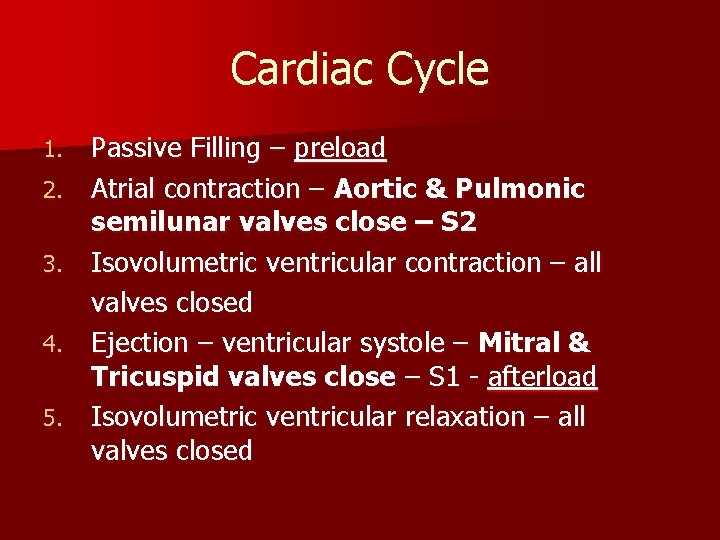
Cardiac Cycle 1. 2. 3. 4. 5. Passive Filling – preload Atrial contraction – Aortic & Pulmonic semilunar valves close – S 2 Isovolumetric ventricular contraction – all valves closed Ejection – ventricular systole – Mitral & Tricuspid valves close – S 1 - afterload Isovolumetric ventricular relaxation – all valves closed
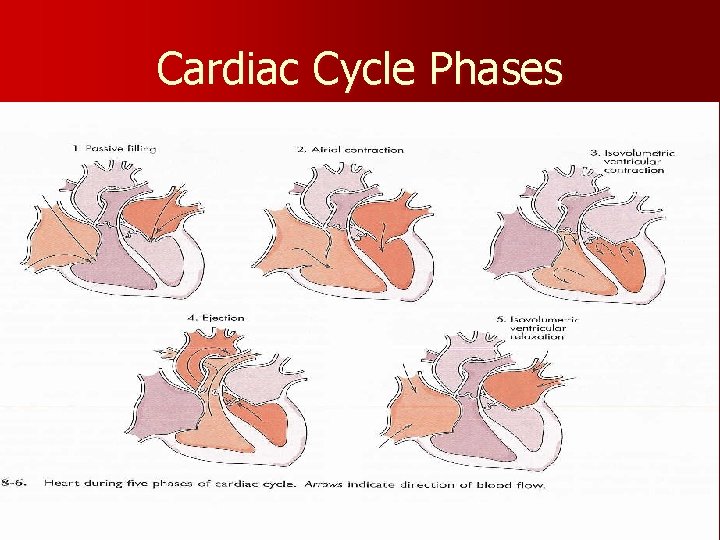
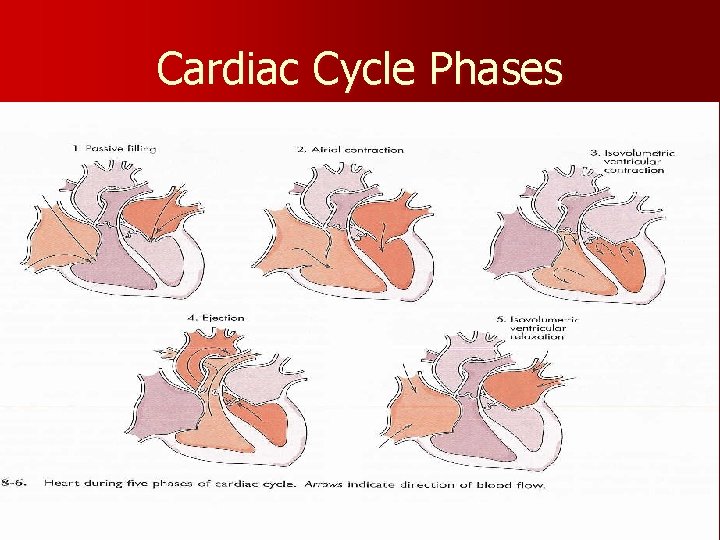
Cardiac Cycle Phases
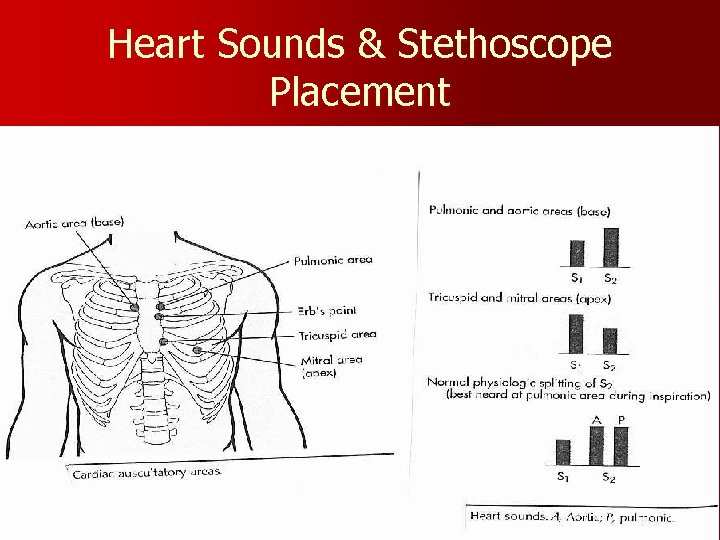
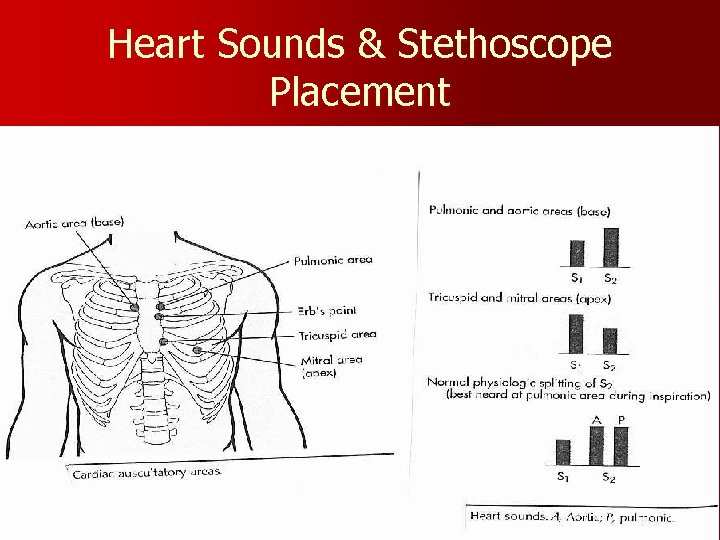
Heart Sounds & Stethoscope Placement
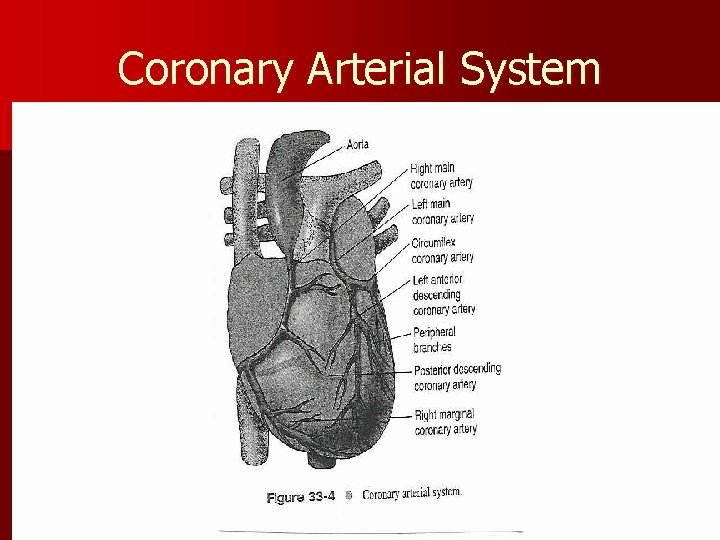
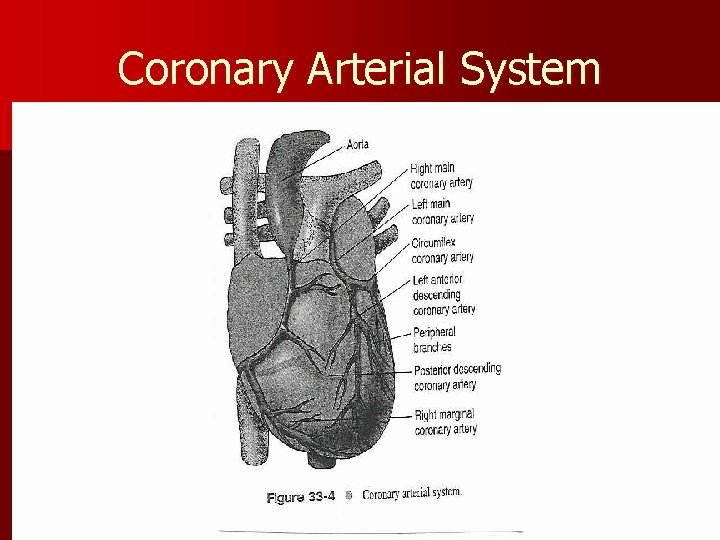
Coronary Arterial System
Physiology: Oxygen Supply to the Cardiac Muscle during the Cardiac Cycle v Coronary artery oxygen deficit vduring ventricular contraction & ejection (systole) v Coronary artery filling vduring ventricular filling (diastole) What is the impact of heart rate on coronary artery filling?
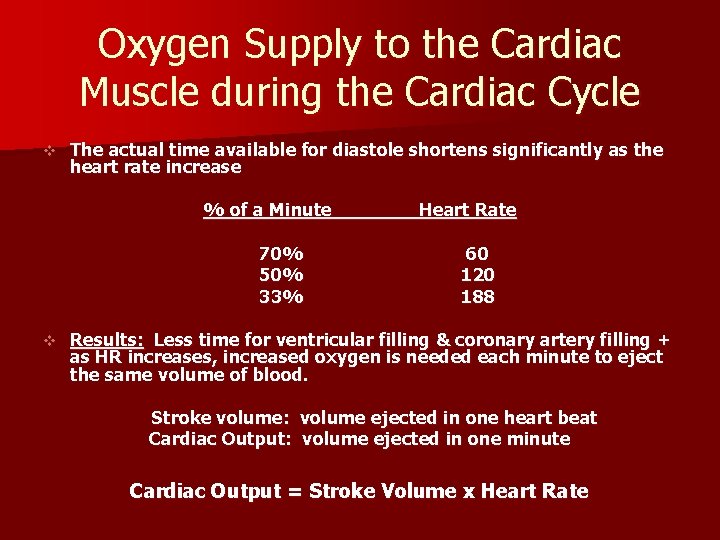
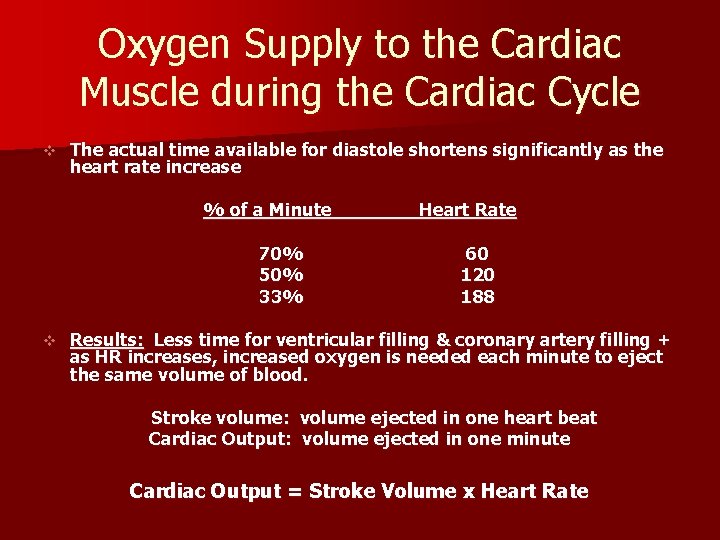
Oxygen Supply to the Cardiac Muscle during the Cardiac Cycle v The actual time available for diastole shortens significantly as the heart rate increase % of a Minute 70% 50% 33% v Heart Rate 60 120 188 Results: Less time for ventricular filling & coronary artery filling + as HR increases, increased oxygen is needed each minute to eject the same volume of blood. Stroke volume: volume ejected in one heart beat Cardiac Output: volume ejected in one minute Cardiac Output = Stroke Volume x Heart Rate
Factors Determining Myocardial Oxygen Needs v Decreased Oxygen Supply: v Noncardiac: Anemia, hypoxemia, pneumonia, asthma, COPD, low blood volume v Cardiac: Arrhythmias/dysrhythmias, congestive heart failure (CHF), coronary artery spasm, coronary artery thrombosis, valve disorders v Increased Oxygen Demand or Consumption: v Noncardiac: anxiety, cocaine use, hypertension, hyperthermia, hyperthyroidism, physical exertion v Cardiac: aortic stenosis, arrhythmias, cardiomyopathy, hypertension, tachycardia
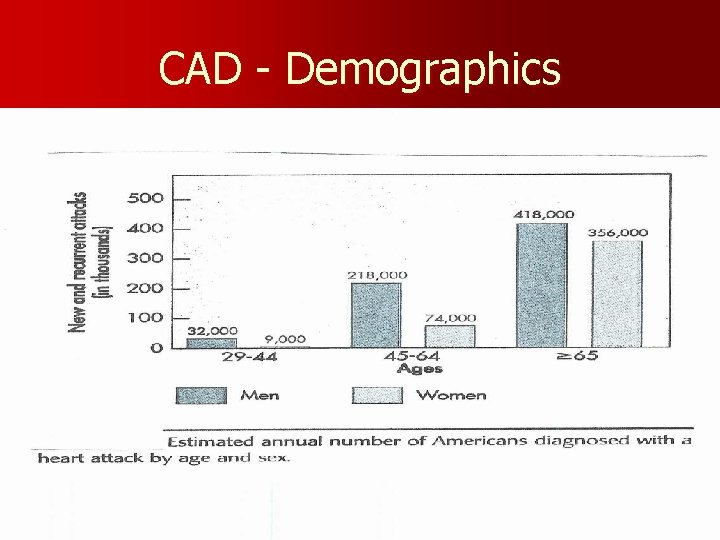
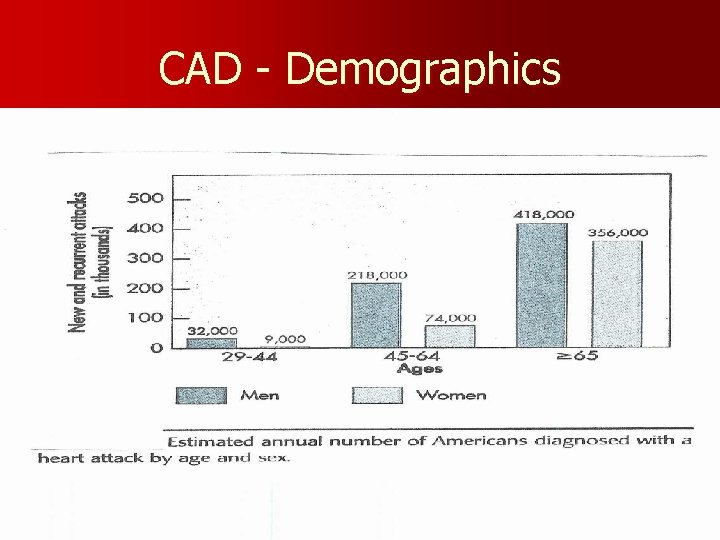
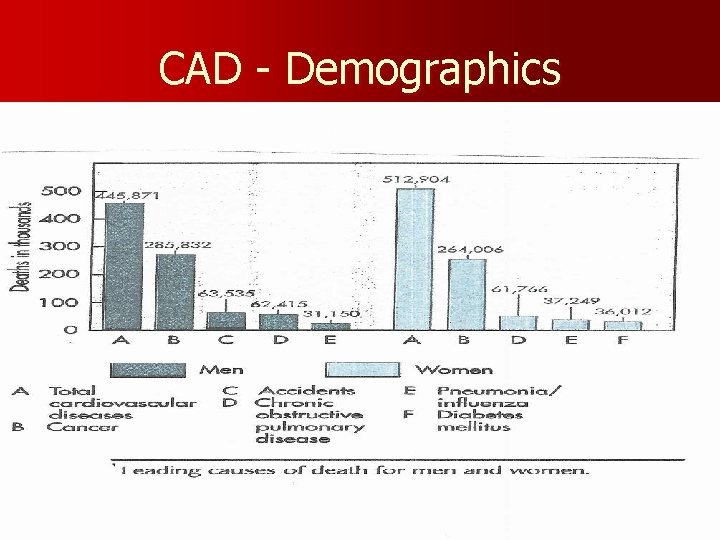
CAD - Demographics
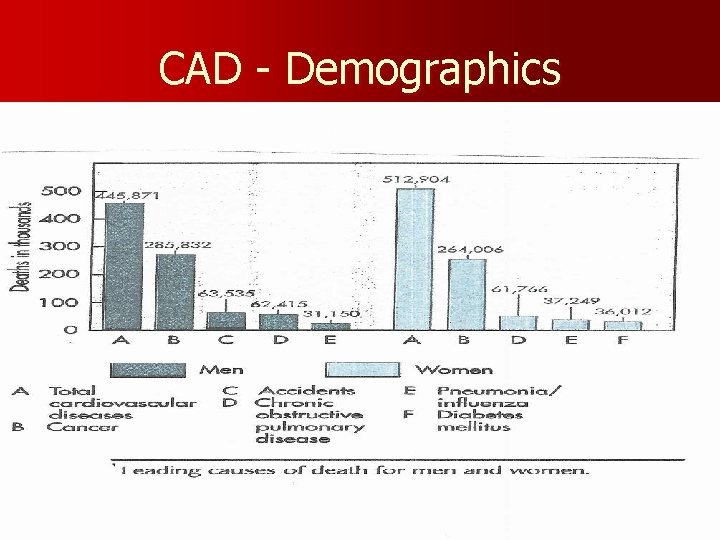
CAD - Demographics
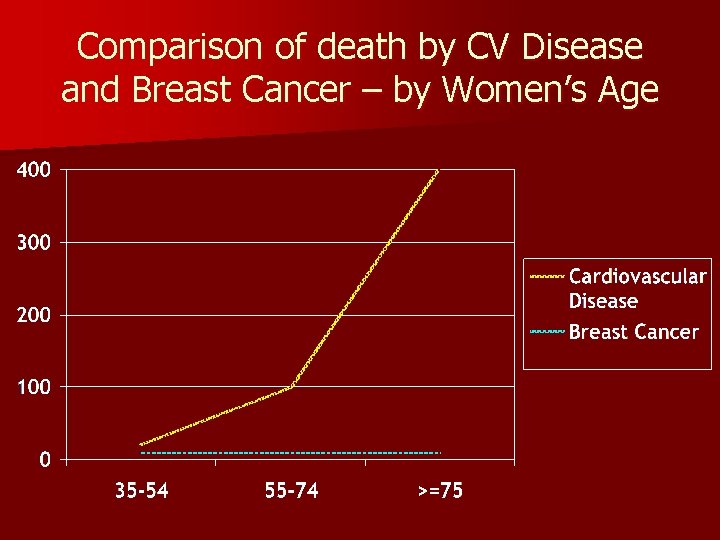
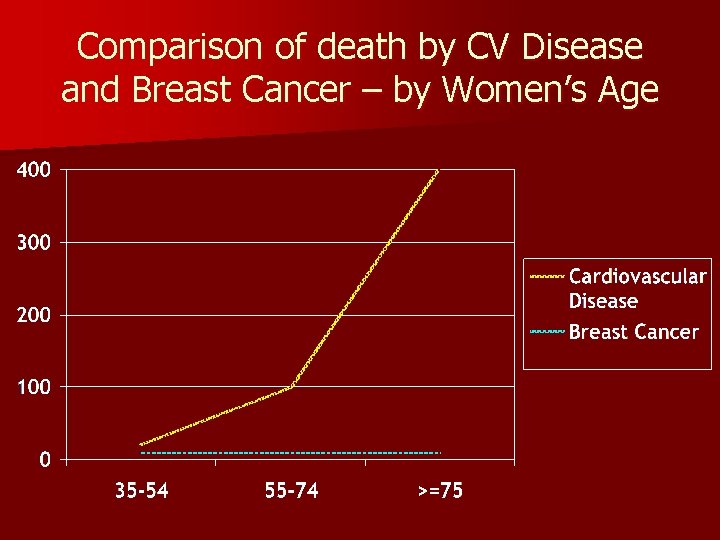
Comparison of death by CV Disease and Breast Cancer – by Women’s Age
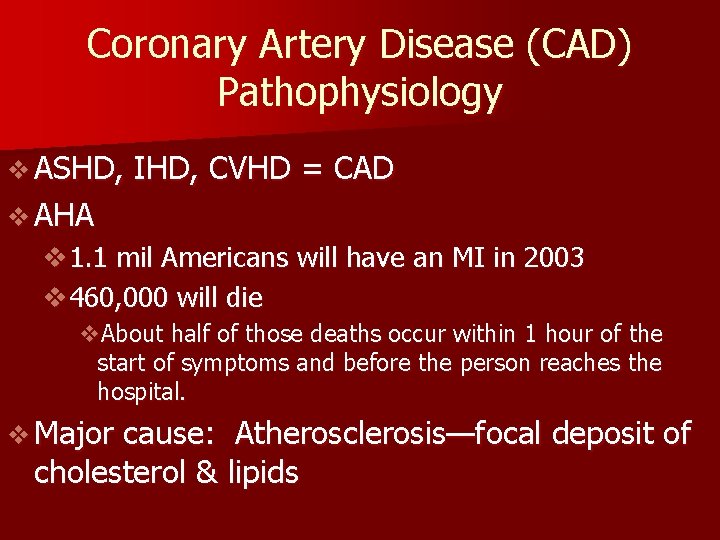
Coronary Artery Disease (CAD) Pathophysiology v ASHD, IHD, CVHD = CAD v AHA v 1. 1 mil Americans will have an MI in 2003 v 460, 000 will die v. About half of those deaths occur within 1 hour of the start of symptoms and before the person reaches the hospital. v Major cause: Atherosclerosis—focal deposit of cholesterol & lipids
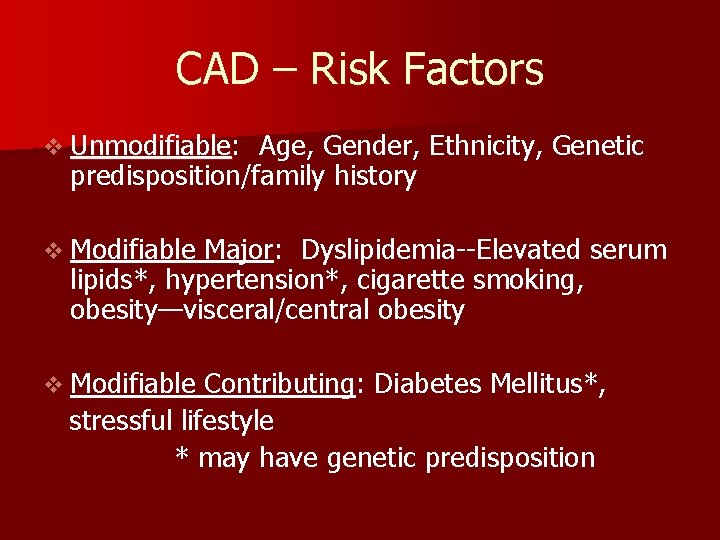
CAD – Risk Factors v Unmodifiable: Unmodifiable Age, Gender, Ethnicity, Genetic predisposition/family history v Modifiable Major: Dyslipidemia--Elevated serum lipids*, hypertension*, cigarette smoking, obesity—visceral/central obesity v Modifiable Contributing: Diabetes Mellitus*, stressful lifestyle * may have genetic predisposition
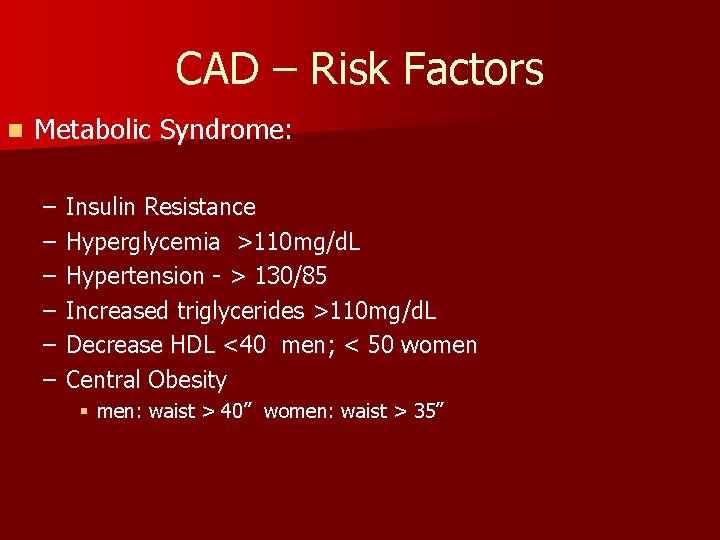
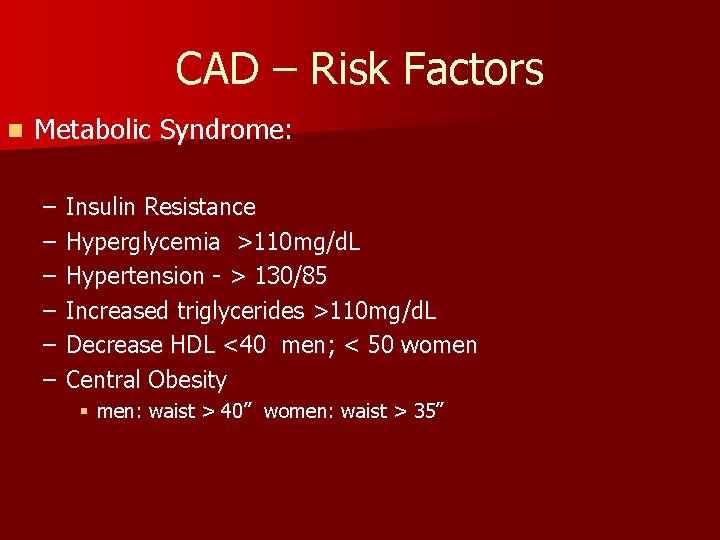
CAD – Risk Factors n Metabolic Syndrome: – – – Insulin Resistance Hyperglycemia >110 mg/d. L Hypertension - > 130/85 Increased triglycerides >110 mg/d. L Decrease HDL <40 men; < 50 women Central Obesity § men: waist > 40” women: waist > 35”
Risk Factors One of the Major Modifiable Physical Inactivity
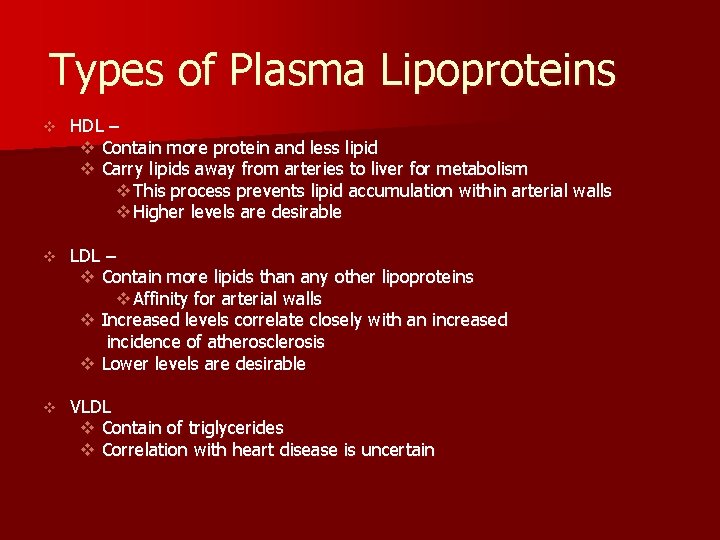
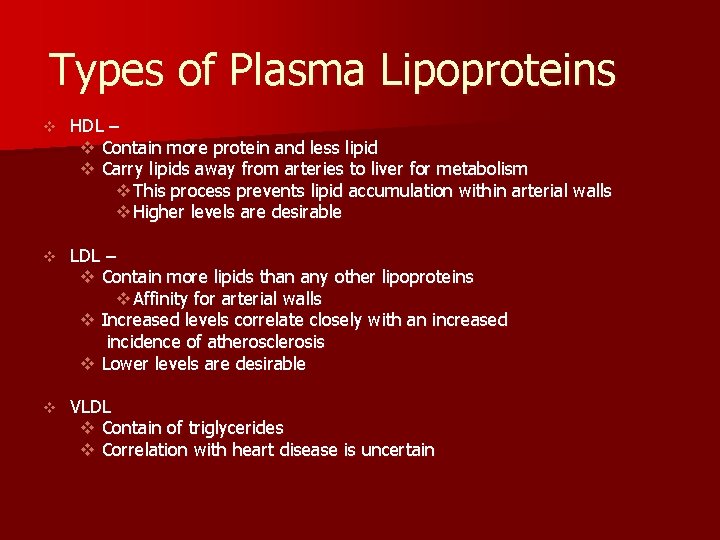
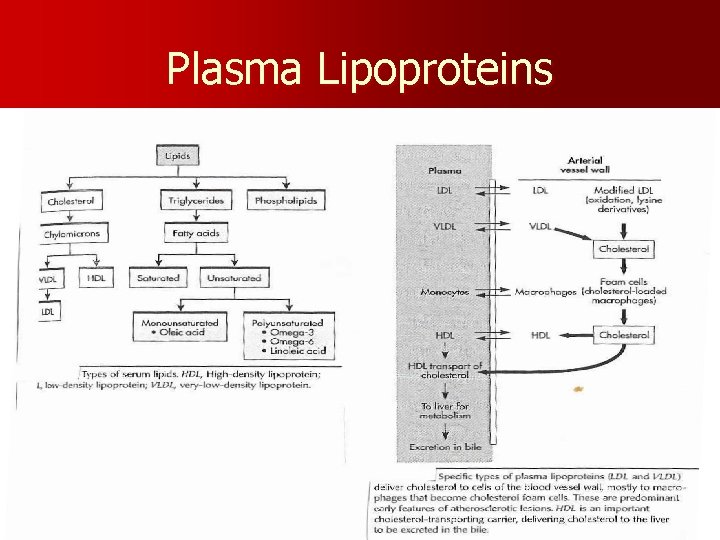
Types of Plasma Lipoproteins v HDL – v Contain more protein and less lipid v Carry lipids away from arteries to liver for metabolism v This process prevents lipid accumulation within arterial walls v Higher levels are desirable v LDL – v Contain more lipids than any other lipoproteins v Affinity for arterial walls v Increased levels correlate closely with an increased incidence of atherosclerosis v Lower levels are desirable v VLDL v Contain of triglycerides v Correlation with heart disease is uncertain
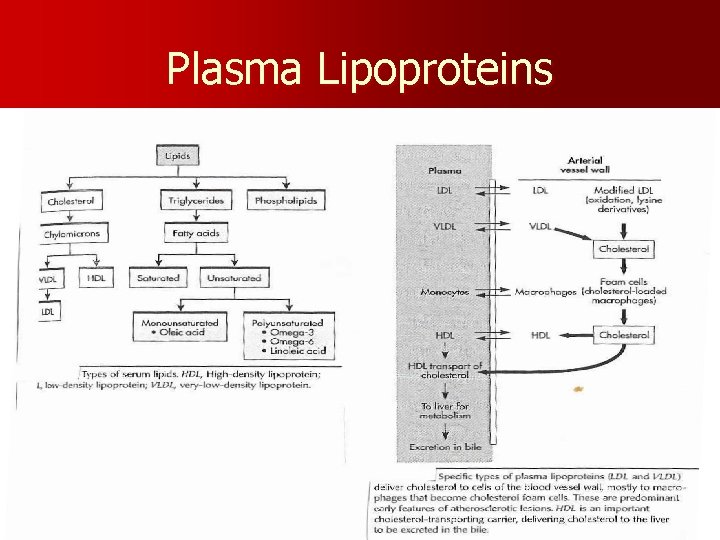
Plasma Lipoproteins
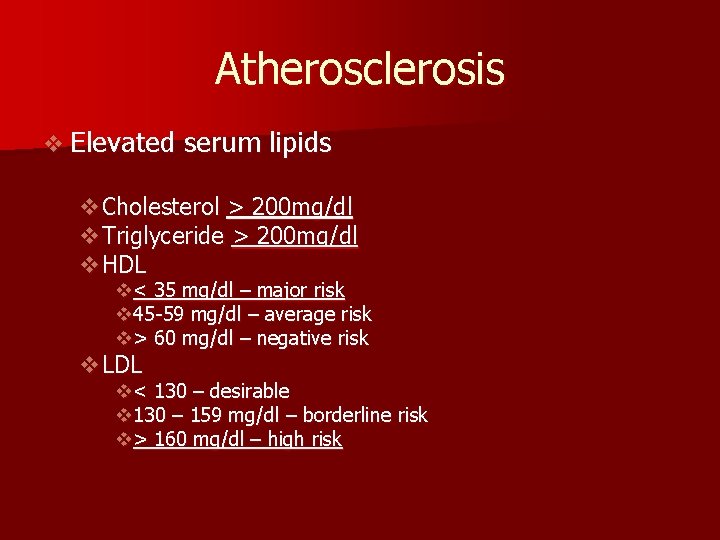
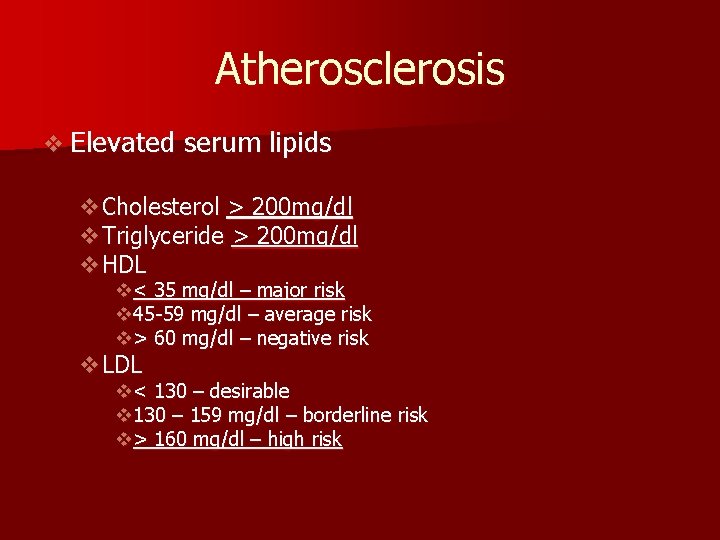
Atherosclerosis v Elevated serum lipids v. Cholesterol > 200 mg/dl v. Triglyceride > 200 mg/dl v. HDL v< 35 mg/dl – major risk v 45 -59 mg/dl – average risk v> 60 mg/dl – negative risk v. LDL v< 130 – desirable v 130 – 159 mg/dl – borderline risk v> 160 mg/dl – high risk
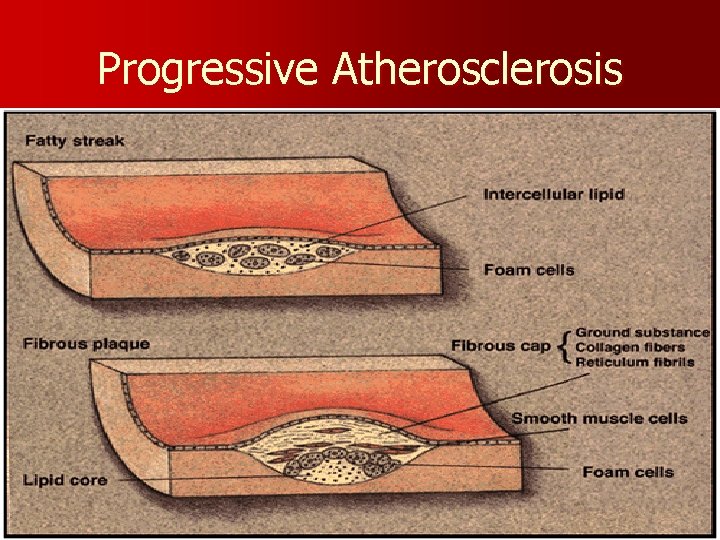
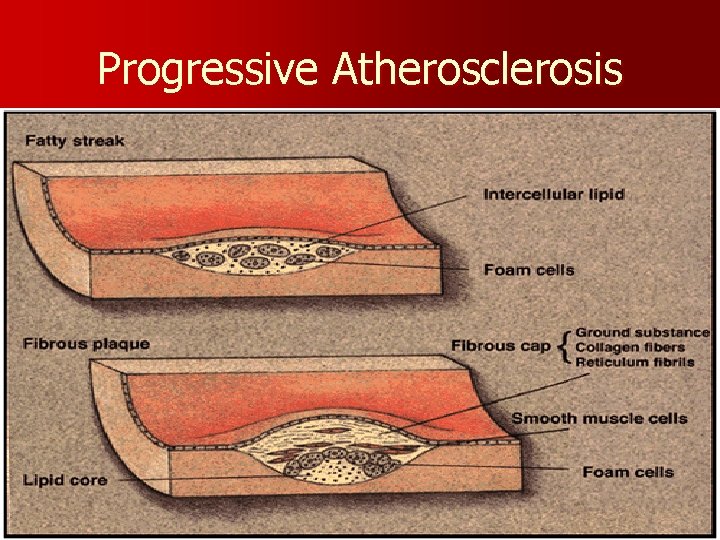
Progressive Atherosclerosis
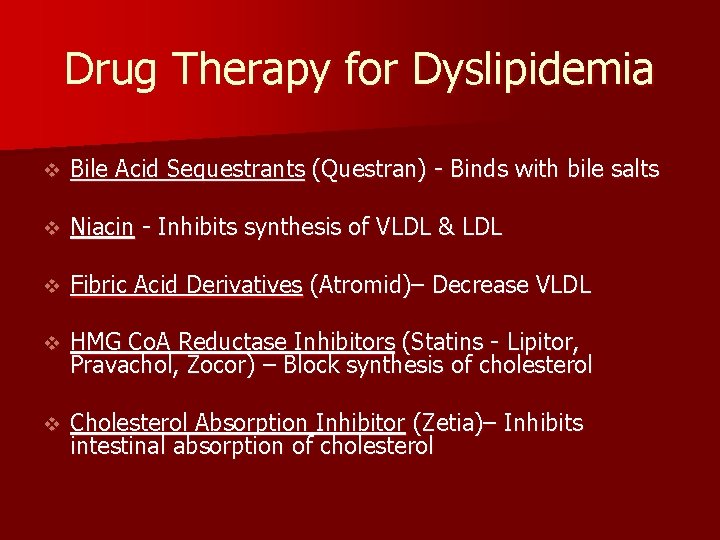
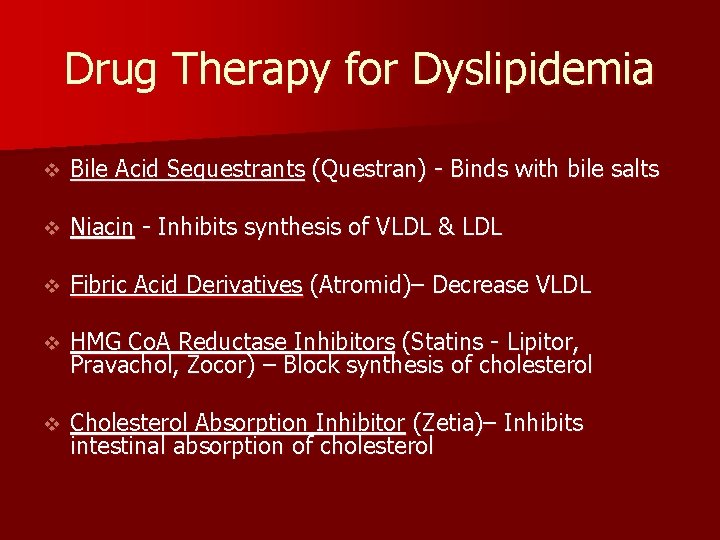
Drug Therapy for Dyslipidemia v Bile Acid Sequestrants (Questran) - Binds with bile salts v Niacin - Inhibits synthesis of VLDL & LDL v Fibric Acid Derivatives (Atromid)– Decrease VLDL v HMG Co. A Reductase Inhibitors (Statins - Lipitor, Pravachol, Zocor) – Block synthesis of cholesterol v Cholesterol Absorption Inhibitor (Zetia)– Inhibits intestinal absorption of cholesterol
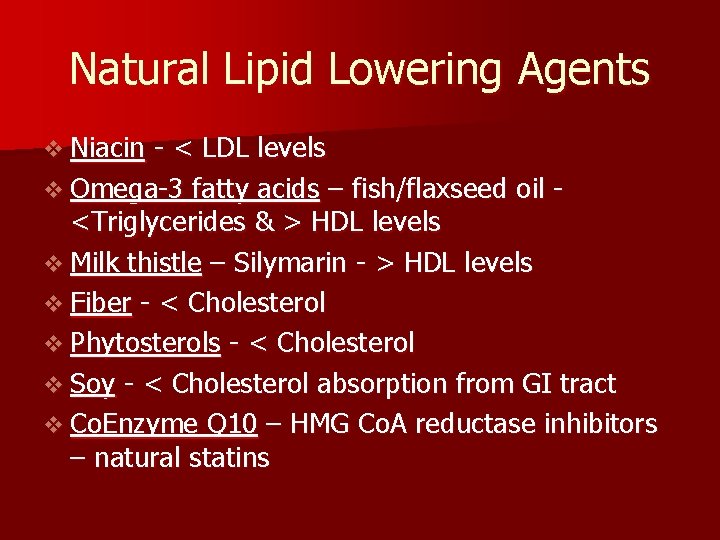
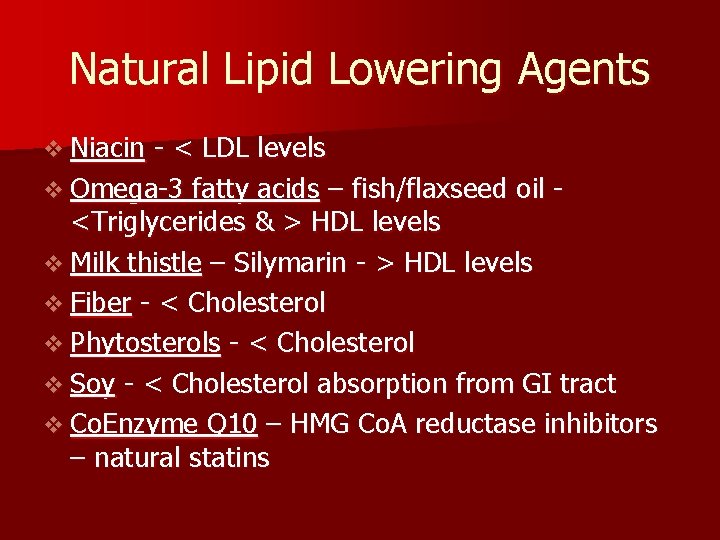
Natural Lipid Lowering Agents v Niacin - < LDL levels v Omega-3 fatty acids – fish/flaxseed oil <Triglycerides & > HDL levels v Milk thistle – Silymarin - > HDL levels v Fiber - < Cholesterol v Phytosterols - < Cholesterol v Soy - < Cholesterol absorption from GI tract v Co. Enzyme Q 10 – HMG Co. A reductase inhibitors – natural statins
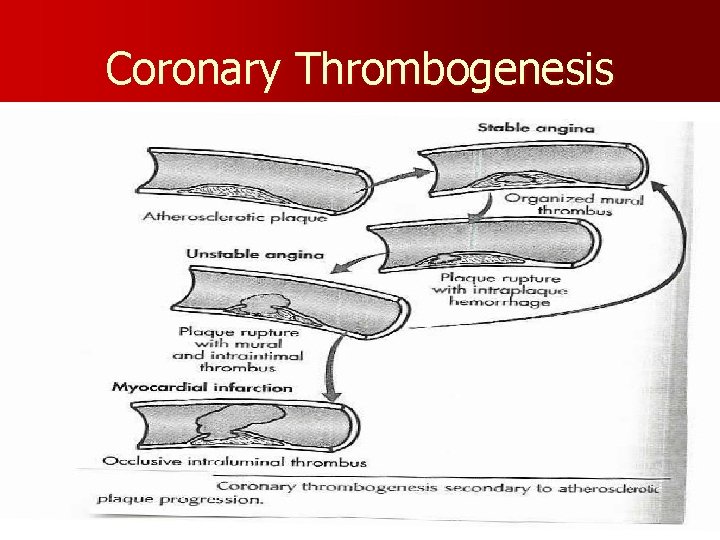
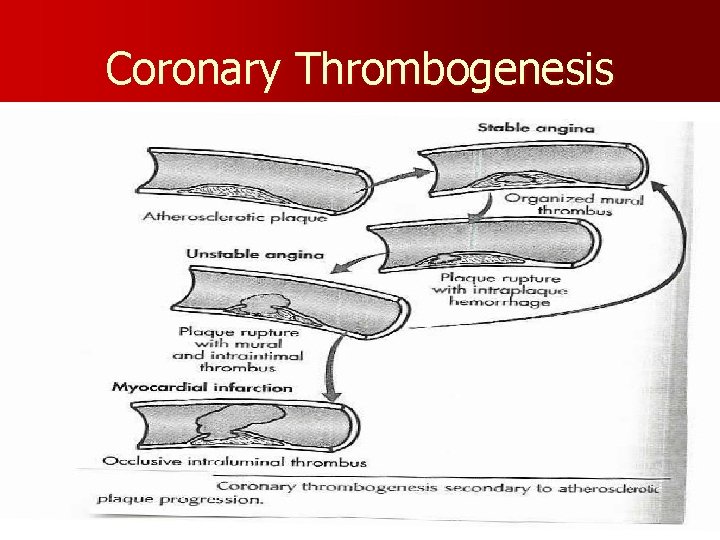
Coronary Thrombogenesis
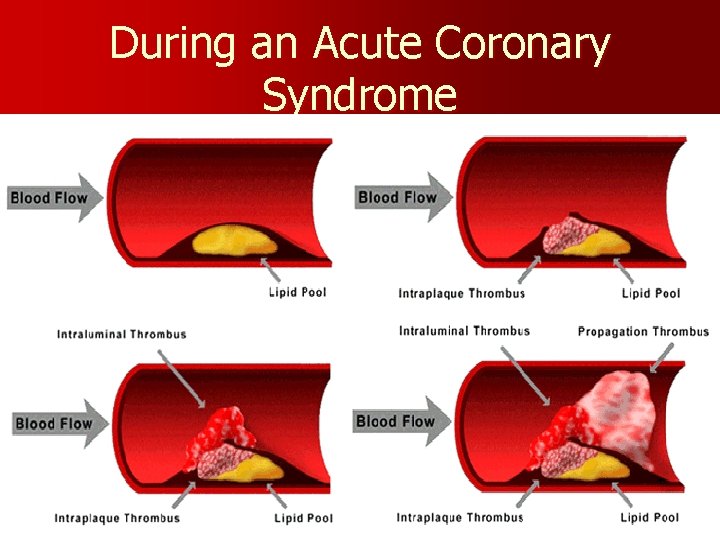
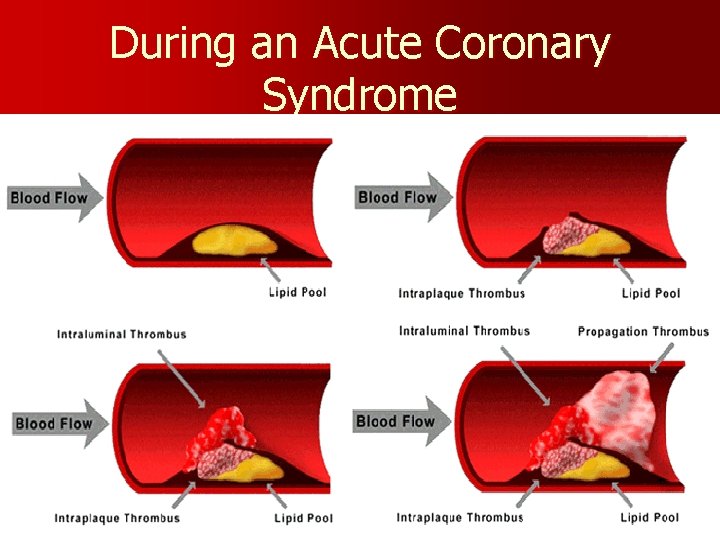
During an Acute Coronary Syndrome
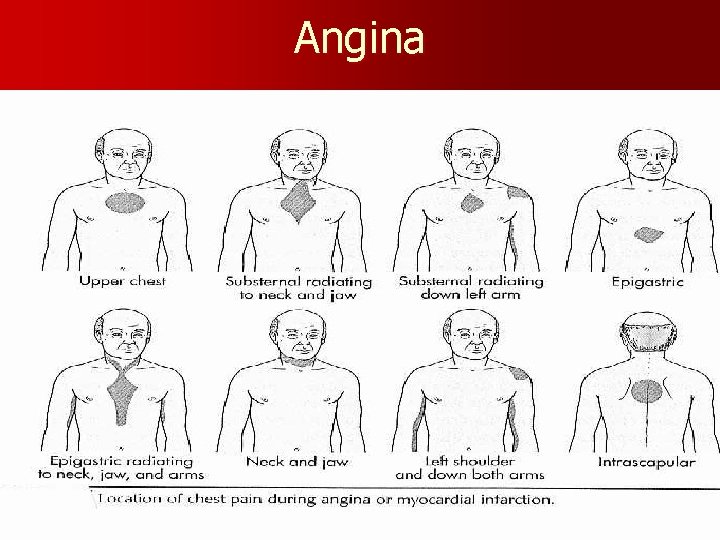
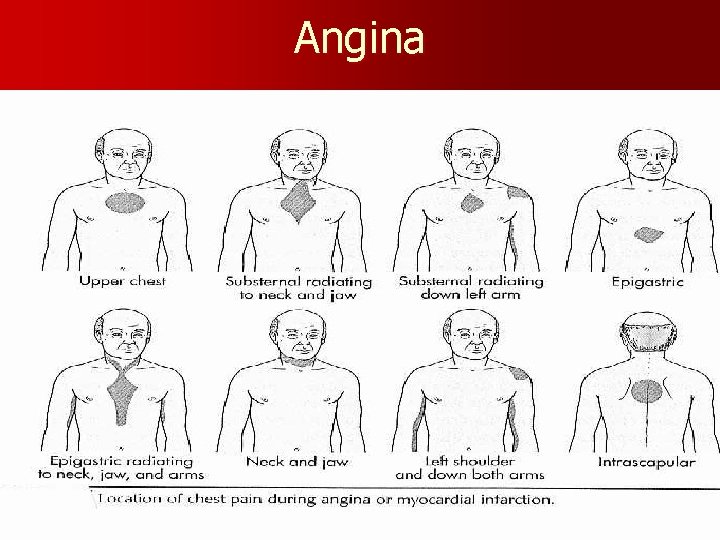
Angina
Clinical Manifestations Angina – Chest Pain v Stable Angina Pectoris – intermittent, same pattern of onset, duration, intensity of symptoms - 3 -5 mins. v Silent Ischemia – 80% of patients with ischemia are asymptomatic v Prinzmetal’s Angina – variant – not precipitated by physical activity – may be due to spasm v Nocturnal Angina – occurs at night but not necessarily during sleep or in recumbent position v Angina Decubitis – recumbent position – relieved by standing v Unstable Angina – Unpredictable or may evolve from stable angina – increasing frequency, duration, intensity
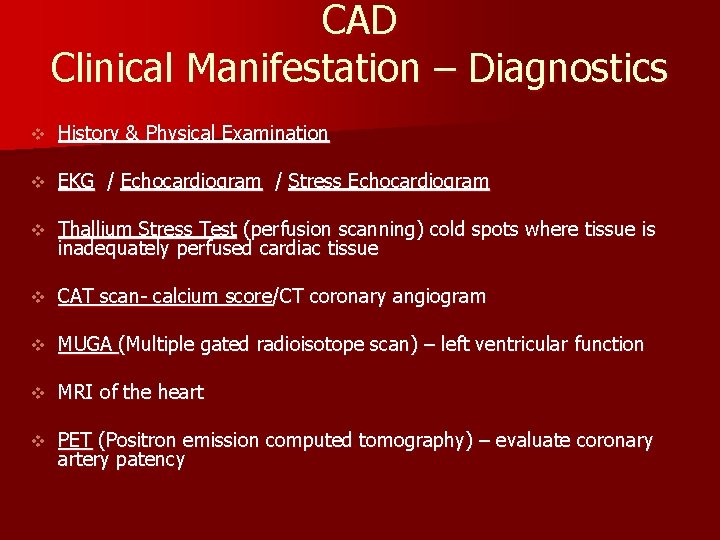
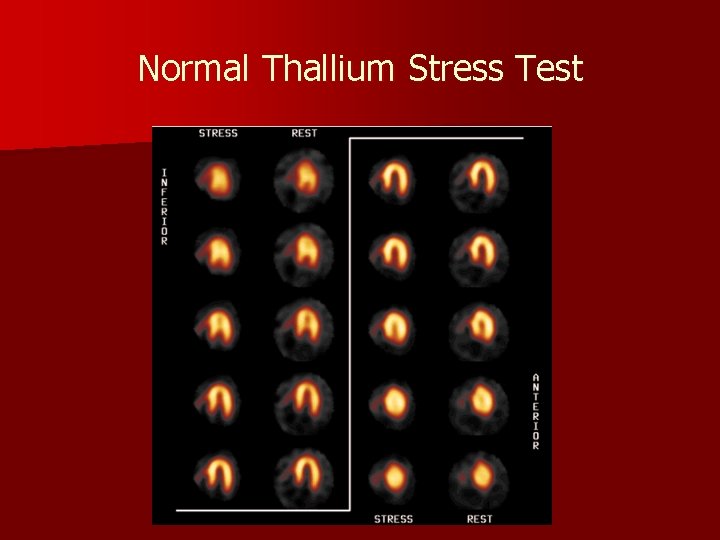
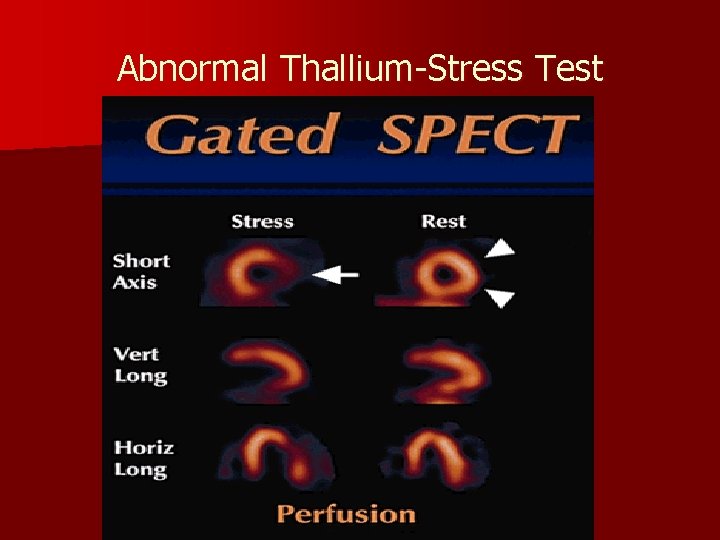
CAD Clinical Manifestation – Diagnostics v History & Physical Examination v EKG / Echocardiogram / Stress Echocardiogram v Thallium Stress Test (perfusion scanning) cold spots where tissue is inadequately perfused cardiac tissue v CAT scan- calcium score/CT coronary angiogram v MUGA (Multiple gated radioisotope scan) – left ventricular function v MRI of the heart v PET (Positron emission computed tomography) – evaluate coronary artery patency
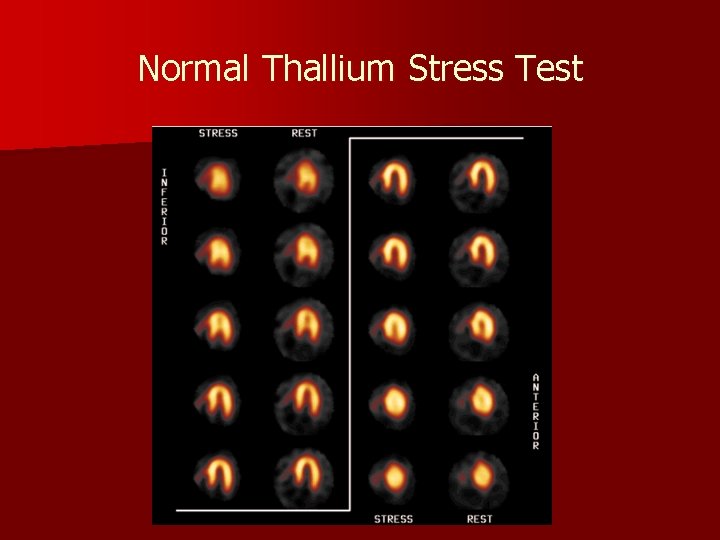
Normal Thallium Stress Test
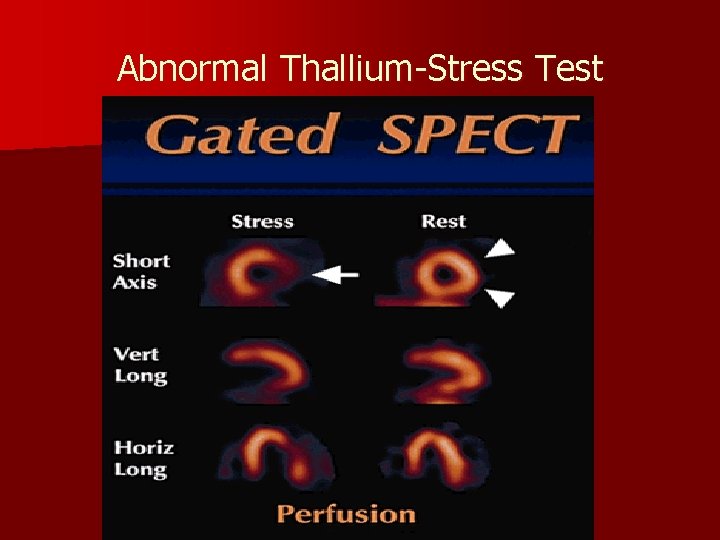
Abnormal Thallium-Stress Test
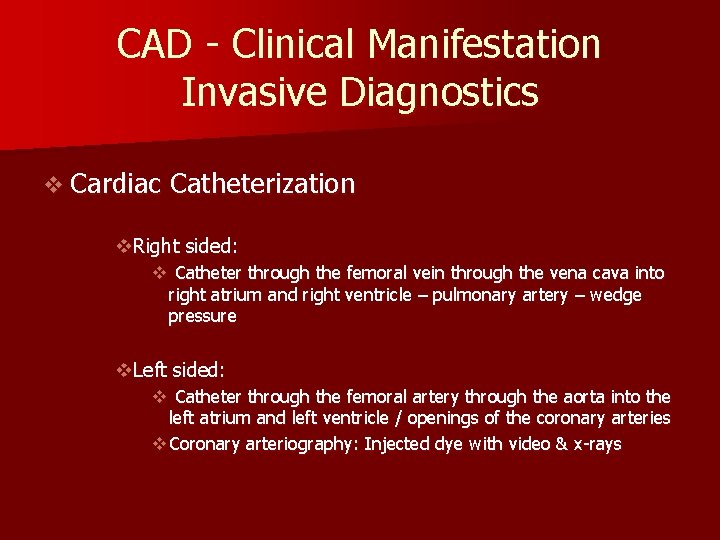
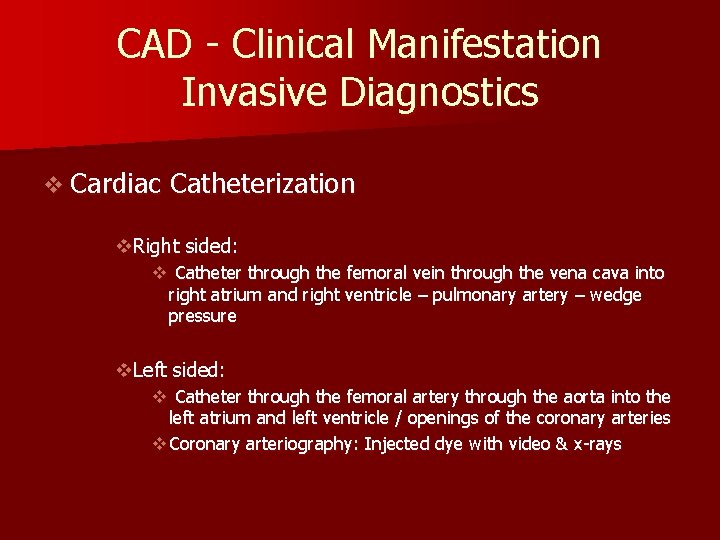
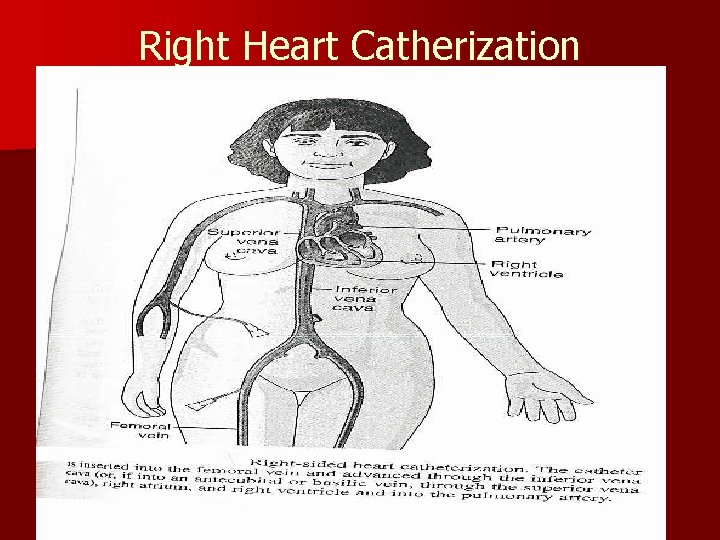
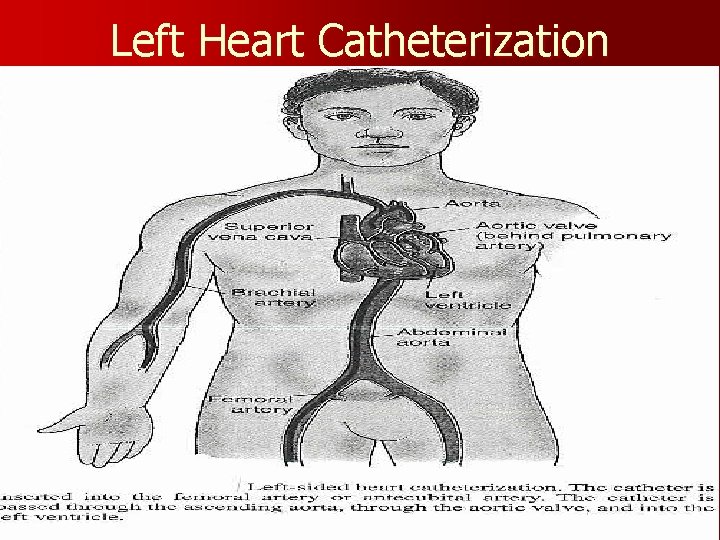
CAD - Clinical Manifestation Invasive Diagnostics v Cardiac Catheterization v. Right sided: v Catheter through the femoral vein through the vena cava into right atrium and right ventricle – pulmonary artery – wedge pressure v. Left sided: v Catheter through the femoral artery through the aorta into the left atrium and left ventricle / openings of the coronary arteries v Coronary arteriography: Injected dye with video & x-rays
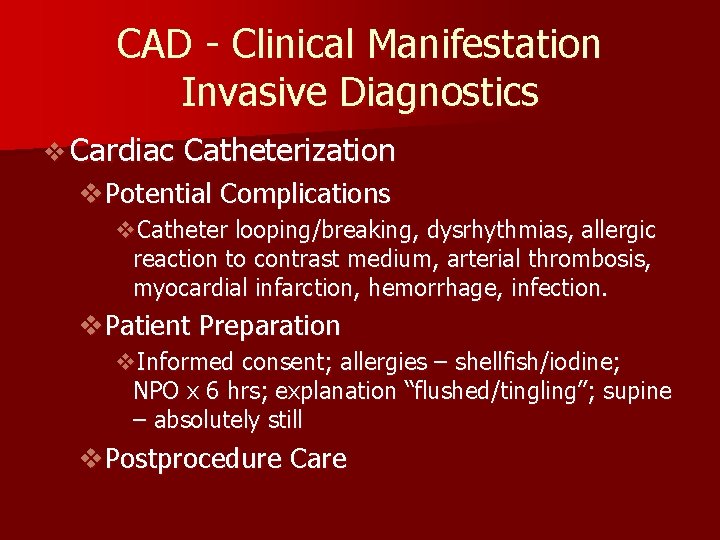
CAD - Clinical Manifestation Invasive Diagnostics v Cardiac Catheterization v. Potential Complications v. Catheter looping/breaking, dysrhythmias, allergic reaction to contrast medium, arterial thrombosis, myocardial infarction, hemorrhage, infection. v. Patient Preparation v. Informed consent; allergies – shellfish/iodine; NPO x 6 hrs; explanation “flushed/tingling”; supine – absolutely still v. Postprocedure Care
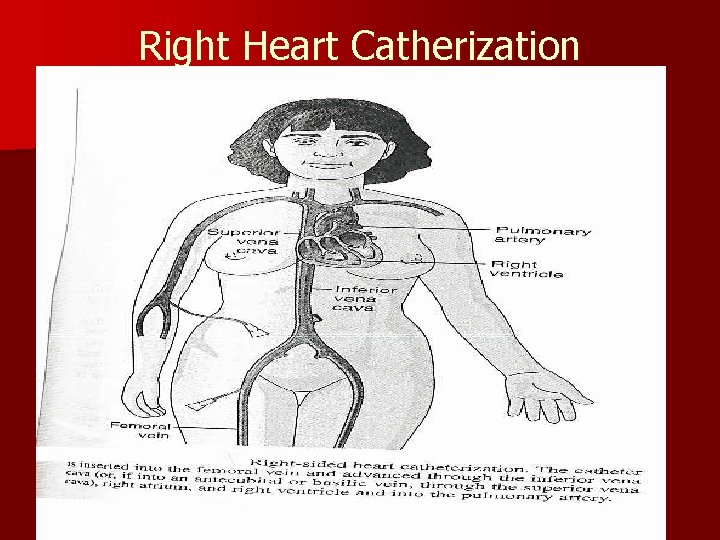
Right Heart Catherization
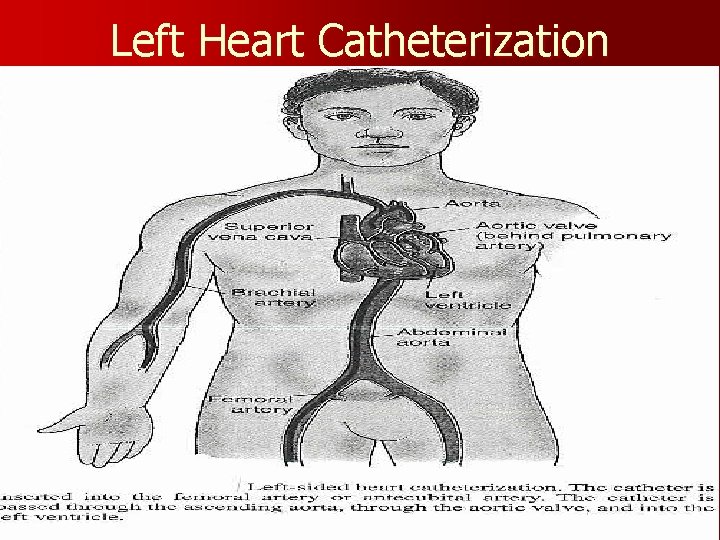
Left Heart Catheterization
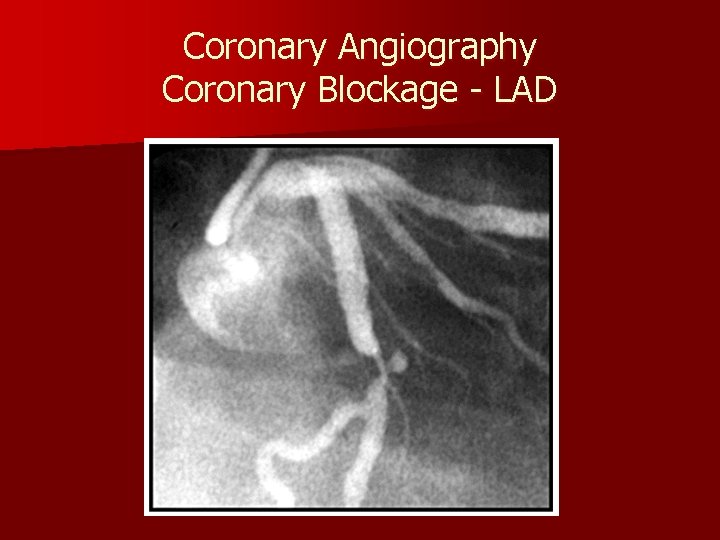
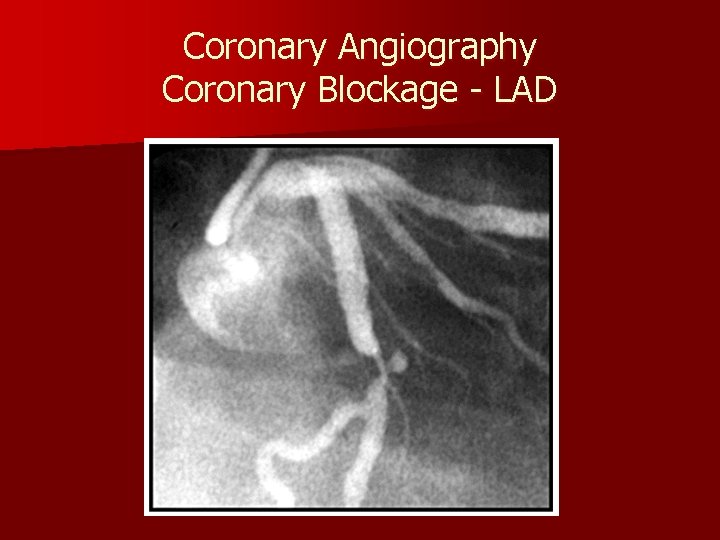
Coronary Angiography Coronary Blockage - LAD
Cardiac Catheterization Post Procedure Care v Assess: v v v Nursing Action: v v VS q 15 mins. x 2 hrs; q 30 min x 2 hrs Monitor cardiac rate and rhythm Check site for bleeding Extremity: Peripheral pulse check, temperature, color, sensation, mobility Assess for chest pain, dizziness, dyspnea Straight at groin x 24 hours; pressure at site x 30 mins. Maintain IV KVO for 2 hrs; IV capped x 2 hrs; then d/c Encourage oral fluids Patient/Family Education: v v Rationale for all nursing actions No squatting, sitting, lifting for 24 – 48 hours++ Report bleeding, swelling, discoloration, drainage Change dressing after 24 hours – small dressing to bandaid
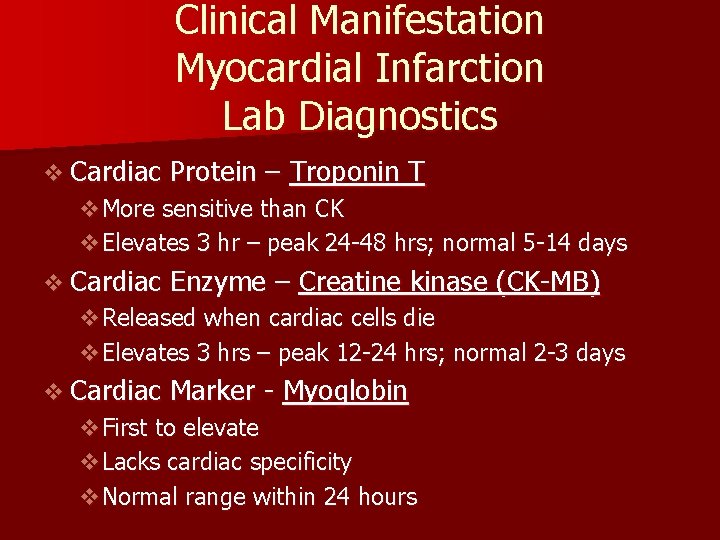
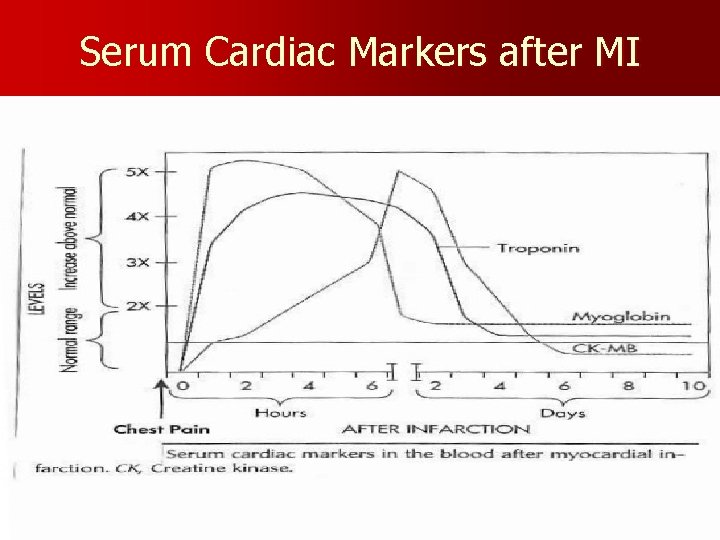
Clinical Manifestation Myocardial Infarction Lab Diagnostics v Cardiac Protein – Troponin T v. More sensitive than CK v. Elevates 3 hr – peak 24 -48 hrs; normal 5 -14 days v Cardiac Enzyme – Creatine kinase (CK-MB) v. Released when cardiac cells die v. Elevates 3 hrs – peak 12 -24 hrs; normal 2 -3 days v Cardiac Marker - Myoglobin v. First to elevate v. Lacks cardiac specificity v. Normal range within 24 hours
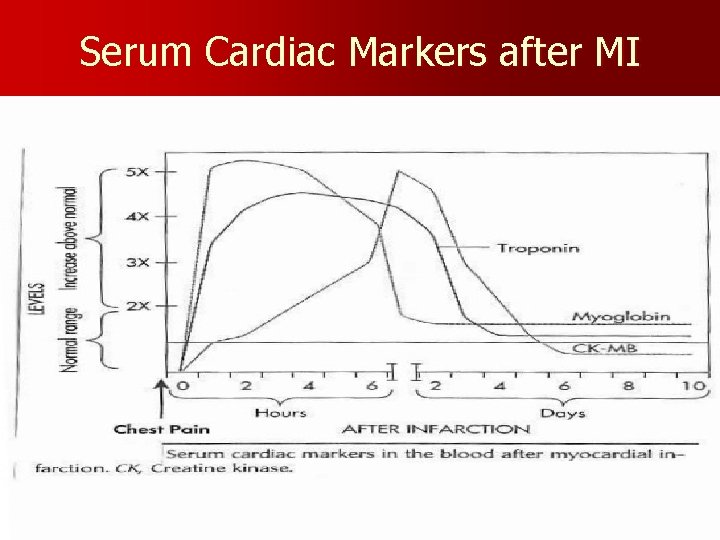
Serum Cardiac Markers after MI
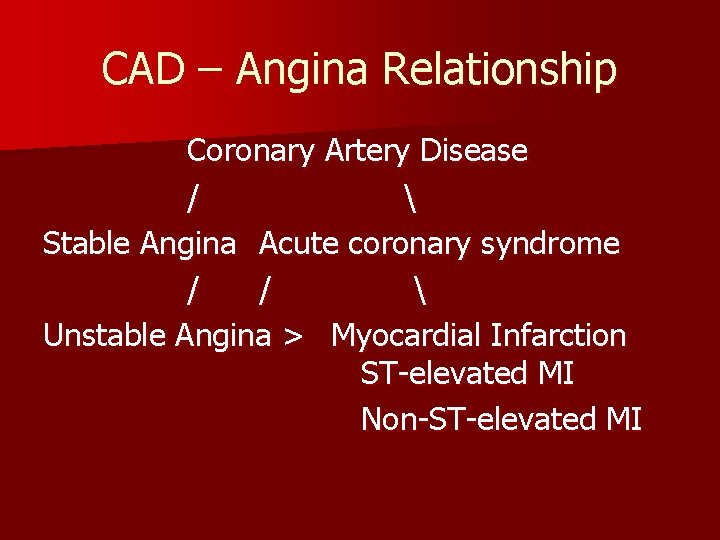
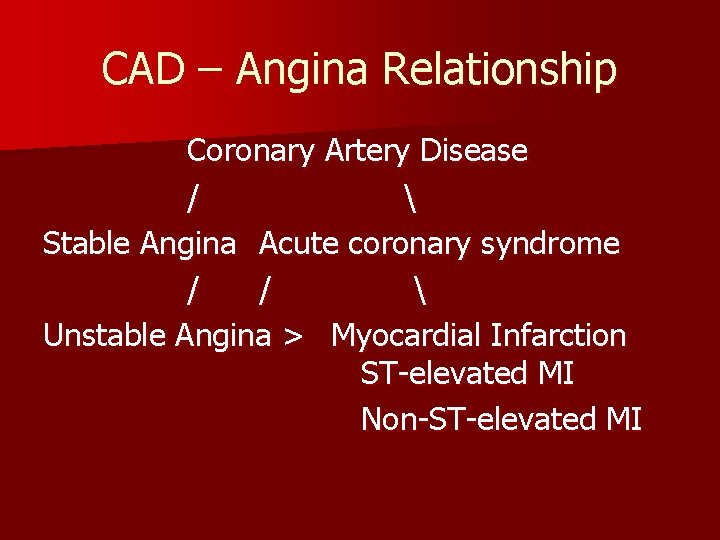
CAD – Angina Relationship Coronary Artery Disease / Stable Angina Acute coronary syndrome / / Unstable Angina > Myocardial Infarction ST-elevated MI Non-ST-elevated MI
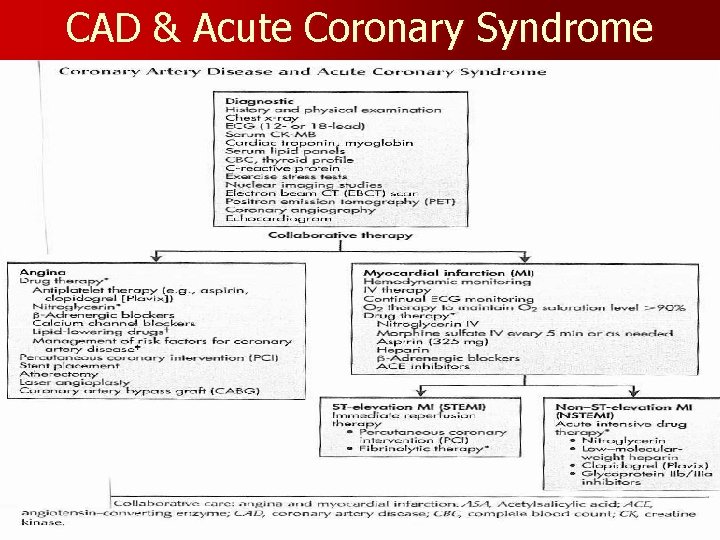
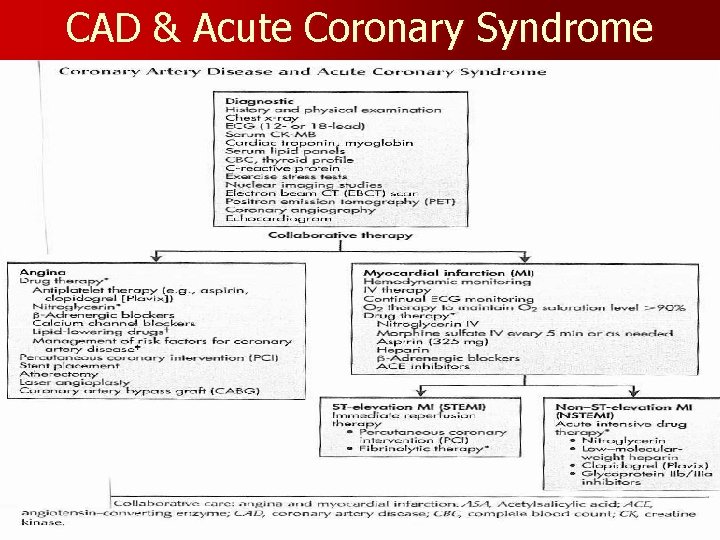
CAD & Acute Coronary Syndrome
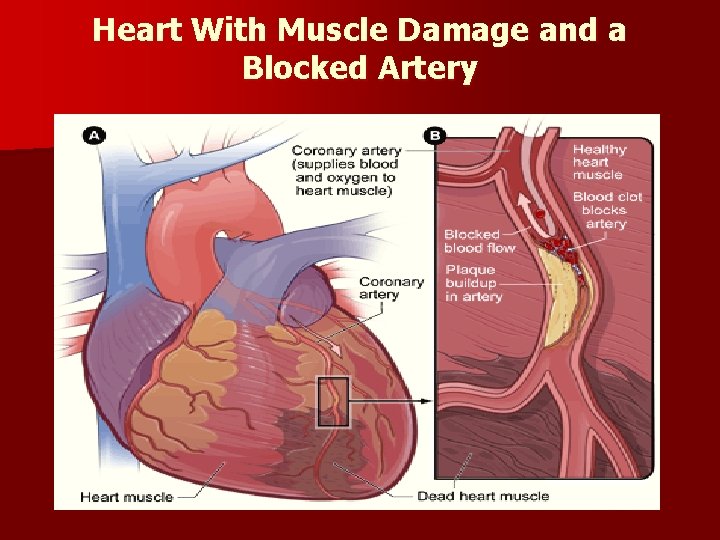
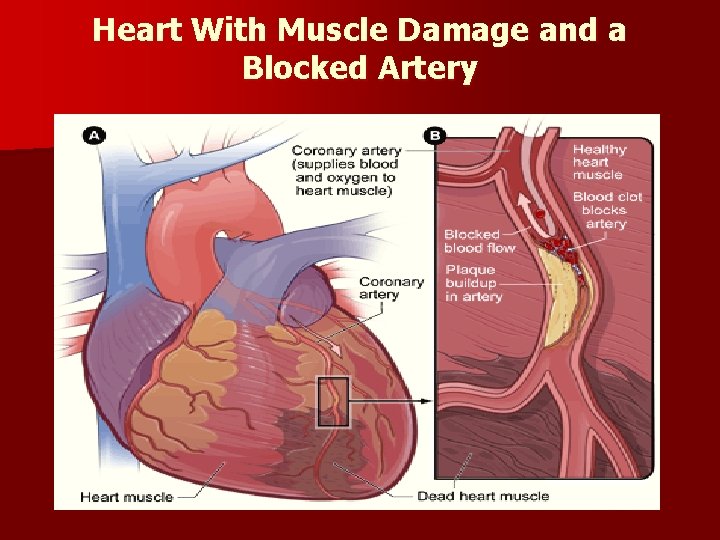
Heart With Muscle Damage and a Blocked Artery
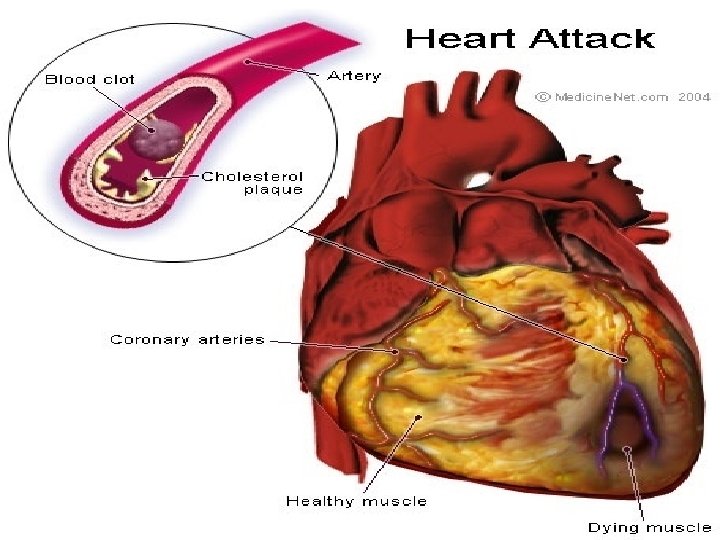
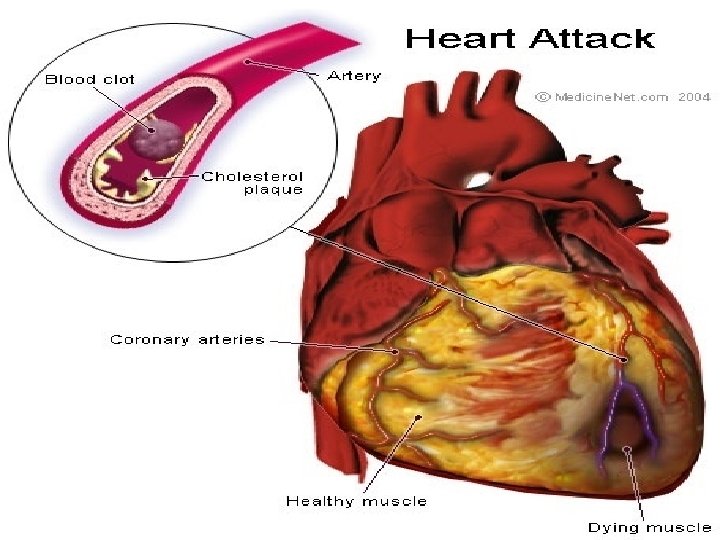
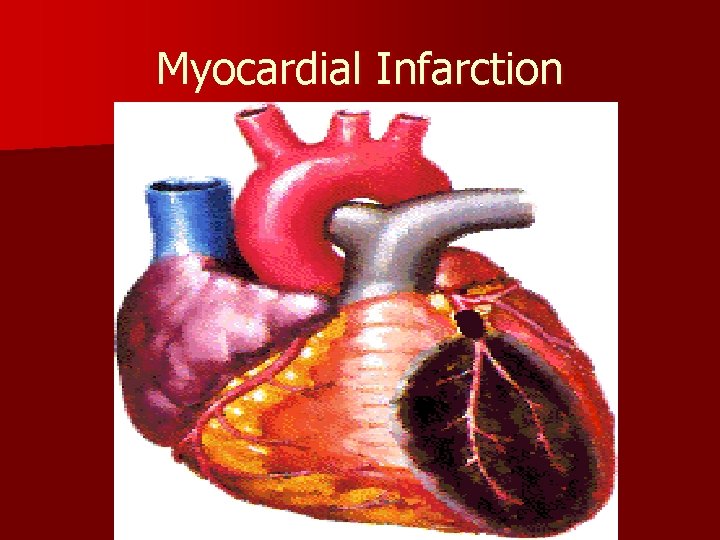
Myocardial Infarction
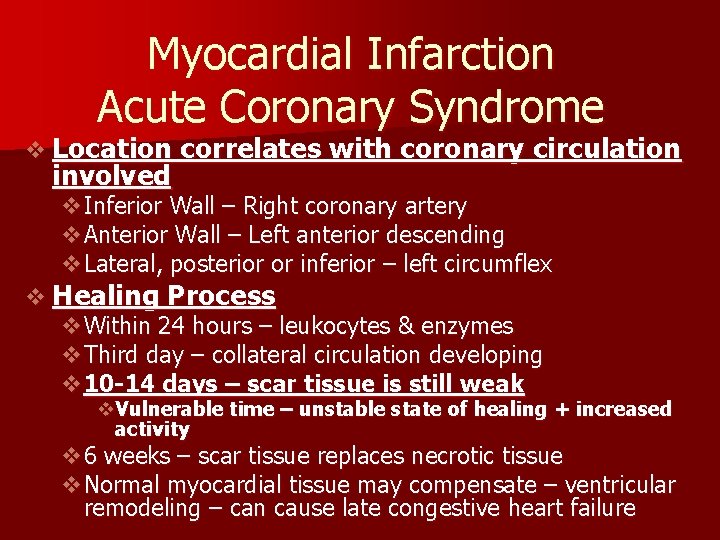
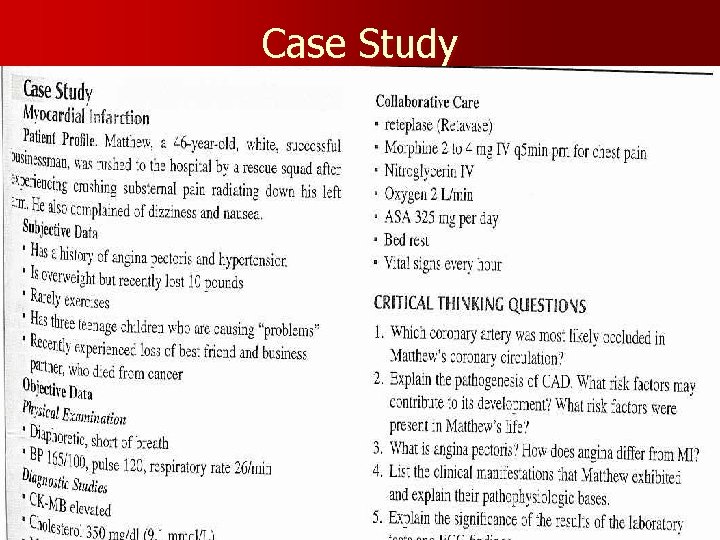
Myocardial Infarction Acute Coronary Syndrome v Location involved correlates with coronary circulation v. Inferior Wall – Right coronary artery v. Anterior Wall – Left anterior descending v. Lateral, posterior or inferior – left circumflex v Healing Process v. Within 24 hours – leukocytes & enzymes v. Third day – collateral circulation developing v 10 -14 days – scar tissue is still weak v. Vulnerable time – unstable state of healing + increased activity v 6 weeks – scar tissue replaces necrotic tissue v. Normal myocardial tissue may compensate – ventricular remodeling – can cause late congestive heart failure
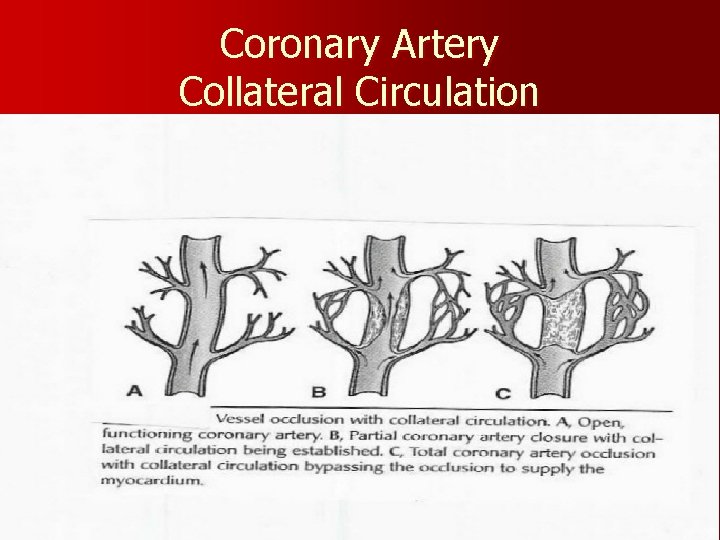
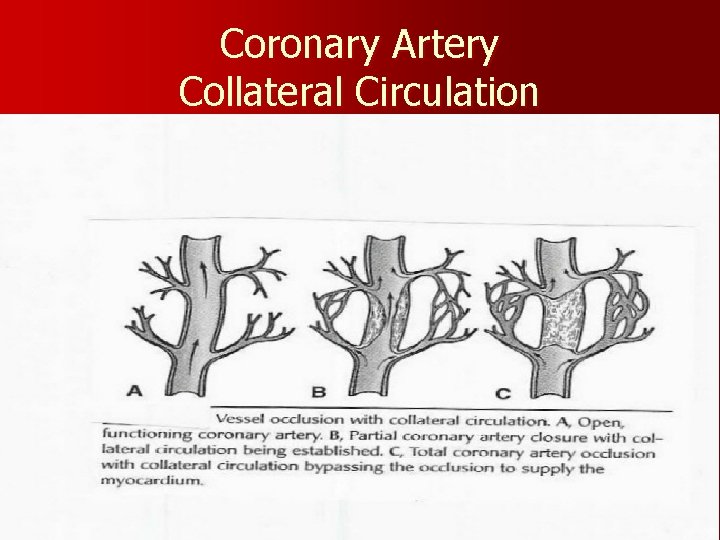
Coronary Artery Collateral Circulation
Angina Medical Management v. A Aspirin / Antianginal therapy / ACE Inhibitor v. B b-Adrenergic blocker / blood pressure v. C Cigarette smoking / Cholesterol v. D Diet / Diabetes v. E Education / Exercise
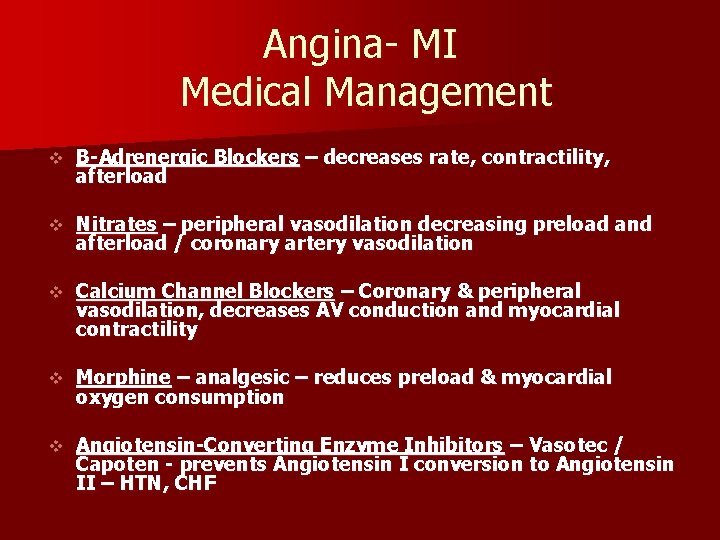
Angina- MI Medical Management v B-Adrenergic Blockers – decreases rate, contractility, afterload v Nitrates – peripheral vasodilation decreasing preload and afterload / coronary artery vasodilation v Calcium Channel Blockers – Coronary & peripheral vasodilation, decreases AV conduction and myocardial contractility v Morphine – analgesic – reduces preload & myocardial oxygen consumption v Angiotensin-Converting Enzyme Inhibitors – Vasotec / Capoten - prevents Angiotensin I conversion to Angiotensin II – HTN, CHF
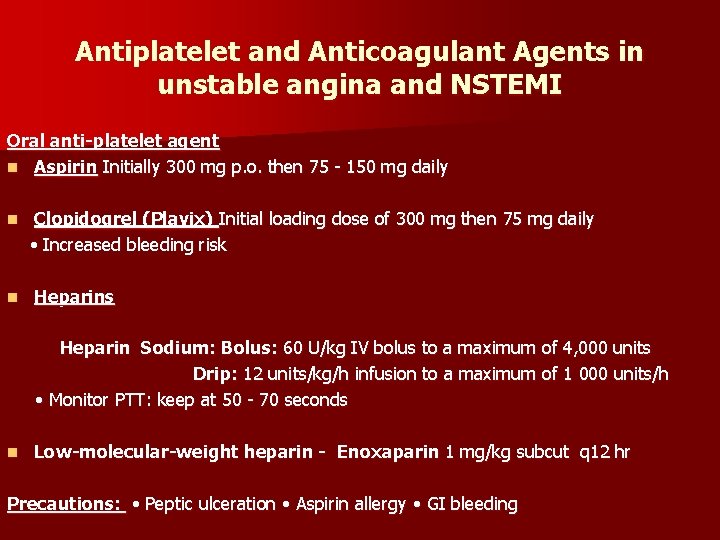
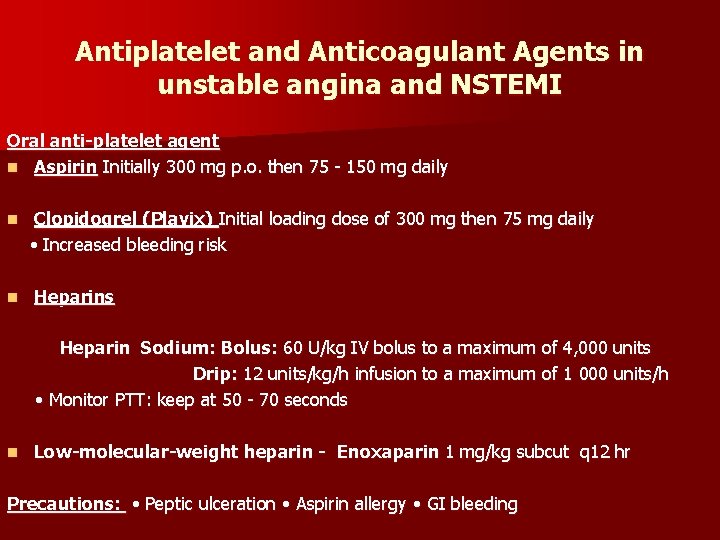
Antiplatelet and Anticoagulant Agents in unstable angina and NSTEMI Oral anti-platelet agent n Aspirin Initially 300 mg p. o. then 75 - 150 mg daily n n Clopidogrel (Plavix) Initial loading dose of 300 mg then 75 mg daily • Increased bleeding risk Heparins Heparin Sodium: Bolus: 60 U/kg IV bolus to a maximum of 4, 000 units Drip: 12 units/kg/h infusion to a maximum of 1 000 units/h • Monitor PTT: keep at 50 - 70 seconds n Low-molecular-weight heparin - Enoxaparin 1 mg/kg subcut q 12 hr Precautions: • Peptic ulceration • Aspirin allergy • GI bleeding
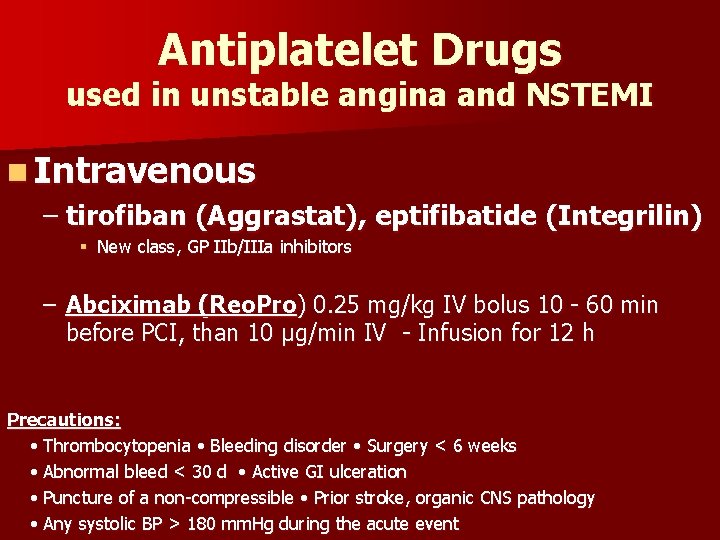
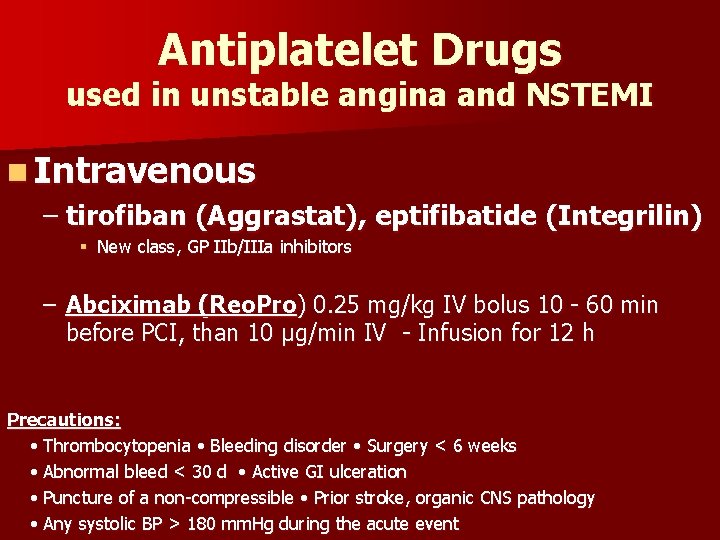
Antiplatelet Drugs used in unstable angina and NSTEMI n Intravenous – tirofiban (Aggrastat), eptifibatide (Integrilin) § New class, GP IIb/IIIa inhibitors – Abciximab (Reo. Pro) 0. 25 mg/kg IV bolus 10 - 60 min before PCI, than 10 μg/min IV - Infusion for 12 h Precautions: • Thrombocytopenia • Bleeding disorder • Surgery < 6 weeks • Abnormal bleed < 30 d • Active GI ulceration • Puncture of a non-compressible • Prior stroke, organic CNS pathology • Any systolic BP > 180 mm. Hg during the acute event
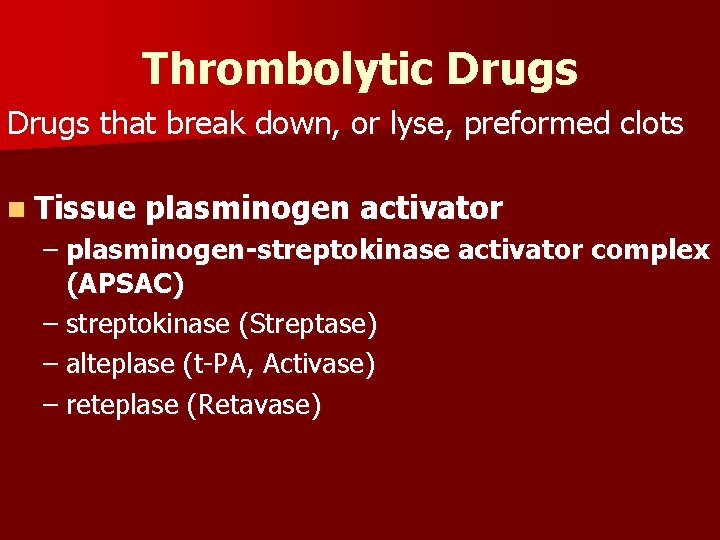
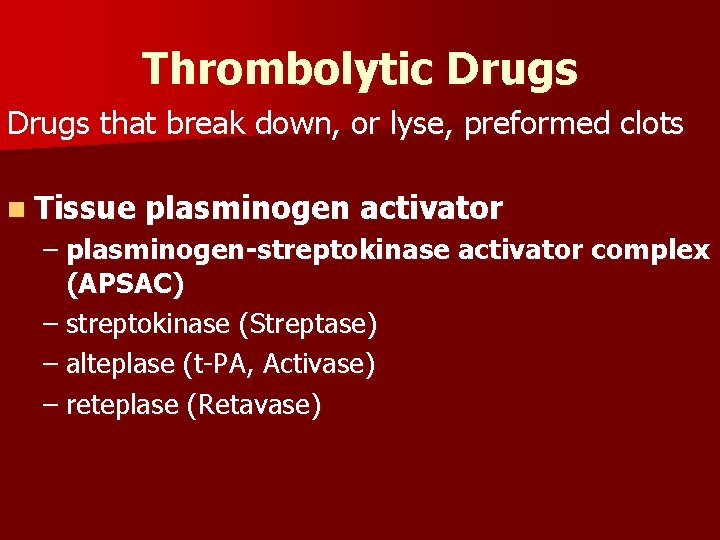
Thrombolytic Drugs that break down, or lyse, preformed clots n Tissue plasminogen activator – plasminogen-streptokinase activator complex (APSAC) – streptokinase (Streptase) – alteplase (t-PA, Activase) – reteplase (Retavase)
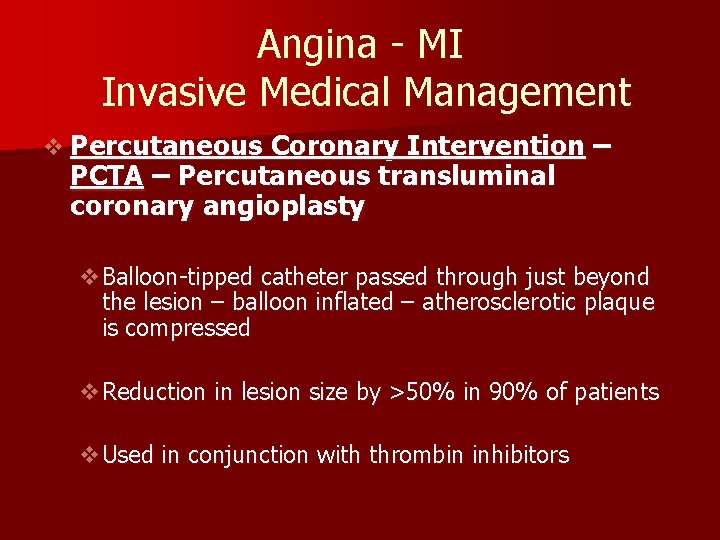
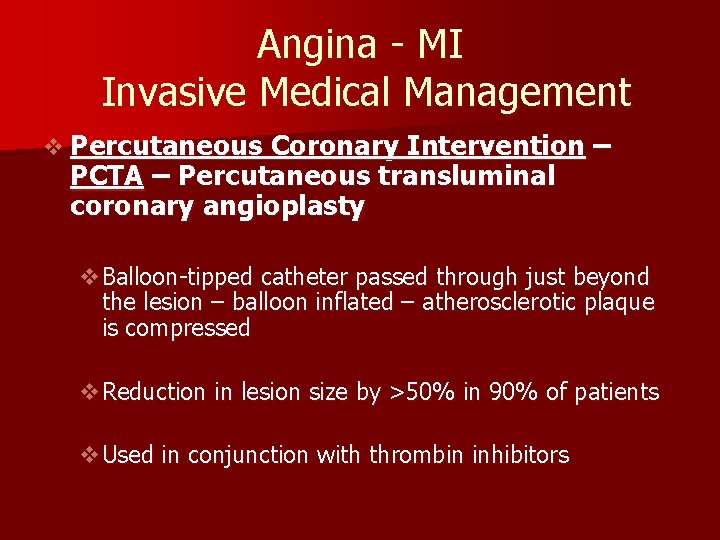
Angina - MI Invasive Medical Management v Percutaneous Coronary Intervention – PCTA – Percutaneous transluminal coronary angioplasty v. Balloon-tipped catheter passed through just beyond the lesion – balloon inflated – atherosclerotic plaque is compressed v. Reduction in lesion size by >50% in 90% of patients v. Used in conjunction with thrombin inhibitors
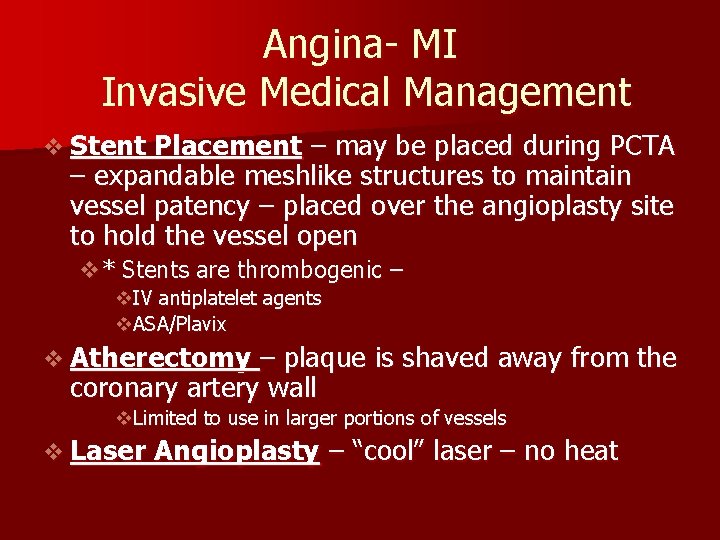
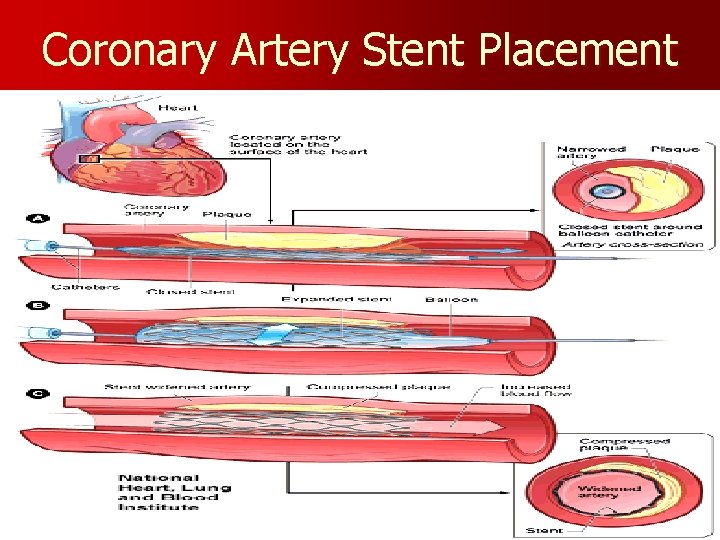
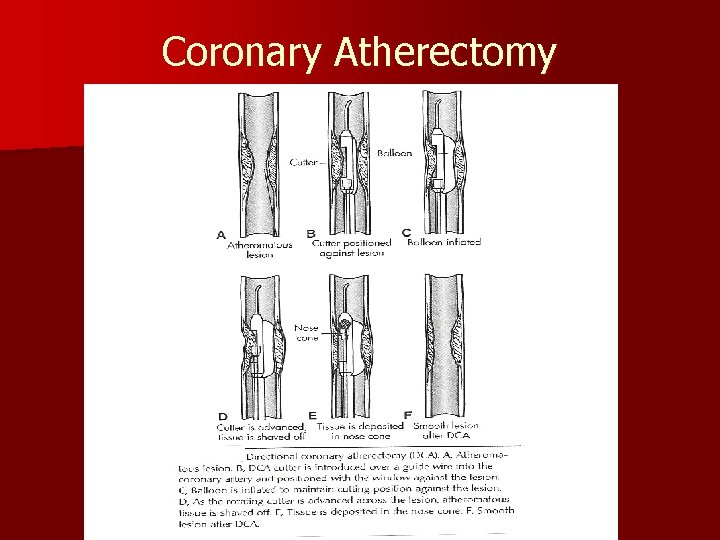
Angina- MI Invasive Medical Management v Stent Placement – may be placed during PCTA – expandable meshlike structures to maintain vessel patency – placed over the angioplasty site to hold the vessel open v* Stents are thrombogenic – v. IV antiplatelet agents v. ASA/Plavix v Atherectomy – plaque is shaved away from the coronary artery wall v. Limited to use in larger portions of vessels v Laser Angioplasty – “cool” laser – no heat
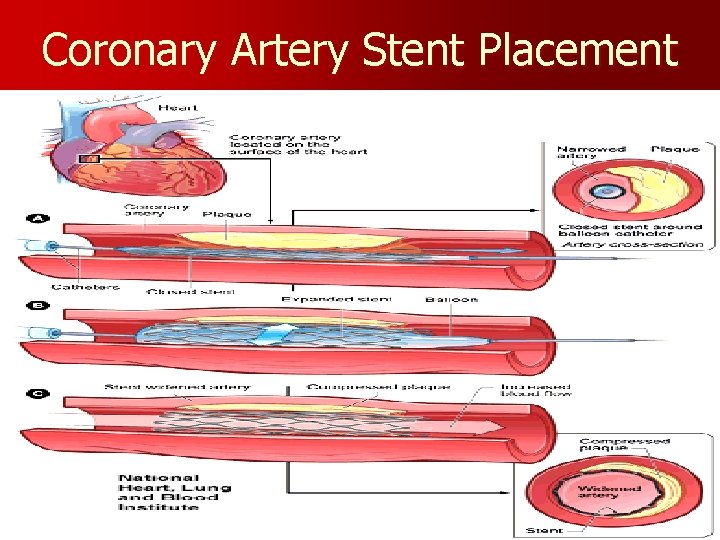
Coronary Artery Stent Placement
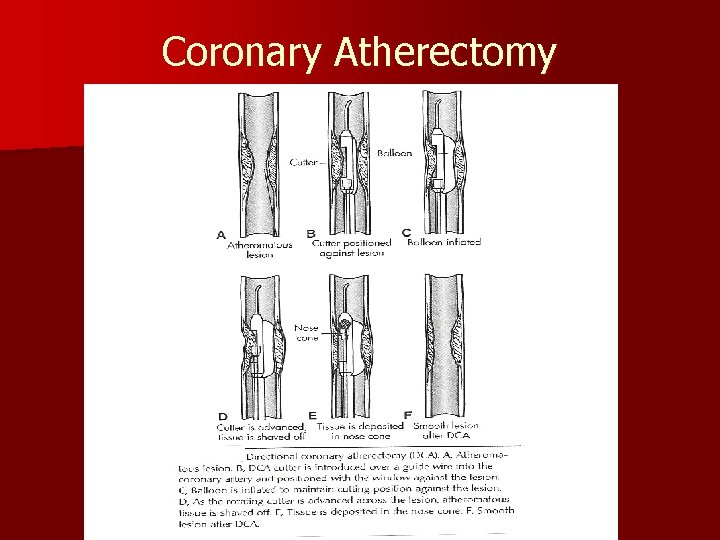
Coronary Atherectomy
Angina - MI Invasive Medical Management v Complications v. Abrupt closure of angioplasty site v Stent thrombosis / embolization v. Hemorrhage / vascular damage v. Coronary spasm, Acute MI v. Need for emergent coronary artery bypass graft (CABG)
Fibrinolytic Contraindications v Absolute Contraindications v. Active internal bleeding, active inflammatory bowel disease, active peptic ulcer disease, acute pericarditis, GI/GU bleeding within 6 months, Hx of hemorrhage CVA, Neurosurgical procedure within 2 months, Pregnancy, Suspected aortic dissection, Uncontrolled HTN, >180/110 v Relative Contraindications v. Bacterial endocarditis, chronic Coumadin Therapy, Diabetic hemorrhagic retinopathy, Poorly controlled HTN
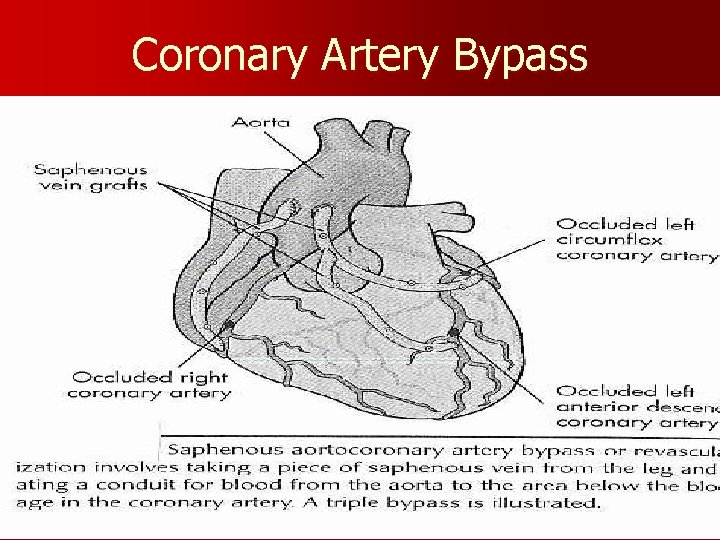
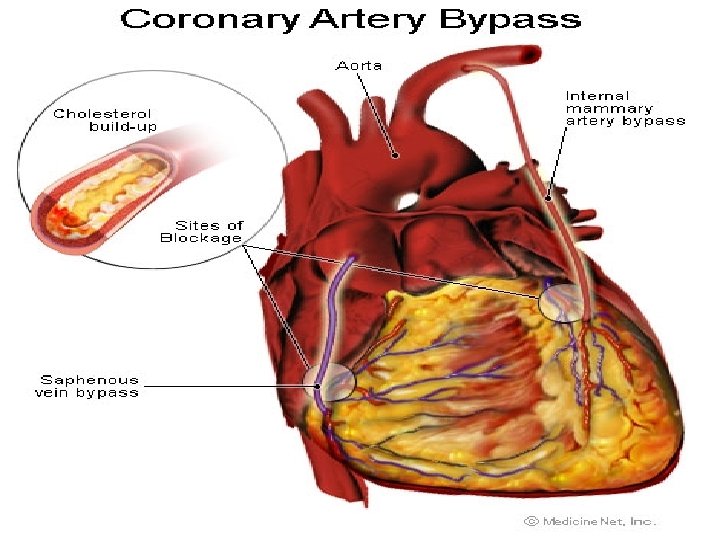
Angina - MI Surgical Management Coronary Artery Bypass Graft (CABG) construction of new vessels between the aorta to beyond the obstructed coronary artery (or arteries) v. Saphenous vein or internal mammary artery v. Palliative treatment for CAD – not a cure v. Postoperative care: Care of cardiac patient with chest tubes / sternotomy; pain management; short ventilator support; early ambulation; 4 -5 day hospital stay
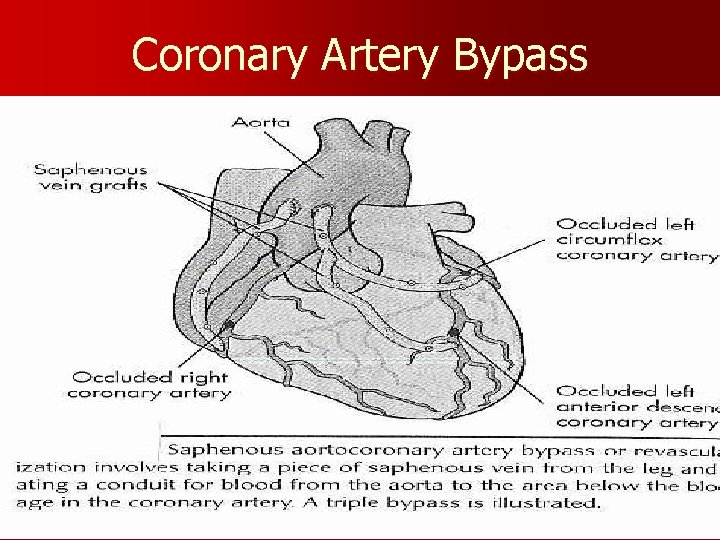
Coronary Artery Bypass
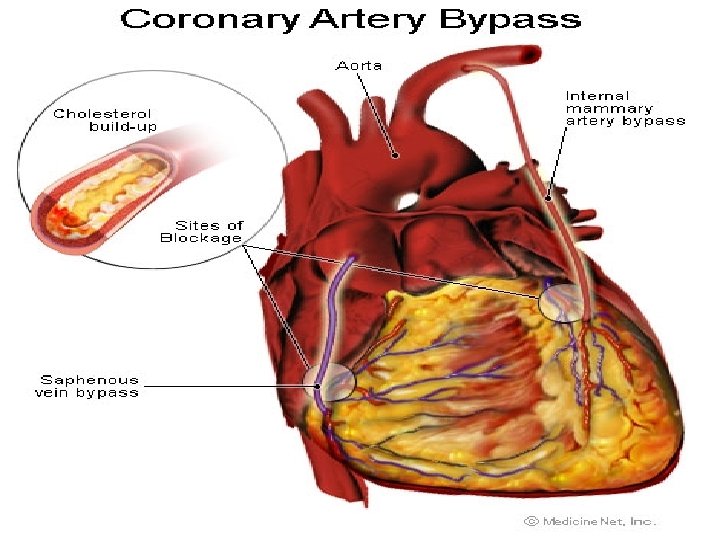
Coronary Artery Bypass
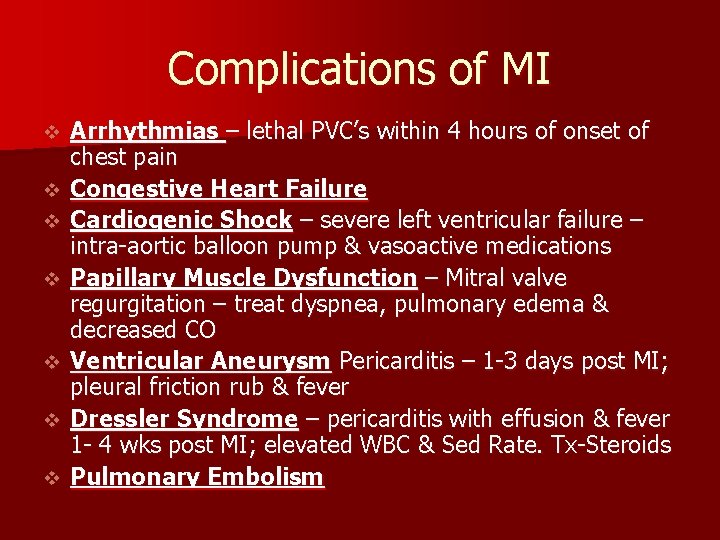
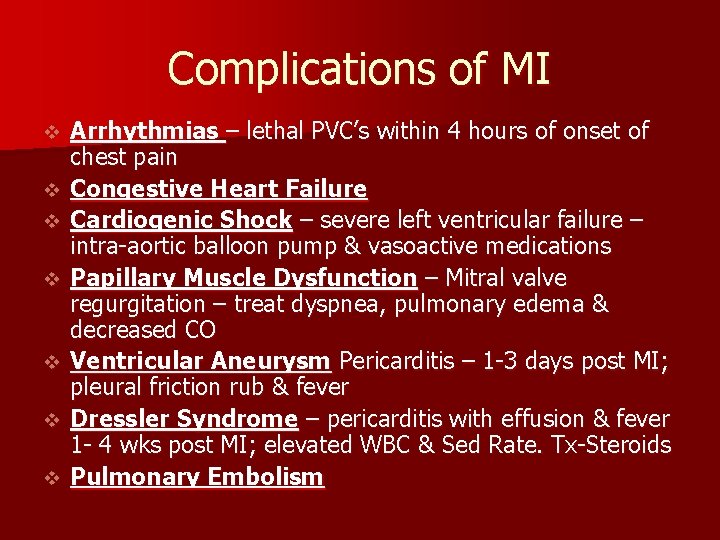
Complications of MI v v v v Arrhythmias – lethal PVC’s within 4 hours of onset of chest pain Congestive Heart Failure Cardiogenic Shock – severe left ventricular failure – intra-aortic balloon pump & vasoactive medications Papillary Muscle Dysfunction – Mitral valve regurgitation – treat dyspnea, pulmonary edema & decreased CO Ventricular Aneurysm Pericarditis – 1 -3 days post MI; pleural friction rub & fever Dressler Syndrome – pericarditis with effusion & fever 1 - 4 wks post MI; elevated WBC & Sed Rate. Tx-Steroids Pulmonary Embolism
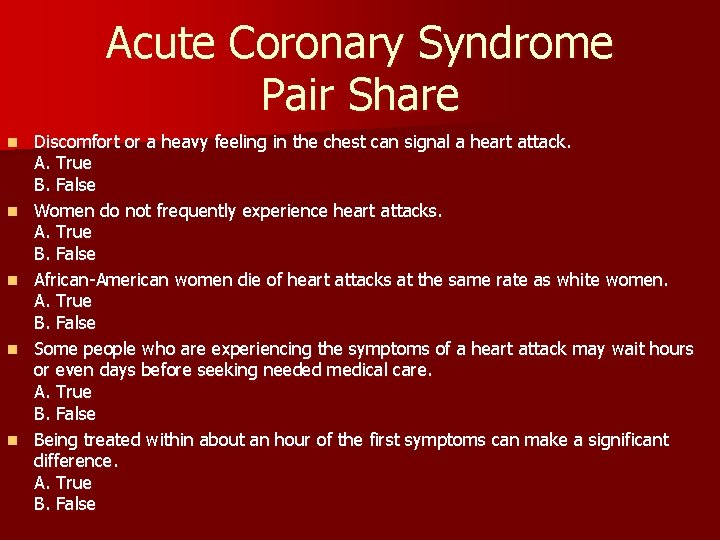
Acute Coronary Syndrome Pair Share n n n Discomfort or a heavy feeling in the chest can signal a heart attack. A. True B. False Women do not frequently experience heart attacks. A. True B. False African-American women die of heart attacks at the same rate as white women. A. True B. False Some people who are experiencing the symptoms of a heart attack may wait hours or even days before seeking needed medical care. A. True B. False Being treated within about an hour of the first symptoms can make a significant difference. A. True B. False
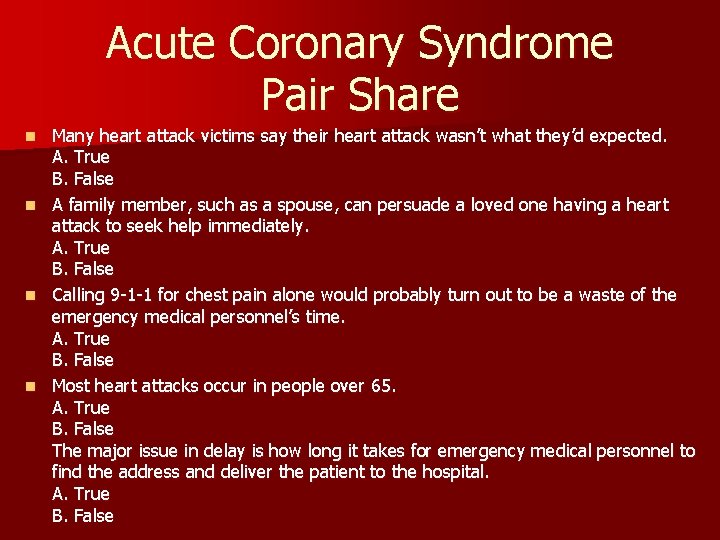
Acute Coronary Syndrome Pair Share Many heart attack victims say their heart attack wasn’t what they’d expected. A. True B. False n A family member, such as a spouse, can persuade a loved one having a heart attack to seek help immediately. A. True B. False n Calling 9 -1 -1 for chest pain alone would probably turn out to be a waste of the emergency medical personnel’s time. A. True B. False n Most heart attacks occur in people over 65. A. True B. False The major issue in delay is how long it takes for emergency medical personnel to find the address and deliver the patient to the hospital. A. True B. False n
Nursing Diagnoses TOP 4 ? ? ?
Nursing Process Nsg Dx: Acute Pain related to Cardiac Ischemia v Assess: Chest pain—intensity, location, duration, precipitating, alleviating factors; Monitor cardiac rate & rhythm; effect of pain medication; peripheral pulses; VS; Pulse Oximetry v Nsg Action: Administer O 2 NC; IV access; position of comfort v Patient Education: Rationale for all procedures; pain scale; instruct to report pain
Nsg Dx: Ineffective Tissue Perfusion related to Myocardial Injury v Assess: VS & Pulse Oximetry qh; continuous cardiac monitoring; respiratory status if Morphine IV is used; fluid balance – strict I&O peripheral edema; heart & breath sounds v Nsg Action: Rest periods; Administer meds & oxygen as ordered v Patient Education: Rationale for rest; energy conservation
Nsg Dx: Anxiety related to perceived or actual threat of death v Assess: verbal & nonverbal queues v Nsg Action: Calm, reassuring approach; encourage verbalization of feelings, fears, perceptions; family involvement; v Patient Education: Relaxation techniques; simple instructions
Nsg Dx: Ineffective therapeutic regimen management related to lack of knowledge v Assess: Current knowledge level & readiness to learn; family dynamics v Nsg Action: Assist pt in identifying small successes; Assist pt is identifying lifestyle that needs to be changed; Community referrals— smoking cessation, cardiac rehab, support groups, v Patient Education: Lifestyle changes, Medications—desired effect/side effects; comprehensive discharge plan—continuity with community cardiac rehabilitation
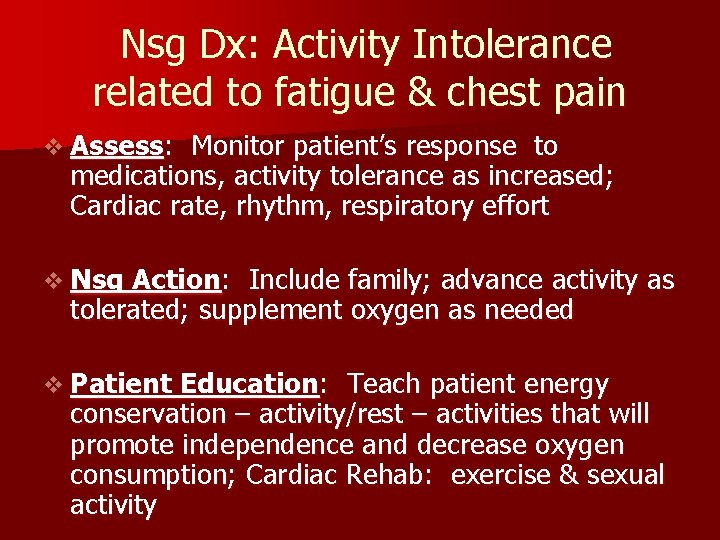
Nsg Dx: Activity Intolerance related to fatigue & chest pain v Assess: Monitor patient’s response to medications, activity tolerance as increased; Cardiac rate, rhythm, respiratory effort v Nsg Action: Include family; advance activity as tolerated; supplement oxygen as needed v Patient Education: Teach patient energy conservation – activity/rest – activities that will promote independence and decrease oxygen consumption; Cardiac Rehab: exercise & sexual activity
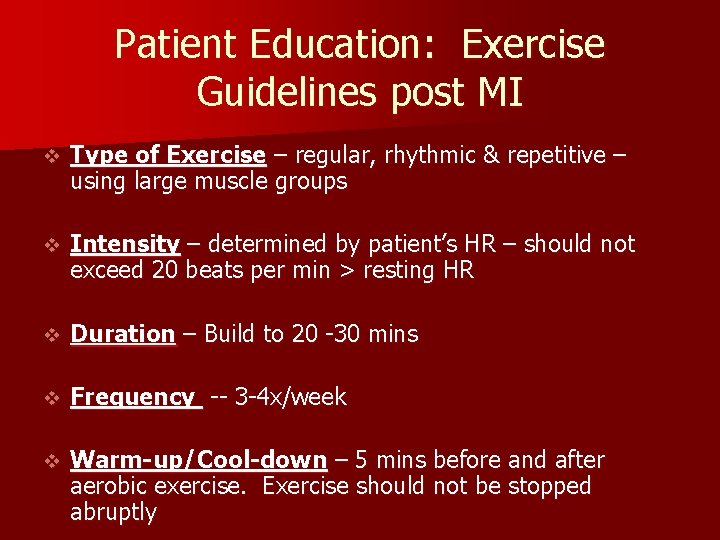
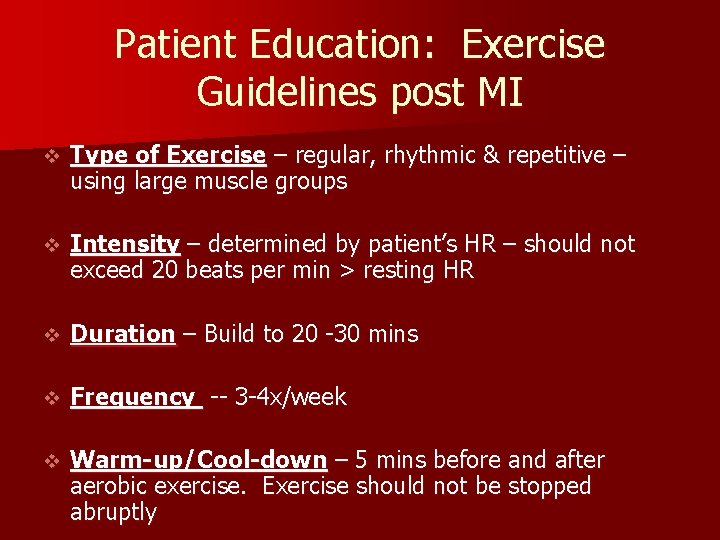
Patient Education: Exercise Guidelines post MI v Type of Exercise – regular, rhythmic & repetitive – using large muscle groups v Intensity – determined by patient’s HR – should not exceed 20 beats per min > resting HR v Duration – Build to 20 -30 mins v Frequency -- 3 -4 x/week v Warm-up/Cool-down – 5 mins before and after aerobic exercise. Exercise should not be stopped abruptly
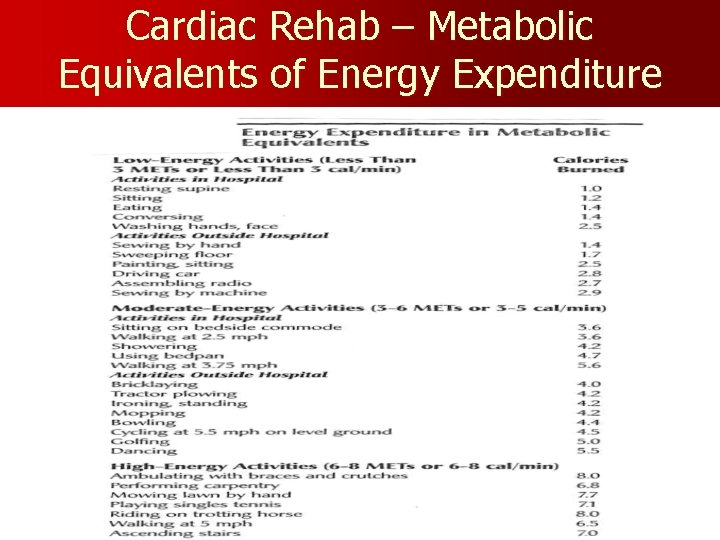
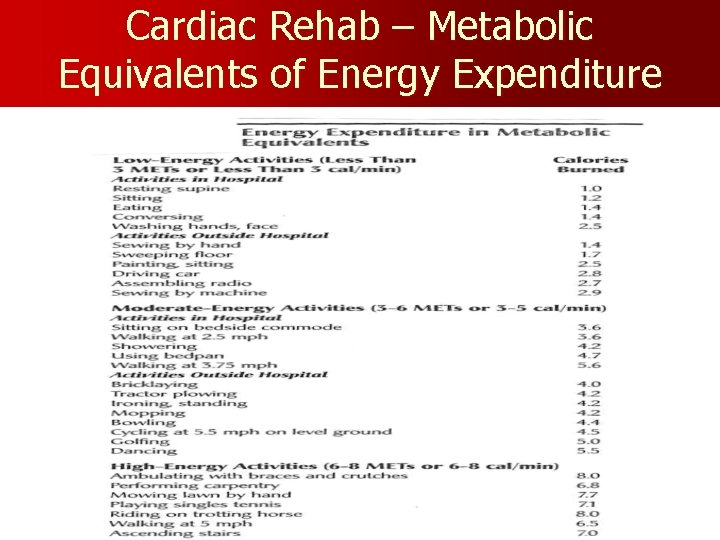
Cardiac Rehab – Metabolic Equivalents of Energy Expenditure
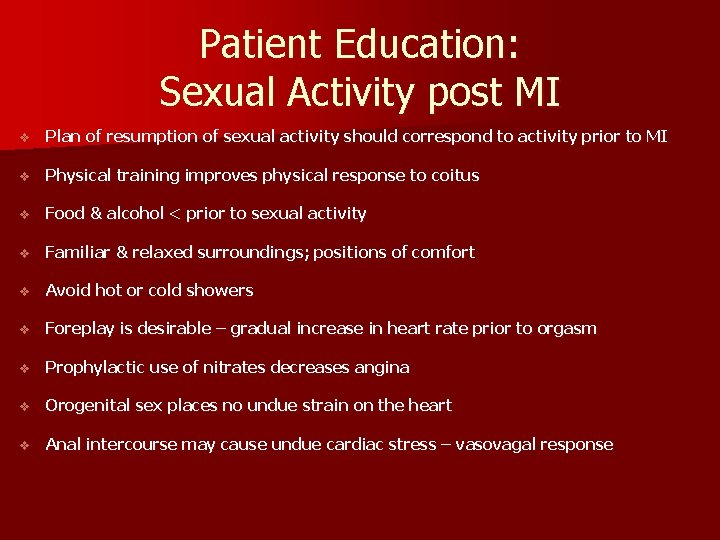
Patient Education: Sexual Activity post MI v Plan of resumption of sexual activity should correspond to activity prior to MI v Physical training improves physical response to coitus v Food & alcohol < prior to sexual activity v Familiar & relaxed surroundings; positions of comfort v Avoid hot or cold showers v Foreplay is desirable – gradual increase in heart rate prior to orgasm v Prophylactic use of nitrates decreases angina v Orogenital sex places no undue strain on the heart v Anal intercourse may cause undue cardiac stress – vasovagal response
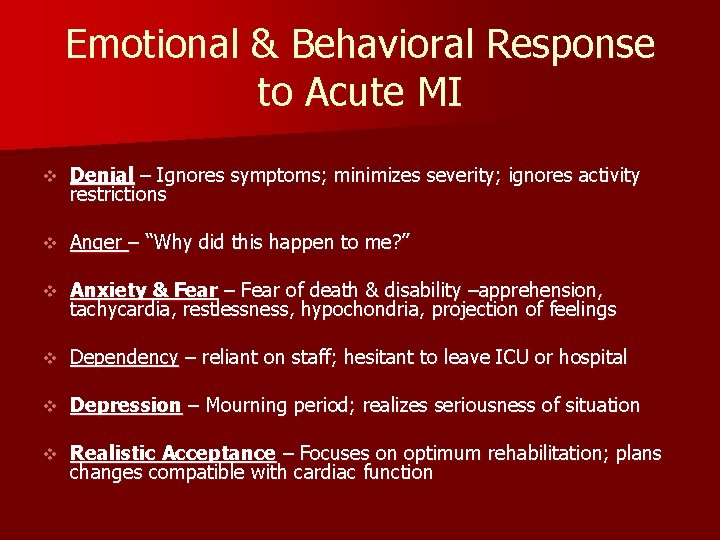
Emotional & Behavioral Response to Acute MI v Denial – Ignores symptoms; minimizes severity; ignores activity restrictions v Anger – “Why did this happen to me? ” v Anxiety & Fear – Fear of death & disability –apprehension, tachycardia, restlessness, hypochondria, projection of feelings v Dependency – reliant on staff; hesitant to leave ICU or hospital v Depression – Mourning period; realizes seriousness of situation v Realistic Acceptance – Focuses on optimum rehabilitation; plans changes compatible with cardiac function