Anatomy Physiology SIXTH EDITION Lecture 20 The Heart


- Slides: 48
Anatomy & Physiology SIXTH EDITION Lecture 20, The Heart Lecturer: Dr. Ebadi Room P 313 Phone: (718) 260 -5285 E-Mail: ibarjis@citytech. cuny. edu Copyright © 2004 Pearson Education, Inc. , publishing as Benjamin Cummings Frederic H. Martini Fundamentals of
Learning Objectives • Describe the organization of the cardiovascular system. • Describe the location and general features of the heart, including the pericardium. • Discuss the differences between nodal cells and conducting cells and describe the components and functions of the conducting system of the heart. • Identify the electrical events associated with a normal electrocardiogram.
Learning Objectives • Explain the events of the cardiac cycle including atrial and ventricular systole and diastole, and relate the heart sounds to specific events in the cycle. • Define cardiac output, heart rate and stroke volume and describe the factors that influence these variables. • Explain how adjustments in stroke volume and cardiac output are coordinated at different levels of activity.
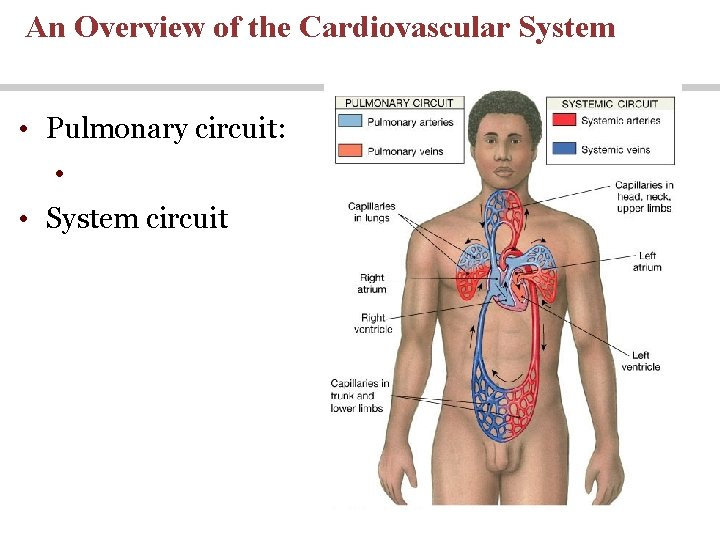
The cardiovascular system is divided into two circuits • Pulmonary circuit • Delivers blood from the right ventricle of the heart to the lungs and from the lungs to the left atrium of the heart • System circuit • Delivers blood from the left ventricle of the heart to the rest of the body and collects blood from the rest of the body and delivers it to the right atrium of the heart.
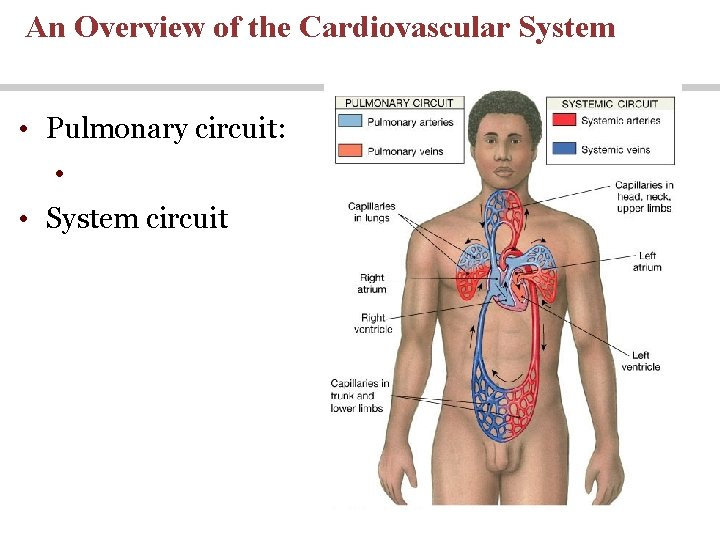
An Overview of the Cardiovascular System • Pulmonary circuit: • • System circuit
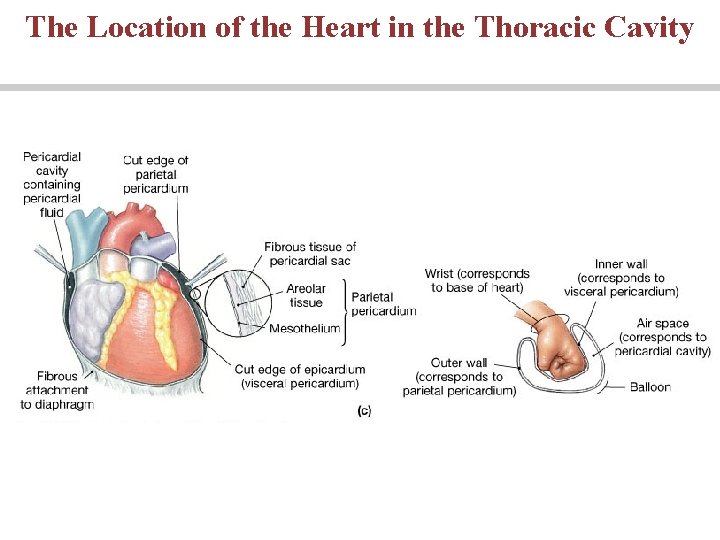
Anatomy of the Heart The pericardia • Visceral pericardium or epicardium • Parietal pericardium • Pericardial fluid
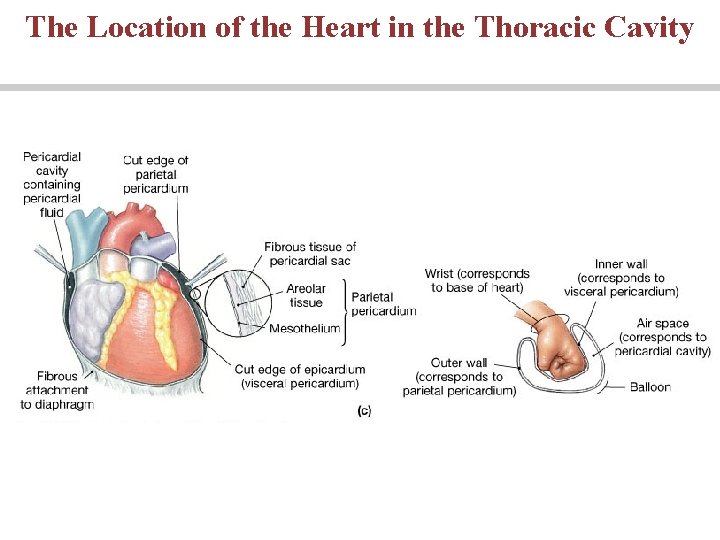
The Location of the Heart in the Thoracic Cavity
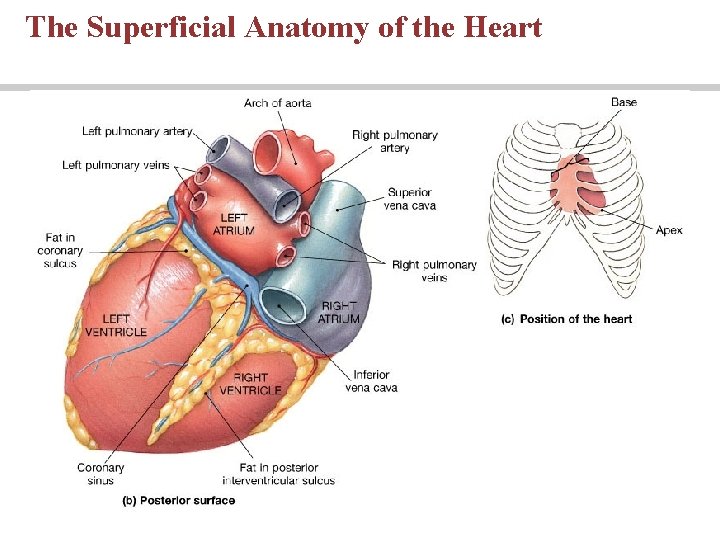
Superficial Anatomy of the Heart • The heart consists of four chambers • Two upper chamber called atria • Two lower chambers called ventricles • The two upper and two lower chambers are separated by atrioventricular valve
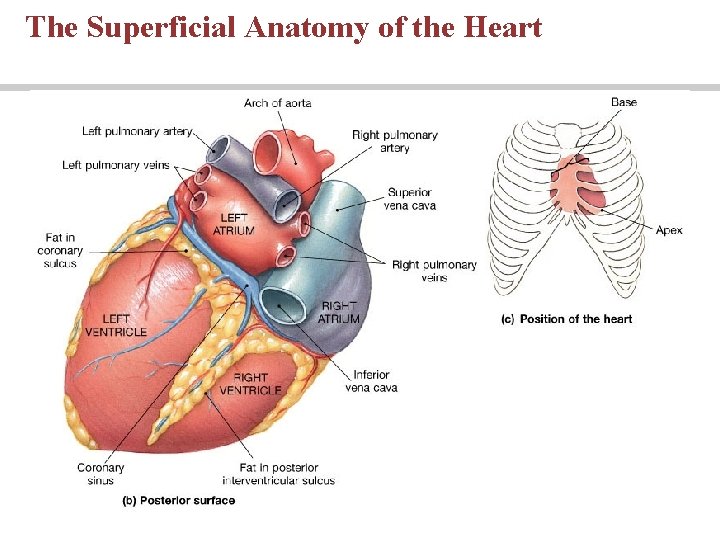
The Superficial Anatomy of the Heart
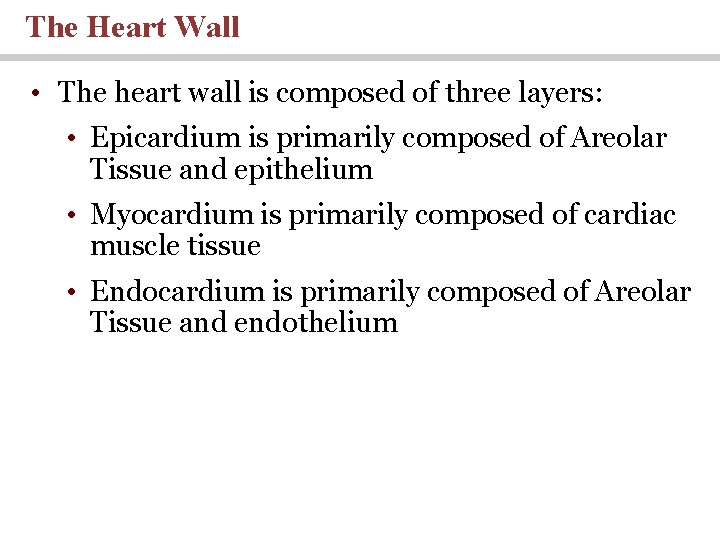
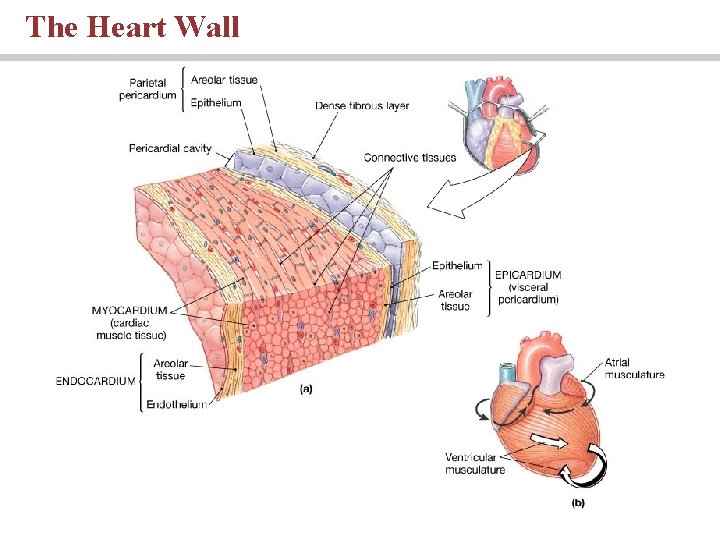
The Heart Wall • The heart wall is composed of three layers: • Epicardium is primarily composed of Areolar Tissue and epithelium • Myocardium is primarily composed of cardiac muscle tissue • Endocardium is primarily composed of Areolar Tissue and endothelium
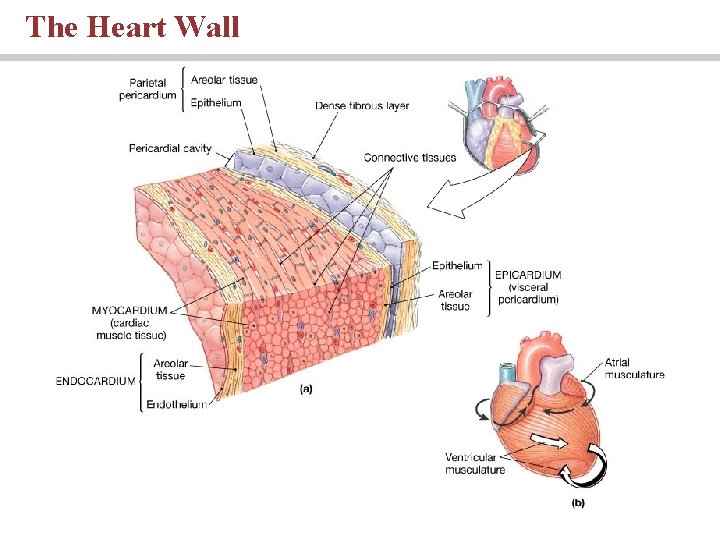
The Heart Wall
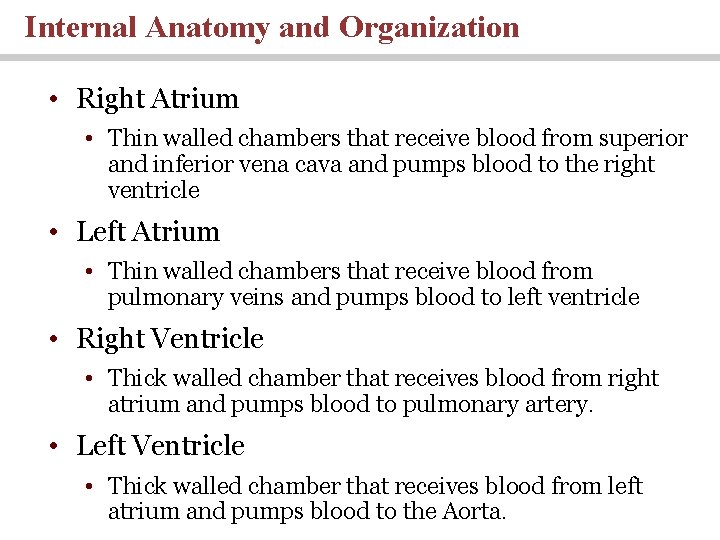
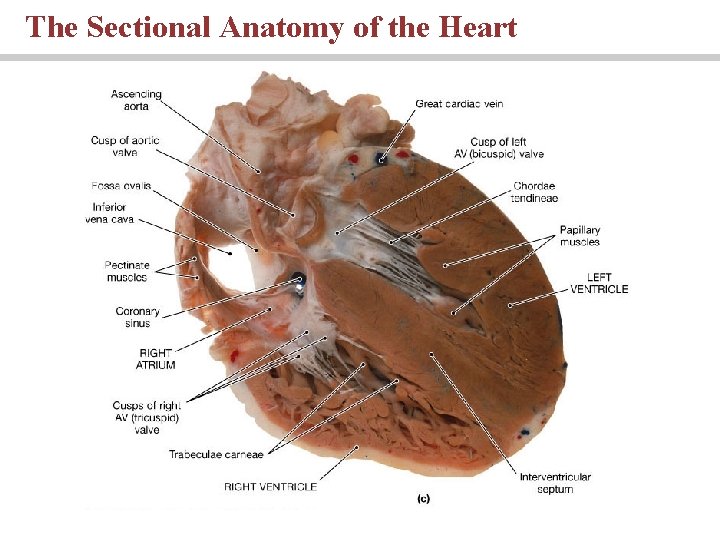
Internal Anatomy and Organization • Right Atrium • Thin walled chambers that receive blood from superior and inferior vena cava and pumps blood to the right ventricle • Left Atrium • Thin walled chambers that receive blood from pulmonary veins and pumps blood to left ventricle • Right Ventricle • Thick walled chamber that receives blood from right atrium and pumps blood to pulmonary artery. • Left Ventricle • Thick walled chamber that receives blood from left atrium and pumps blood to the Aorta.
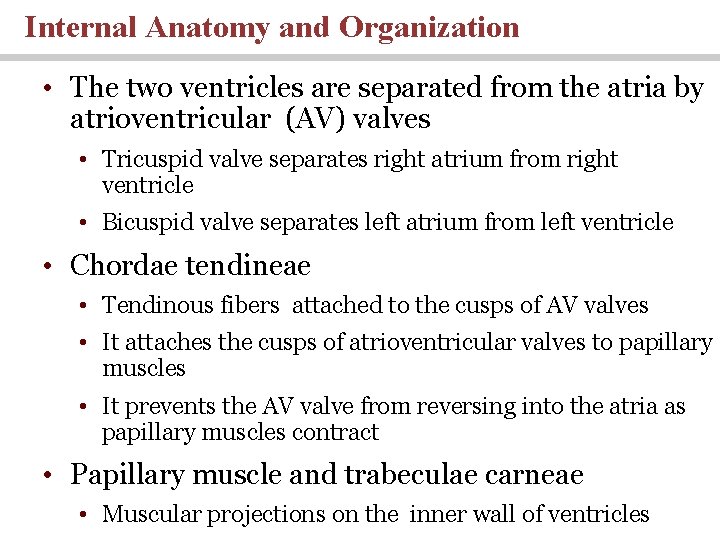
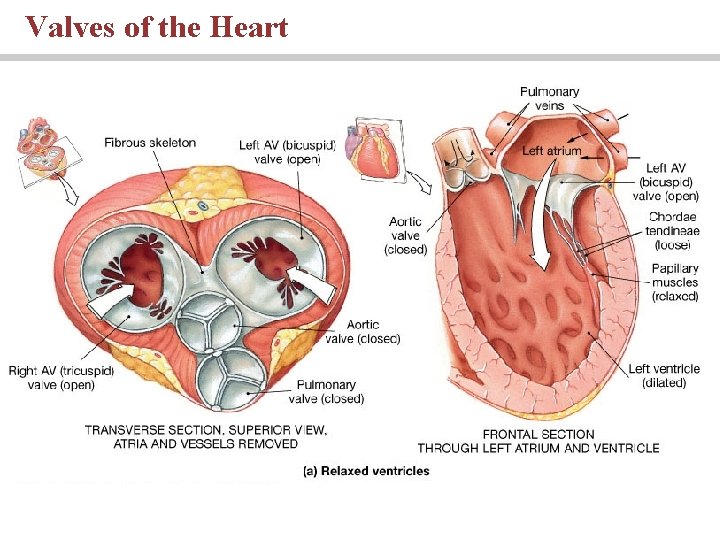
Internal Anatomy and Organization • The two ventricles are separated from the atria by atrioventricular (AV) valves • Tricuspid valve separates right atrium from right ventricle • Bicuspid valve separates left atrium from left ventricle • Chordae tendineae • Tendinous fibers attached to the cusps of AV valves • It attaches the cusps of atrioventricular valves to papillary muscles • It prevents the AV valve from reversing into the atria as papillary muscles contract • Papillary muscle and trabeculae carneae • Muscular projections on the inner wall of ventricles
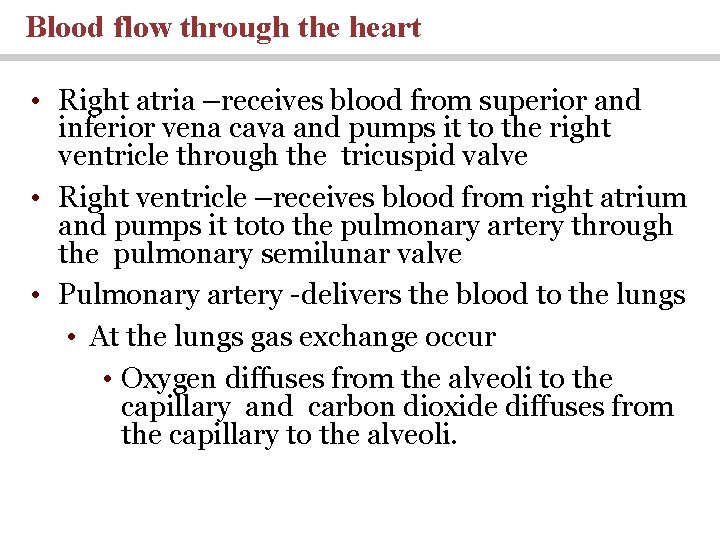
Blood flow through the heart • Right atria –receives blood from superior and inferior vena cava and pumps it to the right ventricle through the tricuspid valve • Right ventricle –receives blood from right atrium and pumps it toto the pulmonary artery through the pulmonary semilunar valve • Pulmonary artery -delivers the blood to the lungs • At the lungs gas exchange occur • Oxygen diffuses from the alveoli to the capillary and carbon dioxide diffuses from the capillary to the alveoli.
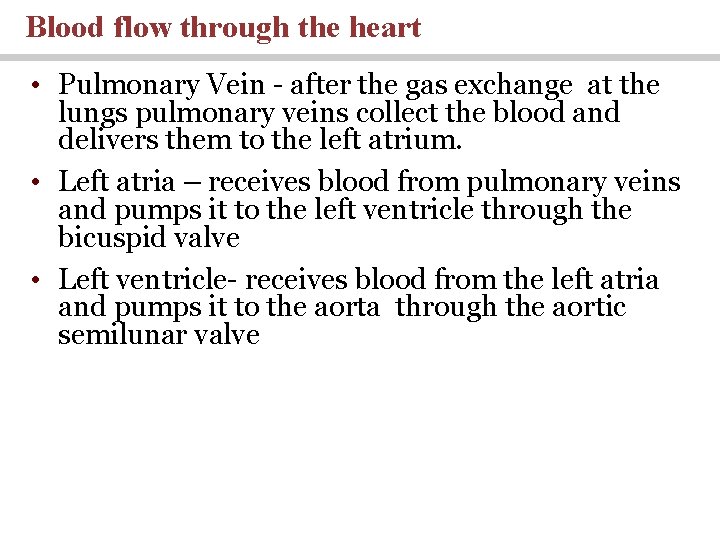
Blood flow through the heart • Pulmonary Vein - after the gas exchange at the lungs pulmonary veins collect the blood and delivers them to the left atrium. • Left atria – receives blood from pulmonary veins and pumps it to the left ventricle through the bicuspid valve • Left ventricle- receives blood from the left atria and pumps it to the aorta through the aortic semilunar valve
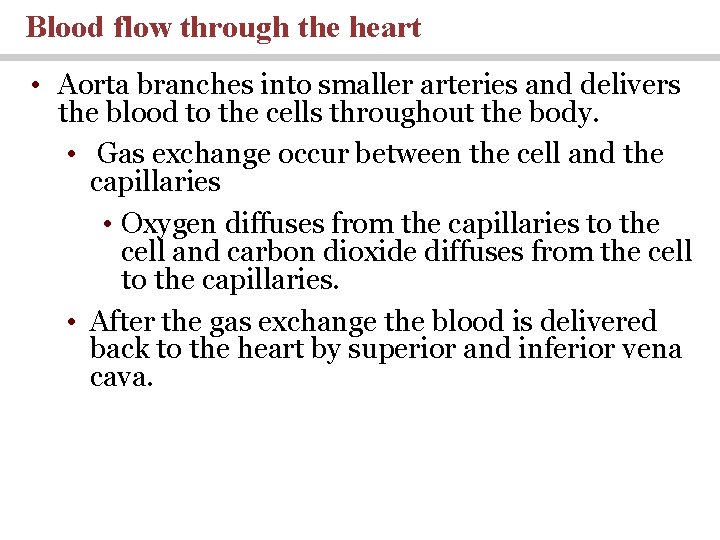
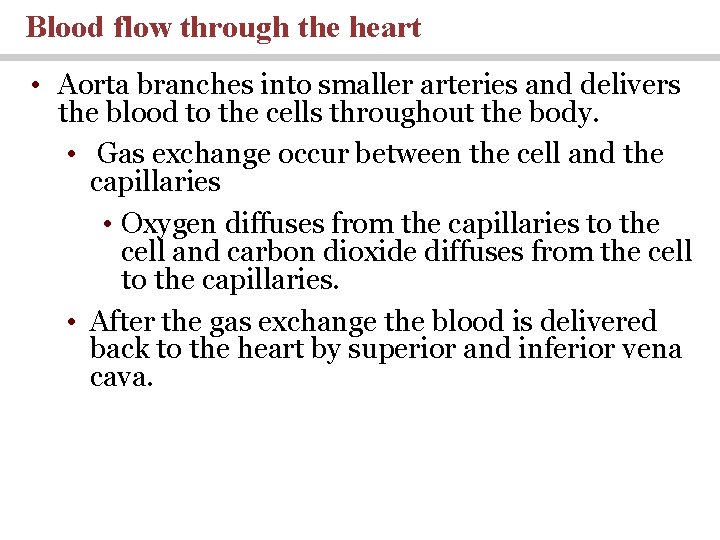
Blood flow through the heart • Aorta branches into smaller arteries and delivers the blood to the cells throughout the body. • Gas exchange occur between the cell and the capillaries • Oxygen diffuses from the capillaries to the cell and carbon dioxide diffuses from the cell to the capillaries. • After the gas exchange the blood is delivered back to the heart by superior and inferior vena cava.
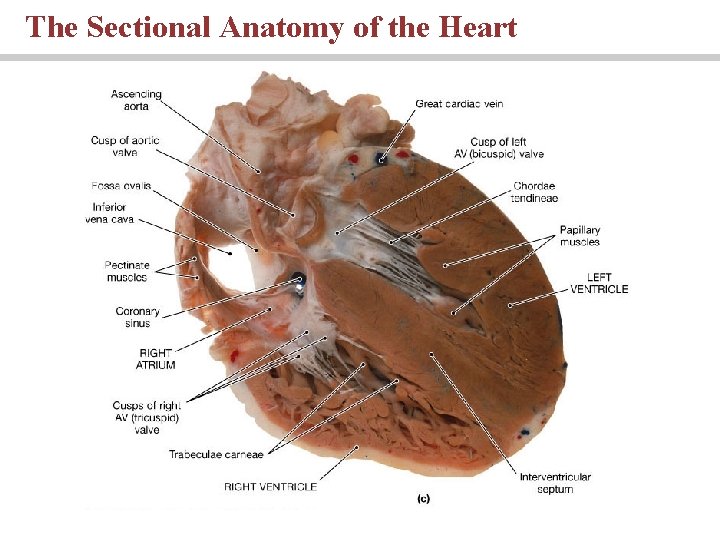
The Sectional Anatomy of the Heart
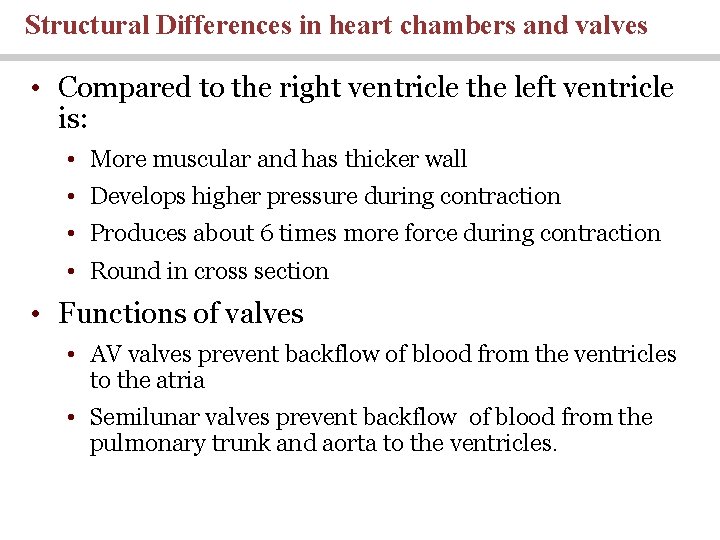
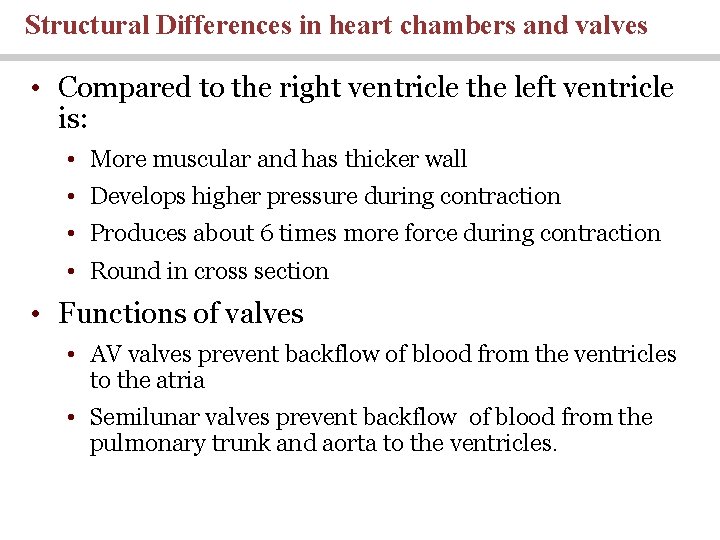
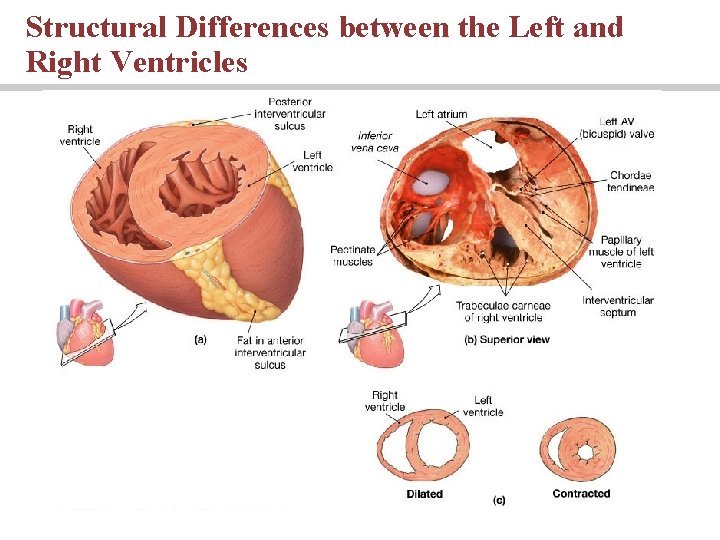
Structural Differences in heart chambers and valves • Compared to the right ventricle the left ventricle is: • More muscular and has thicker wall • Develops higher pressure during contraction • Produces about 6 times more force during contraction • Round in cross section • Functions of valves • AV valves prevent backflow of blood from the ventricles to the atria • Semilunar valves prevent backflow of blood from the pulmonary trunk and aorta to the ventricles.
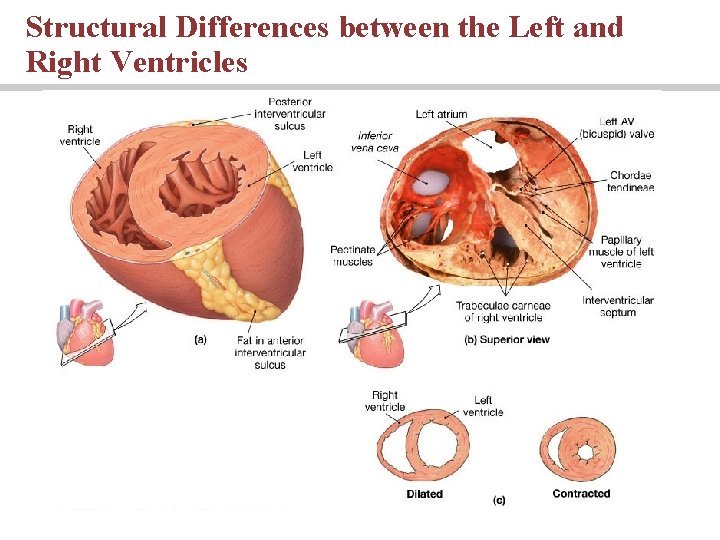
Structural Differences between the Left and Right Ventricles
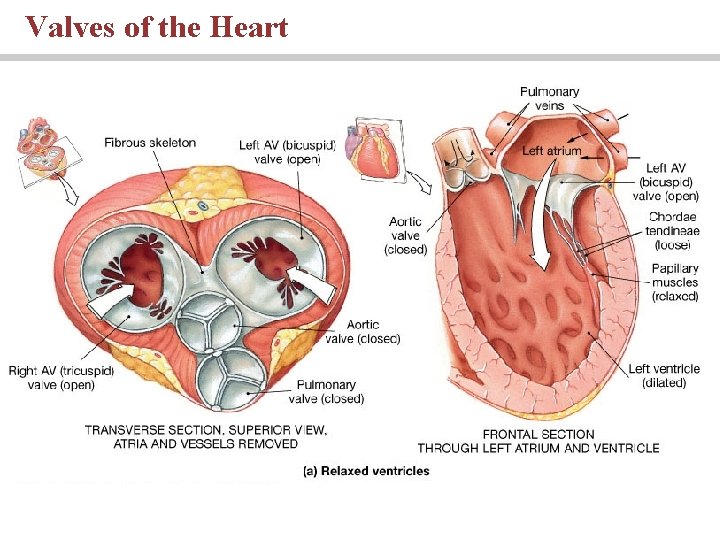
Valves of the Heart
Connective Tissues • Connective tissue fibers of the heart • Provide physical support and elasticity • Distribute the force of contraction • Prevent overexpansion
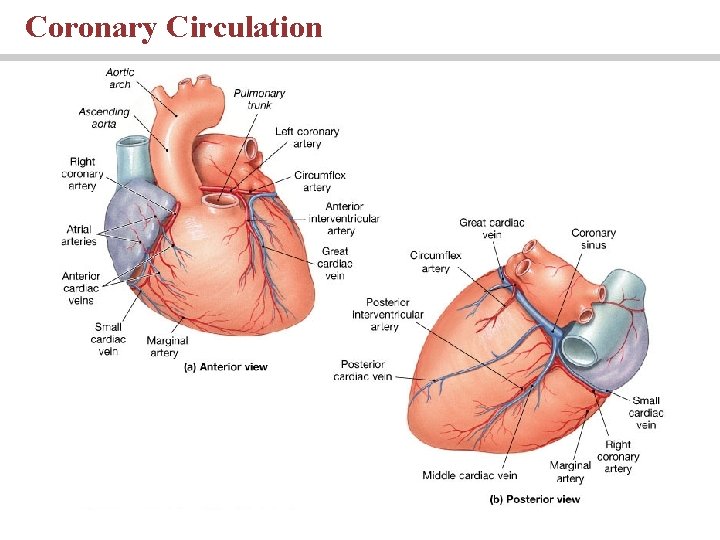
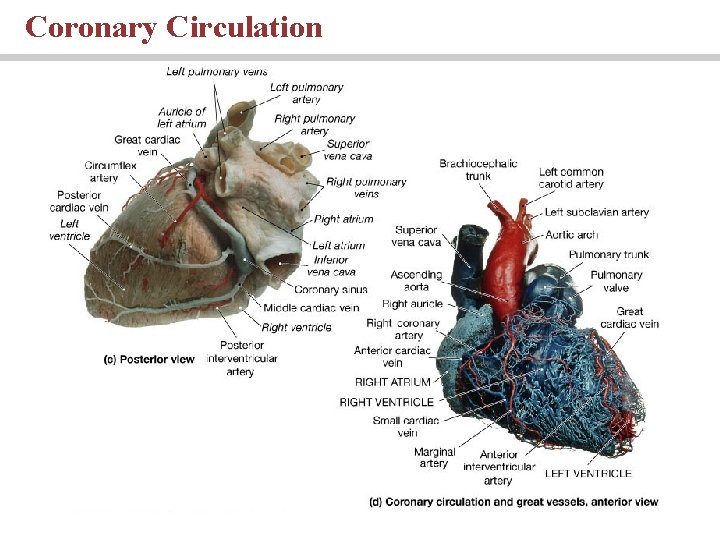
Blood Supply to the Heart • Coronary arteries are the first blood vessels to branch from the aorta • Coronary arteries supply blood to the heart and coronary veins collect the blood from the heart • Arteries include the right and left coronary arteries, marginal arteries, anterior and posterior interventricular arteries, and the circumflex artery • Veins include the great cardiac vein, anterior and posterior cardiac veins, the middle cardiac vein, and the small cardiac vein
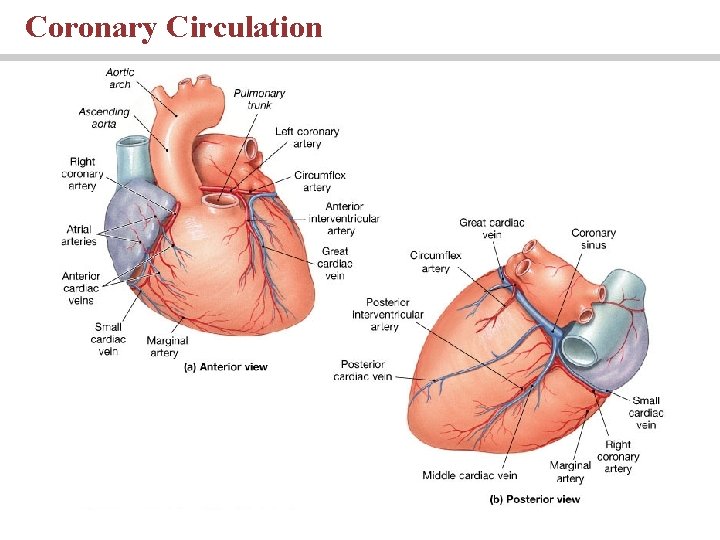
Coronary Circulation
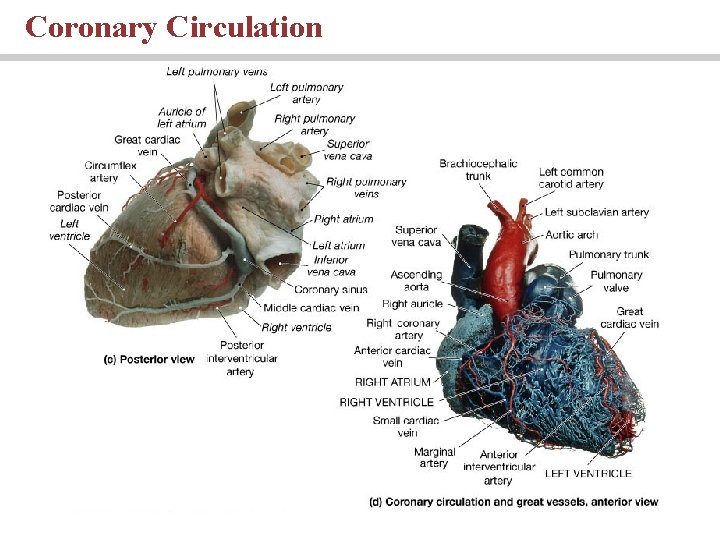
Coronary Circulation
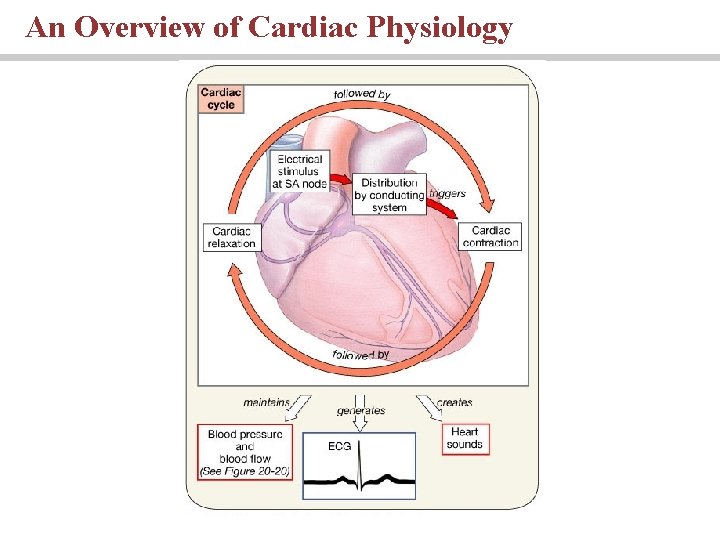
The Heartbeat Cardiac Physiology • Two classes of cardiac muscle cells • Specialized muscle cells of the conducting system • Contractile cells
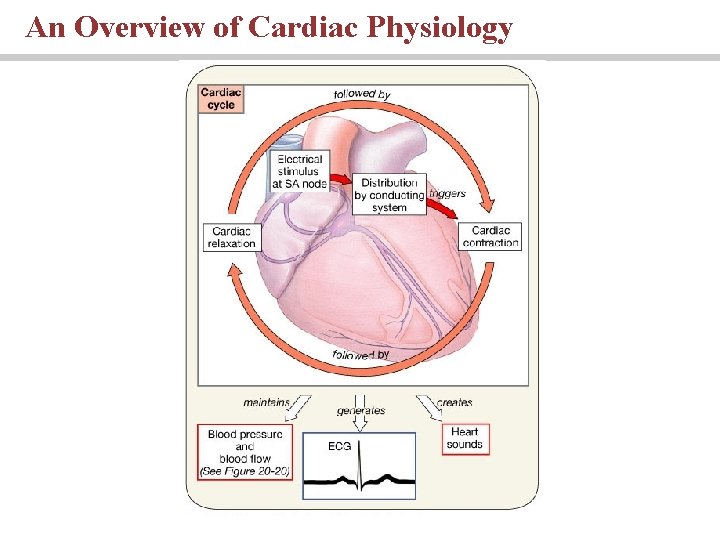
An Overview of Cardiac Physiology
The Conducting System • The conducting system includes: • Sinoatrial (SA) node - Pacemaker cells are located in the SA node • Atrioventricular (AV) node • AV bundle, • bundle branches, and • Purkinje fibers Animation: Heart flythrough (see tutorial)
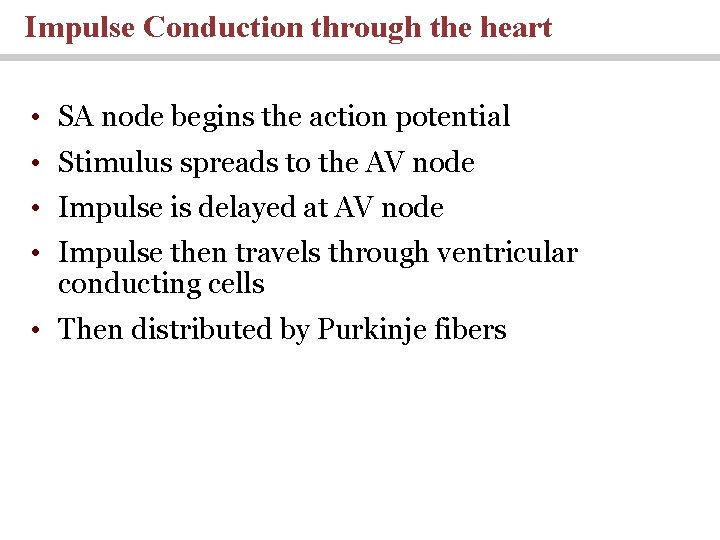
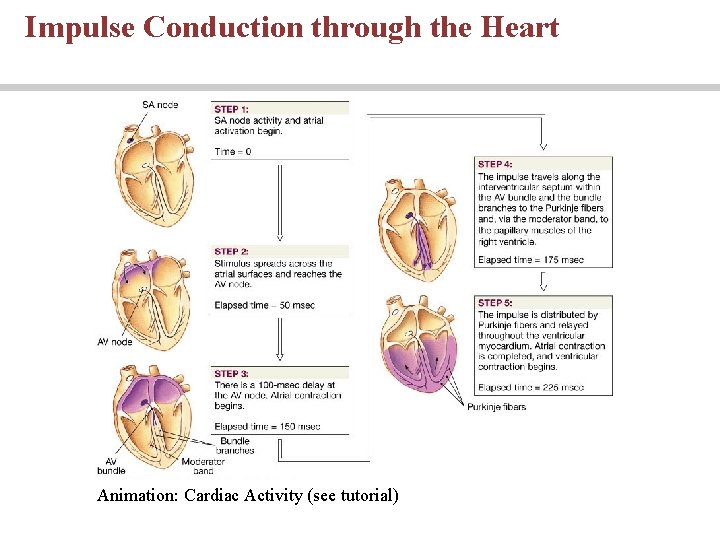
Impulse Conduction through the heart • SA node begins the action potential • Stimulus spreads to the AV node • Impulse is delayed at AV node • Impulse then travels through ventricular conducting cells • Then distributed by Purkinje fibers
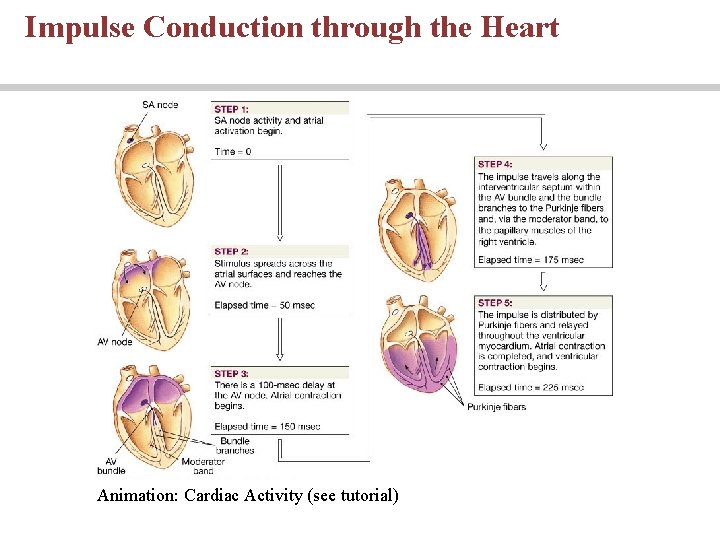
Impulse Conduction through the Heart Animation: Cardiac Activity (see tutorial)
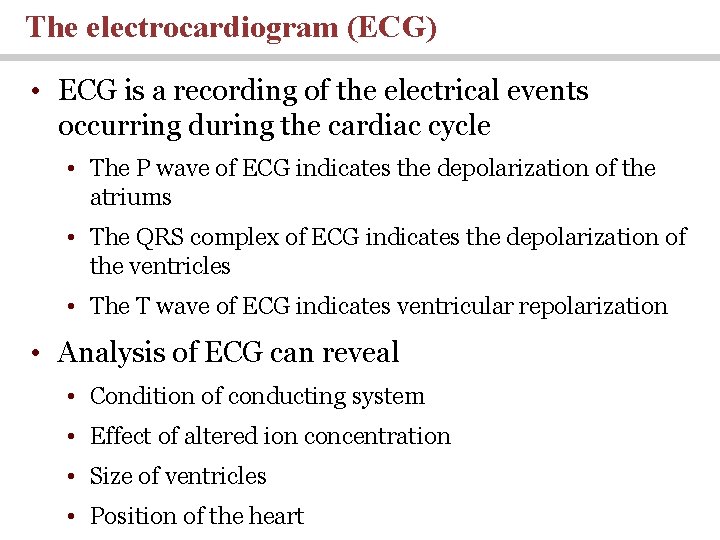
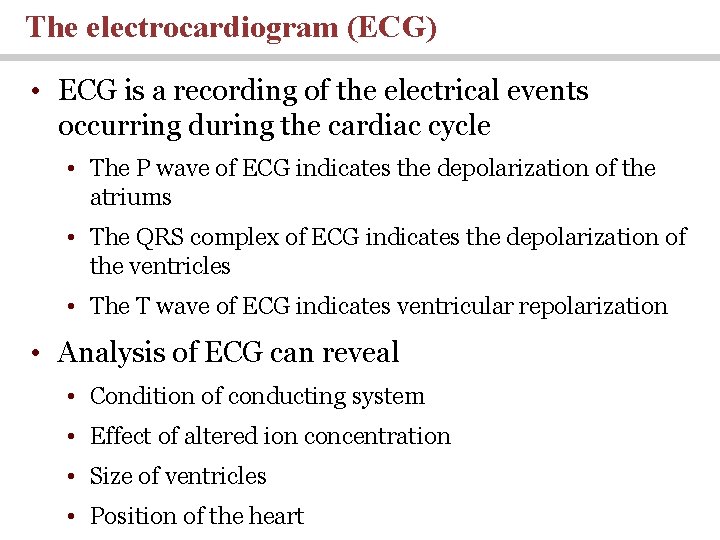
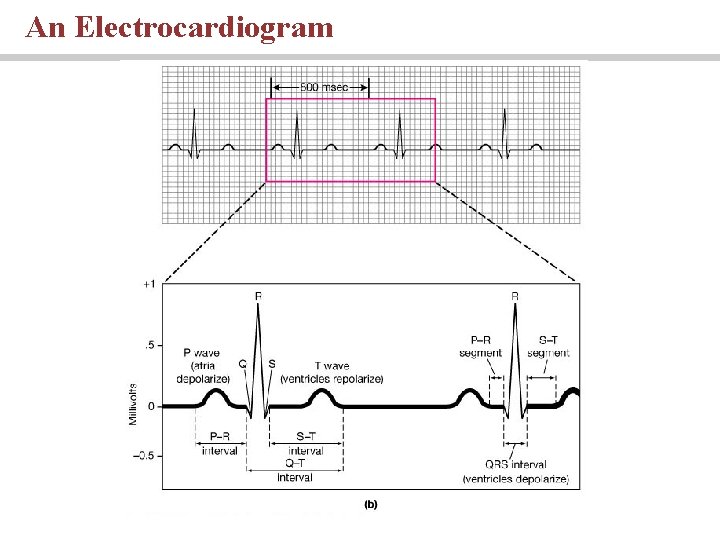
The electrocardiogram (ECG) • ECG is a recording of the electrical events occurring during the cardiac cycle • The P wave of ECG indicates the depolarization of the atriums • The QRS complex of ECG indicates the depolarization of the ventricles • The T wave of ECG indicates ventricular repolarization • Analysis of ECG can reveal • Condition of conducting system • Effect of altered ion concentration • Size of ventricles • Position of the heart
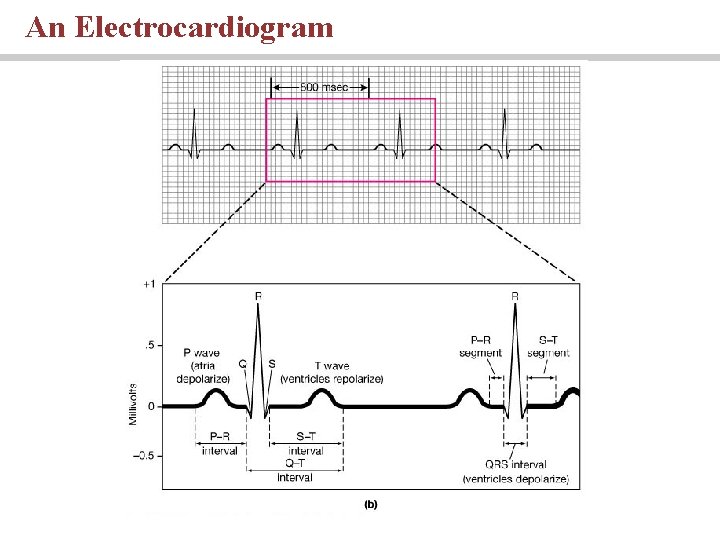
An Electrocardiogram
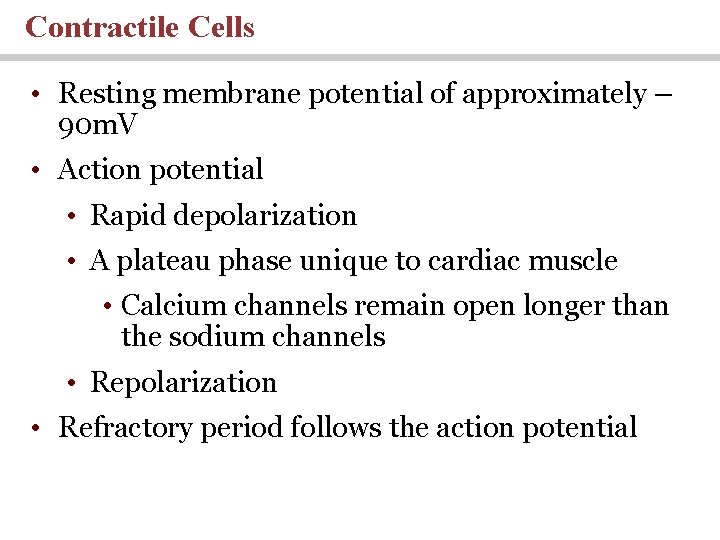
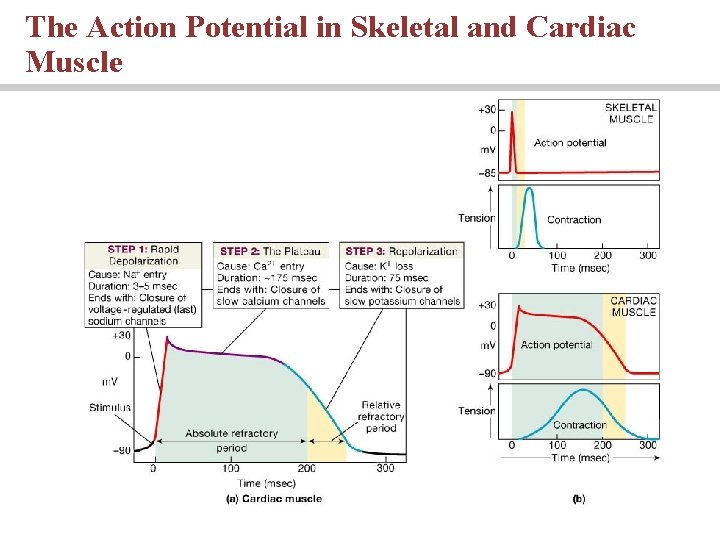
Contractile Cells • Resting membrane potential of approximately – 90 m. V • Action potential • Rapid depolarization • A plateau phase unique to cardiac muscle • Calcium channels remain open longer than the sodium channels • Repolarization • Refractory period follows the action potential
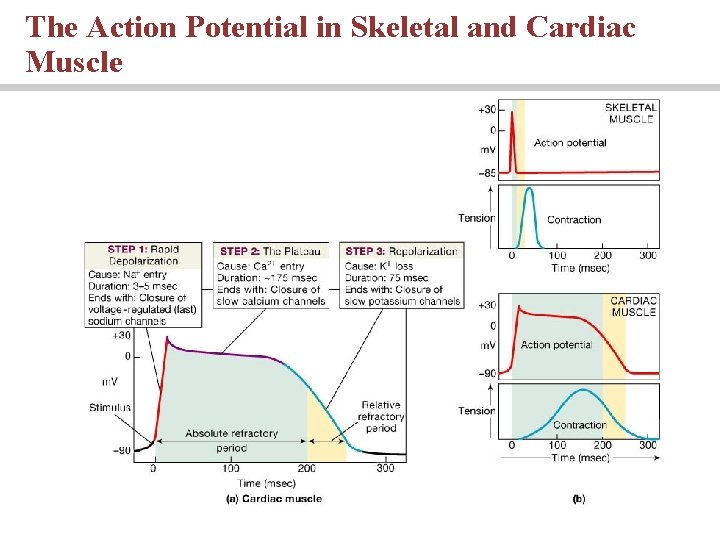
The Action Potential in Skeletal and Cardiac Muscle
The cardiac cycle • The period between the start of one heartbeat and the beginning of the next • During a cardiac cycle • Each heart chamber goes through systole and diastole • Correct pressure relationships are dependent on careful timing of contractions Animation: Intrinsic Conduction System (see tutorial)
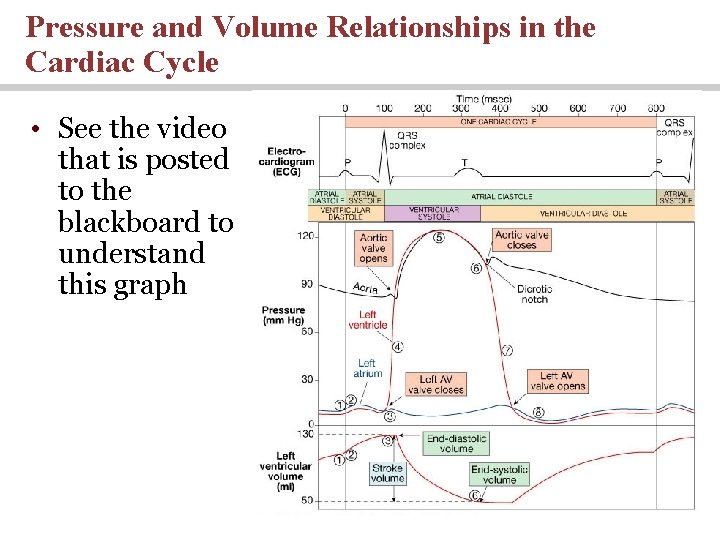
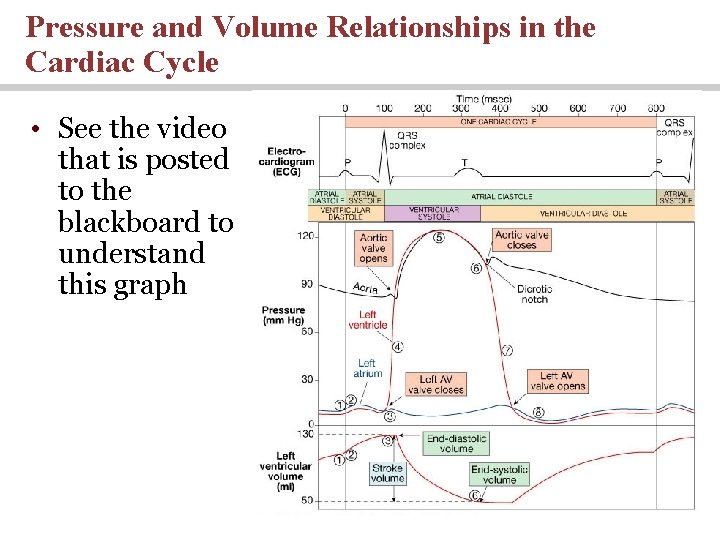
Pressure and Volume Relationships in the Cardiac Cycle • See the video that is posted to the blackboard to understand this graph
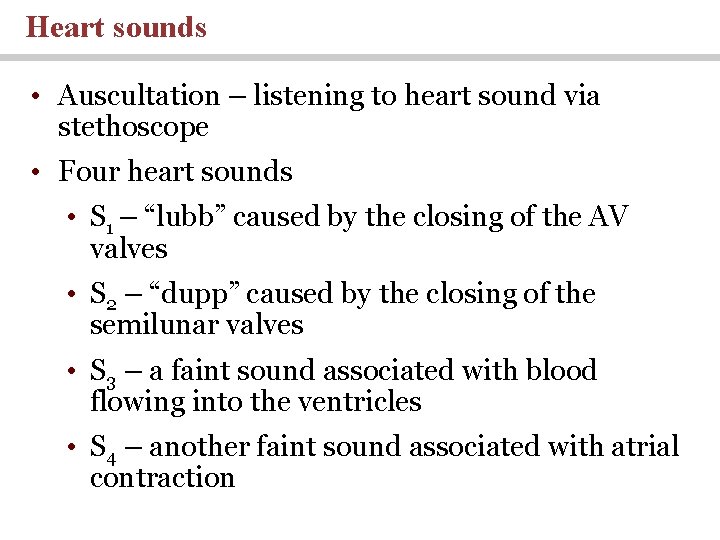
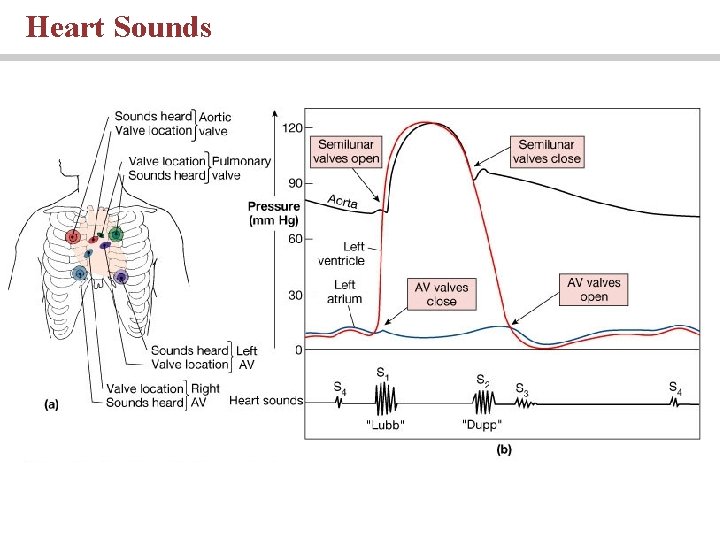
Heart sounds • Auscultation – listening to heart sound via stethoscope • Four heart sounds • S 1 – “lubb” caused by the closing of the AV valves • S 2 – “dupp” caused by the closing of the semilunar valves • S 3 – a faint sound associated with blood flowing into the ventricles • S 4 – another faint sound associated with atrial contraction
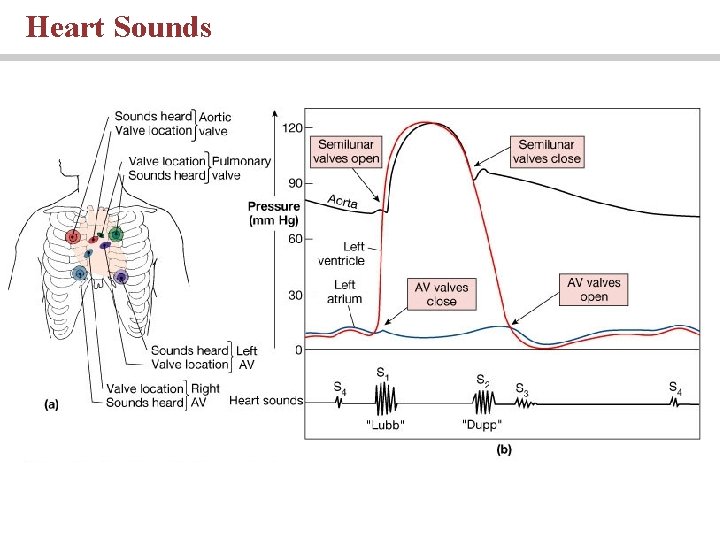
Heart Sounds

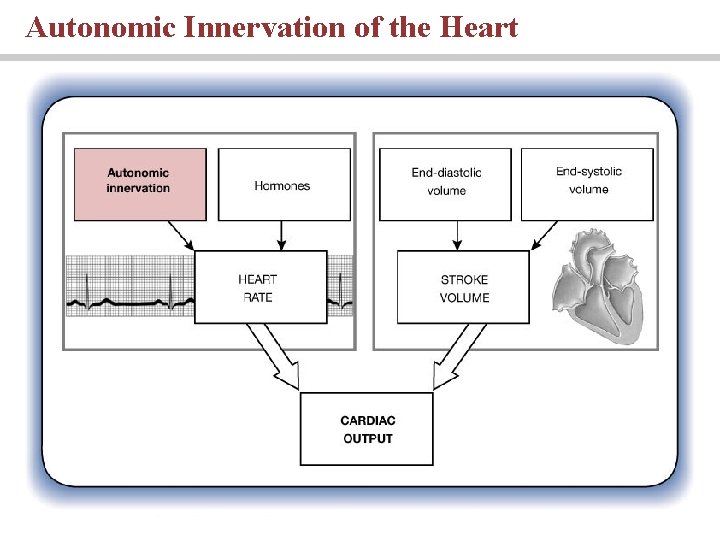
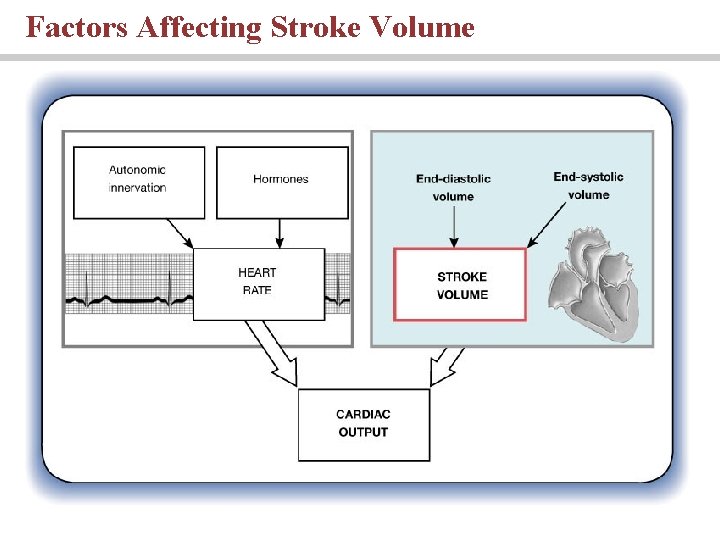
Cardiodynamics Stroke Volume and Cardiac Output • Stroke volume - is the volume of blood ejected with each ventricle contraction • Cardiac output – is the amount of blood pumped by each ventricle in one minute • Cardiac output equals heart rate times stroke volume

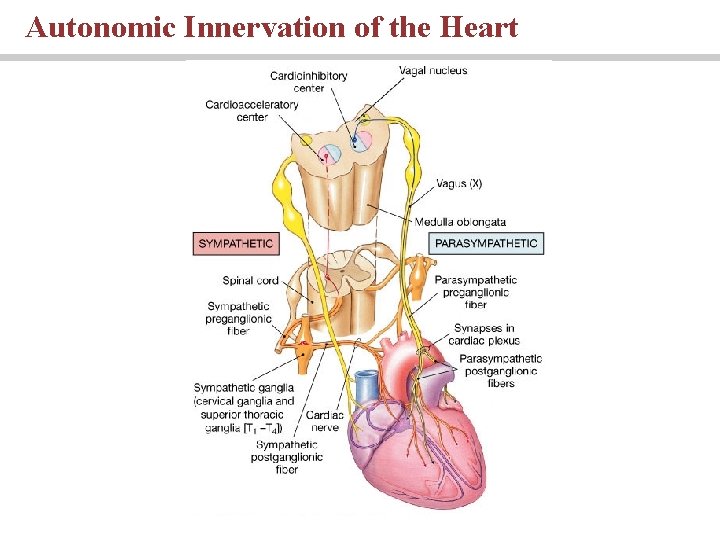
Medulla Oblongata centers affect autonomic innervation • Cardioacceleratory center activates sympathetic neurons • Cardioinhibitory center controls parasympathetic neurons • Medulla Oblongata centers receives input from higher centers, monitoring blood pressure and dissolved gas concentrations
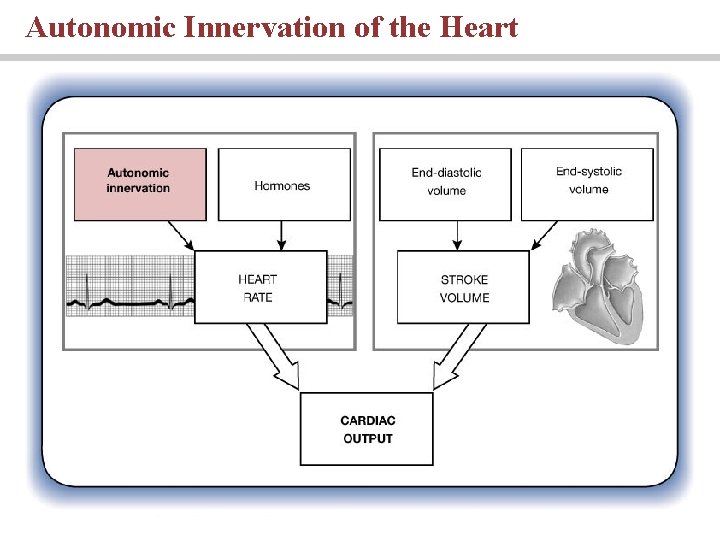
Autonomic Innervation of the Heart
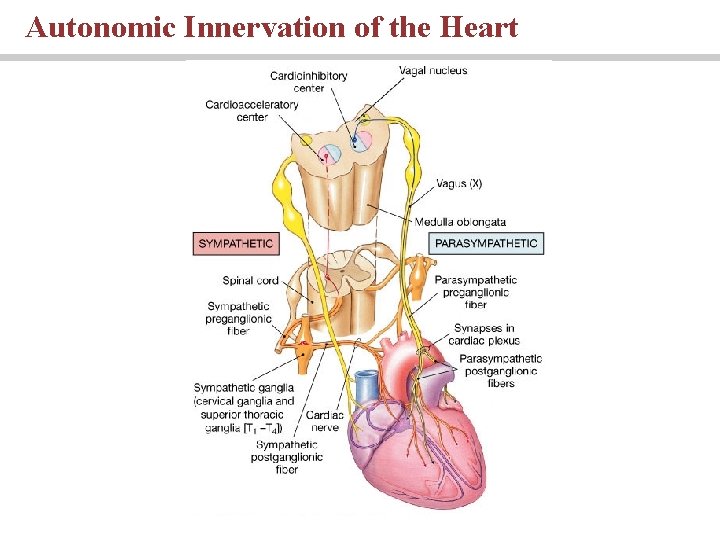
Autonomic Innervation of the Heart
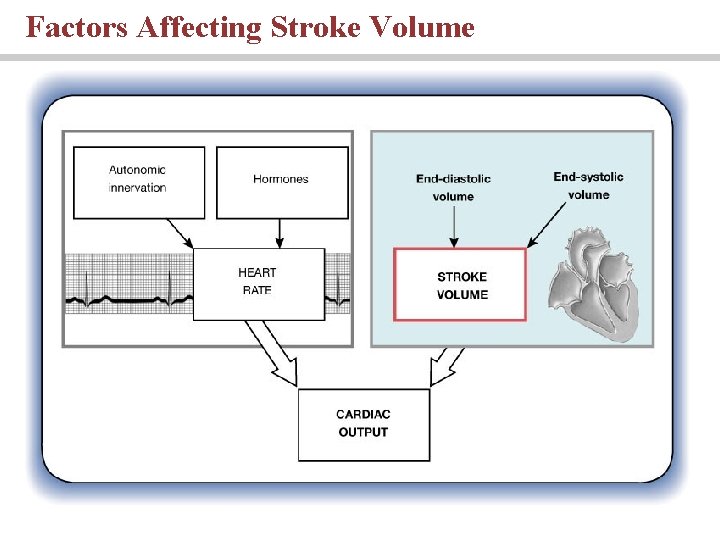
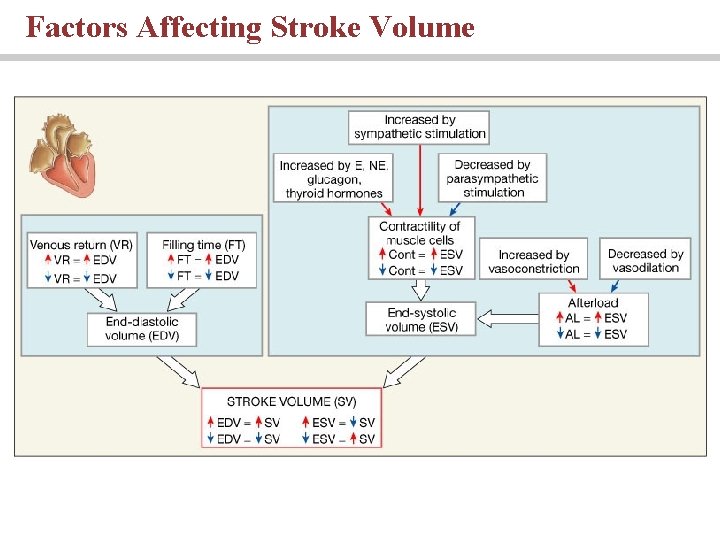
Factors Affecting Stroke Volume
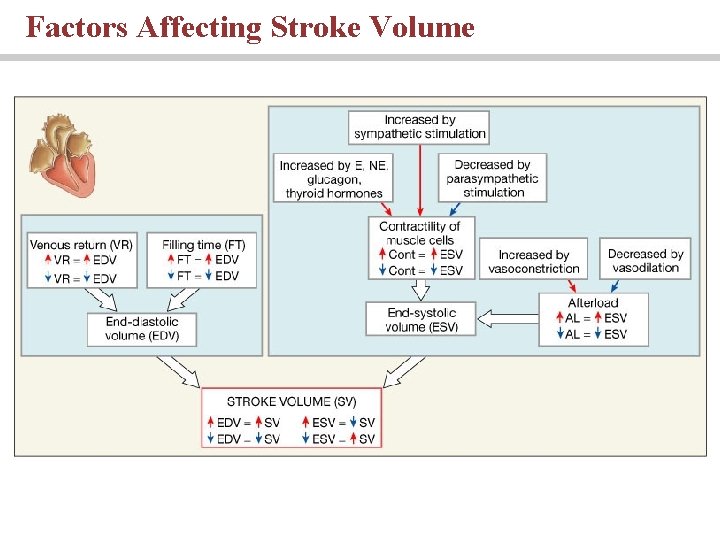
Factors Affecting Stroke Volume
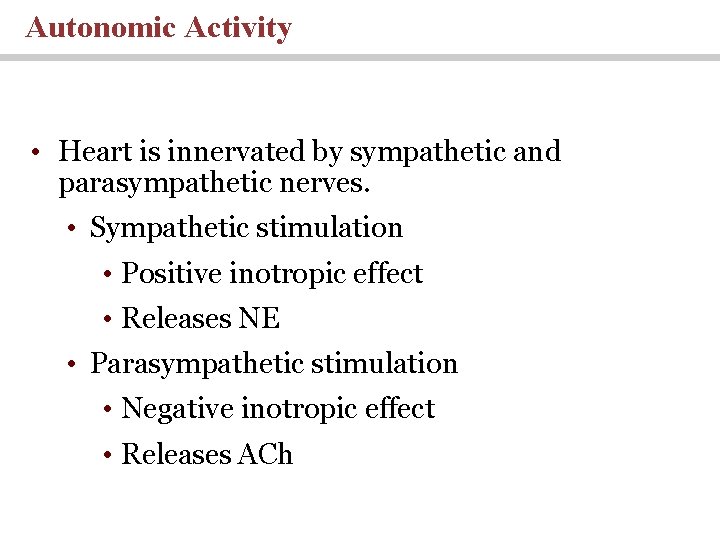
Autonomic Activity • Heart is innervated by sympathetic and parasympathetic nerves. • Sympathetic stimulation • Positive inotropic effect • Releases NE • Parasympathetic stimulation • Negative inotropic effect • Releases ACh
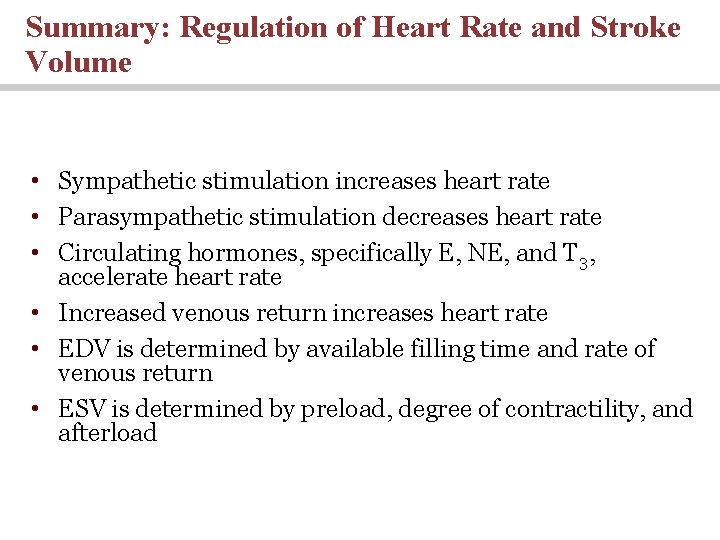
Summary: Regulation of Heart Rate and Stroke Volume • Sympathetic stimulation increases heart rate • Parasympathetic stimulation decreases heart rate • Circulating hormones, specifically E, NE, and T 3, accelerate heart rate • Increased venous return increases heart rate • EDV is determined by available filling time and rate of venous return • ESV is determined by preload, degree of contractility, and afterload
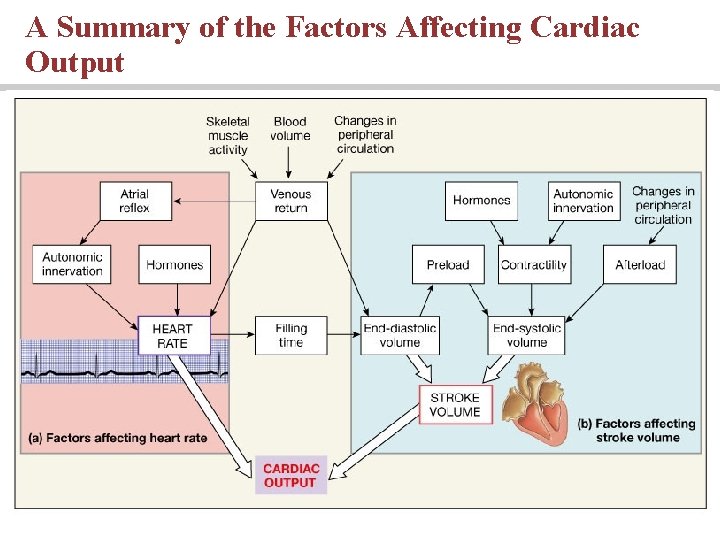
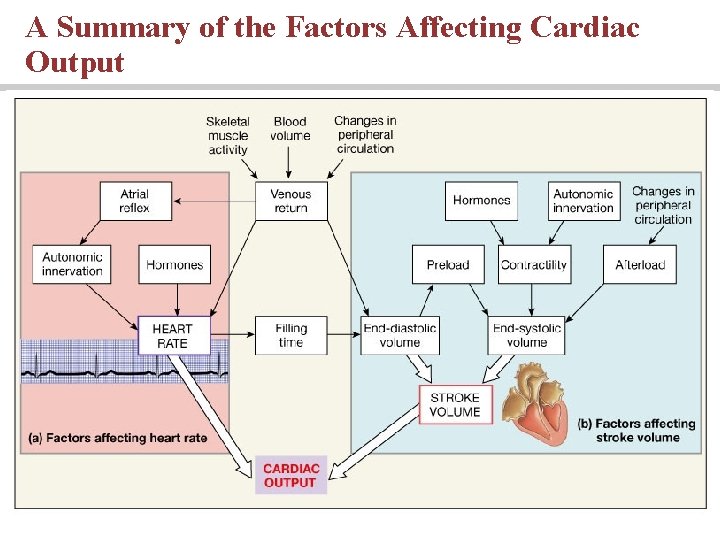
A Summary of the Factors Affecting Cardiac Output
You should now be familiar with: • The organization of the cardiovascular system. • The location and general features of the heart, including the pericardium. • The differences between nodal cells and conducting cells as well as the components and functions of the conducting system of the heart. • The electrical events associated with a normal electrocardiogram.
You should now be familiar with: • The events of the cardiac cycle including atrial and ventricular systole and diastole, and the heart sounds related to specific events in the cycle. • Cardiac output, heart rate and stroke volume and the factors that influence these variables. • How adjustments in stroke volume and cardiac output are coordinated at different levels of activity.
 3 layers of muscle
3 layers of muscle Human anatomy & physiology edition 9
Human anatomy & physiology edition 9 Uterus perimetrium
Uterus perimetrium Peter pickle tongue twister
Peter pickle tongue twister Rubber baby buggy bumpers tongue twister lyrics
Rubber baby buggy bumpers tongue twister lyrics Biochemistry sixth edition
Biochemistry sixth edition Computer architecture a quantitative approach sixth edition
Computer architecture a quantitative approach sixth edition Automotive technology principles diagnosis and service
Automotive technology principles diagnosis and service Automotive technology sixth edition
Automotive technology sixth edition Apa sixth edition
Apa sixth edition Computer architecture a quantitative approach 6th
Computer architecture a quantitative approach 6th Precalculus sixth edition
Precalculus sixth edition Rational people think at the margin
Rational people think at the margin Computer architecture a quantitative approach sixth edition
Computer architecture a quantitative approach sixth edition Microbial physiology lecture notes
Microbial physiology lecture notes Physiology of sport and exercise 5th edition
Physiology of sport and exercise 5th edition 01:640:244 lecture notes - lecture 15: plat, idah, farad
01:640:244 lecture notes - lecture 15: plat, idah, farad Physiology of lungs
Physiology of lungs Tattoo anatomy and physiology
Tattoo anatomy and physiology Anatomy science olympiad
Anatomy science olympiad Woody stem parts
Woody stem parts Bone anatomy and physiology
Bone anatomy and physiology Anatomy and physiology of peptic ulcer ppt
Anatomy and physiology of peptic ulcer ppt Liver hilus
Liver hilus Epigastric region
Epigastric region Iliac regions
Iliac regions Anatomy and physiology of rbc
Anatomy and physiology of rbc The central sulcus divides which two lobes? (figure 14-13)
The central sulcus divides which two lobes? (figure 14-13) Http://anatomy and physiology
Http://anatomy and physiology Waistline
Waistline Physiology of appendix
Physiology of appendix Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 2
Aohs foundations of anatomy and physiology 2 Anatomy and physiology of swine
Anatomy and physiology of swine Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Unit 26 animal anatomy physiology and nutrition
Unit 26 animal anatomy physiology and nutrition Science olympiad anatomy and physiology 2020 cheat sheet
Science olympiad anatomy and physiology 2020 cheat sheet Chapter 2 basic chemistry anatomy and physiology
Chapter 2 basic chemistry anatomy and physiology Degluttination
Degluttination Anatomy and physiology of diabetes
Anatomy and physiology of diabetes Chapter 7:9 lymphatic system
Chapter 7:9 lymphatic system Anatomy and physiology coloring workbook figure 14-1
Anatomy and physiology coloring workbook figure 14-1 Chapter 10 blood anatomy and physiology
Chapter 10 blood anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 What produces bile
What produces bile Anatomy and physiology chapter 15
Anatomy and physiology chapter 15 Cornell notes for anatomy and physiology
Cornell notes for anatomy and physiology