Virtual Ward Round 2020 Case 1 First tonicclonic










- Slides: 66
Virtual Ward Round 2020
Case 1: First tonic-clonic seizure
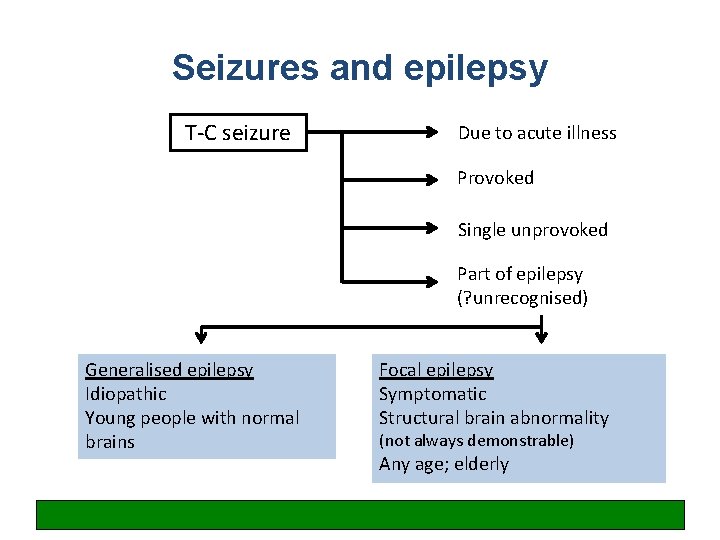
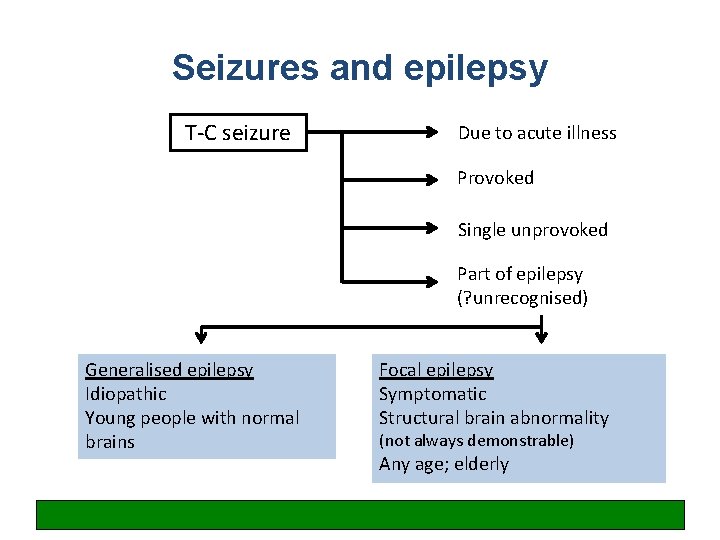
Seizures and epilepsy T-C seizure Due to acute illness Provoked Single unprovoked Part of epilepsy (? unrecognised) Generalised epilepsy Idiopathic Young people with normal brains Focal epilepsy Symptomatic Structural brain abnormality (not always demonstrable) Any age; elderly
4 key questions to ask • • Was this a seizure? Were there any obvious provoking factors? Is there evidence of unrecognised epilepsy? What is the patient’s job and driving status?
Summary of NICE guideline: general • All adults with a new suspected seizure should be screened first by a physician then referred to a specialist and seen within 2 weeks • Good communication, including written communication, is vital • A specialist is ‘a doctor with expertise and training in epilepsy’ • The diagnosis of epilepsy in adults should be established by a specialist • When NEAD is suspected, patients should be referred to psychology/psychiatry services • AED treatment needs to be tailored to type of seizures and type of patient • Women must be given information about contraception, pregnancy, breastfeeding etc. • All patients with epilepsy should have a regular structured review • If seizures are not controlled, or there is diagnostic uncertainty, patients should be referred to a specialist centre ‘soon’ for further assessment
Summary of NICE guideline: investigations • An EEG should be performed only in patients where the history suggests an epileptic seizure – EEG is not diagnostic and should not be used to ‘rule out’ epilepsy • An EEG should be performed ‘soon’ (within 4 weeks) • MRI is the imaging of choice in epilepsy and should be performed ‘soon’ • Imaging is not routinely required when a diagnosis of idiopathic generalised epilepsy has been made • CT can be used acutely to determine whether a seizure has been caused by an acute neurological problem • A 12 -lead ECG should be performed in all patients with suspected epilepsy • Serum prolactin measurement is not recommended • Epileptic seizures should be classified using a) a description of the seizure, b) seizure type, and c) aetiology or syndrome.
Summary of NICE guideline: treatment (brief summary for non-specialists) Focal seizures • Carbemazepine or Lamotrigine as first-line • Leveteracitam is not considered cost-effective (2011 analysis) • Leveteracitam, oxcarbazepine, sodium valproate second-line • Be aware of the teratogenic risks of sodium valproate • (Other drugs in refractory seizures should be prescribed by a tertiary epilepsy specialist) T-C seizures • Sodium valproate first-line • Be aware of the teratogenic risks of sodium valproate • Offer Lamotrigine if sodium valproate not suitable, but be aware this can exacerbate myoclonic seizures in JME • (Leveteracitam may be used for myoclonic seizures) • Lamotrigine, Leveteracitam, Topiramate second-line
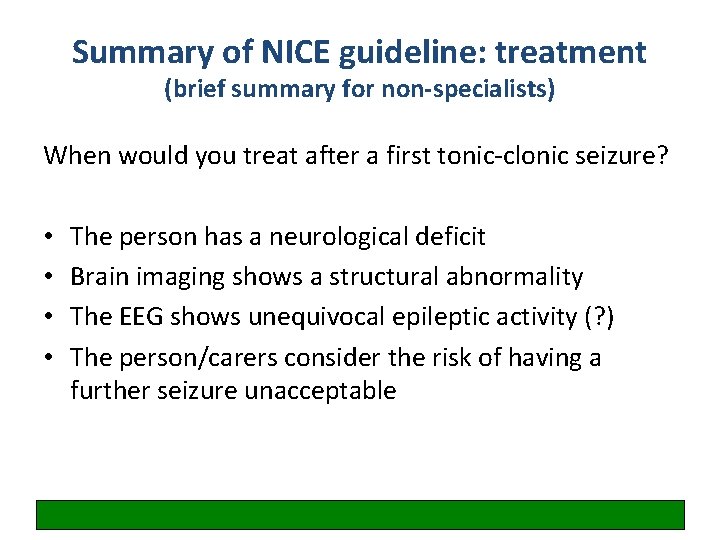
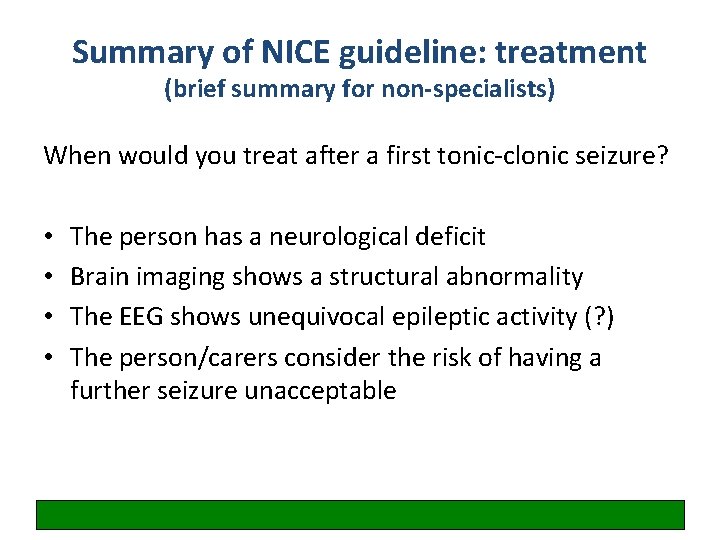
Summary of NICE guideline: treatment (brief summary for non-specialists) When would you treat after a first tonic-clonic seizure? • • The person has a neurological deficit Brain imaging shows a structural abnormality The EEG shows unequivocal epileptic activity (? ) The person/carers consider the risk of having a further seizure unacceptable
Case 3: Chest pain
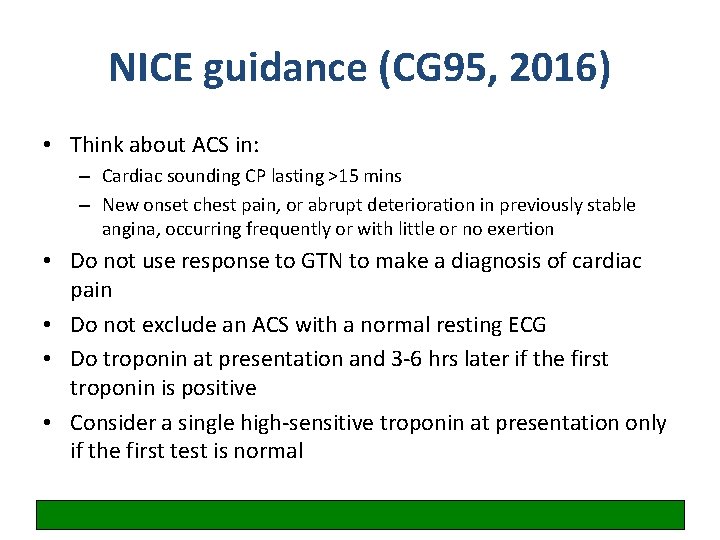
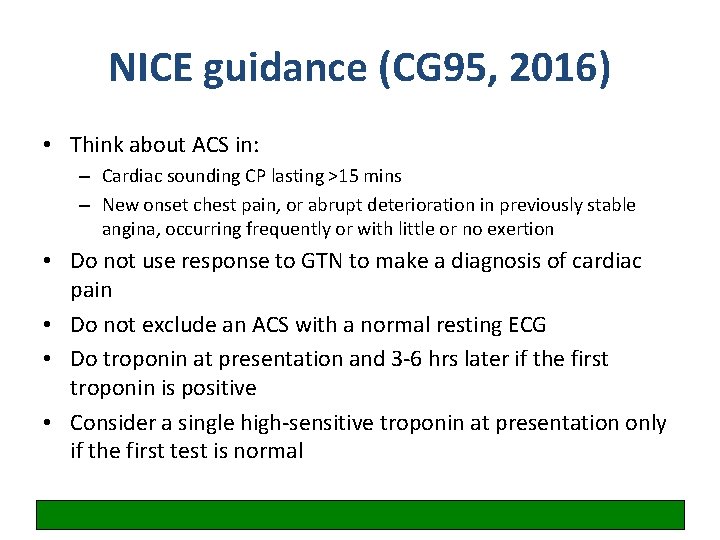
NICE guidance (CG 95, 2016) • Think about ACS in: – Cardiac sounding CP lasting >15 mins – New onset chest pain, or abrupt deterioration in previously stable angina, occurring frequently or with little or no exertion • Do not use response to GTN to make a diagnosis of cardiac pain • Do not exclude an ACS with a normal resting ECG • Do troponin at presentation and 3 -6 hrs later if the first troponin is positive • Consider a single high-sensitive troponin at presentation only if the first test is normal
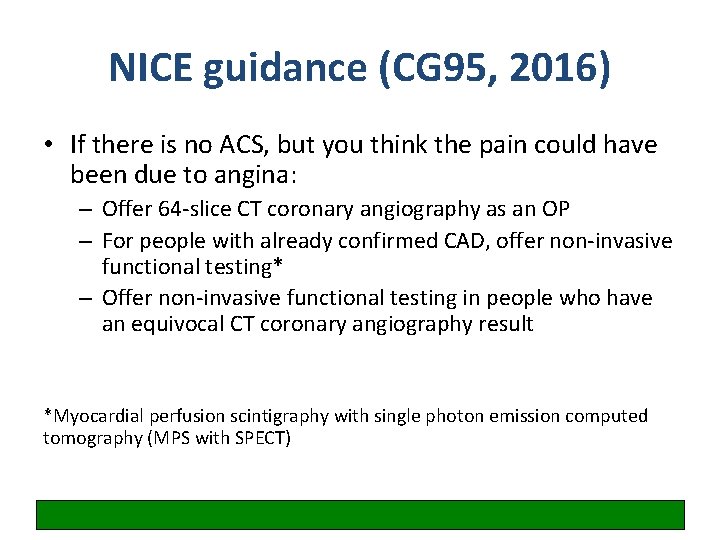
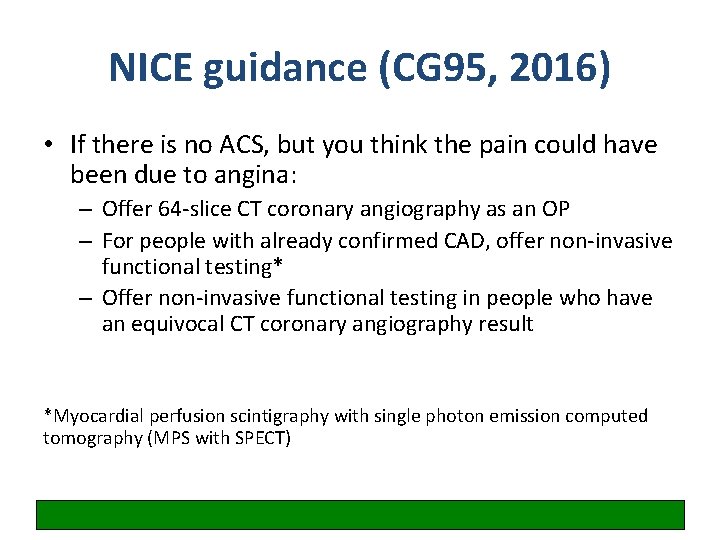
NICE guidance (CG 95, 2016) • If there is no ACS, but you think the pain could have been due to angina: – Offer 64 -slice CT coronary angiography as an OP – For people with already confirmed CAD, offer non-invasive functional testing* – Offer non-invasive functional testing in people who have an equivocal CT coronary angiography result *Myocardial perfusion scintigraphy with single photon emission computed tomography (MPS with SPECT)
Classification of unstable angina • • New onset severe angina (e. g. at min exertion) Angina at rest >20 mins Crescendo angina Post-MI angina (30 days) Roffi M, Patrono C, Collet JP, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent STSegment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016; 37(3) : 267 -315 Hamm CW and Braunwald E. Circulation 2000; 102: 118 -122
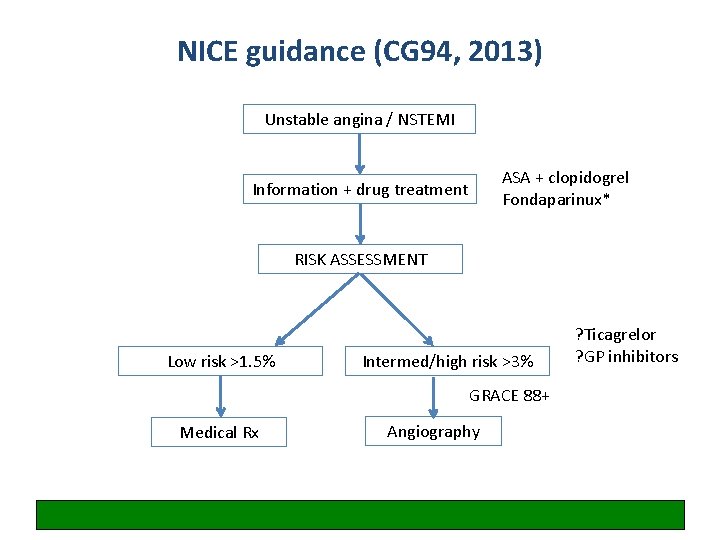
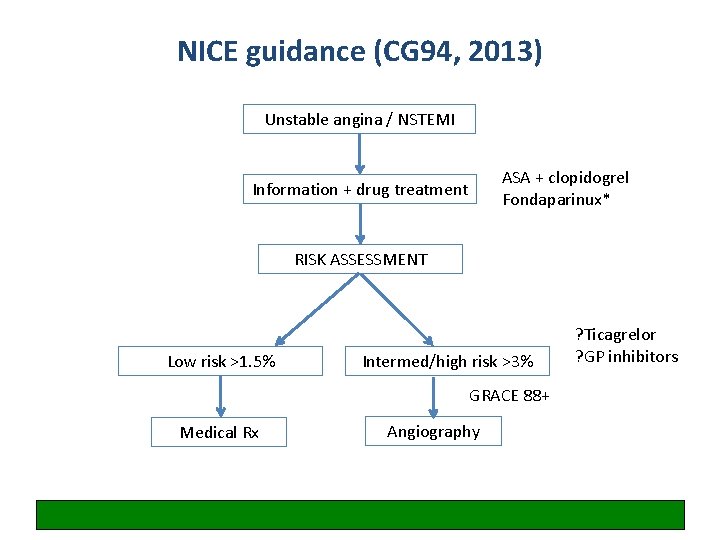
NICE guidance (CG 94, 2013) Unstable angina / NSTEMI ASA + clopidogrel Fondaparinux* Information + drug treatment RISK ASSESSMENT Low risk >1. 5% Intermed/high risk >3% GRACE 88+ Medical Rx Angiography ? Ticagrelor ? GP inhibitors

Case 5: Paracetamol overdose
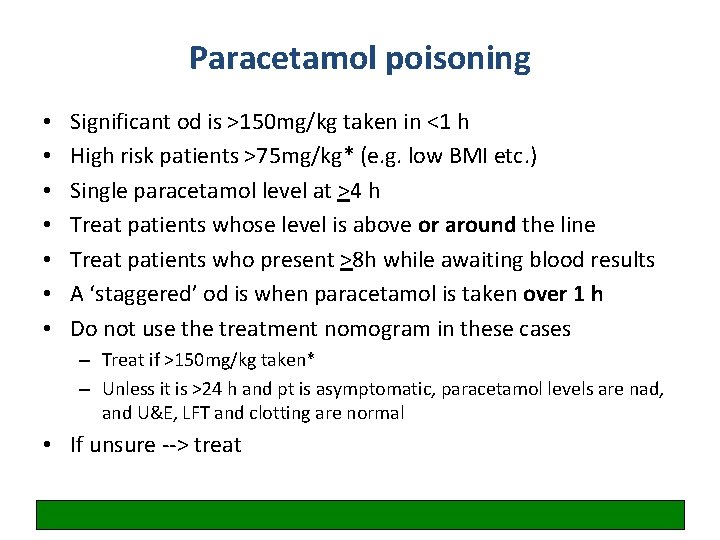
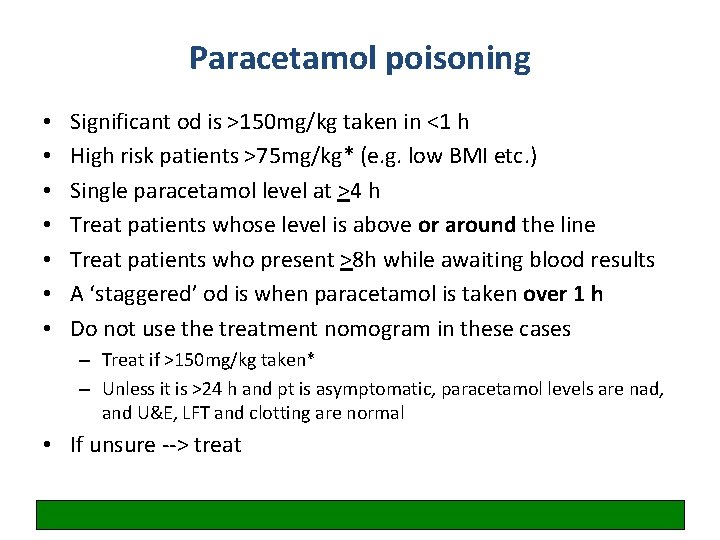
Paracetamol poisoning • • Significant od is >150 mg/kg taken in <1 h High risk patients >75 mg/kg* (e. g. low BMI etc. ) Single paracetamol level at >4 h Treat patients whose level is above or around the line Treat patients who present >8 h while awaiting blood results A ‘staggered’ od is when paracetamol is taken over 1 h Do not use the treatment nomogram in these cases – Treat if >150 mg/kg taken* – Unless it is >24 h and pt is asymptomatic, paracetamol levels are nad, and U&E, LFT and clotting are normal • If unsure --> treat

True or false? Activated charcoal should be administered without delay FALSE Gut decontamination with activated charcoal may reduce absorption of paracetamol minimising the need for NAC but is only effective if given within 1 h of overdose. Gastric lavage is not recommended and may actually enhance early absorption.
True or false? If the patient develops wheeze, itching and a red rash, NAC should be stopped immediately and the patient treated with IM adrenaline, IV antihistamines, nebulised beta-agonists and IV hydrocortisone FALSE This is not anaphylaxis (BP is normal). This is a pseudoallergic (anaphylactoid) reaction which occurs in up to 20% of people given intravenous NAC. Treatment is with antihistamines only ± bronchodilators if wheezy (NAC may precipitate acute asthma). The infusion can usually be restarted after a short interval e. g. 30 mins or at half the rate (the reaction tends to occur during the first bag as it is concentration dependent).
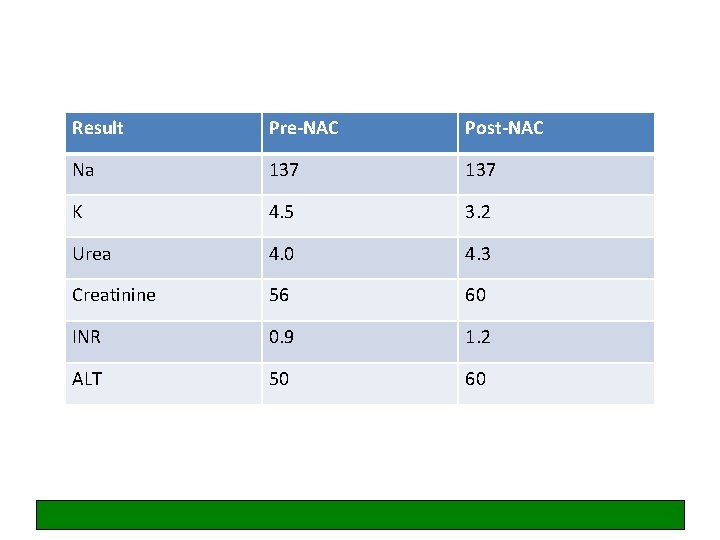
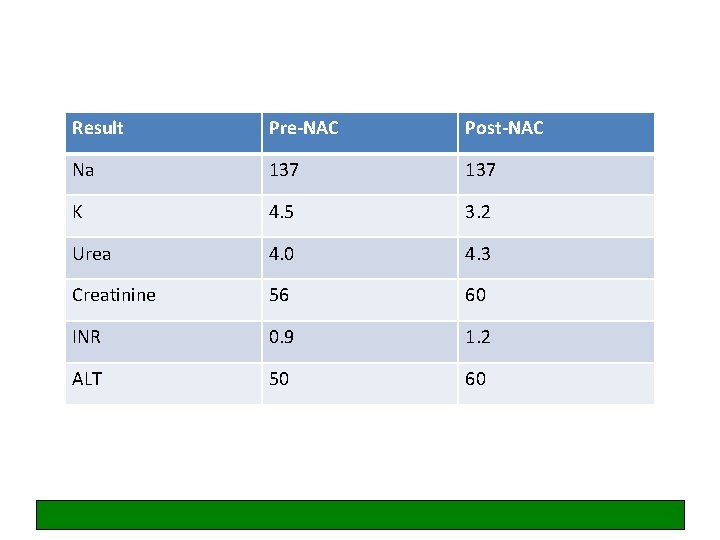
Result Pre-NAC Post-NAC Na 137 K 4. 5 3. 2 Urea 4. 0 4. 3 Creatinine 56 60 INR 0. 9 1. 2 ALT 50 60
True or false? The NAC infusion should be continued as the INR has risen from 1. 0 to 1. 3 indicating early hepatotoxicity FALSE NAC treatment itself may cause mild increases in PT (destabilises proteins including clotting factors) and an INR of ≤ 1. 3 post-infusion is acceptable (especially as the ALT has not risen from baseline).
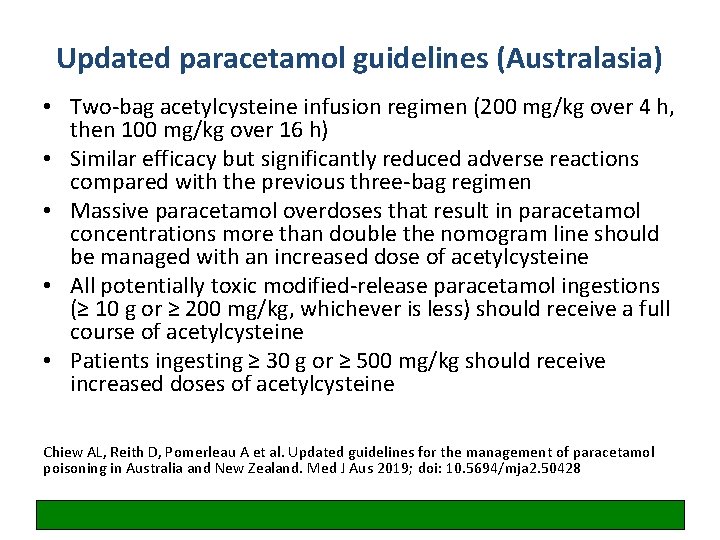
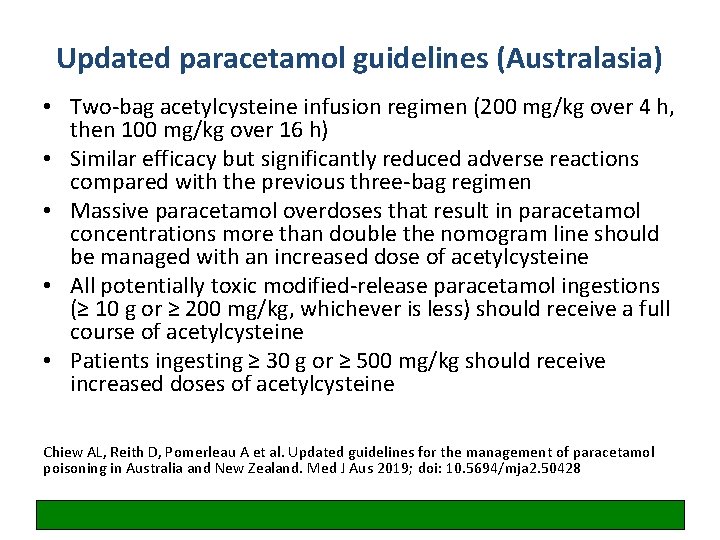
Updated paracetamol guidelines (Australasia) • Two-bag acetylcysteine infusion regimen (200 mg/kg over 4 h, then 100 mg/kg over 16 h) • Similar efficacy but significantly reduced adverse reactions compared with the previous three-bag regimen • Massive paracetamol overdoses that result in paracetamol concentrations more than double the nomogram line should be managed with an increased dose of acetylcysteine • All potentially toxic modified-release paracetamol ingestions (≥ 10 g or ≥ 200 mg/kg, whichever is less) should receive a full course of acetylcysteine • Patients ingesting ≥ 30 g or ≥ 500 mg/kg should receive increased doses of acetylcysteine Chiew AL, Reith D, Pomerleau A et al. Updated guidelines for the management of paracetamol poisoning in Australia and New Zealand. Med J Aus 2019; doi: 10. 5694/mja 2. 50428
Gov. uk safety update
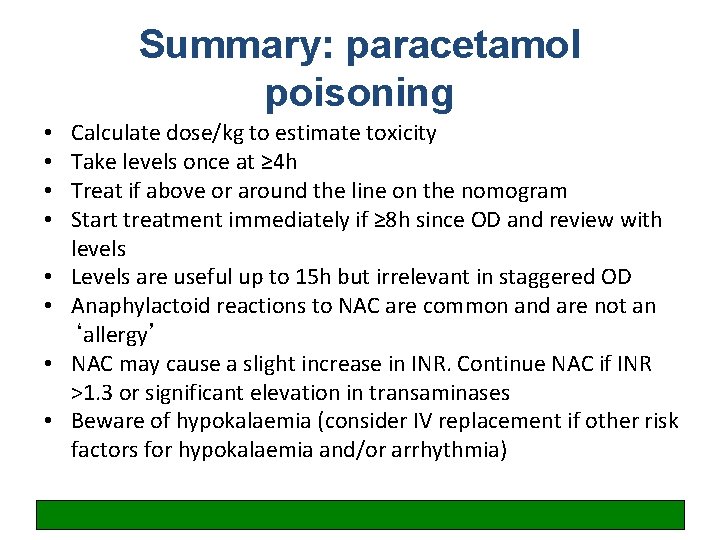
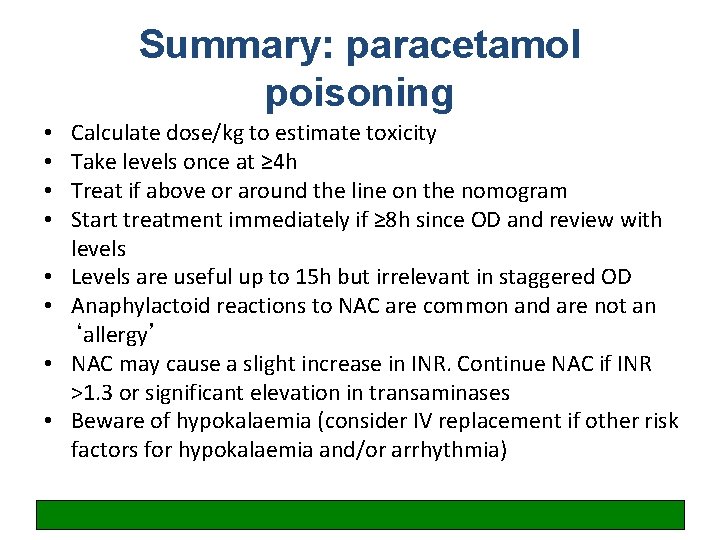
Summary: paracetamol poisoning • • Calculate dose/kg to estimate toxicity Take levels once at ≥ 4 h Treat if above or around the line on the nomogram Start treatment immediately if ≥ 8 h since OD and review with levels Levels are useful up to 15 h but irrelevant in staggered OD Anaphylactoid reactions to NAC are common and are not an ‘allergy’ NAC may cause a slight increase in INR. Continue NAC if INR >1. 3 or significant elevation in transaminases Beware of hypokalaemia (consider IV replacement if other risk factors for hypokalaemia and/or arrhythmia)
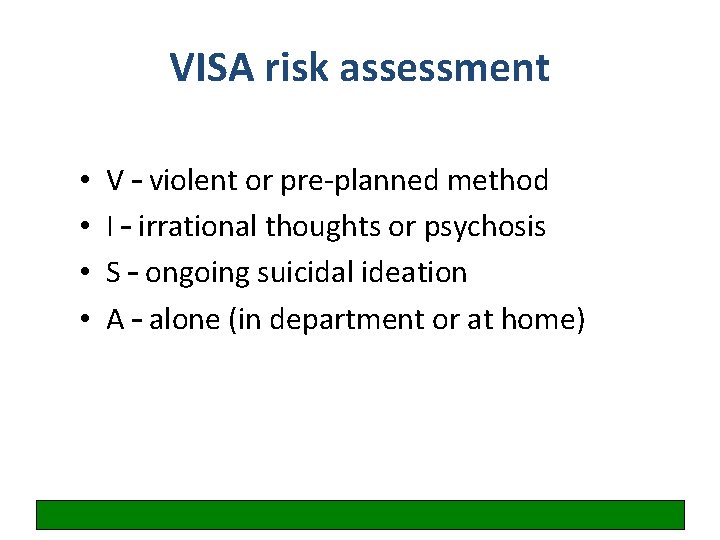
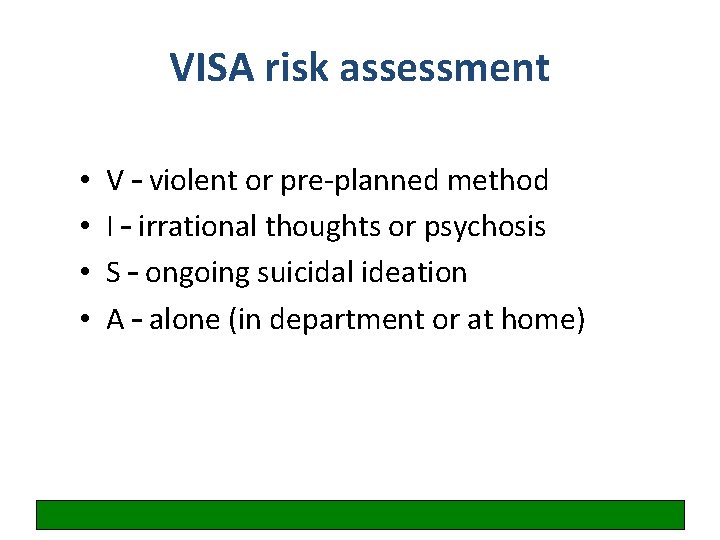
VISA risk assessment • • V – violent or pre-planned method I – irrational thoughts or psychosis S – ongoing suicidal ideation A – alone (in department or at home)
Case 6: Fall
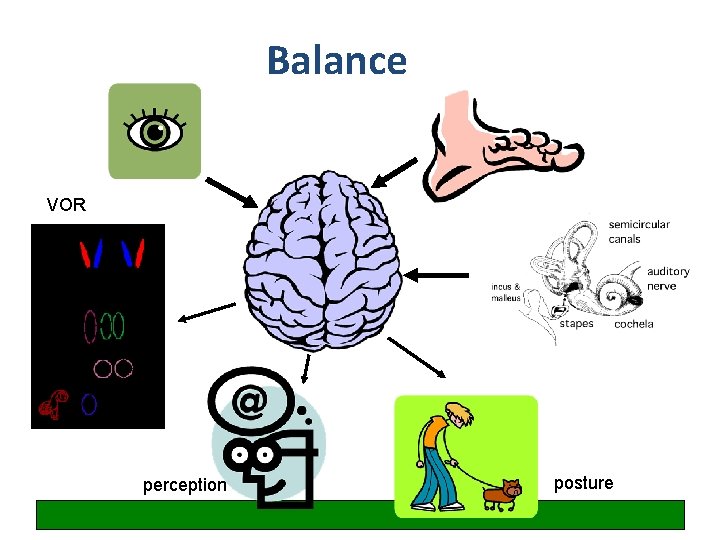
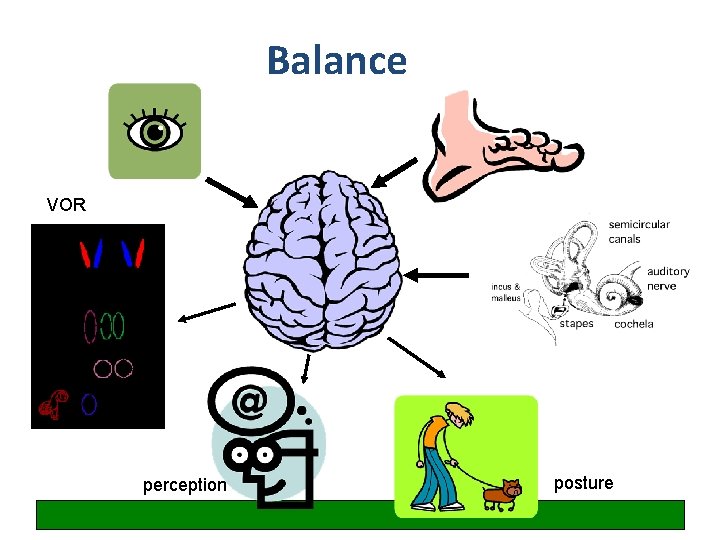
Balance VOR perception posture
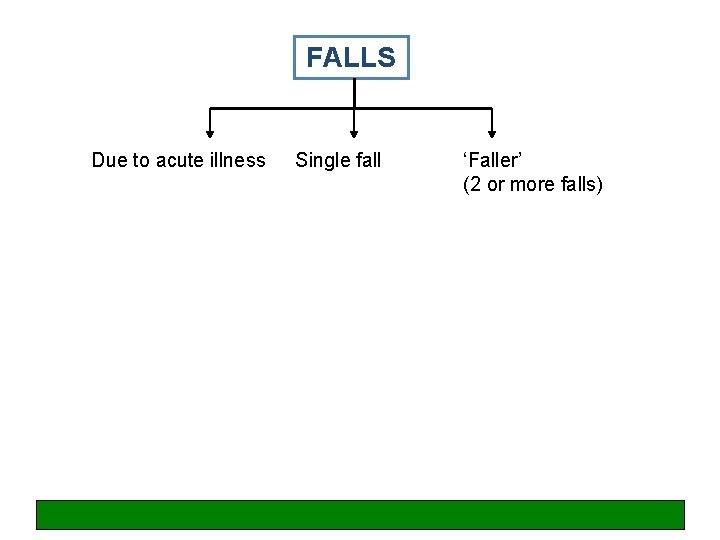
FALLS Due to acute illness Single fall ‘Faller’ (2 or more falls)
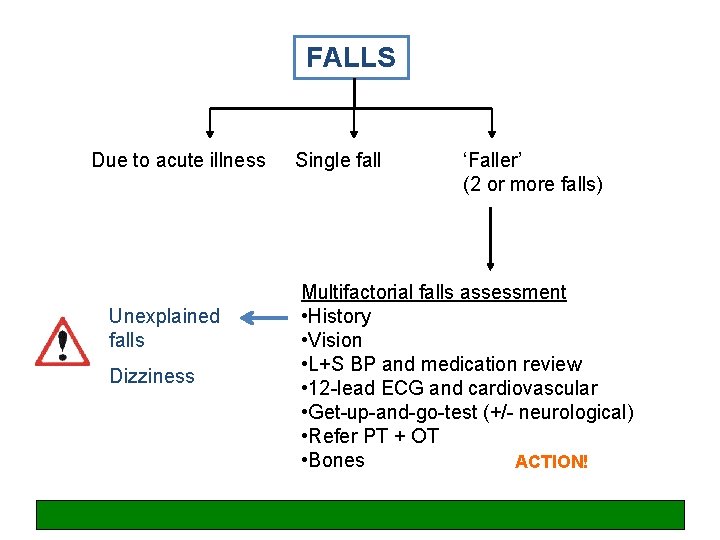
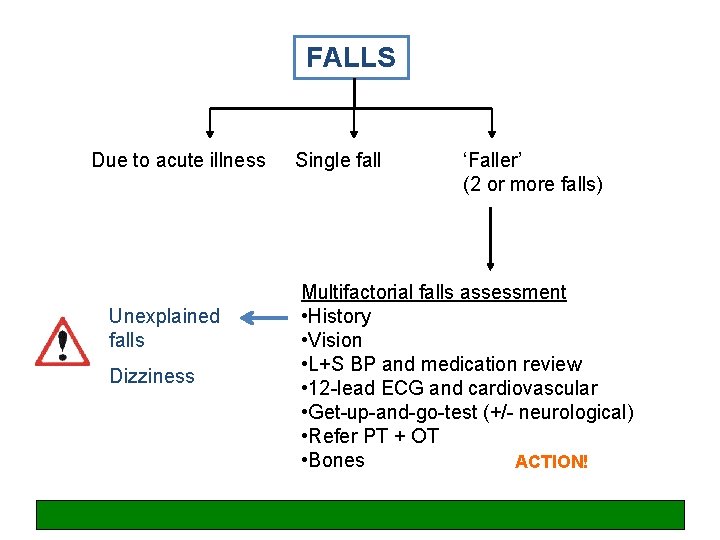
FALLS Due to acute illness Unexplained falls Dizziness Single fall ‘Faller’ (2 or more falls) Multifactorial falls assessment • History • Vision • L+S BP and medication review • 12 -lead ECG and cardiovascular • Get-up-and-go-test (+/- neurological) • Refer PT + OT • Bones ACTION!

There is no such thing as a ‘mechanical fall’ in older people (at least, it is very uncommon)
Stairs with a swirly-patterned carpet
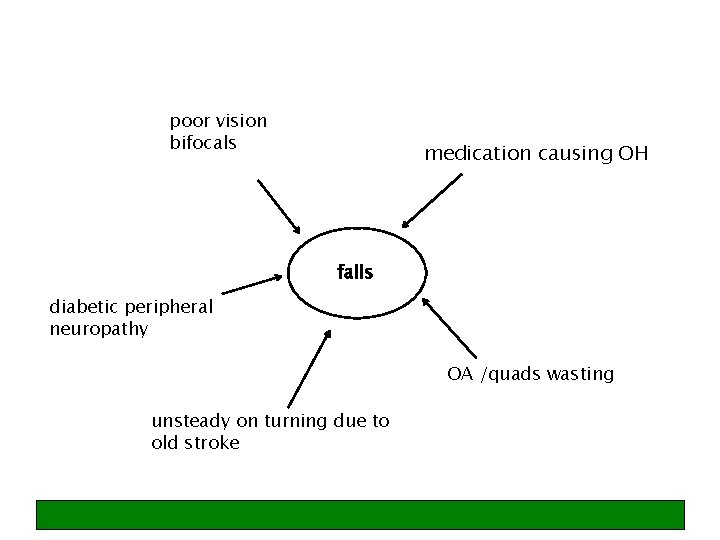
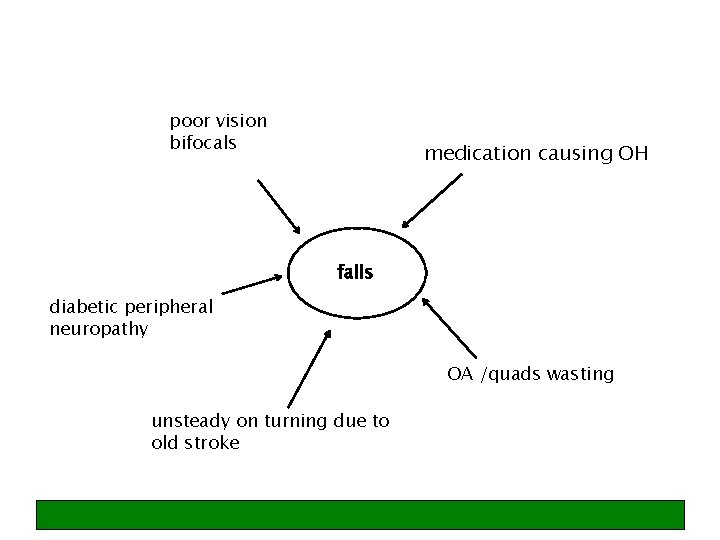
poor vision bifocals medication causing OH falls diabetic peripheral neuropathy OA /quads wasting unsteady on turning due to old stroke
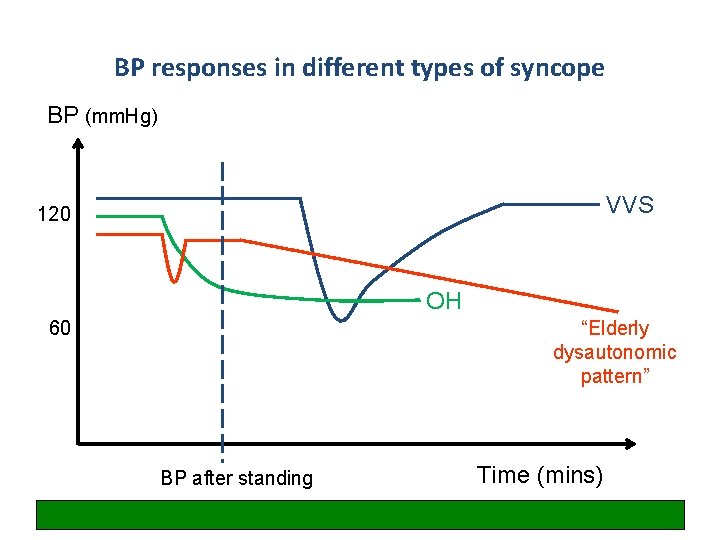
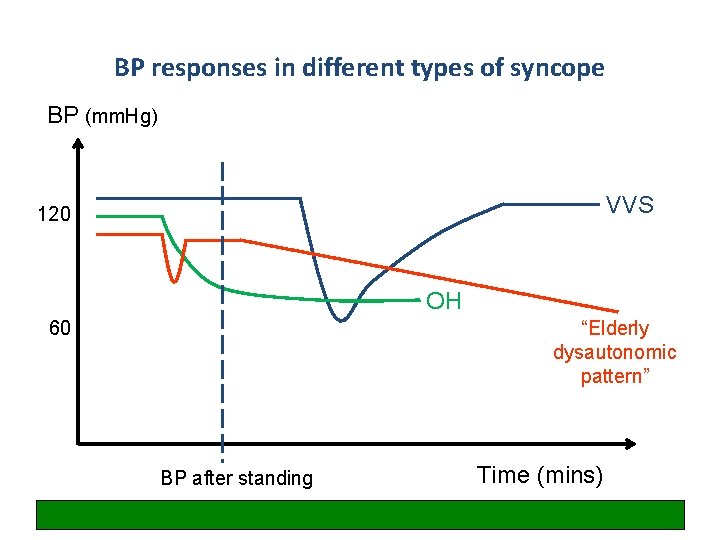
BP responses in different types of syncope BP (mm. Hg) VVS 120 OH 60 “Elderly dysautonomic pattern” BP after standing Time (mins)
NICE guideline CG 161, 2013
Case 12: Acute unilateral monoarthropathy (hot joint)

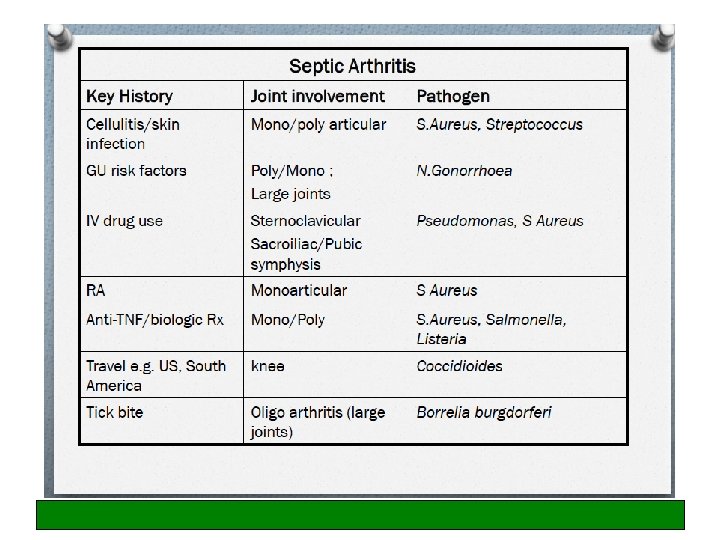
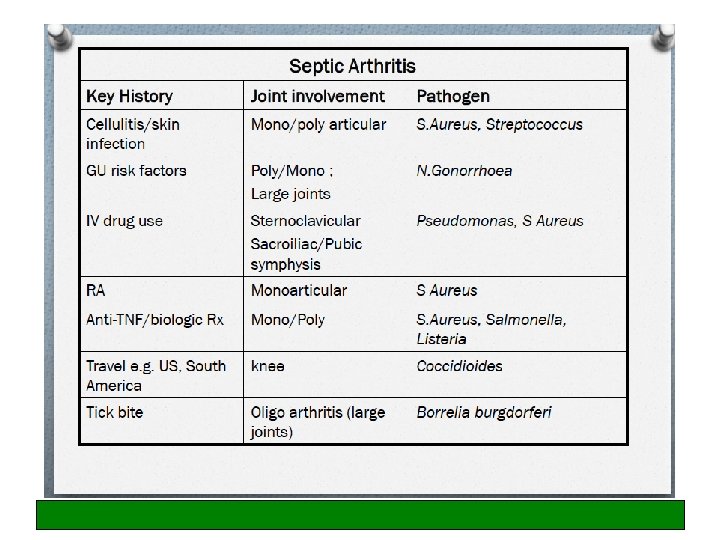
Management of hot swollen joint in adults • Short history, hot swollen joint with restricted movement should be treated as septic arthritis until proven otherwise (mortality 11%) • Even in absence of fever • Aspirate, aspirate !!! • Refer prosthetic joints to Orthopaedics • Organisms on Gram stain has 60% sensitivity • Always take blood cultures • Serum urate is of no diagnostic value
Management of hot swollen joint in adults • Commonest hot joint in GP/ED is the metatarsalphalangeal joint which is almost always due to gout and can be diagnosed clinically • Plain X-rays may show chondrocalcinosis but otherwise are of no value • If there is any doubt re: septic joint, do not inject steroids • In septic arthritis, half of pts have pre-existing joint disease • Differentials: reactive arthritis (especially younger pts), gout/pseudogout, septic arthritis, flare of existing arthritis

Case 14: Iron deficiency anaemia
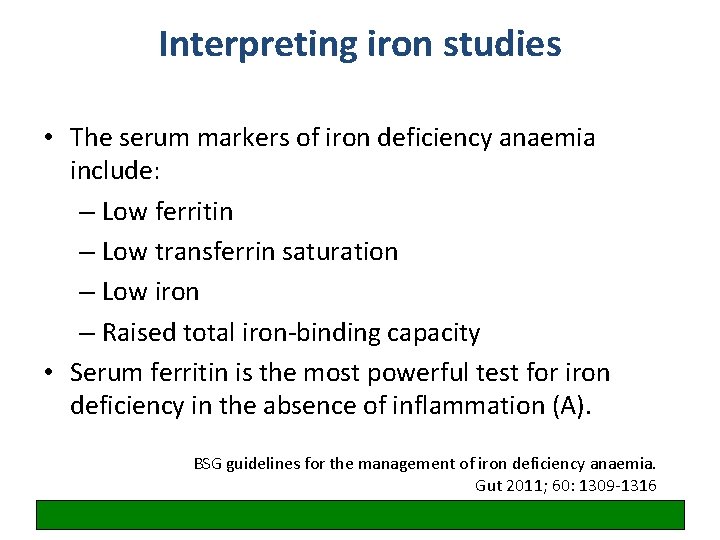
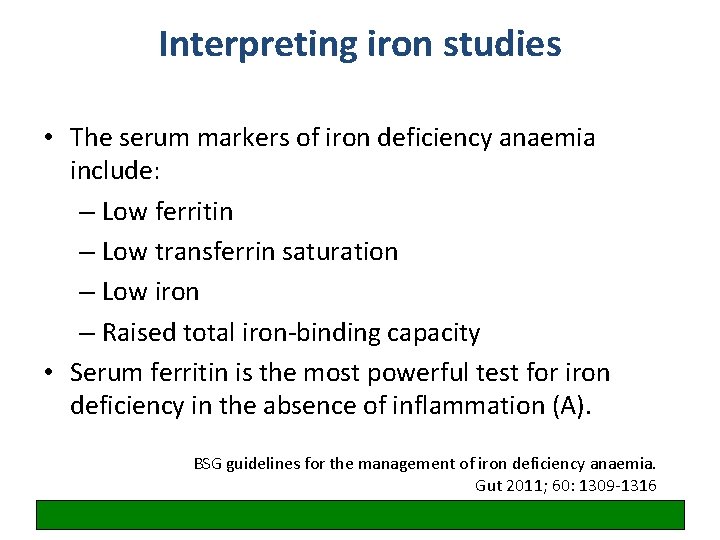
Interpreting iron studies • The serum markers of iron deficiency anaemia include: – Low ferritin – Low transferrin saturation – Low iron – Raised total iron-binding capacity • Serum ferritin is the most powerful test for iron deficiency in the absence of inflammation (A). BSG guidelines for the management of iron deficiency anaemia. Gut 2011; 60: 1309 -1316
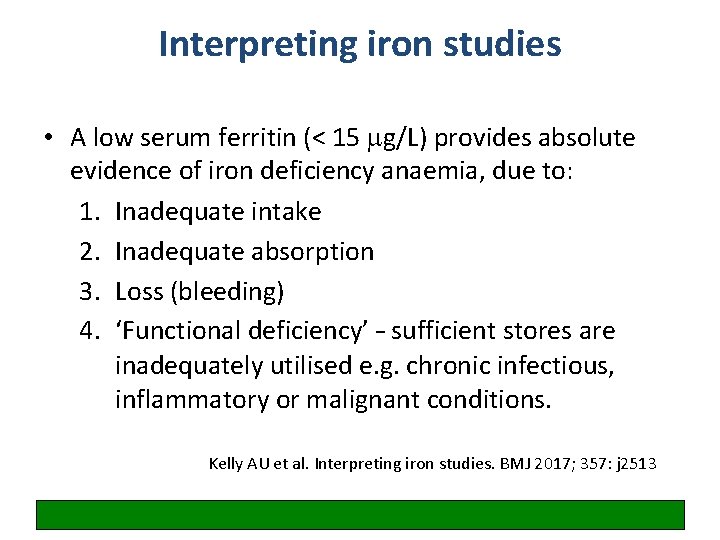
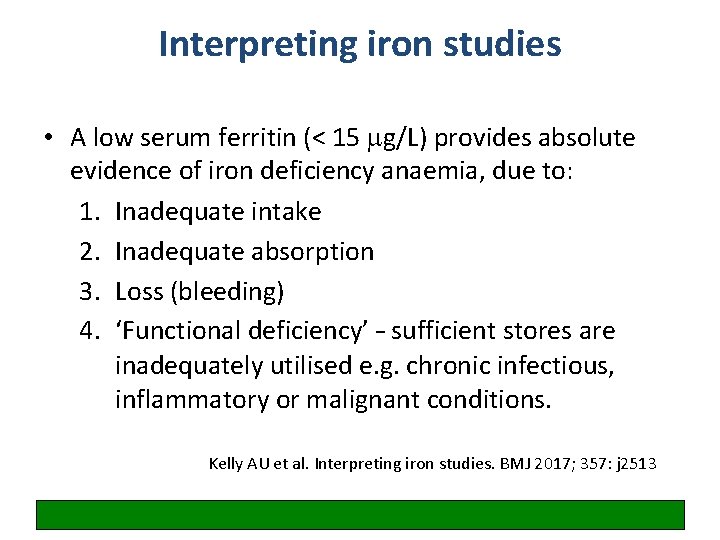
Interpreting iron studies • A low serum ferritin (< 15 mg/L) provides absolute evidence of iron deficiency anaemia, due to: 1. Inadequate intake 2. Inadequate absorption 3. Loss (bleeding) 4. ‘Functional deficiency’ – sufficient stores are inadequately utilised e. g. chronic infectious, inflammatory or malignant conditions. Kelly AU et al. Interpreting iron studies. BMJ 2017; 357: j 2513
Interpreting iron studies • Ferritin levels of more than 15 mg/L are difficult to interpret if infection or inflammation is present • A serum ferritin concentration of greater than 100 mg/L usually rules out iron deficiency anaemia • For people in whom the ferritin level is indeterminate (16 to 99 mg/L), further tests may be required to ascertain iron status … (in anaemia) NICE CKS iron deficiency

Interpreting iron studies • Haemoglobin electrophoresis is recommended when microcytosis and hypochromia are present in patients of appropriate ethnic background to prevent unnecessary GI investigation BSG guidelines for the management of iron deficiency anaemia. Gut 2011; 60: 1309 -1316
Interpreting iron studies • In the second and third trimesters of pregnancy, ferritin levels fall independently of iron stores – but a level of < 15 mg/L indicates iron depletion, and treatment should be considered when levels fall below 30 mg/L as this indicates early iron depletion which will continue to fall unless treated. NICE CKS iron deficiency
Interpreting iron studies • In patients with CKD, normal or high ferritin cannot exclude functional iron deficiency - % of hypochromic red cells (%HRC) is recommended if the sample can be processed within 6 hours • In chronic kidney disease, a cutoff of 100 mg/L has been suggested, while a cutoff of 200 mg/L has been suggested for people undergoing haemodialysis … Kelly AU et al. Interpreting iron studies. BMJ 2017; 357: j 2513
BSG guidelines for the management of iron deficiency anaemia. Gut 2011; 60: 1309 -1316

Case 15: ? PE – see PE pathway
Case 16: Syncope
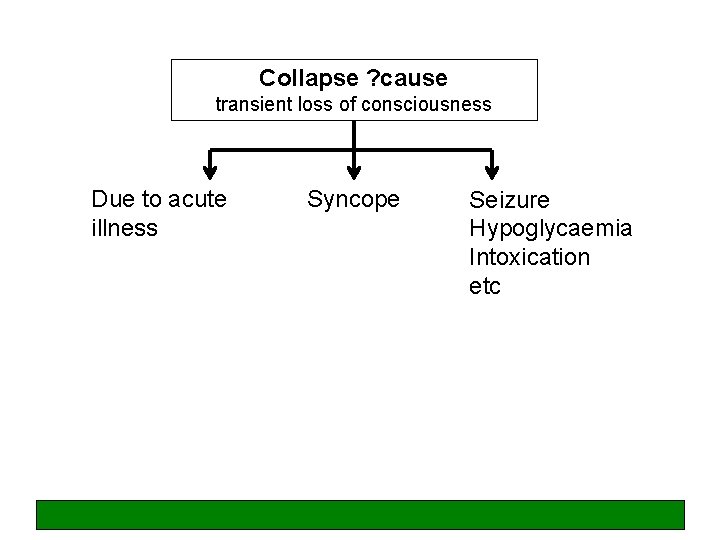
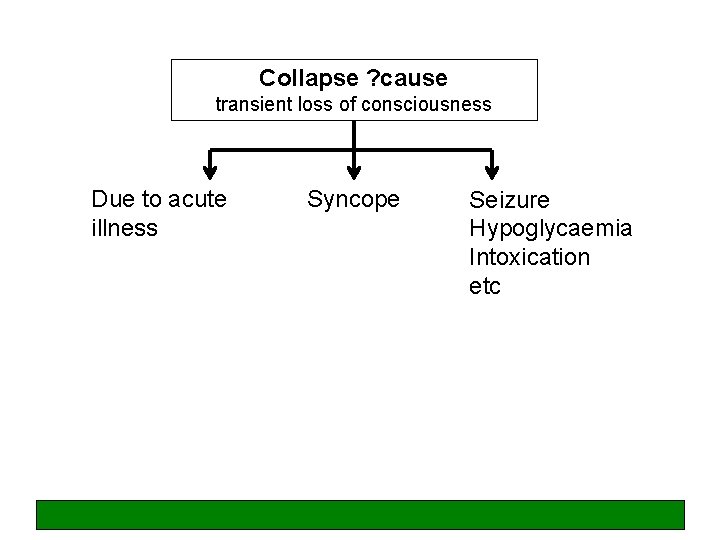
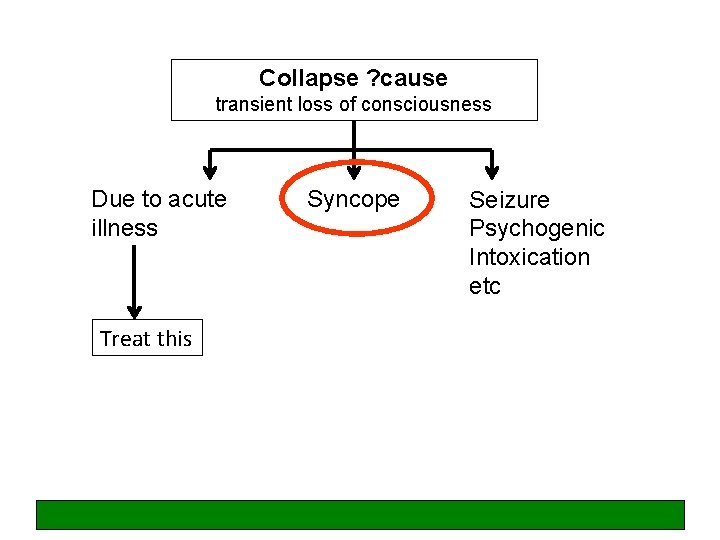
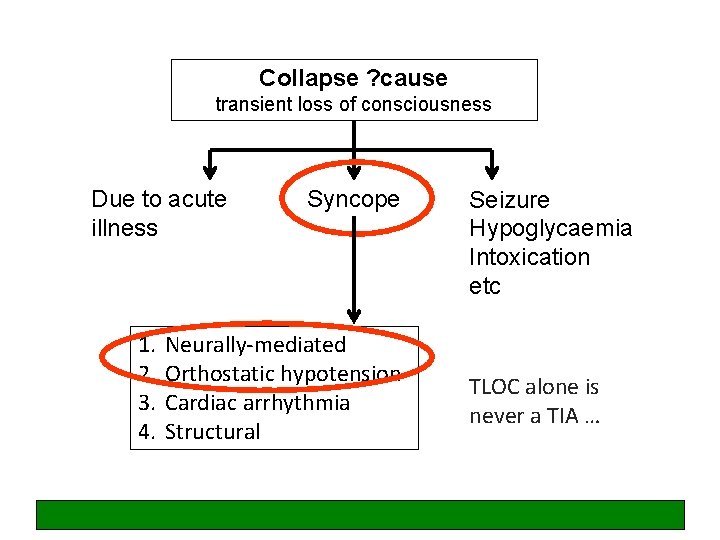
Collapse ? cause transient loss of consciousness Due to acute illness Syncope Seizure Hypoglycaemia Intoxication etc
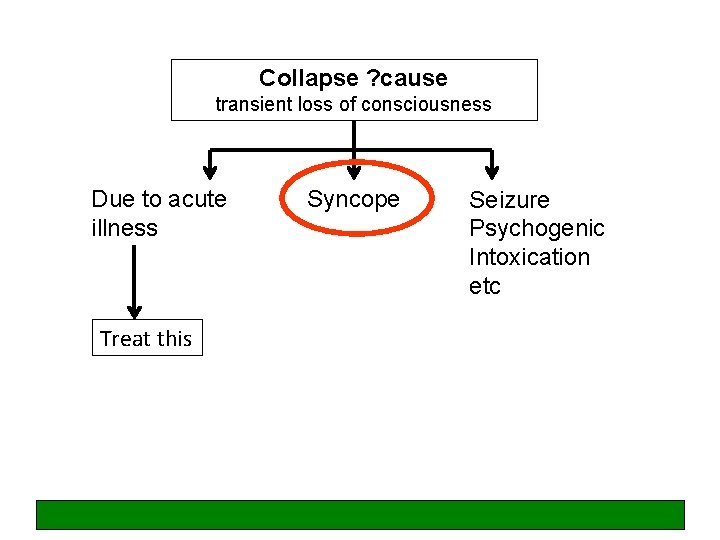
Collapse ? cause transient loss of consciousness Due to acute illness Treat this Syncope Seizure Psychogenic Intoxication etc
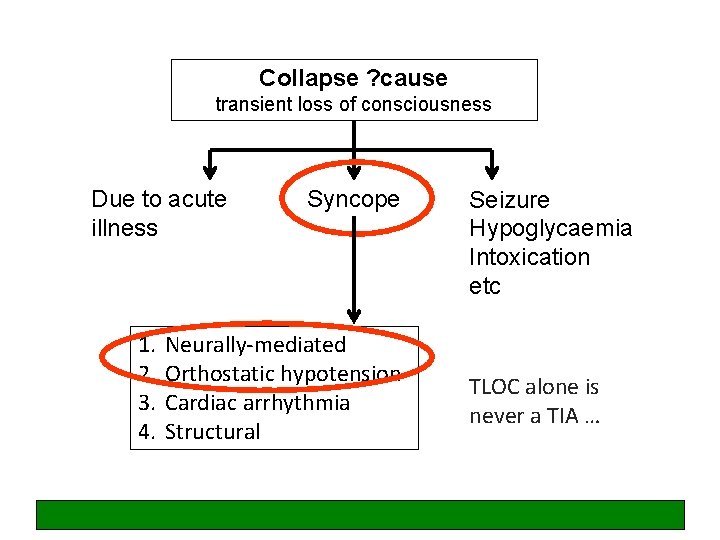
Collapse ? cause transient loss of consciousness Due to acute illness 1. 2. 3. 4. Syncope Neurally-mediated Orthostatic hypotension Cardiac arrhythmia Structural Seizure Hypoglycaemia Intoxication etc TLOC alone is never a TIA …
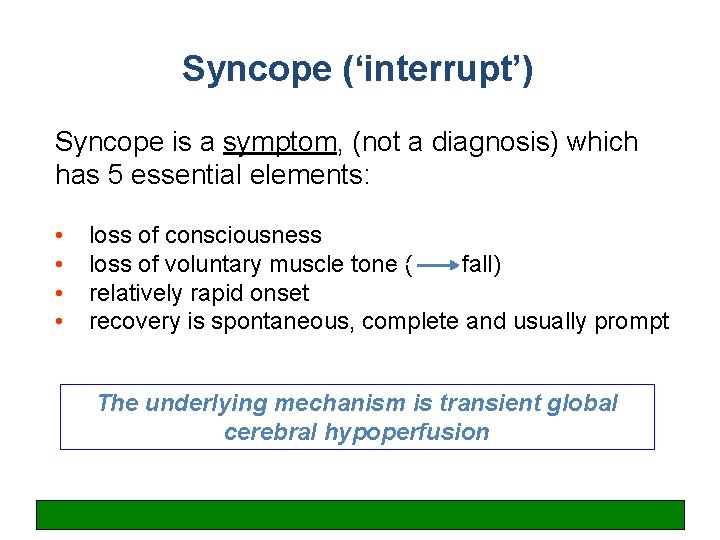
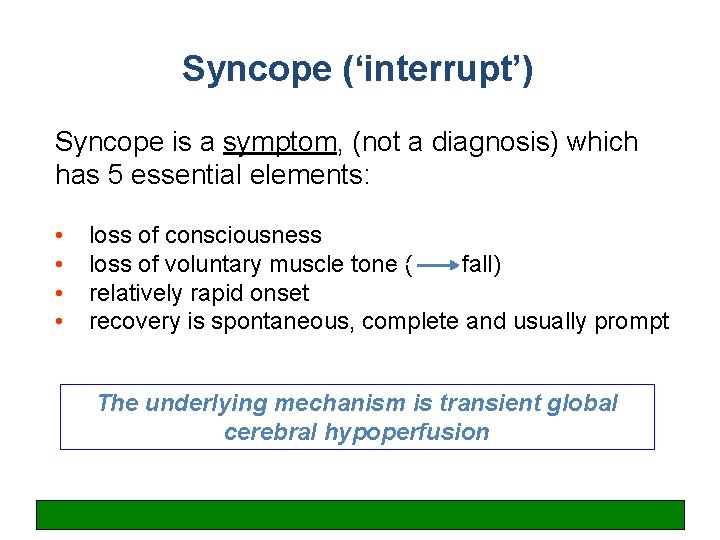
Syncope (‘interrupt’) Syncope is a symptom, (not a diagnosis) which has 5 essential elements: • • loss of consciousness loss of voluntary muscle tone ( fall) relatively rapid onset recovery is spontaneous, complete and usually prompt The underlying mechanism is transient global cerebral hypoperfusion
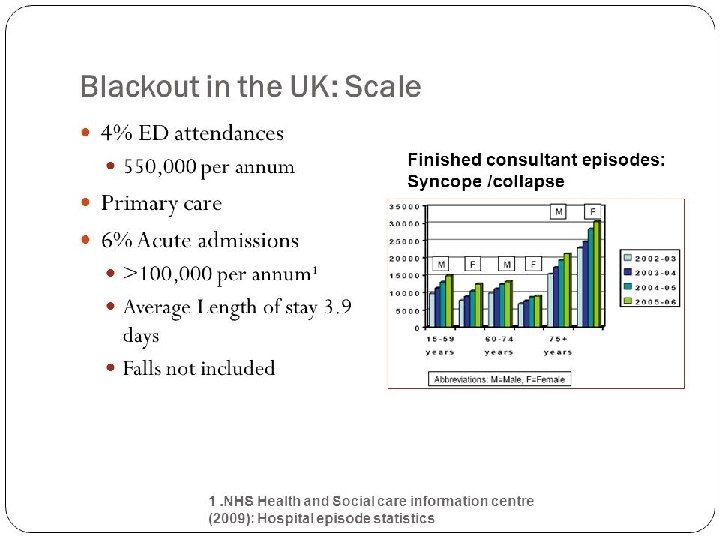
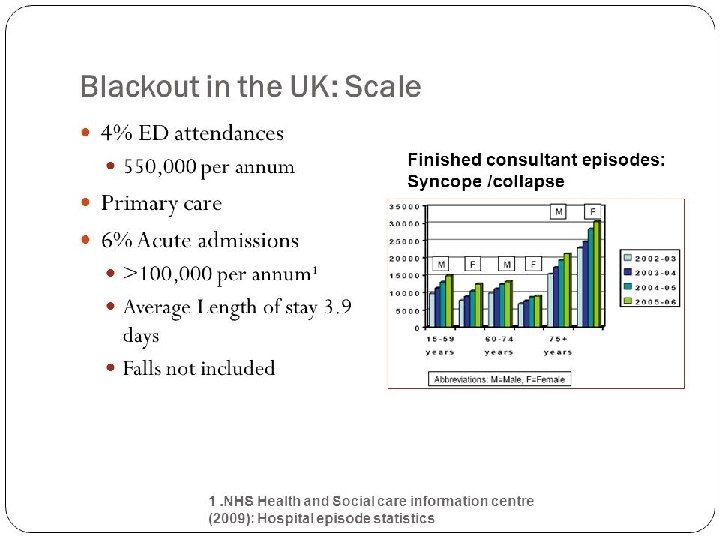
England data: syncope and collapse

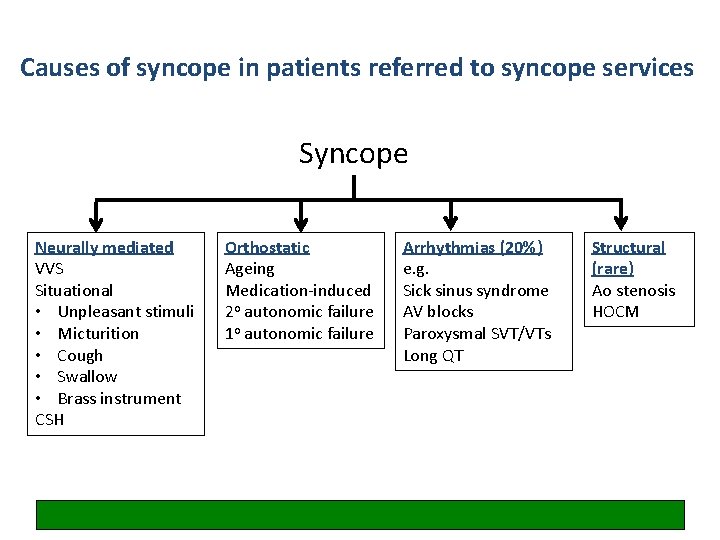
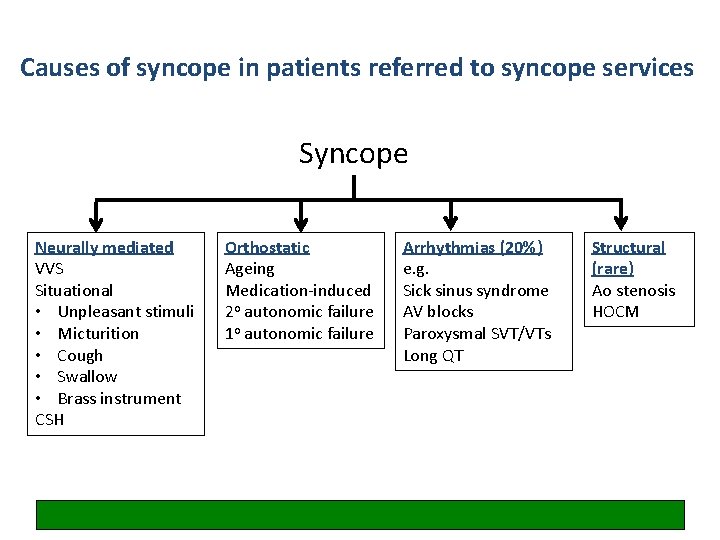
Causes of syncope in patients referred to syncope services Syncope Neurally mediated VVS Situational • Unpleasant stimuli • Micturition • Cough • Swallow • Brass instrument CSH Orthostatic Ageing Medication-induced 2 o autonomic failure 1 o autonomic failure Arrhythmias (20%) e. g. Sick sinus syndrome AV blocks Paroxysmal SVT/VTs Long QT Structural (rare) Ao stenosis HOCM
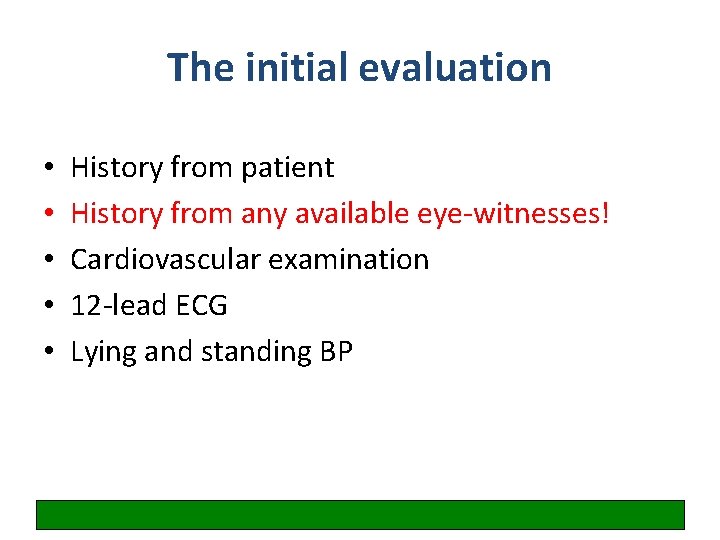
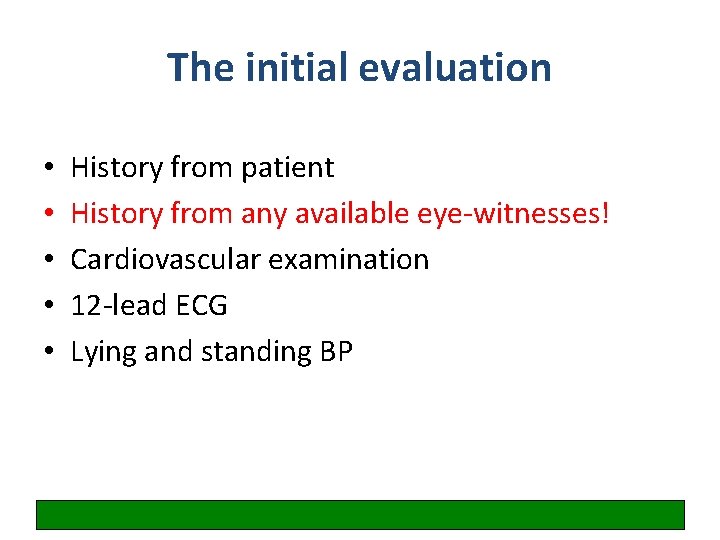
The initial evaluation • • • History from patient History from any available eye-witnesses! Cardiovascular examination 12 -lead ECG Lying and standing BP
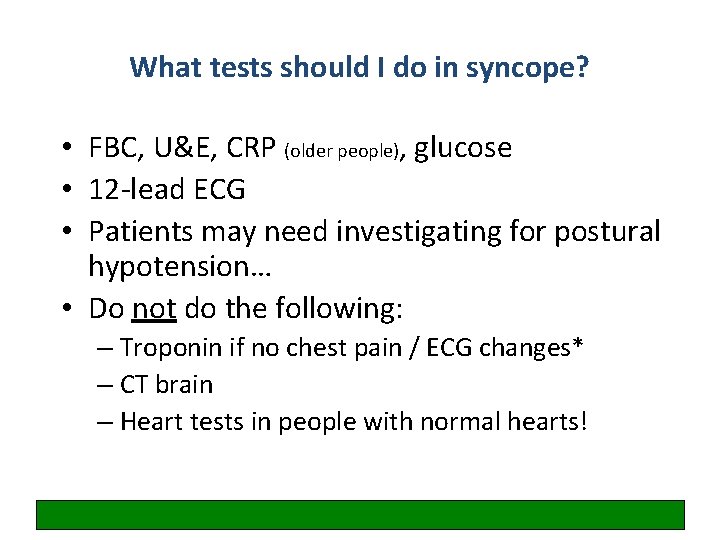
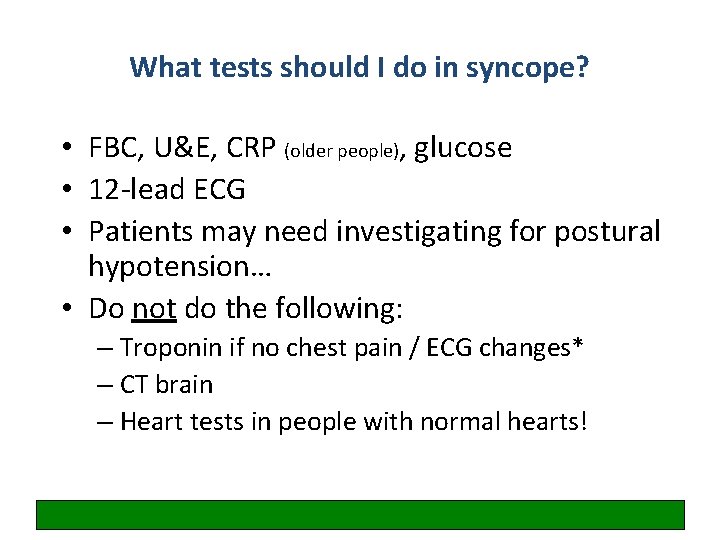
What tests should I do in syncope? • FBC, U&E, CRP (older people), glucose • 12 -lead ECG • Patients may need investigating for postural hypotension… • Do not do the following: – Troponin if no chest pain / ECG changes* – CT brain – Heart tests in people with normal hearts!

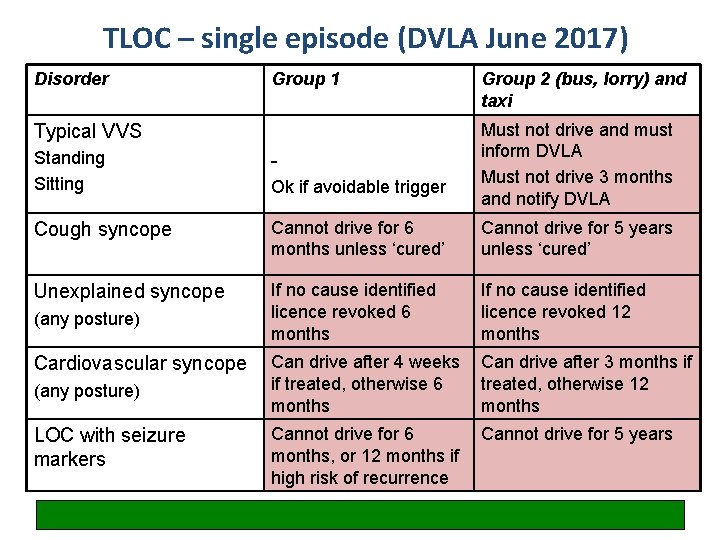
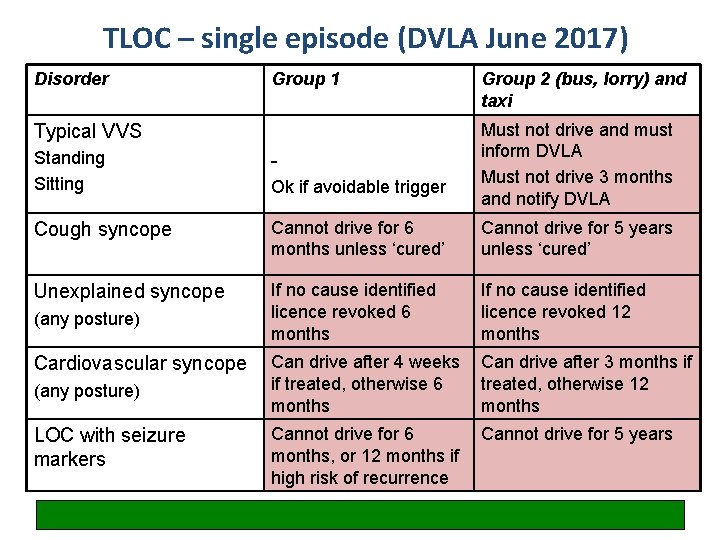
TLOC – single episode (DVLA June 2017) Disorder Group 1 Typical VVS Group 2 (bus, lorry) and taxi Must not drive and must inform DVLA Must not drive 3 months and notify DVLA Standing Sitting - Cough syncope Cannot drive for 6 months unless ‘cured’ Cannot drive for 5 years unless ‘cured’ Unexplained syncope If no cause identified licence revoked 6 months If no cause identified licence revoked 12 months (any posture) Can drive after 4 weeks if treated, otherwise 6 months Can drive after 3 months if treated, otherwise 12 months LOC with seizure markers Cannot drive for 6 months, or 12 months if high risk of recurrence Cannot drive for 5 years (any posture) Cardiovascular syncope Ok if avoidable trigger
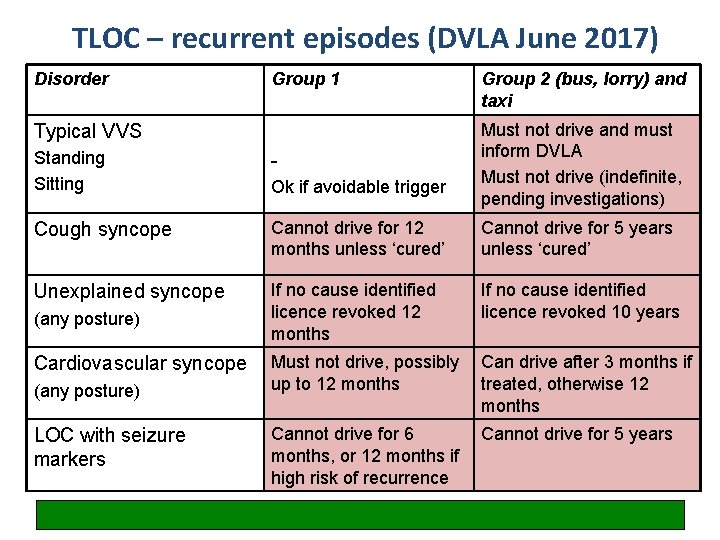
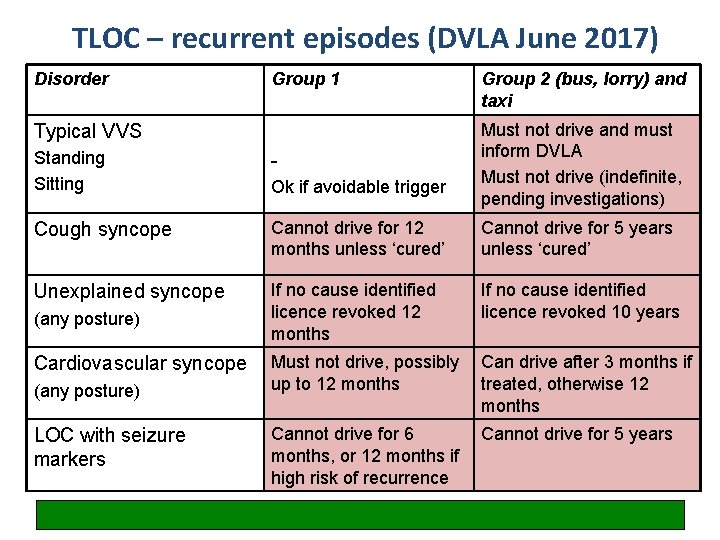
TLOC – recurrent episodes (DVLA June 2017) Disorder Group 1 Typical VVS Group 2 (bus, lorry) and taxi Must not drive and must inform DVLA Must not drive (indefinite, pending investigations) Standing Sitting - Cough syncope Cannot drive for 12 months unless ‘cured’ Cannot drive for 5 years unless ‘cured’ Unexplained syncope If no cause identified licence revoked 12 months If no cause identified licence revoked 10 years Must not drive, possibly up to 12 months Can drive after 3 months if treated, otherwise 12 months Cannot drive for 6 months, or 12 months if high risk of recurrence Cannot drive for 5 years (any posture) Cardiovascular syncope (any posture) LOC with seizure markers Ok if avoidable trigger

What three things have you learned this morning?