Airway Management Part 2 Prof M H MUMTAZ















- Slides: 90
Airway Management: Part 2 Prof. M. H. MUMTAZ
Risks/Protective Measures z. Be prepared for: y. Coughing y. Spitting y. Vomiting y. Biting z. Body Substance Isolation y. Gloves y. Face, eye shields y. Respirator, if concern for airborne disease
ALS Airway/Ventilation Methods z. Gastric Tubes y. Nasogastric x. Caution with esophageal disease or facial trauma x. Tolerated by awake patients, but uncomfortable x. Patient can speak x. Interferes with BVM seal y. Orogastric x. Usually used in unresponsive patients x. Larger tube may be used x. Safe in facial trauma
ALS Airway/Ventilation Methods z. Nasogastric Tube Insertion y. Select size (French) y. Measure length (nose to ear to xiphoid) y. Lubricate end of tube (water soluble) y. Maintain aseptic technique y. Position patient sitting up if possible
ALS Airway/Ventilation Methods z. Nasogastric Tube Insertion y. Insert into nare towards angle of jaw y. Advance gradually to measured length y. Have patient swallow y. Assess placement x. Instill air, ausculate xaspirate gastric contents y. Secure y. May connect to low vacuum (80 -100 mm Hg)

ALS Airway/Ventilation Methods z. Orogastric Tube Insertion y. Select size (French) y. Measure length y. Lubricate end of tube y. Position patient (usually supine) y. Insert into mouth y. Advance gradually but steadily y. Assess placement (instill air or aspirate) y. Secure y. Evacuate contents as needed
ET Introduction z. Endotracheal Intubation y. Tube into trachea to provide ventilations using BVM or ventilator y. Sized based upon inside diameter (ID) in mm y. Lengths increase with increased ID (cm markings along length) y. Cuffed vs. Uncuffed
Endotracheal Intubation z. Advantages y. Secures airway y. Route for a few medications (LANE) y. Optimizes ventilation, oxygenation y. Allows suctioning of lower airway
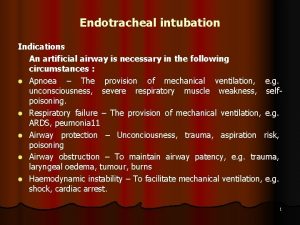
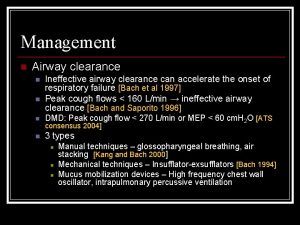
Endotracheal Intubation z. Indications y. Present or impending respiratory failure y. Apnea y. Unable to protect own airway
Endotracheal Intubation z. These are NOT Indications y. Because I can intubate y. Because they are unresponsive y. Because I can’t show up at the hospital without it
Endotracheal Intubation z Complications y. Soft tissue trauma/bleeding y. Dental injury y. Laryngeal edema y. Laryngospasm y. Vocal cord injury y. Barotrauma y. Hypoxia y. Aspiration y. Esophageal intubation y. Mainstem bronchus intubation
Endotracheal Intubation z. Insertion Techniques y. Orotracheal Intubation (Direct Laryngoscopy) y. Blind Nasotracheal Intubation y. Digital Intubation y. Retrograde Intubation y. Transillumination

Orotracheal Intubation z. Technique y. Position, ventilate patient y. Monitor patient x. ECG x. Pulse oximeter y. Assess patient’s airway for difficulty y. Assemble, check equipment (suction) y. Hyperventilate patient (30 -120 sec)

ALS Airway/Ventilation Methods z. Orotracheal Intubation y. Position patient y. Open mouth y. Insert laryngoscope blade on right side y. Sweep tongue to left y. Identify anatomical landmarks y. Advance laryngoscope blade x. Vallecula for curved (Miller) blade x. Under epiglottis for straight (Miller) blade
ALS Airway/Ventilation Methods z. Orotracheal Intubation y. Elevate epiglottis y. Directly with straight (Miller) blade y. Indirectly with curved (Macintosh) blade y. Visualize vocal cords, glottic opening y. Enter mouth with tube from corner of mouth
ALS Airway/Ventilation Methods z. Orotracheal Intubation y. Advance tube into glottic opening about 1/2 inch past vocal cords y. Continue to hold tube, note location y. Ventilate, ausculate x. Epigastrium x. Left and right chest y. Inflate cuff until air leak around cuff stops y. Reassess tube placement
ALS Airway/Ventilation Methods z. Orotracheal Intubation y. Secure tube y. Reassess tube placement, ventilation effectiveness
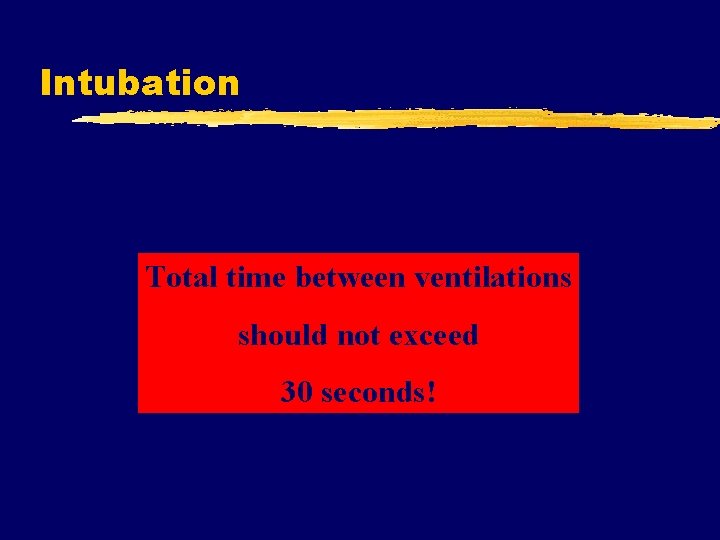
Intubation Total time between ventilations should not exceed 30 seconds!
Intubation Death occurs from failure to Ventilate, not failure to Intubate
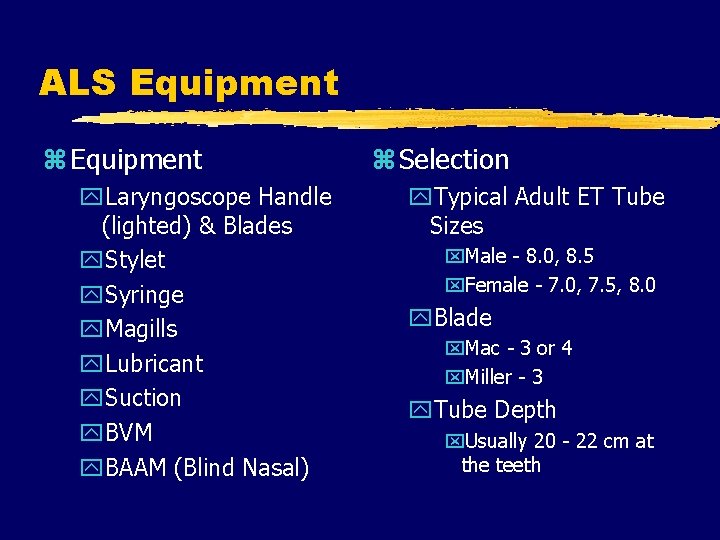
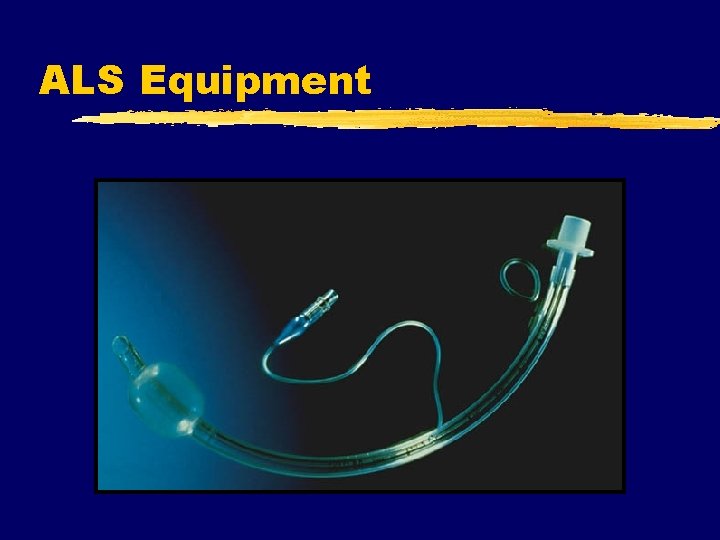
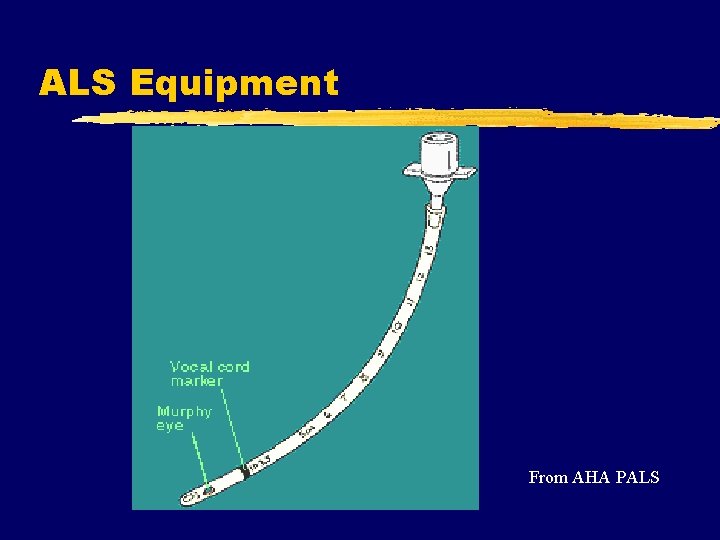
ALS Equipment z Equipment y. Laryngoscope Handle (lighted) & Blades y. Stylet y. Syringe y. Magills y. Lubricant y. Suction y. BVM y. BAAM (Blind Nasal) z Selection y. Typical Adult ET Tube Sizes x. Male - 8. 0, 8. 5 x. Female - 7. 0, 7. 5, 8. 0 y. Blade x. Mac - 3 or 4 x. Miller - 3 y. Tube Depth x. Usually 20 - 22 cm at the teeth
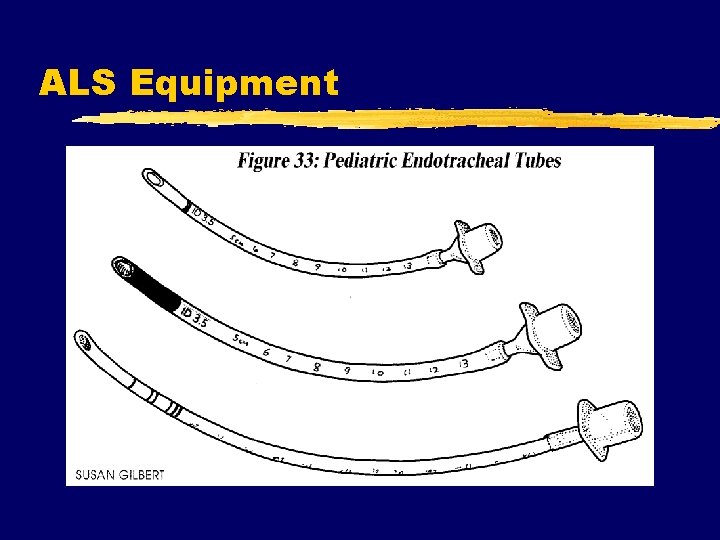
ALS Equipment
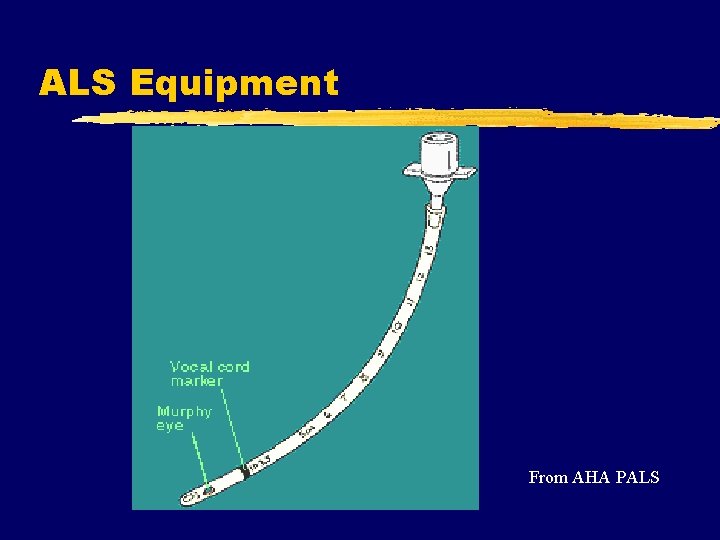
ALS Equipment From AHA PALS
ALS Equipment
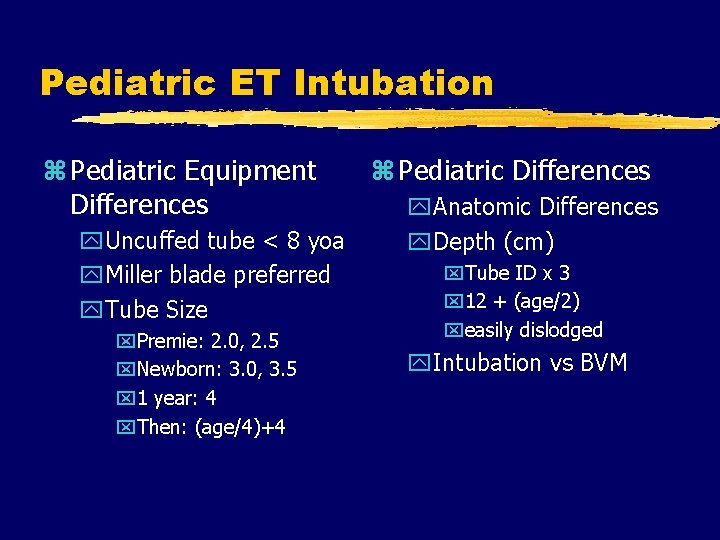
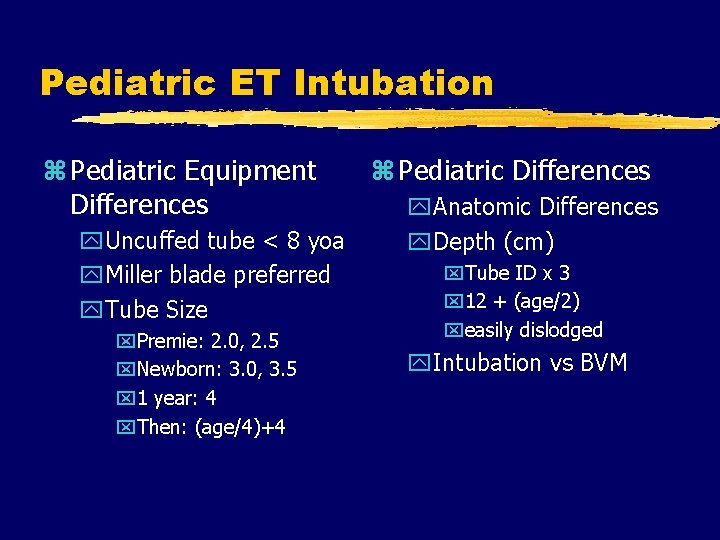
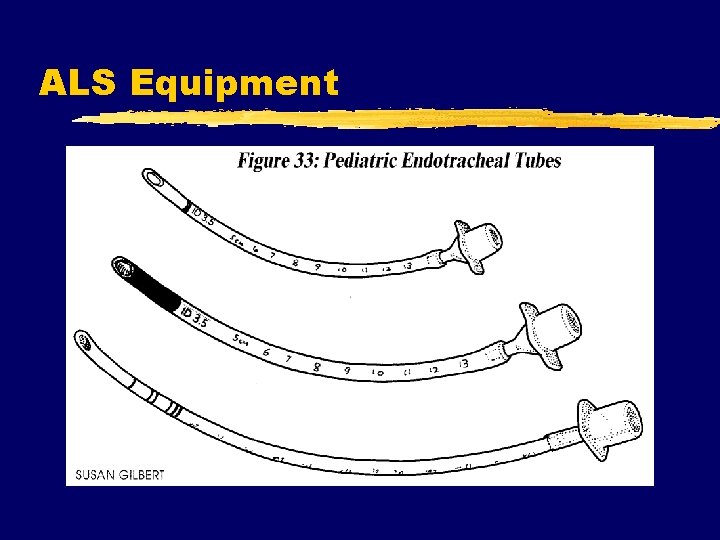
Pediatric ET Intubation z Pediatric Equipment Differences y. Uncuffed tube < 8 yoa y. Miller blade preferred y. Tube Size x. Premie: 2. 0, 2. 5 x. Newborn: 3. 0, 3. 5 x 1 year: 4 x. Then: (age/4)+4 z Pediatric Differences y. Anatomic Differences y. Depth (cm) x. Tube ID x 3 x 12 + (age/2) xeasily dislodged y. Intubation vs BVM
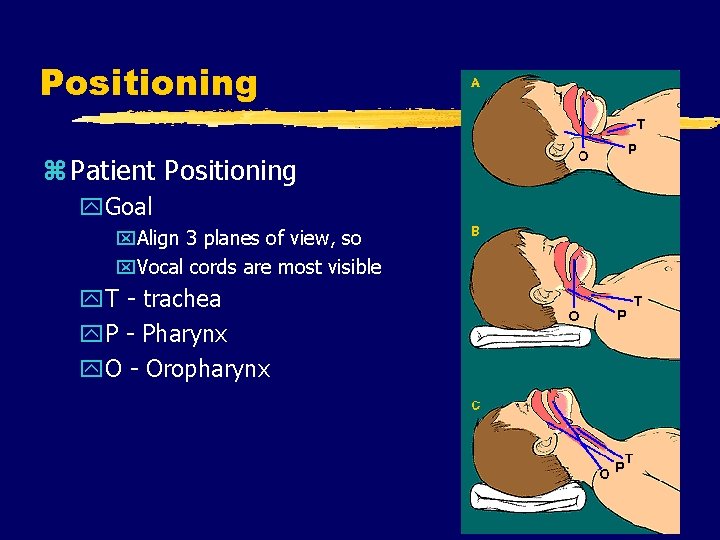
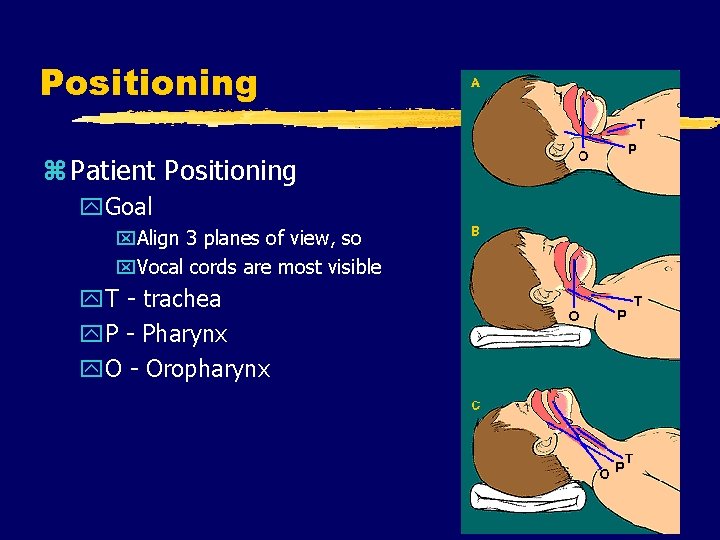
Positioning z Patient Positioning y. Goal x. Align 3 planes of view, so x. Vocal cords are most visible y. T - trachea y. P - Pharynx y. O - Oropharynx

Airway Assessment z. Cervical Spine z. Temporal Mandibular Joint z. A/O Joint z. Neck length, size and muscularity z. Mandibular size in relation to face z. Over bite z. Tongue size
Assessment Acronym z. M z. O z. U z. T z. H z. S Mandible Opening Uvula Teeth Head Silhouette
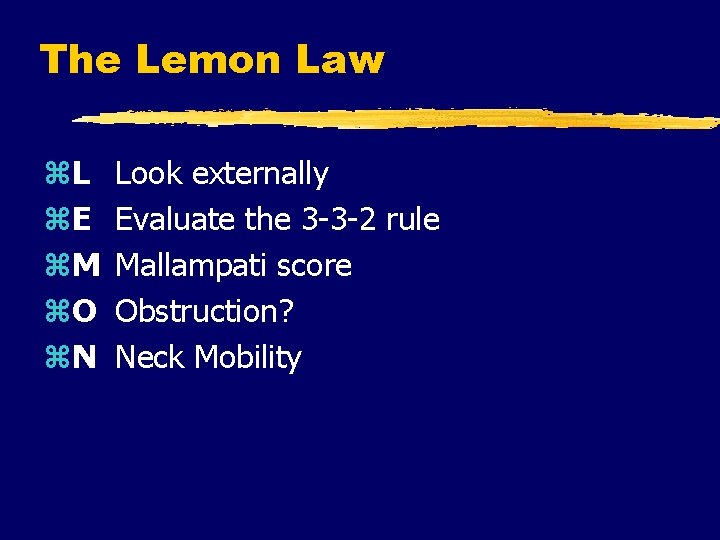
The Lemon Law z. L z. E z. M z. O z. N Look externally Evaluate the 3 -3 -2 rule Mallampati score Obstruction? Neck Mobility
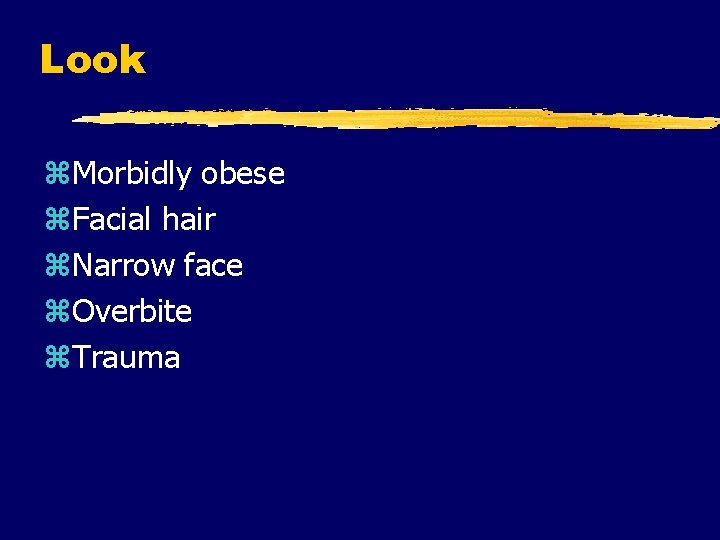
Look z. Morbidly obese z. Facial hair z. Narrow face z. Overbite z. Trauma

Evaluate 3 -3 -2 z. Temporal Mandibular Joint y. Should allow 3 fingers between incisors y 3 -4 cm
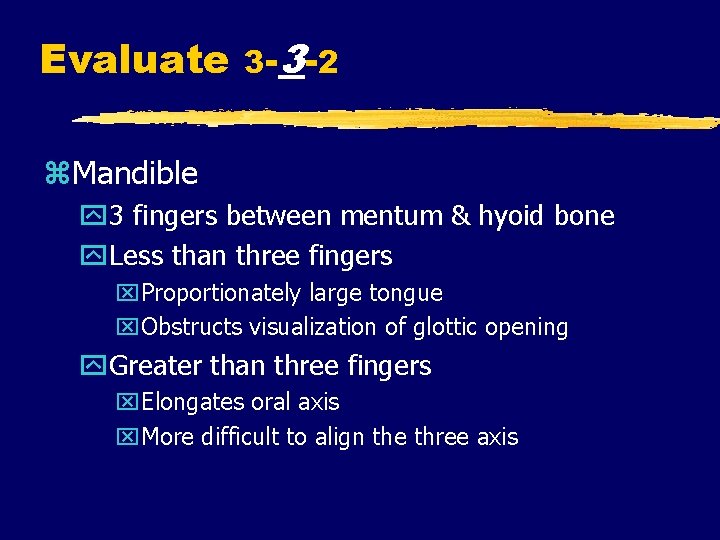
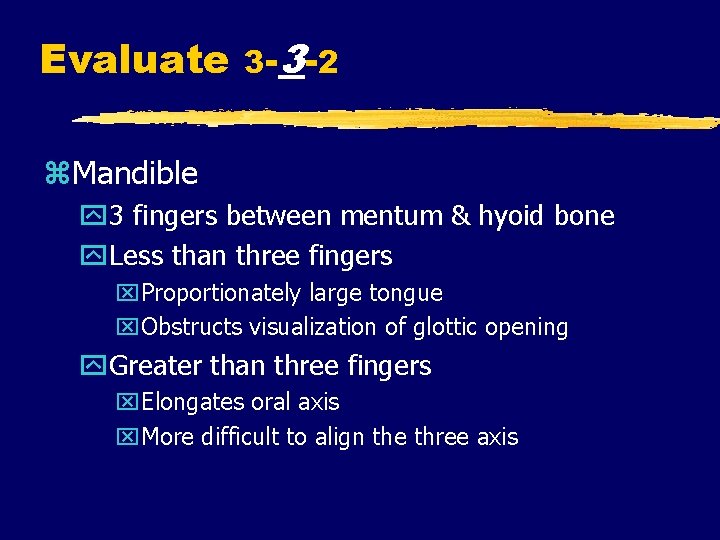
Evaluate 3 -3 -2 z. Mandible y 3 fingers between mentum & hyoid bone y. Less than three fingers x. Proportionately large tongue x. Obstructs visualization of glottic opening y. Greater than three fingers x. Elongates oral axis x. More difficult to align the three axis

Evaluate 3 -3 -2 z. Larynx y. Adult located C 5, 6 y. If higher, obstructive view of glottic opening y. Two fingers from floor of mouth to thyroid cartilage
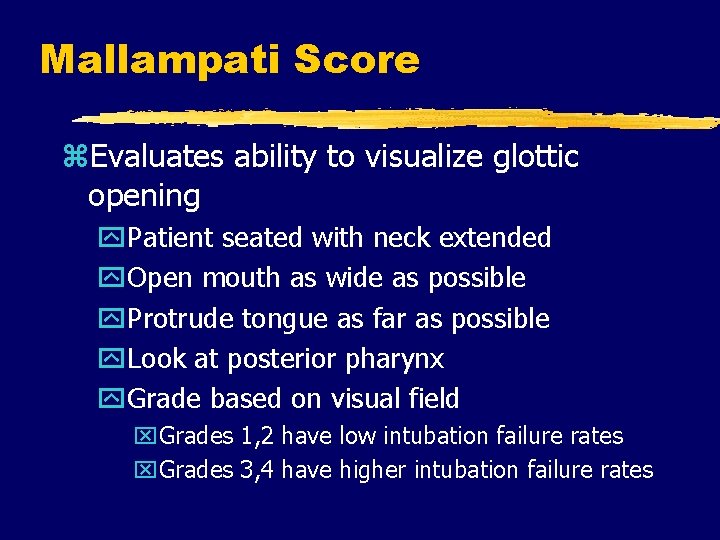
Mallampati Score z. Evaluates ability to visualize glottic opening y. Patient seated with neck extended y. Open mouth as wide as possible y. Protrude tongue as far as possible y. Look at posterior pharynx y. Grade based on visual field x. Grades 1, 2 have low intubation failure rates x. Grades 3, 4 have higher intubation failure rates
Mallampati Score z. Not useful in emergent situations z. Informal version y. Use tongue blade to visualize pharynx
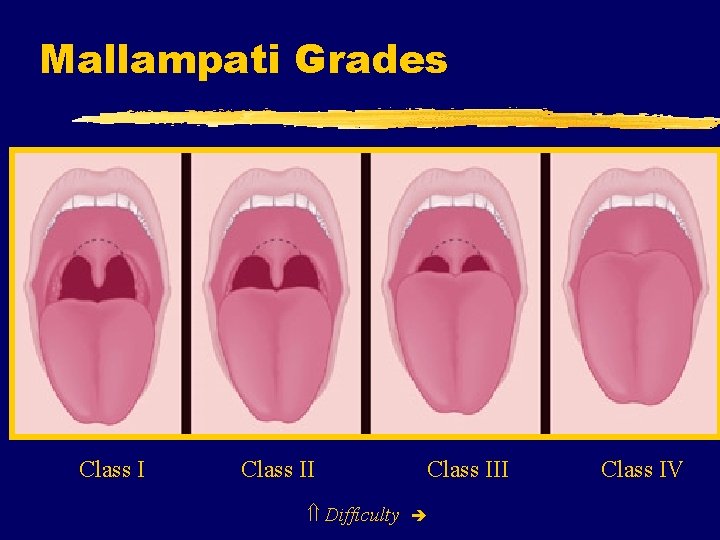
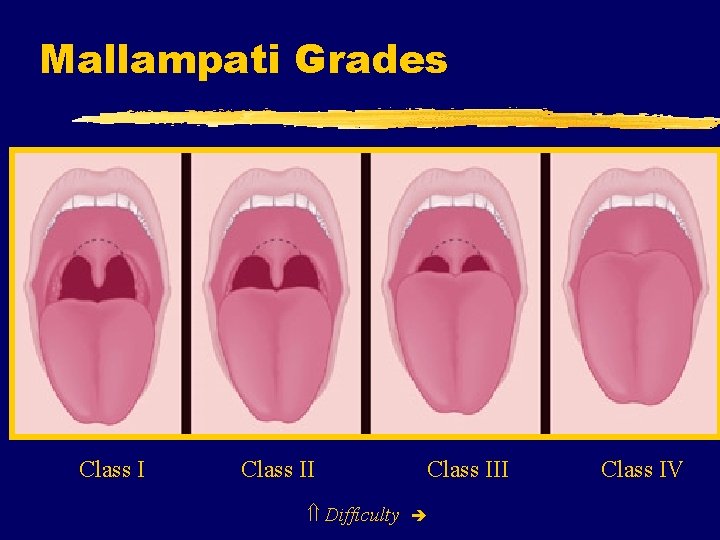
Mallampati Grades Class II Difficulty Class III Class IV
Obstruction z. Know or suspected y. Foreign bodies y. Tumors y. Abscess y. Epiglottitis y. Hematoma y. Trauma
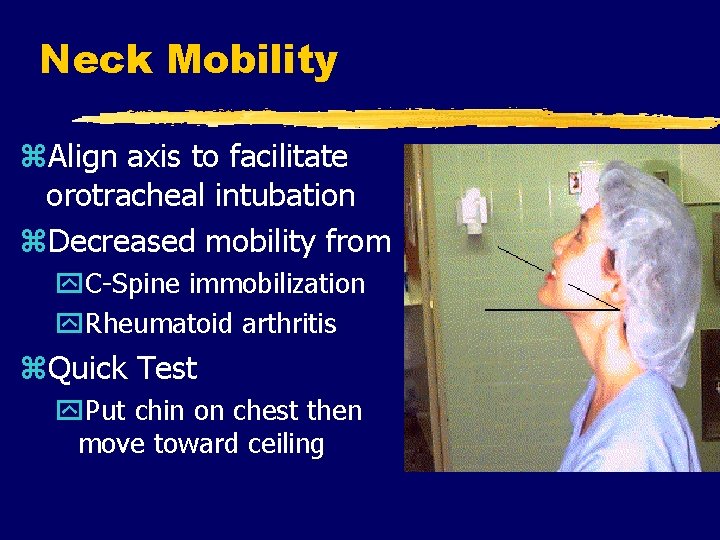
Neck Mobility z. Align axis to facilitate orotracheal intubation z. Decreased mobility from y. C-Spine immobilization y. Rheumatoid arthritis z. Quick Test y. Put chin on chest then move toward ceiling
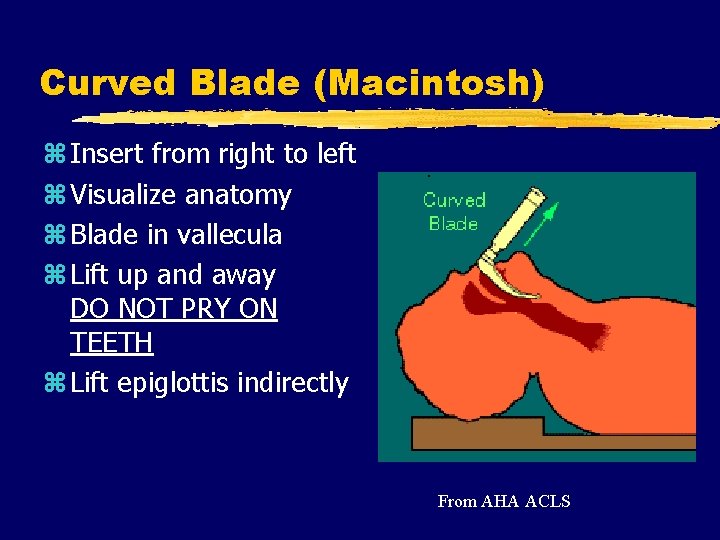
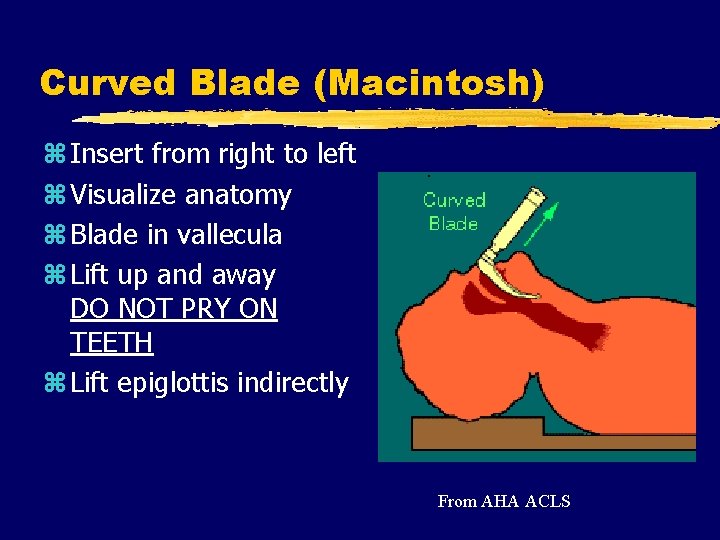
Curved Blade (Macintosh) z Insert from right to left z Visualize anatomy z Blade in vallecula z Lift up and away DO NOT PRY ON TEETH z Lift epiglottis indirectly From AHA ACLS
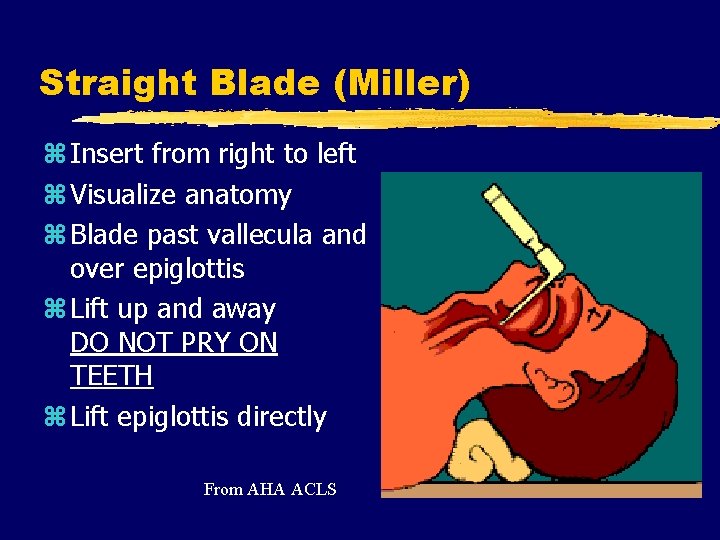
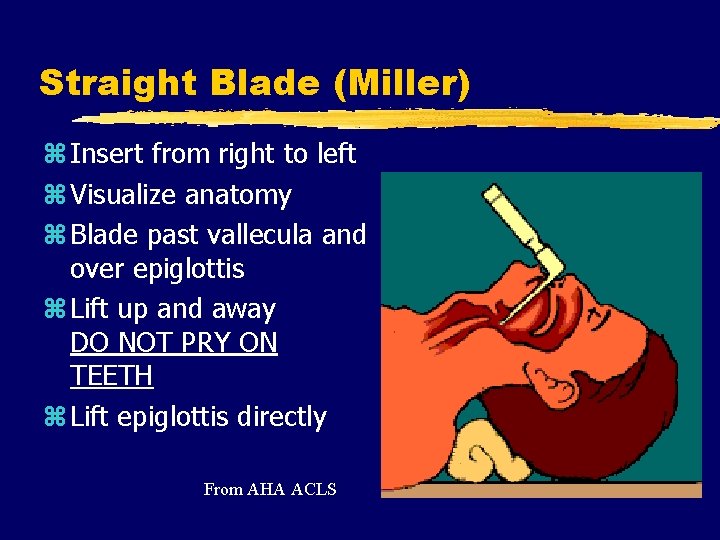
Straight Blade (Miller) z Insert from right to left z Visualize anatomy z Blade past vallecula and over epiglottis z Lift up and away DO NOT PRY ON TEETH z Lift epiglottis directly From AHA ACLS
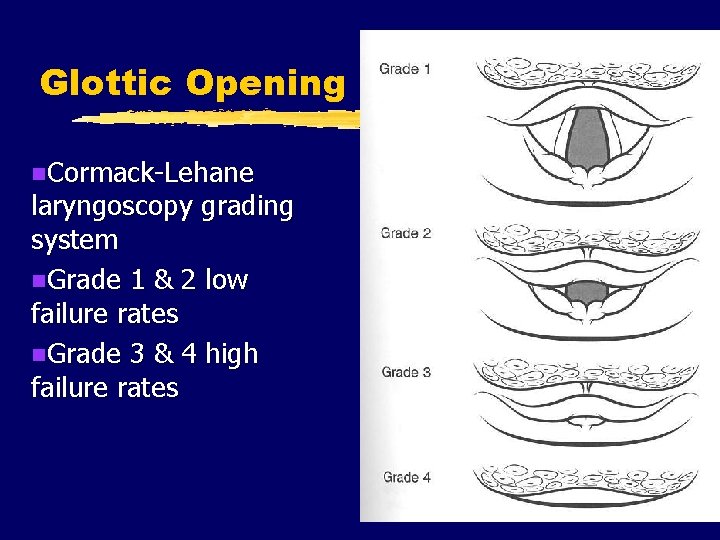
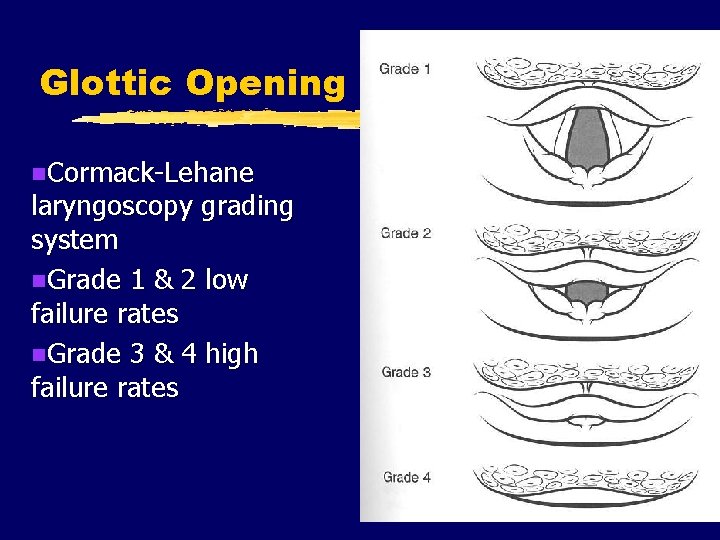
Glottic Opening n. Cormack-Lehane laryngoscopy grading system n. Grade 1 & 2 low failure rates n. Grade 3 & 4 high failure rates

Tube Placement From TRIPP, CPEM
Confirmation of Placement
Placement of the ETT within the esophagus is an accepted complication. However, failure to recognize and correct is not!
Traditional Methods z. Observation of ETT passing through vocal cords. z. Presence of breath sounds z. Absence of epigastric sounds z. Symmetric rise and fall of chest z. Condensation in ETT z. Chest Radiograph
All of these methods have failed in the clinical setting
Additional Methods z. Pulse Oximetry z. Aspiration Techniques z. End Tidal CO 2
Confirming ETT Location z. Fail Safe z. Near Fail Safe z. Non-Fail Safe
Fail Safe z. Improvement in Clinical Signs z. ETT visualized between vocal cords z. Fiberoptic visualization of y. Cartilaginous rings y. Carina

Near Failsafe z. CO 2 detection z. Rapid inflation of EDD
Non-Failsafe z. Presence of breath sounds z. Absence of epigastric sounds z. Absence of gastric distention z. Chest Rise and Fall z. Large Spontaneous Exhaled Tidal Volumes
Non Failsafe z. Condensation in tube disappearing and reappearing with respiration z. Air exiting tube with chest compression z. Bag Valve Mask having the appropriate compliance z. Pressure on suprasternal notch associated with pilot balloon pressure

ALS Airway/Ventilation Methods z. Blind Nasotracheal Intubation y. Position, oxygenate patient y. Monitor patient x. ECG monitor x. Pulse oximeter
ALS Airway/Ventilation Methods z. Blind Nasotracheal Intubation y. Assess for difficulty or contraindication x. Mid-face fractures x. Possible basilar skull fracture x. Evidence of nasal obstruction, septal deviation y. Assemble, check equipment x. Lubricate end of tube; do not warm x. Attach BAAM (if available)
ALS Airway/Ventilation Methods z. Blind Nasotracheal Intubation y. Position patient (preferably sitting upright) y. Insert tube into largest nare y. Advance slowly, but steadily y. Listen for sound of air movement in tube or whistle via BAAM y. Advance tube y. Assess placement y. Inflate cuff, reassess placement y. Secure, reassess placement

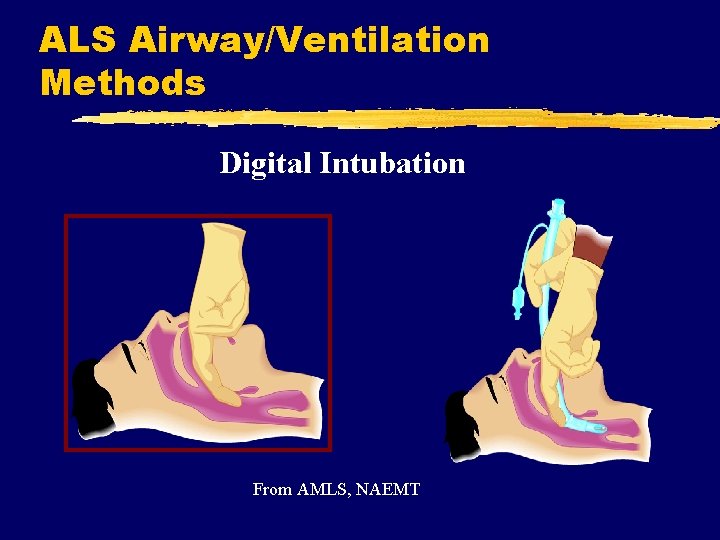
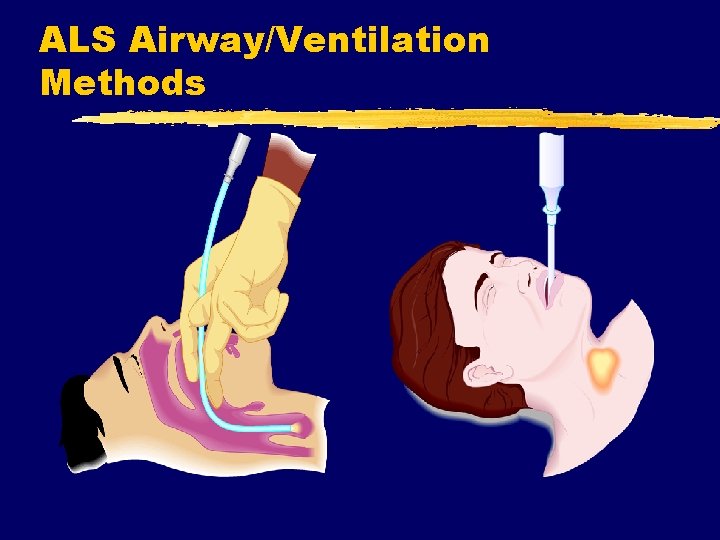
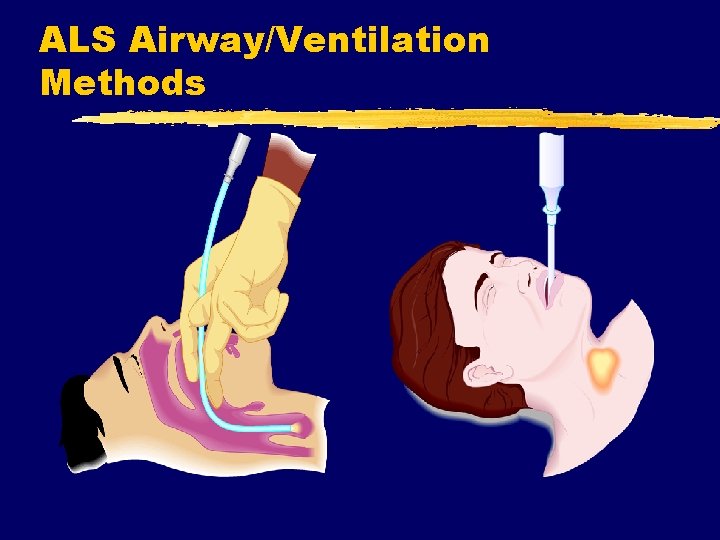
ALS Airway/Ventilation Methods z. Digital Intubation y. Blind technique y. Variable probability of success y. Using middle finger to locate epiglottis y. Lift epiglottis y. Slide lubricated tube along index finger y. Assess tube placement/depth as with orotracheal intubation
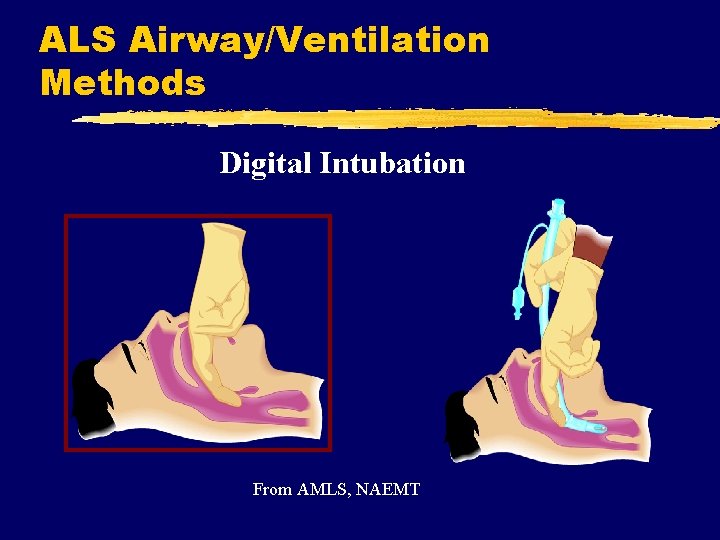
ALS Airway/Ventilation Methods Digital Intubation From AMLS, NAEMT
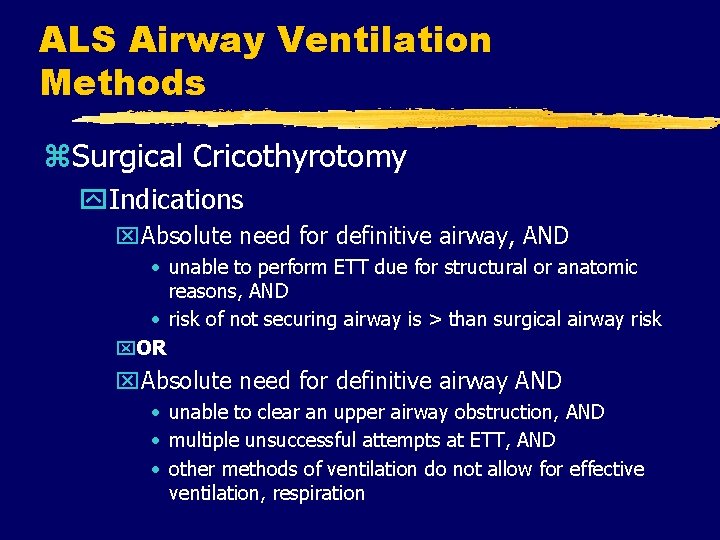
ALS Airway Ventilation Methods z. Surgical Cricothyrotomy y. Indications x. Absolute need for definitive airway, AND • unable to perform ETT due for structural or anatomic reasons, AND • risk of not securing airway is > than surgical airway risk x. OR x. Absolute need for definitive airway AND • unable to clear an upper airway obstruction, AND • multiple unsuccessful attempts at ETT, AND • other methods of ventilation do not allow for effective ventilation, respiration

ALS Airway/Ventilation Methods z. Surgical Cricothyrotomy y. Contraindications (relative) x. No real demonstrated indication x. Risks > Benefits x. Age < 8 years (some say 10, some say 12) x. Evidence of fractured larynx or cricoid cartilage x. Evidence of tracheal transection
ALS Airway/Ventilation Methods z. Surgical Cricothyrotomy y. Tips x. Know anatomy x. Short incision, avoid inferior trachea x. Incise, do not saw x. Work quickly x. Nothing comes out until something else is in x. Have a plan x. Be prepared with backup plan
ALS Airway/Ventilation Methods z. Needle Cricothyrotomy/Transtracheal Jet Ventilation y. Indications x. Same as surgical cricothyrotomy with x. Contraindication for surgical cricothyrotomy y. Contraindications x. None when demonstrated need x. Caution with tracheal transection

ALS Airway/Ventilation Methods z Jet Ventilation y. Usually requires highpressure equipment y. Ventilate 1 sec then allow 3 -5 sec pause y. Hypercarbia likely y. Temporary: 20 -30 mins y. High risk for barotrauma
ALS Airway/ Ventilation Methods z. Alternative Airways y. Multi-Lumen Devices (Combi. Tube, PTLA) y. Laryngeal Mask Airway (LMA) y. Esophageal Obturator Airways (EOA, EGTA) y. Lighted Stylets
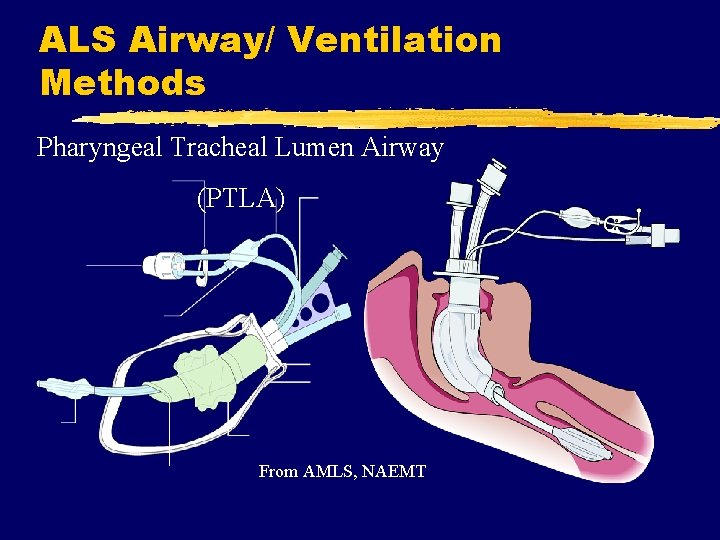
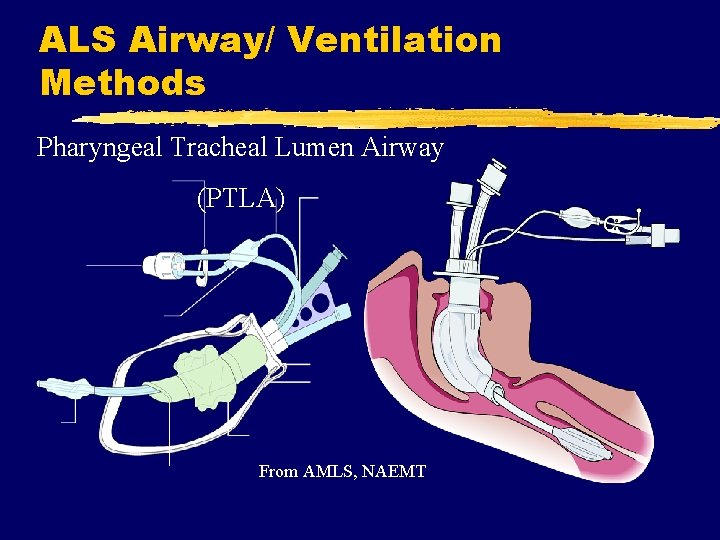
ALS Airway/ Ventilation Methods Pharyngeal Tracheal Lumen Airway (PTLA) From AMLS, NAEMT
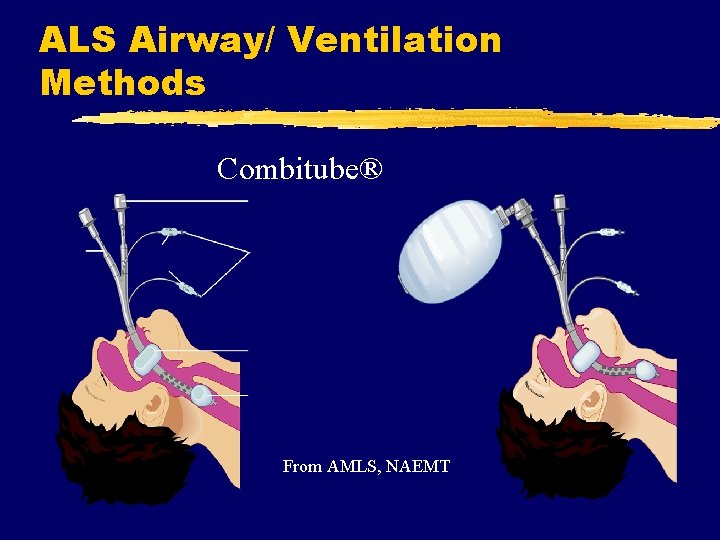
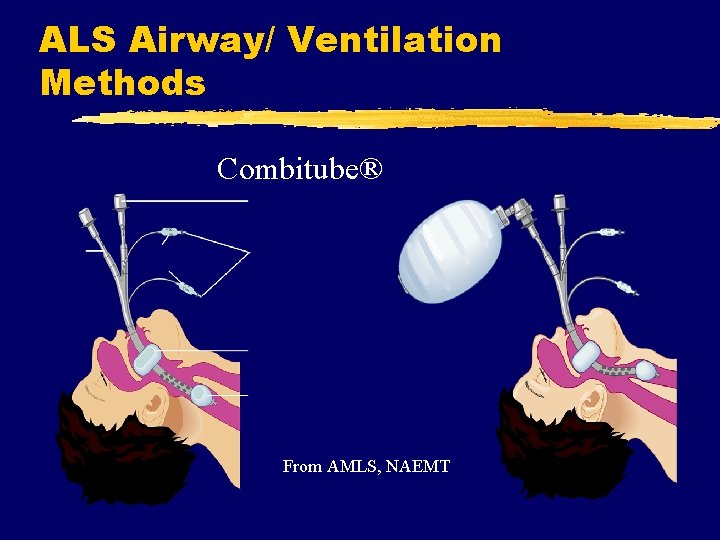
ALS Airway/ Ventilation Methods Combitube® From AMLS, NAEMT
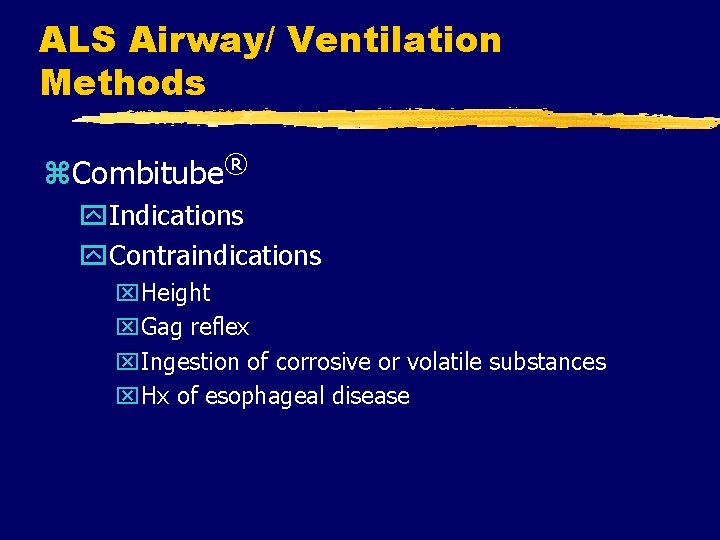
ALS Airway/ Ventilation Methods z. Combitube® y. Indications y. Contraindications x. Height x. Gag reflex x. Ingestion of corrosive or volatile substances x. Hx of esophageal disease
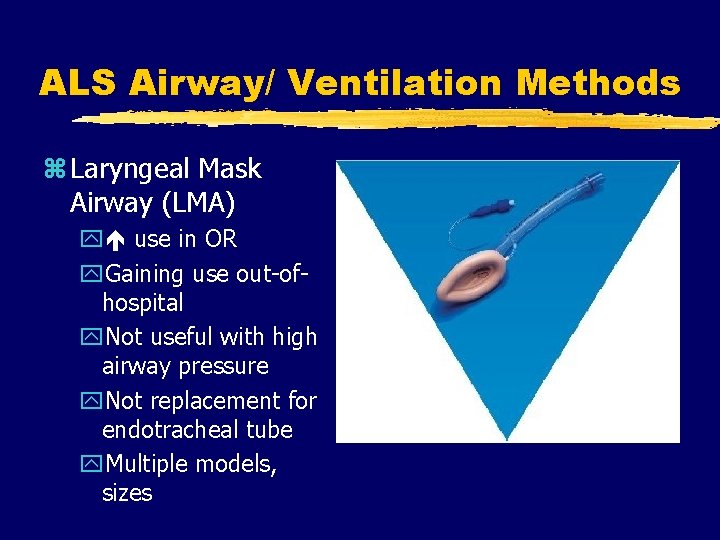
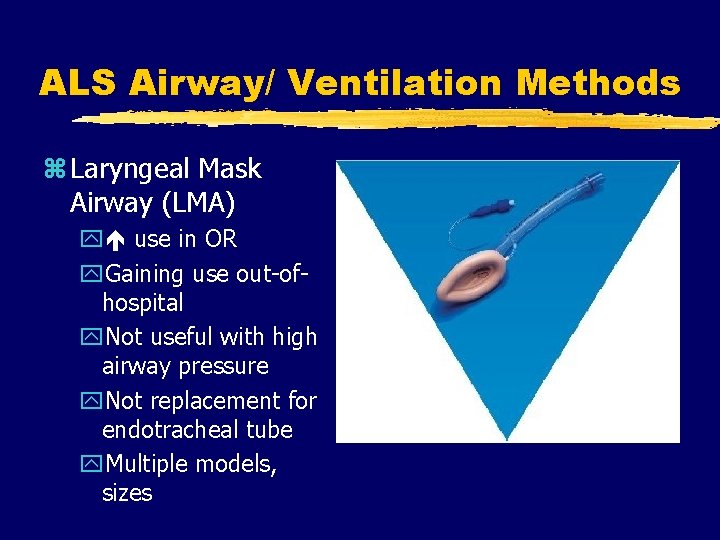
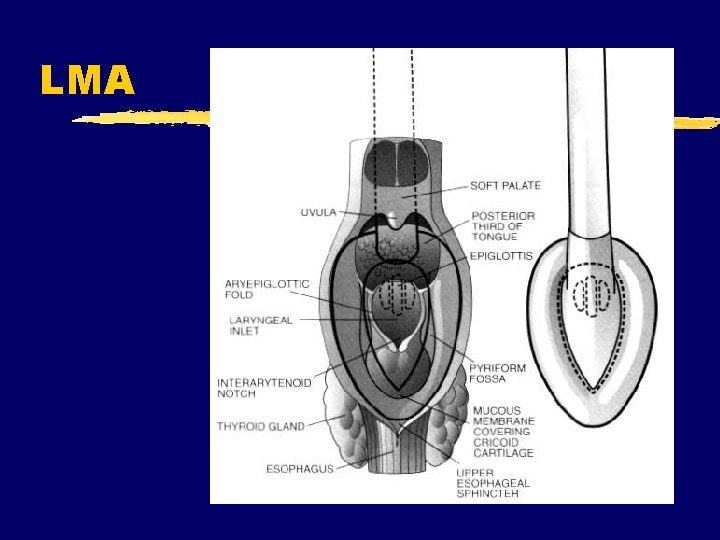
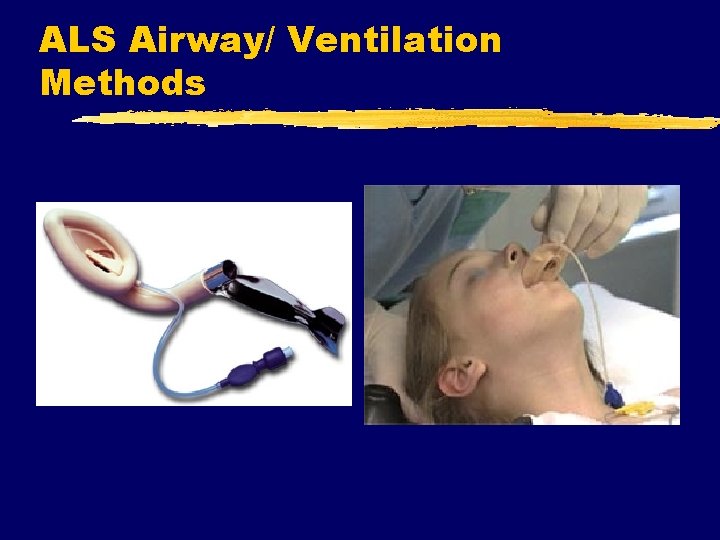
ALS Airway/ Ventilation Methods z Laryngeal Mask Airway (LMA) y use in OR y. Gaining use out-ofhospital y. Not useful with high airway pressure y. Not replacement for endotracheal tube y. Multiple models, sizes
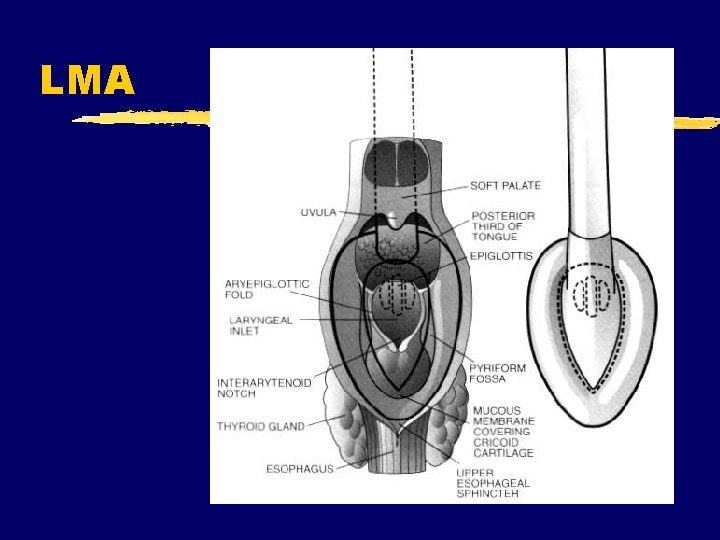
LMA
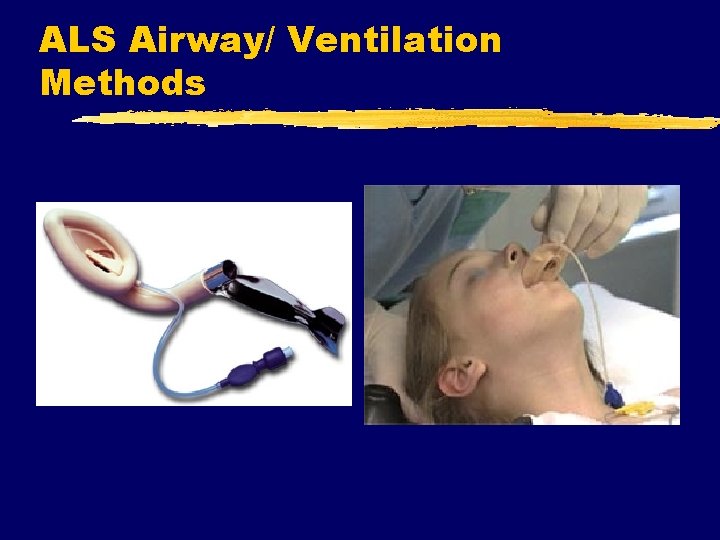
ALS Airway/ Ventilation Methods
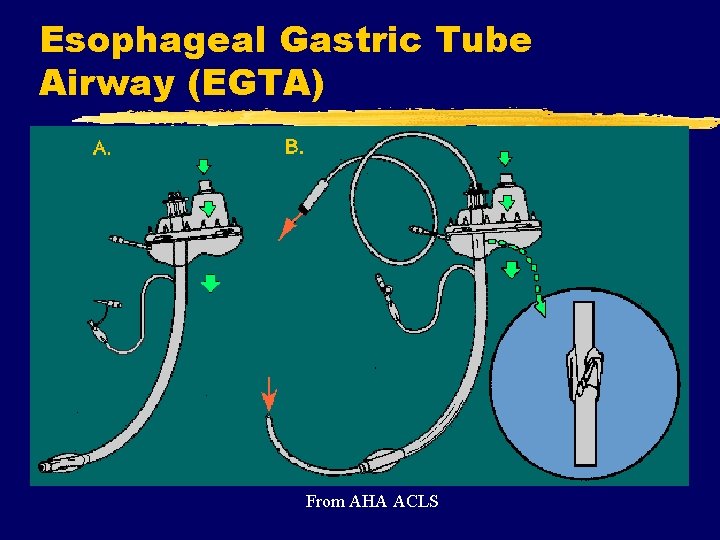
BLS & ALS Airway/ Ventilation Methods z. Esophageal Obturator Airway, Esophageal Gastric Tube Airway y. Used less frequently today y. Increased complication rate y. Significant contraindications x. Patient height x. Caustic ingestion x. Esophageal/liver disease y. Better alternative airways are now available
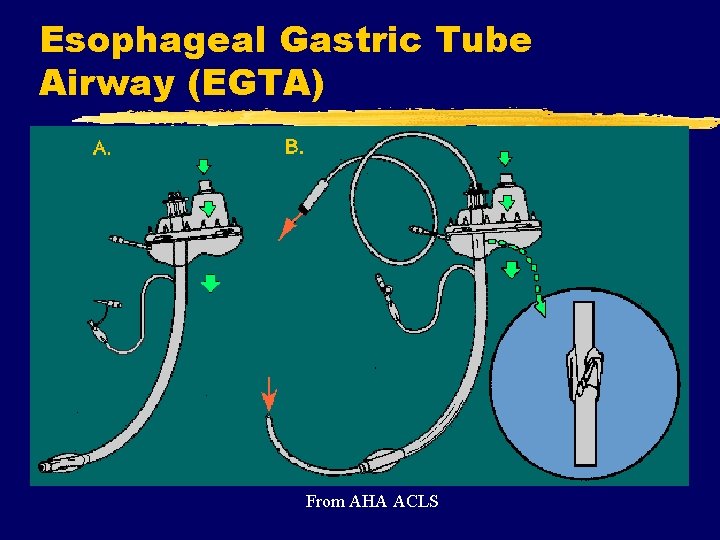
Esophageal Gastric Tube Airway (EGTA) From AHA ACLS
ALS Airway/ Ventilation Methods z. Lighted Stylette y. Not yet widely used y. Expensive y. Another method of visual feedback about placement in trachea

Lighted Slyest
ALS Airway/Ventilation Methods
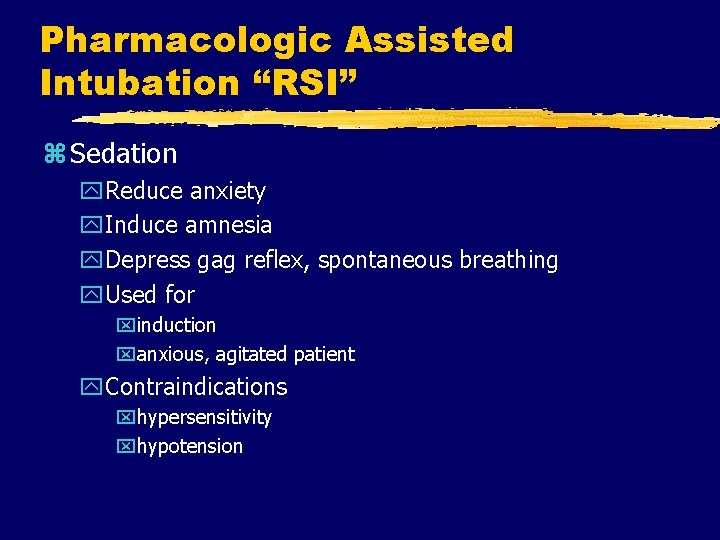
Pharmacologic Assisted Intubation “RSI” z Sedation y. Reduce anxiety y. Induce amnesia y. Depress gag reflex, spontaneous breathing y. Used for xinduction xanxious, agitated patient y. Contraindications xhypersensitivity xhypotension
Pharmacologic Assisted Intubation “RSI” z. Common Medications for Sedation y. Benzodiazepines (diazepam, midazolam) y. Narcotics (fentanyl) y. Anesthesia Induction Agents x. Etomidate x. Ketamine x. Propofol (Diprivan®)
Pharmacologic Assisted Intubation z. Neuromuscular Blockade y. Temporary skeletal muscle paralysis y. Indications x. When intubation required in patient who: • is awake, • has gag reflex, or • is agitated, combative

Pharmacologic Assisted Intubation z. Neuromuscular Blockade y. Contraindications x. Most are specific to medication x. Inability to ventilate once paralysis induced y. Advantages x. Enables provider to intubate patients who otherwise would be difficult, impossible to intubate x. Minimizes patient resistance to intubation x. Reduces risk of laryngospasm
Pharmacologic Assisted Intubation z NMB Agent Mechanism of Action y. Acts at neuromuscular junction where ACh normally allows nerve impulse transmission y. Binds to nicotinic receptor sites on skeletal muscle y. Depolarizing or non-depolarizing y. Blocks further action by ACh at receptor sites y. Blocks further depolarization resulting in muscular paralysis
Pharmacologic Assisted Intubation z. Disadvantages/Potential Complications y. Does not provide sedation, amnesia y. Provider unable to intubate, ventilate after NMB y. Aspiration during procedure y. Difficult to detect motor seizure activity y. Side effects, adverse effects of specific drugs
Pharmacologic Assisted Intubation z. Common Used NMB Agents y. Depolarizing NMB agents xsuccinylcholine (Anectine®) y. Non-depolarizing NMB agents xvecuronium (Norcuron®) xrocuronium (Zemuron®) xpancuronium (Pavulon®)
Pharmacologic Assisted Intubation y. Summarized Procedure x. Prepare all equipment, medications while ventilating patient x. Hyperventilate x Administer induction/sedation agents and pretreatment meds (e. g. lidocaine or atropine) x. Administer NMB agent x. Sellick maneuver x. Intubate per usual x. Continue NMB and sedation/analgesia prn

Pharmacologic Assisted Intubation Failure is not an option!
ALS Airway/Ventilation Methods z. Needle Thoracostomy y. Indications x. Positive signs/symptoms of tension pneumothorax x. Cardiac arrest with PEA or asystole with possible tension pneumothorax y. Contraindications x. Absence of indications
ALS Airway/Ventilation Methods z. Tension Pneumothorax Signs/Symptoms y. Severe respiratory distress y or absent lung sounds (usually unilateral) y resistance to manual ventilation y. Cardiovascular collapse (shock) y. Asymmetric chest expansion y. Anxiety, restlessness or cyanosis (late) y. JVD or tracheal deviation (late)
ALS Airway/Ventilation Methods z Needle Thoracostomy y. Prepare equipment x. Large bore angiocath y. Locate landmarks: 2 nd intercostal space at midclavicular line y. Insert catheter through chest wall into pleural space over top of 3 rd rib (blood vessels, nerves follow inferior rib margin) y. Withdraw needle, secure catheter like impaled object
ALS Airway/Ventilation Methods z. Chest Escharotomy y. Indications x. Presence of severe edema to soft tissue of thorax as with circumferential burns xinability to maintain adequate tidal volume, chest expansion even with assisted ventilation y. Considerations x. Must rule out upper airway obstruction x. Rarely needed
ALS Airway/Ventilation Methods z. Chest Escharotomy y. Procedure x. Intubate if not already done x. Prepare site, equipment x. Vertical incision to anterior axillary line x. Horizontal incision only if necessary x. Cover, protect
Airway & Ventilation Methods z Saturday’s class y. Practice using equipment xorotracheal intubation xnasotracheal intubation xgastric tube insertion xsurgical airways xneedle thoracostomy xcombitube xretrograde intubation
 Epiglottic
Epiglottic Akından akına şiiri
Akından akına şiiri Sevgili anneciğim noktalama işareti
Sevgili anneciğim noktalama işareti Mumtaz baby food
Mumtaz baby food Negotiation
Negotiation Iqra mumtaz
Iqra mumtaz Mumtaz awan
Mumtaz awan Airway management acls
Airway management acls Chapter 10 airway management
Chapter 10 airway management Supraglotal
Supraglotal Chapter 9 airway management
Chapter 9 airway management Airway abcde
Airway abcde Sandwich manuver adalah
Sandwich manuver adalah Stepwise airway management
Stepwise airway management Cricothyroidotomy
Cricothyroidotomy Upper respiratory system labeled
Upper respiratory system labeled Mechanism of respiration class 10
Mechanism of respiration class 10 Respiratory airway secretary
Respiratory airway secretary Intubation anatomy
Intubation anatomy Intubation view grade
Intubation view grade Jarak thyromental adalah
Jarak thyromental adalah Servo pressure on jet ventilator
Servo pressure on jet ventilator What is gag reflex
What is gag reflex Mean airway pressure
Mean airway pressure Hava yolu anatomisi
Hava yolu anatomisi Vareculla
Vareculla Retroglottic airway
Retroglottic airway Pharyngo-tracheal lumen airway
Pharyngo-tracheal lumen airway Mean airway pressure formula
Mean airway pressure formula Automatic positive airway pressure
Automatic positive airway pressure Push hard push fast fully recoil
Push hard push fast fully recoil Airway numaraları
Airway numaraları Asa airway classification
Asa airway classification Aprv indications
Aprv indications What is this picture from
What is this picture from Pharyngo-tracheal lumen airway
Pharyngo-tracheal lumen airway Rae
Rae Sniffing position intubation
Sniffing position intubation Actual diagnosis
Actual diagnosis Indications for artificial airway
Indications for artificial airway Three emergency action steps
Three emergency action steps Airway gym
Airway gym Airway breathing c
Airway breathing c Ideal dat
Ideal dat Norwich terrier upper airway syndrome
Norwich terrier upper airway syndrome Moans airway
Moans airway Asa airway
Asa airway Generations of supraglottic airway devices
Generations of supraglottic airway devices Nasopharyngeal airway
Nasopharyngeal airway Nasopharyngeal airway
Nasopharyngeal airway Diagram of alveolus
Diagram of alveolus Difficult airway algorithm asa
Difficult airway algorithm asa Mouth gag airway
Mouth gag airway Open a casualty's airway
Open a casualty's airway Abcde methode ehbo
Abcde methode ehbo Thyromental distance of 7cm
Thyromental distance of 7cm Classroom.cloud
Classroom.cloud Noratbj
Noratbj Definitive airway
Definitive airway Part whole model subtraction
Part whole model subtraction Unit ratio definition
Unit ratio definition Part part whole
Part part whole Technical description examples
Technical description examples Bar layout
Bar layout The phase of the moon you see depends on ______.
The phase of the moon you see depends on ______. 미니탭 gage r&r 해석
미니탭 gage r&r 해석 Scientific management
Scientific management Management pyramid
Management pyramid Top level management
Top level management Prof. dr. marcus eckert
Prof. dr. marcus eckert Agamenon roberto
Agamenon roberto Prof david toback
Prof david toback Prof dr ali hossain
Prof dr ali hossain Prof suganda
Prof suganda Prof david kipping
Prof david kipping Tracce svolte prova scritta tfa sostegno secondaria
Tracce svolte prova scritta tfa sostegno secondaria Texte incitatif exemple
Texte incitatif exemple Syzyfowe prace cechy epiki
Syzyfowe prace cechy epiki Prof. grace schneider
Prof. grace schneider Sonnet 29 edna st vincent millay poem
Sonnet 29 edna st vincent millay poem Akuisita
Akuisita Prof dr orhan canbolat
Prof dr orhan canbolat Obsatar sinaga widyatama
Obsatar sinaga widyatama Pem hastalığı
Pem hastalığı Professor mark ferguson
Professor mark ferguson Prof paolo bellioni
Prof paolo bellioni Ramlimusa
Ramlimusa Prof aris
Prof aris Brometo de ciclopentila
Brometo de ciclopentila Prof dr bilgin arda
Prof dr bilgin arda Prof dr halil ak
Prof dr halil ak