Paediatric Sepsis Recognizing the many faces KPA Annual



- Slides: 58

Paediatric Sepsis: Recognizing the many faces KPA Annual congress 9 th April 2019 Wahu g. r ID specialist

A B D C
Outline Background and Introduction Sepsis Overview and New Guidelines? ? thoughts Management Principles The oldest and most elusive syndrome in medical history
How do we recognize sepsis? • Busy OPDs • Fever is the commonest cause for hospital visits Lab investigations in OPDs for suspected sepsis: Blood collection not easy in sick kids Often unavailable in OPD settings Take time Cost
Case I • Three year old child; presents with four days of fever, rash and right cervical adenopathy • Very irritable and hard to examine • Nodes erythematous and tender • HR 155 RR 45 BP 65/35; WBC 27 K with 75% neutrophils, 5% bands; CRP 195 ug/d. L; Lactate 2. 5 • Sepsis? ? • Given fluids; Blood Cultures done; Antibiotics given • U/S of node—no drainable focus • Sepsis? ?
Case I • Following day‐ Tachycardic to 200 with gallop rhythm • BP in the 50 s systolic • Hands and feet cool and poorly perfused • New rash in groin, trunk and extremities • Blood cultures negative • Node still enlarged • WBC now 35, 000 and CRP over 250 ug/d. L • Sepsis? ?
Case I • Transferred to the PICU‐ • Cardiac echo with mitral and tricuspid insufficiency and regurgitation, cardiac output ~ 23%; Started pressors; • Diagnosis? ? ? • Given IVIG and during the infusion his cardiac insufficiency began to abate and within 24 hours he was markedly improved and recovered slowly without cardiac sequelae
Case II • Three week old male with “UTI” and elevated WBC (>50, 000) who just did not get better with antibiotics for his UTI. • Transferred when WBC reached 90, 000 after 4 days of antibiotics and fever was still around 400 C • Tachycardia for age with elevated respiratory rate but BP was WNL for his age. Hands and feet swollen red and tender…. CRP very elevated over 200 ug/d. L. • Does he have sepsis? • Flow cytometry revealed a clonal Acute myelogenous leukemia (type MM 3) • He was started on chemotherapy and rapidly defervesced
Case III • Three month old former 32 week preemie twin with past history of necrotizing enterocolitis (NEC) • Surgical intervention and ostomy/stoma creation in first week of life; Re‐anastomosis 1 month ago. • Presents with respiratory and circulatory collapse. • Initially felt to have gram negative sepsis‐abdominal origin. • Within 24 hours after admission, noted to have small (1 cm) “purple” splotch—within hours this blossomed into…. • What is this diagnosis?
Case III • “stool” E coli, Enterococcus, Bacteroides, • Blood‐Streptococcus viridans; Staphylococcus epidermidis, • Most likely this was a synergistic infection; Polymicrobial (anaerobes and E coli+/‐ enterococcus) in a compromised host due to age and multiple surgeries)
Background • A significant public health burden and a leading cause of morbidity and mortality among infants and children across the world • Prevalence of pediatric severe sepsis has increased from 6. 2% to 7. 7% over the past decade • Mortality has decreased over time‐ continues to be high‐ estimated to be 9% for all‐cause mortality, and as high as 25% for those patients admitted to the intensive care unit (ICU) • Among sepsis survivors, approximately one‐fifth have at least moderate disability; long‐term physical, psychological, and cognitive disabilities • Pediatric sepsis is also associated with significant resource utilization and accounts for $4. 8 billion in healthcare costs in the United States
Background • A life‐threatening condition; affects many children regardless of some underlying healthcare issues • Timely recognition, evaluation, and treatment of pediatric sepsis are crucial when considering the pediatric patient who presents in shock • Many children reported to die from other underlying conditions actually die directly from sepsis. • The management of pediatric sepsis was comprehensively advocated through systematic review process in the Surviving Sepsis Campaign guidelines (SSCG) 2008 and 2012 • Many recommendations and suggestions based on low quality evidence and expert consensus, and sometimes only on evidence in adult sepsis. • Latest version of SSCG did not include a specific description of the management of pediatric sepsis
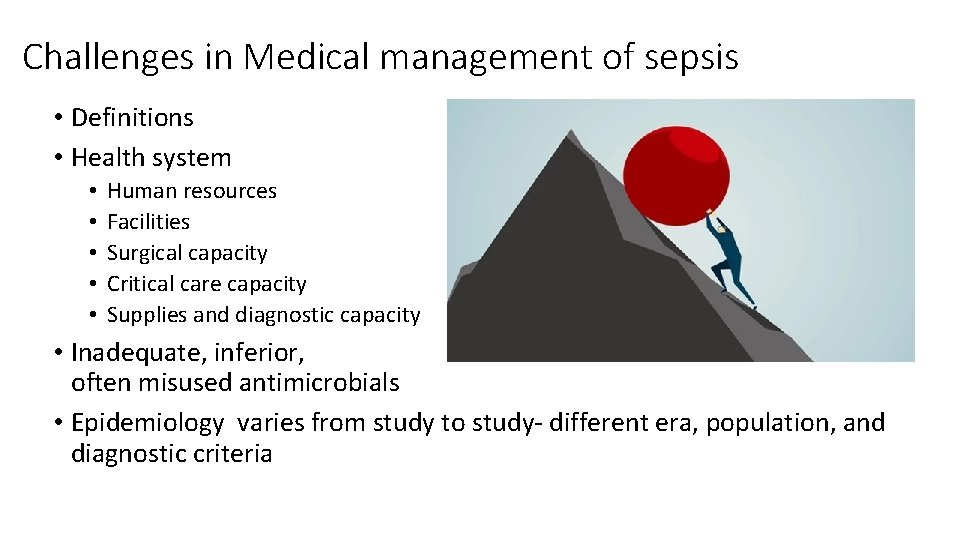
Challenges in Medical management of sepsis • Definitions • Health system • • • Human resources Facilities Surgical capacity Critical care capacity Supplies and diagnostic capacity • Inadequate, inferior, and often misused antimicrobials • Epidemiology varies from study to study‐ different era, population, and diagnostic criteria
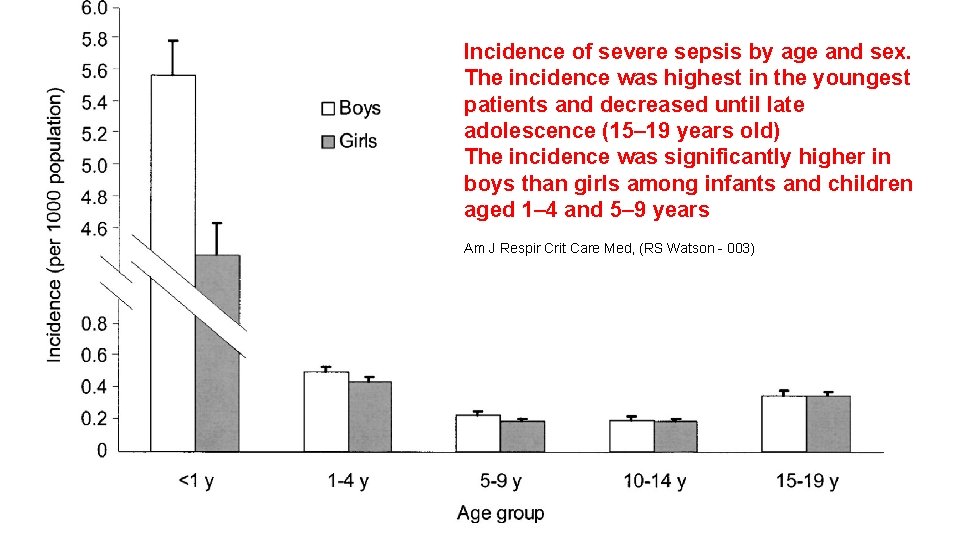
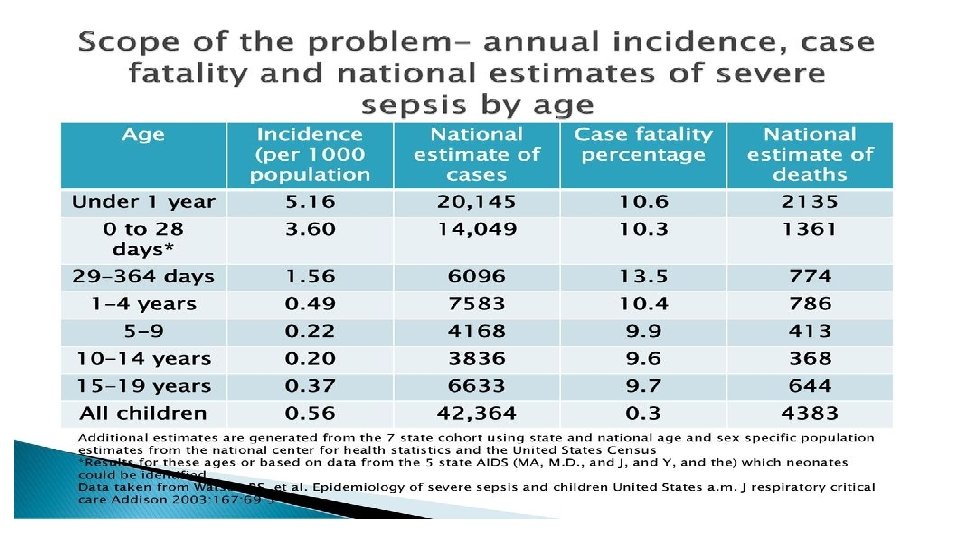
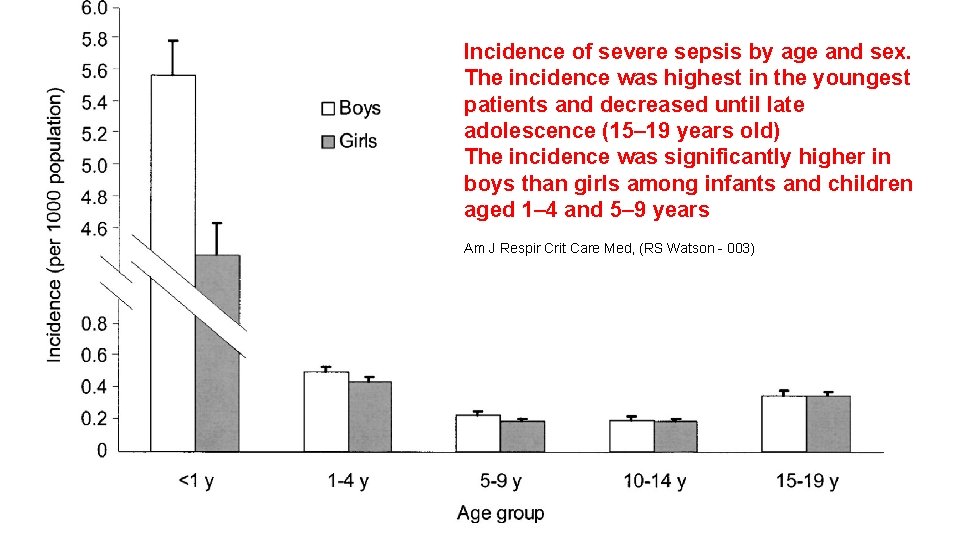
Incidence of severe sepsis by age and sex. The incidence was highest in the youngest patients and decreased until late adolescence (15– 19 years old) The incidence was significantly higher in boys than girls among infants and children aged 1– 4 and 5– 9 years Am J Respir Crit Care Med, (RS Watson - 003)
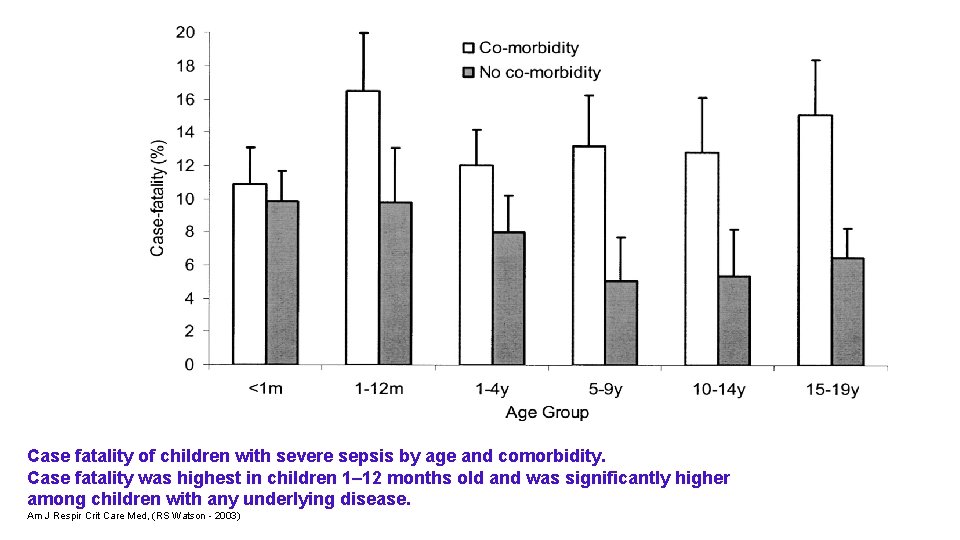
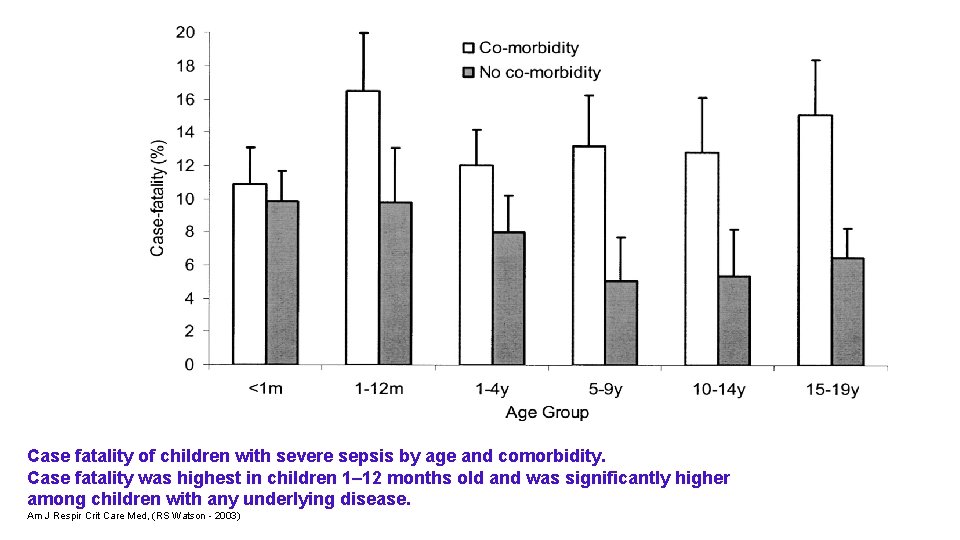
Case fatality of children with severe sepsis by age and comorbidity. Case fatality was highest in children 1– 12 months old and was significantly higher among children with any underlying disease. Am J Respir Crit Care Med, (RS Watson - 2003)
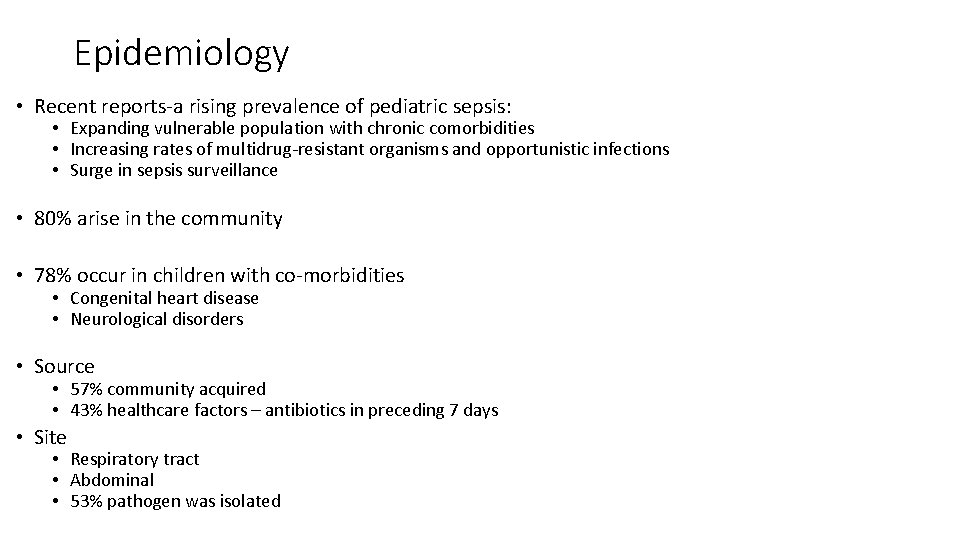
Epidemiology • Recent reports‐a rising prevalence of pediatric sepsis: • Expanding vulnerable population with chronic comorbidities • Increasing rates of multidrug‐resistant organisms and opportunistic infections • Surge in sepsis surveillance • 80% arise in the community • 78% occur in children with co‐morbidities • Congenital heart disease • Neurological disorders • Source • 57% community acquired • 43% healthcare factors – antibiotics in preceding 7 days • Site • Respiratory tract • Abdominal • 53% pathogen was isolated
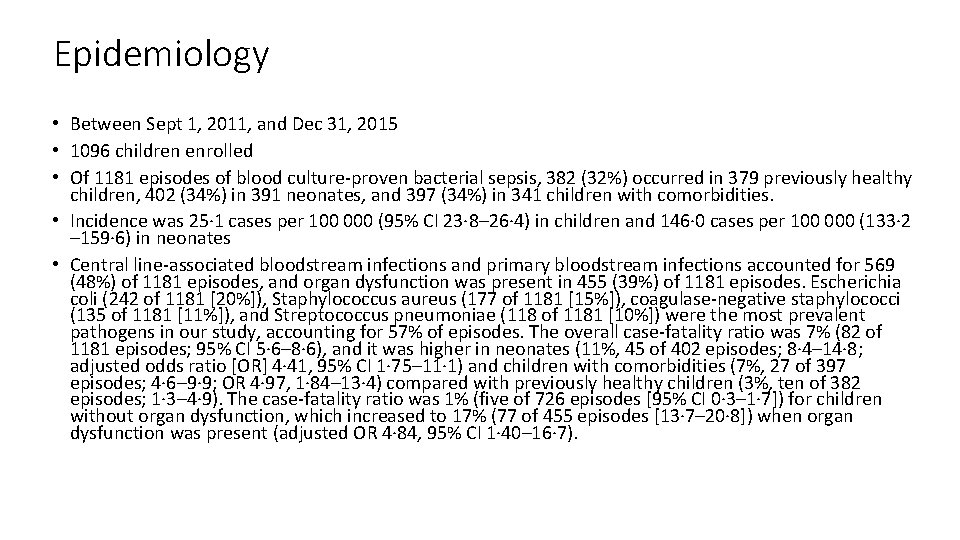
Epidemiology • Between Sept 1, 2011, and Dec 31, 2015 • 1096 children enrolled • Of 1181 episodes of blood culture‐proven bacterial sepsis, 382 (32%) occurred in 379 previously healthy children, 402 (34%) in 391 neonates, and 397 (34%) in 341 children with comorbidities. • Incidence was 25· 1 cases per 100 000 (95% CI 23· 8– 26· 4) in children and 146· 0 cases per 100 000 (133· 2 – 159· 6) in neonates • Central line‐associated bloodstream infections and primary bloodstream infections accounted for 569 (48%) of 1181 episodes, and organ dysfunction was present in 455 (39%) of 1181 episodes. Escherichia coli (242 of 1181 [20%]), Staphylococcus aureus (177 of 1181 [15%]), coagulase‐negative staphylococci (135 of 1181 [11%]), and Streptococcus pneumoniae (118 of 1181 [10%]) were the most prevalent pathogens in our study, accounting for 57% of episodes. The overall case‐fatality ratio was 7% (82 of 1181 episodes; 95% CI 5· 6– 8· 6), and it was higher in neonates (11%, 45 of 402 episodes; 8· 4– 14· 8; adjusted odds ratio [OR] 4· 41, 95% CI 1· 75– 11· 1) and children with comorbidities (7%, 27 of 397 episodes; 4· 6– 9· 9; OR 4· 97, 1· 84– 13· 4) compared with previously healthy children (3%, ten of 382 episodes; 1· 3– 4· 9). The case‐fatality ratio was 1% (five of 726 episodes [95% CI 0· 3– 1· 7]) for children without organ dysfunction, which increased to 17% (77 of 455 episodes [13· 7– 20· 8]) when organ dysfunction was present (adjusted OR 4· 84, 95% CI 1· 40– 16· 7).
Epidemiology • The burden of blood culture‐proven bacterial sepsis on child health remains considerable • Key differences in predominant organisms, severity, and outcome between neonates, previously healthy children, and children with comorbidities recorded • Although for most episodes of blood culture‐proven bacterial sepsis, no organ dysfunction was seen, presence of organ dysfunction was strongly associated with mortality • Dr Philipp K A Agyeman et al; Epidemiology of blood culture-proven bacterial sepsis in children in Switzerland: a population-based cohort study. Lancet adolescent and child health 2017
Epidemiology • Out of 187 cases, 61 were in the intensive care unit (ICU), 98 in the infectious disease ward, and 28 in the internal medicine ward. • Correct diagnosis of sepsis in the ICU, internal and infectious diseases wards were made in 16 (26. 2%), 4 (14. 3%) and 71 (72. 4%) cases, respectively. • Appropriate treatments for sepsis in the ICU, internal and infectious wards were applied in 12 (19. 7%), 3 (10. 7%) and 61 (78. 2%) cases, respectively • Ninety‐one patients (48. 6%) were diagnosed correctly (true sepsis) and 76 (40. 6%) were treated with proper regimes. • Conclusions: Inappropriate and unnecessary use of antibiotics by patients with preliminary diagnosis of sepsis in our hospital, similar to other parts of the world, was high. • Bacterial Sepsis: Challenges of Diagnosis and Treatment in a Teaching Hospital Southwest of Iran; Jundishapur J Microbiol. 2014 Mar; 7(3): e 9082
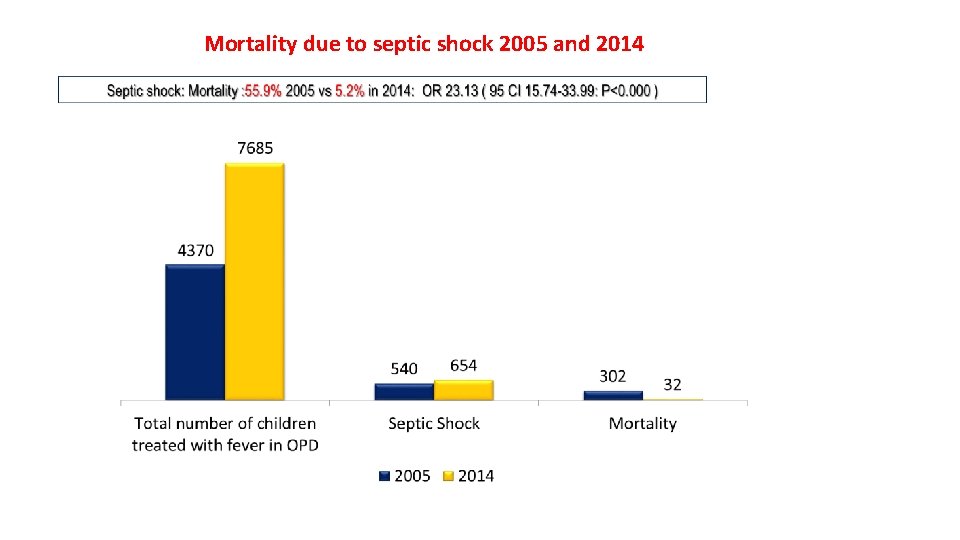
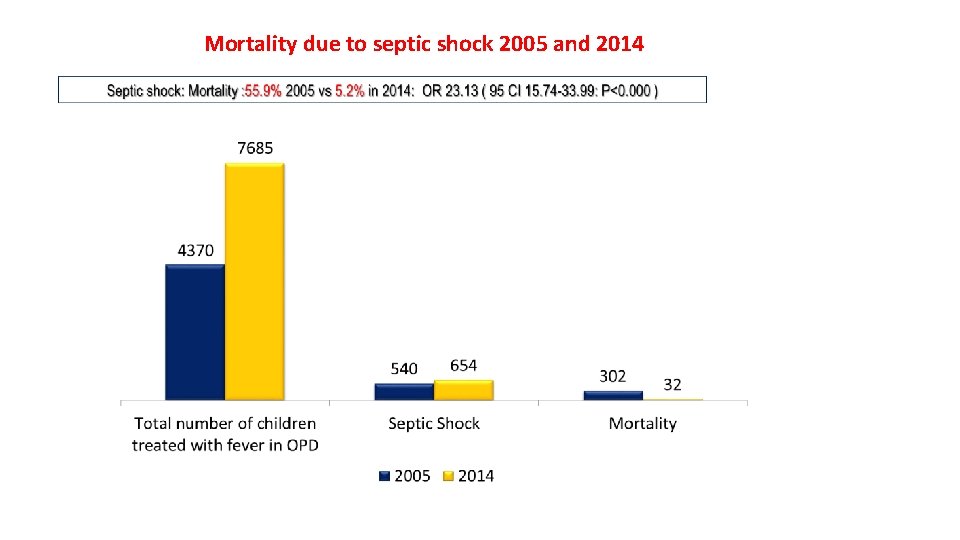
Mortality due to septic shock 2005 and 2014
Definition-What is sepsis? • 1991 consensus conference‐ initial definitions‐ focused on then prevailing view that sepsis resulted from a host’s systemic inflammatory response syndrome • Sepsis complicated by organ dysfunction was termed severe sepsis, which could progress to septic shock, defined as “sepsis‐induced hypotension persisting despite adequate fluid resuscitation. ” • 2001 task force, recognizing limitations with these definitions, expanded the list of diagnostic criteria‐ did not offer alternatives because of the lack of supporting evidence
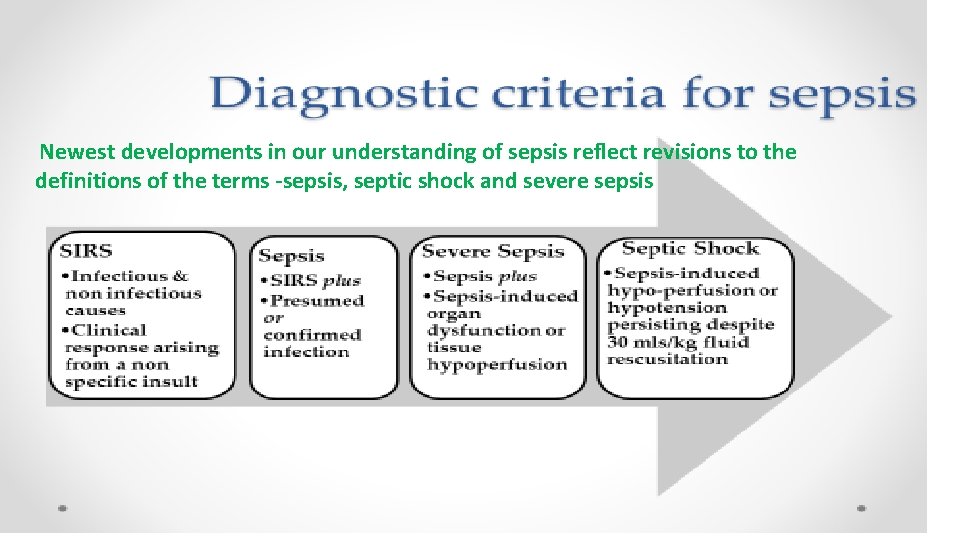
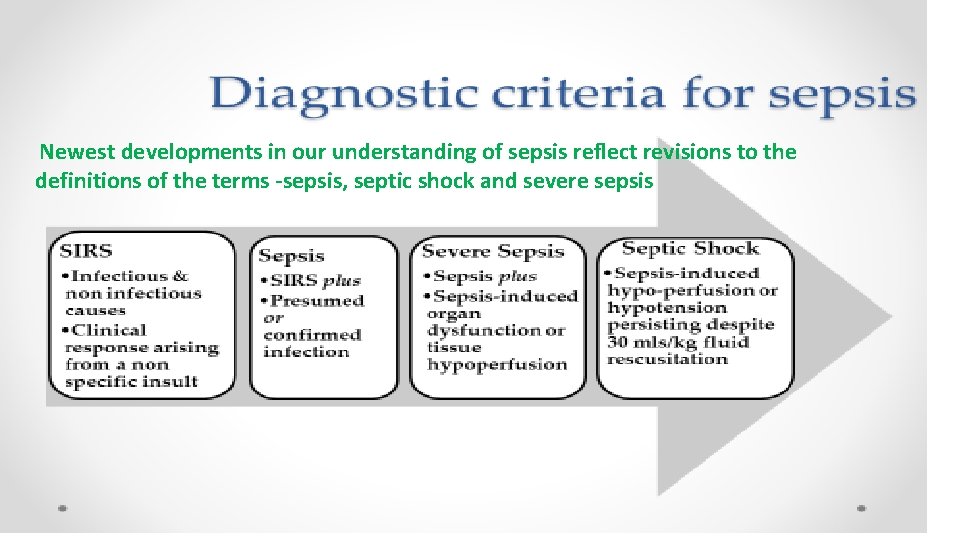
Newest developments in our understanding of sepsis reflect revisions to the definitions of the terms -sepsis, septic shock and severe sepsis
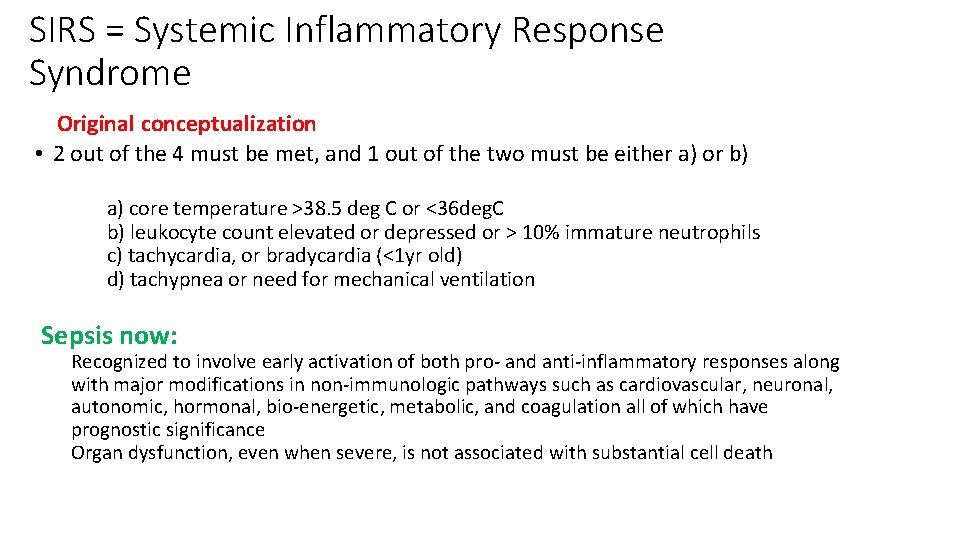
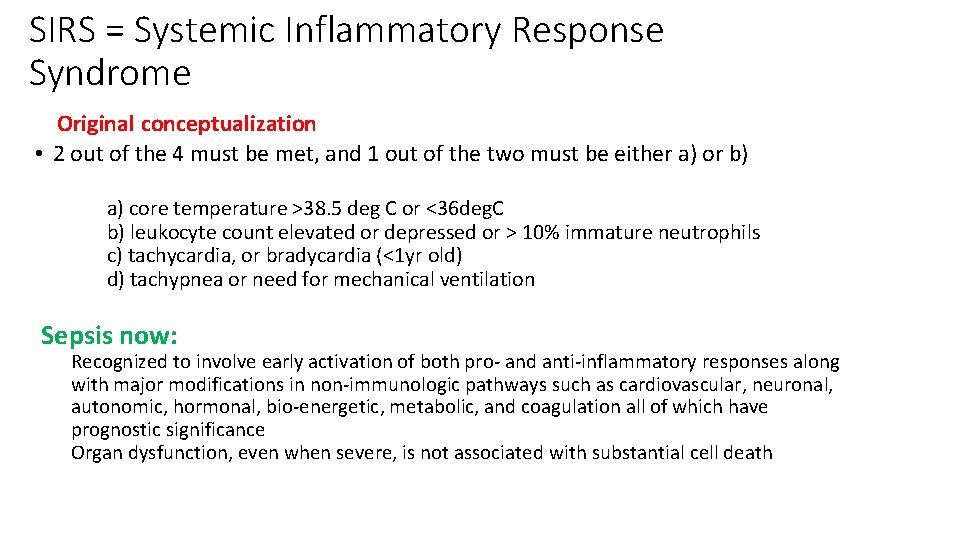
SIRS = Systemic Inflammatory Response Syndrome Original conceptualization • 2 out of the 4 must be met, and 1 out of the two must be either a) or b) a) core temperature >38. 5 deg C or <36 deg. C b) leukocyte count elevated or depressed or > 10% immature neutrophils c) tachycardia, or bradycardia (<1 yr old) d) tachypnea or need for mechanical ventilation Sepsis now: Recognized to involve early activation of both pro‐ and anti‐inflammatory responses along with major modifications in non‐immunologic pathways such as cardiovascular, neuronal, autonomic, hormonal, bio‐energetic, metabolic, and coagulation all of which have prognostic significance Organ dysfunction, even when severe, is not associated with substantial cell death
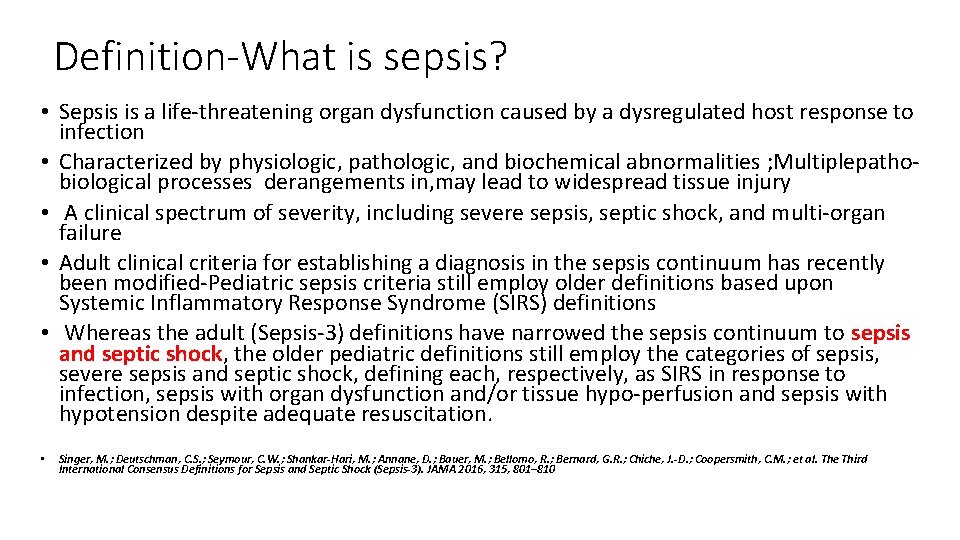
Definition-What is sepsis? • Sepsis is a life‐threatening organ dysfunction caused by a dysregulated host response to infection • Characterized by physiologic, pathologic, and biochemical abnormalities ; Multiplepatho‐ biological processes derangements in, may lead to widespread tissue injury • A clinical spectrum of severity, including severe sepsis, septic shock, and multi‐organ failure • Adult clinical criteria for establishing a diagnosis in the sepsis continuum has recently been modified‐Pediatric sepsis criteria still employ older definitions based upon Systemic Inflammatory Response Syndrome (SIRS) definitions • Whereas the adult (Sepsis‐ 3) definitions have narrowed the sepsis continuum to sepsis and septic shock, the older pediatric definitions still employ the categories of sepsis, severe sepsis and septic shock, defining each, respectively, as SIRS in response to infection, sepsis with organ dysfunction and/or tissue hypo‐perfusion and sepsis with hypotension despite adequate resuscitation. • Singer, M. ; Deutschman, C. S. ; Seymour, C. W. ; Shankar-Hari, M. ; Annane, D. ; Bauer, M. ; Bellomo, R. ; Bernard, G. R. ; Chiche, J. -D. ; Coopersmith, C. M. ; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801– 810
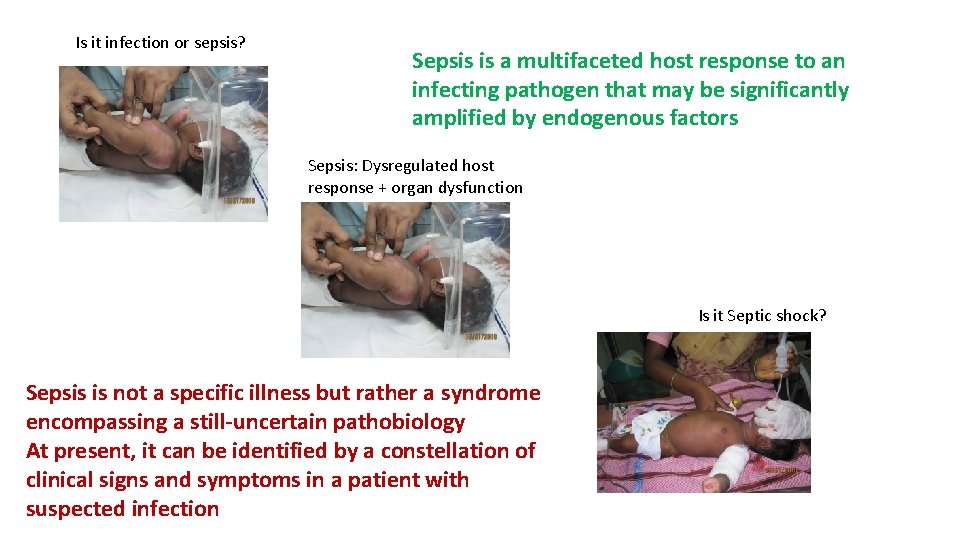
Is it infection or sepsis? Sepsis is a multifaceted host response to an infecting pathogen that may be significantly amplified by endogenous factors Sepsis: Dysregulated host response + organ dysfunction Is it Septic shock? Sepsis is not a specific illness but rather a syndrome encompassing a still-uncertain pathobiology At present, it can be identified by a constellation of clinical signs and symptoms in a patient with suspected infection
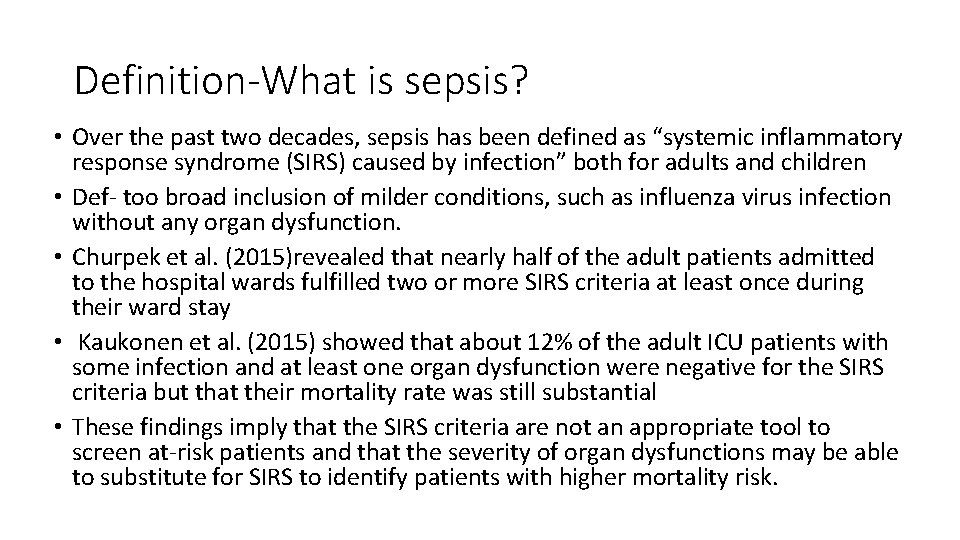
Definition-What is sepsis? • Over the past two decades, sepsis has been defined as “systemic inflammatory response syndrome (SIRS) caused by infection” both for adults and children • Def‐ too broad inclusion of milder conditions, such as influenza virus infection without any organ dysfunction. • Churpek et al. (2015)revealed that nearly half of the adult patients admitted to the hospital wards fulfilled two or more SIRS criteria at least once during their ward stay • Kaukonen et al. (2015) showed that about 12% of the adult ICU patients with some infection and at least one organ dysfunction were negative for the SIRS criteria but that their mortality rate was still substantial • These findings imply that the SIRS criteria are not an appropriate tool to screen at‐risk patients and that the severity of organ dysfunctions may be able to substitute for SIRS to identify patients with higher mortality risk.
Variable Definitions-Sepsis • Current use of 2 or more SIRS criteria to identify sepsis was unanimously considered by the task force to be unhelpful • Changes in white blood cell count, temperature, and heart rate reflect inflammation, the host response to “danger” in the form of infection or other insults • The SIRS criteria do not necessarily indicate a dysregulated, life‐threatening response • SIRS criteria are present in many hospitalized patients, including those who never develop infection and never incur adverse outcomes (poor discriminant validity) • 1 in 8 patients admitted to critical care units in Australia and New Zealand with infection and new organ failure did not have the requisite minimum of 2 SIRS criteria to fulfill the definition of sepsis (poor concurrent validity) yet had protracted courses with significant morbidity and mortality. • Discriminant validity(present in many hospitalized patients, including those who never develop infection and never incur adverse outcomes) and convergent validity constitute the 2 domains of construct validity; the SIRS criteria thus perform poorly on both counts.
Sepsis-3 • Inclusion of two SIRS criteria did not provide appropriate discrimination between those suffering sepsis and an appropriate physiological response to insult (infection or otherwise) • Likewise, many patients with two or more SIRS criteria never go on to develop an infection or sepsis • Taking these issues into consideration, new sepsis criteria were advocated as “Sepsis‐ 3” in 2017, which redefined sepsis as infection complicated by one or more organ dysfunctions • Organ system dysfunctions are assessed with an increase in the Sequential Organ Failure Assessment (SOFA) score by 2 or more points • Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016; 315(8): 801 – 10
New definitions from Sepsis-3: Sepsis, severe sepsis and the SOFA score • The 2012 sepsis guidelines defined sepsis as ‘the presence (probable or documented) of infection together with systemic manifestations of infection'. • In the 2016 guidelines, sepsis is redefined by the taskforce as ‘a life‐ threatening organ dysfunction caused by a dysregulated host response to infection' • This new definition highlights the three critical components of sepsis: v. Presence of infection v. Abnormal regulation of the host response to infection v. Resulting organ system dysfunction as a result of the host response
New definitions from Sepsis-3: Sepsis, severe sepsis and the SOFA score • One of the most significant changes in the new definitions was the elimination of a defined condition of systemic inflammatory response syndrome (SIRS). • The SIRS criteria have included temperature >38°C or <36°C, heart rate more than 90 beats per minute, respiratory rate of more than 20 breaths per minute and white blood cell count >12000/µL or <4000/µL or >10%immature (band) forms • Traditionally, more than two SIRS criteria were felt to represent patients at risk of or suffering from sepsis • The taskforce determined that the inclusion of two SIRS criteria did not provide appropriate discrimination between those suffering sepsis and an appropriate physiological response to insult (infection or otherwise) • Likewise, many patients with two or more SIRS criteria never go on to develop an infection or sepsis
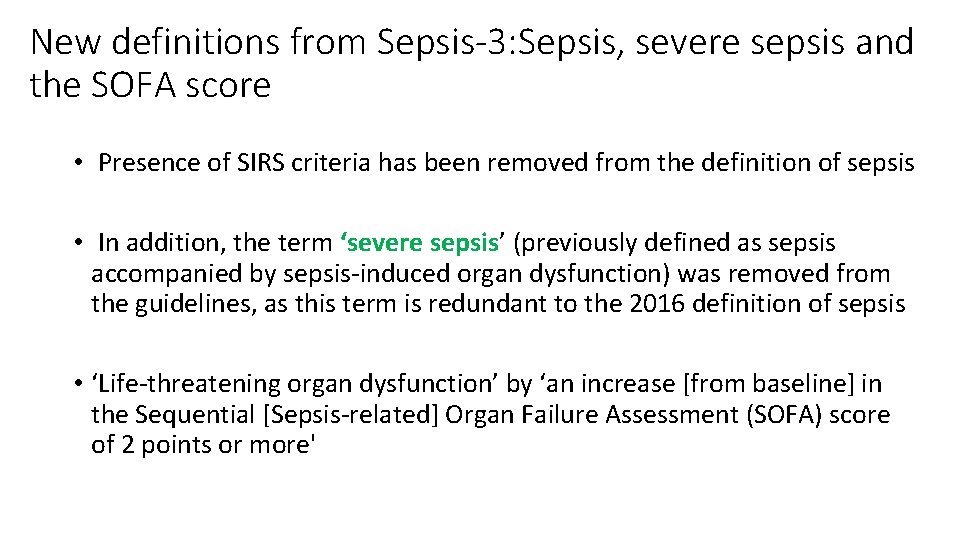
New definitions from Sepsis-3: Sepsis, severe sepsis and the SOFA score • Presence of SIRS criteria has been removed from the definition of sepsis • In addition, the term ‘severe sepsis’ (previously defined as sepsis accompanied by sepsis‐induced organ dysfunction) was removed from the guidelines, as this term is redundant to the 2016 definition of sepsis • ‘Life‐threatening organ dysfunction’ by ‘an increase [from baseline] in the Sequential [Sepsis‐related] Organ Failure Assessment (SOFA) score of 2 points or more'
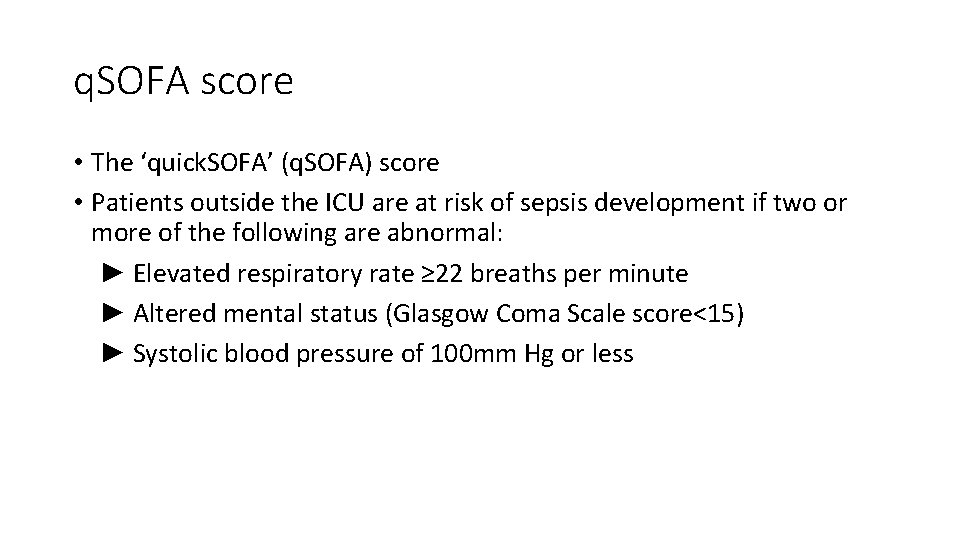
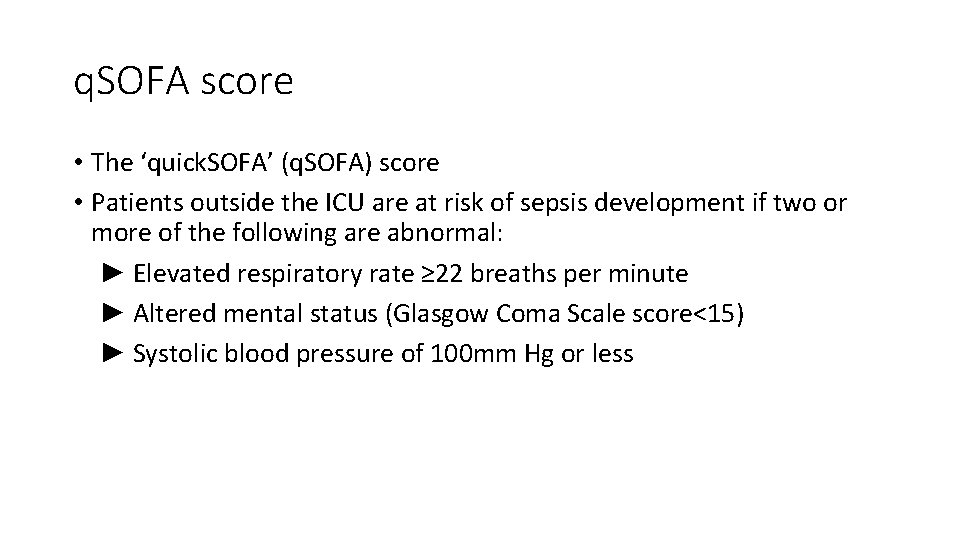
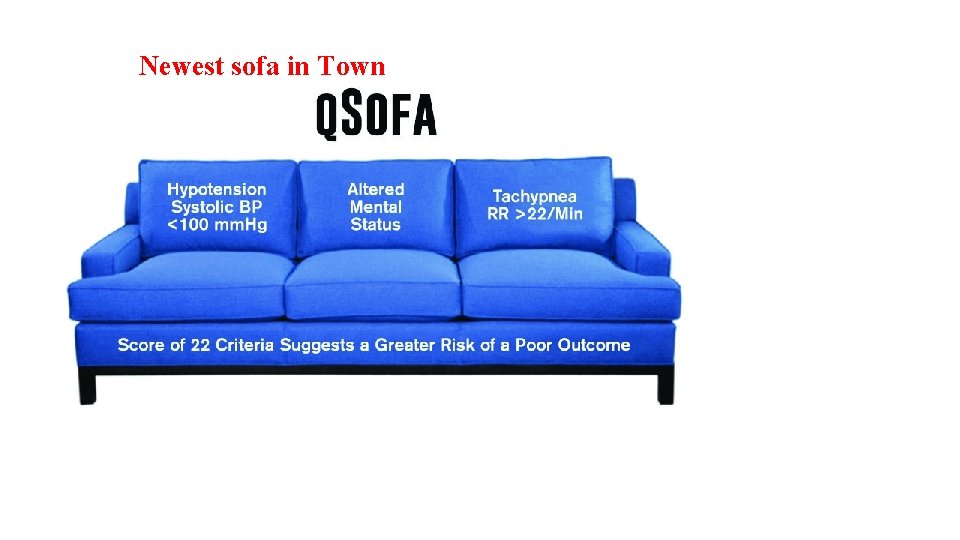
q. SOFA score • The ‘quick. SOFA’ (q. SOFA) score • Patients outside the ICU are at risk of sepsis development if two or more of the following are abnormal: ► Elevated respiratory rate ≥ 22 breaths per minute ► Altered mental status (Glasgow Coma Scale score<15) ► Systolic blood pressure of 100 mm Hg or less
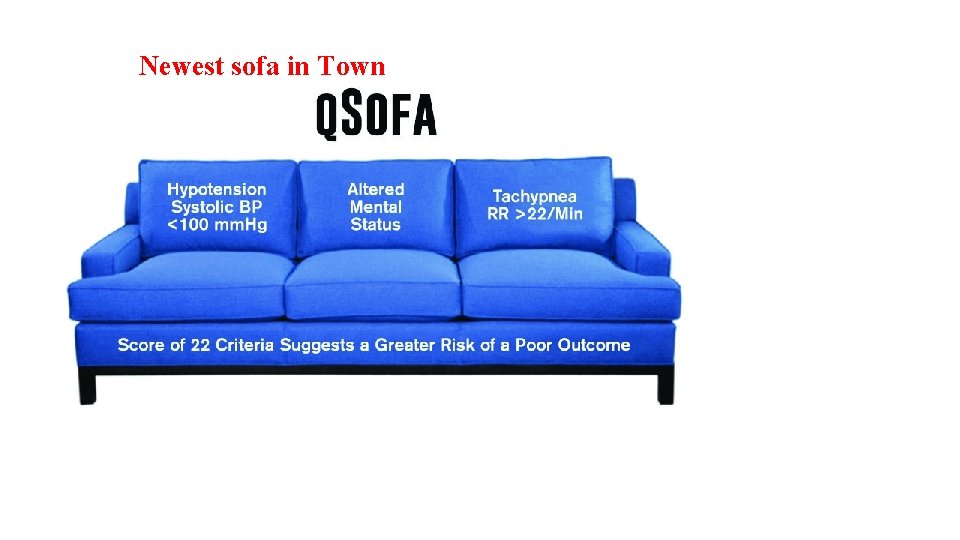
Newest sofa in Town
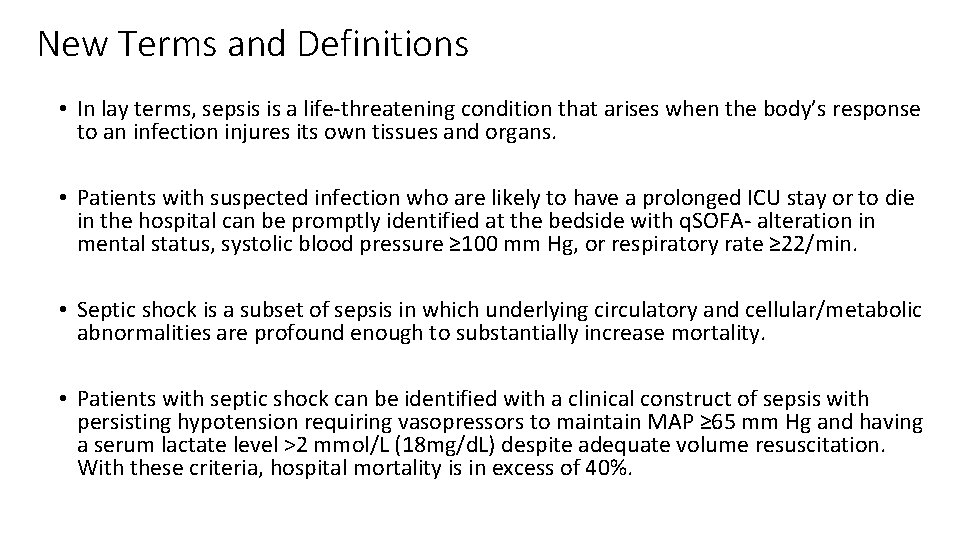
New Terms and Definitions • In lay terms, sepsis is a life‐threatening condition that arises when the body’s response to an infection injures its own tissues and organs. • Patients with suspected infection who are likely to have a prolonged ICU stay or to die in the hospital can be promptly identified at the bedside with q. SOFA‐ alteration in mental status, systolic blood pressure ≥ 100 mm Hg, or respiratory rate ≥ 22/min. • Septic shock is a subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality. • Patients with septic shock can be identified with a clinical construct of sepsis with persisting hypotension requiring vasopressors to maintain MAP ≥ 65 mm Hg and having a serum lactate level >2 mmol/L (18 mg/d. L) despite adequate volume resuscitation. With these criteria, hospital mortality is in excess of 40%.
New definitions from Sepsis-3: Sepsis, severe sepsis and the SOFA score • Baseline SOFA score is zero unless a patient has known pre‐existing organ dysfunction before the onset of current infection • SOFA score‐used as an indicator of organ dysfunction: ØFamiliar to most clinicians ØChange in SOFA score is more predictive of in‐hospital mortality from sepsis than the presence of SIRS criteria • Patients with an increase of 2 or more in the SOFA score have an estimated in hospital mortality of 10% due to sepsis and a 2‐fold to 25‐fold increased risk of death compared with patients with a SOFA score of <2. 3 • Patients with sepsis meeting this definition are recommended to be observed in a location with a ‘greater level of monitoring’ than a routine inpatient floor environment
Variable Definitions-Organ Dysfunction or Failure • The predominant score in current use is the Sequential Organ Failure Assessment (SOFA) (originally the Sepsis‐related Organ Failure Assessment) • The score grades abnormality by organ system and accounts for clinical interventions • Laboratory variables, namely, Pa. O 2, platelet count, creatinine level, and bilirubin level, are needed for full computation • Selection of variables and cutoff values were developed by consensus, and SOFA is not well known outside the critical care community
Variable Definitions-Septic Shock • Septic shock is defined as a subset of sepsis in which underlying circulatory and cellular metabolism abnormalities are profound enough to substantially increase mortality • The 2001 task force definitions described septic shock as “a state of acute circulatory failure. ” • The task force favored a broader view to differentiate septic shock from cardiovascular dysfunction alone and to recognize the importance of cellular abnormalities • There was unanimous agreement that septic shock should reflect a more severe illness with a much higher likelihood of death than sepsis alone.
A Need for Sepsis Definitions for the Public and for Health Care Practitioners • Despite its worldwide importance, public awareness of sepsis is poor • Various manifestations of sepsis make diagnosis difficult, even for experienced clinicians • Underscore the fact. S: • Public needs an understandable definition of sepsis • Health care practitioners require improved clinical prompts and diagnostic approaches to facilitate earlier identification and an accurate quantification of the burden of sepsis
A Need for Sepsis Definitions for the Public and for Health Care Practitioners • If we have the right diagnosis we have more targeted treatment and less unnecessary treatment with antimalarials, antivirals and antibiotics, anti‐fungals • It is important to focus on health care workers skills; they should know how to diagnose sepsis and that it looks different in neonates and older chidren • In countries with high malaria prevalence it is important to recognize that not every fever is malaria • Antigen tests, polymerase chain reaction and other tests all have a cost. What kind of test is appropriate? Accurate diagnosis of tropical diseases is crucial. • Tools that will help them health care workers to decide whether the patient has an infection or sepsis need to be availed • In the case of sepsis, time is life • Critical care services in LMICs lack resources‐ Clinical vital signs are very important in diagnosis.
Key Concepts of Sepsis • Sepsis is the primary cause of death from infection, especially if not recognized and treated promptly‐ Its recognition mandates urgent attention. • Sepsis is a syndrome shaped by pathogen factors and host factors (eg, sex, race and other genetic determinants, age, comorbidities, environment) with characteristics that evolve over time. What differentiates sepsis from infection is an aberrant or dysregulated host response and the presence of organ dysfunction. • Sepsis‐induced organ dysfunction may be occult; therefore, its presence should be considered in any patient presenting with infection. Conversely, unrecognized infection may be the cause of new‐onset organ dysfunction. Any unexplained organ dysfunction should thus raise the possibility of underlying infection • The clinical and biological phenotype of sepsis can be modified by preexisting acute illness, long‐standing comorbidities, medication, and interventions. • Specific infections may result in local organ dysfunction without generating a dysregulated systemic host response
New Terms and Definitions • In lay terms, sepsis is a life‐threatening condition that arises when the body’s response to an infection injures its own tissues and organs. • Patients with suspected infection who are likely to have a prolonged ICU stay or to die in the hospital can be promptly identified at the bedside with q. SOFA, ie, alteration in mental status, systolic blood pressure ≥ 100 mm Hg, or respiratory rate ≥ 22/min. • Septic shock is a subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality. • Patients with septic shock can be identified with a clinical construct of sepsis with persisting hypotension requiring vasopressors to maintain MAP ≥ 65 mm Hg and having a serum lactate level >2 mmol/L (18 mg/d. L) despite adequate volume resuscitation. With these criteria, hospital mortality is in excess of 40%.
Diagnosis-Laboratory Studies Blood and urine studies Complete blood count (CBC) Clotting function and coagulation parameters Electrolyte level tests, renal and liver function tests, and other chemistry Serum transaminase levels and other measures of liver dysfunction are often elevated in situations such as disseminated viral and anaerobic infections. • Etiology‐specific serologies may be helpful, and urinalysis may have a role in clarifying the level of risk of urinary tract infection in infants and children. • Non–culture‐based molecular modalities and other diagnostic methods are becoming increasingly important • Inflammatory markers and acute‐phase reactants (e. g. , erythrocyte sedimentation rate [ESR], C‐reactive protein [CRP], interleukin [IL]– 1 b, IL‐ 6, IL‐ 8, tumor necrosis factor–alpha, leukotriene B 4, procalcitonin [PCT]) • • •
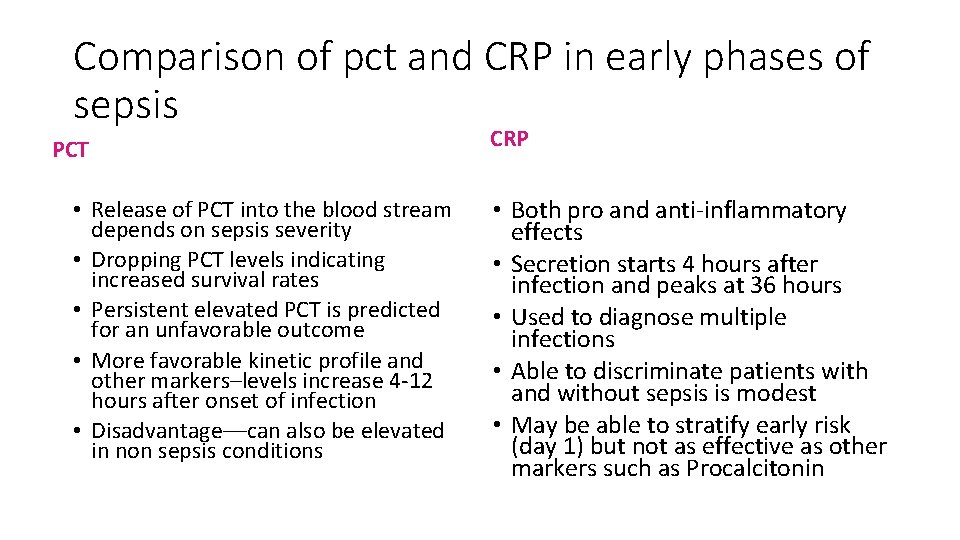
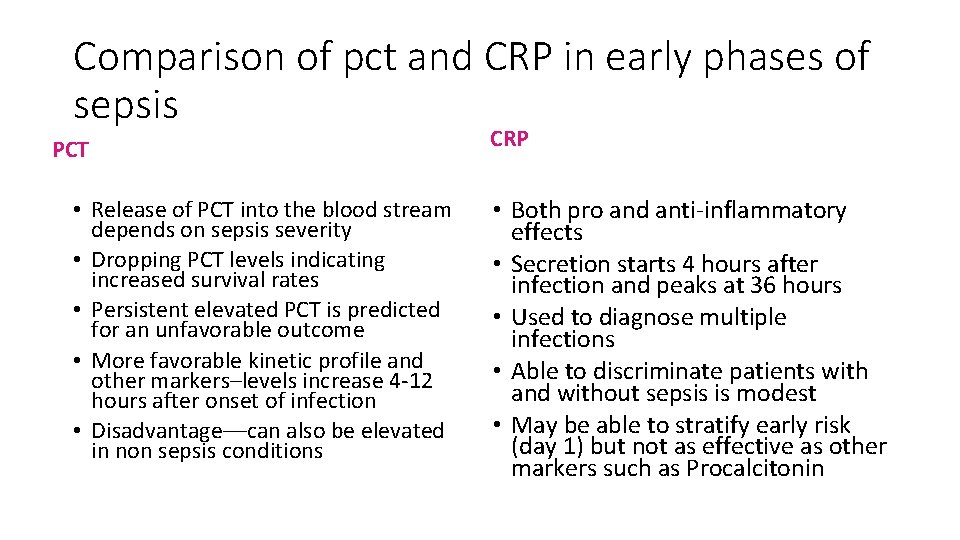
Comparison of pct and CRP in early phases of sepsis PCT • Release of PCT into the blood stream depends on sepsis severity • Dropping PCT levels indicating increased survival rates • Persistent elevated PCT is predicted for an unfavorable outcome • More favorable kinetic profile and other markers–levels increase 4‐ 12 hours after onset of infection • Disadvantage––can also be elevated in non sepsis conditions CRP • Both pro and anti‐inflammatory effects • Secretion starts 4 hours after infection and peaks at 36 hours • Used to diagnose multiple infections • Able to discriminate patients with and without sepsis is modest • May be able to stratify early risk (day 1) but not as effective as other markers such as Procalcitonin
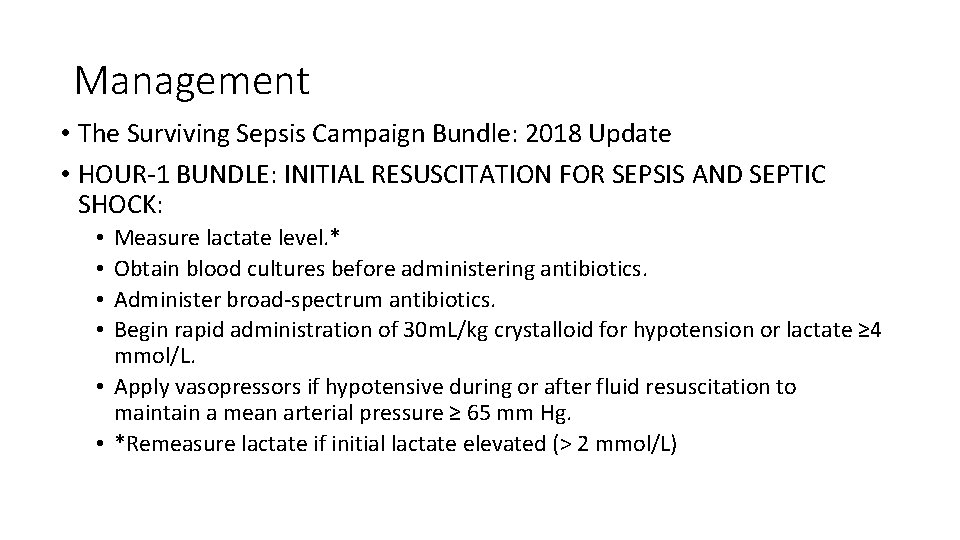
Management • The Surviving Sepsis Campaign Bundle: 2018 Update • HOUR‐ 1 BUNDLE: INITIAL RESUSCITATION FOR SEPSIS AND SEPTIC SHOCK: Measure lactate level. * Obtain blood cultures before administering antibiotics. Administer broad‐spectrum antibiotics. Begin rapid administration of 30 m. L/kg crystalloid for hypotension or lactate ≥ 4 mmol/L. • Apply vasopressors if hypotensive during or after fluid resuscitation to maintain a mean arterial pressure ≥ 65 mm Hg. • *Remeasure lactate if initial lactate elevated (> 2 mmol/L) • •
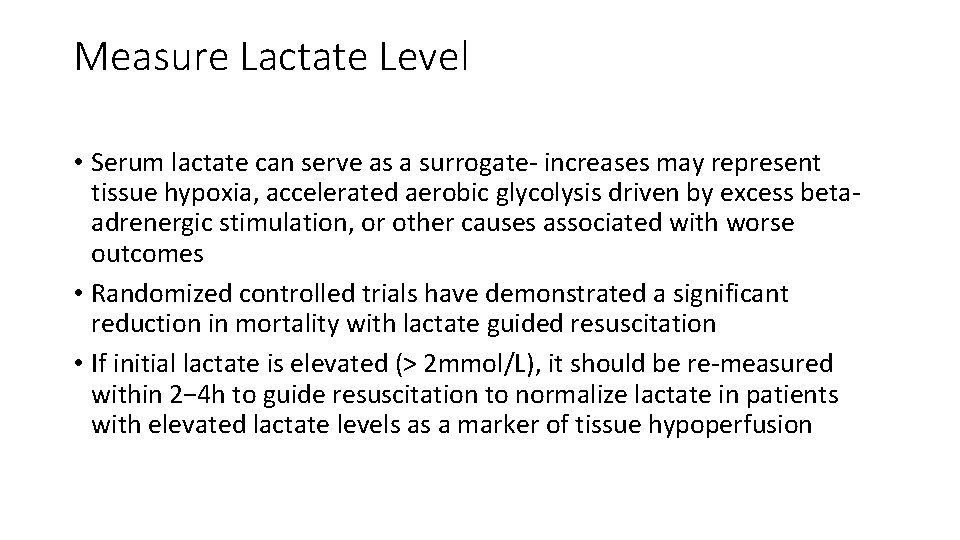
Measure Lactate Level • Serum lactate can serve as a surrogate‐ increases may represent tissue hypoxia, accelerated aerobic glycolysis driven by excess beta‐ adrenergic stimulation, or other causes associated with worse outcomes • Randomized controlled trials have demonstrated a significant reduction in mortality with lactate guided resuscitation • If initial lactate is elevated (> 2 mmol/L), it should be re‐measured within 2− 4 h to guide resuscitation to normalize lactate in patients with elevated lactate levels as a marker of tissue hypoperfusion
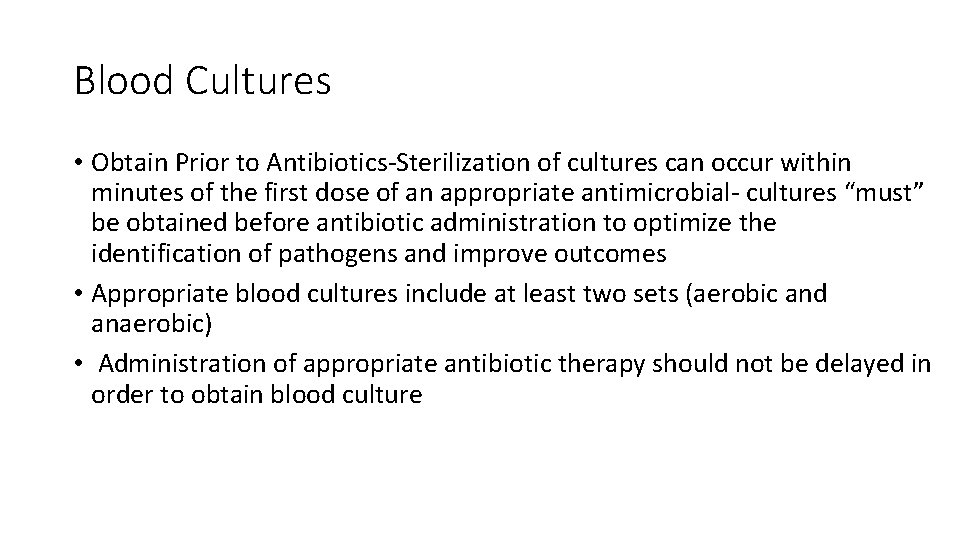
Blood Cultures • Obtain Prior to Antibiotics‐Sterilization of cultures can occur within minutes of the first dose of an appropriate antimicrobial‐ cultures “must” be obtained before antibiotic administration to optimize the identification of pathogens and improve outcomes • Appropriate blood cultures include at least two sets (aerobic and anaerobic) • Administration of appropriate antibiotic therapy should not be delayed in order to obtain blood culture
Administer Broad-Spectrum Antibiotics • Empiric broad‐spectrum therapy with one or more intravenous antimicrobials to cover all likely pathogens should be started immediately • Give soon, go broad • Empiric antimicrobial therapy should be narrowed once pathogen identification and sensitivities are established, or discontinued if a decision is made that the patient does not have infection • The link between early administration of antibiotics for suspected infection and antibiotic stewardship remains an essential aspect of high‐quality sepsis management.
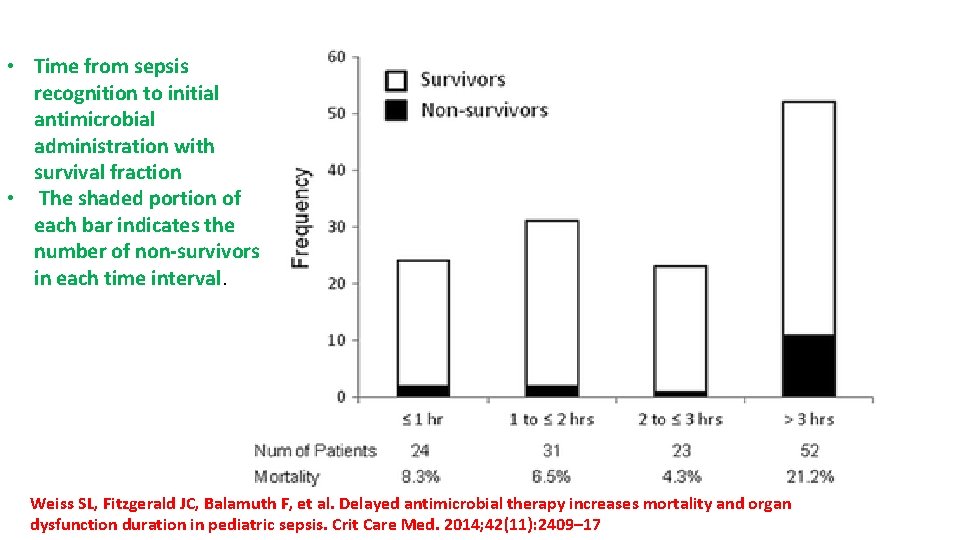
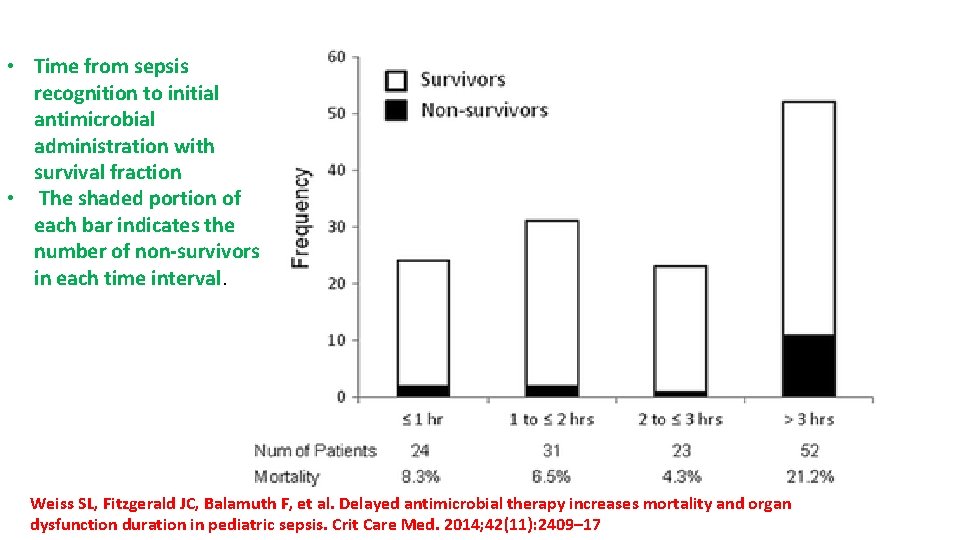
• Time from sepsis recognition to initial antimicrobial administration with survival fraction • The shaded portion of each bar indicates the number of non-survivors in each time interval. Weiss SL, Fitzgerald JC, Balamuth F, et al. Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Crit Care Med. 2014; 42(11): 2409– 17
Administer IV Fluid • Early effective fluid resuscitation is crucial for the stabilization of sepsis‐ induced tissue hypo‐perfusion or septic shock. • Initial fluid resuscitation should begin immediately upon recognizing a patient with sepsis and/or hypotension and elevated lactate, and completed within 3 hours of recognition‐ 30 m. L/kg of intravenous crystalloid fluid • Recent interventional studies have described this as usual practice in the early stages of resuscitation, and observational evidence is supportive • Strong recommendation for the use of crystalloid solutions in the initial resuscitation of patients with sepsis and septic shock. • Some evidence indicates that a sustained positive fluid balance during ICU stay is harmful, fluid administration beyond initial resuscitation requires careful assess
Administer IV Fluid • Some evidence indicates that a sustained positive fluid balance during ICU stay is harmful, fluid administration beyond initial resuscitation requires careful assess • IV fluids‐medication • Proper fluid , dose and amount • Tailor therapy for each patient • Hyperchloraemic solution (like normal saline) appear to have detrimental effects of somatic and renal functions (in large quantities) • • More volume retention and peripheral edema Less vigorous UOP response to bolus Increase severity of AKI/and more dialysis need Lower MAP and increased mortality • Balanced crystalloid should be considered for large volume resuscitations such as shock, DKA, volume depletion
Apply Vasopressors • Urgent restoration of an adequate perfusion pressure to the vital organs is a key part of resuscitation • If blood pressure is not restored after initial fluid resuscitation, then vasopressors should be commenced within the first hour to achieve mean arterial pressure (MAP) of ≥ 65 mm Hg.
Fluid and Catecholamine Resistant Shock • When fluid boluses and inotropes have not corrected poor perfusion, decreased LOC and urine output • Consider hydrocortisone therapy especially for those patients at risk: • • Adrenal or pituitary insufficiency Purpura fulminans History of steroid treatment Dosing: 2‐ 50 mg/kg/day (if possible take random cortisol level first) (should be >496 nmol/L or >18 mcg/d. L)
Supportive care • Screening and diagnosis of septic source‐Elimination of pathogen • Maintenance of Oxygen delivery‐ Mechanical ventilation • Administration of blood products • Venous thromboembolism and stress ulcer prophylaxis • Nutrition • Management of additional end‐organ dysfunction
Take Home • The last few decades of sepsis research have helped clinicians better understand the importance of identifying sepsis early and treating aggressively • There is still much debate about how to identify these patients and which criteria are most predictive for the development of sepsis and septic shock • The recent updates, particularly the recommendations regarding SOFA and q. SOFA scores, operationalize the definitions of sepsis into a clinically useful model that can be used by clinicians to identify the patients most at risk of deterioration • The lack of progress in mortality reduction in sepsis treatment despite extraordinary investment of research resources underscores the variability in patients with sepsis • No single solution is likely to be universally beneficial and sepsis continues to be an entity that should receive high priority for the development of precision health approaches for treatment

References • Watson RS, Carcillo JA, Linde‐Zwirble WT, et al. The epidemiology of severe sepsis in children in the United States. Am J Respir Crit Care Med. 2003; 167(5): 695– 701. • Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. 2008; 34(1): 17– 60. • Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013; 41(2): 580– 637 • Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med. 2017; 45(3): 486– 552. • Churpek MM, Zadravecz FJ, Winslow C, et al. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med. 2015; 192(8): 958– 64 • Kaukonen K‐M, Bailey M, Pilcher D, et al. Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med. 2015; 372(17): 1629– 38. Casserly B, Phillips GS, Schorr C, et al: Lactate measurements in sepsis‐induced tissue hypoperfusion: Results from the Surviving Sepsis Campaign database. Crit Care Med 2015; 43: 567– 573. • Jansen TC, van Bommel J, Schoonderbeek FJ, et al: LACTATE study group. Early lactate‐guided therapy in intensive care unit patients: A multicenter, open‐label, randomized controlled trial. Am J Respir Crit Care Med 2010; 182: 752– 761 • Fleischmann C, Scherag A, Adhikari NKJ, Hartog CS, Tsaganos T, Schlattmann P, et al. Assessment of global incidence and mortality of hospital‐treated sepsis—current estimates and limitations. Am J Respir Crit Care Med. 2016; 193: 253– 72. • Reinhart K, Daniels R, Kissoon N, Machado FR, Schachter RD, Finfer S. Recognizing sepsis as a global health priority—a WHO resolution. N Engl J Med 2017; 377: 414– 17 Singer, M. ; Deutschman, C. S. ; Seymour, C. W. ; Shankar‐Hari, M. ; Annane, D. ; Bauer, M. ; Bellomo, R. ; • Bernard, G. R. ; Chiche, J. ‐D. ; Coopersmith, C. M. ; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis‐ 3). JAMA 2016, 315, 801– 810.
References • Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013; 369(9): 840– 851 • Deutschman CS, Tracey KJ. Sepsis: current dogma and new perspectives. Immunity. 2014; 40(4): 463 – 475. • Singer M, De Santis V, Vitale D, Jeffcoate W. Multiorgan failure is an adaptive, endocrinemediated, metabolic response to overwhelming systemic inflammation. Lancet. 2004; 364(9433): 545– 548 • Levy MM, Fink MP, Marshall JC, et al. International Sepsis Definitions Conference. 2001 SCCM/ ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003; 29(4): 530– 538 • Magee JC, Krishnan SM, Benfield MR, Hsu DT, Shneider BL. Pediatric transplantation in the United States, 1997– 2006. Am J Transplant 2008; 8: 935– 945 • Kunz AN, Brook I. Emerging resistant Gram‐negative aerobic bacilli in hospital‐acquired infections. Chemotherapy 2010; 56: 492– 500 Cruz AT, Perry AM, Williams EA, Graf JM, Wuestner ER, Patel B. • Implementation of goal‐directed therapy for children with suspected sepsis in the emergency department. Pediatrics 2011; 127: e 758–e 766