2018 Addiction Health Summit Pain and Addiction June








- Slides: 91
2018 Addiction Health Summit Pain and Addiction June 8, 2018 Michael Baron, MD, MPH, FASAM Medical Director Tennessee Medical Foundation Physician’s Health Program
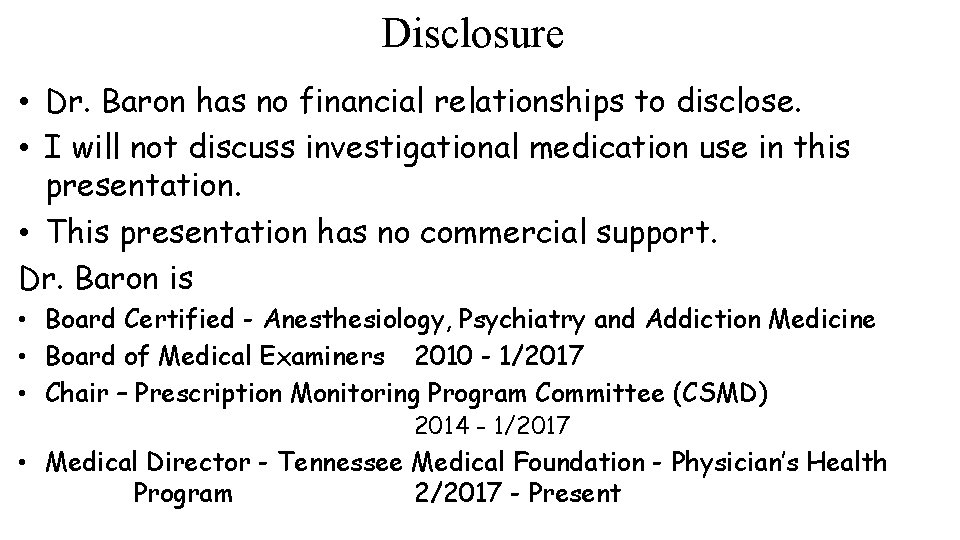
Disclosure • Dr. Baron has no financial relationships to disclose. • I will not discuss investigational medication use in this presentation. • This presentation has no commercial support. Dr. Baron is • Board Certified - Anesthesiology, Psychiatry and Addiction Medicine • Board of Medical Examiners 2010 - 1/2017 • Chair – Prescription Monitoring Program Committee (CSMD) 2014 - 1/2017 • Medical Director - Tennessee Medical Foundation - Physician’s Health Program 2/2017 - Present
Conflicts of Interest?
Objectives Review the signs and symptoms of aberrant behavior including diversion related to controlled prescription drugs. Understand best practice methods for working with patients that have addiction and for patients suspected of drug seeking or other aberrant behavior. Define and classify the types of pain. Review the different treatments that correspond to the many types of pain. 4
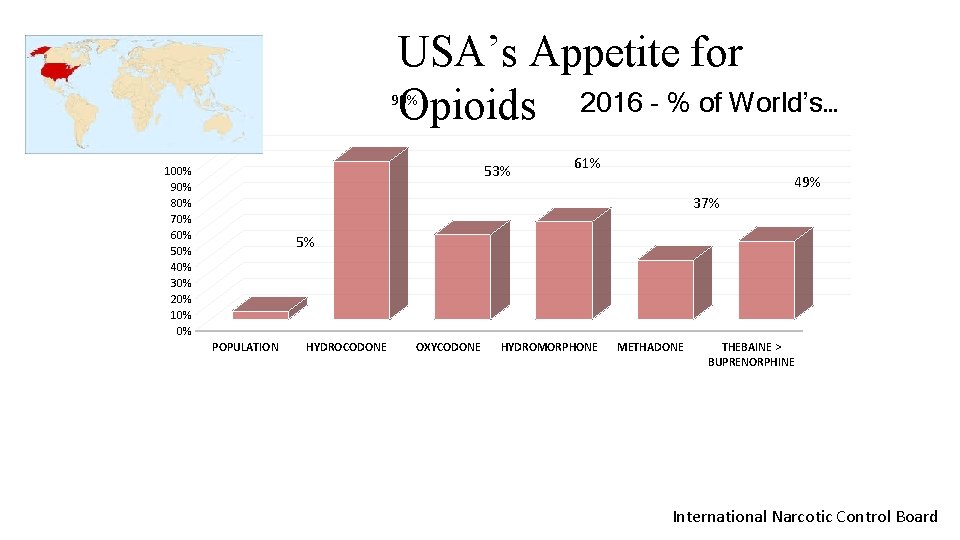
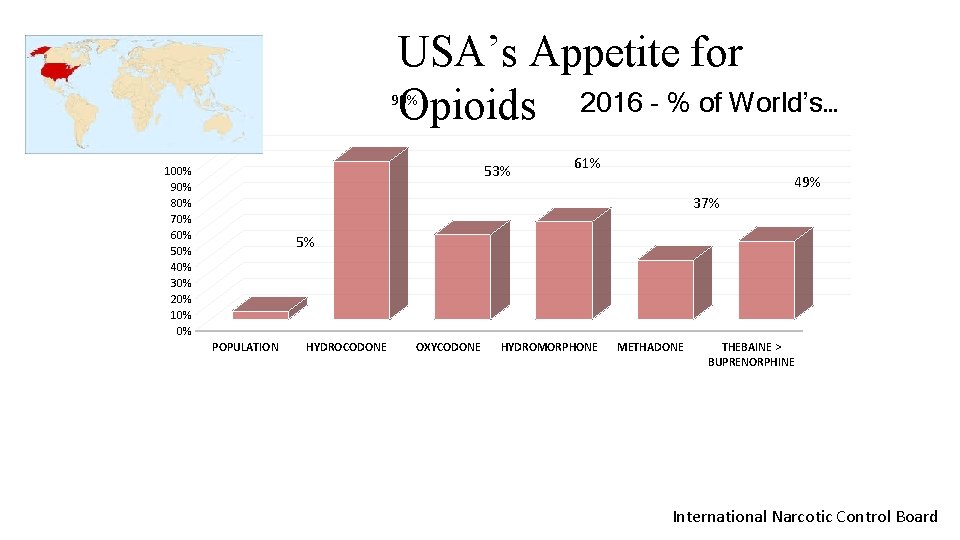
USA’s Appetite for Opioids 2016 - % of World’s… 99% 53% 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 61% 49% 37% 5% POPULATION HYDROCODONE OXYCODONE HYDROMORPHONE METHADONE THEBAINE > BUPRENORPHINE International Narcotic Control Board
Opioid Consumption ↑ 5 th Vital sign: Pain assessed in all patients: Industry promotion: Evidenced Based Medicine:
Industry Told Us Opioids are safe and effective for chronic, non-cancer pain. The risk of addiction is rare in patients. Opioid therapy can be easily discontinued.
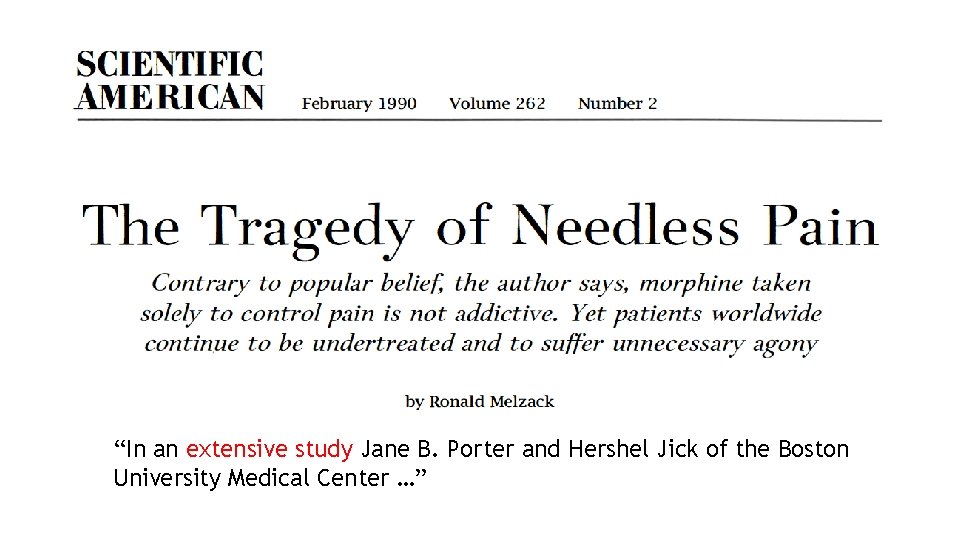
“In an extensive study Jane B. Porter and Hershel Jick of the Boston University Medical Center …”
“Many physicians now concede … an exaggerated fear that patients would become addicted. This fear, … is basically unwarranted. A landmark study, published in 1980, …”
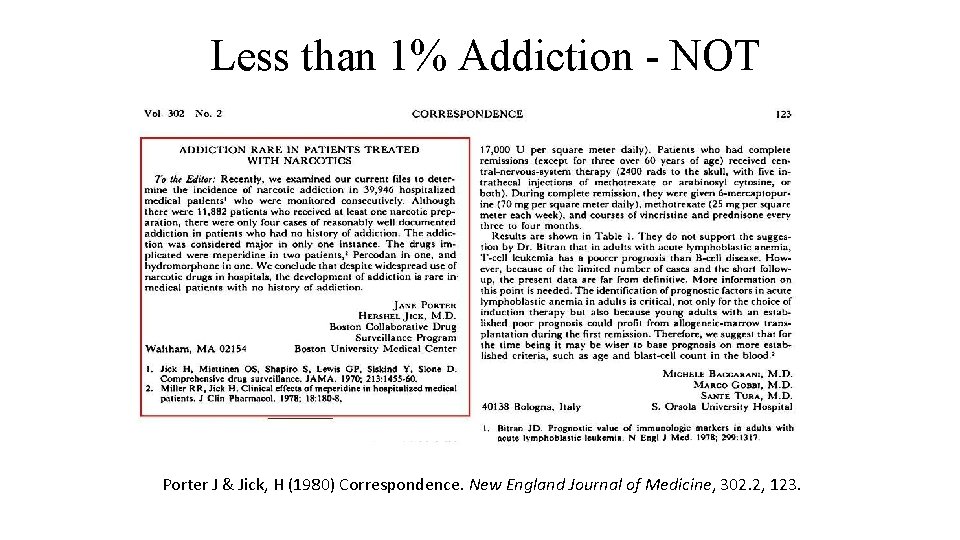
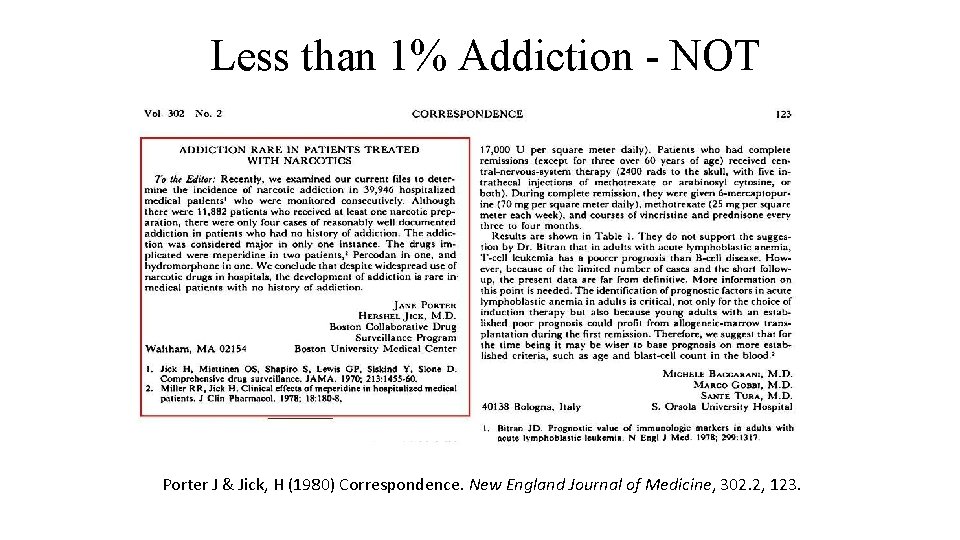
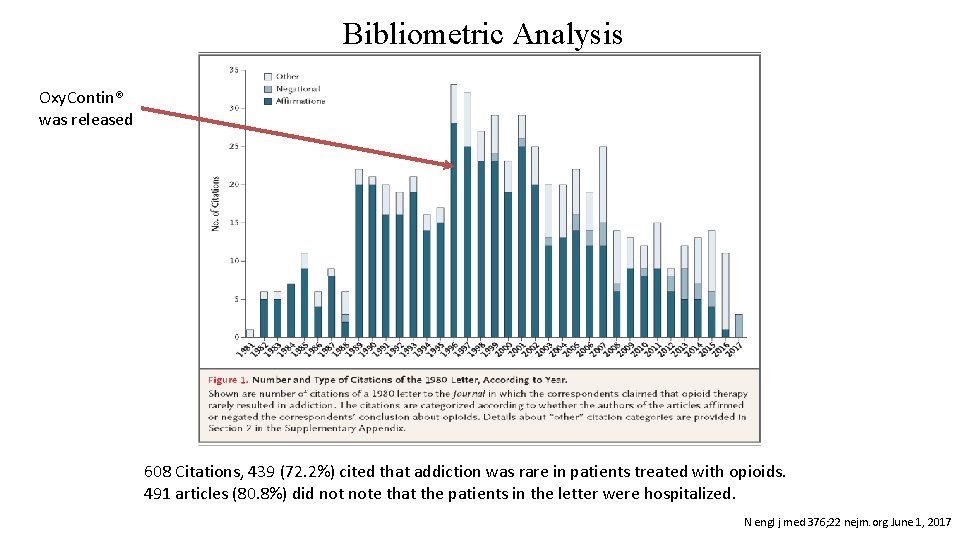
Less than 1% Addiction - NOT Porter J & Jick, H (1980) Correspondence. New England Journal of Medicine, 302. 2, 123.
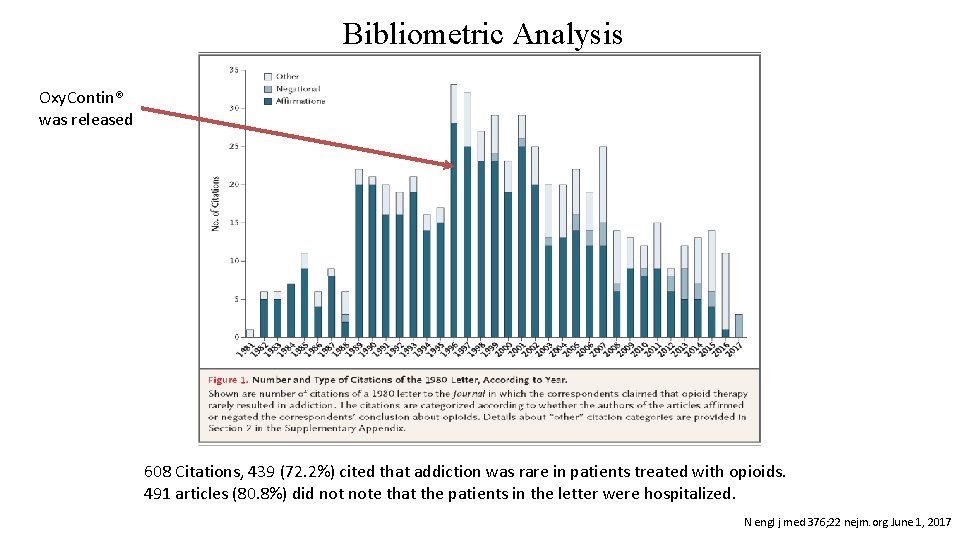
Bibliometric Analysis Oxy. Contin® was released 608 Citations, 439 (72. 2%) cited that addiction was rare in patients treated with opioids. 491 articles (80. 8%) did note that the patients in the letter were hospitalized. N engl j med 376; 22 nejm. org June 1, 2017
“Pseudoaddiction” Symptoms that appear similar to addiction such as: • Overuse of prescription opioids • Use of non prescribed opioids • Early refills Because pain was not adequately treated. A fallacy based without evidence:

Analgesic Vignette Mr. Pele comes to the E. D. after hurting his foot playing indoor soccer. He has a 5 th metatarsal mid shaft spiral fracture confirmed by X-ray. As part of the social history Mr. Pele tells the doctor that he is a recovering alcoholic with 8 years of sobriety. He is referred to an orthopedic surgeon and placed in a Bledsoe boot. He is prescribed hydrocodone/APAP, 5 mg/325 mg, # 21 and told not to worry about the narcotics, “its not alcohol. ” Mr. Pele had good pain relief from APAP 1000 mg he took prior to coming to ED.
Analgesic Vignette What are the red flags? Addiction is one disease with many faces. Patients in recovery can be inadvertently triggered by a medication that activates the reward - craving process. All scheduled medications have this potential. Iatrogenic relapse frequently occurs. He was not asked about his current pain, pain control, PMP was not checked. Mr. Pele throws out the Rx and takes APAP 1000 mg with good pain relief.
Patient with a Substance Use Disorder • Analgesic requirements are dependent on state of receovery • May need opioid analgesics • Ensure safeguards – No control over Rx – Use S. O. , sponsor or other responsible person to handle and dispense out medication. – Take as directed. – On and Off, ASAP
Pain - Definition An unpleasant sensory and emotional experience associated with actual or potential tissue damage. Pain is always subjective, always unpleasant and therefore an emotional experience. International Association for the Study of Pain
Pain - Nomenclature Allodynia: Pain due to a stimulus which does not normally provoke pain. Low threshold & Increased response Dysesthesia: Pain characterized by burning or by a distortion of the sense of touch. “MS hug” Low threshold & extreme response Hyperesthesia: Increased sensitivity to a stimulation that causes mild or no pain. Low threshold & increased response Hyperalgesia: Increased response to a stimulus which is normally painful. Increased response
Pain - Nomenclature Analgesia: Absence of pain response to stimulation which would normally be painful. No response Hypoalgesia: Diminished pain response to a normally painful stimulus. Lowered response
Pain - Treatment Goals Improve quality of life: • Improve Function Reduce and control pain • Not eliminate pain Functional Restoration • Ability to work, volunteer, be a productive person.
Pain - Assessment • Location – Use an anatomic drawing • Intensity - (0 -10)… • Quality – aching, cramping, throbbing, shooting, burning… • Duration - onset, how long, constant, change… • Frequency – Occurrence, breakthrough… • Radiation – migration or path of pain • Alleviating and worsening triggers – Cold, hot, barometric pressure • Pain Behaviors – grimacing, crying, bracing, tense, restless… • Psychological impact - anxiety, depression, sleep…
Pain – General Management Empower and enable patients and families to control their course to the greatest extent possible. • Ask about pain regularly, assess pain systematically • Listen to the patient and family, what exacerbates and what relieves the pain. • Choose pain control options appropriately for the patient, family and setting. • Deliver interventions in a timely manner

Choose treatment options that are appropriate for the patient.
Pain - Categories Acute: The pain is expected to be over soon, but it can last seconds, weeks or longer. Chronic: The pain lasts beyond the healing of the causative injury and continues for several months. Commonly pain lasting > 3 months.
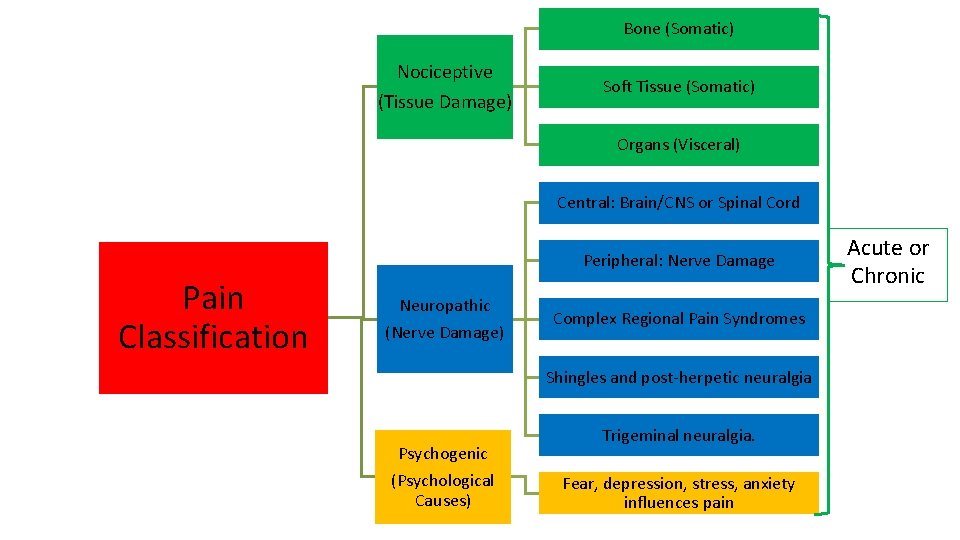
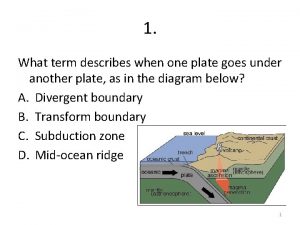
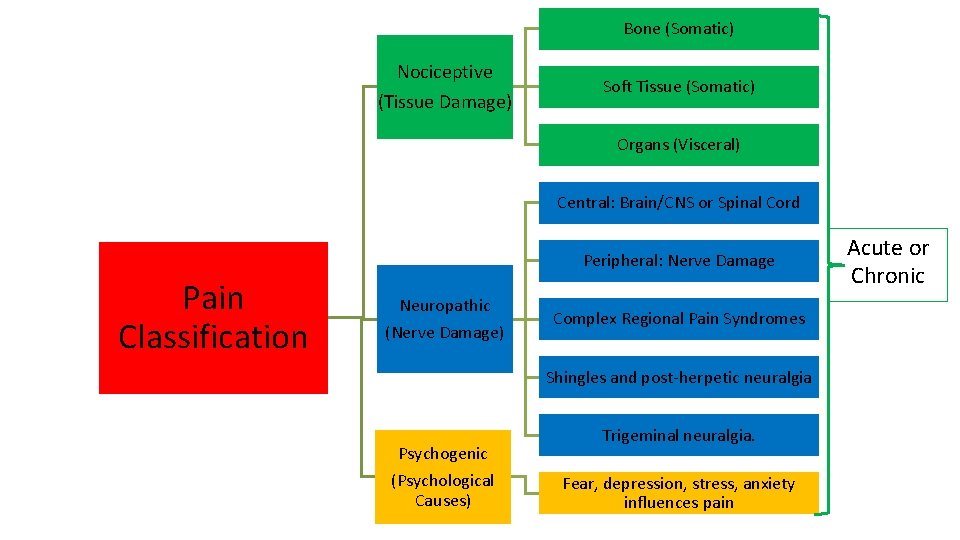
Bone (Somatic) Nociceptive (Tissue Damage) Soft Tissue (Somatic) Organs (Visceral) Central: Brain/CNS or Spinal Cord Peripheral: Nerve Damage Pain Classification Neuropathic (Nerve Damage) Complex Regional Pain Syndromes Shingles and post-herpetic neuralgia Psychogenic (Psychological Causes) Trigeminal neuralgia. Fear, depression, stress, anxiety influences pain Acute or Chronic
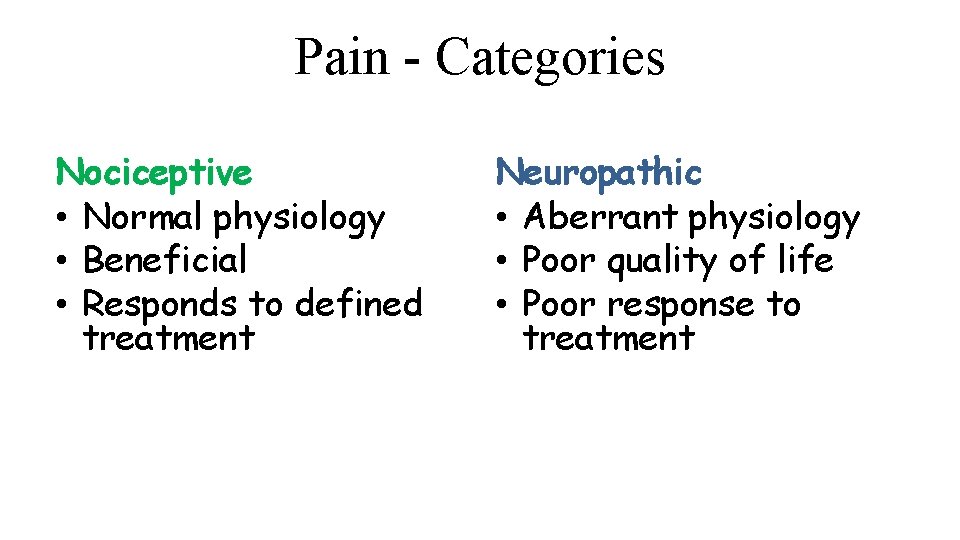
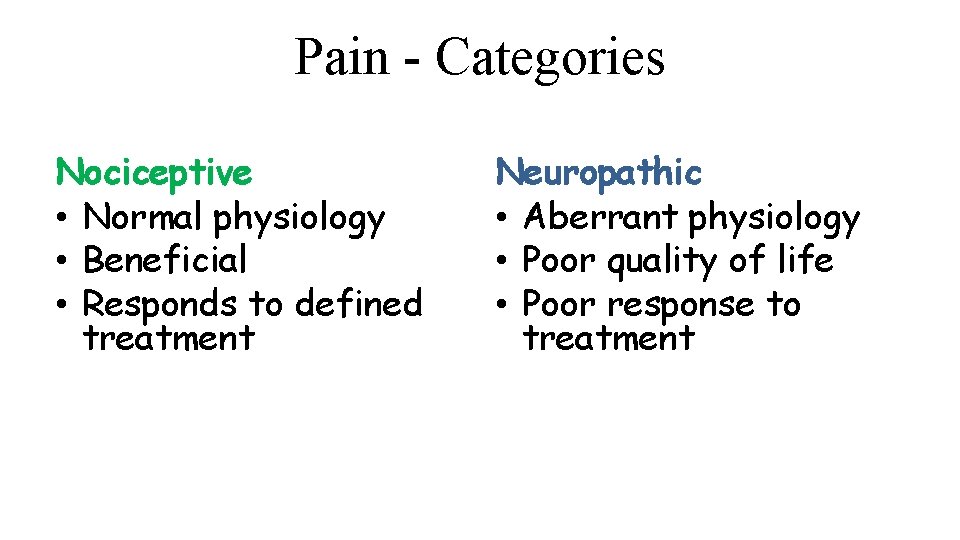
Pain - Categories Nociceptive • Normal physiology • Beneficial • Responds to defined treatment Neuropathic • Aberrant physiology • Poor quality of life • Poor response to treatment
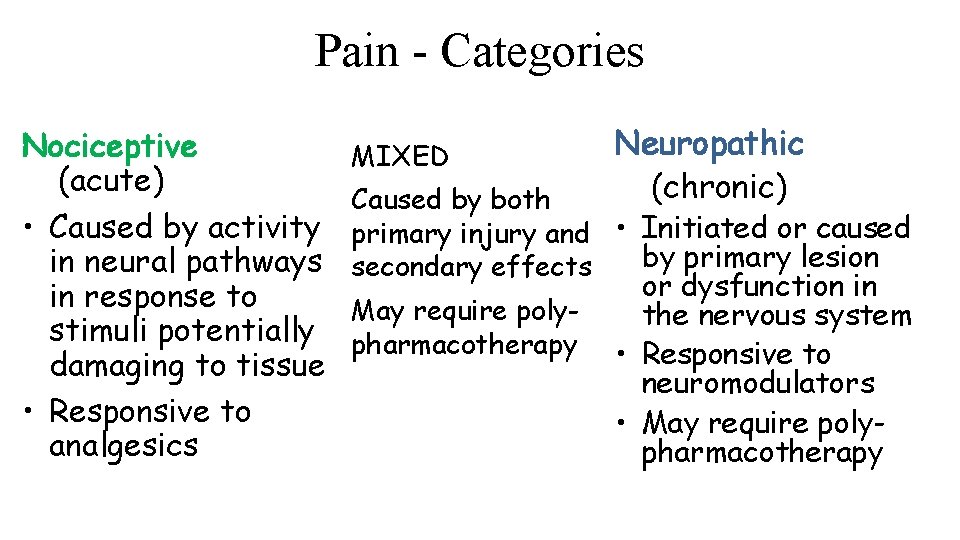
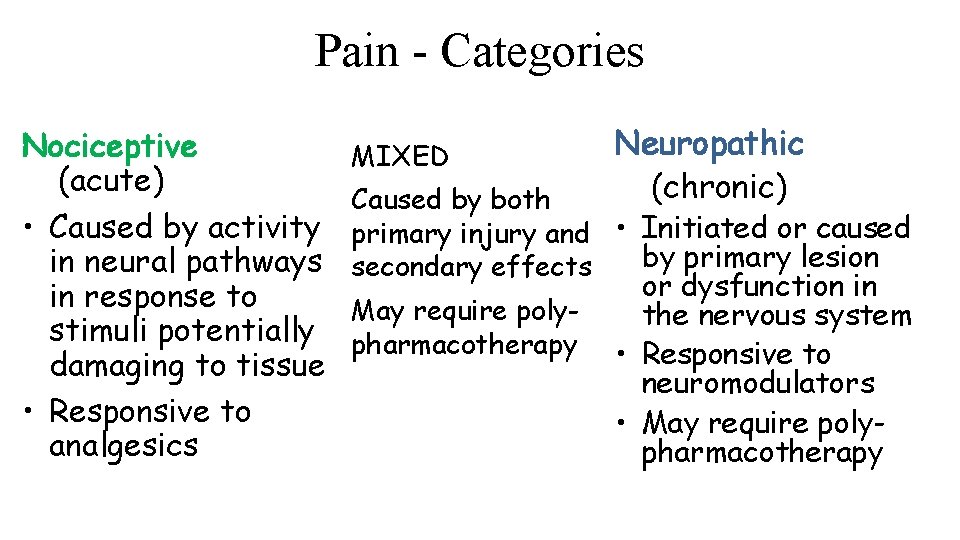
Pain - Categories Nociceptive (acute) • Caused by activity in neural pathways in response to stimuli potentially damaging to tissue • Responsive to analgesics MIXED Neuropathic (chronic) Caused by both primary injury and • Initiated or caused by primary lesion secondary effects May require polypharmacotherapy or dysfunction in the nervous system • Responsive to neuromodulators • May require polypharmacotherapy
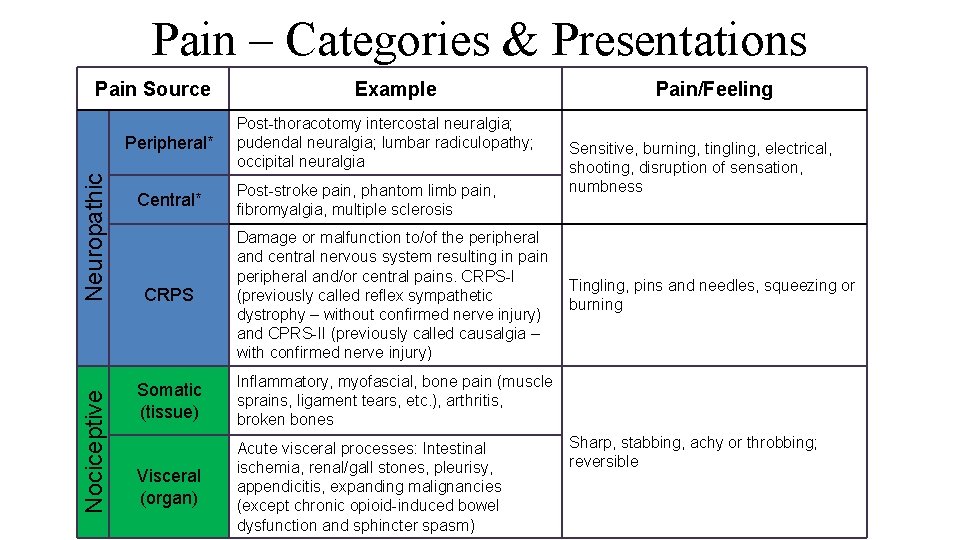
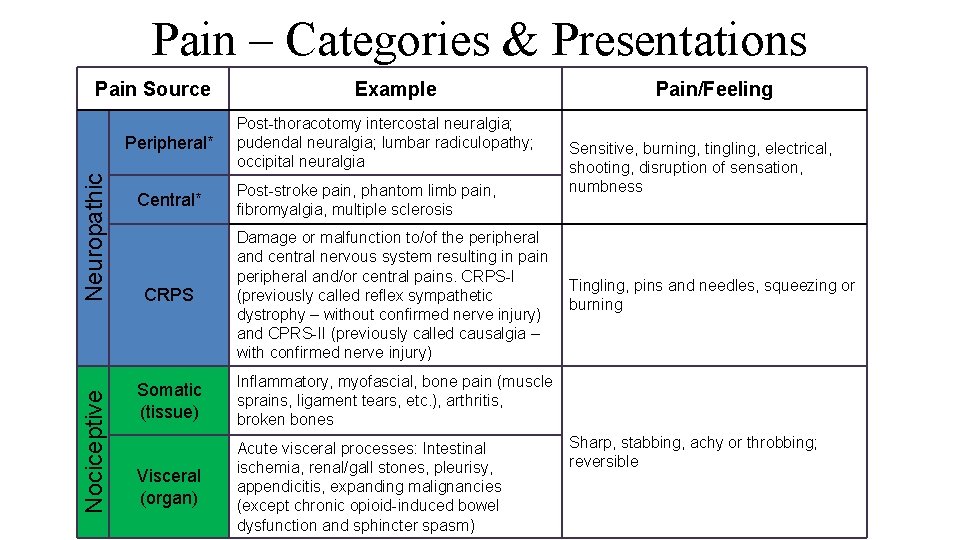
Pain – Categories & Presentations Pain Source Nociceptive Neuropathic Peripheral* Central* Example Post-thoracotomy intercostal neuralgia; pudendal neuralgia; lumbar radiculopathy; occipital neuralgia Post-stroke pain, phantom limb pain, fibromyalgia, multiple sclerosis CRPS Damage or malfunction to/of the peripheral and central nervous system resulting in pain peripheral and/or central pains. CRPS-I (previously called reflex sympathetic dystrophy – without confirmed nerve injury) and CPRS-II (previously called causalgia – with confirmed nerve injury) Somatic (tissue) Inflammatory, myofascial, bone pain (muscle sprains, ligament tears, etc. ), arthritis, broken bones Visceral (organ) Acute visceral processes: Intestinal ischemia, renal/gall stones, pleurisy, appendicitis, expanding malignancies (except chronic opioid-induced bowel dysfunction and sphincter spasm) Pain/Feeling Sensitive, burning, tingling, electrical, shooting, disruption of sensation, numbness Tingling, pins and needles, squeezing or burning Sharp, stabbing, achy or throbbing; reversible
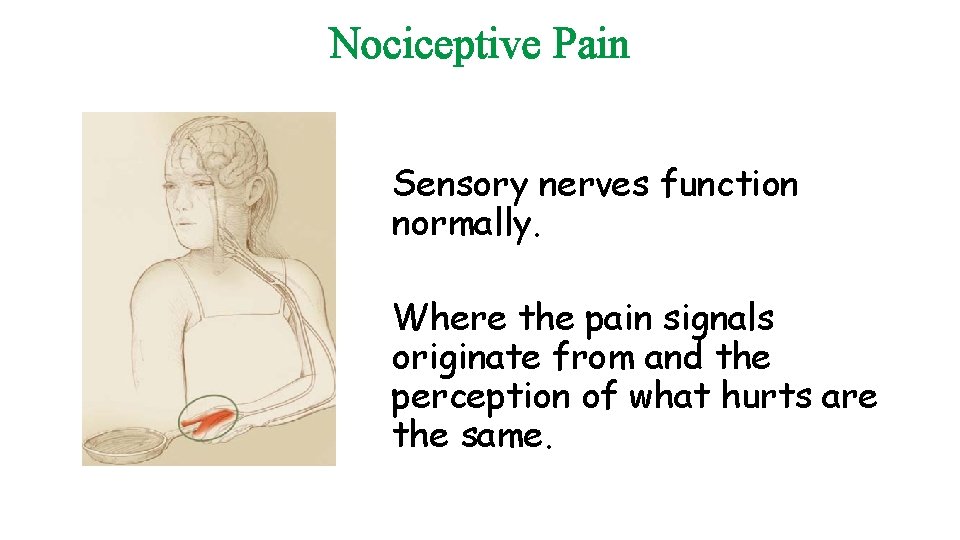
Nociceptive Pain Sensory nerves function normally. Where the pain signals originate from and the perception of what hurts are the same.
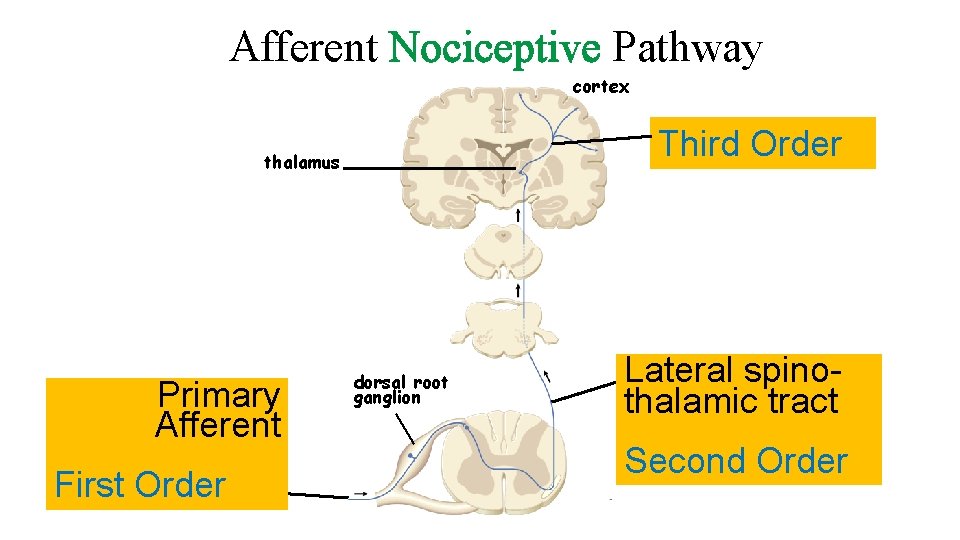
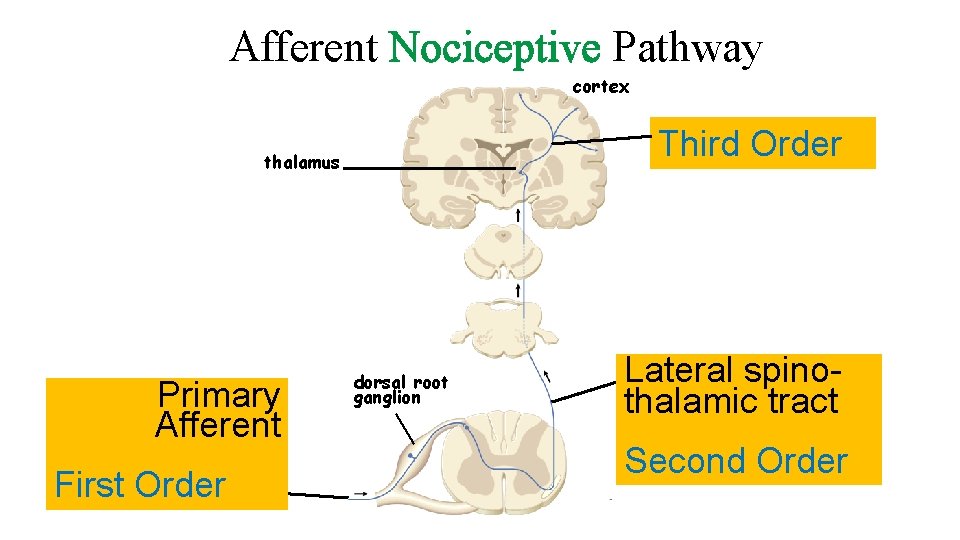
Afferent Nociceptive Pathway cortex Third Order thalamus Primary Afferent First Order dorsal root ganglion Lateral spinothalamic tract Second Order
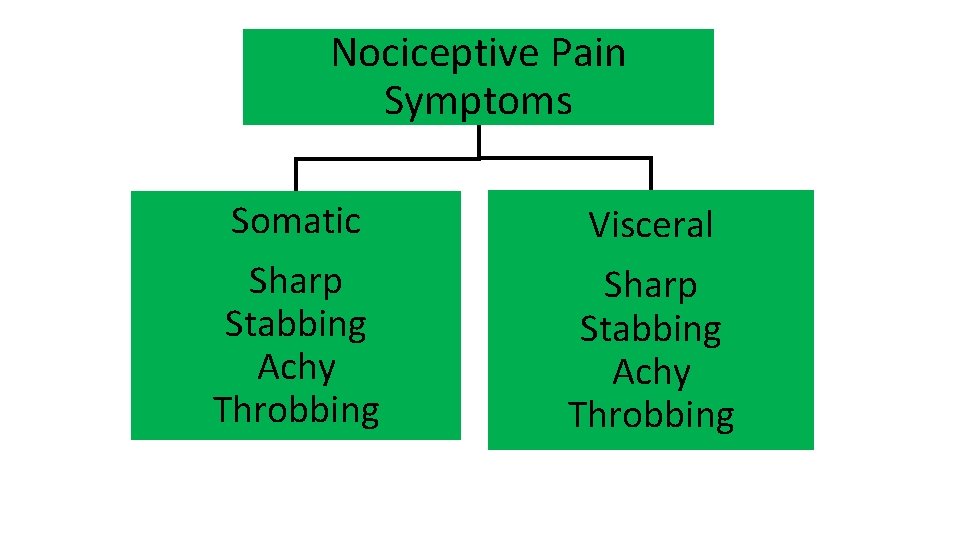
Nociceptive Pain Symptoms Somatic Visceral Sharp Stabbing Achy Throbbing
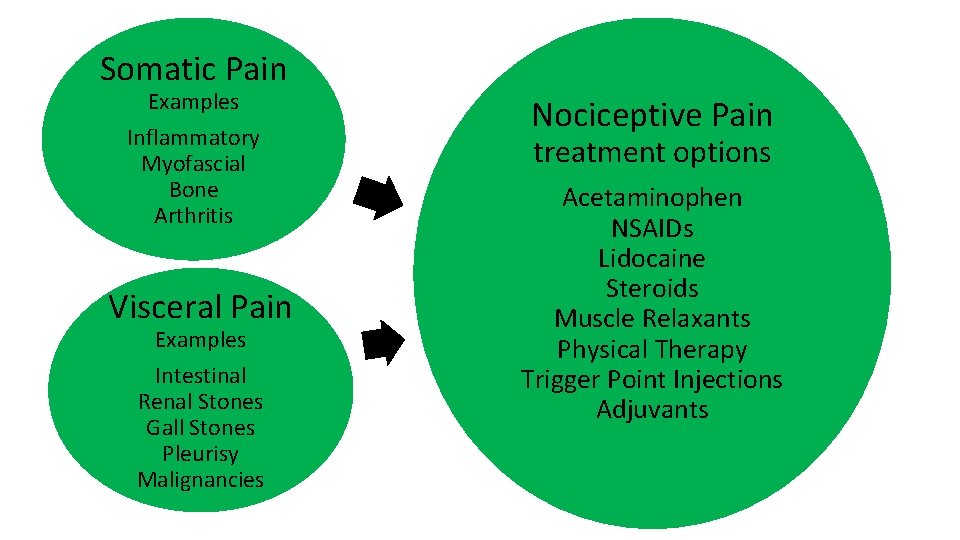
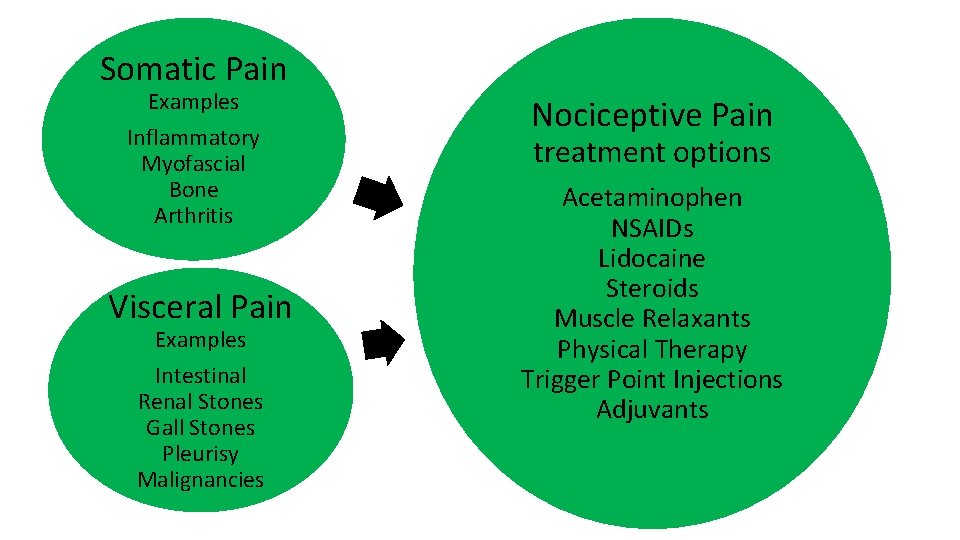
Somatic Pain Examples Inflammatory Myofascial Bone Arthritis Visceral Pain Examples Intestinal Renal Stones Gall Stones Pleurisy Malignancies Nociceptive Pain treatment options Acetaminophen NSAIDs Lidocaine Steroids Muscle Relaxants Physical Therapy Trigger Point Injections Adjuvants
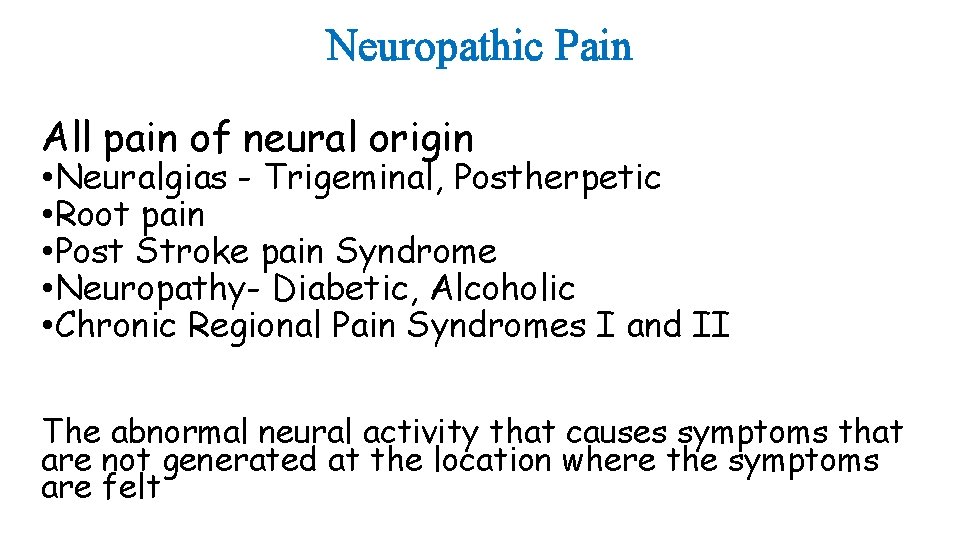
Neuropathic Pain All pain of neural origin • Neuralgias - Trigeminal, Postherpetic • Root pain • Post Stroke pain Syndrome • Neuropathy- Diabetic, Alcoholic • Chronic Regional Pain Syndromes I and II The abnormal neural activity that causes symptoms that are not generated at the location where the symptoms are felt
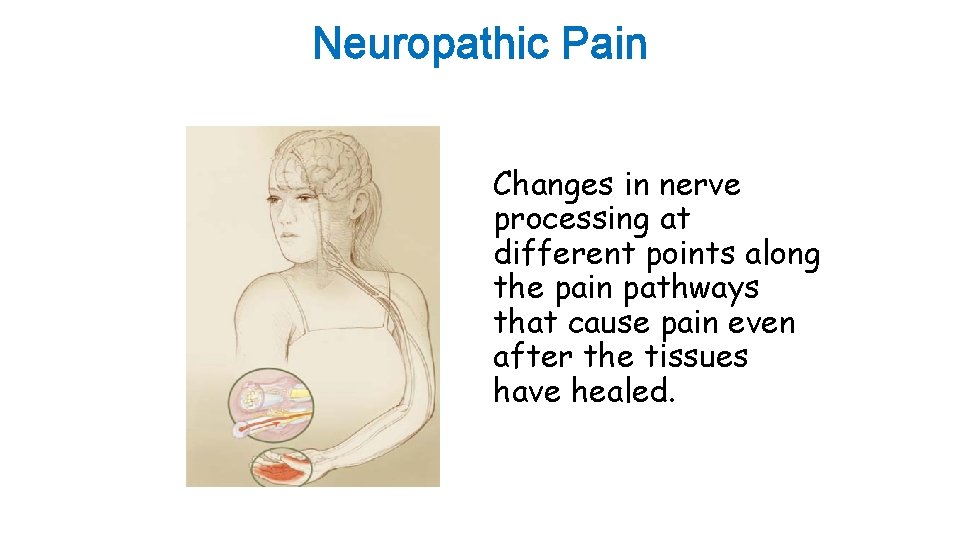
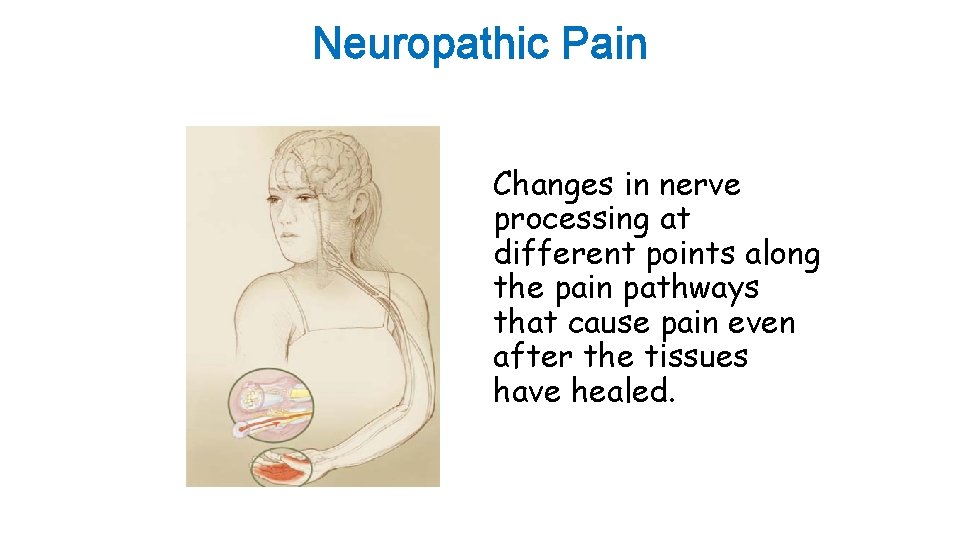
Neuropathic Pain Changes in nerve processing at different points along the pain pathways that cause pain even after the tissues have healed.
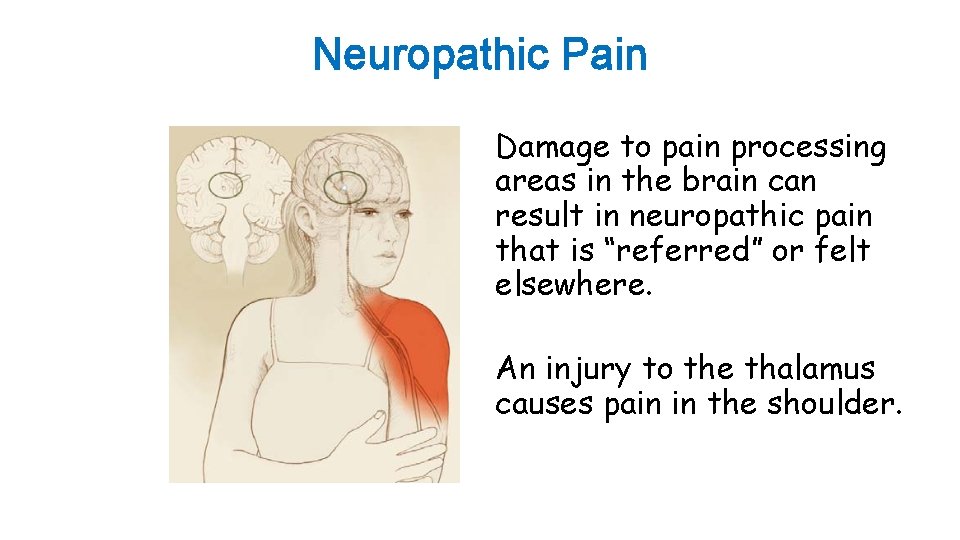
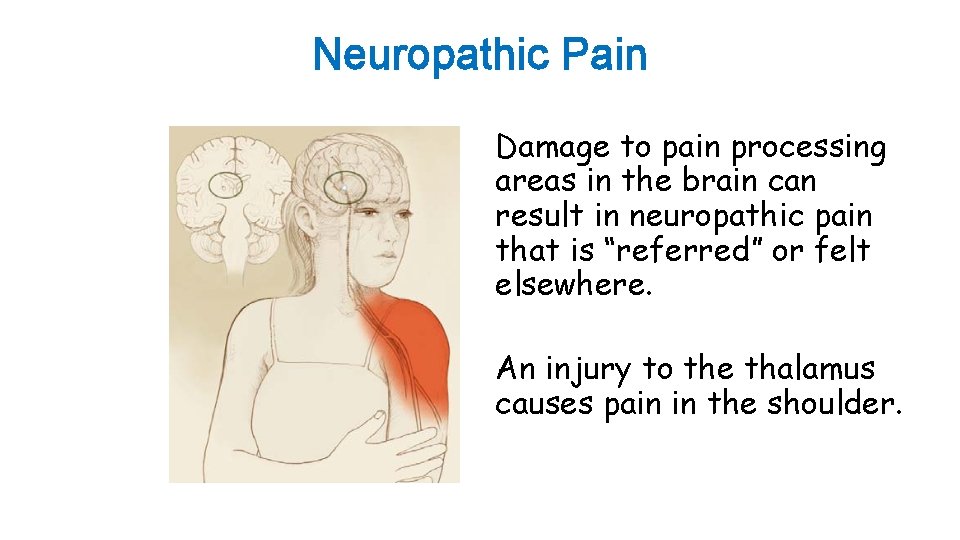
Neuropathic Pain Damage to pain processing areas in the brain can result in neuropathic pain that is “referred” or felt elsewhere. An injury to the thalamus causes pain in the shoulder.
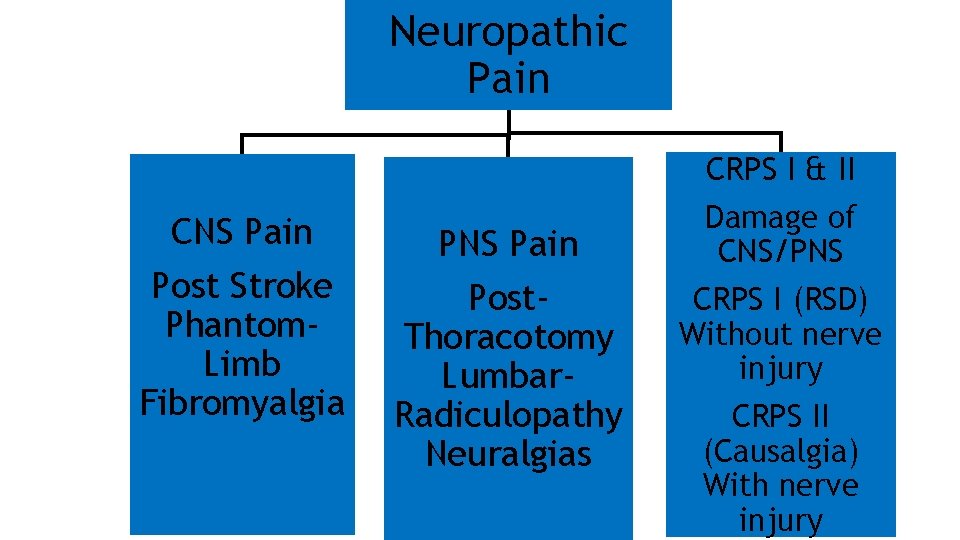
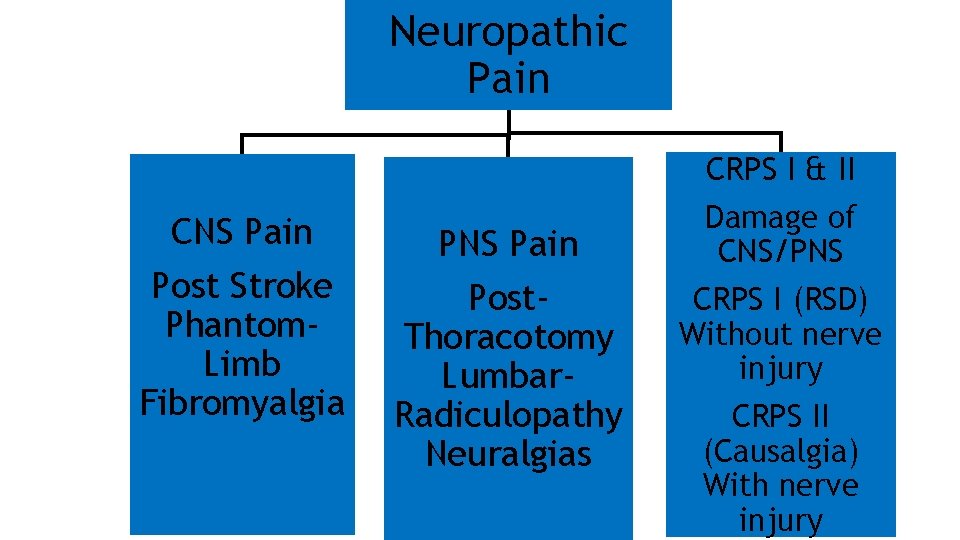
Neuropathic Pain CRPS I & II CNS Pain Post Stroke Phantom. Limb Fibromyalgia PNS Pain Post. Thoracotomy Lumbar. Radiculopathy Neuralgias Damage of CNS/PNS CRPS I (RSD) Without nerve injury CRPS II (Causalgia) With nerve injury
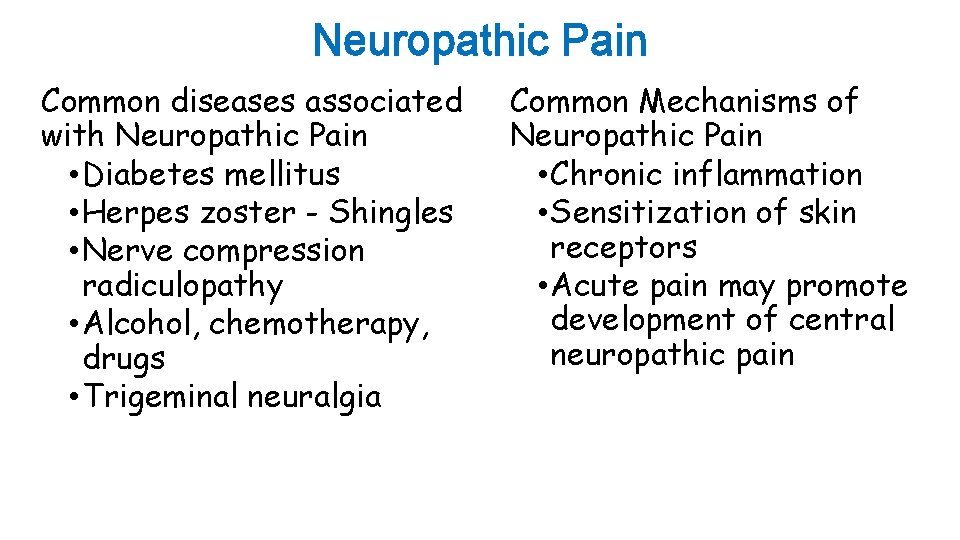
Neuropathic Pain Common diseases associated with Neuropathic Pain • Diabetes mellitus • Herpes zoster - Shingles • Nerve compression radiculopathy • Alcohol, chemotherapy, drugs • Trigeminal neuralgia Common Mechanisms of Neuropathic Pain • Chronic inflammation • Sensitization of skin receptors • Acute pain may promote development of central neuropathic pain
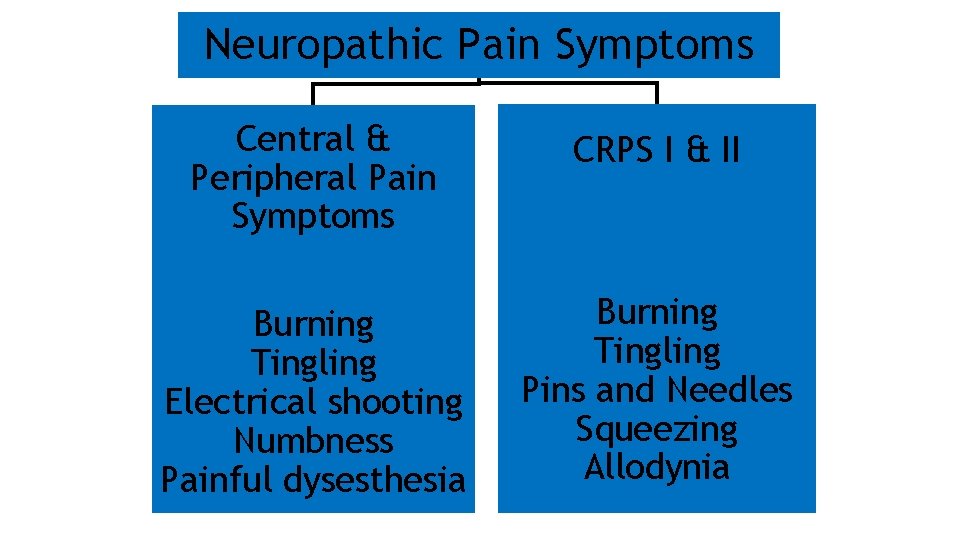
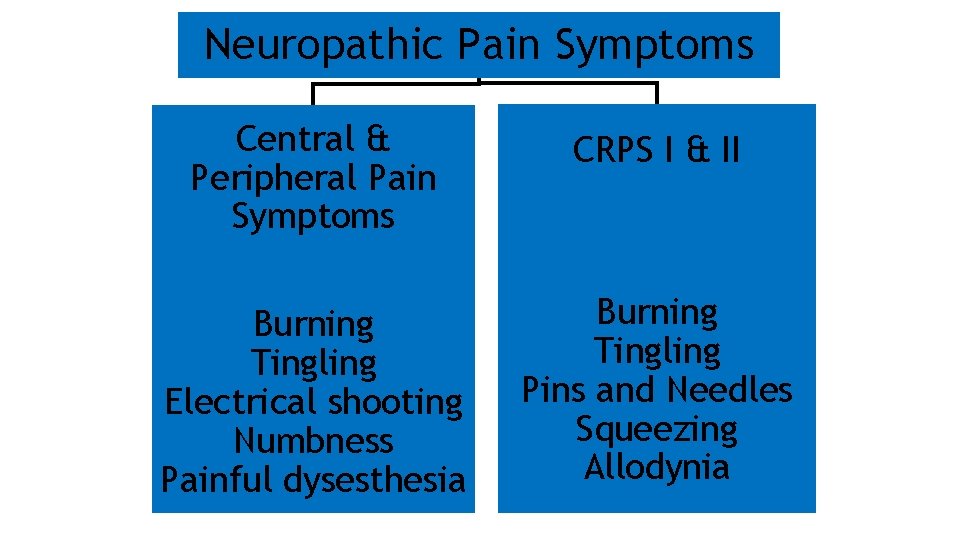
Neuropathic Pain Symptoms Central & Peripheral Pain Symptoms CRPS I & II Burning Tingling Electrical shooting Numbness Painful dysesthesia Burning Tingling Pins and Needles Squeezing Allodynia
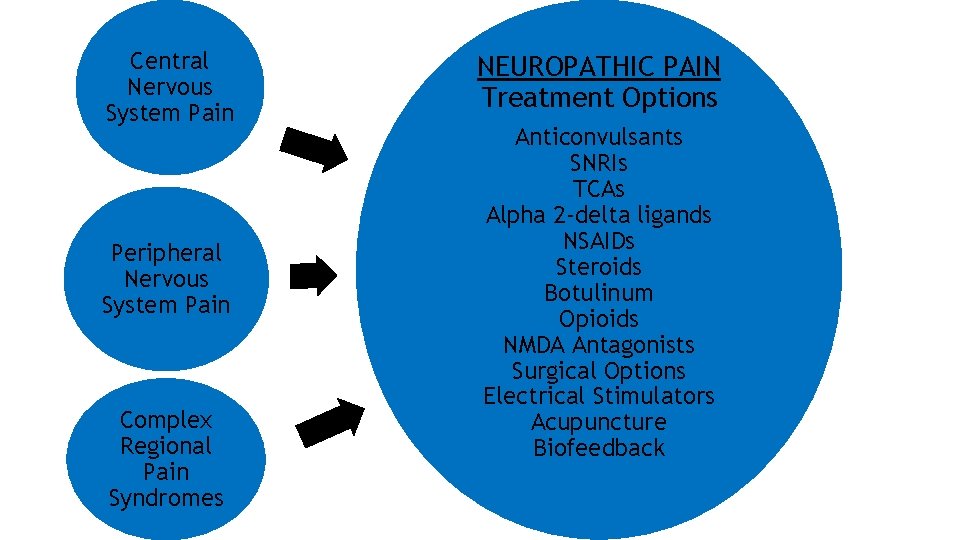
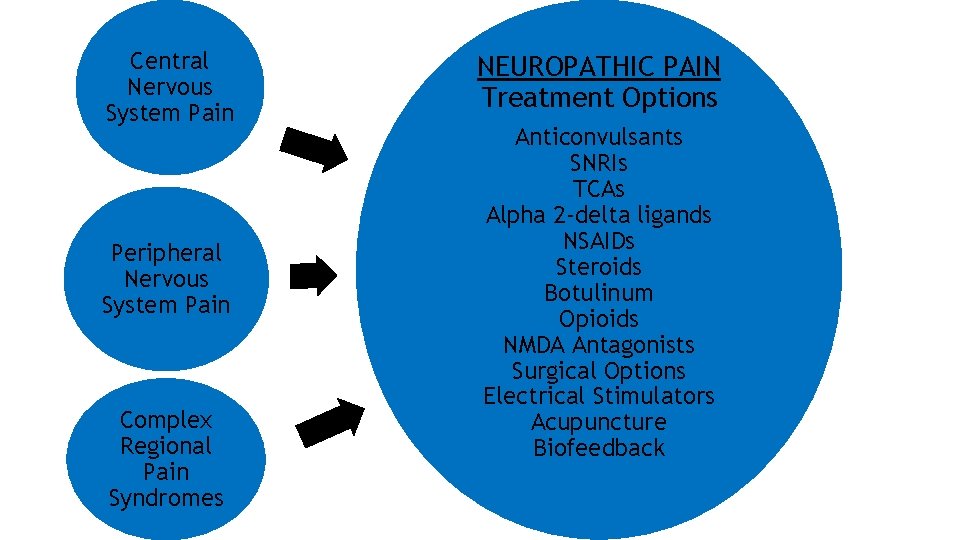
Central Nervous System Pain Peripheral Nervous System Pain Complex Regional Pain Syndromes NEUROPATHIC PAIN Treatment Options Anticonvulsants SNRIs TCAs Alpha 2 -delta ligands NSAIDs Steroids Botulinum Opioids NMDA Antagonists Surgical Options Electrical Stimulators Acupuncture Biofeedback
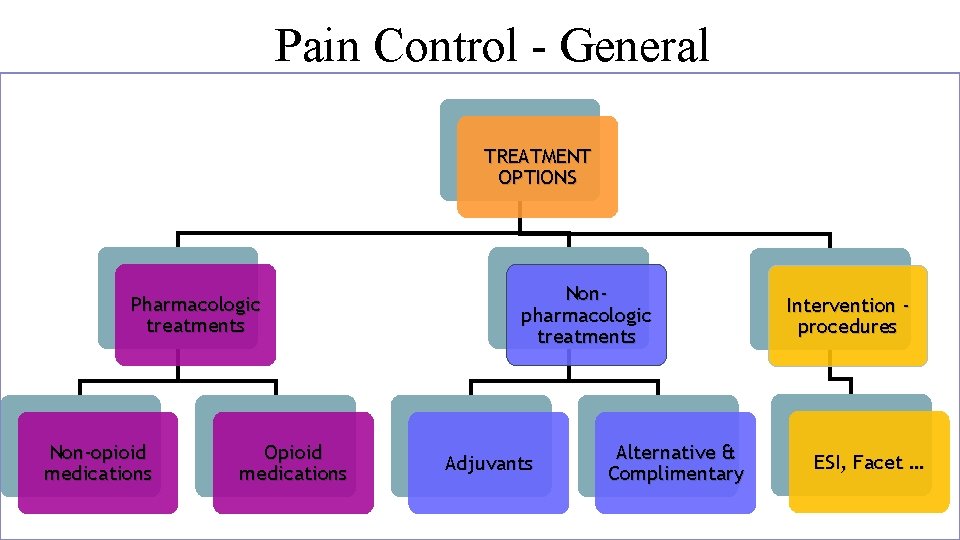
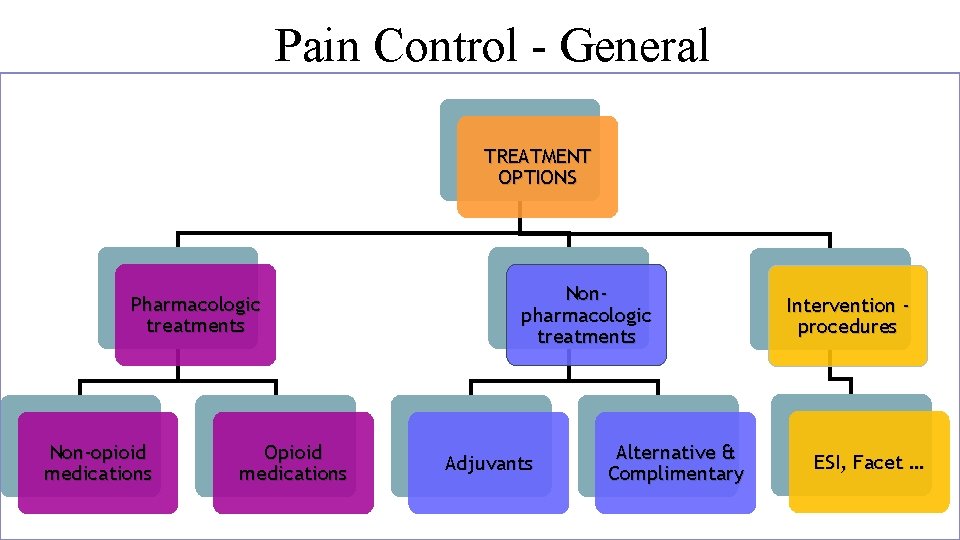
Pain Control - General TREATMENT OPTIONS Pharmacologic treatments Non-opioid medications Opioid medications Nonpharmacologic treatments Adjuvants Alternative & Complimentary Intervention procedures ESI, Facet …
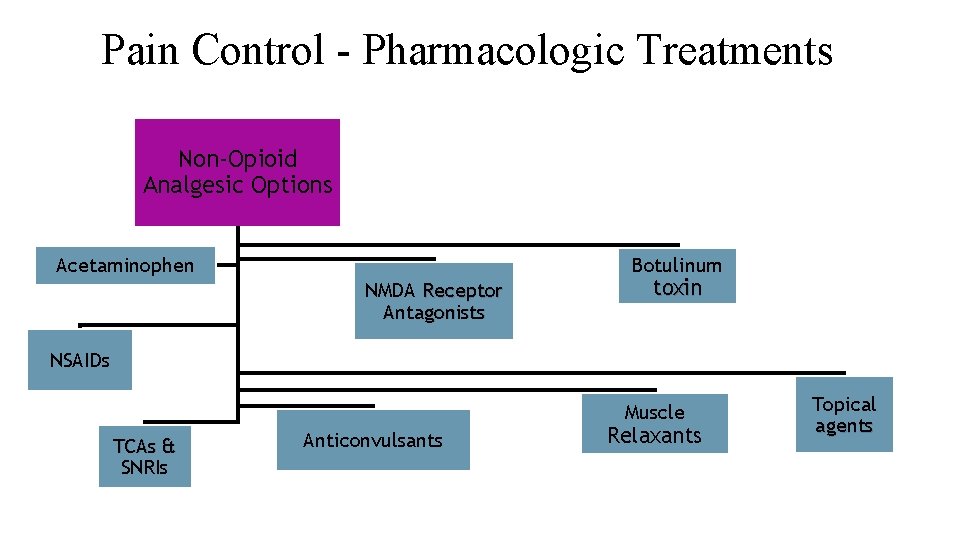
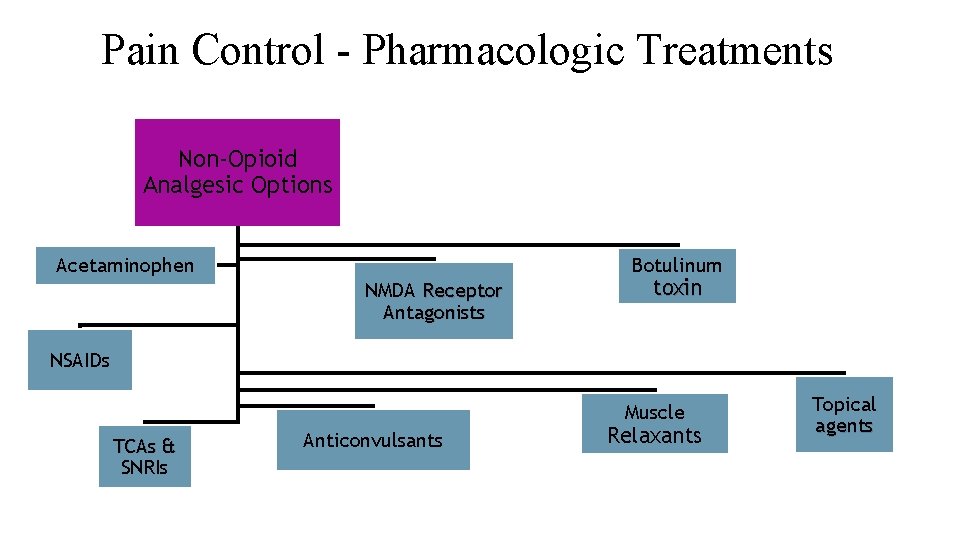
Pain Control - Pharmacologic Treatments Non-Opioid Analgesic Options Botulinum Acetaminophen NMDA Receptor Antagonists toxin NSAIDs Muscle TCAs & SNRIs Anticonvulsants Relaxants Topical agents
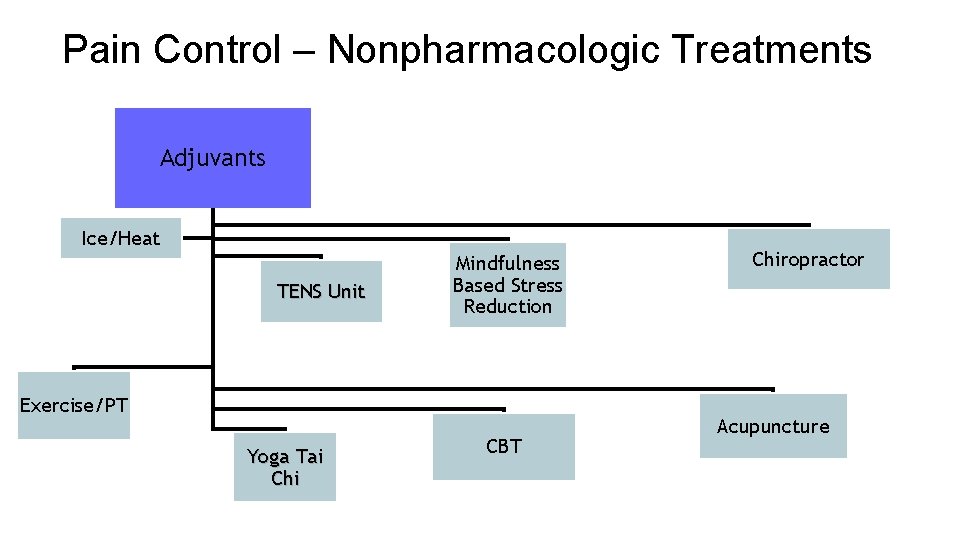
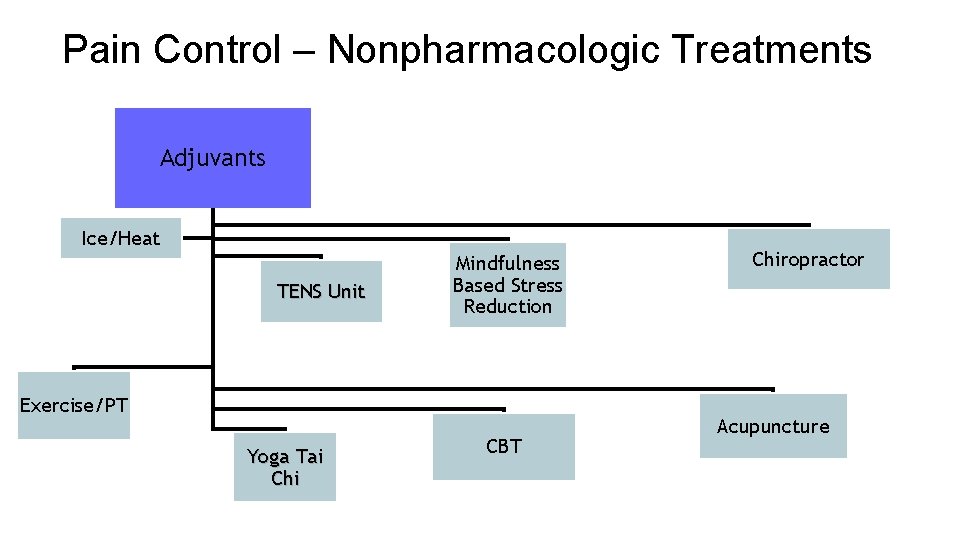
Pain Control – Nonpharmacologic Treatments Adjuvants Ice/Heat TENS Unit Mindfulness Based Stress Reduction Exercise/PT Yoga Tai Chi CBT Chiropractor Acupuncture
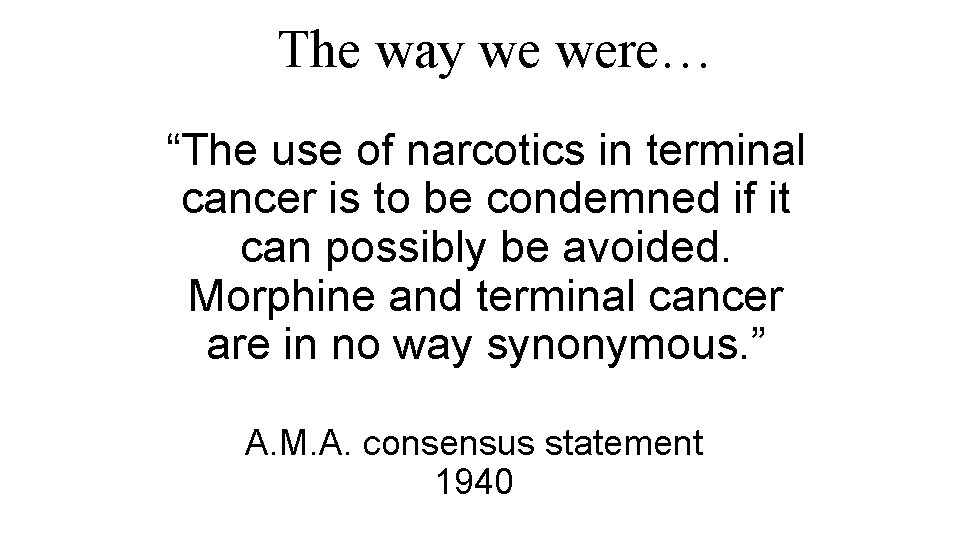
The way we were… “The use of narcotics in terminal cancer is to be condemned if it can possibly be avoided. Morphine and terminal cancer are in no way synonymous. ” A. M. A. consensus statement 1940
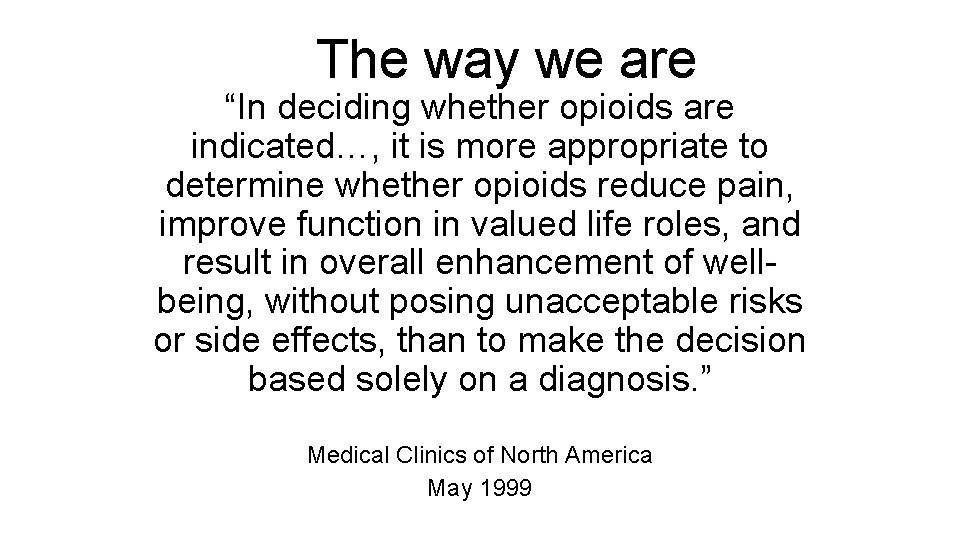
The way we are “In deciding whether opioids are indicated…, it is more appropriate to determine whether opioids reduce pain, improve function in valued life roles, and result in overall enhancement of wellbeing, without posing unacceptable risks or side effects, than to make the decision based solely on a diagnosis. ” Medical Clinics of North America May 1999
Original Research “Significant Pain Reduction in Chronic Pain Patients after Detoxification from High Dose Opiates” Journal of Opioid Management 2: 5 September/October 2006 Michael Baron, MD
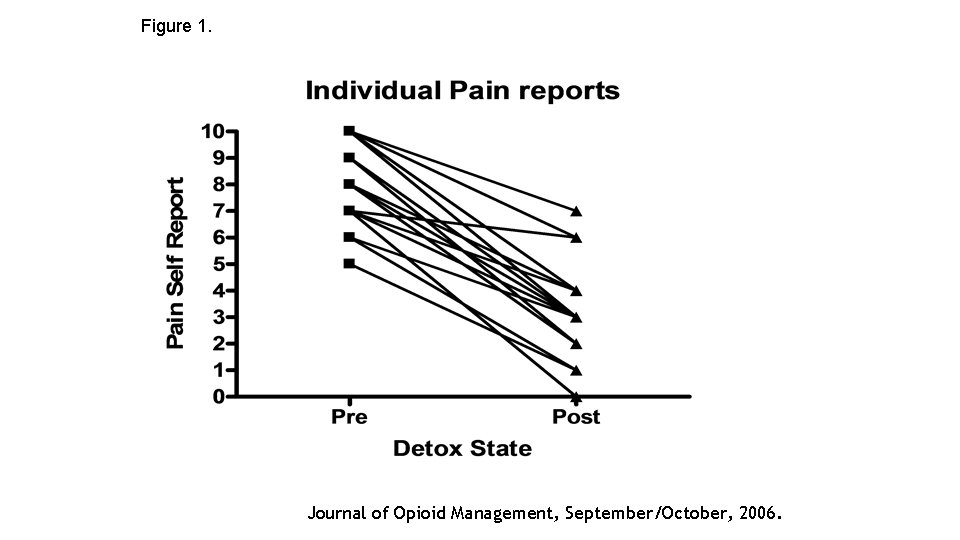
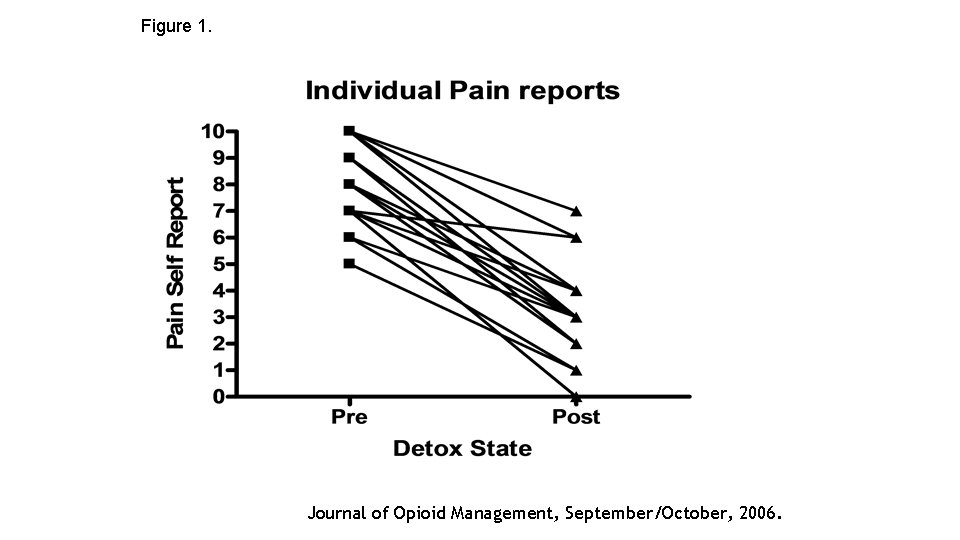
Figure 1. Journal of Opioid Management, September/October, 2006.
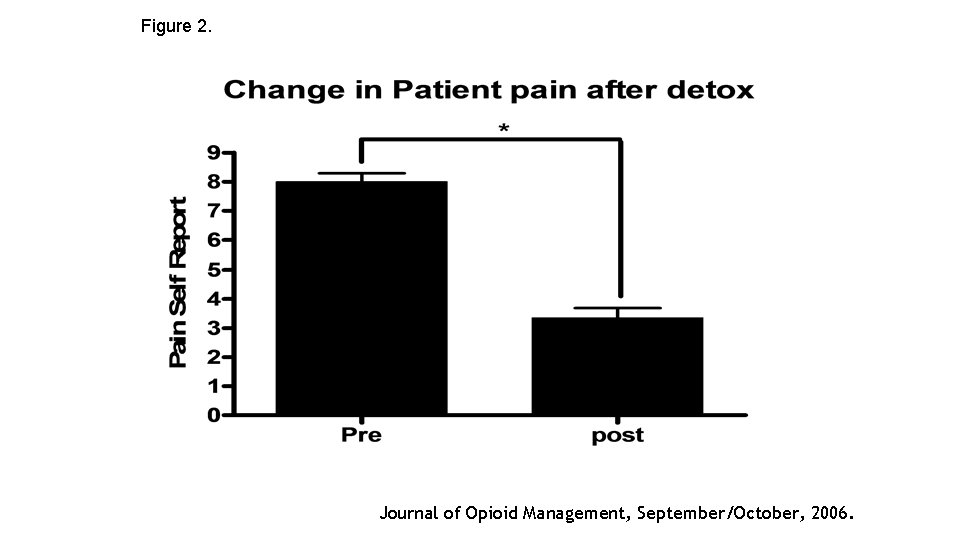
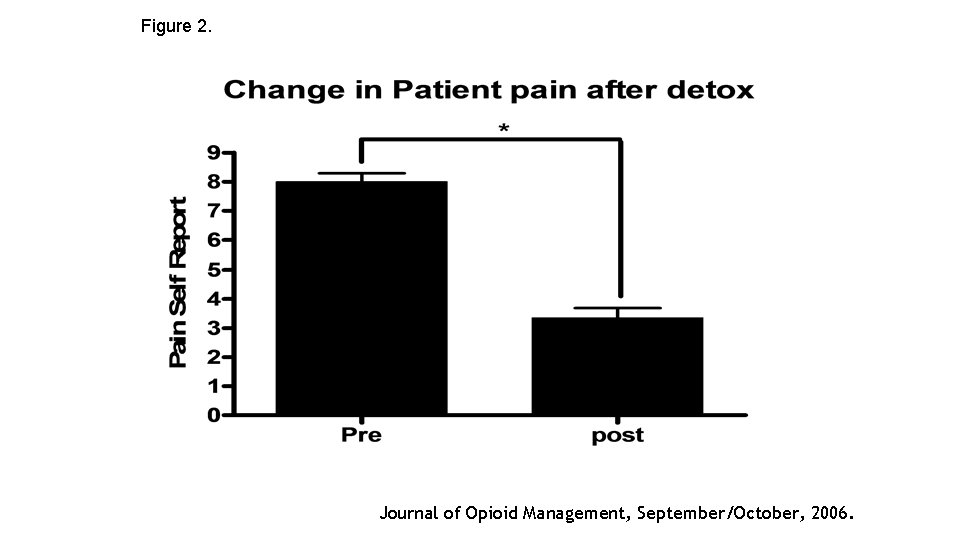
Figure 2. Journal of Opioid Management, September/October, 2006.
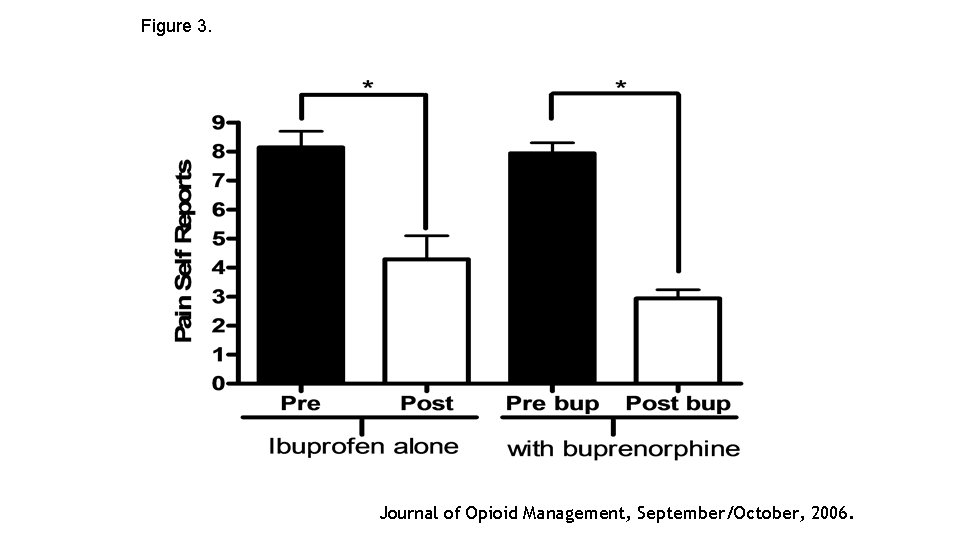
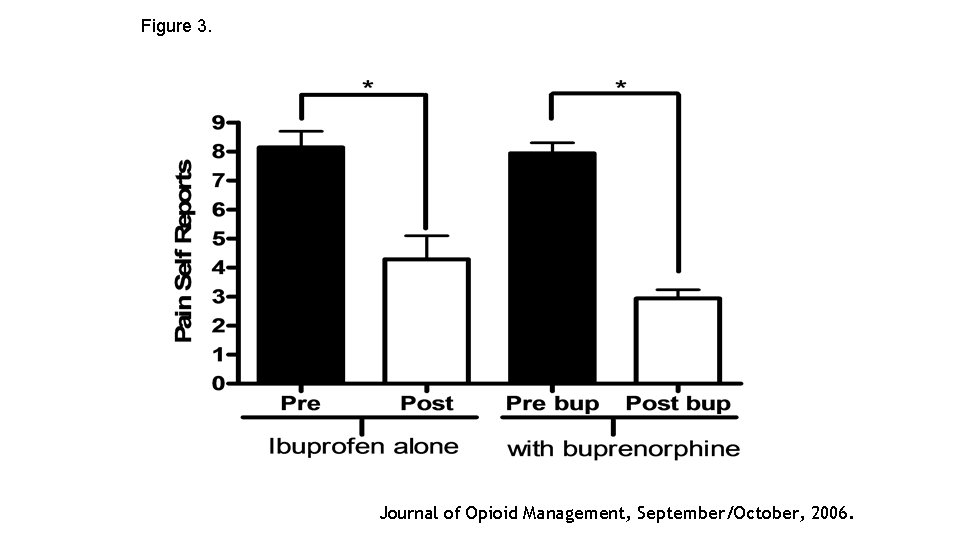
Figure 3. Journal of Opioid Management, September/October, 2006.

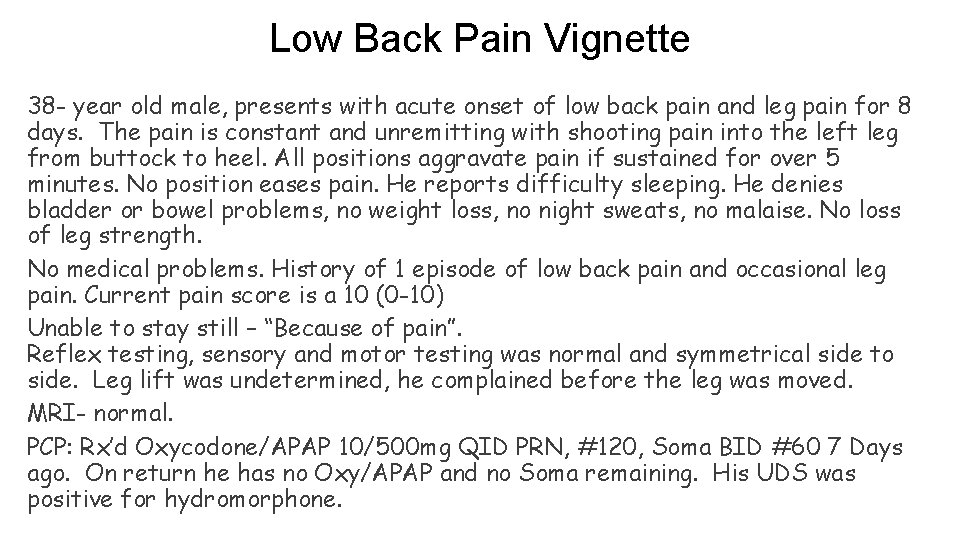
Low Back Pain Vignette 38 - year old male, presents with acute onset of low back pain and leg pain for 8 days. The pain is constant and unremitting with shooting pain into the left leg from buttock to heel. All positions aggravate pain if sustained for over 5 minutes. No position eases pain. He reports difficulty sleeping. He denies bladder or bowel problems, no weight loss, no night sweats, no malaise. No loss of leg strength. No medical problems. History of 1 episode of low back pain and occasional leg pain. Current pain score is a 10 (0 -10) Unable to stay still – “Because of pain”. Reflex testing, sensory and motor testing was normal and symmetrical side to side. Leg lift was undetermined, he complained before the leg was moved. MRI- normal. PCP: Rx’d Oxycodone/APAP 10/500 mg QID PRN, #120, Soma BID #60 7 Days ago. On return he has no Oxy/APAP and no Soma remaining. His UDS was positive for hydromorphone.
Low Back Pain Vignette What are the red flags? Addiction history not obtained. (Don’t ask don’t tell. ) Family history not obtained. Rx Monitoring Program (PMP) not queried. UDS: positives and negatives – hydromorphone? ? ? Patient used(? ) 60 carisoprodol and 120 Oxy/APAP 10/500 in 7 days = @ 8 carisoprodol and @ 17 Oxy/APAP per day = 170 mg of Oxycodone and 7500 mg of APAP per day. = 255 MME per day.

Low Back Pain ICD– 10 Diagnosis Code = M 54. 5 Acute or chronic pain in the lumbar or sacral regions, which may be associated with musculo-ligamentous sprains and strains; intervertebral disk displacement; and other conditions.
Low Back Pain Epidemiology • 60 -90% Lifetime prevalence • 80 -90% Have recurrent episode Natural History • 80 -90% Resolves in 1 month • 20 -30% Remains chronic • 5 -10% Disabling
Low Back Pain Generally benign • 90% resolution within 2 weeks in one study • Bigger studies • 1/3 improved in 2 weeks • 2/3 improved in 7 weeks • 40% recurrence within 6 months Smoking (and number of cigarettes per day) correlated with both LBP and severity of LBP Deyo and Weinstein, NEJM, 2001
Low Back Pain - Generators • • • Annulus Fibrosis Periosteum Neural Membranes - Dura Ligaments, joint Capsules Muscles
Low Back Pain DDD does not equal Low Back Pain DDD - Normal aging process includes • Dehydration of nucleus • Collapse of the disc space • Sclerosis of the endplates
Low Back Pain - History • Trauma • Age > 50 years • History of Cancer • Weight loss • Fever • Immunosuppression • IV drug use • Neurologic deficit
Low Back Pain - Symptoms • Pain location, radiation, quality • Exacerbates and relieves pain • Neurologic Symptoms • Paresthesia • Bladder or Bowel retention or incontinence • Weakness

Low Back Pain - Examination Reflexes • L 2, 3, 4 Quads • L 5 Medial Hamstring • S 1 Achilles Sensation • Pin prick - Spinothalamic Tract • Vibration and Position - Dorsal Column
60
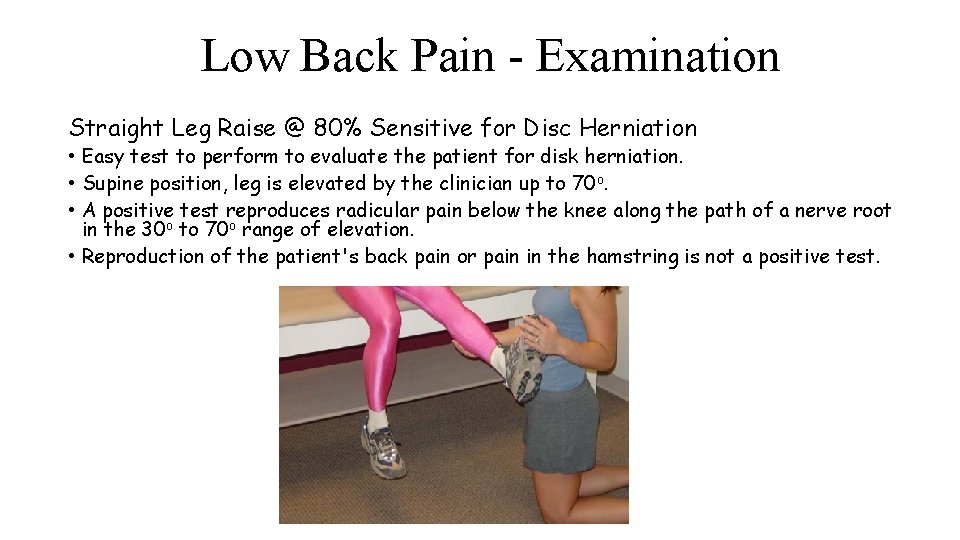
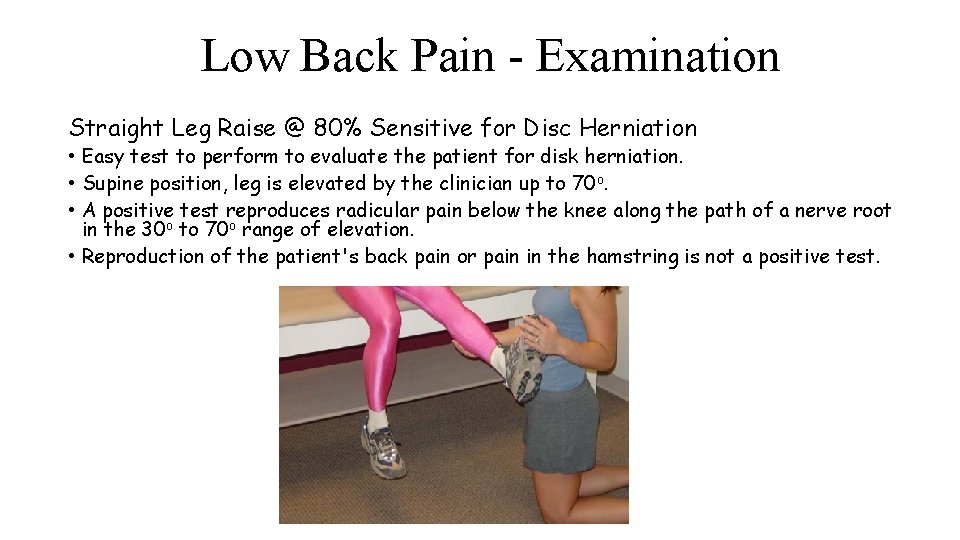
Low Back Pain - Examination Straight Leg Raise @ 80% Sensitive for Disc Herniation • Easy test to perform to evaluate the patient for disk herniation. • Supine position, leg is elevated by the clinician up to 70 o. • A positive test reproduces radicular pain below the knee along the path of a nerve root in the 30 o to 70 o range of elevation. • Reproduction of the patient's back pain or pain in the hamstring is not a positive test.

Low Back Pain - Therapy Bed Rest - Less than 2 days Physical Therapy • Better than medical management alone • Flexion and extension exercises • No one program shown most effective • Massage shown to be effective • Traction unproven
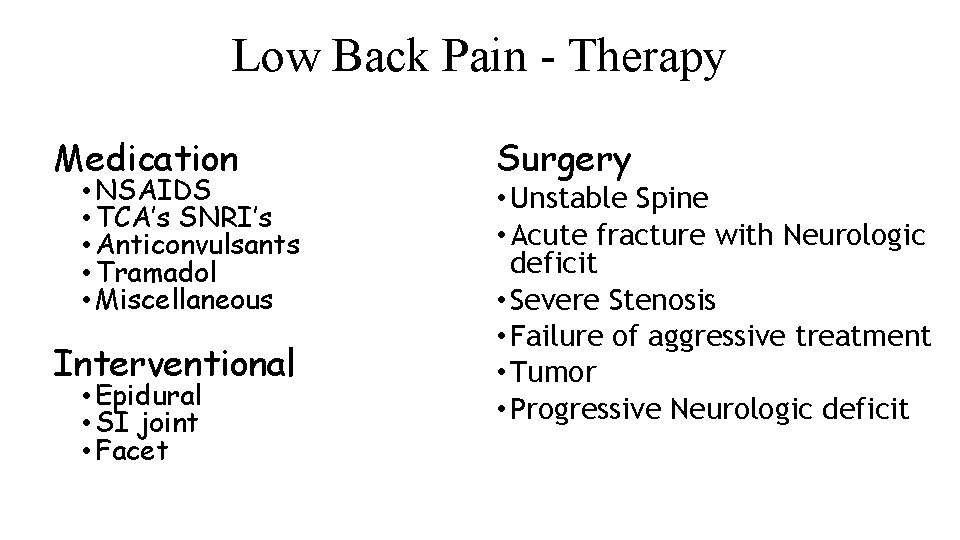
Low Back Pain - Therapy Medication • NSAIDS • TCA’s SNRI’s • Anticonvulsants • Tramadol • Miscellaneous Interventional • Epidural • SI joint • Facet Surgery • Unstable Spine • Acute fracture with Neurologic deficit • Severe Stenosis • Failure of aggressive treatment • Tumor • Progressive Neurologic deficit
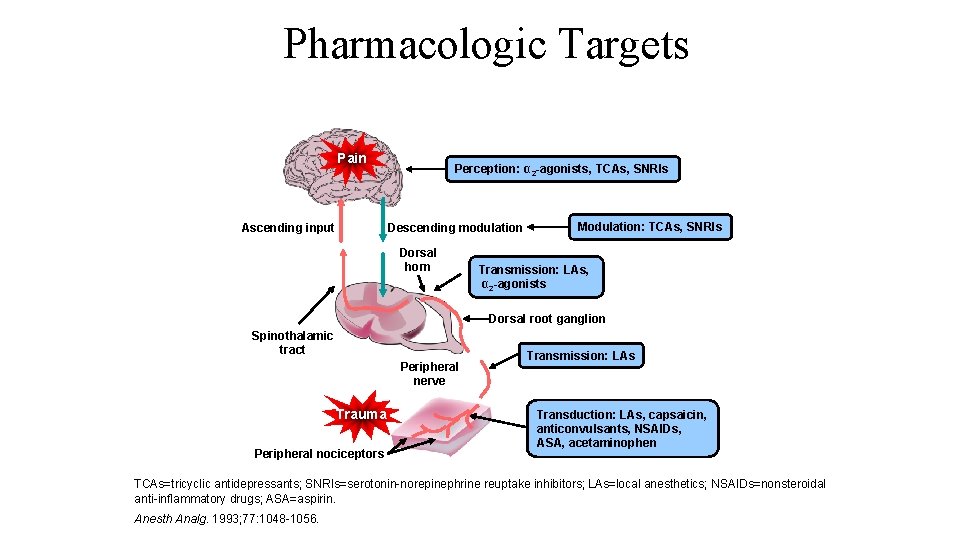
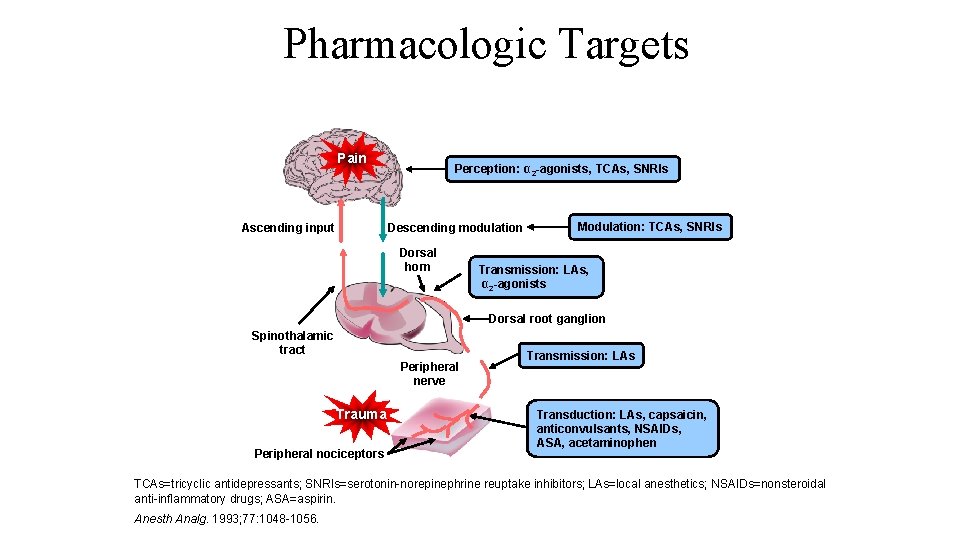
Pharmacologic Targets Pain Ascending input Perception: α 2 -agonists, TCAs, SNRIs Descending modulation Dorsal horn Modulation: TCAs, SNRIs Transmission: LAs, α 2 -agonists Dorsal root ganglion Spinothalamic tract Peripheral nerve Trauma Peripheral nociceptors Transmission: LAs Transduction: LAs, capsaicin, anticonvulsants, NSAIDs, ASA, acetaminophen TCAs=tricyclic antidepressants; SNRIs=serotonin-norepinephrine reuptake inhibitors; LAs=local anesthetics; NSAIDs=nonsteroidal anti-inflammatory drugs; ASA=aspirin. Anesth Analg. 1993; 77: 1048 -1056.
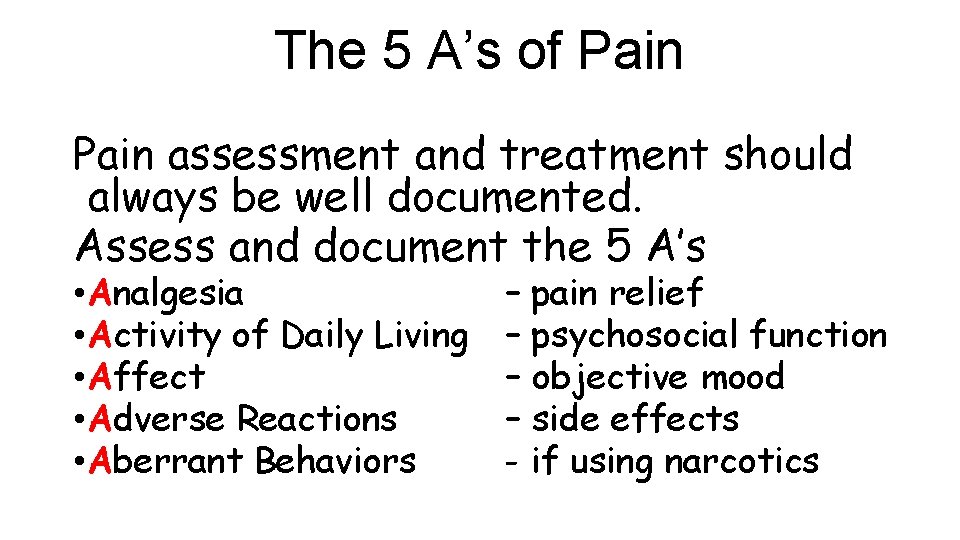
The 5 A’s of Pain assessment and treatment should always be well documented. Assess and document the 5 A’s • Analgesia • Activity of Daily Living • Affect • Adverse Reactions • Aberrant Behaviors – pain relief – psychosocial function – objective mood – side effects - if using narcotics
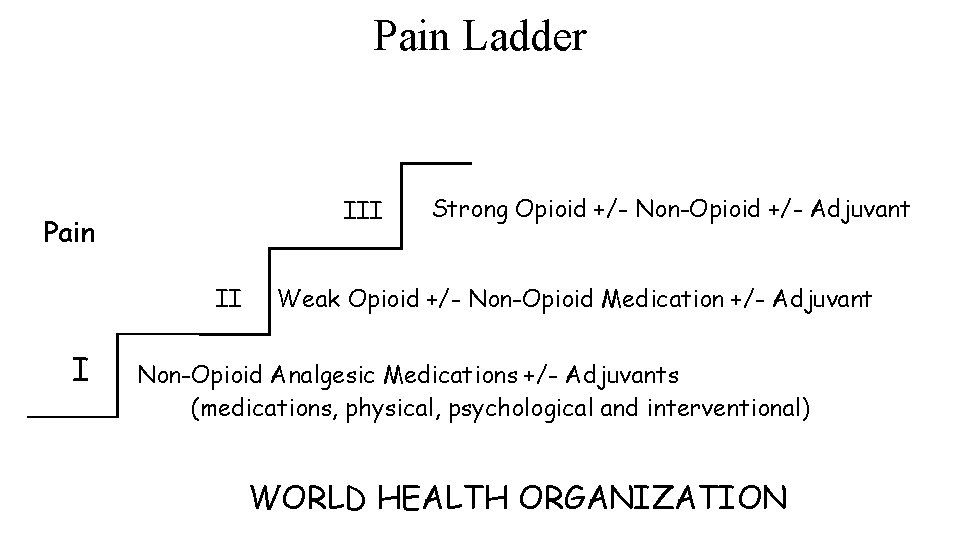
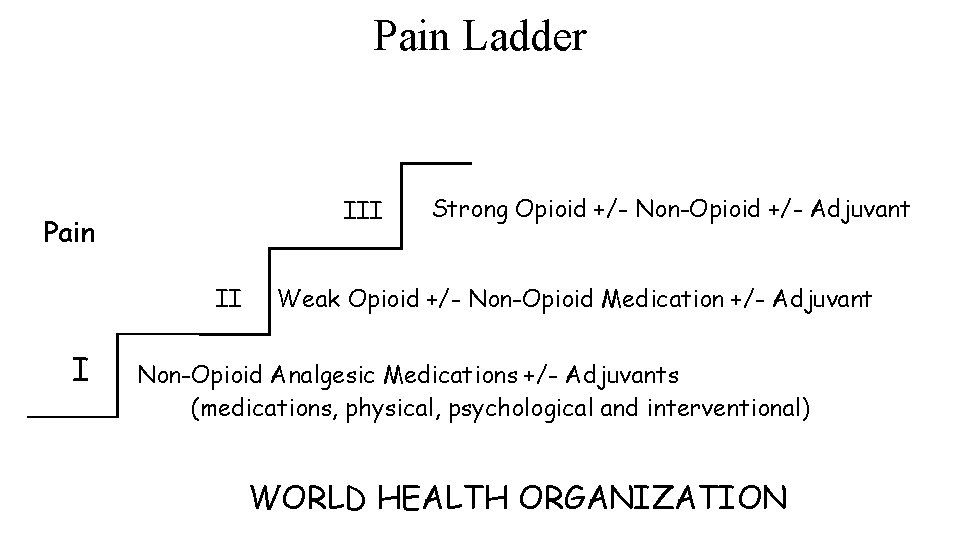
Pain Ladder III Pain II I Strong Opioid +/- Non-Opioid +/- Adjuvant Weak Opioid +/- Non-Opioid Medication +/- Adjuvant Non-Opioid Analgesic Medications +/- Adjuvants (medications, physical, psychological and interventional) WORLD HEALTH ORGANIZATION
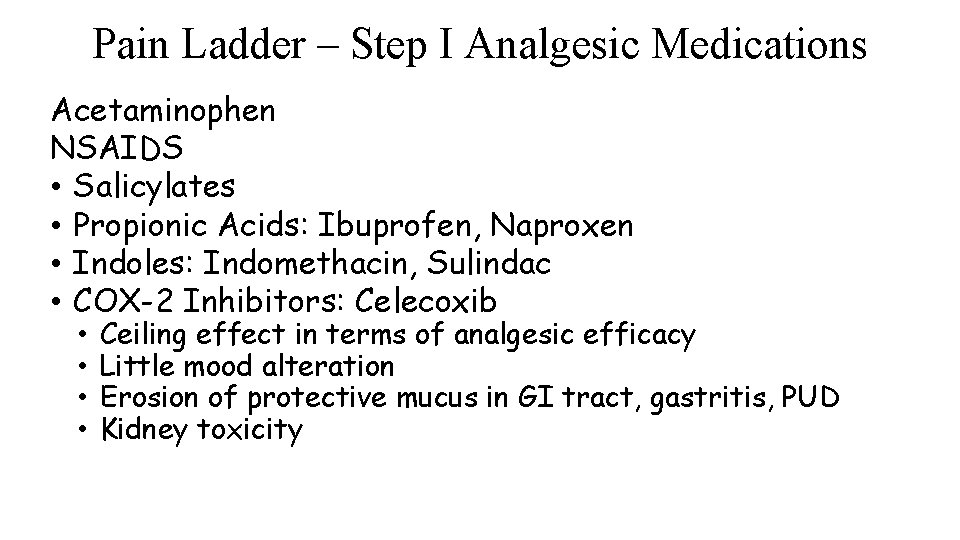
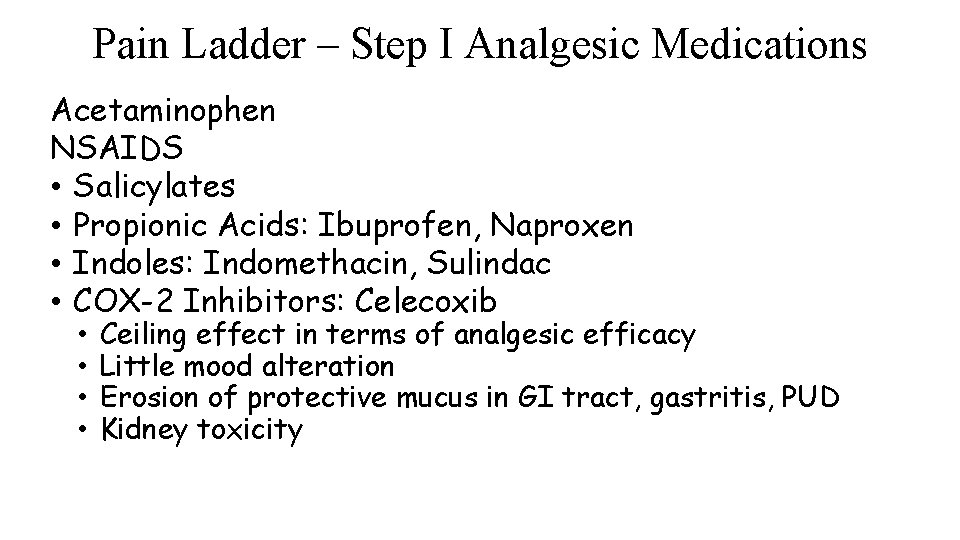
Pain Ladder – Step I Analgesic Medications Acetaminophen NSAIDS • Salicylates • Propionic Acids: Ibuprofen, Naproxen • Indoles: Indomethacin, Sulindac • COX-2 Inhibitors: Celecoxib • • Ceiling effect in terms of analgesic efficacy Little mood alteration Erosion of protective mucus in GI tract, gastritis, PUD Kidney toxicity
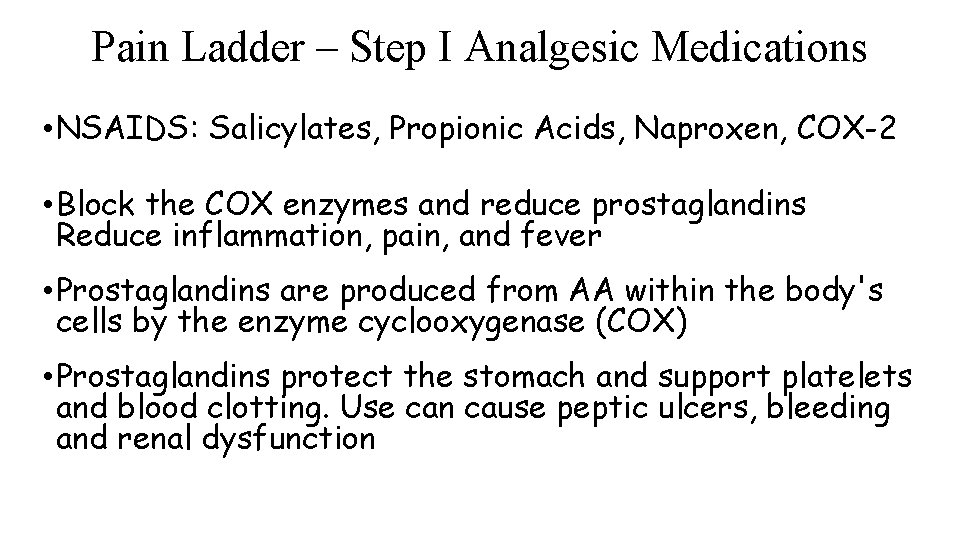
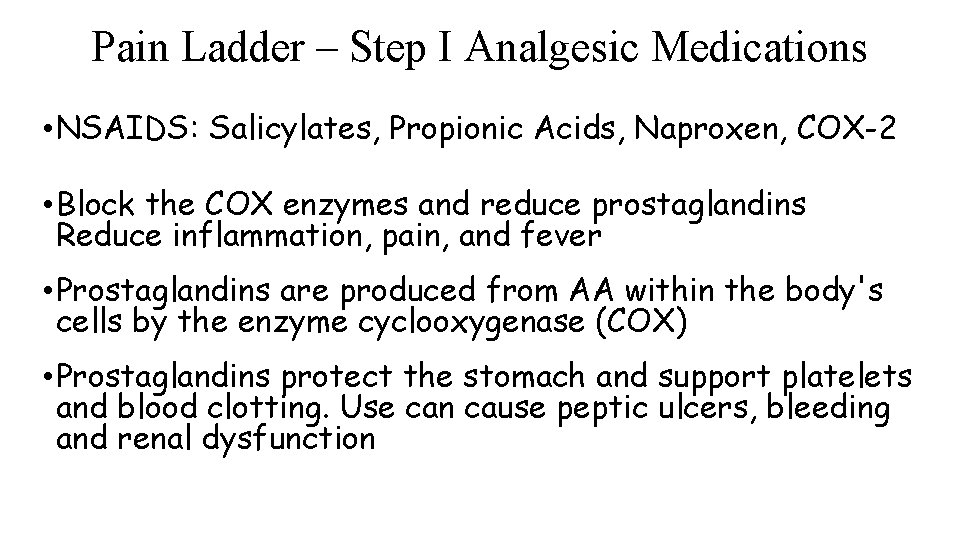
Pain Ladder – Step I Analgesic Medications • NSAIDS: Salicylates, Propionic Acids, Naproxen, COX-2 • Block the COX enzymes and reduce prostaglandins Reduce inflammation, pain, and fever • Prostaglandins are produced from AA within the body's cells by the enzyme cyclooxygenase (COX) • Prostaglandins protect the stomach and support platelets and blood clotting. Use can cause peptic ulcers, bleeding and renal dysfunction
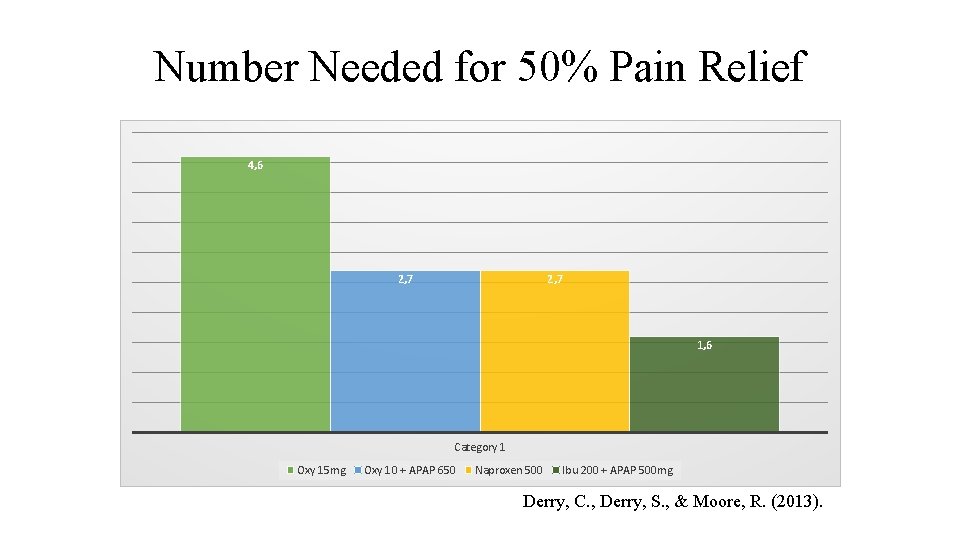
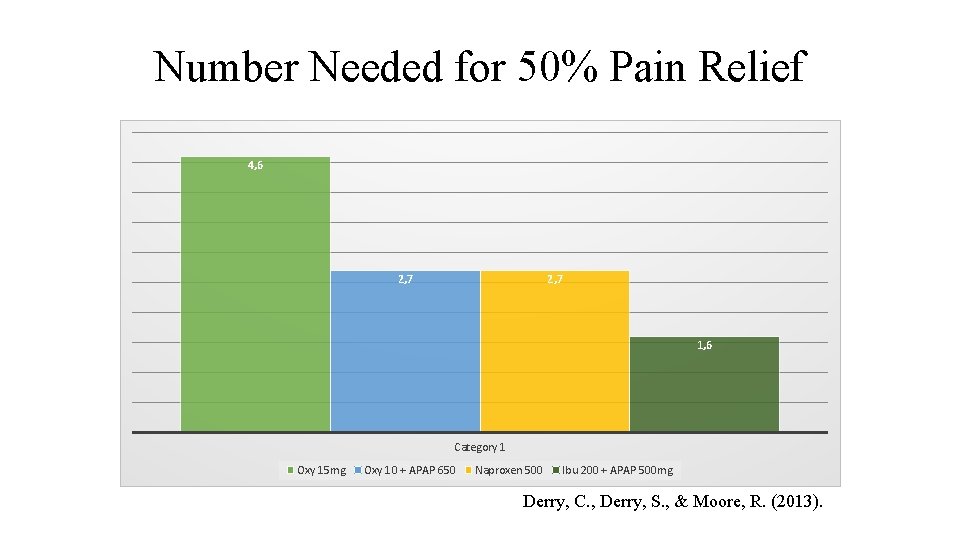
Number Needed for 50% Pain Relief 4, 6 2, 7 1, 6 Category 1 Oxy 15 mg Oxy 10 + APAP 650 Naproxen 500 Ibu 200 + APAP 500 mg Derry, C. , Derry, S. , & Moore, R. (2013).
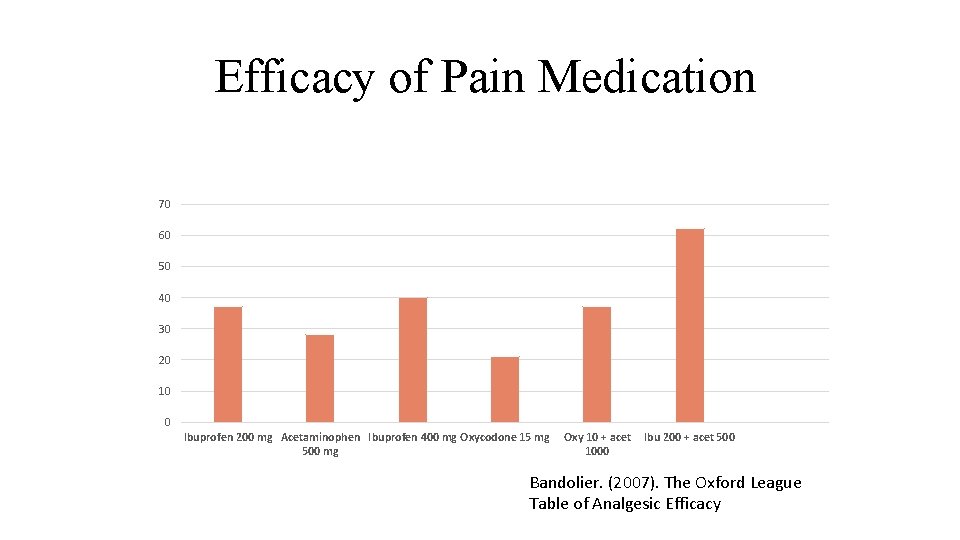
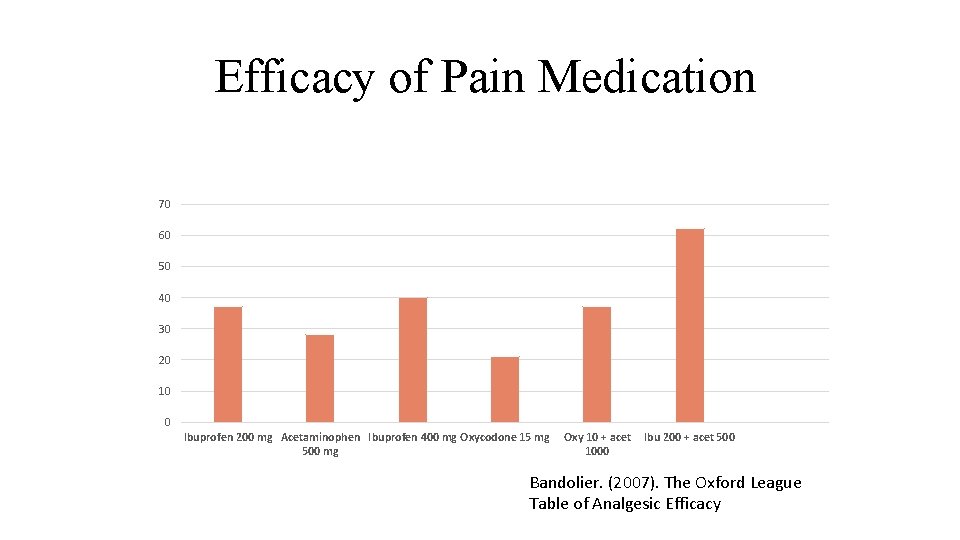
Efficacy of Pain Medication 70 60 50 40 30 20 10 0 Ibuprofen 200 mg Acetaminophen Ibuprofen 400 mg Oxycodone 15 mg 500 mg Oxy 10 + acet 1000 Ibu 200 + acet 500 Bandolier. (2007). The Oxford League Table of Analgesic Efficacy
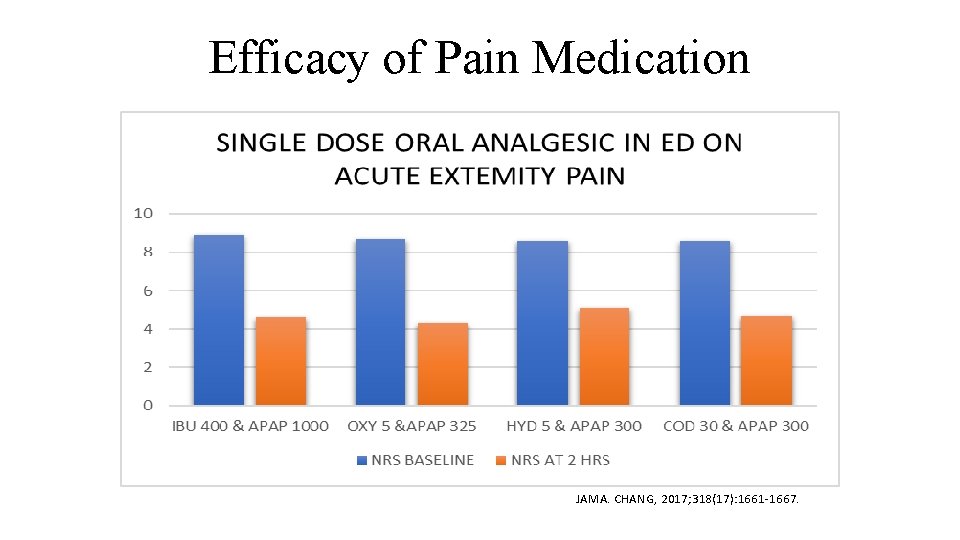
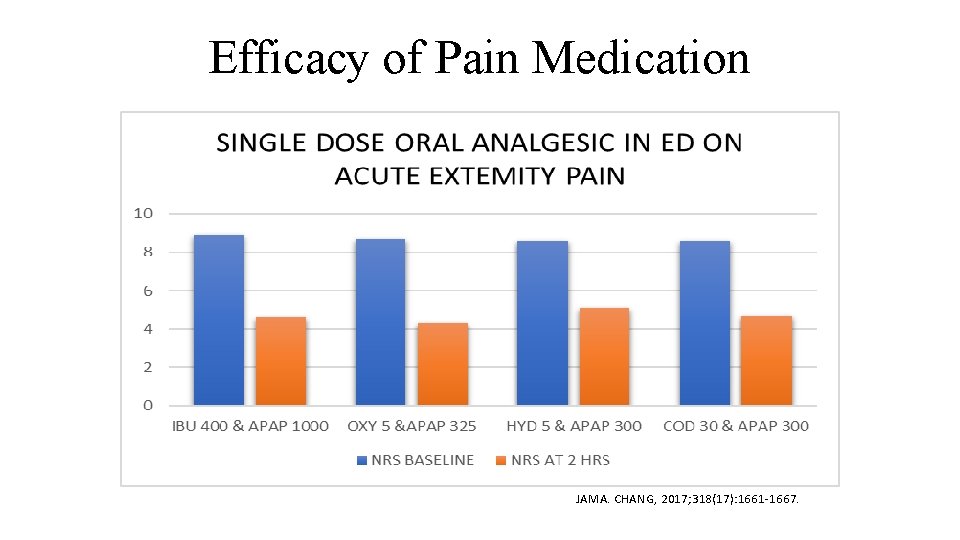
Efficacy of Pain Medication JAMA. CHANG, 2017; 318(17): 1661 -1667.
Effect of Opioid vs Nonopioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain. 240 randomized patients – 12 months Pain was significantly better in the nonopioid group. Adverse medication-related symptoms were significantly more common in the opioid group. Treatment with opioids was not superior to treatment with nonopioid medications for improving pain-related function over 12 months. Results do not support initiation of opioid therapy for moderate to severe chronic back pain or hip or knee osteoarthritis pain. JAMA. 2018: 319(9): 872 -882
Pain Ladder – Step I Adjuvant Medications Antidepressants with noradrenergic effects Anticonvulsants Topicals Muscle Relaxants Neutraceuticals
Pain Ladder – Step I Adjuvant Antidepressants Tricyclic Antidepressants (TCAs) - amitriptyline Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) - duloxetine Increases the central nervous system’s production of endogenous pain killers. • Enhances the descending inhibitory pathways from the brain • Improves sleep hygiene
Pain Ladder – Step I Adjuvant Anticonvulsants Carbamazepine, oxcarbazepine, topiramate • Modulate peripheral sensitization by inactivating voltagedependent sodium channels. Gabapentin, pregabalin • Inhibits Ca++ channel current in a voltage-dependent manner. Pregabalin also decreases the release of the neurotransmitters-glutamate, noradrenalin and substance P
Pain Ladder – Step I Adjuvant Topicals Capsaicin • Derivative of Red Pepper • Depletes substance P at nociceptive transmission Local Anesthetics • Lidocaine
Pain Ladder – Step I Adjuvant Miscellaneous Muscle relaxants • Tizanidine Zanaflex® - Centrally acting α 2 -adrenergic agonist Neutraceuticals • Glucosamine & Chondroitin NMDA Receptor Antagonist • Ketamine

Pain Ladder – Step I Adjuvants Physical Modalities • Thermal Modalities Cold/Heat Packs • Counter stimulation TENS, Vibration, Topical Aromatics • Manual/ Active movement Therapy Massage, Manipulation, Yoga, Tai Chi, Exercise, PT, Stretching, Conditioning and strengthening • Orthotics Splints, Braces, Pillows, Supports • Acupuncture • Chiropractic
Pain Ladder – Step I Adjuvant Psychological Modalities • Deep relaxation • • Sleep Management Biofeedback Guided imagery Mindfulness Based Stress Reduction Affective Disorders treatment Family, couple, individual therapy Cognitive Behavioral Therapy

Pain Ladder – Step I Adjuvant Interventional Procedures • Trigger Point Injection • • • Tendon, bursa or intra-articular Steroid Injection Peripheral nerve block Sympathetic nerve block Implanted peripheral nerve Spinal stimulator
Pain Ladder – Step II Weak Opioid TRAMADOL: Mode of action • Modulation of the noradrenergic and serotonergic systems • Mild agonist at the μ-opioid receptor • Mild NMDA-type antagonist Increased risk of serotonin syndrome when used in combination with SSRIs Hepatic metabolism - CYP 2 D 6 • SSRI’s inhibit metabolism 5 metabolites - O-Desmethyltramadol has • 200 times the μ-affinity of tramadol • T-1/2 9 hours, tramadol T-1/2 is 6 hours
THANK YOU!
If Time Permits
Suspect Drug-Seeking Behavior in the Patient who. . .
Possible Drug-Seeking Behavior • • A dramatic, compelling but vague complaint Pressures for an increases in dose Drug screens are negative for Rx’d medicine Symptoms contradict clinical observation Patient asks for a specific drug Patient has no interest in the diagnosis Rejects all treatment that is not opioids
Possible Drug-Seeking Behavior • • Reports an NSAID Allergy Has abundant pharmacologic knowledge Patient makes veiled threats Patient is very flattering Primary doctor is out of town Travels long distance or past other clinics to clinic Primary doctor just retired
THANK YOU!
Misprescribing Prescribing in quantities or frequency inappropriate for the complaint or illness as seen with: • Large quantities • Frequent intervals with a crescendo pattern • Progression to multiple drugs • For trivial complaints • Family members • Patient with a known Substance Use Disorder
Categories of Misprescribing Dated: – Fails to keep current Duped – Didn’t detect deception Dismayed – Rx is to make up for no available time Dysfunctional – Can’t say no Dishonest – Rx’ing for financial gain Disabled – impaired judgment Disempowered – Skewed perception of power Disorganized – No systems in place Disregard for Scope – Practicing out of specialty Dodging – Avoiding refills and patient visits.
Aberrant Drug Taking Behavior Selling prescription drugs Prescription forgery Stealing or using another patient’s drugs Injecting oral formulation Obtaining prescription drugs from nonmedical sources • Concurrent use of related illicit drugs • Multiple unsanctioned dose escalations • Recurrent prescription losses • • •
THANK YOU!
 David lewis mad pain and martian pain
David lewis mad pain and martian pain Sore boobs early pregnancy
Sore boobs early pregnancy Spanish flacs exam 2018 answers
Spanish flacs exam 2018 answers June 2018 geometry regents answers
June 2018 geometry regents answers Flacs checkpoint b spanish exam june 2017 answers
Flacs checkpoint b spanish exam june 2017 answers Cxc results 2018 may/june date
Cxc results 2018 may/june date June 2018 chemistry regents
June 2018 chemistry regents Tungsten fabric
Tungsten fabric Customer service summit 2018
Customer service summit 2018 Pms vs pregnancy symptoms
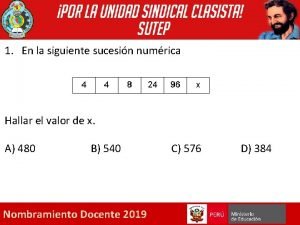
Pms vs pregnancy symptoms Que letra continua m v t m j
Que letra continua m v t m j Iu health pain management
Iu health pain management National business group on health conference 2018
National business group on health conference 2018 Health and social care component 3 health and wellbeing
Health and social care component 3 health and wellbeing 30 days has september april june and november
30 days has september april june and november April may june july
April may june july Gartner infrastructure and operations summit
Gartner infrastructure and operations summit Gartner cio agenda
Gartner cio agenda Gartner application portfolio management
Gartner application portfolio management Elevated land with sloping sides and rounded summit
Elevated land with sloping sides and rounded summit Atd data and analytics summit
Atd data and analytics summit Spirituality and addiction
Spirituality and addiction Differentiate between health education and health promotion
Differentiate between health education and health promotion Chapter 3 health wellness and health disparities
Chapter 3 health wellness and health disparities Difference between counselling and health education
Difference between counselling and health education Chapter 1 lesson 2 what affects your health
Chapter 1 lesson 2 what affects your health Chapter 1 understanding health and wellness
Chapter 1 understanding health and wellness June 2010 physics regents answers
June 2010 physics regents answers June 2005 calendar
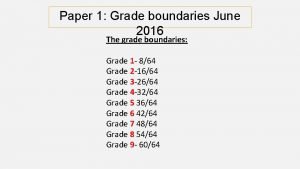
June 2005 calendar June 2016 grade boundaries
June 2016 grade boundaries Good morning 1 june
Good morning 1 june Corn be heavy soon meaning
Corn be heavy soon meaning June 2010 chemistry regents
June 2010 chemistry regents Welcome june blessings
Welcome june blessings English paper 1 june 2021
English paper 1 june 2021 Grade 7 life orientation term 2 notes
Grade 7 life orientation term 2 notes Good morning welcome june
Good morning welcome june Britney spears educational background
Britney spears educational background Lessons by lenore hetrick
Lessons by lenore hetrick June cheetah wegener
June cheetah wegener Symbolism in the lottery
Symbolism in the lottery June canavan foundation
June canavan foundation Liz owns stock in nar heating/cooling and cilla shipping
Liz owns stock in nar heating/cooling and cilla shipping Nasa june 19 2008
Nasa june 19 2008 New irpwm june 2020
New irpwm june 2020 June 20 2008
June 20 2008 Simplissimus
Simplissimus June's journey
June's journey Good morning please
Good morning please Flacs b exam
Flacs b exam Summary period: june 2021 poem
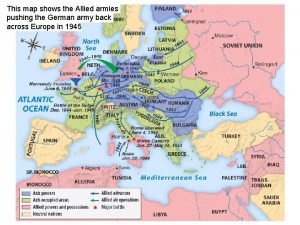
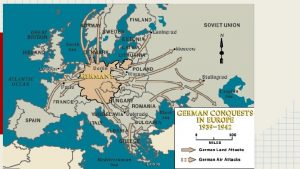
Summary period: june 2021 poem The map shows that allied forces
The map shows that allied forces Proper noun girl names
Proper noun girl names Elephant riding in phuket respuestas
Elephant riding in phuket respuestas June too soon july stand by
June too soon july stand by Ciara earley
Ciara earley Chapter 2 childhood years in calamba summary
Chapter 2 childhood years in calamba summary June 22 to july 22
June 22 to july 22 June 6th 1944
June 6th 1944 June budhooram
June budhooram 1215 king
1215 king June preschool newsletter
June preschool newsletter June 23
June 23 Confined placental mosaicism
Confined placental mosaicism June f
June f June safety tips
June safety tips June 23
June 23 January 2012 chemistry regents
January 2012 chemistry regents John 20:19-22
John 20:19-22 Holy june
Holy june Companies in june
Companies in june 1 june children's day
1 june children's day Lake june head start
Lake june head start Dr june james
Dr june james Network weaver
Network weaver Milton glaser biography
Milton glaser biography June ward
June ward 2019 june calendar
2019 june calendar Solar installation summit county
Solar installation summit county Summit county probation
Summit county probation Summit county continuum of care
Summit county continuum of care Microsoft summit sydney 2017
Microsoft summit sydney 2017 What is rio de janeiro earth summit 1992
What is rio de janeiro earth summit 1992 Mashup summit
Mashup summit Summit oak ridge
Summit oak ridge Open infrastructure summit 2019
Open infrastructure summit 2019 Jd edwards summit
Jd edwards summit Misys summit ft
Misys summit ft Summit iptv
Summit iptv Jmp summit 2017
Jmp summit 2017 Gdrc business summit
Gdrc business summit Gartner bi summit 2016
Gartner bi summit 2016