Airway Management in the Critically Ill Dr CHAN



- Slides: 97
Airway Management in the Critically Ill Dr. CHAN King-chung June 7, 2006
Learning Airway Management
Case Scenario M/65 n Admitted for COAD exacerbation n Put on Bi. PAP n Found to be unresponsive n Sp. O 2 = 87%. BP = 160/90. HR = 120 n What would you do ? n
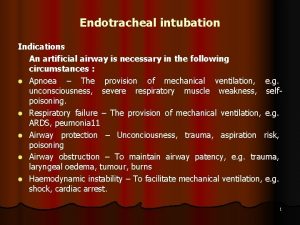
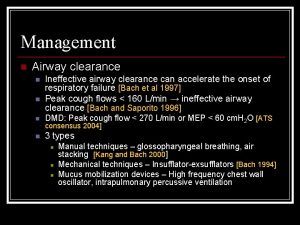
Indication for Airway n Obstruction n Assisted Ventilation n Aspiration n Secretion Clearance
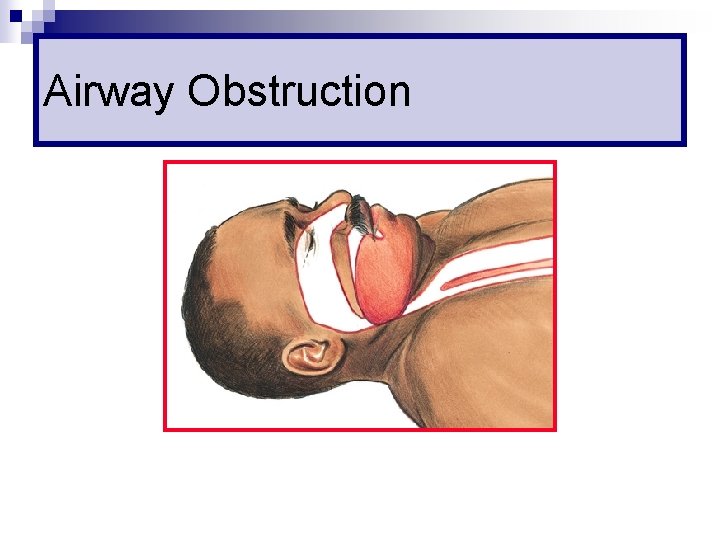
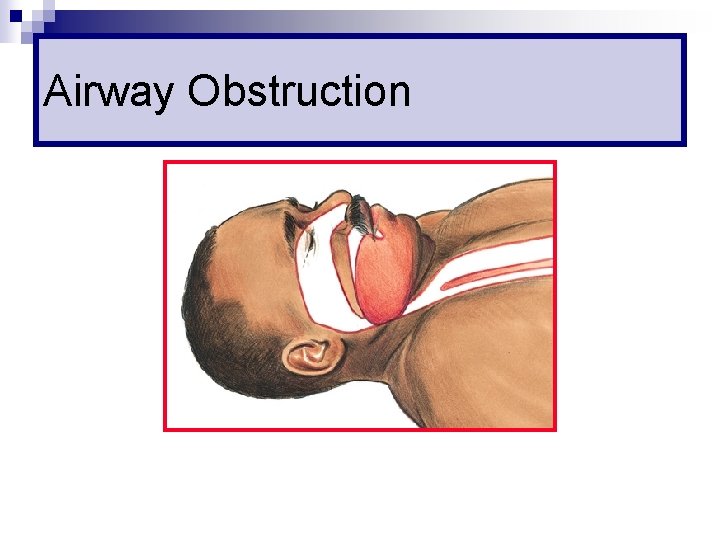
Airway Obstruction
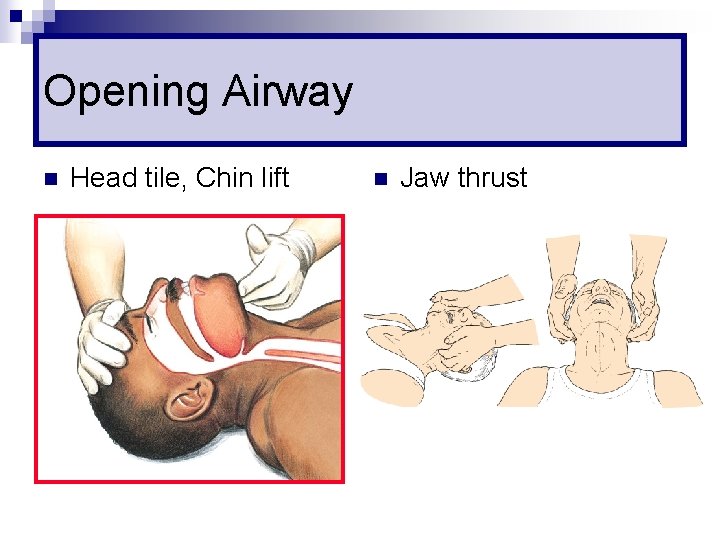
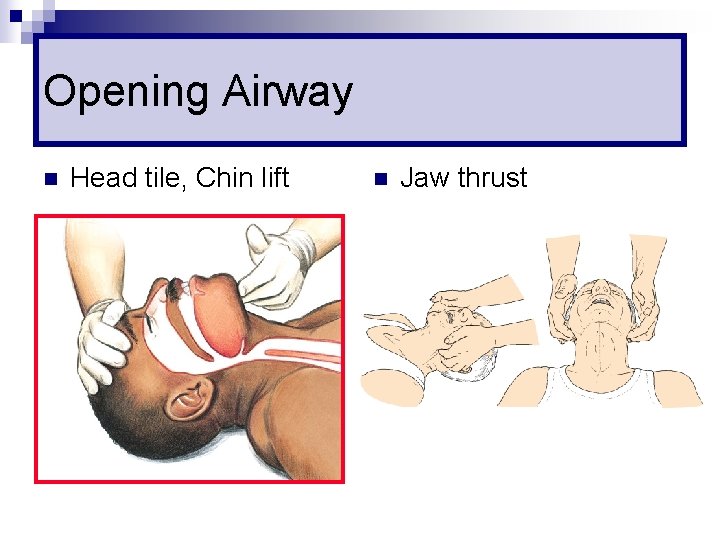
Opening Airway n Head tile, Chin lift n Jaw thrust
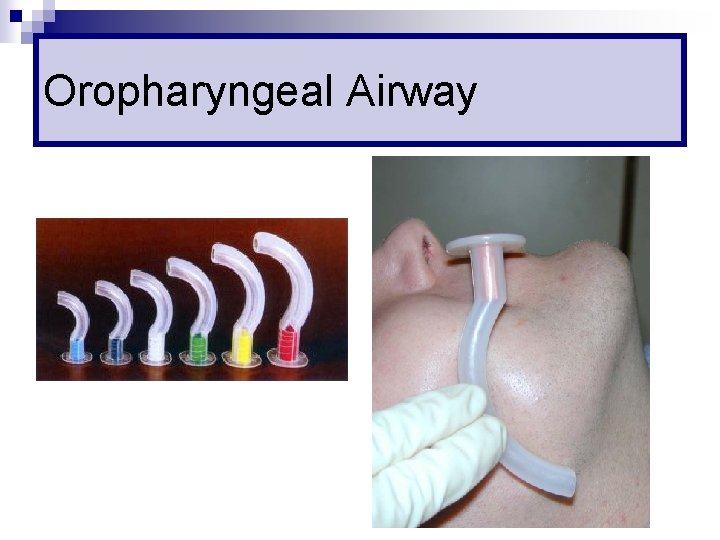
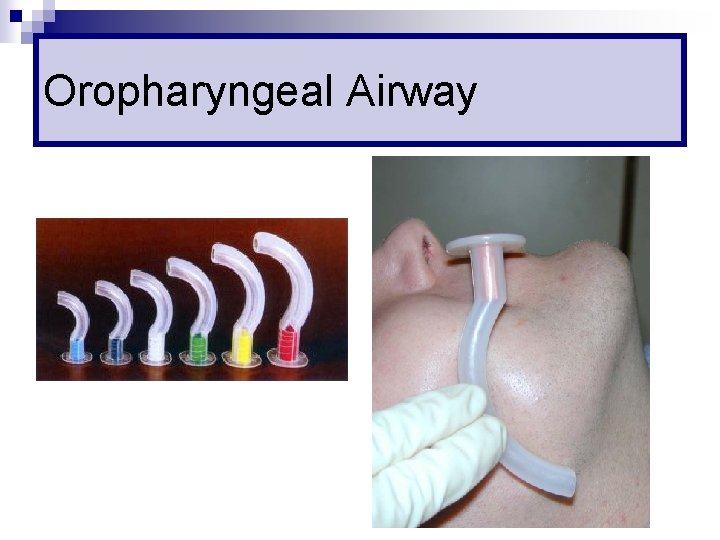
Oropharyngeal Airway
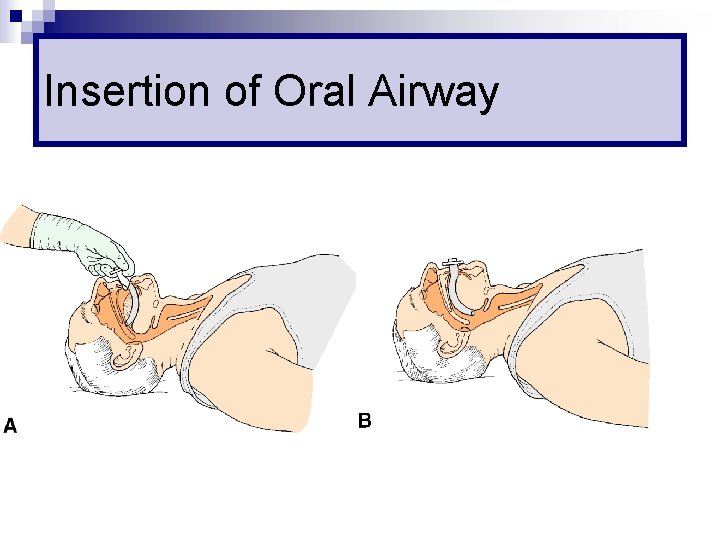
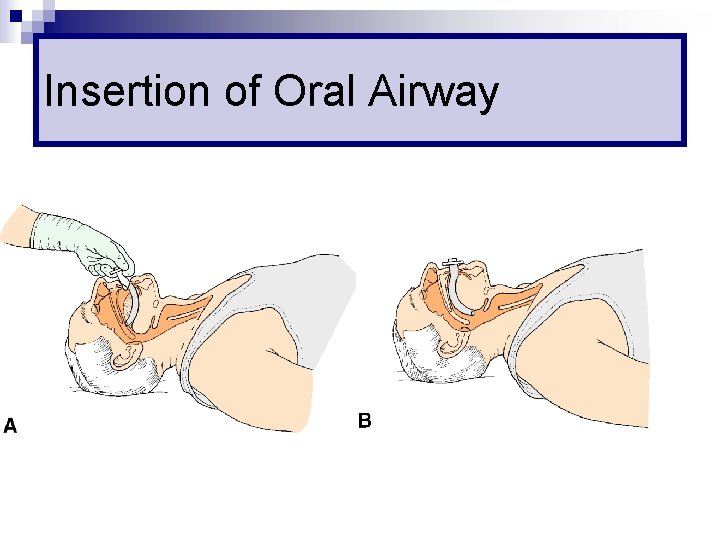
Insertion of Oral Airway
Nasopharyngeal Airway
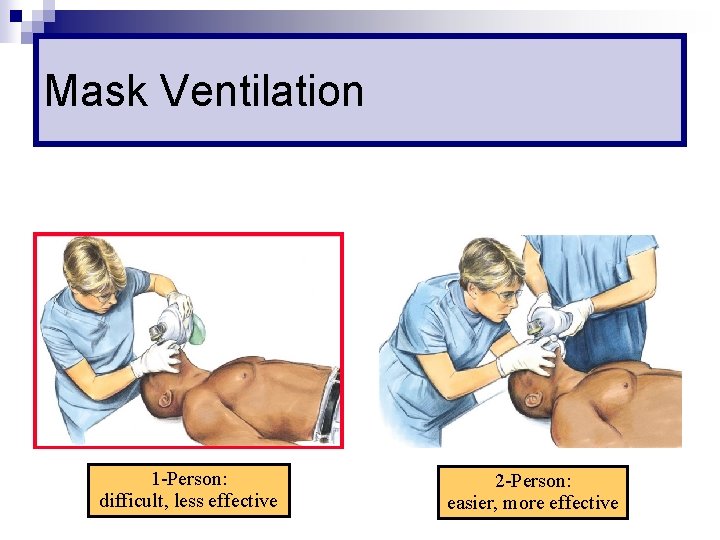
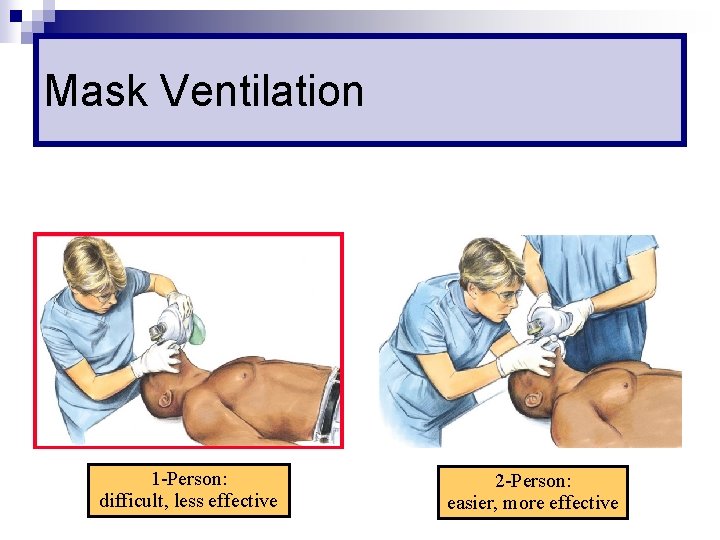
Mask Ventilation 1 -Person: difficult, less effective 2 -Person: easier, more effective
Difficult Mask Ventilation n Leak around the mask n No clear chest expansion during ventilation n Ventilation possible only with 2 -person
Prediction (MOANS) n Mask seal ¨ Beard, n Obese / Obstruction ¨ BMI n n >26 Age ¨ >55 n facial injury years No teeth Stiff lung
Complications n Gastric distension n Aspiration n Pressure injury to eyes, nose or lips n Facial nerve palsy
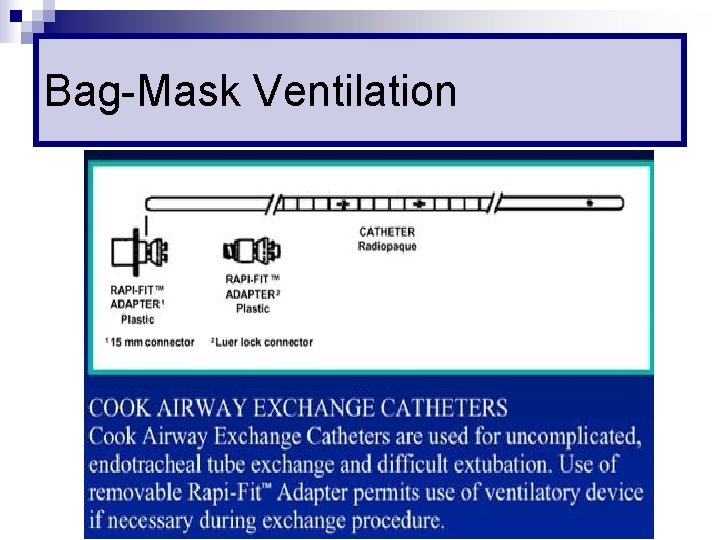
Bag-Mask Ventilation
Rapid Sequence Intubation n Virtually simultaneous administration, after preoxygenation, of a potent sedative agent and a rapidly acting neuromuscular blocking agent to facilitate rapid tracheal intubation without interposed mechanical ventilation
Why RSI ? n Minimize risk of aspiration n Optimal intubating condition n High success rate
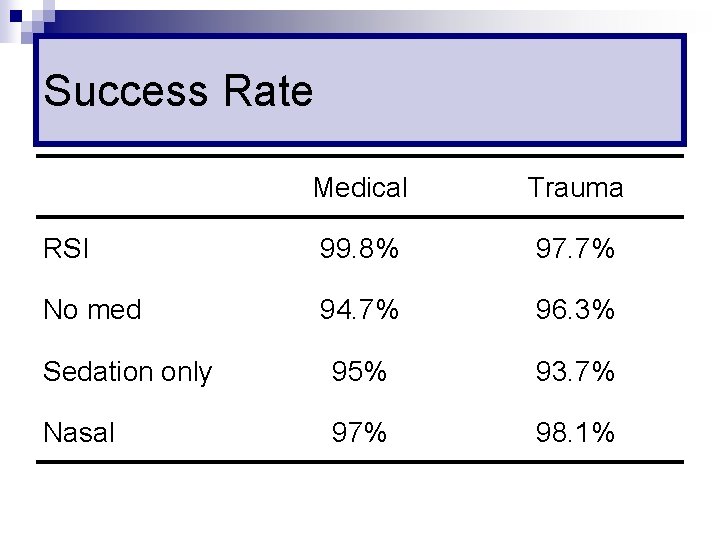
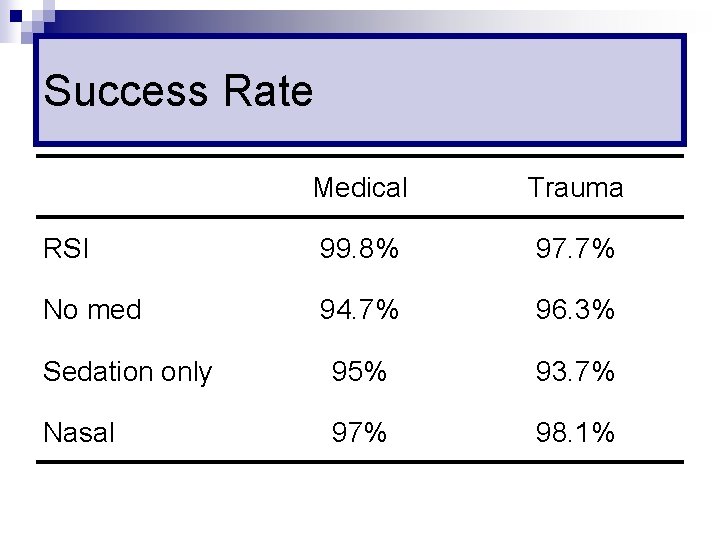
Success Rate Medical Trauma RSI 99. 8% 97. 7% No med 94. 7% 96. 3% Sedation only 95% 93. 7% Nasal 97% 98. 1%
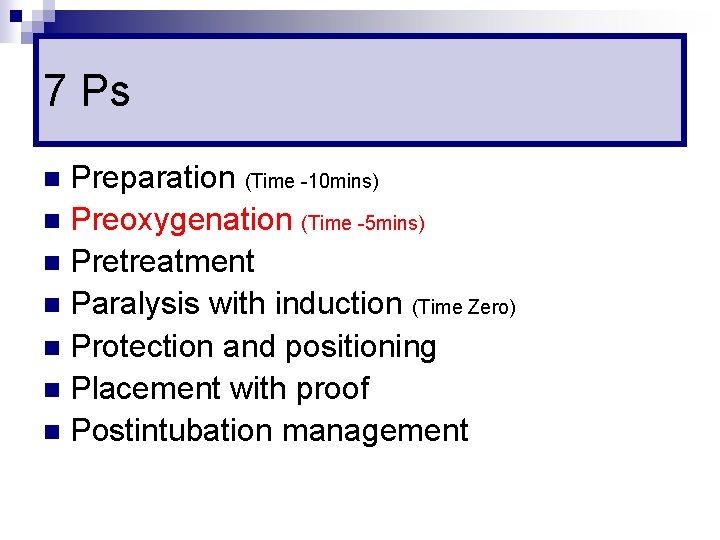
7 Ps Preparation n Preoxygenation n Pretreatment n Paralysis with induction (Time Zero) n Protection and positioning n Placement with proof n Postintubation management n
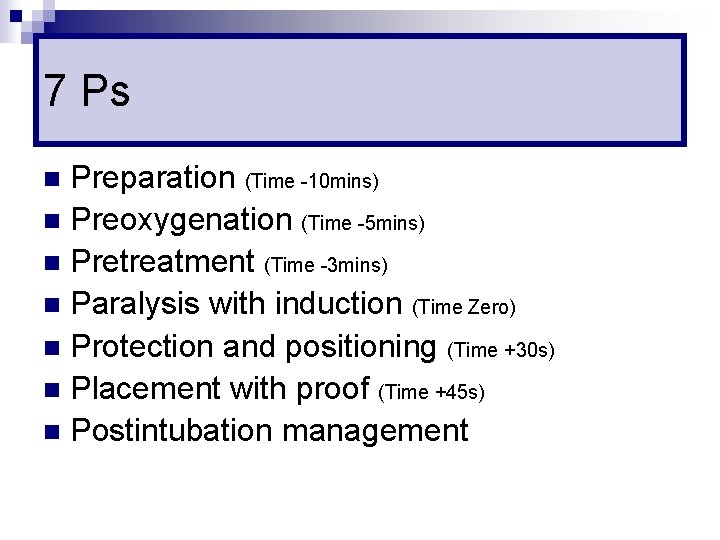
7 Ps Preparation (Time -10 mins) n Preoxygenation n Pretreatment n Paralysis with induction (Time Zero) n Protection and positioning n Placement with proof n Postintubation management n
Preparation (T -10 mins) n Assess for possible difficult airway n Assemble equipments and prepare drugs n Attach monitors n Establish IV access
Preparation (T -10 mins) n Assess for possible difficult airway n Assemble equipments and prepare drugs n Attach monitors n Establish IV access
Difficult Intubation n Intubationist with >2 years of experience ¨ More than 3 attempts ¨ Intubation time >10 minutes
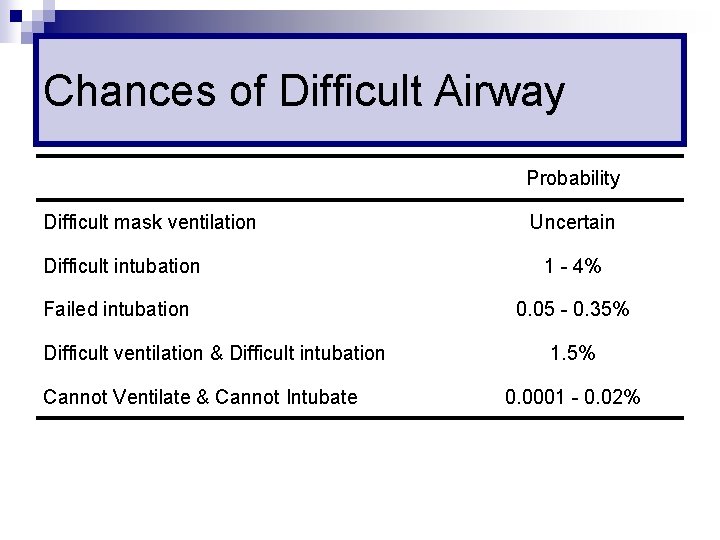
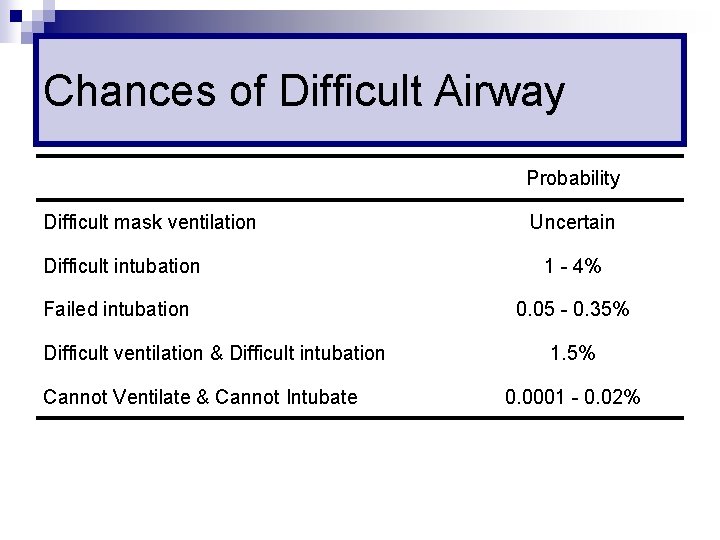
Chances of Difficult Airway Probability Difficult mask ventilation Uncertain Difficult intubation 1 - 4% Failed intubation 0. 05 - 0. 35% Difficult ventilation & Difficult intubation Cannot Ventilate & Cannot Intubate 1. 5% 0. 0001 - 0. 02%
Assessment of Airway n The LEMON rule ¨ Look externally ¨ Evaluate 3 -3 -2 ¨ Mallampati score ¨ Obstruction ¨ Neck Mobility
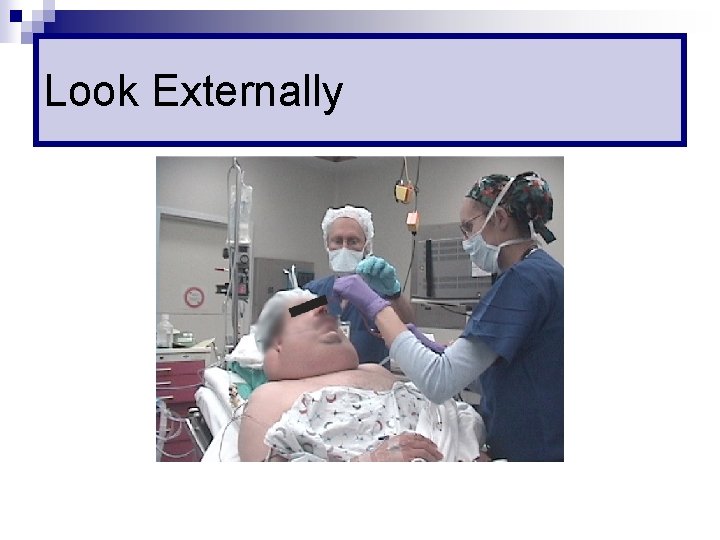
Look Externally Receding mandible (Micrognathia) n Large tongue (Macroglossia) n Protruding teeth n Short neck n Obese n Head & neck injury n
Look Externally
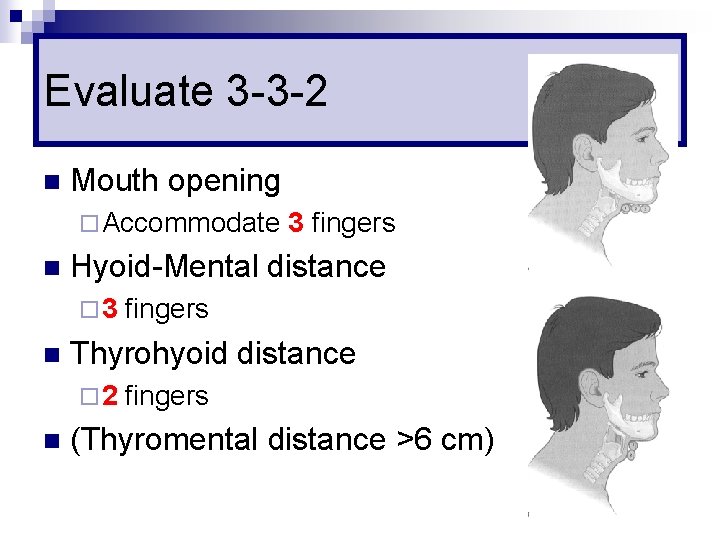
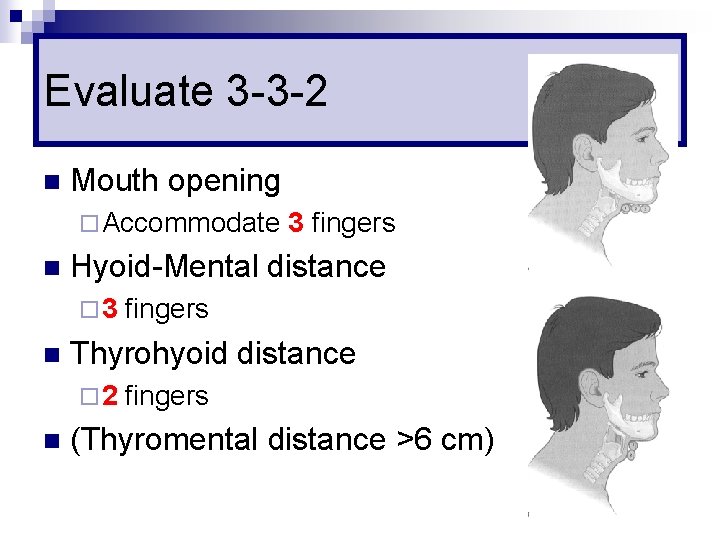
Evaluate 3 -3 -2 n Mouth opening ¨ Accommodate n Hyoid-Mental distance ¨ 3 n fingers Thyrohyoid distance ¨ 2 n 3 fingers (Thyromental distance >6 cm)
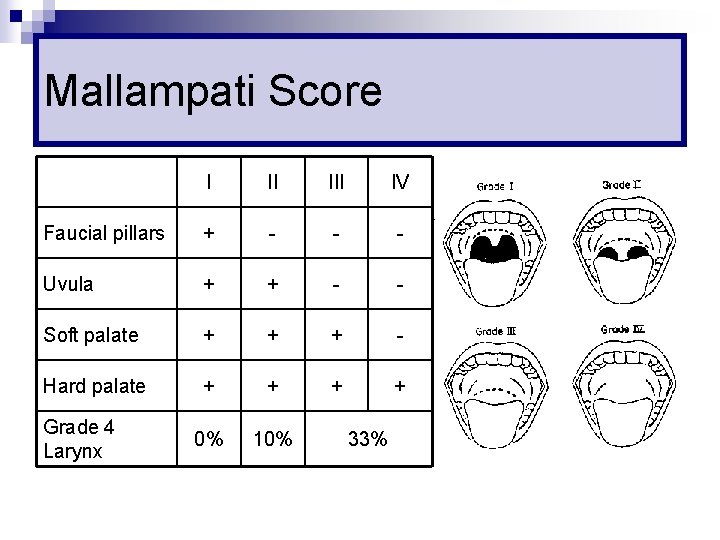
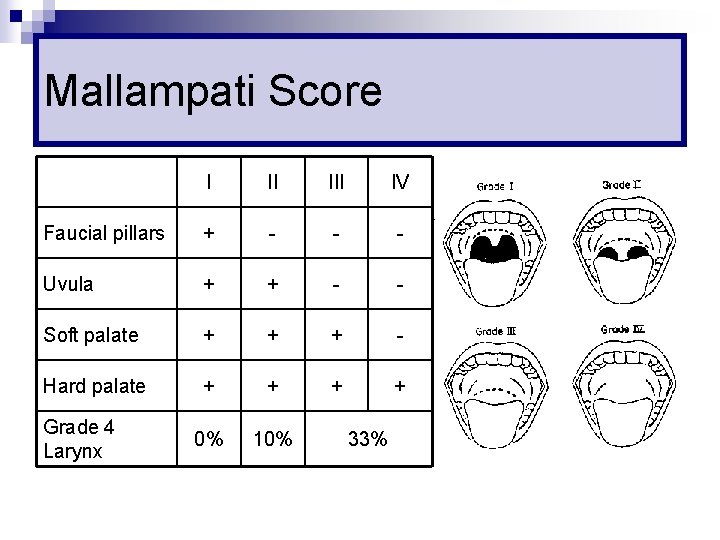
Mallampati Score I II IV Faucial pillars + - - - Uvula + + - - Soft palate + + + - Hard palate + + 0% 10% Grade 4 Larynx 33%
Assess this Lion
Obstruction Foreign body n Upper airway tumour n Epiglottitis n Peritonsillar abscess n Neck infection n Goitre n Haematoma n
Neck Mobility n Necessary for a good laryngoscopy view n Sternomental distance <12. 5 cm (normal 15 cm)
Preparation (T= -10 mins) n Assess for possible difficult airway n Assemble equipments and prepare drugs n Attach monitors n Establish IV access
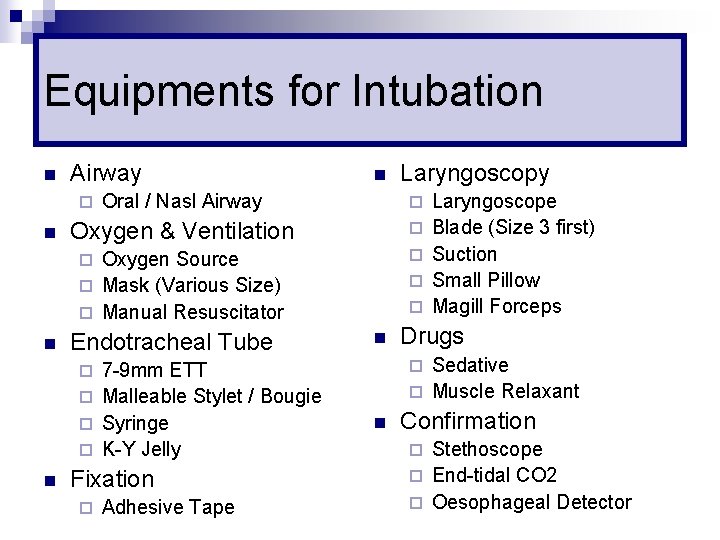
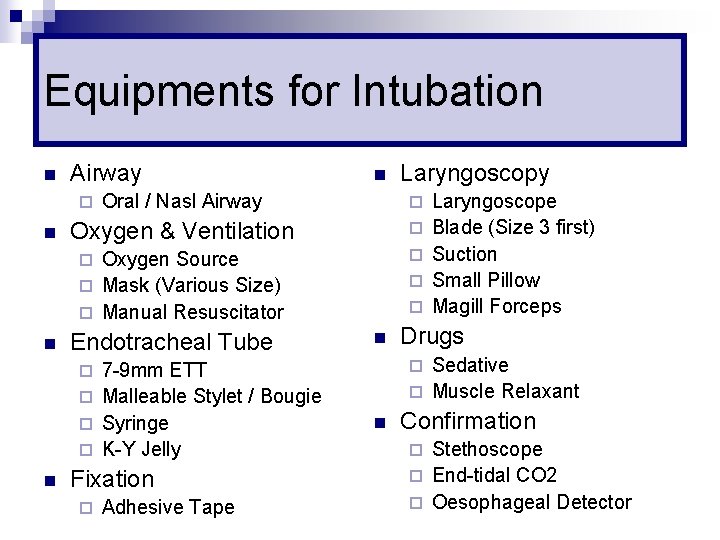
Equipments for Intubation n Airway ¨ Oxygen & Ventilation ¨ Oxygen Source ¨ Mask (Various Size) ¨ Manual Resuscitator ¨ ¨ n Endotracheal Tube 7 -9 mm ETT ¨ Malleable Stylet / Bougie ¨ Syringe ¨ K-Y Jelly ¨ ¨ n Fixation ¨ Adhesive Tape Laryngoscope Blade (Size 3 first) Suction Small Pillow Magill Forceps Drugs Sedative ¨ Muscle Relaxant ¨ ¨ n Laryngoscopy Oral / Nasl Airway ¨ n n n Confirmation Stethoscope ¨ End-tidal CO 2 ¨ Oesophageal Detector ¨
Shape of ETT n Hockey Stick ¨ To manoeuvre within oral cavity ¨ Expect some resistance in removing stylet ¨ Lubricate stylet
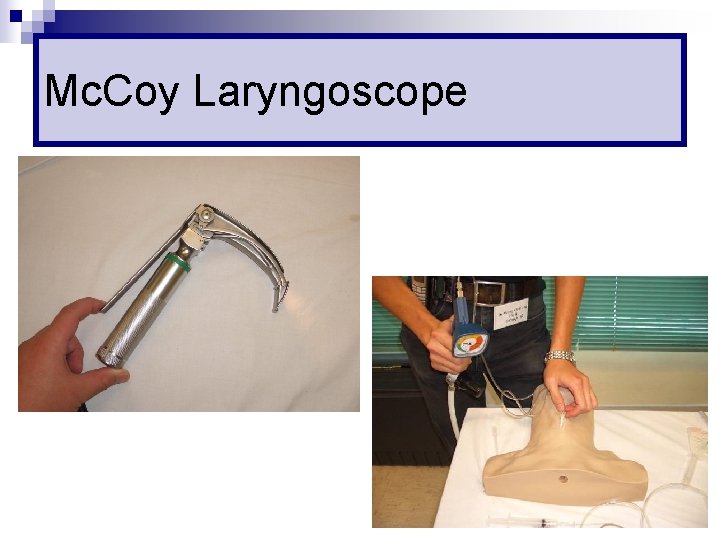
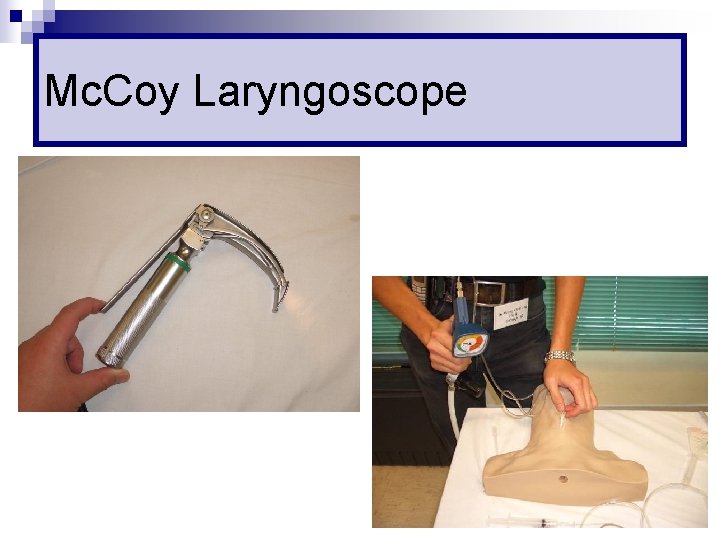
Mc. Coy Laryngoscope
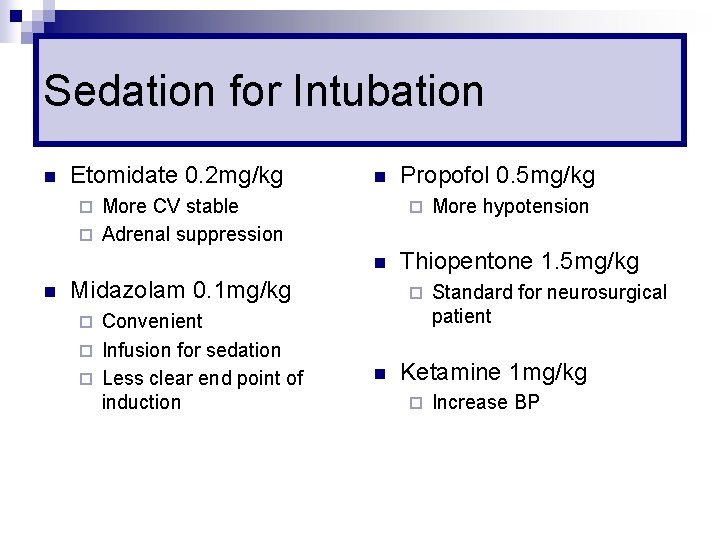
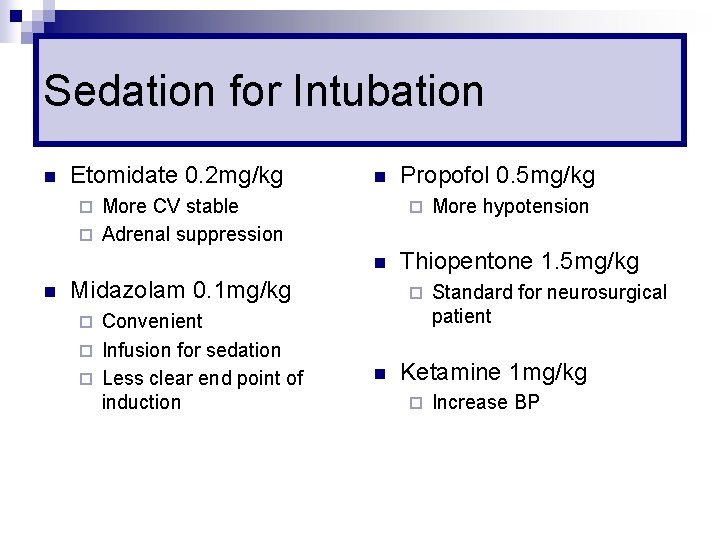
Sedation for Intubation n Etomidate 0. 2 mg/kg n More CV stable ¨ Adrenal suppression ¨ ¨ n n Midazolam 0. 1 mg/kg Convenient ¨ Infusion for sedation ¨ Less clear end point of induction Propofol 0. 5 mg/kg Thiopentone 1. 5 mg/kg ¨ ¨ n More hypotension Standard for neurosurgical patient Ketamine 1 mg/kg ¨ Increase BP
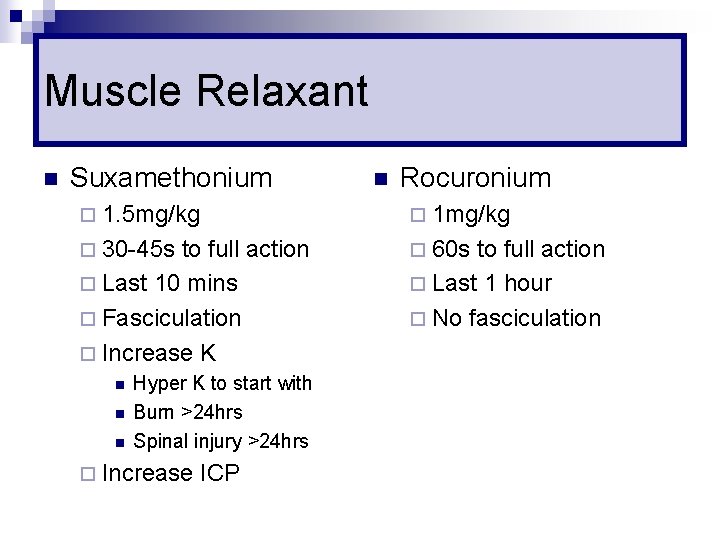
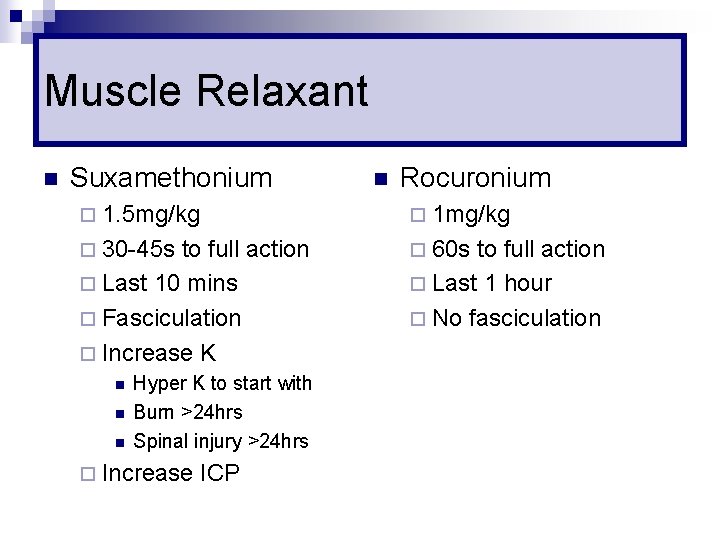
Muscle Relaxant n Suxamethonium n Rocuronium ¨ 1. 5 mg/kg ¨ 1 mg/kg ¨ 30 -45 s ¨ 60 s to full action ¨ Last 10 mins ¨ Fasciculation ¨ Increase K n n n Hyper K to start with Burn >24 hrs Spinal injury >24 hrs ¨ Increase ICP to full action ¨ Last 1 hour ¨ No fasciculation
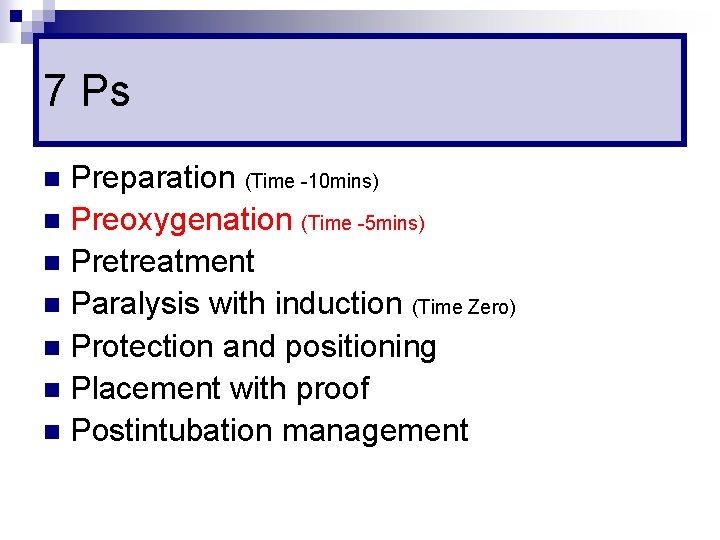
7 Ps Preparation (Time -10 mins) n Preoxygenation (Time -5 mins) n Pretreatment n Paralysis with induction (Time Zero) n Protection and positioning n Placement with proof n Postintubation management n
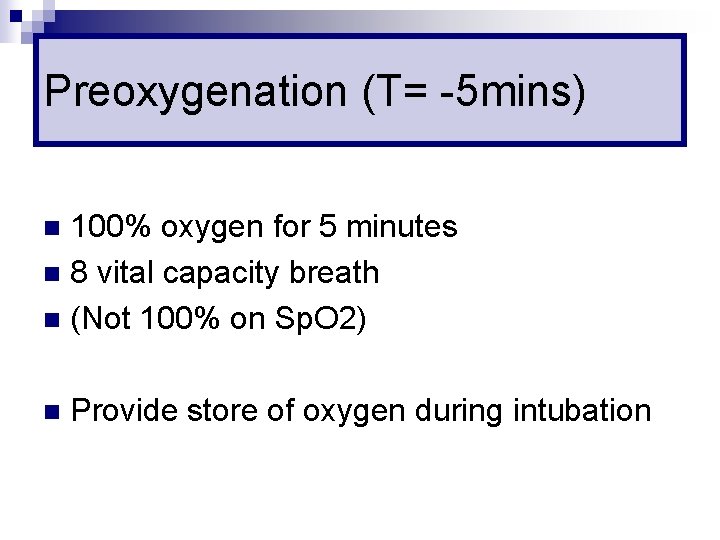
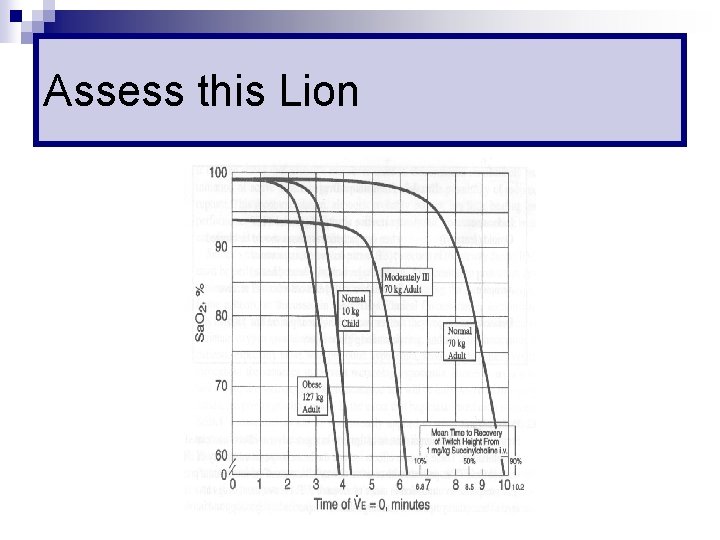
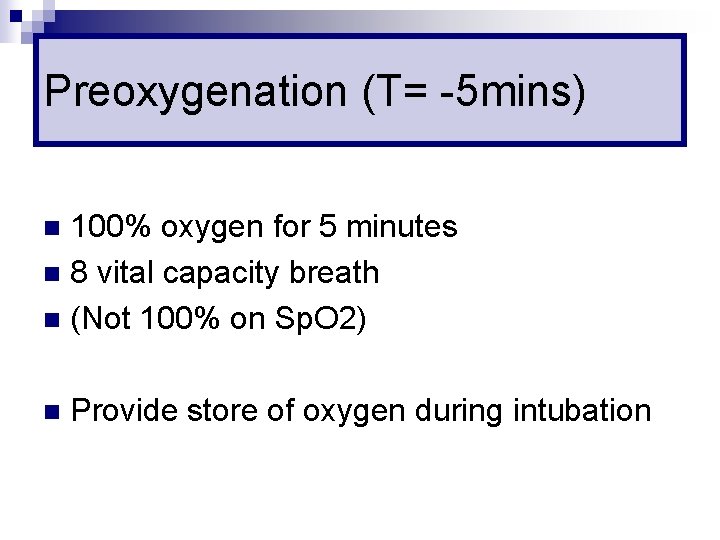
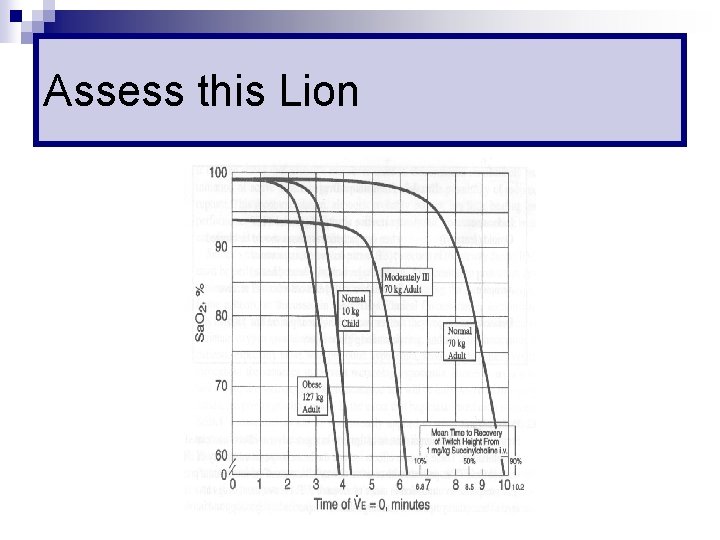
Preoxygenation (T= -5 mins) 100% oxygen for 5 minutes n 8 vital capacity breath n (Not 100% on Sp. O 2) n n Provide store of oxygen during intubation

Time to Desaturation
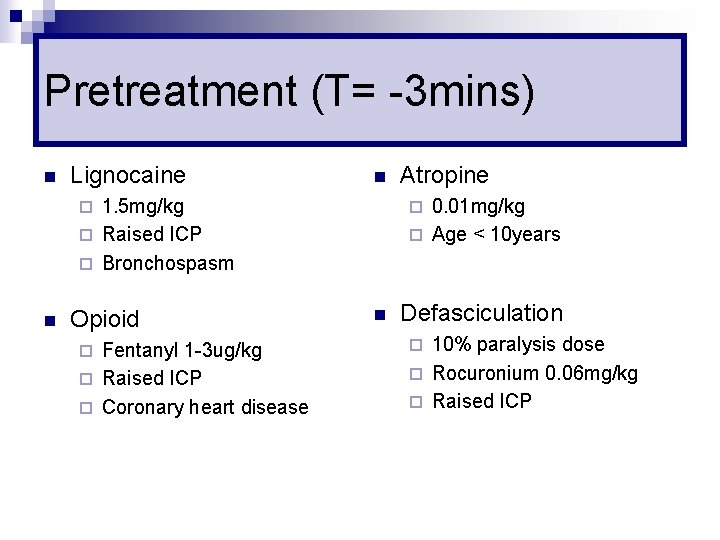
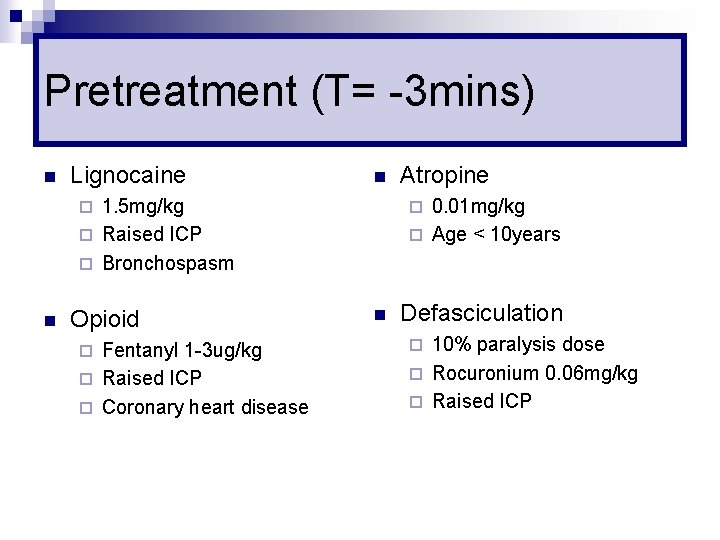
Pretreatment (T= -3 mins) n Lignocaine n 1. 5 mg/kg ¨ Raised ICP ¨ Bronchospasm 0. 01 mg/kg ¨ Age < 10 years ¨ n Opioid Fentanyl 1 -3 ug/kg ¨ Raised ICP ¨ Coronary heart disease ¨ Atropine ¨ n Defasciculation 10% paralysis dose ¨ Rocuronium 0. 06 mg/kg ¨ Raised ICP ¨
Paralysis with Induction (T= 0 s) n Ascertain everyone is ready n Sedative → Relaxant → NS flush ¨ As quickly as possible ¨ Don’t flush between sedative & relaxant
Protection & Positioning (T= +30 s) n Cricoid Pressure n Position patient n Do not bag unless Sp. O 2<90 ¨ Increase risk of aspiration
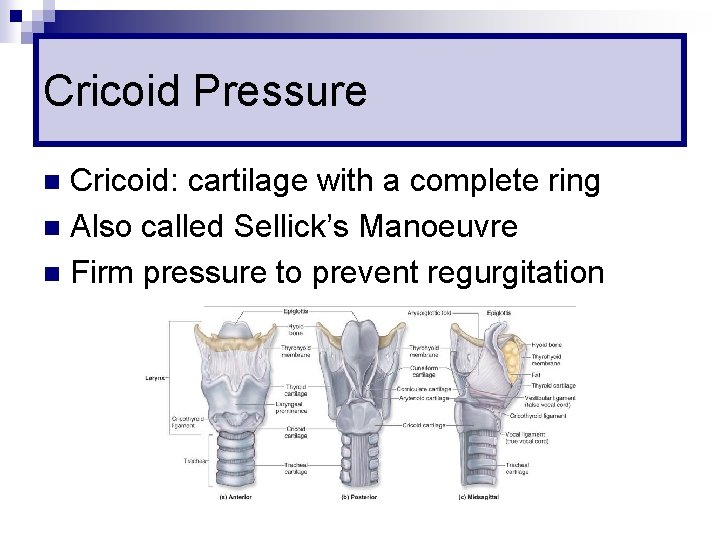
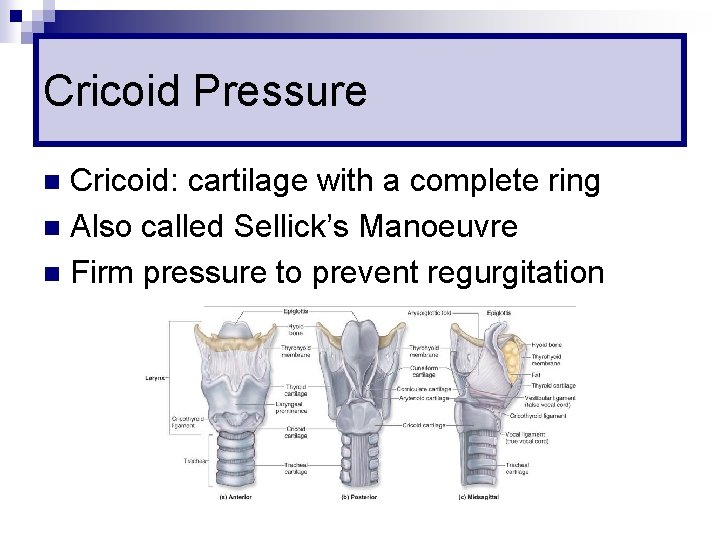
Cricoid Pressure Cricoid: cartilage with a complete ring n Also called Sellick’s Manoeuvre n Firm pressure to prevent regurgitation n
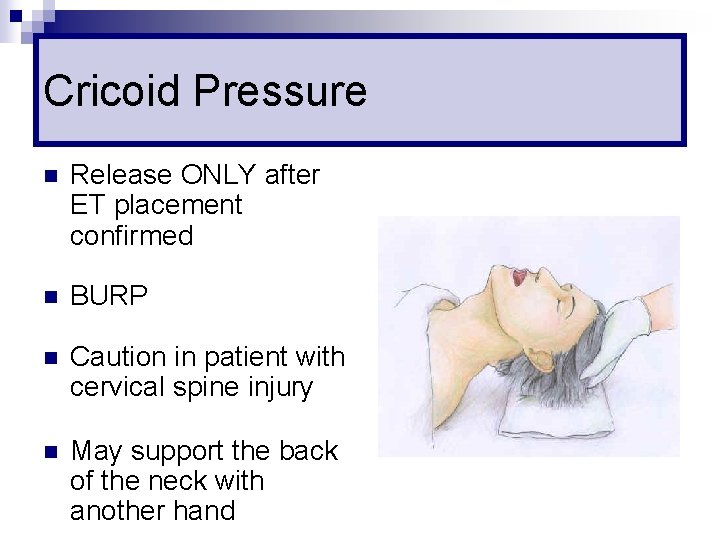
Cricoid Pressure n Release ONLY after ET placement confirmed n BURP n Caution in patient with cervical spine injury n May support the back of the neck with another hand
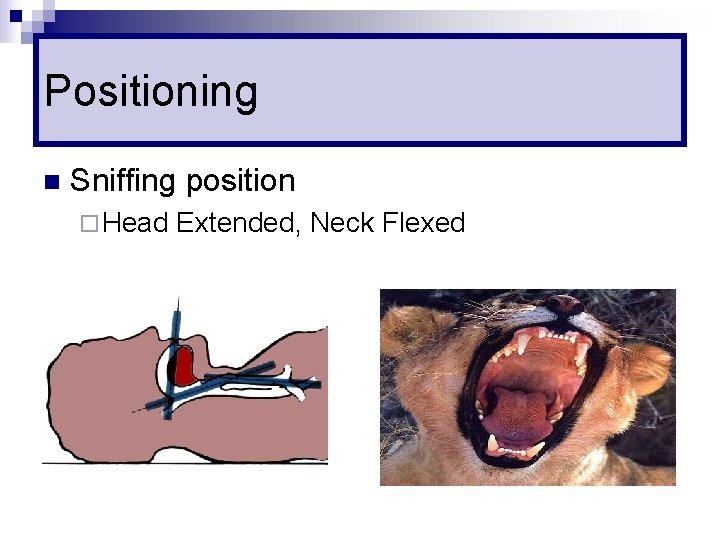
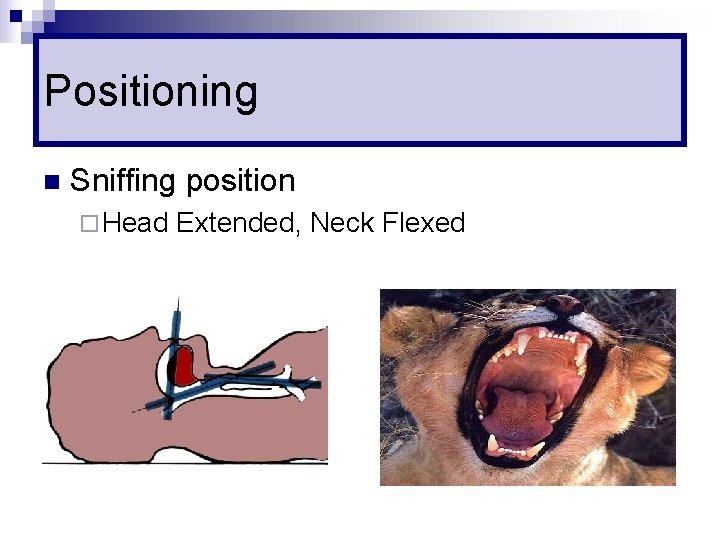
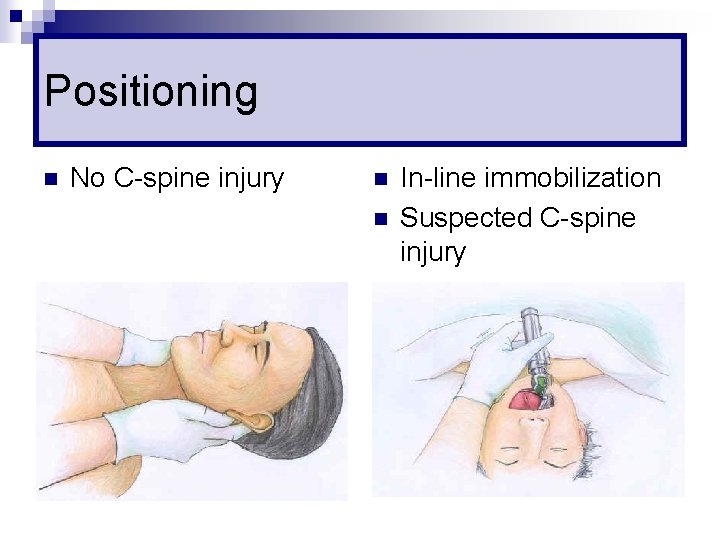
Positioning n Sniffing position ¨ Head Extended, Neck Flexed
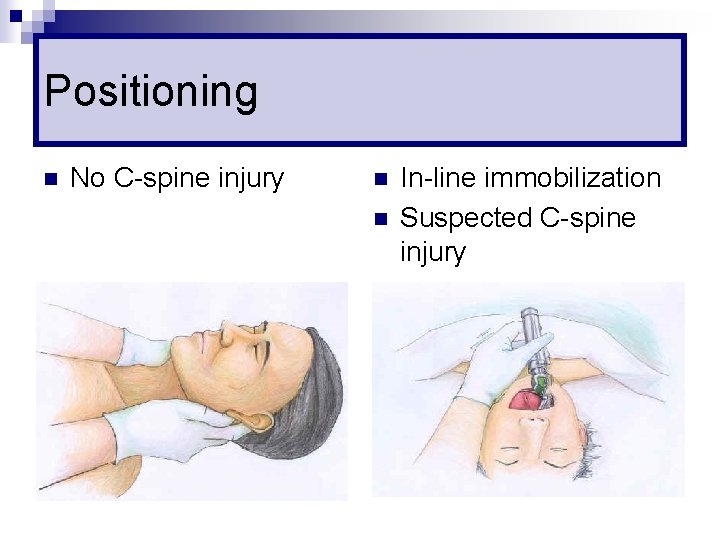
Positioning n No C-spine injury n n In-line immobilization Suspected C-spine injury
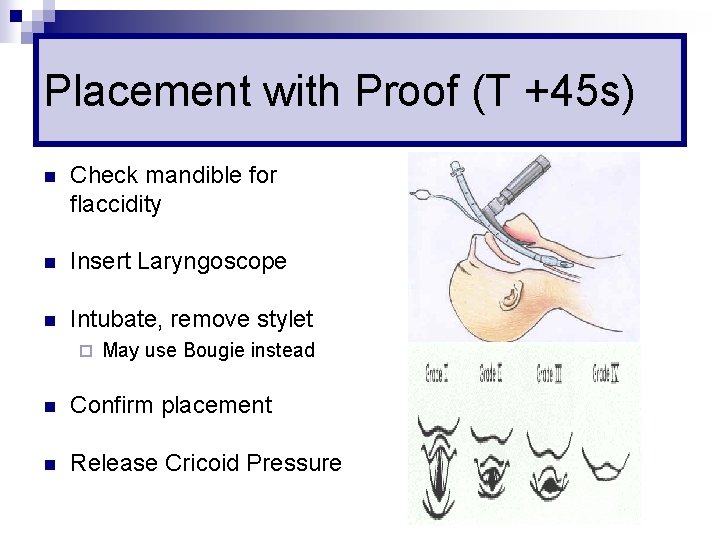
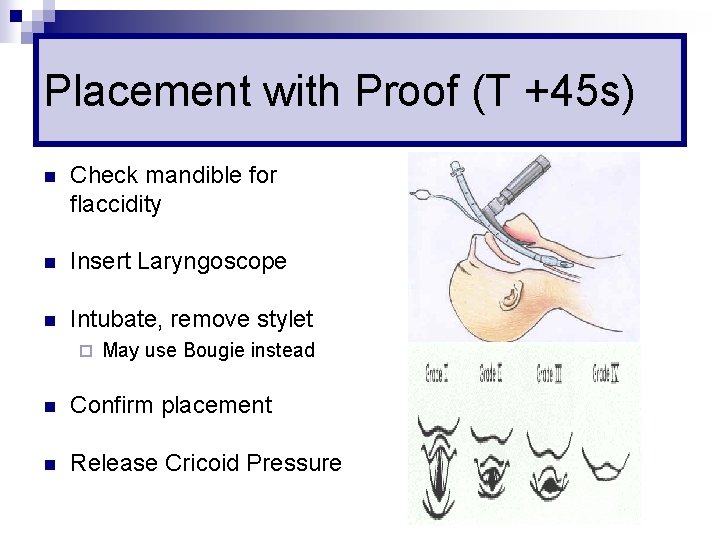
Placement with Proof (T +45 s) n Check mandible for flaccidity n Insert Laryngoscope n Intubate, remove stylet ¨ May use Bougie instead n Confirm placement n Release Cricoid Pressure
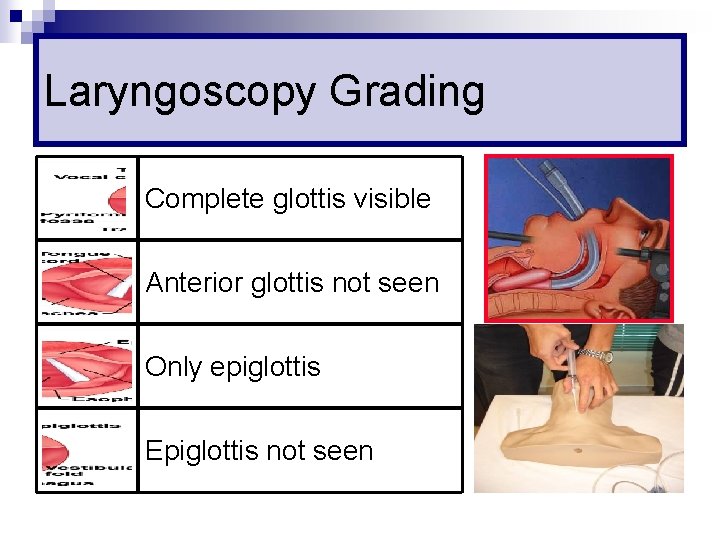
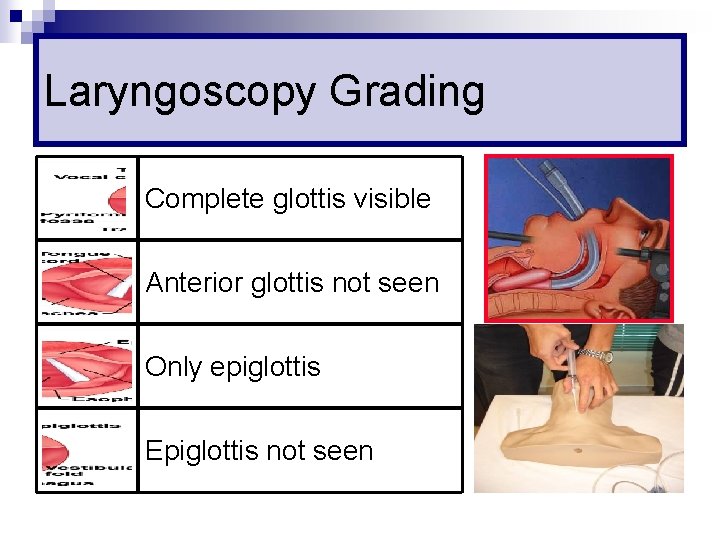
Laryngoscopy Grading Complete glottis visible Anterior glottis not seen Only epiglottis Epiglottis not seen
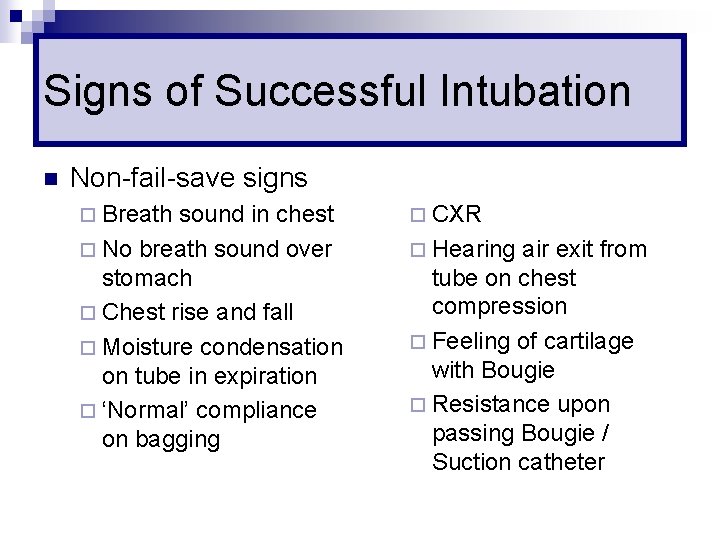
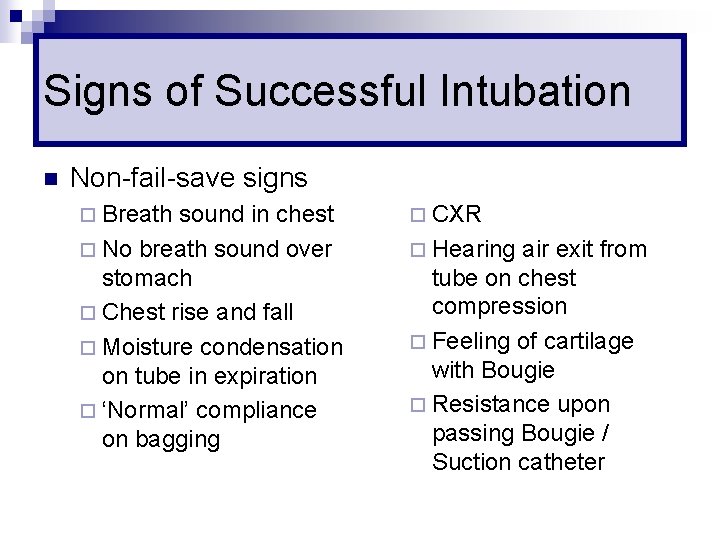
Signs of Successful Intubation n Non-fail-save signs ¨ Breath sound in chest ¨ No breath sound over stomach ¨ Chest rise and fall ¨ Moisture condensation on tube in expiration ¨ ‘Normal’ compliance on bagging ¨ CXR ¨ Hearing air exit from tube on chest compression ¨ Feeling of cartilage with Bougie ¨ Resistance upon passing Bougie / Suction catheter
Signs of Successful Intubation n Near-fail-save signs ¨ ETCO 2 n n (6 breaths / 1 min) False negative in cardiac arrest False positive after carbonated drinks ¨ Oesophageal n Detector Gastric distension
Signs of Successful Intubation n Fail-save signs ¨ Fiberoptic visualization of the bronchial tree ¨ Visualization of tube between cord n DL not always reliable
Postintubation Management n Secure Tube n CXR n Sedation +/- paralysis n Set ventilator
7 Ps Preparation (Time -10 mins) n Preoxygenation (Time -5 mins) n Pretreatment (Time -3 mins) n Paralysis with induction (Time Zero) n Protection and positioning (Time +30 s) n Placement with proof (Time +45 s) n Postintubation management n
Failed Intubation n Summon Help n Mask ventilation n Think about why n Change blade or intubator n Optimize patient n ? ? Impossible to intubate
Maintain Ventilation n Patient die not from failed intubation but failed ventilation Rescue from failed intubation is bagging n Rescue from failed bagging is ‘better’ bagging n n Another dose of relaxant often KILLS
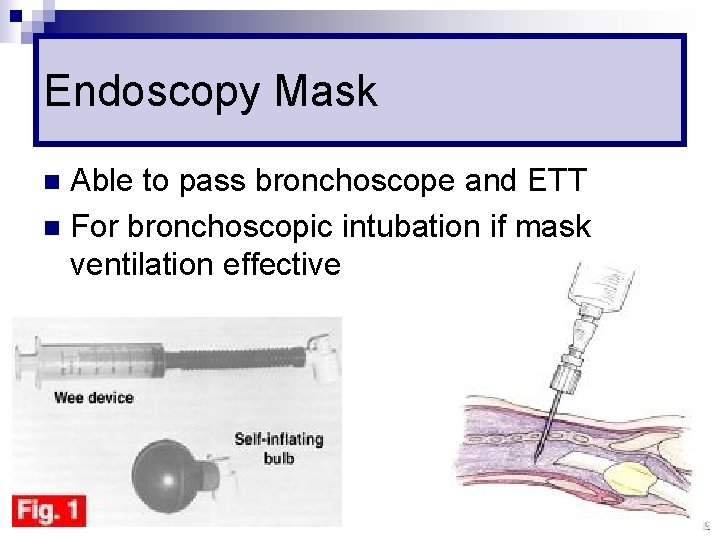
Endoscopy Mask Able to pass bronchoscope and ETT n For bronchoscopic intubation if mask ventilation effective n
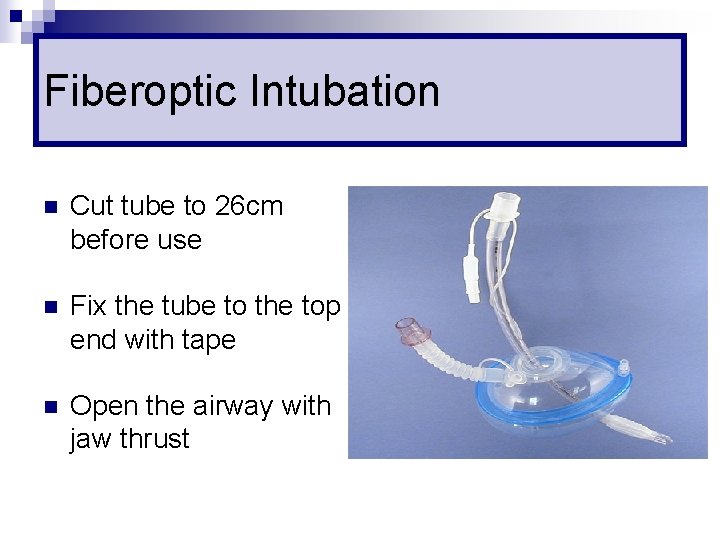
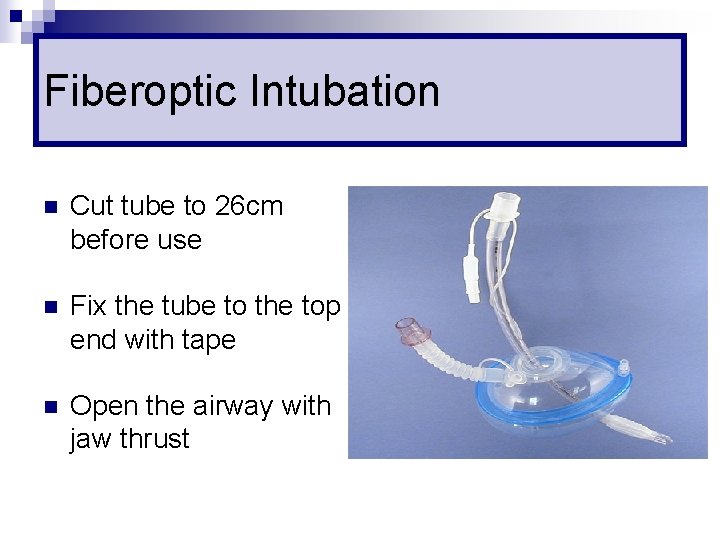
Fiberoptic Intubation n Cut tube to 26 cm before use n Fix the tube to the top end with tape n Open the airway with jaw thrust
Difficult Bagging n Insertion of oral / nasal airway n Other Airway adjuncts ¨ Laryngeal n Mask Airway Intubating Laryngeal Mask ¨ Combitube n Laryngeal Tube
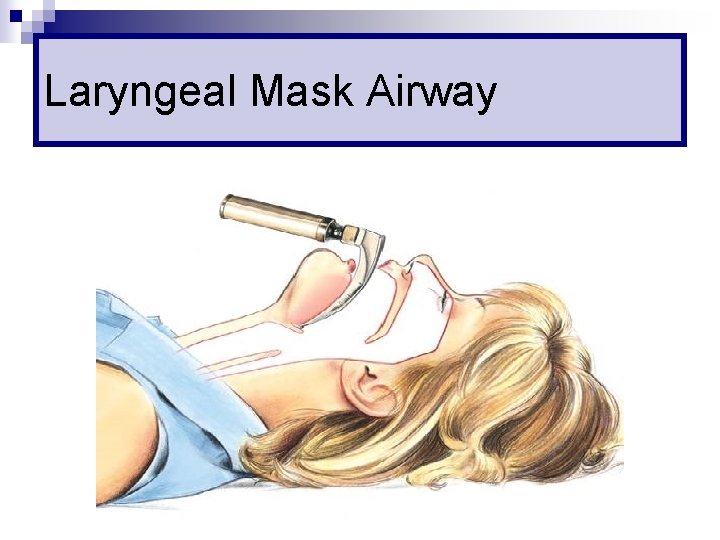
Laryngeal Mask Airway
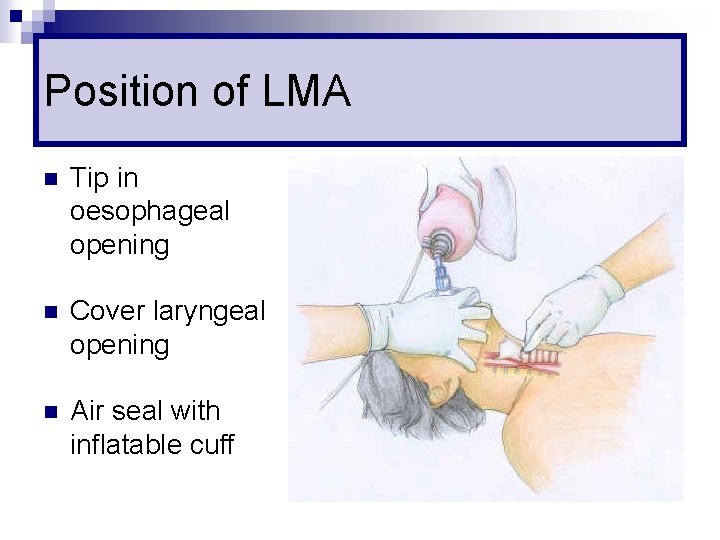
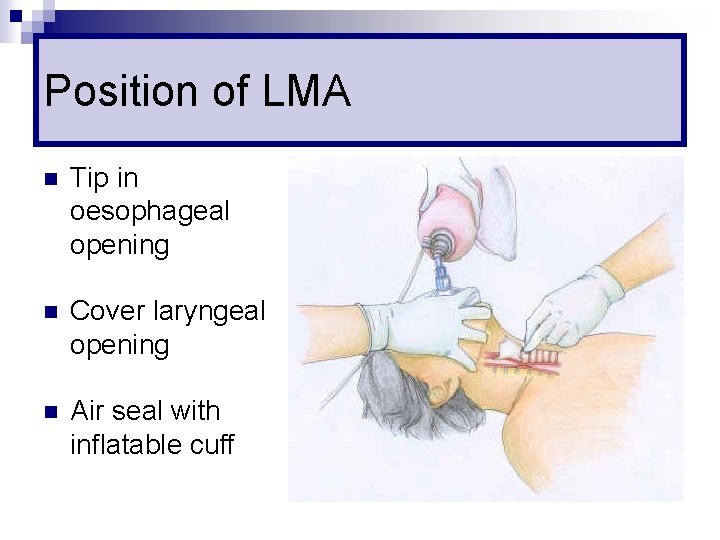
Position of LMA n Tip in oesophageal opening n Cover laryngeal opening n Air seal with inflatable cuff
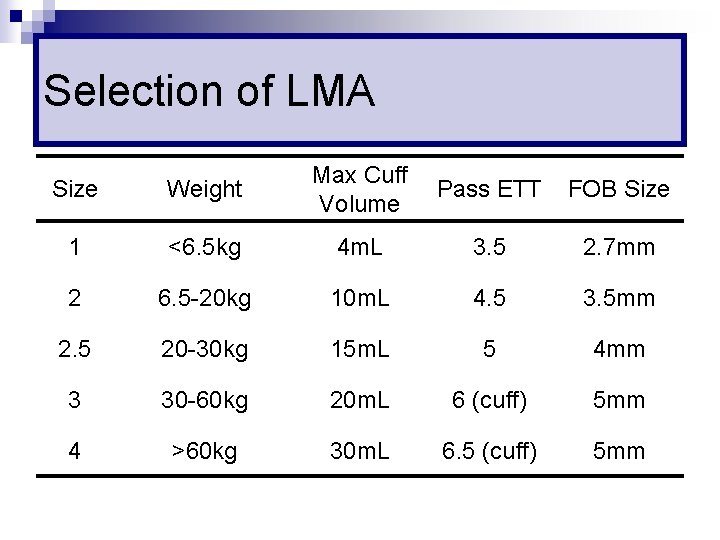
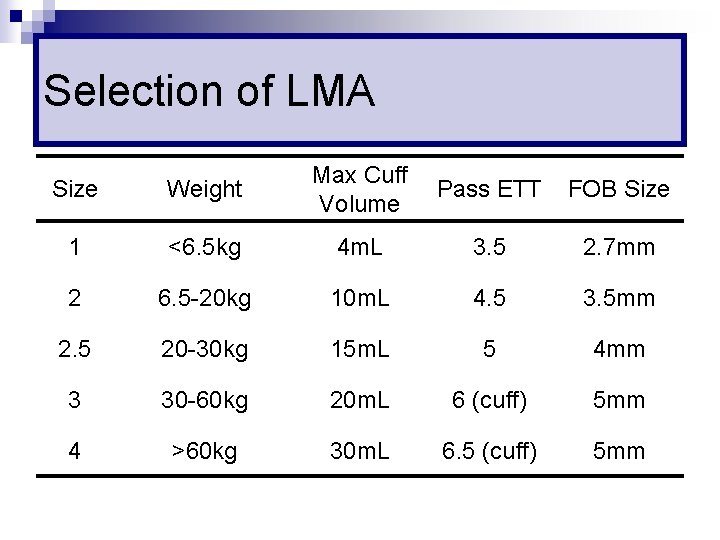
Selection of LMA Size Weight Max Cuff Volume 1 <6. 5 kg 4 m. L 3. 5 2. 7 mm 2 6. 5 -20 kg 10 m. L 4. 5 3. 5 mm 2. 5 20 -30 kg 15 m. L 5 4 mm 3 30 -60 kg 20 m. L 6 (cuff) 5 mm 4 >60 kg 30 m. L 6. 5 (cuff) 5 mm Pass ETT FOB Size
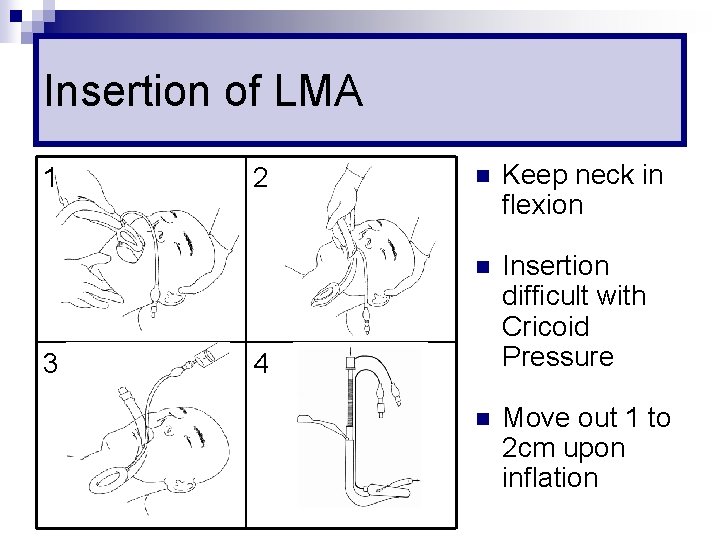
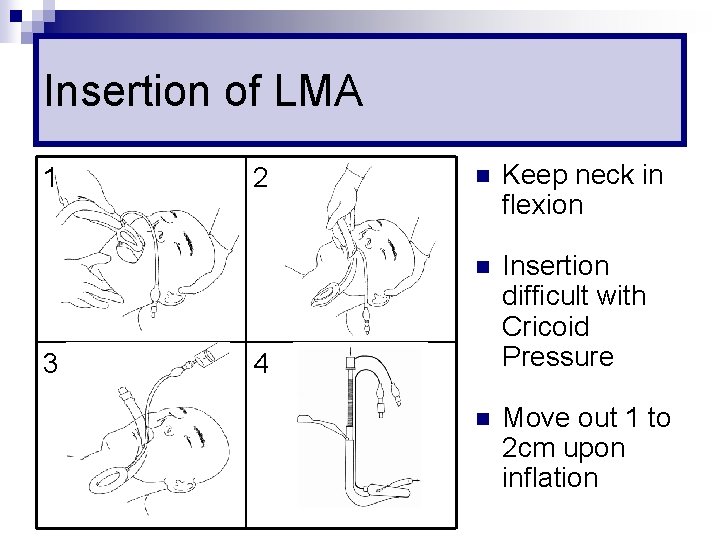
Insertion of LMA 1 3 2 n Keep neck in flexion n Insertion difficult with Cricoid Pressure n Move out 1 to 2 cm upon inflation 4
Advantage of LMA n High success rate ¨ 87 -94% with only brief training n No muscle relaxation required n Conduit for subsequent intubation ¨ Fiberoptic / Bougie / 6 mm ETT
Disadvantage of LMA n Risk of Aspiration ¨ Partially n Failure Rate 1 to 5% ¨ Improve n reduced with the newer Proseal with training Airway obstruction with over inflation
LMA Insertion
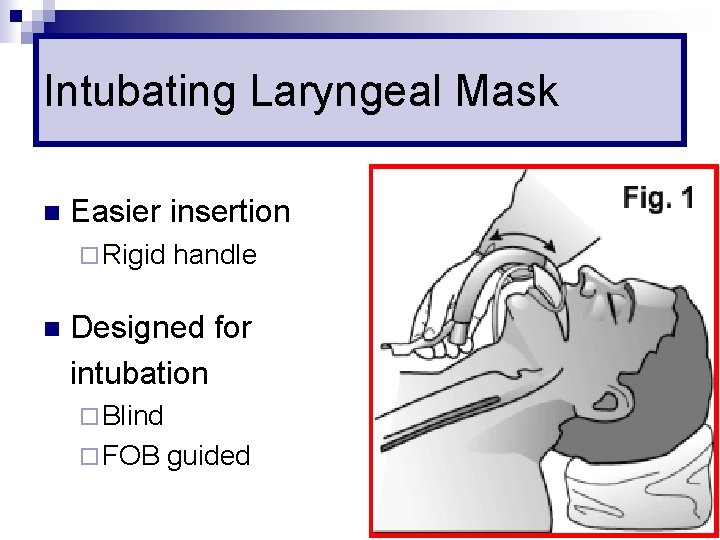
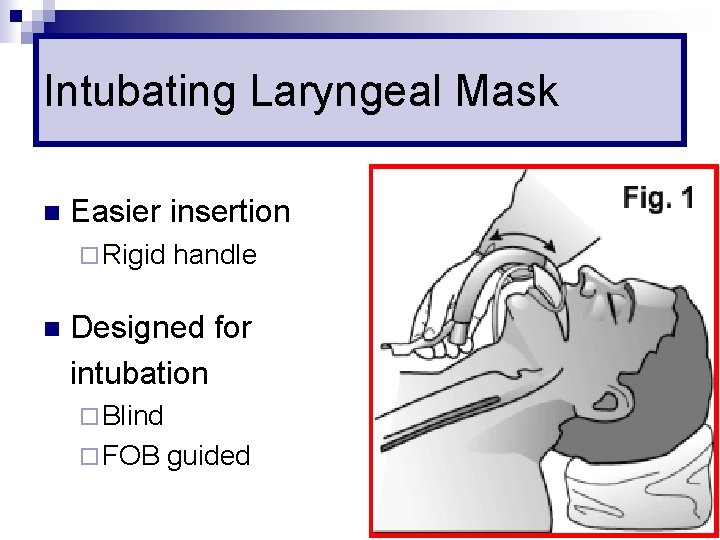
Intubating Laryngeal Mask n Easier insertion ¨ Rigid n handle Designed for intubation ¨ Blind ¨ FOB guided
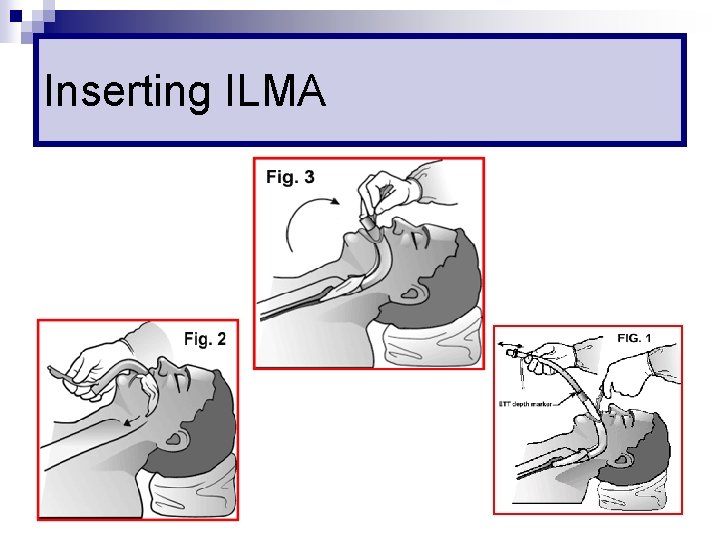
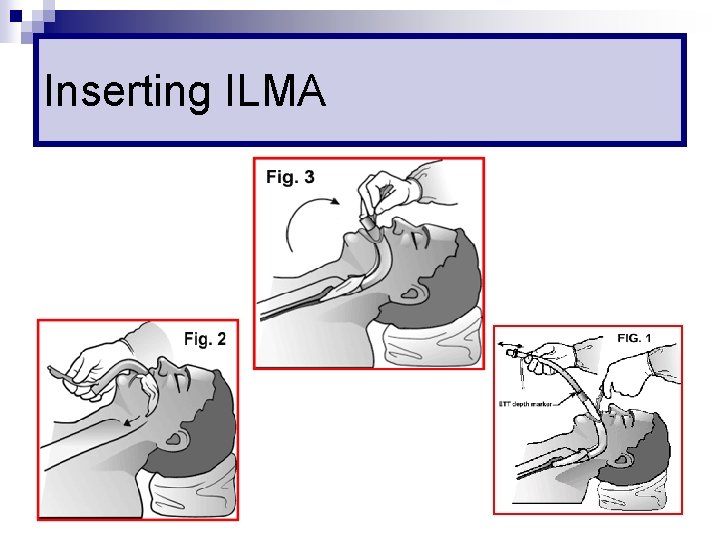
Inserting ILMA
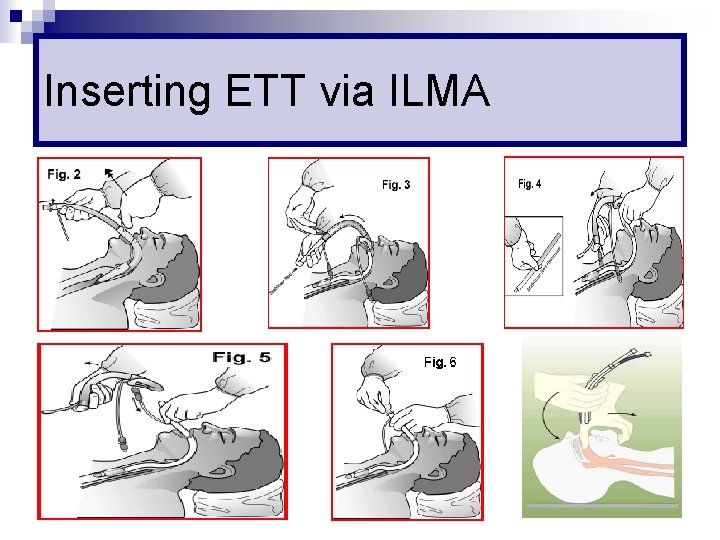
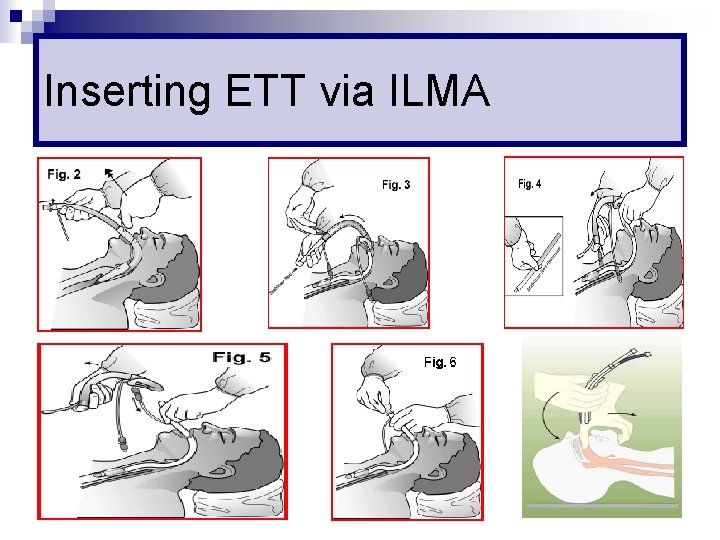
Inserting ETT via ILMA
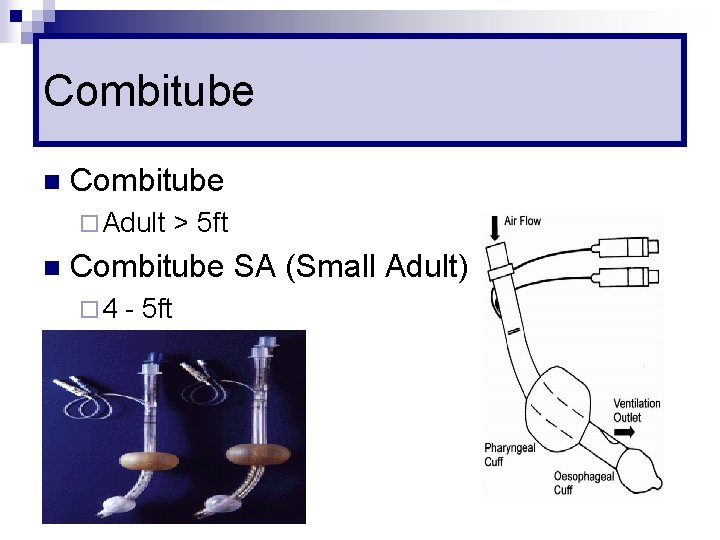
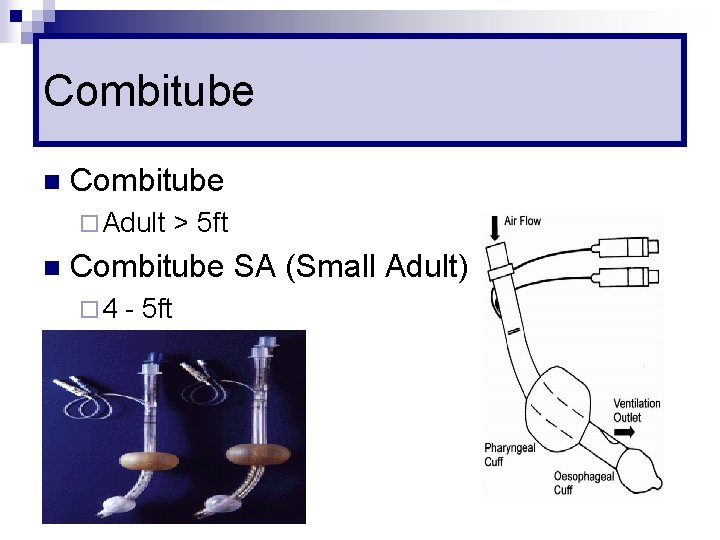
Combitube n Combitube ¨ Adult n > 5 ft Combitube SA (Small Adult) ¨ 4 - 5 ft
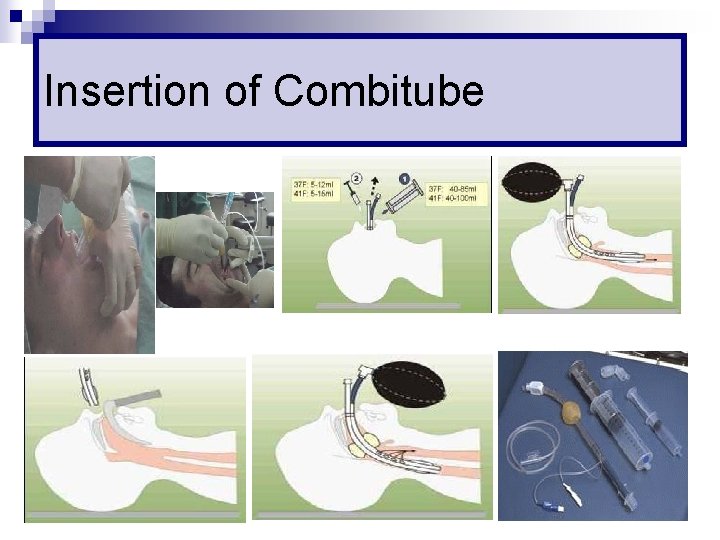
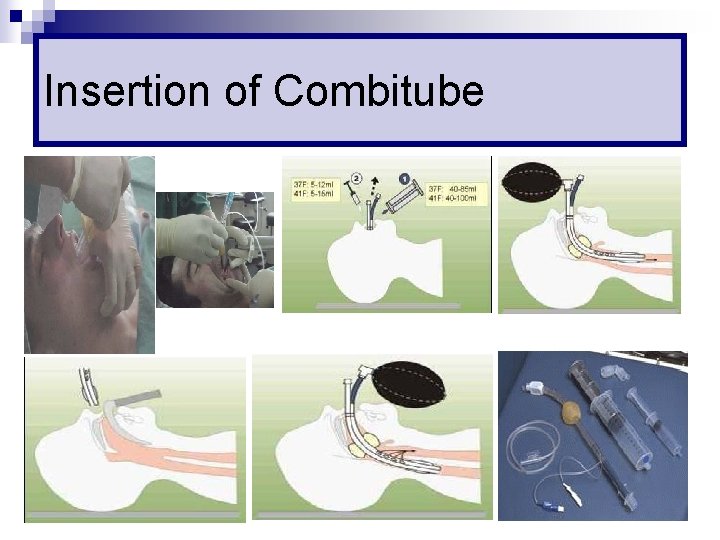
Insertion of Combitube
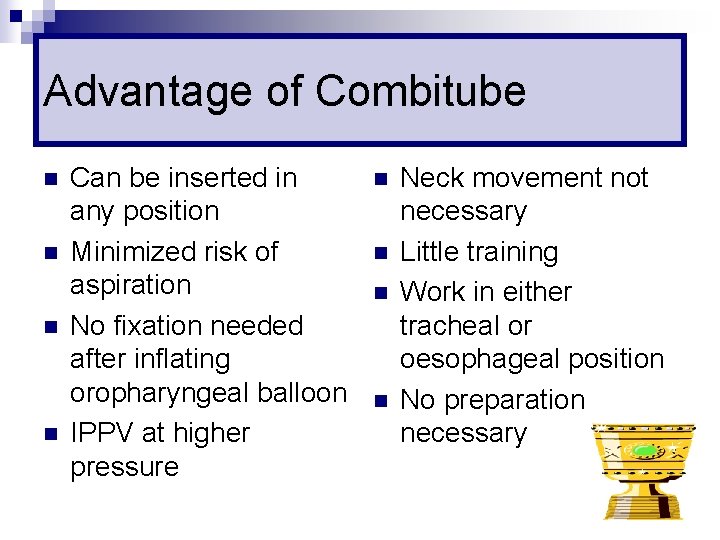
Advantage of Combitube n n Can be inserted in any position Minimized risk of aspiration No fixation needed after inflating oropharyngeal balloon IPPV at higher pressure n n Neck movement not necessary Little training Work in either tracheal or oesophageal position No preparation necessary
Problem with Combitube n Clearance of airway secretion no possible n No conduit to change to ETT
Contraindication n Intact gag reflex n Under 4 feet n Central airway obstruction n Known oesophageal pathology n Caustic ingestion
Combitube Insertion
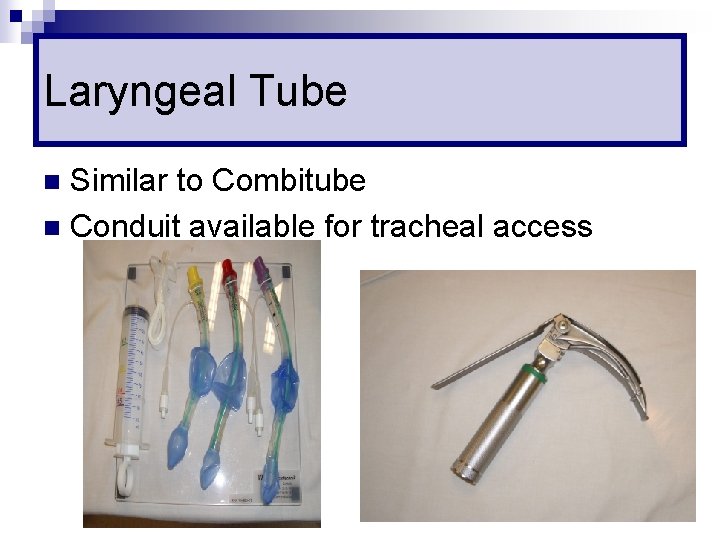
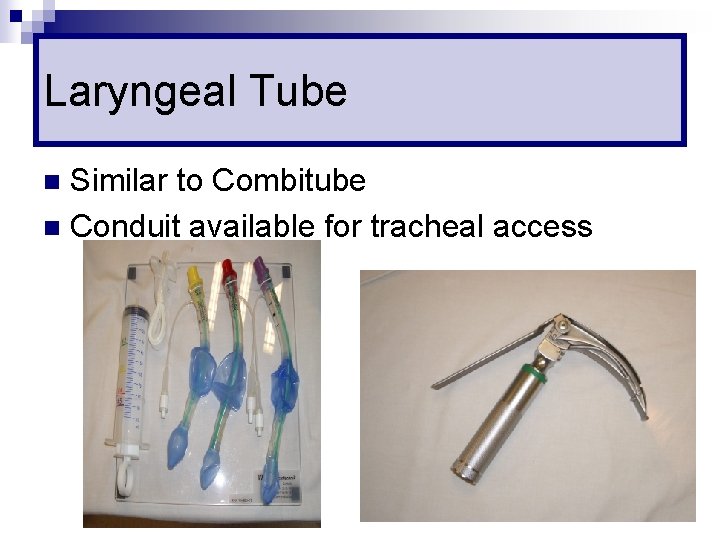
Laryngeal Tube Similar to Combitube n Conduit available for tracheal access n
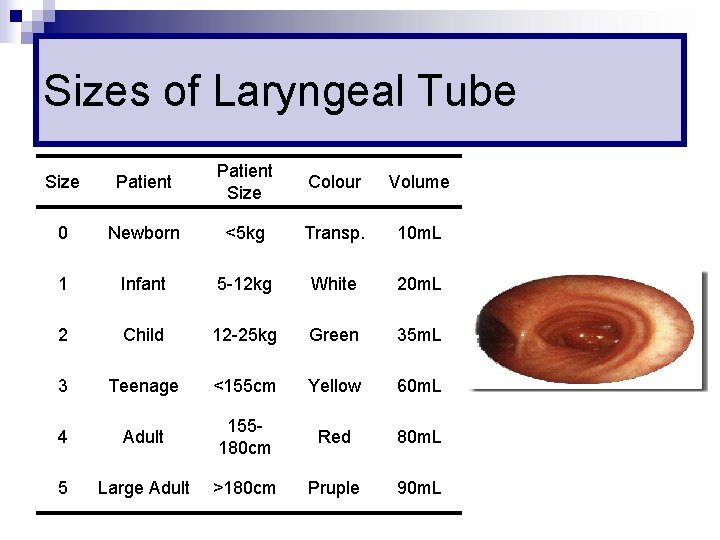
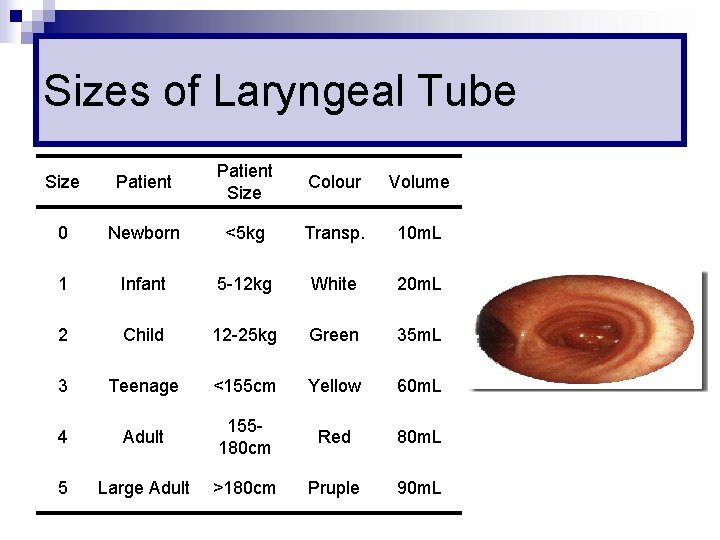
Sizes of Laryngeal Tube Size Patient Size Colour Volume 0 Newborn <5 kg Transp. 10 m. L 1 Infant 5 -12 kg White 20 m. L 2 Child 12 -25 kg Green 35 m. L 3 Teenage <155 cm Yellow 60 m. L 4 Adult 155180 cm Red 80 m. L 5 Large Adult >180 cm Pruple 90 m. L
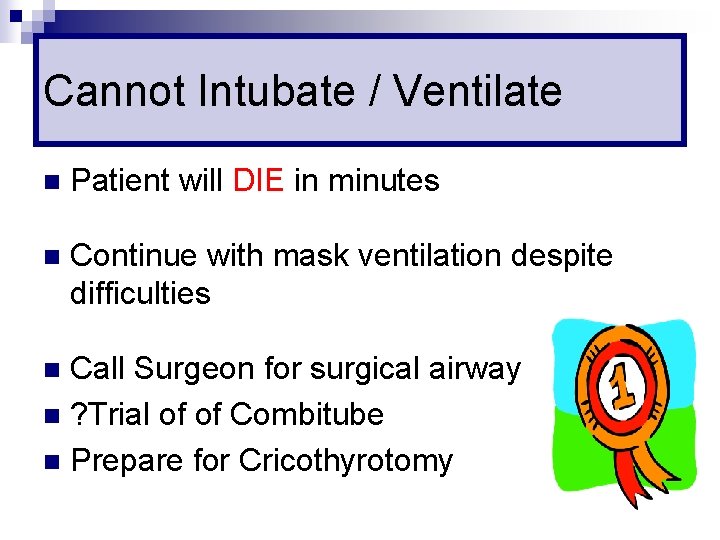
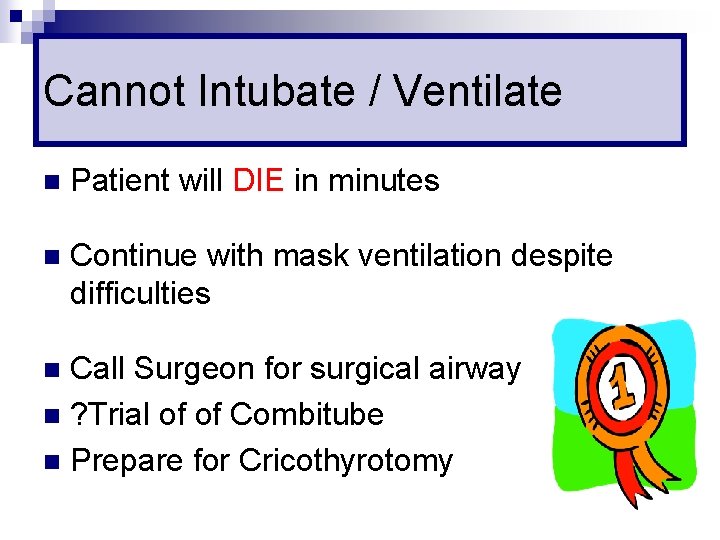
Cannot Intubate / Ventilate n Patient will DIE in minutes n Continue with mask ventilation despite difficulties Call Surgeon for surgical airway n ? Trial of of Combitube n Prepare for Cricothyrotomy n
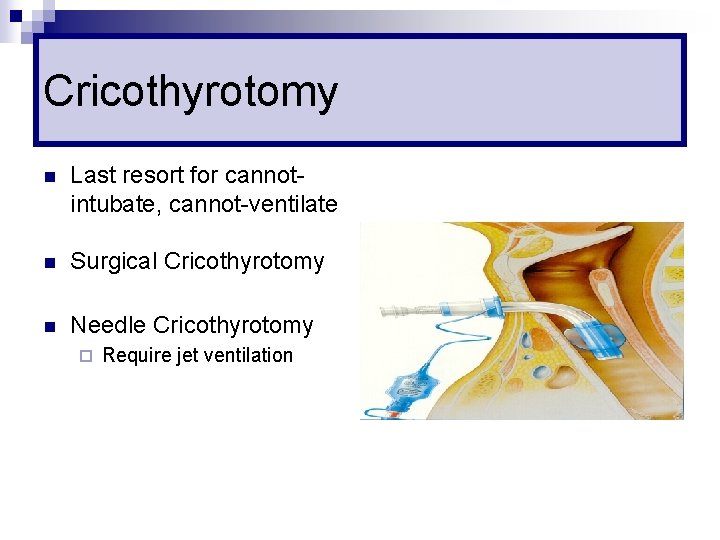
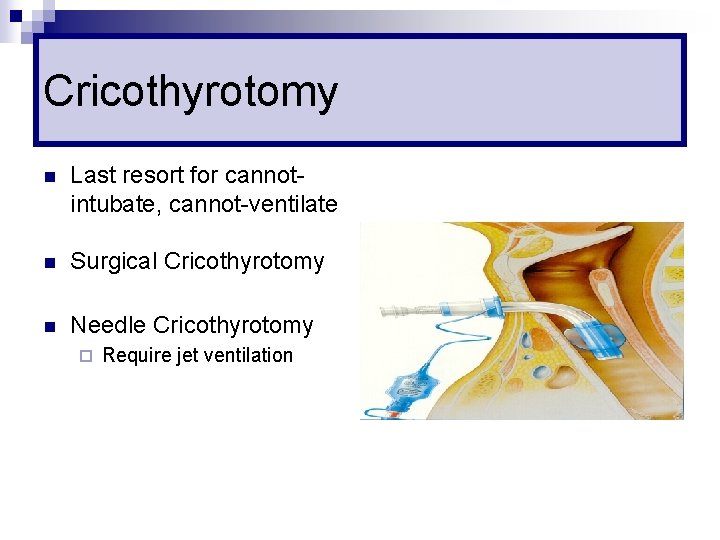
Cricothyrotomy n Last resort for cannotintubate, cannot-ventilate n Surgical Cricothyrotomy n Needle Cricothyrotomy ¨ Require jet ventilation
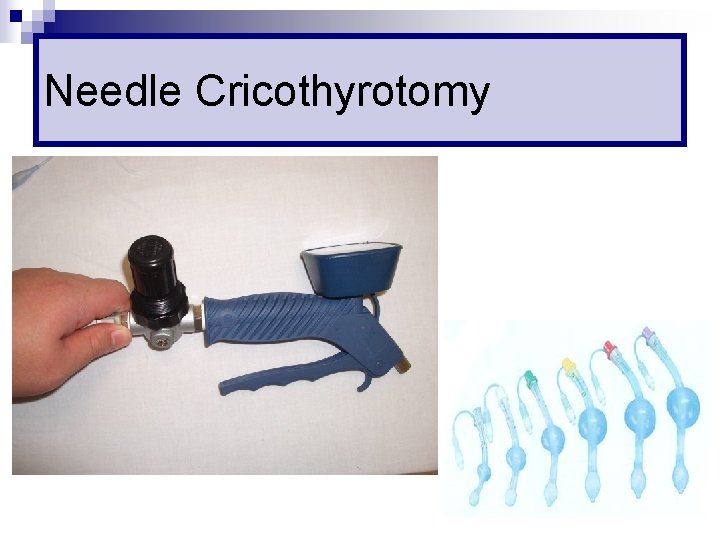
Needle Cricothyrotomy

Needle Cricothyrotomy
Difficult Cricothyrotomy Surgery of neck n Haematoma, infection, or other neck swelling n Obesity n Radiation distortion n Tumour of the neck n

Percutaneous Tracheostomy n Elective procedure n At least 2 doctors ¨ Surgeon ¨ Anaesthetist n / Airway management Usually under LA & sedation
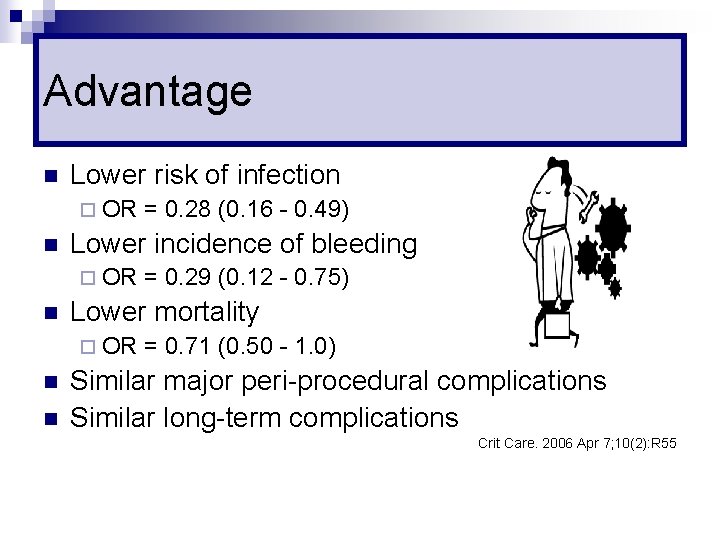
Advantage n Lower risk of infection ¨ OR n Lower incidence of bleeding ¨ OR n n = 0. 29 (0. 12 - 0. 75) Lower mortality ¨ OR n = 0. 28 (0. 16 - 0. 49) = 0. 71 (0. 50 - 1. 0) Similar major peri-procedural complications Similar long-term complications Crit Care. 2006 Apr 7; 10(2): R 55
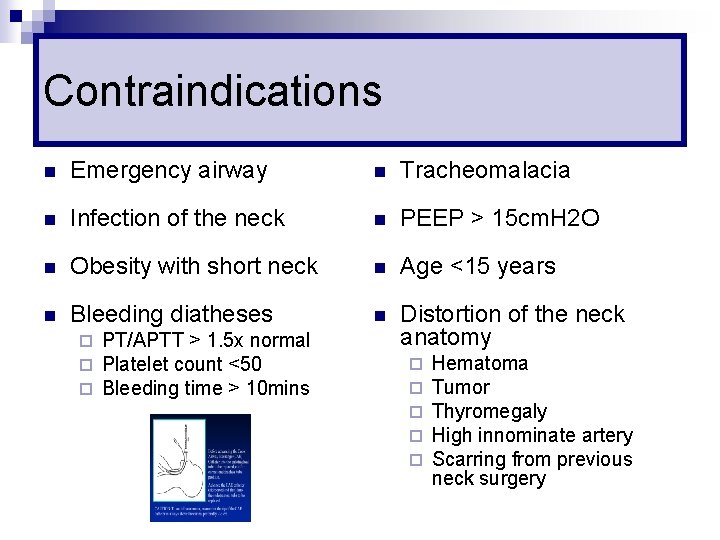
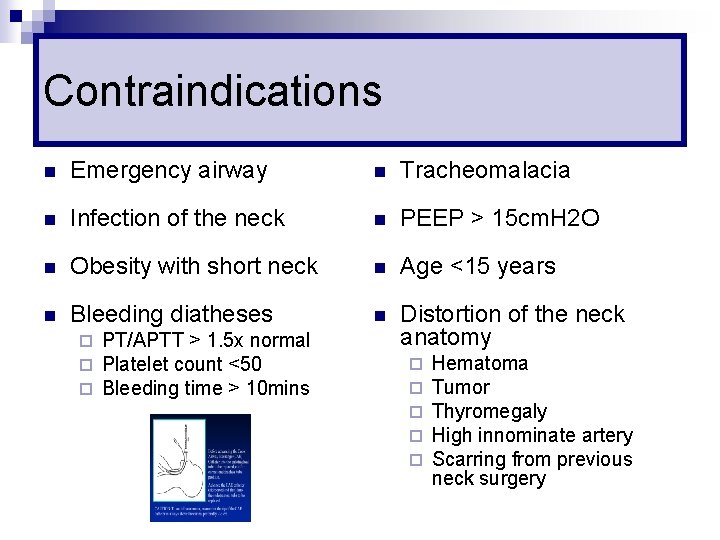
Contraindications n Emergency airway n Tracheomalacia n Infection of the neck n PEEP > 15 cm. H 2 O n Obesity with short neck n Age <15 years n Bleeding diatheses n Distortion of the neck anatomy ¨ ¨ ¨ PT/APTT > 1. 5 x normal Platelet count <50 Bleeding time > 10 mins ¨ ¨ ¨ Hematoma Tumor Thyromegaly High innominate artery Scarring from previous neck surgery
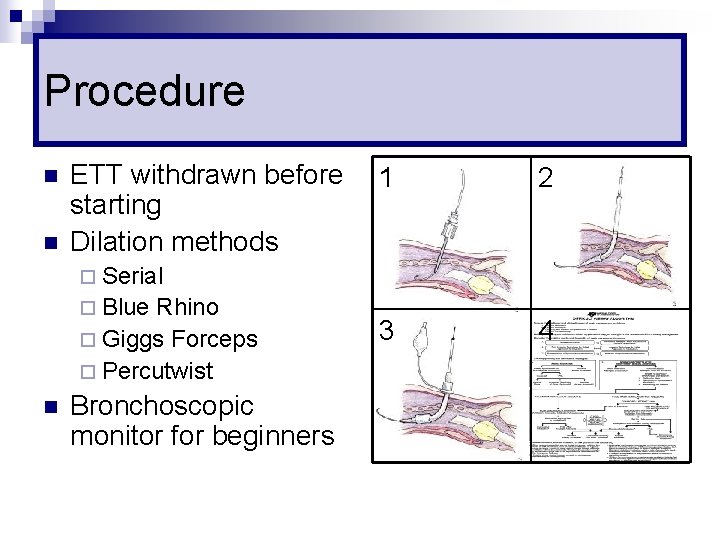
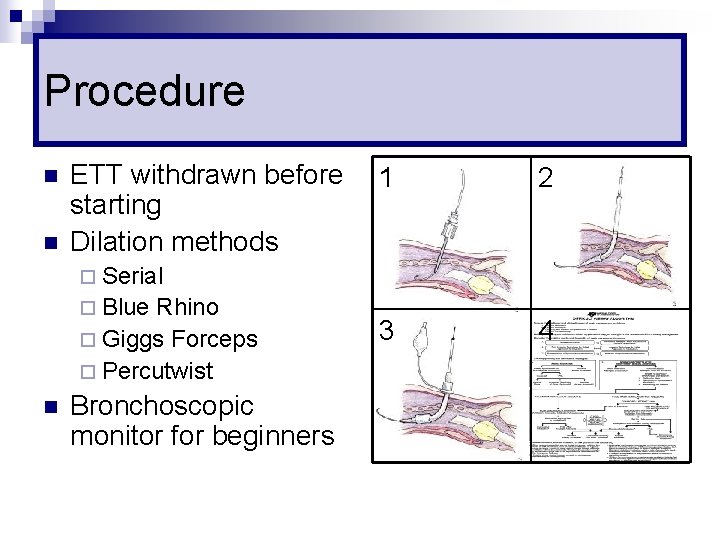
Procedure n n ETT withdrawn before starting Dilation methods 1 2 3 4 ¨ Serial ¨ Blue Rhino ¨ Giggs Forceps ¨ Percutwist n Bronchoscopic monitor for beginners
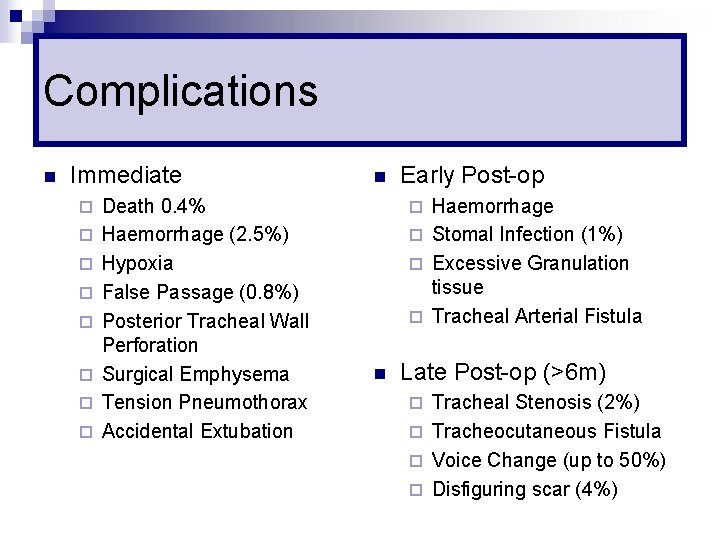
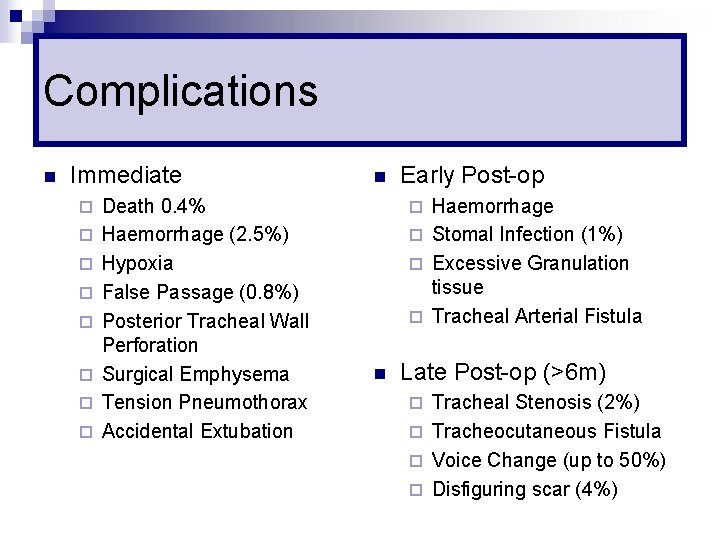
Complications n Immediate ¨ ¨ ¨ ¨ Death 0. 4% Haemorrhage (2. 5%) Hypoxia False Passage (0. 8%) Posterior Tracheal Wall Perforation Surgical Emphysema Tension Pneumothorax Accidental Extubation n Early Post-op Haemorrhage ¨ Stomal Infection (1%) ¨ Excessive Granulation tissue ¨ Tracheal Arterial Fistula ¨ n Late Post-op (>6 m) Tracheal Stenosis (2%) ¨ Tracheocutaneous Fistula ¨ Voice Change (up to 50%) ¨ Disfiguring scar (4%) ¨
Dislodged Tracheostomy n Confirm dislodgement ¨ Cannot pass suction catheter ¨ No ETCO 2 Remove Tracheostomy tube n Do not re-insert tracheostomy if track is not formed (< 1 to 2 weeks) n Start mask ventilation n Reintubate trans-laryngeally n
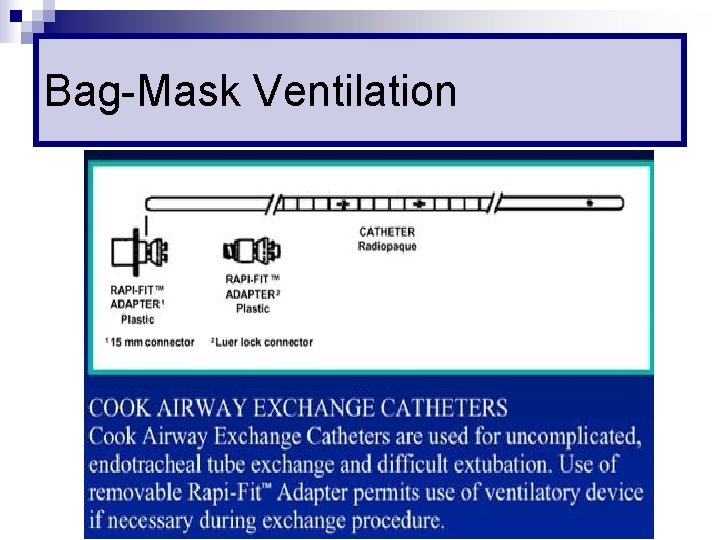
Changing ETT n Adequate fasting n Sedation + paralysis n Cook’s Airway Exchange Catheter ¨ NOT Bougie as it has to be at least twice the length of ETT
Cook’s Catheter
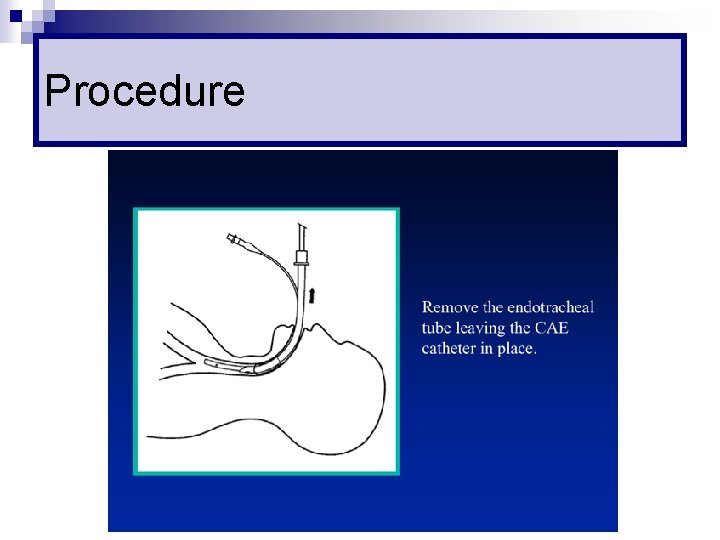
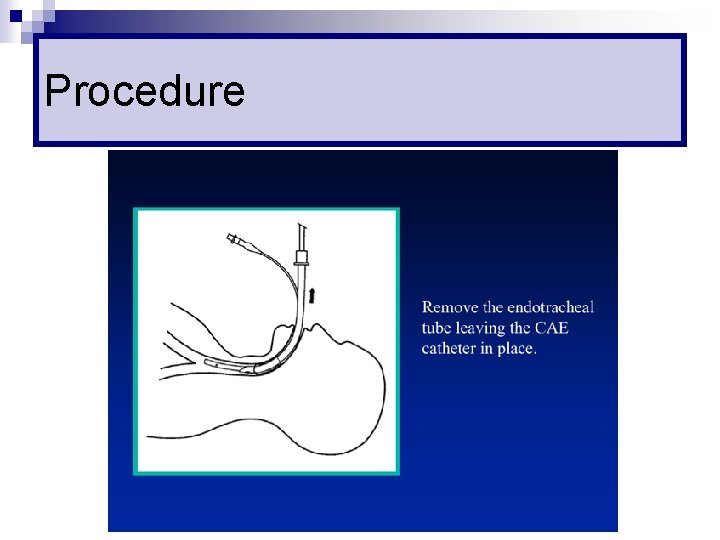
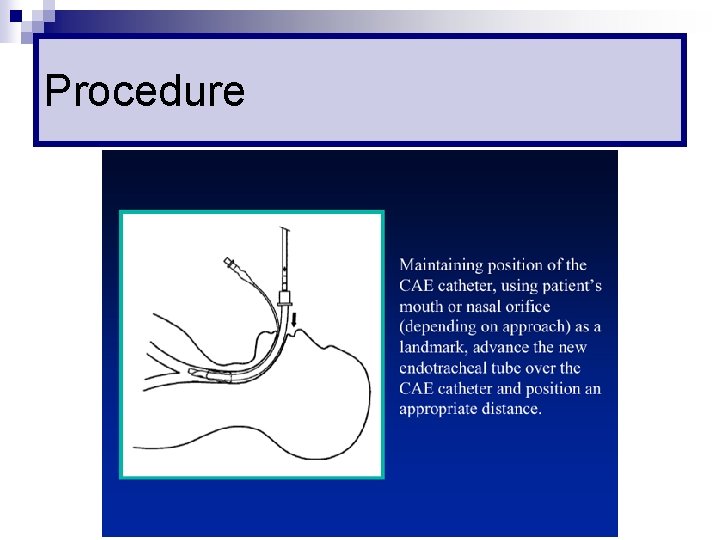
Procedure
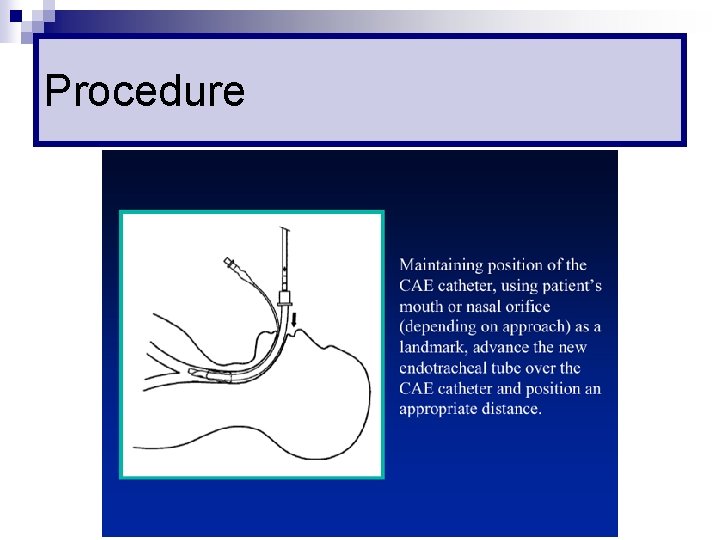
Procedure
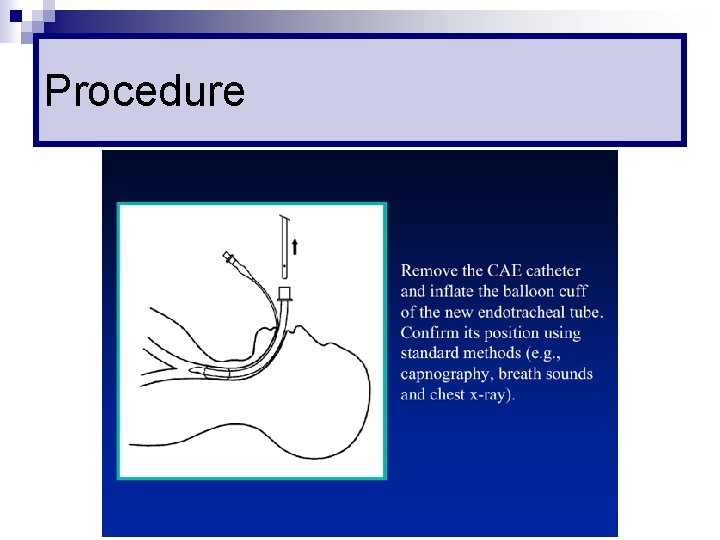
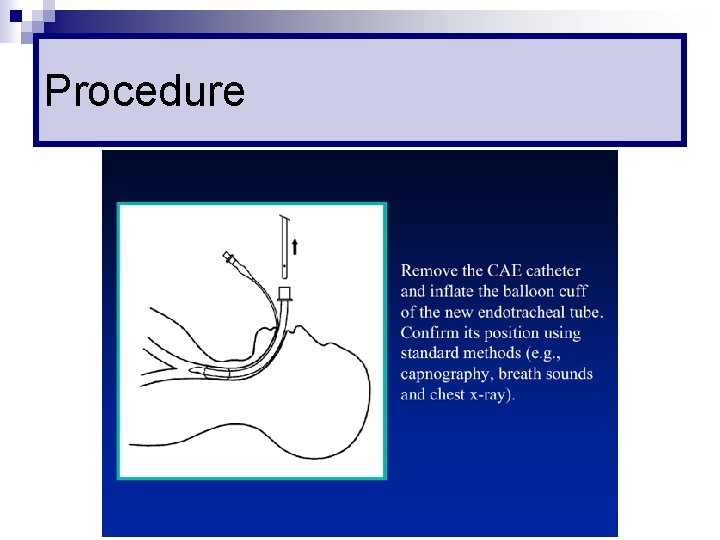
Procedure
Procedure
Reference n Video on the use of various adjuncts ¨ n Use of LMA ¨ n http: //www. lmana. com/prod/components/education_center. html Percutaneous Tracheostomy ¨ n http: //www. trucorp. co. uk/sections/insertion. asp http: //www. emedicine. com/ent/topic 682. htm General airway management http: //theairwaysite. com/education. html ¨ http: //www. aic. cuhk. edu. hk/web 8/Airway. htm ¨
Reference n n BLS Provider Manual (2006) by American Heart Association ACLS Provider Manual (2003) by American Heart Association Airway Management: Principles and Practice (1995) by Benumof et. al. Manual of Emergency Airway Management (2004) by Walls et. al.
 Care of the critically ill surgical patient
Care of the critically ill surgical patient Surgical metabolism
Surgical metabolism Epiglottic
Epiglottic Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Bé thì chăn nghé chăn trâu
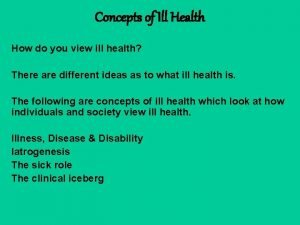
Bé thì chăn nghé chăn trâu Ill project management
Ill project management Tatalaksana acls
Tatalaksana acls Chapter 10 airway management
Chapter 10 airway management Airway management ladder
Airway management ladder Npa measurement
Npa measurement Technique abcde
Technique abcde Airway breathing management
Airway breathing management Stepwise approach to airway management
Stepwise approach to airway management Critically thoughful
Critically thoughful Listening critically
Listening critically Thinking critically with psychological science
Thinking critically with psychological science Pico cat voorbeeld
Pico cat voorbeeld Thinking critically with psychological science
Thinking critically with psychological science General aseptic field
General aseptic field Thinking critically
Thinking critically Thinking critically
Thinking critically Define critical thinking in nursing
Define critical thinking in nursing Sonnet 27 translation
Sonnet 27 translation Negative issues
Negative issues Thinking critically with psychological science answer key
Thinking critically with psychological science answer key General aseptic fields are managed critically
General aseptic fields are managed critically What did you do on weekend
What did you do on weekend Rapid ill
Rapid ill Ticls
Ticls This supernatural soliciting cannot be ill
This supernatural soliciting cannot be ill It is an immediate and temporary care given
It is an immediate and temporary care given Stalling objection
Stalling objection Doing nothing is doing ill
Doing nothing is doing ill V
V Hypothetical meaning exercises
Hypothetical meaning exercises Concepts of ill health
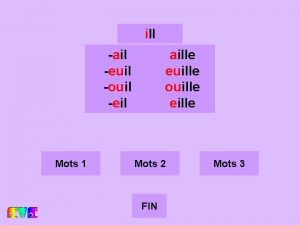
Concepts of ill health Euill
Euill Where you go i'll go where you stay ill stay
Where you go i'll go where you stay ill stay Stupid suffix
Stupid suffix You said i am feeling ill
You said i am feeling ill Rising action of the sob sisters story
Rising action of the sob sisters story Tell me and ill forget
Tell me and ill forget She worked hard. she made herself ill
She worked hard. she made herself ill Horrible manners
Horrible manners Scream and ill tell your mom
Scream and ill tell your mom What is the difference between neurosis and psychosis
What is the difference between neurosis and psychosis Waiting on the lord song
Waiting on the lord song Ill methodology workshop
Ill methodology workshop Daughter and dad
Daughter and dad Ill kill him
Ill kill him I think ill
I think ill Fabiana will not go to work today __ a bit ill
Fabiana will not go to work today __ a bit ill 332 rule intubation
332 rule intubation Pulmonary tract
Pulmonary tract Mechanism of respiration
Mechanism of respiration Respiratory airway secretary
Respiratory airway secretary Intubation anatomy
Intubation anatomy Cormack lehane grading
Cormack lehane grading Airway definitif adalah
Airway definitif adalah What is mean airway pressure
What is mean airway pressure Site:slidetodoc.com
Site:slidetodoc.com Mean airway pressure
Mean airway pressure Combitüp
Combitüp Nasopharyngeal airway
Nasopharyngeal airway Chandys maneuver
Chandys maneuver Larangoscopy
Larangoscopy Mean airway pressure formula
Mean airway pressure formula Automatic positive airway pressure
Automatic positive airway pressure Push hard push fast fully recoil
Push hard push fast fully recoil Airway numaraları
Airway numaraları Asa classification
Asa classification Aprv indications
Aprv indications Airway view
Airway view Pharyngo-tracheal lumen airway
Pharyngo-tracheal lumen airway Head tilt chin lift
Head tilt chin lift Intubation airway anatomy
Intubation airway anatomy Actual diagnosis
Actual diagnosis Indications for artificial airway
Indications for artificial airway What are the emergency action steps?
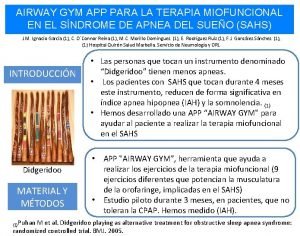
What are the emergency action steps? Airway gym app
Airway gym app A airway b breathing c circulation
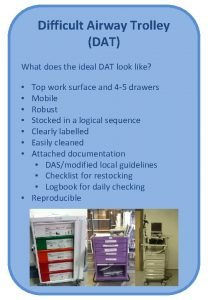
A airway b breathing c circulation Difficult airway trolley
Difficult airway trolley Norwich terrier upper airway syndrome
Norwich terrier upper airway syndrome Moans airway
Moans airway Silverstein fire risk assessment tool
Silverstein fire risk assessment tool Generations of supraglottic airway devices
Generations of supraglottic airway devices Thyromental distance
Thyromental distance Nasopharyngeal airway
Nasopharyngeal airway Pulmonary arterioles
Pulmonary arterioles Difficult airway algorithm asa
Difficult airway algorithm asa Mouth gag airway
Mouth gag airway How will you open the casualty's airway
How will you open the casualty's airway Airway breathing circulation disability exposure
Airway breathing circulation disability exposure Thyromental distance of 7cm
Thyromental distance of 7cm Difficult airway ppt
Difficult airway ppt Constricted airway
Constricted airway Definitive airways
Definitive airways Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay